Ulcerative Colitis: Causes, Symptoms and Natural Support Strategies
Ulcerative colitis is a major form of inflammatory bowel disease that affects millions of people worldwide. The incidence of ulcerative colitis is rapidly rising around the world and is expected to reach epidemic proportions.
Ulcerative colitis is a chronic relapsing condition that causes inflammation and sores in the digestive tract. Symptoms of ulcerative colitis usually develop over time and have times of remission. For some people, the symptoms can be debilitating and lead to life-threatening complications.
Current standard treatments for ulcerative colitis are largely ineffective and may have unwanted and serious side effects. Fortunately, there are natural support strategies that work to improve digestive health and the inflammatory response.
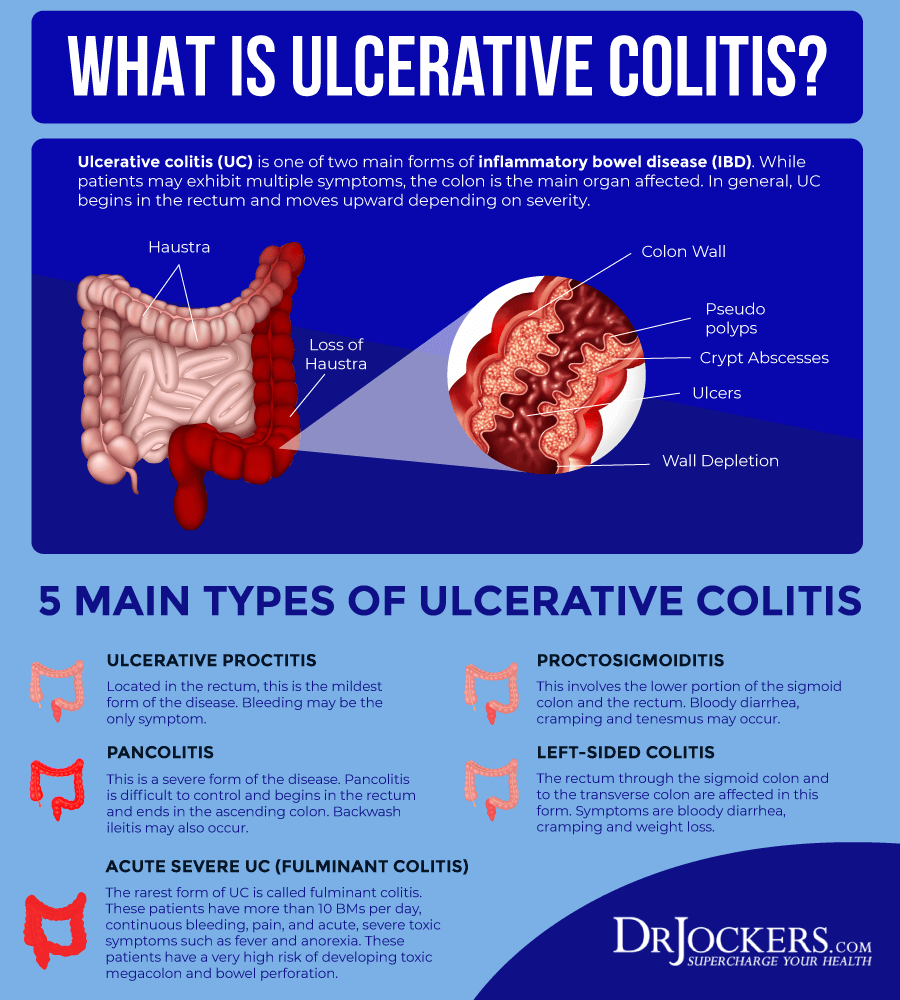
What is Ulcerative Colitis?
Your colon, or large intestine, is a hollow muscular tube that processes digestive waste (1). When your colon is inflamed, this is known as colitis. Colitis is a general term for inflammation in the large intestine. It can be caused by a variety of reasons including parasites, viruses, or bacteria.
Colitis may be acute or long term. There are several types of colitis, including ulcerative colitis, Crohn’s colitis (a type of Crohn’s disease), and microscopic colitis. Ulcerative colitis and Crohn’s disease are chronic inflammatory bowel diseases (IBD).
Both ulcerative colitis and Crohn’s are persistent and relapsing inflammatory conditions of the gastrointestinal tract (2). They are usually only diagnosed after a person becomes symptomatic. By that time, the inflammatory process has often already caused considerable damage and the disease is less responsive or unresponsive to conventional therapies (3). Late diagnosis of IBD is one reason for the steep increase in these conditions around the world.
Crohn’s disease and ulcerative colitis share overlapping pathological and clinical symptoms. However, Crohn’s can affect one or several segments of the digestive tract. When it affects the large intestine, it is Crohn’s colitis. Ulcerative colitis is mainly restricted to the mucosal layer of the colon or rectum.
Ulcerative colitis can affect people of any age. However, it is most likely to develop between the ages of 15 and 30 or in a person older than 60.
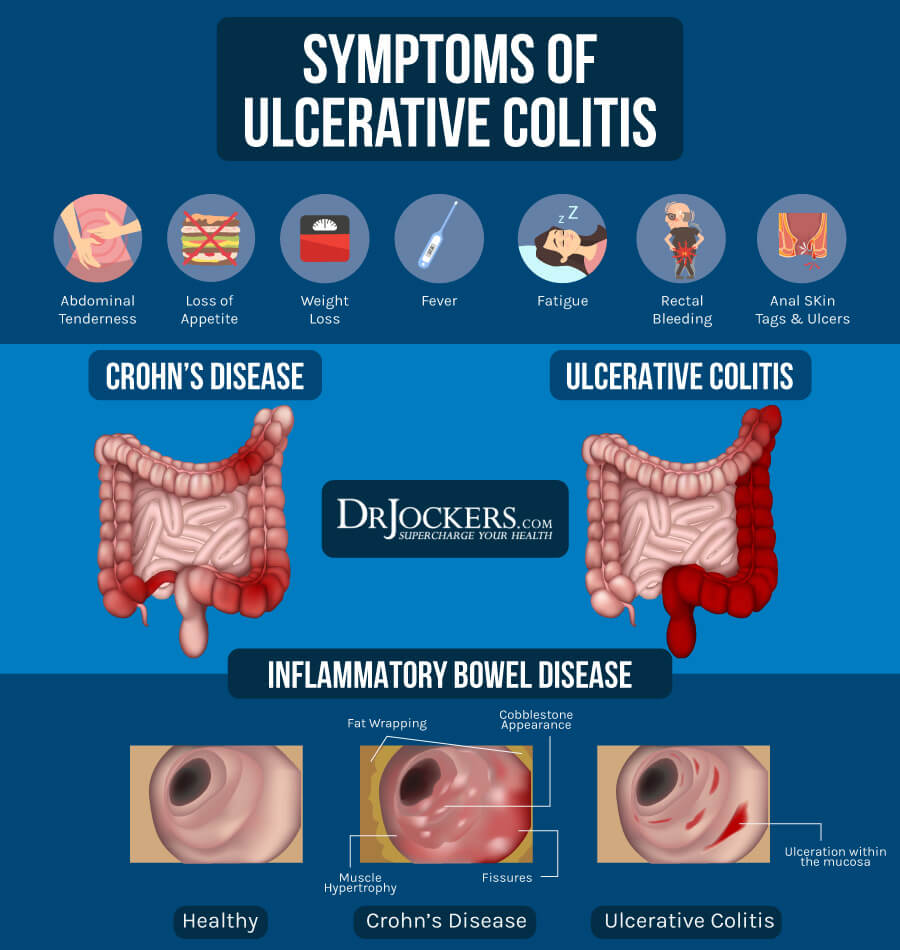
Symptoms of Ulcerative Colitis
Symptoms of ulcerative colitis range from mild to severe and most people have periods of remission that can last for weeks or years. Approximately 10% of people with ulcerative colitis experience severe symptoms.
People with ulcerative colitis may experience one or more of the following symptoms:
- Abdominal pain or cramping
- Weight loss
- Diarrhea, often with blood or pus
- Rectal pain
- Nausea or loss of appetite
- Blood in stool
- Urgent need to move the bowels
- Fatigue
- Chills or fever
- Anemia
- Vomiting
Less common symptoms include joint pain or soreness, eye irritation, and certain rashes (1).
