 C. Diff Infection: Risk Factors, Symptoms, and Support Strategies
C. Diff Infection: Risk Factors, Symptoms, and Support Strategies
Did you know that there are about half a million C. diff infections in the United States alone each year? C. diff is a bacterium that can cause severe diarrhea and clostridium difficile colitis. Infection and re-infection rates are high, but certain natural support strategies can reduce your risk and improve your health.
In this article, you will learn what C. diff is. You will understand its signs and symptoms. You will learn about its risk factors. I will explain how C. diff is diagnosed. You will learn about conventional treatment strategies for C. diff. I will explain the root causes of C. diff infection. I will also offer some natural support strategies to improve your health.
What Is C. Diff?
C diff is also known as C. difficile or Clostridioides difficile. It is a bacterium that causes severe diarrhea and clostridium difficile colitis. Clostridium difficile colitis is characterized by inflammation of the wall of the colon and a list of related symptoms (1).
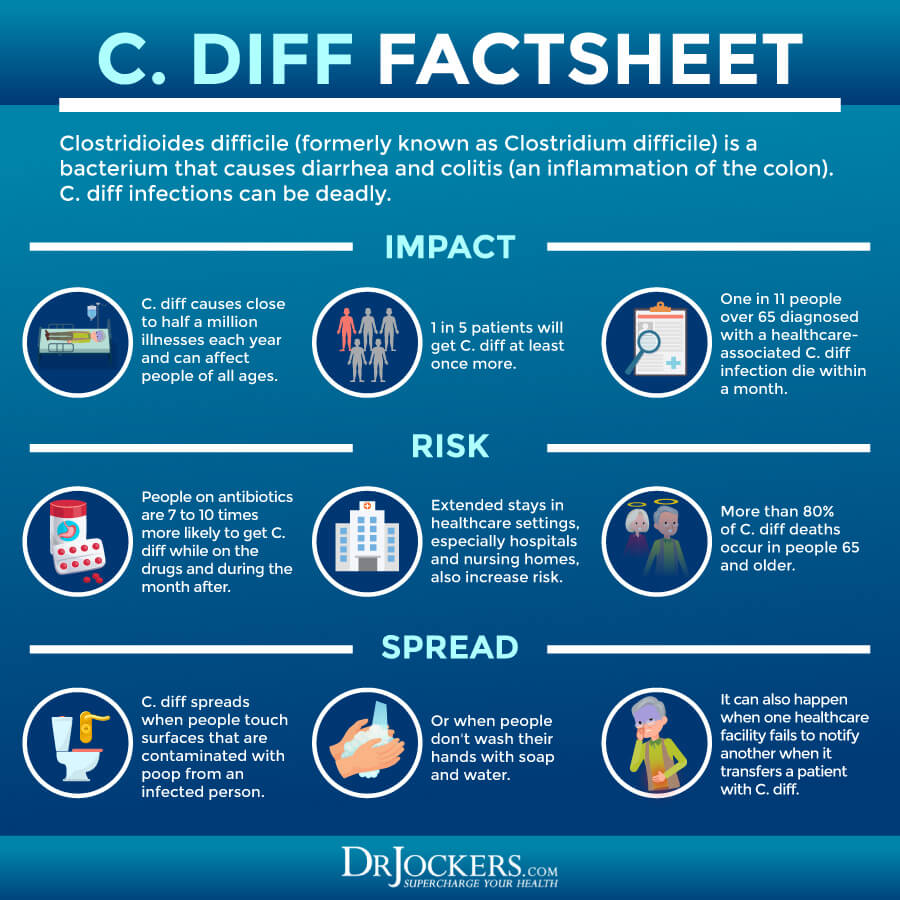
According to the Centers for Disease Control and Prevention (CDC), there are about half a million C. diff infections in the United States per year (1). Reinfection rates are also high. About 1 in 6 people with a C. diff infection will get reinfected within 2 to 8 weeks (1).
C diff is particularly problematic in older people. One in 11 among those over 65 with healthcare-related C. diff dies in less than a month after the infection (1).
Signs & Symptoms of C. Diff Infection
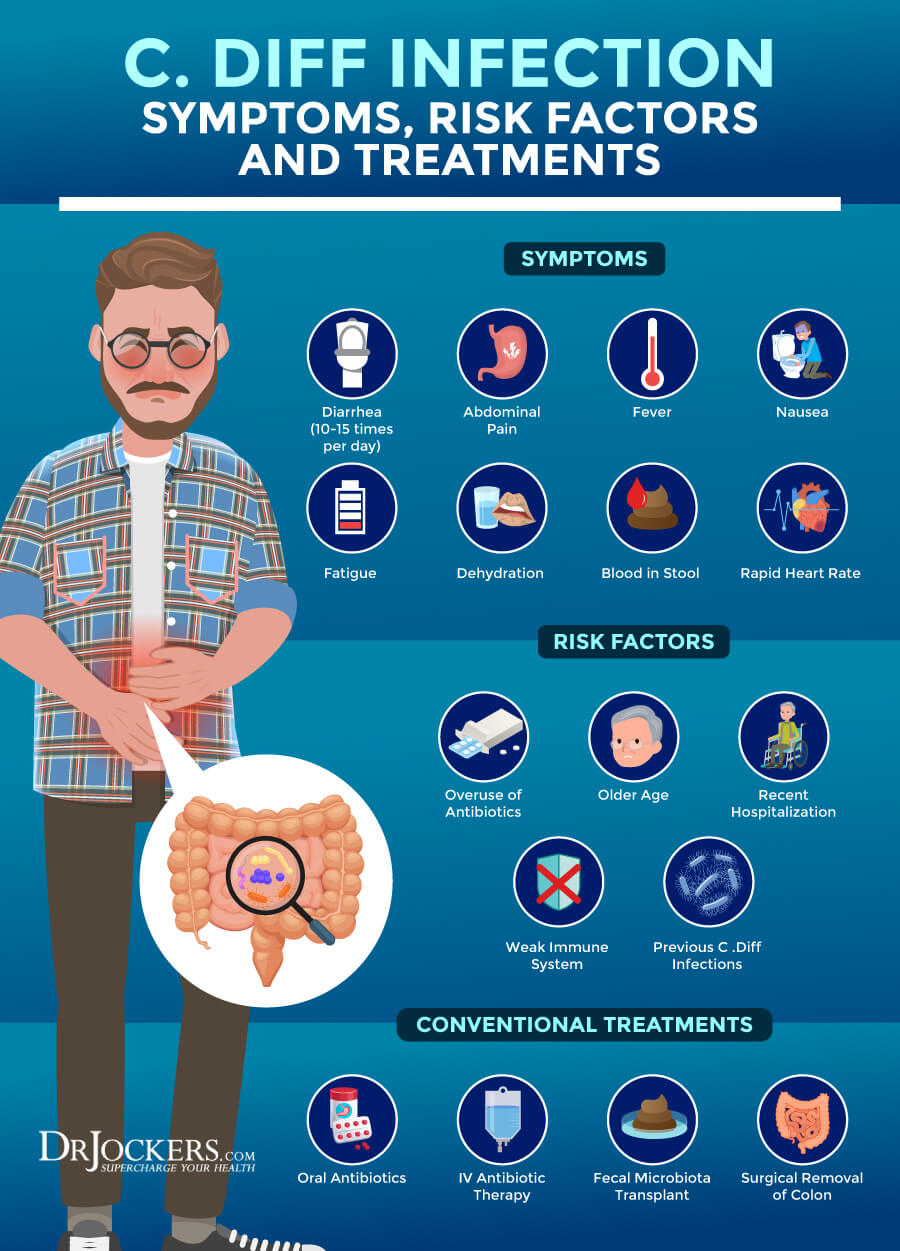
Signs and Symptoms of a C. diff infection may include (1):
- Severe diarrhea
- Stomach pain or tenderness
- Fever
- Nausea
- Loss of appetite
- Dehydration
- Blood in stool
Major Risk Factors for C. Diff Infection
C diff infection can occur in anyone, but certain factors can increase your risk (1):
- Antibiotic use: C. diff most often occurs while taking antibiotics or soon after finishing a course of antibiotics.
- Older Age: C. diff is more common among those over 65.
- Hospitalization: Healthcare-related C. diff infections during a stay at a hospital or nursing home are common.
- Weak immune system: Weakened immunity due to cancer, HIV/AIDS, or taking immunosuppressive drugs after an organ transplant can increase your risk.
- Previous C. diff infection: a previous C. diff infection or exposure can increase your risk of reinfection.
Diagnosis and Conventional Therapies
After reviewing your symptoms and medical history, your doctor will likely order a stool sample to look for toxins or toxin genes of C. diff. In more severe cases, they may perform a sigmoidoscopy. A sigmoidoscopy is a procedure that uses a sigmoidoscope. A sigmoidoscope is a long, thin device inserted into your colon to look for inflammation, abnormalities, and infections.
In most cases, the conventional treatment for C. diff is antibiotic therapy. The most common antibiotics used as the first line of treatment are oral fidaxomicin or oral vancomycin. If these two are not available, your doctor may recommend oral metronidazole (1, 2).
While in most cases oral antibiotics are enough, severe infections may require intravenous (IV) antibiotic treatment. To avoid dehydration, drinking enough water is critical. In severe cases, IV fluids may be necessary to avoid or treat dehydration.
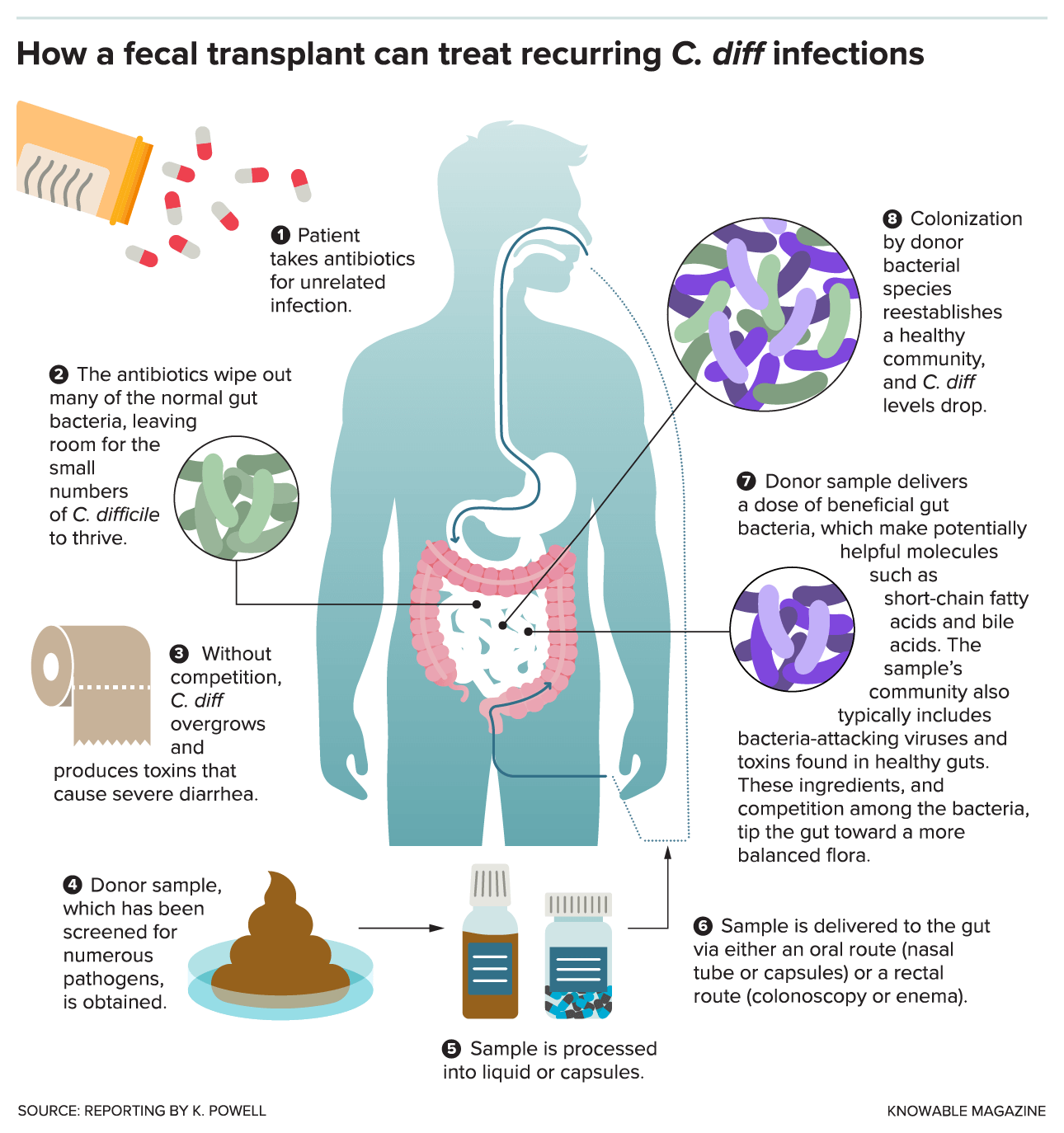
In those with at least two rounds of recurrent C. diff, a fecal microbiota transplant may be recommended after a course of antibiotics. In rare and very affected cases, surgery may be required to remove a part of the colon.
