 The 9 Best Ways to Test Blood Sugar Levels
The 9 Best Ways to Test Blood Sugar Levels
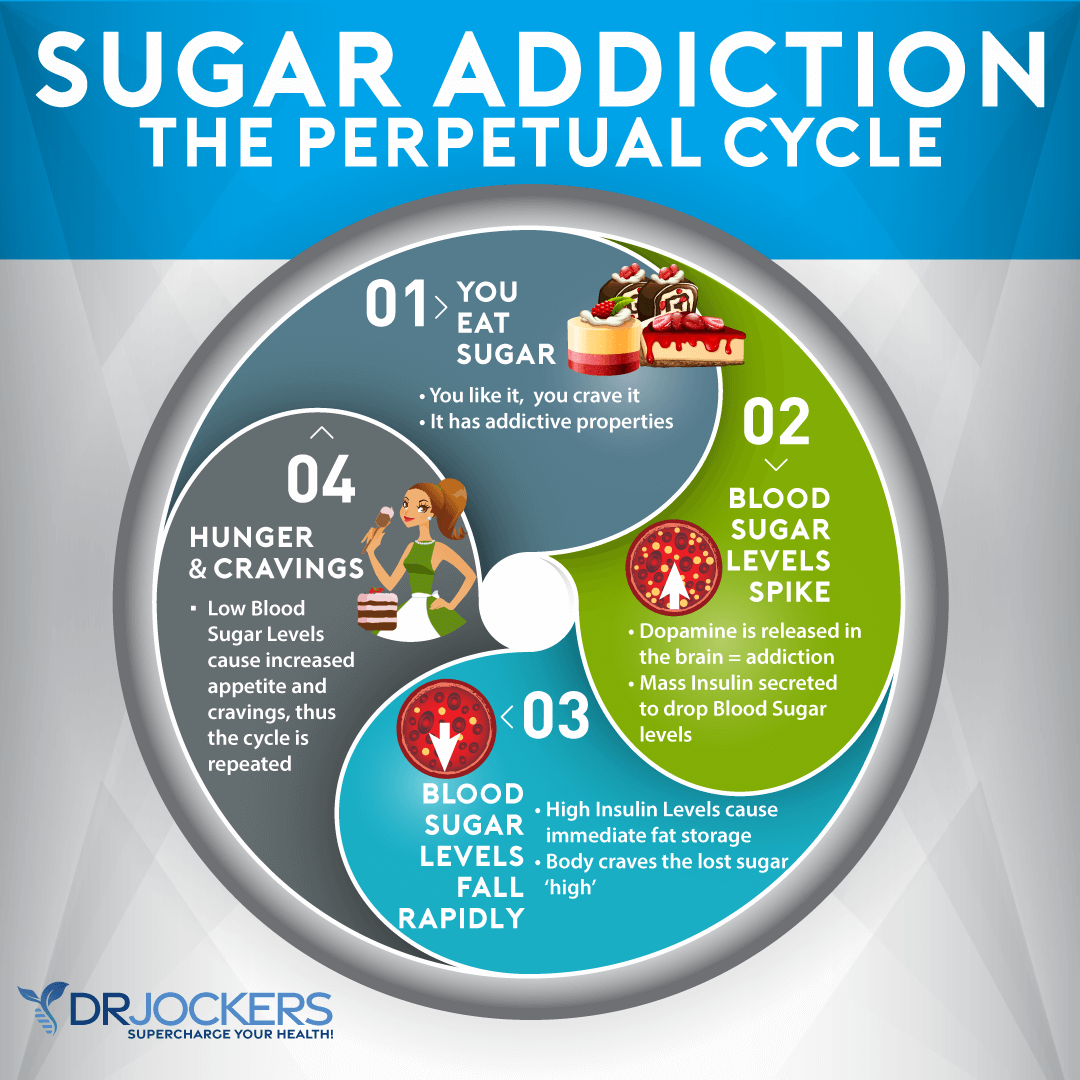
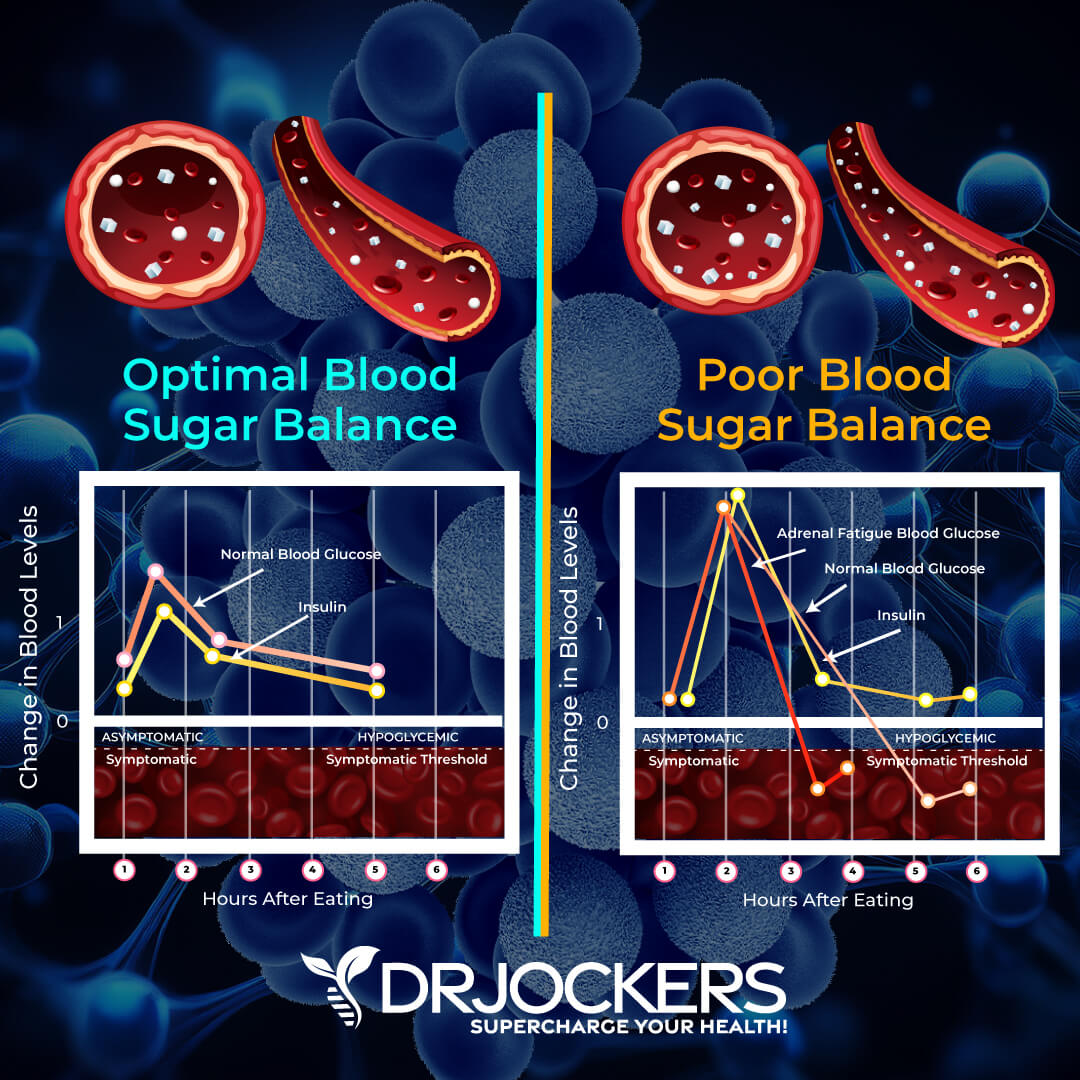
Blood sugar instability is one of the most overlooked foundations for healthy living. If you have poor blood sugar control, you will feel like you are riding the energy rollercoaster complete with intense cravings, unwanted weight gain, and chronic inflammation. Taking advantage of ways to test blood sugar control can help you reach balance and take control of your ability to burn fat.
Once you are armed with the knowledge of your own blood sugar control, you can take steps to get it back where it needs to be. Most people have no idea that this one aspect of health could be the single thing holding them back from reaching their health goals.
