 Irritable Bowel Syndrome: 8 Strategies to Heal Your Gut
Irritable Bowel Syndrome: 8 Strategies to Heal Your Gut
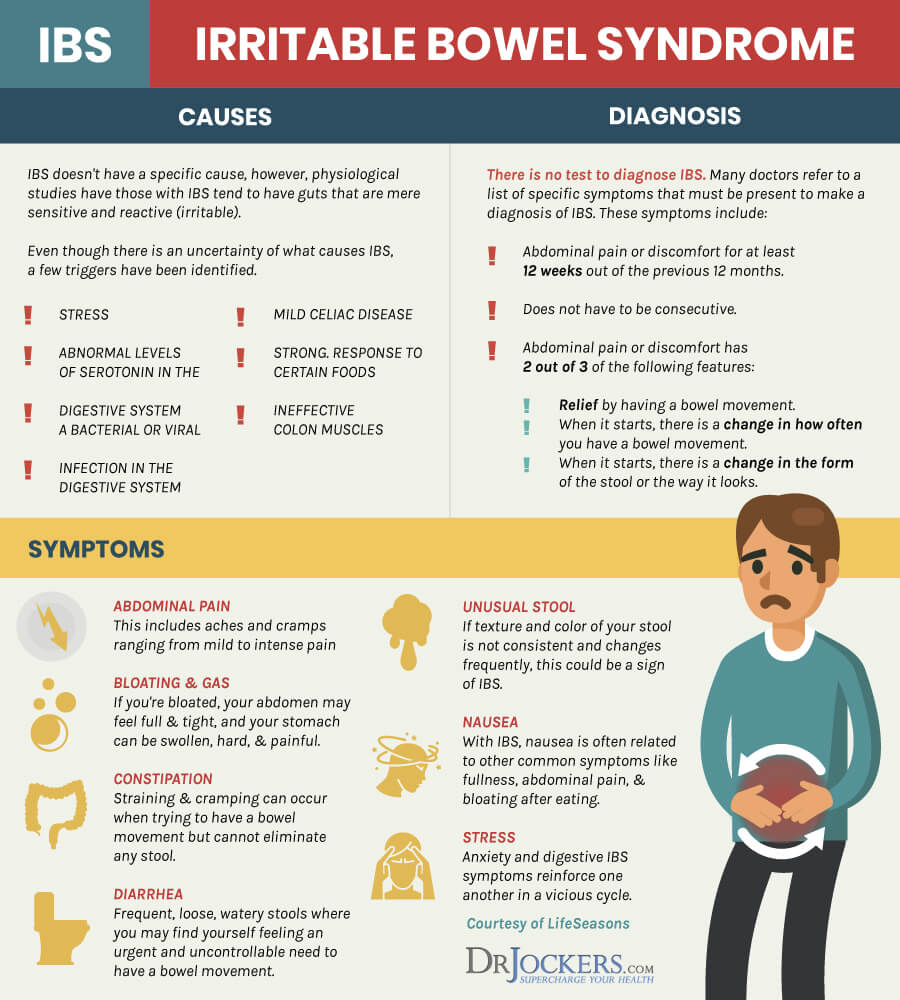
Irritable bowel syndrome (IBS) is a common disorder that affects millions of people. It is a cluster of symptoms that can substantially reduce your quality of life. There are many factors which contribute to the development of IBS including food sensitivities, gut infections, dysbiosis, and leaky gut. Stress is a major contributing factor to IBS.
If you are suffering with IBS, learning to recognize your triggers and addressing underlying causes can bring significant improvement. This article will discuss symptoms and causes of IBS, strategies for improving IBS, and ways to test your gut health and possible food triggers.
What is Irritable Bowel Syndrome?
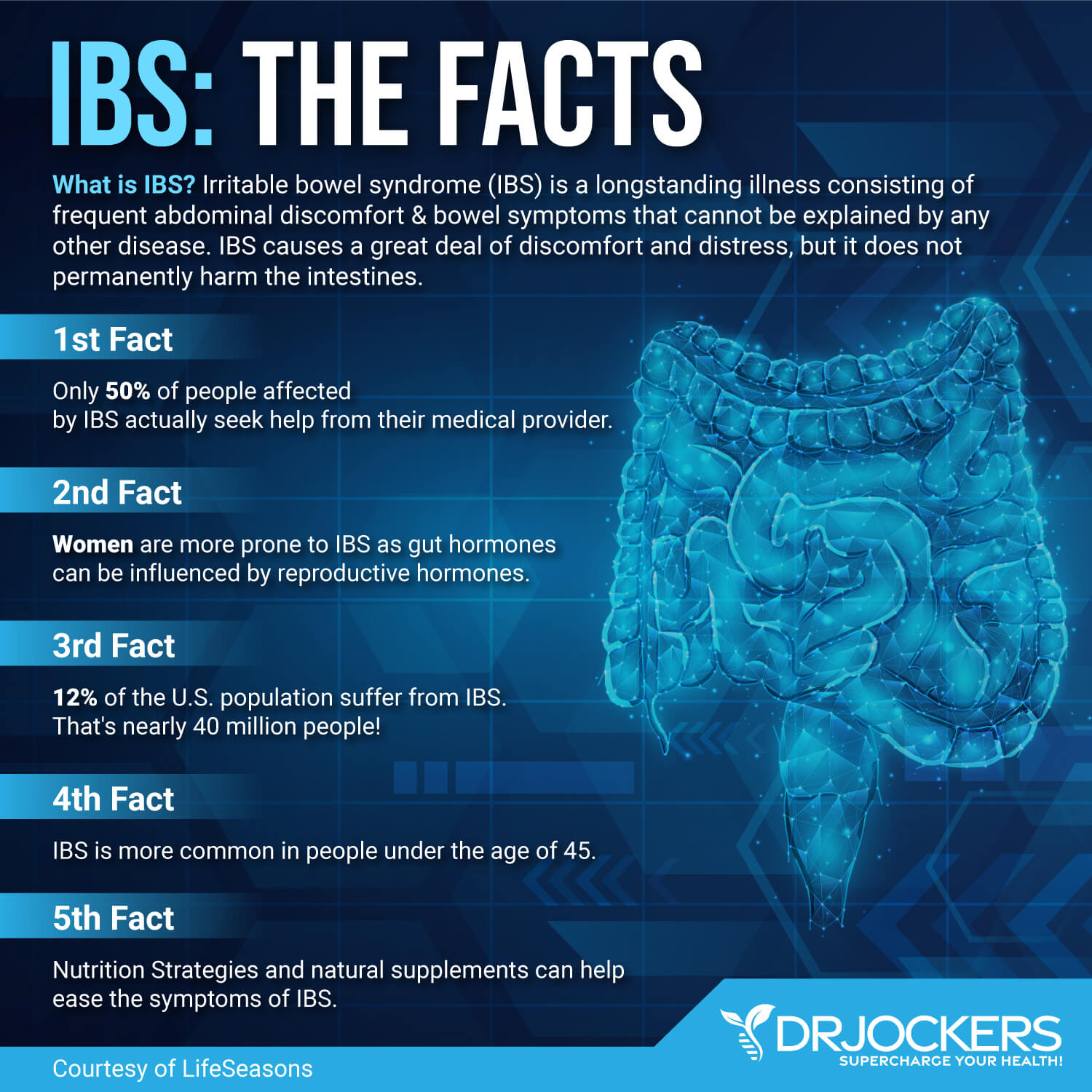
Irritable bowel syndrome (IBS) is the most common functional bowel disorder. It affects around 11% of people worldwide and 20% of people in the United States (1). As a syndrome, IBS is a group of symptoms that occur together. There is no visible disease, inflammation or injury to account for the symptoms.
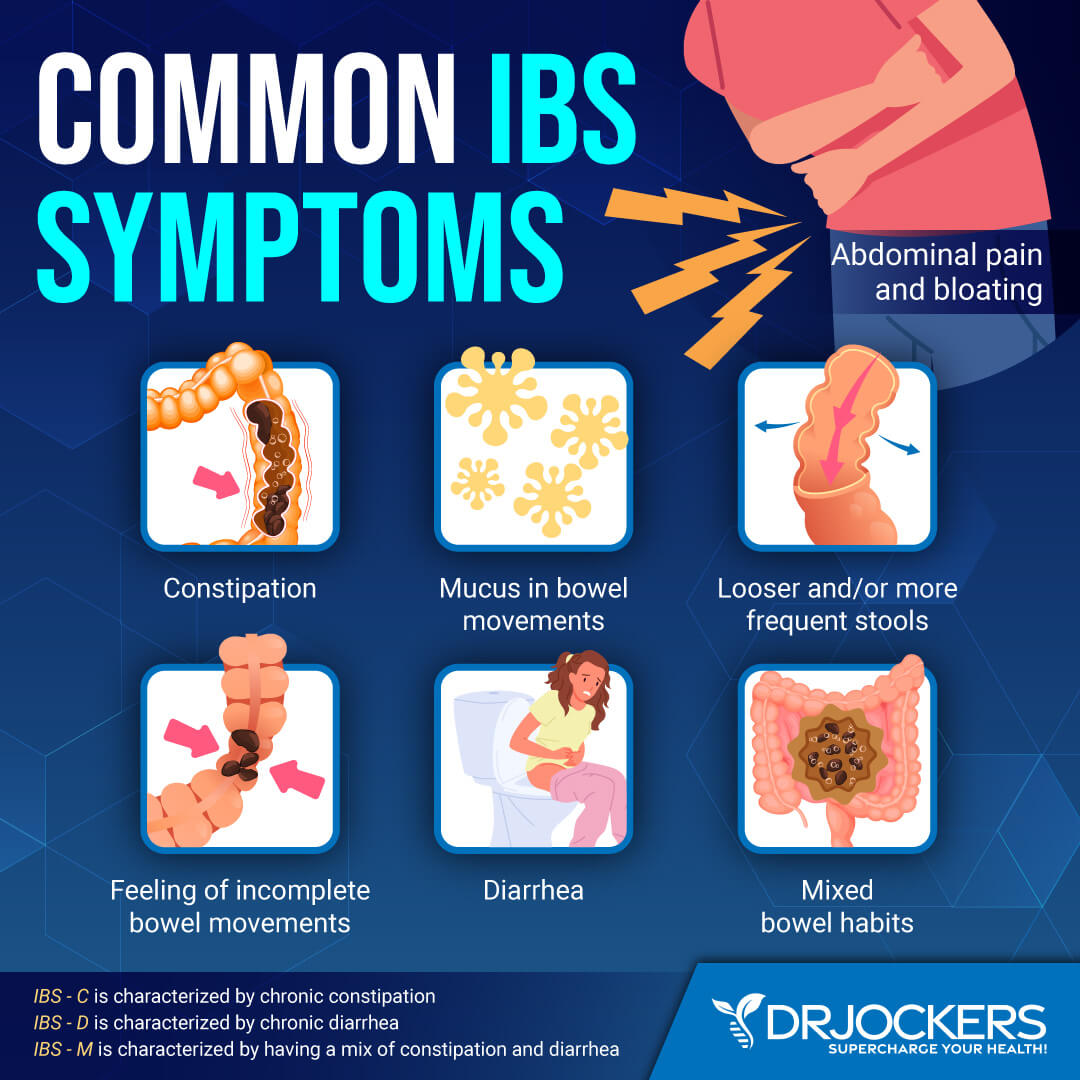
The signs and symptoms of IBS include:
- Abdominal pain, cramping, or bloating that may be relieved or partially relieved by passing a bowel movement
- Excess gas
- Diarrhea, constipation, or alternating diarrhea and constipation
- Mucus in the stool
Women are more likely than men to have IBS. IBS occurs in all age groups, but around half of people with IBS begin experiencing symptoms before they are 35 years old. Depression and anxiety often accompany IBS due to the gut-brain axis connection.
