 Mastitis During Breastfeeding: Symptoms and Support Strategies
Mastitis During Breastfeeding: Symptoms and Support Strategies
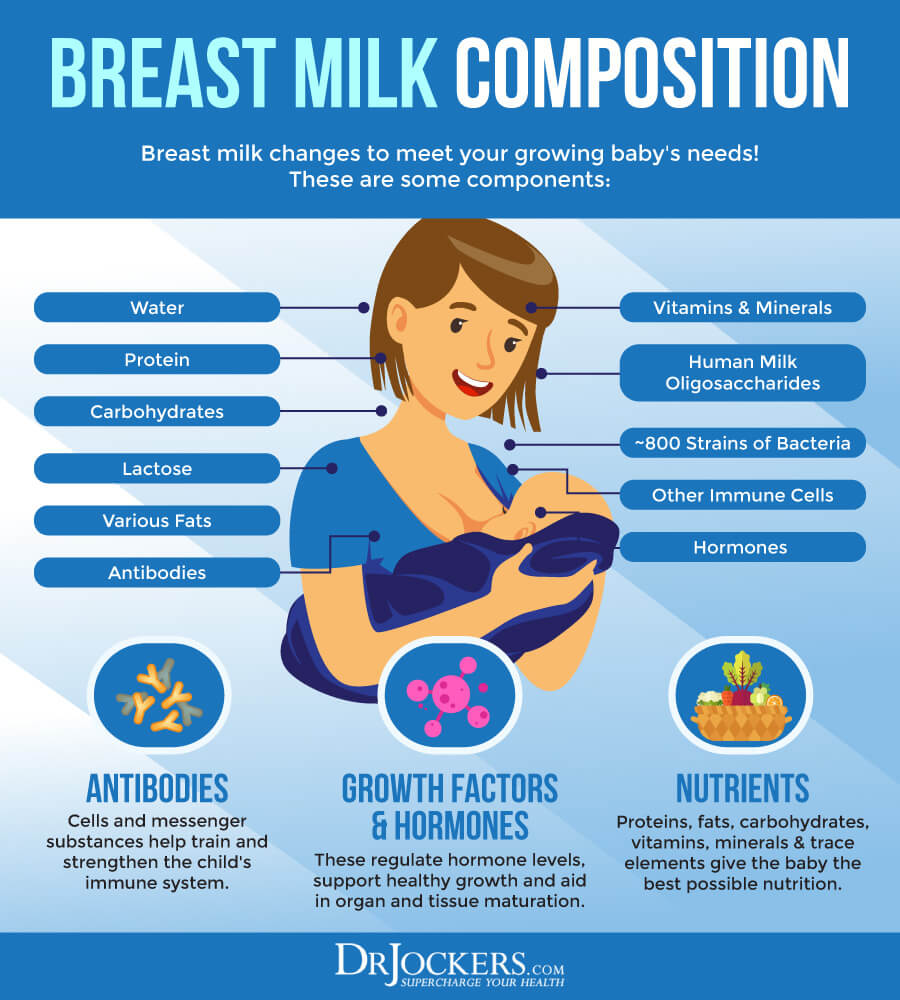
Breastfeeding is incredibly important not only for the baby but the mother as well. Of course, breast milk is the best nourishment for the baby, necessary for healthy growth and development. But it’s also important for bonding between mother and child.
Unfortunately, breastfeeding can sometimes lead to mastitis, a painful breast infection in breastfeeding mothers. Though mastitis is a painful condition, treating it naturally is more simple than you’d think. Today, I want to offer some natural options for mastitis, as well as some natural ways for supporting your body and reducing your risks. With the help of these tips, you should be able to continue this worthwhile, nutritious, and important journey of breastfeeding your child.
In this article, you will learn about mastitis. You will understand the symptoms of mastitis and the types of mastitis. I will explain the risk factors for mastitis. You will understand potential complications and conventional treatment options for mastitis. I will offer some natural support strategies for mastitis. I will discuss the importance of continuing breastfeeding. I will also offer some lifestyle strategies to support your health through breastfeeding.
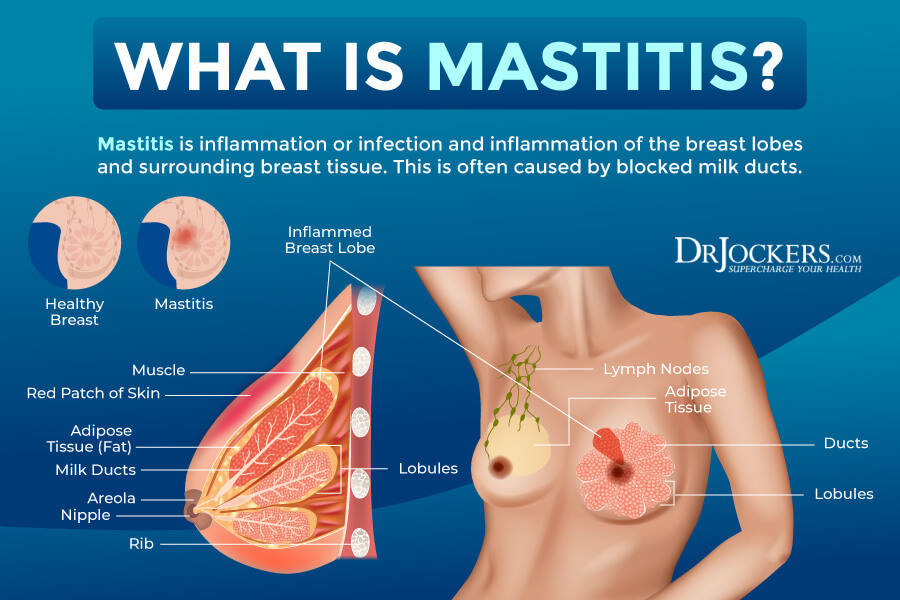
What Is Mastitis
Mastitis is also known as puerperal mastitis or lactation mastitis. It is a common breast infection that affects breastfeeding women. According to the American Family Physician, it affects about 10 percent of breastfeeding women (1). Some women may develop mastitis when not breastfeeding. Breast infection in non-breastfeeding women it’s called periductal mastitis (2).
