Colon Cancer: Symptoms, Causes, and Support Strategies
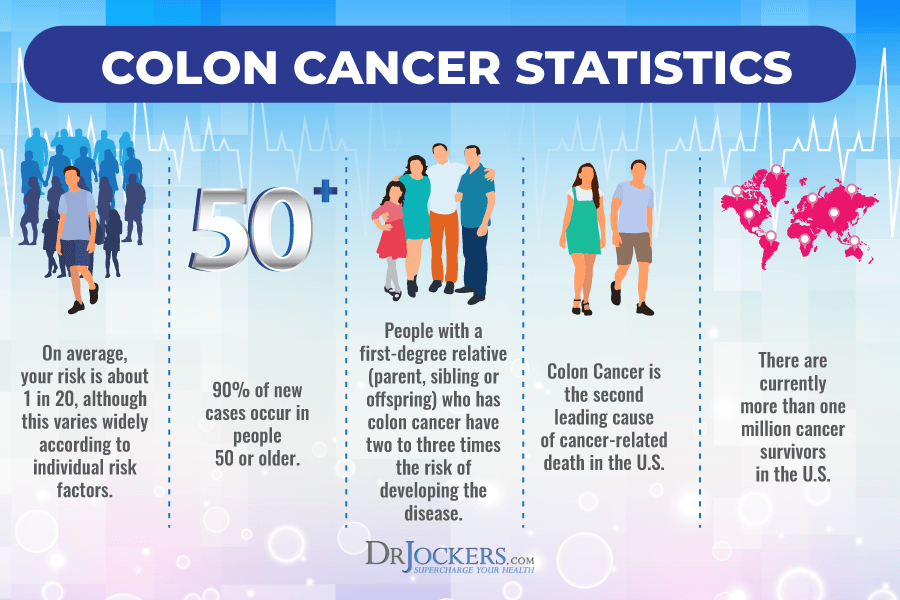
Did you know that colon cancer is the third most common cancer-related death in the United States? It’s a form of cancer that develops in the large intestine. Colon cancer will affect 1 in 23 men and 1 in 25 women at one point in their life. Clearly, colon cancer is a serious issue that we need to talk about. Natural support strategies can support your health and improve dietary and lifestyle risk factors of the disease.
In this article, you will learn what colon cancer is. You will learn about the signs and symptoms of colon cancer. I will discuss its risk factors, stages, and grades. I will discuss conventional treatment options for colon cancer. You will learn about the top root cause risk factors of colon cancer. I will also share my top natural support strategies to support your health.
What Is Colon Cancer
Colon cancer is a very prevalent form of cancer that develops in your colon or large intestine. It is often mentioned under the umbrella of colorectal cancer. Your colon is the area where your body pulls out water and salt from solid waste. This waste will move to the rectum, the last about six inches of your large intestine, to be released through your anus. Colon cancer affects the colon and rectal cancer affects the rectum, however, the two are often co-occurring or spread from one area to another (1).
According to the American Cancer Society, there are 104,270 new cases of colon cancer and 45,230 new cases of rectal cancer a year (2). About 1 in 23 men and 1 in 25 women will develop colorectal cancer in their life (2). It is the third most common cause of cancer-related deaths in the United States (2). Since your risks of colon cancer seem to increase by age, most healthcare professionals recommend regular screening after the age of 50.
Signs & Symptoms of Colon Cancer
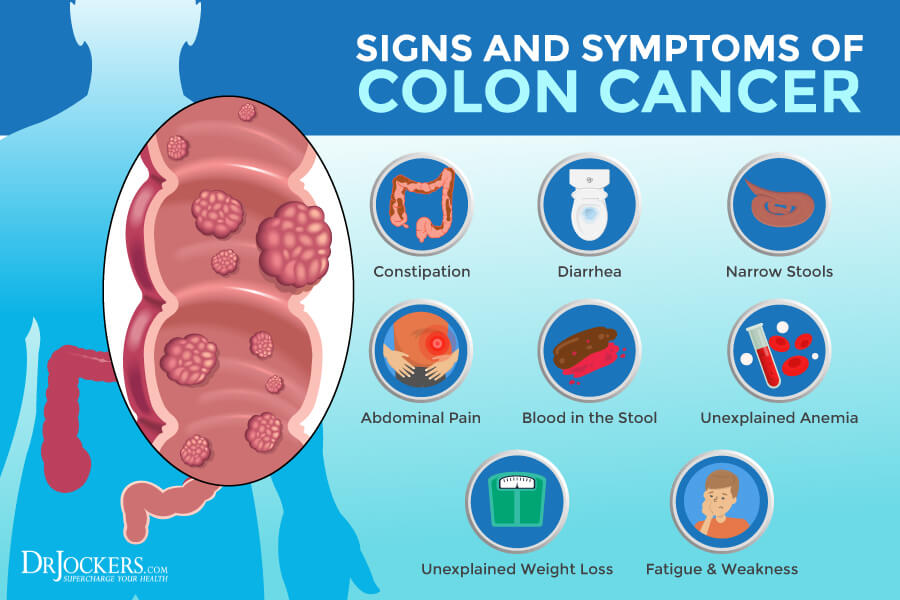
Signs and symptoms of colon cancer may include (3):
- Changes in bowel habits, including constipation, diarrhea, or narrow stools, or anything unusual that lasts for more than just a few days
- Rectal bleeding with bright red blood
- Blood in the stool that may make your stool look dark brown or black
- Feeling like you need to have a bowel movement which cannot be relieved even after having one
- Abdominal pain or cramping
- Unexplained Anemia
- Weakness
- Fatigue
- Weight loss without trying or any clear cause
Noticing any of the symptoms can be scary. However, many of these symptoms can be the result of other issues as well, including hemorrhoids, infections, irritable bowel syndrome (IBS), or inflammatory bowel disease (IBD). It’s important that if you notice any of these symptoms of colon cancer, you visit your doctor for an accurate diagnosis (3). Screening is recommended and staying in tune with your body is particularly important because, in the early stages of colon cancer, you may not notice any symptoms right away.
Risk Factors for Colon Cancer
There are several risk factors for colon cancers that you need to know about. Some, like age, family history, or ethnicity are things that you cannot change. Other factors, including diet, exercise, and alcohol use are things you have more control over. If you belong to one or several of the higher risk categories that you don’t have control over, it is even more important for you to pay attention to factors that you can improve, including your diet and lifestyle.
Risks for colon cancer include (4):
- Age, being over the of 50
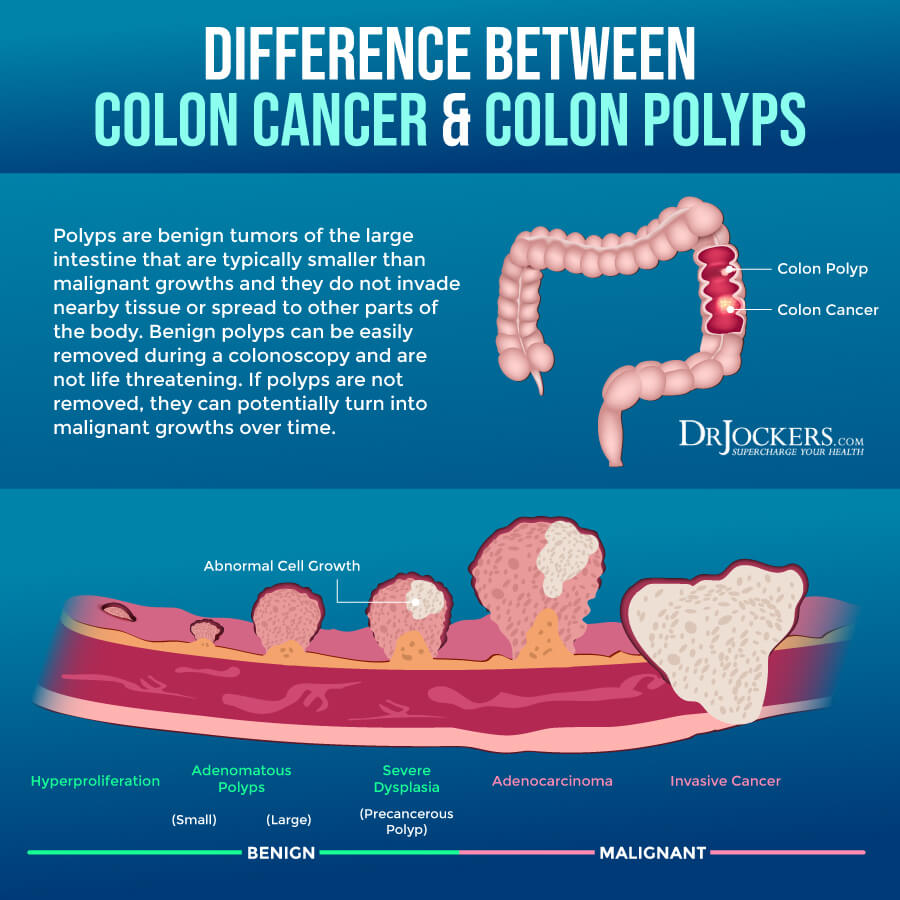
- Personal history of adenomatous polyps or cancer in the colon
- History of inflammatory bowel disease
- Family history of colon cancer or adenomatous polyps
- Genetic inheritance
- Lynch syndrome
- Familial adenomatous polyps (FAP)
- Some rare inherited syndrome, including Peutz-Jeghers syndrome (PJS) and MUTYH-associated polyposis (MAP)
- Racial or ethnic history, being black, or having an Ashkenazi Jew ethnic background
- Having type 2 diabetes
- Being overweight or obese
- Living a sedentary lifestyle
- Certain dietary factors, including too much processed meat, red meat, or meats cooked at high temperatures
- Low vitamin D levels
- Smoking
- Moderate to heavy alcohol use

Stages of Colon Cancer
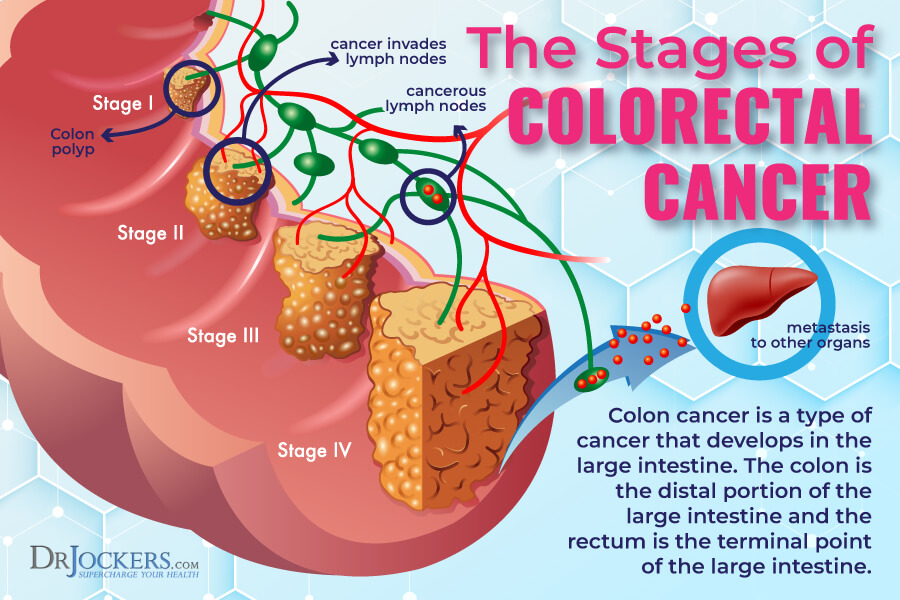
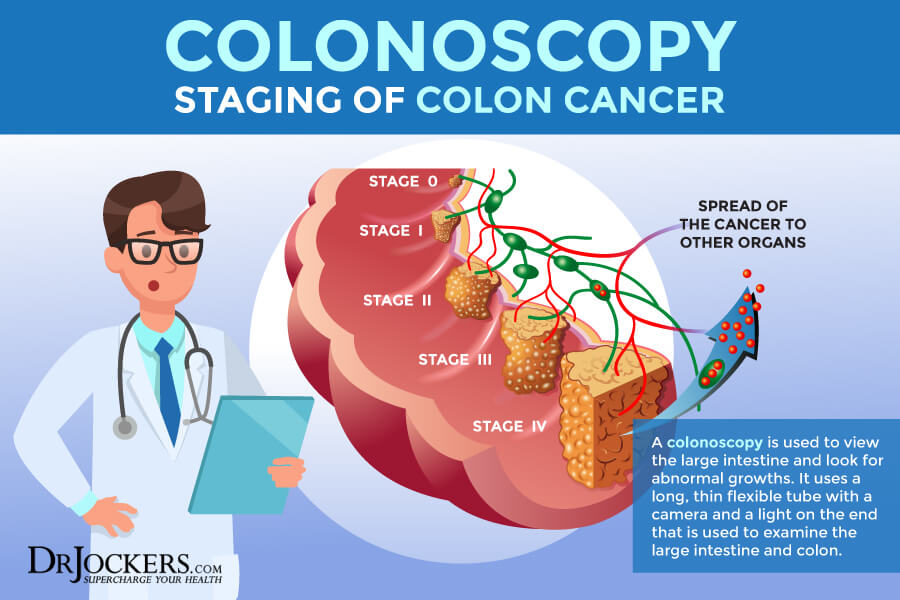
If you get diagnosed with colon cancer – or any cancer -, one of the first things that happens is determining what stage your cancer is. The stage of your cancer is determined by the severity of cancer and how far it has spread in your body. Staging is very important to find the best treatment approach.