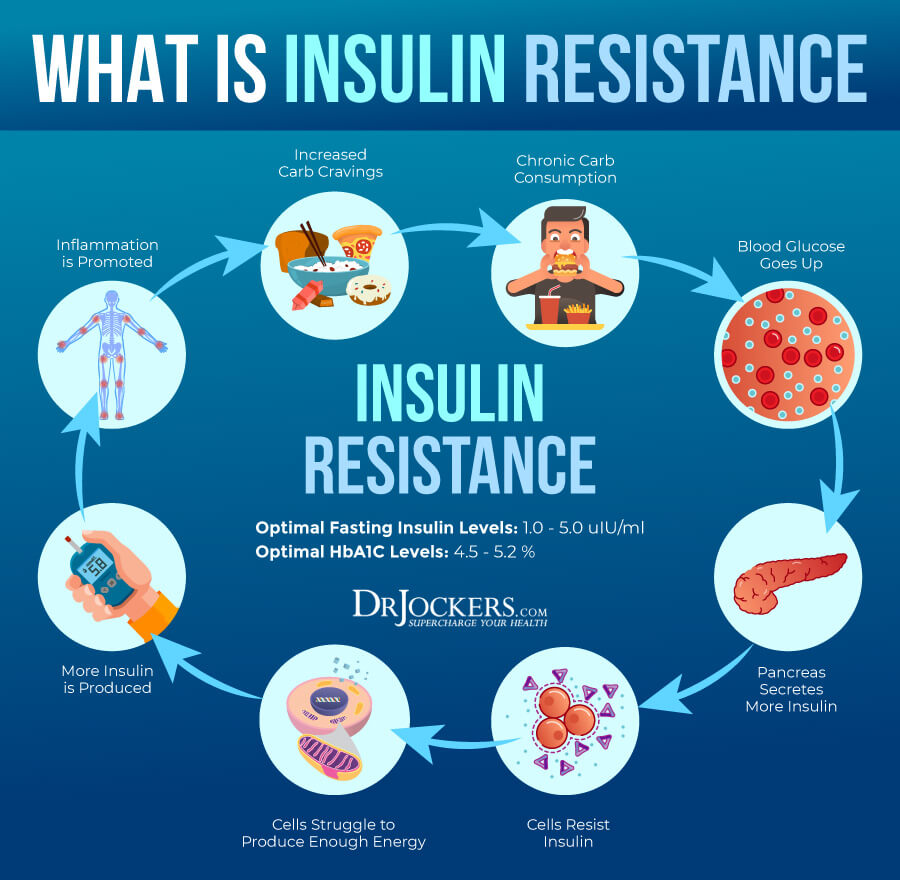
Insulin Resistance
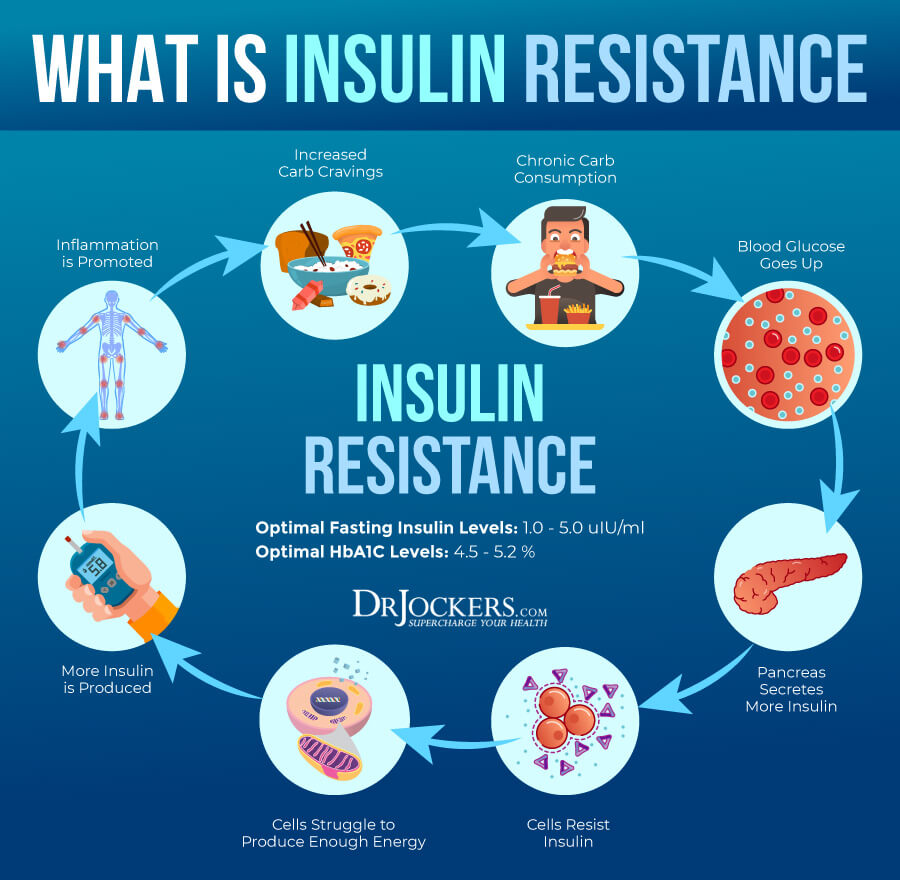
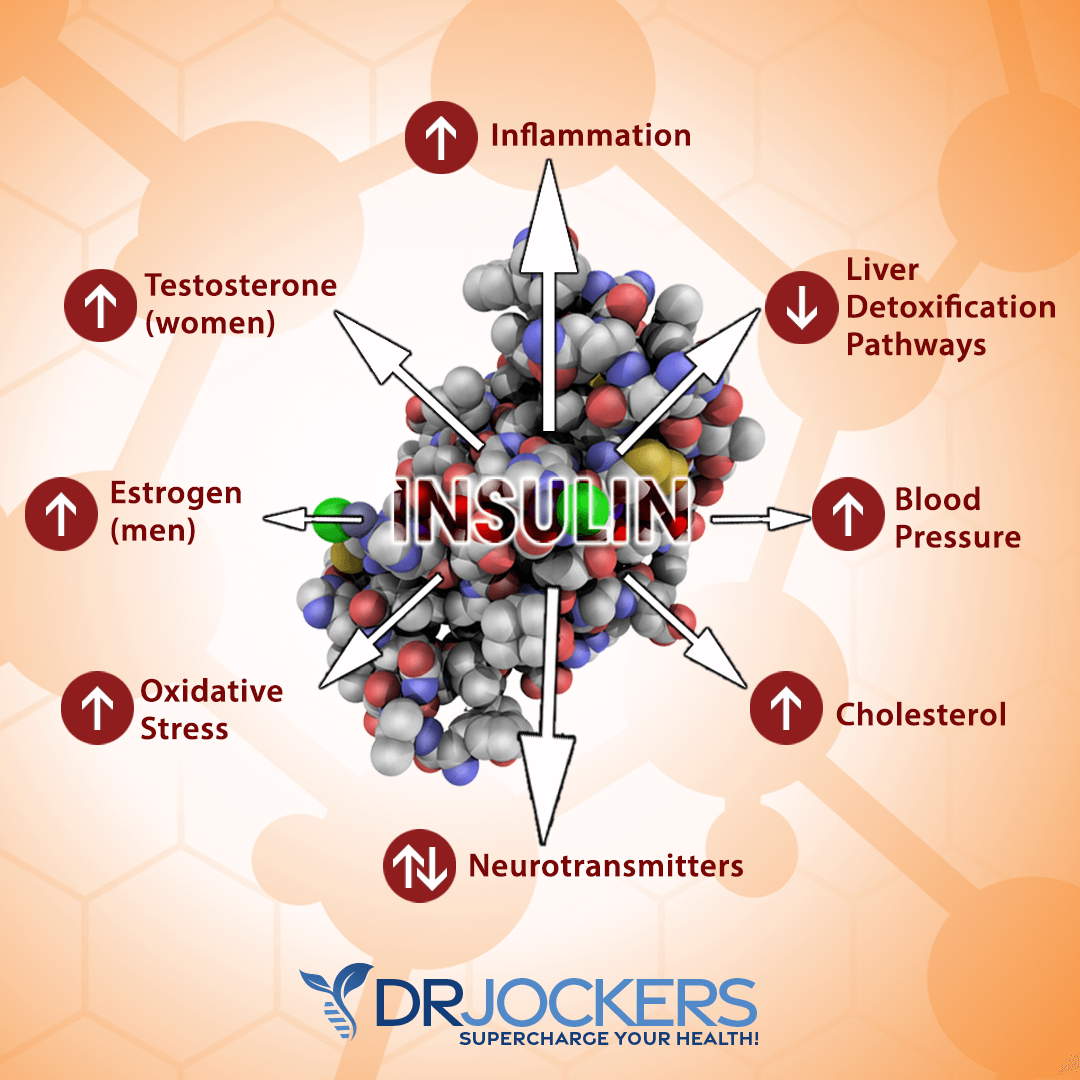
Insulin is a transport molecule in the body that takes sugar in the blood and helps transport it into cells for energy. When we are constantly consuming high amounts of sugar, it is possible to develop insulin resistance. Essentially, cells become desensitized to insulin and stop responding to it. When this happens, sugar cannot get into your cells.
Over time, the body produces more insulin to get sugar into the cells. Unfortunately, there is a threshold where more insulin starts to create problems in the body.
Consistently high insulin levels will increase inflammation, promote fat gain, and ultimately open the doors to many different chronic diseases. You can prevent this from happening by using the methods in this article to test blood sugar periodically.
