 Eczema: Symptoms, Causes & Support Strategies
Eczema: Symptoms, Causes & Support Strategies
Eczema is a common skin condition that affects over 31 million people in the United States alone. Eczema causes skin inflammation, itchiness, scaly rashes, dryness, crusting and flaky skin. It can become a chronic condition that appears regularly when triggered by environmental factors or stress. It can be mildly frustrating or downright debilitating for some. The good news is that with the proper nutritional support strategies you can improve your skin health.
The word eczema is derived from the Greek word ekzein meaning “to boil out”; the Greek word ek means “out,” while the Greek word zema means “boiling.” Research indicates that eczema is caused by chronic inflammation that affects the skin cells and causes scarring.
In this article, you will learn what eczema is. You will understand its main symptoms, triggers, and causes. I will share my top natural support strategies for eczema and skin health.
What Is Eczema
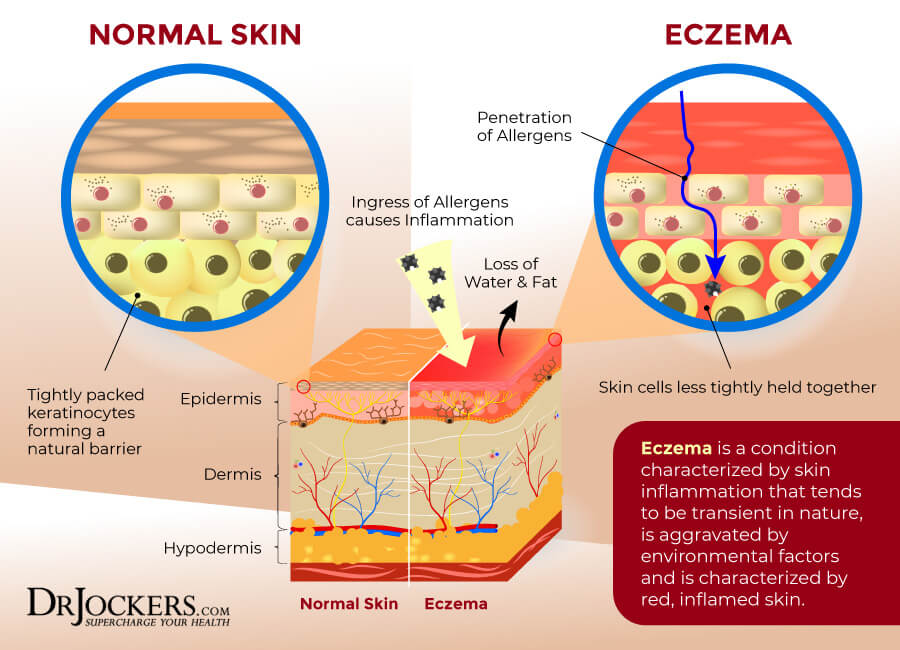
Eczema (pronounced: eg-zuh-MUH) is a group of skin conditions that over 31 million Americans experience from time to time or regularly. It is characterized by itchy and inflamed skin, often with a rash-like appearance. Eczema can develop during childhood, adolescence, or adulthood. It may happen only occasionally, but it may be recurrent or chronic. Symptoms can range from mild to severe (1).
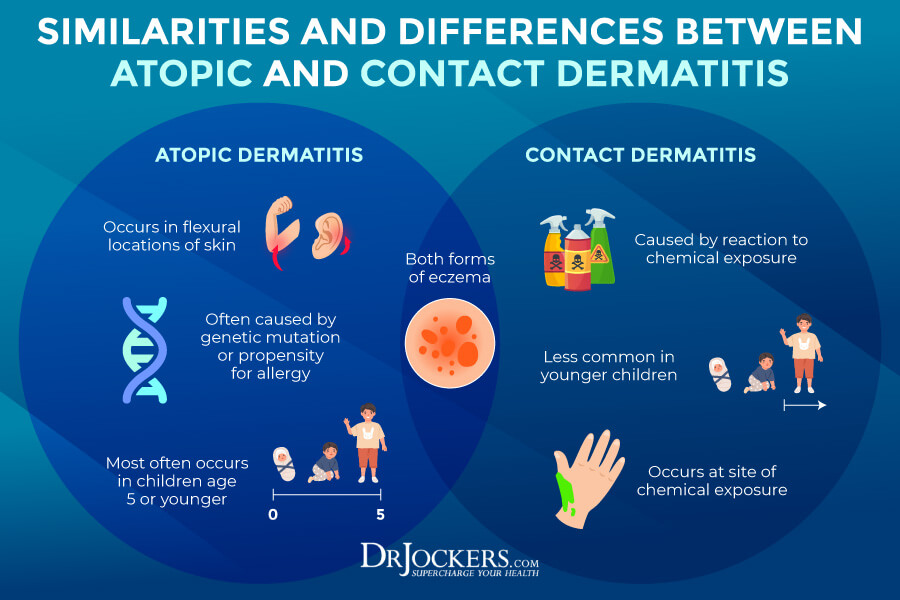
There are seven different types of eczema, including contact dermatitis, atopic dermatitis, seborrheic dermatitis, stasis dermatitis, dyshidrotic dermatitis, and nummular eczema. It is not contagious, so you can’t catch it from someone else through touch or any other contact. The exact causes of eczema are not known and may depend on person to person.
It is believed that the causes of eczema are the combination of genetics and environmental triggers, including allergens, irritants, or toxins outside or inside the body that turn on your immune system causing inflammation and symptoms (1).
Symptoms of Eczema
Symptoms of eczema include (1):
- Itching
- Dry skin
- Sensitive skin
- Red or discolored skin
- Skin inflammation
- Rough, scaly, or leathery skin
- Itchy skin
- Swelling
- Oozing
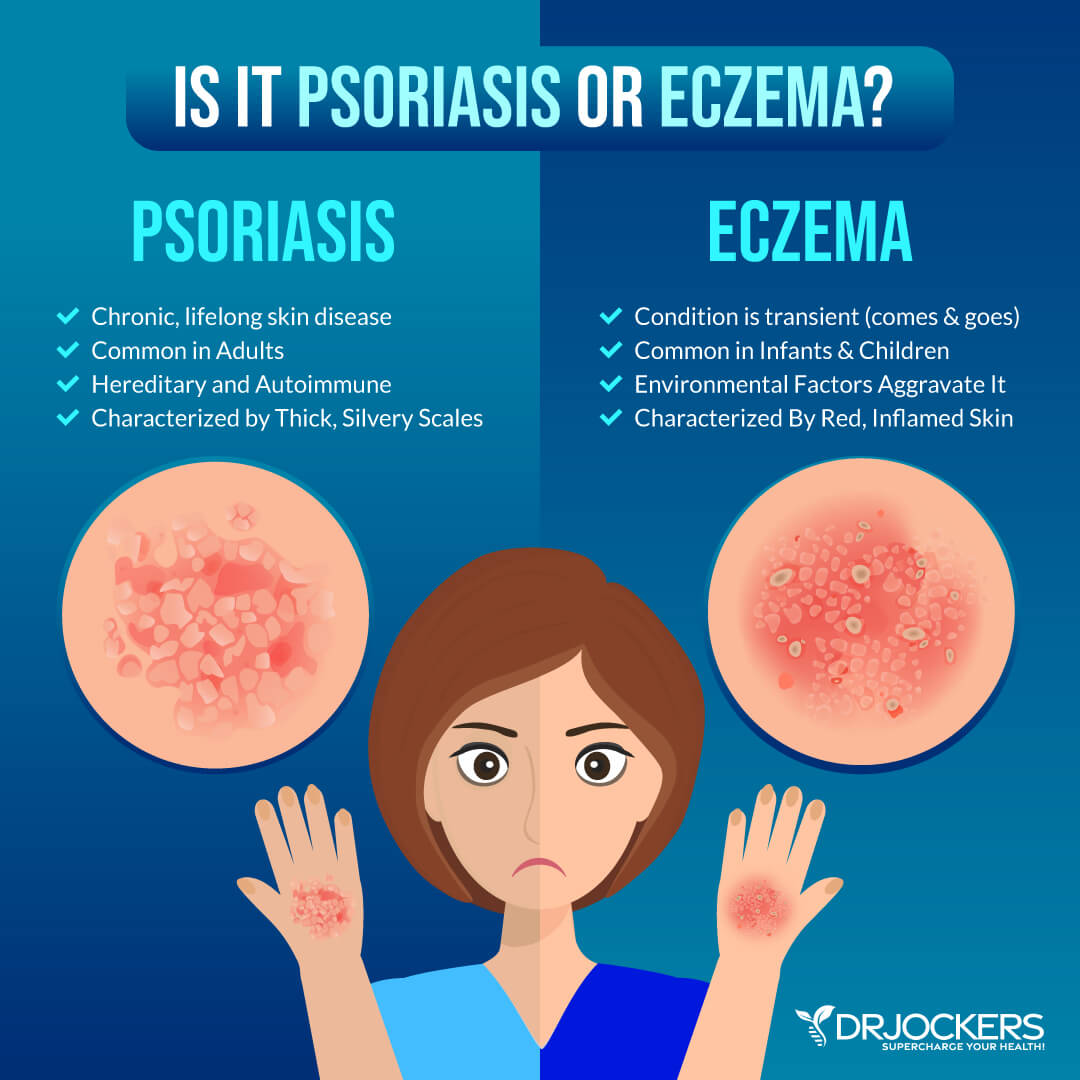
- Crusting
You may experience all or only some of these symptoms of eczema. Since symptoms of eczema may resemble symptoms of other skin issues including psoriasis, an autoimmune disease affecting the skin, it’s important that you visit your healthcare practitioner for proper diagnosis or treatment.
