 Chronic Lyme Disease: Symptoms, Causes, and Coinfections
Chronic Lyme Disease: Symptoms, Causes, and Coinfections
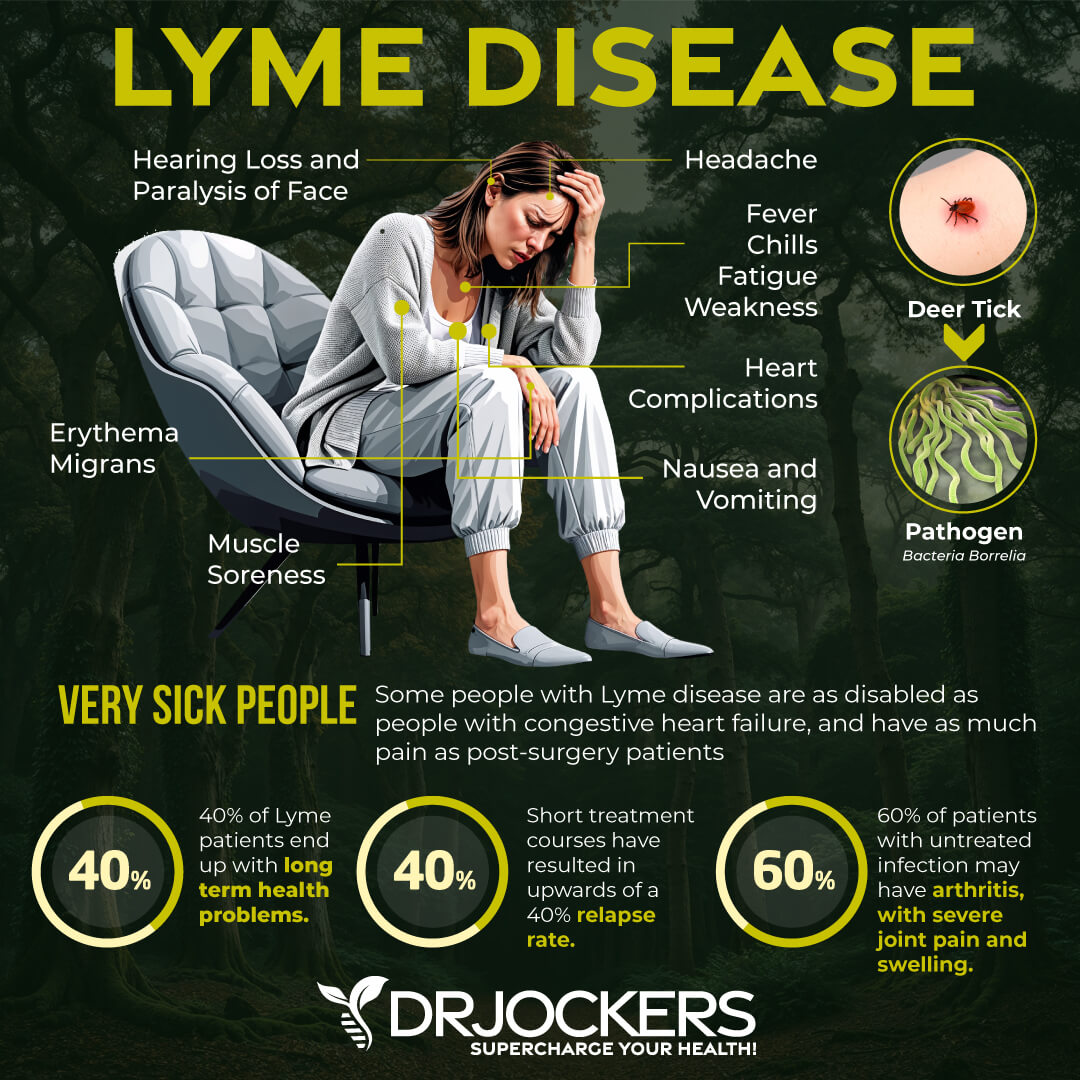
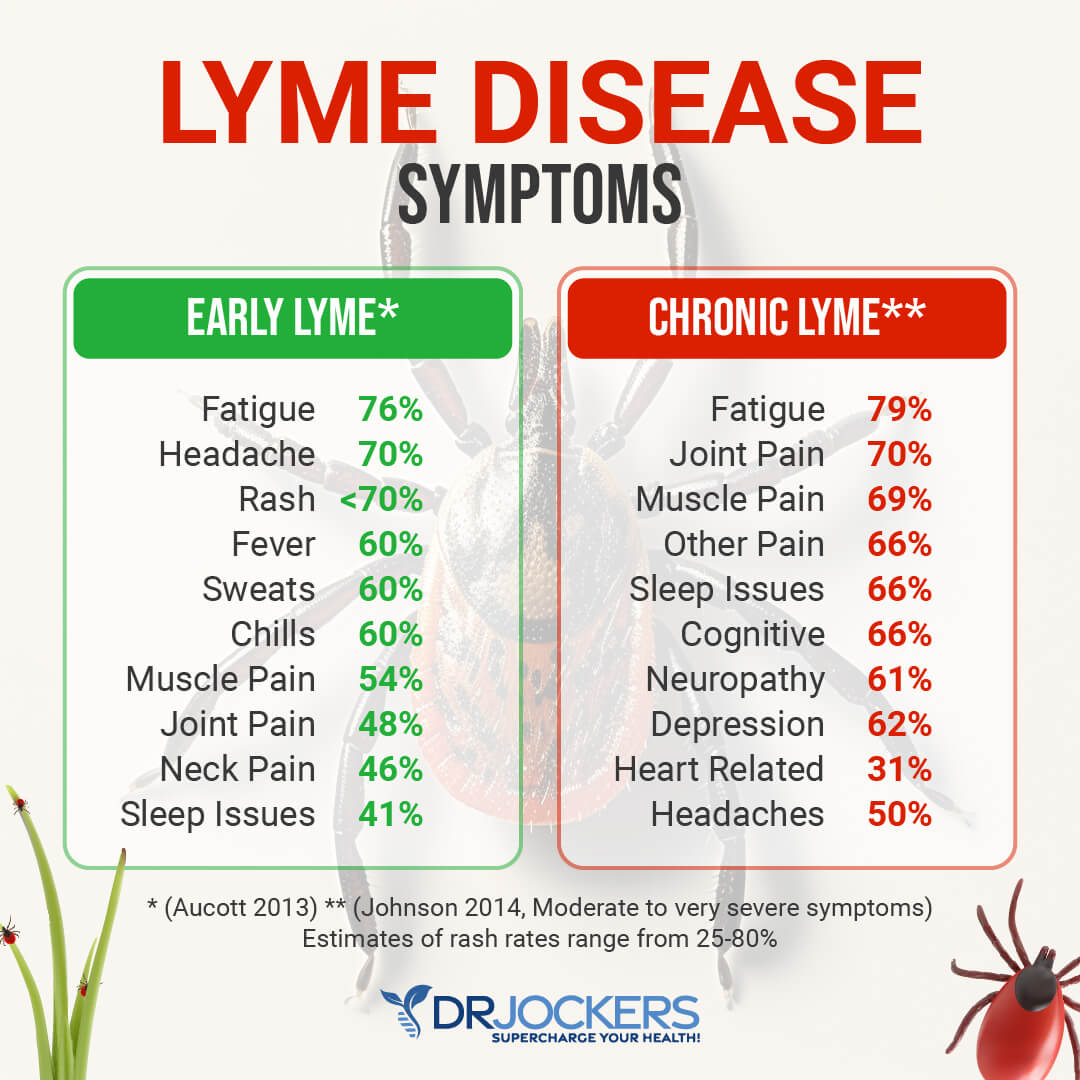
Are you experiencing fatigue, headaches, joint pain, muscle aches, sleep issues, memory and concentration troubles, neurological issues, body pains, or other chronic symptoms without a known explanation? You may have chronic Lyme disease.
