Asthma: Symptoms, Causes and Natural Support Strategies
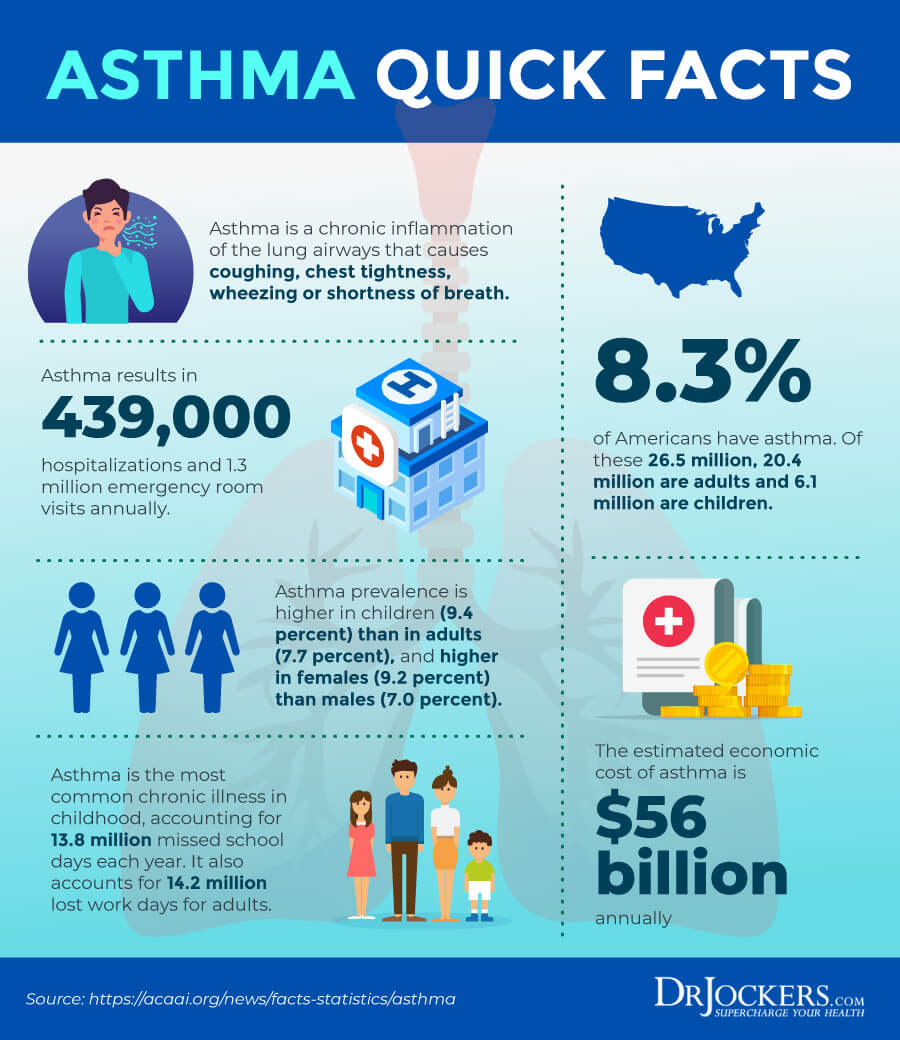
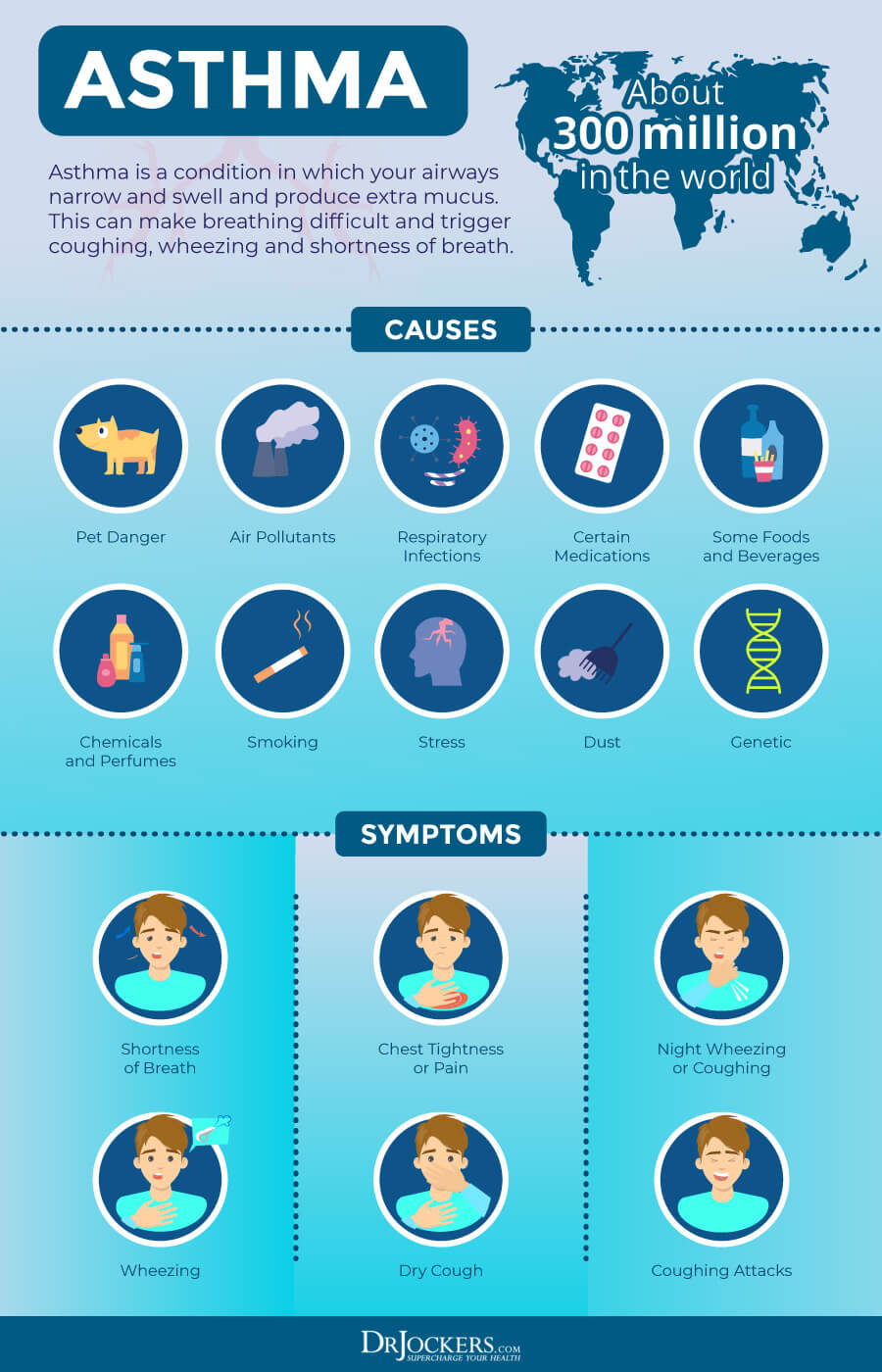
Asthma is one of the most common inflammatory conditions of the lung. It is characterized by variable and recurring symptoms, bronchial spasm and reversible airflow obstructions. In this article, I will go over the major symptoms and root causes of asthma as well as some natural support strategies to improve immune and respiratory health.