For many years, IBS was dismissed by conventional doctors as a psychosomatic disorder. Now recognized as a legitimate condition, doctors diagnose IBS when a person has recurrent abdominal pain at least three days per month in a three-month period associated with two or more of the following: improvement with bowel movement, onset associated with a change in stool frequency and/or consistency (1).
For most people, the signs and symptoms of IBS may be worse at times and improve or disappear at other times. Usually, the signs and symptoms of IBS are not severe and can be controlled with diet, lifestyle and stress management. However, some people do experience severe IBS symptoms.
Different Types of Irritable Bowel
IBS can show up in different ways, causing different symptoms from one person to another. There are four types of IBS depending on the type of bowel movement problems: constipation-predominant, diarrhea-predominant, mixed, and unsubtyped.
1. IBS-D
Around a third of people with IBS have diarrhea-predominant IBS. People with IBS-D typically experience frequent episodes of diarrhea with abdominal pain. This will include loose stools, frequent bowel movements, and feelings of urgency. Abdominal pain, gas and bloating, mucus in the stool, and a feeling of incomplete evacuation are common with IBS-D.
2. IBS-C
Constipation-predominant IBS (IBS -C) is a condition characterized by chronic constipation with abdominal pain. IBS-C affects approximately one-third of people with IBS.
With IBS-C, people experience hard or lumpy stools, need to strain during a bowel movement, and have fewer than three bowel movements in a week. Other common symptoms include abdominal pain, gas and bloating, a feeling of incomplete evacuation, and mucous in the stool, and a sensation of blockage in the anus and/or rectum.
3. IBS-M or IBS-A
IBS-M (mixed) or IBS-A (alternating) occurs when people have an alternating pattern of constipation and diarrhea. They may also experience the additional symptoms of IBS-D or IBS-C.
4. IBS-U
For people who do not fit into the above categories, they are classified as unsubtyped IBS, or IBS-U.
Major Causes of Irritable Bowel
While a specific cause of IBS is unknown, intestinal inflammation, poor diet, gut dysbiosis, food sensitivities, and gut infections may play a role. Stress and anxiety are also key factors which cause IBS.
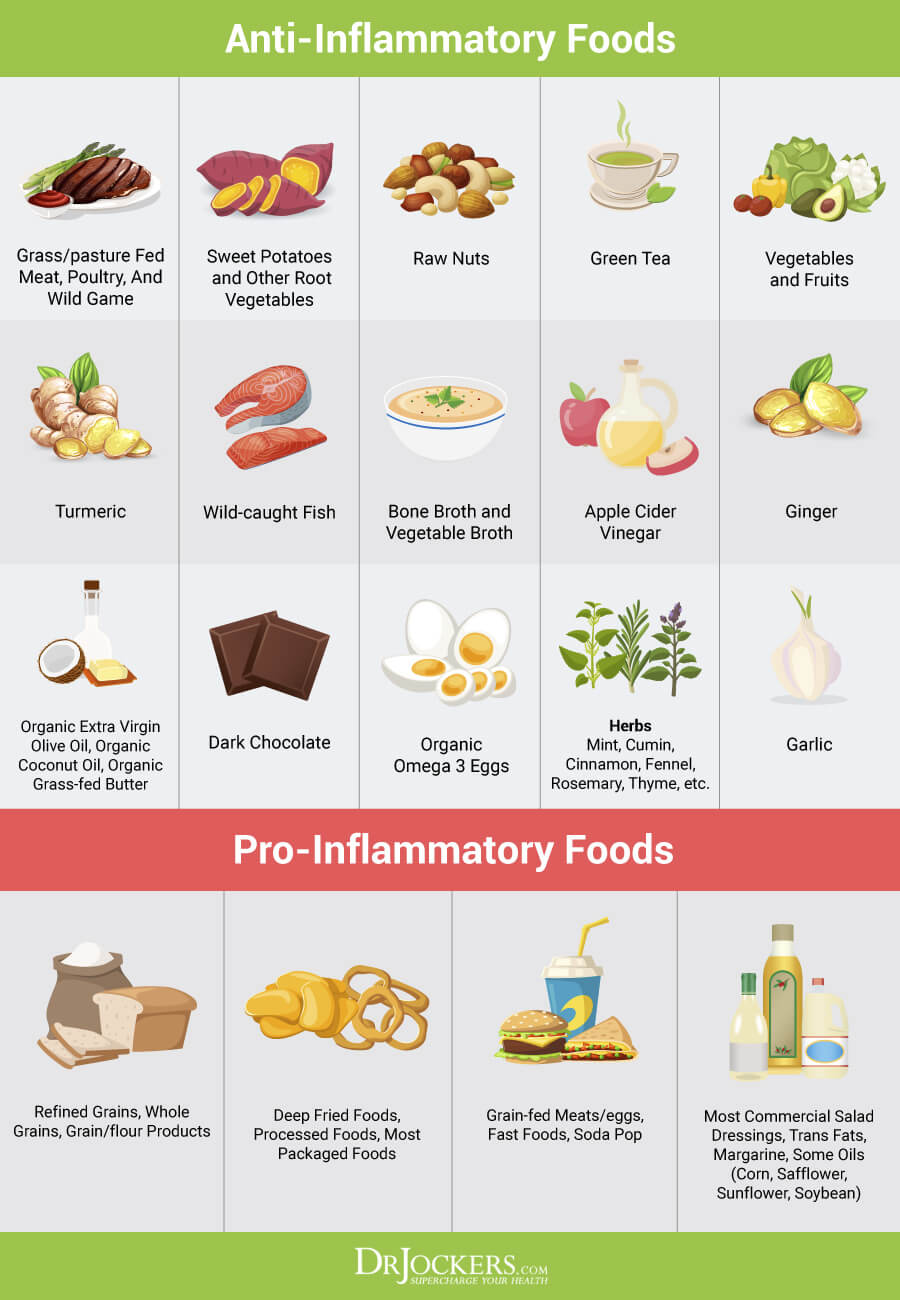
1. Poor Diet
Diet has a big impact on IBS symptoms. Eating a highly processed, standard American diet can initiate and worsen IBS symptoms. Pro-inflammatory foods such as refined sugars and starches, factory farmed meats, processed foods, and toxic oils activate the immune system and lead to inflammation.
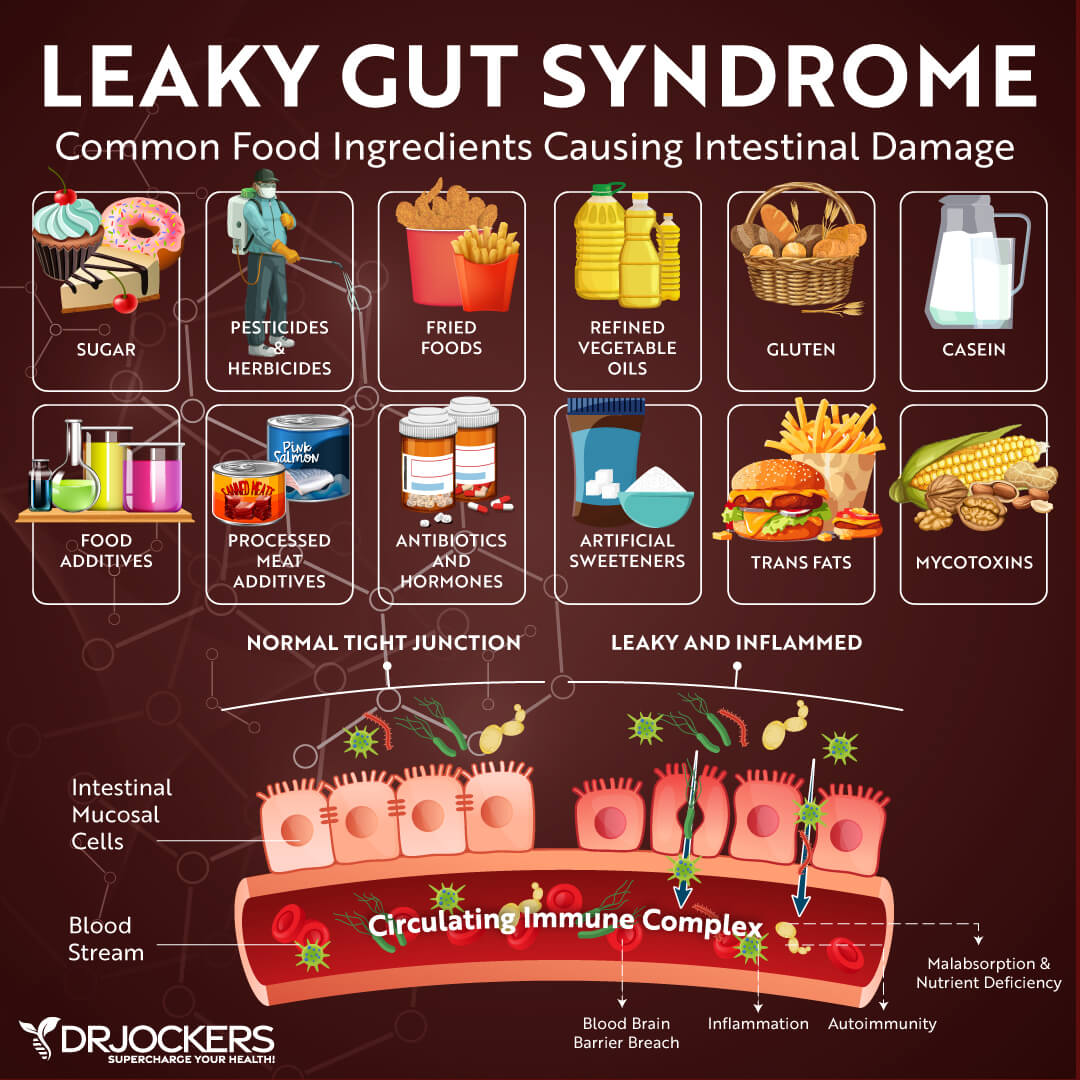
A poor diet damages the gut lining causing leaky gut syndrome (or intestinal permeability). Your gut lining houses the gut microbiome, aids in the absorption of nutrients, and has tight junctions to protect us from pathogens, toxins, and dietary antigens. Leaky gut syndrome occurs when the tight junctions in the gut lining become too large and abnormally permeable.