Factors That Trigger Eczema
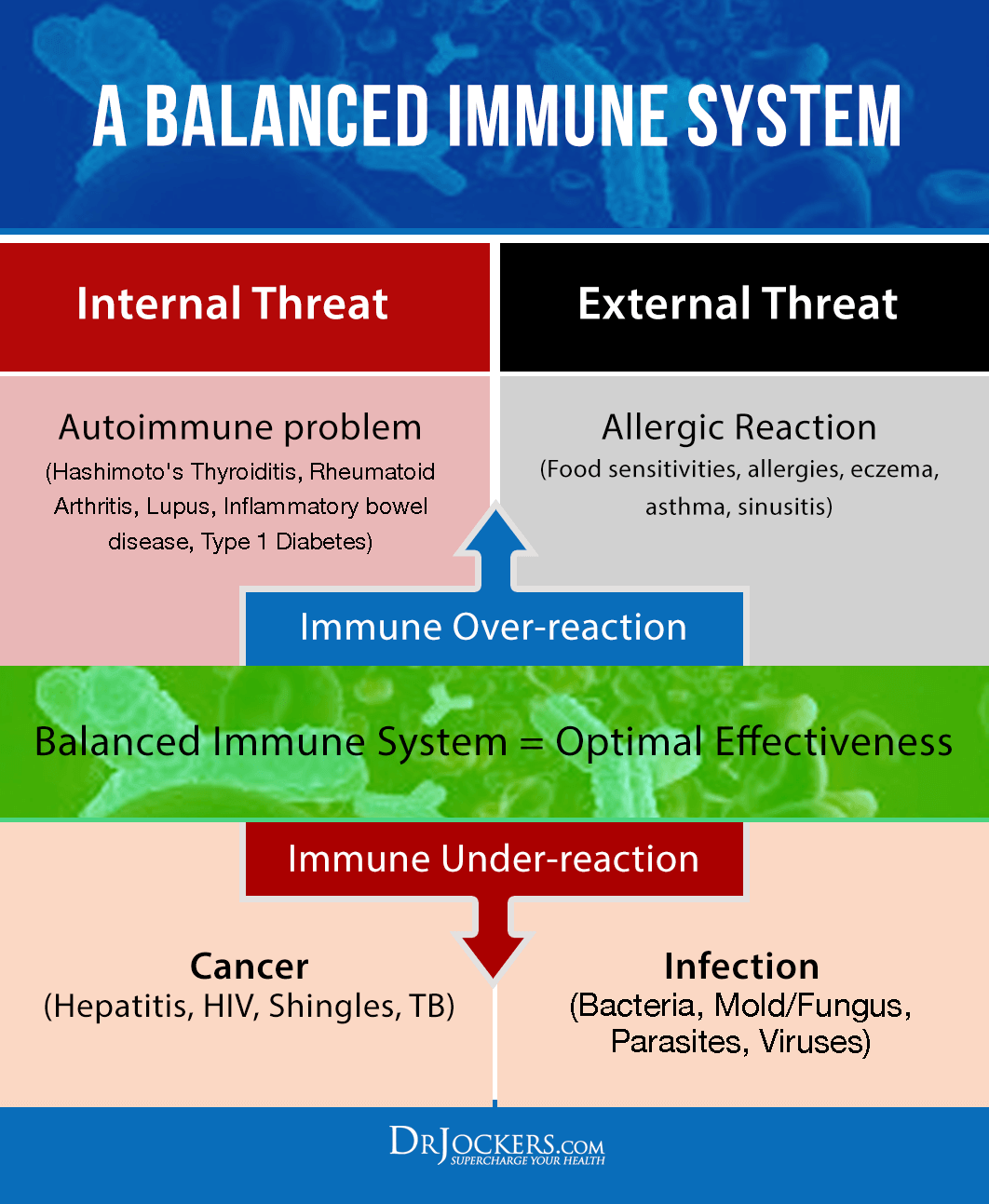
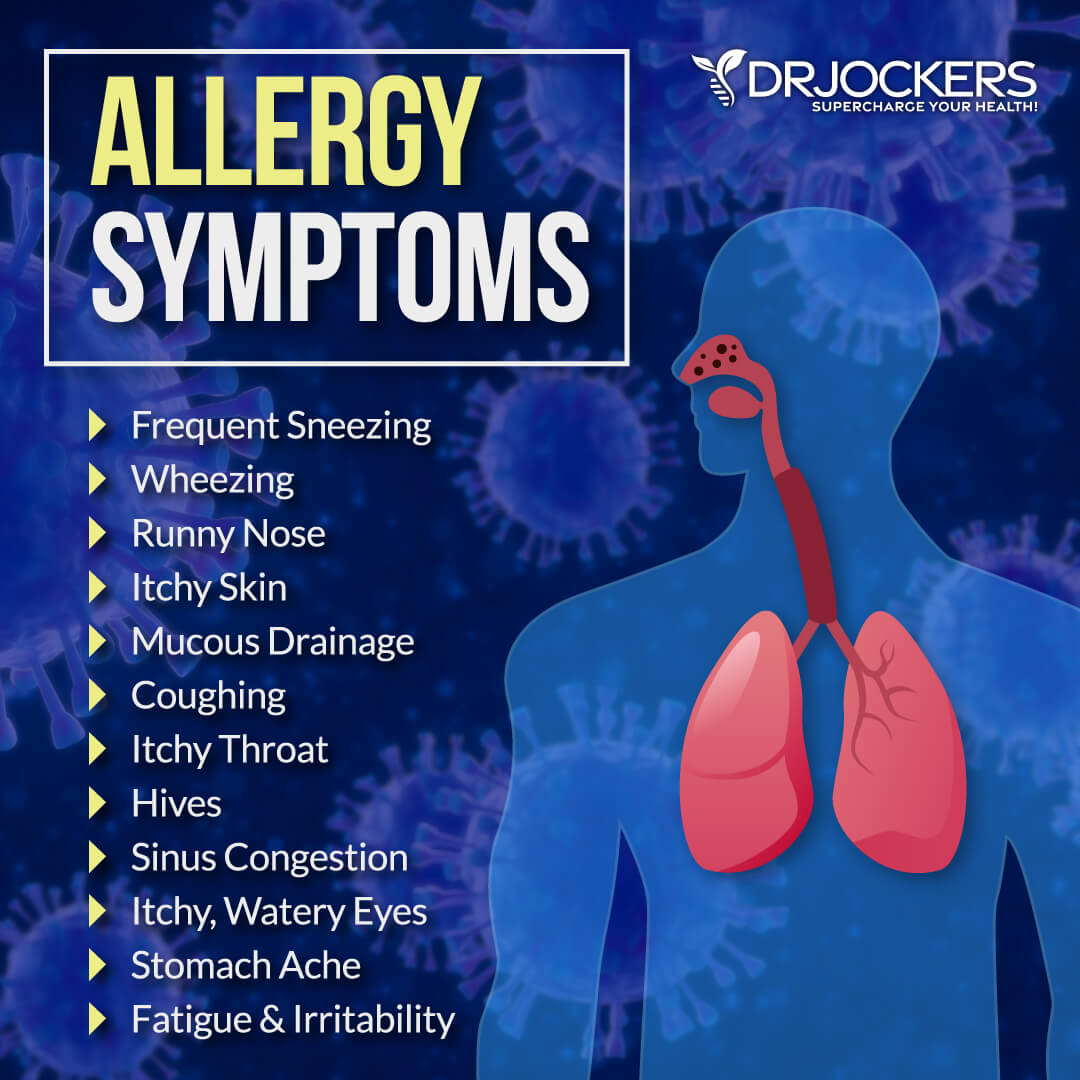
Eczema is characterized by chronic inflammation and a hyper-responsive immune system. Many people with eczema also deal with other hyperinflammatory disorders, including allergies, hay fever, or asthma.
Eczema is not something that most people live with 24/7. You go through periods of remission until something triggers an inflammatory skin response leading to symptoms. Some of the major triggers for eczematic reactions and symptoms include:
Factors That Trigger Eczema:
Chronic inflammatory disorders such as eczema are characterized by a hyper responsive immune system. Individuals with eczema often also suffer from other hyperinflammatory disorders such as asthma, allergies, and hay fever. Here are some of the major triggers of eczematic reactions:
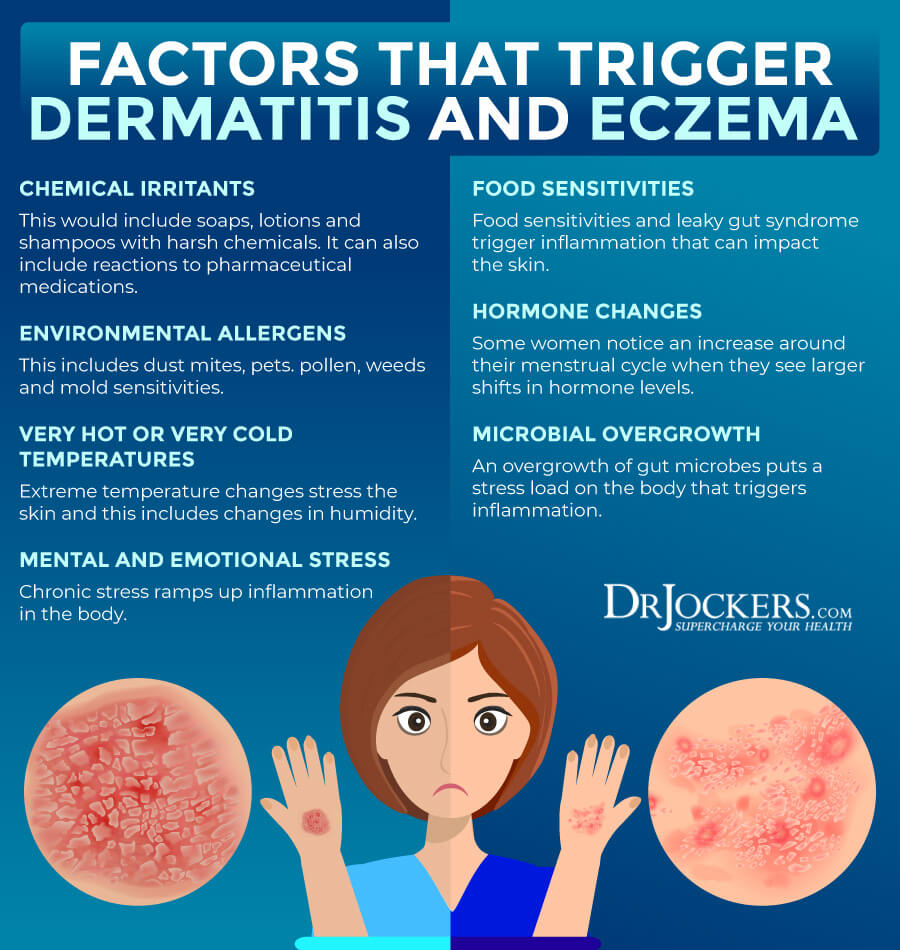
Chemical Irritants
Chemical irritants can often lead to inflammation and eczematic reactions. Some chemical irritants you may react to may come from conventional soaps, lotions, shampoo, cosmetics, laundry detergents, dish soap, disinfectants with chlorine or bleach, and hand sanitizers. You may also react to certain jewelry, clothing materials, medications, excessive hand washing, and electric blankets.
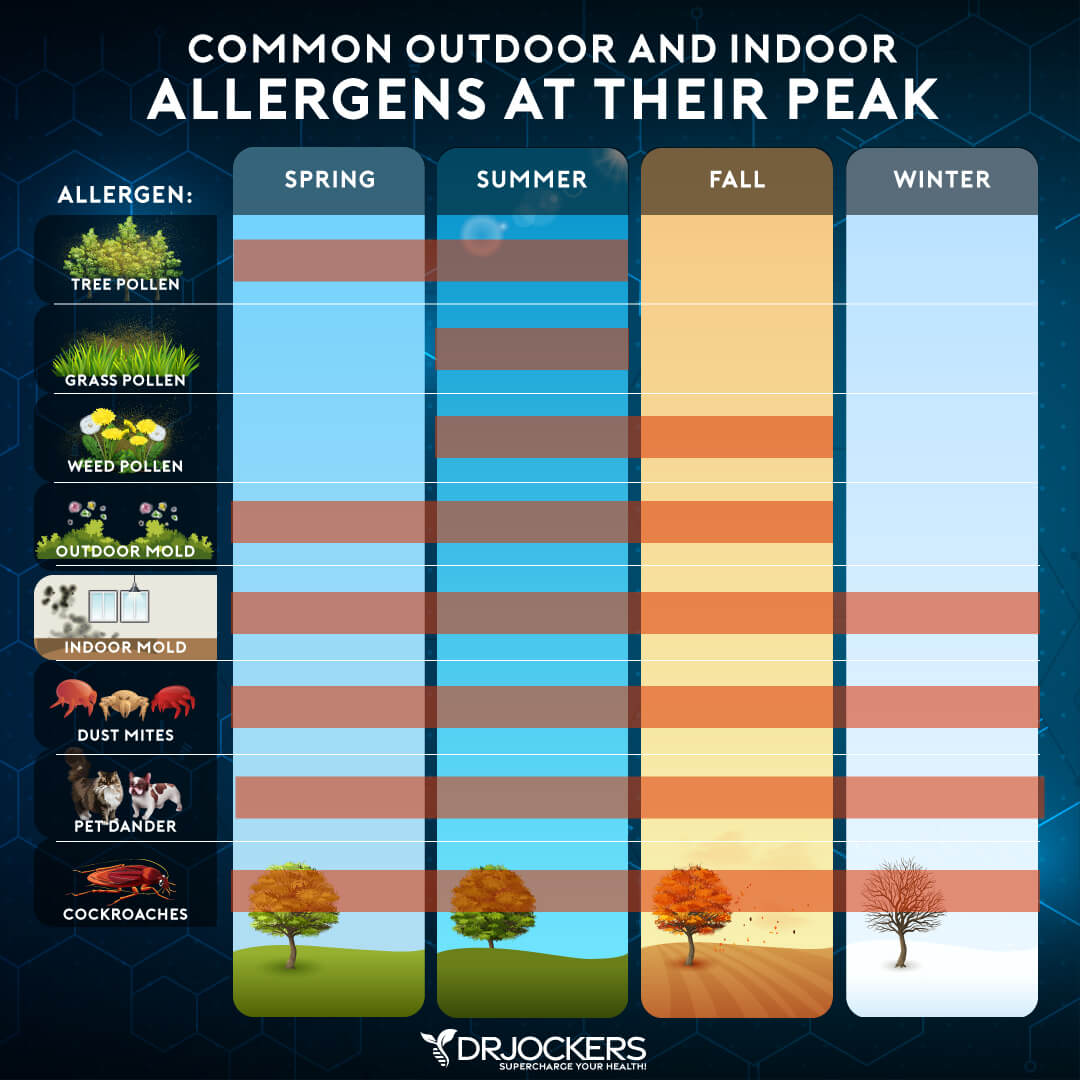
Environmental Allergens
Environmental allergens are a common culprit that can lead to a strong immune response with physical reactions, including eczema. Environmental allergens that may cause eczema include mold, seasonal pollen, pets (cats > dogs), house dust mites, and dandruff.
Very Hot or Very Cold Temperature
Extreme temperatures and major weather changes can be a shock to your body and can cause a hyperimmune response and eczematic reactions. Hot weather over 80 F, cold weather below 30 F, very high or low humidity, sweating from exercise can all trigger eczema.
