 Anemia: Causes, Symptoms & Support Strategies
Anemia: Causes, Symptoms & Support Strategies
Globally, anemia impacts 1.62 billion people or 24.8% of the population. Preschool-age children have the highest percentage rate of anemia in their population, coming in at 47.4%. However, non-pregnant women have the highest prevalence overall, with approximately 468.4 million women in the world that are suffering from anemia (3).
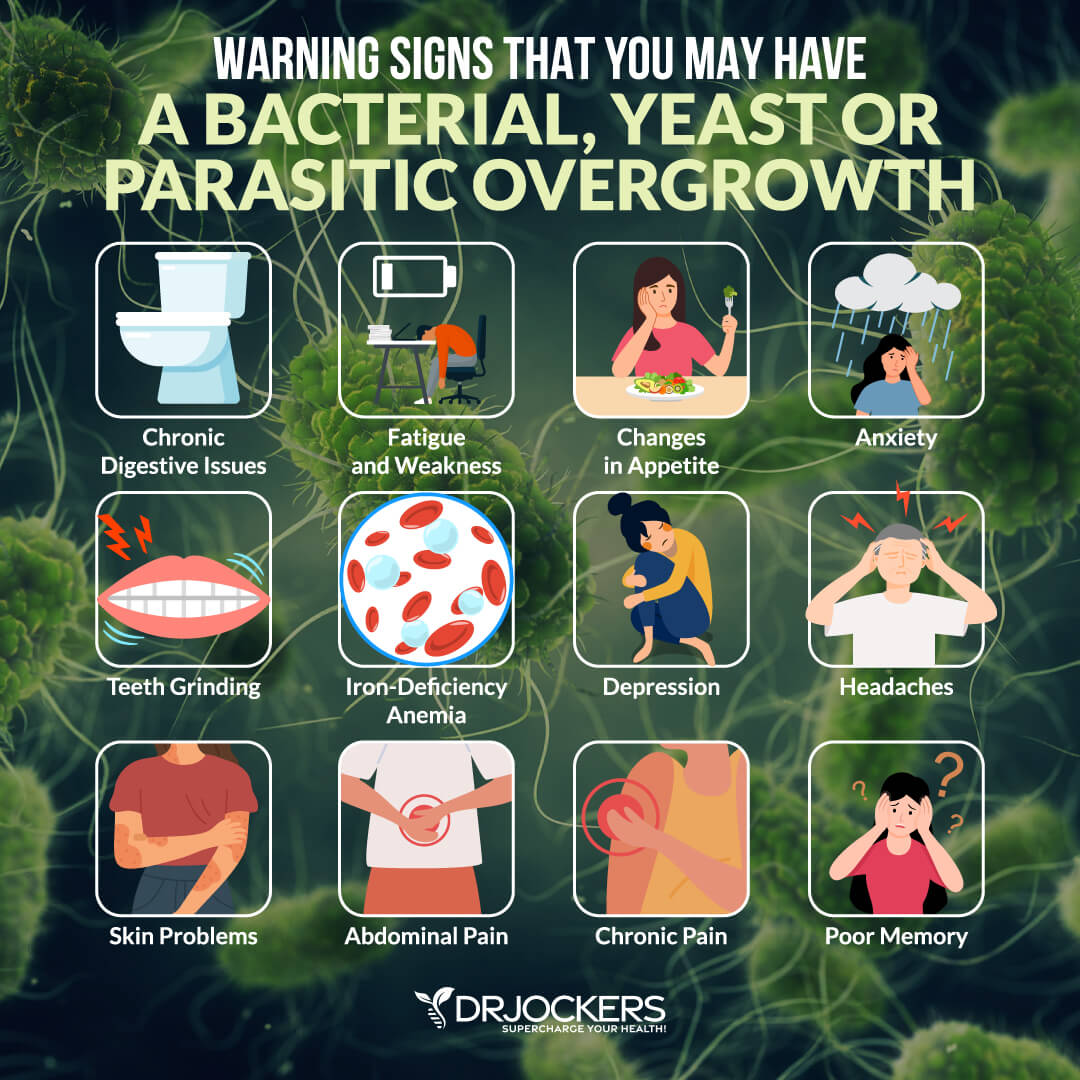
As a clinician, I see many clients who struggle with anemia and the resulting side effects. I have noticed that it is especially common with people who have yeast or bacterial overgrowth, follow a vegetarian diet, or consume inflammatory foods.
I have seen improvements with clients who take the initiative to seek out the root cause of their anemia and address the diet as needed or include supplementation if necessary.
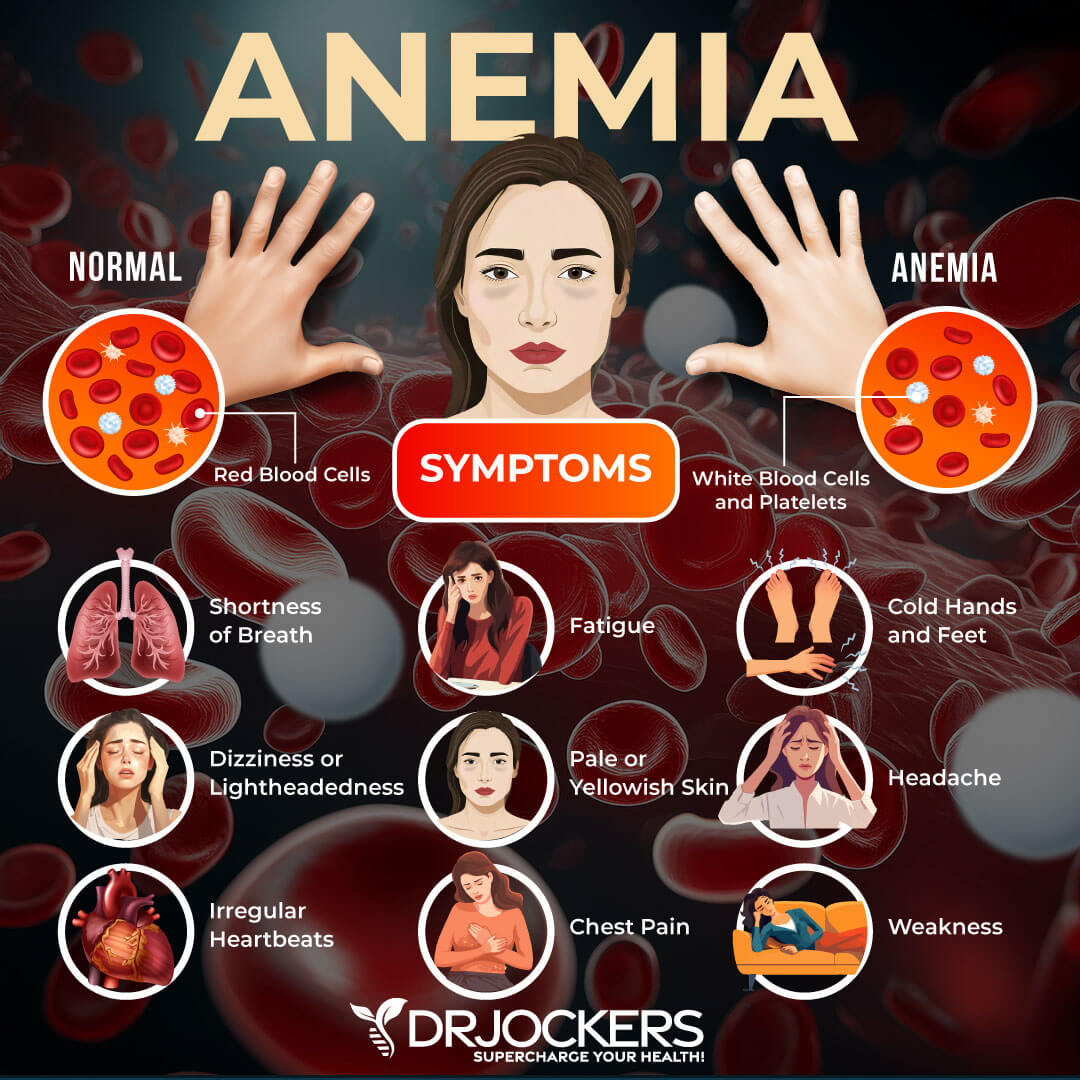
Warning Signs
- Fatigue
- Weakness
- Pale skin
- A fast or irregular heartbeat
- Shortness of breath
- Chest pain
- Dizziness
- Cognitive problems
- Cold hands and feet
- Headache (1).
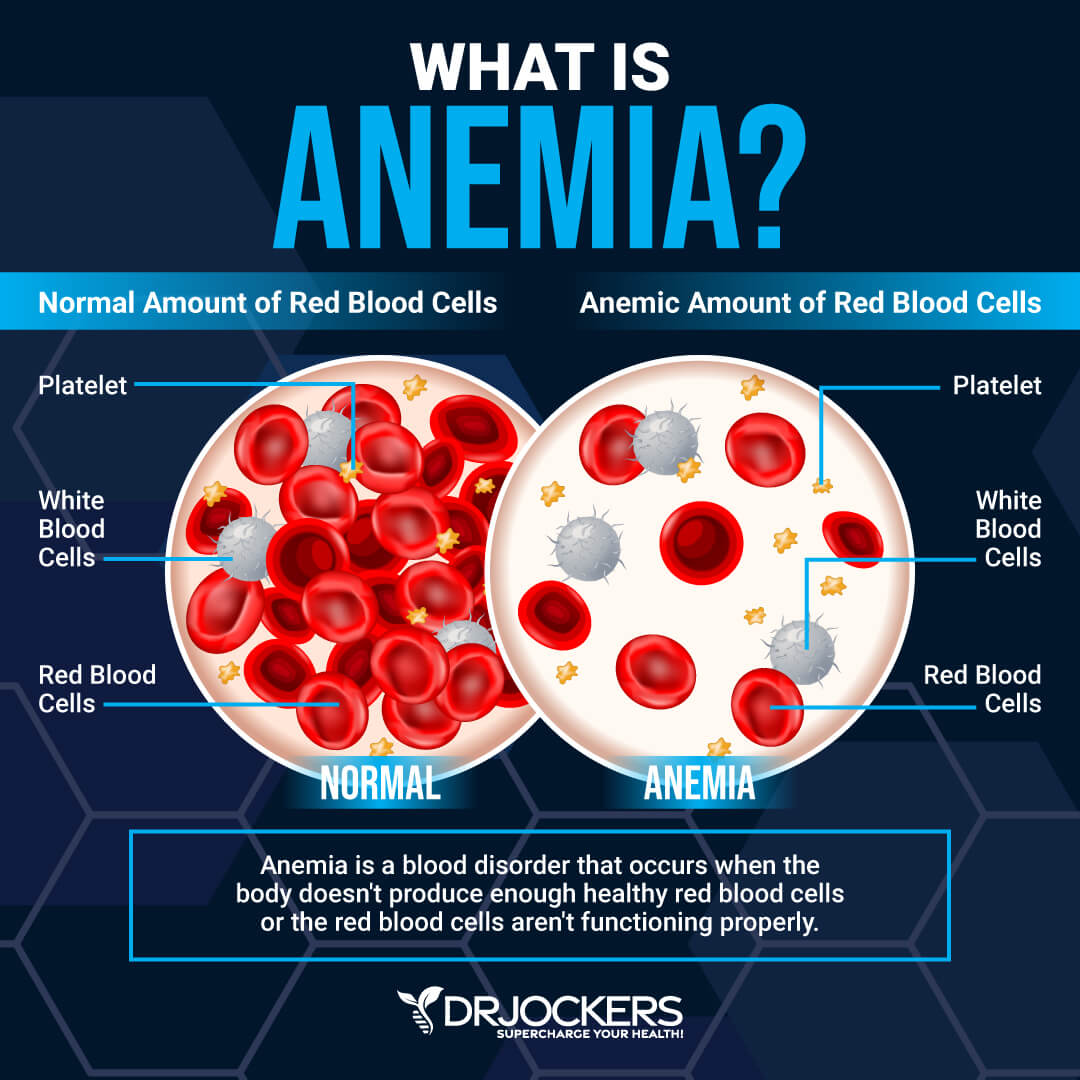
Anemia is characterized by an impaired production of red blood cells. Red blood cells are responsible for carrying oxygen to our tissues as well as removing carbon dioxide, a waste product, from our tissues and eliminating it through the kidneys or lungs.