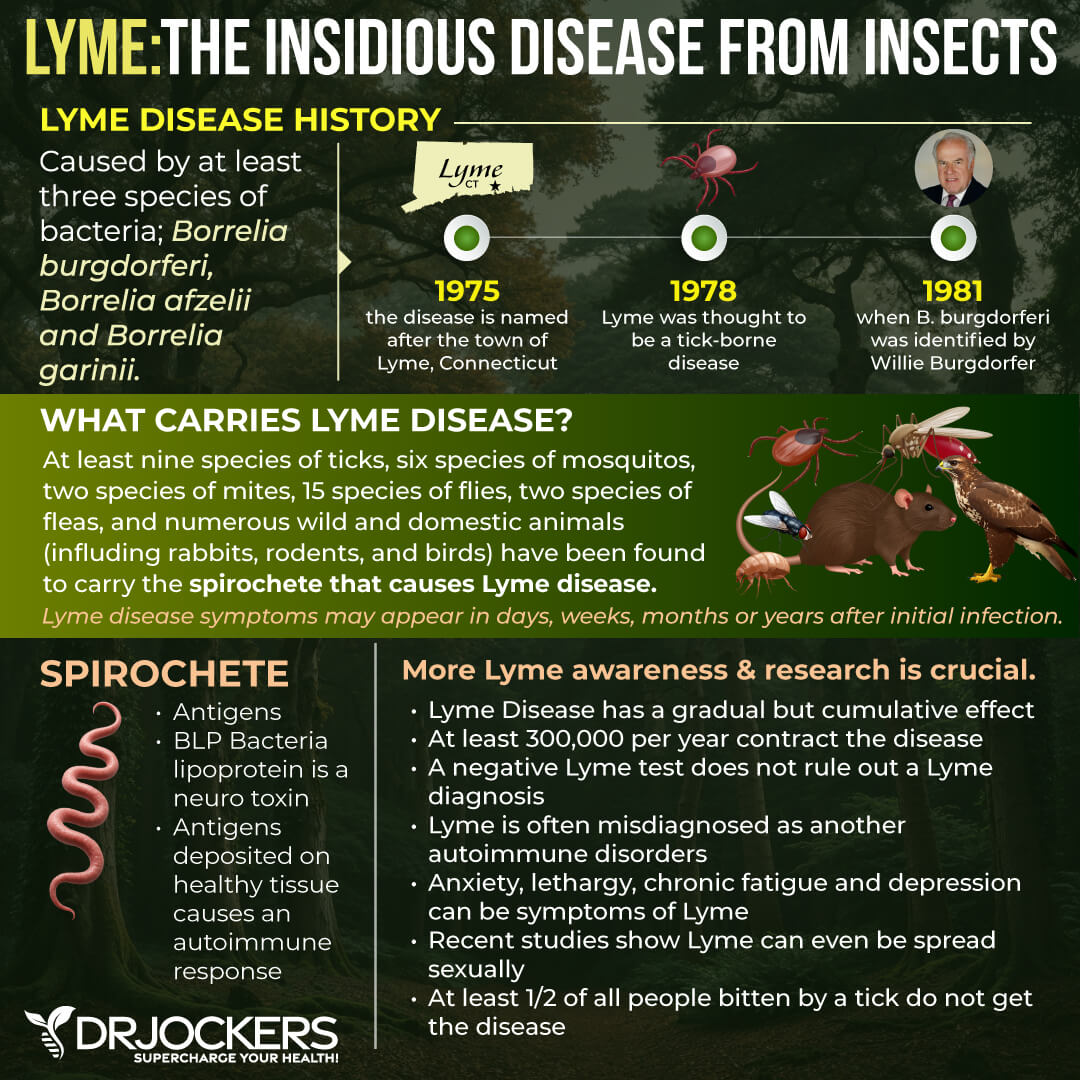
Chronic Lyme disease is increasingly prevalent and a very serious health issue. It is caused by Borrelia burgdorferi bacteria transmitted by infected ticks. When Lyme disease is not diagnosed and properly addressed during the acute phase during the first weeks, it can turn chronic leading to countless symptoms and health complications.
Unfortunately, testing is not reliable and the conventional medical community is not equipped to adequately address this rampant health issue. Fortunately, there are Lyme-literate healthcare professionals, like myself, who can help you to get the right diagnosis. You can overcome chronic Lyme disease following some natural supports strategies and using a 6-month protocol.
In this article, you will learn what Lyme disease is and the difference between acute and chronic Lyme disease. You will understand the symptoms of chronic Lyme disease. I will explain what co-infections you may encounter if you have chronic Lyme disease. I will discuss the problems with standard testing methods and offer more reliable testing alternatives. I will offer some natural support strategies to get started with.
What Is Lyme Disease
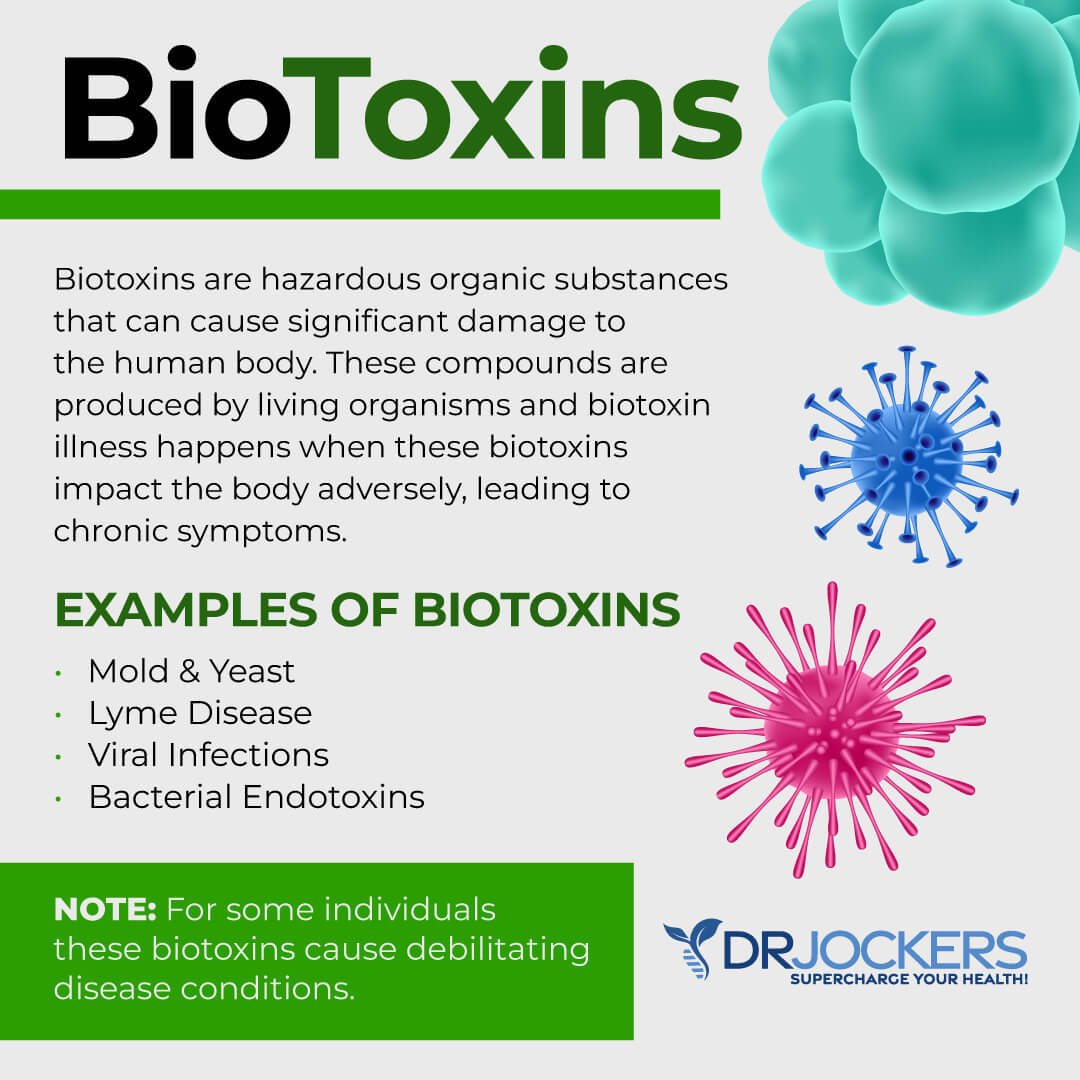
Lyme disease is a serious infectious disease. It is caused by the Borrelia burgdorferi bacteria found in and transmitted by infected black-legged or deer tick. It falls in the category of a biotoxic illness. Biotoxins are hazardous organic substances produced by living organisms that can cause detrimental problems within the body.