When a person has leaky gut, undigested food particles and toxins pass through the holes in the intestinal wall and into the bloodstream. This causes the immune system to overreact and leads to chronic inflammation, food sensitivities, autoimmunity, and reduced nutrient absorption. People with leaky gut often experience digestive issues such as gas, bloating, indigestion, and constipation.

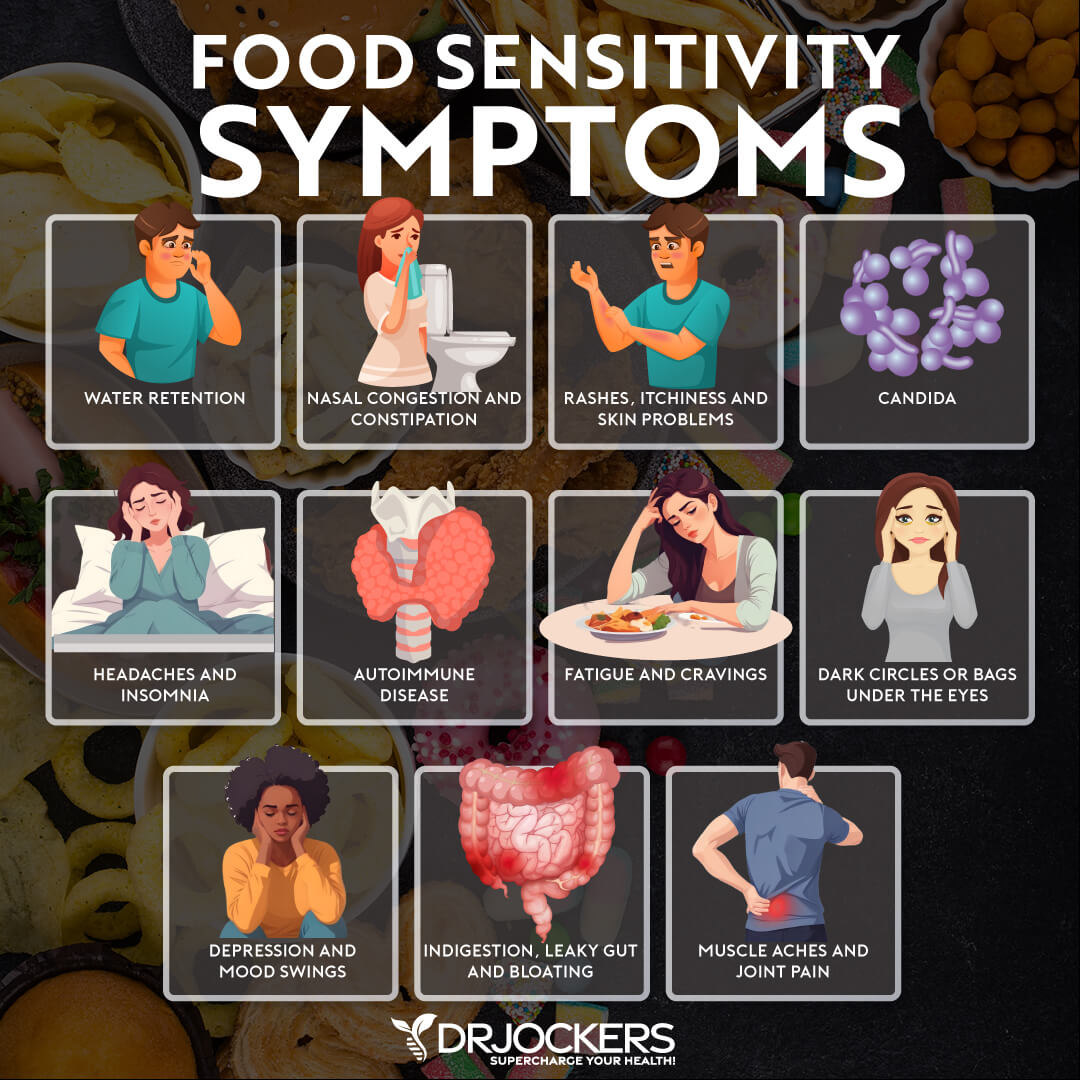
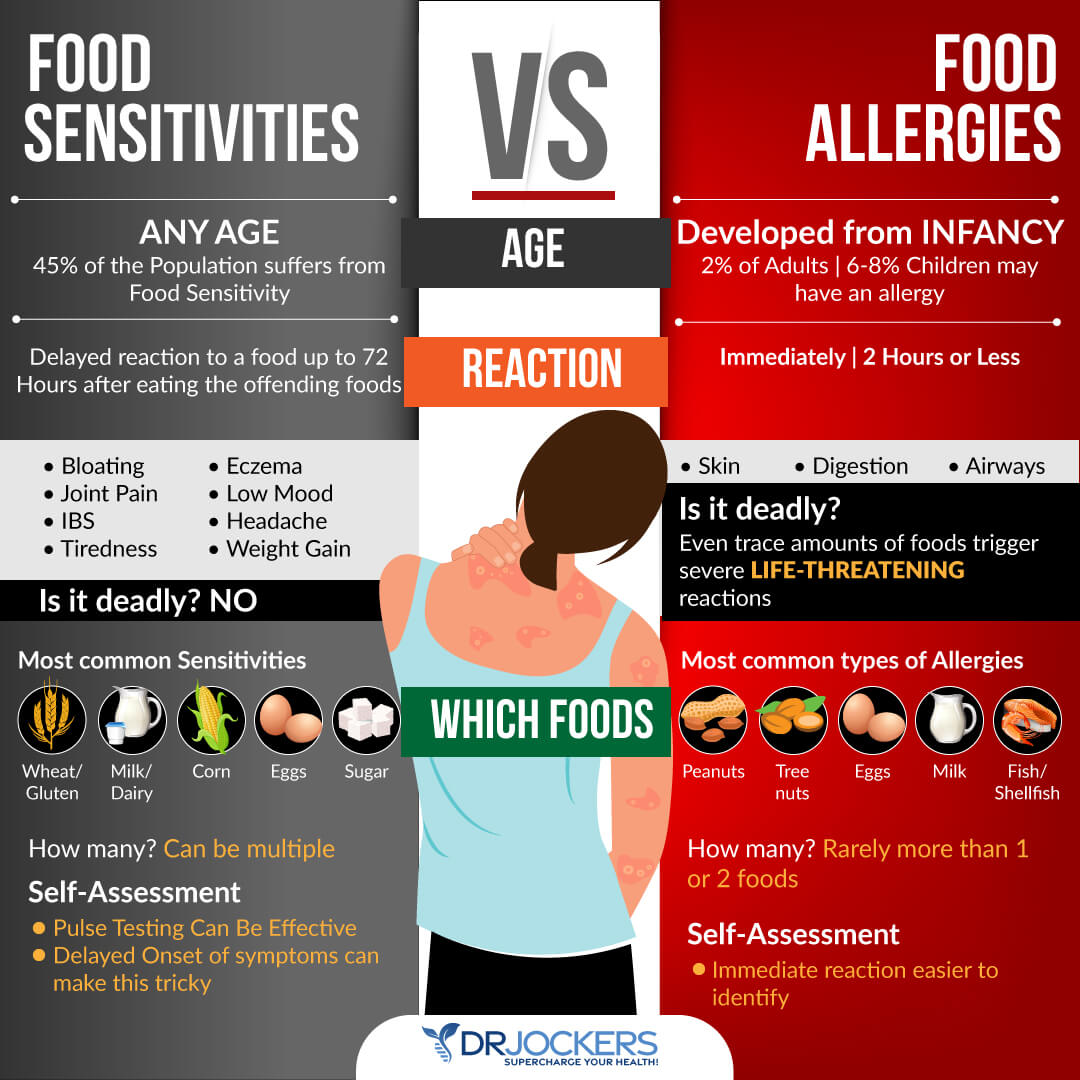
2. Food Sensitivities and Irritable Bowel
People with IBS often have one or more food sensitivities. A food sensitivity is an immune-mediated response to certain foods. When you have a food sensitivity, your immune system produces antibodies (or immunoglobulins) to the food. Food sensitivities are very common and affect 45-75% of individuals.
Gluten, dairy, corn, soy, nuts, eggs, and nightshades are common food sensitivities. If you are sensitive, repeated exposure to these foods inflames the gut lining causing intestinal permeability and digestive problems. This irritates the bowel and leads to IBS symptoms.
