 Pancreatic Cancer: Symptoms, Causes, and Support Strategies
Pancreatic Cancer: Symptoms, Causes, and Support Strategies
Pancreatic cancer is uncontrolled cancerous cell growth that affects your pancreas. It is responsible for about 3 percent of all cancers in the United States. Unfortunately, pancreatic cancer is often asymptomatic until later stages, and diagnosis can be difficult. However, through healthy lifestyle choices and natural support strategies, you can protect your body and improve your health.
In this article, I will explain what pancreatic cancer is. You will learn about the signs and symptoms, stages, and risk factors of pancreatic cancer. I will discuss diagnosis and conventional treatment options. I will explain the root causes of pancreatic cancer. I will also offer my top natural support strategies to protect your health.
What Is Pancreatic Cancer
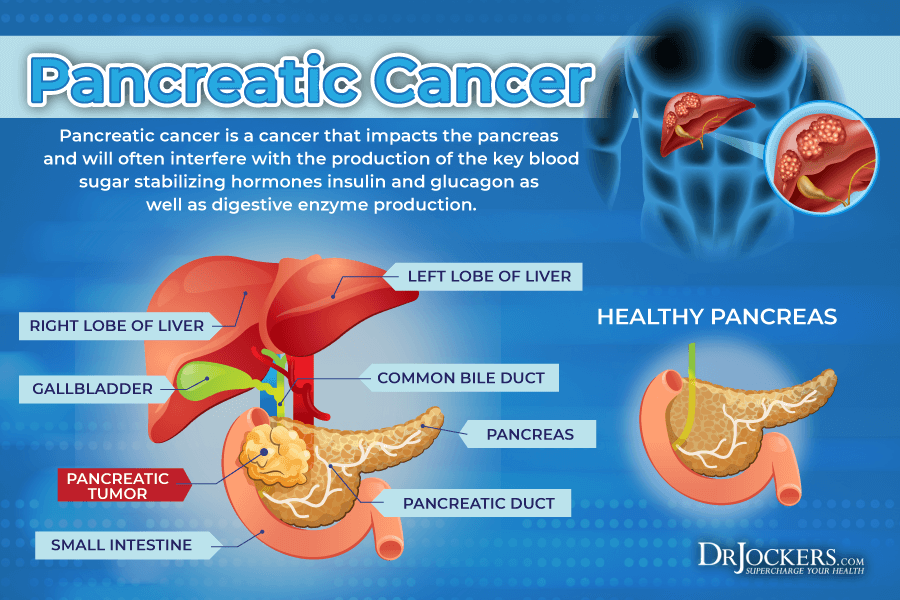
Your pancreas is a six to ten inches long flat, pear-shaped organ located behind your stomach in the upper left abdomen. It is surrounded by your small intestine, spleen, and liver. Your pancreas plays two essential roles in your body: exocrine and endocrine function.
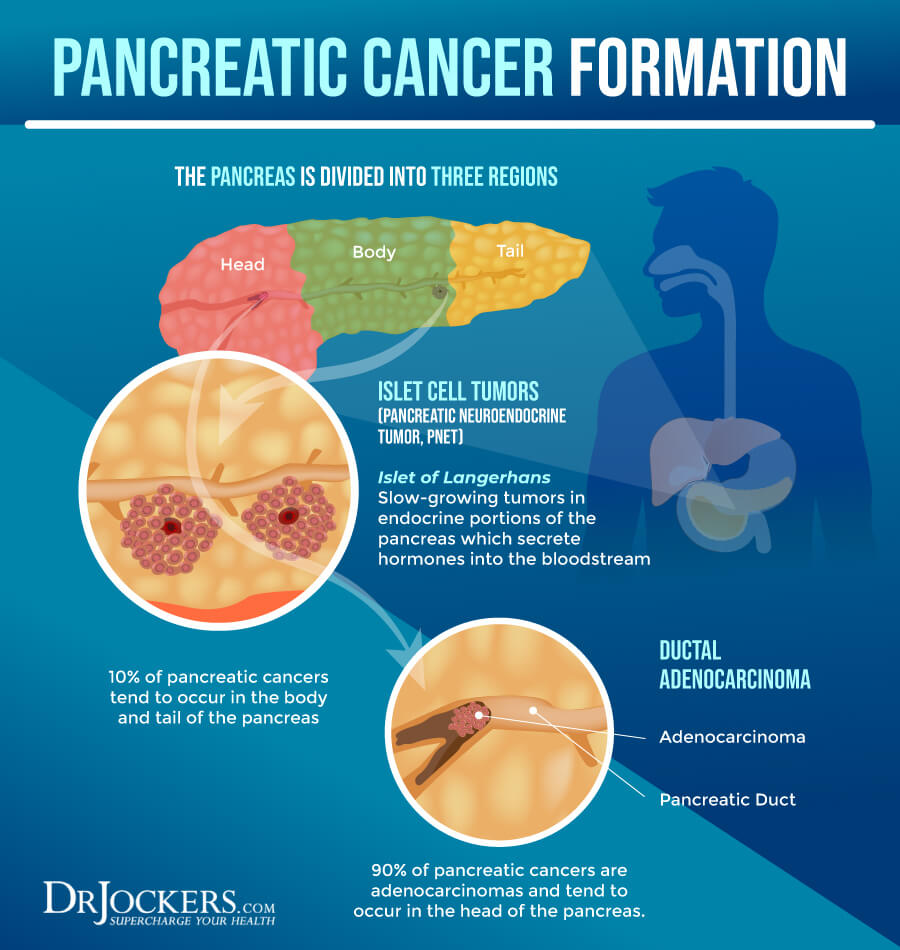
About 95 percent of your pancreas is made up of exocrine tissue responsible for making pancreatic enzymes for digestion. Trypsin and chymotrypsin help to break down protein, lipase helps to break down fats, and amylase helps to break down carbs. The remaining parts are endocrine cells called islets of Langerhans that are similar to grapes. They are responsible for creating hormones, such as insulin and glucagon, to regulate your blood sugar and pancreatic secretions. Insulin helps to lower your blood sugar, while glucagon helps to raise it as necessary.
A healthy pancreas helps to balance chemicals that support digestion. Its healthy function, especially regulating your blood sugar, is critical for your kidneys, liver, digestive system, brain, and overall health. However, a lot can go wrong with your pancreas. Pancreatic cancer is one of the significant health issues that may develop in your pancreas (1).
When there is uncontrolled cell growth in your pancreas, pancreatic cancer develops, interfering with pancreatic function. According to the American Cancer Society, pancreatic cancer affects about 55,440 people each year, and it is responsible for about 3 percent of all cancers in the United States (2). Pancreatic cancer may affect your endocrine or exocrine glands. Because symptoms often don’t appear until later stages, pancreatic cancer can be challenging to manage or treat.
Signs & Symptoms of Pancreatic Cancer
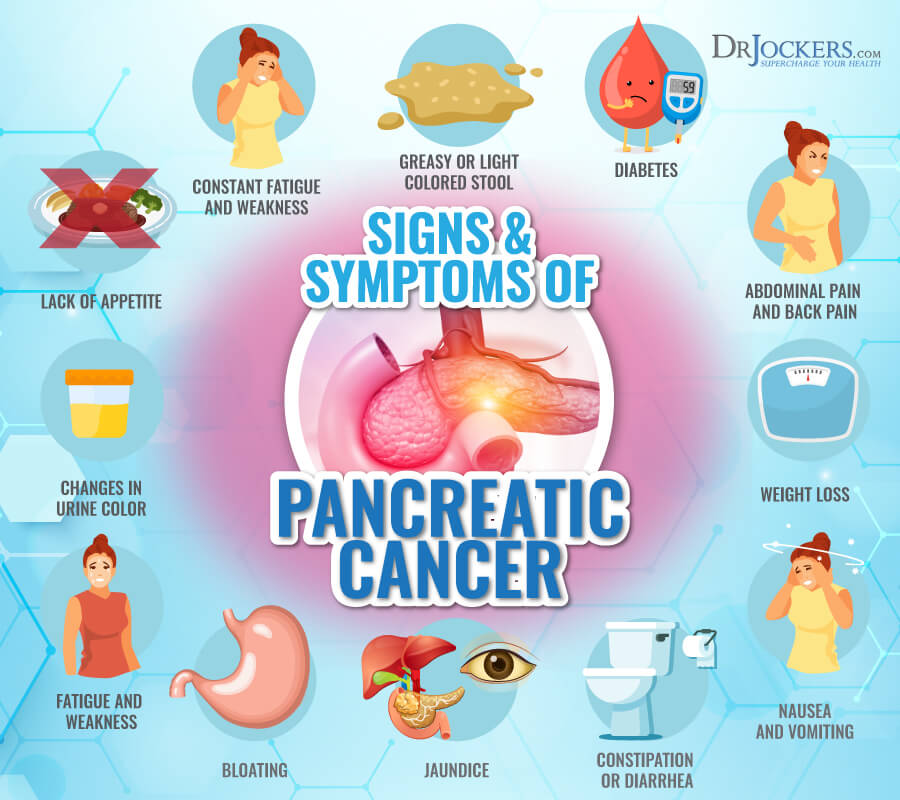
Early-stage pancreatic cancer often doesn’t have any signs and symptoms that can overlap with the signs of other digestive health diseases. This can make early diagnosis very difficult (1).
Signs and symptoms of pancreatic cancer may include (1):
- Jaundice (yellowing of the whites of your eyes or skin)
- Light-colored stools
- Dark-colored urine
- Weight loss without a known reason
- Loss of appetite
- Pain in the middle or upper abdomen and back
- Fatigue
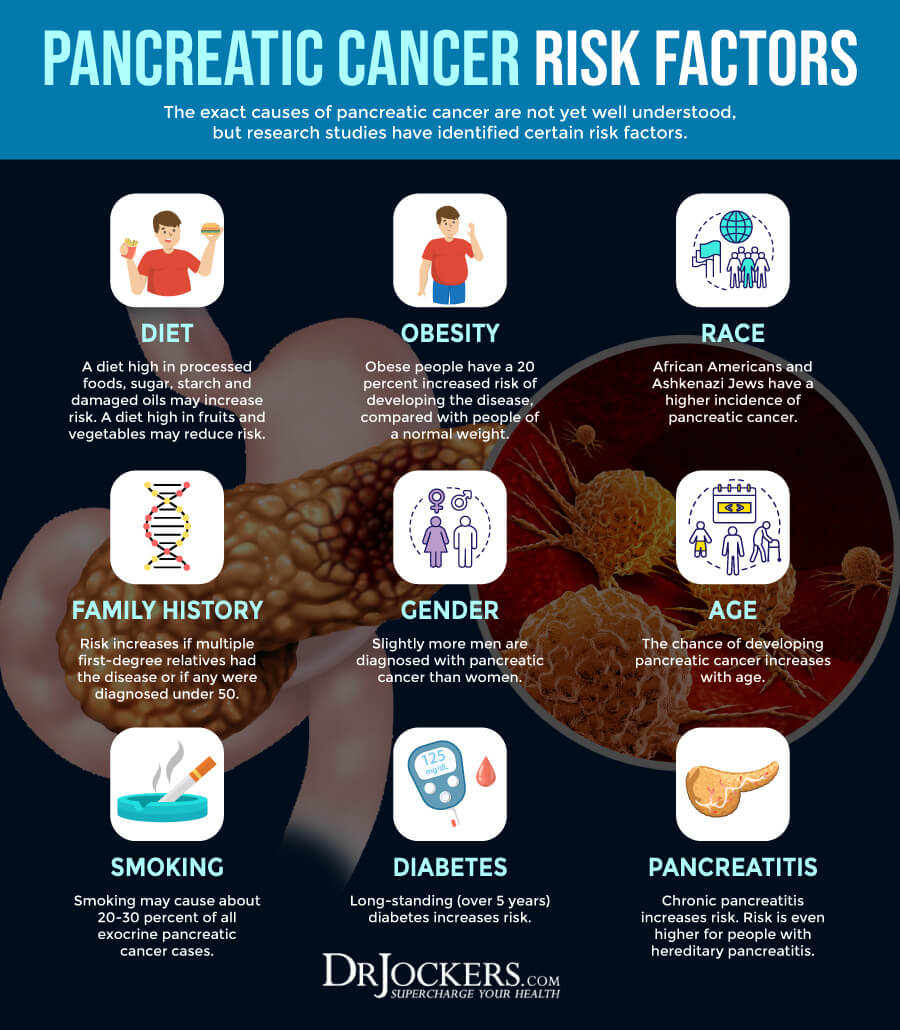
Risk Factors for Pancreatic Cancer
There as several factors that may increase your risk for pancreatic cancer, including (1):
- Being overweight or obese
- Smoking and alcohol abuse
- Family history of pancreatitis or pancreatic cancer
- Personal history of chronic pancreatitis or diabetes
- Diet high in processed foods, sugar, starch, and damaged oils.
- Men have a slightly higher risk than women.