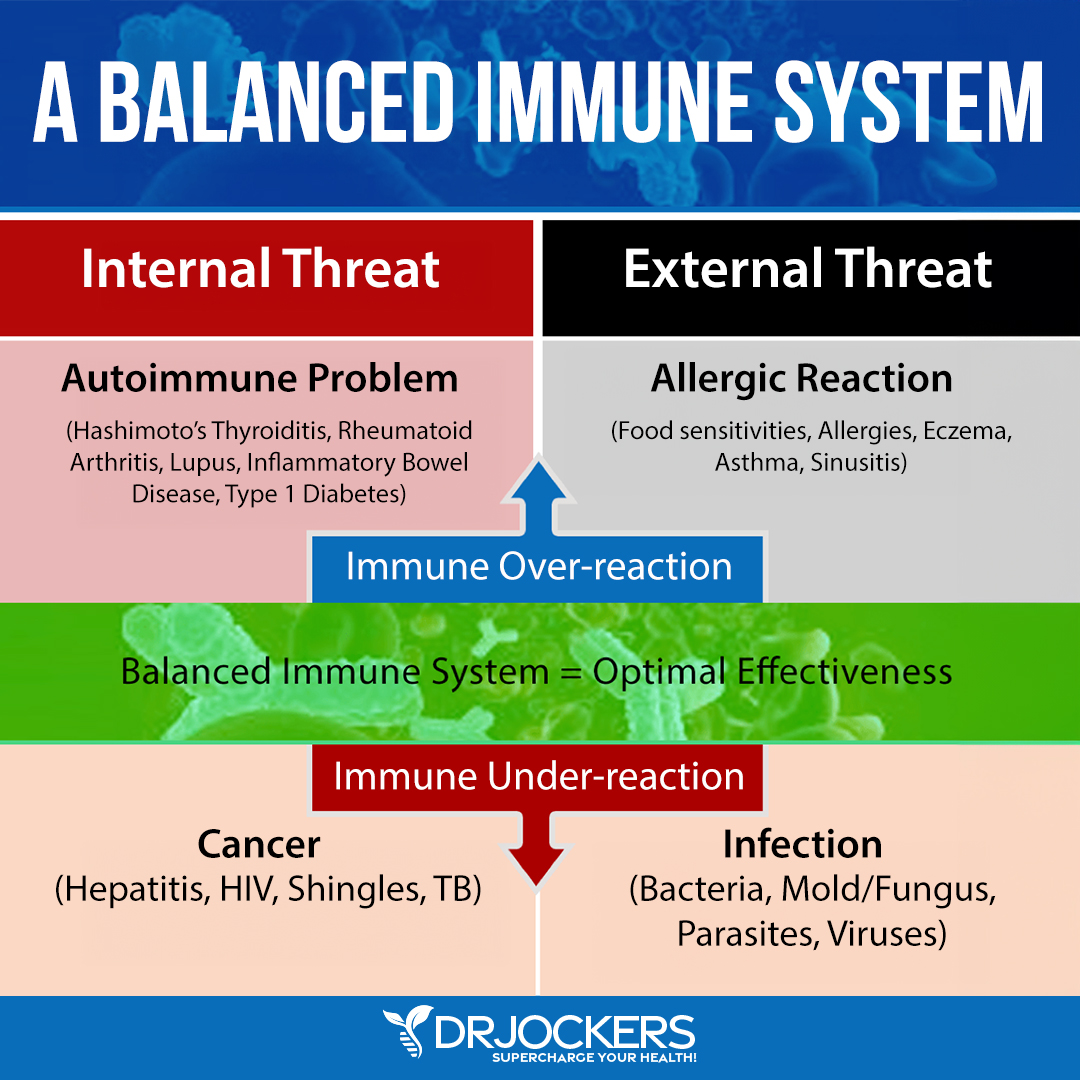
Asthma is more of an immune imbalance than it is a lung disease (1, 2). When the immune system gets triggered, it causes an inflammatory reaction to occur within the lung epithelial tissue. The bronchial tubes swell with fluid and mucous in order to isolate the insulting allergen. This swelling irritates the airways even further, which results in an increased level of sensitivity.