Advanced Glycation End Products
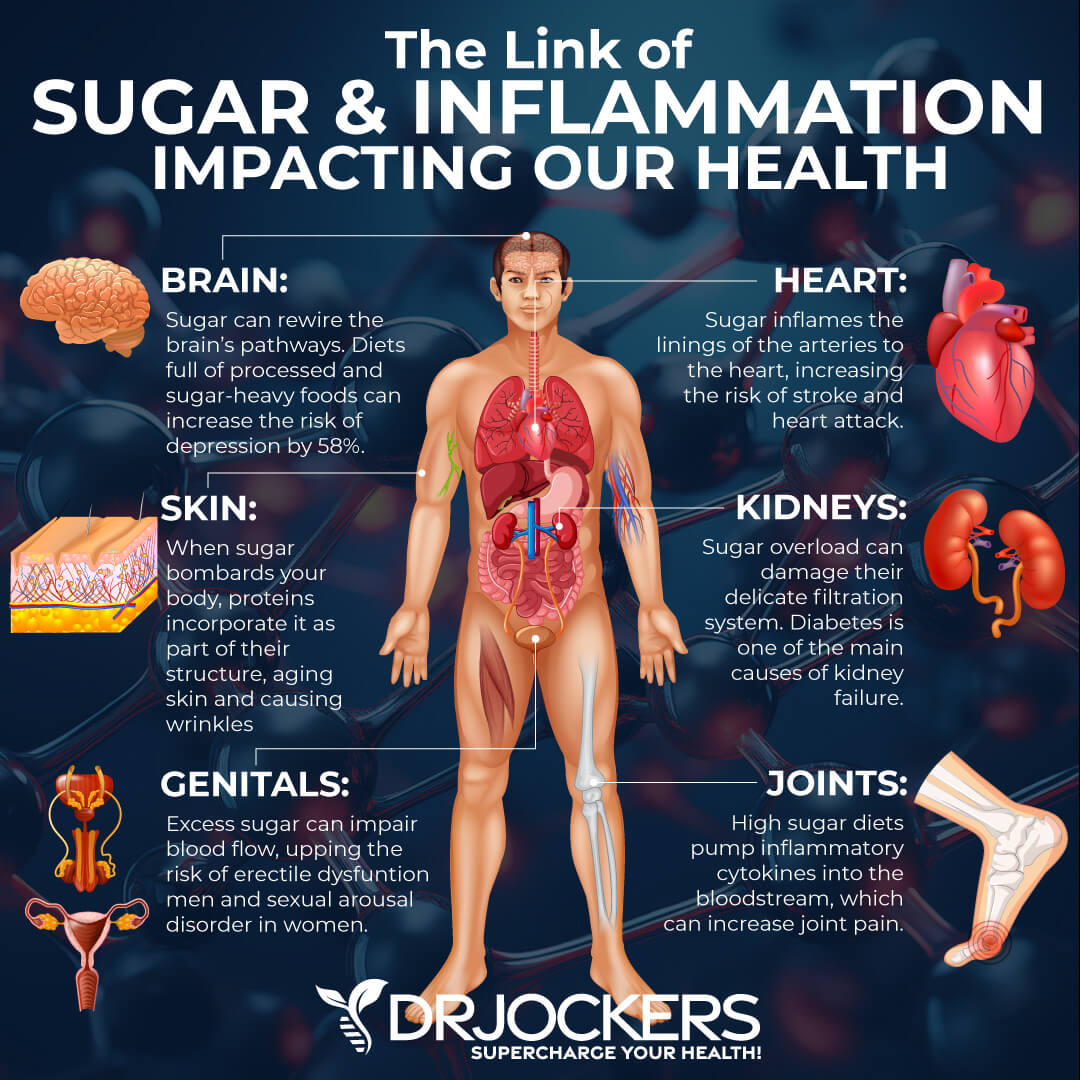
One of the biggest problems with high blood sugar is that the sugar molecules bind to proteins and enzymes in the bloodstream and create advanced glycation end products otherwise known as AGEs. AGEs are highly unstable and break down structural proteins throughout the body and accelerate the aging and degenerative processes of all organs and tissues in the body (1).
When the body has healthy insulin sensitivity, insulin clears the bloodstream of sugar and keeps AGEs under control. However, when we develop insulin resistance, we are no longer able to effectively manage AGE formation, and we end up with increased inflammation and tissue damage.
By the time, we develop diabetes, our bodies have been ravaged by AGEs and all of our organ systems are 10-20+ years older than they should be due to the accelerated degeneration brought on by this glycation process. In uncontrolled diabetes, these AGEs destroy the nerves leading to optic neuritis, peripheral neuropathy, and dementia (2).
The kidneys are also hit hard by these AGEs, which results in kidney failure for many diabetics and congestive heart failure as the blood vessels are highly damaged (3, 4).
Blood Sugar Instability Symptoms
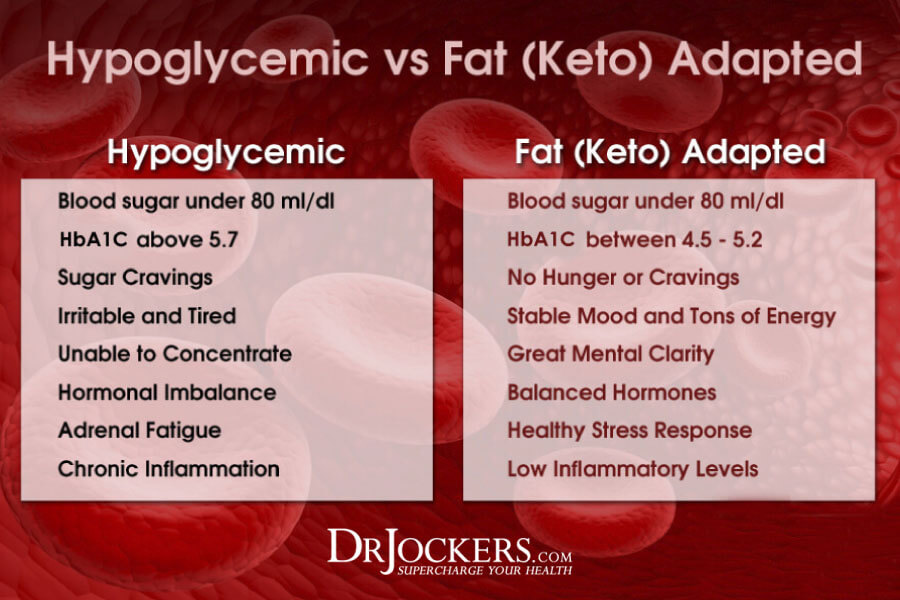
Insulin resistance does not happen all-of-a-sudden. Rather it builds over time and increasingly contributes to health problems. Understanding the signs of poor blood sugar control is the best way to be proactive in this regard. There are several telling signs that your body is not stabilizing blood sugar effectively.
Some of the most common include:
- Cravings
- Weight Gain
- Brain Fog
- Unstable Energy Levels
- Sudden Intense Hunger
Most commonly, these symptoms arise simply because someone is consuming too many carbohydrates and sugar throughout the day. This is why I always start with a low-carb, anti-inflammatory nutrition plan to kick start a fat-burning state and help people step off the blood sugar rollercoaster. If you are commonly experiencing these symptoms, it is imperative to test blood sugar levels periodically as these symptoms can be effectively controlled by doing so.
Pre-Diabetes
You may not know this, but prediabetes is actually much more common than you might think. If you are experiencing the symptoms above, you likely are living in a pre-diabetic state. Insulin resistance is characteristic of pre-diabetes, and it is estimated that about 18% of all Americans are currently experiencing it (5).
Clinically, prediabetes is diagnosed when you test blood sugar and fasting blood glucose is between 100-126 mg/dl. Ideally, you would want this number to be less than 90 mg/dl. I am going to cover how to test blood sugar for yourself in a moment.
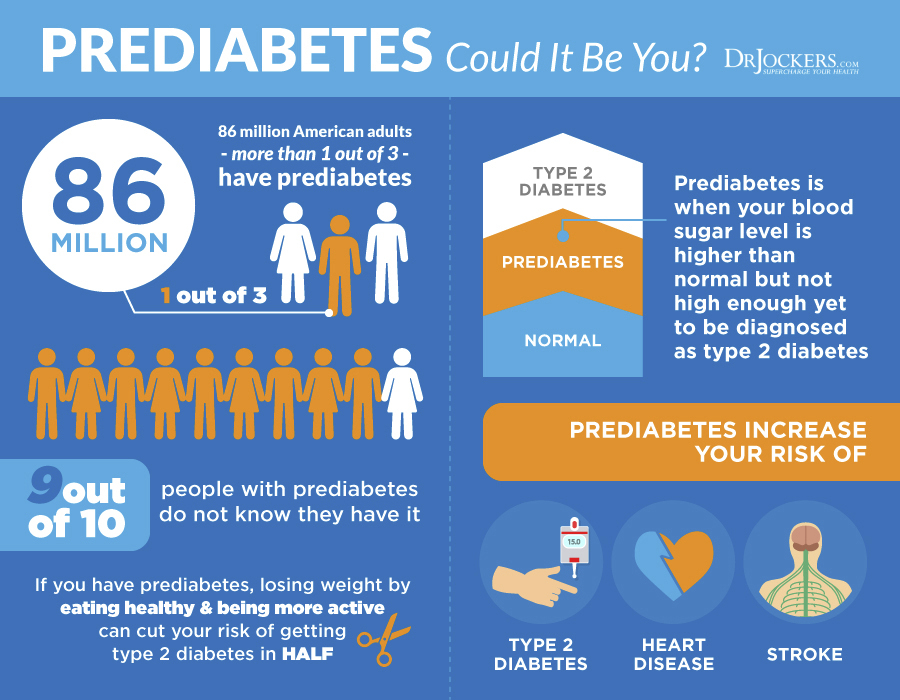
Diabetes
Clinically, diabetes is when fasting blood glucose reaches a level above 126 mg/dl. This is when insulin resistance really begins showing up and health consequences become more pronounced.
It is at this stage that someone is much more likely to be classified as having metabolic syndrome. Metabolic syndrome is a combination of symptoms which include poor blood sugar regulation, increased weight gain, increased blood pressure, and undesirable increases in cholesterol values.
This combination of factors is what ultimately increases the risk of suffering from heart disease or stroke (6). If you do not test blood sugar, you may be silently inching towards this summation of health consequences.
Blood Sugar and Heart Disease
As was just briefly mentioned, poor blood sugar regulation ultimately contributes to heart disease. This is because chronically elevated insulin drives up inflammation and contributes to the oxidation of cholesterol within the arteries. Chronic elevation in insulin also increases blood pressure and LDL cholesterol, creating the perfect storm for heart disease development.
This is likely the reason why it is so common for those who have heart issues to also have diabetes and general metabolic disorders. Whenever I am working with someone concerned about heart disease, the first thing I recommend is to test blood sugar regularly and use strategies to ensure it remains stable.

Common Factors Causing Blood Sugar Imbalance
Many choices you make daily affect the body’s ability to regulate blood sugar effectively. Once you understand these factors, you can control them to benefit your health.
Of course, in addition to considering these factors, actually monitoring your blood sugar simultaneously is the best way to know that the choices you are making are creating a positive impact.

Poor Nutrition
First and foremost, most people are simply eating too many carbs and sugar. The dietary pattern of relying on carbs as a primary energy source is what ultimately leads to blood sugar imbalances and associated symptoms.