TNM Staging System
According to the American Joint Committee on Cancer, doctors are using the so-called TNM staging system, which looks at the following three factors (5):
- T: T refers to the primary tumor, which is the original tumor. Doctors look at the size of this primary tumor and whether or not it has grown into the wall of the colon or has spread to other areas.
- N: N refers to your regional lymph nodes. Doctors check whether cancer has spread to nearby lymph nodes.
- M: M refers to distant metastases. When looking for distant metastases, doctors look at whether cancer has spread to further areas and other organs, such as your liver or lungs.
Using this system, doctors can classify your colon cancer into five stages. The stages of colon cancer include (6):
Stage 0 Colon Cancer
Stage 0 is the earliest stage. It means that your cancer hasn’t grown beyond the mucosa or the innermost layer of your colon. This stage is the easiest to treat (6).
Stage 1 Colon Cancer
At stage 1, your cancer has grown into the mucosa and reached the next layer of the colon, called the submucosa. Since it hasn’t spread into your lymph nodes yet, chances of recovery are still good (6).
Stage 2 of Colon Cancer
At stage 2 the cancer has grown beyond the mucosa and submucosa to other areas. Depending on how far it has grown, there are three sub-stages you need to know about (6):
- Stage 2A: At this stage, the cancer has reached the outer layers of your colon but hasn’t moved beyond yet and hasn’t spread to your lymph nodes or other tissues either.
- Stage 2B: At this stage, the cancer has grown beyond the outer layer of your colon into the visceral peritoneum that keeps your abdominal organs together, but it hasn’t moved to your lymph nodes yet.
- Stage 2C: At this stage, the cancer has moved to nearby organs or structures, but not the lymph nodes yet.
Stage 3 of Colon Cancer
Stage 3 is a serious stage of colon cancer where the cancer has significantly grown and spread already. There are 3 sub-stages of colon cancer (6):
- Stage 3A: At this stage, the cancer has grown through muscular layers and nearby lymph nodes, but not distant lymph nodes or organs (6).
- Stage 3B: At this stage, the cancer has spread outside the outermost layer of your colon and the visceral peritoneum or other organs and it has also spread to 1 to 3 lymph nodes. In other cases, the cancer hasn’t spread outside the outer layer but can be found in 4 or more lymph nodes (6).
- Stage 3C: At this stage, the cancer has moved beyond the muscular layers and into 4 or more lymph nodes, but only nearby and not distant ones (6).
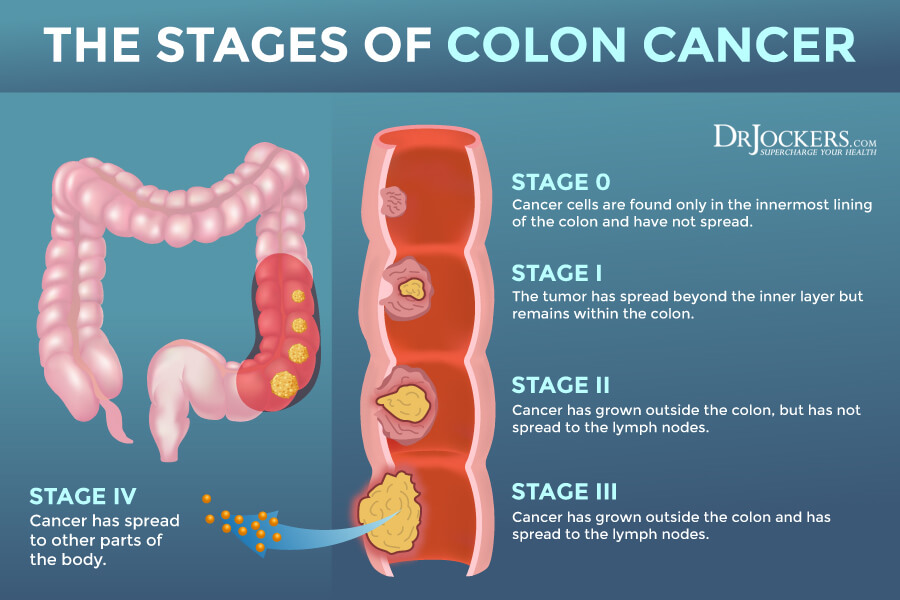
Stage 4 of Colon Cancer
Stage 4 colon cancer is the last stage. It is broken down into two sub-stages:
- Stage 4A: At this stage, the cancer has already spread to distant areas, such as the lungs, liver, or other organs (6).
- Stage 4B: At this stage, the cancer has spread to two or more distant areas. Stage 4B is the most advanced stage of colon cancer (6).
Low-Grade vs High-Grade Colon Cancer
Beyond staging, colon cancer can be classified into two categories. Pathologists look at cancer cells and check for abnormalities and how much they look like normal, healthy cells.
Low-grade colon cancer has more normal-looking cancer cells that seem to grow slower. Low-grade colon cancer has a better prognosis. High-grade colon cancer has more abnormal-looking cancer cells that tend to grow faster. High-grade colon cancer usually has a worse prognosis (7).
Conventional Treatments for Colon Cancer
According to the American Cancer Society, there are currently seven different conventional treatment options out there for colon cancer, including surgery, radiofrequency ablation, cryosurgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. The recommended treatment option would depend on the stage and grade of your cancer (8).
Surgery removes cancer from the colon. Radiofrequency ablation uses tiny electrodes to kill cancer cells. Cryosurgery freezes the cancerous tissue with the help of an instrument. Chemotherapy uses chemotherapy drugs to stop cancer growth and kill existing cancer cells. Some chemotherapy drugs are injected while others are taken orally.
Radiation therapy uses high-energy x-ray radiation to kill cancer. It may be internal or external radiation. Targeted therapy is a drug treatment that targets and attacks cancer cells. It is less harmful to healthy cells than chemotherapy. Immunotherapy is a biological therapy that helps to boost the immune system and uses the body’s natural defenses to fight cancer. Besides their options, there are various studies for new treatment options. You may also choose to enroll in a clinical trial (8).
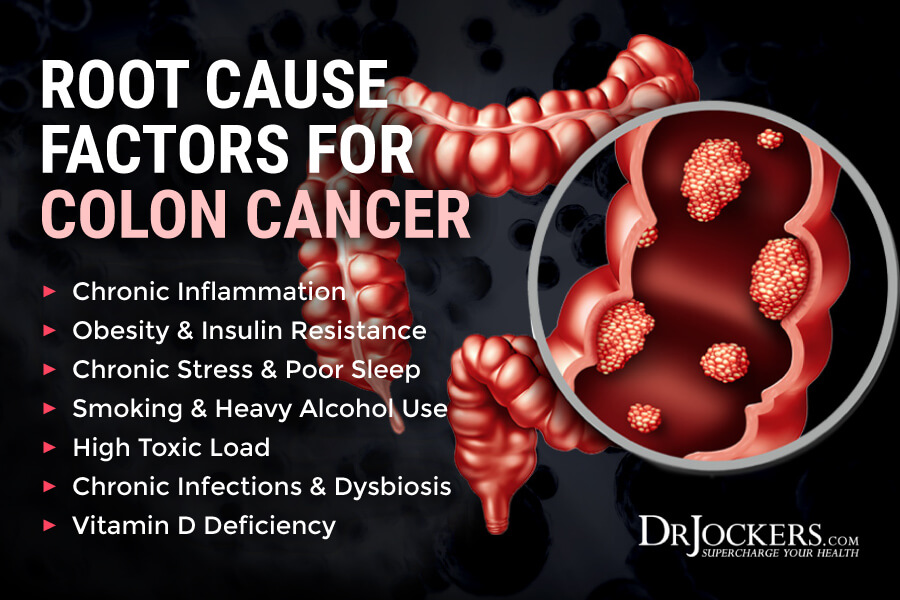
Root Cause Factors for Colon Cancer
Colon cancer may develop for a variety of reasons. Health issues, lifestyle factors, and nutrition can all play a role. Here are the top root cause factors for colon cancer:
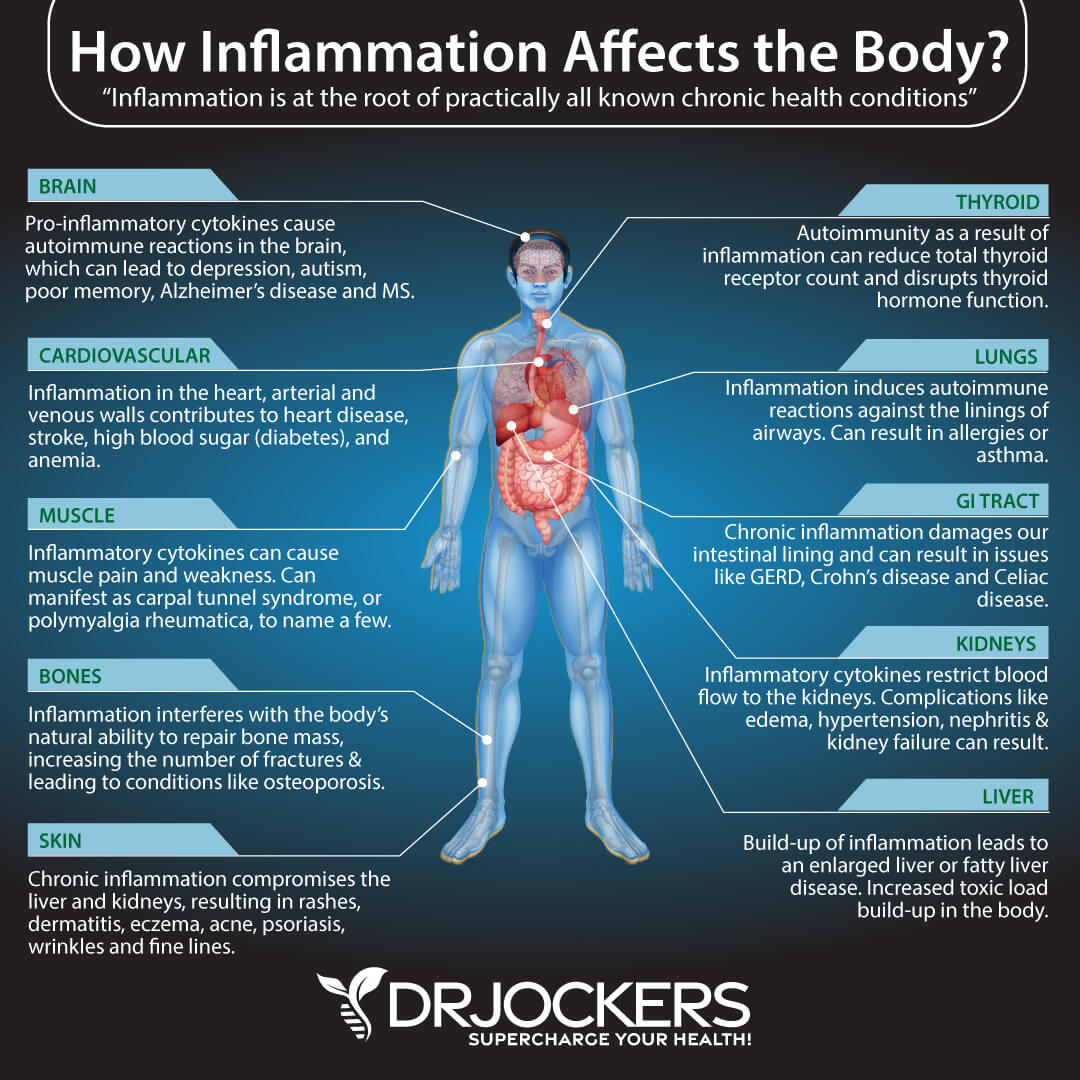
Chronic Inflammation
Inflammation is a healthy physiological response to injuries, infections, and toxins. The inflammatory process increases white blood cells and helps tissue repair. However, healthy inflammation is acute inflammation that only occurs in case of an injury, infection, or toxin exposure. It supports recovery and gradually disappears within a few days, or several weeks as your body heals.
Chronic inflammation on the other hand is a problem. It is an ongoing inflammation that develops without acute events, like an injury or infection, but develops and continues because of an inflammatory diet, obesity, a lack of exercise, constant environmental toxin overload, chronic stress, poor sleep, and another unhealthy lifestyle, dietary, and environmental factors.
According to the National Institute of Health (NIH) – National Cancer Institute, chronic inflammation can cause oxidative damage and DNA damage and lead to cancer (9). People with chronic inflammatory bowel disease also have a higher risk of developing colon cancer. A 2013 study published in Seminars in Immunopathology has found that IBDs can trigger further inflammation and tumorigenesis and increase the risk of the development of colon cancer (10).