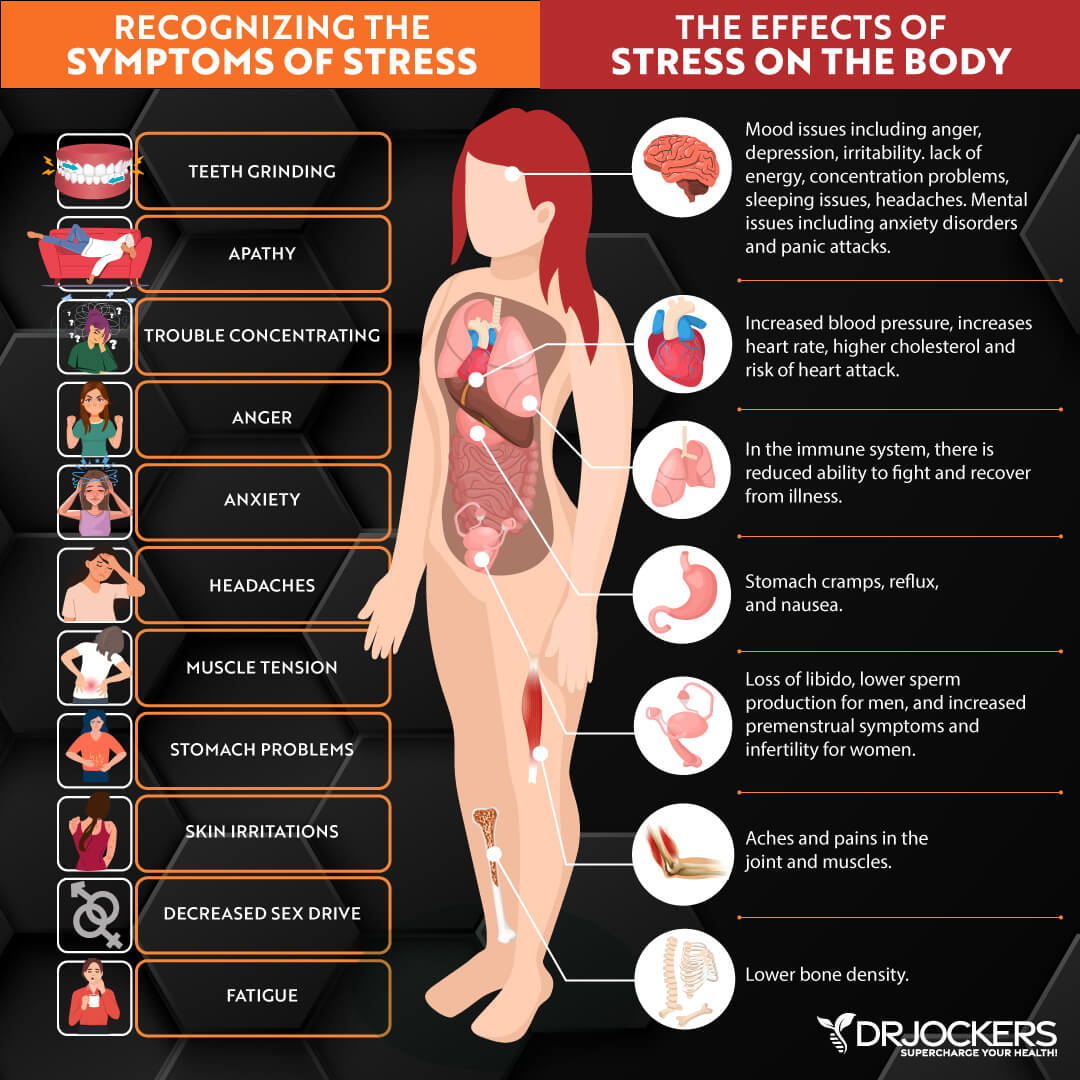
Mental and Emotional Stress
Mental and emotional stress can also lead to an immune response, inflammation, and eczema. You may notice that your eczema appears or becomes the worst at the most stressful times.
Food Sensitivities
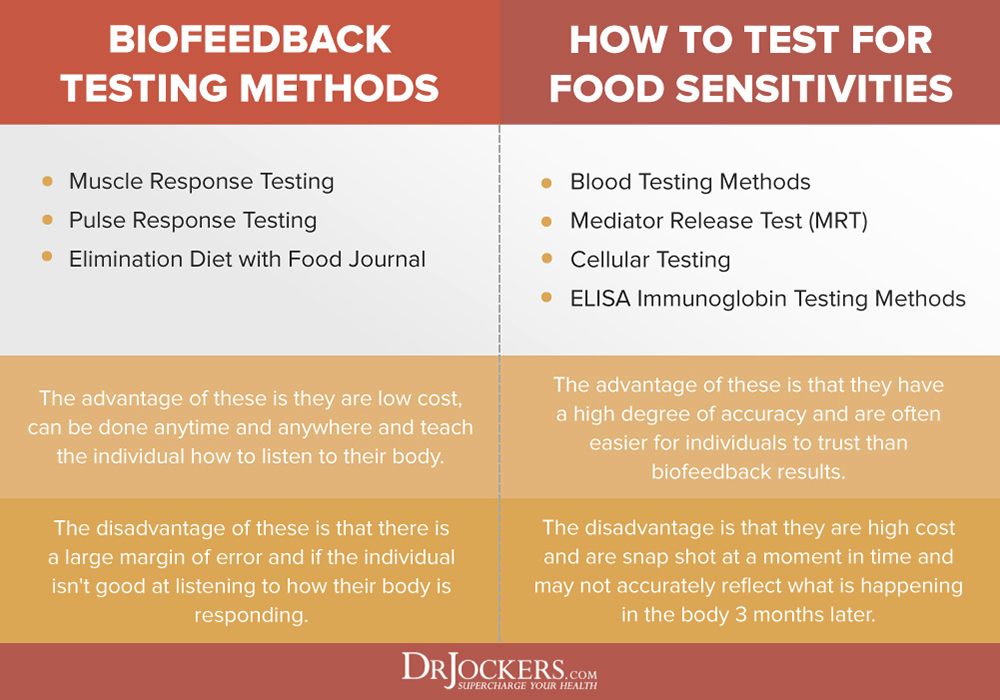
Certain foods can trigger an immune reaction and eczema. The most common food sensitivities include gluten, dairy, corn, eggs, soy, nuts, chocolate, and sugar, however, you may also have some less common, personal sensitivities.
Hormonal Levels
Hormonal changes and hormonal imbalance can also trigger inflammation and flare-ups. Some women notice eczema before or during their menstrual cycle.
Microbial Overgrowth
Bacteria like E Coli and Staph, Candida and yeasts, and certain viruses can aggravate eczema if they overpopulate, disrupt your gut flora, and increase inflammation.
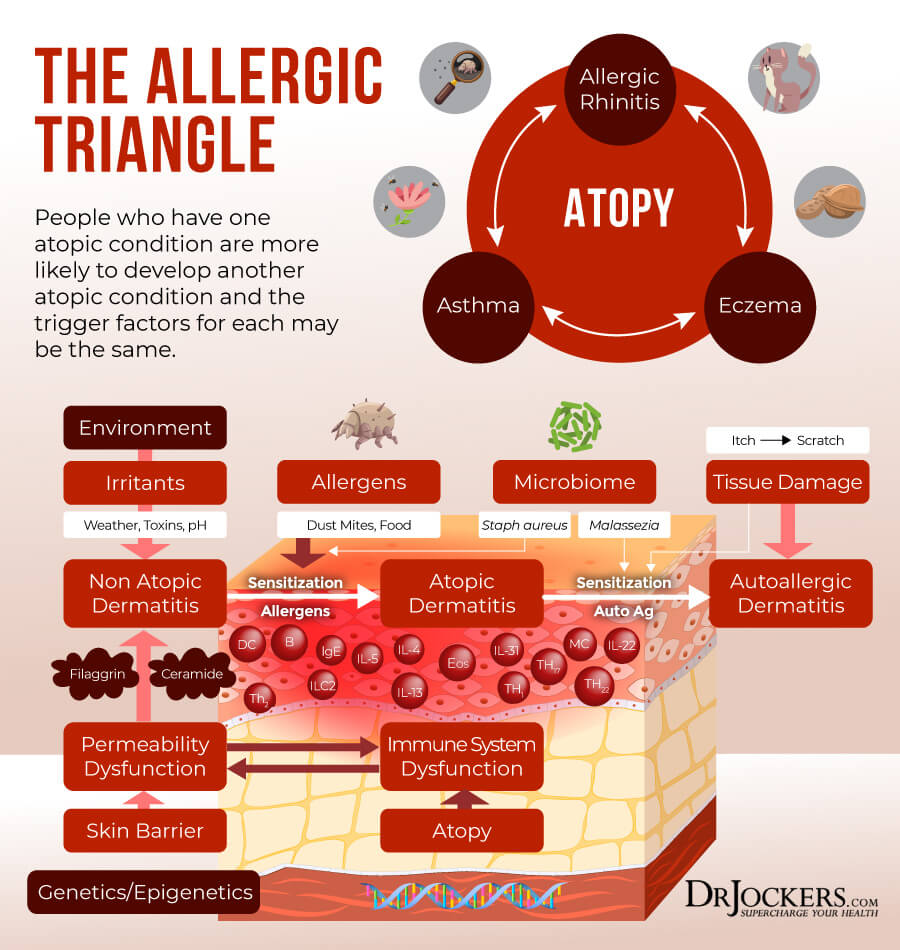
The Allergy Triangle
If you have eczema, it is important that you understand the Allergy Triangle, which is a triangle of allergy-related conditions that many people with allergies are dealing with. The Allergy Triangle included food or environmentally related allergies, asthma, and eczema. If you have one of these conditions, you are at higher risk of also developing the other two. Many people struggle with all three at least from time to time, though they can also occur in isolation.
A 2015 study published in the Annals of Nutrition and Metabolism has found that 50 percent of those with atopic dermatitis also develop asthma within the first year and 85 percent of patients have their first experience before they turn 5 years old (2). This is a very high rate considering that only about 9 percent of children and 7 percent of adults have asthma.
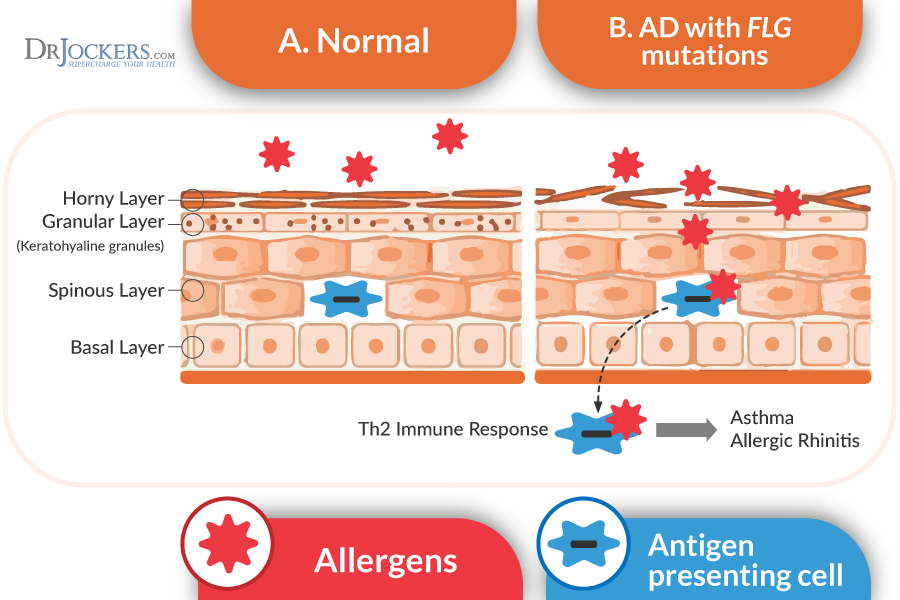
A 2012 study published in Allergology International and another 2012 study published in the International Archives of Allergies and Immunology have also found some interesting connections (3, 4). Scientists discovered a compound called thymic stromal lymphopoietin (TSLP) as a possible link between eczema and asthma. When your skin is damaged, it secretes TSLP to alarm your body that there is skin damage.
Since your skin is first in line to protect you from microscopic invaders that could lead to life-threatening infections, this is an important mechanism. TSLP, however, is not an ordinary compound, but an interleukin-7 cytokine that can create a Th2 mediated immune response throughout your body. TSLP can also travel across your body via your bloodstream. As a result, it can make it to your lungs and trigger a hypersensitive response through an asthma attack.
Conventional Treatments
If you have eczema, as the first course of treatment, your doctor will likely recommend that you avoid environmental triggers and irritants, and maintain proper bathing and moisturizing practices. Conventional treatments of eczema can also include prescription topicals for symptom relief, immunosuppressants, phototherapy, and biologic drugs depending on the severity of your symptoms.
Some conventionally-trained doctors may also be open to a more integrative approach and some alternative strategies to support conventional methods, including natural and herbal products, vitamins, acupuncture, relaxation strategies, therapy, or bodywork (5).
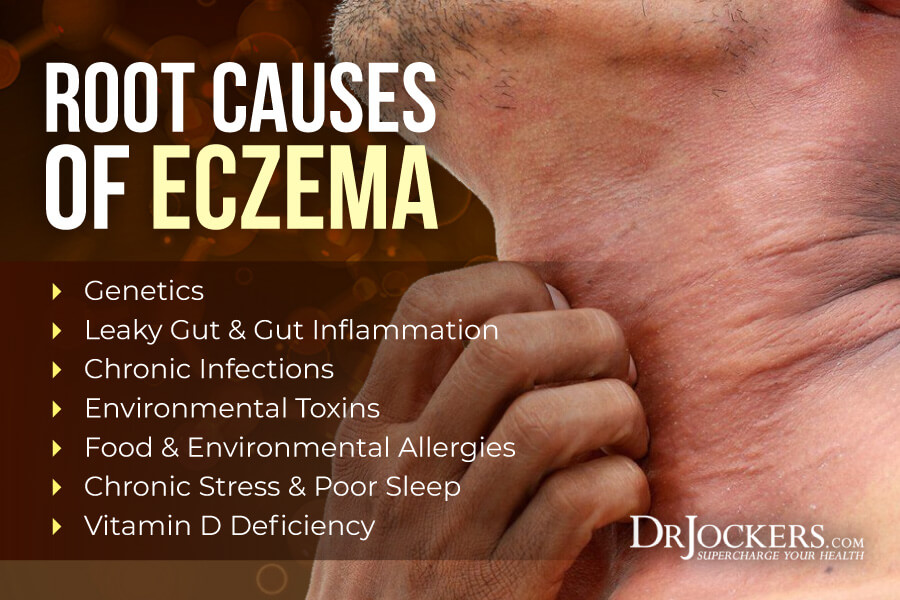
Root Causes of Eczema
Causes of eczema may depend on person to person and are often the combination of various factors. The most common root causes of eczema include:
Genetics
Genetics can play an enormous role and can increase your developing eczema when your body is stressed. A 2011 study published in Allergology International has found that the FLG gene, which encodes the spiderman barrier protein filaggrin, is one of the variants that may be linked to eczema and atopic dermatitis (AD) (6).
