 Mast Cell Activation Syndrome: Symptoms and Solutions
Mast Cell Activation Syndrome: Symptoms and Solutions
Mast Cell Activation Syndrome (MCAS) is a complex and chronic immune disorder. It affects multiple systems in the body including the skin, gastrointestinal tract, heart, respiratory, and neurologic systems. Unfortunately, most people with MCAS suffer for months, or even years, without a diagnosis due to the lack of awareness within the medical community.
Mast cells are immune cells that have the central role of protecting the body. When these cells are overactive and release too many mediators, this can be harmful to the body. MCAS may play a role in cancer, stroke, Lyme disease, and many other serious conditions.
The first step to improving symptoms of MCAS is to identify and address a person’s individual triggers. This may include certain foods, mold, chemicals, and other toxins. A low histamine and/or low FODMAP diet may help to improve symptoms of MCAS. In this article, I will also discuss targeted supplements to support the immune system.

What are Mast Cells?
Mast cells were discovered in 1878 by Nobel Prize winner and immunologist Paul Ehrlich. Ehrlich discovered these small immune cells which reside in the tissues and are mediators of allergic, inflammatory, and autoimmune conditions.
Mast cells are involved in both the innate and adaptive immune systems. They are the body’s first line of defense against pathogens and form barriers against foreign substances entering the body.
Mast cells are found in most tissues of the body. They are abundant in mucosal surfaces that are in close contact with the external environment, such as our skin, respiratory system, and gastrointestinal system (1).
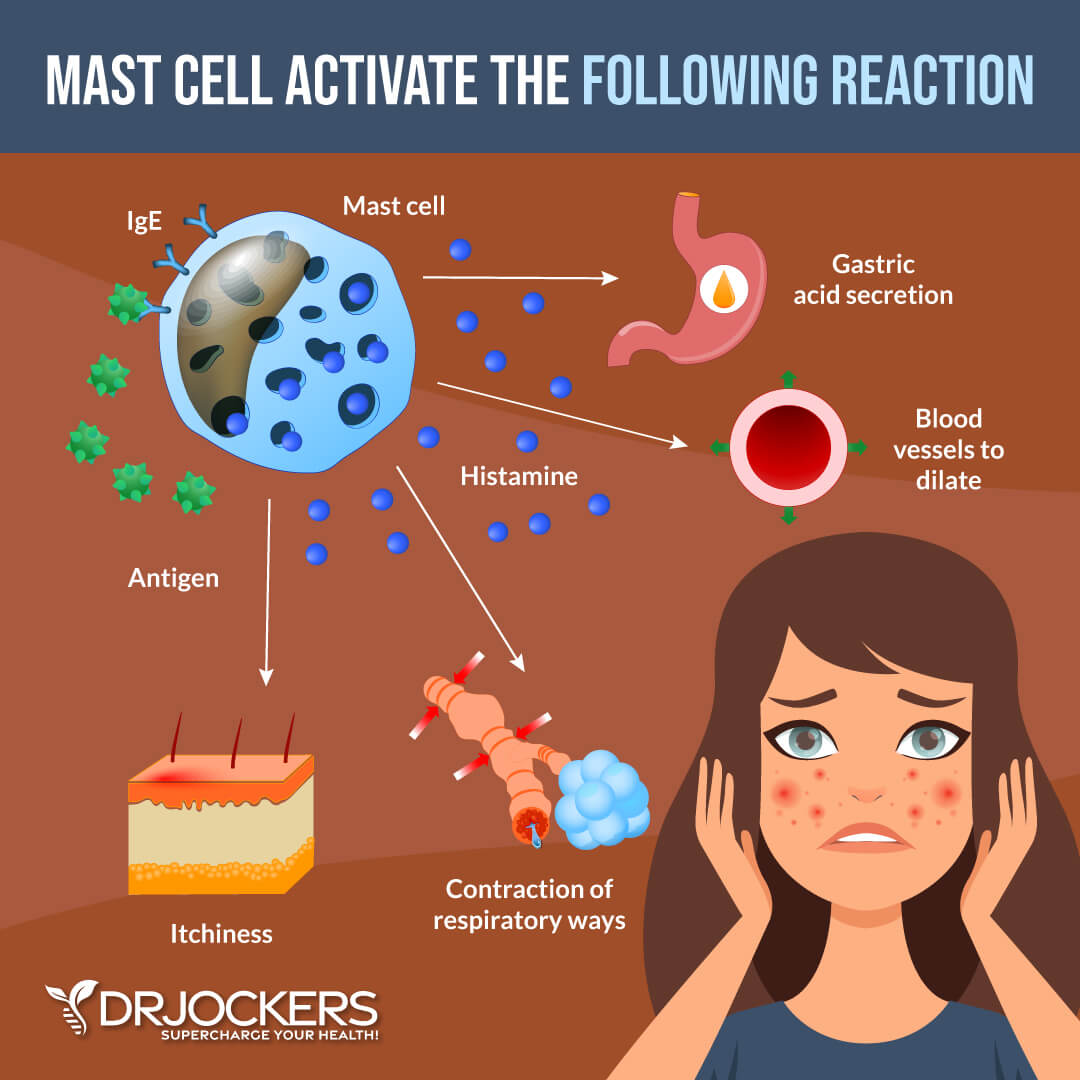
When activated, mast cells produce many chemical mediators. These include histamine, leukotrienes, heparin, cytokines, phospholipases, tryptase, chymase, chemokines, growth factors, and cholinesterase. These mediators are released into the surrounding tissue. This leads to swelling and inflammation, which are necessary for healing to occur.
While generally associated with an allergic response, mast cells are also involved in the regulation of many other functions in the body. These include immune tolerance, innate immunity, wound healing, and angiogenesis (formation of new blood vessels).

MCAD and MCAS
Mast Cell Activation Disorder or Disease (MCAD) is an umbrella term for the realm of diseases of the mast cell. There are three types of MCAD: primary, secondary, and idiopathic (2). Primary MCAD includes mastocytosis, a rare disease characterized by an overgrowth of mast cells with inappropriate mast cell activation.
There are two principal types of mastocytosis, cutaneous (limited to the skin) and systemic (throughout the body). More common mast cell disorders include allergies, urticaria, angioedema, and anaphylaxis.
Secondary MCAD is the reactive form of MCAD. This occurs in allergies, chronic inflammatory diseases, neoplastic disorders, physical urticarias, and chronic autoimmune urticaria (3). With secondary MCAD, mast cells are produced normally and can be increased in response to an underlying inflammatory process.
Mast Cells and MCAS
Idiopathic MCAS is a type of MCAD that is a more nebulous activation of the mast cells. It is not caused by an abnormally large amount of mast cells, but rather a normal amount of mast cells that are overactive and malfunctioning.
When your body is exposed to a perceived threat, the overactive mast cells secrete massive amounts of chemical mediators from the cytoplasm of the cells. This cellular process is called degranulation.
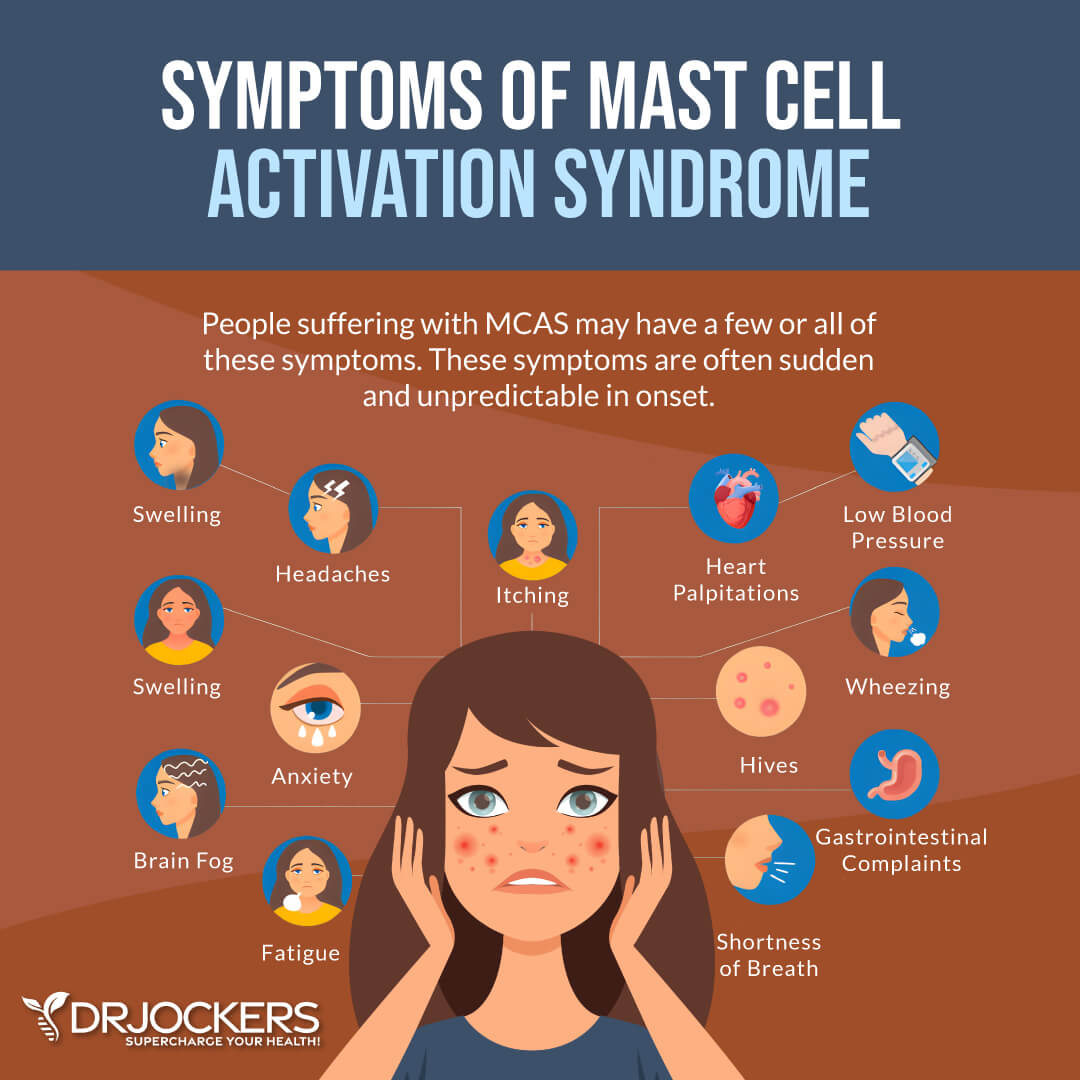
MCAS occurs when degranulation occurs too much and too often. Chronic release of chemical mediators triggers a negative immune response rather than a protective response. This can lead to chronic, multisystem inflammation. MCAS most commonly affects women.