Anemia can become dangerous when oxygenation and waste elimination are impaired enough to cause a person to become symptomatic (4). It has been known to cause permanent cognitive impairments and delayed physical development in infants if not addressed. The simple fix is typically supplemental iron.
However, if iron depletion is not the source of the problem, this can result in iron overload and still leave the person suffering from anemia and its effects. Therefore, it is extremely important to figure out the type and cause of each anemic case and address the underlying issue (5).
This article will address the different types of anemia, how to differentiate between them with testing, and solutions for resolving anemia.
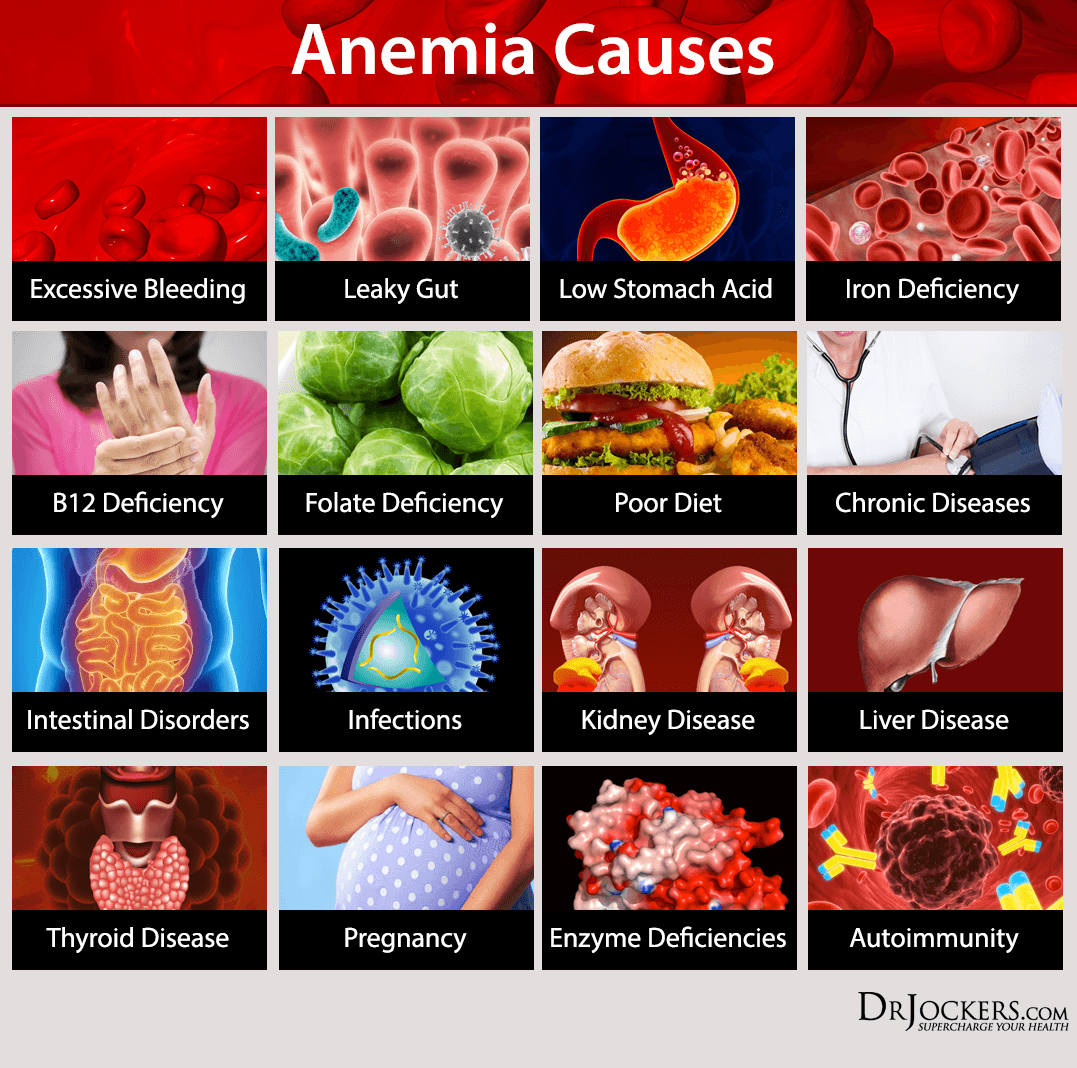
Causes of Anemia:
- Excessive Bleeding
- Leaky Gut
- Low Stomach Acid
- Iron Deficiency
- B12 Deficiency
- Folate Deficiency
- Poor Diet
- Chronic Diseases
- Intestinal Disorders
- Infections
- Kidney Disease
- Liver Disease
- Thyroid Disease
- Pregnancy
- Enzyme Deficiencies
- Autoimmunity (10).
Different Types of Anemia
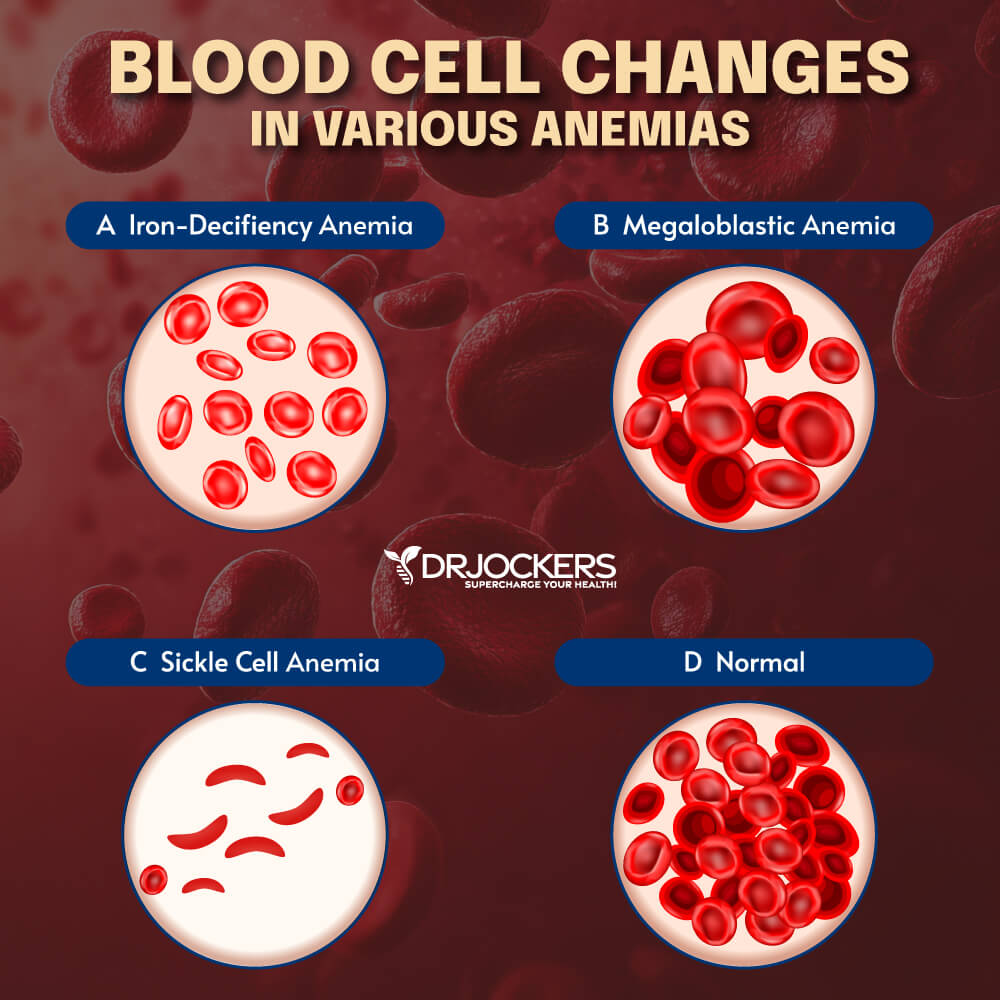
1. Microcytic (Iron Deficiency) Anemia: This is the most common type of anemia worldwide. It is characterized by small, often hypochromic (pale), red blood cells in a peripheral blood smear. This type of anemia is mostly caused by an iron deficit; this deficit occurs either because the body is not getting enough iron or it is not absorbing it properly.