Since Lyme is transmitted by ticks, it is more common in wooded areas, however, there is still a risk elsewhere, for example in city parks or even your backyard. In the past, doctors believed that in order to get Lyme disease, the tick has to stay in your body for at least 24 to 48 hours, however, according to new research, it seems that even if a tick is attached to the human body for even 15 minutes, that may be enough to transmit the variety of microbes into the victim (1, 2, 3, 4, 5, 6, 7).
Acute vs Chronic Lyme Disease
When we talk about Lyme disease, we must differentiate between acute and chronic Lyme disease. Acute Lyme disease is a short-term or recent infection. Chronic Lyme disease is a long-term on-going one. When caught early, within the first few days to weeks of a tick bite and infection, acute Lyme disease can be treated with a course of antibiotics.
Holistic health professionals can also offer various supplements and nutritional strategies to help resolve acute Lyme disease. While there is still a risk of long-term health issues, usually, acute Lyme disease can be treated effectively.
One of the most commonly believed symptoms of acute Lyme disease is a flat, circular rash with a bull’s eye, however, not all people notice a bull’s eye rash. In fact, according to newer data, it is only the minority who notice a bull’s eye rash which may lead to people not seeking treatment, misdiagnosis, a lack of early treatment, and the risk of chronic Lyme disease.
Other symptoms of acute Lyme disease include fatigue, joint and muscle pain, headaches, sleep issues, fever, concentration issues, and swollen lymph nodes. This can be easily mistaken with the flu or often written up as stress, fatigue, or psychosomatic symptoms.
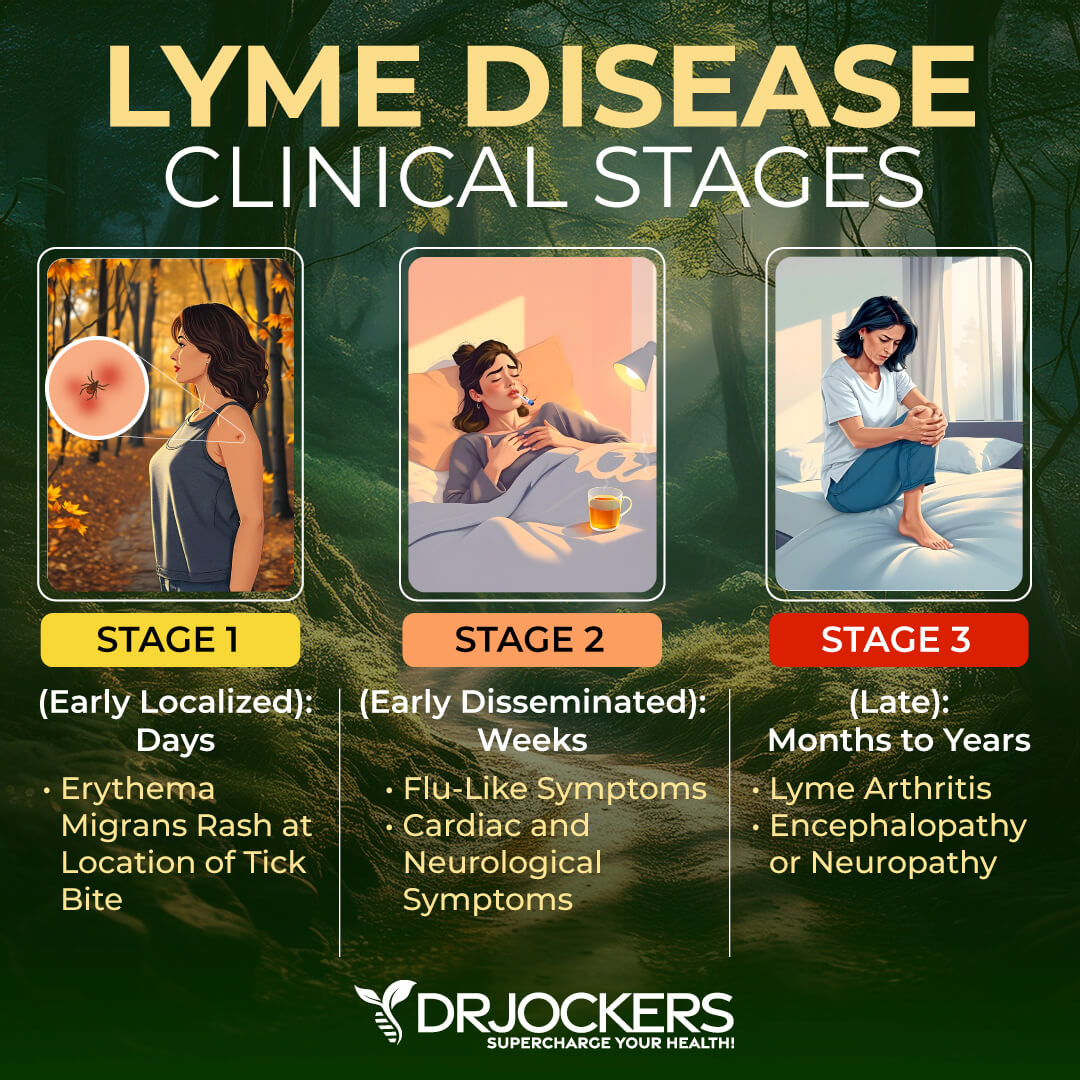
The Stages of Chronic Lyme Disease
If you spend time outdoors, it is very important that you always check for tick bites. If you believe that you have been bitten or you notice symptoms of acute Lyme disease, it is absolutely critical that you don’t wait and seek help from a Lyme specialist.
Later in this article, I will discuss the problems with testing. You will understand that it is not always enough to rely on testing, even when it comes to acute Lyme disease. It is important that your doctor takes this issue seriously and treat it right away to avoid chronic Lyme disease.
Chronic Lyme disease is increasingly prevalent and a very serious issue. Unfortunately, some people are resistant to treatment or Borrelia lingers in their body even after receiving adequate treatment for Lyme.
In most situations, however, the symptoms of acute Lyme disease are too mild and people don’t seek medical attention, in other cases, doctors misdiagnose them and don’t treat them right away. When not treated properly or quickly enough, the bacteria can integrate itself into your system leading to chronic Lyme disease. Chronic Lyme disease is very complex with an array of symptoms and health complications making it much more difficult to identify and treat (1, 2, 3, 4, 5, 6, 7).
Major Symptoms of Chronic Lyme Disease
Chronic Lyme disease may have a variety of symptoms that can be easily confused with fibromyalgia, autoimmune conditions, chronic fatigue syndrome, psychosomatic illness, or mental health issues. Unfortunately, without proper diagnosis and treatment, chronic Lyme disease gets worse over time and people with chronic Lyme may never recover without adequate treatment.
It is critical that if you experience the following symptoms, you work with a doctor that is well-versed in chronic Lyme disease so you can receive the right diagnosis, get started with proper treatment, relieve your symptoms, and recover from the condition. Major symptoms of chronic Lyme disease that you need to pay attention to may include but not limited to:
- Fatigue
- Pain
- Sleep troubles
- Memory and concentration problems
- Migrating and intermittent joints and muscle pains
- Migrating pains or swelling in elbows, knees, and shoulders
- Speech problems
- Neurological issues
- Migrating numbness, tingling, or burning pains
- Fibromyalgia-like pain
- Other chronic health issues
Types of Co-infections
Lyme disease is caused by the bacteria Borrelia. However, it is not the only infection that may occur in your body if you have Lyme disease. There are other co-infections that commonly occur alongside your original infection that were usually transmitted at the same time as the Lyme bacteria through the tick bite. In fact, about 30 percent of those with chronic Lyme disease have at least two co-infections (8, 9, 10, 11, 12).