Common Symptoms of MCAS
MCAS can affect every system in the body and cause a large array of possible symptoms (4). Common symptoms of MCAS divided by body system include:
- Constitutional: fatigue, malaise, chronic fatigue syndrome; flushing pr feels cold much of the time, chemical and/or physical environmental sensitivities, sweats, increased or decreased appetite
- Cardiovascular: pulse and blood pressure variability (low blood pressure and rapid pulse are common), palpitations, tachycardia, vascular permeability (inflammation and swelling), lightheadedness
- Respiratory: wheezing, shortness of breath, cough, sinusitis, rhinitis, increased mucus production, asthma-like symptoms, runny nose
- Neurological: headaches, irritability, anxiety, depression, brain fog, difficulty concentrating, vertigo, tingling, tremors, tics
- Psychological: anger, anxiety, depression, ADHD, PTSD, cognitive dysfunction, insomnia and other sleep issues
- Gastrointestinal: reflux, nausea, diarrhea, constipation, alternating diarrhea and constipation, vomiting, abdominal cramping, bloating
- Dermatological: rashes, itching, swelling, flushing, hives
- Musculoskeletal: joint pain, fibromyalgia-type pain, arthritis, joint hypermobility
- Skeletal: osteopenia and osteoporosis, scoliosis
- Genitourinary: pain and irritation in the urinary tract and/or genitals, urinary frequency or hesitancy
Diagnosing MCAS
There are no definitive tests for MCAS. Mast cells release over 200 mediators, and there are less than ten of these mediators that are specific to mast cells and can be measured clinically.
Serum tryptase, the most abundant protein in mast cells, can be helpful in diagnosing mastocytosis (4). With mastocytosis, tryptase levels may be double or more than the upper limit of normal. Mastocytosis is confirmed with a bone marrow biopsy. For MCAS, tryptase is usually normal, or slightly abnormal, and bone marrow biopsies are usually unrevealing.
In addition to tryptase, serum chromogranin A and plasma prostaglandin D2, histamine, leukotriene, and heparin can be helpful in diagnosing MCAS (5). In the urine, the metabolites of prostaglandin D2 and histamine and a molecule called leukotriene E4 can be measured. It is important that most of these be chilled for reliability exemplifying the importance of working with a knowledgeable practitioner.
In addition to increased levels of mediators, proposed diagnostic criteria includes 1) episodic multisystem symptoms consistent with mast cell mediator release; 2) clinical improvement with H1 and H2-receptor antagonists, anti-leukotriene medications, or mast cell stabilizing agents; and 3) no evidence of a primary or secondary MCAD (3).

How Does MCAS Differ from Histamine Intolerance?
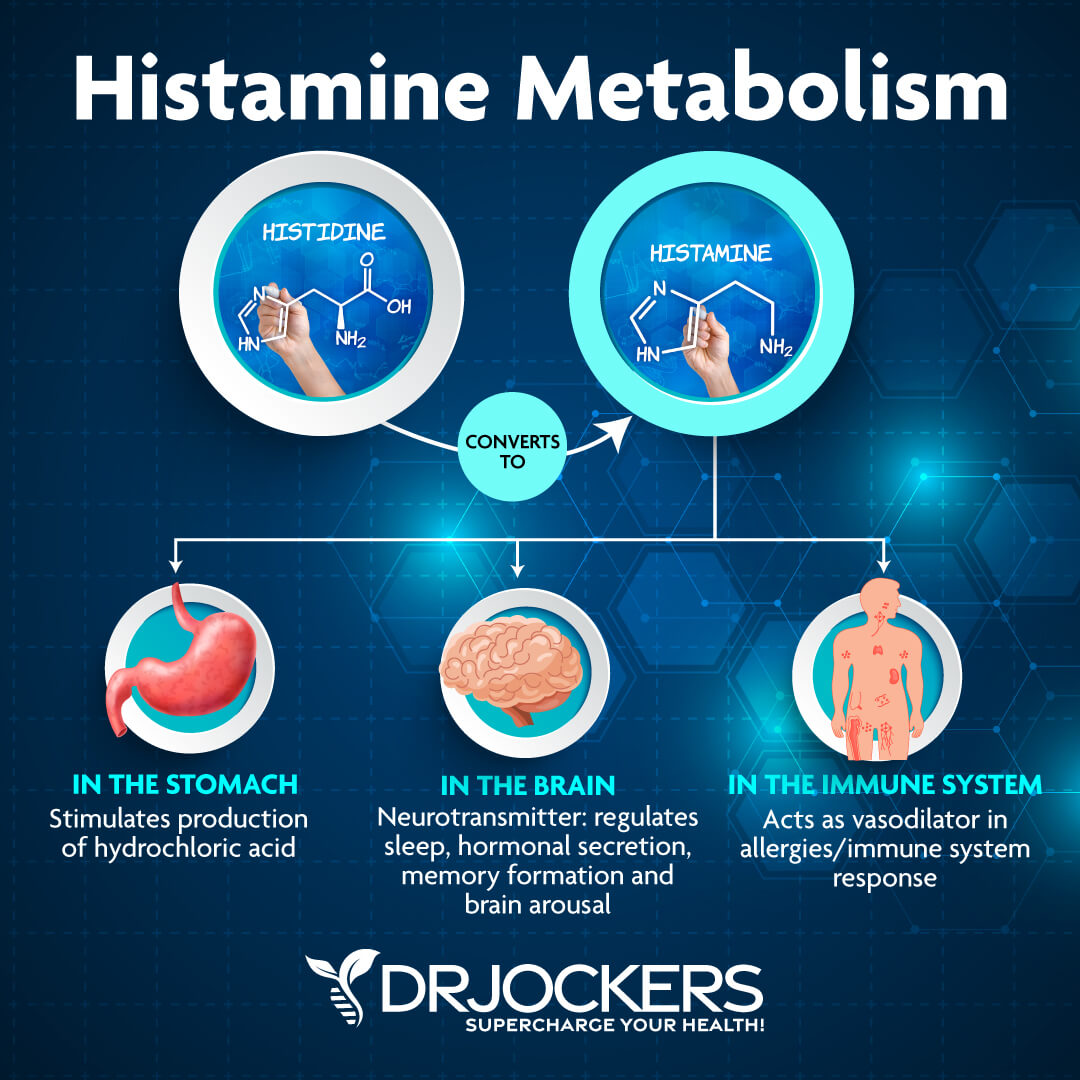
Histamine intolerance and MCAS are related conditions. Histamine is an amine that is produced by your cells and found in foods. It is an inflammatory molecule that helps regulate immunity. As part of the immune response, histamine is produced by basophils and by mast cells found in connective tissue.
Most people with MCAS have an exaggerated sensitivity to histamines, but not everyone who is histamine intolerant has MCAS. Instead, there is a spectrum from histamine intolerance to MCAS with symptoms ranging from mild to severe.
An individual with histamine intolerance has an exaggerated reaction to high histamine foods or foods that produce histamine. The causes of this exaggerated reaction could be insufficient DAO enzyme production (needed for proper histamine metabolism) or elevated histamine levels.
With histamine intolerance, a person will notice improvement with a low histamine diet and supportive supplements. A person with MCAS may still be very sensitive even with diet, supplement, and lifestyle strategies. Additionally, MCAS is a potentially more debilitating condition than histamine intolerance affecting multiple organ systems. For more information on histamine intolerance, check out this article.