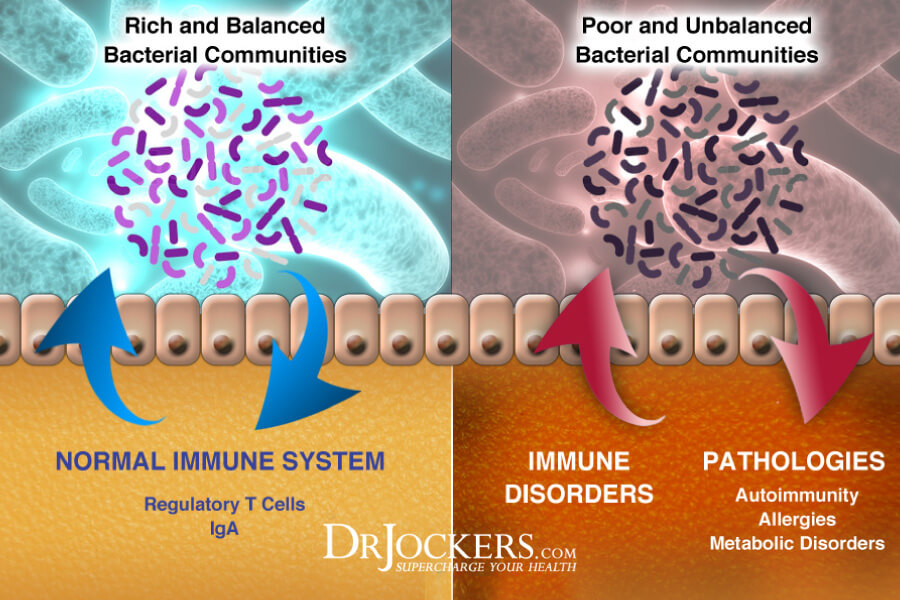
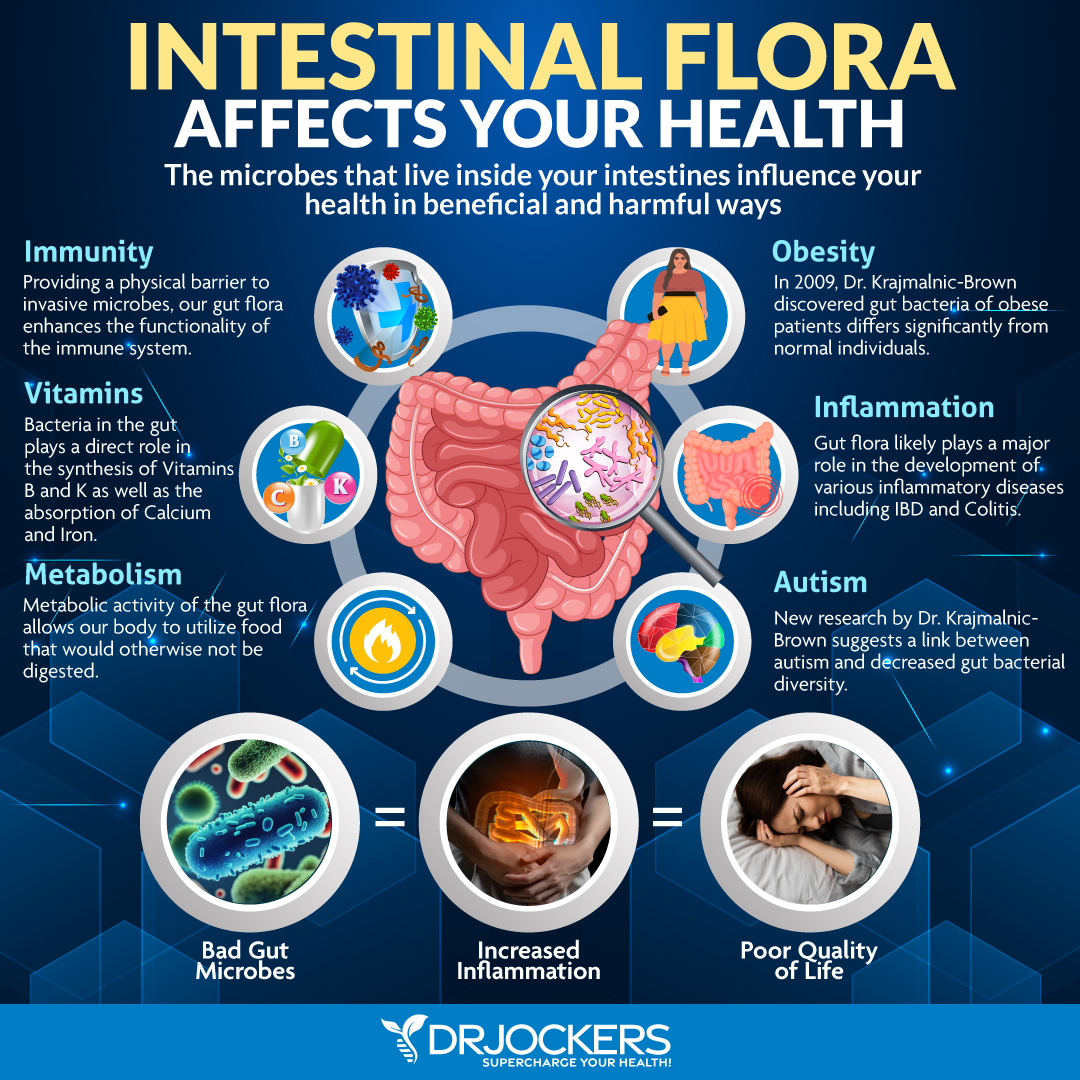
3. Imbalances in Gut Flora
Imbalances in the gut flora (or microbiome) have been linked to IBS symptoms. The gut microbiome is made up of trillions of microbes, ten times more than the number of human cells. The ideal ratio of beneficial to pathogenic microbes is around 85:15.
Unfortunately, most people have dysbiosis, an inverse ratio with bad bacteria outnumbering the good bacteria. Imbalances in the gut flora are linked to IBS and a number of diseases including obesity, Crohn’s disease, and colorectal cancer (2).
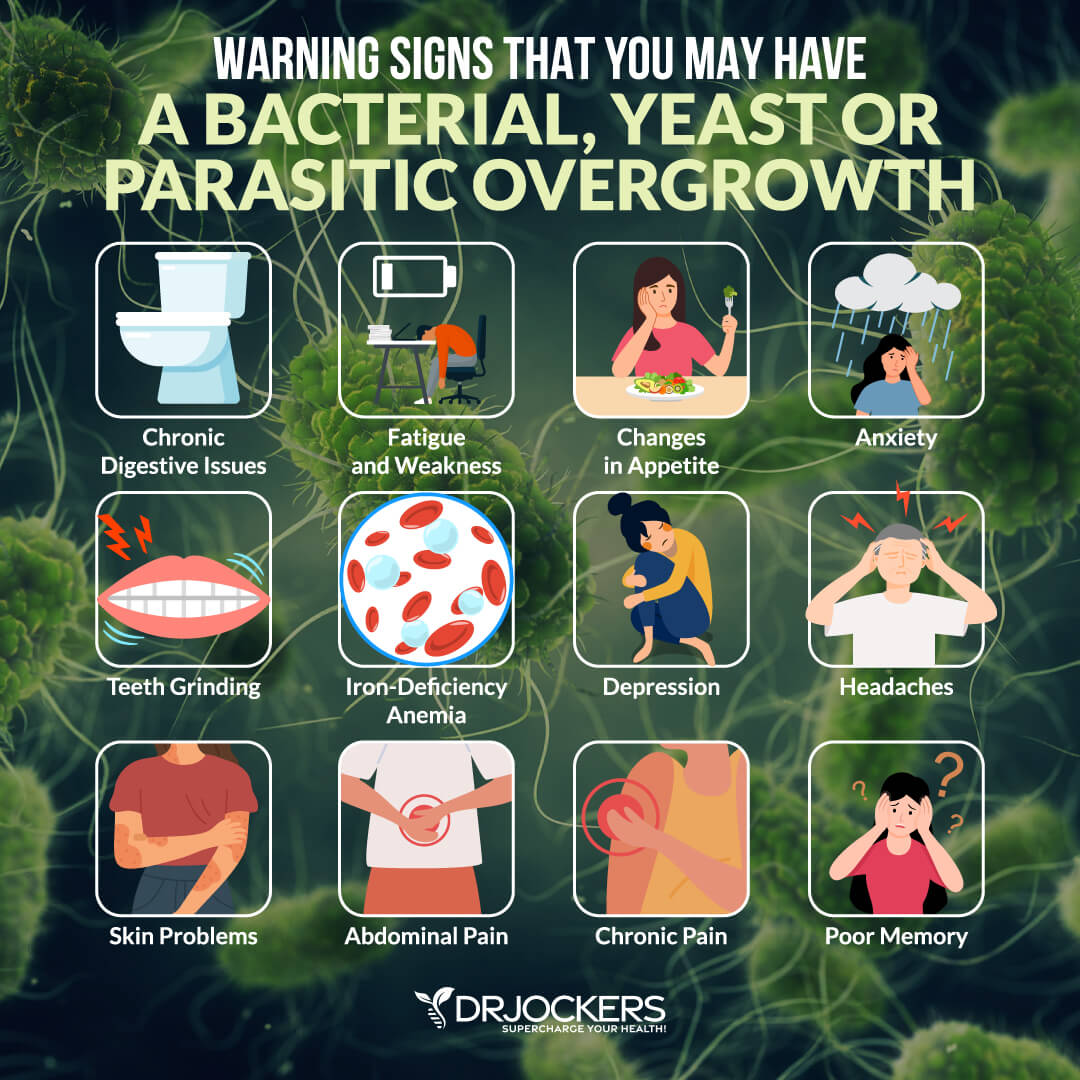
4. Gut Infections and Irritable Bowel
Our GI tracts are constantly exposed to pathogens including bacteria, viruses, parasites, and fungi. When our gut immune system is compromised, gut infections often result from these pathogens (3). These infections damage the gut, cause inflammation, and can trigger or exacerbate IBS.
Gastroenteritis is inflammation of the stomach and intestines typically resulting from bacterial toxins or viral infection. Infectious gastroenteritis is a significant risk factor in the development of IBS (4).
One of the most common gut infections linked to IBS is small intestinal bacterial overgrowth (SIBO). SIBO is present in at least one-third of people with IBS, and people with IBS are five times more likely to have SIBO (5). Parasites such as Blastocystis hominis, Dientamoeba fragilis, and Giardia are also linked to IBS (6).
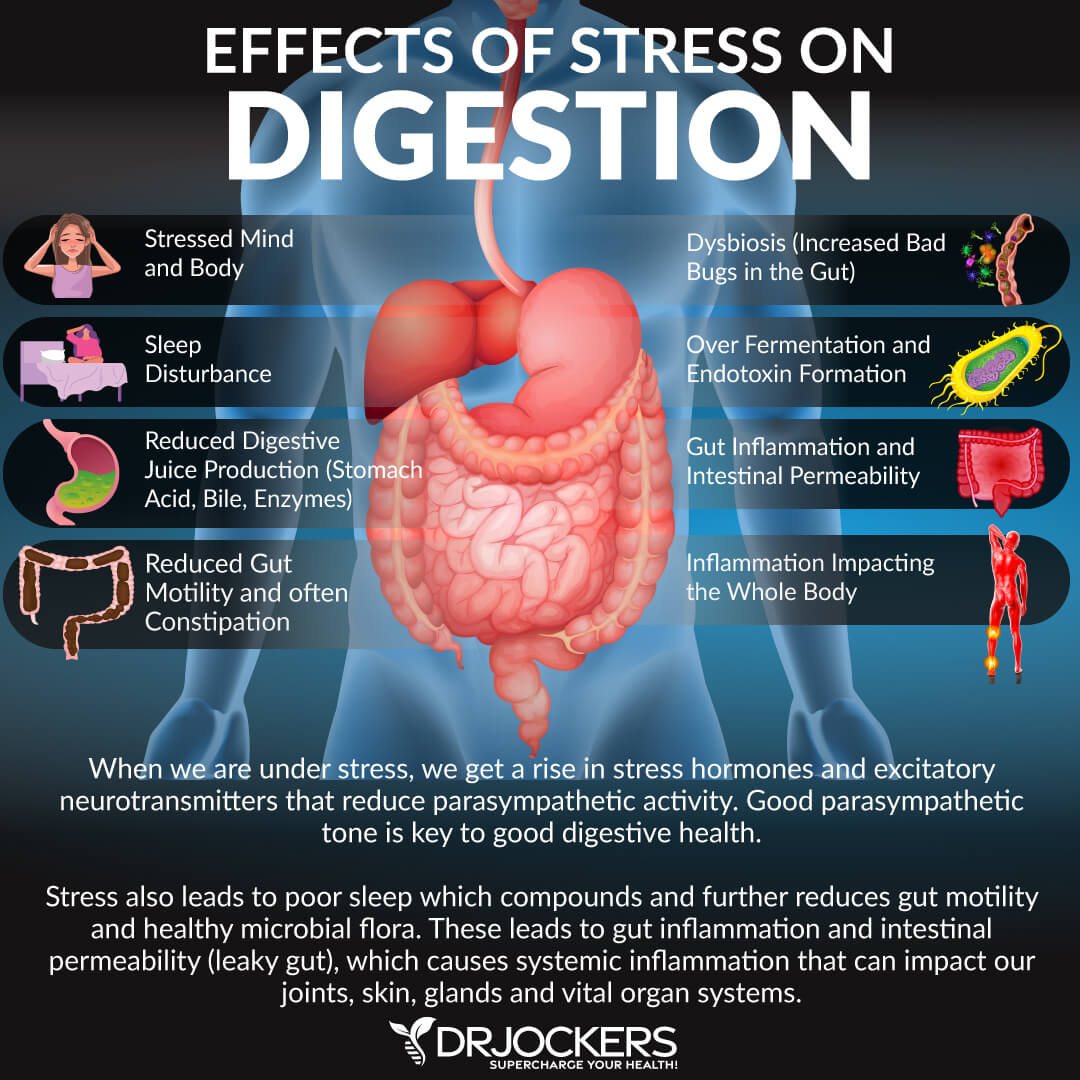
5. Chronic Stress and Irritable Bowel
Stress has a prominent role in the development and presentation of IBS symptoms (7). Up to 40% of people with IBS have increased anxiety.