How Asthma Develops
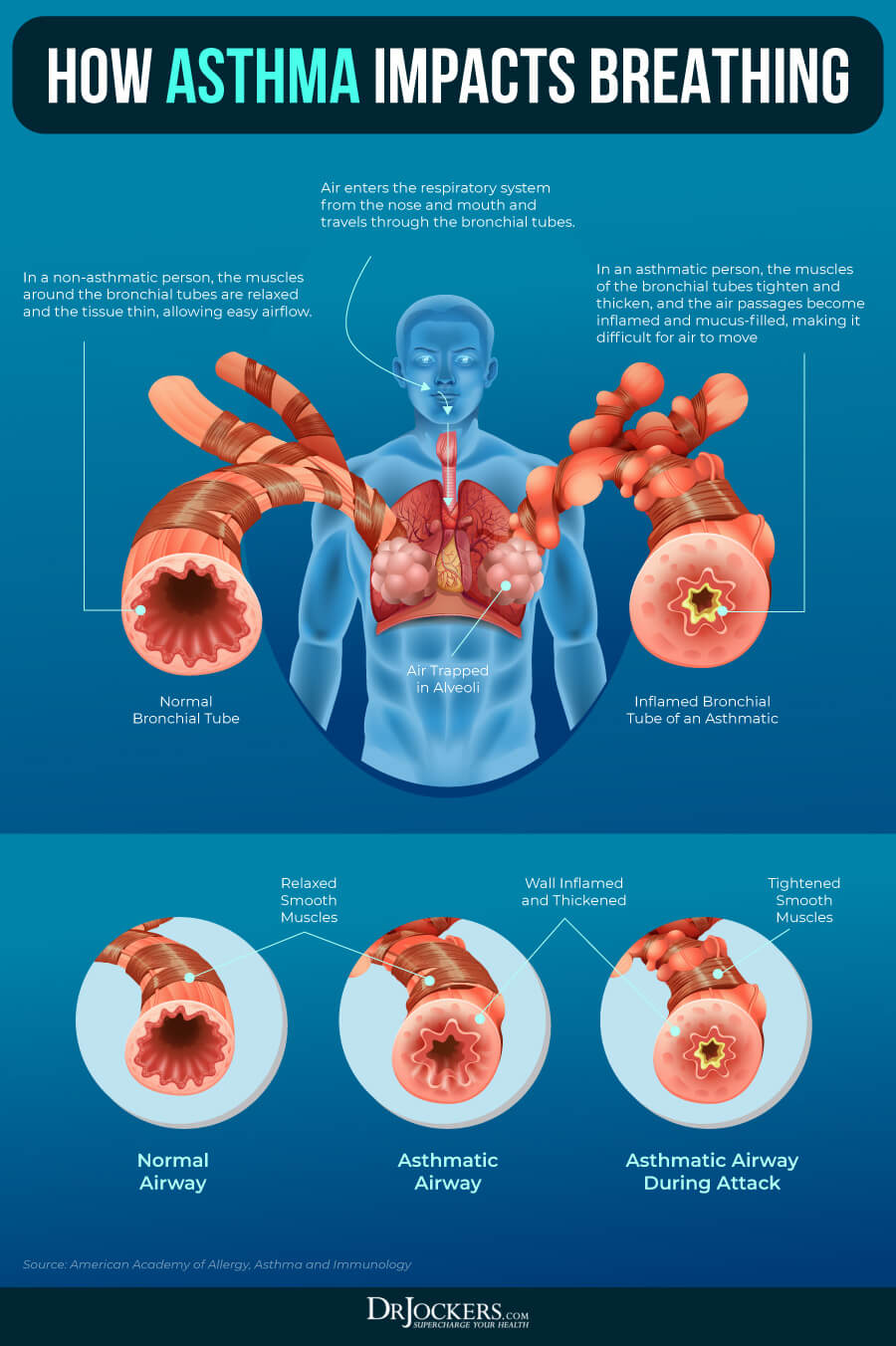
Imagine your lungs as an upside-down tree inside your chest, within your respiratory system. Your upper respiratory system includes your nose, sinuses, pharynx (parts of your airways), and parts of your larynx just above your vocal cords. Your lower respiratory system includes your trachea, bronchi, bronchioles, and parts of your larynx located below your vocal cords.
The muscles around your airways tighten and contract to make sure that the passageways open and allow healthy airflow. If you have asthma, when you inhale any triggering allergens or irritants, you may experience wheezing or coughing and have difficulty breathing. This experience is called bronchospasm.
Bronchospasm and Asthma
Bronchospasm is a symptom of asthma that happens because of a sudden constriction of your airways due to inflammation and sensitivity. This can lead to audible wheezing, shortness of breath, and coughing. These noisy and visible symptoms are the ones that instantly come to mind when we think about asthma. However, there is more to asthma than bronchospasms.
While bronchospasm is the audible and visible part of asthma, airway inflammation is the silent part. Asthma starts with inflammation that causes the lining of your airways to turn inflamed, swollen, and clogged with fluid and mucus. In a non-asthmatic person, the muscles around the bronchial tubes relax and the tissue thins.
This allows easy airflow when the air enters the respiratory system from the nose and mouth and travels through the bronchial tubes. In an asthmatic person, however, the muscles of the bronchial tubes tighten and thicken.
The air passages become inflamed and mucus-filled, which makes it difficult for the air to move. Even though you can see it, asthma inflammation is a quiet yet very important part of asthma. Every time you encounter your asthma triggers, it increases inflammation and increases your chances of more frequent and increased symptoms (3, 4).