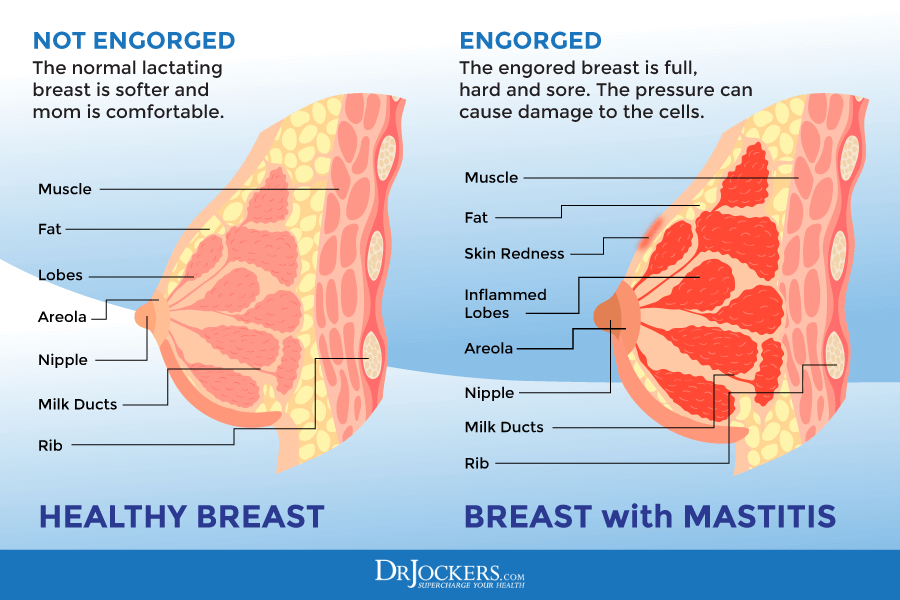
Breastfeeding women may develop mastitis because of milk status, which is a buildup of milk within the breast. This may happen when the baby is having problems attaching to the breast during feeding time, the baby is having difficulties feeding, or there is missed feeding or infrequent feeding for any reason.
In some instances, women may experience infective mastitis. This means that the milk that has been built up in the breast has been infected with bacteria. Bacteria, usually Staphylococcus aureus, may enter through cracked or sore nipples leading to an infection during the postpartum period. Staphylococcus aureus is a common bacteria behind skin infections and skin rashes. Since most breastfeeding women experience some nipple soreness and redness and many experiences cracked nipples or more severe nipple pain, it’s not surprising that infections can occur.
Symptoms of Mastitis
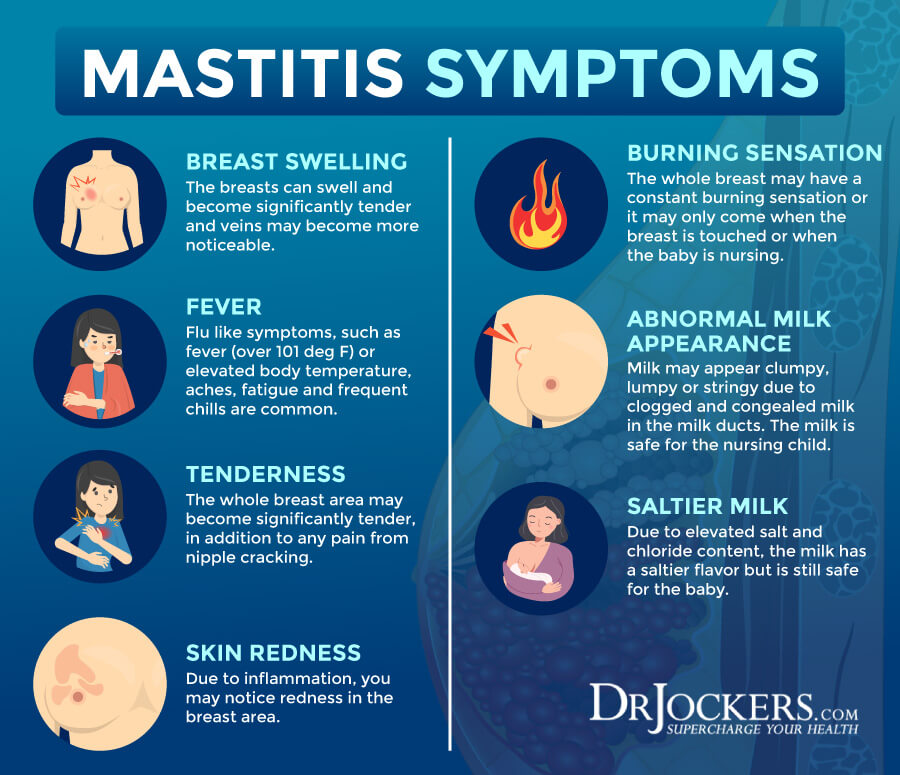
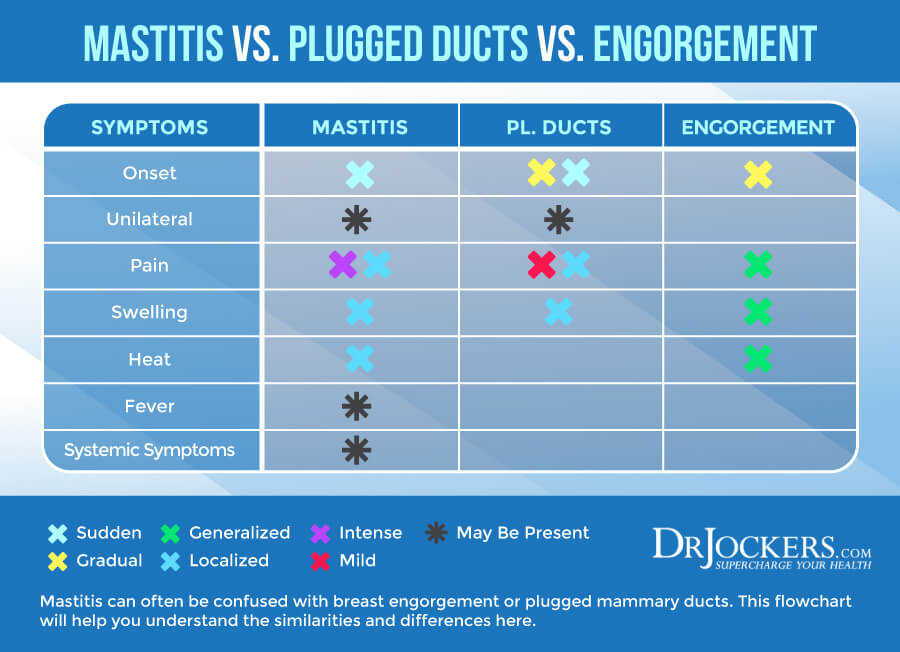
Symptoms of mastitis may develop suddenly. They may start with flu-like symptoms before other symptoms occur. Symptoms may include:
- Abnormal swelling of one breast that makes it bigger than the other one
- Breast tenderness or pain in one breast
- Painful lump in one breast
- Pain or a burning sensation during breastfeeding
- Itching
- Warm breast
- Nipple discharge with pus or blood
- Skin redness around the nipple
- Enlarged lymph nodes in the neck or armpit areas
- Chills
- Fever (over 101F/38.3C)
- Feeling generally run down and unwell
Types of Mastitis
There are two major types of mastitis:
- Lactation mastitis: Lactation mastitis affects breastfeeding women.