Psychological and physical stressors have effects on gut function and gut-brain interactions. Stress can damage the gut by modulating key inflammatory pathways. It also decreases mucosal blood flow and thereby compromising the integrity of the gut mucosal barrier.
Stress causes bowel dysfunction in different ways, including through the HPA axis, the autonomic nervous system, or directly on the bowel itself (8). It activates the “fight or flight” response in the central nervous system which can slow down or even stop the digestive process as the body diverts its energy to face the perceived threat. Stress also alters the gut flora and increases intestinal permeability, which may lead to IBS symptoms.
IBS-D Quick Fix Protocol
If you are having an IBS flare up with diarrhea, this protocol may be helpful. If you want to learn more about diarrhea in general, then read this article.
1. Take Activated Charcoal
Activated charcoal is a powerful detoxifying remedy that can stop diarrhea. It is very absorbent and will bind to and eliminate toxins from the body.
For acute diarrhea, start with around 250 mg of activated charcoal for every 50 pounds of body weight. Take this amount of charcoal every 2 hours or so with and without meals and continue to take it and you may even double the dosage until the diarrhea stops.

2. Use Anti-Microbial Herbs
If your diarrhea is caused by gut infections, using an antimicrobial may be helpful. Finding a blend of botanical extracts with antimicrobial properties to help to reduce pathogenic bacteria, yeast, and parasites which create infections in your gut and may cause diarrhea.
I like using supplements with berberine, black walnut, wormwood, tribulus and clove. You can typically find supplements that combine a few of these or you. It is always best to start with a low dosage to make sure you don’t overwhelm your system and work your way up gradually.

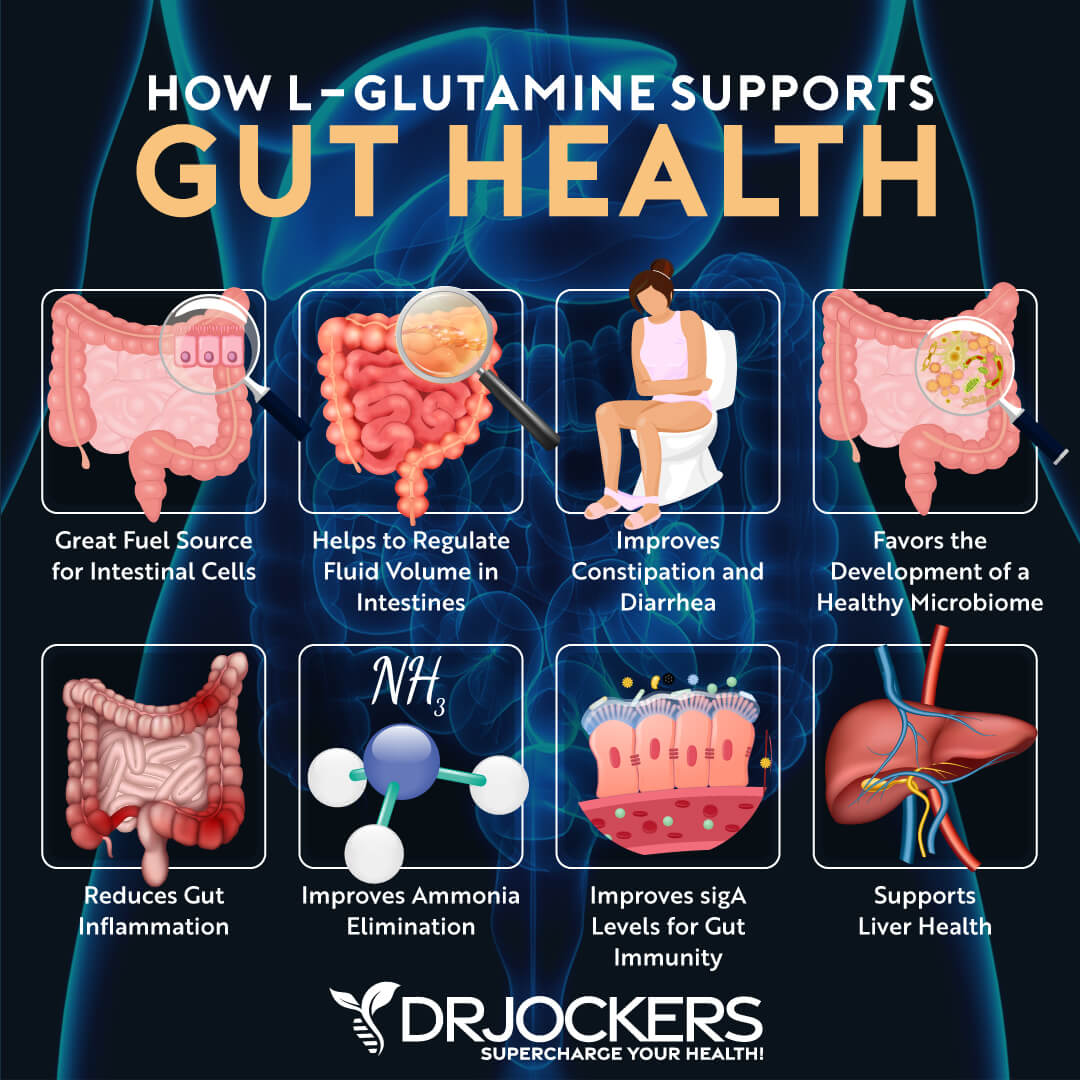
3. Use L-Glutamine:
Glutamine is the most abundant amino acid in the body and in the intestinal cells. It is the primary nutrient for the cells of the intestinal lining where it helps regulate cellular reproduction. Through this mechanism, glutamine helps prevent and rebuild a leaky gut, which is common in people with inflammatory and auto-immune conditions.
Glutamine also helps regulate cells by absorbing water across the junction between the small intestine and blood stream. This is a very important part of keeping the body from losing fluid and becoming dehydrated. When water is not absorbed back into the body diarrhea is the result. Glutamine has been shown to reduce the frequency and severity of diarrhea. I recommend using 1-2 scoops (4-8 grams) – 3 times daily in water or in broth until the diarrhea stops.
3. Close Ileocecal Valve
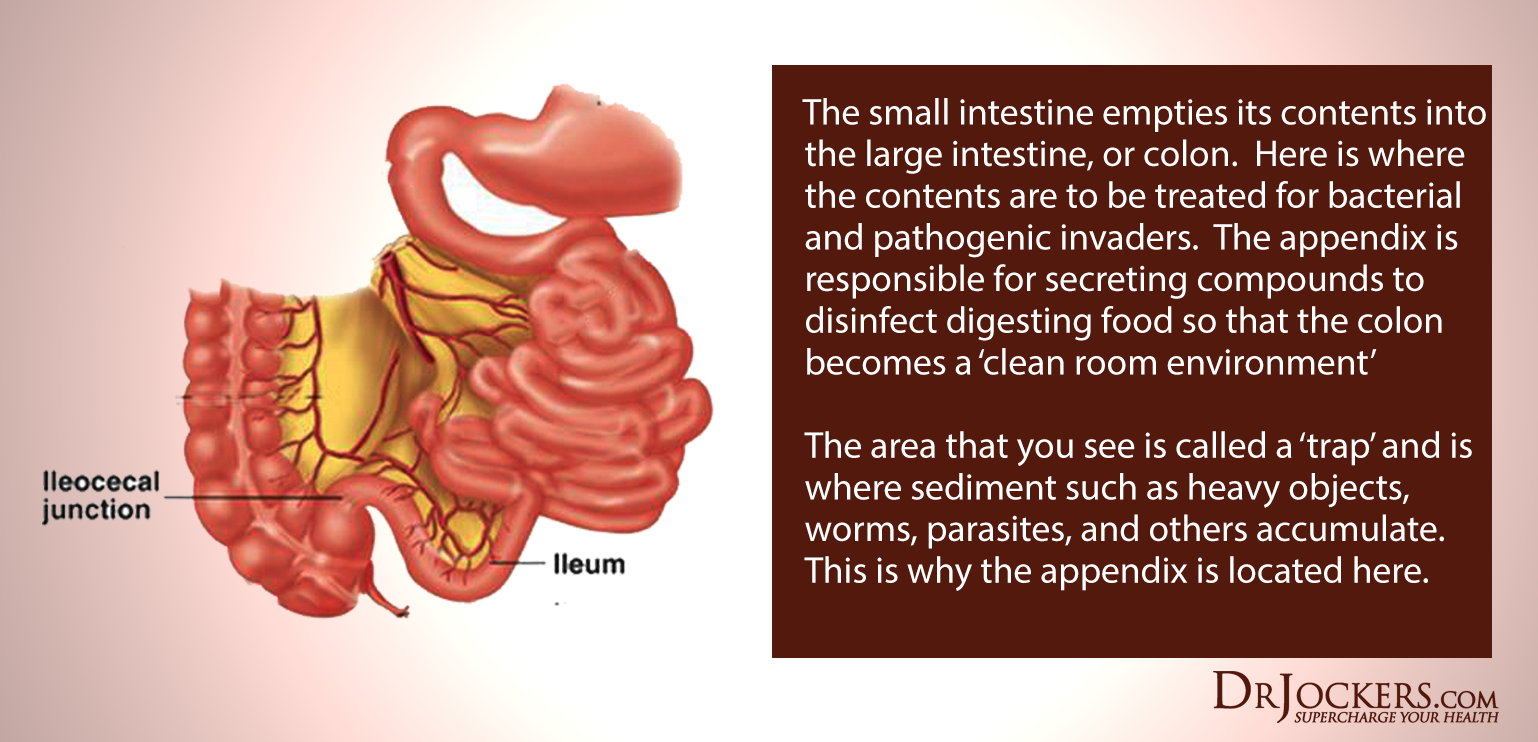
An open ileocecal valve will often result in SIBO or diarrhea. The ileocecal valve connects the large intestine to the small intestine and acts as a barrier between the two. It has the unique and important function of allowing each environment to support different temperatures, pH levels, microflora and digestive processes. The ileocecal valve also prevents harmful toxins and microbes from backing up into the small intestine.