Obesity and Insulin Resistance
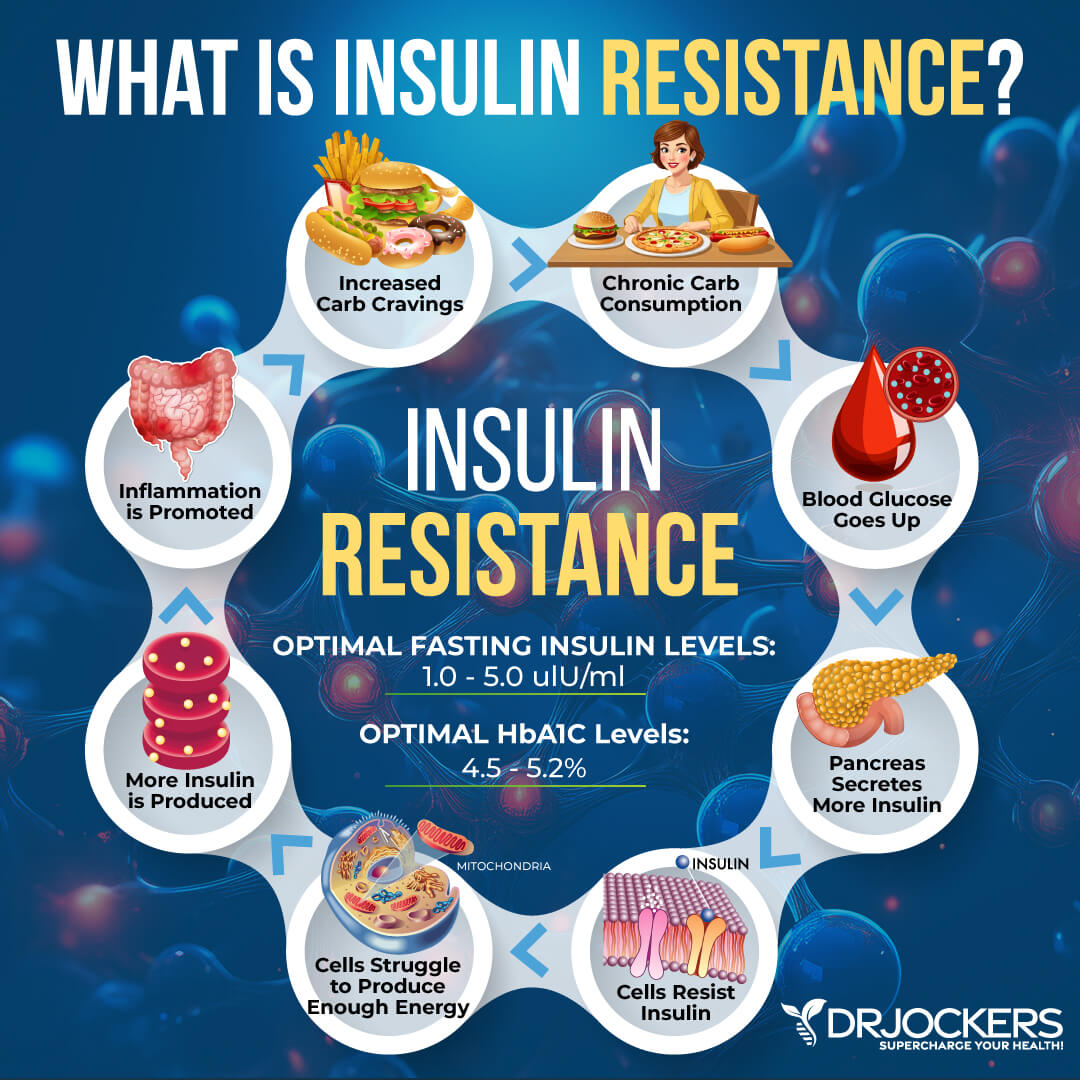
According to the CDC, about 42 adults in the US are obese (11). In addition to that, about 60 to 70 million people in the US and about 40 percent of people over the age of 60 have insulin resistance (12). Considering that obesity and insulin resistance are both risk factors for colon cancer, which is more common after the age of 50, this is not good news.
Insulin resistance means that your body is unable to respond well to insulin and properly deal with the blood glucose circulating in your system. Insulin resistance increases your risk of prediabetes and diabetes. Obesity can increase your risk of insulin resistance, prediabetes, and diabetes. A 2019 study published in the International Journal of Molecular Sciences that due to low-grade inflammation found in obesity and miRNA dysregulation, obesity and insulin resistance may increase the risk of colon cancer (13).
A 2003 review published in Experimental Biology and Medicine (Maywood, NJ) has found that by increasing growth factor levels and increasing inflammation, insulin resistance can contribute to carcinogenesis in the colon and increase the risk of colon cancer (14). A 2020 study published in the Journal of Gastrointestinal Cancer has also found that insulin resistance and obesity can contribute to colon cancer by increasing plasma resistance levels (15).
Chronic Stress & Poor Sleep
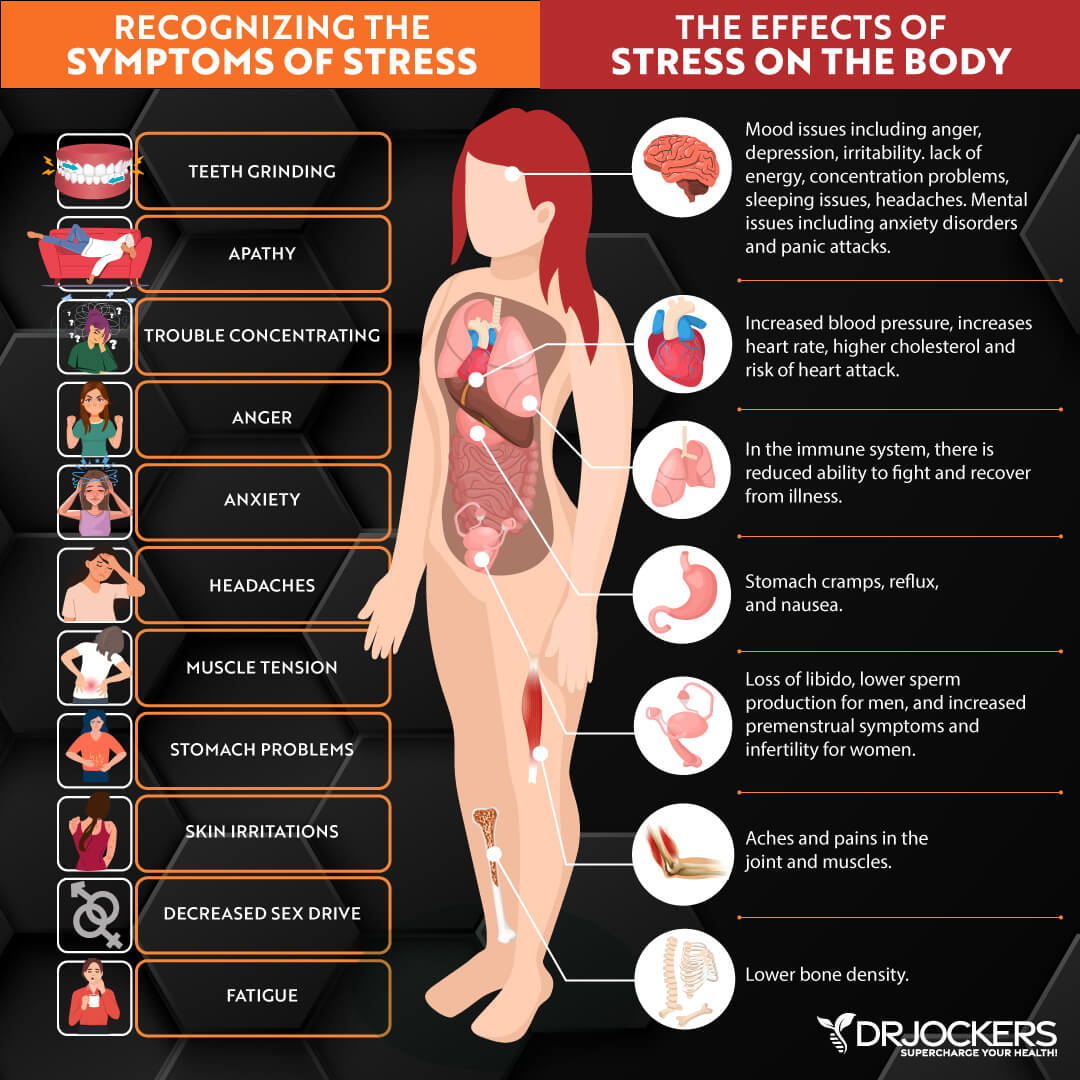
As you just learned, chronic inflammation can increase your risk of colon cancer. (9, 10). But what causes chronic inflammation? Chronic stress and poor sleep are just two factors that play a major role in chronic inflammation and the development of the disease.
A 2019 study published in the Journal of Clinical Medicine has found that there is a correlation between chronic stress, inflammation, and colon cancer on a molecular level, however, to fully understand this relationship, more research is needed (16). A 2017 study has found that psychological stress may increase the risk of colorectal cancer (17).
A 2011 study published in Cancer has found that a lack of sleep or short duration sleep can increase the risk of colon cancer (18). A four-year population-based case-control study on 7355 patients published in 2019 in In Vivo has found that sleep disorders can also increase the risk of colon cancer (19). Patients with a sleep disorder and depression had an even higher risk.
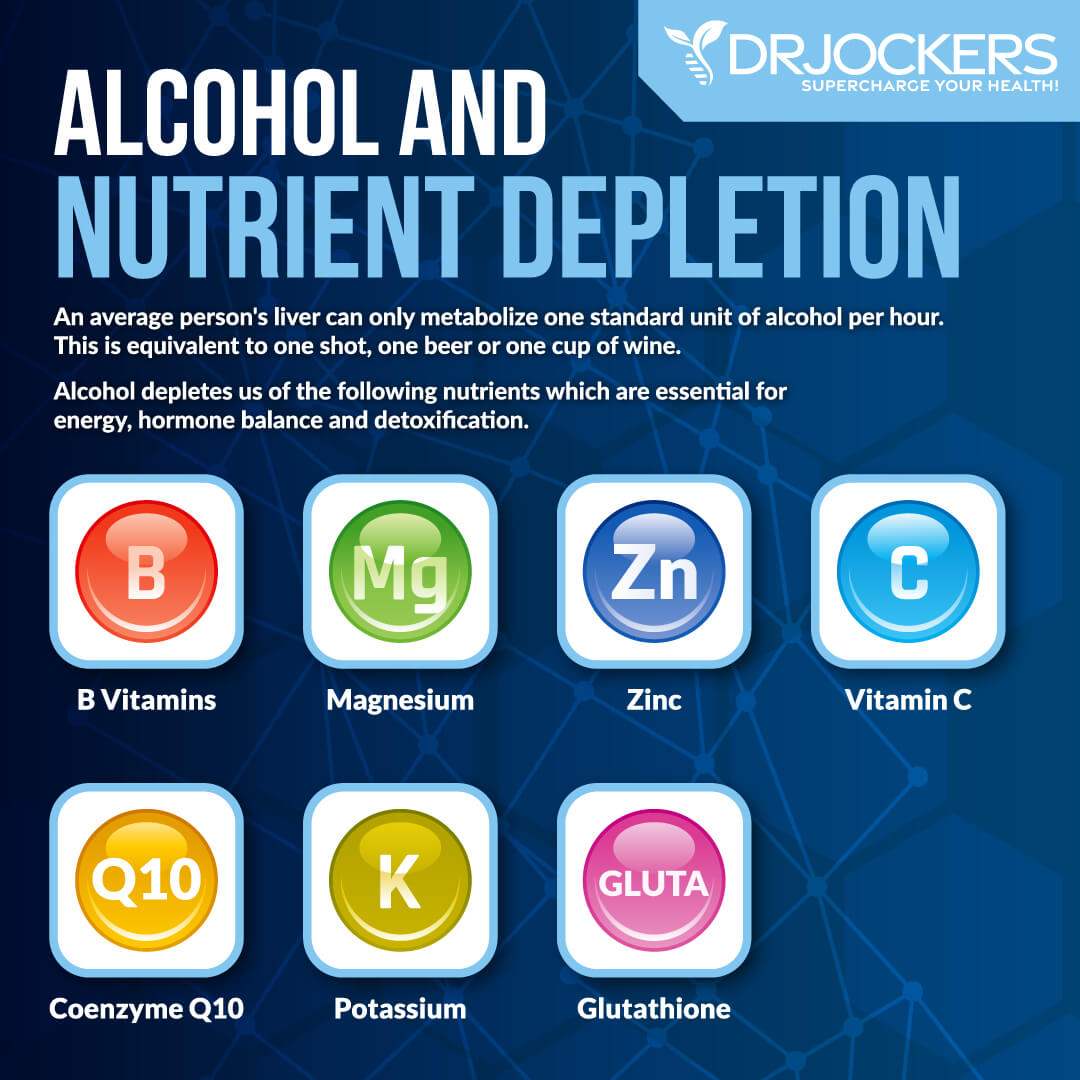
Smoking & Heavy Alcohol Use
According to the American Cancer Society, smoking and heavy alcohol use can both increase your risk of colon cancer (4). A 2010 study published in the Journal of National Cancer Institute has found that cigarette smoking can increase the risk of colon cancer (20). If you are a smoker, you are inhaling chemicals and toxins that increase free radical and DNA damage in your body. This can contribute to the mutation of healthy cells and the development of precancerous polyps, and increase the risk of colon cancer.