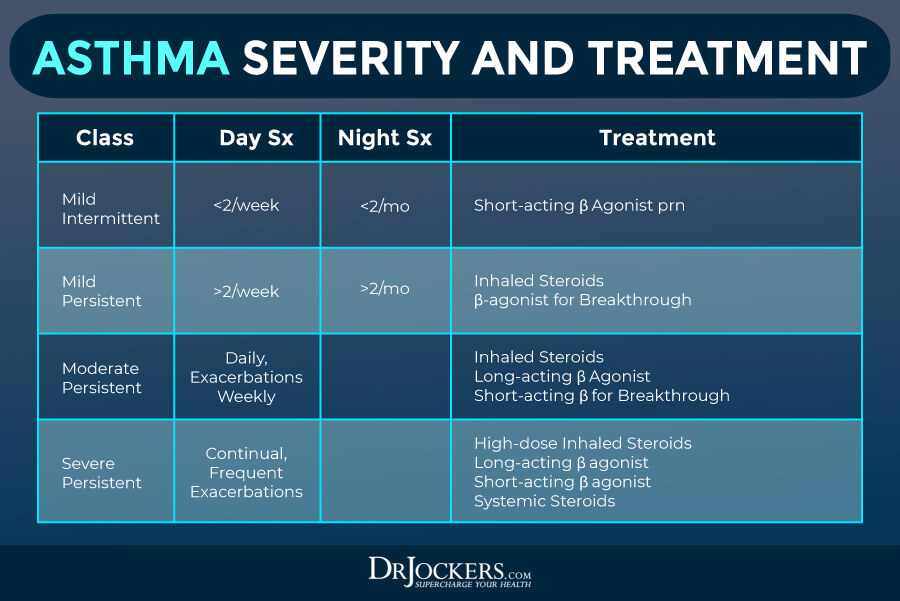
Conventional Treatments For Asthma
Conventional treatments for asthma use various medications aiming to stop asthma attacks before they start. Preventative, long-term control medications are designed to lower inflammation and decrease swelling in your airways to prevent asthma symptoms and attacks.
There are a variety of long-term asthma control medications. Inhaled corticosteroids, such as fluticasone propionate, budesonide, ciclesonide, beclomethasone, mometasone, and fluticasone furoate, are used to lower your risk of asthma attacks with relatively few side effects. Leukotriene modifiers, including zafirlukast, zileuton, and montelukast ,are used for relieving asthma symptoms.
Montelukast may have serious psychological side effects, including depression, aggression, hallucinations, and suicidal thoughts. Combination inhalers, such as fluticasone-salmeterol, budesonide-formoterol, formoterol-mometasone, and fluticasone furoate-vilanterol are often used along with cortisosteroids to reduce your asthma attacks. Theophylline is used to help relax your muscles around your airways. These medications need to be taken daily to lower your risk of asthma attacks.

Asthma Medication Usage:
Additionally, they also use quick-relief inhalers to stop attacks and offer relief. They are created to quickly open up swollen airways and allow normal breathing again. Some may be used just before exercising to prevent exercise-induced asthma symptoms.
Short-acting beta agonists, such as albuterol and levalbuterol, are quick-relief bronchodilators that act quickly to relieve symptoms when inhaled through a nebulizer or portable, hand-held inhaler. Anticholinergic agents, such as ipratropium and tiotropium, similarly to bronchodialators, act quickly to relax your airways and offer relief.
They are also used for chronic bronchitis and emphysema. Oral and intravenous corticosteroids, such as prednisone and methylprednisolone offer relief for airway inflammation in case of a severe asthma attack. They can only be used on a short-term basis due to possible serious side effects when used long-term.
Allergy Medication Usage
In some cases, allergy medications may be used for your asthma symptoms if your asthma attacks are triggered or worsened by allergies. Allergy shots (immunotherapy) may help to gradually decrease your body’s reactions to allergies. Biologics, such as omalizma, mepolizumab, dupilumab, reslizumab, and benralizumab are designed for those with severe asthma.
Additionally, for those with severe asthma, when inhaled corticosteroids or other long-term asthma medications don’t seem to be effective, bronchial thermoplasty may be used. In this case, your doctor heats the inside of your airways with an electrode to smooth the muscles inside your airways, making breathing easier and lowering your risk of asthma attacks.
These conventional asthma treatments do not address the underlying cause of your asthma inflammation and attacks, and may come with unwanted side effects.
Environmental Allergens:
Common environmental allergens that trigger the inflammatory immune response include mold, mites, dust, dander, chemicals & pollutants. It is critical to keep the home clean by using natural cleaning products with grape seed extract, which is a potent anti-fungal that keeps mold down. Dust and vacuum the house regularly and use high quality air filters.
The most common food allergens include processed and refined foods of all kinds. Food additives and preservatives like sodium bisulfite, potassium metabisulfite, and sulfur dioxide have caused severe attacks in asthmatics (5, 6). Pasteurized dairy products, gluten containing grains, soy products, & peanuts are also highly inflammatory and mucous forming foods.