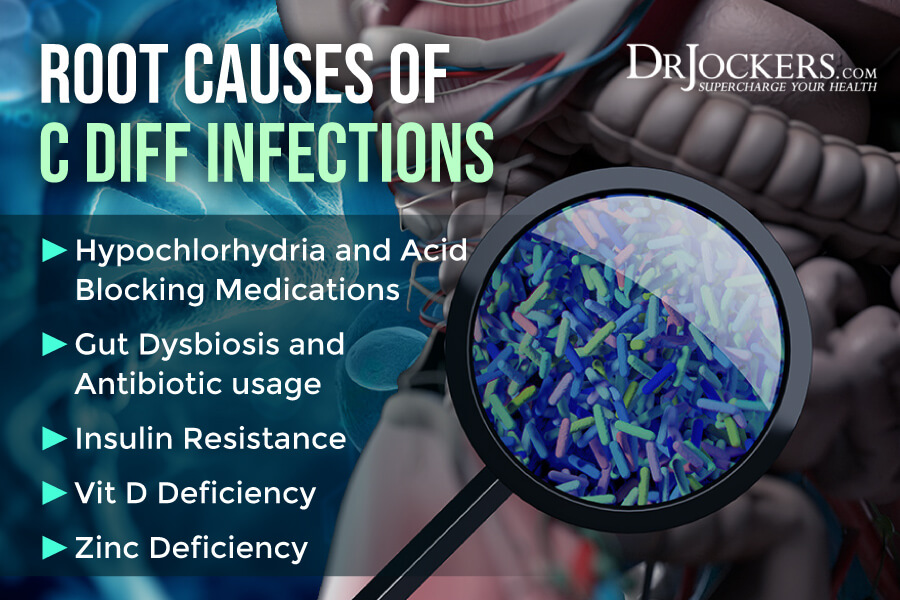
Root Causes of C. Diff Infections
Certain medications, health issues, and nutrient deficiencies can make you more vulnerable to a C. diff infection. Let’s talk about the root cause of C. diff infections:
Hypochlorhydria and Acid-Blocking Medications
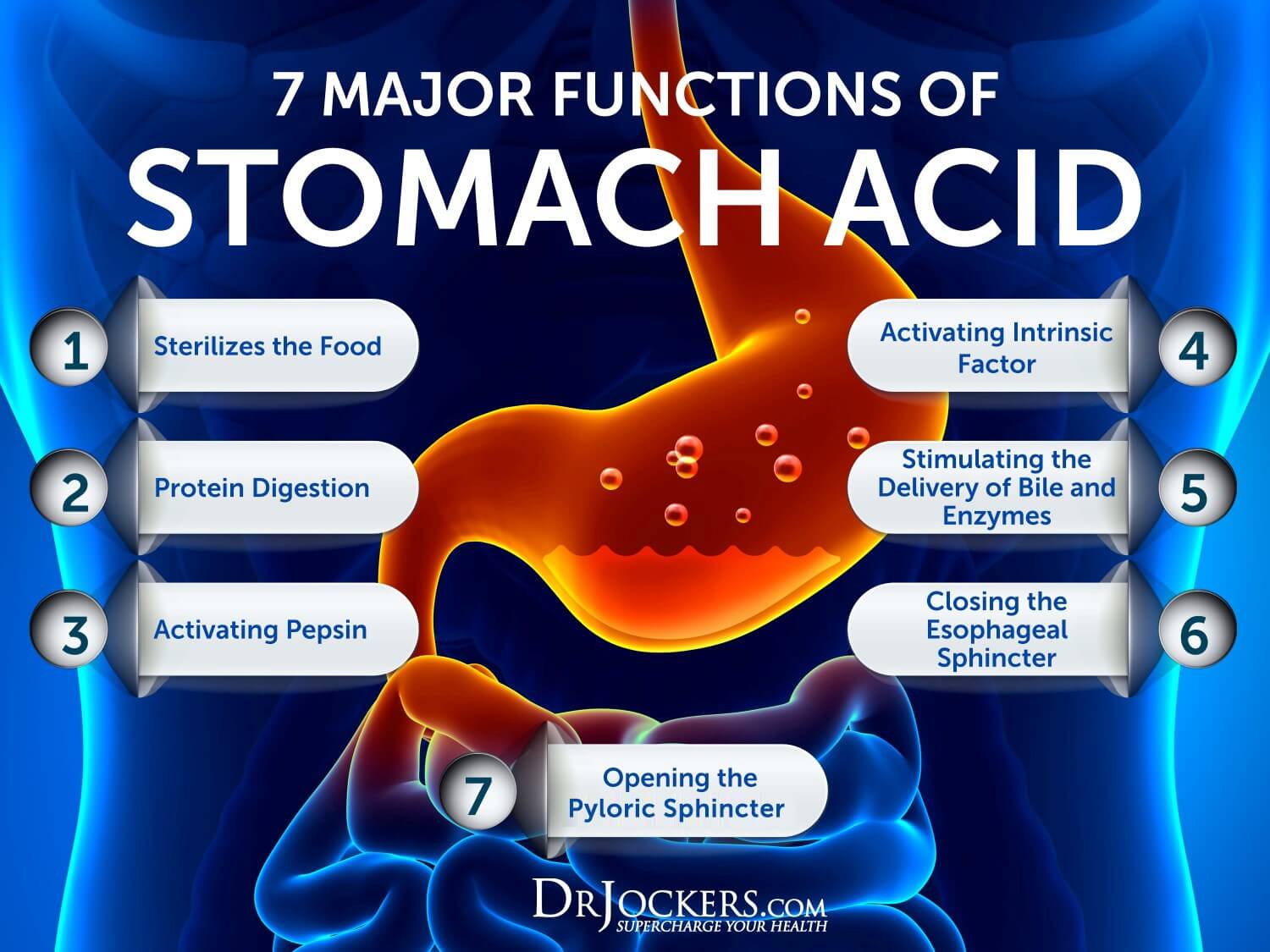
Hydrochloric acid or stomach acid allows your body to break down, digest, and absorb protein and other nutrients. It also sterilizes your gut environment and removes bacteria and viruses in your stomach, reducing your risk of infections. Clearly, stomach acid is critical for your digestive system, gut function, and overall health.
Hypochlorhydria means that you have low levels of stomach acid. Hypochlorhydria can increase your risk of digestive problems, nutritional deficiencies, and gastrointestinal infections.
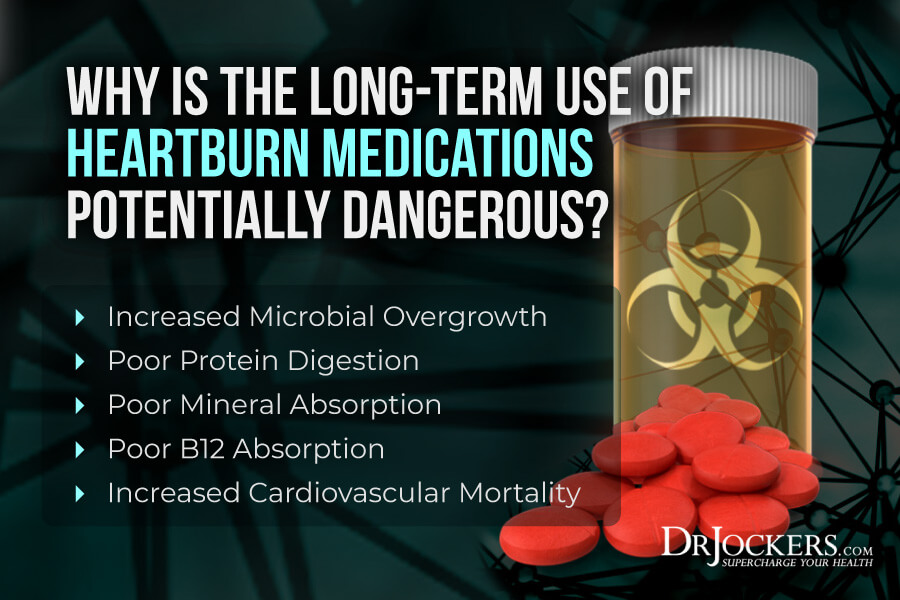
Acid-blocking medications, on the other hand, reduce stomach acid levels in your gut. The problem is that these medications are often overprescribed and given to people who have normal or low levels of stomach acid. For example, acid reflux and heartburn are caused by low levels of stomach acids, yet, conventional doctors still commonly recommend antacids for your symptoms. Taking acid-blocking medication, especially when it’s not needed, can result in too low stomach acid levels and related symptoms.
C Diff Infections and Acid Blocking Medications
Research suggests that hypochlorhydria and acid-blocking medications can both increase your risk for a C. diff infection. This may cause a problem in both children and adults.
A 2014 study published in the Journal of Pediatrics has found a link between acid suppression medications and C. diff infections in children between age 2 and 18 (3). A 2014 study published in Critical Care has found a link between proton pump inhibitor acid-suppressants and C. diff infection among critically ill patients in an ICU hospital setting (4).
A 2017 systematic review and meta-analysis of 16 studies and 7703 patients published in JAMA Internal Medicine has also found a link between stomach acid suppression and C. diff (5). They looked at 16 studies and 7703 patients and found that proton pump inhibitors and histamine H2 blockers may increase the risk of recurrent C. diff infection.
Gut Dysbiosis and Antibiotic usage
Your body is full of colonies of microorganisms, referred to as your microbiome. There are billions of beneficial bacteria living in your gut that have positive effects on your health. They support your digestion, immune function, brain and neurological health, and other functions.
Having a good microbiome balance with more beneficial bacteria than harmful bacteria and pathogens is critical for your health. When the bacterial colonies in your microbiome become out of balance, and you have too many bad bugs, you can develop gut dysbiosis. Gut dysbiosis refers to an imbalance in your gastrointestinal (GI) tract). It can lead to digestive problems and an array of non-gut symptoms, including headaches, fatigue, brain fog, and poor immunity.