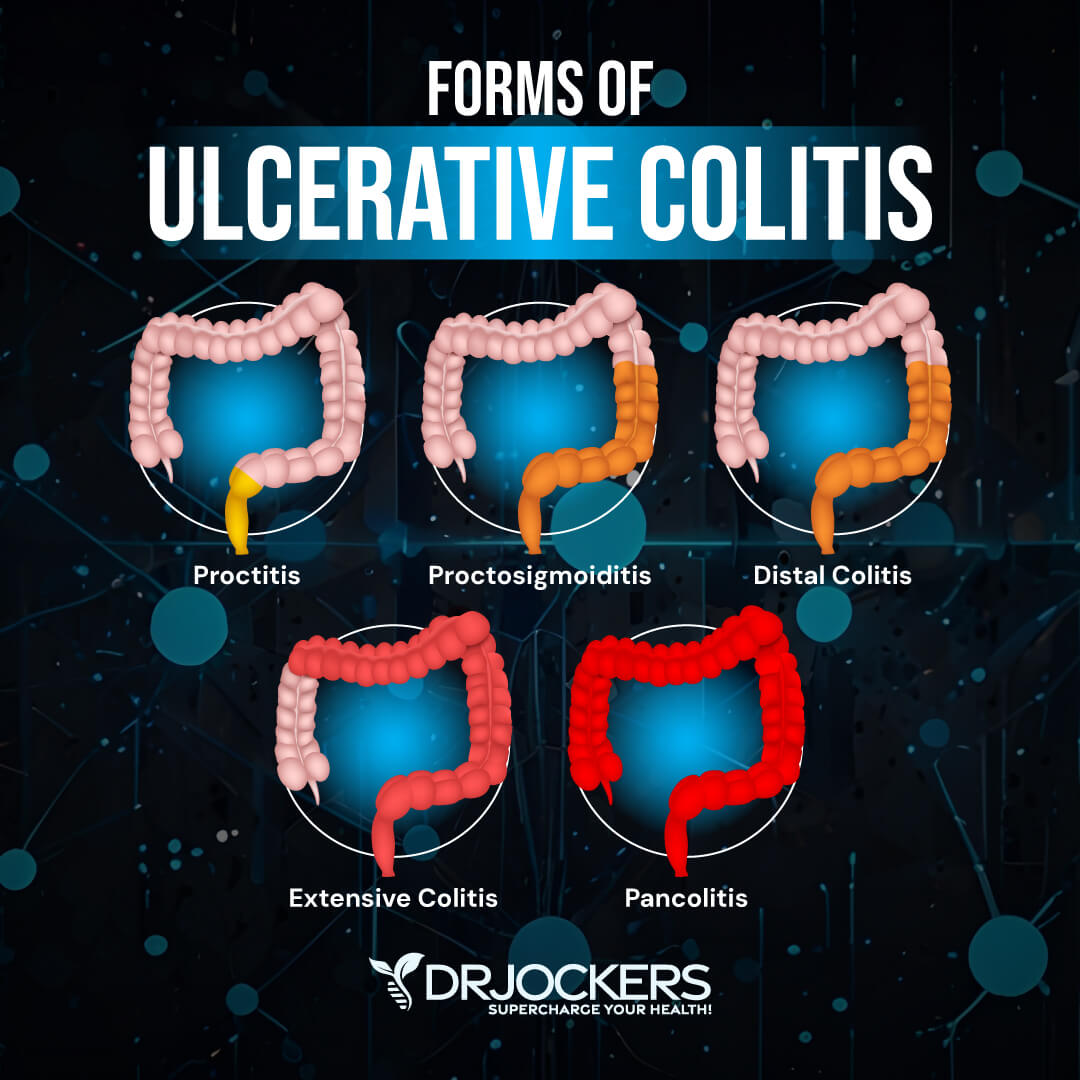
Types of Ulcerative Colitis
Ulcerative colitis is classified according to its location. Types of ulcerative colitis include:
- Proctosigmoiditis: affects the rectum and lower portion of the colon
- Left-sided colitis: affects the left side of the colon beginning at the rectum
- Pancolitis: affects the entire large intestine
- Ulcerative proctitis: inflammation is confined to the rectum and rectal bleeding may be the only sign of the disease. This form tends to be the mildest.
- Acute severe ulcerative colitis: a rare form that affects the entire colon and causes severe pain, profuse diarrhea, bleeding, fever, and inability to eat.
Major Causes of Ulcerative Colitis
While the exact etiology of ulcerative colitis is unknown, researchers believe it is driven by genetic susceptibility and internal and external factors. The internal and external factors include:
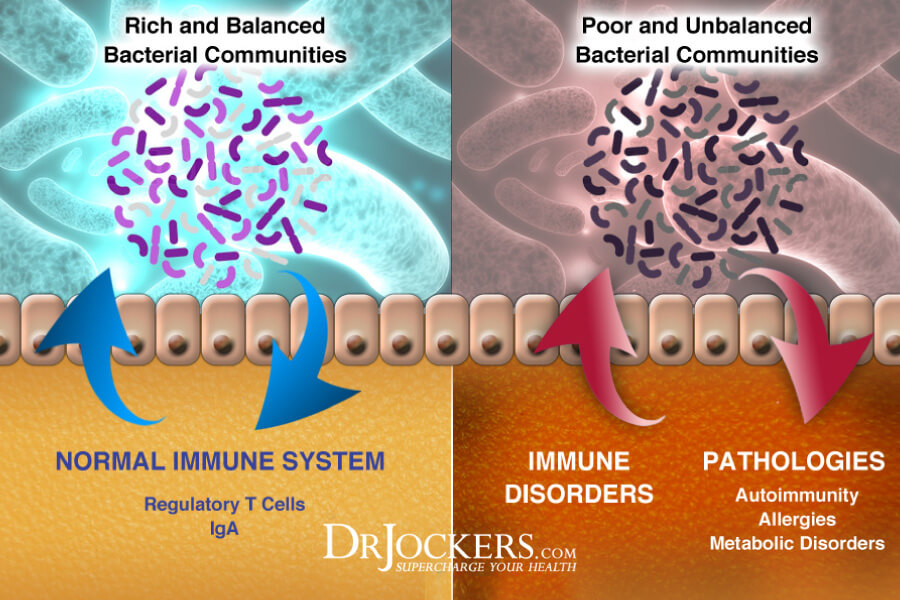
Imbalances in Gut Microbiome
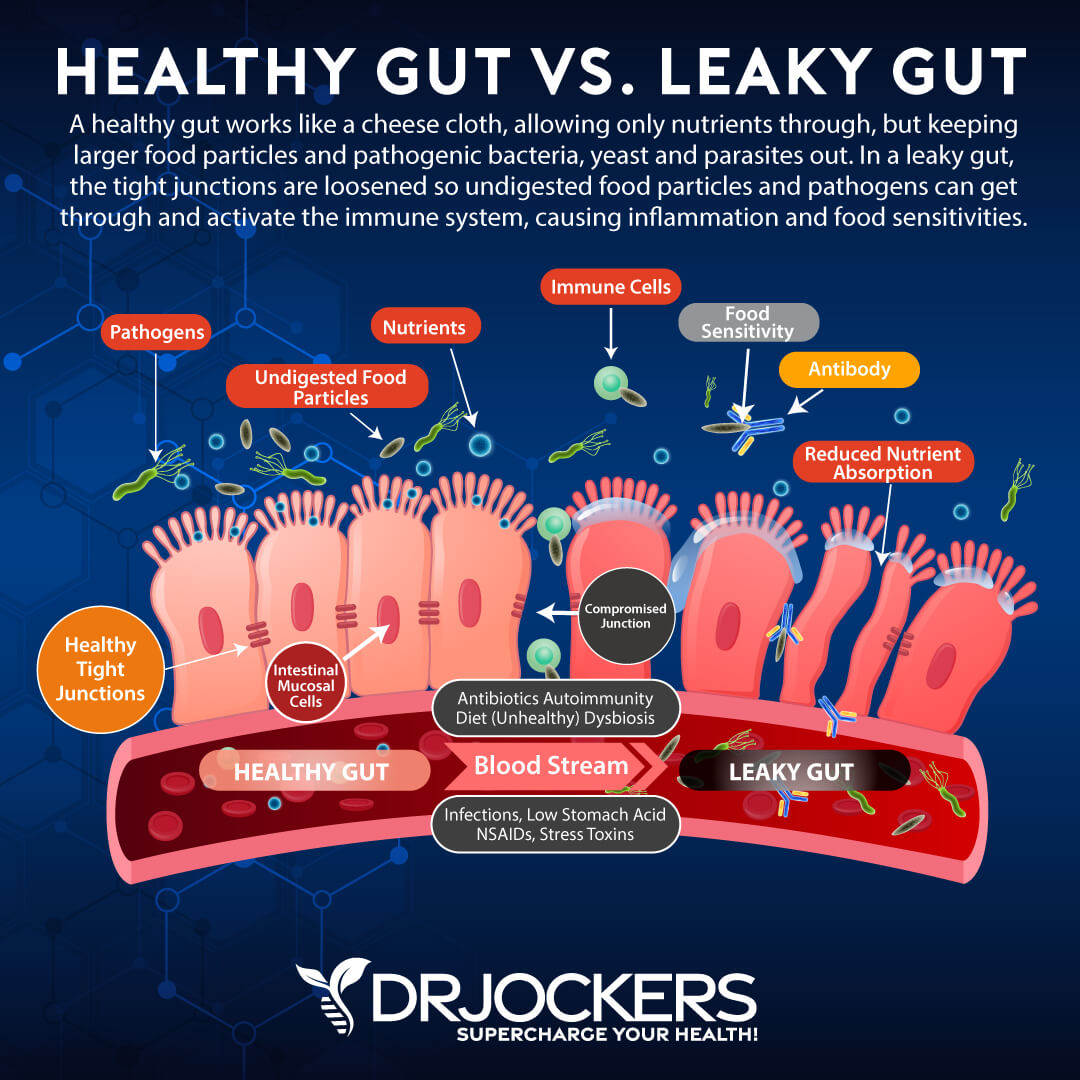
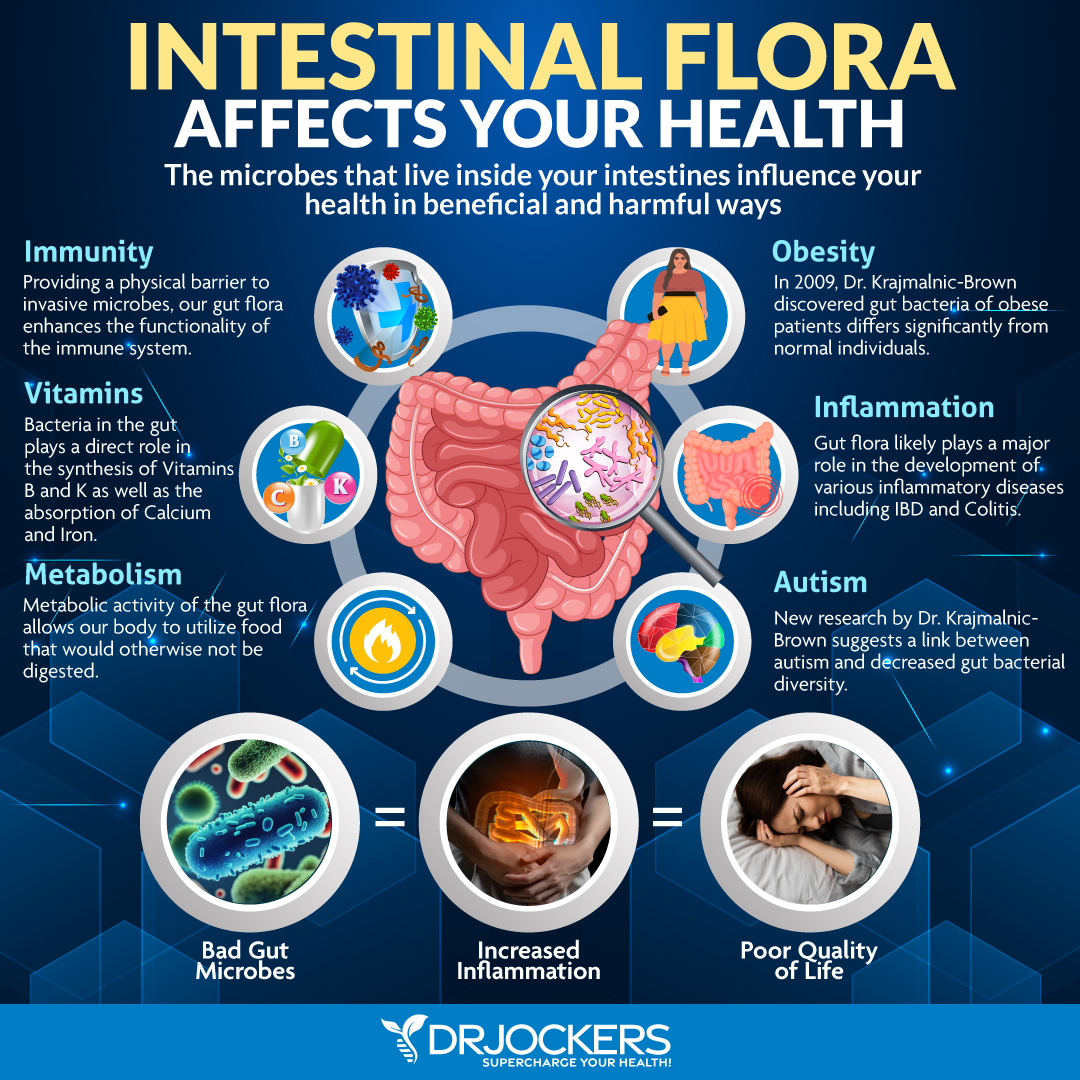
The mechanism leading to ulcerative colitis is thought to involve a complex interaction between the immune system, the gut, and gut microbes. Emerging research suggests that people with ulcerative colitis and other inflammatory bowel diseases have different and abnormal gut microbes (4).
