Lipoprotein a Lp (a) and Heart Disease:
The twenty-first century has seen a significant rise in research looking deeper into cholesterol subparticles. Lipoprotein (a) or Lp(a) is a small LDL-like particle that has emerged as a major risk factor in heart disease, stroke, and other cardiovascular problems (1, 2, 3).
Studies have shown that higher Lp(a) levels in the blood are directly correlated with more plaque in the arteries and a greater risk of cardiovascular disease. There are natural strategies to utilize to lower Lp(a) levels.
What is Lipoprotein Lp (a):
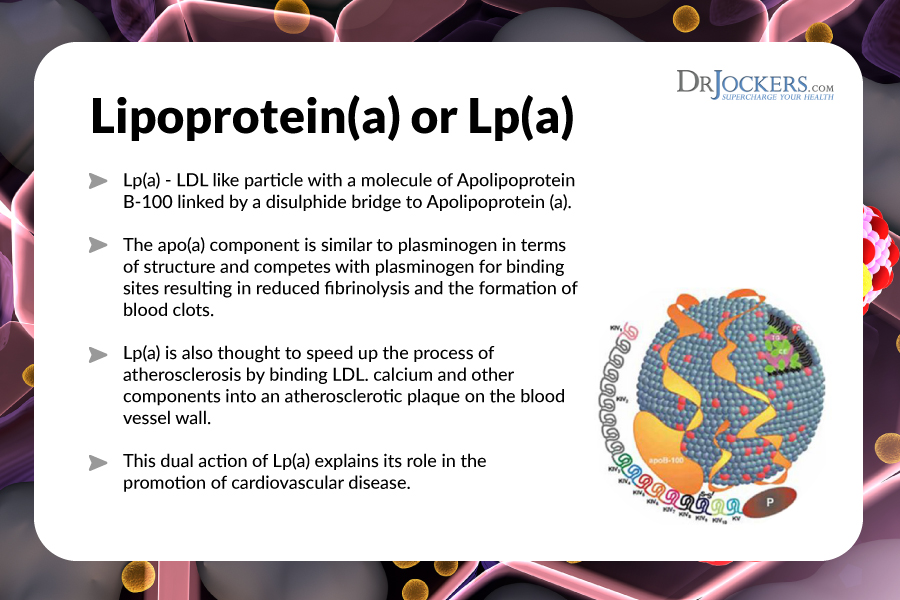
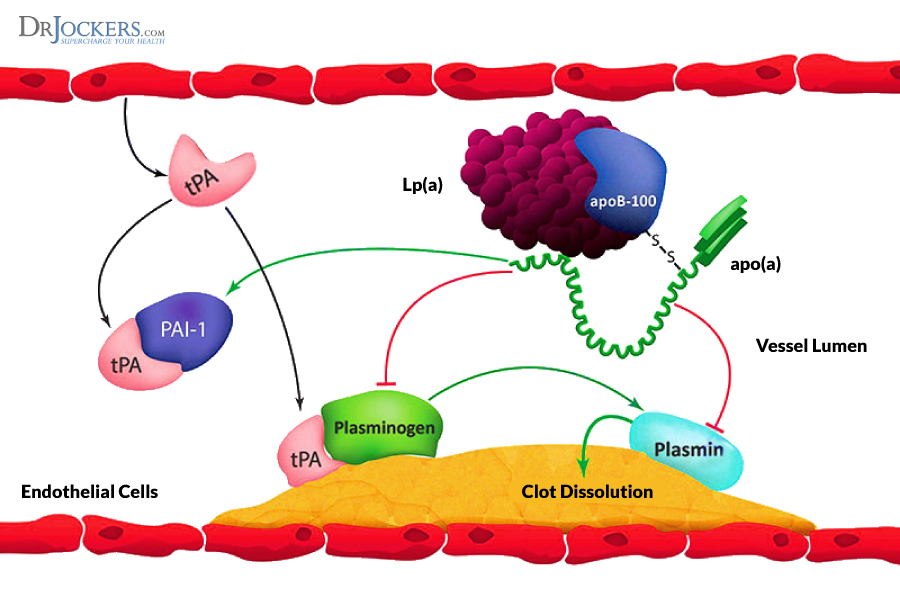
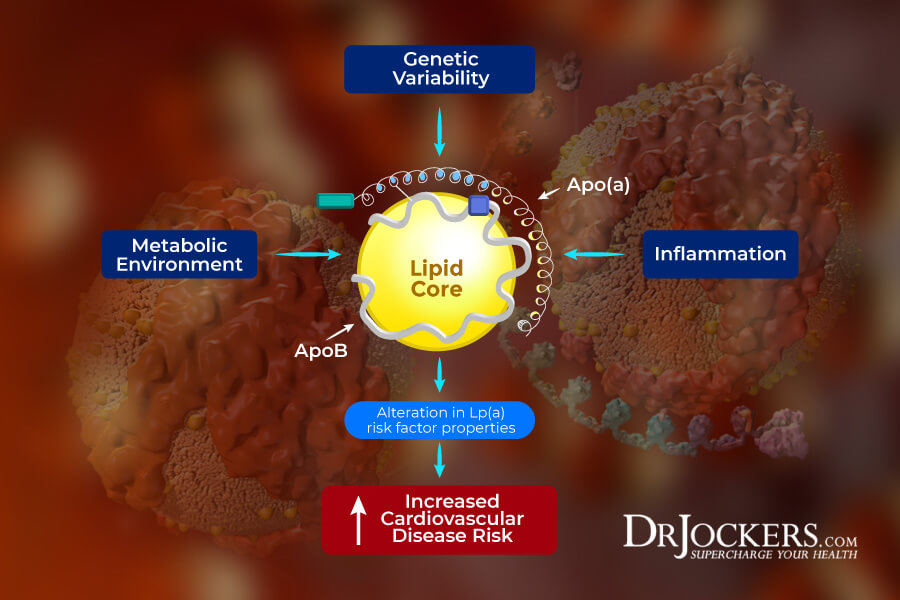
Lipoproteins are molecules of fat (lipo) and protein that carry cholesterol molecules and fat soluble vitamins through the blood. Lp(a) is a particular subtype of LDL cholesterol that is bound to a protein called apolipoprotein (a) (4).
Lp(a) is known to accumulate in plaques and promote atherosclerosis in the walls of the arteries. It is also involved with blood coagulation and increased risk of blood clots within blood vessels (5, 6).
Factors Involved With Elevated Lp(a)