The dietary pattern that I have found to most effectively improve blood sugar regulation is either a ketogenic or low-carb approach with an emphasis on plenty of healthy fats (7, 8). Getting off of processed foods, grains, and sugars and consuming a lot of grass-fed meats, avocados, olives olive oil, coconut oil, and grass-fed butter will stabilize blood sugar and improve your metabolic health.
Additionally, there are a number of foods and strategies you can use to further improve blood sugar regulation. Of course, not everyone responds the same (although the majority does) and the only way to be sure that your dietary choices are optimized for you in this regard is to test blood sugar.

Poor Sleep
A far too overlooked aspect of blood sugar regulation is actually sleep quality. In fact, many studies have found that one night of poor sleep can induce pre-diabetic conditions the day following (9). Consequently, people who consistently get poor sleep have more food cravings and higher instances of diabetes (10).
If you test your blood sugar every morning upon waking, you will likely notice that on nights when you have less than ideal sleep, you have elevated blood sugar. It is important to optimize sleep if you wish to get your blood sugar under control. Here are some great tips to improve your sleep quality.

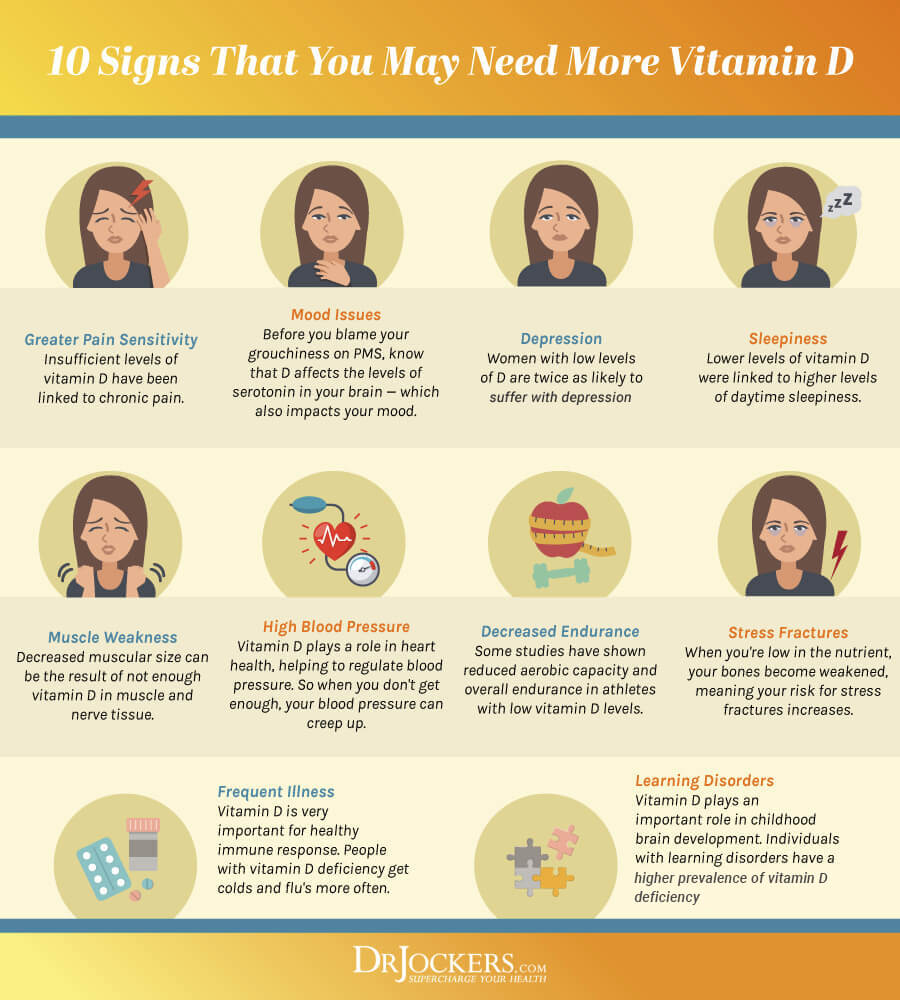
Low Vitamin D
Consequently, poor sleep is associated with a lack of sunlight exposure. Lack of sunlight exposure will cause low vitamin D levels and low vitamin D levels are another big factor in poor blood sugar control. In fact, simply adding a vitamin D supplement to your daily regimen has been shown to improve blood sugar in some individuals (11).
Periodically testing your vitamin D levels should become an important part of living a healthy life. I consider levels between 60-100 ng/ml to be optimal yet I often find that individuals fall far below this range.
Increasing sun exposure and using strategic supplementation reliably improves many aspects of an individual’s health.
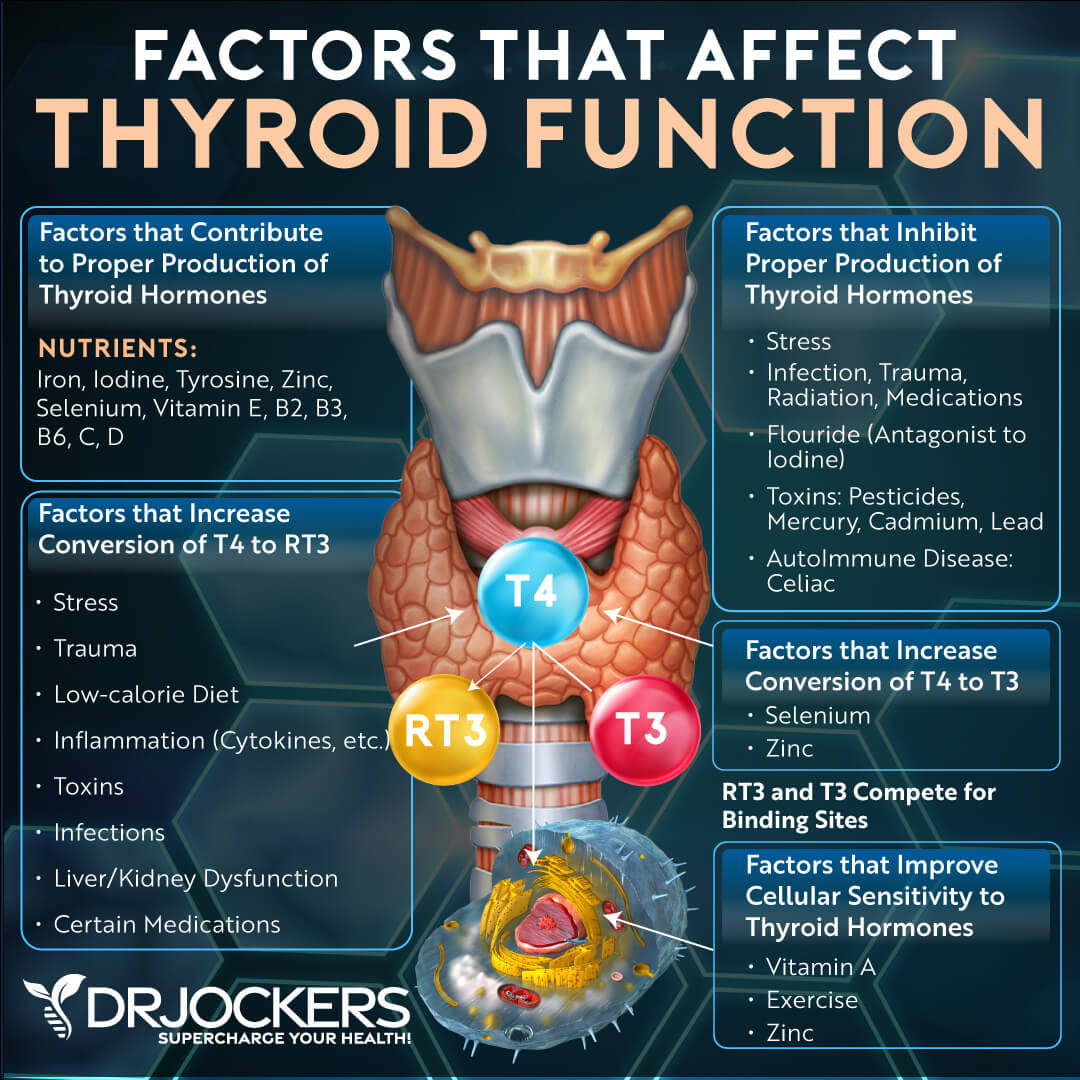
Thyroid Problems
The thyroid is, in a way, the driver of your metabolism. When blood sugar gets out of control and insulin levels rise, stress is placed on the liver. The liver has an important job of assisting in the conversion of thyroid hormone into its active form, T3.
When T3 levels drop due to blood sugar dysregulation, this slows the metabolism and makes it even more difficult for the cells to burn sugar. This leads to a vicious cycle of blood sugar imbalance and thyroid hormone disruption, a perfect storm for metabolic diseases (12).
Therefore, it is imperative to correct thyroid issues if you would like to stabilize blood sugar. Paradoxically, it is imperative to assist your body in stabilizing blood sugar if you would like to resolve thyroid issues.
Chronic Stress
If you are constantly being stressed by your lifestyle, underlying infections, or poor eating habits, this is going to stimulate the chronic release of cortisol. Cortisol is a stress hormone that is very useful for quickly boosting energy to help you meet the demands at hand. The problem with this is that it does so by rapidly increasing blood sugar.
Repeated stress leads to a pattern of cortisol release and blood sugar fluctuations that ultimately contribute to the metabolic issues we have discussed so far. Therefore, it is important to address as many stressors in your life as possible (and periodically test your blood sugar as you do so to monitor your progress).
Some things about a stressful lifestyle can’t be changed, however, things like supporting detoxification, getting adequate sleep, and using adaptogenic herbs can all assist in reducing the burden stress places on your body.