Triggers of MCAS
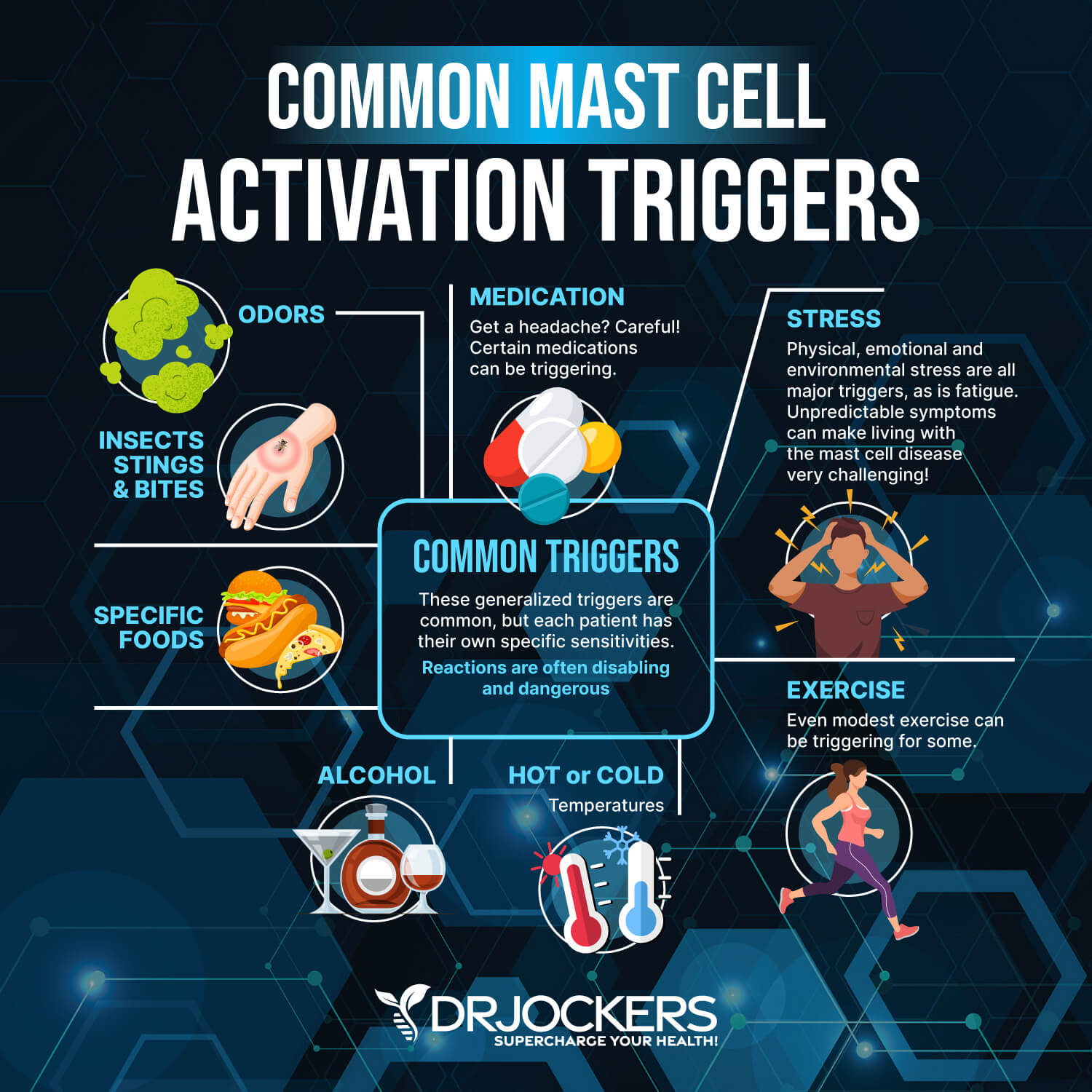
People with MCAS are more sensitive to toxins and environmental changes. Antigens and toxins overwhelm the mast cells and exceed the ability of mast cells to respond.
There are a number of antigens or toxins that can trigger MCAS. These include mold, chemicals, parasites, bacterial infections, allergens, viruses, heavy metals, and toxins. Stress (mental, physical, and emotional), heat or cold, hormonal changes, and excessive exercise may also trigger an overreaction of mast cells.

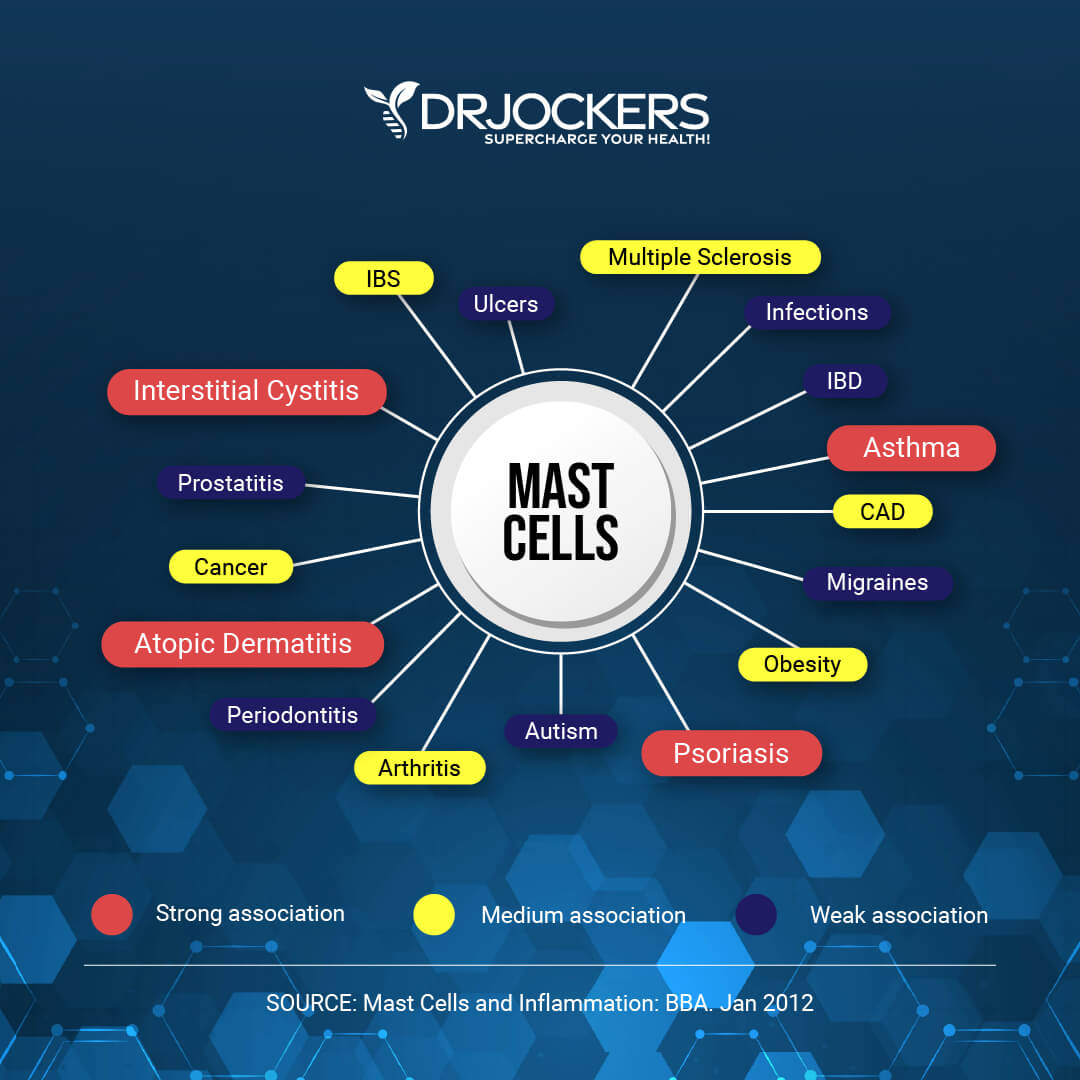
Conditions Linked to MCAS
Mast cell activation is linked to certain cancers, cardiovascular diseases, connective tissue disorders, inflammation, allergies, asthma, irritable bowel syndrome, skin conditions, and autoimmune diseases (5). Mast cells and inflammation of the brain are linked to mental health conditions, including depression and anxiety.
Let’s look at how mast cells play a role in certain conditions:
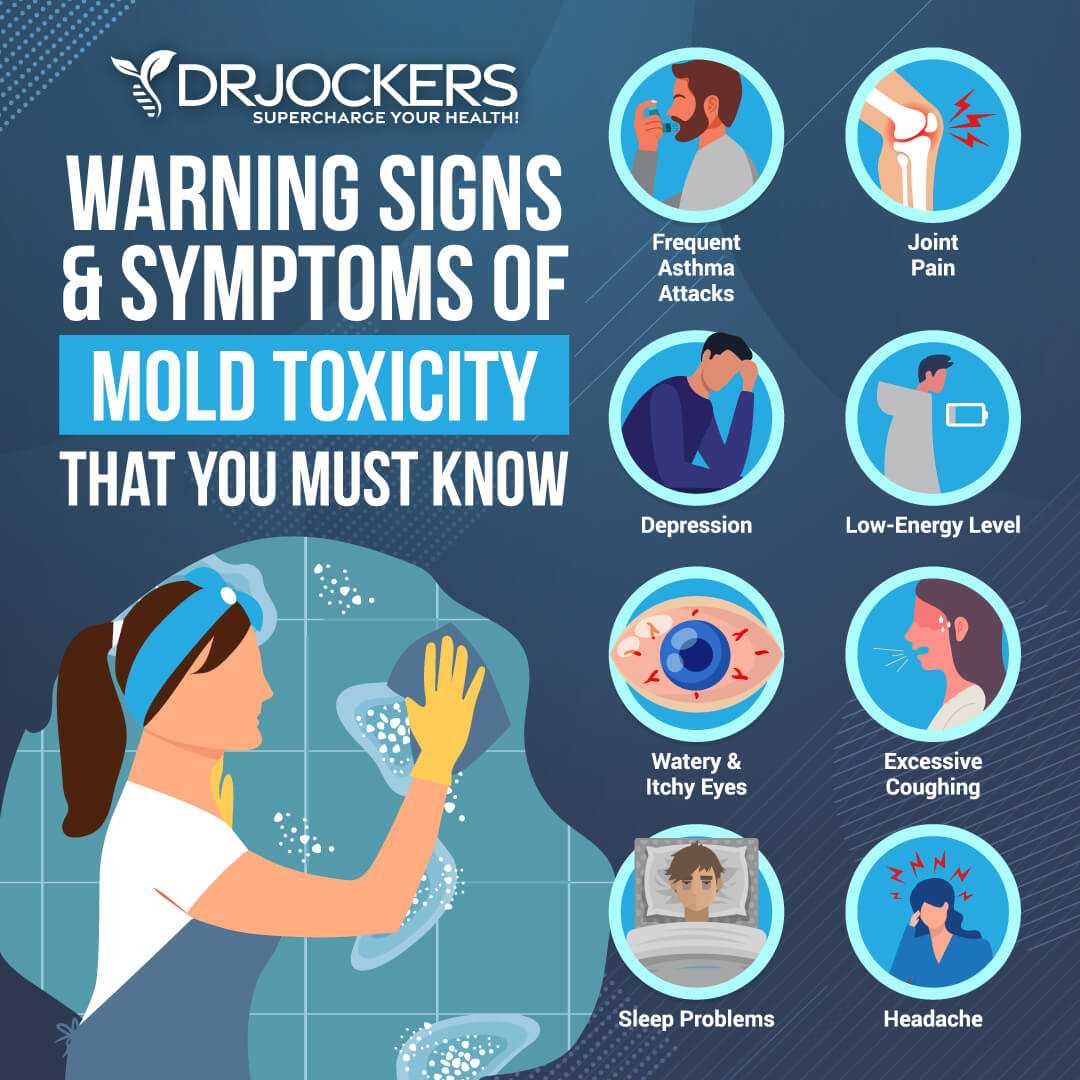
Mold Toxicity
An inflammatory response to mold exposure can be a driver of MCAS. If you have MCAS, it is important to check for mold exposure and remove yourself from any water damaged buildings.