While smoking cigarettes should be avoided completely, drinking alcohol occasionally can be okay. However, heavy alcohol consumption can cause problems. According to a 2017 study published in the Journal of Clinical Oncology, alcohol use can increase the risk of cancer (21).
According to a 2014 study published in the British Journal of Cancer, this increased risk can be 1.44 folds for colon cancer (22). A 2011 meta-analyses published in the Annals of Oncology has also found that even moderate drinking can increase your risk (23).
Drinking moderately or occasionally was defined as 2 to 3 drinks a day and they found that the relative risk for 1.21 versus 1.52 in heavy drinkers drinking 4 or more drinks a day. The study suggests that drinking anything over 1 drink a day regularly can increase your risk of colon cancer.
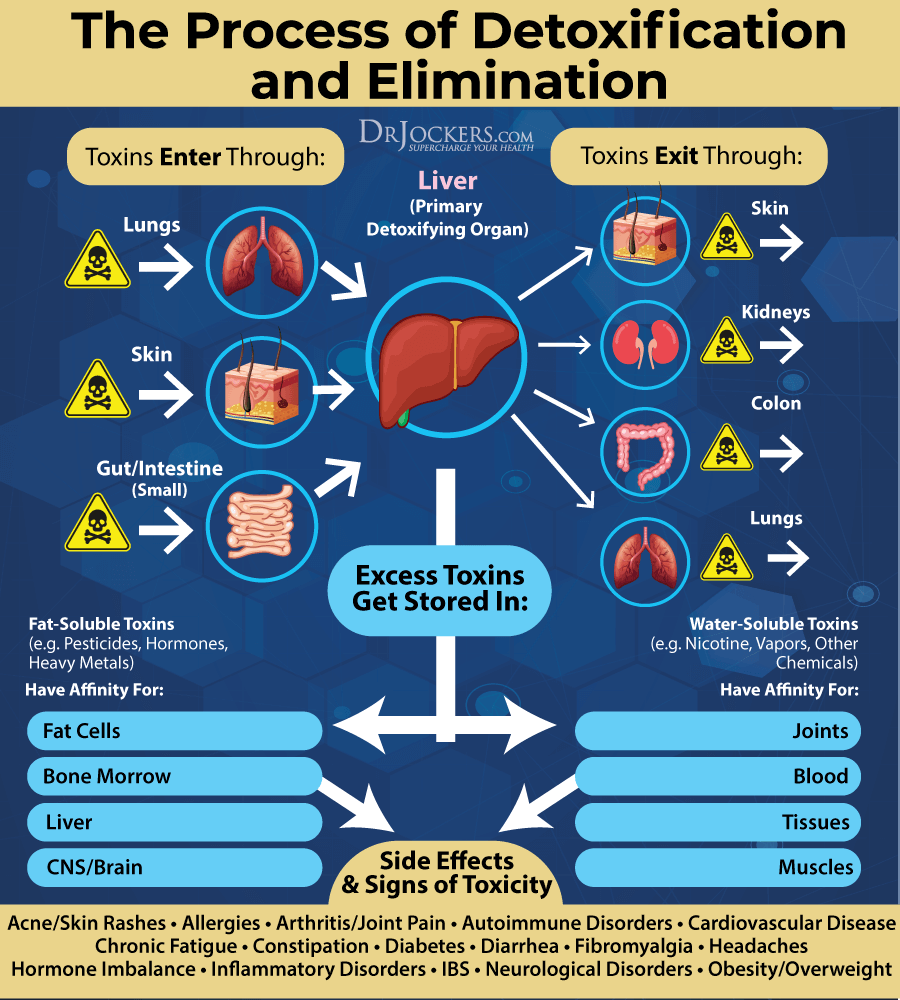
High Toxic Load
Environmental toxins can be detrimental to your health, and a high toxic load can increase your risk of colon cancer. A 2019 systematic review and meta-analysis published in Occupational and Environmental Medicine has found that workers who are regularly exposed to asbestos have an elevated risk of colon cancer and other forms of cancer, including lung, larynx, and ovarian cancer (24). A 2008 study published in the Journal of Toxicology and Environmental Health has found that arsenic exposure can increase the risk and mortality in colon cancer (25).
While asbestos and arsenic exposure is not that common among the general population and you may not have to worry about them as much, some toxins, like pesticides and mycotoxins, are a relevant issue for all of us.
A 2018 study published in Chemosphere has found that increased exposure to pesticides can elevate the risk of colon cancer (26). A 2016 study published in the Journal of Biochemical and Molecular Toxicology has found that exposure to mycotoxins can also increase your risk of colon cancer (27).
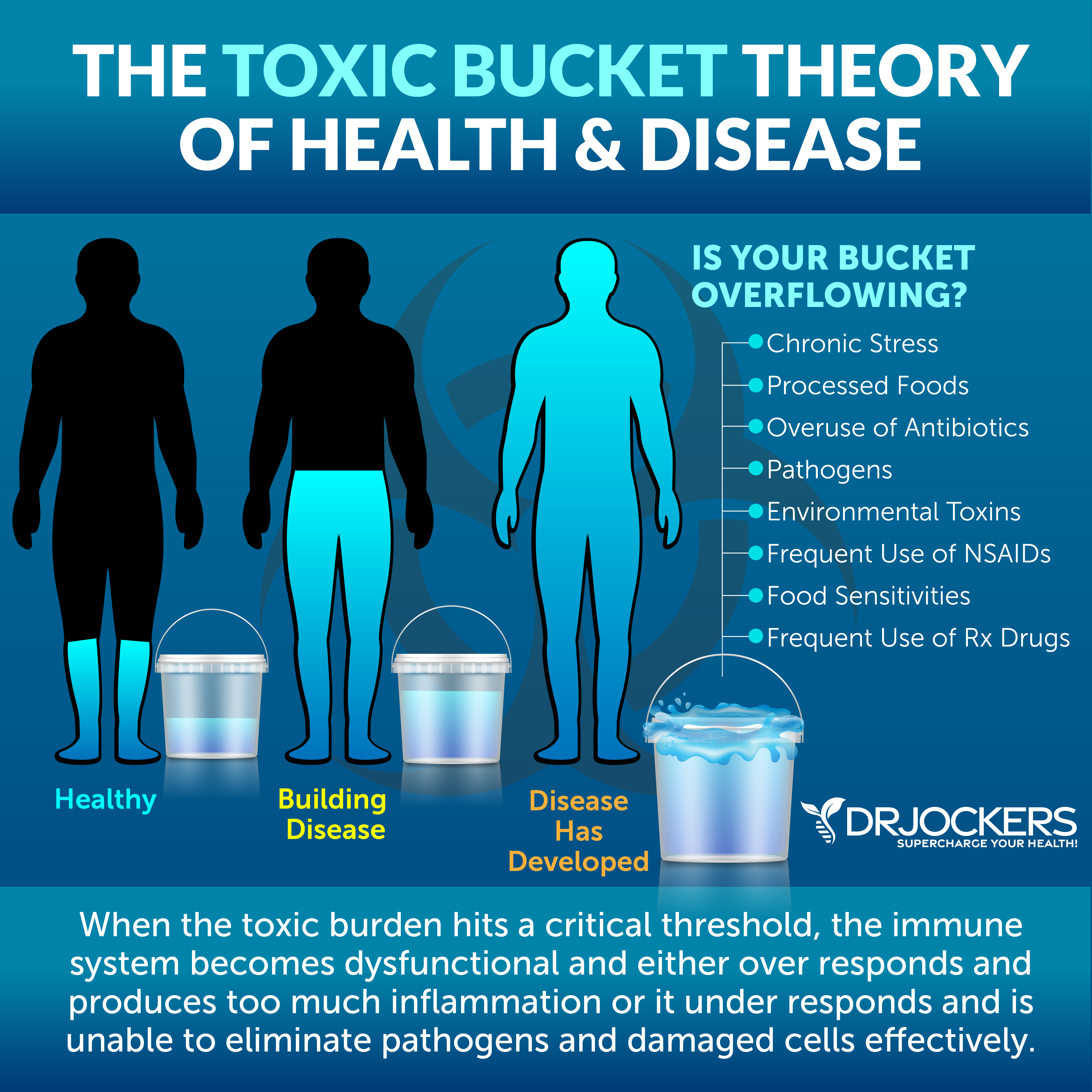
Chronic Infections & Dysbiosis
Your gut health is the base of your entire body’s health, but when it comes to colon cancer, it is clearly important. Chronic gut infections and gut dysbiosis can significantly increase your risk of colon cancer.
According to a 2012 review published in Parasite, parasites, and specifically, Cryptosporidium parvum can increase the risk of cancer impacting the digestive tract (28). A 2017 study published in PLoS Pathology has found that parasitic infections can increase the risk of colitis-related colon cancer (29).
A 2018 study published in the Journal of Laboratory and Precision Medicine has found that gut dysbiosis is associated with chronic inflammation, obesity, and inflammatory bowel disease, and can increase the risk of the development of colon cancer (30). A 2020 review published in Digestion has found that a diverse microbiota is important for colon health and gut dysbiosis can increase the risk of colon cancer (31).