Ways to Test Blood Sugar
Working with a functional medicine or nutrition practitioner to monitor your metabolism can be a game changer for your health. There are a number of blood sugar and metabolism markers that can be observed to determine the current state of your health.
Upon receiving these values, it is possible to create a really solid plan to get your body back in balance based on your lifestyle choices.
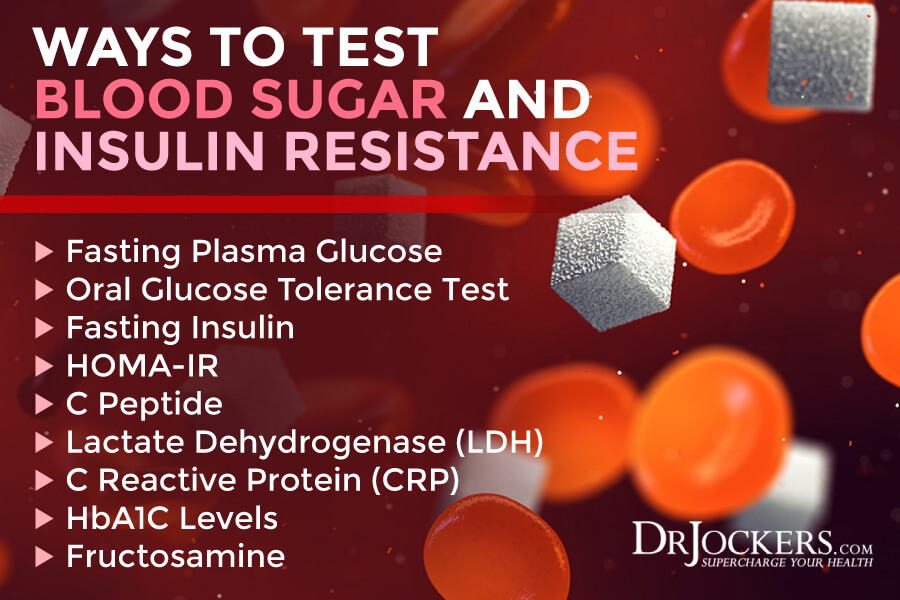
Fasting Plasma Glucose
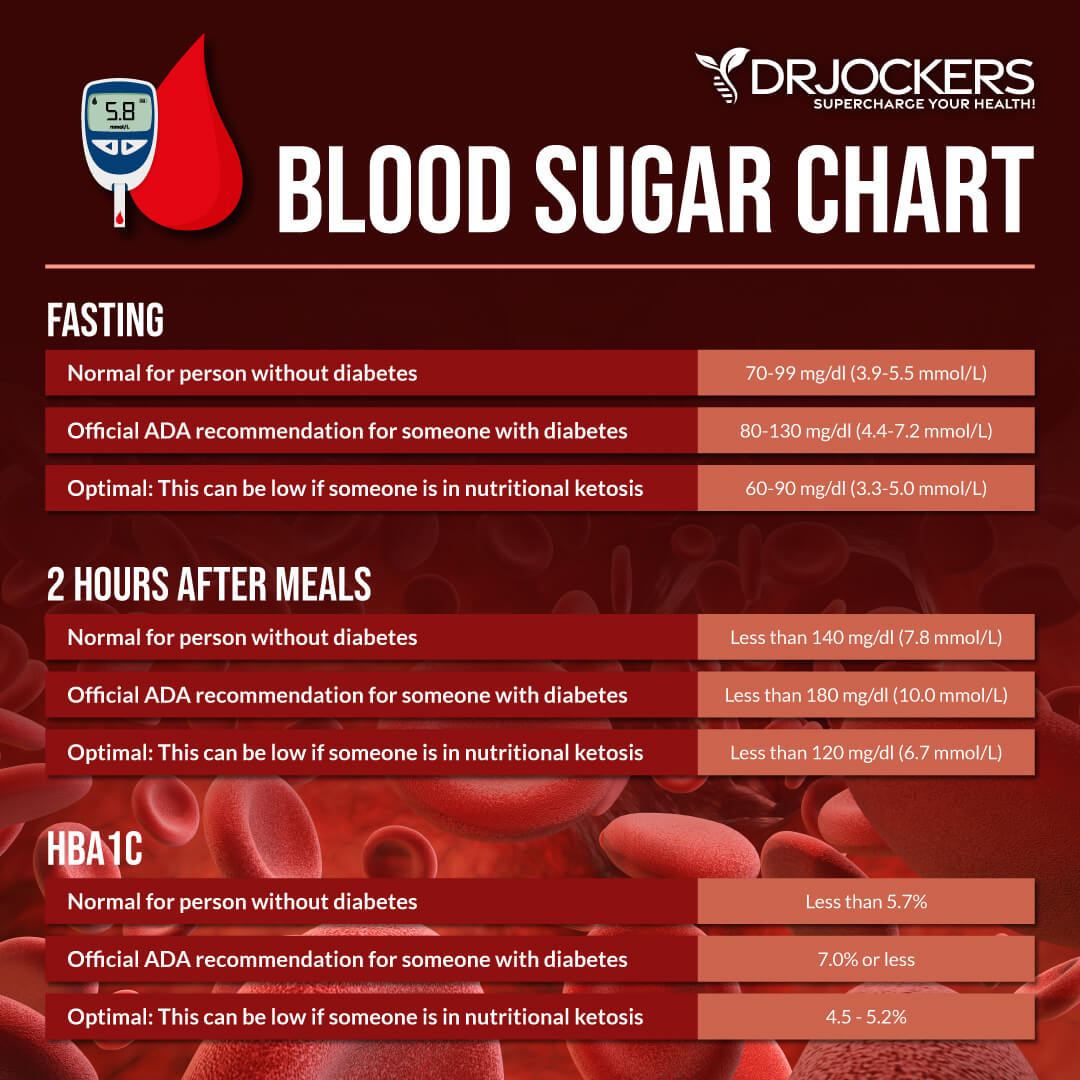
Fasting Plasma Glucose is pretty much exactly what it sounds like. You are instructed to refrain from eating for at least a 12-hour window before taking a blood measurement of your glucose levels. Most individuals simply skip breakfast and perform the measurement in the mid-morning.
After consuming a meal, any sugar from that meal should be efficiently shuttled to the cells or stored as glycogen. Having an elevated blood sugar after a 12-hour fasting window is a sign that this process is not occurring efficiently.
Ideally, this measurement should be below 90 mg/dl. 100-126 mg/dl is considered pre-diabetic while over 126 mg/dl is considered diabetic.
Oral Glucose Tolerance Test (OGTT):
This test measures an individual’s response to a glucose load. They are instructed to fast in a similar way to the FPG and then they are given a measured dose of glucose (75g for adults) to consume within 5 minutes and the blood is measured both immediately after the drink is finished and 2 hours afterward. The 2 hour measurement is a major recording.
Normal OGTT levels should be under 140 mg/dl although most functional medicine doctors want to see them under 120 mg/dl. The pre-diabetic range is from 140-200 mg/dl and over 200 mg/dl is considered diabetic.
Fasting Insulin
As we have discussed somewhat already, insulin helps to shuttle glucose into the cells for energy. When too much sugar is consumed on a routine basis, cells start to become deaf to insulin signals. As a result, more insulin is produced to get the same effect. Eventually, the cells stop responding to insulin and this is characteristic of Type 2 diabetes.
This means that someone who is in the prediabetes phase will have elevated insulin levels. While there is not a generally agreed-upon value for fasting insulin, it seems that evidence points to a value under 5-6 uIU/mL being desirable.
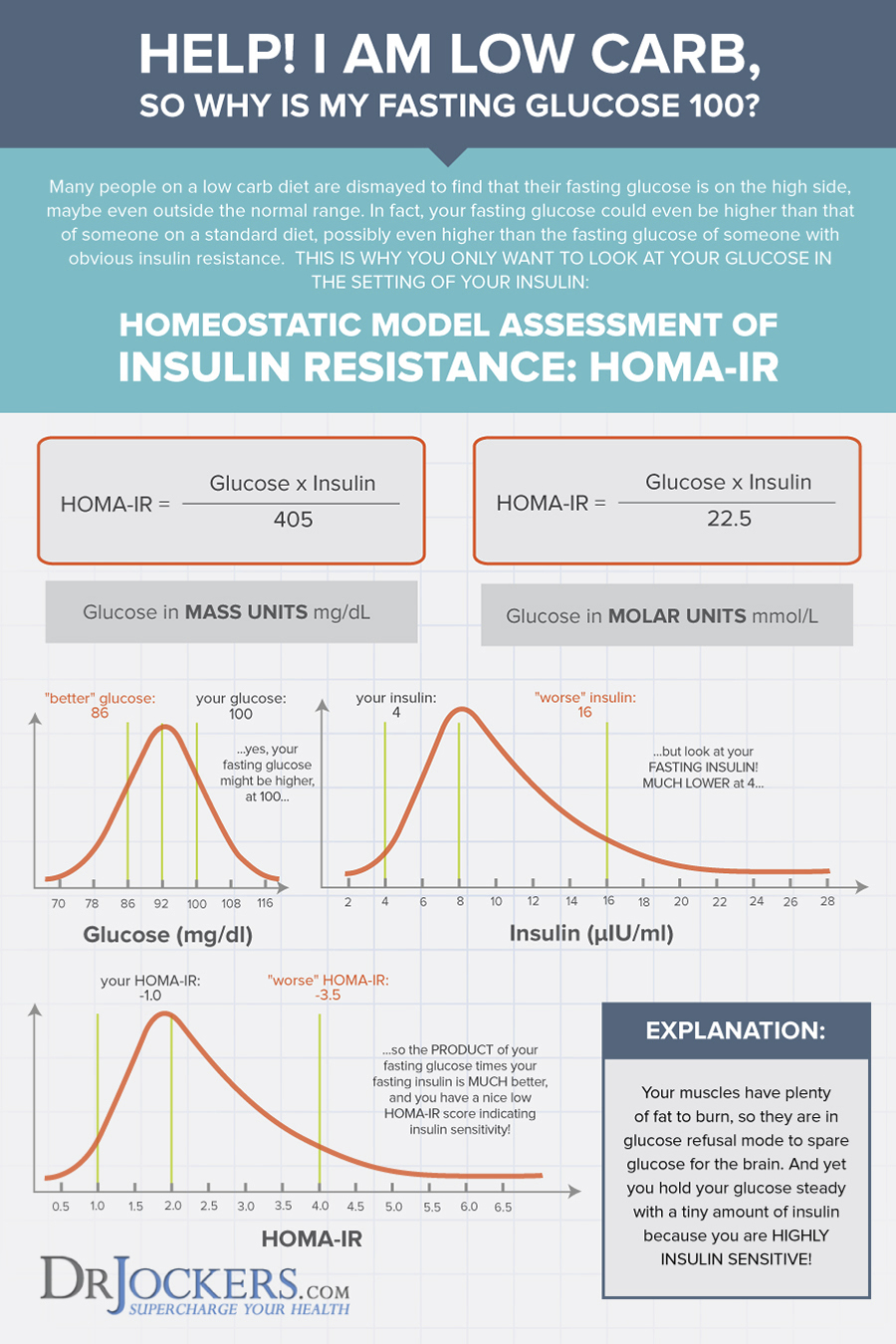
HOMA-IR:
This is a key measurement for understanding insulin resistance. We will often see someone with normal fasting blood glucose but high fasting insulin and the reverse is where someone has high fasting blood glucose and low fasting insulin levels. The HOMO-IR helps determine the level of insulin resistance when one of these scenarios occurs.