Mold toxicity occurs when mycotoxins produced by mold lead to a chronic inflammatory immune response. This can be very damaging to the body. To test for mold toxicity, you can do a Mycotoxin Test. This urine test screens for seven different mycotoxins from four species of mold.
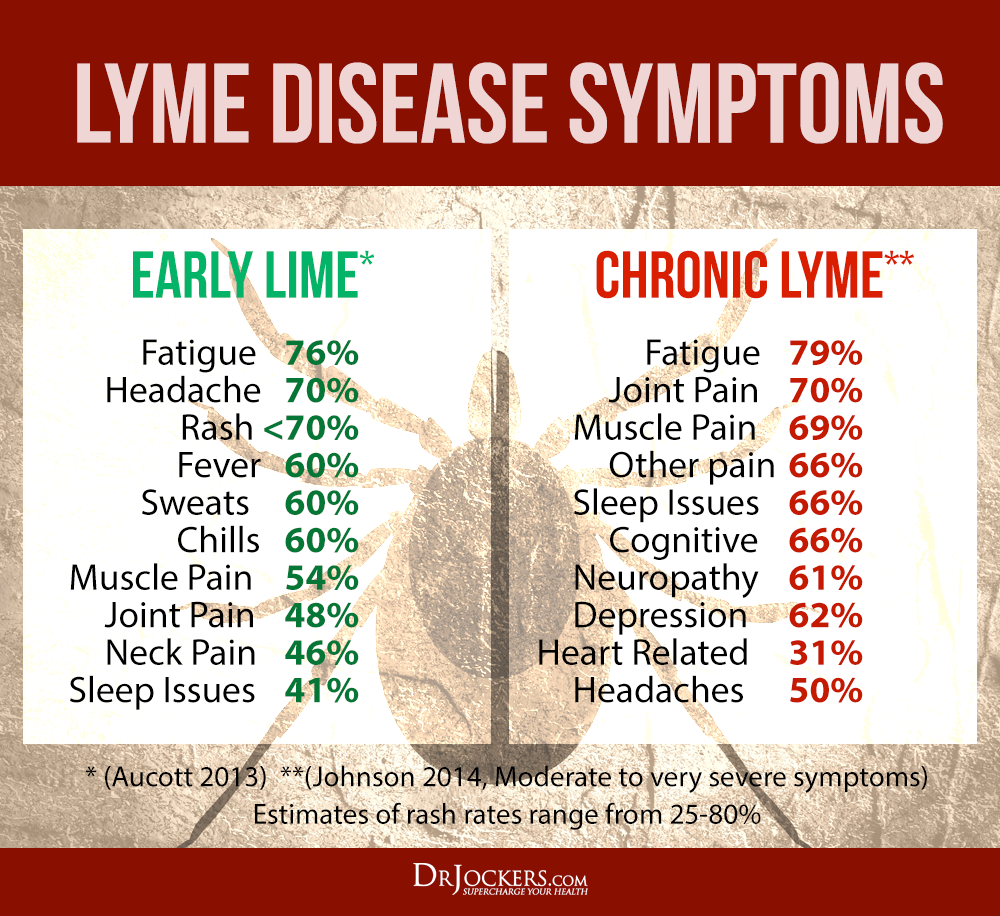
Lyme Disease
Lyme disease is an infectious disease caused by four main species of Borrelia bacteria. It is transmitted by the bite of an infected tick. Lyme disease, as with other infections, can cause mast cells to react and secrete proinflammatory cytokines (6).
There are a number of symptoms associated with Lyme disease, many of which are also common with MCAS. Lyme disease can be very difficult to accurately diagnose. To test for Lyme disease, the Igenex Lyme Test is a sensitive and reliable antibody screening that also screens for the DNA of Borrelia.
Lyme disease can be very challenging to overcome. However, you can find effective natural strategies here.
MTHFR Gene Mutations
Methylation is one of the most essential metabolic functions in the body. It is dependent upon a variety of enzymes that transfer methyl groups onto proteins, amino acids, DNA, and enzymes in every cell and tissue. It helps to regulate healing, cellular energy, genetic expression of DNA, liver detoxification, immunity, and neurology. This article explains the role of methylation in human health.
Methylation one of the most important pathways through which the body breaks down histamine. The most common genetic variant affecting methylation is the methylenetetrahydrofolate reductase (MTHFR) gene.
If methylation is not working well, there are not enough methyl groups to bind to a receptor site on histamine. Histamine is not broken down, and high levels of histamine can accumulate in the body. This causes histamine overload and results in symptoms associated with histamine intolerance and MCAS.

Ehlers-Danlos Syndrome
Mast cells are found in connective tissues throughout the body. Researchers have found that dysregulation of mast cells may play a role in Ehlers-Danlos Syndrome (EDS) (7).
EHS is a group of complex and multisystem connective tissue disorders. They are caused by varying genetic defects primarily in the structure, production, and/or processing of collagen. There are 13 subtypes of EDS, each with a specific genetic basis and protein involvement.
EDS mostly affects the joints and skin. An unusually large range of joint movement (hypermobility) occurs in most forms of EDS. Loose joints are unstable and prone to dislocation and chronic pain. Soft, velvety skin that is highly elastic and fragile, and easily bruised, is also common. Bone, gastrointestinal, eye, and heart issues are also common with EDS.

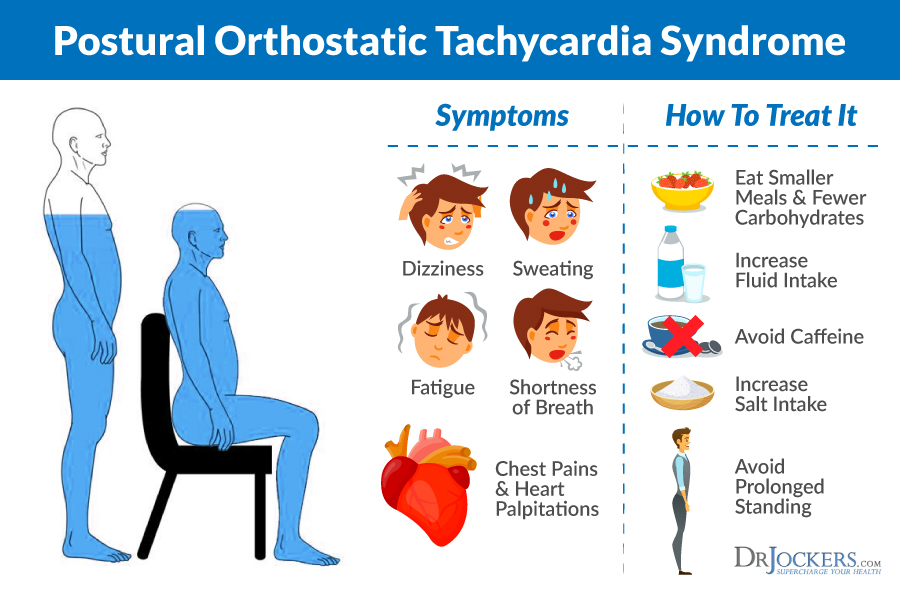
POTS
Postural Tachycardia Syndrome (POTS) is associated with MCAS (8). POTS is a condition that affects the autonomic nervous system and alters blood flow throughout the body. A person with POTS has an increased heart rate and dizziness or lightheadedness when standing.
When a person also experiences flushing, MCAS should be considered. For more information on POTS and strategies to improve this condition, check out this article.
Neuroinflammatory Conditions and Mast Cells
Mast cells are in the central nervous system where they contribute to normal behavioral development and functioning (9). They have also been linked to numerous neuroinflammatory conditions of the central nervous system.