- African Americans and Ashkenazi Jews have a higher incidence rate
- Certain hereditary conditions, including multiple endocrine neoplasia type 1 (MEN1) syndrome, hereditary nonpolyposis colon cancer (HNPCC, Lynch syndrome), Peutz-Jehers syndrome, hereditary breast or ovarian cancer syndrome, Hipper-Lindau syndrome, ataxia-telangiectasia, or familial atypical multiple mole melanoma (FAMMM) syndrome
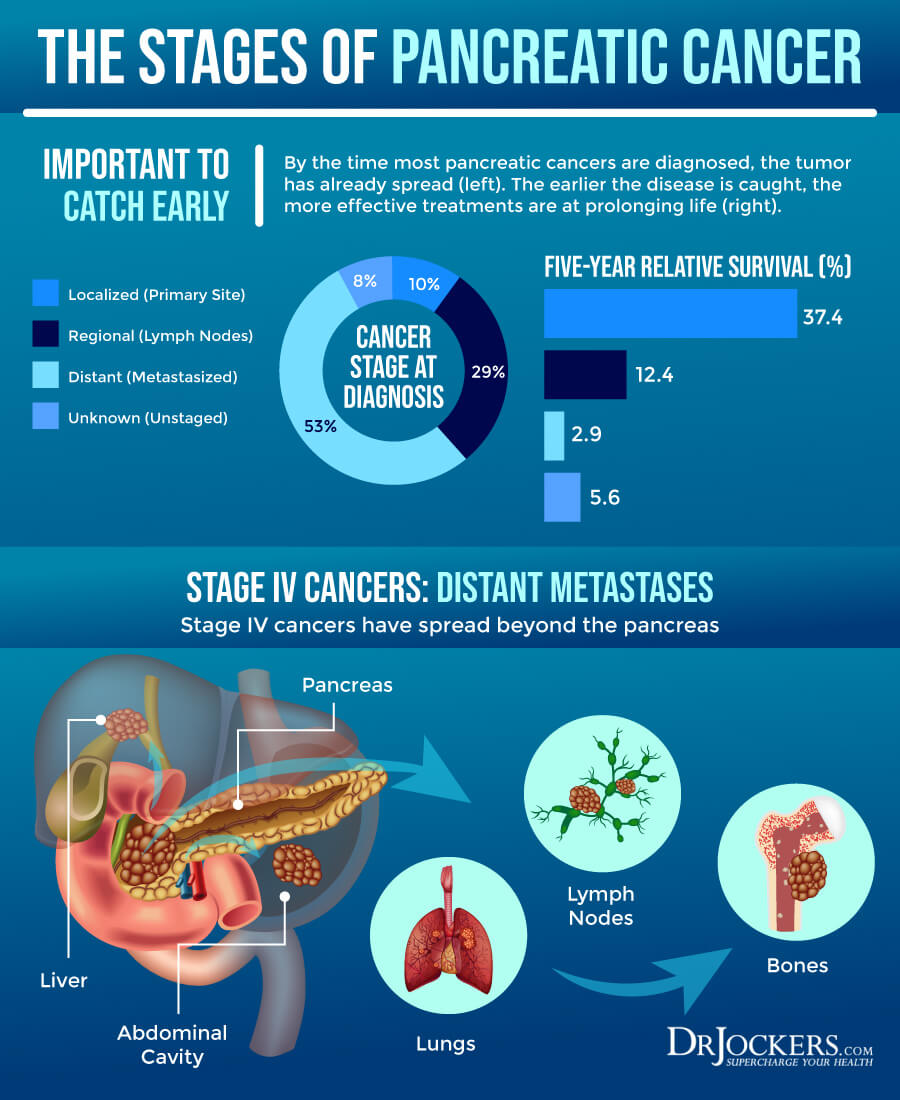
Stages of Pancreatic Cancer
There are five stages of pancreatic cancer, including (1):
- Stage 0: This stage is also called carcinoma in situ. In this stage, there are some abnormal cells in the lining of the pancreas that may turn cancerous and may spread to other tissues.
- Stage 1: In this stage, cancer is only located in the pancreas. There are two substages: stage 1A and 1B. In stage 1A, the tumor is 2 centimeters or less. In stage 1B, it’s between 2 and 4 centimeters.
- Stage 2: Stage 2 has two sub-stages: 2A and 2B. In stage 2A, the tumor is larger than 4 centimeters, and in stage 2B, the tumor may be bigger or smaller than 4 centimeters but has spread to 1 to 3 lymph nodes nearby.
- Stage 3: In stage 3, cancer has spread to 4 or more lymph nodes or major blood vessels nearby.
- Stage 4: In stage 4, cancer has spread to other parts of the body, such as the lungs, liver, peritoneal cavity, or other areas.
Beyond staging, when diagnosing pancreatic cancer, doctors consider the following groups to determine your treatment options and whether or not surgery is a possible option (1):
- Resectable pancreatic cancer: This cancer has not grown into blood vessels, so your surgeon can remove it.
- Borderline resectable pancreatic cancer: This means that the cancer has spread to other organs, tissues, or blood vessels. Your surgeon may still be able to remove it, but there is a higher chance that they can only remove some of the cancer cells, but not all.
- Locally advanced pancreatic cancer: Since the cancer has spread to nearby blood vessels and/or lymph nodes, it’s impossible to remove it completely through surgery.
- Metastatic pancreatic cancer: This cancer has already spread to other organs, and it’s not possible to surgically remove it.
- Recurrent pancreatic cancer: This is a type of pancreatic cancer that has returned after it has already been treated. It may return in your pancreas or other organs.
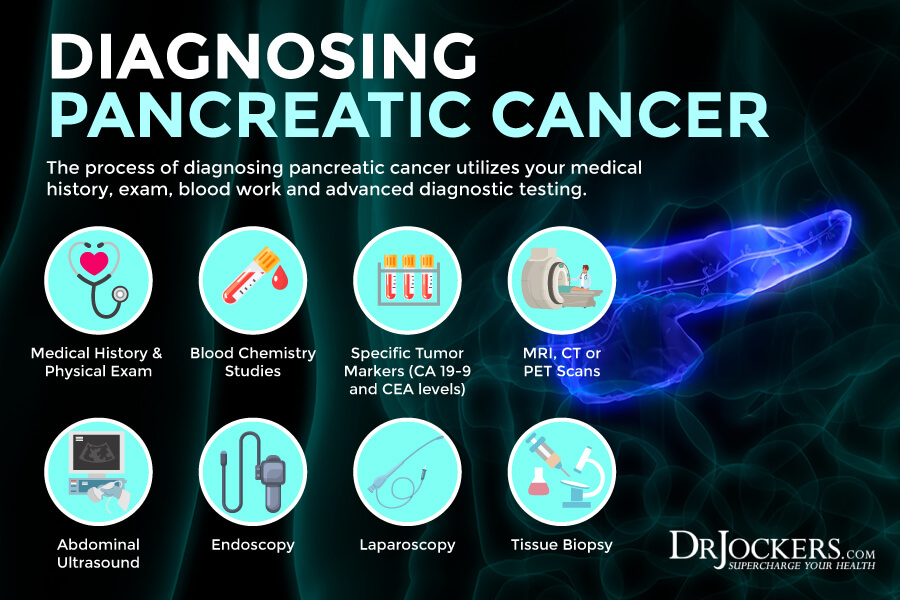
Diagnosis & Conventional Treatments
After going over your health history, family history, and symptoms, and a physical exam, our doctor and medical team may use a number of tests and procedures to diagnose and stage pancreatic cancer, including (1):
- Blood chemistry studies: Doctors use this to check for bilirubin and other substances released into your blood by certain organs. Abnormal (high or low) levels may indicate disease.
- Tumor marker tests: These tests include blood, urine, and tissue samples that look at CA 19-9 and carcinoembryonic antigen (CEA) levels that may be associated with certain types of cancer.
- Magnetic resonance imaging (MRI) scan, CT scans, or positron emission tomography (PET) scan: These are various scans that look for tumors and other abnormalities in your body.
- Abdominal ultrasound: By taking pictures of the inside of your abdomen with the help of high-energy sound waves (ultrasound), this procedure looks for tumors and abnormalities.
- Endoscopic ultrasound (EUS): During this test, your doctor will insert an endoscope through your mouth or rectum to look at your internal tissues and check for abnormalities.
- Endoscopic retrograde cholangiopancreatography (ERCP): This test uses an x-ray to look at your bile ducts, as pancreatic cancer can cause slow bile flow and bile duct issues.
- Percutaneous transhepatic cholangiography PTC): This procedure is an X-ray that looks at your liver and bile ducts after a dye is injected into them.
- Laparoscopy: This procedure uses small incisions on your abdomen to look at signs of disease inside through a thin, lighted tube (laparoscope).
- Biopsy: A biopsy removes small cells or pieces of tissue to look for abnormalities.
The conventional treatment for pancreatic cancer may depend on the stage of your cancer and your overall health. Conventional treatment options may include (1):
- Whipple procedure: surgery to remove the head of the pancreas
- Total pancreatectomy: surgery to remove the pancreas
- Biliary bypass: surgery if the cancer is blocking the bile duct, causing bile build-up
- Endoscopic stent placement: inserting a stent if the cancer is blocking the bile duct
- Gastric bypass: surgery if the cancer is blocking the flow of food from the stomach
- Radiation therapy: using radiation or beams of intense energy to kill cancer cells
- Chemotherapy: using chemicals to kill cancer cells
- Chemoradiation: combining radiation and chemotherapy
- Targeted therapy: using specific drugs to target tumor cells
Root Causes of Pancreatic Cancer
As a functional medicine doctor, I always look for the root cause of any health issue. There are certain dietary, nutritional, environmental, and health factors that may play a role as the root cause and increase your risk of pancreatic cancer.
It is important to understand the factors that you can control today to reduce your risk of pancreatic cancer. Here are the root causes of pancreatic cancer:
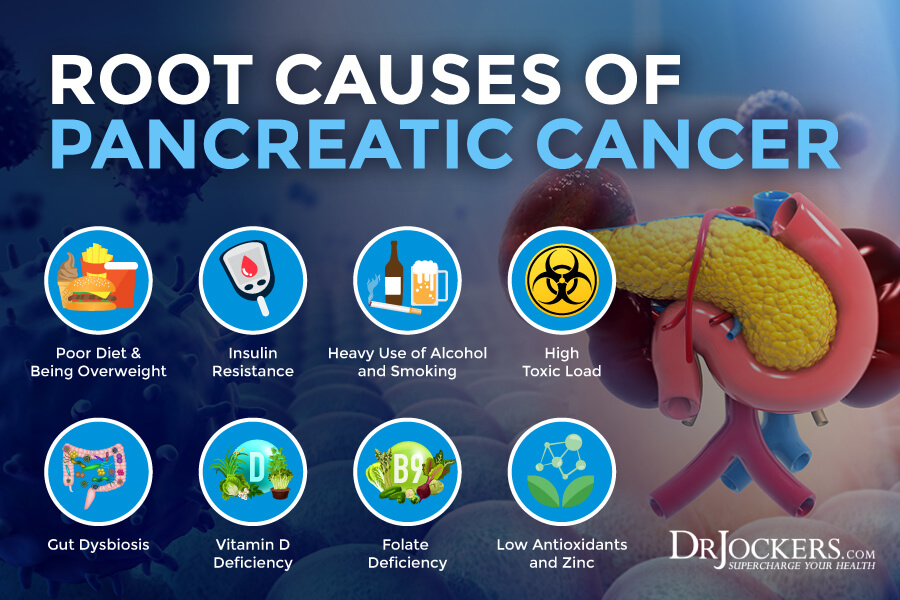
Poor Diet & Being Overweight
Eating a poor diet and being overweight can increase your risk of inflammation, disease, and cancer. Inflammatory foods, such as refined sugar, refined oil, gluten, conventional dairy, canned meat, additives, artificial ingredients, food allergens, highly processed food, and junk food, can lead to chronic inflammation, digestive dysfunction, poor gut health, and pancreatic cancer.
According to a 2018 study published in Pancreas, obesity is linked to an increased risk of pancreatic cancer, and weight loss can lower these risks (3). If you are overweight, it is important to know that excess fat increases inflammation and puts more stress on your pancreas.