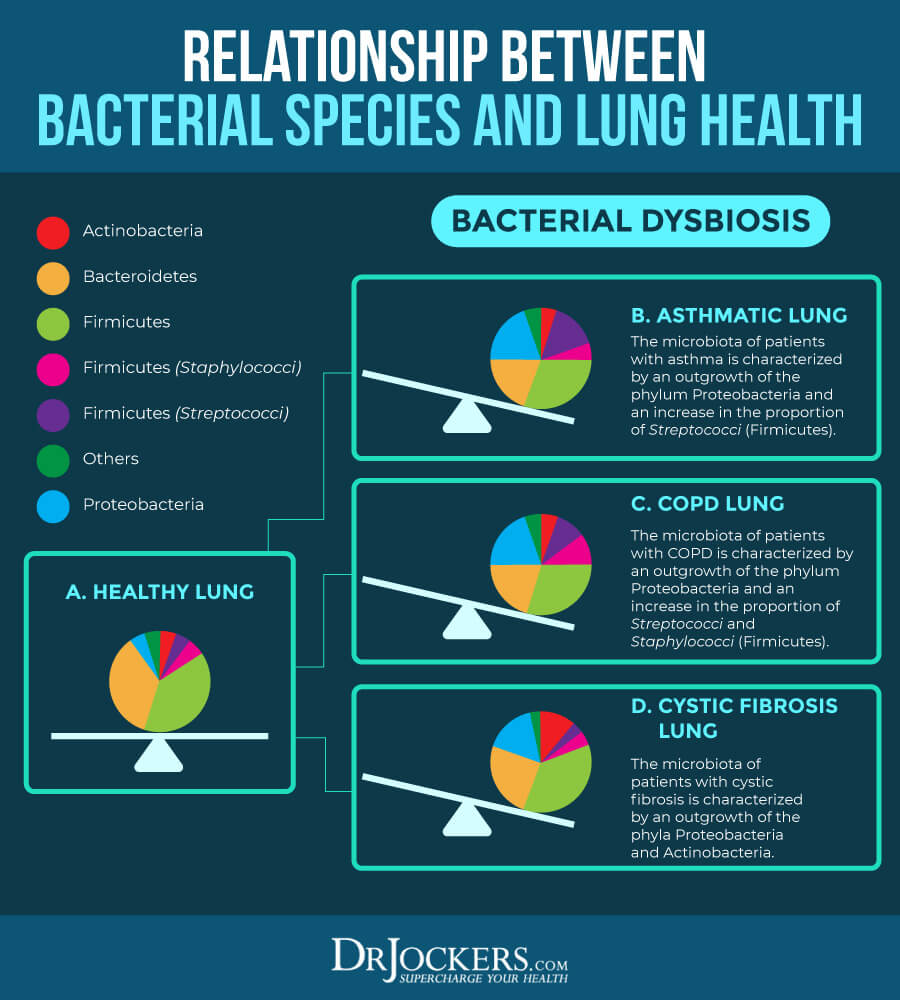
The MicroBiome and Asthma:
The gut microflora is responsible for 70% of our body’s innate immune response (7, 8, 9). The natural makeup should help the body recognize between safe environmental particles (pollen, dust, weeds, etc) and unsafe environmental particles (bad bacteria, fungal/yeast overgrowth, and viruses).
When the gut microflora is altered early in life, it can create an immune malcoordination where the immune system is oversensitive to safe environmental particles. This may lead to seasonal allergies in some and autoimmunity and/or chronic inflammatory conditions such as asthma in others (10, 11, 12).
Asthmatics also have an altered lung microbiota. Asthmatic patients are found to have a much higher level of Proteobacteria and Streptococci bacteria. They had reduced levels of both bacteroidetes and firmicutes (13, 14).