- Periductal mastitis: Periductal mastitis or mammary duct ectasia affects menopausal and postmenopausal women. It also affects smokers. The mammary glands of people with periductal mastitis become thick, their nipples turn inverted and they experience a milky discharge.
There are a variety of infections that may lead to mastitis, including (1, 2, 3, 4):
- Central or subareolar infection: Central or subareolar infection may occur when the milk ducts become infected, causing a discharge. This is common in smokers.
- Granulomatous lobular mastitis: Granulomatous lobular mastitis may result in a noncancerous painful mass.
- Peripheral, nonlactating infection: Peripheral, nonlactating infection may cause inflammation. It is common in smokers and women with diabetes.
- Cellulitis: Cellulitis is a skin infection. It is more common in women with larger breasts or women who have gone through radiation therapy or breast surgery.
- Inflammatory carcinoma: Inflammatory carcinoma is not very common. It’s only responsible for 1 to 5 percent of breast cancers. It may cause swollen and discolored breasts and other symptoms.
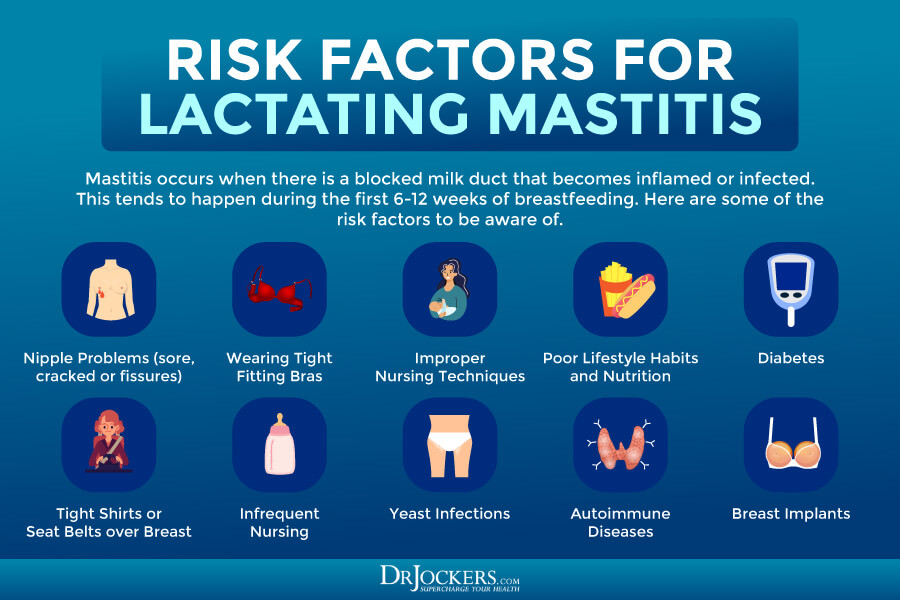
Risk Factors for Mastitis
Risk factors for mastitis include:
- The time during to first 6 to 12 weeks of breastfeeding
- Sore and cracked nipples
- Breast Engorgement
- Nipple fissures
- Wearing tight or ill-fitting bras
- Tight seatbelts over the breast
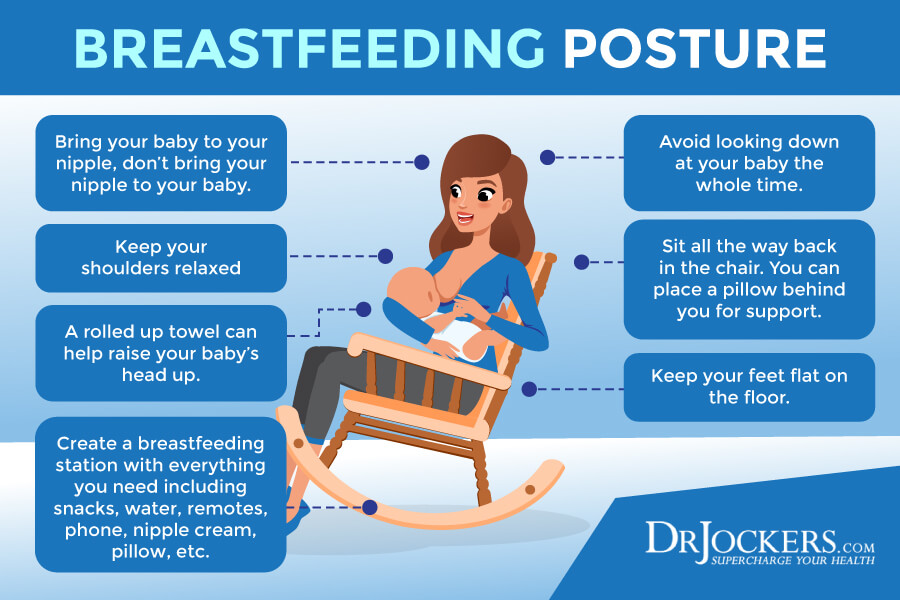
- Improper nursing techniques
- Infrequent nursing
- Yeast infections
- Ill-fitting mouth of the baby
- Stress and fatigue
- Poor nutrition
- Smoking
Other factors that may increase the risk of mastitis, including non-breastfeeding-related mastitis may include:
- Diabetes
- Autoimmune diseases
- Breast implants
- Eczema or other skin issues
- Plucking or shaving chest hair
- Nipple piercing
Potential Complications and Conventional Treatment Options
In most cases, mastitis can be treated successfully naturally. In some cases, they may require oral antibiotics. Treating mastitis, however, is very important. If the blockage in the duct is not eliminated, the collection of pus can lead to a firmness with thickening or breast mass known as an abscess. In most cases, this requires surgical drainage. To avoid this from happening, work with your healthcare provider and address mastitis right away.