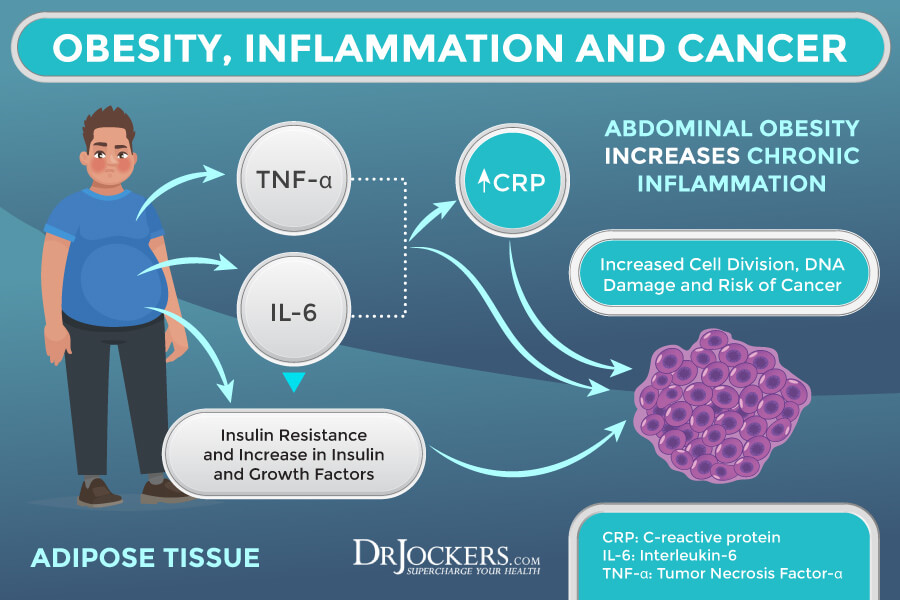
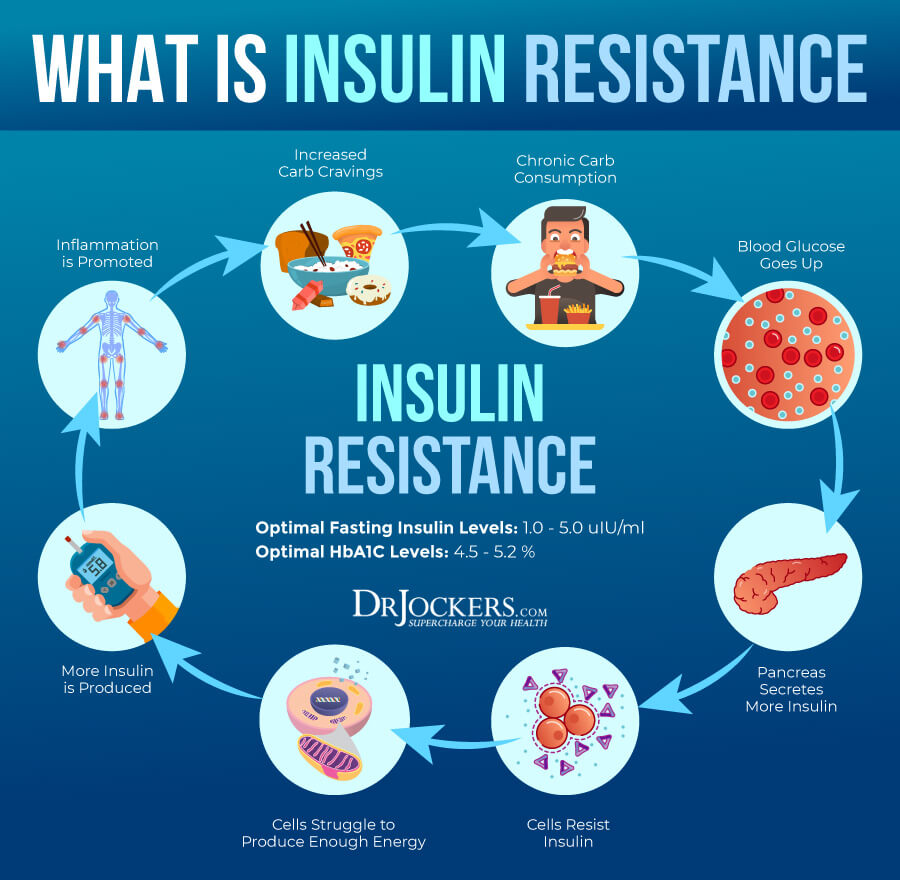
Insulin Resistance
Insulin resistance means that your body is unable to respond to insulin well and can’t take care of all the sugar in your blood. It increases your risk of prediabetes and diabetes. It may also contribute to the development of pancreatic cancer. A 2012 study published in Molecular Carcinogenic has found that type 2 diabetes is a risk factor for pancreatic cancer, right behind smoking and drinking alcohol (4).
A 2013 study published in the Journal of the National Cancer Institute has found that insulin resistance and hypoglycemia can lead to impaired pancreatic function and pancreatic cancer (5). While diabetes is a risk factor for pancreatic cancer, it turns out that insulin resistance without diabetes can increase your risk, too. A 2020 study published in the American Journal of Gastroenterology has found that insulin resistance can increase mortality from pancreatic cancer, whether they have diabetes or not (6).
Heavy Use of Alcohol, Smoking, Pesticides/Herbicides, and Hydrocarbons
Heavy use of alcohol, smoking, and heavy exposure to pesticides, herbicides, and hydrocarbons can increase your risk of developing pancreatic cancer. A 2020 study published in Pancreas has found that smoking increases the risk and outcome of pancreatic ductal adenocarcinoma (PDAC), a form of pancreatic cancer (7).
After reviewing 484 cases over a four-year period, a 2001 comparative study published in the American Journal of Indian Medicine found that occupational pesticide exposure can increase the risk of pancreatic cancer (8). A 2009 cohort study of 89,000 participants published in the International Journal of Cancer has also found that agricultural pesticides can contribute to the development of pancreatic cancer (9).
A 2012 review published in Molecular Carcinogenesis has found that occupational factors, including exposure to chlorinated hydrocarbon compounds, pesticides, polycyclic aromatic hydrocarbons (PAHs), metals, nitrosamines, radiation, and various airborne particles, can increase pancreatic cancer risk (10). A 14-year clinic-based case-control study published in Cancer Causes & Control in 2015 has also found that environmental chemicals and heavy metal exposure can increase the risk for pancreatic cancer (11).
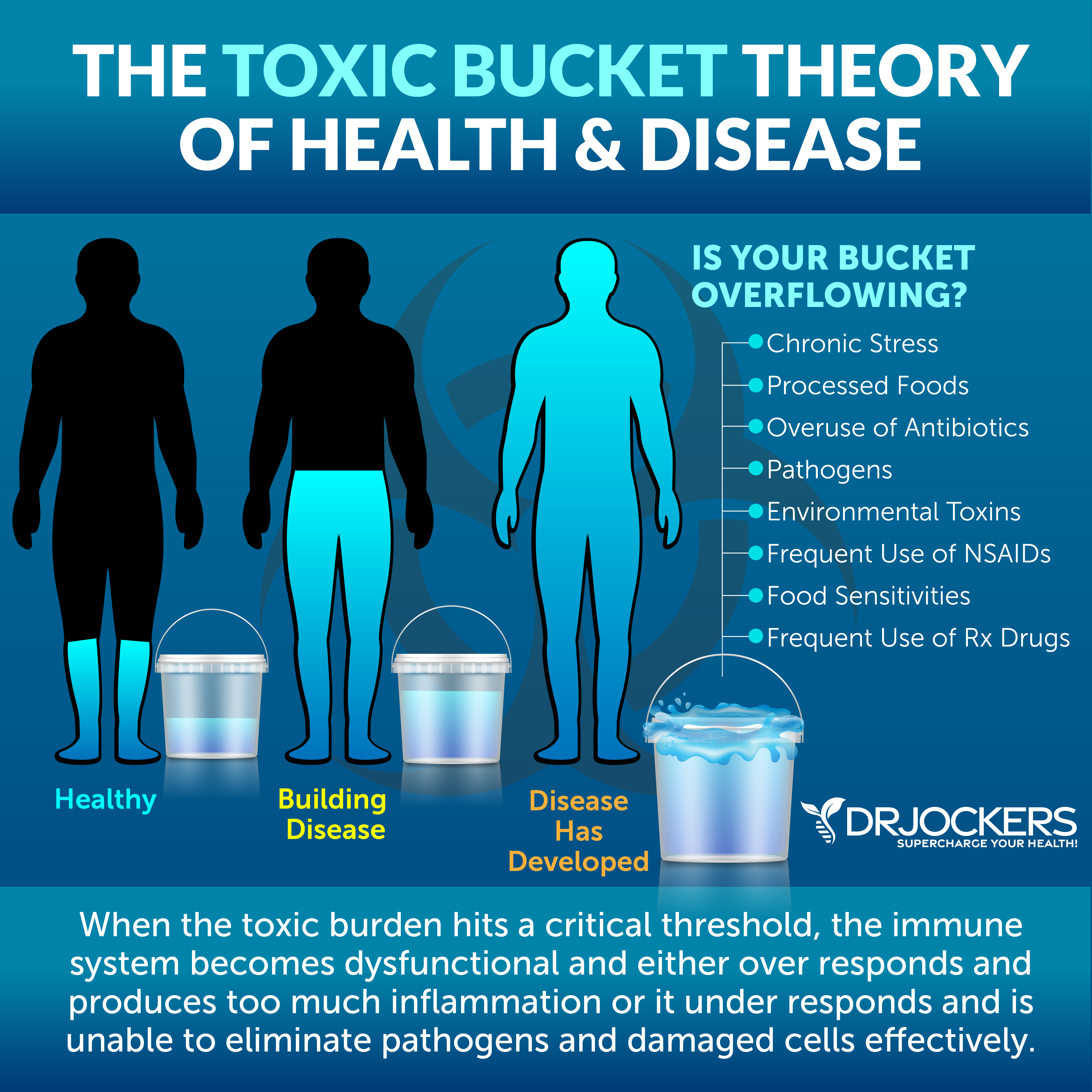
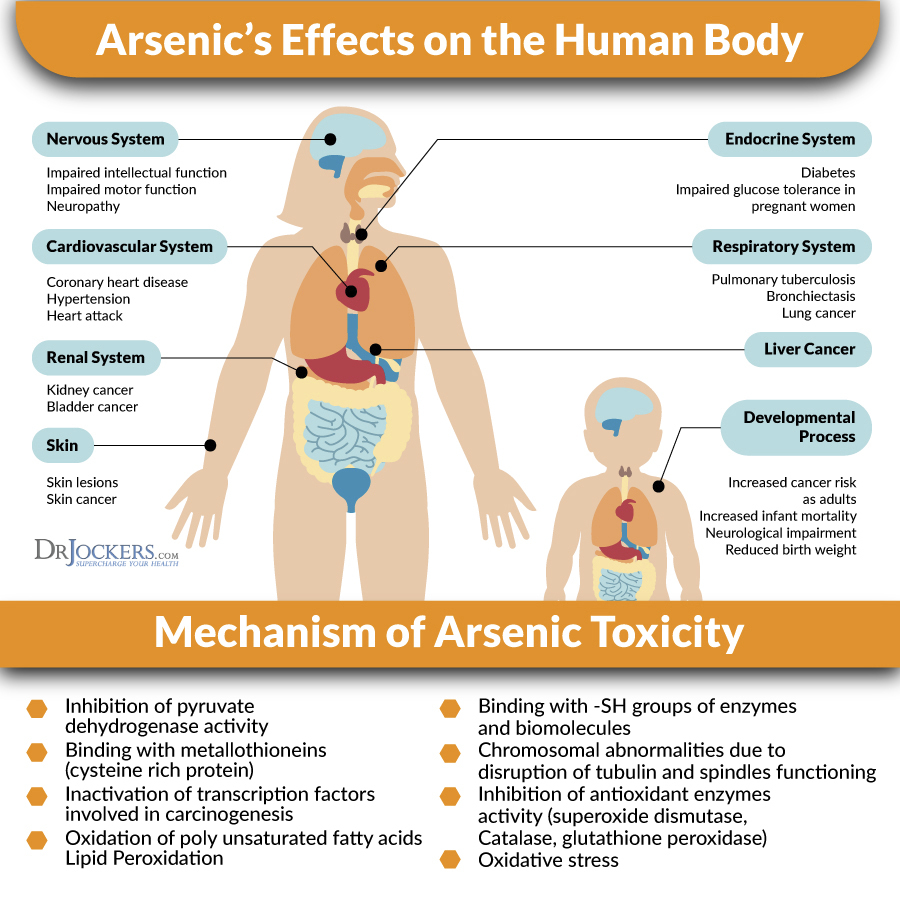
Heavy Metal Exposure and High Toxic Load
Heavy metal exposure and high toxic load can also increase your risk of pancreatic cancer. A 2020 study published in the International Journal of Environmental Research and Public Health has explained that mercury exposure is widespread. For example, it’s common through dental amalgam fillings. It can increase your risk of pancreatic cancer (12).
A 2000 meta-analysis published in Cancer Epidemiology Biomarkers Preview has found that cadmium can increase the risk of pancreatic cancer (13). A 2017 study published in Biomedical Research International has also found evidence that cadmium exposure increases oxidative stress, apoptotic changes, and carcinogenic, and is a big risk factor for pancreatic cancer (14).
A 2013 Florida study published in BMC Cancer has found a link between arsenic-contaminated drinking water from wells and the risk of pancreatic cancer (15). A 2011 study published in Gut has found that certain trace elements, such as cadmium, arsenic, can increase the risk of pancreatic cancer (16).
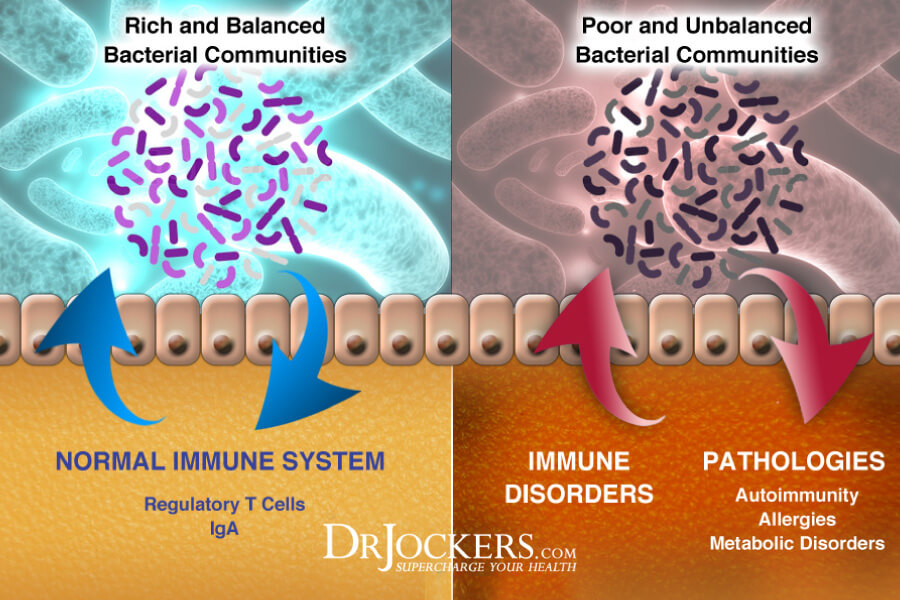
Gut Dysbiosis
Your pancreas plays an important role in your digestion. It’s no wonder that your gut microbiome health greatly affects your pancreatic health as well. Gut dysbiosis means that your gut microbiome is out of balance, and there are too many bad bacteria and too few beneficial bacteria in your gut. Gut dysbiosis may increase your risk for pancreatic cancer.