There is a strong correlation between alterations in the gut microbiota and irritable bowel diseases. People with ulcerative colitis may have more bacteria with pro-inflammatory properties and fewer bacteria with anti-inflammatory properties. The concentration of sulfate-reducing bacteria is higher in IBD patients which can result in the metabolic production of hydrogen sulfide. This is toxic to intestinal epithelial cells and induces mucosal inflammation, leading to ulcerative colitis (2).
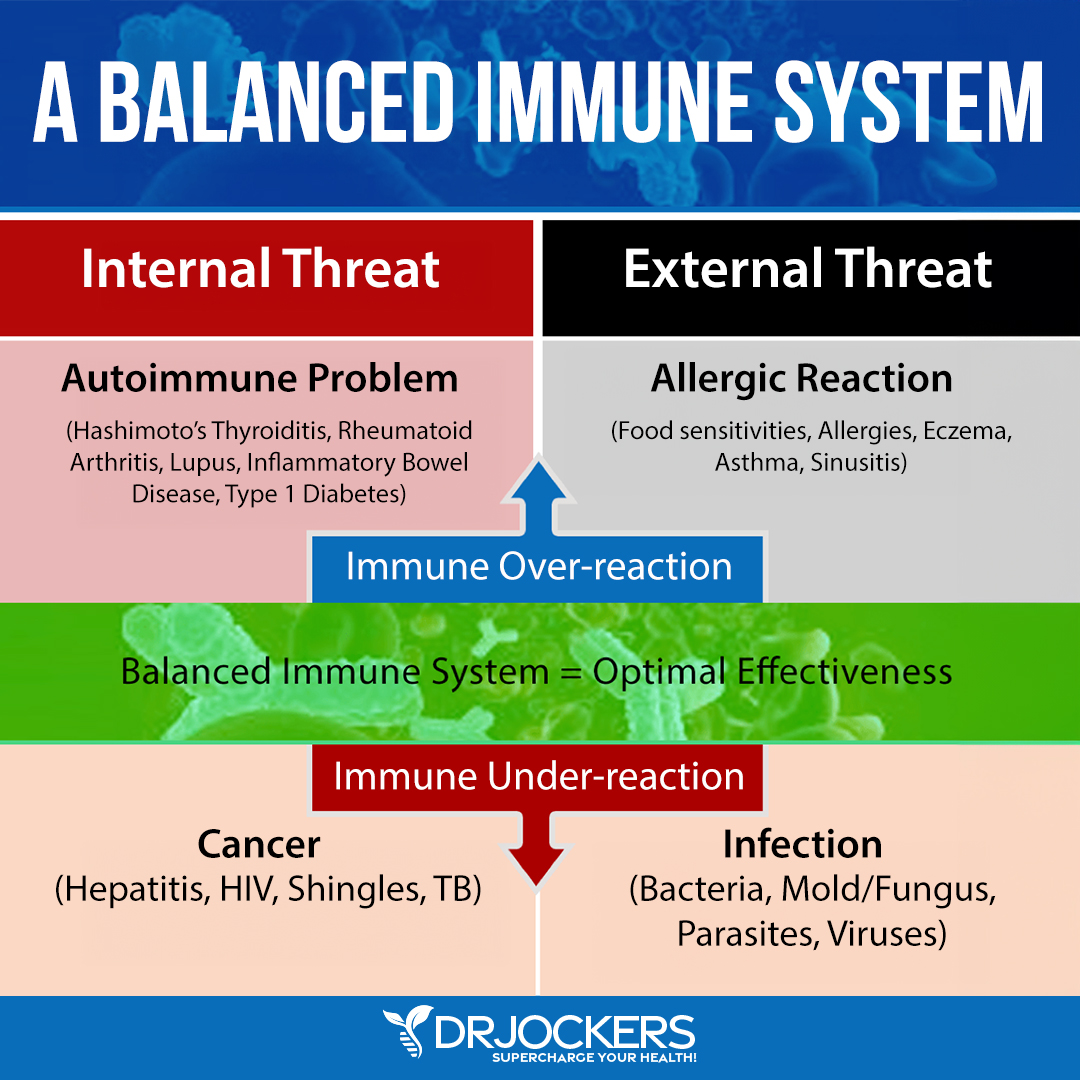
Overactive Immune System and Ulcerative Colitis
The immune system protects the intestinal epithelial cells from pathogens, dietary antigens, and toxins. These factors trigger and activate the immune response creating inflammation as a protective mechanism.
Ulcerative colitis is currently thought to be an autoimmune, or immune-mediated condition. Autoimmune conditions occur when the immune response is overactive and targets healthy tissue. With ulcerative colitis, the immune system has an abnormal immune reaction that targets the large intestine and causes inflammation (1).
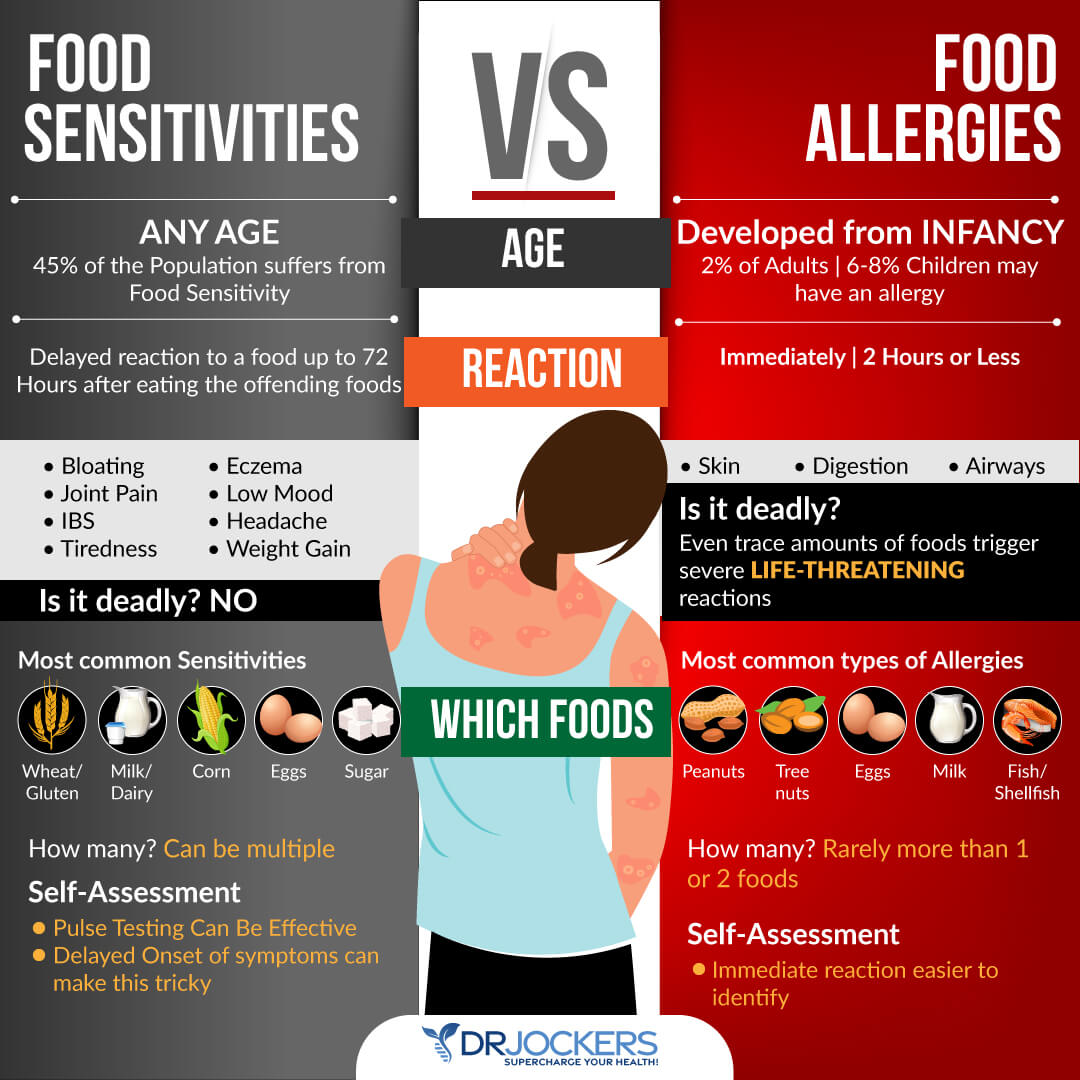
Foods, toxins, and pathogens may cause this overactive immune response. Food sensitivities are one of the primary culprits. When a person has an overactive immune response to certain foods, exposure to these causes the immune system to react to the foods as a threat and produce antibodies (or immunoglobulins) to the food.