Elevated Lp(a) is thought to be a genetic factor and levels are not influenced by diet, exercise, weight loss, stress, or other environmental factors. Lp(a) is one of the major issues involved in cardiovascular disease. In fact, many leading experts believe that Lp(a) abnormalities are the key factor in younger individuals (30’s-50’s) having heart attacks (7, 8).
Most conventional lipid panels never measure Lp(a) levels but more sophisticated tests such as the Vertical AutoProfile (VAP) and the Lipoprotein Particle Profile include Lp(a). A normal Lp(a) is less than 30 mg/dL. Anyone with a level of Lp(a) greater than 30 mg/DL has a significantly increased risk of heart disease.
Individuals with low thyroid function often have higher Lp(a) levels (9, 10). Individuals with genetically elevated Lp(a) should be proactive about taking care of their thyroid. Elevated Lp(a) levels can also cause high blood pressure, especially in women over 55 years old. There is often a triad effect of low thyroid, high blood pressure, and elevated Lp(a) levels.
Lifestyle Tips to Stabilize Lp(a):
Individuals with elevated Lp(a) must take good measure to reduce inflammation. Elevated Lp(a) is like a gas leak in the house and inflammation is the spark that sets off the fire. To keep inflammation down, one should be on a ketogenic diet keeping carbohydrates to a minimum.