A 2019 study published in the Turkish Journal of Gastroenterology has found that small intestinal bacterial overgrowth (SIBO) has a high prevalence in pancreatic carcinoma (17). A 2014 study published in Cancer Journal has found that pancreatic cancer is an inflammation-driven cancer that can be linked to a poor microbiome (18).
Specific parasites and bacteria may play a significant role in the development of the disease. A 2011 case study has found that pancreatic ascariasis, a roundworm infection, may actually mimic a pancreatic tumor (19).
A 2013 study in PLoS One found a link between a helicobacter pylori (H pylori) infection and pancreatic cancer (20). A 2015 meta-analysis published in Cancer, Causes & Control and a 2016 meta-analysis published in the Journal of Cancer Research and Theory have both found that an H pylori infection may increase the risk of pancreatic cancer (21, 22).
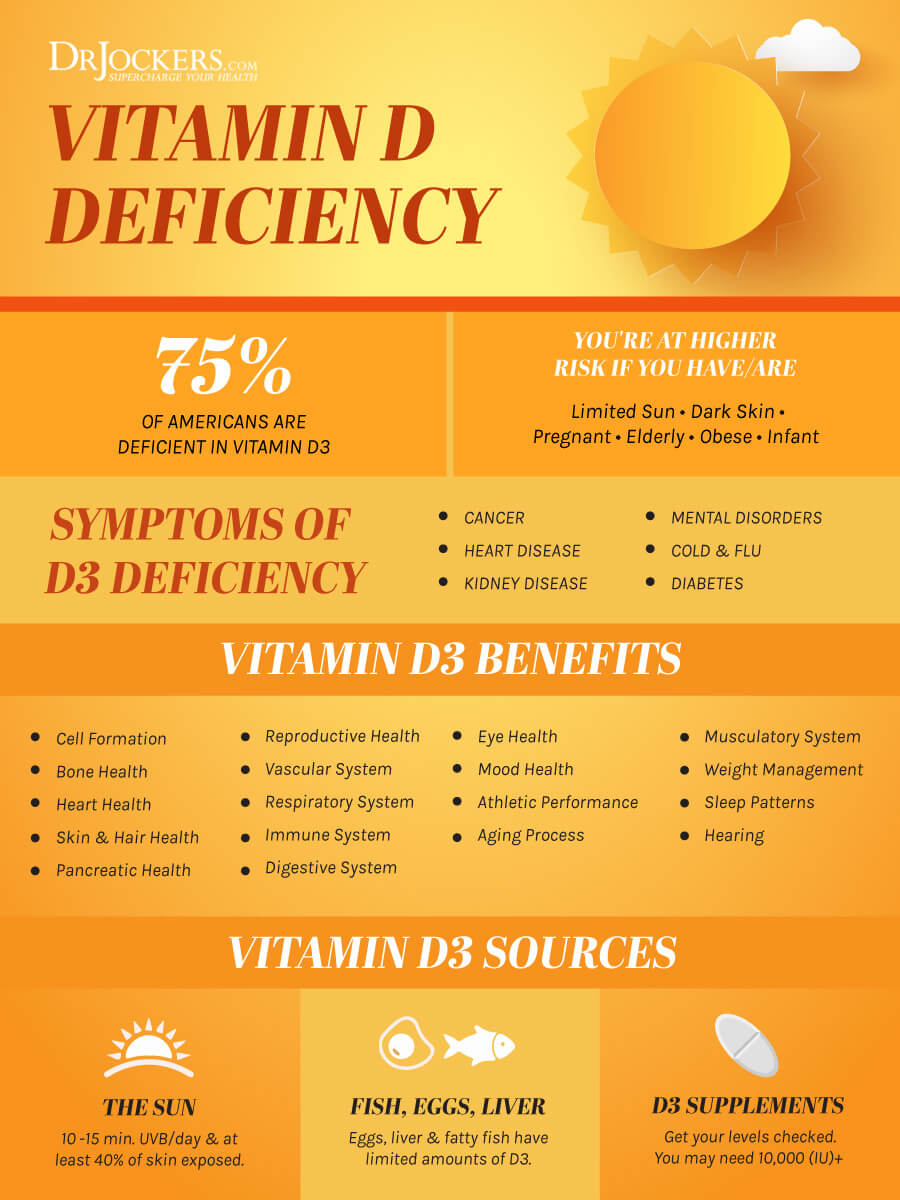
Vitamin D Deficiency
Vitamin D is an essential vitamin for your immune system, bones, muscles, heart health, digestion, and brain health. According to a 2016 study published in Frontiers in Physiology, vitamin D is important for your gut microbiome and improving metabolic disorders. Deficiencies in vitamin D can cause gut dysbiosis, obesity, and metabolic syndrome, which are risk factors for pancreatic cancer (23).
A 2006 scientific paper published in Cancer, Epidemiology, Biomarkers, and Prevention found that a deficiency in vitamin D can increase the risk of pancreatic cancer (24). Researchers conducted two cohort studies and a follow-up 16 years later, and found the lowest vitamin D levels in participants with pancreatic cancer. A 2017 meta-analysis published in Oncotarget has found that vitamin D deficiency may be linked to both the risk and mortality rates of pancreatic cancer (25).
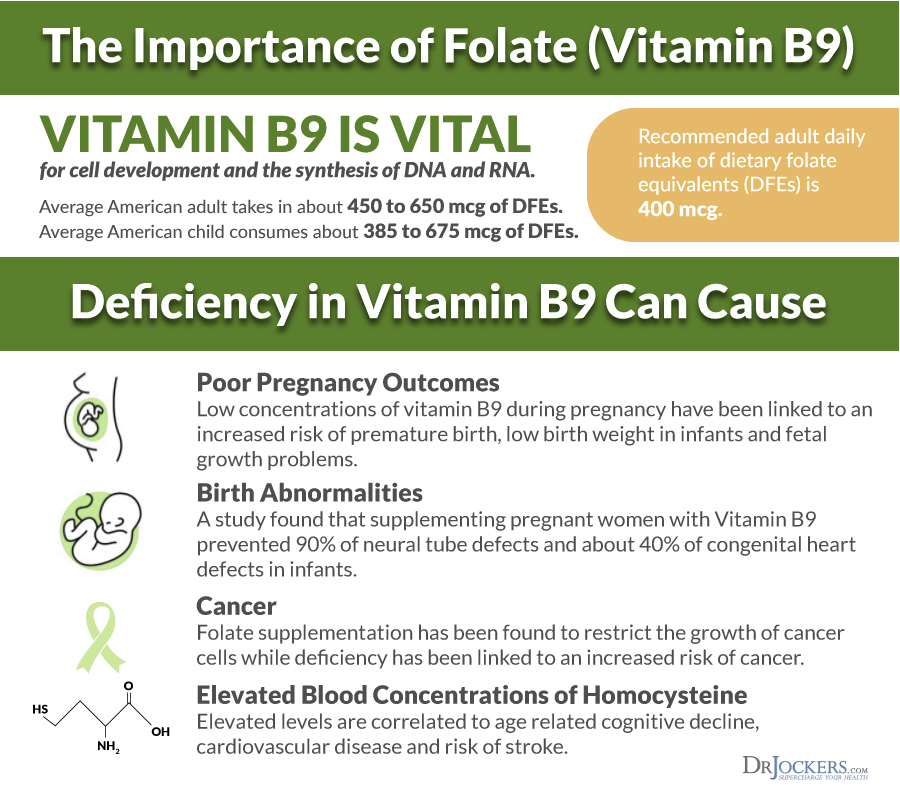
Folate Deficiency
Folate is an essential B vitamin that helps your body make red blood cells. Folate deficiency may also contribute to the development of pancreatic cancer. According to a 2018 clinical trial published in PLoS One, folate levels, among other nutrient deficiencies, can be linked to your risk for pancreatic cancer (26).
A 2013 review published in Public Health has found that folate supplementation may be protective against pancreatic carcinogenesis (27). A 2014 systematic review and meta-analysis of nine studies found that folate deficiencies can increase the risk of gastrointestinal cancers (28).
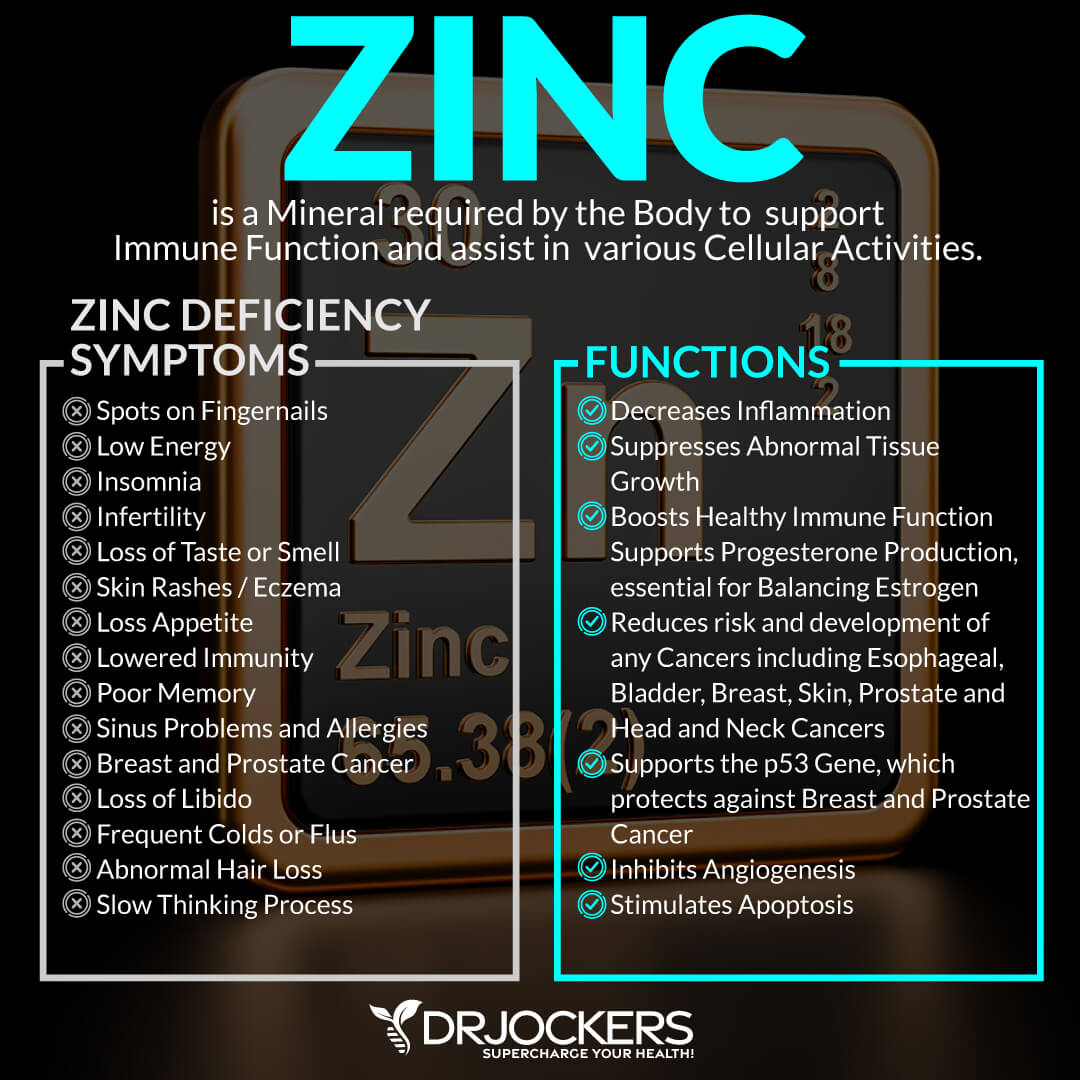
Low Antioxidants and Zinc
Antioxidants are nutrients that help to slow free radicals and oxidative damage and reduce your risk of cancer. A 2016 meta-analysis of 11 studies has found a link between low vitamin A levels and pancreatic cancer risk (29). A 2015 study published in Science Reports has found a connection between low vitamin C and pancreatic cancer (30). According to a 2015 meta-analysis published in Medical Science Monitor, low vitamin E is also linked to an increased risk for pancreatic cancer (31).
Zinc is an essential nutrient that helps your immune function. Zinc deficiencies are widespread and can increase the risk of various diseases, including pancreatic cancer. According to a 2016 review published in the European Journal of Cancer Prevention, zinc supplementation may serve a role in the prevention and treatment of pancreatic, prostate, and breast cancer (32). A 2017 meta-analysis published in Bioscience Reports has found that low zinc levels may be linked to increasing pancreatic cancer risk (33).