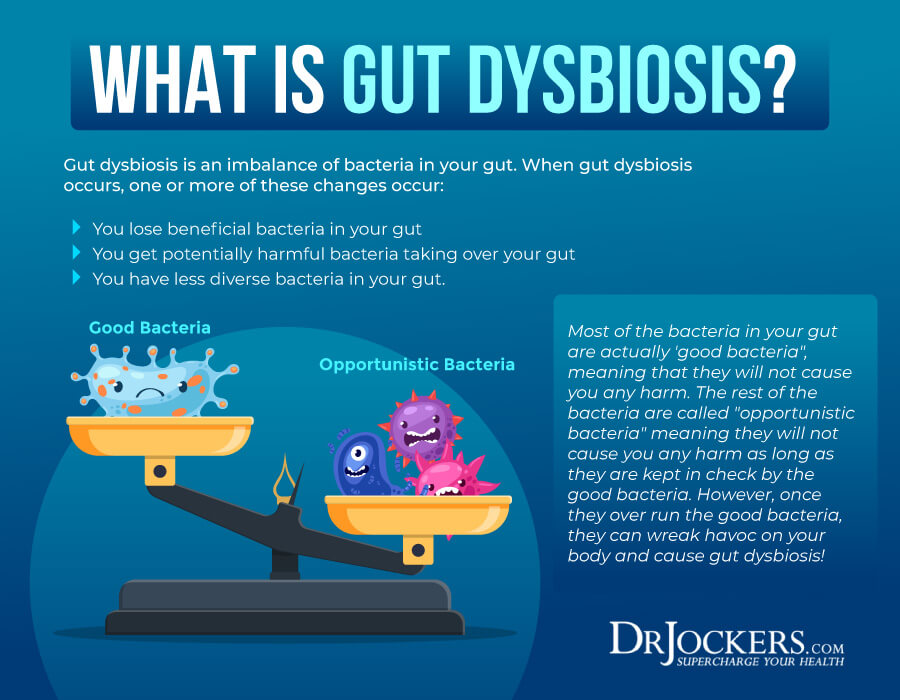
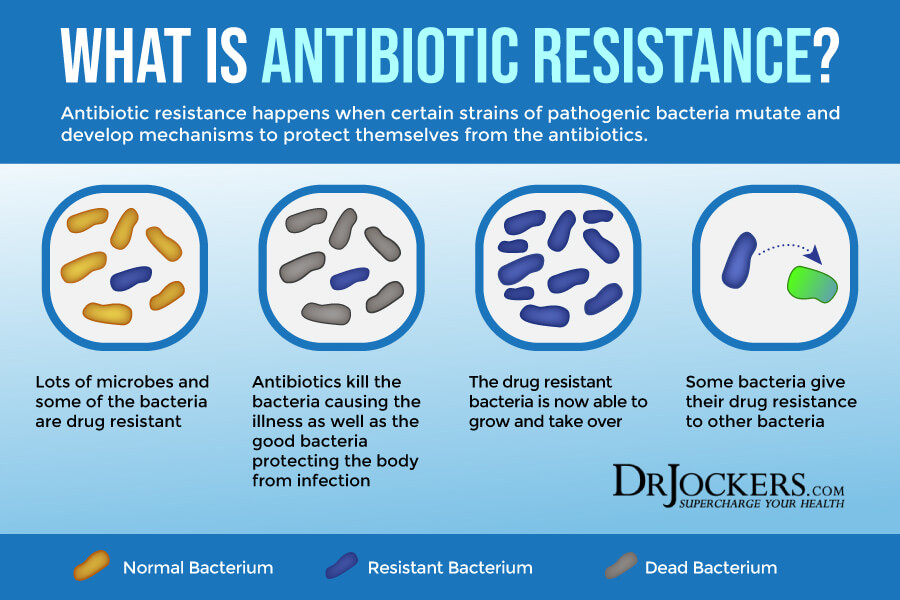
There are a number of factors that can increase your risk of developing gut dysbiosis, including dietary and lifestyle choices. One of the main contributing factors that can lead to gut dysbiosis is antibiotic use. Antibiotics are designed to tackle bacterial infections. While they do a good job at killing bad bacteria, antibiotics also kill beneficial bacteria. Yes, they wipe out the good guys as well.
Taking probiotics and eating probiotic-rich foods is critical to repopulate the good bacteria population after antibiotic use. However, antibiotic use, especially if you haven’t been taking high-quality probiotics, can increase your risk of gut dysbiosis, pathogenic overgrowth, and new bacterial infections. Both gut dysbiosis and antibiotic use can increase your risk of a C. diff infection.
A 2013 study published in Therapeutic Advances in Gastroenterology has found a connection between gut dysbiosis and C. diff (6). According to the study, gut dysbiosis increases the risk of gut infections, particularly the risk of a C. diff infection which may contribute to the development of inflammatory bowel disease (IBD).
A 2016 study published in the Human Microbiome Journal has also found a connection between the gut microbiome and C. diff (7). According to the paper, taking antibiotics or proton pump inhibitors can compromise gut microbiome balance increasing the risk of C. diff. The author recommended considering microbiome-based therapeutic approaches such as fecal microbiota transplantation to improve the gut microbiome and reduce infections.
A 2013 meta-analysis published in Antimicrobial Agents and Chemotherapy has found that antibiotic use may play a role in the development of C. diff (8). Researchers found that by reducing the use of high-risk antibiotics, they can reduce the risk of infections. A 2019 review published in Cureus has found that probiotics can help prevent and mitigate C. diff by improving the gut microbiome (9).
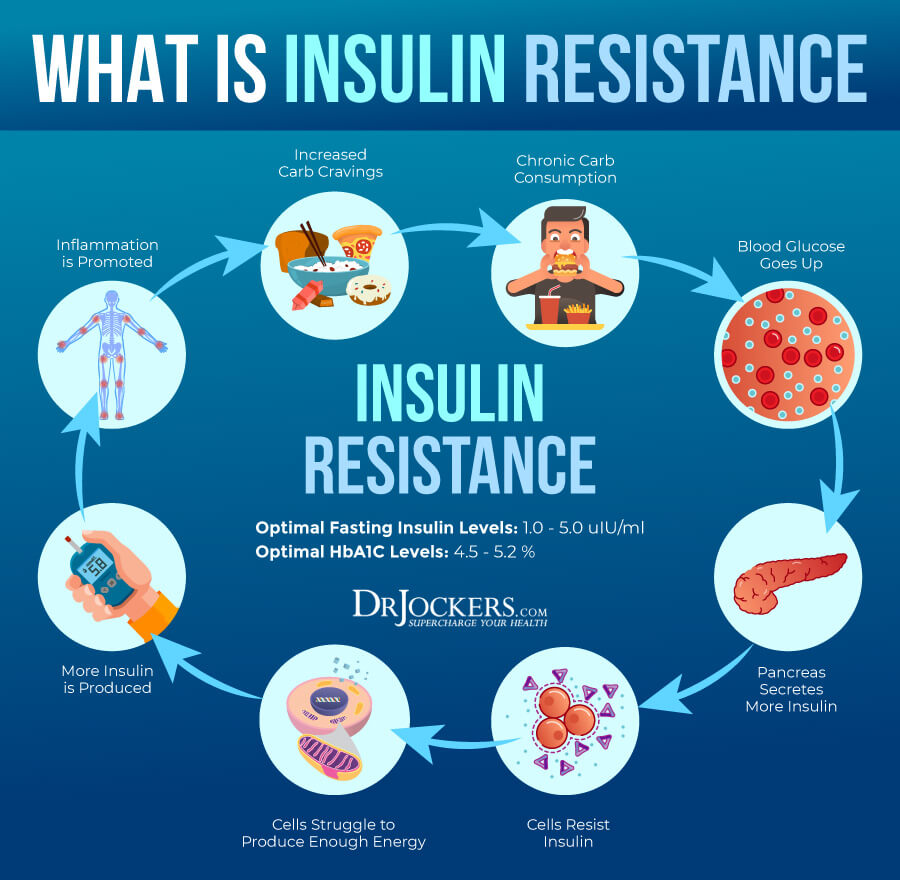
Insulin Resistance
Insulin resistance means that your body is unable to respond to insulin well and, as a result, can’t process your blood glucose properly. Insulin resistance increases the risk of prediabetes and type 2 diabetes. Type 2 diabetes is a chronic health condition characterized by high blood sugar levels and your body’s inability to control blood sugar. It is a serious health issue that may increase your risk of a variety of symptoms and health issues, including C. diff.
A 2013 study published in the Journal of Royal College of Physicians in Edinburgh has found that C. diff infections are very common among type 2 diabetes patients in hospital settings (10). A 2014 review published in Diabetes Research and Clinical Practice has also found a connection between diabetes and C. diff (11). Researchers found that diabetes-related problems that require hospitalization may be further aggravated by C. diff. They also found that diabetes may increase the risk of recurrent C. diff infections.
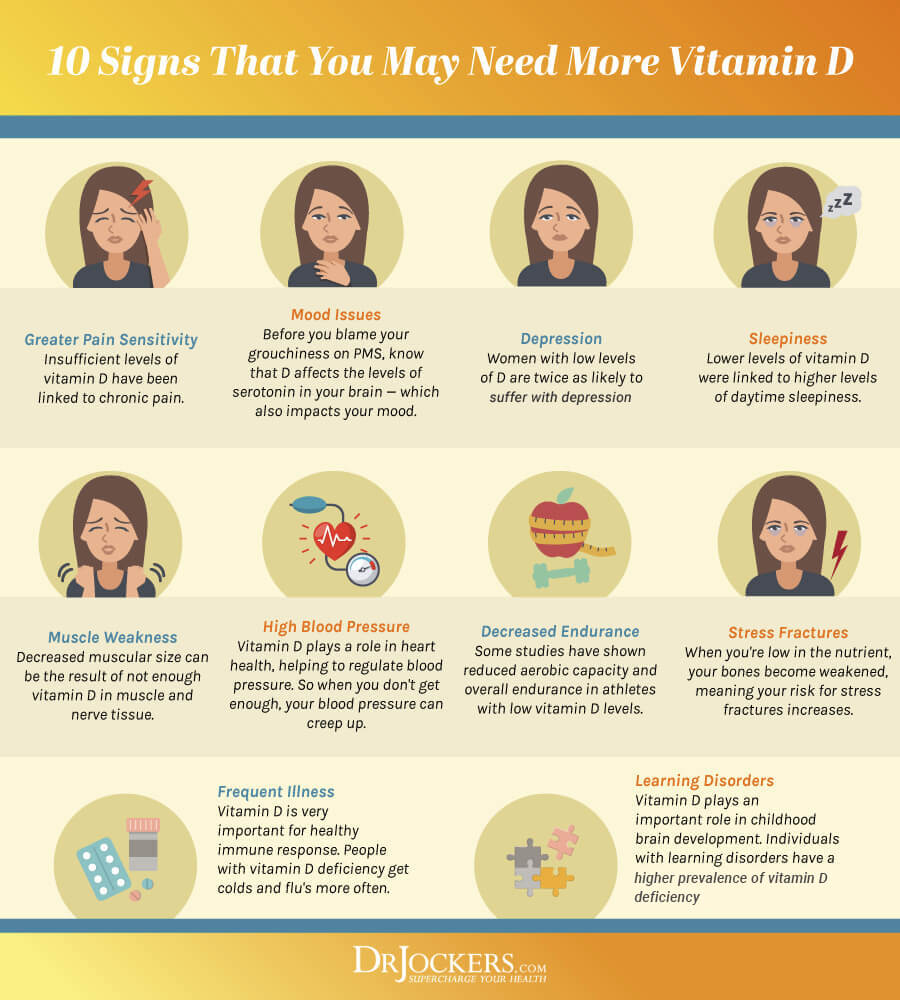
Vitamin D Deficiency
Vitamin D is one of the most important nutrients. It is also a vitamin that most people are deficient in. Vitamin D is critical for your immune system, intestinal health, muscles, bones, teeth, brain and mental health, and overall wellness.