Filaggrin plays a role in skin barrier integrity. It is a vital epidermal protein necessary to develop corneocytes and for the generation of intracellular metabolites for skin pH and hydration. According to a 2013 study published in the British Journal of Dermatology, the SPINK5/LEKT1 skin-related genes may also play a role in eczema (7). However, while genetics can certainly play a role and increase your risk of eczema, we cannot forget about environmental factors that can further trigger the condition and lead to eczema even in those without a genetic predisposition.
Leaky Gut & Gut Inflammation
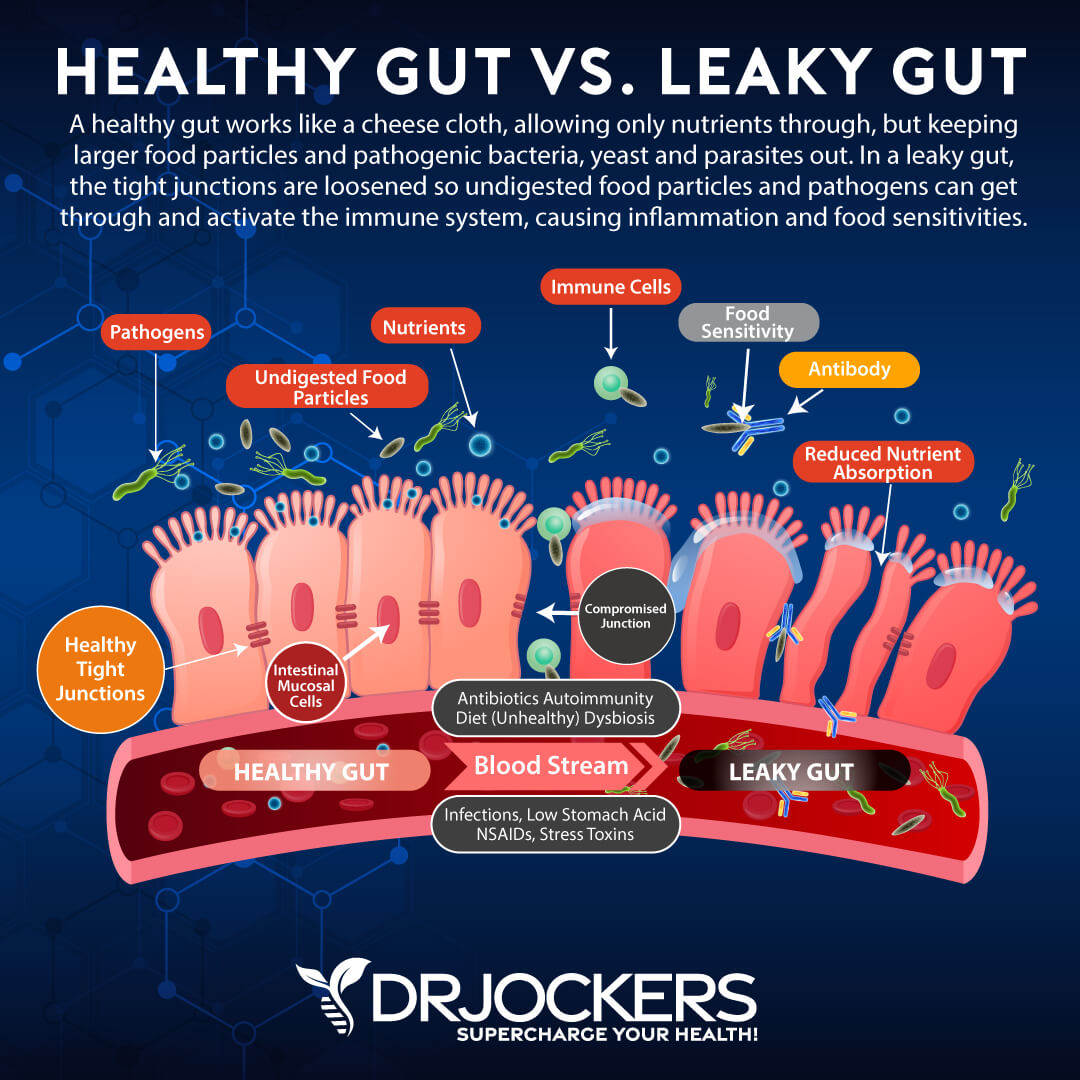
Eczema is connected to the skin barrier dysfunction, which may be connected to or triggered by leaky gut syndrome and gut inflammation. Poor diet, poor lifestyle choices, antibiotic use, environmental toxins, and stress can lead to holes in your gut lining that allow toxins, microbes, and undigested food particles to pass through into your bloodstream, creating gut inflammation, chronic inflammation, and a variety of symptoms and health issues.
The main goal of the skin is to act as a defense system to protect the body from physical, chemical, and microbial stressors. Inflammation along the gut lining, along with a genetic polymorphism, can break down the protective epidermal barrier of the skin. This process decreases the antimicrobial proteins produced in the skin and can lead to skin infections or hyperinflammatory processes (27).
The gut flora has a profound influence on the structural components of the skin, including the fatty acid profiles and sebum production. Altered fatty acid and sebum production leads to increased inflammation and possible infection of the skin cells and increases the development of acne, rosacea, and eczema.
When the skin is irritated, a neuropeptide called substance P is produced that triggers an inflammatory response. Individuals with dysbiosis or abnormal bacterial balance have increased substance P production. Substance P increases sebum production along with mast cell degranulation and a hyperinflammatory response.
According to a 2008 randomized clinical trial published in Clinical Gastroenterology and Hepatology, small intestinal overgrowth (SIBO), which is also connected to leaky gut and gut inflammation, can contribute to skin inflammation and skin issues (8). According to a 2004 review published in the Journal of Pediatric Gastroenterology and Nutrition, skin problems, such as dermatitis and eczema, are common in those with Celiac disease, Crohn’s disease, and ulcerative colitis (9).
Chronic Infections
Chronic infections, such as Lyme disease and the Epstein-Barr Virus (EBV), are also characterized by chronic inflammation and can trigger eczema. According to a 1984 study published in the International Archives of Allergy and Applied Immunology, high serum levels of EBV antibodies are common in those with atopic dermatitis (10).
A more recent, 2018 study published in the Anais Brasileiros de Dermatologia has also found that EBV, a virus that may affect 90 percent of the population, can affect the skin (11).
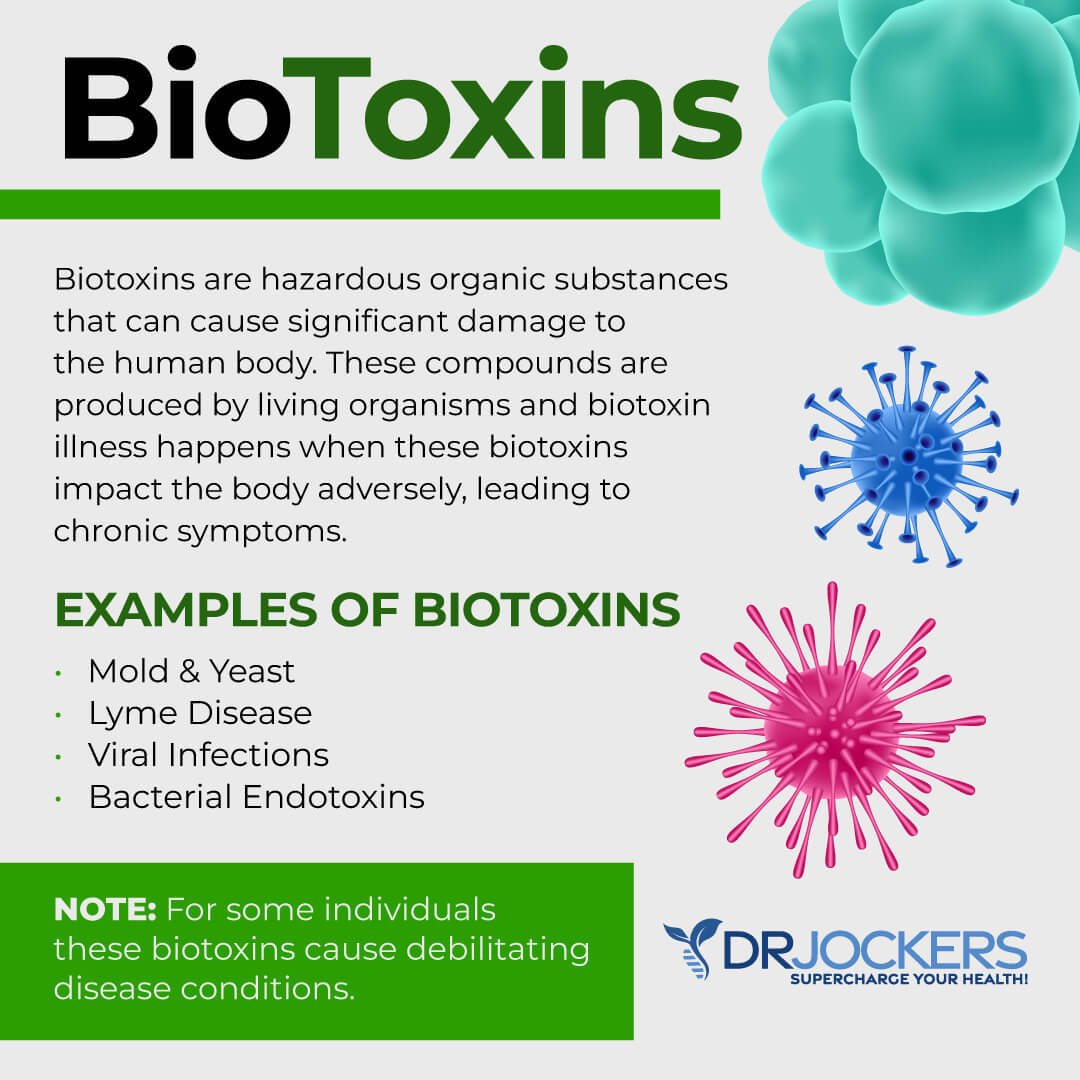
Environmental Toxins
As we discussed earlier, environmental toxins are one of the top triggers of eczema flare-ups. They are also one of the top underlying root causes leading to the disease in the first place. Mold is one of the top environmental toxins that can hide in your home, especially in the bathroom, kitchen, damp basement, or other moist areas (12).
According to a 2015 study published in Clinical Immunology, mold exposure has been associated with atopic dermatitis (AD). It can be especially problematic in children with AG+GG genotype of GSTP1 because mold can trigger Th2 inflammation and increase symptoms of atopic dermatitis.
Food & Environmental Allergies
Food and environmental allergies can also trigger eczema. As you’ve learned, the Allergy Triangle is a common problem, and many people experience both allergies and eczema.
According to a 2016 review published in the Journal of Allergy and Clinical Immunology, the weakened skin barrier of eczema and food allergies may be interlinked (13). Up to 81 percent of participants with eczema had a food allergy and up to 66 percent had food sensitivities, much higher than those without eczema. Results suggest a strong connection between allergies and eczema.
Chronic Stress & Poor Sleep
Chronic stress and poor sleep can lead to chronic inflammation, immune compromise, and gut imbalance, which can all increase your risk of eczema. According to a 2012 study published in the Acta Derma Venerologica, psychological stress can increase inflammation and immune response and can contribute to atopic dermatitis (14).
The study suggests that treatment should take psychological and stress components into consideration.