Natural Support Strategies
There are a number of natural support strategies you can try to improve your health and well-being. While these strategies are not FDA-approved to prevent, mitigate, treat, or cure pancreatic cancer, there is data that suggests they are very helpful. Please discuss these with your physician or health care practitioner.
Anti-Inflammatory Nutrition Plan
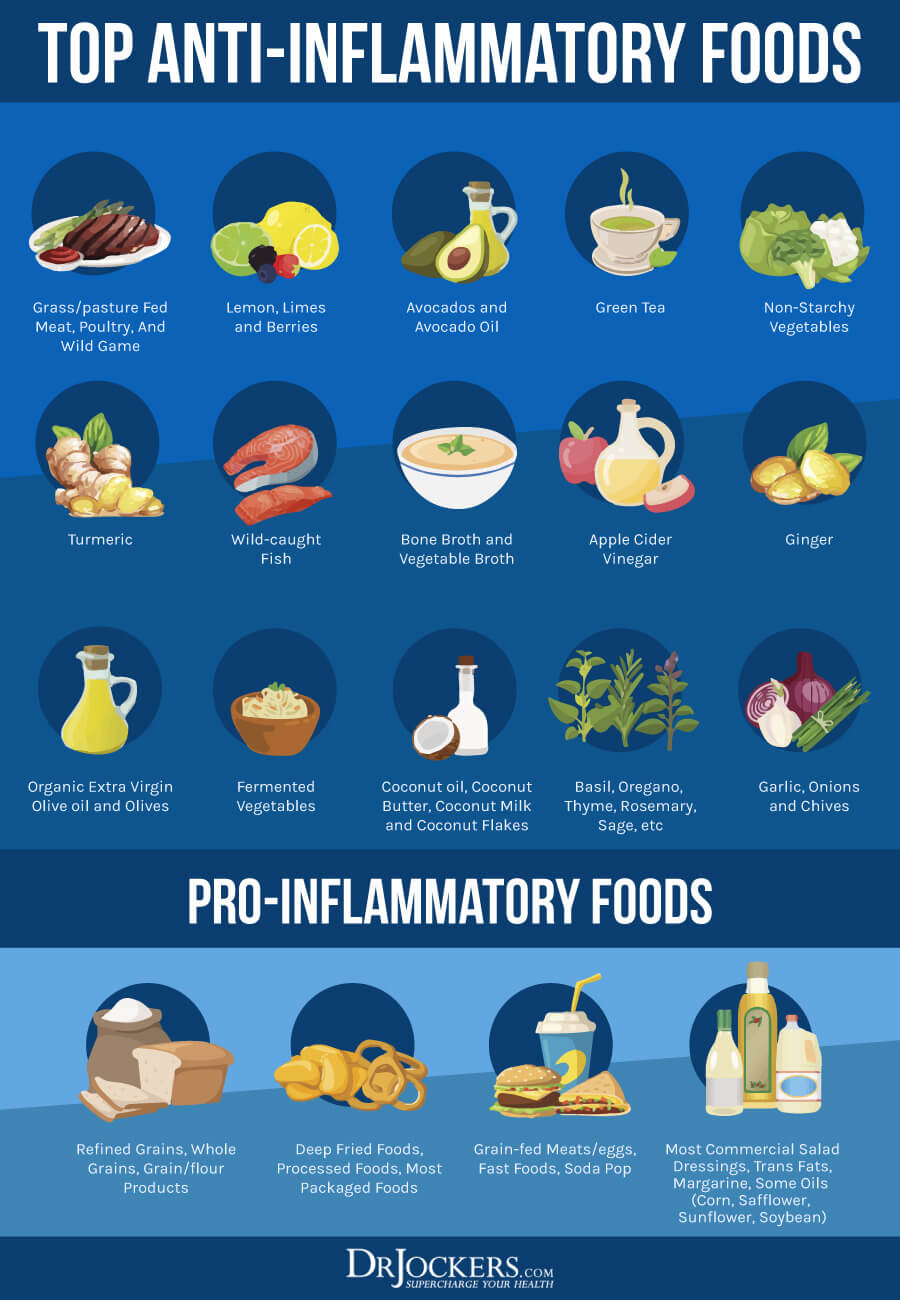
Eating a poor, inflammatory diet, chronic inflammation, obesity, and nutrient deficiencies are all risk factors for pancreatic cancer (3 2, 27, 28, 29, 30, 31, 32, 33). An anti-inflammatory diet can help reduce inflammation, nutrient deficiencies, the risk of chronic health issues, and obesity.
First, remove inflammatory foods from your diet, including refined sugar, refined oils, conventional dairy, conventionally raised and processed animal products, gluten, artificial ingredients, highly processed foods, deep-fried foods, and junk food. Follow a nutrition plan rich in greens, vegetables, herbs, spices, fermented foods, low glycemic index fruits, healthy fats, and clean animal protein, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
Eat plenty of folates, zinc, and antioxidant-rich foods to avoid and improve deficiencies that can increase your risk of pancreatic cancer. Some folate-rich foods include broccoli, Brussels sprouts, leafy greens, liver, peas, and chickpeas. Zinc-rich foods include meat, poultry, eggs, nuts, seeds, lentils, and beans.
Foods that are rich in antioxidants include blueberries, strawberries, blackberries, other berries, artichokes, kale, red cabbage, beets, cauliflower, orange bell pepper, pecans, pistachios, chestnuts, flax seeds, oregano, basil, cloves, cinnamon, green tea, and cacao.
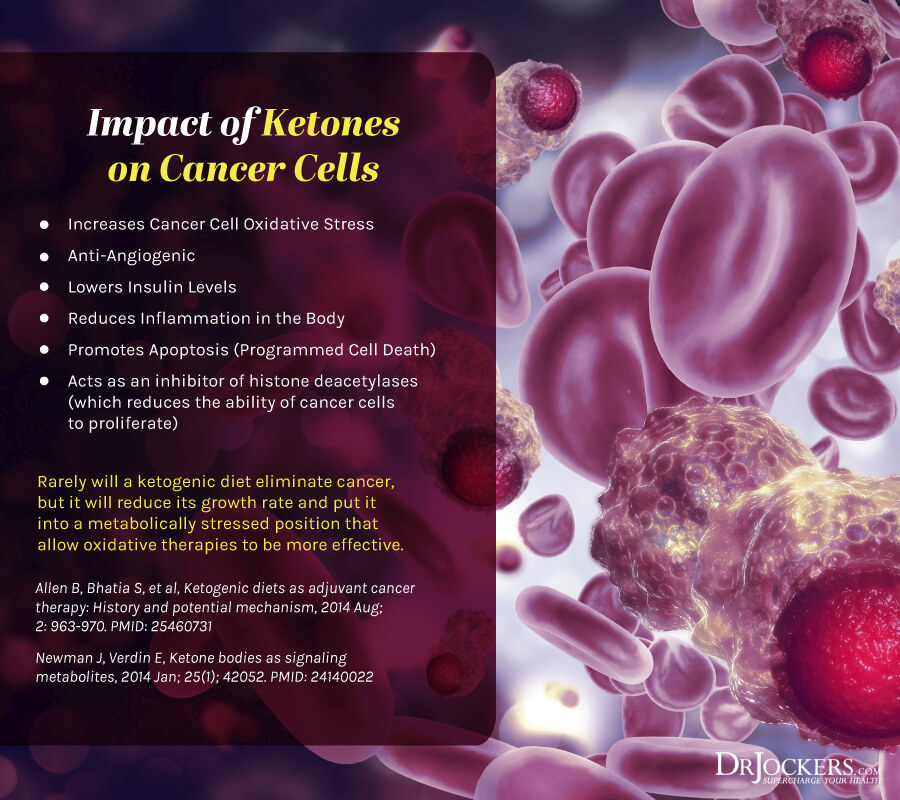
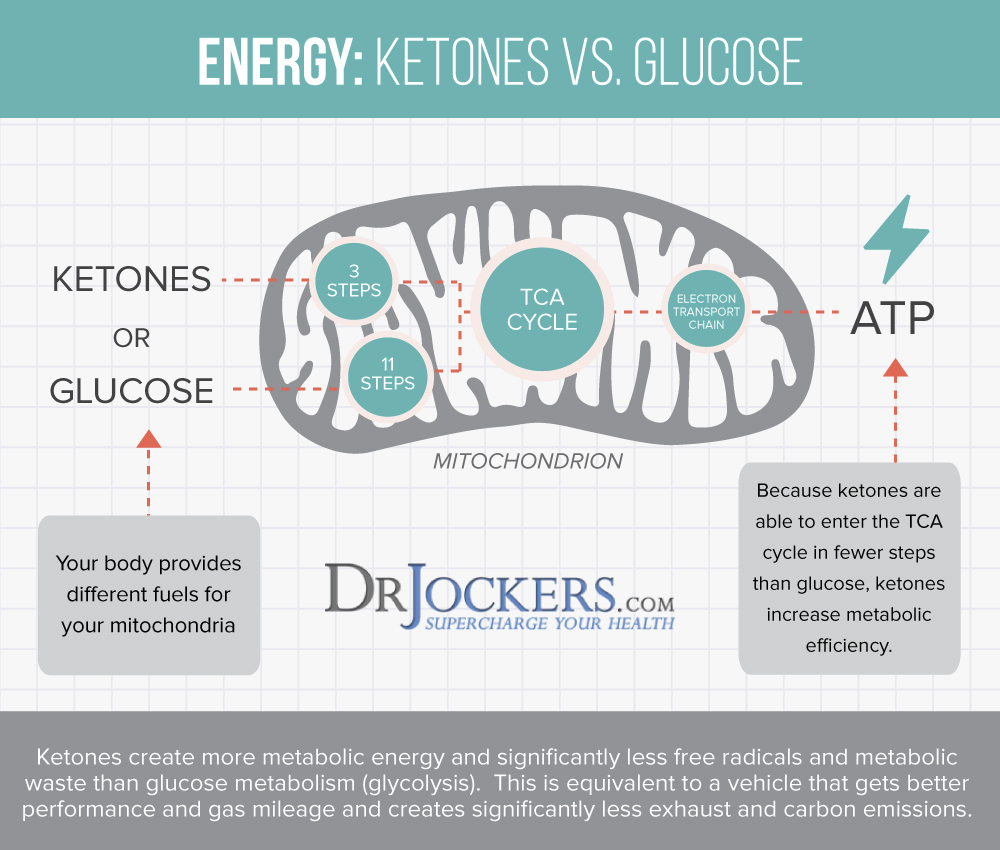
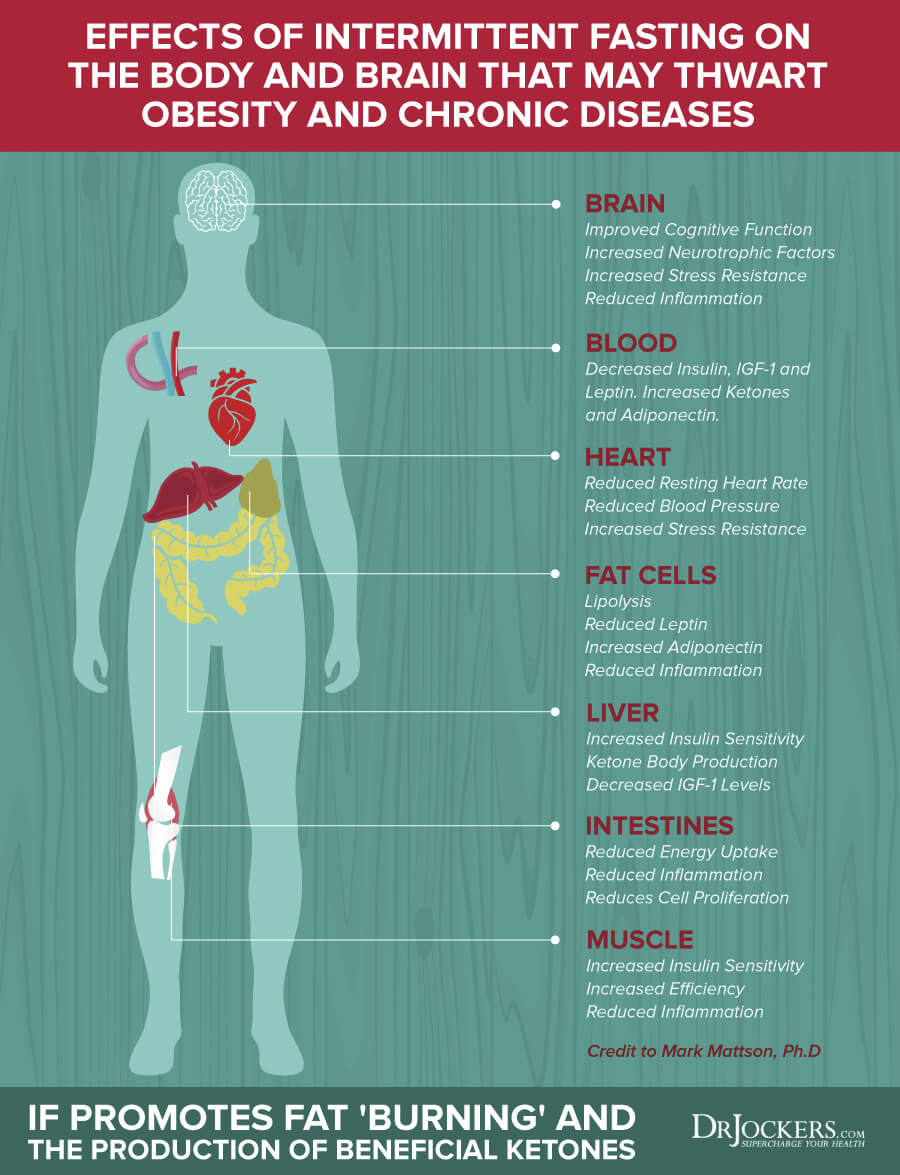
Get Into Ketosis
Under ordinary circumstances, your body burns glucose for energy. However, when your body doesn’t have enough dietary glucose to burn for energy because of caloric or carbohydrate restriction, it will turn to fat for energy instead and start to make ketones in the process. Ketosis has many health benefits, including reduced inflammation, increased insulin sensitivity, improved cellular renewal, and a decreased risk of disease.