HOMA-IR is a simple equation that multiplies fasting glucose (in mg/dL) by fasting insulin (in μIU/mL). This total is then divided by 405. The following ranges are then compared:
Less than 1 = Optimal Insulin Sensitivity
Above 1.9 = Early stage insulin resistance
Greater than 2.9 = Significant Insulin Resistance
Essentially, HOMA-IR looks at the relationship between insulin and glucose in your body rather than each as a separate value. I learned about the HOMA-IR and got the ideas for this graphic below from our friends at Heads Up Health.
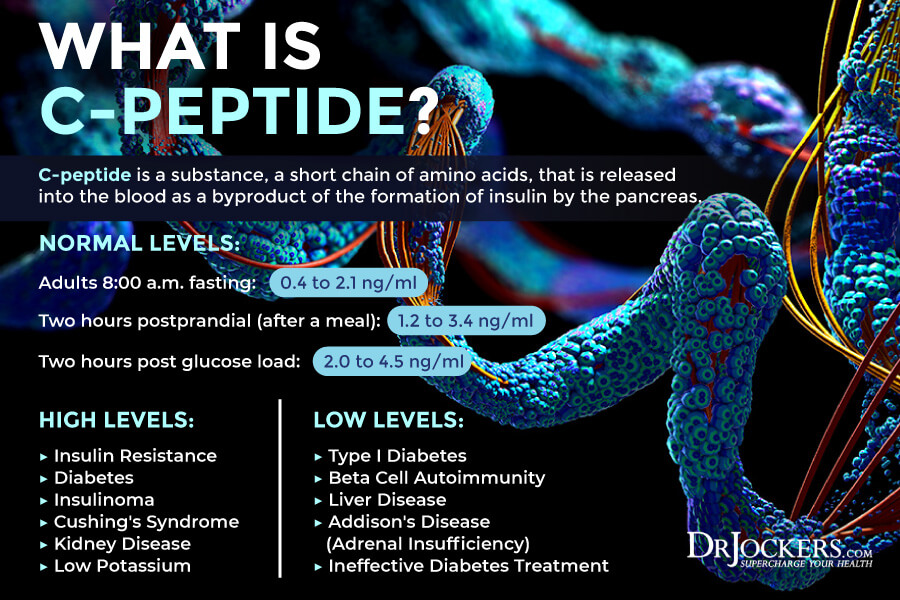
C Peptide
C-peptide is a substance, a short chain of amino acids, that is released into the blood as a byproduct of the formation of insulin by the pancreas.
In the pancreas, within specialized cells called beta cells, proinsulin, a biologically inactive molecule, is split apart to form one molecule of C-peptide and one molecule of insulin. When insulin is released from the beta cells into the blood in response to increased levels of glucose, equal amounts of C-peptide are also released.
Since C-peptide is produced at the same rate as insulin, it is useful as a marker of insulin production. Additionally, this test may even be a better way to measure insulin levels because C-peptide tends to stay in the body longer than insulin
In particular, C-peptide testing can be used to help evaluate the production of insulin made by the body (endogenous) and to help differentiate it from insulin taken in as diabetic medication (exogenous) which does not generate C-peptide.
Adult Range: 8:00 a.m. fasting: 0.4 to 2.1 ng/ml
Two hours postprandial (after a meal): 1.2 to 3.4 ng/ml
Two hours post glucose load: 2.0 to 4.5 ng/ml
LDH
LDH stands for lactic acid dehydrogenase. LDH is an enzyme that is involved in energy production. When looking at this value on labs, it is common to see a low value for someone who experiences reactive hypoglycemia.
Reactive hypoglycemia is when blood sugar rapidly drops after a meal, leading to fatigue and a number of other undesirable symptoms. If you frequently become tired after meals, it is likely you are experiencing this phenomenon. It is ideal to see this number within the range of 140-180 IU/L.
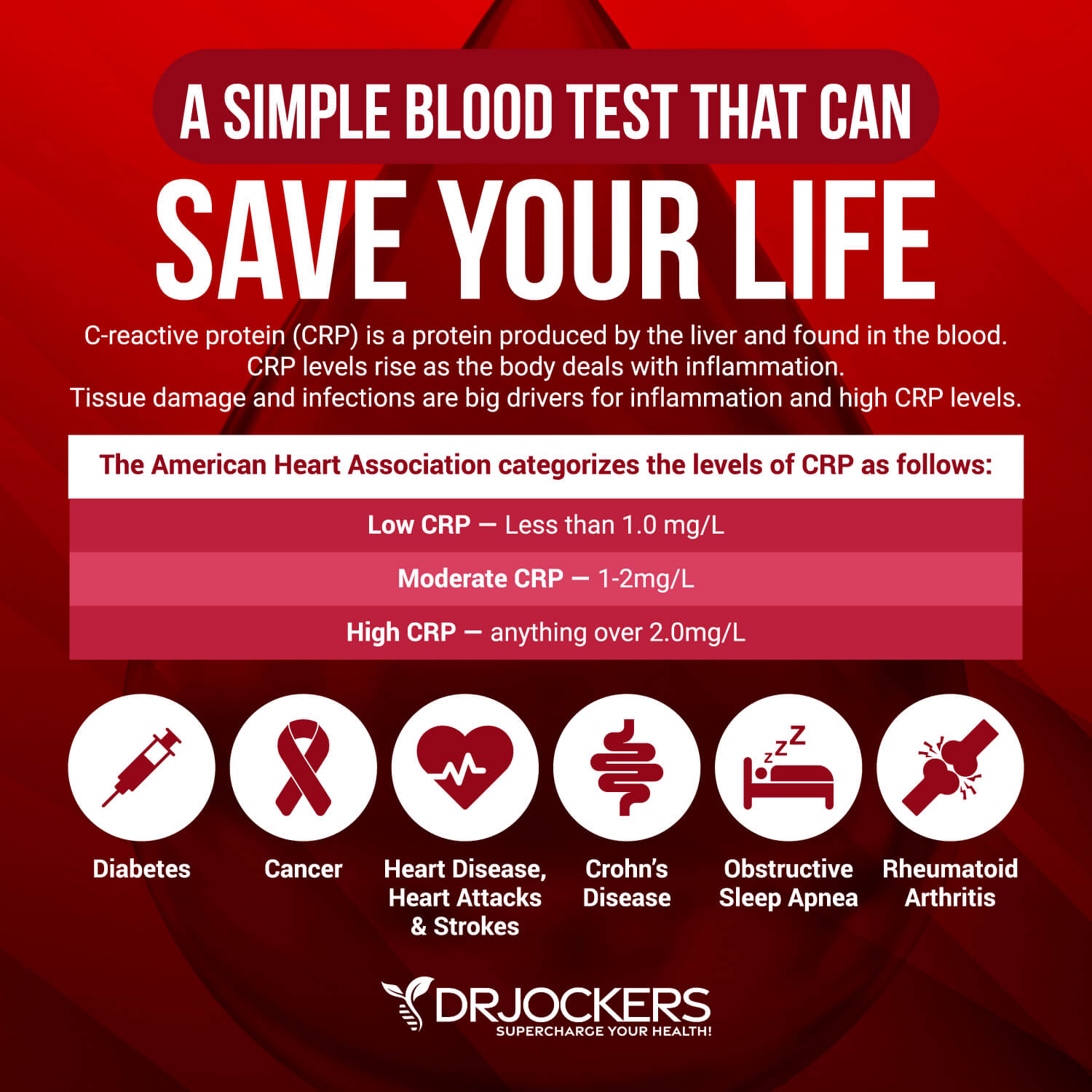
CRP
CRP, or C-Reactive Protein is a measure of inflammation. CRP increases whenever there is inflammation in the body and is often telling of a person’s blood sugar stability. This is because rapidly fluctuating blood sugar and elevated insulin tend to be highly inflammatory in the body.