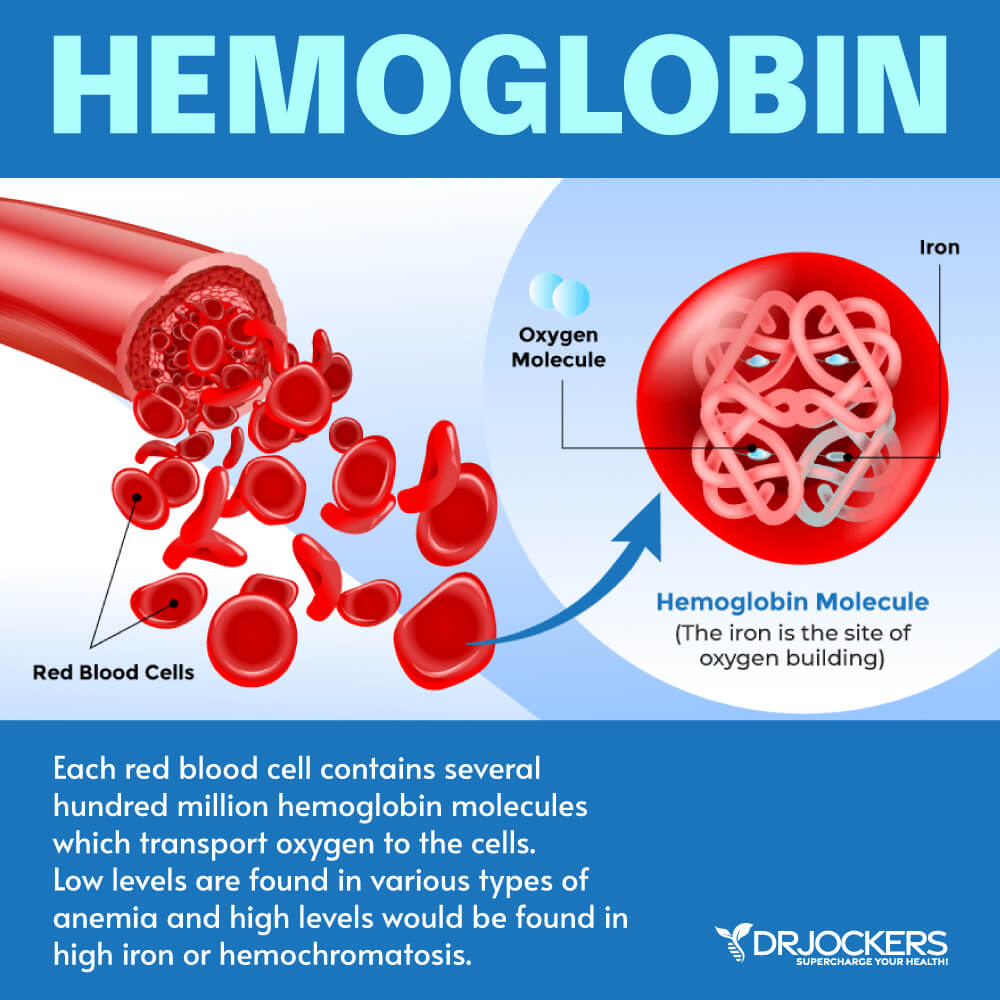
Iron is a necessity for hemoglobin production, and without it, the body cannot produce enough hemoglobin to make healthy red blood cells (5).
2. Megaloblastic (Vitamin Deficiency) Anemia: In addition to iron, your body needs folate and vitamin B-12 to produce enough healthy red blood cells. A diet lacking in these and other key nutrients can cause decreased red blood cell production. Additionally, some people may consume enough B-12, but their bodies aren’t able to process the vitamin. This can lead to vitamin deficiency anemia, also known as pernicious anemia (9).
3. Anemia of Chronic Disease: Certain diseases — such as cancer, HIV/AIDS, rheumatoid arthritis, kidney disease, Crohn’s disease, and other chronic inflammatory diseases — can interfere with the production of red blood cells.
4. Aplastic Anemia: This rare, life-threatening anemia occurs when your body does not produce enough red blood cells. Causes of aplastic anemia include infections, certain medicines, autoimmune diseases, and exposure to toxic chemicals.
5. Anemias Associated With Bone Marrow Disease: A variety of diseases, such as leukemia and myelofibrosis, can cause anemia by affecting blood production in your bone marrow. The effects of these types of cancer and cancer-like disorders vary from mild to life-threatening.
6. Hemolytic Anemias: This group of anemias develops when red blood cells are destroyed faster than bone marrow can replace them. Certain blood diseases increase red blood cell destruction. You can inherit hemolytic anemia, or you can develop it later in life. This is typically the result of an autoimmune issue where a person’s immune system attacks their own red blood cell producing tissues.
7. Sickle Cell Anemia: This inherited and sometimes serious condition that is an inherited hemolytic anemia. It’s caused by a defective form of hemoglobin that forces red blood cells to assume an abnormal crescent (sickle) shape. These irregular blood cells die prematurely, resulting in a chronic shortage of red blood cells.
8. Other Anemias: There are several other forms of anemia, such as thalassemia and malarial anemia.
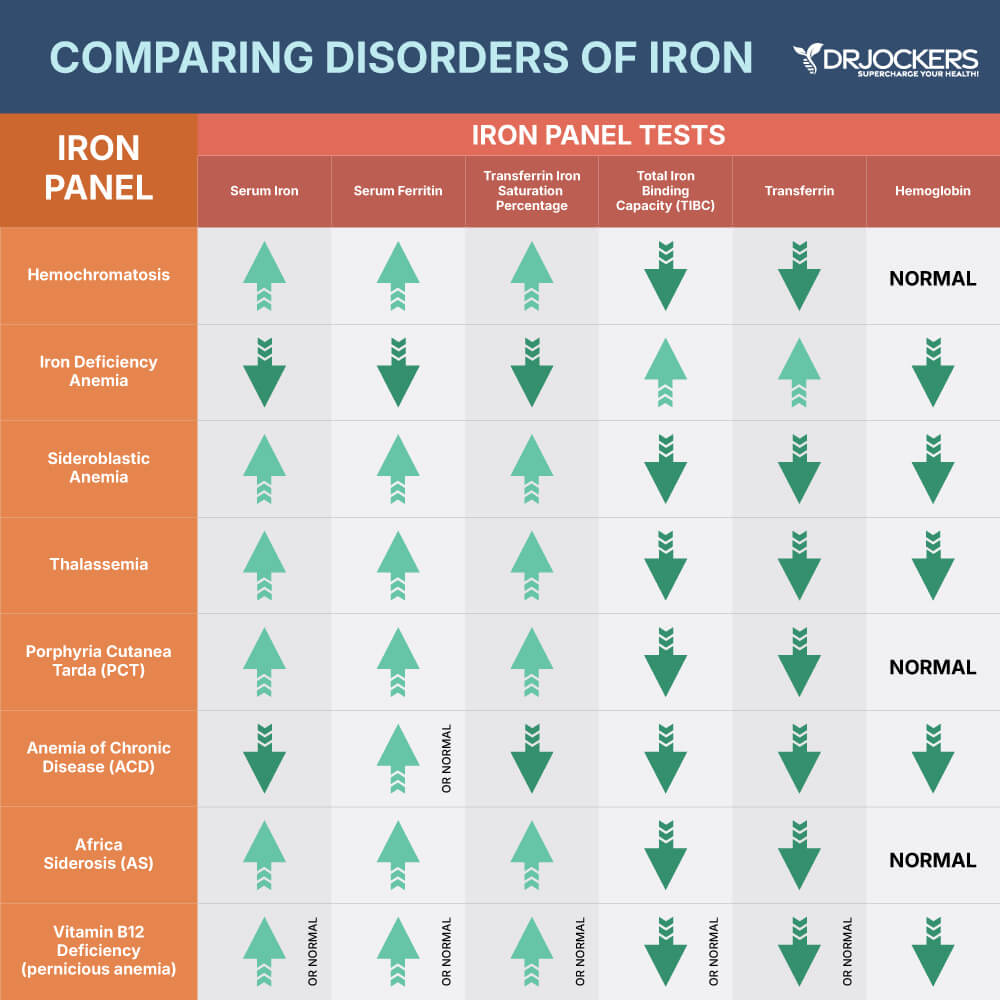
Testing For Anemia
Making the diagnosis of anemia and then differentiating between the causes can be a challenge, but it is important to identify the root cause of anemia to address it appropriately. The most accurate test is a bone marrow test, but this is expensive and invasive.
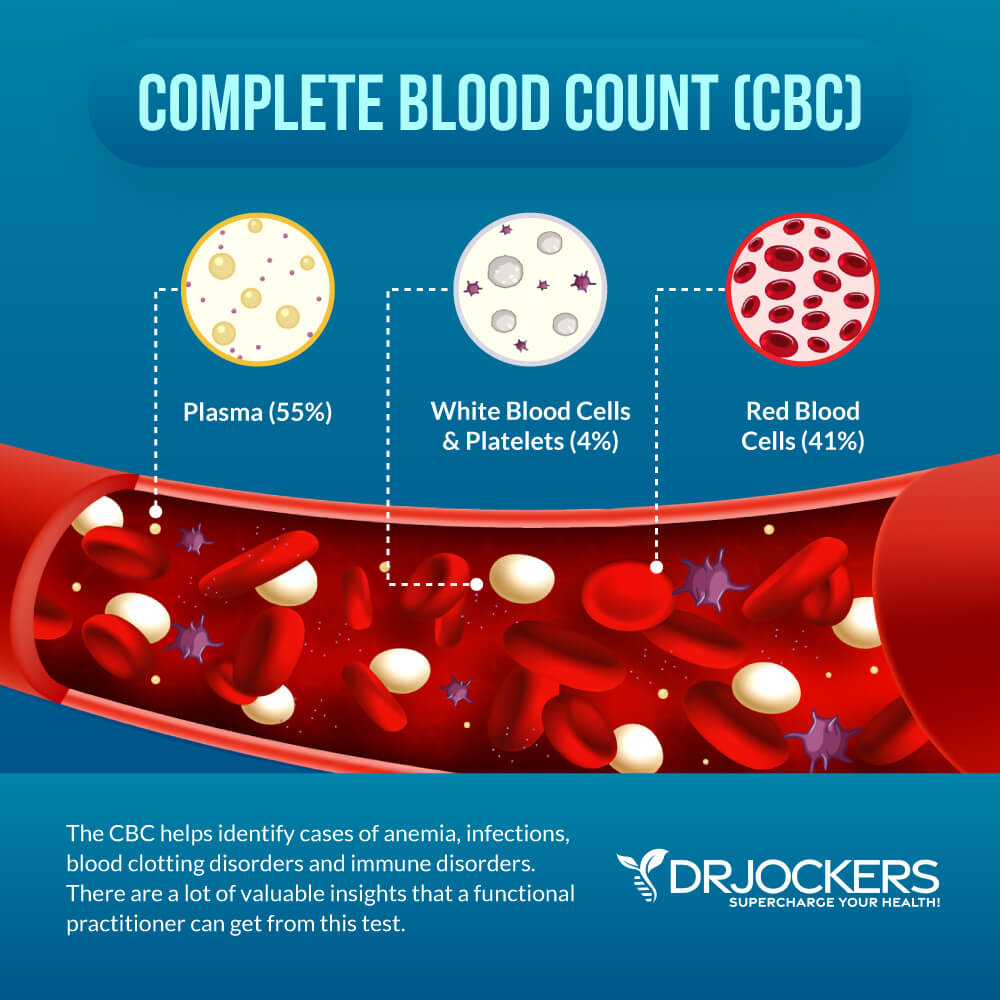
The most efficient and non-invasive way to test for iron deficient anemia is by looking at ferritin, serum iron, total iron binding capacity, and MCV levels in a blood sample (6). Other reliable indicators that aid in diagnosis include: hemoglobin, hematocrit, MCH, MCHC, and red blood cells.