The ketogenic diet is a great way to get into ketosis, which may help to improve your health. Following a keto diet may help to optimize your diet and improve your health. While using a keto diet or getting into ketosis for pancreatic cancer is controversial in the natural health space, there are a number of studies that suggest that it may be beneficial.
A 2020 animal study published in Current Developments in Nutrition suggests that a ketogenic diet may be beneficial for pancreatic cancer (33). About pancreatic ductal adenocarcinoma (PDA) experience cachexia, and about one-fifth of them die from it. After feeding mice a keto diet, the study found that a keto diet may mitigate cachexia associated with pancreatic cancer.
But it’s not just animals. Human studies have also shown the benefits of ketosis for pancreatic cancer. A 2018 study published in Anticancer Research has found that following a ketogenic diet can help to improve the energy levels and recovery of pancreatic cancer patients after pancreatectomy (34). A 2020 study published in Nutrients has found that carbohydrate restriction on a keto diet has helped to reduce mortality in advanced pancreatic cancer patients (35).
A 2014 study published in Cancer Metabolism has found that a ketogenic diet may help to reduce tumor cell growth and weight loss, muscle wasting, and cachexia in pancreatic cancer patients (36). A 2017 study published in Radiation Research has found that following a ketogenic diet may support pancreatic and lung cancer patients and reduce toxicity while receiving radiation or chemotherapy (37).
Real Food Keto Diet
To follow the ketogenic diet, keep your carbohydrate levels very low at 5 to 10 percent, your protein levels moderate at 30 to 35 percent, and your fats high at 55 to 60 percent of your calories. I recommend that you follow a real food ketogenic diet. The dirty keto diet only focuses on your macronutrient ratios instead of nutrients. However, loading up on fatty junk foods is not going to do much for your health, even if you keep it at keto-approved low-carb ratios.
High nutritional content is critical. Use the principles of the anti-inflammatory nutrition plan we discussed earlier while focusing on healthy fats and keto-approved macronutrient ratios.
Most of your diet should be full of healthy fats, including avocados, coconut oil, coconut butter, coconuts, avocado oil, extra-virgin olive oil, pasture-raised butter and ghee, lard, flax seeds, hemp seeds, chia seeds, pumpkin seeds, other seeds, olives, nuts, and any fats from clean animal foods, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
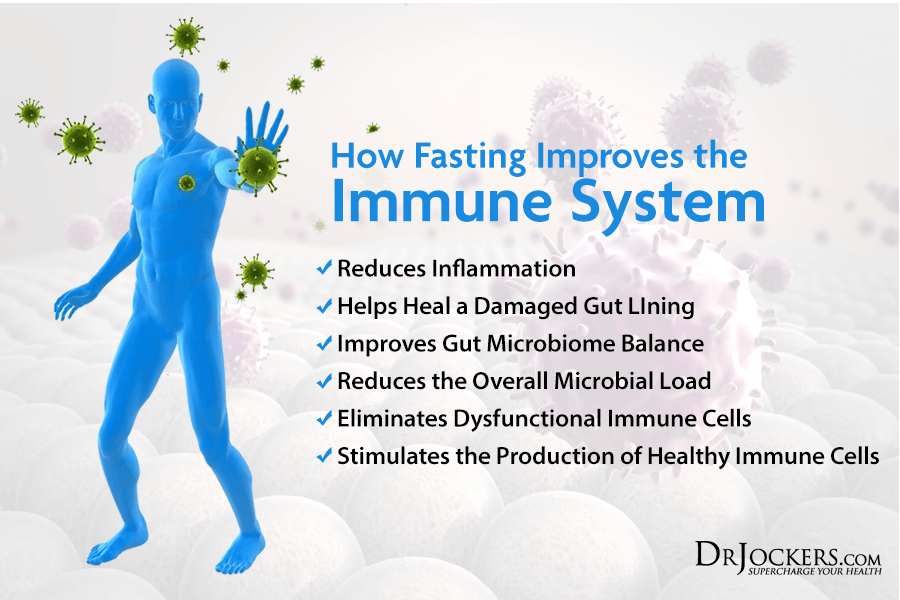
Intermittent, Partial, and Extended Fasting
Another great way to get into ketosis, improve your inflammation levels, support cellular renewal, and reduce the risk of disease is fasting. A 2018 study published in the National Reviews Cancer has found that fasting may support cancer treatment methods without serious risks or side effects (38).
Intermittent fasting is a form of fasting that cycles between periods of fasting and periods of eating within one day. If you are new to intermittent fasting, I recommend that you begin by practicing Simple Fasting. A Simple Fast involves 12 hours of fasting, including your overnight sleep. It’s simple to follow. All you have to do is stop eating and start fasting after dinner, and don’t eat for 12 hours until breakfast. During your eating window, load up on a nutrient-dense, anti-inflammatory, and ketogenic diet.
Gradually increase your fasting window over the next few weeks until you find what works for your body. While most people do the best with a 16-hour fasting window using the 16:8 method, a shorter or longer window may work better for your body. It’s important that you know that intermittent fasting is not about starving or nutrient restriction. Make sure to eat enough to meet your nutrient and caloric needs during the eating window.
Partial Fasting
Partial fasting is a step between intermittent fasting and extended fasting. If you are ready to challenge yourself but not quite ready to go completely without food. Partial fasts usually involve a strategy that focuses on liquids or caloric reduction.
You may try a liquid partial fast. Green Juice and Bone Broth Fasting have been very popular in recent years. You may even order a Green Juice or Bone Broth Cleansing kit to avoid preparation and make it simple for yourself. Green Juice Fasting focuses on green juices, while Bone Broth Fasting recommends drinking bone broth for a few days.
You may benefit from the Fasting Mimicking Diet® or FMD®. It is a partial fasting plan that is high in nutrients, low in protein, and low in carbohydrates. On Day 1, restrict your calories to 1,100 calories a day. 500 of these calories should come from complex carbohydrates and 500 from healthy fats. About 100 calories or 25 grams of plant-based proteins are also allowed, mainly from nuts. On Days 2 to 5, your calories are restricted to 800 calories only, with 400 calories from complex carbs and 400 calories from healthy fats.
You may also turn to a Fat or Keto Fast or the Daniel Fast. The Fat or Keto Fast combines Partial Fasting with the principles of the ketogenic diet. It recommends that you eat 500 to 1000 calories a day, with 90 percent of those calories coming from healthy fats.
The Daniel Fast is a Biblical fast focusing on a plant-based, vegetarian diet for 21 days. While I generally don’t recommend following a vegetarian or vegan diet long-term, you may benefit from this shorter 3-week plant-based diet. The Daniel Fast is a high-nutrient plant-based plan that may help to correct nutrient deficiencies while taking the toll on your digestive system. Following a plant with Biblical roots may also offer spiritual benefits and some emotional healing that is critical during times of illness.
If you are ready and doing well on longer intermittent fasting or partial fasting strategies, you may try an extended fast. During an extended fast or water fast, you are only drinking non-caloric drinks, including purified water and herbal tea, for a day or several days. This strategy is only for those who are experienced in other fasting methods and doing well on them. I recommend that you talk to your healthcare provider if you are about to embark on an extended fast, especially if you are dealing with pancreatic cancer or other serious health issues. You may learn about all these fasting methods by searching my website.
Reduce Stress & Improve Sleep
Chronic stress and poor sleep can greatly increase chronic inflammation in your body, which can contribute to the increased risk of pancreatic cancer. Not to mention that it is very difficult to focus on healing and allow your cells to recover when you are constantly stressed and tired. Reducing stress and improving your sleep is critical.
Reduce stress in your life as much as possible. Stop scrolling the news all day, but pick a designated time to check it instead. Stop scrolling your social media all day, reading comments. Follow pages and groups that inspire or uplift you and remove the rest. Avoid stressful situations and people that bring you down as much as possible.
Since avoiding stressful situations, people, and things completely is impossible, it is important that you learn to respond to stress better, reduce your anxiety, and learn to calm your mind and body. Create positive mindset shifts. Working with a therapist, counselor, or life coach can help you with that. Practice gratitude. Try meditation, guided relaxation, breathwork, visualization, prayer, spiritual practices, journaling, and positive affirmations. Time in nature, taking a healing bath, calming essential oils, like lavender, or sipping on herbal tea may also help.
Reduce the use of electronics at night and use blue-light blocking glasses if you must turn on your screen. Avoid sugar, caffeine, alcohol, heavy foods, and stress in the evening. Engage in calming conversations. Choose board games, cards, crossword puzzles, singing, listening to calming music, reading, knitting, crocheting, coloring, drawing, or other calming activities.
An evening gratitude practice, prayer, meditation, and visualization exercises are great before going to bed. Support your body’s circadian rhythms by going to bed and waking up around the same time every day. Invest in a supportive and comfortable mattress, pillows, and beddings, and use blackout curtains or eye pillows.

Movement & Exercise
Movement and exercise can also reduce stress and inflammation. It also helps to reduce the risk of being overweight or obese, which is a huge risk factor for pancreatic cancer (3).
Stay active throughout the day. Start your day with a little stretching, yoga, rebounding, or a short walk. Get up and stretch, move, or walk around throughout the day regularly. Take a walk or try a workout during your lunch hour or midday before you eat. Take the stairs instead of the elevator. Park away from the store to add some steps to your day. Stop for a little dance session when your favorite song is on. Choose to walk or bike instead of driving for shorter distances.
Exercise at least five days a week, 20 to 30 minutes a day. Choose a mix of cardiovascular workouts, such as jogging, swimming, biking, spinning, dancing, or aerobics, strength and resistance training, such as body weight workouts, weight lifting, CrossFit, TRX, or kettlebell training, and low-impact workouts, such as yoga, pilates, barre, and TaiChi.
If you are currently undergoing treatment for pancreatic cancer, you may feel tired and unable to complete harder workouts. That is completely okay. Listen to your body and do what you are able to and what supports your body. If that’s a short walk or even stretching in your bed, that’s great. You will slowly regain your strength and health and will be able to do more.