Conventional treatment strategies for mastitis usually include a 10-day course of antibiotics to clear up the infection and reduce the risk of recurrence. Your healthcare provider may recommend some over-the-counter pain relievers, such as ibuprofen or acetaminophen. Since breastfeeding can help to clear the infection and reduce issues related to abrupt weaning off your baby, continuing to breastfeed is normally safe and recommended.
While in some cases, natural support strategies are not enough and antibiotics may be necessary, it is important not to overuse antibiotics. Frequent use of antibiotics may lead to antibiotic resistance, less effective treatment, and more frequent infections. According to a 2020 study published in Wiadomosci Lekarski, antibiotic resistance can be a problem in developing and treating mastitis (5). In the next section, I will offer some natural support strategies to help recovery and pain relief for mastitis.

Natural Support Strategies
I recommend the following natural support strategies for mastitis:
Use Breast Milk
Using breast milk may just be one of the best natural solutions for mastitis. Your body is incredibly smart. Breast milk is readily available to remedy your issue. Breast milk helps to fight bacterial infections and may help healing and recovery.
According to a 2005 randomized clinical trial published in the Saudi Medical Journal, using breast milk on sore nipples may be a safe, free, and effective strategy for mastitis (6). All you need to do is to rub some breast milk on your painful nipples and area before and after each breastfeeding.
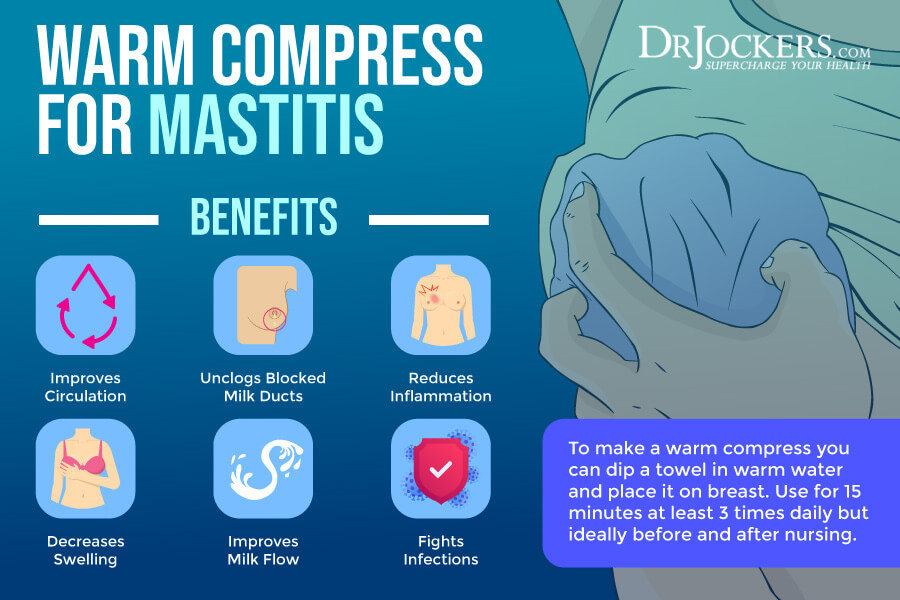
Use a Warm Compress
Using heat for mastitis is a simple and effective natural remedy. Warmth may improve circulation, reduce inflammation, decrease swelling, and fight infections in the affected area. It may also increase milk flow.
According to a 2020 research published in the Journal of Clinical Medicine, warming the nipple and breast with warm water or compress may help with mastitis (7). A 2008 study published in the Indian Journal of Community Medicine has found that using a warm compress, alternating between warm and cold compress, or using cabbage leaves may all help to reduce pain and swelling in mastitis (8).
I recommend using a warm compress on the affected breast for about 15 minutes three times per day. It may particularly be helpful before breastfeeding. Massaging your affected breast before and after using a warm compress may help to reduce symptoms and improve milk flow. You may also benefit from warm showers or warm baths, especially before or after breastfeeding. Your baby will more likely latch on and feed happily on a warm breast instead of a hard and swollen one.
Use a Saline Rinse
Using a saline rinse is another effective and simple natural strategy for mastitis during breastfeeding. According to a 2010 review published in Breast Care, saline may help with abscesses (9). Saline rinses may help to decrease swelling and pain.
They may also be a great option to reduce the risk of mastitis. To make a saline rinse, mix 1 teaspoon of salt in 8 ounces of water. Soak your nipples in the mix after nursing.

Sunflower Lecithin
Lecithin is another great natural strategy for breastfeeding mothers dealing with mastitis. Lecithin may help to reduce the risk of blockages in the milk ducts. Lecithin may help to lower the viscosity of milk and increase polyunsaturated fats in the milk.
This helps the milk to move easier through the milk ducts (10). Eggs, dairy products, beef, soy, sunflower, peanuts, and some fruits or vegetables are good sources of lecithin. I recommend taking Sunflower Lecithin for mastitis.