A 2014 case-control study published in BMC Infectious Diseases explained that vitamin D plays a critical role in intestinal immunity (12). Researchers found that vitamin D deficiency may increase the risk of community-acquired C. diff infections. A 2015 prospective cohort study published in the Journal of Parenteral and Enteral Nutrition has found that vitamin D deficiency can worsen the symptoms of C. diff infections (13).
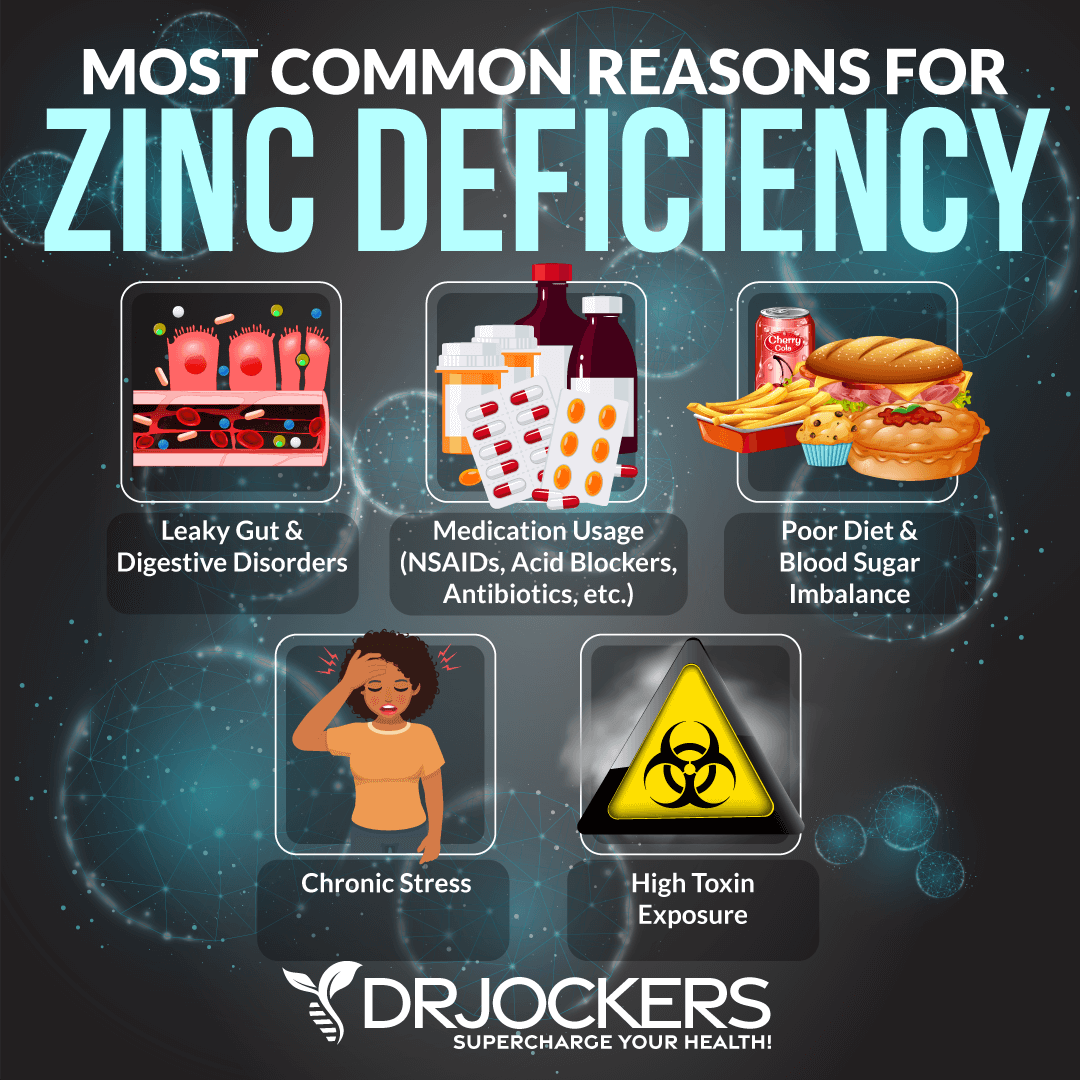
Zinc Deficiency
Zinc is a critical mineral. It is essential for your immune system and your body’s ability to fight infections. It is also necessary for reducing inflammation, supporting your metabolism, and offering anti-aging benefits.
A 2016study published in Nature Medicine has found that dietary zinc affects the microbiome (14). Your zinc levels may determine your risk factor to C. diff and your body’s ability to resist and fight off the infection.
A 2020 case report and literature review published in the Journal of Investigative Medicine High Impact Case Reports have found similar results (15). Researchers found that low zinc levels may play a role in and increase the risk of recurrent C. diff infections. They found that zinc supplementation may help to reduce infections.
When we talk about zinc, we have to talk about another mineral, copper as well though. Zinc and copper compete against each other as antagonists to regulate physiological pathways. A proper balance between the two is essential for maintaining good gut and overall health.
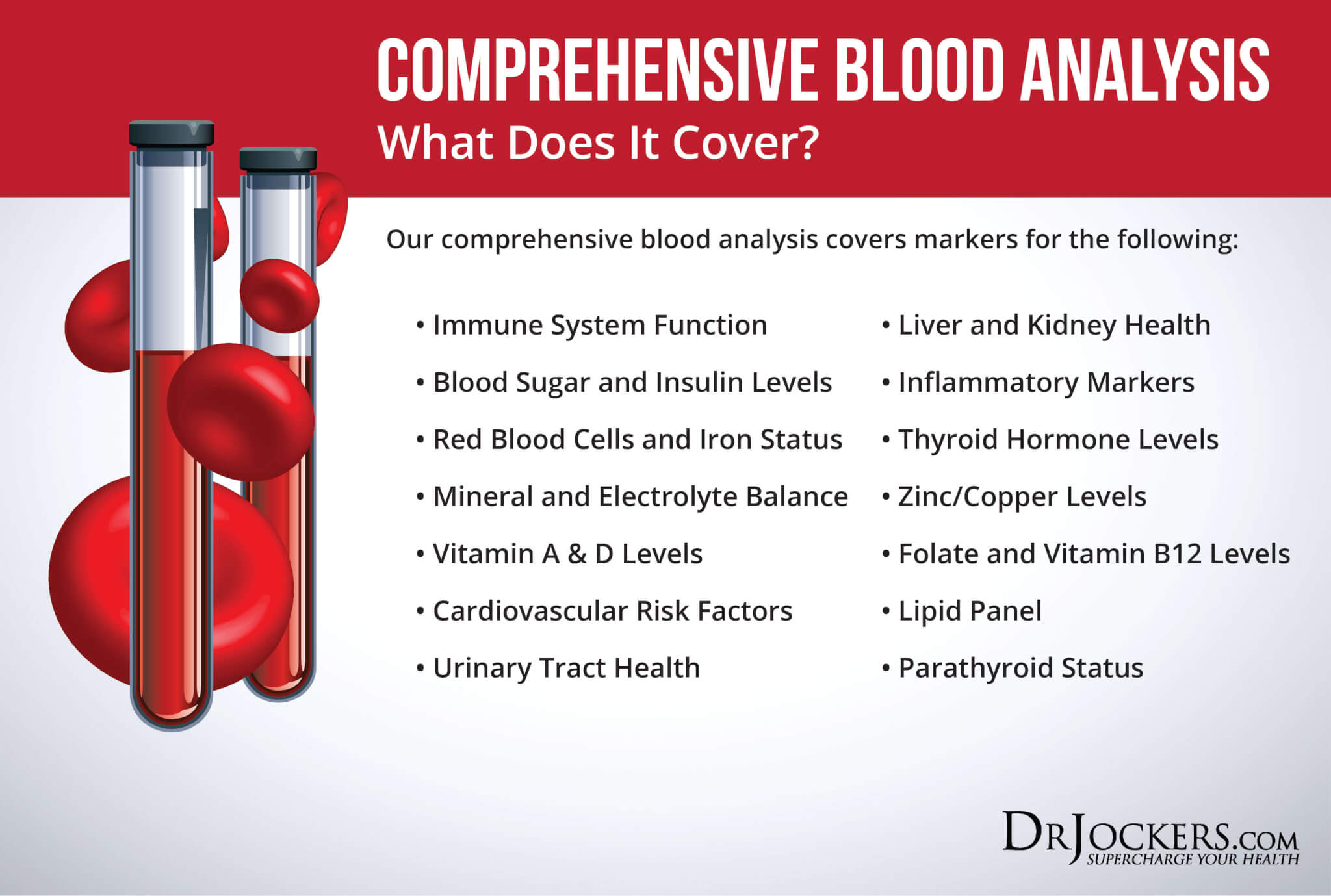
I recommend checking your plasma zinc and serum copper levels and their balance. I recommend a Comprehensive Blood Analysis to check your zinc levels and zinc:copper ratio. The proper zinc:copper ratio should be 1:8, the normal range for zinc is 150 – 240µg/gram, and the serum copper ratio should be between 1 and 1.2.
Natural Support Strategies
There are several natural support strategies I recommend to improve your gut health and reduce the risk of infections. While these strategies are not FDA approved to prevent, mitigate, treat, or cure C Diff infections, there is data that suggests they are very helpful. Please discuss these with your physician or health care practitioner.
Avoid Antibiotics
You already know that gut dysbiosis and antibiotic use can increase your risk of a C. diff infection (6, 7, 8, 9). Avoiding antibiotics is critical to keep your gut microbiome health and reduce the risk of infections.
However, sometimes taking antibiotics is necessary. If you must use antibiotics for any reason, be sure to take Saccharomyces Boulardii. This is a beneficial yeast that is not impacted by antibiotics and can help prevent C. diff overgrowth.
A 1993 study published in Gastroenterology has found that Saccharomyces boulardii may help to prevent the binding of C. diff and prevent infections (16). Other studies since then have found similar results.
A 2009 systematic review published in the Canadian Journal of Gastroenterology has found that antibiotic-associated C. diff infections and diarrhea are common in hospitals, however, Saccharomyces Boulardii probiotics may help to prevent infections (17). A 2018 study published in the European Journal of Clinical Microbiology and Infectious Diseases has also found that Saccharomyces Boulardii may help to prevent C. diff (18).