These include multiple sclerosis (MS), traumatic brain injury, Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, neuropathic pain, migraines, depression, autism, fibromyalgia, and stroke.
Cancer
There is growing research on the relationship between mast cells and cancer (10). Researchers have found a significant increase in the prevalence of melanoma and cancers of the breast, cervix, ovaries, lungs, and thyroid in people with MCAS (11). Mast cells can be directly activated by cancer cells.
Mast cells appear to have a dual role in cancer. They can infiltrate tumors and function to promote or restrict tumor growth and invasiveness. By releasing chemokines and initiating an immune response, mast cells may lead to tumor eradication.
However, mast cells may release other mediators that support tumor malignancy. Regulating mast cell activation, recruitment, and type of released mediators at the tumor site can be useful for managing and controlling tumor growth (12).
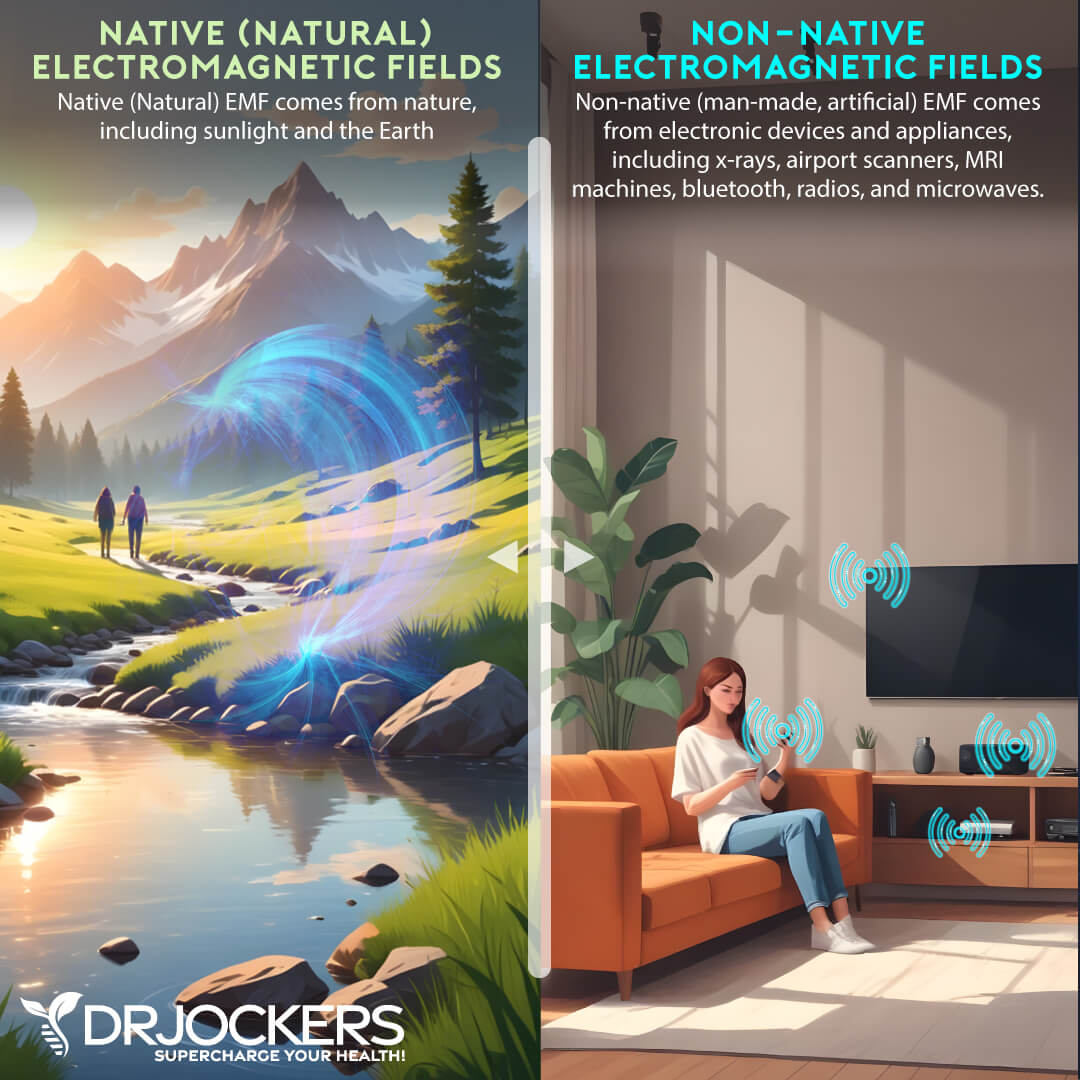
EMF Sensitivity
Sensitivity to electromagnetic fields (EMFs) can play a role in activating mast cells. There are a broad range of symptoms associated with EMF sensitivities. These include cognitive issues, insomnia, fatigue, dizziness, joint pain, palpitations, and ringing in the ears.
It is important to reduce the amount of exposure to non-native EMF and to increase exposure to natural forms of EMF available by being outside grounded on the Earth and getting quality sun exposure. For more information on the dangers of EMFs along with ways to protect yourself from exposure, see this article.
Natural Strategies to Improve MCAS
MCAS is a challenging condition to deal with and each individual suffering from this will need their own specific health plan. There are several things that are common and effective for the vast majority of people dealing with MCAS. While these aren’t all FDA-approved to prevent, mitigate, treat, or cure MCAS, many have found these strategies to be extremely helpful.
Some individuals will need to avoid all higher histamine foods while others can tolerate some of them. Experimentation will be key to trying to understand what your body tolerates and what it cannot and the supplements that seem to offer the most support.
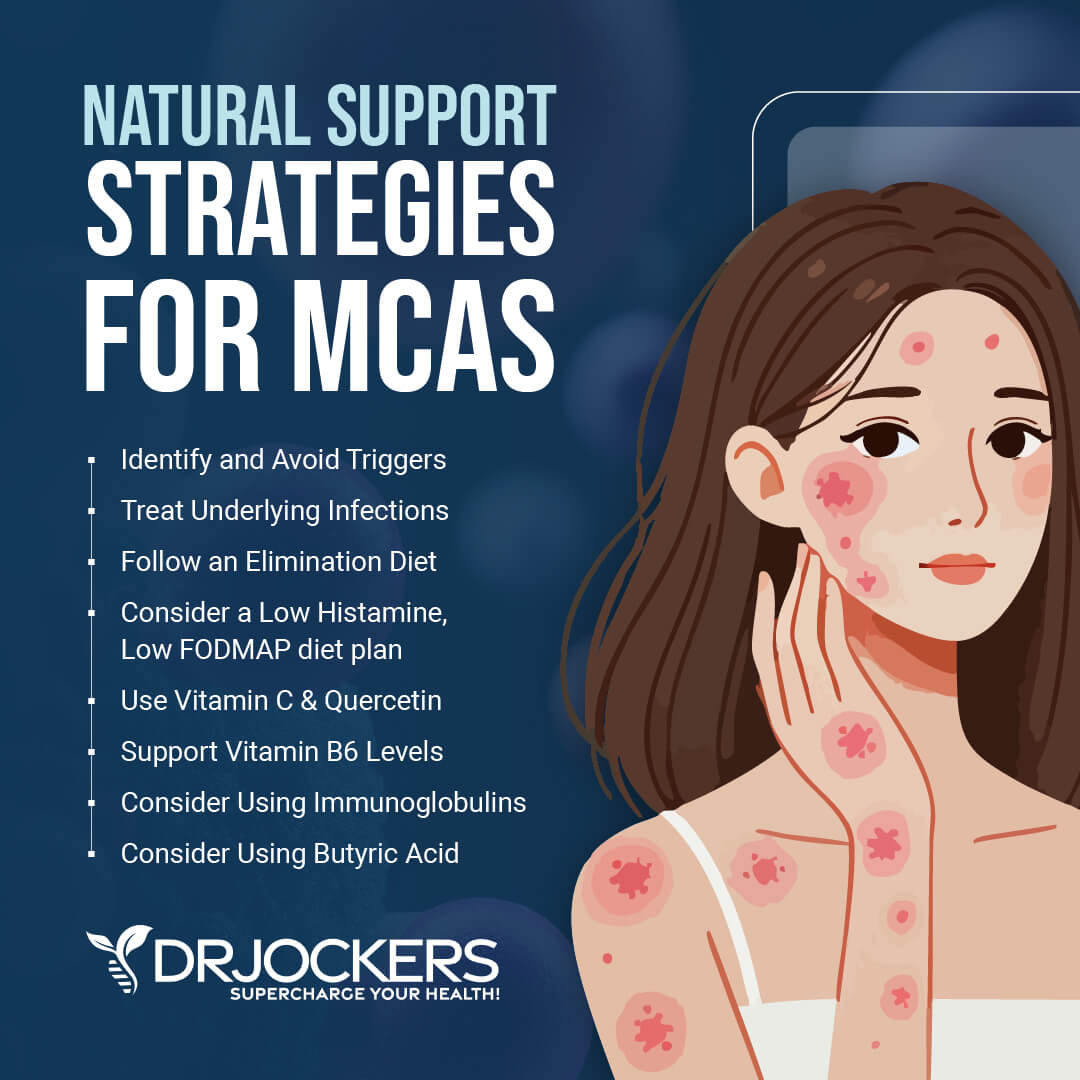
1. Identify and Avoid Triggers
The first step to improving MCAS is to identify and avoid a person’s specific triggers. As you can see from the list above, there are a variety of things that may be triggering MCAS. It can take time to identify and address these issues.