Improve the Microbiome:
Asthmatic individuals need to really focus on improving their microbiome. This begins by reducing the intake of antibiotics and NSAIDs. These have a negative effect on the microbiome (15). An anti-inflammatory diet and lifestyle are key to improving the microbiome and reducing inflammatory activity.
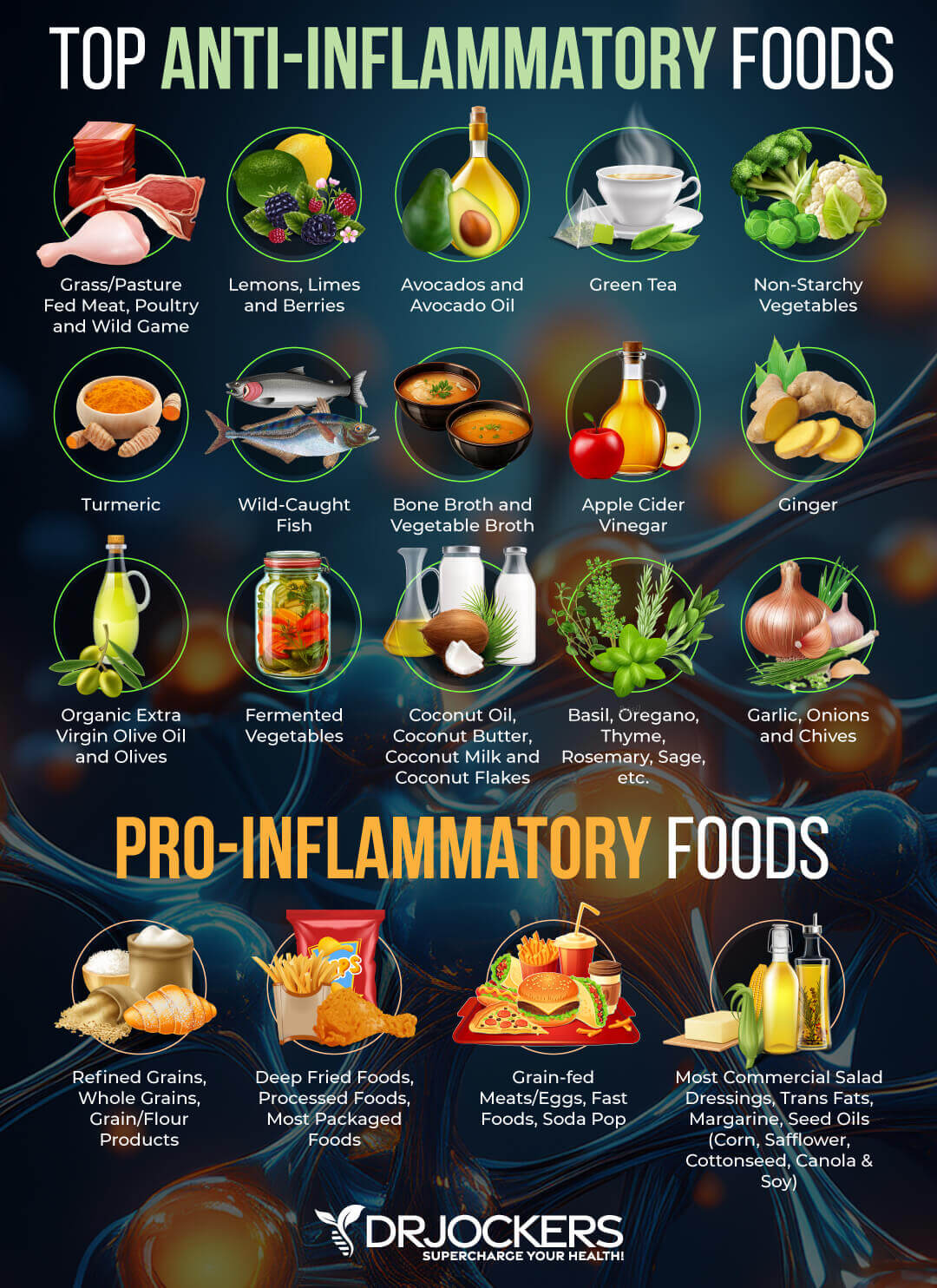
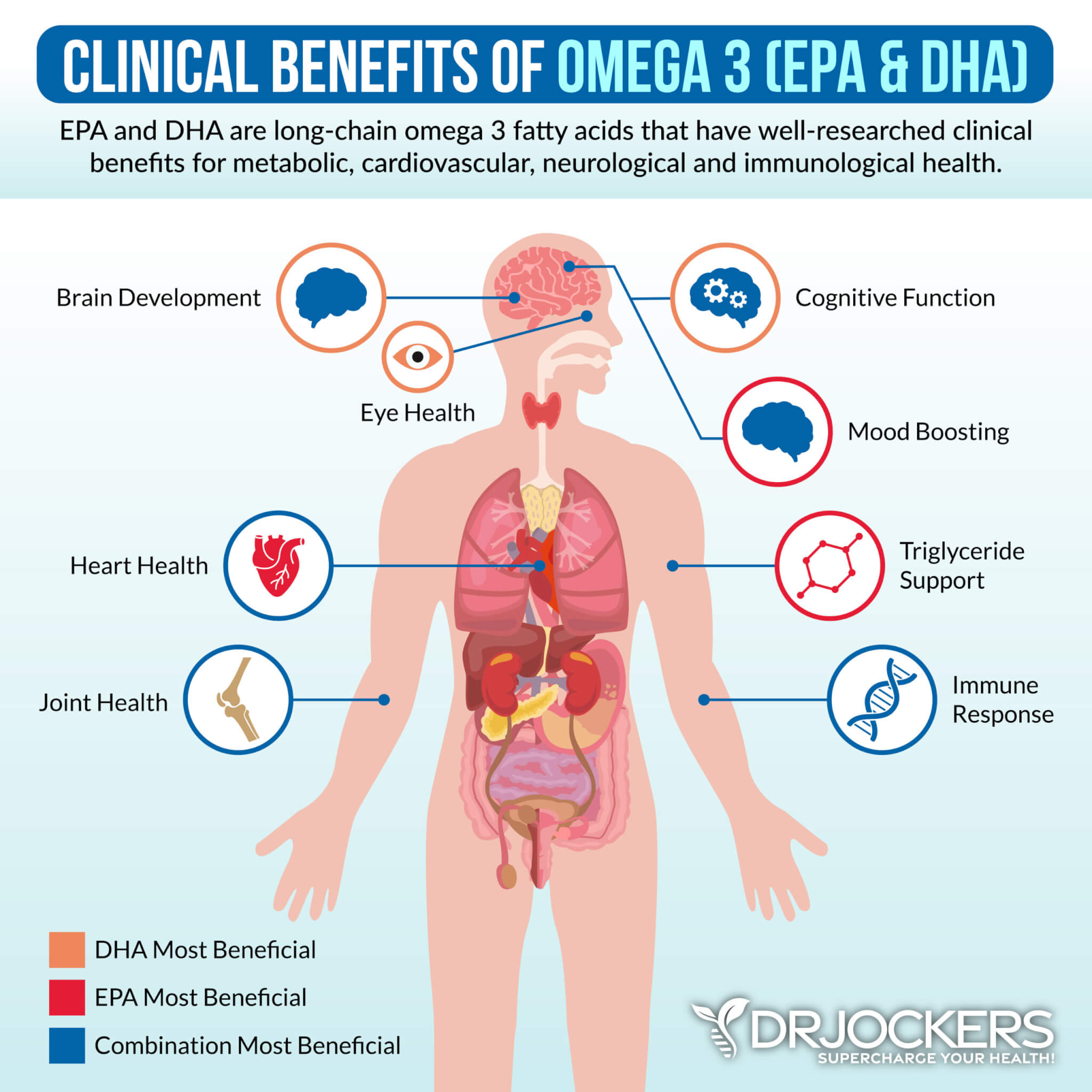
Anti-inflammatory foods help to modulate the immune system and give it a more accurate pair of eyes so as not to over-inflame when stimulated. To effectively de-inflame, it is key to completely avoid man-made foods, sugars, and food allergens as listed above. The long chain omega 3 fatty acids EPA and DHA powerfully de-inflame the body by restoring natural balance to the lipid wall of the cell membrane (16).