Gut-Friendly Nutrition Strategies
Gut microbiome imbalance is one of the leading root causes of C. diff infections (6, 7, 8, 9). One of the best ways to support your microbiome health, reduce the risk of gut dysbiosis, and lower your risk of gut infections is by following gut-friendly nutrition strategies. Here is what I recommend:
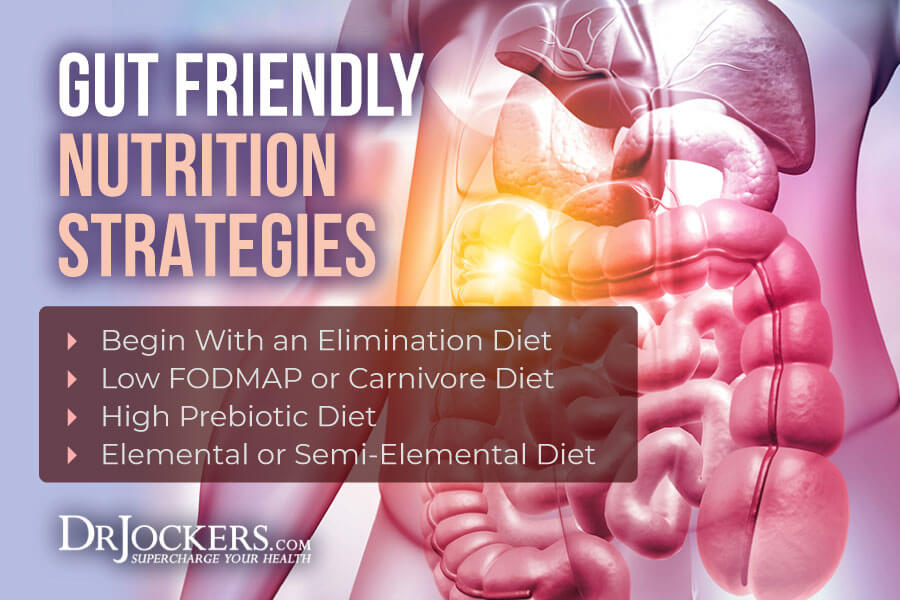
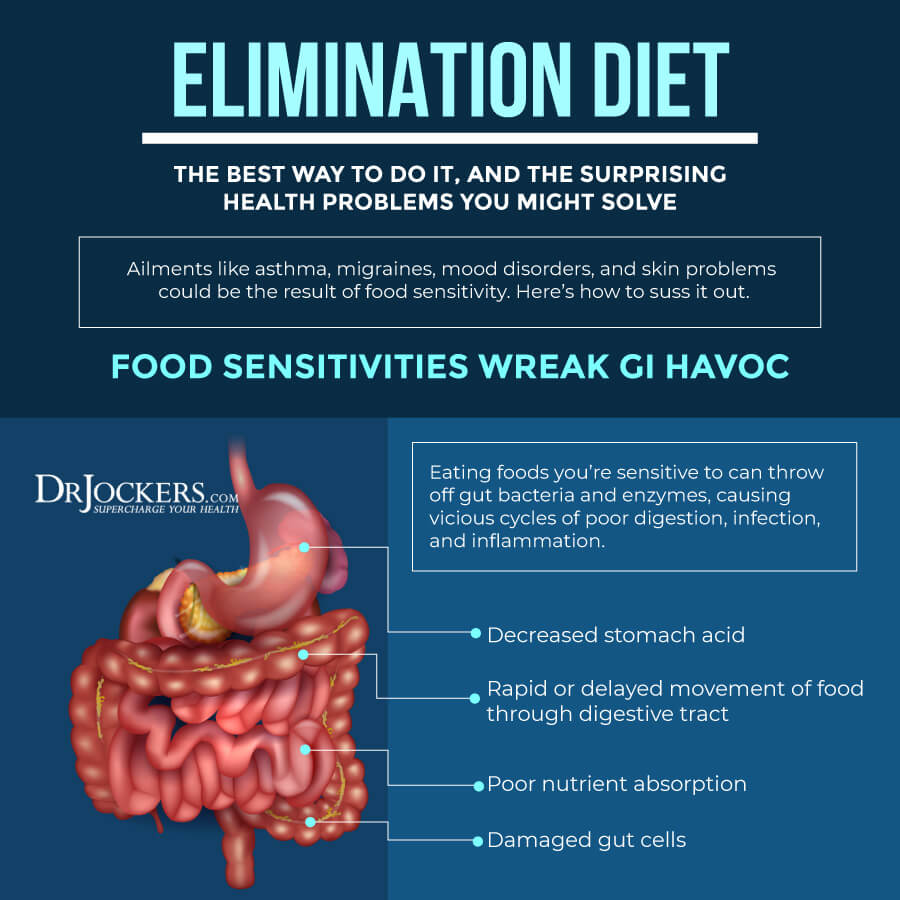
Try an Elimination Diet
Food sensitivities can increase chronic inflammation and gut dysbiosis which may make you more vulnerable to C. diff. Trying an elimination diet is the best strategy to figure out what food sensitivities you may have.
To start, take out the following food groups from your diet for two weeks: gluten, dairy, refined sugar, corn, soy, eggs, all grains, vegetable oils, shellfish, tree nuts, legumes, and nightshade vegetables. Make sure that you follow the plan and don’t cheat. Eating just a bit of these foods can cause symptoms and throw your efforts off.
After a two-week elimination period, introduce foods to your diet one by one. Eat new food for two to three days. Notice your symptoms. If you have symptoms, remove them. Add a new food, note your symptoms, and continue. Generally, I recommend that you remove highly inflammatory foods, such as gluten, refined sugar, vegetable oils, and conventional dairy from your diet for good.
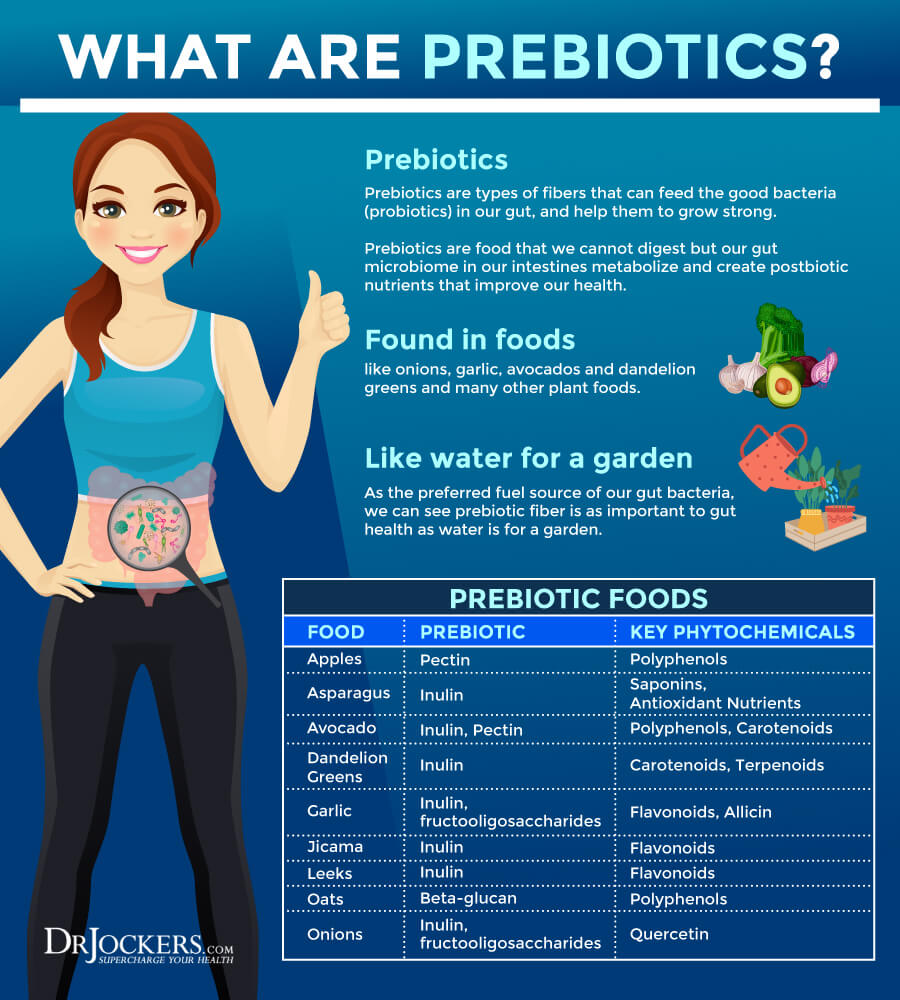
Try a Prebiotic-Rich Diet
Prebiotics can be very beneficial for your digestion. They are a specific dietary fiber that feeds the good bacteria or probiotics in your gut. Probiotics are not enough. You have to feed and support them with prebiotics. Prebiotic-rich foods include Jerusalem artichokes, leek, onion, garlic, asparagus, dandelion, chicory greens, jicama, apples, and bananas.
However, prebiotics is not right for everyone. Some people find too many prebiotics are triggering for them. If you are following a low-FODMAP diet, prebiotics is not the right choice. I recommend that you try a prebiotic-rich diet. Pay attention to your symptoms. If you find it triggering, back of an reduce your intake.
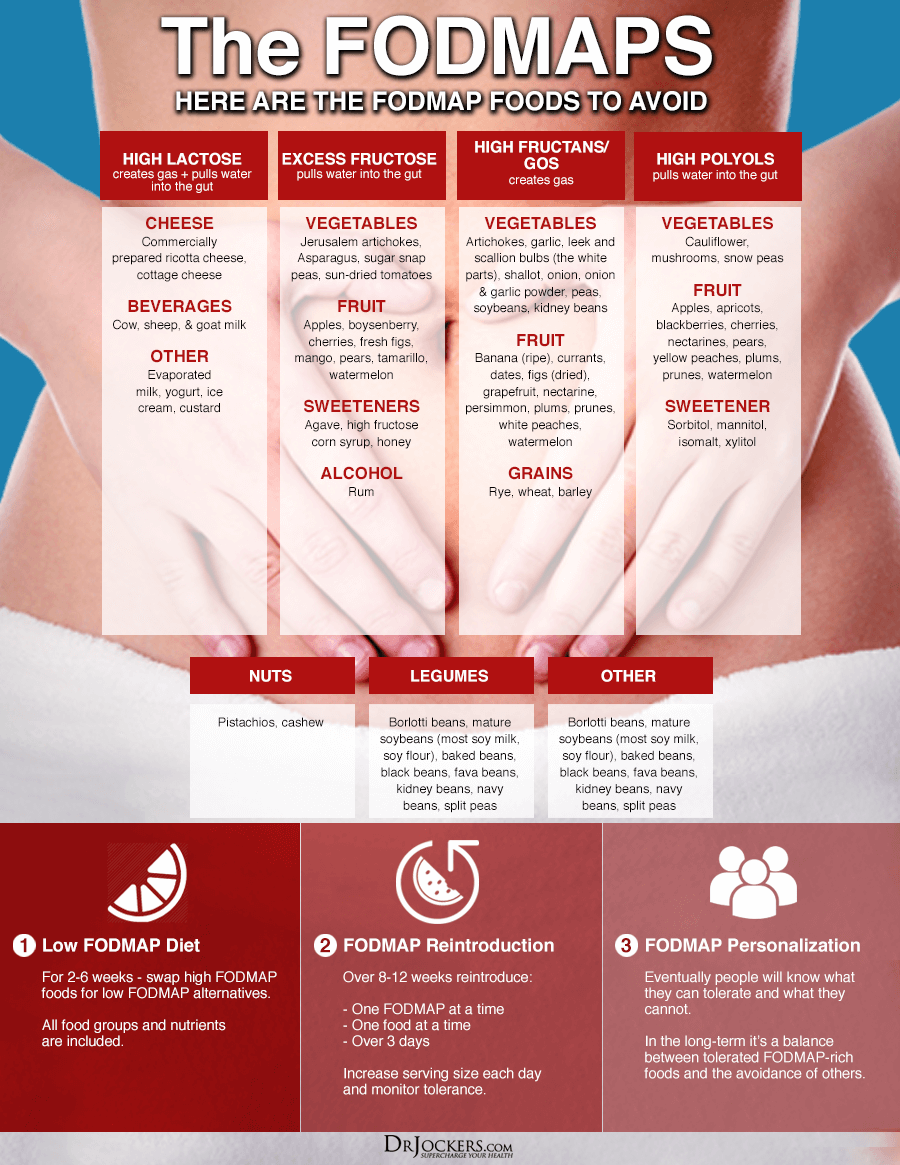
Try a Low-FODMAP Diet
The low-FODMAP diet is a diet low in fermentable oligo-, di-, monosaccharides, and polyols or FODMAPS, certain sugars that may cause intestinal distress. The low-FODMAP diet is generally recommended for people with small intestinal overgrowth (SIBO). However, they may also be beneficial for those with other gut infections and digestive discomfort.