However, as a person’s symptoms improve, tolerance for these triggers may also improve.
2. Use Targeted Supplementation Vitamin C
One of the top supplements for MCAS is vitamin C. Studies show that vitamin C can relieve most of the symptoms of diseases that involve the activation of mast cells (13).
Vitamin C is a powerful antioxidant that is critical for supporting the immune system. It reduces histamine-mediated inflammation and plays an important role in the synthesis of collagen.
Other natural antihistamines include stinging nettle, butterbur, bromelain, probiotics, and astragalus. Allergy Defense has many of these along with N-Acetyl Cysteine. This combination of bioflavonoids, micronutrients, proteolytic enzymes, and herbs is a powerful supplement for addressing immune hypersensitivity.

Quercetin
Mast cell stabilizers prevent degranulation and stabilize the cell. This prevents the release of histamines.
One of the most powerful mast cell stabilizers is quercetin. Quercetin is a natural antihistamine. It is a powerful antioxidant and the “king of flavonoids.”
Quercetin works best when it is combined with vitamin C, zinc and resveratrol. The synergy of these compounds helps to reduce excess histamine, mast cell activation and balance the immune system.
Immunocharge contains quercetin along with vitamin C, resveratrol, zinc, NAC, vitamin D3, magnesium and vitamin K2. This powerful blend works synergistically to improve the inflammatory response and down regulate mast cell activation (14).
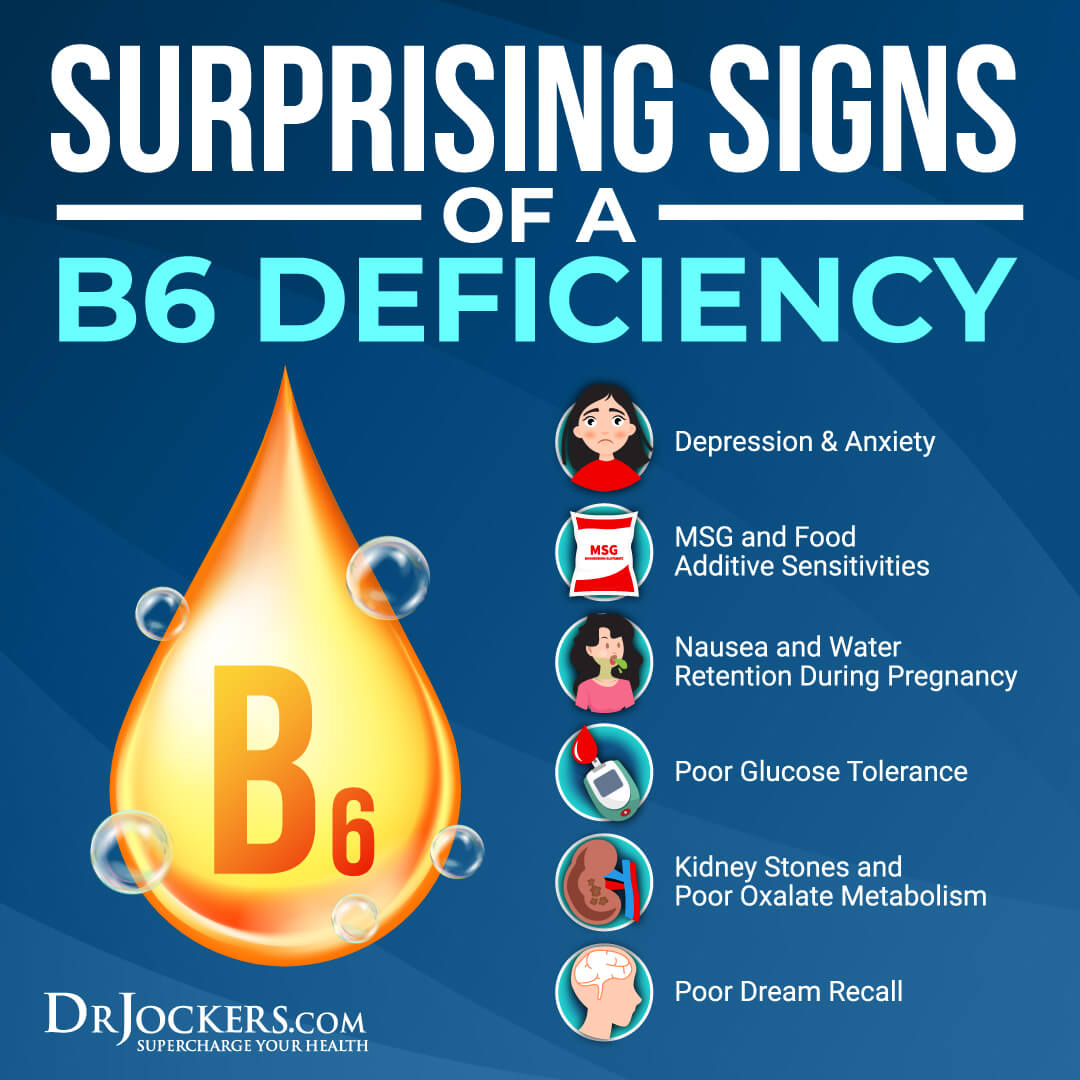
 Vitamin B6
Vitamin B6
Vitamin B6 is critical for your central nervous system, cellular function, and metabolism. It helps to make neurotransmitters, including dopamine and serotonin. It also helps metabolize protein, fats, and carbohydrates from food and turn them into energy.
It helps create new blood cells and keep your cell healthy. It also plays an important role in over 100 enzyme reactions. It is essential for brain development during pregnancy and infancy. It also supports the immune system.
Vitamin B6 is a key cofactor that enables DAO to degrade histamine. Without adequate DAO, histamine levels can increase, leading to symptoms of histamine intolerance or MCAS. B6 Power is a bioactive form of vitamin B6 (P-5-P) that is more readily used by the body than other forms of B6.
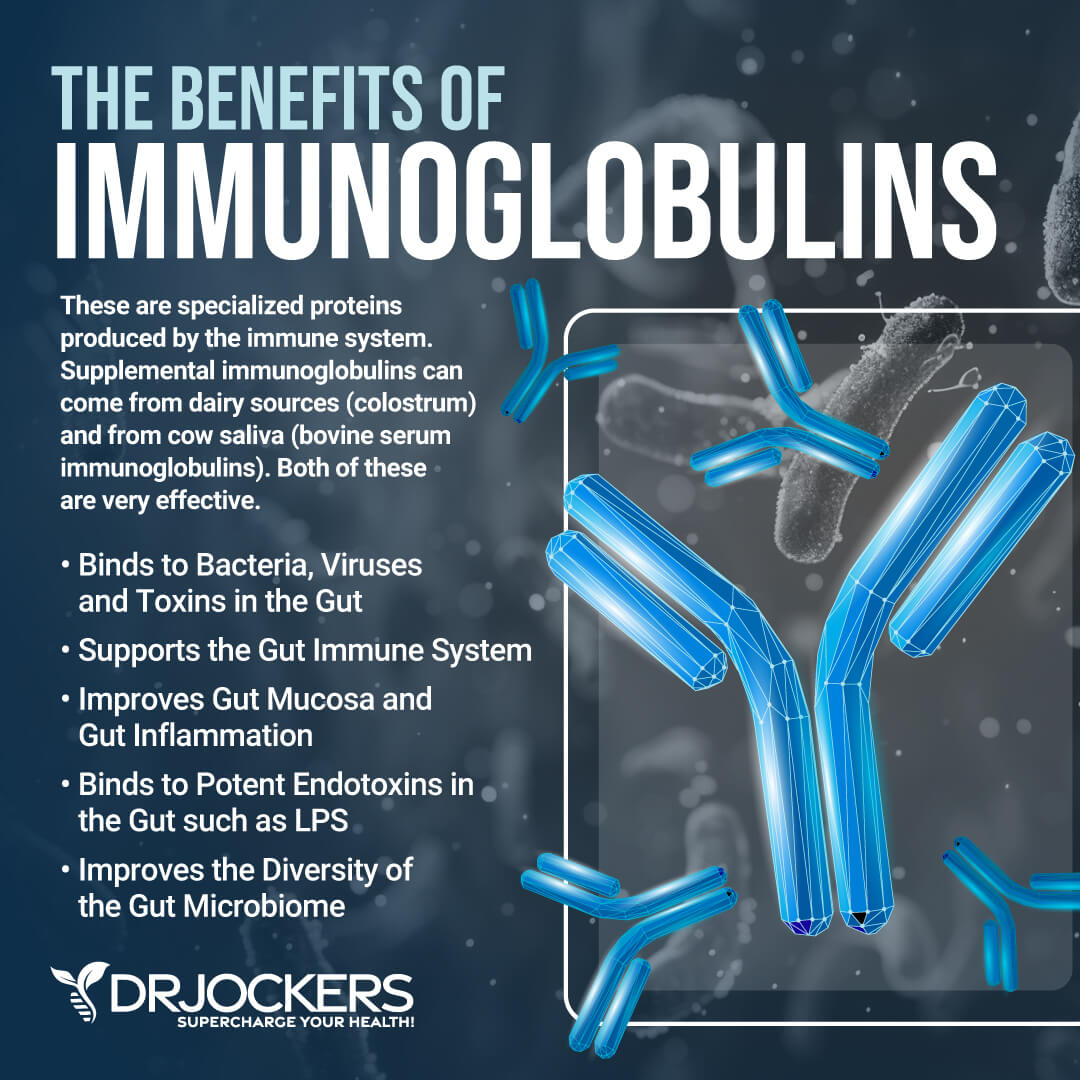
Consider Using Immunoglobulins
I also recommend using some immunoglobulins. Immunoglobulins, commonly known as antibodies, are specialized proteins produced by the immune system. They are designed to identify and neutralize foreign invaders like bacteria, viruses, and toxins.