Let’s break down each of these components:
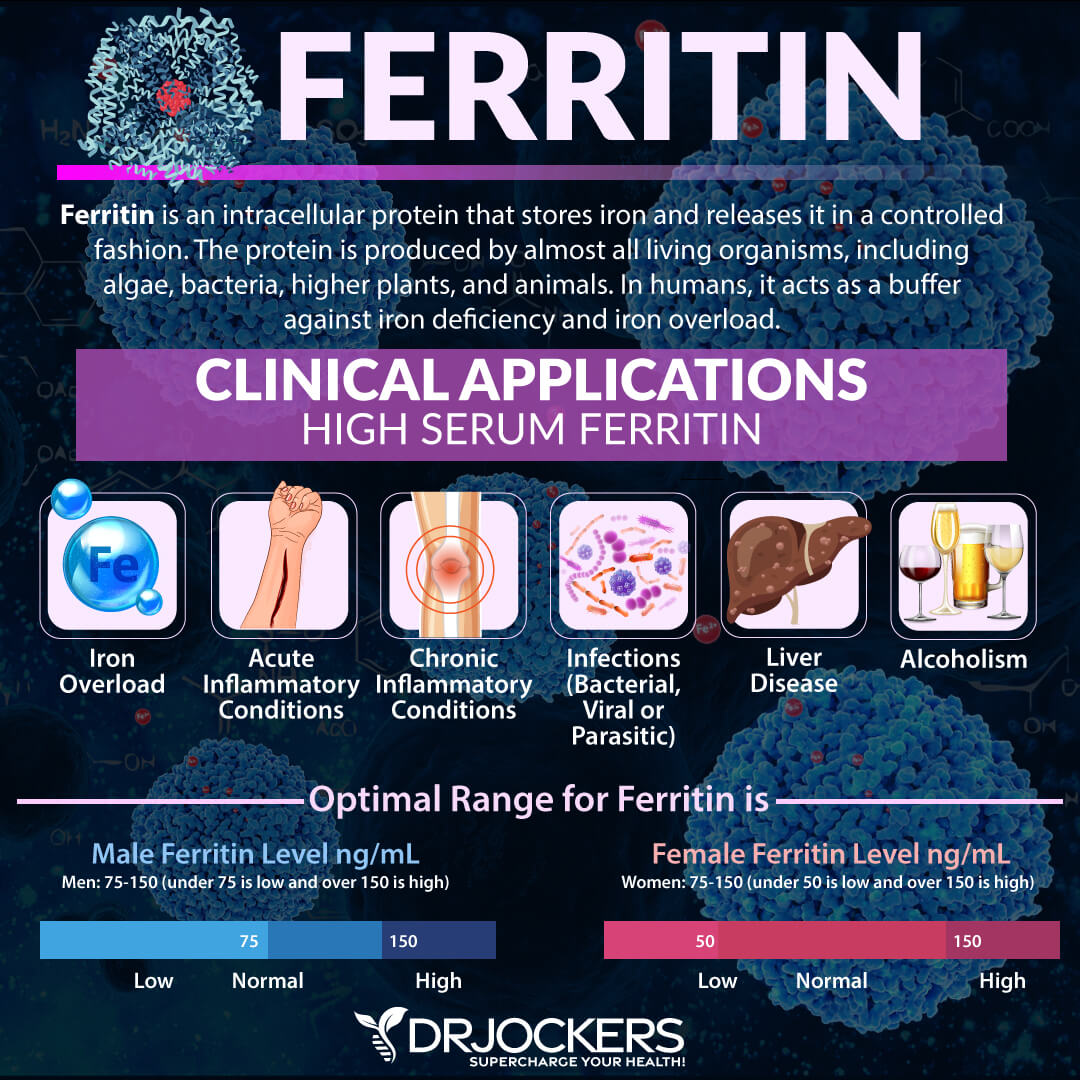
1. Ferritin: This is a blood cell protein that contains iron. This is the most reliable indicator of total iron status in the body. When it is low it indicates iron deficiency. (7). This is the first marker for early iron depletion.
However, ferritin is an acute phase reactant and is elevated with inflammatory conditions. In inflammatory conditions where iron is elevated, it is important to evaluate Total Iron Binding Capacity to identify iron insufficiency. Clinical ranges are between 15-150 ng/mL, while the functional range is between 50-150 for women and 75-150 for men.
2. Serum Iron: This is the amount of iron in the blood that is bound to transferrin and is not an accurate representation of total iron present in the body. Ferritin is a better indicator of iron deficiency due to iron being bound up in different forms that are highly variable.
However, if this is low, it is considered to be one of the indicators of iron deficiency anemia. Serum iron is elevated in hemochromatosis, which occurs when the body is iron overloaded. The lab range for serum iron is 27-159 ug/dL, while the functional range is 85-130 ug/dL.
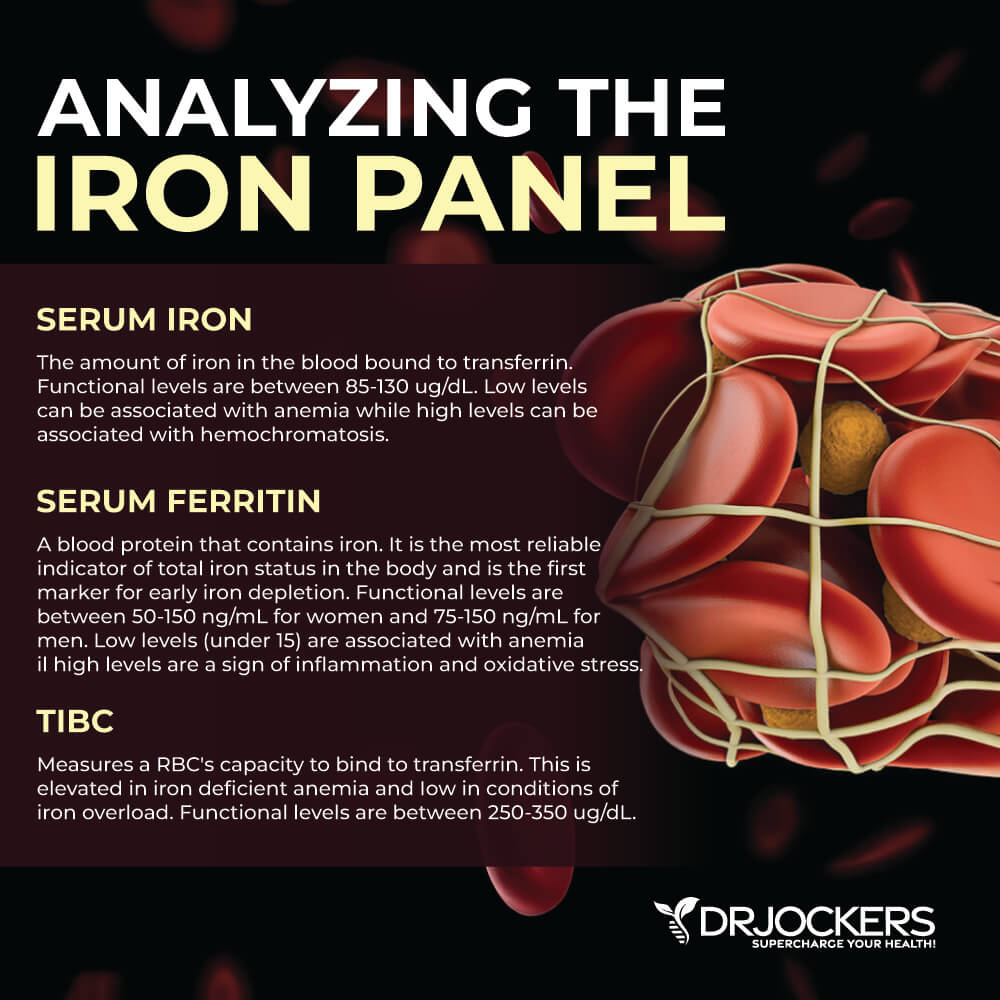
3. Total Iron Binding Capacity (TIBC): This measures a red blood cell’s capacity to bind to transferrin. This will be elevated in iron deficiency, pregnancy, and blood loss. Low TIBC can also occur in chronic disease, elevated iron loads, liver disease, and infections (8).
TIBC may be normal in anemia associated with chronic disease. The clinical lab range for TIBC is 250-450 ug/dL, while functional practitioners like to see this between 250-350 ug/dL for optimal health.
4. Hemoglobin: Hemoglobin (Hgb) carries oxygen to the cells and carries carbon dioxide to the lungs to be exhaled. This value may be low in iron deficient anemia and high in iron overload. For anemia, most labs flag this if the level is under 11.1 g/dL. For functional Hgb, the optimal ranges are between 13.5-14.5 for females and 14-15 for men.
5. Hematocrit: This is the whole blood volume that consists of red blood cells. This can be low in iron deficient anemia or if excessive bleeding has occurred. This value may be high in times of dehydration or polycythemia, which is the overproduction of hemoglobin. The clinical lab ranges are between 34-46.6%. The functional ranges for men are 39-45% while for women they are between 37-44%.
6. MCH: MCH stands for mean corpuscular hemoglobin. This is the average mass of hemoglobin per red blood cell. High levels indicate a megaloblastic anemia associated with deficiencies in folate or B12. Low levels indicate a microcytic anemia, which is typically associated with blood loss or low iron levels. The clinical lab ranges are between 26-33 pg, while the functional ranges for optimal health are between 28-32 pg.
7. MCHC: MCHC stands for mean corpuscular hemoglobin concentration. This is the average concentration of hemoglobin in red blood cells. A decrease in MCHC is an indicator of hypochromic, or iron deficient anemia. A high MCHC value indicates methylation issues and is a megaloblastic anemia. Lab ranges are between 31.5 – 35.7 g/dL. Functional ranges are between 32-35 g/dL.
8. Red blood cells are the cells designed to carry oxygen and carbon dioxide. This value can be low due to blood loss or could be associated with hemolytic anemia, which is an autoimmune disorder where the body attacks its own red blood cells. For anemia, most labs flag these if they are below 3.77 x10E6/uL. For functional analysis, we like to see these between 4-5 x10E6/uL.
9. MCV: MCV stands for the mean corpuscular volume and is the average volume of a red blood cell. Low MCV is related to a microcytic, or iron deficient, red blood cell. High MCV is related to a megaloblastic, or vitamin deficient, red blood cell. Labs will flag this if it is between 79-97 fl. From a functional perspective, we like to see it between 85-92 fl.
The Phases in the Development of Anemia
You can see the development of anemia in lab work in various phases. Once you understand these phases, you should be able to catch this condition much earlier than traditionally trained medical physicians. Here is the breakdown:
Phase I: Early iron storage depletion is marked by low ferritin levels. All the other iron and blood markers are typically normal but may even be slightly high.
Phase II: Iron deficiency non-anemia is marked by low ferritin, low iron, low iron saturation, and high total iron binding capacity.
Phase III: Iron-deficiency anemia (microcytic) is marked by low RBC, hemoglobin, hematocrit, MCV, MCH, MCHC, ferritin, iron, iron saturation, and elevated TIBC.
Phase IV: Megaloblastic anemia is marked by high MCV, MCH, and MCHC, and the individual needs B12, folate, and B6 (9).