Use Nano Silver
Using nano silver may be another great option for mastitis. An animal 2019 study published in the International Journal of Molecular Sciences has found that silver or copper nanoparticles may be an alternative strategy for mastitis (11).
It may help to fight pathogens and inflammation. I recommend this Silver Spray. Spray on nipples between feedings and take orally. I recommend 6 sprays 3 times daily.
Consider Using Cabbage Leaves
Using raw, green cabbage leaves is possibly the most well-known natural remedy for mastitis that had been used for centuries. A 2008 study published in the Indian Journal of Community Medicine has found that using cabbage leaves may all help to reduce pain and swelling in mastitis (7). A 2013 review published in the Indian Journal of Surgery has also found that cold cabbage leaves may be beneficial for mastitis (12).
Using cabbage leaves for mastitis is simple. Just put a leaf of cabbage inside your bra for a few hours per day. Keep the cabbage in the fridge so the leaves are cool and soothing. Change the cabbage leaves every couple of hours.

Consider Using Poultices
You may also try to make a poultice or compress with various dried herbs, including fenugreek seed, dandelion, rosemary, yarrow root, or comfrey for mastitis. These herbs may offer antibacterial and anti-inflammatory properties to reduce inflammation and symptoms. According to a 2013 study published in the Iranian Red Crescent Medical Journal, besides a poultice, drinking fenugreek tree may also help with milk production and breast health (13).
To make a fenugreek poultice, first, grind the fenugreek, then add it to a bowl. Mix it with enough hot water to create a thick paste. Put the fenugreek paste between two layers of gauze or light cotton cloth. Use the same process with the other herbs. Use the poultice on the affected area. Alternate between using cold and warm poultices. A warm poultice may help circulation, but cold can reduce pain. Use it for about 10 minutes on the infected breast on and off alternating between cold and warm.

Consider Using Aloe Vera
Finally, you may want to consider using aloe vera for mastitis. Aloe vera may offer soothing benefits for mastitis-related pain. According to a 2019 review published in the Iranian Journal of Medical Science, aloe vera may help to reduce inflammation and support repairing broken or wounded skin (14).
It may also help to repair damaged, dry, broken, and inflamed skin around the nipples. You can apply fresh aloe vera gel directly on your infected breast. Once it has dried, wash it off with water and pat dry it with a towel. Repeat it throughout the day as needed.

Importance of Continuing to Breastfeed
According to a 2020 research published in the Journal of Clinical Medicine, continuing to breastfeed and using breast milk is important in mastitis (7). Breastfeeding through mastitis can be an important part of your recovery unless your baby has oral thrush. The bacteria causing mastitis don’t like the environment of breast milk. Maintaining a regular breastfeeding schedule thus can help recovery. A regular breastfeeding schedule also keeps the milk healthy and stagnant. Stagnant milk can increase the risk of infections and mastitis (1).
Sudden weaning can also be incredibly stressful for the baby and cause psychological distress for both mother and the baby. Readjusting to a regular breastfeeding schedule after sudden weaning and a period off may also be difficult. Nutritionally speaking, breast milk is the best for the baby and should be the number one option as long as breastfeeding is possible. If you have trouble breastfeeding with or without mastitis, you may benefit from working with a lactation consultant to find strategies that work best for you and your baby.
If you are breastfeeding with mastitis, I recommend that you start feeding with the infected breast. It will help to empty this breast and relieve your symptoms. However, if you find that your infected breast is too hard and painful to start with, begin with the other breast first. The milk flow in the healthy breast will allow the other breast to turn softer as well and make it easier to breastfeed on that side.

Lifestyle Strategies to Follow
I recommend the following lifestyle strategies to follow to support your help, enhance your recovery, and reduce your risks of mastitis:
Anti-Inflammatory Nutrition Plan
According to a 2017 study published in Pediatrics Research, mastitis may be linked to inflammatory changes in breast milk (15). According to a 2019 review published in Nutrition and Metabolic Insights, the diet of the mother’s health affects the quality of breast milk and the baby’s health (16). Following an anti-inflammatory nutrition plan may help to fight infections, reduce inflammation, and improve the quality of the milk.
Focus on anti-inflammatory, nutrient-dense whole foods, such as greens, vegetables, sprouts, herbs, spices, fermented food, grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game. Eat plenty of healthy fats, such as coconut oil, grass-fed butter and ghee, avocados, olives, and extra-virgin olive oil. Use anti-inflammatory spices, such as turmeric, ginger, onion, garlic, oregano, basil, rosemary, and cinnamon. Hydrate your body by drinking plenty of purified water.