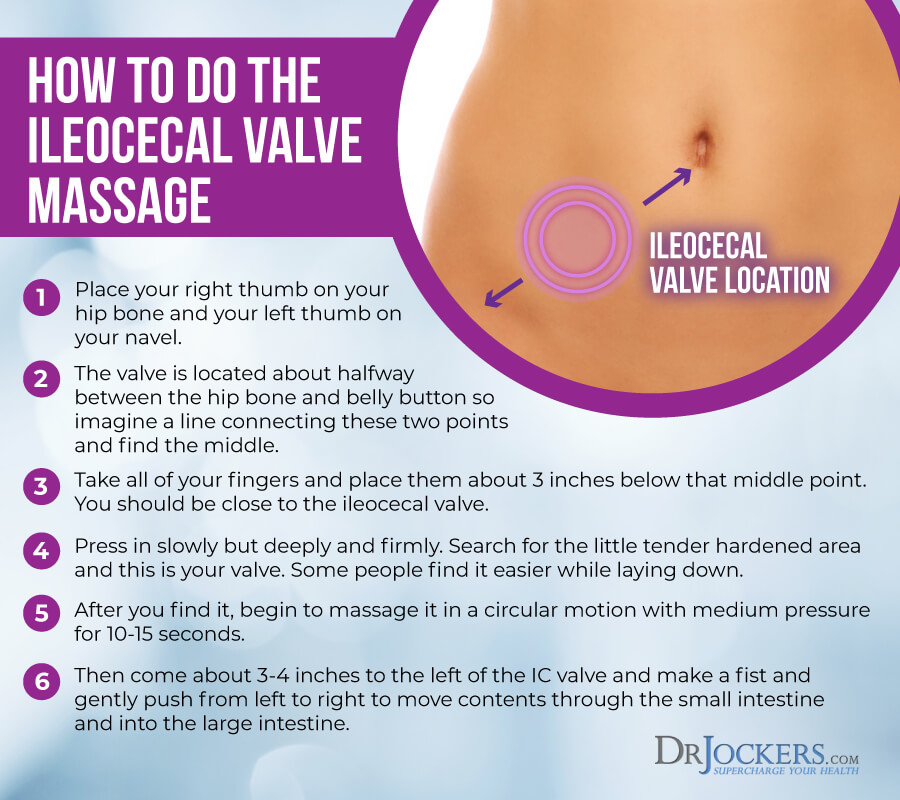
Problems occur when the ileocecal valve malfunctions and is stuck open or closed. To close this valve, you can try pushing it closed with your fingers or using an ice pack over the value for 15-20 minutes. You can learn more about the ileocecal valve here.
IBS-C Quick Fix Protocol
If your IBS symptoms include constipation, try this protocol. If you want to learn more about constipation in general, then read this article.
1. Oxy Powder or Bowel Mover
Oxy-Powder is a scientifically formulated, all-natural oxygen colon cleanser. It safely relieves bloating, irritation, and constipation. Oxy-Powder gently cleanses and detoxifies the whole digestive tract and supports the microbiome.
Another option for natural, gentle relief from constipation is Bowel Mover. This is an herbal based product that is specifically designed to promote digestive and detoxification support without causing cramping or dependency.
2. Open Ileocecal Valve
Constipation occurs when the ileocecal valve is stuck closed. Fecal matter and toxins are not able to get through to the large intestine and are absorbed by the small intestine.
This is a major cause of SIBO. To open the ileocecal valve, you can massage the valve to help move contents from the small intestine to the large intestine.
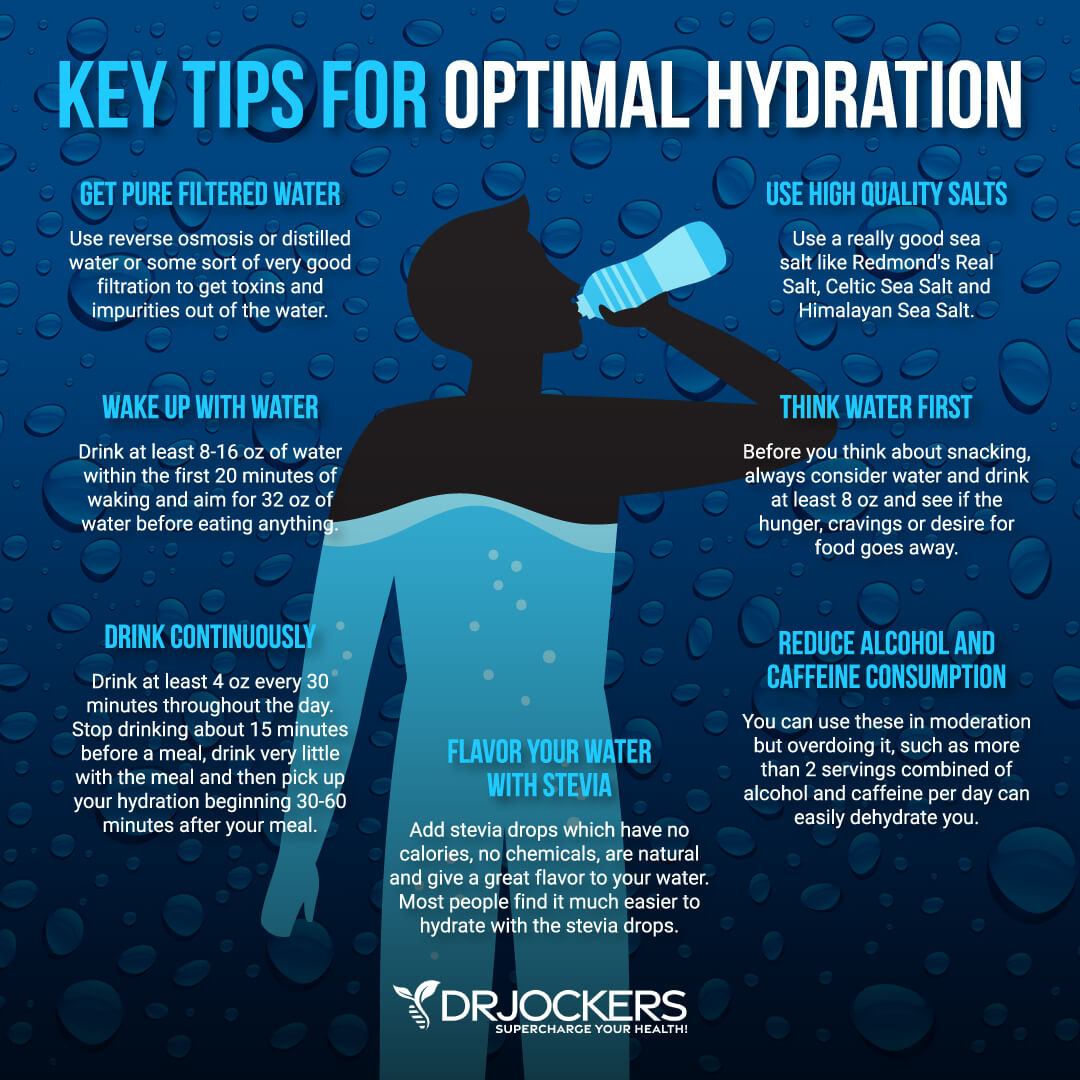
3. Optimal Hydration
Super hydrating with clean, filtered water helps to improve bowel motility. You need plenty of water to remove waste and toxins through your stool. To be well hydrated, you should consume at least one half and up to your full body weight in ounces of water every day.
Strategies to Heal Your Gut
To improve your digestive symptoms related to IBS, it is important to follow an anti-inflammatory diet, reduce stress, use targeted supplements, and implement other healing strategies. While these aren’t FDA approved to prevent, mitigate, treat or cure IBS, they can be very beneficial.
1. IBS Anti-Inflammatory Nutrition Plan
One of the most effective strategies for relieving IBS symptoms is to consume an anti-inflammatory diet. You should remove foods that promote inflammation and damage the gut lining and replace them with healing foods.
The most important foods to avoid are refined sugars, processed foods, vegetable oils, meat and dairy from conventionally-raised animals, and farmed fish. These foods contain chemicals, trans-fats, and other toxic ingredients which are highly inflammatory, create extra acidity in the tissues, and damage the gut.
For IBS, be sure to eat whole, unprocessed foods: clean protein, organic vegetables, and healthy fats. Healthy fats are found in coconut, olives, avocados, and their oils, and in grass-fed butter and ghee. Clean protein sources are grass-fed meats, pasture-raised, organic chicken and eggs, and wild-caught salmon.
It is important to eat foods that are easy to digest. Non-starchy, organic cooked vegetables are great to include on an IBS diet. Bone broth and probiotic foods like kefir may also be helpful.
How you eat is also important. Eat smaller meals which will not overwhelm your digestive system. It is important to chew your food well and eat in a relaxing environment.
2. Heal Leaky Gut
To heal from IBS, it is critical to heal your gut. Reducing stress on the gut with liquid nutrition and fasting, along with targeted supplements to repair the gut, can be very effective.
Intermittent fasting is going longer periods of time, such as 12-14 hours without eating. This is a good starting point for anyone with leaky gut. Water or bone broth fasting are additional strategies that can be very helpful.
Using liquid nutrition for is great for stimulating the digestive process, increasing nutrient absorption, and improving gut health. Liquid nutrition does not require as much energy to digest, so your body can focus on healing and repair.
For mucosal support, I like nutrients like L-glutamine, aloe vera, licorice root, vitamin C, colostrum and dairy-free, bovine serum-derived (BSD) immunoglobulin concentrate. These all act to support gut barrier function, improve immunity, and decrease inflammation in the gut. The immunoglobulins in colostrum and BSD immunoglobulin concentrate work to bind to environmental toxins, neutralizes pathogens, and improve gut mucosal immunoglobulin sIgA levels.