Low-FODMAP vegetables include carrots, green beans, arugula, mint, basil, pepper, olive, pumpkin, tomato, potatoes, sweet potatoes, cucumber, zucchini, Swiss chards, lettuce, radishes, parsnip, sprouts, kale, and collard greens. Low-FODMAP fruits include lemon, lime, kiwi, grapes, papayas, strawberries, raspberries, blueberries, melon, pineapples, and tangerines. Other low-FODMAP foods include egg, meats, fish, brazil nuts, chestnuts, butter, bone broth, seafood, quinoa, millet, rice, walnuts, and pine nuts.
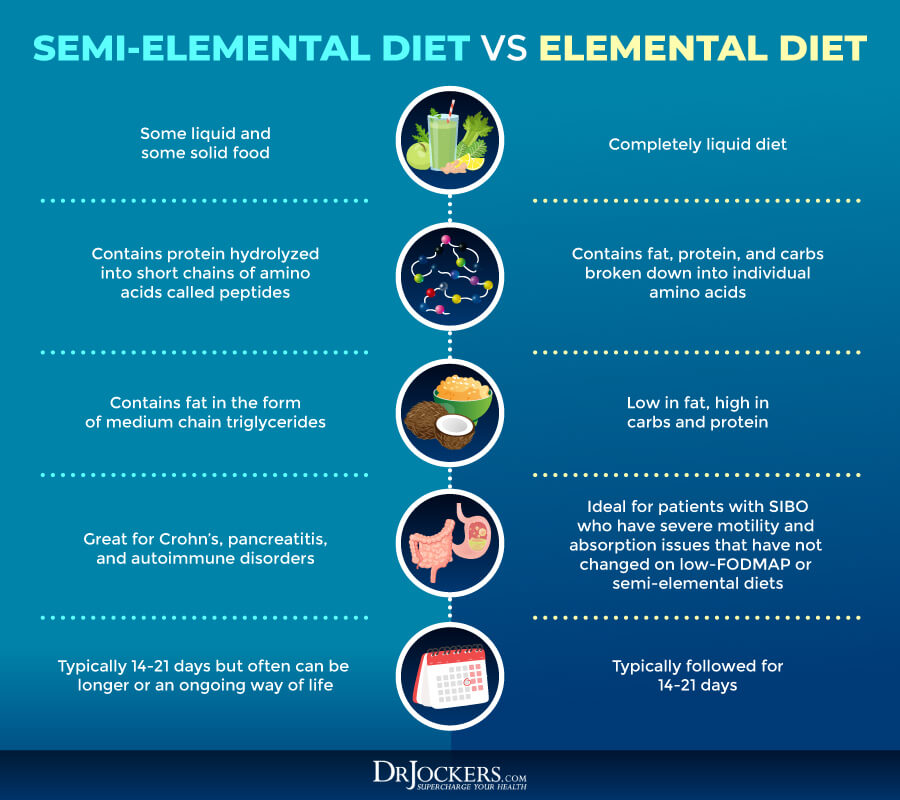
Try a Semi-Elemental or Elemental Diet
The elemental diet is a diet using nutritional formulas with pre-digested foods. These powders include vitamins, minerals, and complete macronutrients, and are used to replace all or some of your meals.
The elemental diet or a semi-elemental diet is used for SIBO, Crohn’s disease, and eosinophilic esophagitis. I only recommend this diet short-term and with the guidance of your healthcare professional until you resolve your issues.
Reduce Stress & Optimize Sleep
Chronic stress and poor sleep can contribute to chronic inflammation and gut dysbiosis that may increase your risk for C. diff infections (6, 7, 8, 9). Reducing your stress levels and optimizing your sleep is vital for reducing inflammation, supporting your gut flora, and reducing your risk of infections. They also support your body while fighting and healing from C. diff or another infection.
Try to avoid stressful situations and people that bring stress into your life as much as possible. Instead of scrolling the news or social media all day, select a designated time for it. Say no to stressful situations. Try to avoid rush hour traffic if you can.
Of course, avoiding stressful situations completely is impossible. Learning better coping mechanisms and bringing your stress levels down is critical. I recommend meditation, breathwork, gratitude, guided relaxation, visualization, and prayer.
You may also benefit from journaling, spending time with supportive people, taking a relaxing bath, practicing positive affirmations, spending time in nature, and having regular me-time. Working with a therapist, counselor, spiritual counselor, or life coach can help you with tools that reduce stress and help to improve your mindset.
To optimize your sleep, I recommend that you go to bed and wake up around the same time every day. This will help to support your natural circadian rhythms or sleep-wake cycle. Avoid sugar, heavy foods, alcohol, electronics, and stress close to bedtime.
Try calm conversations, reading, relaxing music, crossword puzzles, journaling, meditation, or prayer as your bedtime is approaching. Support your sleep with a supportive mattress and pillow, comfortable bedding, and blackout curtains or sleep mask.

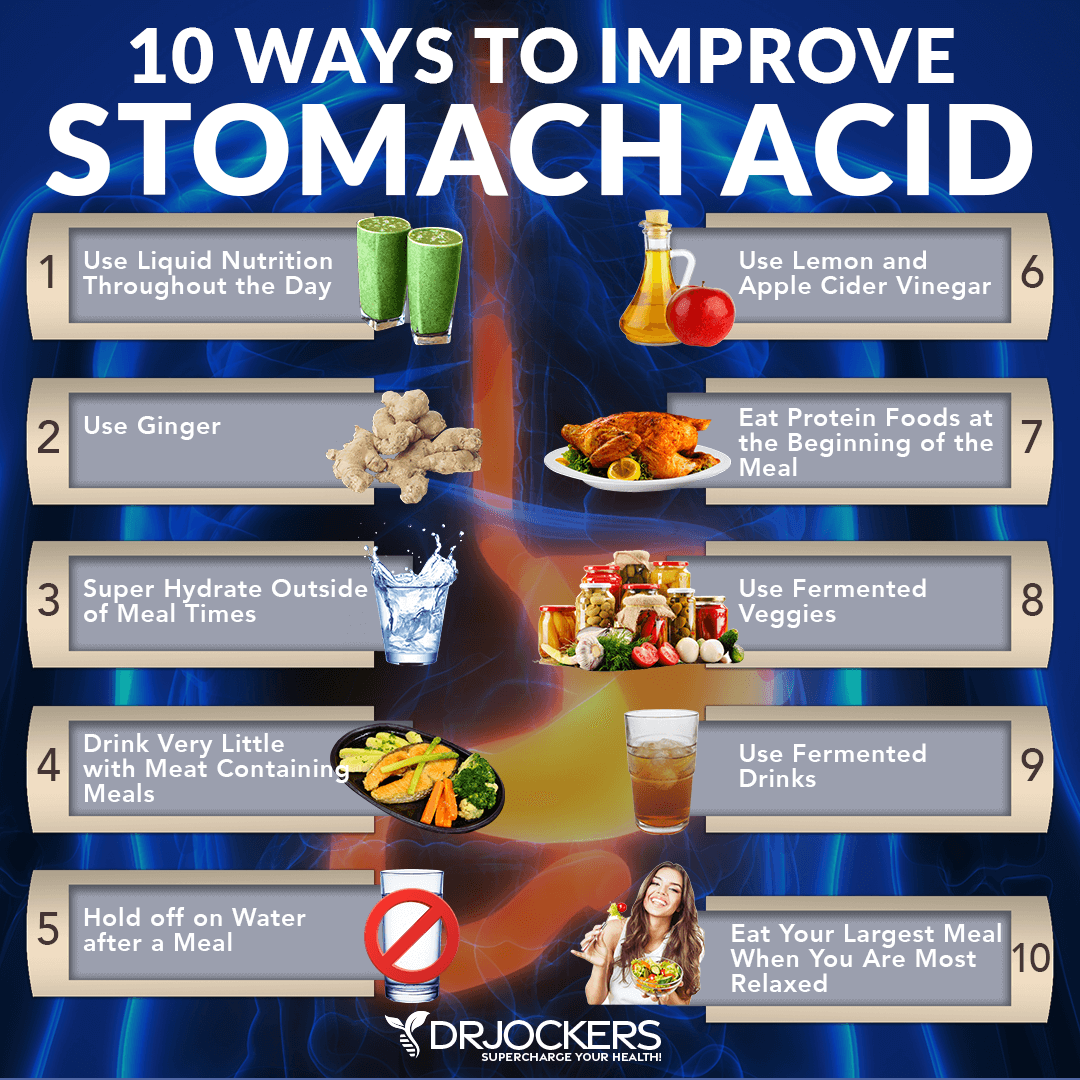
Stop PPI’s and Improve Stomach Acid Levels
Acid suppression medications can increase your risk of C. diff (3, 4, 5). I recommend that you stop using proton pump inhibitors and improve your stomach acid levels. To support your stomach acid levels, I recommend the following:
- Use Liquid Nutrition Throughout the Day: Try to make sure that at least half of your meals are in a liquid form, such as a protein shake or green smoothie. Protein shakes are pre-metabolized and very easy to digest, and do not depend upon HCL production. If you have low HCL, it may be helpful to drink one to two protein shakes daily to support amino acid absorption, reduce extra stress on your digestion, and support healthy stomach acid levels.
- Use Ginger: Ginger is one of the best things for improving digestive juices. I recommend drinking 2 to 3 cups of ginger tea each day. You can put ginger essential oil in water (2 to 3 drops in 8 oz. of water), juice a ½ inch of fresh ginger root in a green juice each day, and use ground ginger on your foods. You can also add fermented ginger to your diet, which is common in Asian dishes such as kimchi.
- Super Hydrate Outside of Meal Times: Good hydration can help activate bowel motility and push contents through the digestive system, which will reduce microbial fermentation and toxicity in the body. This can help to support your stomach acid levels.
- Drink Very Little With Meat Containing Meals: When you are eating meat or any sort of heavier food, you should stop drinking water or other liquids at least 30 minutes before the meal, except if you need to take a supplement with 2 ounces of water. Holding off water during these meals will reduce any potential dilution of the gastric juices and allow for better digestion.
- Hold Off On Water After a Meal: To allow for optimal digestion, I also recommend not drinking water or other liquids until at least 30 minutes after a meal. This allows for proper stomach acid activity, sterilization, and protein metabolism.
- Use Lemon and Apple Cider Vinegar: Squeezing fresh lemon or using lemon juice or apple cider vinegar on your meat and vegetables helps to pre-metabolize the food and support better digestion and nutrient absorption. You can either marinate foods in a lemon or ACV base or just add them as a dressing right before consuming them.
- Eat Protein Foods at the Beginning of the Meal: The stomach will begin churning out its stomach acid when you start eating, especially when consuming protein. While it’s culturally common to a salad before their protein dish, this is not great for your HCL production. It is a much better idea to eat your protein with the salad or vegetables instead of after.
- Use Fermented Veggies: Fermented foods such as sauerkraut, kimchi, pickles, pickled ginger, and other fermented vegetables all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions. I recommend using one of these with all of your heavier meals and especially any meal with protein.
- Use Fermented Drinks: Fermented drinks such as apple cider vinegar, coconut kefir, and kombucha offer anti-microbial benefits and help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Keeping H Pylori levels down is critical for the body to be able to produce enough stomach acid.