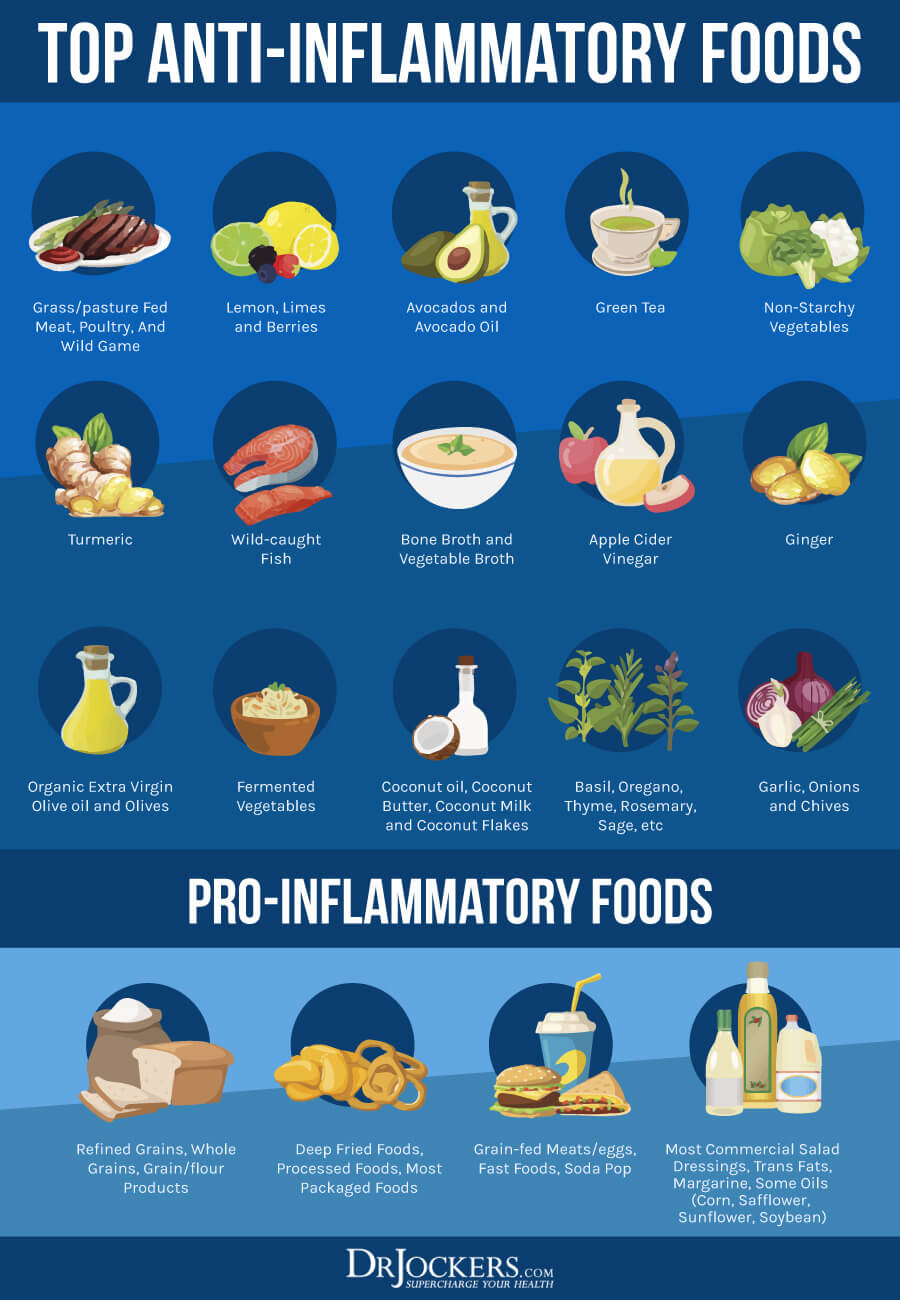
Eat Garlic and Onions
As part of your anti-inflammatory nutrition plan, I recommend that you eat plenty of anti-inflammatory and immune-supporting foods. Include garlic and onion in your daily diet. Garlic and onion both offer natural antibiotic properties.
According to a 2014 review published in the Avicenna Journal of Phytomedicine, garlic may have antimicrobial and other therapeutic benefits (17). According to a 2018 study published in the Journal of Food and Drug Analysis, onion offers antibacterial, antifungal, and anti-inflammatory benefits (18). Eating garlic and onion may help to support inflammation, fight pathogens, and reduce inflammation.

Get Plenty of Rest
Rest is so important if you are a breastfeeding mother. Ideally, an adult should get 7 to 9 hours of sleep at night. As you know, as a breastfeeding mother, getting that much uninterrupted sleep is impossible with a baby who needs to eat and may have other needs during the night.
However, mastitis may be a sign that you are doing too much, experiencing stress, and your body needs rest. Sleep and rest as much as possible. Try resting in bed with your baby cuddled up next to you. Take naps while your baby is napping. If it’s an option for you, ask for support from your partner or a nanny. While you are recovering, avoid doing more than you absolutely need to.
Optimize Vitamin D Levels
A 2016 study published in the International Breastfeeding Journal has found that vitamin D deficiency is more common in breastfeeding women than those women who are not breastfeeding (19). According to a 2017 randomized controlled trial published in the Journal of Medical Association of Thailand, supplementing with vitamin D during breastfeeding may improve breast milk (20). A 2011 animal study published in PLoS One has found that supplementing with vitamin D may help to reduce bacterial infection and mastitis (21).
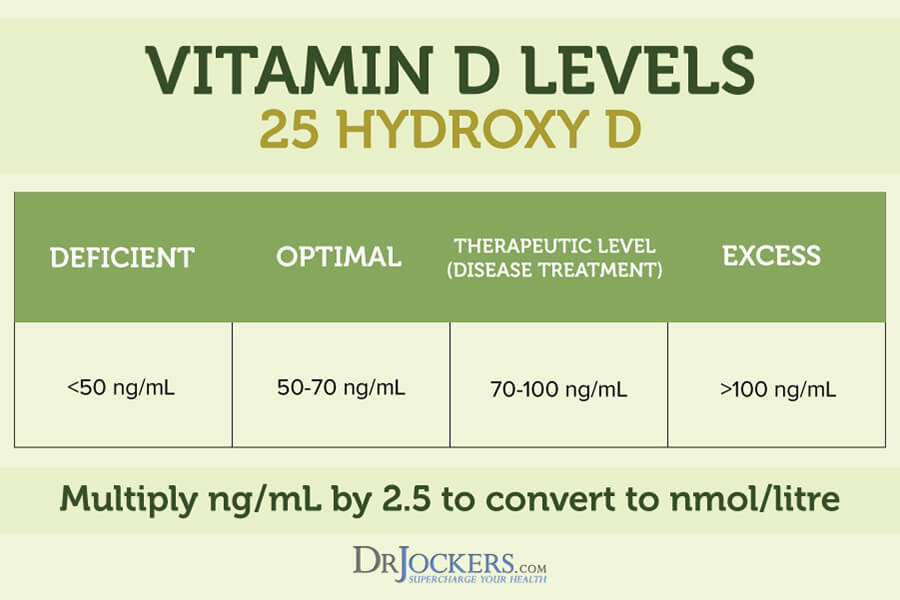
To improve your vitamin D levels, I recommend spending time out in the sun and eating vitamin D-rich fatty fish, egg yolks, and beef liver. Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need supplements to optimize their vitamin D levels.
Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2. I highly recommend this Vitamin D3/K2 Power. Both of these supplements support your immune, skin, cardiovascular, and bone health.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1 – 2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
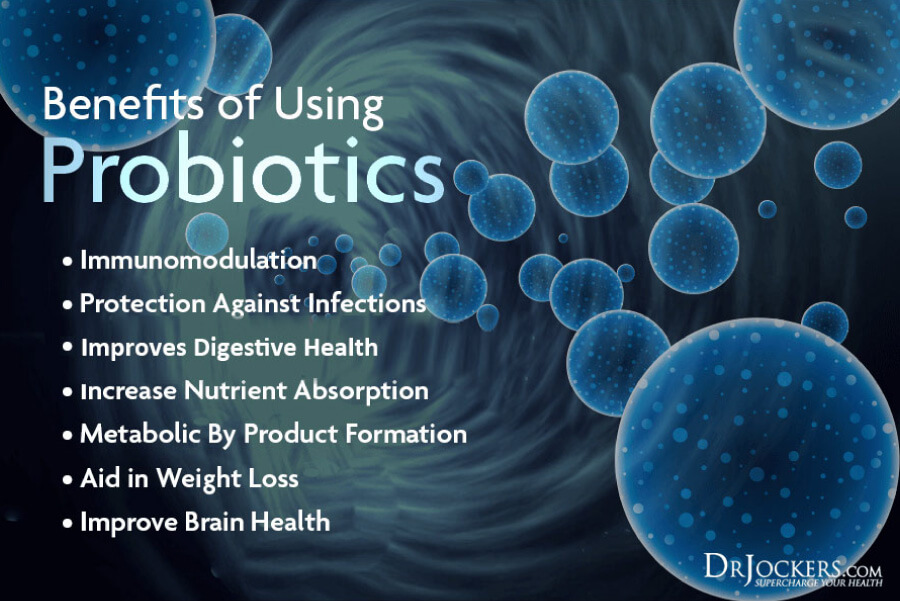
Use Probiotics
Probiotics may help to improve the gut microbiome, reduce infection, support overall health, and improve breast milk. Using antibiotics for mastitis can also seriously disrupt the gut flora and increase the risk of future infections and health issues.
If you are currently using or have used antibiotics for mastitis, using probiotics is critical. Even if you haven’t used antibiotics, probiotics may help to support recovery from mastitis and reduce your future risks.
According to a 2011 article published by the American Family Physician, using probiotics may be effective and may be an alternative to antibiotics for mastitis (22). A 2017 randomized controlled trial published in BMC Pregnancy and Childbirth has found that probiotics may help to reduce the risk of mastitis and reduce the need for antibiotics (23). I recommend that you eat lots of probiotic-rich foods, including sauerkraut, kimchi, fermented vegetables, fermented herbs, coconut kefir, and kombucha. I also recommend that you take a daily probiotic supplement.
Mastitis Prevention
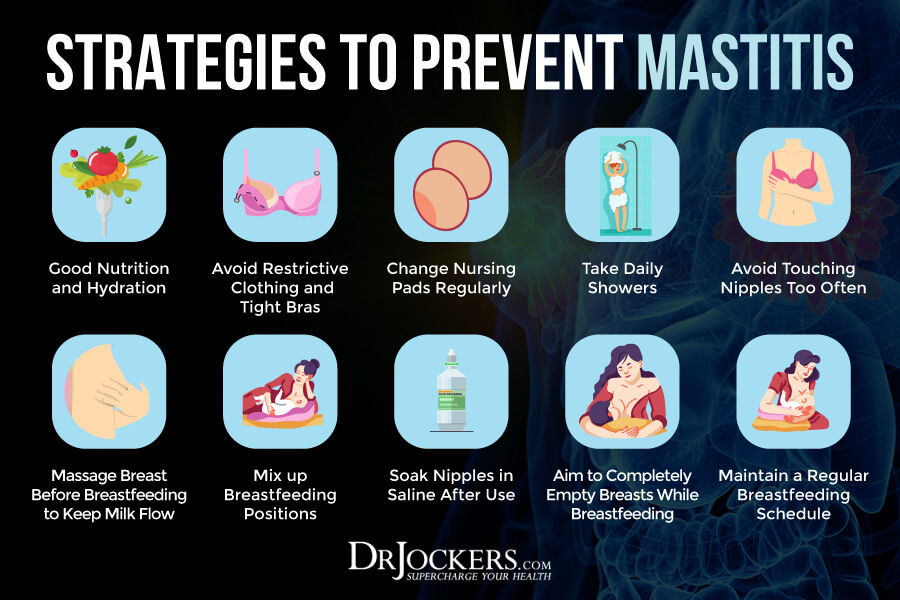
I recommend the following strategies for mastitis prevention, including healthy breast care and breastfeeding strategies:
- Hydrate your body well.
- Follow an anti-inflammatory nutrition plan.
- Avoid alcohol and smoking.
- Reduce stress.
- Wear a supportive bra that fits well and is not too tight.
- Avoid any restrictive clothing, tight clothing, and underwire bras.
- Change your nursing pads regularly as they get wet.
- Avoid any impacts or blows to the breast.
- Don’t sleep on your stomach. Try a pregnancy pillow to support sleeping and resting.
- Avoid any soaps, deodorants, and powders on your breasts. The ones that contain triclosan can be particularly irritating.
- Take daily showers, but avoid washing your nipples with soap.
- Avoid touching your breast, especially your nipples, too often.
- Soak your nipples in a saline rinse.
- Use aloe vera for cracked nipples.
- Massage your breast before breastfeeding to keep milk flow.
- Maintain a regular breastfeeding schedule, especially during the first 6 months.
- Make sure your baby is latching on and well-attached to your breasts.
- Aim to completely empty your breasts while breastfeeding.
- Allow your baby to naturally end their feeding sessions and release themselves.
- Mix up your breastfeeding positions.
- If you are using a breast pump, learn how to use it, and avoid incorrect use.
- Work with a lactation consultant if you need to.
- Inform your doctor about any unusual pain or symptoms.