You may be surprised to hear that there are over 200 different bacterial, viral, and parasitic infections that ticks may carry. According to research, the most common Lyme co-infections include:
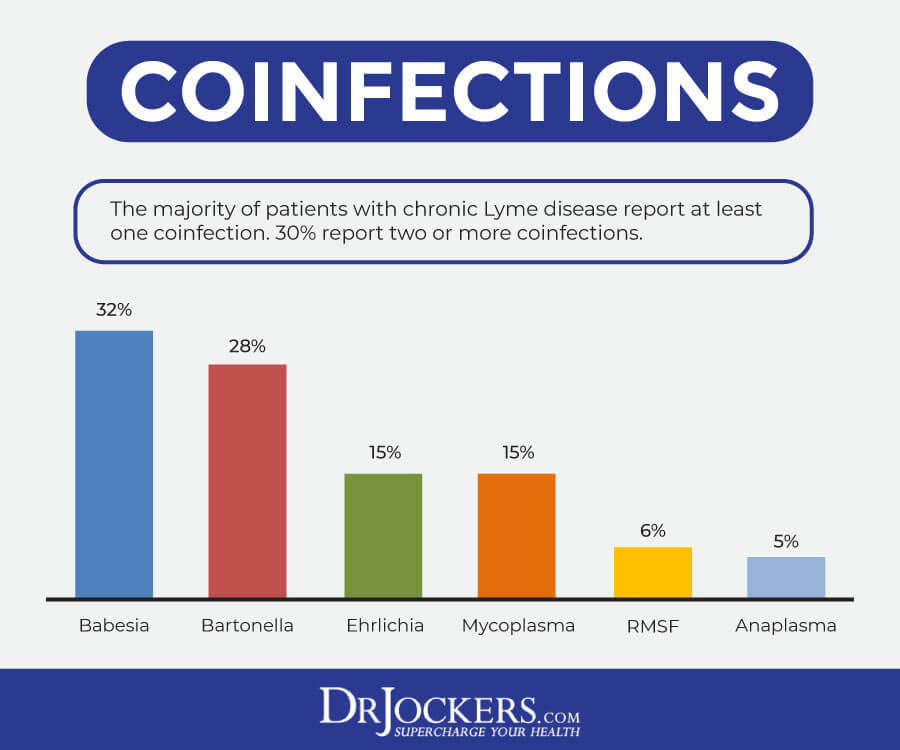
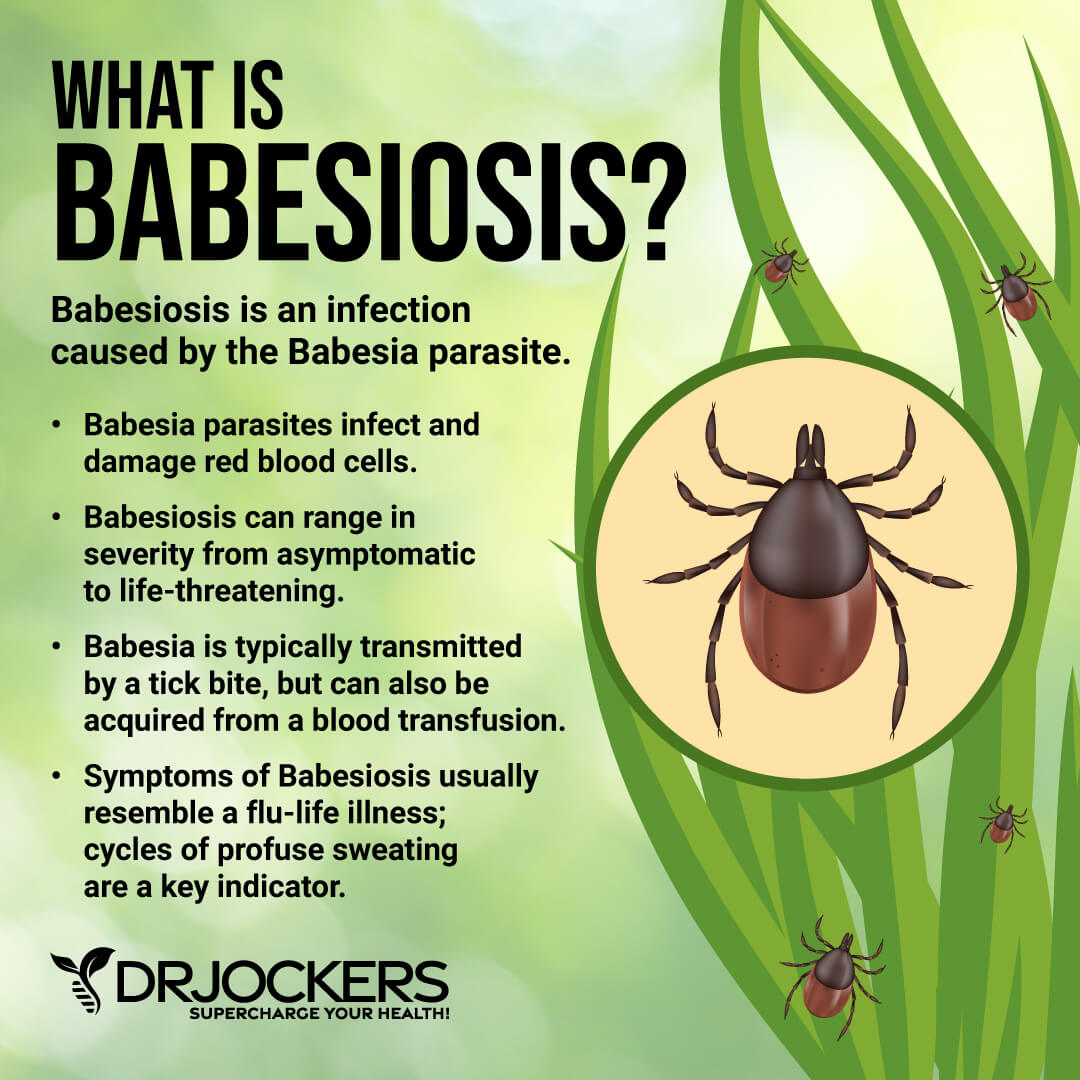
Babesia
Babesia is a parasite that is distantly related to malaria. It is affecting 32.3 percent of chronic Lyme disease patients. While there are over 100 different species of this, Babesia microti affects people most commonly. It is usually transmitted through ticks, however, you can get it through blood transfusion or organ transplant as well.
Babesia attacks your red blood cells and damages your cell membranes. It can rapidly change its gene expression making it difficult for your immune system to recognize and fight it. It can lead to liver or kidney failure and heart issues (13, 14, 15, 16).
Symptoms of Babesia include:
- Chills
- Cough
- Fatigue
- Headaches
- Sweats
- Joint and muscle pain
- Nausea
- Low appetite
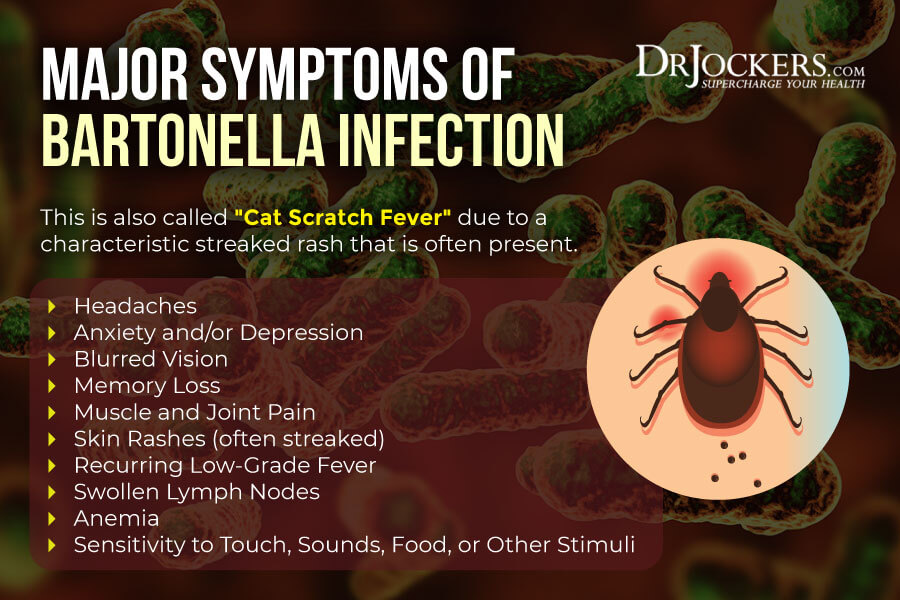
Bartonella
Bartonella is a bacteria affecting 28.3 percent of chronic Lyme disease patients. It has about 20 strains. The most common ones include Bartonella henselae carried by infected cats, Bartonella bacilliformis transmitted by certain sand flies, and Bartonella quintana found in lice. Bartonalla infections may also come from ticks, fleas, bed bugs, spiders, mite, and red ants.