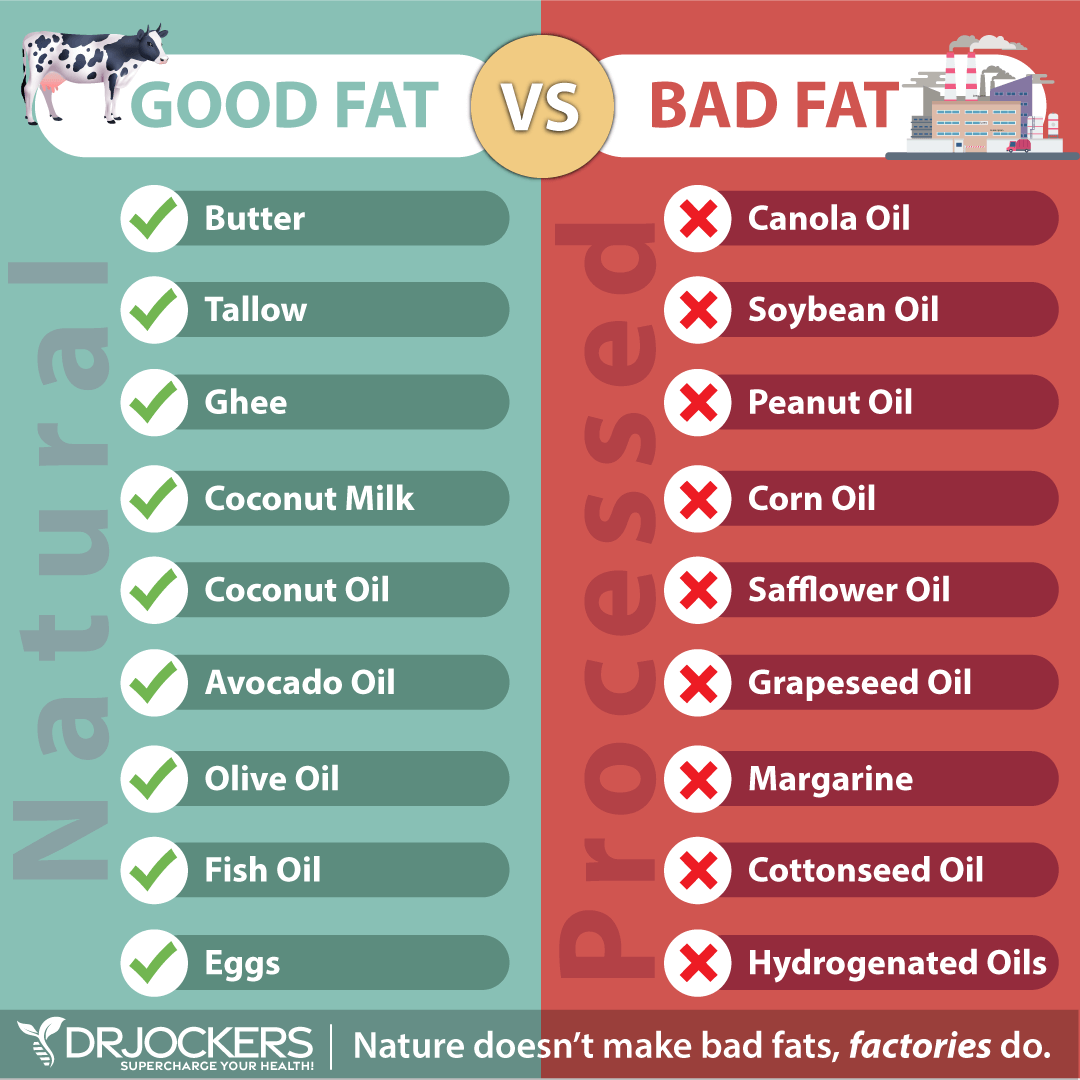
The goal should be 60-70% of calories coming from good fat sources such as coconut products, avocado, olive oil, pasture-raised butter, pastured egg yolk, and low carbohydrate nuts and seeds. The good fats, and in particular healthy saturated fats, help to reduce Lp(a) levels. Clean protein from grass-fed beef and pasture raised poultry should make up 25-30% of calories. Be careful not to overcook meat and oils as this elevates the production of inflammatory free radicals.
Carbohydrates have been shown to elevate Lp(a) levels so these individuals should keep carbohydrates in the 10-15% of calorie load range. It is best to stick with non-starchy vegetables, low-glycemic fruit such as berries, lemons, and limes as carbohydrate sources. They should only use stevia as a sweetener as the fructose content of other natural sweeteners such as honey, coconut nectar, and maple syrup will drive up their inflammation and Lp(a) levels.
Hormones and Lipoprotein Lp(a) Levels:
Hormone levels have a very important influence over Lp(a) levels. Improving DHEA and testosterone levels will lower Lp(a) levels in men and improving DHEA and estrogen/progesterone balance in women will help to lower Lp(a) levels (11, 12, 13).
Proper lifestyle activities including good sleep cycles (going to bed early and waking up early) and high intensity exercise are key for healthy hormones. They must use good stress reduction techniques to minimize heavy periods of mental and emotional stress.