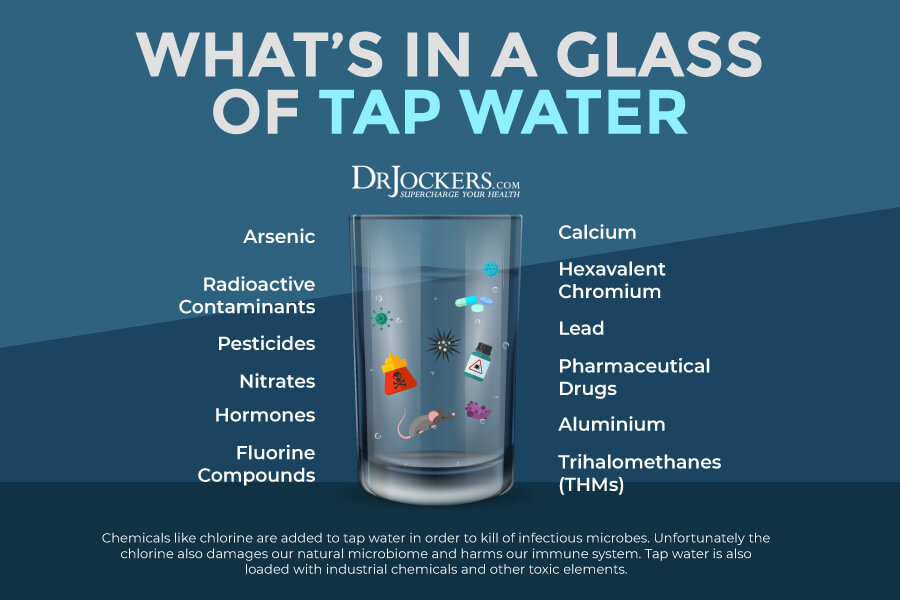
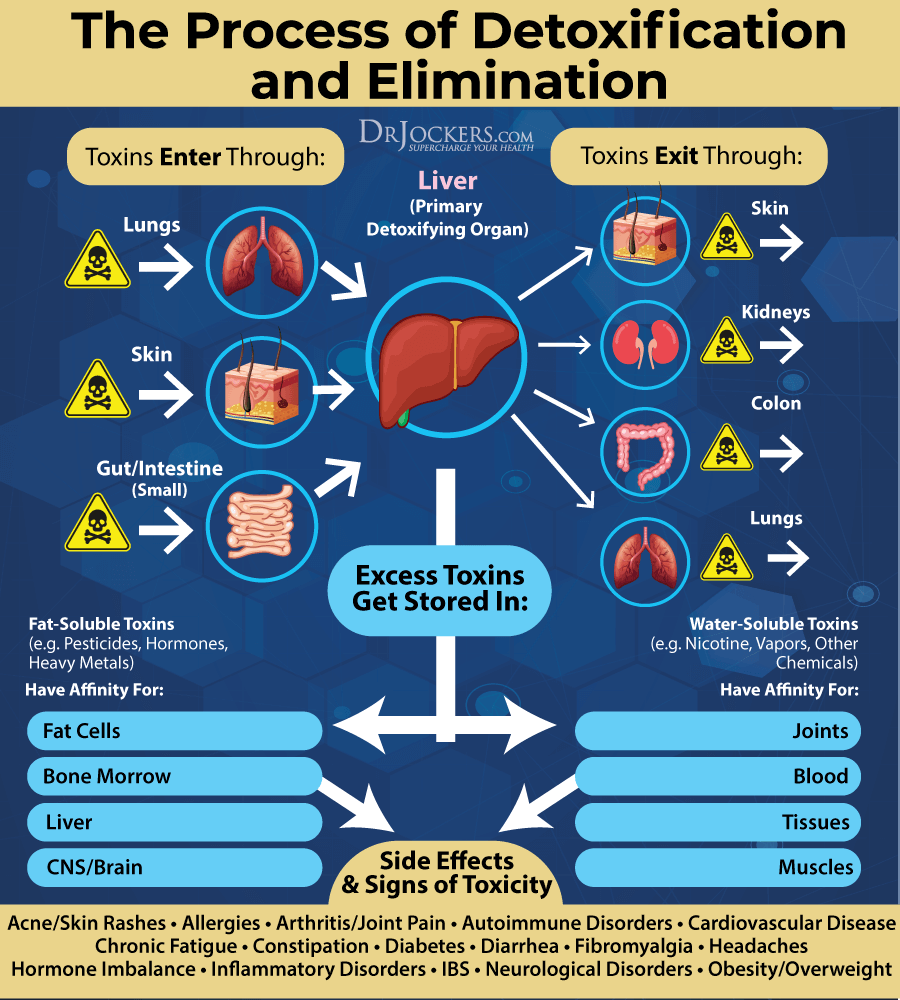
Reduce Toxin Exposure
Toxin exposure is one of the major root causes that can increase your risk of pancreatic cancer (7, 9,10, 11, 12, 13, 14, 15, 16). Reducing your toxin exposure is critical for decreasing your risks and improving your health.
If you are a smoker, stop smoking. Reduce your exposure to second-hand smoke as much as possible. If you live in a polluted area, make sure to spend plenty of time in nature and get fresh air. Improve your indoor air by investing in HEPA air filtration systems. Check your home for mold, and if you find any, get it professionally eradicated or move.
Avoid toxins in tap water by using a water purification and filtration system that removes chemicals, heavy metals, and microbes from the water. Avoid plastic bottles and opt for glass or aluminum bottles, mason jars, glasses, and ceramic mugs. Avoid the use of plastics and choose glass, wood, bamboo, cloth, and other natural, toxin-free options.
Remove any chemical-filled conventional cleaning, body, and beauty products, and choose toxin-free, natural, organic, and homemade alternatives. Choose organic food to avoid exposure to pesticides, herbicides, and hormones. Avoid processed foods and junk foods that are full of additives and unnatural ingredients. Visit a biological dentist to remove amalgam mercury fillings.
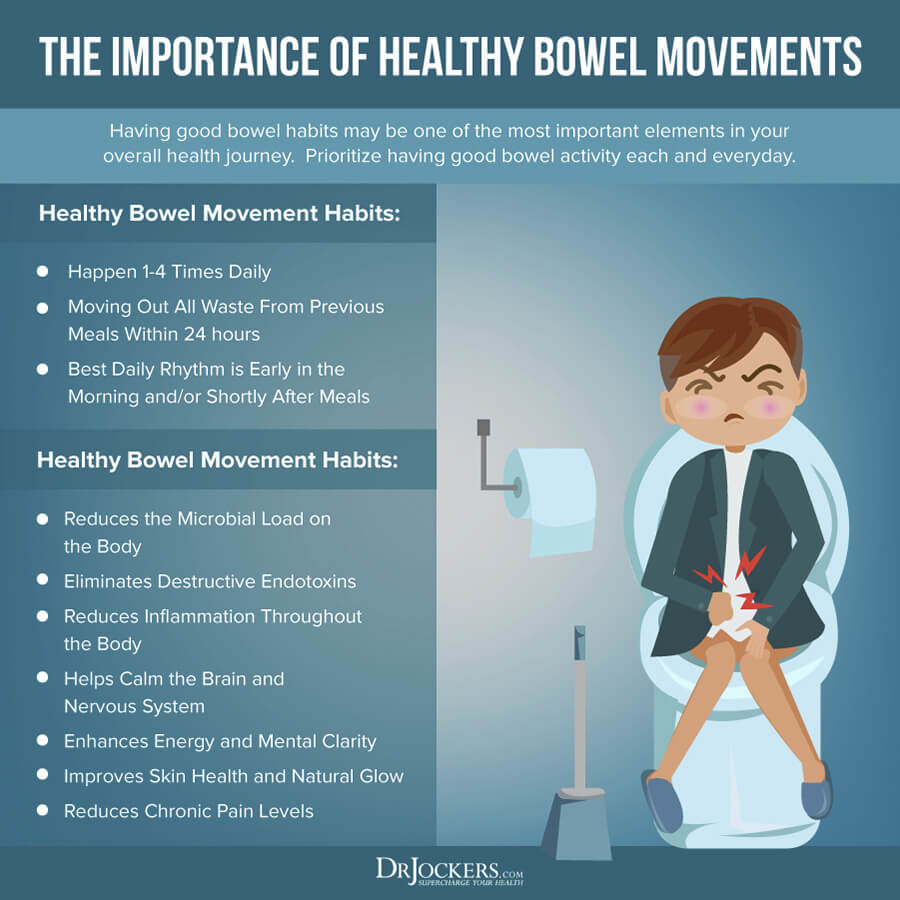
Detoxify Your Body
Removing toxins is not enough to reduce your risks. You need to detoxify your body from past toxin exposure (7, 9,10, 11, 12, 13, 14, 15, 16). Support your digestion, absorption, and elimination pathways through a healthy diet. Drink plenty of water to support elimination through urine and sweating, and avoid dehydration. Support detoxification through the skin by sweating, by using an infrared sauna regularly, and exercising.
Try activated coconut charcoal that binds to heavy metals and toxins. It supports the elimination of these toxins and reduces oxidative stress and inflammation. Use bioactive carbons derived from multiple sources of humic acid, fulvic acid, and humic acid to support the elimination of heavy metals and other toxins and improve detoxification pathways. Try coffee enemas to help pull out and eliminate toxins and old waste from your colon.
Reduce Gut Infections
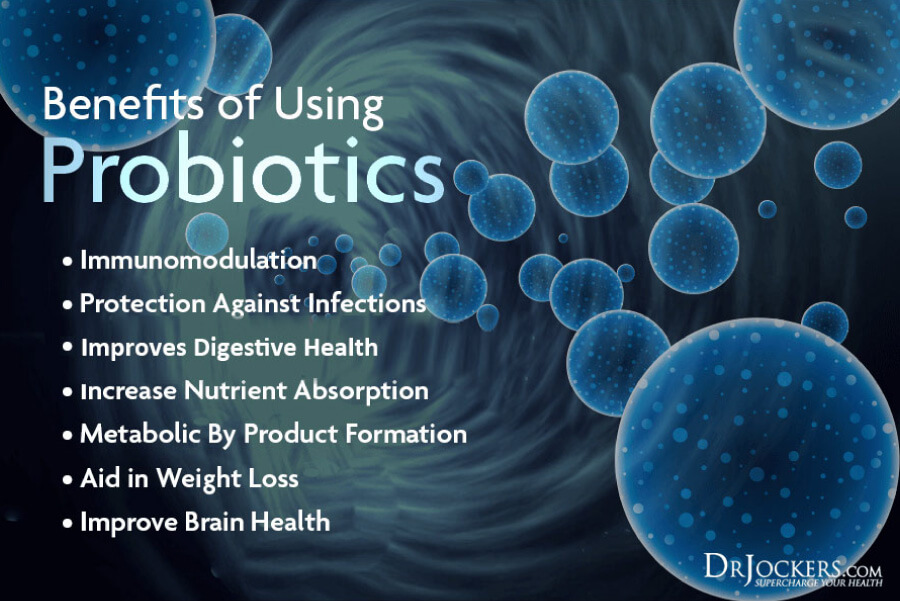
Gut dysbiosis and gut infections, like H pylori or parasites, are a serious underlying cause of pancreatic cancer (17, 18, 19, 20, 21, 22). Eating a healthy, gut-friendly, anti-inflammatory diet, as I explained earlier in this article. Supporting your microbiome with probiotics and if they are right for you, prebiotics can help to reduce gut infections.
In addition, I recommend supplementation for your specific gut infections. Testing for gut infections with a GI Map Stool Test or another high-quality stool testing can help identify what infections you are dealing with. Mimosa pudica seed is a great option for parasites. Oregano oil, garlic, olive leaf extract, Pau d’arco, berberine, and grapefruit seed extract are some other herbs that help to reduce and remove gut infections. I recommend that you work with a functional medicine professional who can guide you with a personalized protocol. My team and I would be happy to support your journey.
Support the Microbiome with Probiotics
Supporting your body with probiotics is critical. According to a 2016 study published in Advances in Bioscience and Biotechnology, probiotics may support the prevention of pancreatic cancer (39). A 2018 study published in Gastroenterology and Hepatology from Bed to Bench has also found that probiotics may play a role in the prevention of gastrointestinal cancer by reducing inflammation, microbiome imbalances, and nutritional absorption issues (40).
Probiotic-rich foods include sauerkrauts, kimchi, fermented vegetables, kefir, pickles, and kombucha. Additionally, I recommend daily supplementation with a high-quality probiotic supplement. If you have SIBO, I recommend that you choose soil-based (SBO) probiotics. Other probiotics may have some bacteria in them that are beneficial for most people, but may be harmful and trigger SIBO.
Since prebiotics feed probiotics, you may benefit from prebiotic-rich foods, including jicama, Jerusalem artichokes, apples, leeks, garlic, onions, asparagus, and dandelion greens. Prebiotics are not right for everyone, however. Some people thrive on a prebiotic-rich diet, while others get worse and need to minimize prebiotics by following a low-FODMAP diet or even a carnivore diet for a period of time.
Try out a high prebiotic diet and see if you feel better, and if not, try a low-FODMAP or carnivore diet and see if that helps you feel better. Experiment to find the right amount of prebiotics for your body type. Working with a functional medicine doctor can also help you figure out what’s right for you.
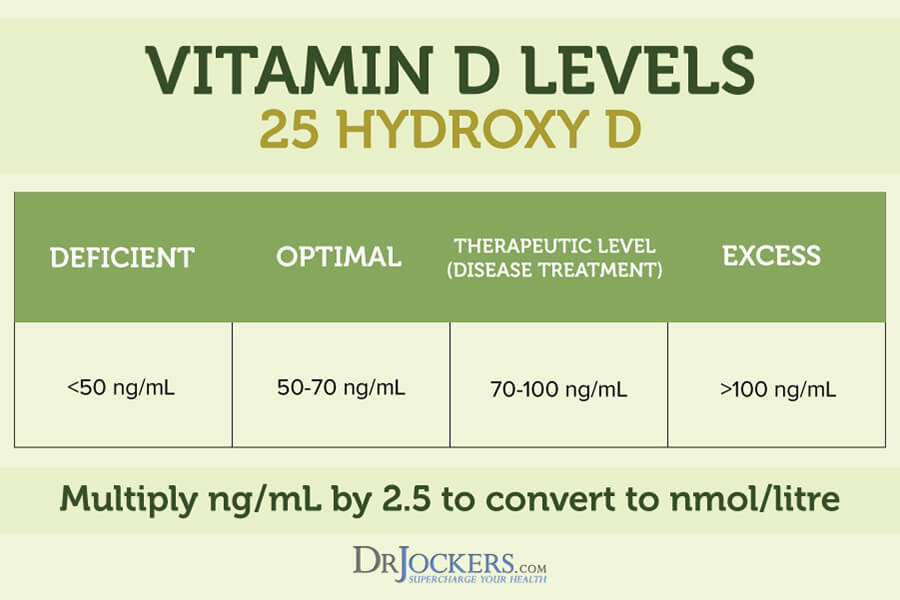
Optimize Vitamin D Levels
Vitamin D deficiency can increase your risk of pancreatic cancer, while improving your vitamin D levels can improve your health (23, 24, 25). Spending time outside in the sun regularly is important for your vitamin D levels and overall well-being.
The problem is that with our indoor lifestyle and many of us living in cloudy, gloomy, rainy, or snowy climates for a large part of the year, sunshine alone is not enough and not reliable for optimizing your vitamin D levels. Eating foods rich in vitamin D, such as fatty fish, liver, and egg yolks, is critical, but also not enough.
This makes daily vitamin D3 supplementation essential for optimal vitamin D levels for many individuals. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and control inflammation. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for diseases like pancreatic cancer is going to be between 70-100 ng/ml.