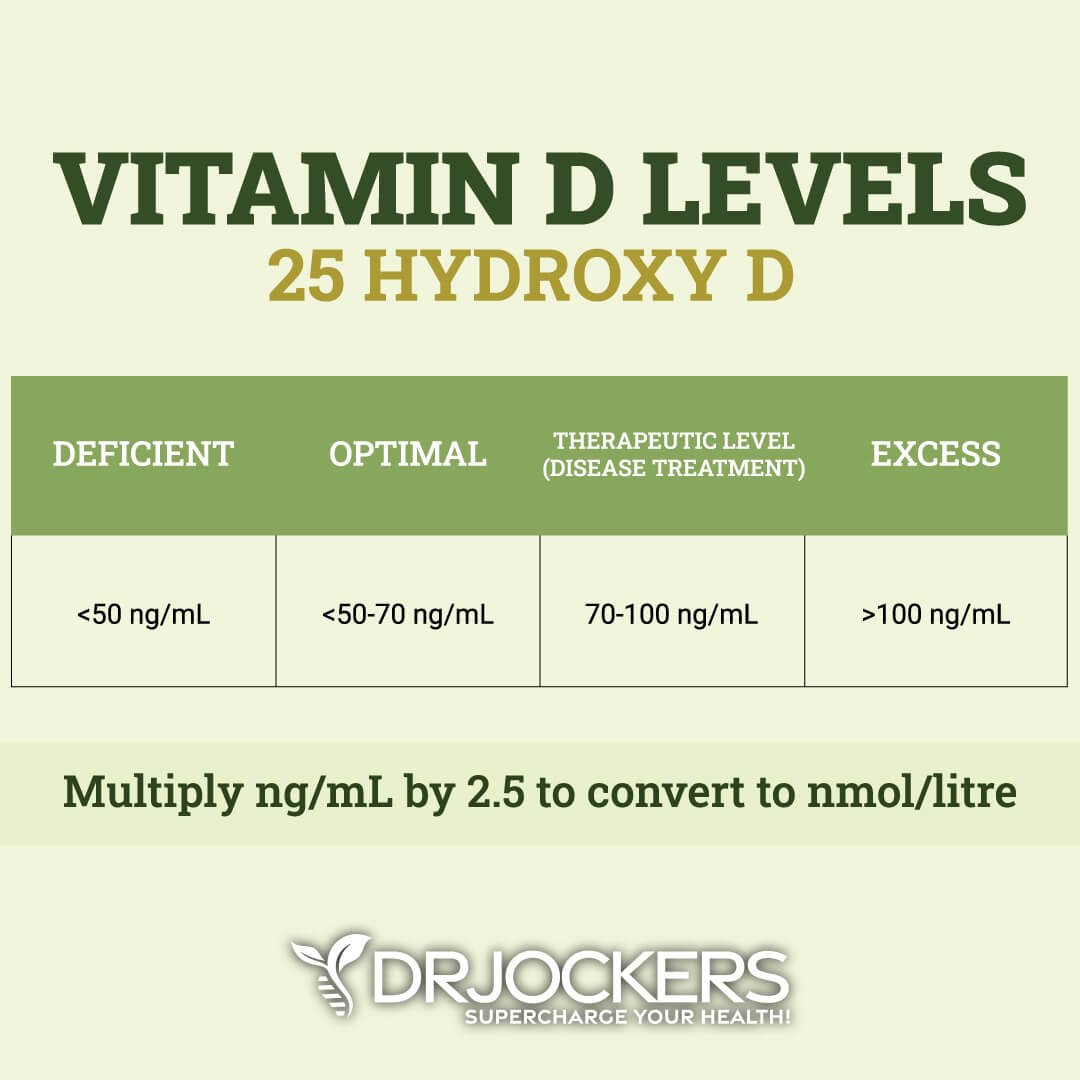
Vitamin D Deficiency
Vitamin D is a very important vitamin that plays a role in your skin, bone, muscle, immune, and brain health. Vitamin D has been shown to reduce inflammation and lower the risk of developing eczema, acne, seborrheic dermatitis and psoriasis. A 2011 study looked at children with mild, moderate, and severe eczema and found a direct relationship between the vitamin D status and severity of eczema. The children with the most severe eczema had the lowest levels of 25 (OH) vitamin D3 (15).
Vitamin D has been shown to be active in the nuclei of the epidermis tissue where it enhances keratinocyte differentiation. It is able to modulate skin cell growth in such a way as to favor keratinocyte proliferation in normal tissue and inhibit the proliferation in psoriatic tissue (which is marked by excessive proliferation (16).
Vitamin D also reduces inflammatory cytokine production in the dermal and epidermal tissue and strengthens the permeability barrier of the epidermis. This reduces the occurrence of infection in the skin and makes it resist stress more effectively (17, 18).
A 2016 systematic review and meta-analysis published in Nutrients has found that supplementation with vitamin D may be beneficial for atopic dermatitis (19). According to a 2019 systematic review and meta-analysis in both adults and children published in Nutrients, vitamin D supplementation may reduce the symptoms of atopic dermatitis (20).

Natural Support Strategies for Eczema
Considering common triggers and root causes of eczema and addressing dietary and lifestyle factors are important to improve your condition. Here are the top natural support strategies I recommend for eczema:
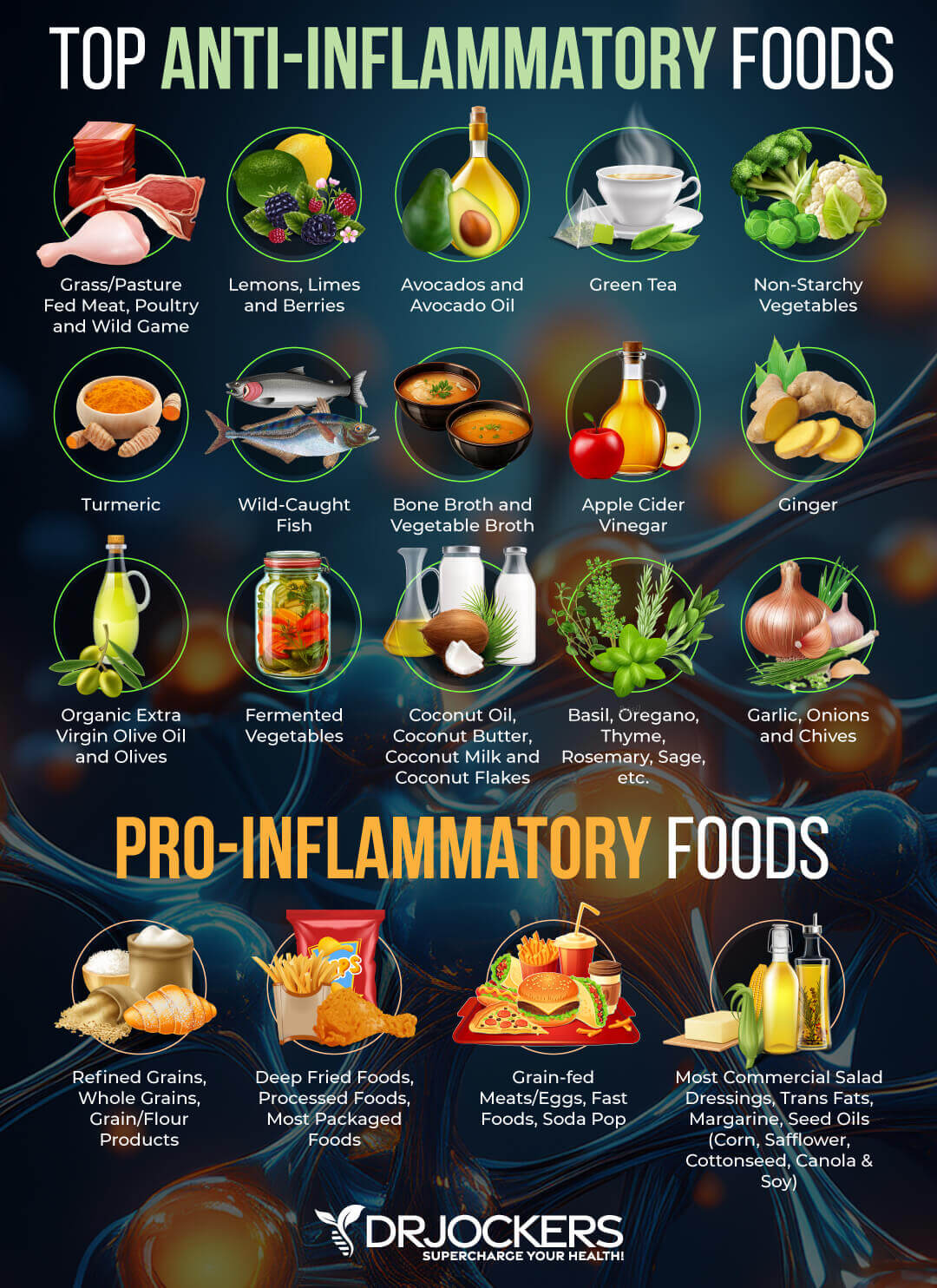
Anti-Inflammatory Nutrition Plan
Eczema is an inflammatory condition that causes inflammation in the skin. You are probably not surprised to hear that an anti-inflammatory nutrition plan is part of your recommended natural support strategies. Remove all refined sugar, refined oils, conventional meat and dairy, artificial ingredients, gluten, sodas and sugary drinks, junk food, and highly processed foods.
Follow an anti-inflammatory nutrition plan full of greens, vegetables, herbs, spices, low glycemic index fruits, healthy fats, and clean animal protein from pasture-raised beef, free-range poultry and eggs, wild-caught fish, and wild game. For more information on how to apply an autoimmune anti-inflammatory diet, read this article.
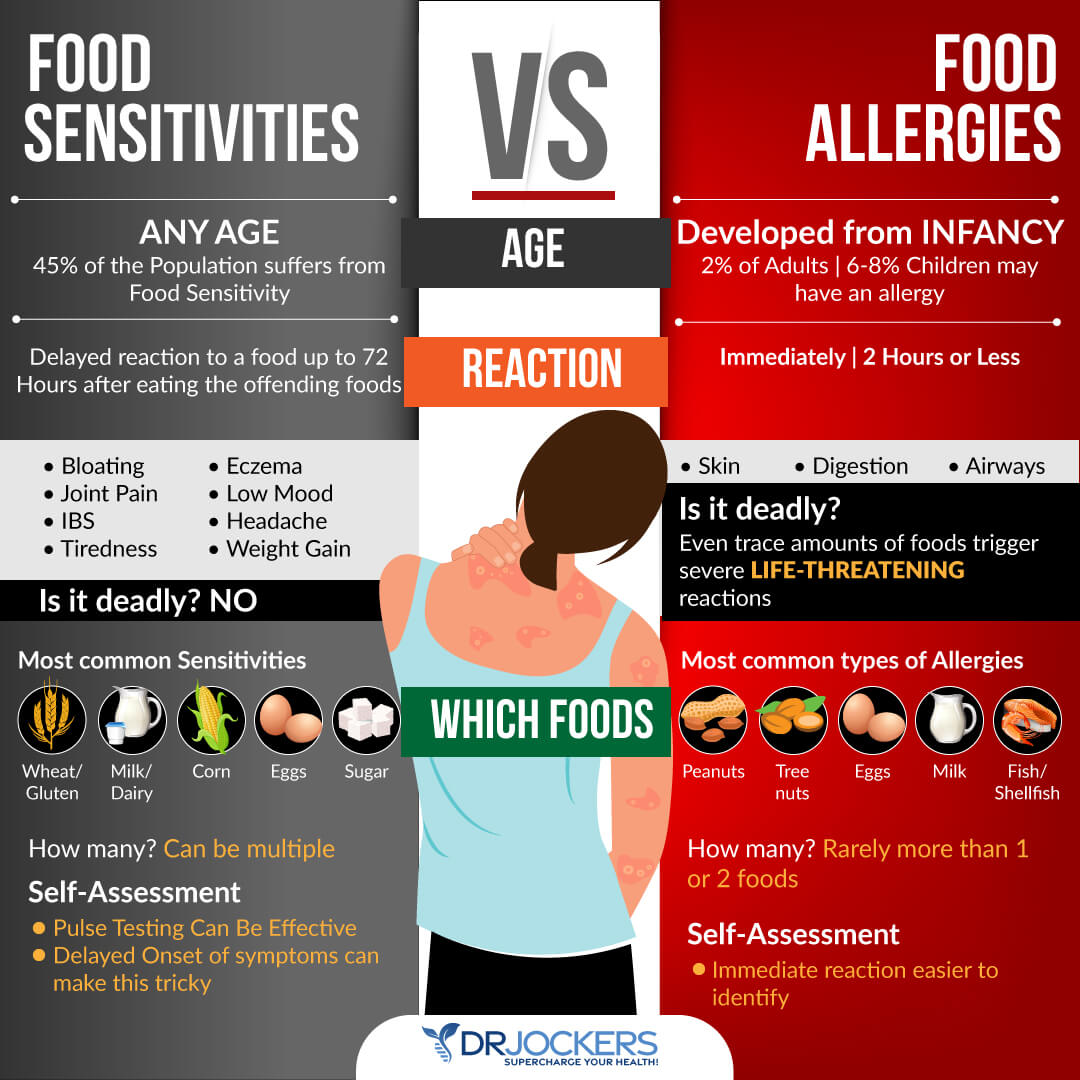
Test For Food Sensitivities
Since food sensitivities can cause chronic inflammation, skin issues, and eczema, testing for food sensitivities is critical. While there are various blood tests available for food sensitivity testing, they are not always accurate and can’t test for all foods. I recommend biofeedback testing strategies, such as muscle testing and pulse testing as well.
However, the most accurate method to discover your personal food sensitivities is an elimination diet. If you find out that you are sensitive to food, remove it from your diet. Regardless of your results, everyone can benefit from removing refined sugar, gluten, conventional (or all) dairy, soy, and corn from their diet.
Since food sensitivities change, I recommend that you test regularly, once a year or when new symptoms pop up. I recommend reading this article to learn about both biofeedback testing and clinical lab testing options for food sensitivities.
Consider a Low Histamine Diet Trial
Histamines are important neurotransmitters and immune messenger molecules. They are involved in processes involving hydrochloric acid secretion for digestion, triaging water reserves to key areas of the body, and the inflammatory response.