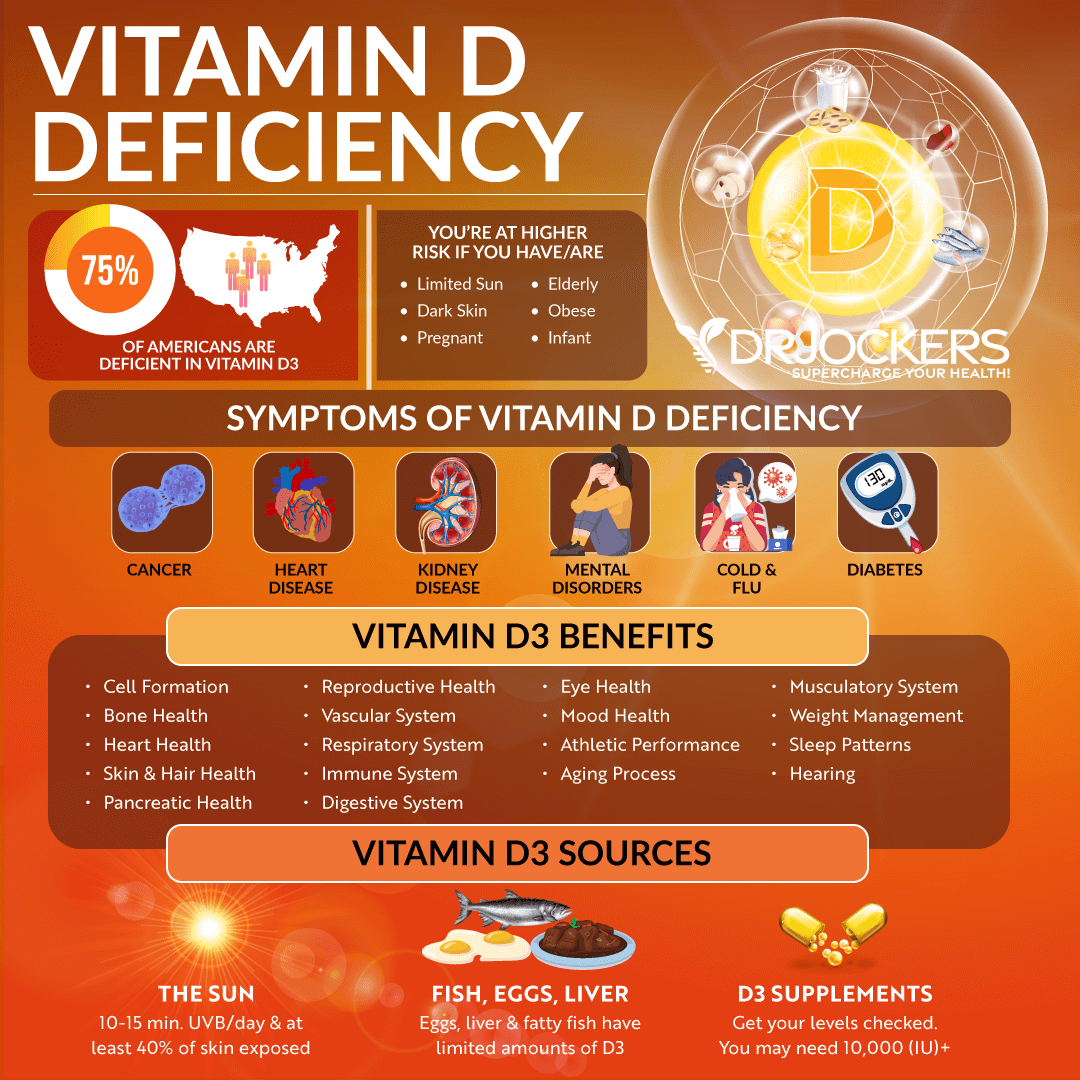
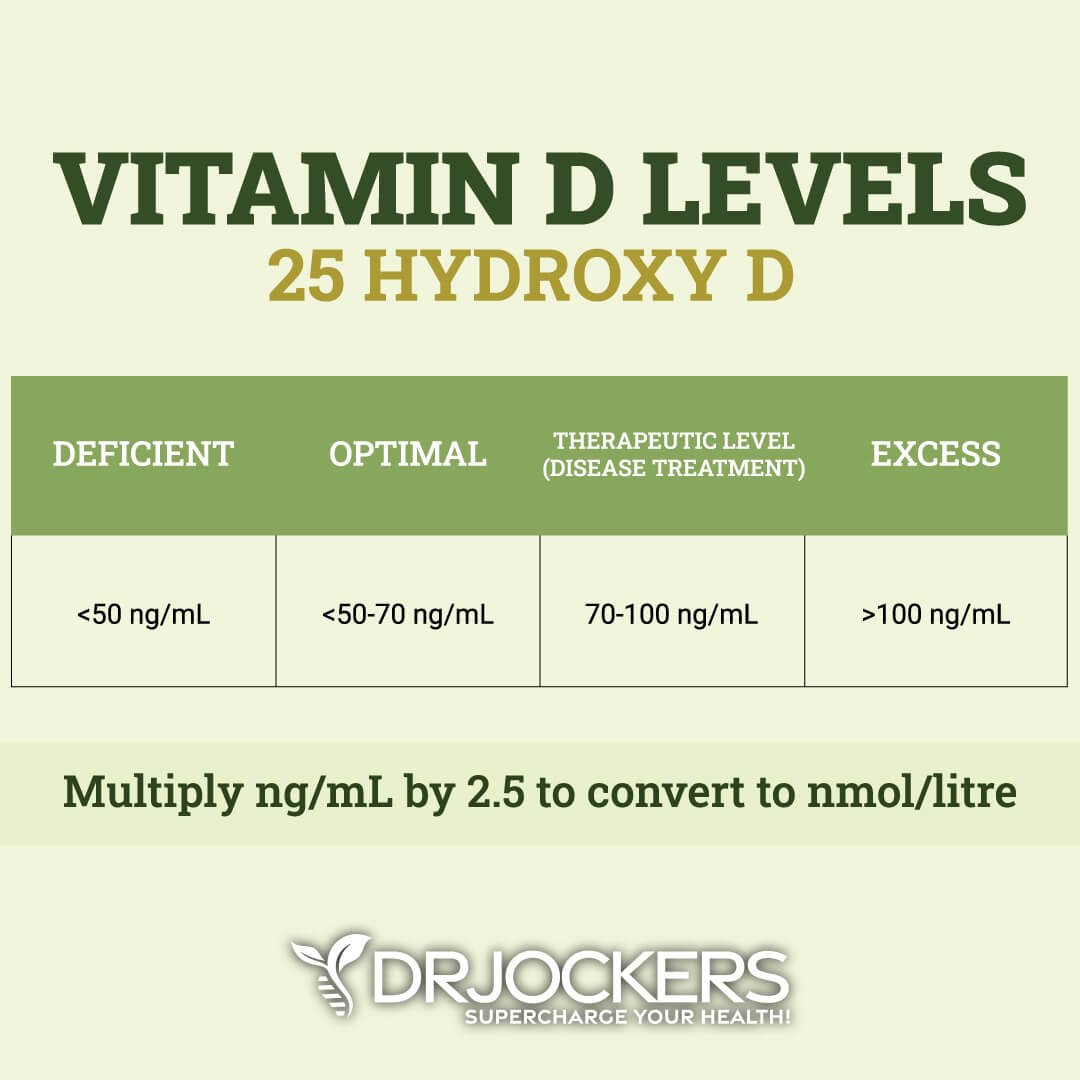
Vitamin D Deficiency
According to the American Cancer Society, vitamin D deficiency is one of the top diet and nutrition-related risk factors for colon cancer (4). According to a 2009 study published in the Journal of Environmental Pathology, Toxicology, and Oncology, low vitamin levels have been observed and play a risk in a variety of cancers, including colon cancer (32).
A 2019 study published in the Journal of Gastrointestinal Cancer has found that vitamin D supplementation can be beneficial for colorectal cancer patients receiving chemotherapy (33).
Natural Support Strategies
Reducing inflammation, balancing your blood sugar, improving your vitamin and mineral levels, and other factors play a role when it comes to reducing your risk of any disease and supporting recovery. You can support your health naturally through a variety of dietary and lifestyle strategies and smart supplementation.
While these strategies are not FDA approved to prevent, mitigate, treat or cure colon cancer, there is data that suggests they are very helpful. Please discuss these with your physician or health care practitioner.
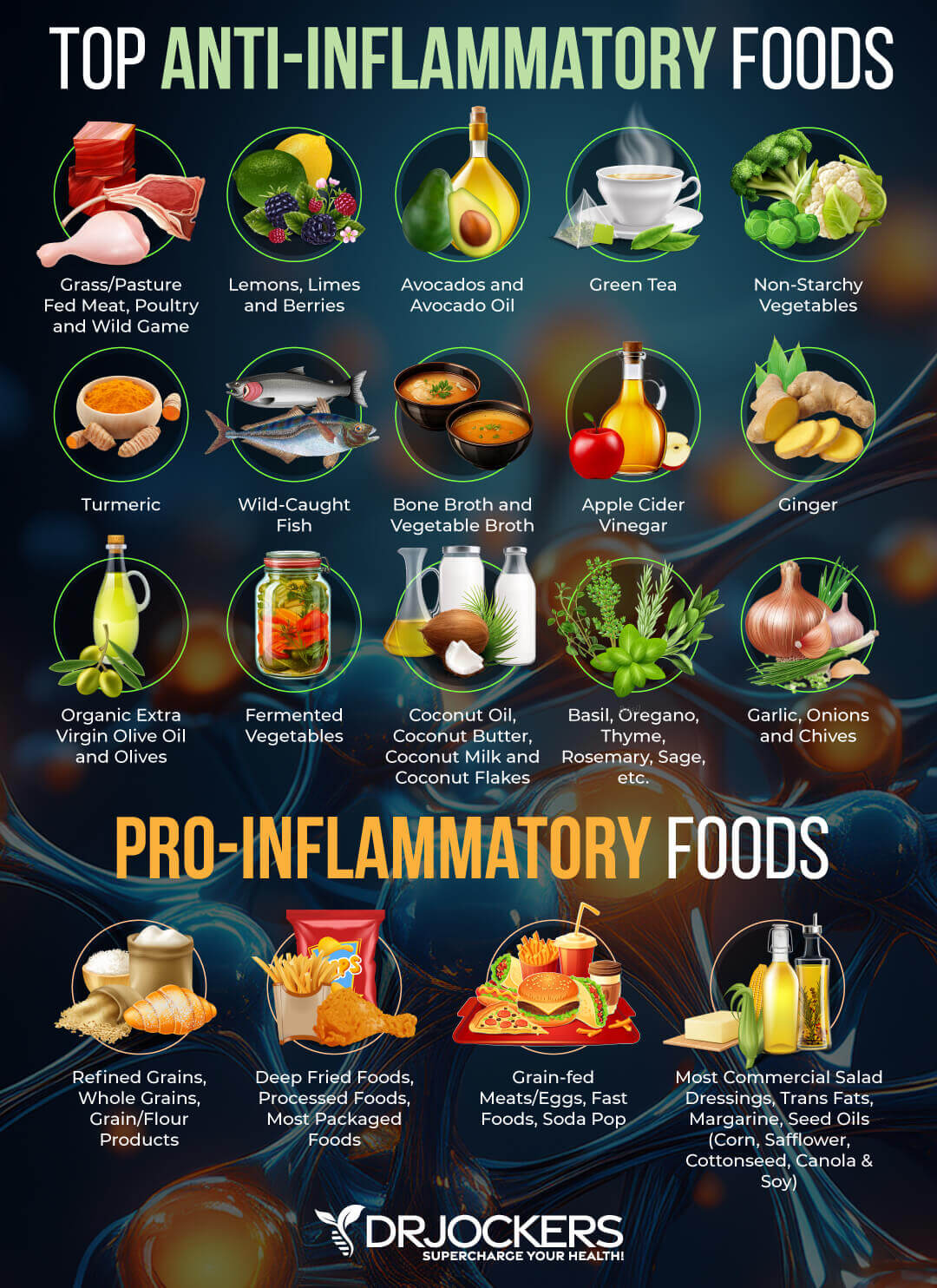
Anti-Inflammatory Nutrition Plan
Chronic inflammation can increase your risk of colon cancer (9, 10). One of the best ways to reduce chronic inflammation and support your body is by following an anti-inflammatory nutrition plan. Remove any inflammatory foods from your diet, including refined sugar, refined oils, gluten, artificial ingredients, conventional dairy, processed and canned meat, conventional animal products, heavily processed foods, deep-fried foods, junk food, and food sensitivities.
Follow an anti-inflammatory nutrient plan high in greens, vegetables, low-glycemic index fruits, herbs, spices, fermented foods, grass-fed beef, grass-fed butter and ghee, pasture-raised poultry and eggs, wild-caught fish and seafood, and wild game. Prioritize healthy fats such as olives, extra virgin olive oil, avocados and coconut oil.
Choose organic options whenever it’s possible and available to you. If you are unable to find or afford organic options for all your produce, follow the rule of the dirty dozen and clean fifteen. If a food is on the list of dirty dozen, always choose organic. If it’s on the list of clean fifteen, organic is still ideal, but if it’s not available, you may choose non-organic. If your product is not organic, make sure to wash it very well and peel it if possible.
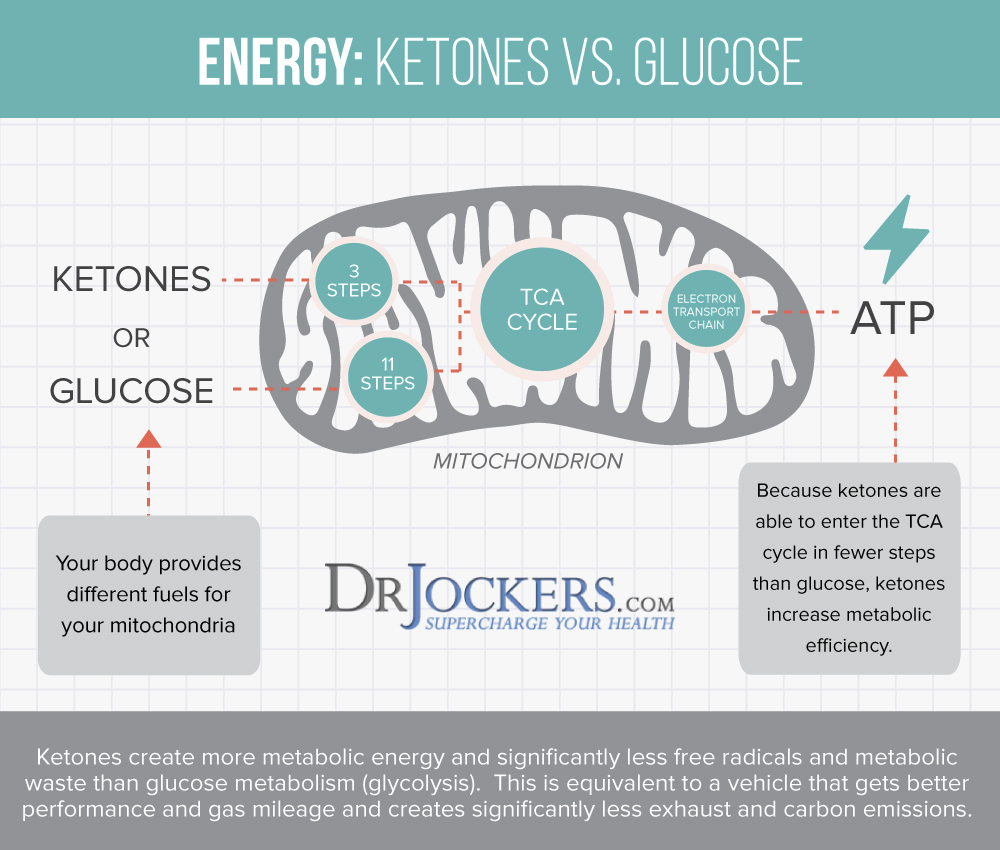
Get Into Ketosis
In normal circumstances or when following a higher carbohydrate diet, your body burns glucose for energy. When your body doesn’t have enough dietary glucose to burn for energy, it will turn to fat for energy instead and starts to make ketones in the process.
This may happen because of following a low-carbohydrate diet, fasting, famine, or high caloric restriction. Nutritional ketosis has many health benefits including reduced inflammation, increased insulin sensitivity, improved cellular renewal to a decreased risk of disease.
A ketogenic diet is a low-carbohydrate diet where you keep your carbohydrate levels very low at 5 to 10 percent, your protein levels moderate at 30 to 35 percent, and your fats high at 55 to 60 percent of your calories. A 2017 systematic review published in the International Journal of Preventive Medicine has found that a ketogenic diet can reduce tumor growth and increase survival time in colon cancer and other forms of cancer (34).