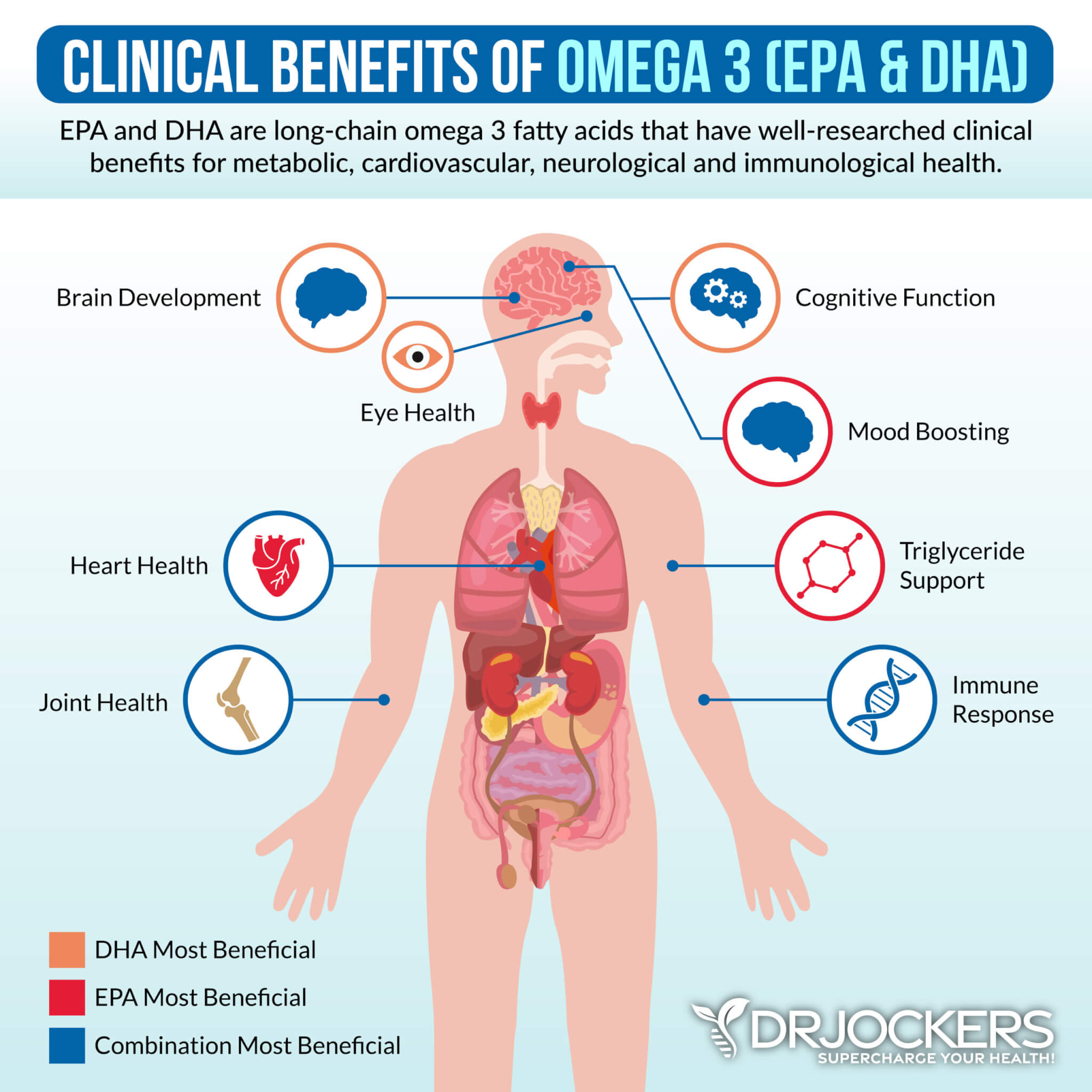
It is also advisable to supplement with omega-3 fatty acids EPA and DHA as well as vitamin D. The individual at risk should take great care of their gut and adrenals by using probiotics, and adrenal adaptogens and consuming a diet rich in antioxidants and naturally fermented foods. Good fats as explained above are the building blocks for healthy hormones and should be the foundation for this nutrition plan.
Supplementation to Lower Lp(a):
High doses of vitamin B3 or Niacin are the most effective way to bring down Lp(a) levels (14, 15). The challenge with high doses of niacin is that it causes annoying hot flushes where the face and neck get red and the individual feels very warm. This is quite scary for the individual if they are not educated on the flush beforehand and most doctors do not understand that this is a normal phenomenon.
Famed cardiologist and author of the NY Times bestselling book “Wheat Belly,” Dr William Davis offers this advice. In order to tolerate niacin, one must take it with a large meal such as dinner, and hydrate vigorously.
Dr Davis advises patients to drink 2 (8-12 oz) glasses of water to put out the flush. He believes this will work for 90%. He advises to never take the niacin more than once per day for any long-acting preparation and twice daily for immediate release (16).
Other key supplements include CoQ10, N Acetyl Cysteine, Acetyl-L-carnitine, and alpha lipoic acid to boost mitochondrial health (17, 18, 19, 20). I put my clients with elevated Lp (a) on Mito Support which contains clinically verified dosages of these mitochondrial enhancing nutrients.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.

Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!