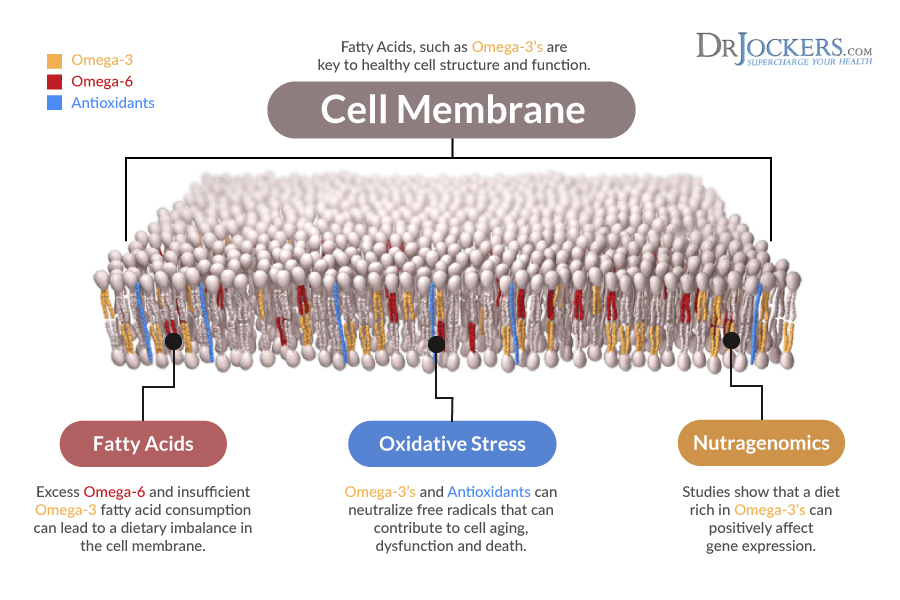
Improve Omega-3 Fatty Acid Levels
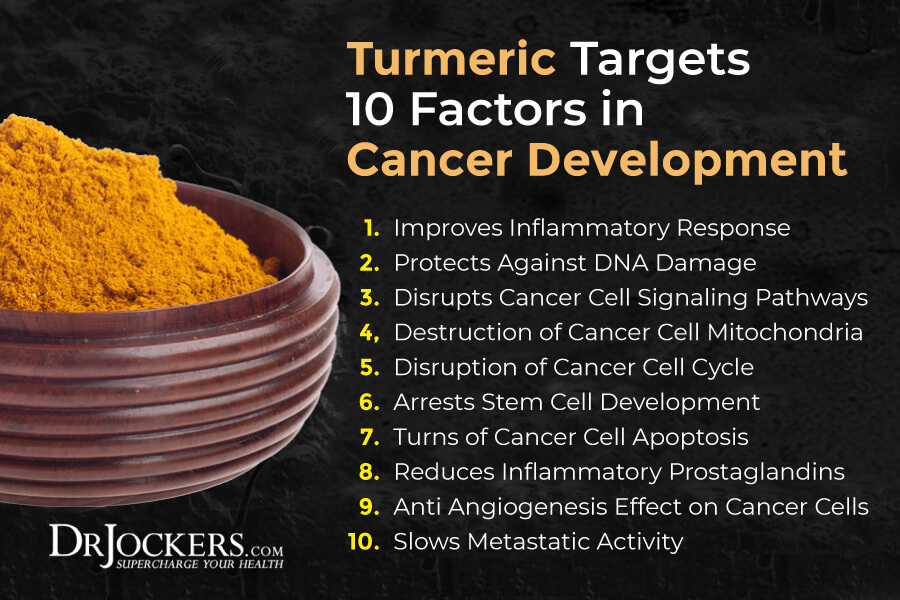
Improving your omega-3 levels with the combination of curcumin can help improve your health and reduce your risk. Omega-3 fatty acids are anti-inflammatory, healthy fatty acids found in fish, seafood, algae, hemp seeds, chia seeds, flax seeds, and walnuts. Curcumin is the active compound of the spice turmeric and offers anti-inflammatory and countless other health benefits.
A 2013 study published in the Journal of Cell Biochemistry has found that omega-3 fatty acids, EPA in specific, can help apoptosis and autophagy in pancreatic cancer cells (41). A 2008 study published in Nutrition and Cancer has found that omega-3 fatty acids taken in combination with curcumin can support the treatment and prevention of pancreatic cancer (42). Along with a diet high in omega-3-rich foods and turmeric, I recommend daily supplementation with a high-quality omega-3 fish oil supplement and curcumin supplement.
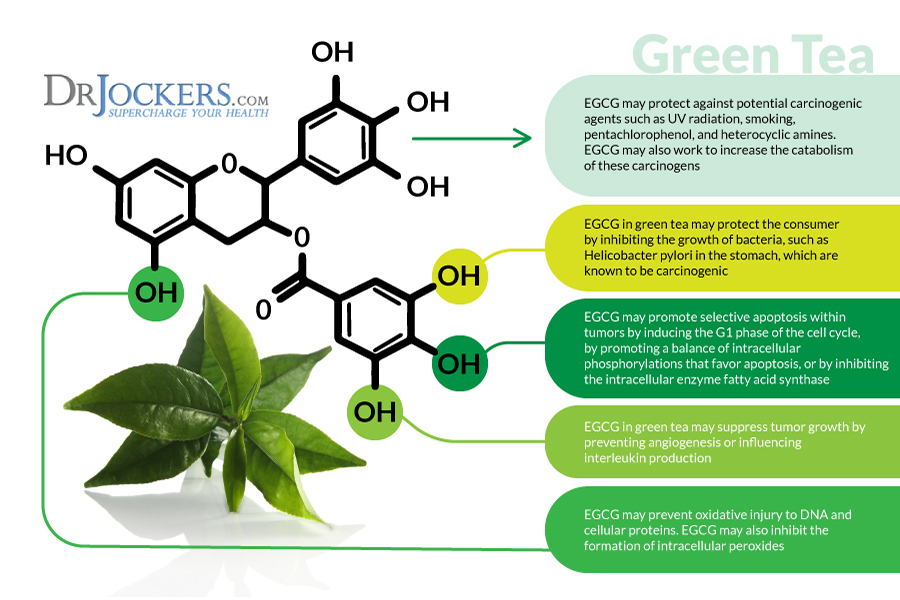
Consider Using Green Tea
Green tea offers antioxidant benefits. A 2019 study published in Nutrient found that epigallocatechin-3-Gallate (EGCG) in green tea may help reduce pancreatic cancer growth (43). A 2013 study published in Molecular and Cellular Biochemistry has found that EGCG can suppress pancreatic tumor growth (44).
I recommend drinking green tea regularly. You may also benefit from green tea extract supplementation.
Consider Using Turmeric or Curcumin
You already know that turmeric or curcumin combined with omega-3 fatty acids may help the prevention and treatment of pancreatic cancer (42). It turns out curcumin is beneficial on its own as well. According to a 2016 study published in Pancreas, curcumin can trigger cell death in pancreatic cancer by decreasing apoptosis inhibitors (45).
According to a 2018 prospective trial published in Pharmacological Research, curcumin may serve as a safe complementary therapy for pancreatic cancer patients in advanced stages (46). A 2014 study published in the World Journal of Gastroenterology has found that curcumin may serve as a therapeutic agent with or without cancer drugs for pancreatic cancer patients (47).
You can use turmeric as a spice in your juices, smoothies, dressings, soups, curries, baked vegetable dishes, and salads. I also recommend curcumin supplementation for reduced inflammation and overall health.
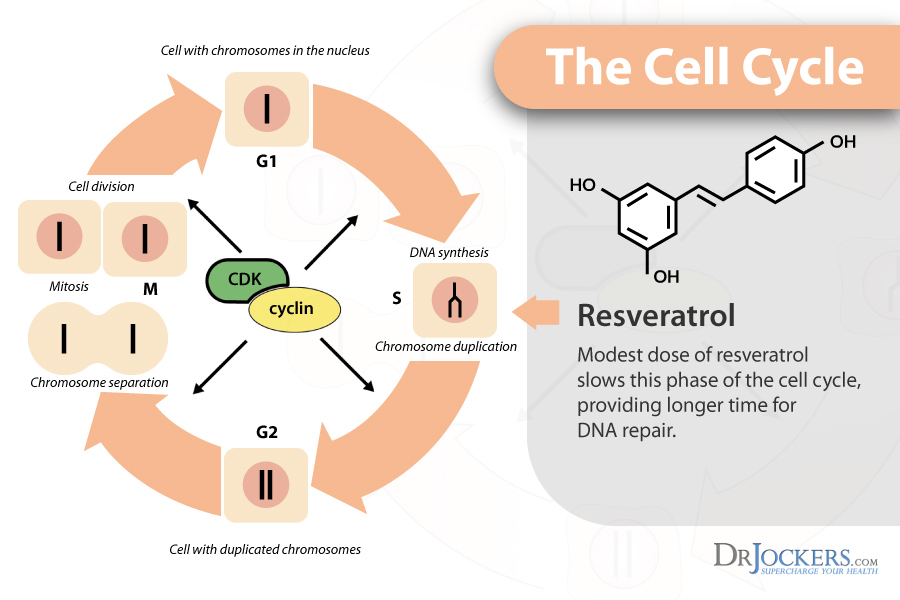
Consider Using Resveratrol
Resveratrol is an antioxidant plant compound found in the skin of grapes, berries, and red wine. A 2011 study published in the Chinese Medical Journal (English) has found that resveratrol supports apoptosis in pancreatic cancer cells (48). A 2014 study published in the Journal of Cancer Research and Clinical Oncology has found that resveratrol offers anticancer benefits in pancreatic cancer (49). A 2018 study published in Cell Proliferation has found that resveratrol may serve as a chemotherapy sensitizer and might be a good therapeutic agent for pancreatic cancer (50).
I recommend high-resveratrol foods, such as blueberries, cranberries, grapes, and pistachios. Additionally, I recommend supplementing with resveratrol for anti-inflammatory and antioxidant benefits.
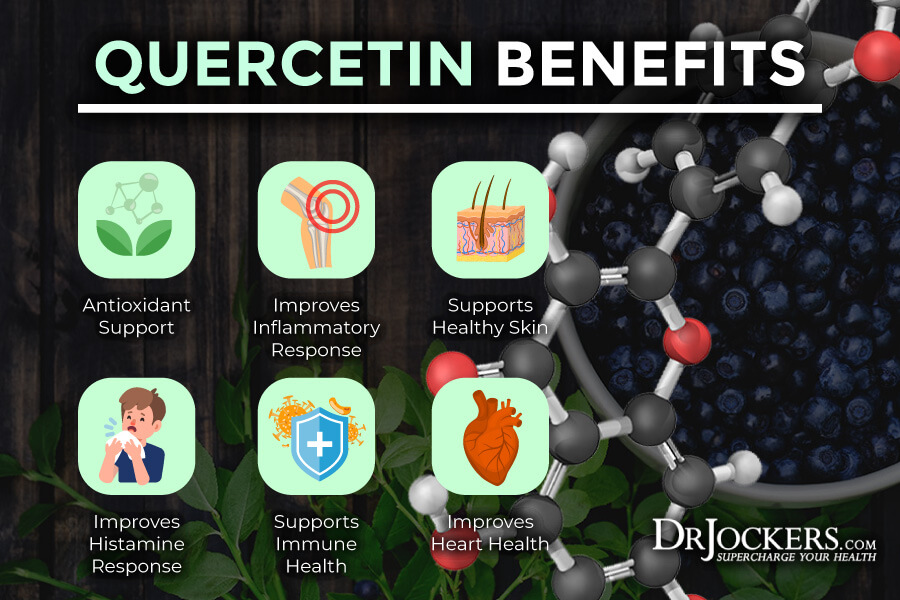
Consider Using Quercetin
Quercetin is a plant flavonoid that works well together with resveratrol, offering similar benefits. A 2016 study published in the International Journal of Biochemistry and Cell Biology has found that quercetin may serve as an anti-cancer agent and help to kill cancer cells (51).
A 2019 study published in Food Function has found that quercetin may help to support the treatment of pancreatic and colorectal cancer (52). A 2018 preliminary in vitro study published in the Journal of Cellular Physiology has also found that quercetin may serve as a therapeutic agent combined with other treatment options for pancreatic cancer (53).
I recommend filling up on quercetin-rich foods, including cabbage, sprout, raw asparagus, snap peas, raw kale, red onion, chicory greens, red leaf lettuce, romaine lettuce, peppers, cruciferous vegetables, olive oils, cherries, grapes, apples, cranberries, blueberries, black plums, black currants, and chokeberries.
I also recommend daily supplementation with quercetin. Quercetin supplements are often combined with resveratrol as they have complementary benefits. You may also find inflammation defense supplements with quercetin, resveratrol, curcumin, and other anti-inflammatory herbs combined.
Final Thoughts
Pancreatic cancer is responsible for 3 percent of cancers in the US. It is cancer that affects your pancreas. Since in the early stages, most people don’t have symptoms, early diagnosis can be difficult. Addressing root cause factors is critical to protect your health. I recommend that you follow my natural support strategies to improve your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.

Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




“located behind your stomach in the upper left abdomen.”
Wouldn’t that be: located upper RIGHT?
Hello Lorrie,
No, the liver is in the upper right quadrant. The pancreas is in the upper center and left quadrant of the abdomen.