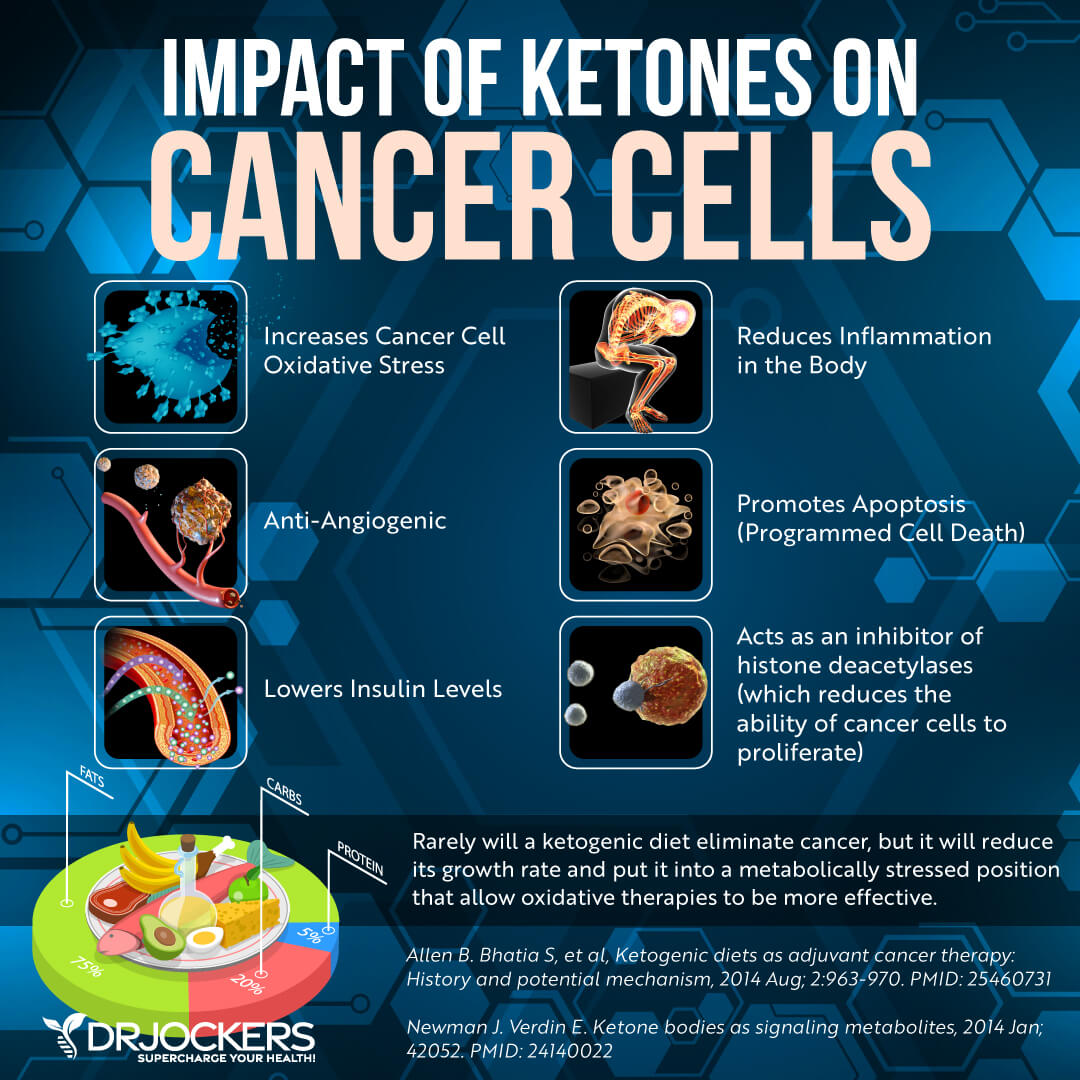
Real Food Keto Diet
I recommend that you follow a real food ketogenic diet. However, when following a ketogenic diet it is important that you eat a real food keto diet instead of dirty keto. Real food keto is a diet rich in anti-inflammatory and nutrient-dense whole foods as described above.
The dirty keto diet only focuses on your macronutrient ratios instead of nutrients. However, loading up on fatty junk foods is not going to do much for your health even if you keep it at keto-approved low-carb ratios.
High nutrition content is critical. Use the principles of the anti-inflammatory nutrition plan we discussed earlier while focusing on healthy fats and keto-approved macronutrient ratios.
Most of your diet should be made up of healthy fats, including avocados, coconut oil, coconut butter, coconuts, avocado oil, extra-virgin olive oil, pasture-raised butter and ghee, lard, flax seeds, hemp seeds, chia seeds, pumpkin seeds, other seeds, olives, nuts, and any fats from clean animal foods, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
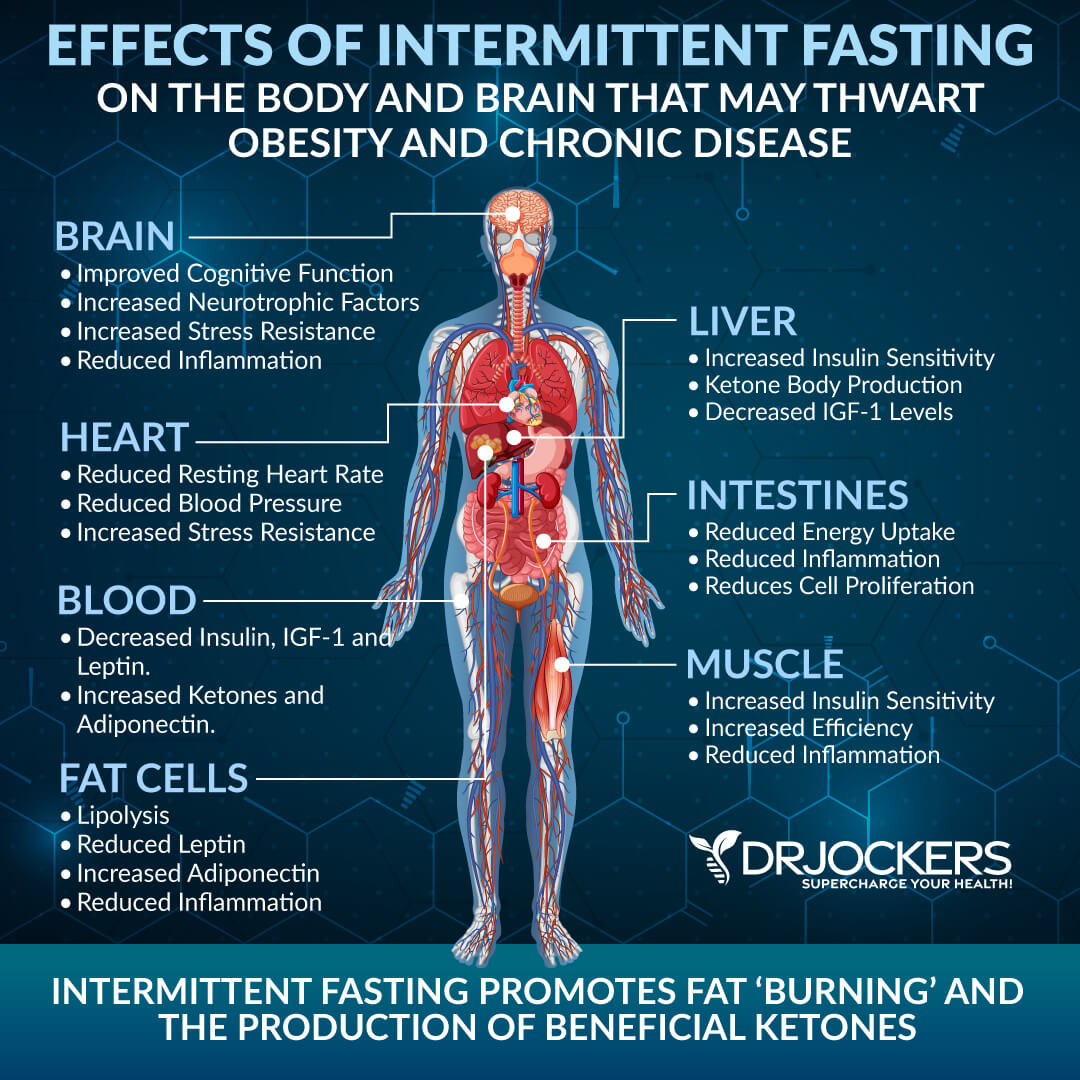
Intermittent Fasting
A 2017 study published in Oncotarget has found that dietary restriction through alternate-day fasting can help to reduce colon cancer growth (35). Fasting can support conventional treatments of colon cancer as well. A 2019 study published in the Journal of Experimental and Clinical Cancer Research has found that short-term fasting can benefit chemotherapy in terms of efficiency and tolerability (36).
According to a 2012 study published in Science Translational Medicine has found that fasting cycles can support the reduction of tumor growth during chemotherapy while protecting healthy cells (37). A 2020 study published in Signal Transduction Target Therapy has found that a fasting-mimicking diet, a form of partial fasting can support cancer treatment (38).
Intermittent fasting is a way of eating that cycles between periods of fasting and periods of eating within one day. If you are new to intermittent fasting, I recommend that you start with the Simple Fast. This method involves 12 hours of fasting including your overnight sleep.
You may start your fast after dinner and don’t eat for 12 hours until breakfast. During your eating window, focus on a nutrient-dense, anti-inflammatory, and ketogenic diet to meet your nutrient and caloric needs. Gradually increase your fasting window until you find what works for you. Most people do the best with a 16-18 hour fasting window using the 16:8 or 18:6 method.
Partial Fasting
If you are ready to experience the benefits but not quite ready to go completely without food, you may experiment with a partial fast. Partial fasts usually involve a strategy that focuses on liquids or caloric reduction. You may trial a liquid partial fast. Green Juice Fasting focuses on green juices, while Bone Broth Fasts focus on drinking bone broth for a few days.
One partial fasting strategy that I particularly recommend is the Fasting Mimicking Diet® or FMD®, a partial fasting plan that is high in nutrients, low in protein, and low in carbohydrates. On Day 1, restrict your calories to 1,100 calories a day. 500 of these calories should come from complex carbohydrates and 500 from healthy fast.
About 100 calories or 25 grams of plant-based proteins are also allowed, mainly from nuts. On Days 2 to 5, your calories are restricted to 800 calories only with 400 calories from complex carbs and 400 calories from healthy fats.
You may also turn to a Fat or Keto Fast or the Daniel Fast. The Fat or Keto Fast focuses on eating 500 to 1000 calories a day with 90 percent of those calories coming from healthy fats and helping your diet to get to ketosis.
The Daniel Fast is a Biblical fast focusing on a plant-based, vegetarian diet for 21 days. While I don’t recommend following a vegetarian diet for long-term, for a short-duration you may benefit from this high-nutrient and light meal plan.
If you are ready and doing well on longer intermittent fasting or partial fasting plans, you may try an extended fast. During an extended fast or water fast, you will be only drinking non-caloric drinks, including purified water and may herbal tea. The extended fast may last for a day or several days. This strategy is only for those who are experienced fasters. You may learn about all these fasting methods by searching my website.
Reduce Stress & Improve Sleep
Chronic stress and poor sleep can increase chronic inflammation and increase your risk of colon cancer (9, 10, 16, 17, 18, 19). Reducing your stress levels and improving your sleep are both important for your health. I recommend that you practice meditation, breathwork, yoga, journaling, guided relaxation, visualization, grounding, and prayer. Spend time in nature. Connect with friends, family, and your community, but also save yourself some me-time.
Develop an evening routine that’s calming and relaxing. Avoid electronics, sugar, alcohol, foods, and stress. Try reading, taking healing baths, sipping on herbal tea, meditation, and journaling to help you relax before going to bed. Make sure that you have a supportive mattress, comfortable pillows, and bedding, and your bedroom is a safe and calming sanctuary.

Movement & Exercise
Leading a sedentary lifestyle and obesity can increase your risk of colon cancer (4). To reduce your risk and help to manage your weight, get moving. Stretch, do a short yoga session, or take a short stroll in the morning. Go for a walk during lunch. Get up and stretch regularly throughout your day. Take the stairs instead of the elevator. Play with your kids or pets. Dance to your favorite song for a short dance session.
Workout regularly, at least five times a week combining cardiovascular workouts, like swimming, biking, jogging, or dancing, strength and resistance training, such as weight-training, bodyweight exercises, kettlebell training, CrossFit, or TRX, and low-impact exercise, including pilates, yoga, barre workouts, and TaiChi.
If you are currently undergoing cancer treatment, exercise may be difficult, but it’s important that you move your body as much as you can. Low-impact exercises and easy walks are your friends and should be done daily.

Reduce Toxin Exposure
High toxin exposure can increase your risk of colon cancer (24, 25, 26, 27). Reducing your toxin exposure is critical. Avoid second-hand smoke and polluted city environments as much as possible. Spend time in nature. Make sure that your home is free from mold. Improve your indoor air with the help of a high-quality HEPA filter system. Avoid city tap water. Invest in a water purification system and drink purified water.
Avoid pesticides, artificial ingredients, and additives in your food. Choose organic food whenever possible. Reduce your use of plastics and opt for glass, wood, bamboo, ceramic, and cloth products depending on their purpose. Avoid toxic cleaning, body, and beauty products. Choose organic, natural, and home-made alternatives instead.