The Comprehensive Blood Analysis is the main blood test we use for testing our clients. This includes all of these levels above and looks into other organ systems such as the thyroid, liver, cholesterol panel, inflammation markers, kidney health, blood sugar regulation, and more. The Comprehensive Blood Analysis allows us to differentiate between causes of anemia.
Natural Support Strategies for Anemia
Here are the best action steps to get started with on your journey to improve anemia. You should always consult with your physician before stopping or changing medications or taking on new health strategies. It is also important to remember that these strategies are not all FDA-approved to prevent, treat, or cure anemia.
Additionally, you should be working with a functional health practitioner to help guide you through these strategies. This is not an exhaustive list and there are other natural therapeutic strategies that I and functional health practitioners will utilize to help individuals with anemia.
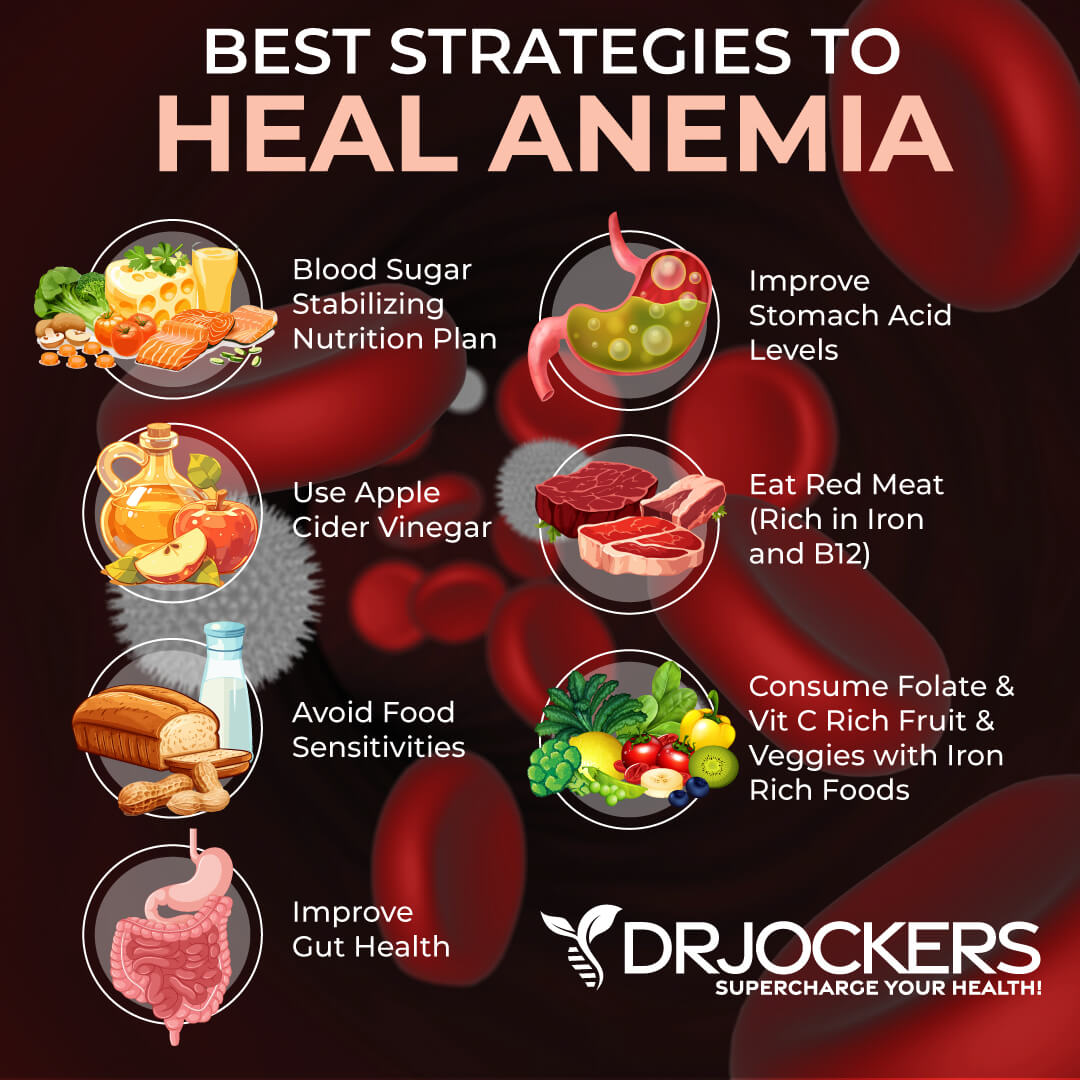
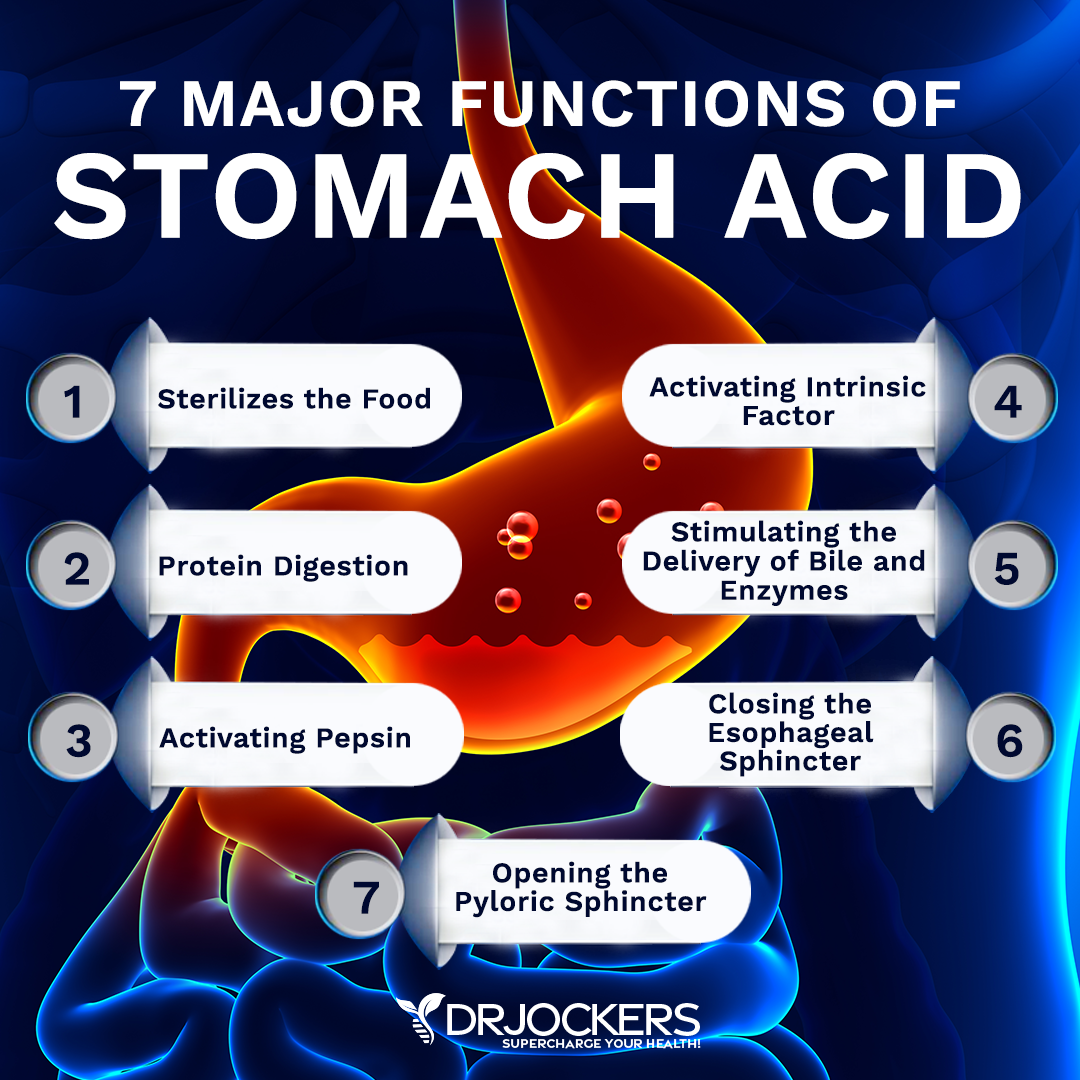
1. Improve Stomach Acid:
Low stomach acid levels are extremely common and often contribute to symptoms such as GERD (gastroesophageal reflux disease) and stomach burning. This is typically attributed to too much stomach acid induced by stress. However, low stomach acid is actually the reason for GERD in the majority of cases.
Intrinsic Factor is necessary for the absorption of vitamin B12. It is secreted by the parietal cells of the stomach lining, and without it, B12 is not absorbed or utilized by our body appropriately.
Factors that cause parietal cell death and ultimately suppress the secretion of intrinsic factors include alcoholism, ulcerative gastritis, H. pylori, and gastric bypass surgery. All of these causes should be addressed in order to repair the parietal cells (11).
Low stomach acid leads to malabsorption of many nutrients, including iron and B vitamins, and improper sterilization of food. This leaves the gastrointestinal tract at increased risk for infection. Read this article to learn methods for improving stomach acid such as an anti-inflammatory diet, apple cider vinegar, lemon, lime, and many more great ideas.
2. Use Apple Cider Vinegar:
Begin using apple cider vinegar to immediately begin improving stomach acid levels. Drink 1 tbsp of apple cider vinegar in 4-6 ounces of water prior to every meal. This provides an acidic environment for food sterilization and the proper breakdown of food.

3. Anti-Inflammatory Diet:
The average American’s diet is filled with grains and sugar that promote total body inflammation due to blood sugar fluctuations and added stress to metabolic processes. Instead, build your diet around good fats, non-starchy veggies, low glycemic fruits, herbs, and clean protein.
When our bodies are inflamed, our organs are not able to properly utilize nutrients and create necessary substances for optimal functioning. This leaves us at risk of developing issues such as anemia and many chronic diseases.