Bartonella also affects your blood vessels, red blood cells, and lymph nodes. It compromises your immune system leading to a variety of symptoms ranging from mild to severe (17, 18, 19, 20).
Symptoms of Bartonella include:
- Headaches
- Anxiety or Depression
- Blurred Vision
- Memory Loss
- Muscle and Joint Pain
- Skin Rashes
- Recurring low-grade fever
- Swollen lymph nodes
- Anemia
- Sensitivity to Touch, Sounds, Food, or Other Stimuli
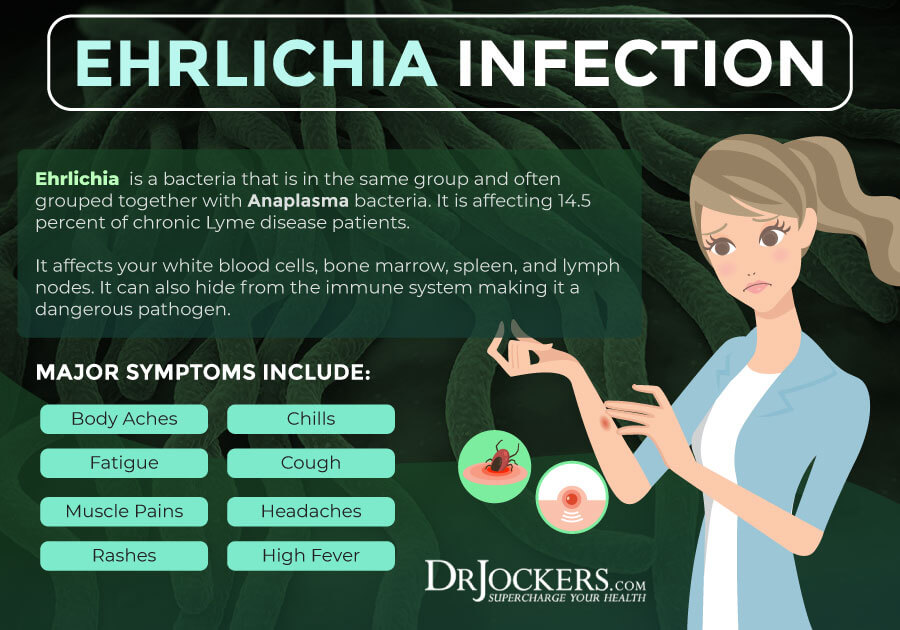
Ehrlichia
Ehrlichia is a bacteria that is in the same group and often grouped together with Anaplasma bacteria. It is affecting 14.5 percent of chronic Lyme disease patients. The three main forms of Ehrlichia that tend to affect people with chronic Lyme disease include Ehrlichia chaffeensis, Ehrlichia ewingii, and Anaplasma phagocytophilum or Ehrlichia phagocytophilum.
It may get transmitted by a lone star tick, blood transfusion, and organ transplants. It affects your white blood cells, bone marrow, spleen, and lymph nodes. It can also hide from the immune system making it a dangerous pathogen (21, 22, 23, 24).
Symptoms of Ehrlichia Include:
- Body Aches
- Chills
- Fatigue
- Cough
- Muscle Pains
- Headaches
- Rashes
- High Fever
Rickettsia
Rickettsia is a bacteria with 26 different species. The most common infection it may cause is Rocky Mountain Spotted Fever. It is affecting 5.6 percent of chronic Lyme disease patients. It is transmitted through ticks. Rickettsia affects the lining of your blood vessels and creates inflammation and issues in your extremities. In some cases, it may lead to amputation (25, 26, 27).
Symptoms of Rickettsia Include:
- Fatigue
- Confusion
- Headaches
- Muscles aches
- Light sensitivity
- Nausea
- Poor appetite
- Stomach pain
- Rashes
- Fever

Opportunistic Pathogens
The co-infections that we talked about tend to enter your body along with the Lyme-causing Borrelia bacteria through a tick bite. However, there are some other bacteria and viruses that cause opportunistic infections. Chronic Lyme disease may increase your risk of other infections or may amplify the symptoms of infections you may have (28).
Opportunities pathogens that may cause infections alongside chronic Lyme disease include:
-
- Epstein-Barr virus (EBV)
- Human parvovirus
- Chlamydia pneumoniae
- Mycoplasma pneumoniae
- Cytomegalovirus
- Coxsackievirus
The problem with these co-infections is that they are very opportunistic in nature. They may weaken your immune system, create further symptoms, and make it more difficult for your body to fight the disease.
The Problem With Standard Testing
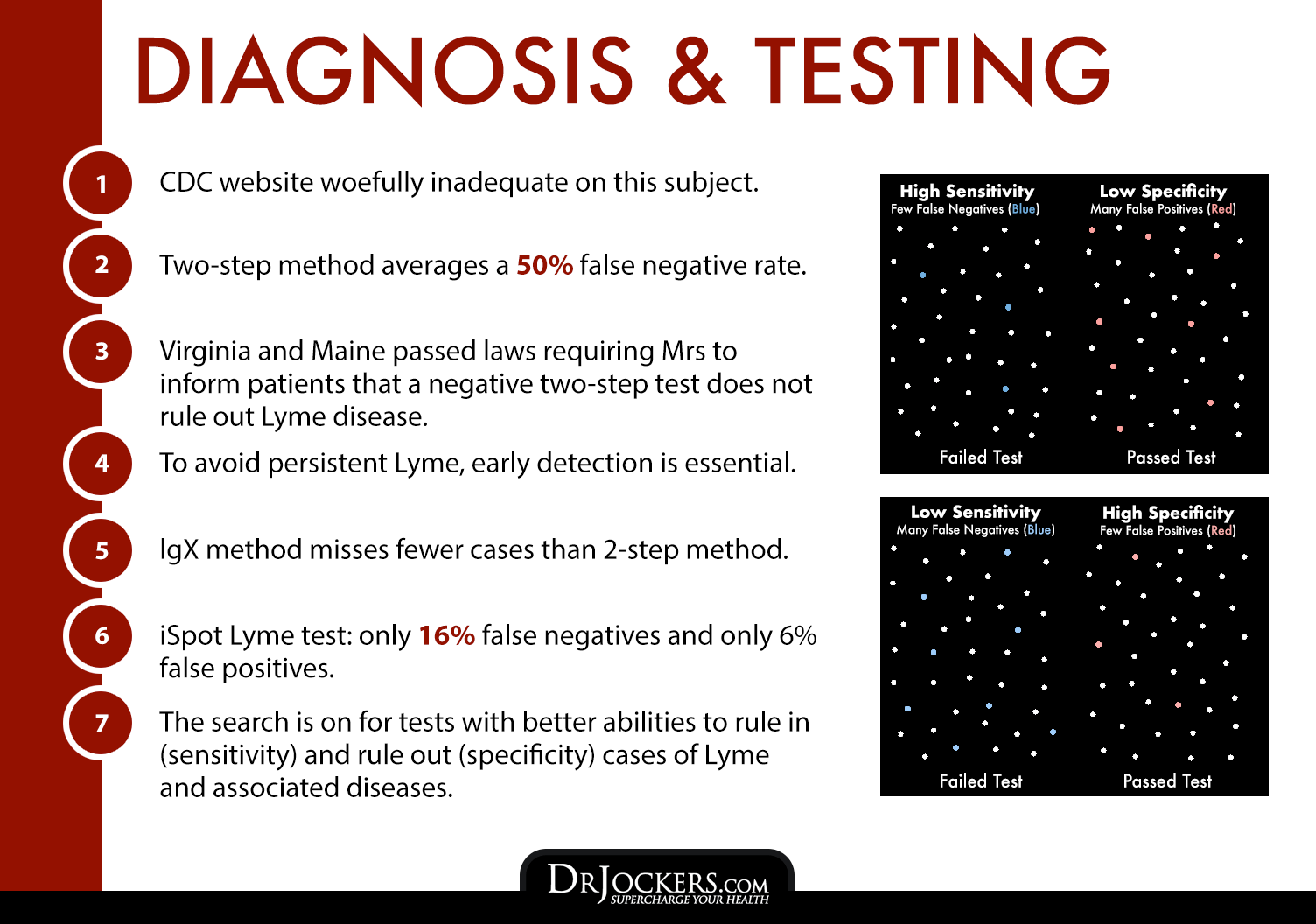
The two major problems that we are facing when it comes to chronic Lyme disease is the lack of understanding from conventional doctors and problems with standard testing. Unfortunately, conventional medicine still mainly focuses on acute Lyme disease. Many doctors reject the idea of chronic Lyme or they are simply not trained on how to deal with it. On the other hand, standard testing is problematic. It doesn’t always catch acute Lyme and is not helpful when it comes to chronic Lyme disease. Without accurate testing, it is difficult to get the right diagnosis and treatment.