They are a critical part of the adaptive immune response. They allow the body to recognize and remember pathogens. Immunoglobulins are produced by B cells and plasma cells in response to the presence of antigens.
A 2024 article published in Nutrients has found that serum-derived bovine immunoglobulin may help to reduce inflammation and improve gut barrier integrity (32). Using immunoglobulins may help the gut to neutralize pathogens and decrease gut inflammation more effectively.
IgA is an immunoglobulin that may be great for improving mucosal immunity, creating a balanced gut microbiome, reducing gut inflammation, and supporting gut health.
3. Treat Underlying Infections
Addressing underlying infections such as small intestinal bacterial overgrowth (SIBO) may help improve symptoms of MCAS. Some gut microbes produce high amounts of histamines as a byproduct of their metabolism.
The difficulty is that it can be hard to address these infections until a person’s MCAS symptoms have improved. People with MCAS are often very sensitive to supplementation, and antimicrobials may be too difficult on their system. Starting with a probiotic and immune support may help improve symptoms so that a person can tolerate antimicrobials.
Large concentrations of mast cells are in the mucous. Mega IgG2000 is a dairy-free immunoglobulin concentrate that supports a healthy mucosal immune system. This formula helps to decrease immune activation and strengthen gut barrier function. Once a person is more stable, infections can be addressed with an antimicrobial protocol.
4. Consider Using Supplemental Butyrate
You may also want to consider using supplemental butyrate. Oral butyrate supplements can be absorbed by your small intestine and also enter your bloodstream.
They may offer anti-inflammatory benefits. However, since your small intestine doesn’t use butyrate well, the benefits may be more apparent in the large intestine versus the small one. By being absorbed in the bloodstream, it can offer anti-inflammatory benefits to various organs.
Still, the best way to benefit from butyric acid is from your microbiome which makes it in your large intestine. Supplementation is an extra step that doesn’t replace the recommendation I just shared earlier to help your body make more butyric acid.
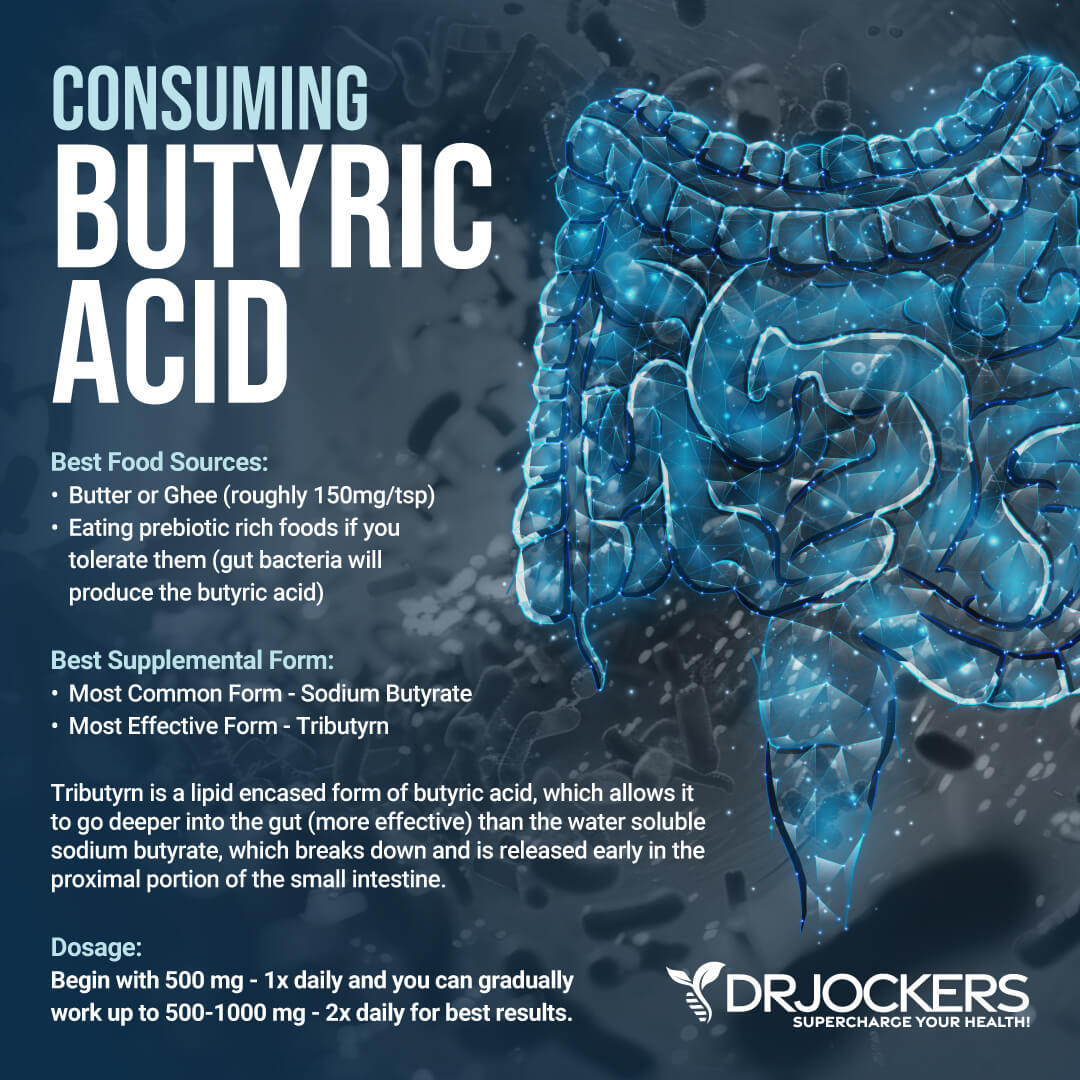
Introducing Tributyrn-X
I recommend using Tributryn-X. If you need support for a dysfunctional immune system, leaky gut, chronic inflammation in the digestive tract, food sensitivities, bloating, or digestive discomfort then your body deserves to try this supplement. It’s the most advanced formula on the market. It’s great for gut health.
Many clinicians we know use around 1,500 mg a day. And in certain cases, higher amounts than that. However, EVERYONE should start slowly with one capsule a day 500mg, as each person’s gut integrity, motility, and microbiome are different.
Each person’s effective dose can also be influenced by alcohol consumption, tobacco consumption, fat mass levels, speed of digestion (too fast might need more, too slow might need less), and other variables. This means you start with 1 soft gel a day and may take 1-3 gel capsules per day of Tributyrin-X or more as directed by your health provider.
Nutrition Plan for Improving MCAS
Individuals with MCAS can be very sensitive to additives, preservatives, and colors in processed foods. Consuming an anti-inflammatory diet of whole, unprocessed foods is critical for anyone with MCAS. These foods include grass-fed, pastured, organic meats, wild-caught fish, organic fruits and vegetables, and healthy fats.
MCAS can make a person highly reactive to histamines and other compounds in foods. It can take time to identify a person’s unique food triggers. However, implementing a low-histamine and/or low-FODMAP diet is a good starting point to help improve the symptoms of MCAS.
Low Histamine Diet
An individual with histamine intolerance has an exaggerated reaction to high histamine foods. The causes of the exaggerated reaction to high histamine foods could be insufficient DAO enzyme production or elevated histamine levels. To improve symptoms of MCAS a low-histamine diet may be very beneficial.
High histamine foods to avoid:
- Fermented dairy, such as cheese, kefir, yogurt, sour cream, buttermilk, and cream cheese
- Fermented alcohol: wine, champagne, beer
- Aged cheeses
- Fermented vegetables and fermented soy products (kimchi, sauerkraut, pickled vegetables, soy sauce)
- Vinegars and foods with vinegars such as pickles, mayonnaise, and olives
- Cured meats such as bacon, salami, pepperoni, lunch meats and hot dogs
- Dried fruits: apricots, prunes, dates, figs, and raisins
- Most citrus fruits, berries, stone fruits
- Vegetables: avocados, eggplant, spinach, tomatoes
- Smoked fish, mackerel, mahi mahi, tuna, anchovies, sardines
- Nuts: walnuts, cashews, and peanuts
Foods that release histamines should also be avoided. These include alcohol, cow’s milk, nuts, chocolate, bananas, papaya, pineapple, shellfish, strawberries, tomatoes, wheat germ, artificial preservatives, and colors. Alcohol, black tea, energy drinks, green tea, and mate tea act as DAO blockers and should be eliminated on a low-histamine diet.
For more information about histamine intolerance and how to know if you could be suffering, read this article.

Low FODMAPs Diet
A low FODMAPs diet has been shown to reduce histamine eightfold (15). A low FODMAP diet may improve histamine issues by down regulating the histamine overreaction or intolerance.
FODMAPs are short-chain carbohydrates that are poorly absorbed in the small intestine. They pass along the gut to the large intestine and are fermented by bacteria. This fermentation results in many digestive symptoms like gas, pain, and bloating. A diet high in FODMAPs can contribute to functional gut disorders like irritable bowel syndrome (IBS).