- Eat Your Largest Meal When You Are Most Relaxed: Your body needs to activate the parasympathetic nervous system to produce enough stomach acids. If you are busy and on the go, you will be in fight or flight sympathetic mode. If you struggle with low stomach acid, this fight or flight state will not allow your body to produce anywhere near enough. Relaxing before the meal is important to improve stomach acid production.
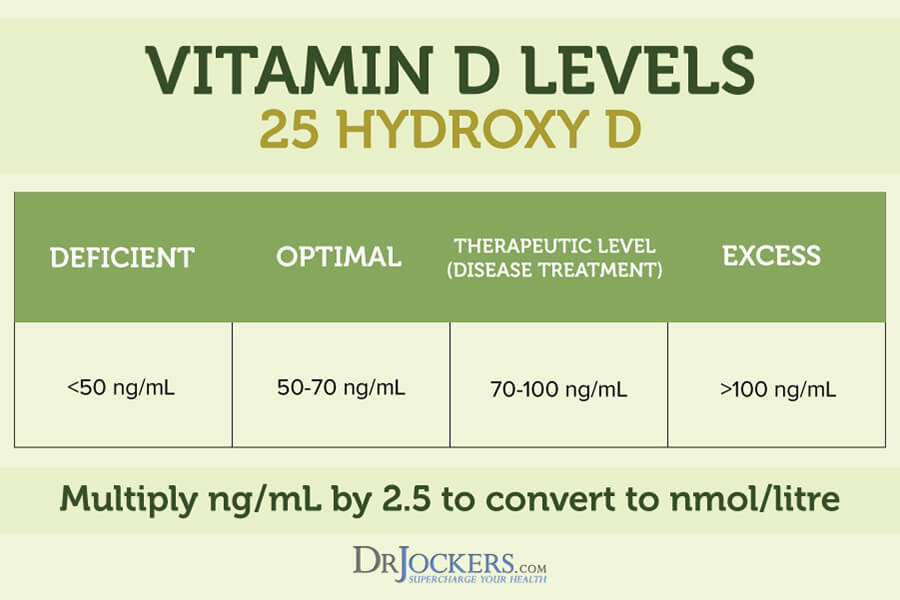
Optimize Vitamin D Levels
Having a deficiency in vitamin D can increase your risk of C. diff or compromise your recovery (12, 13). Optimizing your vitamin levels is critical. I recommend that you spend some time outside in the sun every day if there is sunshine and eat foods rich in vitamin D, including fatty fish, cod liver oil, egg yolk, and mushrooms.
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need to supplement to optimize their vitamin D levels. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
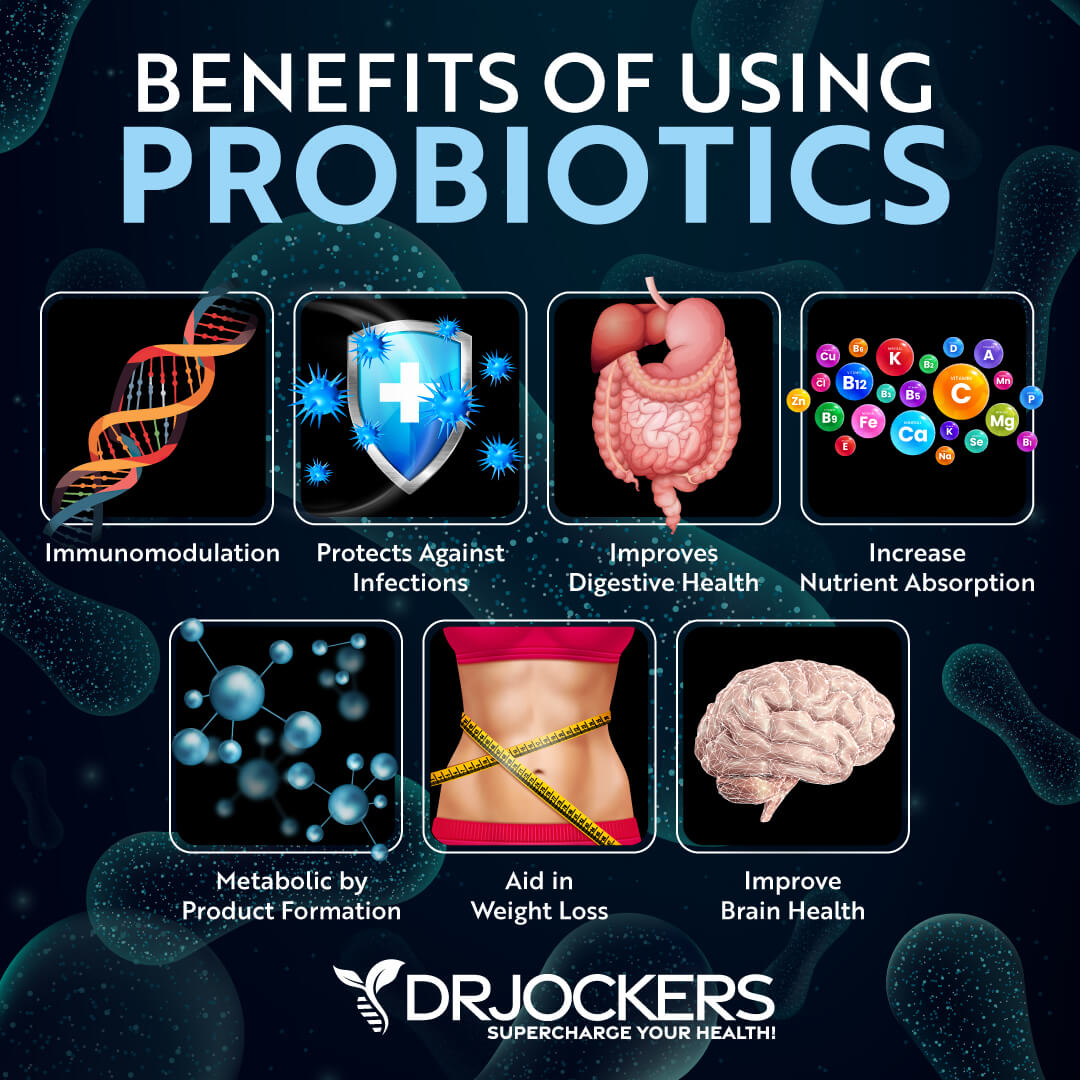
Use Probiotics
Gut dysbiosis and antibiotic use can increase your risk of a C. diff infection (6, 7, 8, 9). Probiotics may help. A 2018 study published in Current Opinions in Gastroenterology has found that probiotics may help to prevent C. diff infections (19). A 2019 review published in Cureus has found that probiotics may help to improve gut dysbiosis and may help to prevent and treat C. diff infections (20).
I recommend that you eat probiotic-rich foods, including sauerkraut, kimchi, fermented vegetable, coconut kefir, pickles, and kombucha. However, these probiotic foods are not enough. I also recommend a daily dose of high-quality probiotics.
There are different types of probiotics and probiotic supplements:
- Food-based Probiotics: Lactobacillus acidophilus La-14 is a common inhabitant of the human mouth, intestinal tract, urinary tract, and vagina. It is found in some traditional fermented milk (e.g., kefir) and is widely used in probiotic foods and supplements. L acidophilus has excellent adhesion to the gut lining. Bifidobacterium lactis is a strain with tremendous probiotic potential based upon its ability to survive the transit through the human gastrointestinal tract, adhere to epithelial cells, and proliferate. The Bifidobacterium longum B1-05 strain is well-accepted as safe for human consumption. It is resistant to low pH and bile salts and is well-suited to the intestinal environment.
- Probiotic Yeasts: Saccharomyces boulardii is a natural, non-pathogenic probiotic yeast. One of the main benefits of Saccharomyces boulardii is that it is resistant to stomach acids and antibiotics. It promotes immune and digestive health. There are many benefits to Saccharomyces boulardii. It improves gut motility to reduce constipation and supports bowel fluid balance to reduce diarrhea. Studies have shown that it can help to prevent and improve C. diff infections (16, 17, 18).
- Soil-Based, Spore-Forming Probiotics: Soil-based probiotics have the ability to form bacterial spores and are often used to treat gastrointestinal disorders. Spore-based strains have an innate resistance to the stressors of heat, light, stomach acid, and time. This ensures long-term viability and protects them against degradation so that they reach the lower GI tract intact and alive. Spore-forming probiotics are a promising alternative for people affected by recurring gut problems. For example, people with SIBO may not always tolerate other probiotics well, and those may even further trigger their issues, but soil-based probiotics can significantly benefit their health. They help to reinforce intestinal barrier integrity and reduce inflammation in the gut.
- Combination Probiotics: Combination probiotics blend different types of probiotics into one formula. For example, a combination probiotic blend may contain food-based lactobacillus and bifidobacterium probiotics, soil-based, spore-forming probiotics Bacillus subtilis and Bacillus coagulans, and beneficial yeast, Saccharomyces boulardii into one capsule. They often contain prebiotic inulin, which feeds and supports the strength of the probiotics in each capsule. This probiotic supports healthy immune system function, healthy gut function, and a healthy gastrointestinal tract.
Everyone tolerates different probiotics differently. I recommend that you give a trial run to each probiotic before you commit to one long-term. If you are a highly sensitive individual, I would recommend starting with a soil-based probiotic formula as those tend to be the most well-tolerated. For C. diff, probiotic yeast may be the best choice. If you feel better after the 7-day trial, then that is a sign that this particular probiotic is benefiting you, and if you feel worse, then it is not.
Never stay with one particular probiotic or brand for too long. Rotating probiotics helps to diversify your gut flora. Once you find the probiotics that are working well for you, it is a good idea to cycle probiotics every 1-3 months or so.
If you are only responding well to one type of probiotic, then stay on that and don’t worry about rotating. However, if you respond well to all three types of probiotics, then rotating between them or between combination probiotics can be very helpful.
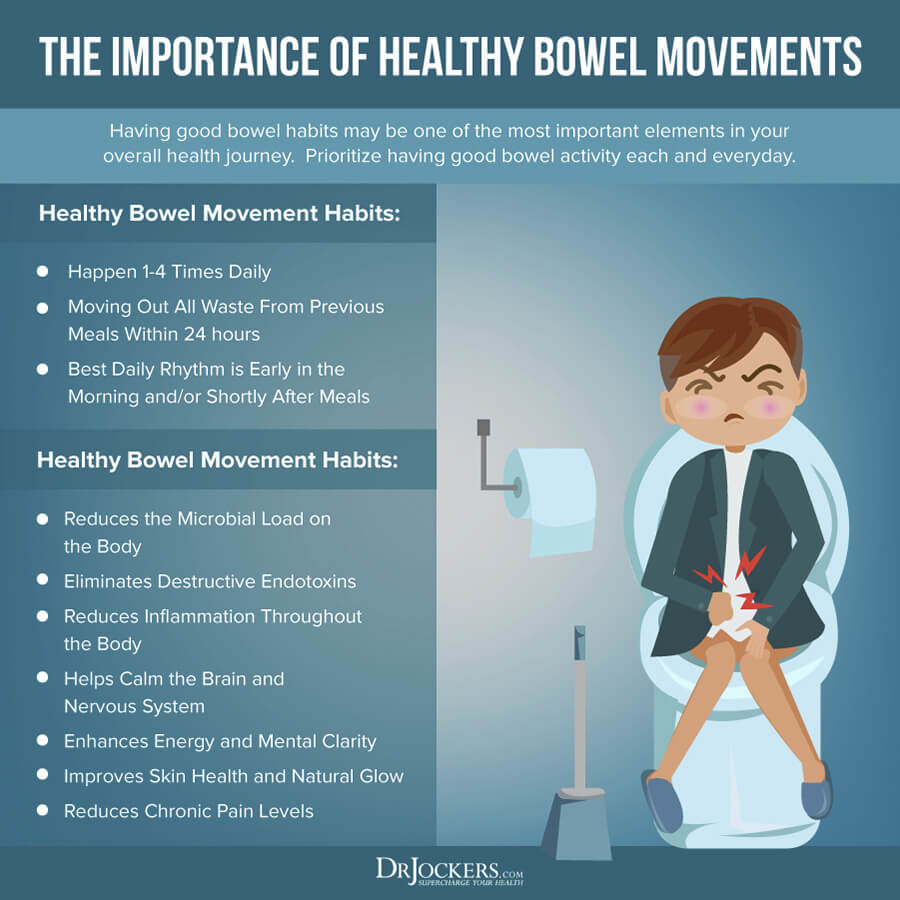
Improve Bowel Motility
I recommend improving your bowel motility to support your digestion and help remove pathogens and toxins through waste. One of the key things for bowel motility is proper hydration and electrolyte balance. I recommend that you start your day with 32 oz of water. Drink regularly throughout the day, at least ten glasses a day or more if you are working out a lot, sweating, sick, or simply thirsty.