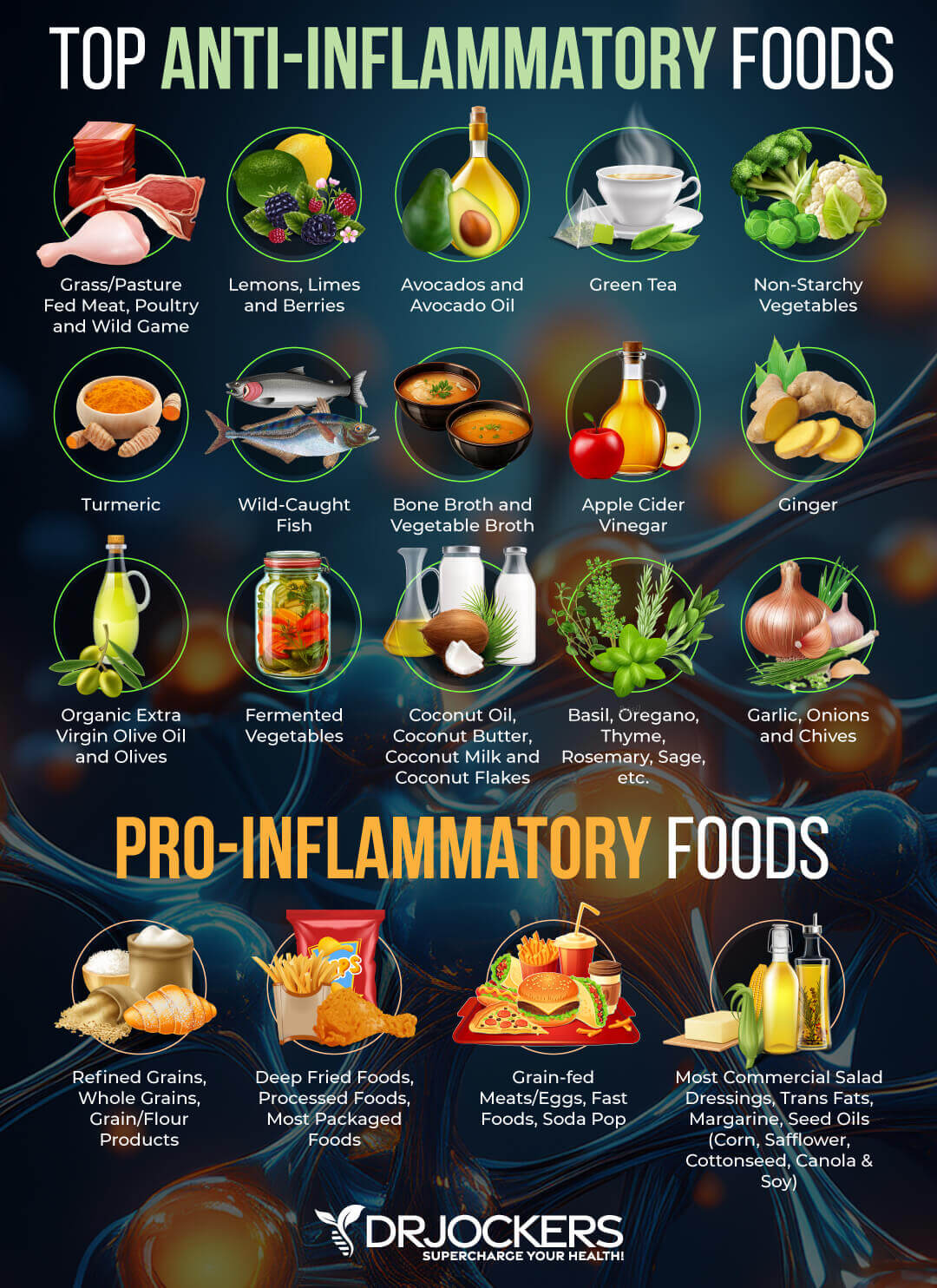
4. Eliminate Food Sensitivities:
An autoimmune condition occurs when the body’s white blood cells produce a specific antibody to target a particular tissue or enzyme within a tissue of the body. For example, when the body produces an attack on red blood cells or bone marrow, this can produce an autoimmune anemia, such as hemolytic anemia or aplastic anemia.
Based on twin studies, we now know that 25% of autoimmunity is genetic, and the other 75% is environmental (12). Dr. Jockers and I believe there are 7 main environmental factors causing autoimmunity:
- Gluten Sensitivity
- GMO’s
- Gut Dysfunction
- Neurological Stress
- Toxins
- Stress and Adrenal Fatigue
- Infections
A food elimination diet takes out the most common gut-irritating foods and allows the intestinal lining a chance to completely heal. This calms down the immune system and decreases inflammation, which will reduce autoimmunity and the side effects of autoimmune diseases.

5. Resolve Gastrointestinal Infections:
H Pylori and small intestinal bacterial overgrowth (SIBO) can result in things such as leaky gut and low stomach acid. Both of these disorders can interfere with the absorption process of iron and essential B vitamins for healthy red blood cells.
Reducing these infections is a key player in helping you get to the root cause of the anemia. You can test for H Pylori with the GI MAP Test and SIBO with the SIBO breath test here.
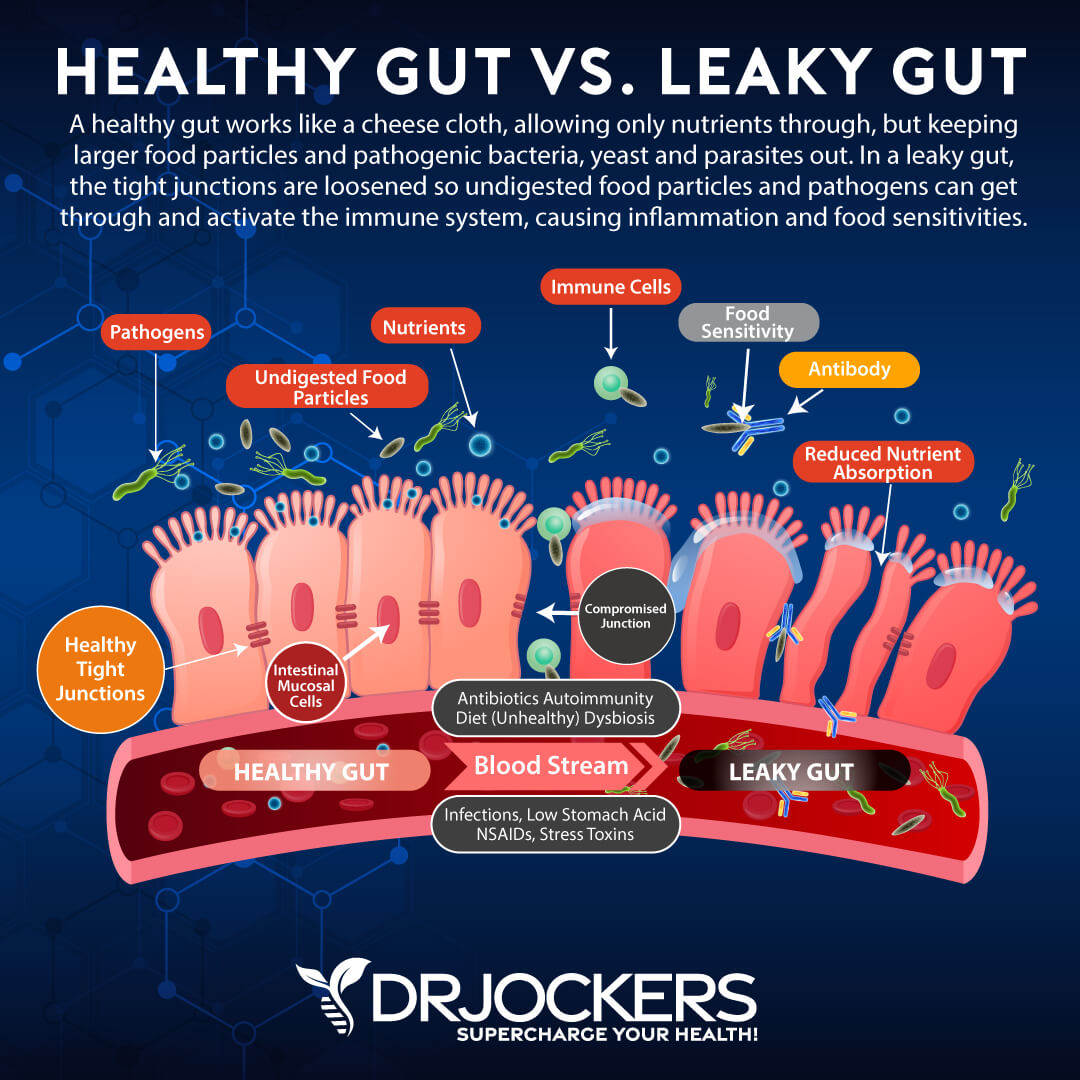
6. Heal Leaky Gut:
Leaky gut occurs when the enterocytes, or cells of the intestinal wall, have widening gap junctions. Things that cause these cells to split apart include: NSAIDs, antibiotics, blood sugar imbalance, environmental toxins, pathogens, pesticides, hormone imbalance, and processed foods.
Once the cells of the intestinal lining have atrophied and have started to loosen, large particles are able to get through that would not normally be able to get through the intestinal lining. This can result in infections, autoimmunity, low stomach, and impaired nutrient absorption. As we have discussed above, these resulting effects can result in diseases such as anemia.
7. Iron Supplementation:
The body does have a physiological response that helps the body increase the absorption of iron in response to feedback telling the body that iron stores are depleted.
However, this response is minimal and, depending on the severity of iron depletion, can take a long time to restore the body to optimal levels. Significant iron loss requires replacement with iron supplements (6).
We carry Iron Power, which is designed to be gentle on the gastrointestinal system and decrease the side effects of constipation that most iron supplements cause.
I only use this product with individuals who have mild to severe iron-deficiency as seen on lab work. The findings would indicate very low serum ferritin (under 25), low iron serum (under 80), and possibly low hemoglobin, red blood cells, and hematocrit.
For milder cases, I will use 1 cap – 1-2 times daily with food and possibly with 500 mg of vitamin C supplementation which helps improve absorption.
For moderate cases, I will use 1 cap 3 times daily with food and with 500 mg of vitamin C supplementation, which helps improve absorption.
For advanced cases, I will use 2 caps – 3 times daily with food and with 500 mg of vitamin C supplementation, which helps improve absorption.
I then retest blood iron levels at 90-day intervals to make sure we are improving the levels and exceeding the amount of iron they need.
8. B12 and Folate Supplementation:
Supplementation with B12 and Folate may be necessary until absorption of these crucial vitamins has improved. These are very important for the proper development of the blood cells.
B Strong™ is the supplement that we use to address these deficiencies. It contains the entire spectrum of B vitamins to support adrenal and neurological functions. It features activated forms of vitamins B2, B6, and B12; benfotiamine, a fat soluble, more physiologically active form of thiamine; and folate as Quatrefolic®, which is proven to have greater stability, solubility, and bioavailability over calcium salt forms of 5-MTHF.
Testing for B vitamin deficiencies can be done by using the Organic Acid Test, which will look at B2, B6, biotin, folate, and B12 levels.