Histamine only becomes a problem when we have metabolic disturbances that do not allow us to effectively metabolize histamine properly. A new study recently found that mast cells (which release histamine molecules) are a key culprit in causing eczema (also known as atopic dermatitis).
The researchers also revealed that a protein known as STAT5, plays an important role in the equation by triggering major mast cell increases in some. Mast cells release histamine, and when their activity is increased, can cause a major histamine reaction leading to inflammation in various tissues of the body (21).
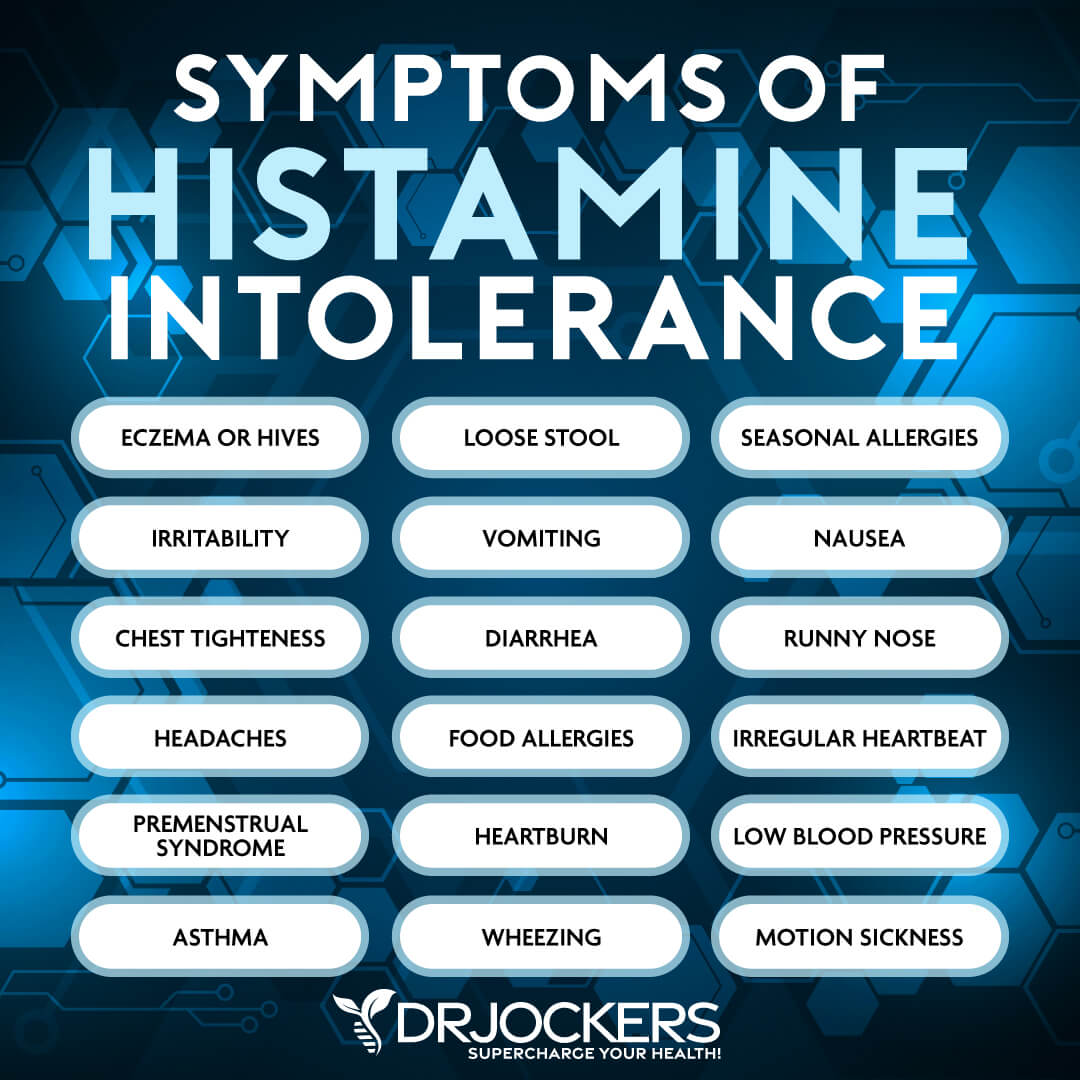
Mast cells are present in most tissues, characteristically surrounding blood vessels and nerves and are especially prominent near the boundaries between the outside world and the internal world. This includes the skin and the mucosa of the lungs, intestines, mouth, and nose.
One study found that an individual showed significant improvement in atopic dermatitis symptoms using a balanced low-histamine dietary regimen (22). I use a nutrient dense low-histamine diet for a period of time to help my clients with eczema, psoriasis, hives and other skin disorders.
This is especially important if I see that they have seasonal allergies, headaches, and other histamine related symptoms.

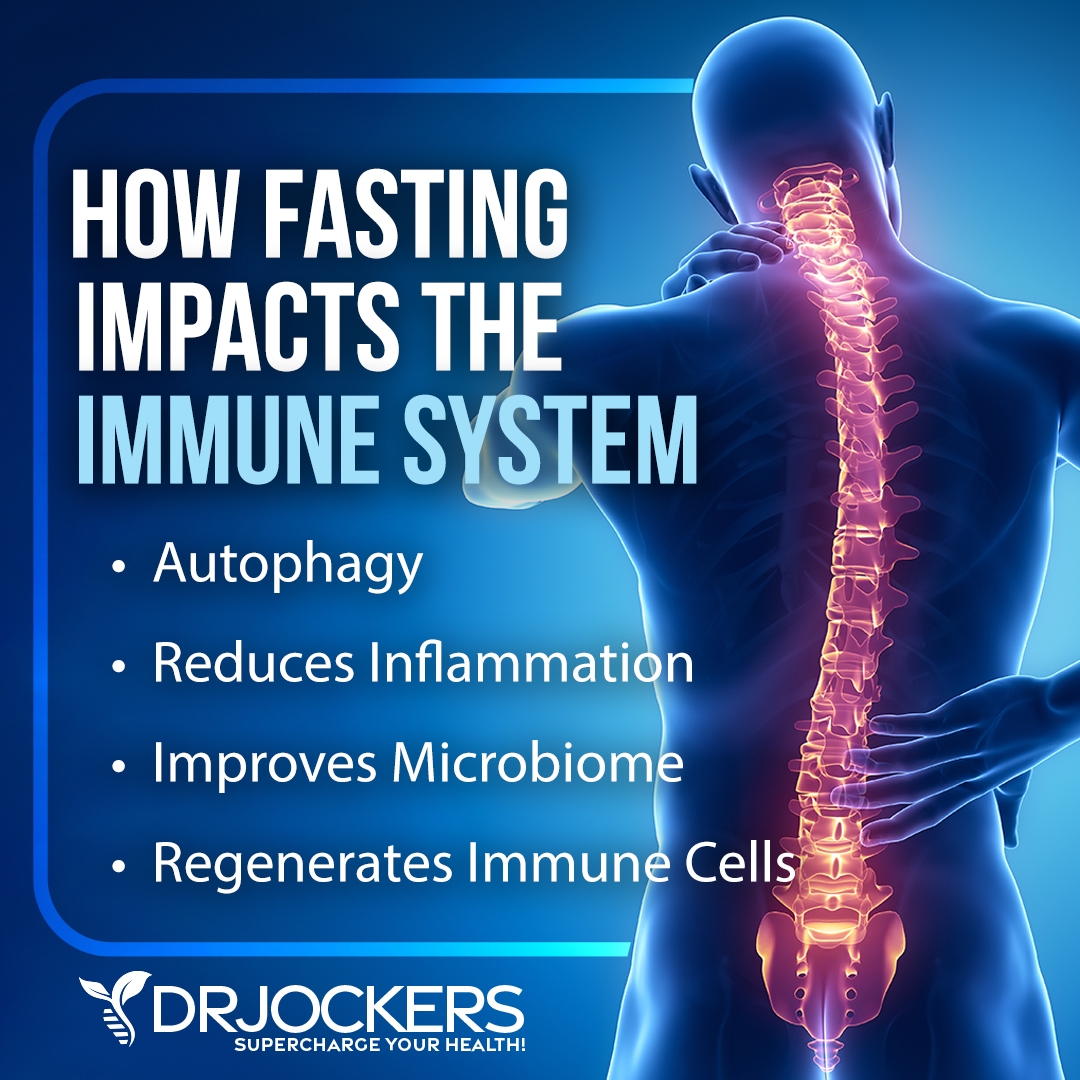
Intermittent Fasting
Intermittent fasting is a way of eating that cycles between a period of fasting and a period of eating within a day. It offers a variety of health benefits, including a reduction in inflammation and cellular renewal. According to a 2003 case study published in the Journal of Physiological Anthropology and Applied Human Science, repeated short-term fasting may improve symptoms of atopic dermatitis (23).
If you are new to intermittent fasting, I recommend that you begin with the easiest method, the simple fast. This intermittent fasting strategy involves 12 hours of fasting including your overnight sleep.
Simply stop eating after dinner and you will be ready for breakfast 12 hours later. Increase your fasting window gradually, until you find what works the best for you. Most people feel their best with a 16-hour fasting period.
Reduce Stress & Improve Sleep
Stress, poor sleep, anxiety, and other psychological factors can contribute to and trigger eczema flare-ups. To reduce stress, I recommend that you try meditation, breathwork, journaling, gratitude practice, prayer, regular movement, nature time, having a dedicated me-time, time with uplifting people and loved ones, engaging in uplifting and relaxing activities or hobbies, drinking calming herbal tea, and taking healing baths.
To improve your sleep, develop a regular sleep schedule that supports your circadian rhythms and allows 7 to 9 hours of sleep. Avoid electronics, sugar, caffeine, alcohol, and heavy foods close to bedtime. Develop a nighttime routine that works for you and make sure that your bedroom is a safe and calming sanctuary with a comfortable bed, mattress, bedding, and pillows.

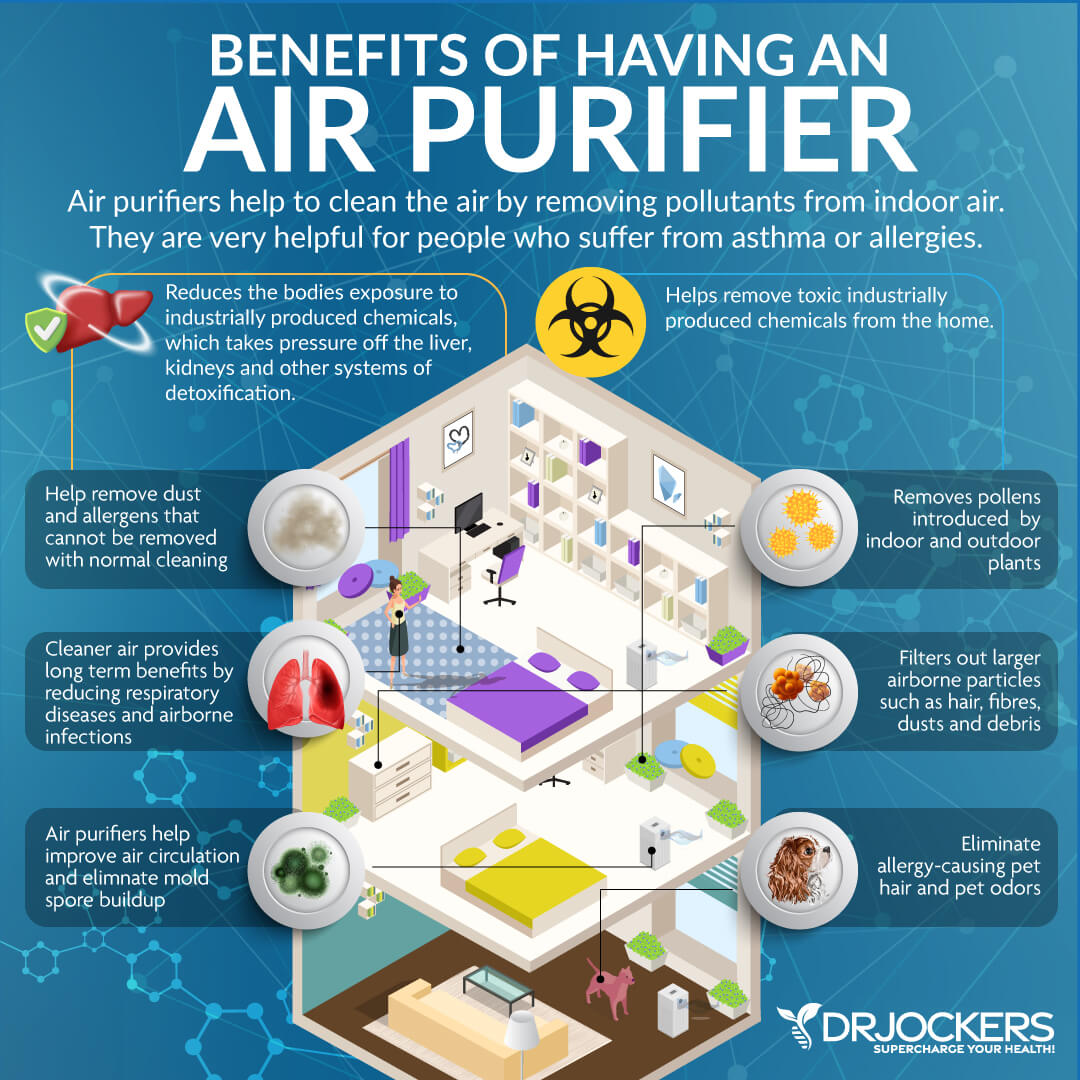
Avoid Molds and Allergens
Avoiding mold and allergies is a key strategy since they can trigger the Allergy Triangle and eczema. Make sure that there is no mold in your home. If there is, get it professionally removed or move, if possible.