Food sensitivities are very common and affect 45-75% of individuals. Gluten, dairy, corn, soy, nuts, eggs, and nightshades are common food sensitivities. If you are sensitive, repeated exposure to these foods inflames the gut lining causing intestinal permeability and digestive problems. For more information on food sensitivities and how to test for food sensitivities, read this article.
Poor Diet
Diet is a huge factor in ulcerative colitis. Eating a highly processed, standard American diet can increase your risk of developing inflammatory bowel diseases (5).
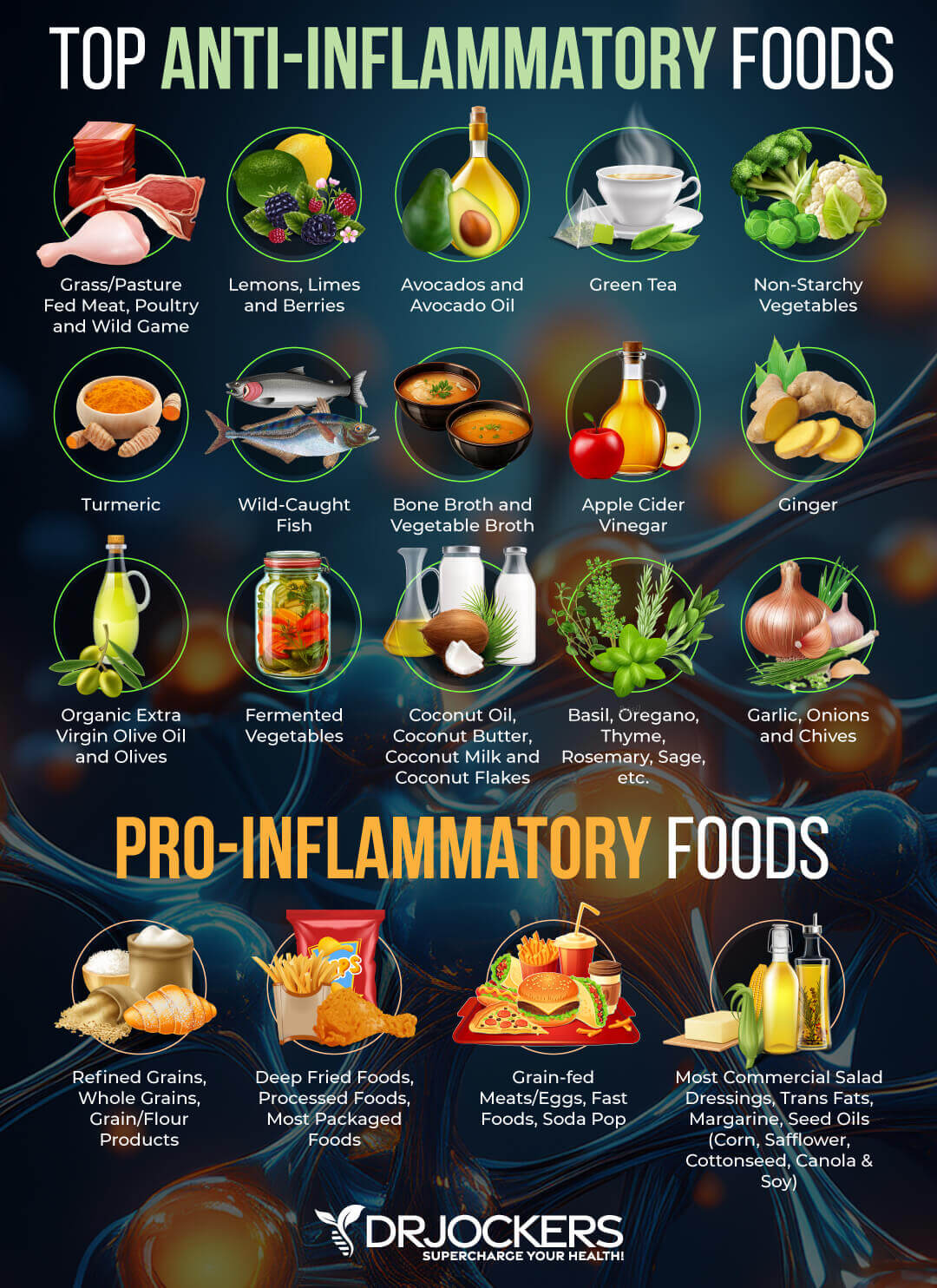
Refined sugars and grains, factory farmed meats, farmed fish, processed foods, and refined seed oils are very inflammatory. When you consume these pro-inflammatory foods, your immune system reacts with an excessive production of pro-inflammatory cytokines and a reduced production of anti-inflammatory cytokines.

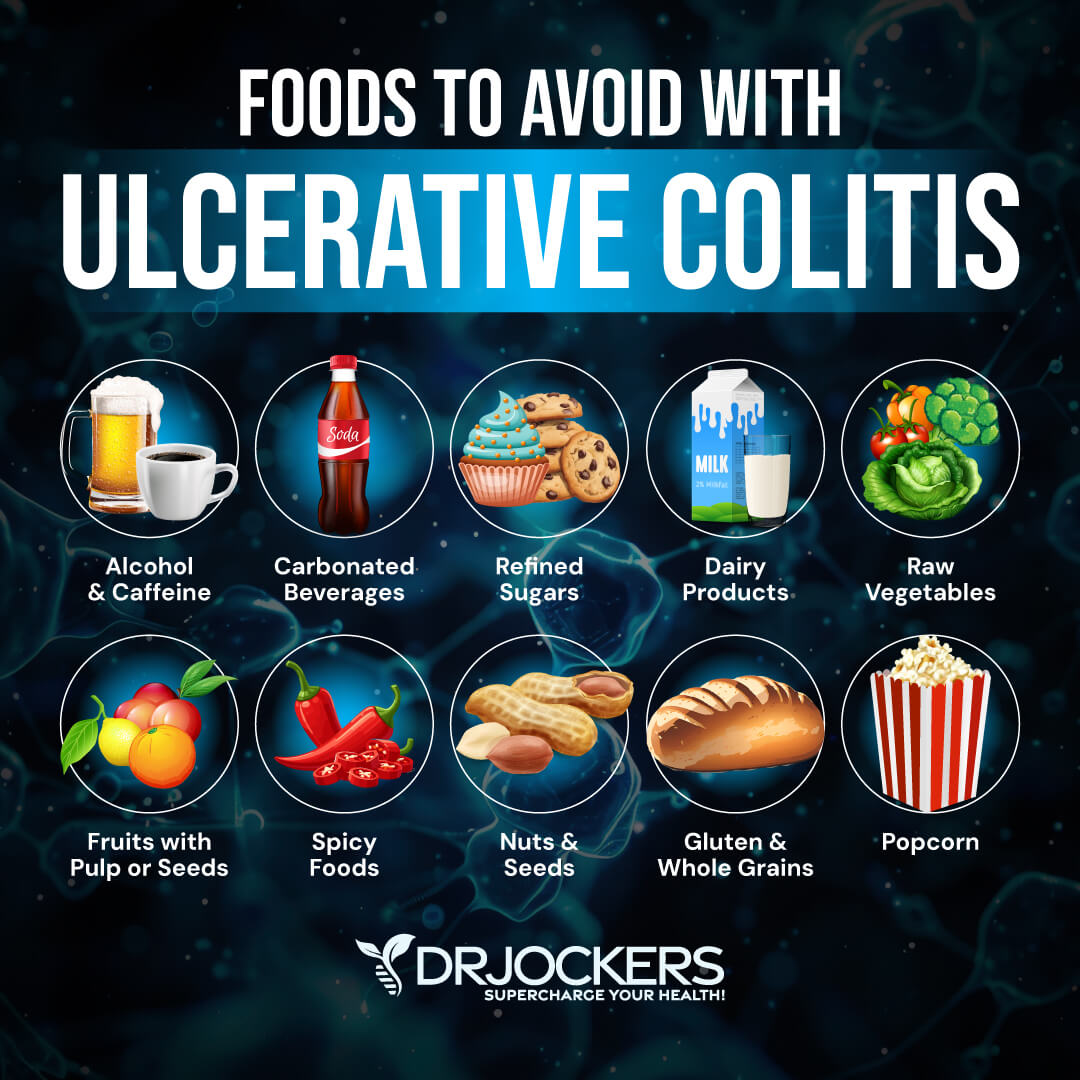
Trigger Foods for Ulcerative Colitis
There are certain foods which may worsen a person’s ulcerative colitis symptoms. Foods that may trigger symptoms of colitis include:
- Alcohol
- Caffeine
- Carbonated beverages
- Refined sugars
- Dairy products
- Raw vegetables
- Dried beans, peas, legumes
- Dried fruits and berries
- Fruits with pulp or seeds
- Sulfur or sulfate containing foods
- High fiber foods
- Spicy foods (including hot sauces)
- Nuts and crunchy nut butters
- Seeds
- Popcorn
- Sorbitol (in many sugar-free gums and candies)
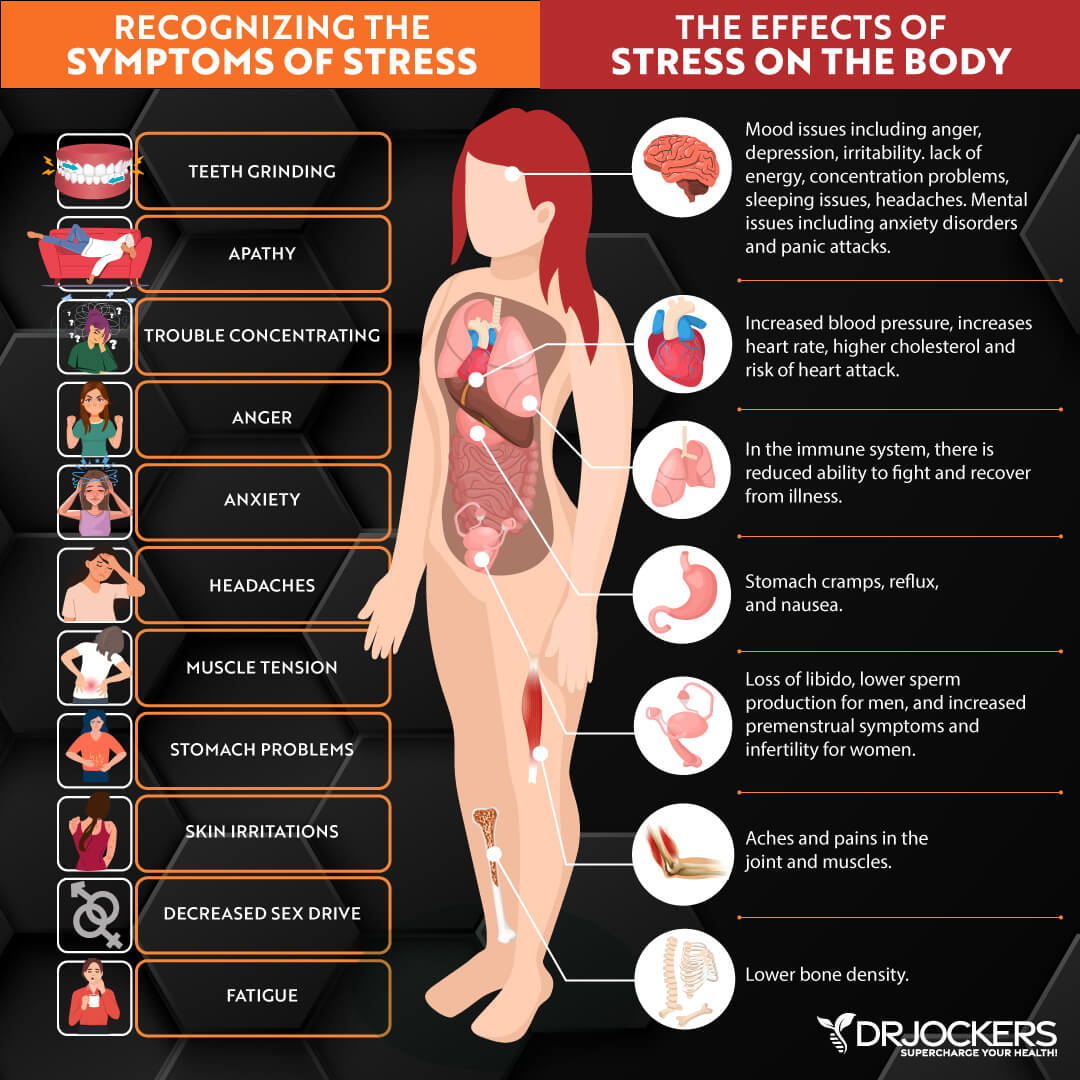
Chronic Stress
Ulcerative colitis is associated with chronic stress (6). This is due to the intricate connection between the brain and the gut. Psychological and physical stressors have effects on gut function and gut-brain interactions. Stress can damage the gut by modulating key inflammatory pathways. It also decreases mucosal blood flow, thereby compromising the integrity of the gut mucosal barrier.