Most non-Lyme literate doctors and labs use a two-step test which is recommended by the Centers for Disease Control and Prevention (CDC) and approved by the US Food and Drug Administration (FDA). The first test is an ELISA test followed by the Western blot test. Both tests are only designed for Borrelia burgdorferi and are unable to detect any co-infections or related pathogens.
The ELISA test is often inaccurate and false negatives may occur. If you get tested too soon after a tick bite and your body doesn’t have enough antibodies yet, your ELISA test will be negative. If your ELISA test is negative, doctors and labs don’t move onto the Western blot and often don’t retest even if you have persistent and consistent symptoms with Lyme disease.
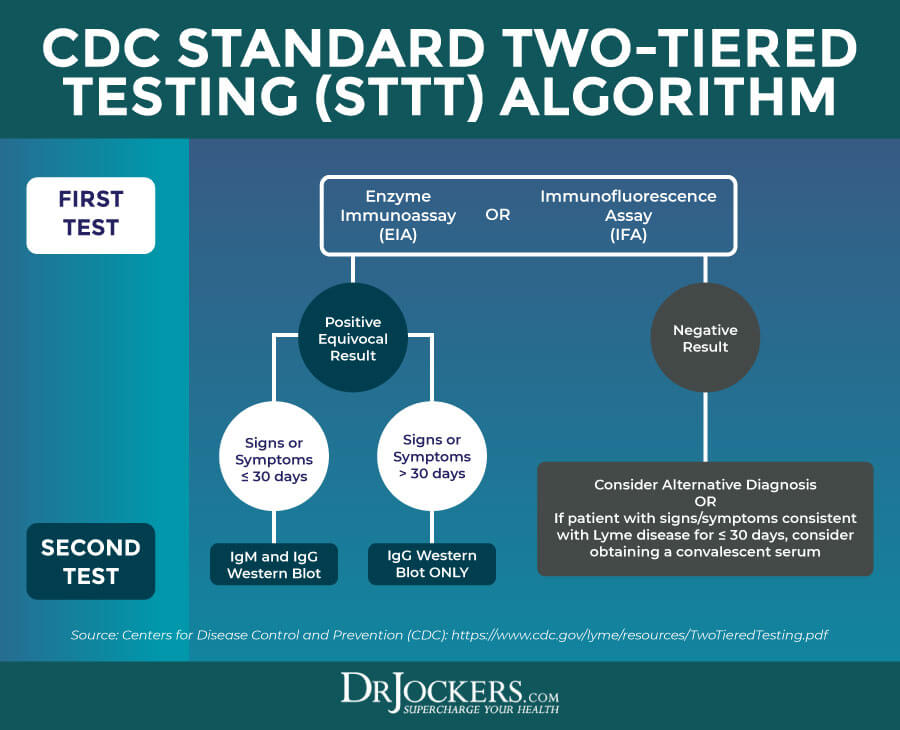
Chronic Lyme Disease Testing
Some people may simply not convert a classic immune response to the testing that conventional healthcare professionals are using. This two-step process may miss up to 60 percent of acute Lyme disease cases which increases the risk of a high number of preventable chronic Lyme disease. This two-step process is also extremely inaccurate and even less reliable when it comes to chronic Lyme disease.
This two-step testing method measures your body’s immune response when a bacteria is present, instead of actually looking for and detecting the pathogen causing the infections. There are a variety of issues with this method that may lead to inaccurate results:
- Timing: During the early stages of Lyme disease, only a few days or a week after the infection, your body may not have created enough antibodies to show up on the ELISA test. In these cases, retesting may be helpful as the antibodies may show up later, but most doctors don’t retest even if your symptoms persist and correspond with Lyme disease.
- Immune suppression: The saliva ticks that cause Lyme disease have an immune-suppressing component that may delay or completely prevent your body’s immune response. If there is no immune response, your body won’t be able to respond to the two-step test that is looking for antibodies to prove an immune response.
- Antibiotics: If you are taking antibiotics or just stop taking antibiotics around the time you were bitten by a tick, it may also be problematic. Antibiotic use may prevent your body from making enough antibodies and they won’t show up on the ELISA test.
- Weakened immune system: If you have a weak or compromised immune system due to an illness, existing co-infection, medication, poor diet, or unhealthy lifestyle, false negatives may also occur.
- A modified form of Borrelia: In some cases, the bacteria may turn into a cyst, which prevents the production of antibodies leading to false negatives.
- Seronegative patients: While it is not common, there are some patients whose bodies simply do not produce antibodies at all making the two-step testing ineffective.
It is important to mention that while false negatives are a problem, false positives may also occur. You may have a Lyme infection but your immune system may not show a positive response with positive young IgM antibodies, and also may not lead to an immune response with old IgG antibodies. It may happen due to early antibiotic use.
This is certainly a problem since the wrong diagnosis leads to wrong treatment methods. It is important that whether or not you have Lyme disease, you receive the appropriate diagnosis to receive an effective treatment plan, overcome your health issues, and regain your health (29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44).
Best Testing Strategies
If you believe that you may have Lyme disease, it is important that you work with a Lyme-literate doctor who understands the best testing strategies and treatment methods. Instead of relying on your body’s antibody response to bacteria, it is important to also use direct testing that is looking at the disease-causing bacteria and co-infections.
Igenex
Igenex offers great testing for Borrelia burgdorferi and co-infections, Babesia, Bartonella, Ehrlichia, Anaplasma, and Rickettsia. It offers comprehensive, effective, and precise diagnostic testing for Lyme-disease and tick-borne infections with a superior sensitivity rate than standard testing methods.
These testing kits include both indirect and direct testing solutions. While indirect tests examine the response of the patient’s immune system to the presence of B. burgdoferi, direct tests look for B. burgdoferi antigens and nucleic acids.
DNA Connexions
DNA ConneXions Lyme is a simple at-home test that detects the presence of DNA from Borrelia burgdorferi and 11 other potential tick-borne co-infections. It is a simple and affordable at-home test that can help you get the right diagnosis and treatment.
Importantly, as DNA Connexions points out on their website, a negative result from their Lyme panel doesn’t necessarily indicate the lack of an infection, but instead indicates the absence of any detectable tick borne or Lyme-based co-infections. In some cases, the timing of antibiotic courses and the patients’ ability to fight the disease will determine the detectability of the DNA spirochetes.