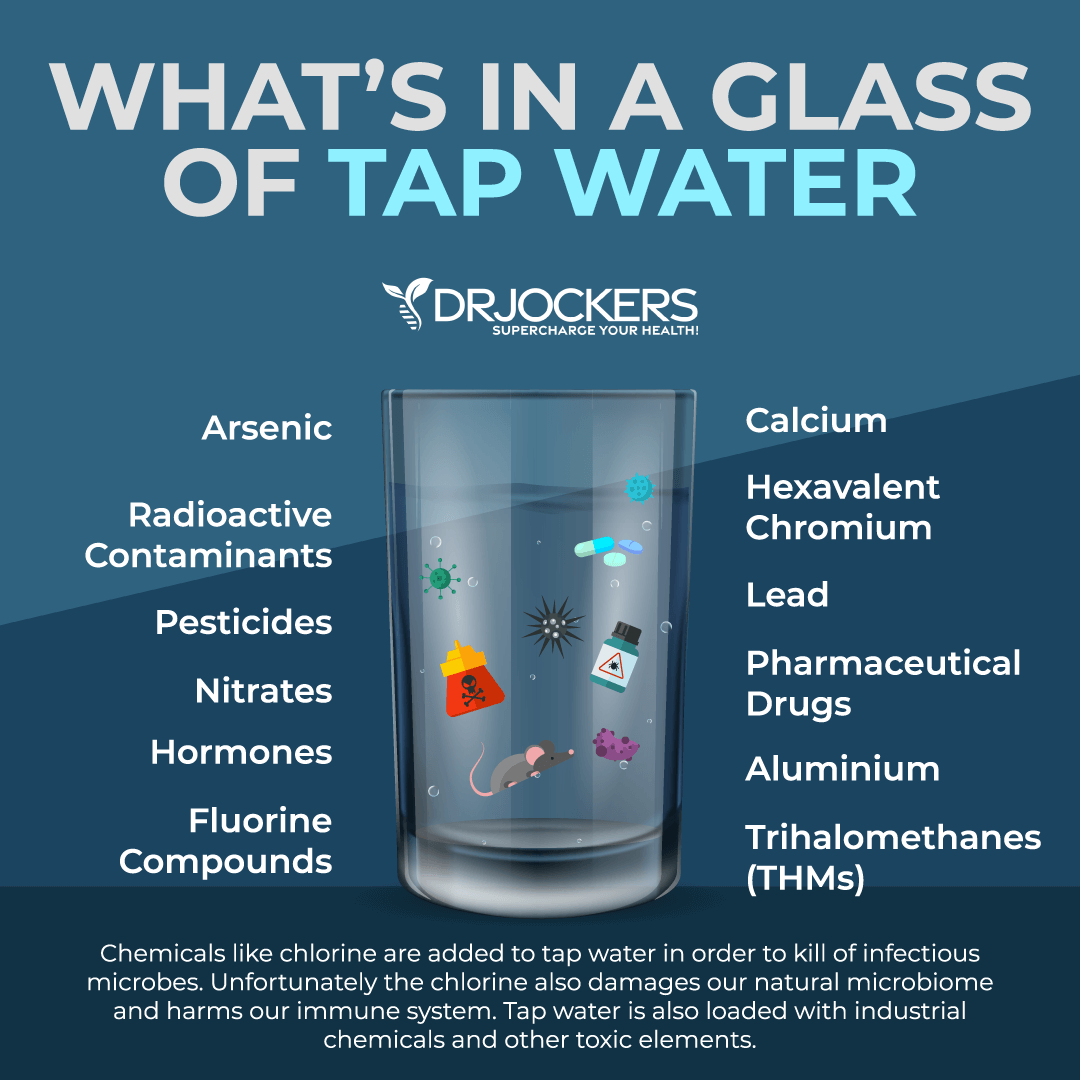
Detoxify Your Body
Avoiding toxin exposure is not enough though (24, 25, 26, 27). You have to detoxify your body from accumulated toxins. Drink plenty of water to support hydration and the elimination of toxins through urine. Try infrared sauna to support detoxification through the skin by sweating in addition to exercise. Make sure that your amalgam mercury fillings are all removed at a biological dentist.
Support your digestion, absorption, and elimination pathways through a healthy diet. Try coffee enemas to support the removal of accumulated toxins and old feces in your intestines through bowel movements.
Try activated coconut charcoal that binds to heavy metals and toxins, supports the elimination of these toxins, and reduces oxidative stress and inflammation. I also recommend Bioactive carbons derived from multiple sources of humic acid, fulvic acid, and humic acid that support the removal of heavy metals and other toxins and improves detoxification pathways.
Reduce Gut Infections
Gut infections and gut dysbiosis can seriously increase your risk of colon cancer (28, 29, 30, 31). I recommend that you test gut infections and understand your digestive health. I recommend a GI Map Stool Test for a comprehensive gut analysis.
Eating a healthy, gut-friendly diet and supporting your microbiome is important to reduce gut infections. In addition, I recommend supplementation for your specific gut infections. Mimosa pudica seed, clove, neem, berberine and oregano are great options for parasites. I recommend that you work with a functional medicine professional who can guide you with a personalized protocol. My team and I would be happy to support your journey.
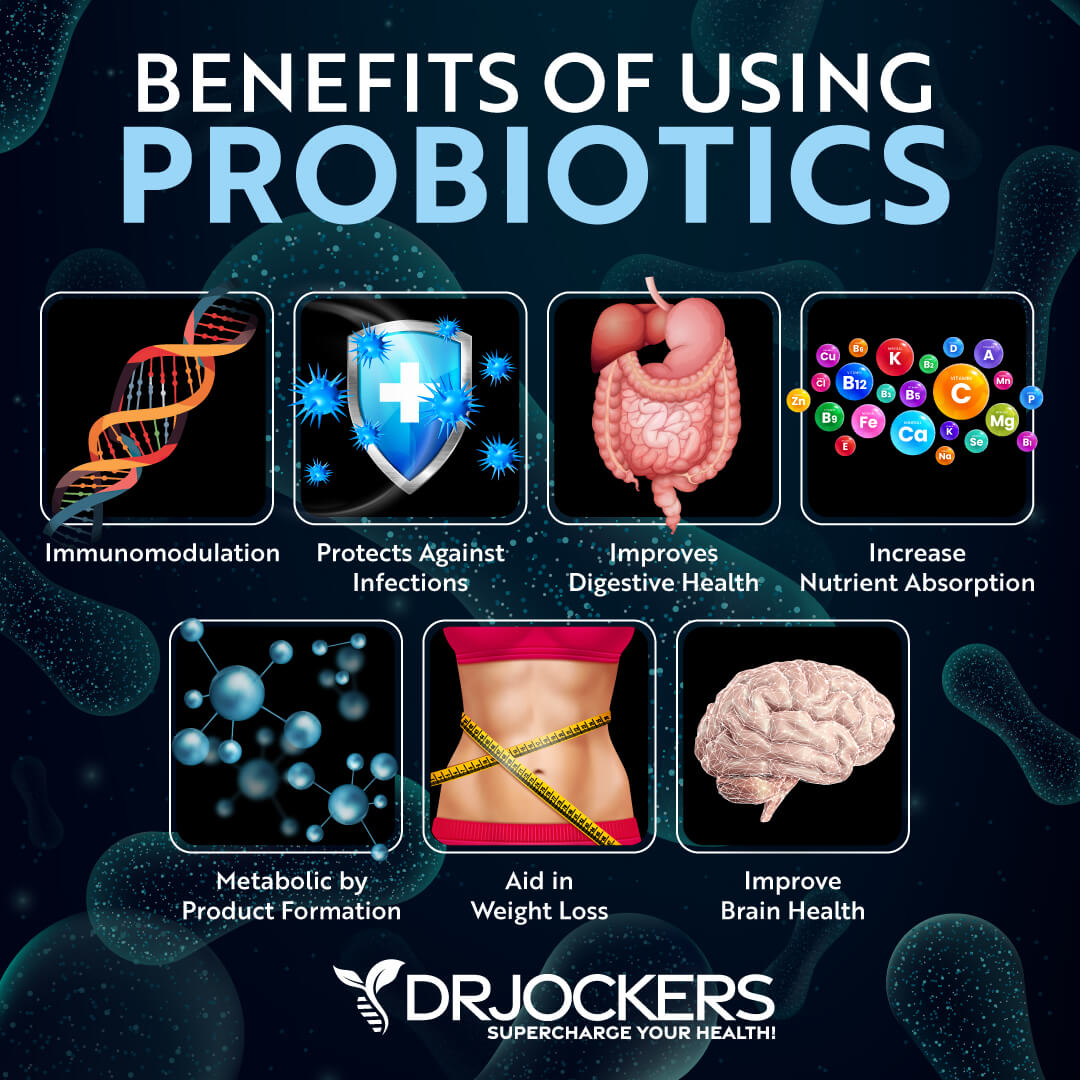
 Support Microbiome with Probiotics
Support Microbiome with Probiotics
Since chronic inflammation, inflammatory gut conditions, gut dysbiosis, and gut infections can all increase your risk of colon cancer, supporting your microbiome with probiotics is important (9, 10, 28, 29, 30, 31). According to a 2019 study published in Nutrients and a 2019 review in the Journal of Cell Physiology, probiotics can play a role in the prevention and treatment of colon cancer (39, 40).
I recommend that you eat plenty of probiotic-rich fermented foods, including sauerkraut, kimchi, fermented vegetables, and coconut kefir. Additionally, it is important that you take a high-quality probiotic supplement daily.
Optimize Vitamin D Levels
Vitamin D deficiency is a common risk factor for colon cancer (4, 32, 33). According to a 2014 study in Current Colorectal Cancer Reports, vitamin D can play a role in the prevention and treatment of colon cancer (41). A 2018 review published in the Journal of Steroid Biochemistry and Molecular Biology has found that active vitamin D metabolites can prevent the proliferation and support epithelial differentiation of colon carcinoma (42).
It can prevent the abnormal activation of cancer and protumor activities. The benefits of vitamin D in colon cancer may be attributed to its benefits on the intestinal microbiota and immune function. To improve your vitamin D levels, regular sun exposure is critical. However, with our indoor lifestyle and many of us living in cloudy, gloomy, rainy, or snowy climates for a large part of the year, sunshine is usually not enough for optimizing your vitamin D levels.
Eating foods rich in vitamin D, such as fatty fish, liver, and egg yolks, is important, but not enough. Daily supplementation is important. Using only vitamin D supplements is not enough, however, you also need vitamin K2 for proper absorption and calcium utilization. This is why, I recommend a daily Vitamin D3/K2 supplement to optimize vitamin D levels.
Typically taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for diseases like colon cancer is going to be between 70-100 ng/ml.
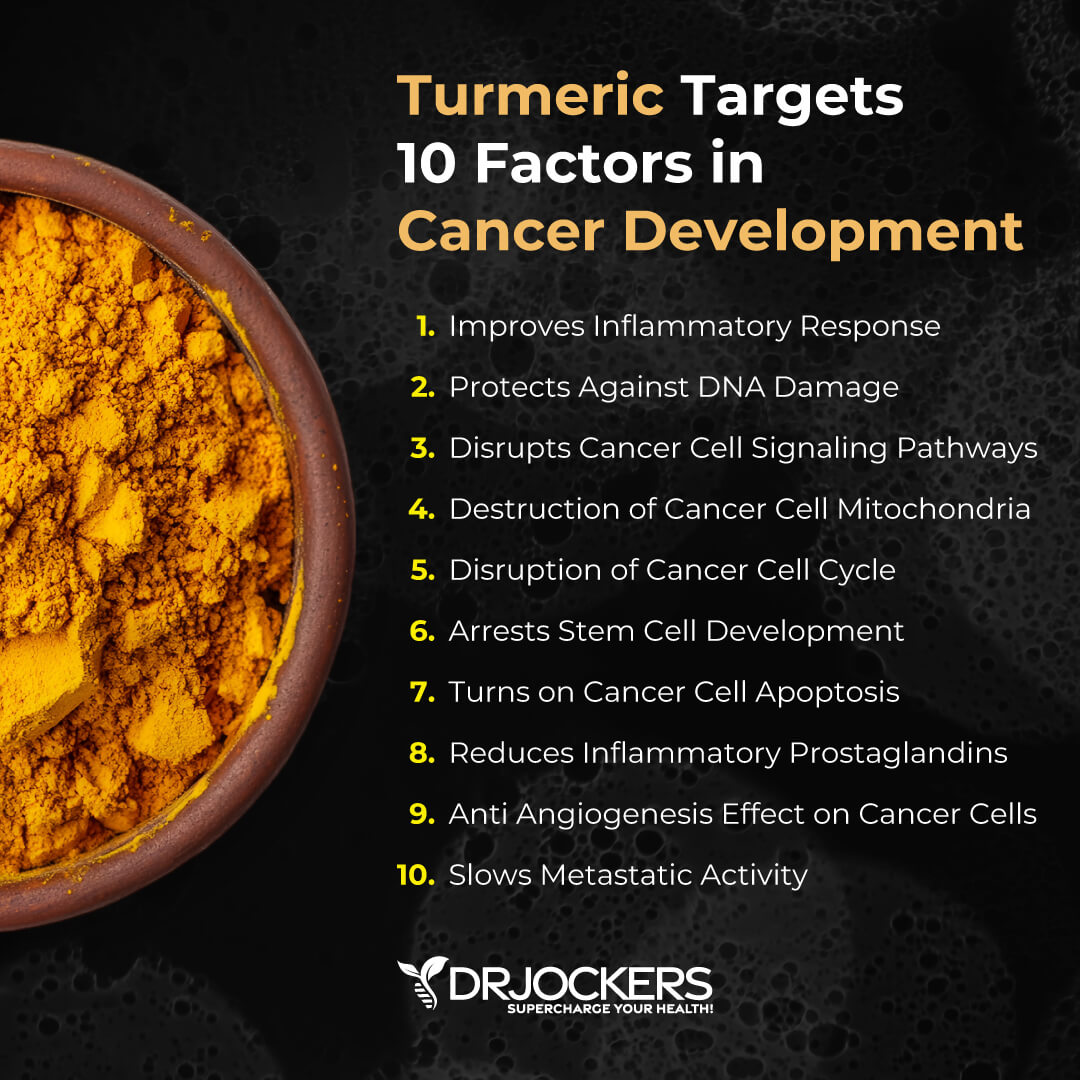
Consider Using Turmeric and Curcumin Supplementation
Curcumin is the active compound of one of the most well-researched anti-inflammatory spices, turmeric. According to a 2020 study published in the International Journal of Molecular Sciences, curcumin offers antioxidant benefits, inflammation reduction, and anticarcinogenic benefits for colon cancer (43).