Getting a good quality bone broth or collagen protein, which are both rich in the amino acids glycine and glutamine, can be very helpful for healing leaky gut. These amino acids seal the holes in the gut by healing damaged cells and building new tissue. Collagen also makes up the villi, small finger-like structures on the intestinal wall and assists with water absorption in the intestines.
3. Identify and Remove Food Sensitivities
To heal from IBS, it is important to identify and remove foods from your diet that cause an overactive immune response. Food elimination based on IgG antibodies is effective in reducing IBS symptoms (9).
Gluten is one of the most common food sensitivities. A gluten-free diet has been found to improve IBS symptoms and treatment outcomes (10).
Food sensitivities can be hard to identify. This is because symptoms of food sensitivities are usually delayed up to 72 hours after consuming the offending food. For information about different methods of testing for food sensitivities, check out this article.
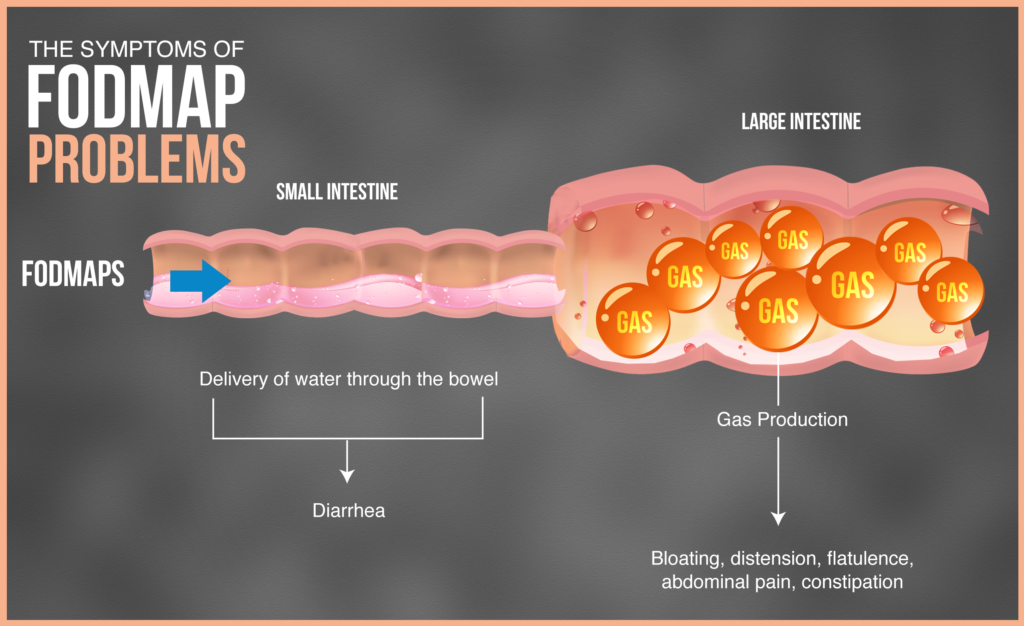
4. Consider a Low-FODMAPs Diet
Reducing fermentable carbohydrates (FODMAPs) may reduce your IBS symptoms. FODMAPs is an acronym for Fermentable Oligo, Di- and Monosaccharides and Polyols. FODMAPs include fructose, glucose, galactans, polyols, and lactose. These foods include cheeses, many fruits, certain vegetables, legumes, and other foods.
Foods high in FODMAPs are fermentable sugar-based carbohydrates. In some individuals, these normally healthy foods are poorly absorbed in the small intestines. When they reach the large intestine, they are fermented by bacteria and cause many digestive symptoms.
Studies show that a diet low in FODMAPs may significantly reduce symptoms and improve quality of life for people with IBS (11, 12). With IBS, I have found that some individuals do better on a moderate to higher FODMAP diet while others do better on a low-FODMAP diet. So you have to experiment and see which works better for you.
For information and guidance on how to implement a low FODMAPs diet for digestive health, read this article.
5. Address Gut Infections
As discussed above, gut infections result from a variety of pathogens that enter through the GI tract (3). It is important to address any gut infections from bacteria, viruses, or parasites which may be contributing to your IBS. This will also help to reestablish a healthy microbial balance and strengthen the gut lining.
A powerful supplement to include in an antimicrobial protocol with a blend of botanical extracts with antimicrobial properties. These herbs help to reduce pathogenic bacteria, yeast, and parasites, support the body’s immune response, and promote mucosal and microbial health. You can do a PCR stool test to look for the presence of specific infectious microbes in your gut and the function of your digestive tract. My team uses the GI MAP Stool Analysis for this.
6. Reduce Stress and Improve Sleep
With chronic stress being major contributor to IBS, it is critical to reduce and manage stress. Prioritizing good sleep is also essential to heal from IBS.
Two of the most effective strategies to reduce stress and optimize sleep are implementing a healing diet and balancing your blood sugar levels. Grounding, deep breathing exercises, sunlight exposure, Epsom salt baths, and dry brushing are additional stress-relieving strategies.
Poor sleep quality is linked to upper and lower GI symptoms (13). To improve sleep, it is important to make sleep a priority. This includes keeping a regular sleep schedule and practicing healthy bedtime habits. Be sure to get sunlight during the day, avoid artificial light and EMFs, black out your room with blackout curtains or using a sleep mask, and be smart about caffeine intake. These factors play a huge role in overall sleep quality.
Supplementing with adaptogenic herbs such as ashwagandha, holy basil, rhodiola and ginseng can be very helpful to balance stress hormones. Most individuals with Celiac need more magnesium and that plays an important role in reducing anxiety and improving sleep quality.

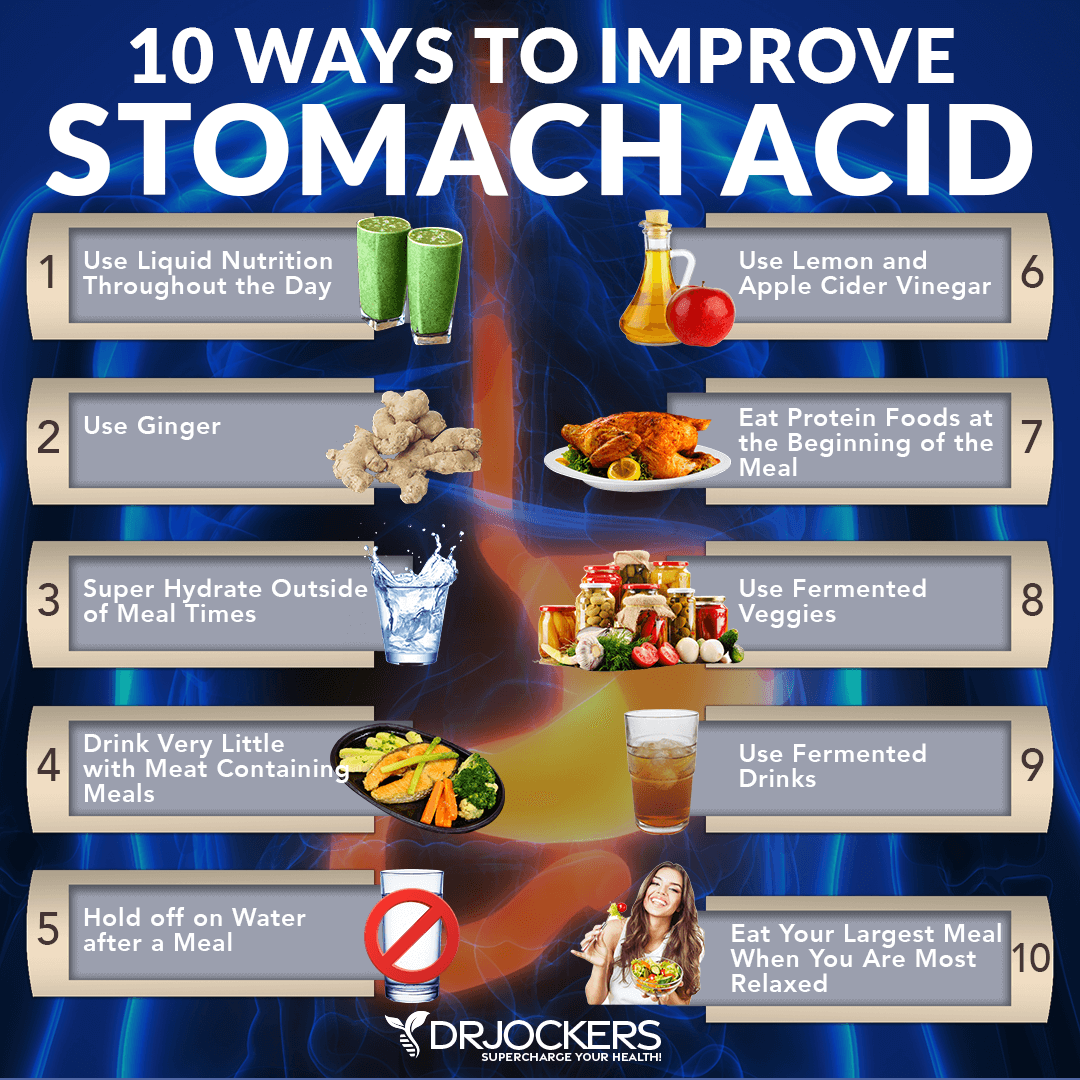
7. Support Stomach Acid and Digestive Enzymes
Many people with digestive issues have low stomach acid and insufficient digestive enzyme levels. Adequate levels of both are necessary for proper digestion and nutrient absorption. If levels are low, diarrhea, indigestion, bloating, nutrient deficiencies, and multiple food sensitivities may occur.
You can improve stomach acid levels by consuming liquid nutrition during the day with at least half of your meals in an easily digestible form. Be sure to hydrate outside of meals because drinking water with or right after a meal will dilute your digestive juices.
Eat your protein first, chew each bite many times, and eat in a relaxing environment. Squeezing fresh lemon juice or apple cider vinegar on meat and vegetables can help pre-metabolize the food. You can stimulate digestive juices with ginger, fermented foods (such as kimchi and sauerkraut), and fermented drinks (like coconut kefir).
Supplementation with hydrochloric acid may be necessary for individuals with low stomach acid. Look for products with betaine HCL, pepsin, l-glutamic acid, ox bile and gentian root to support gastric acidity, digestion and normal gastrointestinal flora.
For people with insufficient digestive enzymes, taking full digestive enzyme complex with meals may be very beneficial. Digestive enzymes help to reduce stress on the digestive system, improve the digestion of food and absorption of nutrients, reduce inflammation in the gut, and improve digestive issues.