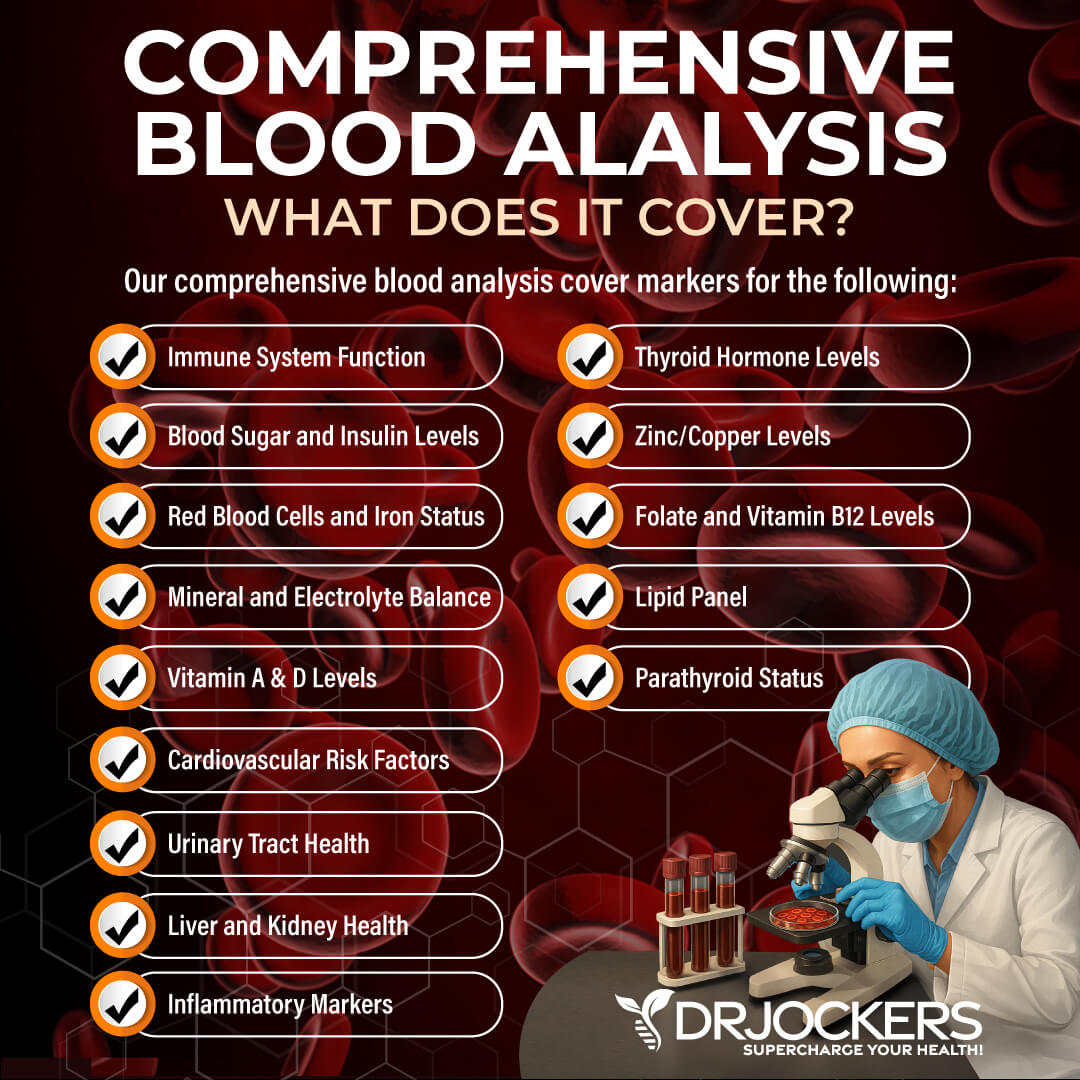
Comprehensive Blood Analysis
Since chronic Lyme disease is very complex, it affects your entire body and leads to a large variety of symptoms and health issues. It may make you more vulnerable to further infections and health problems. To cover everything, a Lyme-literate doctor may include a variety of other tests besides the ones that detect the Lyme-causing bacteria and co-inflections to detect or rule out other issues, including:
- Complete blood count (CBC): white blood cells count (WBC), differential (diff), hemoglobin (HB)
- Blood chemistry: electrolytes, liver function, kidney function
- Glucose metabolism: fasting blood glucose, fasting insulin hemoglobin A1c (HbA1c)
- Minerals: magnesium and calcium
- Lipid panel
- Thyroid function: complete thyroid
- Vitamins: vitamin D and B12
- Iron: ferritin
- Omega-3/omega-6 ratio
- Autoimmune testing rheumatoid factor, ANA titer
- C-reactive protein (CRP)
- Urinalysis: pH, WBCs, nitrites, protein, bilirubin
- Mold and mycotoxins
- Comprehensive stool analysis: yeast, parasites, viruses, and bacteria
- Adrenal hormone testing
- Reproductive hormone testing: estrogen, progesterone, testosterone
- Testing for toxins
- Microbes testing
- Folate and methylation: MTHFR gene mutation
- Testing for neurological, cardiac, and GI symptoms
We offer many of these tests in our comprehensive blood analysis. When you order testing through DrJockers.com, one of our health coaches will help review the results with you and offer helpful advice to guide you on your health journey.
Natural Support Strategies
Chronic Lyme disease is certainly a serious health issue with an array of symptoms and potential complications, however, it is possible to overcome chronic Lyme disease using natural support strategies. While it is a 6-month long program, it’s worth putting your mind and heart into it to regain your health and happiness. Here is what I recommend:
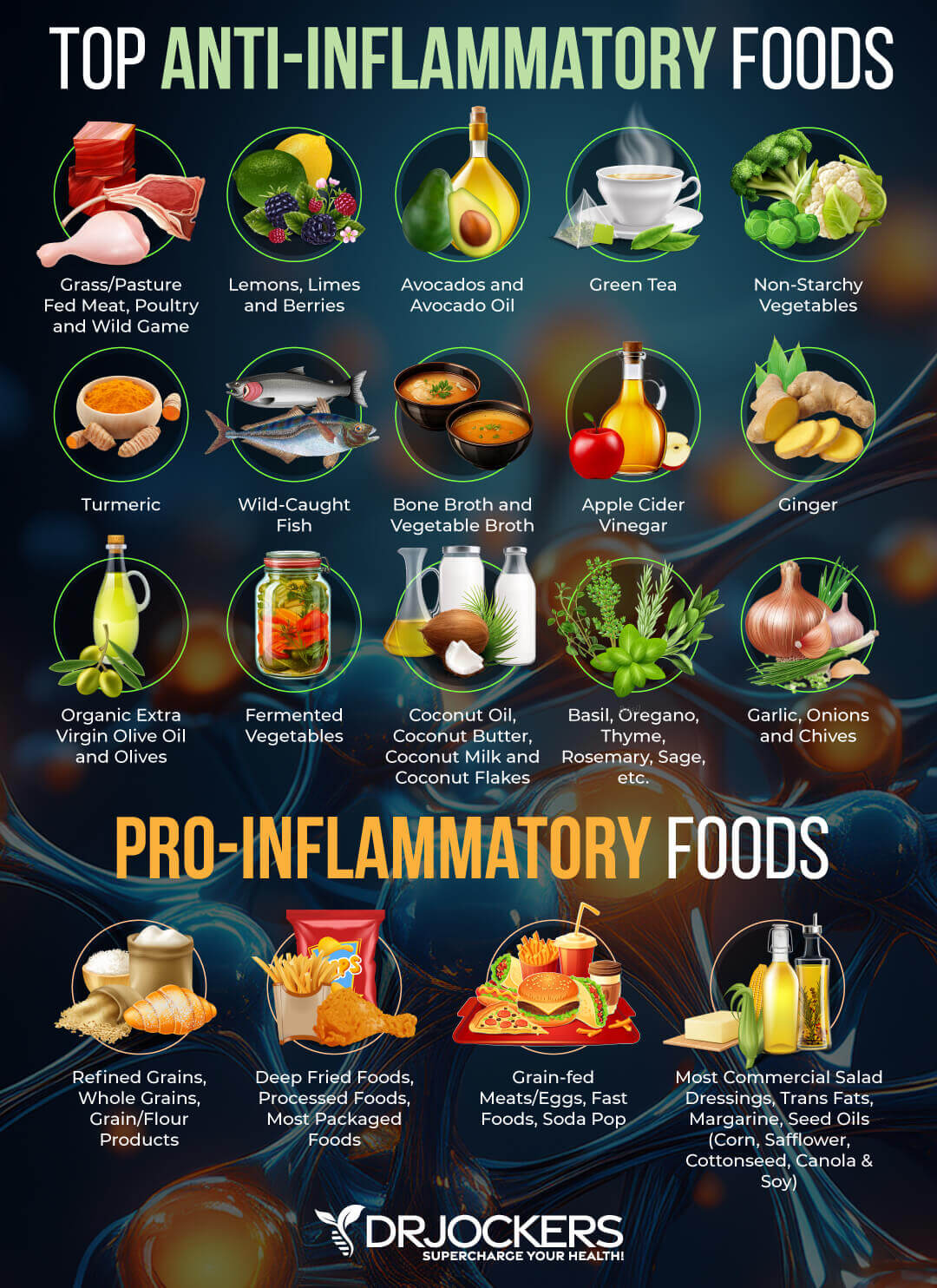
Anti-Inflammatory Nutrition
Anti-inflammatory nutrition is the base of your recovery from chronic Lyme disease. It helps to lower inflammation, reduce symptoms, supports detoxification, and aid cellular repair. Eliminate all inflammatory foods and drinks, including refined sugar, processed foods, refined oils, artificial ingredients, junk food, deep-fried food, soda, and low-fat/diet products. Make sure to eat organic food to avoid exposure to pesticides, chemicals, and hormones.