Under conditions of psychological stress, including lack of sleep, the brain (HPA axis) stimulates the production of pro-inflammatory cytokines. Other inflammatory pathways include oxidative stress, sympathetic activity, and transcription factor nuclear factor kappa B (NF-kB). This can result in increased intestinal permeability and altered gut microbiota.
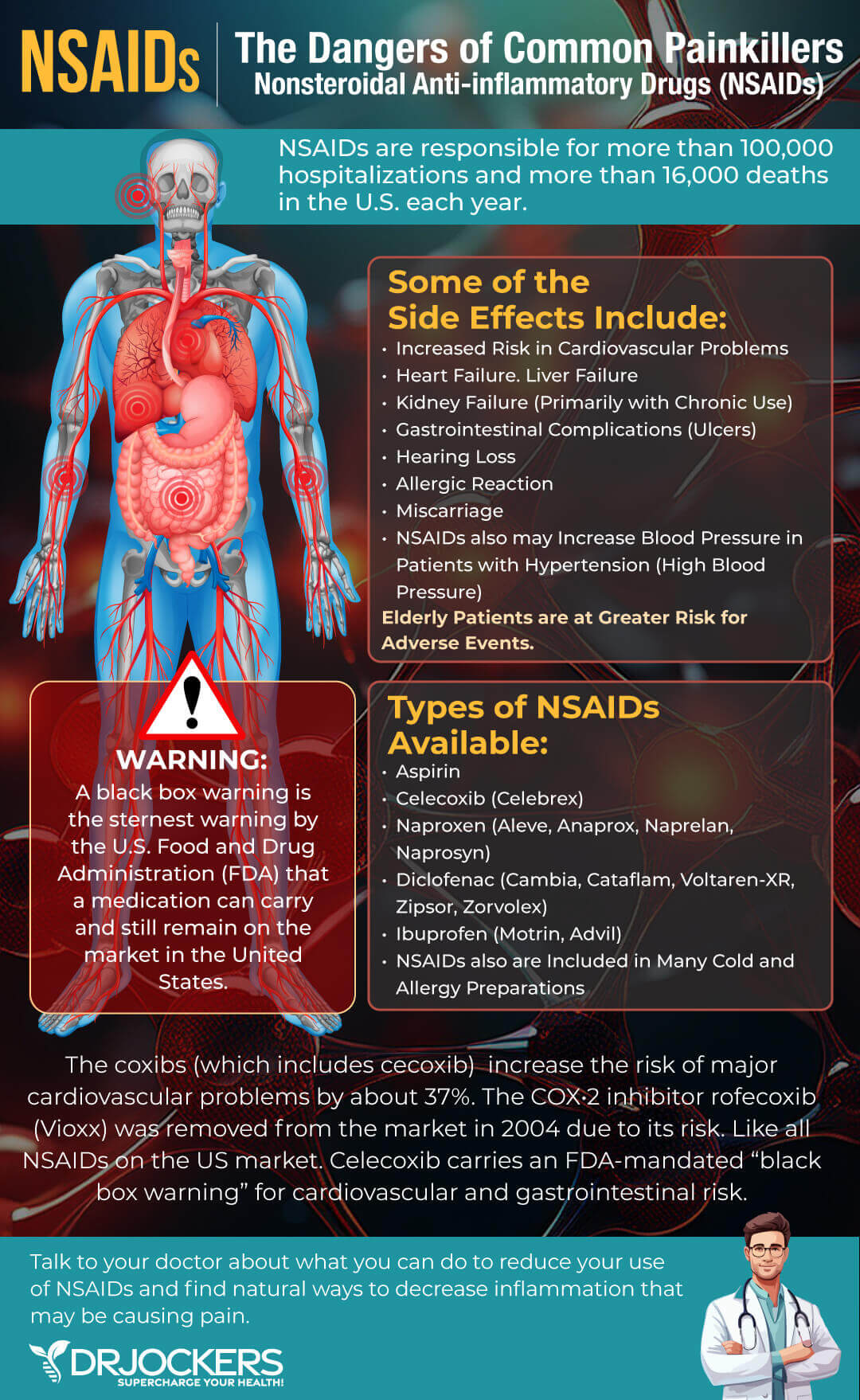
Certain Medications
Anti-inflammatory drugs, antibiotics, and oral contraceptives may increase your risk of developing ulcerative colitis (1). Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) are often used in people with ulcerative colitis. These drugs have the potential to cause irritation and bleeding in the gastrointestinal tract.
Long-term exposure to antibiotics is associated with a higher risk of developing inflammatory bowel diseases. They are often used in the treatment of people with IBD. However, antibiotic usage may lead to adverse outcomes due to their interfering effect on the gut microbiome and influence on the intestinal immune system (2).
Complications of Ulcerative Colitis
There are serious risks and complications associated with ulcerative colitis. These include:
- Perforation of the Bowel: Chronic inflammation weakens the intestinal wall ultimately creating a hole and rupturing the intestine. When there is a hole, a large number of bacteria can spill into the abdomen causing an infection.
- Toxic Megacolon: A rare complication that occurs when the inflammation extends to the deep tissue layers of the large intestine. There is abdominal distention resulting from a dilated colon that loses its ability to contract properly and move intestinal gas along. The distention can be severe and medical attention should be immediately sought to prevent the bowel from rupturing.
- Inflammation in Other Areas of the Body: The immune system can trigger inflammation in the joints, eyes, skin, and liver.
- Dehydration and Malabsorption: This occurs when the large intestine is unable to absorb fluids and nutrients because of diarrhea and inflammation.
- Colon Cancer: The risk of colorectal cancer increases with the severity and duration of colitis.
Digestive Health Support Strategies
Conventional treatment options for ulcerative colitis include medications to reduce symptoms and surgery. These treatments may have serious negative side effects.
Fortunately, alternative natural strategies, including dietary changes and targeted supplementation, may improve digestive health and improve the inflammatory response. While none of these strategies are FDA-approved to prevent, mitigate, treat, or cure ulcerative colitis many people have benefited greatly from implementing them.
Anti-Inflammatory Nutrition Plan
Since ulcerative colitis is an inflammatory disease, one of the most effective strategies for healing is to consume an anti-inflammatory diet. You should remove foods that promote inflammation and replace them with healing foods.
Pro-inflammatory foods to avoid are refined sugars, processed foods, refined vegetable oils, meat and dairy from conventionally raised animals, and farmed fish. These foods contain chemicals, trans-fats, and other toxic ingredients that are highly inflammatory, create extra acidity in the tissues, and damage the gut.
Whole, unprocessed foods that should be included are grass-fed, pastured organic meat and eggs, wild-caught salmon, organic vegetables, and healthy fats. Healthy fats are found in coconut, olives, avocados, and their oils, and in grass-fed butter and ghee.
It is important to eat foods that are easy to digest such as bone broth, soups, and cooked vegetables. Eating smaller meals which will not overwhelm your digestive system may also be helpful.