The best way to measure CRP is by using a high-sensitivity CRP test. CRP levels are indicative of heart disease risk and all-cause mortality. Additionally, CRP levels are helpful for monitoring arthritis, autoimmune conditions, psychological issues, and IBS (among others).
Optimally, this value should fall under 1 mg/L although the lab values often won’t flag it high unless it is over 2.0 mg/L.
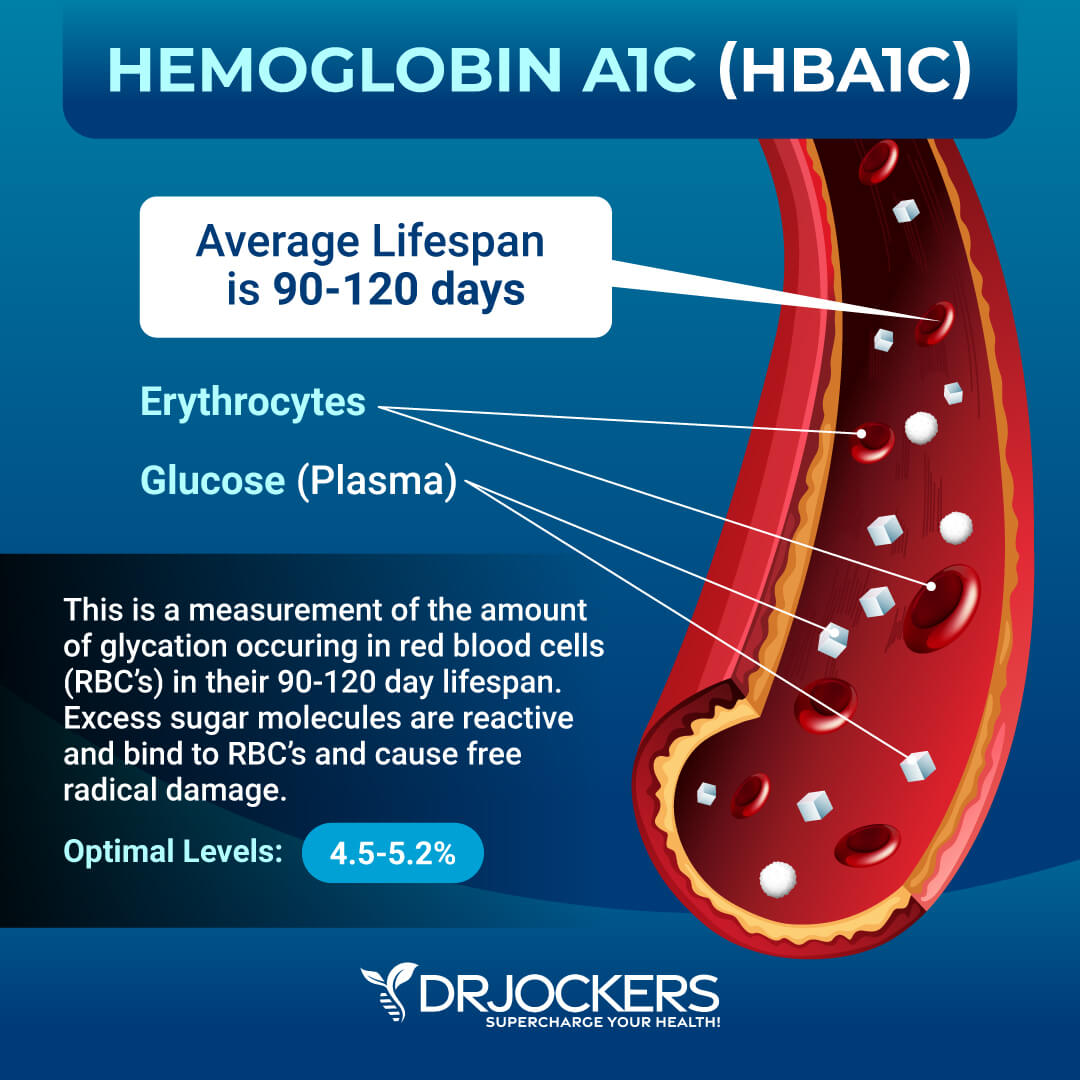
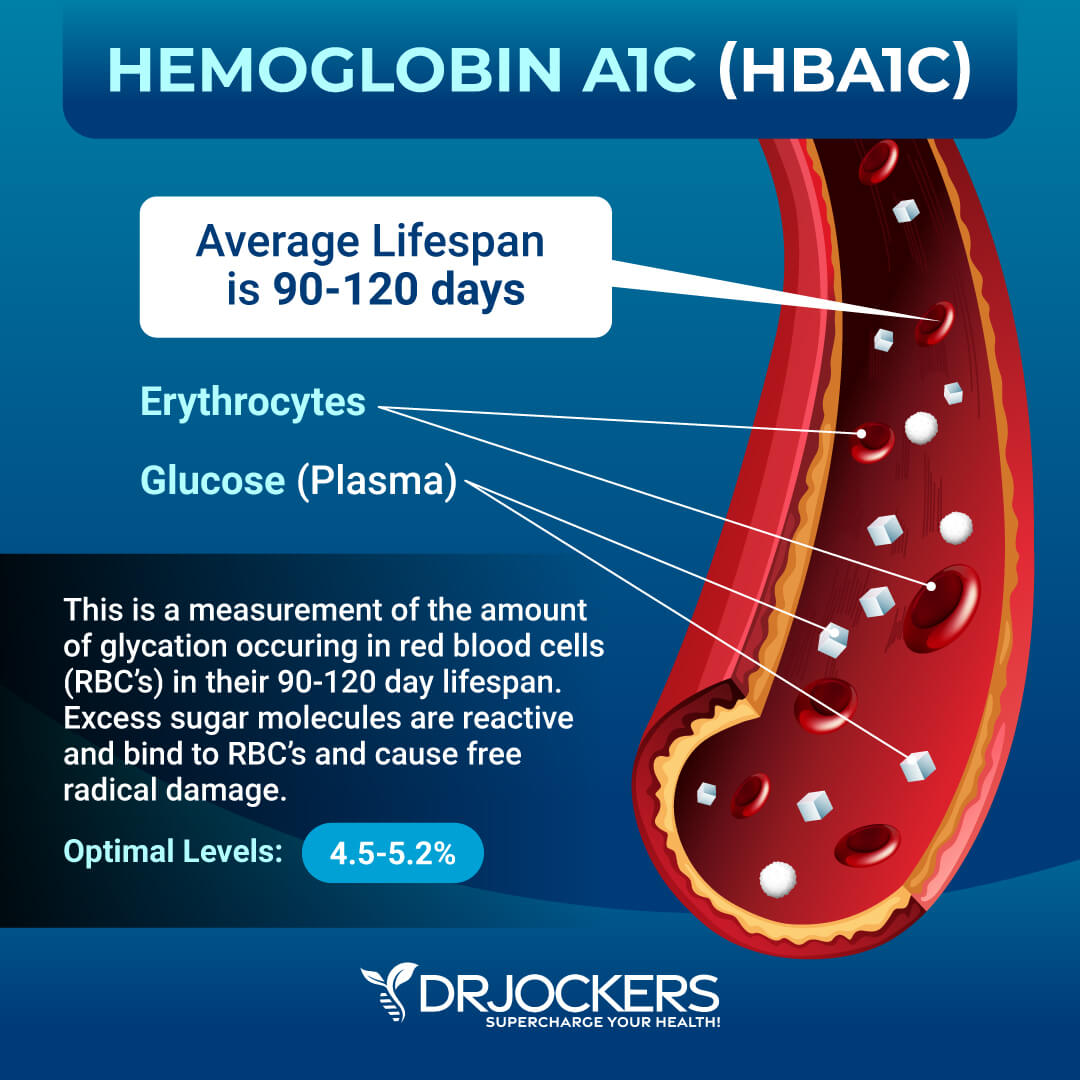
HbA1C
Hemoglobin A1C is one of the best markers to test blood sugar control as it provides insight into the patient’s average blood sugar over a 3-month period. When blood sugar is chronically elevated, sugar molecules attach to hemoglobin, the protein in red blood cells that carries oxygen.
The higher blood sugar remains over a period of time, the more sugar molecules tend to bind with hemoglobin. Because red blood cells have a lifespan of about 3-months, measuring the amount of these sugar-bound hemoglobin molecules gives valuable insight into blood sugar control over a 3-month period.
HbA1C is also a form of advanced glycolytic end product (AGE). These molecules are highly inflammatory and can eventually contribute to neurological and cardiovascular damage.
HbA1C is often used clinically to screen for pre-diabetes or diabetes. An optimal value for this measurement lies between 4.5-5.2.
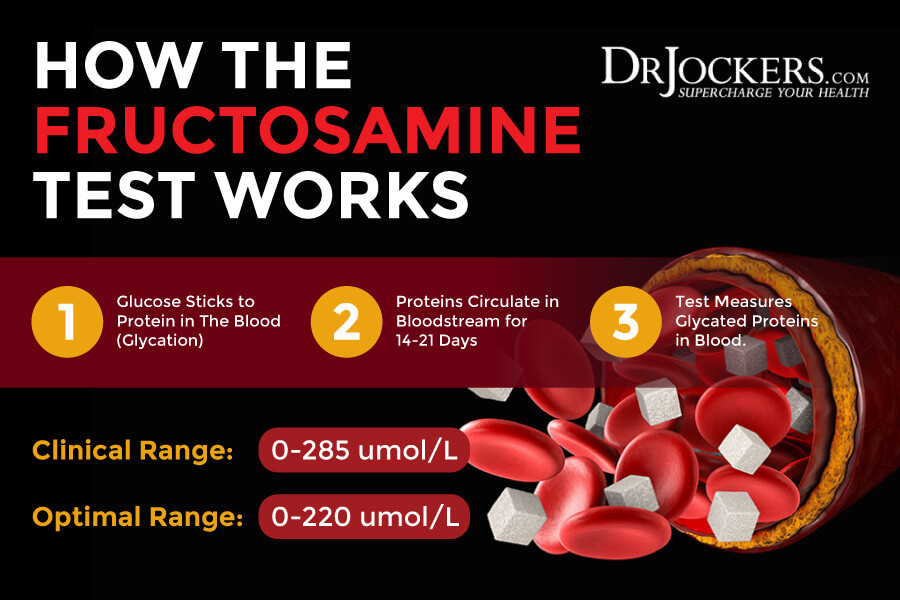
Fructosamine
Fructosamine is a measure of your 2-3 week average blood sugar levels. Blood glucose tends to stick to proteins. Fructosamine is formed when a sugar and a protein (usually albumin, but also globulin, or lipoprotein) are combined.