Final Thoughts
Breastfeeding is essential for both the baby and the mother. Breast milk is the best nourishment for the baby supporting healthy growth and development. It is also important for emotional bonding between mother and child. Breastfeeding may be important and beautiful, but it can be painful sometimes.
Breastfeeding women commonly experience mastitis, a painful breast infection in breastfeeding mothers. Though mastitis is a painful condition, treating it naturally is simple and possible. Follow my natural support strategies and lifestyle strategies for mastitis to support your health through breastfeeding.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Sources in This Article Include:
1. Spencer JP. Management of Mastitis. Am Fam Physician. 2008 Sep 15;78(6):727-731. Link Here
2. Mastitis. American Cancer Society. Link Here
3. Wolfrum A, Kümmel S, Theuerkauf I, Pelz E, Reinisch M. Granulomatous Mastitis: A Therapeutic and Diagnostic Challenge. Breast Care (Basel). 2018 Dec;13(6):413-418. doi: 10.1159/000495146. Epub 2018 Nov 23. PMID: 30800035
4. Inflammatory breats cancer. NIH. Link Here
5. Salmanov AG, Savchenko SE, Chaika K, Vitiuk AD, Ruban I, Dyndar OA, Zhelezov D, Vorobey L, Semeniuk LM, Hetsko NV, Tsmur OV, Suslikova LV, Nykoniuk TR, Shunko YY, Beketova HV, Manzhula LV, Kurochka VV, Abbasova ER. Postpartum mastitis in the breastfeeding women and antimicrobial resistance of responsible pathogens in ukraine: results a multicenter study. Wiad Lek. 2020;73(5):895-903. PMID: 32386365
6. Mohammadzadeh A, Farhat A, Esmaeily H. The effect of breast milk and lanolin on sore nipples. Saudi Med J. 2005 Aug;26(8):1231-4. PMID: 16127520
7. Pevzner M, Dahan A. Mastitis While Breastfeeding: Prevention, the Importance of Proper Treatment, and Potential Complications. J Clin Med. 2020 Jul 22;9(8):2328. doi: 10.3390/jcm9082328. PMID: 32707832
8. Arora S, Vatsa M, Dadhwal V. A Comparison of Cabbage Leaves vs. Hot and Cold Compresses in the Treatment of Breast Engorgement. Indian J Community Med. 2008 Jul;33(3):160-2. doi: 10.4103/0970-0218.42053. PMID: 19876476
9. 2010 BreastCare. Link Here
10. Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006-. Lecithin. [Updated 2021 Sep 20]. Link Here
11. Kalińska A, Jaworski S, Wierzbicki M, Gołębiewski M. Silver and Copper Nanoparticles-An Alternative in Future Mastitis Treatment and Prevention? Int J Mol Sci. 2019 Apr 3;20(7):1672. doi: 10.3390/ijms20071672. PMID: 30987188
12. Kataria K, Srivastava A, Dhar A. Management of lactational mastitis and breast abscesses: review of current knowledge and practice. Indian J Surg. 2013 Dec;75(6):430-5. doi: 10.1007/s12262-012-0776-1. Epub 2012 Dec 12. PMID: 24465097
13. Ghasemi V, Kheirkhah M, Vahedi M. The Effect of Herbal Tea Containing Fenugreek Seed on the Signs of Breast Milk Sufficiency in Iranian Girl Infants. Iran Red Crescent Med J. 2015 Aug 15;17(8):e21848. doi: 10.5812/ircmj.21848. PMID: 26430522
14. Hekmatpou D, Mehrabi F, Rahzani K, Aminiyan A. The Effect of Aloe Vera Clinical Trials on Prevention and Healing of Skin Wound: A Systematic Review. Iran J Med Sci. 2019 Jan;44(1):1-9. PMID: 30666070
15. Tuaillon, E., Viljoen, J., Dujols, P. et al. Subclinical mastitis occurs frequently in association with dramatic changes in inflammatory/anti-inflammatory breast milk components. Pediatr Res 81, 556–564 (2017). Link Here
16. Çavdar G, Papich T, Ryan EP. Microbiome, Breastfeeding and Public Health Policy in the United States: The Case for Dietary Fiber. Nutr Metab Insights. 2019 Aug 21;12:1178638819869597. doi: 10.1177/1178638819869597. PMID: 31488950
17. Bayan L, Koulivand PH, Gorji A. Garlic: a review of potential therapeutic effects. Avicenna J Phytomed. 2014 Jan;4(1):1-14. PMID: 25050296
18. Kavita Sharma, Neelima Mahato, Yong Rok Lee, Systematic study on active compounds as antibacterial and antibiofilm agent in aging onions, Journal of Food and Drug Analysis, Volume 26, Issue 2, 2018, Link Here
19. Gellert, S., Ströhle, A. & Hahn, A. Breastfeeding woman are at higher risk of vitamin D deficiency than non-breastfeeding women – insights from the German VitaMinFemin study. Int Breastfeed J 12, 19 (2016). Link Here
20. Niramitmahapanya S, Kaoiean S, Sangtawesin V, Patanaprapan A, Bordeerat NK, Deerochanawong C. Correlation of 25-Hydroxyvitamin D Levels in Serum vs. Breastmilk in Vitamin D-Supplementation Breastfeeding Women during Lactation: Randomized Double Blinded Control Trial. J Med Assoc Thai. 2017 Feb;100 Suppl 1:S165-71. PMID: 29927558
21. Lippolis JD, Reinhardt TA, Sacco RA, Nonnecke BJ, Nelson CD. Treatment of an intramammary bacterial infection with 25-hydroxyvitamin D(3). PLoS One. 2011;6(10):e25479. doi: 10.1371/journal.pone.0025479. Epub 2011 Oct 3. PMID: 2199131
22. American Family Physican. 2011. LInk Here
23. Bond, D.M., Morris, J.M. & Nassar, N. Study protocol: evaluation of the probiotic Lactobacillus Fermentum CECT5716 for the prevention of mastitis in breastfeeding women: a randomised controlled trial. BMC Pregnancy Childbirth 17, 148 (2017). Link Here