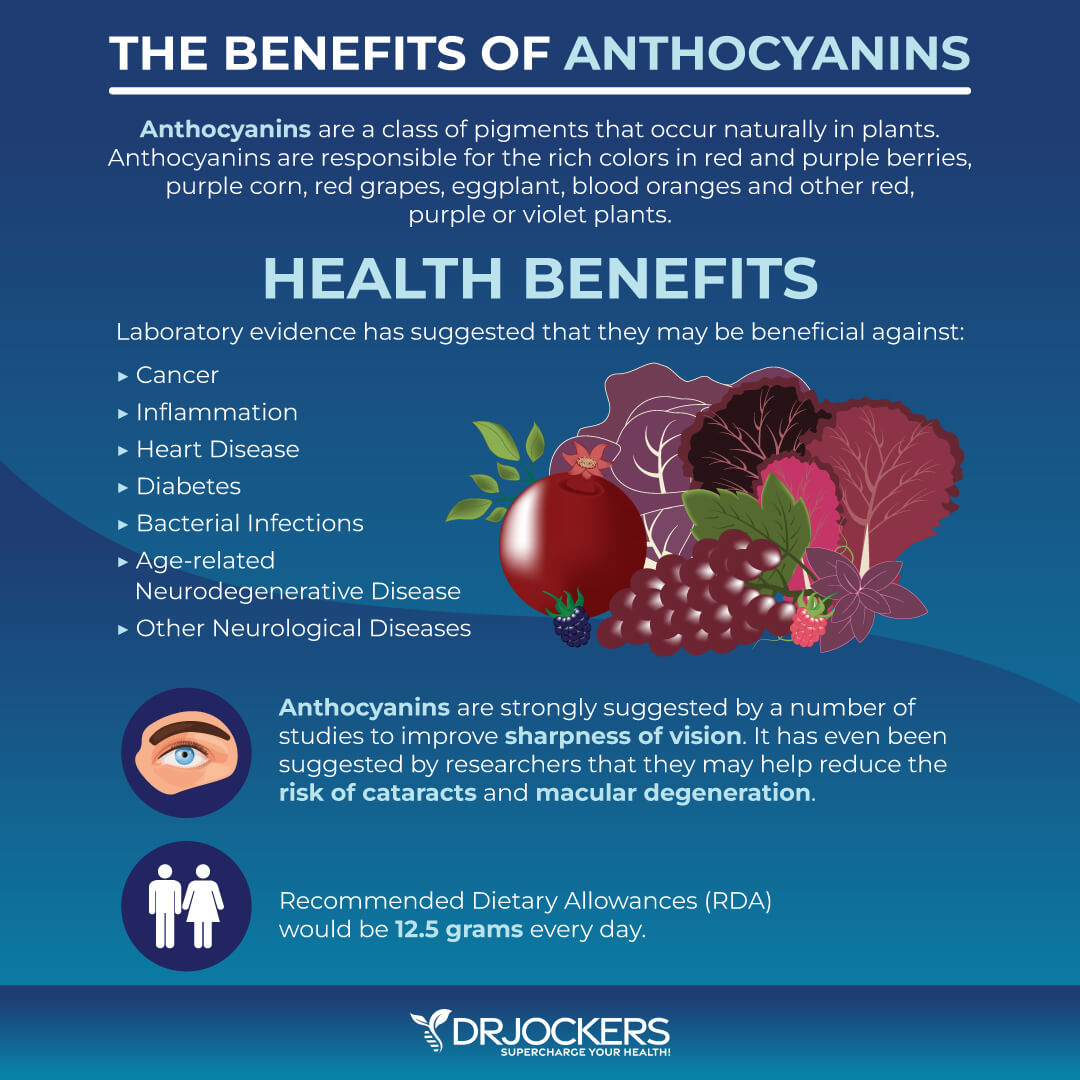
Foods Rich in Anthocyanins
A diet rich in anthocyanins may help with ulcerative colitis (7). Anthocyanins are flavonoids that are responsible for the dark pigments in fruits and vegetables.
Anthocyanins have numerous health benefits due to their anti-inflammatory, antioxidant, anti-obesity, anti-angiogenesis, anti-cancer, anti-diabetes, anti-microbial, neuroprotective, and immunomodulatory properties. They protect against inflammation and increase gut permeability. Anthocyanins also improve colon health through their ability to alter bacterial metabolism and the microbiome within the intestines.
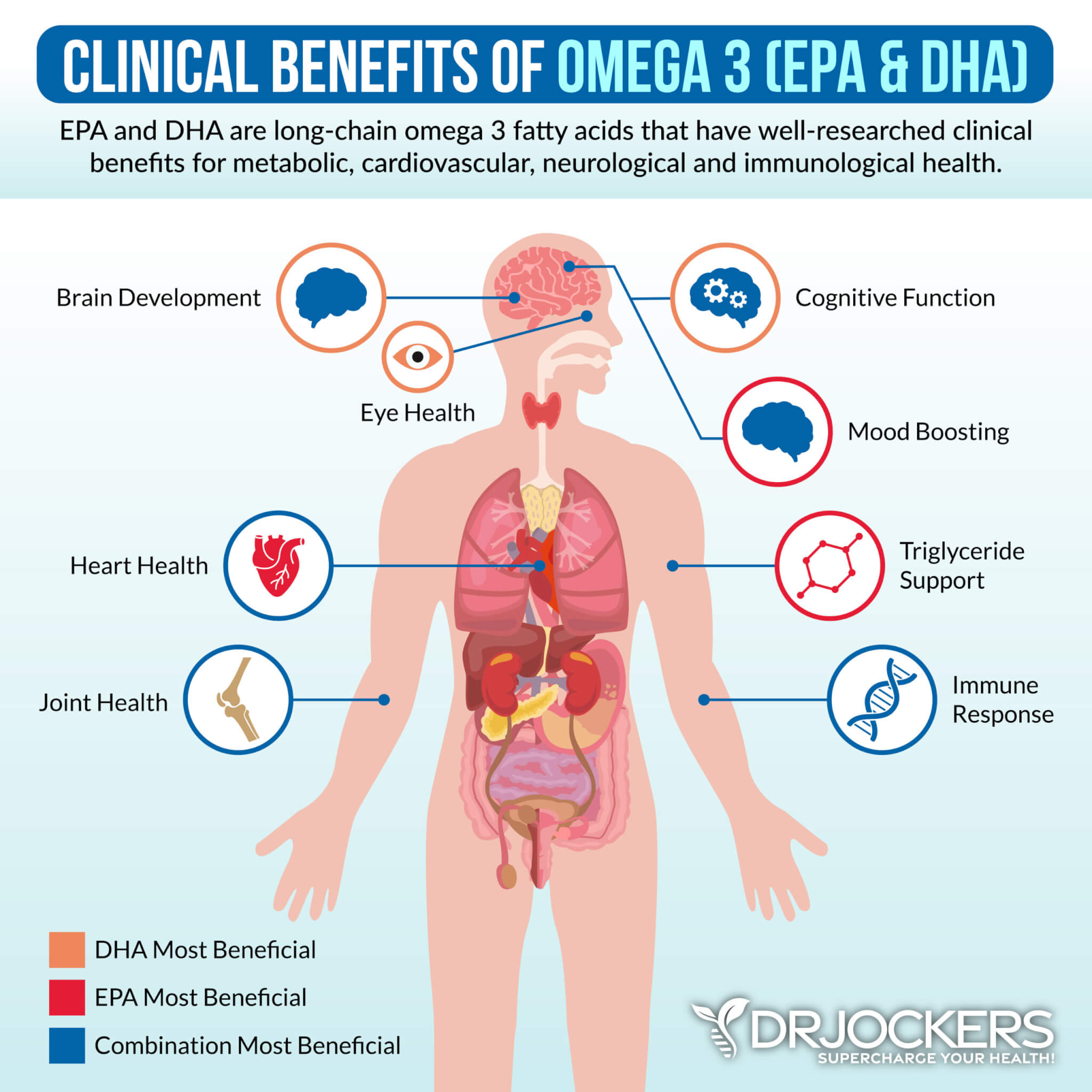
Omega 3 Fatty Acids
Studies show that fish oils have protective benefits and can help heal ulcerative colitis (8). Omega 3 fatty acids reduce intestinal inflammation and induce and maintain clinical remission in people with ulcerative colitis. Consuming fatty acids may also reduce the risk of developing inflammatory bowel disease.
Omega-3 fatty acids are found in fatty fish such as wild-caught salmon and sardines, grass-fed meats, pasture-raised eggs, nuts (especially walnuts), and seeds (flax, hemp, pumpkin, and chia seeds). It can be difficult to maximize your levels of omega-3s with food so supplementation may be beneficial.
Plant-based omega 3’s such as flax oil only contain the small chain omega 3 called ALA and do not have any DHA. It is very hard for our body to convert ALA into DHA, so it is best to get a high-quality fish or krill oil that is rich in EPA and DHA. You want to find a brand that is molecularly distilled to take out any heavy metals and other unwanted contaminants.
Identify and Remove Food Triggers
Ulcerative colitis can be triggered by a variety of foods. To heal from ulcerative colitis, it is important to identify and remove foods from your diet that aggravate your symptoms.
Food sensitivities can be hard to identify. This is because symptoms of food sensitivities are usually delayed up to 72 hours after consuming the offending food. For information about different methods of testing for food sensitivities, check out this article.