Remember, feeling thirsty means that you are already dehydrated. You can prevent this by drinking regularly. You can set a reminder on your phone, use sticky notes, or add a new rubber band on your water bottle after every 8 oz of water you drank. For electrolyte balance, you may add a pinch of salt to your water, eat mineral-rich vegetables, and try an electrolyte balance powder.
Eating prebiotics and fiber may benefit bowel motility and your overall health, but not everyone’s body deals with it well. For some people, prebiotics and fiber are very helpful for digestion. For others, they may lead to problems, and too much can cause diarrhea or constipation. If you are on a LOW-FODMAP diet, for example, prebiotics and fiber are not right for you. Those on the carnivore diet also tend to avoid prebiotics. Know your body and experiment to find what works best for you. If prebiotics and fiber are triggering, reduce the amount of back off completely.
Taking magnesium supplements to support bowel motility and smooth bowel movements. You may want to try magnesium and oxygen-based colon cleanser. It improves bowel motility, prevents and relieves constipation, improves your microbiome balance, and removes toxins from your colon.
Lastly, you may benefit from supporting your vagal nerve activity to improve bowel motility and digestion. Some strategies that help to improve your vagal tone include practicing gratitude and laughter, getting good sleep, meditation, prayer, deep breathing, stimulating your palatal muscles, social connections, cold exposure, exercise and movement, and following an anti-inflammatory nutrition plan.
Optimize Zinc Levels
As you already know, zinc deficiency can increase your risk of a C. diff infection (14, 15). Research also suggests that optimizing your zinc levels may help.
I recommend eating foods that are rich in zinc, including oysters, red meat, poultry, eggs, chickpeas, nuts, and seeds. Dietary sources of zinc are usually not enough, so I also recommend daily zinc supplementation to optimize your health.
As you know, zinc and copper compete against each other as antagonists to regulate physiological pathways. A proper balance between the two is vital for a healthy gut. I recommend checking your plasma zinc and serum copper levels and their balance. I recommend a Comprehensive Blood Analysis to check your zinc levels and zinc:copper ratio. The proper zinc:copper ratio should be 1:8, the normal range for zinc is 150 – 240µg/gram, and the serum copper ratio should be between 1 and 1.2.
Use Anti-Microbial Herbs and Oils
Using certain anti-microbial herbs and oils may also help to support your health. Here is what I recommend:
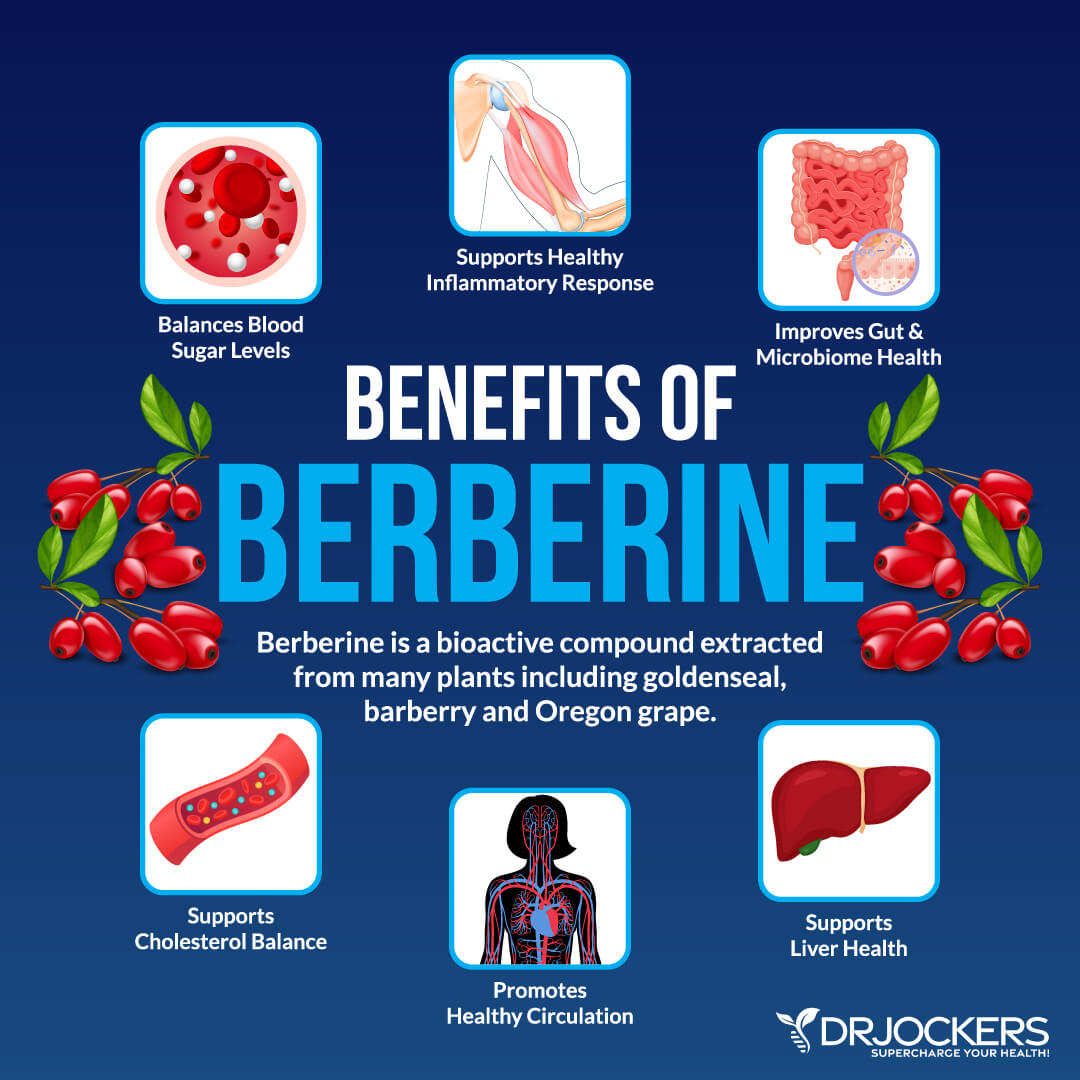
Berberine
Berberine is a bioactive compound found in some plants. It is often recommended for inflammation, obesity, diabetes, and other health issues. A 2015 animal study has found that berberine may prevent the recurrence of C. diff (21).
A 2017 preliminary study published in the Asian Journal of Pharmaceutical and Clinical Research has also found that berberine may be effective against C. diff (22). I recommend supplementing with berberine regularly.
Oil of Oregano
Oil of oregano is a powerful herbal remedy that’s often used for infections, including gut infections and respiratory infections. A 2017 animal study published in Frontiers in Microbiology has found that the oil of oregano may have protective benefits against gut dysbiosis and C. diff infections (23).
A 2014 study published in the International Journal of Molecular Sciences has found that the oil of oregano may reduce toxin production by C. diff (24). I recommend oil of oregano if you are dealing with C. diff, other gut infections, or acute gut symptoms, like diarrhea or traveler’s sickness.

Lauric Acid
Lauric acid is a saturated fat commonly found in coconut oil and palm kernel oil. It is a powerful remedy for viral and other microbial infections. A 2018 in vitro study published in Frontiers in Microbiology has found that lauric acid may decrease inflammation from C. diff (25). I recommend trying lauric acid if you are dealing with C. diff or other gut infections.
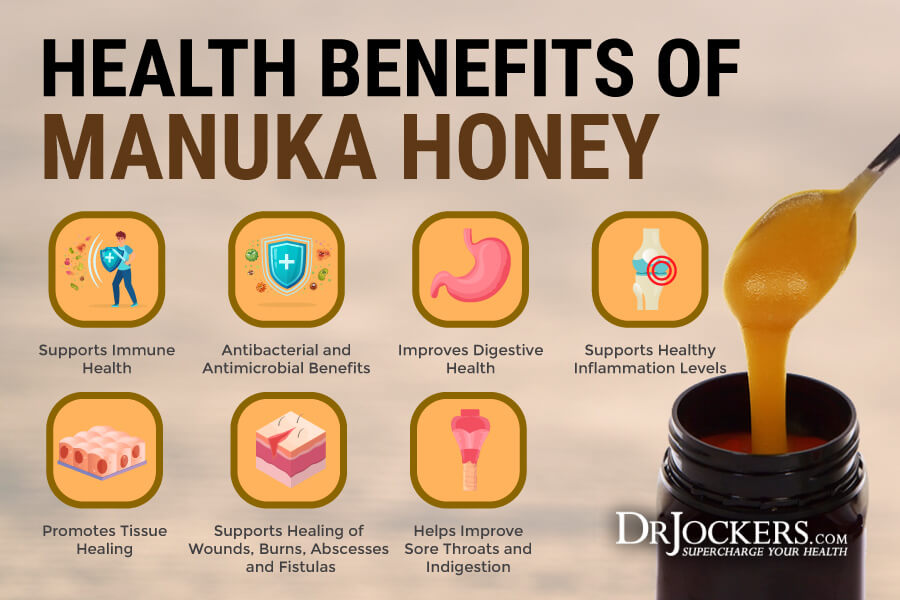
Manuka Honey
Manuka honey is delicious honey that offers antimicrobial and anti-inflammatory benefits. A 2017 in vitro study published in the European Journal of Microbiology and Infectious Diseases found that manuka honey has antimicrobial effects on C. diff infections and supports recovery (26). I recommend incorporating manuka honey into your daily diet.
Consider Fecal Microbiota Transplant Surgery
Fecal microbiota transplant surgery or FMT refers to transferring stool from a healthy donor into the gastrointestinal tract. It is used to treat recurrent C. diff infections and sometimes may be used for other chronic gastrointestinal infections and issues.
A 2019 randomized controlled trial meta-analysis published in PLoS One has found that fecal microbiota transplant may be a promising treatment option and reduce reinfection in C. diff (27). A 2020 study published in Gastroenterology has also found that fecal microbiota transplant may help to treat recurrent C. diff infections (28). If you decide that fecal microbiota transplant surgery is right for you, it’s critical that you work with a healthcare professional who is experienced in performing this procedure. If you are interested in learning more about FMT, check out the infographic below and read this great article from The Scientist.
Final Thoughts
C diff is a bacterium that can cause severe diarrhea and clostridium difficile colitis. There are about half a million C. diff infections each year in the United States with high reinfection rates. I recommend that you try my natural support strategies to reduce your risks and improve your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!