Stabilizing the gut with high quality fermented foods such as red cabbage sauerkraut, kimchee, coconut water kefir, coconut milk kefir, coconut yogurt, raw milk kefir, and amasai is very important. Apple Cider vinegar is very useful for providing useful enzymes and reducing mucous formation. Drink a glass of clean water with 1-2 Tsp of ACV throughout the day to reduce mucous and provide beneficial enzymes to help reduce inflammation.
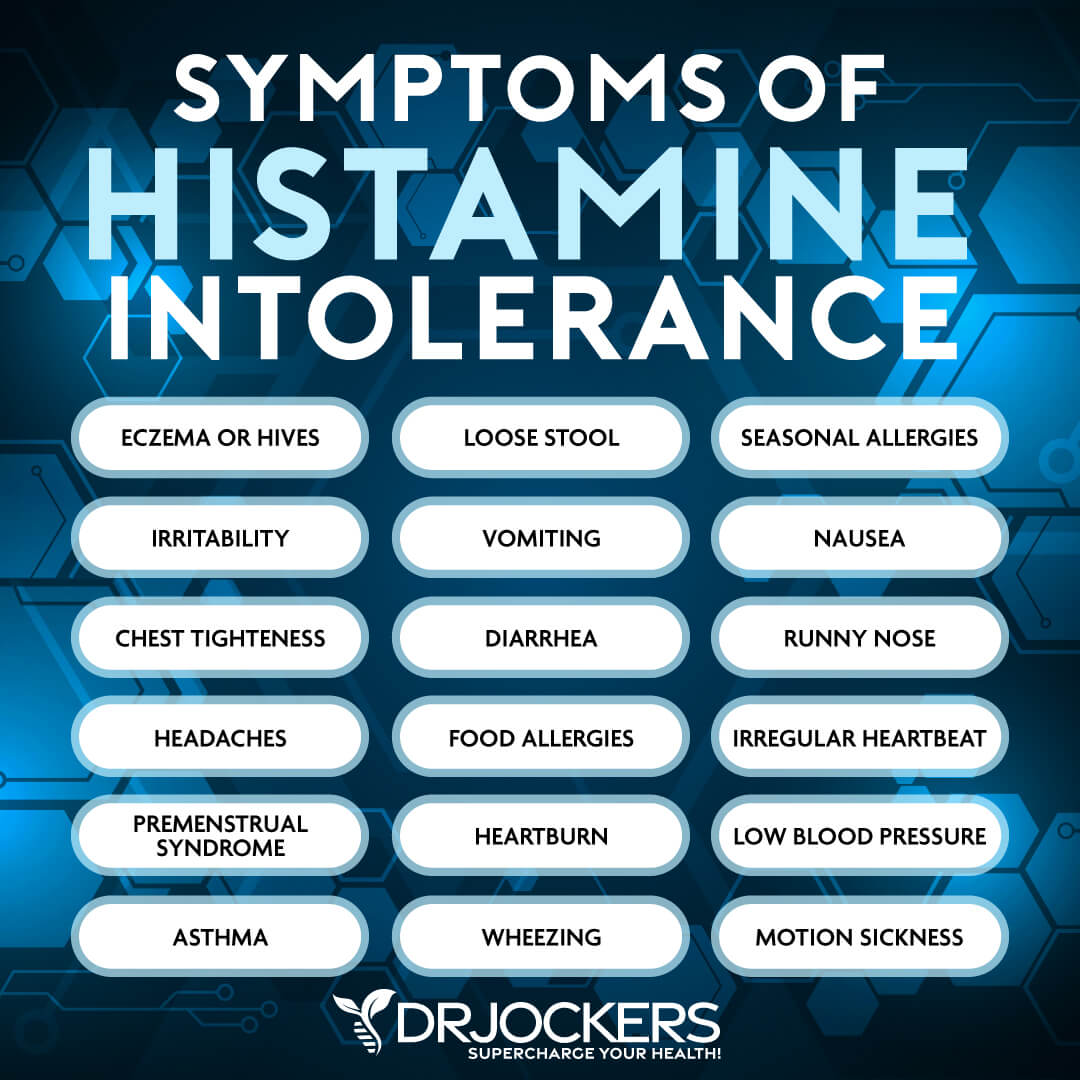
Some individuals with asthma have a histamine intolerance and may not do well with fermented foods. Be careful to notice if you have challenges with fermented foods and they flare up your asthma symptoms or give you hives and allergy symptoms.
Anti-Inflammatory Nutrition Plan:
Be sure to avoid foods that trigger inflammation in the body. This would include gluten, grains, corn, processed sugars, artificial sweeteners, conventional meat and dairy products, and processed starches.
Some great anti-inflammatory foods include coconut products, berries, and bone broth protein powder. This protein source is also loaded with L-glutamine and enhances cellular glutathione stores, which are both necessary for rebuilding the gut and de-inflaming the body. If the individual has a food sensitivity to whey, they can use a high-quality bone broth protein.
Red onions and garlic contain sulfur compounds and the antioxidant flavonoid quercetin. These components have been shown to inhibit an inflammatory enzyme associated with asthma and other inflammatory disorders. Anti-inflammatory herbs such as turmeric, ginger, boswellia, cinnamon, rosemary, and oregano, among others, should be used as much as possible.
Good fibers called arbinogalactans from carrots, onions, radishes, and jicama help to feed the gut microbiome and improve the diversity of beneficial species. Other good fibers include those found in seeds like pumpkin seeds, chia seeds, and flax seeds.