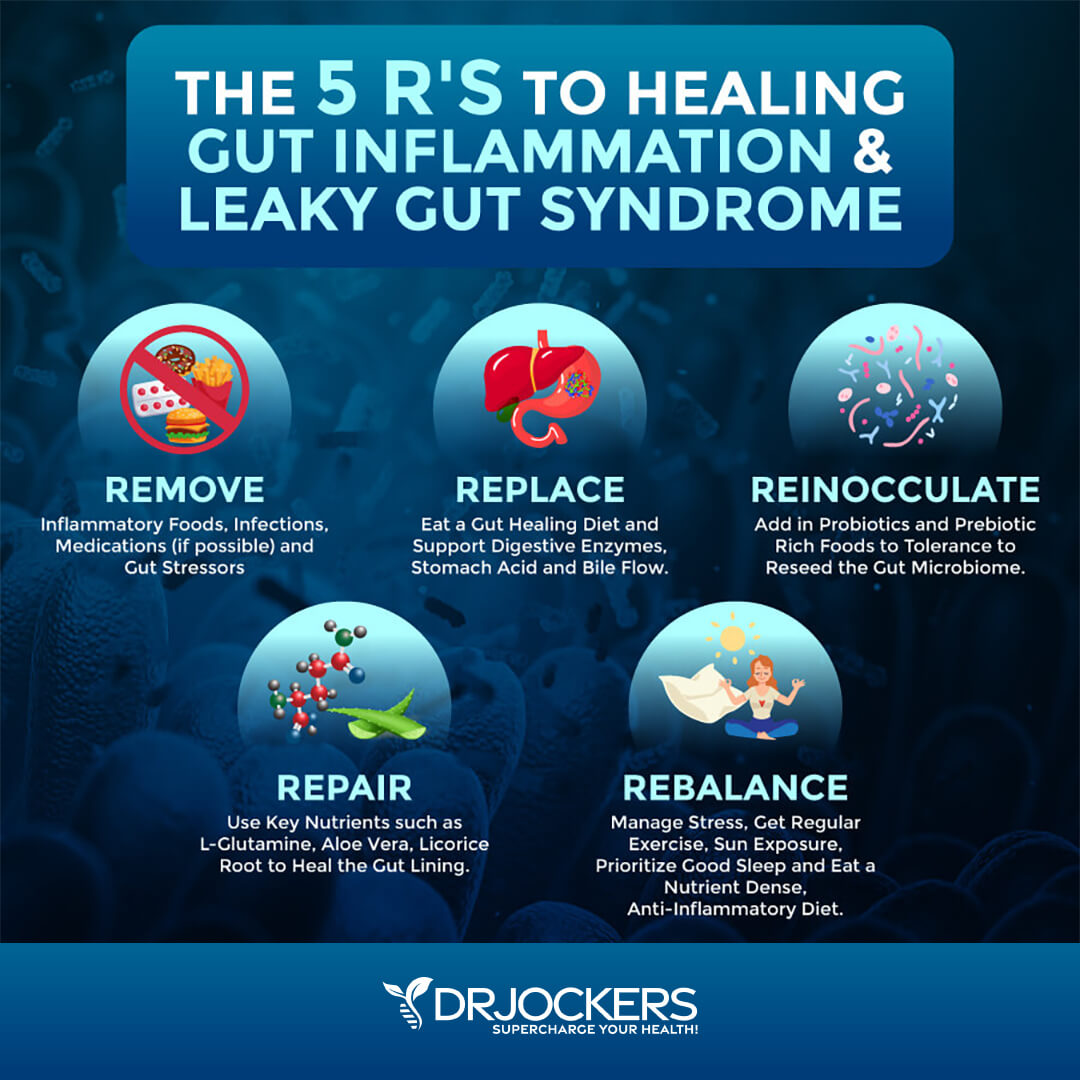
Support the Gut Mucosa
Ulcerative colitis involves inflammation of the gut mucosal layer. To heal from ulcerative colitis, it is critical to support your gut mucosa. Reducing stress on the gut with liquid nutrition and fasting, along with targeted supplements to repair the gut, can be very effective.
Consuming liquid nutrition is great for stimulating the digestive process, increasing nutrient absorption, and improving gut health. Liquid nutrition does not require as much energy to digest, so your body can focus on healing and repair. You can combine liquid nutrition with fasting strategies for quicker healing.
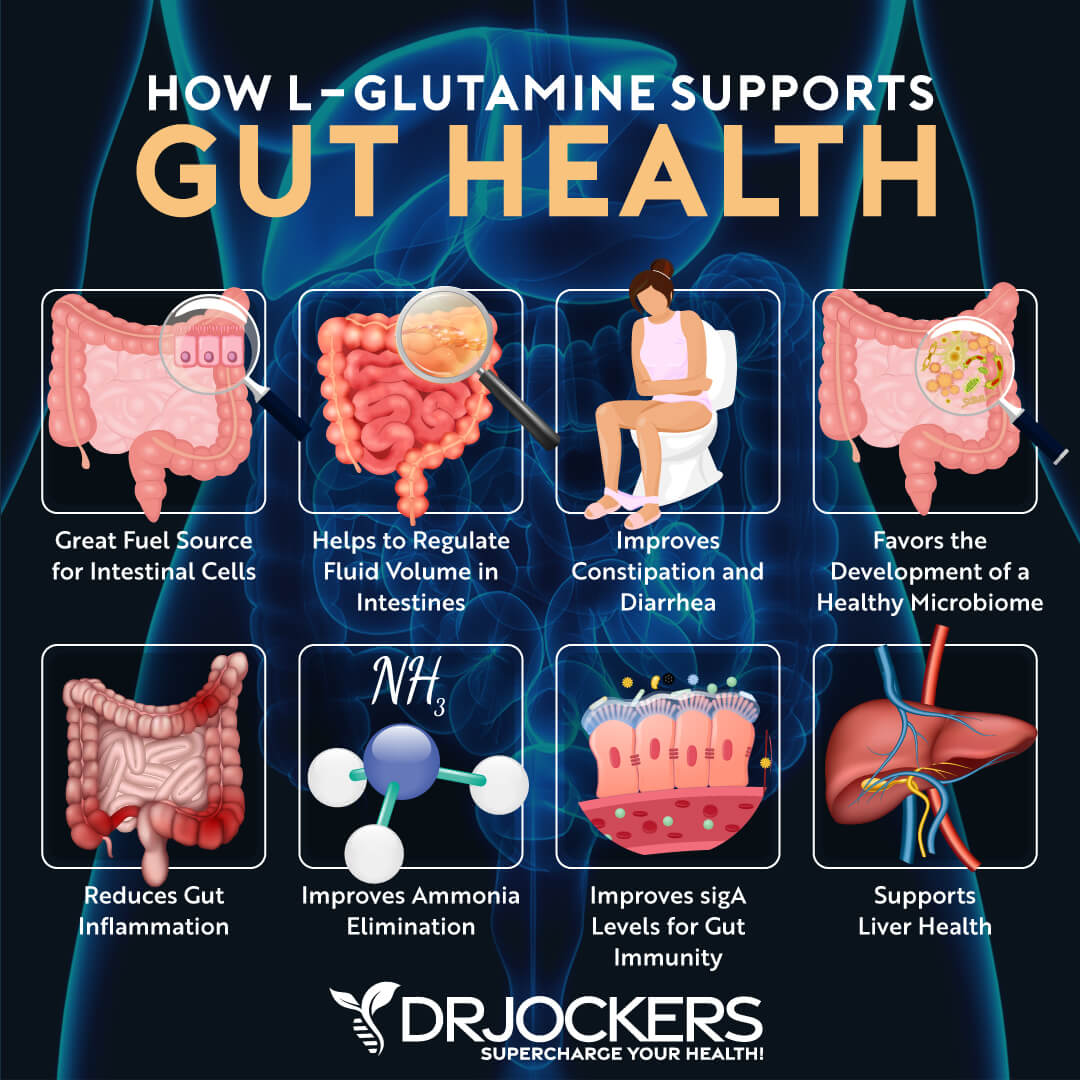
Using a good quality bone broth collagen in a shake or smoothie is a great way to include liquid nutrition in your diet. Collagen contains amino acids, including glycine and glutamine, which are essential for healing leaky gut. These amino acids seal the holes in the gut by healing damaged cells and building new tissue. Collagen also makes up the villi, small finger-like structures on the intestinal wall, and assists with water absorption in the intestines.
Key Supplements for Gut Mucosa
For mucosal support, I also like herbs and nutrients like aloe vera, licorice root, vitamin C, colostrum, and dairy-free, bovine serum-derived (BSD) immunoglobulin concentrate. These all act to support gut barrier function, improve immunity, and decrease inflammation in the gut.
The immunoglobulins in colostrum and BSED immunoglobulin concentrate work to bind to environmental toxins, neutralize pathogens, and improve gut mucosal immunoglobulin sIgA levels. Using L-glutamine supplements can help to repair leaky gut and soothe and protect the gut mucosa as this is the primary amino acid that strengthens the intestinal lining.
Balance Gut Microbiome
Improving the microbial balance in your gut is very important to heal from ulcerative colitis (2). Probiotics are very important in the management of this condition (9) They are used to treat and maintain remission in people with ulcerative colitis.
Probiotics are beneficial microorganisms (bacteria and yeasts) that are similar to the microorganisms that naturally live in our bodies. Probiotics work through different mechanisms to support gut health and downregulate the effects of bacteria in initiating and sustaining an intestinal inflammatory response.
There are 4 main categories of probiotics: food based, spore-forming soil based, probiotic yeast, and combination probiotics. You can rotate these probiotics to see which one you feel the best to take.
Researchers are also using fecal microbiota transplantation in people with ulcerative colitis. While the results are promising, there is uncertainty about the potential side effects of this treatment (4).
Reduce Stress and Improve Sleep
Chronic stress and lack of sleep may lead to the development of ulcerative colitis and worsen symptoms of the condition (6). To help manage stress and improve sleep, it is critical to follow an anti-inflammatory diet and balance your blood sugar levels. Additional stress relieving techniques are grounding, deep breathing exercises, sunlight exposure, Epsom salt baths, and dry brushing.
Sleep deprivation is associated with the production of proinflammatory cytokines and an increased risk of ulcerative colitis (10). Strategies for better sleep are getting sunlight during the day, avoiding artificial light and EMFs, blacking out your room with blackout curtains or using a sleep mask, and being smart about caffeine intake. It is also helpful to turn off electronics, practice good hygiene, stretch, practice gratitude, journal, pray, and implement other healthy sleep habits.
Supplementing with adaptogenic herbs, such as ashwagandha, rhodiola, ginseng, and holy basil may help your body resist and recover from everyday stress and support restful sleep. Using supplemental magnesium may also be helpful as magnesium plays a critical role in stress and sleep.