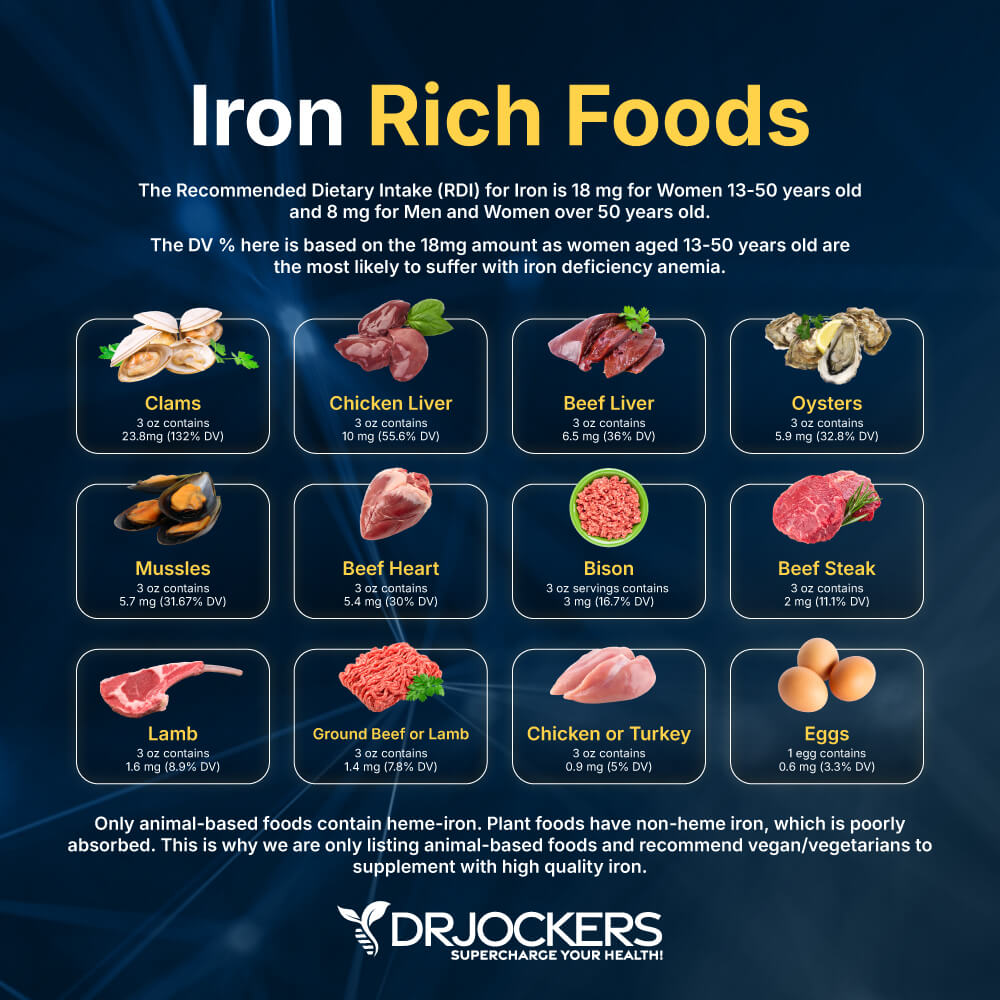
9. Best Food Sources of Iron:
The Recommended Dietary Intake (RDI) for Iron is 18 mg for Women 13-50 years old and 8 mg for Men and Women over 50 years old. The DV % here is based on the 18mg amount as women aged 13-50 years old are the most likely to suffer with iron deficiency anemia.
Only animal-based foods contain heme-iron. Plant foods have non-heme iron, which is poorly absorbed. This is why we are only listing animal-based foods and recommend vegan/vegetarians to supplement with high quality iron.
Clams: 3 oz contains 23.8mg (132% DV)
Chicken Liver: 3 oz contains 10 mg (55.6% DV)
Beef Liver: 3 oz contains 6.5 mg (36% DV)
Oysters: 3 oz contains 5.9 mg (32.8% DV)
Mussles: 3 oz contains 5.7 mg (31.67% DV)
Beef Heart: 3 oz contains 5.4 mg (30% DV)
Bison: 3 oz servings contains 3 mg (16.7% DV)
Beef Steak: 3 oz contains 2 mg (11.1% DV)
Lamb: 3 oz contains 1.6 mg (8.9% DV)
Ground Beef or Lamb: 3 oz contains 1.4 mg (7.8% DV)
Chicken or Turkey: 3 oz contains 0.9 mg (5% DV)
Eggs: 1 egg contains 0.6 mg (3.3% DV)
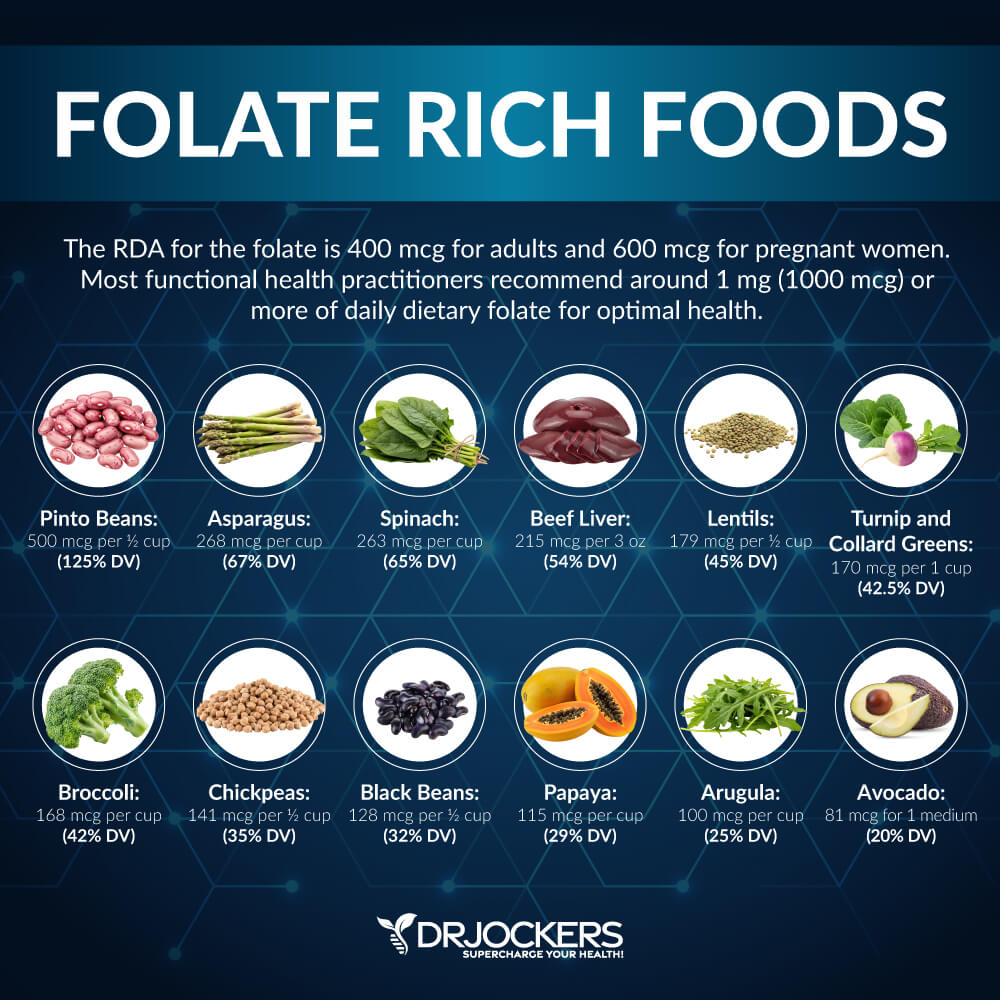
10. Best Food Sources of Folate:
1) Grass Fed Beef or Pasture Raised Chicken Liver (Best Source)
2) Egg Yolk
3) Lentils
4) Almonds
5) Avocados
6) Spinach
7) Beetroot
8) Brussel Sprouts
9) Broccoli
10) Cabbage (14).
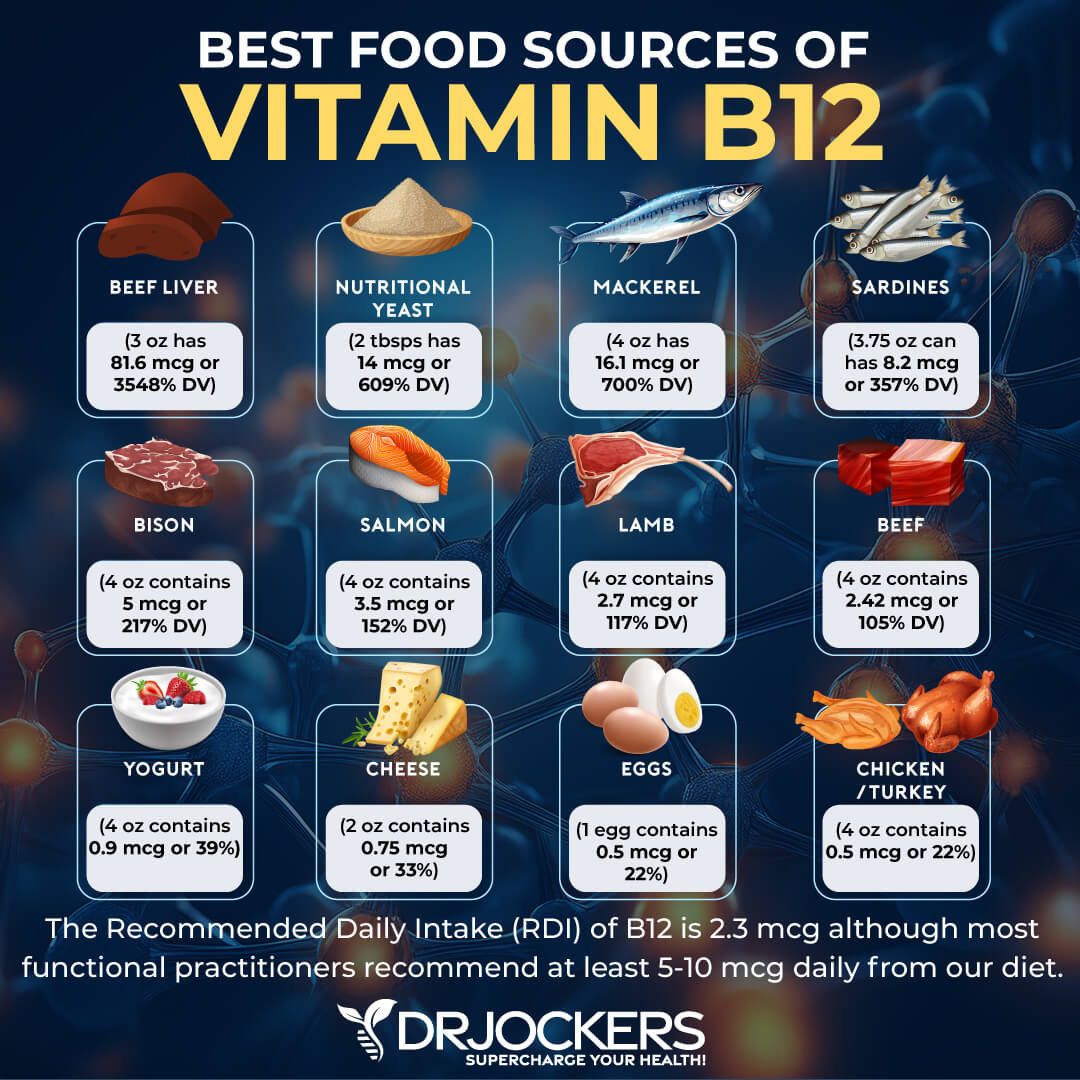
11. Best Food Sources for Vitamin B12
1) Grass Fed Beef Liver or Pasture Raised Chicken Liver (Best Source)
2) Grass Fed Beef
3) Pasture Raised Chicken
4) Pasture Raised Eggs
5) Raw Milk
6) Raw Cheese
7) Grass Fed Yogurt (14).