Remove any materials that you may be allergic to in your home. Avoid conventional cleaning, body, and beauty products, and other chemicals that may be toxic and lead to an allergic or skin reaction. Choose organic, natural, and homemade alternatives instead. Make sure that the indoor air quality in your home is good.
Improve Air & Water Quality
Poor indoor air quality and poor water quality can also trigger allergic reactions, inflammation, and eczema. Vacuum and clean regularly to avoid dust and dust mites. Invest in a good air filtration system that helps to remove mold, allergens, bacteria, viruses, and toxins from your indoor air.
If it’s possible, make sure that your workplace also has a good air filtration system. Get some indoor plants to further improve your indoor air quality and open the windows regularly to air out your home.
To avoid chemicals and toxins from tap water, invest in a high-quality water purification and filtration system. Avoid plastic bottles that can further add to toxin build-up. Use glass bottles, aluminum bottles, mason jars, glasses, and ceramic mugs instead.
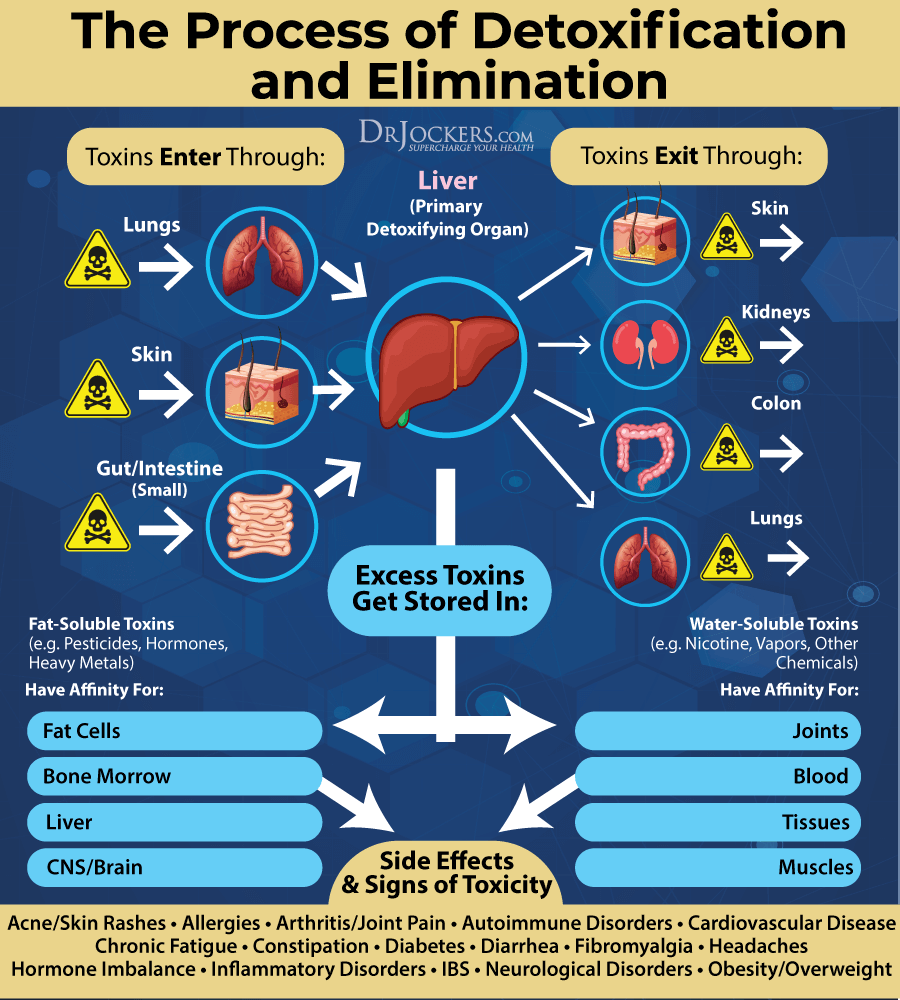
Improve Detoxification Pathways
Toxin build-up from food, plastics, chemicals in various products, environmental toxins, infections, medications, and stress can overwhelm your immune system and contribute to inflammation, hyper-immunity, and eczema. Exercise regularly and use infrared sauna therapy to increase sweating and improve detoxification through the skin.
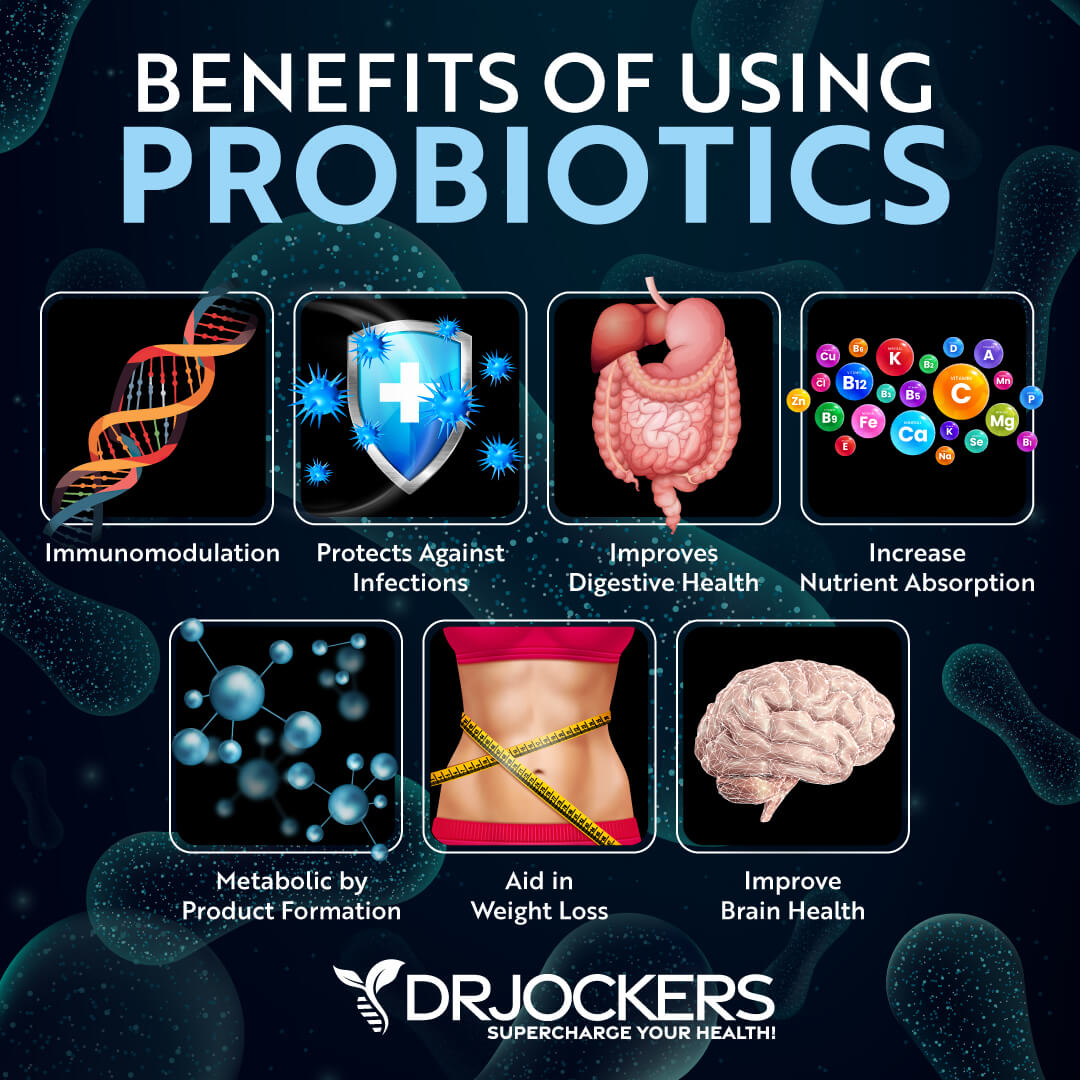
Try dry brushing to improve lymphatic flow, blood circulation, and skin renewal. Consider taking digestive enzymes and probiotics to improve digestion and elimination through food. Try activated charcoal and bioactive carbons to help to remove toxins from your body and if needed, herbal supplements that improve elimination.
Sun Exposure, Phototherapy & Vitamin D Supplementation
Many individuals have found success using phototherapy to reduce symptoms of eczema and psoriasis. Phototherapy is simply narrowband ultraviolet B light that is emitted from a special machine at 311-312 nm. This maximized UVB expression and reduces the more harmful UVA frequencies that are more damaging to the skin.
Phototherapy works by (24)
- Reducing itching and skin proliferation
- Profound anti-inflammatory effects
- Increasing vitamin D production
- Increases immune regulation and bacteria-fighting systems in the skin
I recommend that you spend at least 15 minutes in the sun daily and eat vitamin D-rich foods, such as oily fish, egg yolks, and liver to optimize your vitamin D levels. Since this is not enough for most people, I recommend daily vitamin D supplementation.
Choose a high-quality vitamin D supplement with vitamin K2 to support absorption. You want to test your 25-OH vitamin D levels on a regular basis to get them in the 70-100 ng/mL range for optimal immune health.
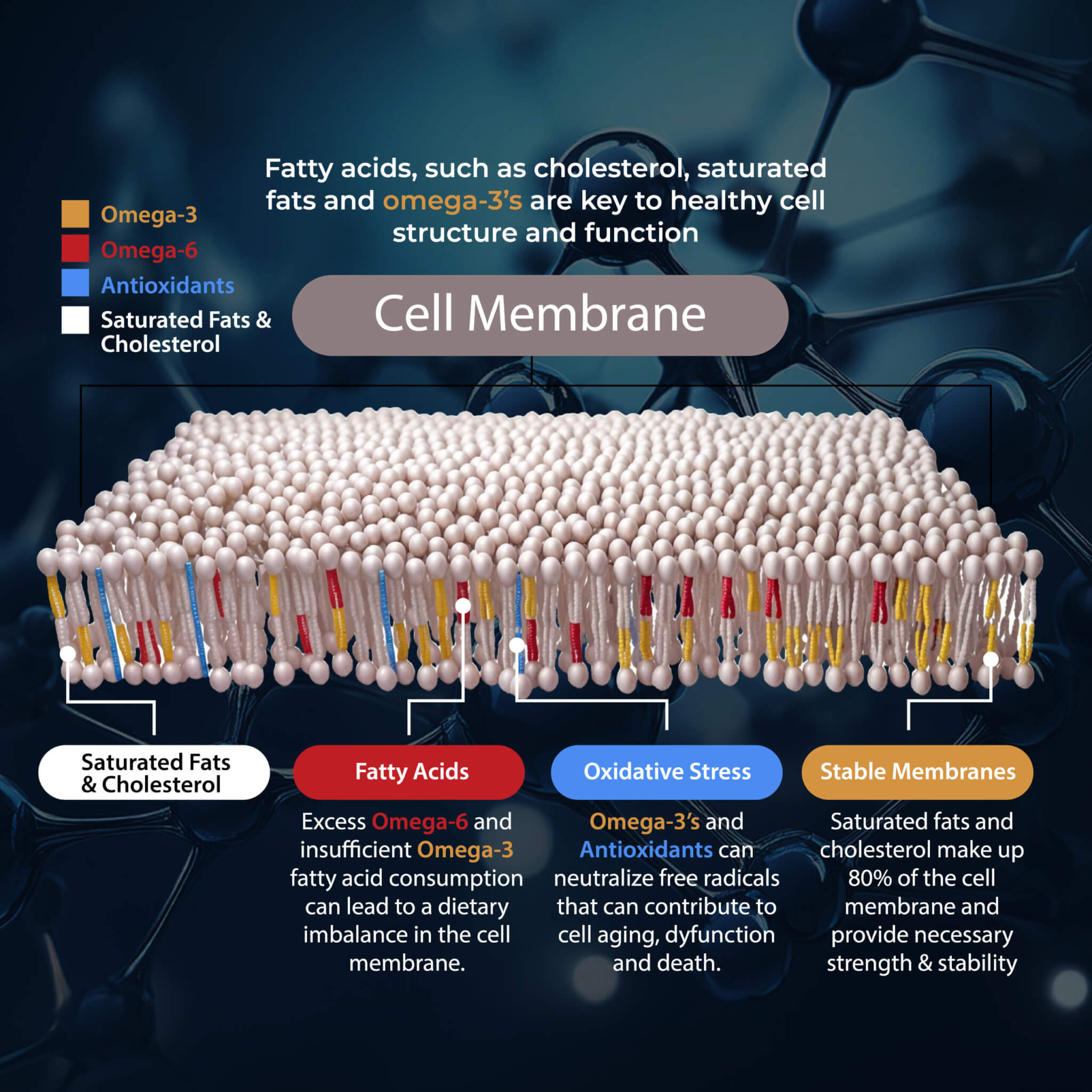
Omega-3 Fatty Acid Supplementation
Omega-3 fatty acids are essential fatty acids that are known for their anti-inflammatory benefits. A 2017 study published in Nutrients has found that omega-3 fatty acids may help to lower the risk of allergic diseases in childhood (25). According to a 2010 study published in The Proceedings of the Nutritional Society, omega-3 fatty acids in early life can help protect the immune system and lower the risk of eczema, allergies, and hay fever (26).