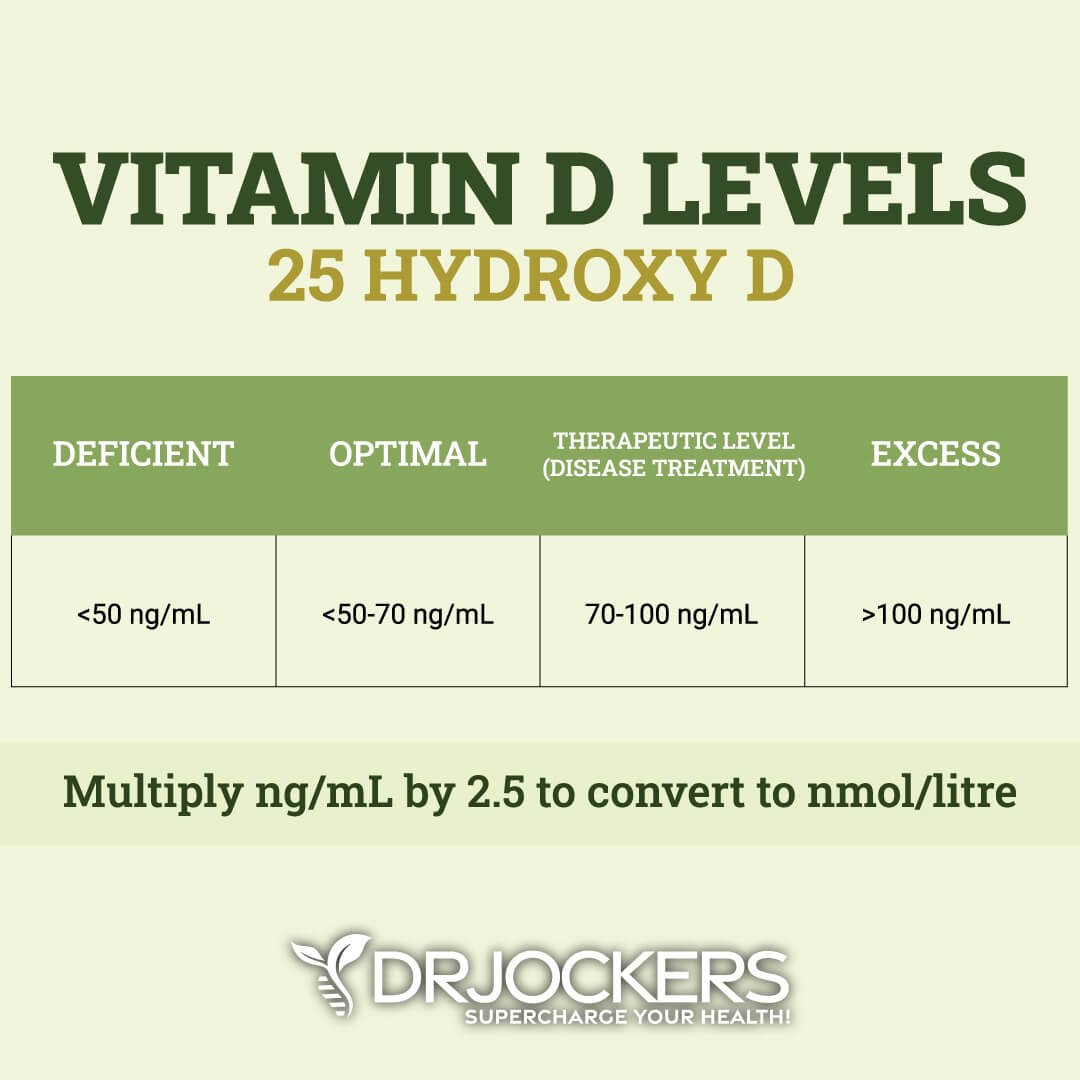
Optimize Vitamin D Levels
Vitamin D is critical for immune regulation. As an immunomodulator, vitamin D targets various immune cells, including monocytes, macrophages, dendritic cells, as well as T-lymphocytes and B-lymphocytes. Several epidemiological studies have linked inadequate vitamin D levels to a higher susceptibility to immune-mediated disorders including chronic infections and autoimmune diseases (11).
Deficiency in vitamin D is associated with the pathogenesis of diverse autoimmune disorders and contributes to inflammatory bowel diseases (6). The ideal range for vitamin D3 levels is between 50-80 ng/ml.
To maintain optimal levels, you can use a high-quality supplement and take around 1,000 IU’s per 25lbs of body weight. I recommend finding a D3 that also has vitamin K2 in it as well and getting your vitamin D3 (25-OH) tested once or twice a year to make sure you know your levels.
Testing for Underlying Causes of IBS
GI Map Stool Analysis
The GI-MAP™ Stool Analysis Test is the most thorough stool test on the market. It is the only FDA-approved DNA test for gastrointestinal microbes and pathogens available. This test includes calprotectin which is a reliable marker for the detection of colonic mucosal inflammation in ulcerative colitis (12).
The GI Map measures imbalances in the gut microbiome which are common with ulcerative colitis. It also tests for candida and other fungi, and parasites, including both protozoa and worms. This comprehensive stool test can reveal if you have H. pylori, viral pathogens, potential autoimmune triggers, and viruses, including cytomegalovirus and Epstein Barr virus. These bacteria and viruses may contribute to the development and worsen symptoms of ulcerative colitis.
The GI Map also reveals the integrity of your gut mucosa with digestion, gastrointestinal, and Secretory IgA levels. This is an important test for anyone with ulcerative colitis. For more information on the GI-MAP and how to order, go here.
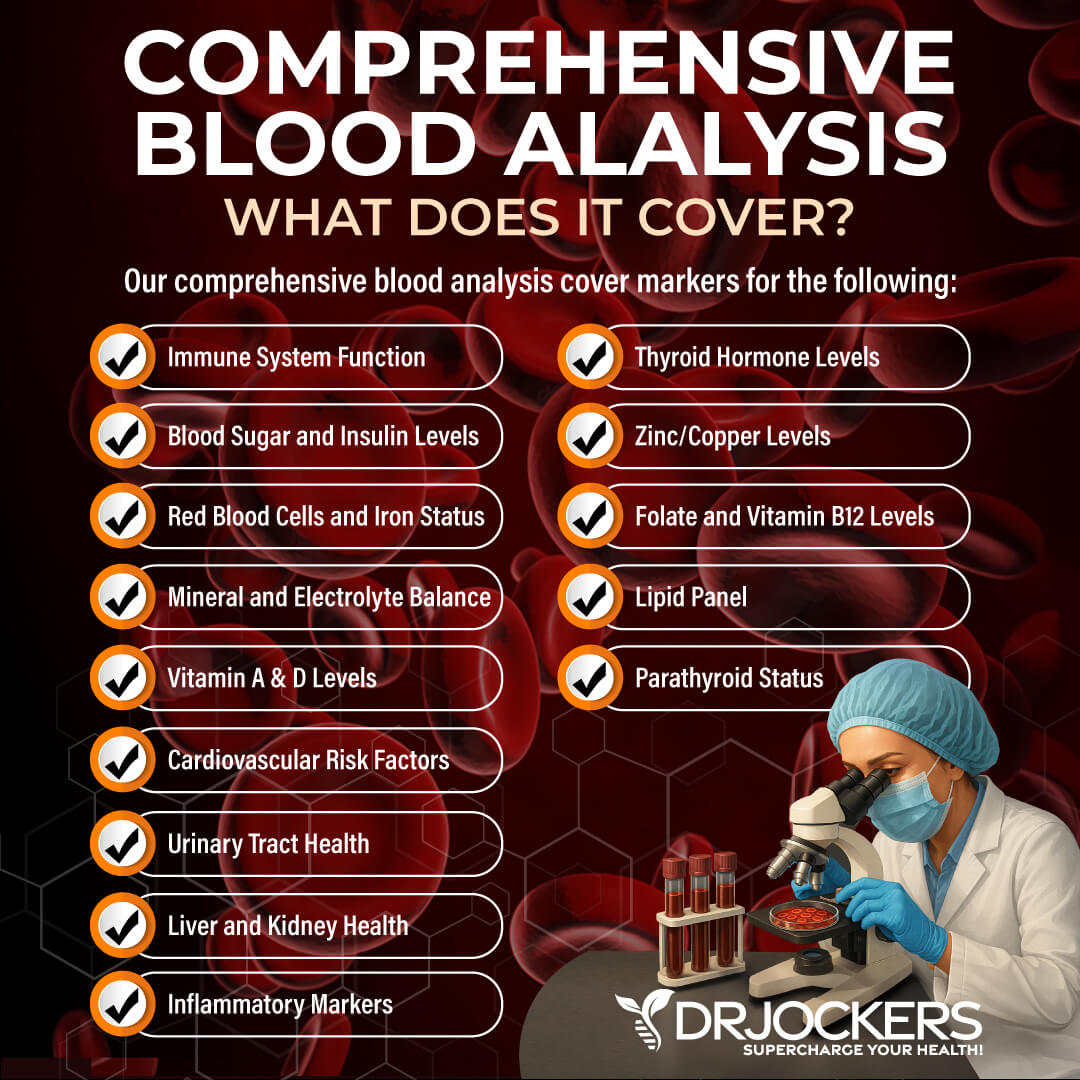
Comprehensive Blood Analysis
A blood test may help diagnose ulcerative colitis. Indications of ulcerative colitis include anemia, inflammation, and low albumin or protein. These tests are included in the Comprehensive Blood Analysis.
The C-Reactive Protein (CRP) test is a blood test used to assess levels of inflammation in the body. CRP is a protein produced in the liver. It is an acute phase reactant, which means it increases or decreases in concentration with inflammation or trauma.
CRP is useful in diagnosing and monitoring chronic inflammatory conditions such as ulcerative colitis. Other tests that measure or indicate inflammation are the Red Blood Cell Width (RBCW), ferritin, and erythrocyte sedimentation rate (ESR).
The Comprehensive Blood Analysis also measures vitamin D, zinc, and iron. Suboptimal levels of these micronutrients are associated with an increased risk of inflammatory bowel diseases. In fact, low vitamin D status is a biomarker for disease activity and a predictor of poor clinical outcomes in IBD patients (13).
Consider Working with a Functional Health Coach
The functional nutrition and functional medicine approach looks at the body as a summation of systems rather than overly specific mechanisms. Hence a functional health coach can offer a truly holistic approach and support for your health.
They can help to run and analyze specific labs, guide you with an anti-inflammatory autoimmune dietary plan, suggest beneficial supplements, and coach you along the way. Your coach is your guide, support, and personal cheerleader who helps to empower you to create the healthiest version of yourself.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Conclusion on Ulcerative Colitis
Ulcerative colitis is a chronic and relapsing intestinal inflammatory condition. It results in inflammation and ulcers of the colon and rectum. There are a number of symptoms of ulcerative colitis, primarily abdominal pain and bloody diarrhea.
When symptoms are severe, ulcerative colitis can lead to serious and even life-threatening complications. Conventional treatments for this condition have unwanted negative side effects, so using natural approaches is beneficial for improving digestive health and the inflammatory response.
Addressing the causes of ulcerative colitis along with implementing natural strategies to improve the condition can lead to major improvements in symptoms. You should also monitor the condition with stool and blood tests to measure inflammation, nutrient deficiencies, and gut health.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!






Hi doctor I have ulcrative colitis from 6 years i am taking medicine pentasa and asacol and I have thyroid and all my muscles pain can you help me what can I eat what food can help me, thank you.
So sorry to hear this! I would recommend working with a functional nutrition practitioner. Here is a helpful article on how to find a good one: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/