Eat plenty of anti-inflammatory greens, vegetables, low glycemic index fruit, herbs, spices, and superfoods. Focus on healthy fats, including avocados, coconut oil, organic butter, and ghee, and clean protein, including pasture-raised beef, free-range poultry and eggs, wild-caught fish, and wild boar.
Make sure to hydrate well. Drink plenty of purified clean water and add some herbal tea, green juices, green smoothies, and bone broth for further hydration. To learn more about anti-inflammatory nutrition, read this article.
Reduce Stress & Prioritize Good Sleep
Reducing stress and prioritizing good sleep is an essential way to reduce inflammation, aid your immune system, support cellular repair, and aid recovery. Avoid stressful situations and learn coping mechanisms to deal with stress better. Practice gratitude, meditation, breathwork, and grounding daily.
Engage in other relaxing activities, including journaling, board games, crossword puzzles, time with family and friends, and time in nature. Develop a regular sleeping schedule and aim for at least 8 to 9 hours of good sleep. Avoid food, stress, and electronics close to bedtime. Engage in relaxing activities, drink herbal tea, take a healing bath, light a candle, or pray to unwind before bedtime. Make sure your bed and bedding are supportive and your bedroom is a calming sanctuary.

Get Regular Light Movement
Moving your body is very important for your health. It strengthens your immune system, supports your lymphatic pathways, aids detoxification, supports your muscles and joints, and enhances your mental health.
However, it is important that you only do light movement and not high-intensity exercise while you are healing to preserve your body’s energy for rest and repair. I recommend stretching, yoga, Tai Chi, Pilates, or light walks daily. Listen to your body and be gentle with yourself.

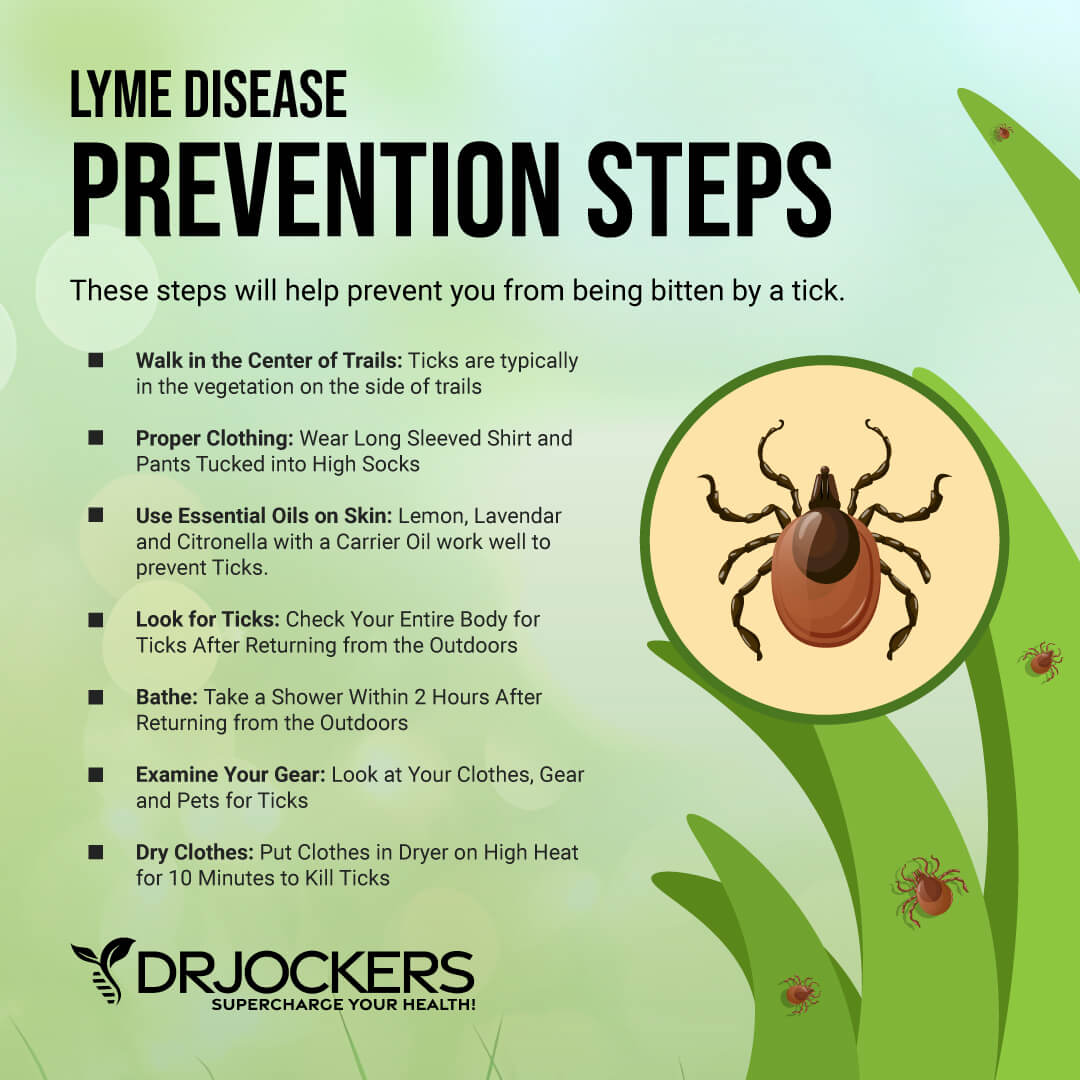
Check Yourself and Your Pets Regularly
One of the best ways to avoid Lyme disease is to make sure that you find and remove ticks as quickly as possible. The less time a tick has access to your skin, the less chance of infection you face. This is what makes checking for ticks so vital – particularly when you’ve visited the areas in which they thrive.
Diligence is essential to protecting yourself from tick bites and Lyme disease, as well as the co-infections that come with them. If you can prevent a tick bite from ever happening, then you won’t have to worry about the symptoms, testing or healing process involved in Lyme recovery. However, if you do suffer from Lyme disease, then hopefully this article will help with some guidance you need to battle through the infection successfully.

Final Thoughts
Chronic Lyme disease is an increasingly prevalent and serious health issue caused by Borrelia burgdorferi bacteria transmitted by infected ticks. Standard testing methods are often unreliable. False-negative test results and a lack of understanding Lyme disease often leads to unaddressed acute Lyme disease, which results in chronic Lyme disease.
Instead of standard testing methods, I recommend the two testing methods I shared in this article and working with a Lyme-literate doctor or natural health practitioner. Here is an article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs with our well-trained functional health team. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!





I have an issue with swelling ankles and calves. An ultrasound shows I have leaky veins. The doctor says I’m a candidate for a new procedure that puts an adhesive in the vein to seal it off and encourage new veins to develop. Can this really be safe? I’m 78, on no meds, have a good health record–except for my swelling ankles and calves. Should I rely on propping my feet, compression stockings, and walking daily?
Sorry to hear this! Here is a helpful article: https://drjockers.com/varicose-veins/
I’ve had Lyme disease symptoms for 15yrs, but in Australia, they don’t believe that it exists here, I grew up in a hot, dry climate, in the summer time, we had ticks climbing the walls, our town was infested with ticks. Even the 48 degree heat wouldn’t kill them. I wish there was a Dr specialising in Lyme disease would help me, I’m a 49 year old woman, I’ve been so sick with this retched illness, how can Drs believe it doesn’t exist in Australia
Sorry to hear this! I would recommend finding a functional nutrition practitioner to work with: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
How do I find a doctor to help with Lyme, and how do diet for Lyme??
Hey Teri – I would recommend finding a great functional health coach: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
My husband was recently diagnosed with a fatty liver and ulcerative colitis. He got lymes disease before this recent diagnosis and did his antibiotics for it. He continues to have fatigue, sore joints and a headache he’s been trying to deal with for years. When he has what we think are colitis flare ups the symptoms match Ehrlichia‘s. During these flare ups we’ve told doctors the symptoms match what he went through when he had lymes. They do a blood test and it always comes back negative. He is sick of all test’s coming back normal and feeling crappy everyday.
Sorry to hear about this!! Praying for you and your family!