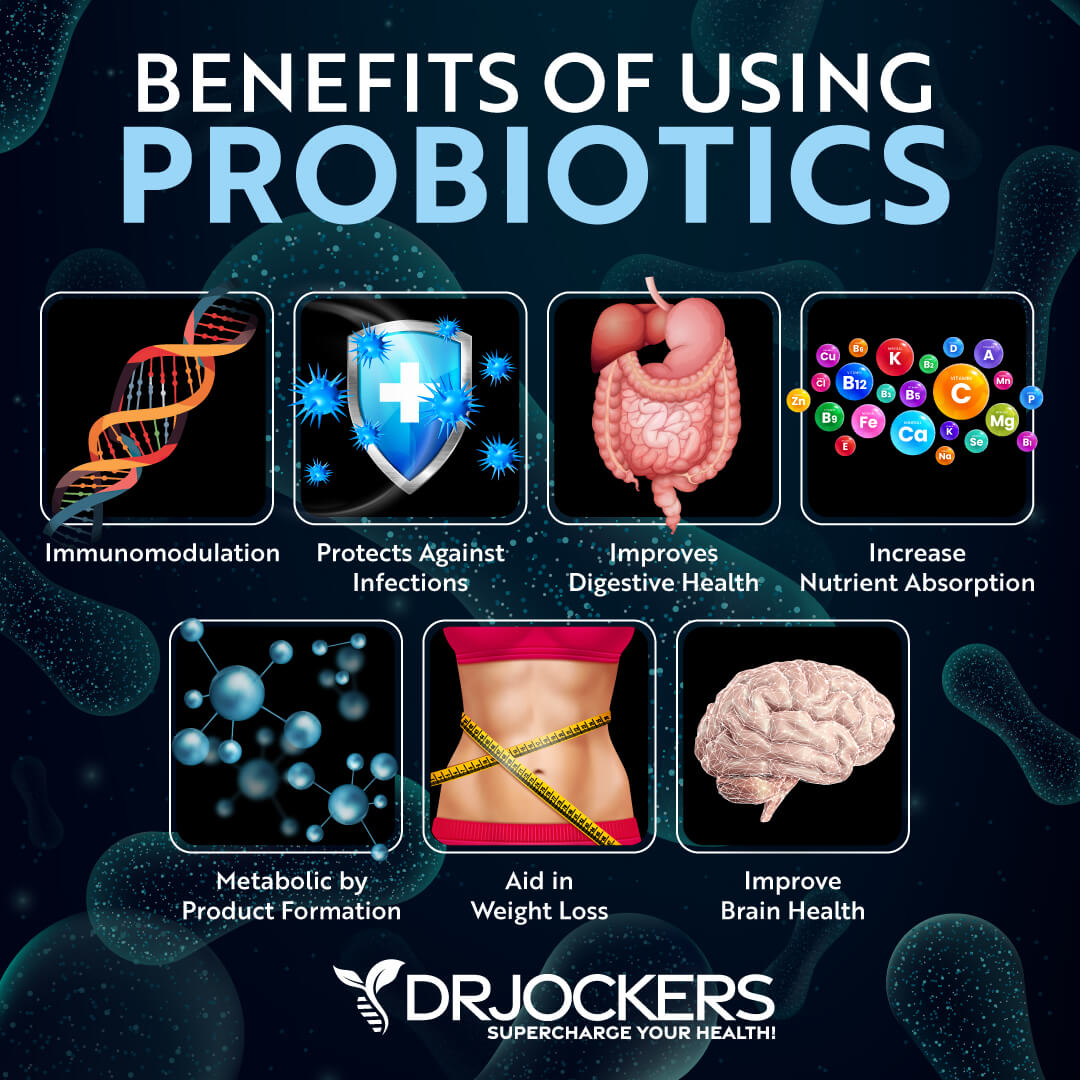
8. Gut Flora
Improving the microbial balance in your gut is very important to heal from IBS. You can support proper diversity of your gut flora with probiotics.
Probiotics are beneficial microorganisms (bacteria and yeasts) that are similar to the microorganisms that naturally live in our bodies. They support digestive health in many ways (14). Probiotics have been extensively studied as a treatment option for gastrointestinal diseases and have been shown to be an effective therapy in IBS patients (15).
There are 4 main categories of probiotics: food based, spore-forming soil based, probiotic yeast, and combination probiotics. Multi-strain probiotics at a concentration of 10 billion CFUs a day or less, have been shown to best improve abdominal pain, global symptoms, and quality of life for people with IBS (16). For more information on the benefits and categories of probiotics along with suggested protocols, check out this article.
Testing for Underlying Causes of Irritable Bowel
If you are suffering with IBS, stool testing and food sensitivity testing can reveal valuable insight as to the root causes.
1. GI-MAP™ DNA Stool Analysis
The GI-MAP is the most thorough stool test on the market. It is a comprehensive stool analysis that identifies the presence of multiple pathogenic microorganisms.
The GI-MAP is the only FDA-approved DNA test for gastrointestinal microbes and pathogens available. The GI Map tests for parasites (protozoa and worms). Candida, fungi, opportunistic and normal bacteria, H. pylori, viral pathogens, potential autoimmune triggers, and viruses.
The GI Map reveals the overall health of your gut with digestive, gastrointestinal, Secretory and Anti-gliadin IgA (immune response), and calprotectin (inflammation) markers. For more information on the GI Map and a sample report, you can look here.
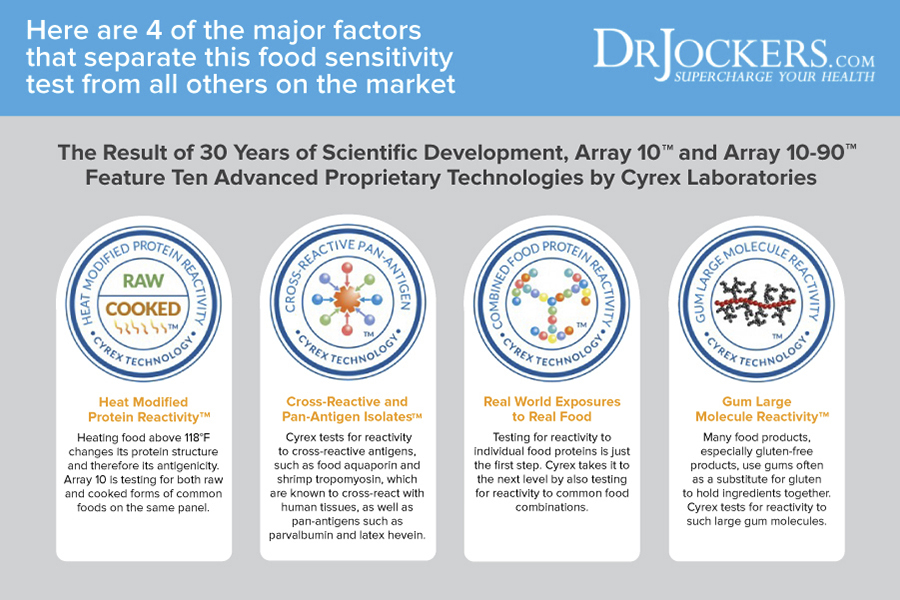
2. Cyrex Array 10-90X
A food sensitivity test can help determine which foods are contributing to IBS symptoms. The Cyrex Array 10-90X is the gold standard in food sensitivity testing. It is one of the best food sensitivity tests on the market.
The Cyrex Array 10-90X is a dual-antibody test, evaluating both IgG and IgA antibodies. It analyzes 180 cooked, raw, and modified foods, depending on how the foods are usually consumed. The Array 10 tests for reactivity to common food combinations, meat glues, large gum molecules, artificial food colors, small-molecule chemicals, and oil proteins. It is a comprehensive and reliable food sensitivity test that can provide valuable insight for anyone with gastrointestinal symptoms.
Final Thoughts on Irritable Bowel
IBS is a common disorder that can be unpredictable and varies from one person to the next. It is important to determine the underlying causes and unique factors that trigger your individual IBS symptoms. Then you can customize your diet and implement natural support strategies to heal your gut.
Testing can be extremely valuable in determining the health of your gut and the root cause of your symptoms. This can expedite the healing process. For a do-it-yourself home program to heal your gut, check out my Digestive Health Restoration Program here.
If you are looking for help improving your health, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




I want to buy a probiotic for my gas, gastritis, irritable bowel problems.
But I want to know if a cold packing is not necessary to converge the good bacteria, I live in the Dominican Republic.
Hey Carlos, Some probiotic supplements do need to be cold packed but many are available that are shelf stable and require no need for refrigeration! Here is a good article on how to decide which one is right for you!
No you can find many that are encased in a way that keeps them alive without refrigeration. We offer several great ones in our online store here: https://store.drjockers.com/search?type=product&q=probiotics
I did just have Covid with pneumonia. It hit hard. I am obese and was border-line diabetic which I know made this be so much worse. I knew I should be working on these problems, but had gotten lazy. As a result of being so sick I have lost over 30 pounds in a month and my blood glucose has been near or just below 100. Basically I haven’t felt like eating so fasting was a no-brainer. I do periodic detoxing using Revelation Health’s “True Cellular Detox” plan. It has literally saved my life. My problem now is in the midst of covid and post covid my body (maybe because of x-rays, Ct scans, and fast weight loss) has decided it needs to detox. So I’ve been using the Brain Phase detox phase and feeling horrible! My gut is so messed up from both detoxification and post covid healing crisis. I didn’t think I should be doing a total fast but have been following your bone broth fasting strategy and green juices for about a week , trying to heal my gut. I have never had gut issues before, but now it is just awful. Diarrhea, nausea with some vomiting, lack of appetite. Sorry this is so long but I need advice. How should I proceed?How should I eat? I’ve read a lot of people are having gut issues post covid. But with detoxing thrown into the mix, I don’t know what to do. I’m not choosing to detox. My body is doing it and I’m just assisting it with the detox plan. I’m a praying believer. I’m praying for Gods grace and guidance. Thank you for any advice you can give.
So sorry to hear this! I would be sure to work with a health care practitioner to get to the root cause here. Praying for you!
I would like to comment on the L-glutamine. I am also diagnosed with epilepsy. Epilepsy medications work by lowering L-glutamine in the brain. There is no guarantee that some of that L-glutamine will not get into your brain, and when it does, it will excite the nerves and cause seizures. It is an excitatory neurotransmitter. You want GABA, the calming one, higher when you have epilepsy. Do not use L-glutamine if you are also diagnosed with epilepsy; You will have more seizures. I wish more websites would warn about this when talking about how L-glutamine repairs the gut lining.
Thanks for sharing Crystal!
I just want to thank you for such a comprehensive and informative article. It’s one of the very few times I feel like I don’t need to jump from website to website to find all the answers I’m looking for! Much, much appreciated 😊
Glad to hear this was very helpful for you!