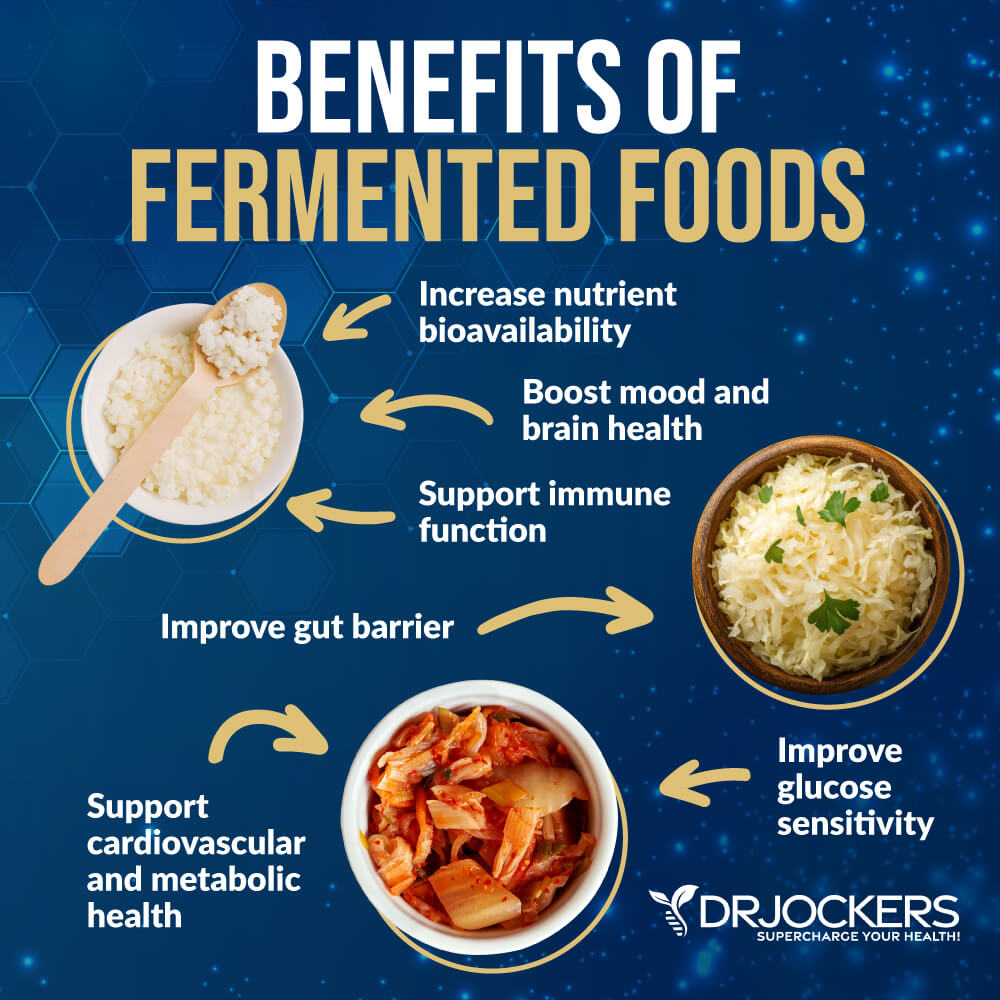
12. Eat Fermented Foods:
Fermented foods such as sauerkraut, kimchi, coconut kefir, assorted fermented vegetables, raw cheeses, and grass-fed yogurt provide natural probiotics that help fertilize the gut with healthy microbes. These microbes help heal the gut lining, absorb nutrients such as iron, B12, and folate, reduce inflammation, and strengthen your immune system.
I personally like to enjoy some fermented foods with nearly every meal. The active enzymes and probiotics help to improve digestion and nutrient assimilation.
13. Eat Liver
Liver is a great source of protein, iron, all of the B vitamins (including B12 and folate), balanced quantities of vitamin A, many trace elements and minerals, including copper, zinc, chromium, phosphorus, and selenium, essential fatty acids EPA, DHA, and AA, as well as the powerful antioxidant CoQ10.
All of these compounds help to support the production of healthy red blood cells, fight disease, decrease inflammation, and improve health. You can also supplement with grass-fed beef organ supplements to get these nutrients.
I recommend Women’s Vitality as one of the best female-specific blends of 12 organs and glands, including adrenal and thyroid, to support healthy bones, hormones, energy, and more. This blend combines organs, glands, and superfoods designed specifically to support women’s liver, thyroid, and adrenal health.

Finally, I recommend Male Performance. This blend combines organs, glands, and superfoods designed specifically for men’s performance and vitality.
That means bovine and ovine liver, heart, adrenals, prostate, orchic (testicular), pituitary, and more.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!
Final Thoughts
Anemia is a serious health problem and can be caused by a number of different issues. If you have anemic symptoms, it is critical to address the root cause factors and get the proper nutrients to support healthy blood cell formation.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.







If the MCHC value is more than 36%, then the result considers as MCHC value is higher than the normal.
hi
thank you for information about anaemia, I’m suffering on it iron deficiency, when mensuration comes I suffer a lot,
I thank you
Thanks for reading Grace!
me too and i am fasting. I just broke my fast abou 15 minutes ago. 22 hour fast hoping to do a 48.
i have good eve..im from philippines i just read ur article this time…ihave a laboratory report of peripheral blood smear..can u please
explain to me wat is mean of this
[THE PERIPHERAL SMEAR SHOWS PREDOMINANLY HYPOCHRONIC AND ANISOCYTIC ERYTHROCYTES,MOSTLY MICROCYTES WITH SOME IRREGULAR FORMS NOTED.THE LEUKOCYTES APPEAR ADEQUATE IN NUMBER WITH RELATIVE LYMPHOCYTOSIS.NO BLASH CELL OR OTHER IMMATURE FORMS NOTED.PLATELETS OCCUR SINGLY,SMALL CLUMPS IM,SUFFICIENT IN NUMBER AND ARE MORPHOLOGICALLY UNREMARKABLE.]
HEMATHOLOGY RESULT
HEMOGLOBIN 119
HEMOTOCRIT 0.35
WBC COUNT 7.2
RBC COUNT 3.74
NEUTROPHILS 0.56
LYMPHOCYTES 0.38
MONOCYTES 0.03
EOSINOPHILS 0.03
THIS IS TEST IS COME FROM MY SON WHICH IS 7YRS HOPE U CAN EXPLAIN TO ME THIS…THANKS IN ADVANCE…
Hi
Please help.. I am suffering from anemia. I have changed my diet because i want to treat it naturally.
How long can it take to see results?.
Follow the strategies above and have a complete blood count done to assess iron levels every 2-3 months Lele!
Hi,
What would it mean if my TIBC and UIBC is out-of-range low and my Total Iron and Saturation % is on the high end (but in range?). My ferritin was not tested during that period, but is typically on the low side (on average 27 ng/mL).
Thanks so much!
That is an interesting pattern, if your ferritin is that low, it could be post menstruation or a low iron level. Ferritin goes down before total iron is impacted.
I have been suffering from anaemia for about 5 months now, and it becomes worse after my menstruation. Please what do I do to correct it though I was diagnosed of kidney infection during this same period
So sorry to hear that! I would be sure to follow what is discussed in this article and this is another one on how to control things during menstruation. https://drjockers.com/8-strategies-relieve-pms-symptoms/
I need to know where to buy Iron power and Be strong supplements
You can get those here: https://store.drjockers.com/products/iron-power
And here: https://store.drjockers.com/products/b-strong
I was diagnosed with a UTI, treated with antibiotics. I was then told I had two ovarian cyst, one that ruptured and one still on the left ovary. My RBC is high, hemoglobin is 11.3. lymphocytes are normal. Mean cells are low. Enlarge spleen and slightly enlarged liver. Is it possible I have an iron defiency? I feel really had two weeks before menstrual period and one week after, basically I feel good one week out the whole month.
Sorry to hear this Mary, this sounds like something more serious than an iron deficiency. I would be sure to work closely with your doctor to get the support you need.
Your wasting your time commenting here! No Drif there was one can give any advice let alone medical advice on the internet! It would be a liability. See a naturopathic physician! The article is great but your wasting your time other then being sympathetic apologizing for your discomfort!
I was diagnosed of severe anemia last two years of which i even received a blood transfusion and i am starting to feel the same symptoms again from which i was diagnosed of anemia also i have been seeing blood in my stool.could it possible is anemia once again?
Hi Arthur, I am sorry to hear this! Blood in stool can be coming from anywhere within the digestive tract. It is important to identify any other additional symptoms you are having with this bleeding. I recommend that you work with a functional health practitioner that will get to the root of the problem and customize a specific plan for you! This article can help: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
Hello. I’m Marium and Im of 25 years .yesterday I’m diagnosed as anaemic patient with iron deficiency. As my last menses were heavy that’s why. Kindly suggest me medication and diet to recover within one month.
Hey Marium, I’m sorry to hear! I would highly recommend that you work with a functional medical practitioner that will get to the root cause of your problem and customize a specific plan that works for you! This article can help: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
Thankyou so much! But my doctor only gave me 1 Iron syrup and Iron Tablets. I’m so worried about my life my health
I’M Marium. I am having Iron deficiency Anaemia. From 1 week I’m taking medicine. But from 2 days my stool color is almost full black and somehow it is showing red red… like blood is mixed in stool. Is this common or serious problem? Please tell me.
Hi Marium, I’m sorry to hear that you are experiencing this! I would recommend that you work with a health practitioner to get to the root cause of what is going on and who will customize a specific plan for you to heal. This article can help: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
Hi,
I was told that I have anemia due to chronic illness. However, I don’t know if any chronic illness I have. I do have mild cardiomyopthy
Hey Lynn, I would imagine that is what your physician is referring too.
Hi,
What does it mean to have high RBC Width distribution and Increased Retic Count?
I was just diagnosed to have severe anemia. My MCV,MCH, hemoglobin, hematocrit, rbc are also decreased.
Would you recommend blood transfusion? I am undecided if I should get blood transfusion, as my doctor advised me.
Many Thanks!
Sorry to hear this! I would highly recommend trying to find the root cause of the anemia. It is typically related to bleeding (excessive menstrual or possibly gastrointestinal) or lack of iron absorption (low stomach acid, leaky gut, celiac disease, etc). In more rare circumstances it can be related to autoimmune condition, genetic condition or cancer. Find out the root cause and fix that if possible.
My Chiropractor shared this article with me after I had contacted him what I have been experiencing, thinking possibly anemic related condition. I just finished reading the article in its entirety. I’m excited about getting to the root of my issues and being healed overall. I will print it out, reread to help guide me “where” to begin my health journey.
Hopeful & seeking guidance!
Wonderful! Let us know if you need anything else! Blessings!