FODMAPs is an acronym for Fermentable Oligo, Di- and Monosaccharides and Polyols. These fermentable sugar-based carbohydrates include fructose, glucose, galactans, polyols, and lactose. FODMAPs can be found in a range of different foods including many healthy foods. The foods that should be avoided are:
- Oligo-saccharides (fructans): found in vegetables (artichokes, beets, asparagus, onions, garlic, mushrooms), wheat, rye
- Galacto-oligosaccharides (galactans): found in legumes and pulses (chickpeas, kidney beans, lentils, butter beans, black-eyed peas, soybeans)
- Disaccharides (lactose): milk, yogurt, and cheeses like cottage cheese, cream cheese, and ricotta
- Mono-saccharides (excess fructose) are found in fruits like apples, apricots, cherries, figs, mangoes, peaches, pears, plums, and watermelon, sweeteners like agave nectar, corn syrup, and honey
- Polyols (sorbitol and mannitol) are found in fruits (apricots, avocados, blackberries, peaches, cherries), vegetables (cauliflower, mushrooms), sweeteners (sorbitol, xylitol, mannitol)
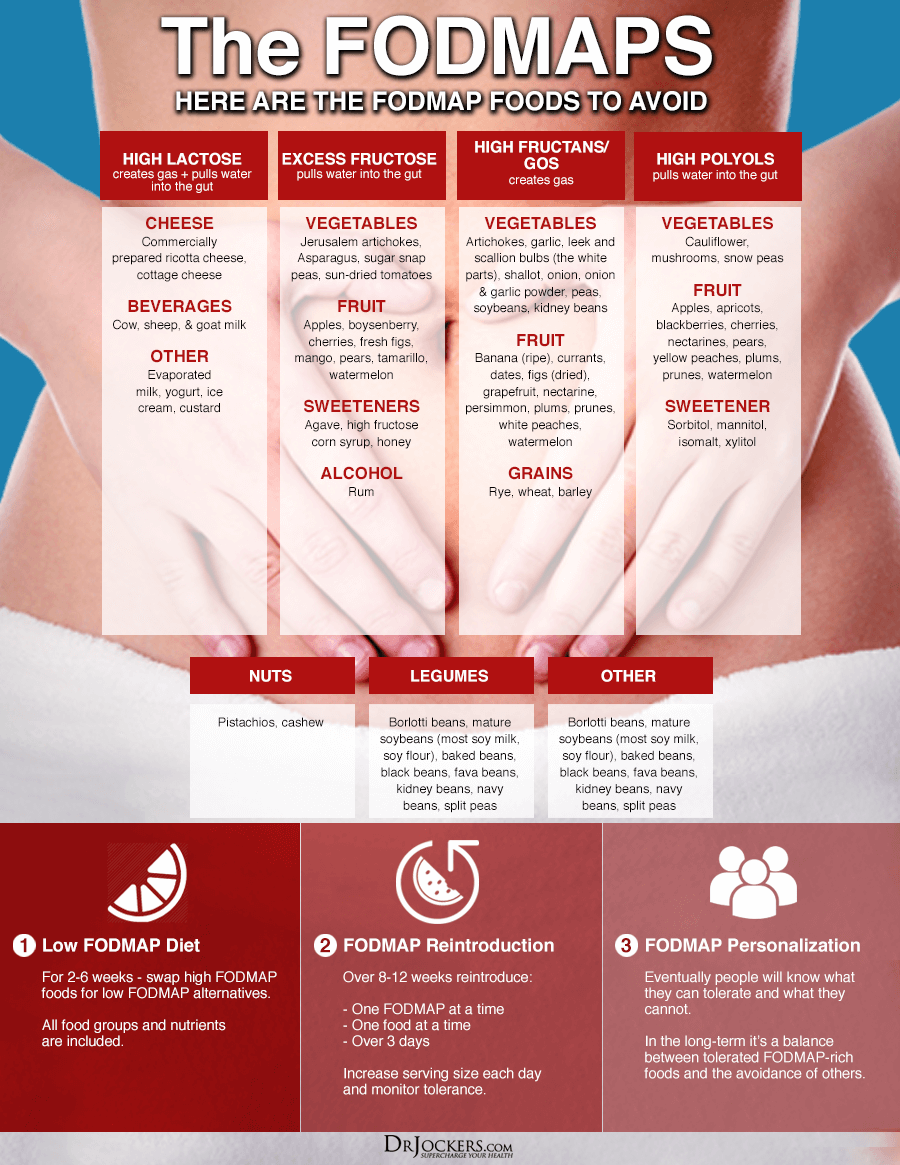
How to Implement an Elimination Diet
To implement an elimination diet, avoid high histamine and/or high FODMAPs foods for around 4-6 weeks. Once you remove these foods, your body can begin to heal, and you may notice improvement in symptoms.
After the elimination period, slowly reintroduce foods that were eliminated. While reintroducing foods, it is important to record all foods consumed with any positive or negative symptoms. You should modify the nutrition plan based on the results of reintroduction and expand the diet to include foods with as much variety and nutrient density as tolerated.

Final Thoughts on MCAS
Mast cells are an important part of your immune system and necessary to heal from injuries. Mast cell activation syndrome occurs when mast cells are overactive and release too many chemical mediators. This can cause serious problems in the body.
There are natural strategies to help people manage the symptoms of MCAS. The first step is to identify and remove any potential triggers of your symptoms. If there are any toxins, infections, pathogens, or other environmental triggers, these must be addressed.
Implementing a low histamine and/or low FODMAP diet may relieve symptoms. Additionally, supplementing with flavonoids and other nutrients that help to stabilize mast cells may be very beneficial for helping improve the immune response.
Follow the tips, strategies, and supplements I recommend for supporting MCAS and see if you notice improvement. If you are doing these things and still struggling with this condition, then I would recommend working with a functional health coach who can help you identify the root causes and customize a specific plan to get well.
On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.






What a tour de force. I have EDS both my daughters have also. My life was alwys different from the other children. My lack of athletic prowess was laughed at. It took until I was in my 60’s before I was diagnosed and only then because both my children were diagnosed.
Both have various autoimmune disorders including Lupus, Tachycardia, Mast cell, Histamine, EDS, Chronic fatigue. Both have lost their jobs because of their inheritance.
I can’t do much to help as their father has PXE, heart disease and a pacemaker as well as being severely visually impaired. I only have Scoliosis in the lumbar region, spondylothesis and Stenosis, Severe osteoarthritis, Gastro paresis and hiatus hernia. I keep going by exercising and taking selected supplements and trying to stay cheerful!
Your daily info. is never boring and always readable and informative, thank you. It’s a pity that this is not compulsary reading for GP’s here in the UK
Sorry to hear about the challenges you have had! Praying for you Marcia and so glad this article was helpful for you!!
My son has autism and hypermobility.
I want a package of her treatment.
So sorry to hear that Tamer. Here is a helpful article https://drjockers.com/autism/
Great article. Don’t you agree that limbic retraining through courses like DNRS (Annie Hooper) could be helpful? I’m a mold patient and I know I need to continue binding the mold and hopefully my MCAS will improve. I’m thinking of doing the DNRS course. What are your thoughts? Do you know where I can get the test for genetic DAO ? I had good improvement in my digestion when I started the DAO enzymes.
Thank you,
Pamela
Yes Pamela, we are big fans of limbic retraining. You can see this article here: https://drjockers.com/limbic-retraining/
We look at DAO enzymes and overall gut permeability with this test here: https://drjockers.com/intestinal-permeability/
Very helpful overview of MCAS, Dr. Jockers. Your articles are so helpful – so nicely laid out with tons of info, along with helpful infographics to illustrate (kudos to your team!). Grateful!
I think I may be dealing with a post-viral issue, which has triggered a rather uncomfortable neuromuscular/TMJ onset, now along with MCAS. Curious if you have heard of (or used) nattokinase for addressing post-viral issues?
Sorry to hear this Carla! Yes nattokinase and other proteolytic enzymes can be very helpful for post viral syndrome.
I was diagnosed with MCAS in 2021 with the root cause being toxic mold exposure and Lyme Disease. Over the last year I have discovered that I am now very sensitive to salicylates – both in foods, supplements and additives to health and beauty products. I have had to stop using many of the supplements that were previously helping to control my MCAS symptoms, such as Quercetin, Curcumin, etc., and any supplement that is described as a “phenol” or “bio-flavinoid.” I am constantly searching for information about how to treat MCAS symptoms without using salicylates, but very few doctors address this problem. I find it interesting, as it is not that uncommon to become sensitive to salicylates when you develop MCAS. It has had a huge impact on my diet – no histamines, no FODMAPs, and now no salicylates! Do you have recommendations for MCAS supplements that are effective and low salicylate?
Yes, I find that zinc, vitamin D and magnesium are very helpful for MCAS. You also may need more methylated B vitamins.
I’m trying to subscribe to your newsletter, etc, and it is asking me if I mean a different e-mail address than what I gave. I gave my correct e-mail address, but it will not let me subscribe. I found your info on MCAS very helpful, as I have been diagnosed with idiopathic MCAS. My name is Margaret, and my e-mail address is: mmthp@ptd.net.
I found this informations about MCAS yesterday, some musician from Australia told about his experience on shorts 🫣. I’m living in Poland Europe and knowledge about MCAS is ”0”. Your article is very comprehensive. First I have to start from test to check if I really have MCAS but every symptoms match. I could never expect that my extreme hypersensitivity to smells may be a symptom. I’m survivor of very terrible neurolyme disease, but winning with lyme unfortunately didn’t mean for me getting fully back my healhy. 😔
Thank you very much for this article. 💓