The levels of omega 6:omega 3 are critical for the development and regulation of epidermal barrier integrity and sebum formation. Individuals with higher omega 6 levels had more inflammatory cytokines in the skin tissue, a weakened epidermal barrier and increased sebum production (27, 28).
One type of omega 6 fat, gamma linoleic acid, happens to be very beneficial for individuals with eczema and other skin disorders. Additionally, supplementing with long-chain omega 3 fatty acids EPA and DHA help to reduce inflammatory cytokines in the skin and strengthen epidermal barrier function (29, 30).
According to a 2002 double-blind, randomized, placebo-controlled study published in the Journal of Parenteral and Enteral Nutrition, an omega-3 fish oil resulted in anti-inflammatory effects and showed benefits for atopic dermatitis (31). I recommend that you eat food that is rich in omega-3 fatty acids, including fish, seafood, chia seeds, hemp seeds, and flax seeds, and supplement daily with a high-quality omega-3 fish oil supplement.
Glutathione Levels and Skin Disorders:
Glutathione is the body’s master antioxidant; it is one of the major modulators of the immune system. A 1982 study looked at 61 healthy subjects and 506 patients with various skin disorders. Depressed glutathione levels were observed in patients with psoriasis, eczema, atopic dermatitis, vasculitis, mycosis fungoides and dermatitis herpetiformis (32).
Some studies have demonstrated that individuals with eczema, psoriasis, vitiligo and other skin disorders have genetic polymorphisms in their glutathione production pathways (33, 34). This would indicate higher glutathione needs through dietary precursors and nutritional supplementation. Studies have demonstrated improvement in these conditions with the addition of glutathione precursors via diet and supplementation (35).

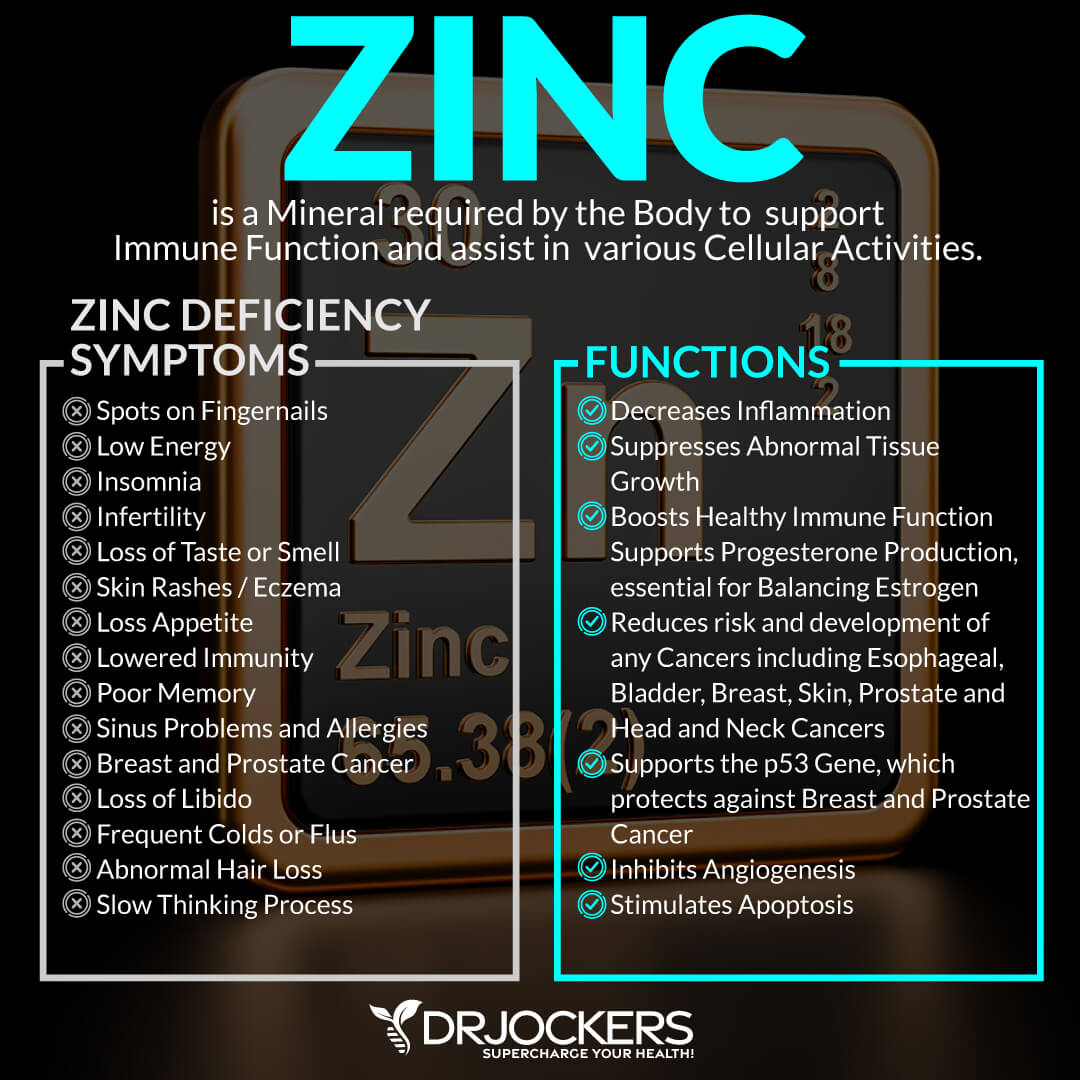
Zinc & Selenium and Eczema
Zinc and selenium deficiencies are rarely known but rather large and widespread issues that promote inflammation and increased risk of inflammatory disorders. Zinc and selenium deficient diets are associated with increased inflammatory cytokines in the skin and reduce epidermal barrier function which predisposes one to developing eczema and other skin disorders (36, 37).
Zinc deficiency is a common issue with infants suffering from eczema (38). Because breast milk is naturally low in zinc, it is important for mothers to supplement and consume a high zinc diet during pregnancy to reduce the risk of eczema in infancy.
When treating eczema with zinc and selenium, it is best to take chelated supplements such as zinc glycinate and selenomethionine. In chelated forms, the zinc and selenium are bound to an amino acid that helps transport it through the gastrointestinal tract. Free selenium and zinc are potentially toxic to humans.
Consider Using Probiotics
Research has shown that oral consumption of probiotics reduced the vasodilation, edema, mast cell degranulation and TNF-alpha release induced by substance P, compared to the control group (39).
Most people think that you have to apply something topically in order to affect the skin, but numerous articles discuss the importance of oral probiotic consumption and reduce skin-related inflammation, reinforce skin barrier function, decrease skin sensitivity, and modulate the skin immune system leading to the preservation of skin homeostasis (40).
Anti-Inflammatory Herbal Compounds
Since inflammation is one of the top root causes and characteristics of eczema, anti-inflammatory herbal compounds may be helpful as a part of your natural support strategies for eczema. Here are the top anti-inflammatory herbal compounds that I recommend. You can find them in individual supplements or together as part of an inflammation defense supplement.
Resveratrol
Resveratrol is a plant compound found in the skin of grapes, berries, and red wine. According to a 2016 study published in Peer Journal, resveratrol affects epithelium-induced cytokines, offers anti-inflammatory benefits, and can benefit those with eczema (41). A 2019 mice study published in Wounds has also found that resveratrol may offer therapeutic benefits for atopic dermatitis (42).
Quercetin
Quercetin is a plant compound with similar and complementary antioxidant and anti-inflammatory benefits to resveratrol. A 2016 single-blind study on human subjects published in Clinical, Cosmetic, and Investigational Dermatology has found that quercetin has anti-itch and soothing benefits for skin inflammation (43).
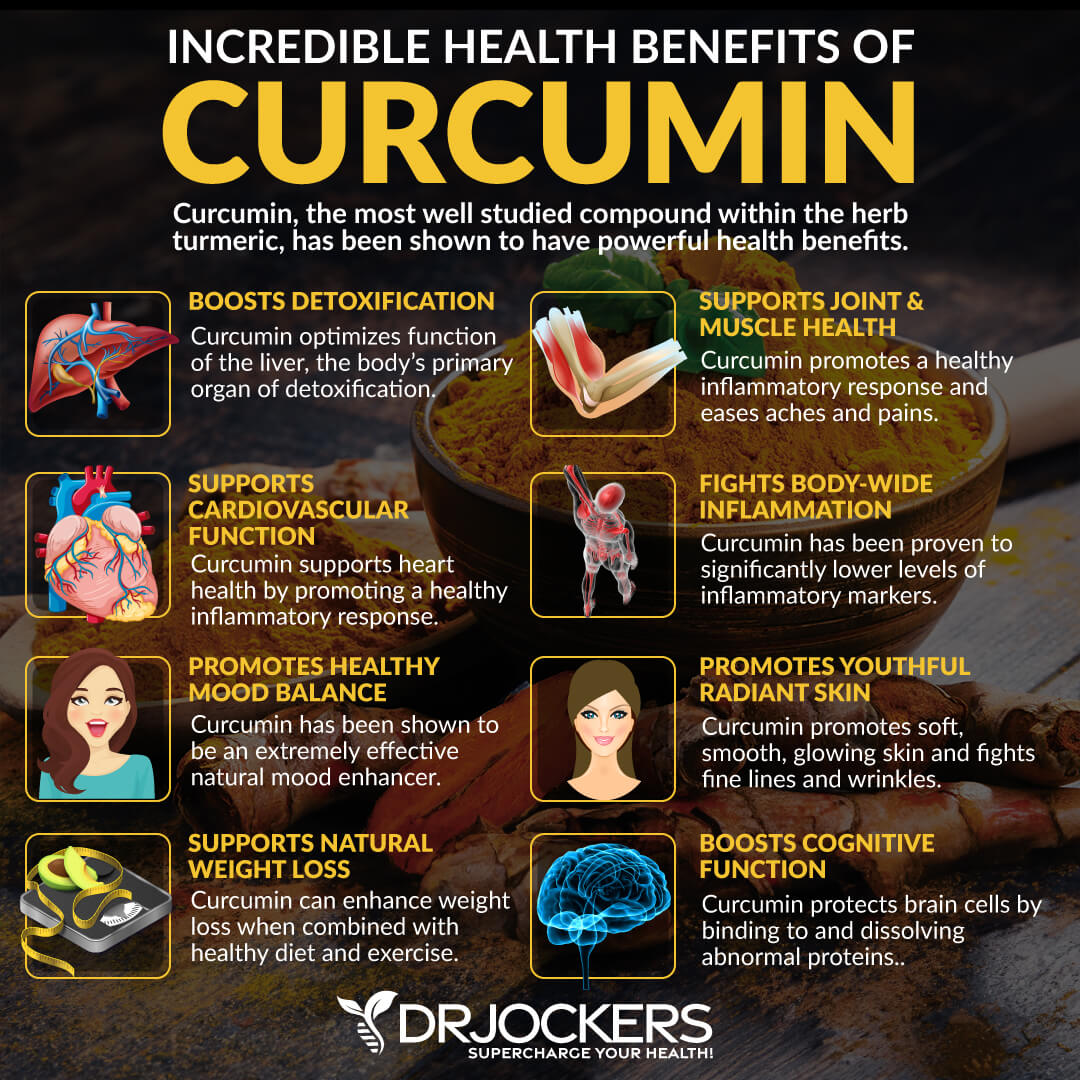
Curcumin
Curcumin is the active compound that provides turmeric all its anti-inflammatory health benefits, including for the skin. A 2019 study published in Nutrients has found that because of its anti-inflammatory benefits, curcumin may be helpful for various skin disorders (44).
Purity Woods Age-Defying Dream Cream
Healthy, radiant looking skin is certainly a confidence booster. It is a goal that everyone tries to achieve (and keep) throughout their lives. As we begin to get older, there are millions of tricks, tips and procedures out there to maintain the same healthy-looking skin we had when we were younger.
That’s why I would like to share my top choice for keeping skin looking young and healthy – the USDA Certified Organic Age-Defying Dream Cream from Purity Woods.
This anti-aging cream is truly a game changer when it comes to achieving and KEEPING your skin looking and feeling spectacular. Now you can save up to 38% on this amazing product, simply click here to learn more!
Final Thoughts
Eczema is a common skin condition that affects over 31 million people in the United States and causes skin inflammation, itchiness, scaly rashes, and sensitivity. If you have eczema or other skin inflammation symptoms, I recommend that you follow my top natural support strategies for eczema and skin health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. We do offer long-distance functional health coaching programs with our world class team of health coaches. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