According to a 2010 study published in Nutrition and Cancer, curcumin and resveratrol both play a chemopreventive role in colon cancer (44). A 2010 study published in the World Journal of Gastrointestinal Oncology has also found curcumin has anti-carcinogenic benefits on colon cancer (45). I recommend curcumin supplementation for reduced inflammation and overall health.
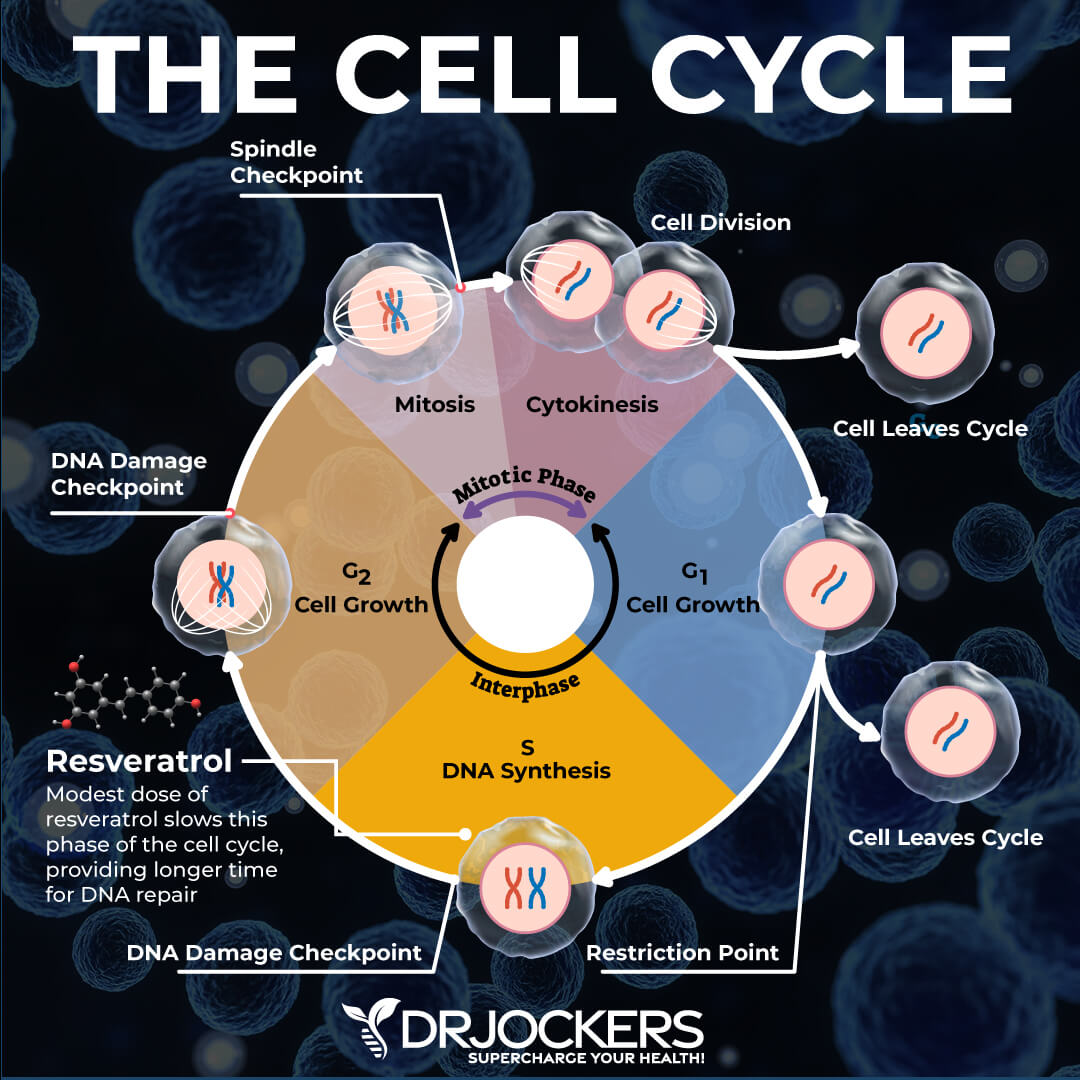
Consider Using Resveratrol
Resveratrol is an antioxidant plant-compound found in the skin of grapes, berries, and red wine. It offers anti-inflammatory and antioxidant benefits. A 2010 study published in Nutrition and Cancer has found that curcumin and resveratrol both play a chemopreventive role in colon cancer (44).
A 2019 study published in Cancer Cell International has found that resveratrol may be a promising compound for the prevention and treatment of colon cancer (46). According to a 2017 study published in Nutrition and Cancer, resveratrol can help to reduce cancer cell replication and support tumor cell death in colon cancer (47). I recommend supplementing with resveratrol for anti-inflammatory and antioxidant benefits.
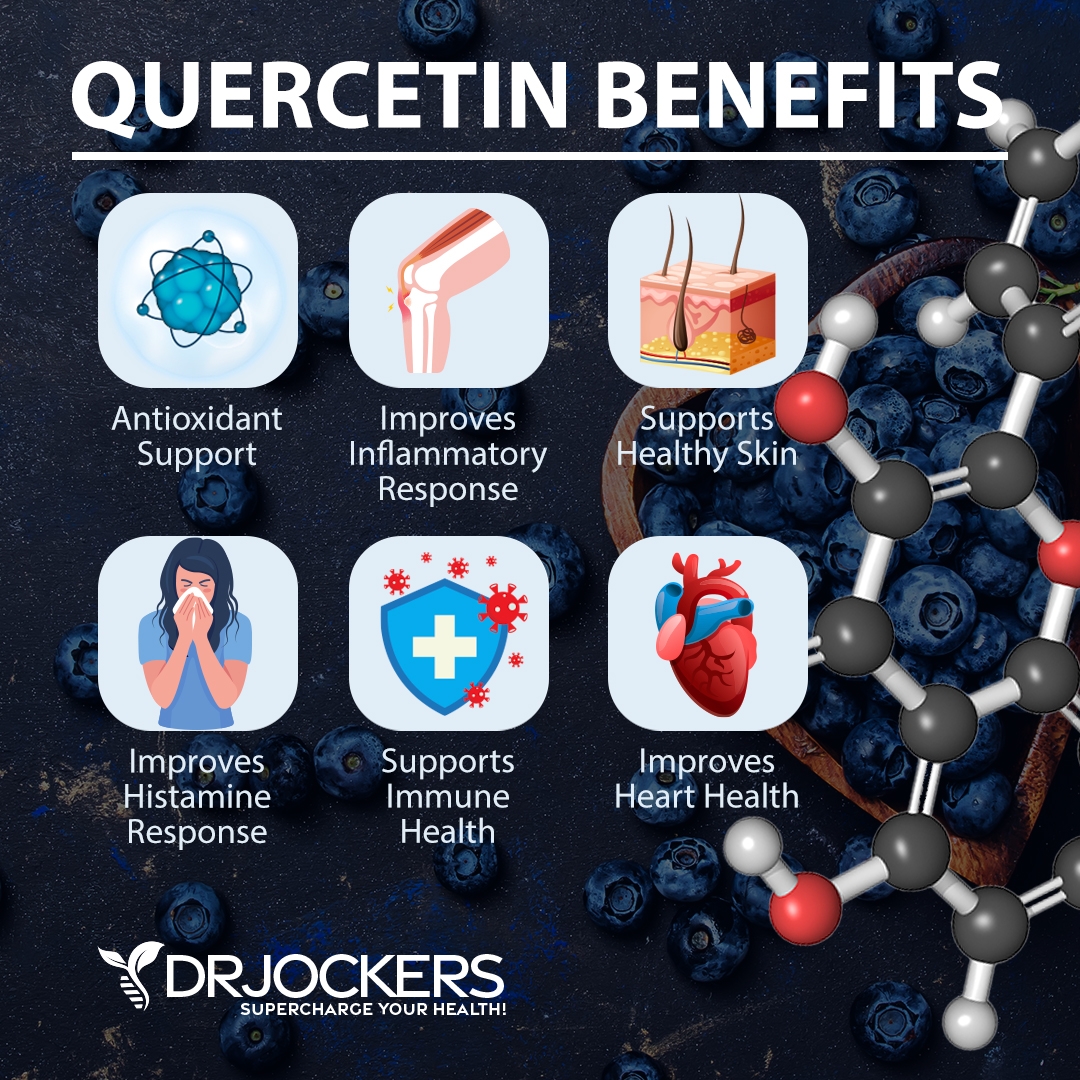
Consider Using Quercetin
Quercetin is a plant flavonoid that works well together with resveratrol, a plant compound and antioxidant found in red wine, grapes, and berries that offers anti-inflammatory benefits. A 2015 study published in Pharmacognosy Magazine has found that quercetin can reduce the growth of cancer cells in colon cancer (48).
A 2020 study published in Anti-cancer Agents in Medicinal Chemistry has found that quercetin offers anti-cancer, anti-inflammatory, antimicrobial, and cardioprotective benefits (49). It may be beneficial against colon cancer growth. I recommend supplementing with quercetin to improve your health.
Quercetin works very well together with resveratrol, but they are also commonly combined with curcumin in anti-inflammatory supplements. I recommend supplementing with all these compounds. You can find some high-quality supplements for inflammation defense that include all there, curcumin, resveratrol, and quercetin, and possibly some other anti-inflammatory herbs.
Final Thoughts
Colon cancer is a form of cancer that develops in the large intestine. It is a highly prevalent form of cancer, and it is the third most common cancer-related death in the United States. Improving your overall health and supporting your intestinal health are clearly important. I recommend that you follow my top natural support strategies to support your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




At the beginning under “signs and symptoms” shouldn’t the last item be “weight loss WITHOUT trying or clear cause??”
Yes our apologies, we have updated this.
My best friend’s daughter has been diagnosed with stage 4 colon cancer. 🙁
She is 55. Her stool test was clear 2 years ago. But she had at least 2 COVID jabs.
She has had surgery.
It has spread already to perineum and some lymph nodes, but not liver or brain.
Now chemo and immunotherapy are on the horizon.
Are there any of your suggestions that SHOULD not be done during chemo?
For example (referring to your stage 3 cancer podcast), she probably should not do coffee enemas yet due to her recent colon surgery, but we would want to ensure she has regular bowel movement.
I am thinking:
* juicing of organic veggies
* Curcumin, resveratrol, vitamin D
* stress management
* exercise (especially breathwork, yoga, walking) daily and as tolerated
* any suggestions to reduce the side effects of chemo or help healthy cells stay alive during chemo?
I hope your friend is better. The best thing to do moving forward is everything David mentions in this article, and without fail.
Eating a nutrient-deficient diet, storing toxins over a lifetime, and not detoxing regularly is what leads to cancer. If you do everything mentioned in this article, then your health will be restored for the long-term. As soon as you can, coffee enemas should be a regular part of your detox routine for life as well as a plant-based diet and veggie juicing. Also, try rebounding because it is the best lymphatic drainage exercise to help the body clear out toxins (aside from coffee enemas). Also, stay away from raw/undercooked meat, which introduces tapeworms/roundworms into the body. Almost everyone has parasites (even from birth) and parasites are a contributing cause of colon cancer. Our bodies create tumors to stop parasites from burrowing into our tissue. Tumors are actually our friend. But when those tumors become cancerous and the cancer proliferates, then we’re in trouble. Stick to the practice mentioned in this article and you’ll be OK. Of course, we’re all going to die, but we can all live a vibrant, long life if we stick to the protocol mentioned in this article.