Similarly to HbA1c (glucose + hemoglobin), fructosamine is a measure of the amount of glucose in the blood. However, while HbA1c measures your 3-month average glucose, fructosamine reflects mean blood glucose over the previous 2-3 weeks. This is due to the shorter life cycle of albumin. The advantage of fructosamine over HbA1c is that it’s not affected by changes in red blood cells and hemoglobin caused by anemia, blood loss, or nutrient deficiencies.
That said, there are also drawbacks to using fructosamine. Temperature, vitamin C, bilirubin, urea, and total protein levels can all affect fructosamine levels.
Approximate Comparison of Blood Glucose, HbA1c , & Fructosamine Levels
Glucose (mg/dl) Fructosamine (µmol) HbA1c (%)
75 193.75 4.5
90 212.5 5.0
120 250 6.0
150 287.5 7.0
180 325 8.0
210 362.5 9.0
240 400 10.0
270 437.5 11.0
300 475 12.0
330 512.5 13.0
360 550 14.0
390 587.5 15.0
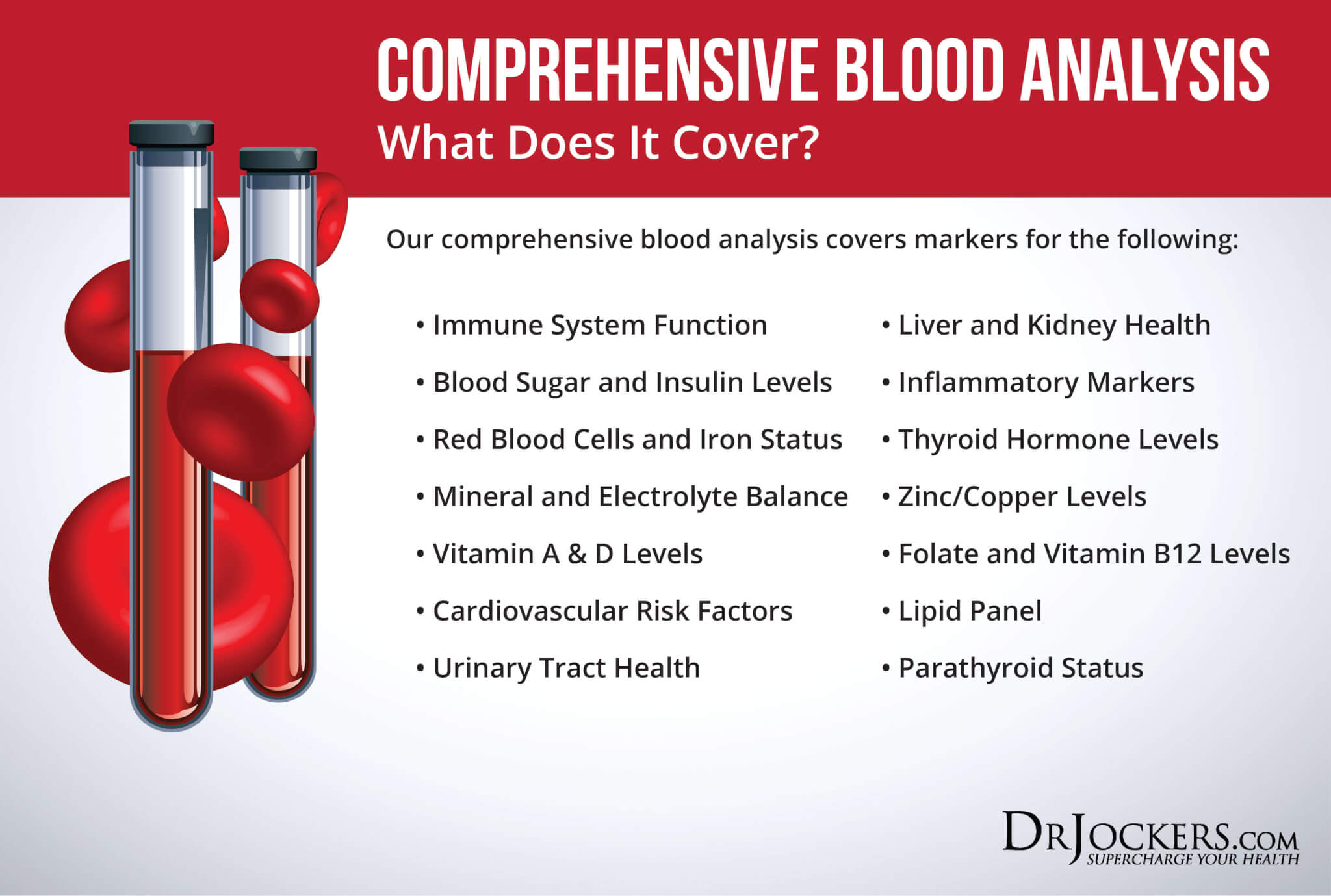
Comprehensive Blood Analysis
The measurements in this article may seem overwhelming if you are considering having them all done. Luckily, many of these things are screened for in a Complete Blood Count. Sometimes doctors will perform a Complete Blood Count as a routine check-up, however, this is not always the case. Even worse, unless your levels are off the charts, they rarely know how to interpret if you are having functional health issues on these labs.
Personally, I use the Comprehensive Blood Analysis as it measures all of the above values along with an in-depth look at blood sugar, inflammation, thyroid function, nutrients like Vitamin A, Vitamin D, zinc, copper, B12 levels, and so much more. For anyone experiencing metabolic issues and wanting to regain their health, this test offers a comprehensive look into your blood sugar stability and fat-burning potential.
Home Testing Methods
Something I often recommend is purchasing a personal monitor and periodically testing blood sugar levels upon waking and before meals. Ideally, you should see that your test blood sugar stays around 90 and doesn’t go above 100.
This measurement can be taken using a monitor such as the Keto Mojo. I like this monitor specifically because it is cost-effective and monitors both blood glucose as well as ketones. For those with blood sugar issues, I often recommend a ketogenic diet, and measuring ketones is a great way to track your fat-burning progress. This tool is a great way to ensure you are burning fat, not sugar.
If you choose to use a personal monitor to test blood sugar levels, be sure to wash hands thoroughly before testing, measure at least 2 hours after a meal (ideally first thing in the morning), and use manufacturer-recommended supplies (test strips, lancets).
Ways to Balance Blood Sugar
There are a number of ways that you can regain control of your blood sugar and turn your body into a fat-burning machine. To get started, one of the best things you can do is perform a keto metabolic makeover (detailed here).
For a more comprehensive approach and accelerated results, you may consider working with a health coach who is well-versed in the ketogenic lifestyle. If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!





Hello Dr.
Thanks for this article so interesting
I know very well this problem, my father is diabetic type 2
It is very complicated to have correct blood sugar levels but other factors such as sleep, exercise, and the correct diet are taken into account.
Thanks again
Thanks for reading Pascual!
This was very informative yet I’m confused about Low Insulin and it’s relation to insulin resistance. I had a blood test done that showed insulin of 1.6 uIU/mL ( stated as LOW) and wonder if that means the same as insulin resistance??????
I appreciate you helping me underatand that.
Hey Amanda, if insulin is low and blood sugar is within range, then this is a sign you are insulin sensitive and insulin is doing its job properly in your body. If insulin is low and blood sugar is high, then this would be a sign that there could be an issue with the islet cells in your pancreas. This would typically be due to autoimmune conditions.
Thank you so much for that! I do have hypothyroidism and HPA Axis dysfunction and if I eat starchy vegetables my blood sugar gets jacked up, so I refrain from them and anything else remotely sweet. I am following your Keto and IF suggestions for 6 weeks now and feel great so I’m hoping to calm that occasional high blood sugar. Thank you again so much for taking the time to explain that to me!
Any suggestions for a prickless BG monitors?
During 2 to 3 days fast I get very weak and very uncomfortable feeling, thinking this may be a hypoglycemic effect. This also leads me to think that I would like a constant BG monitor for overnight.
Any thoughts are appreciated
Yes you can get a continuous blood glucose monitor through Levels Health https://www.levelshealth.com/
I noticed the link to Keto Mojo goes to a different monitor (and not keto mojo) instead to Best Ketone Test – (with an affiliate link) do you know if this is a legit company as I’ve never heard of it and all the reviews on it’s site look fake (most giving five stars). Thanks.
Yes it is the same as the Keto Mojo, they private labeled it. It works great.
This is such a great article, I hope more diabetics see this, I myself using these methods got my A1C from 12 to 7 in just 4 months, lost 60 + pounds, according to my readings, I will soon enter a “normal” state, and I can’t wait to see what my next A1C is… But yeah this is good stuff, you can learn ALOT just from this one page. It pretty much sums up everything I have spent the last few years researching with regards to insulin resistance and diabetes type II.
Wonderful to hear that Joe! Keep up the great work!