Vitamin D Deficiency and Asthma:
Vitamin D deficiency has been linked to increased rates of asthma. In over 60 years of research, scientists have found vitamin D deficiency linked to lower lung function, increased airway reactivity, and worse asthmatic control (17, 18).
Vitamin D plays a strong role in modulating the inflammatory immune response by blocking pro-inflammatory cytokines such as interleukin 10. Asthma typically worsens in the winter and early spring when vitamin D is at its lowest.

5 Key Supplements for Respiratory and Immune Health:
These 5 nutrients are important for helping to improve the inflammatory response and support respiratory health. It is important to know that these strategies are not at this time FDA-approved to prevent, mitigate, treat, or cure asthma and should not be confused as such.
1. Vitamin D3: Vitamin D3 is crucial for immune coordination in the body. Low levels of vitamin D3 are associated with chronic inflammation, asthma and allergies (19). I recommend getting high quality sun exposure regularly or supplementing with 1,000 IU of vitamin D3 with 4.5 mcg of K2 per 25 lbs of body weight daily.
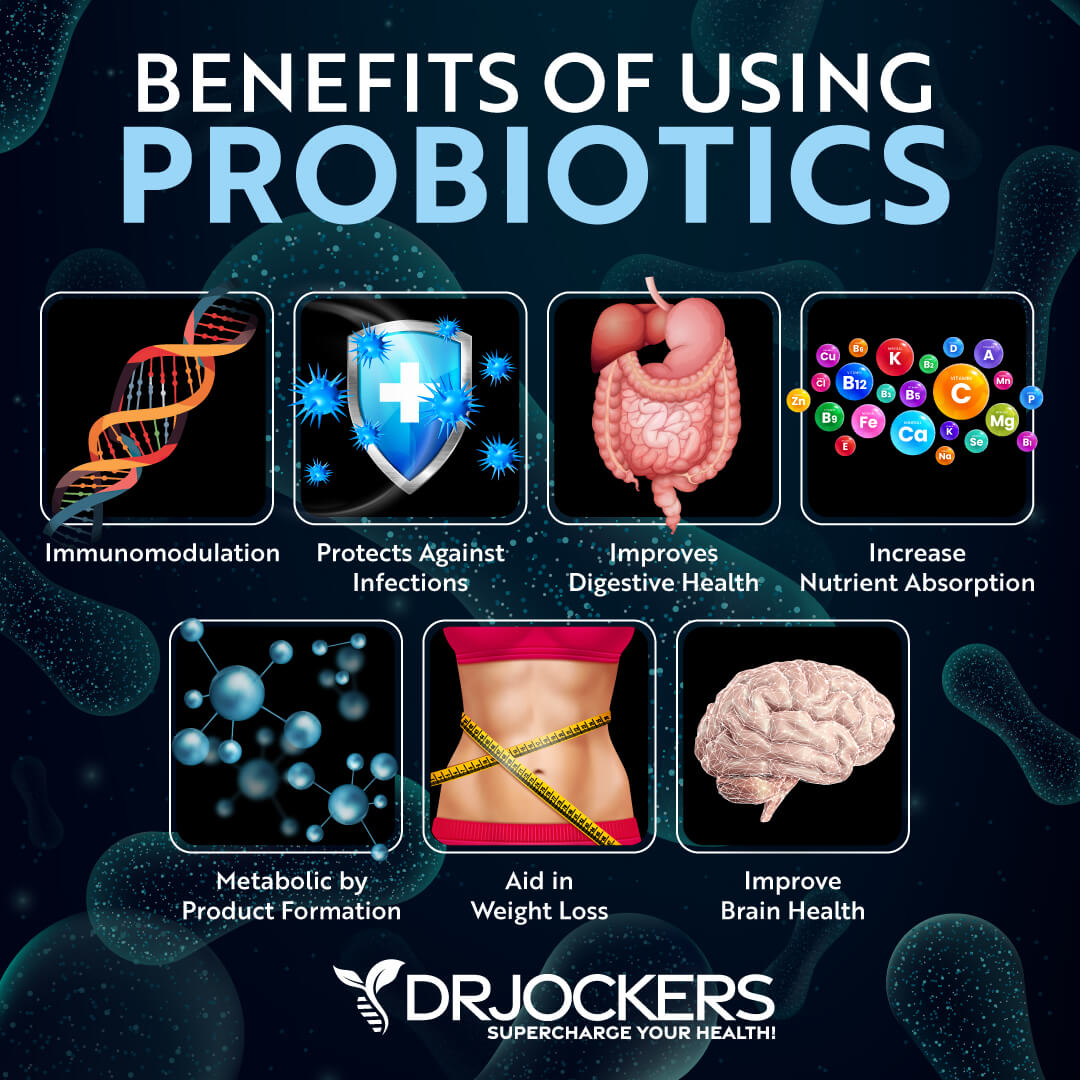
2. Probiotics: Probiotics play an important role in the gut microbiome and immune coordination. Studies have shown that supplemental probiotics are very effective at reducing allergy and asthma symptoms (20).
3. Quercetin & BioFlavonoids: Quercetin, dihydroquercetin (DHQ), and rutin are active bioflavonoids that modulate an exaggerated immune response. Bioflavonoids work synergistically with other antioxidants to protect tissues from the negative effects of oxidation and inflammation often observed during hyperimmune reactions (21).
4. Bromelein: Bromelain is an enzyme complex extracted from the stem and fruit of the pineapple. Its modulation of the inflammatory response is thought to exert a beneficial effect in combating hypersensitive immune reactions (22).
Studies identified its positive effects on controlling edema, tissue permeability, and vasodilation (23). Bromelain is also found to enhance the absorption of quercetin (24).
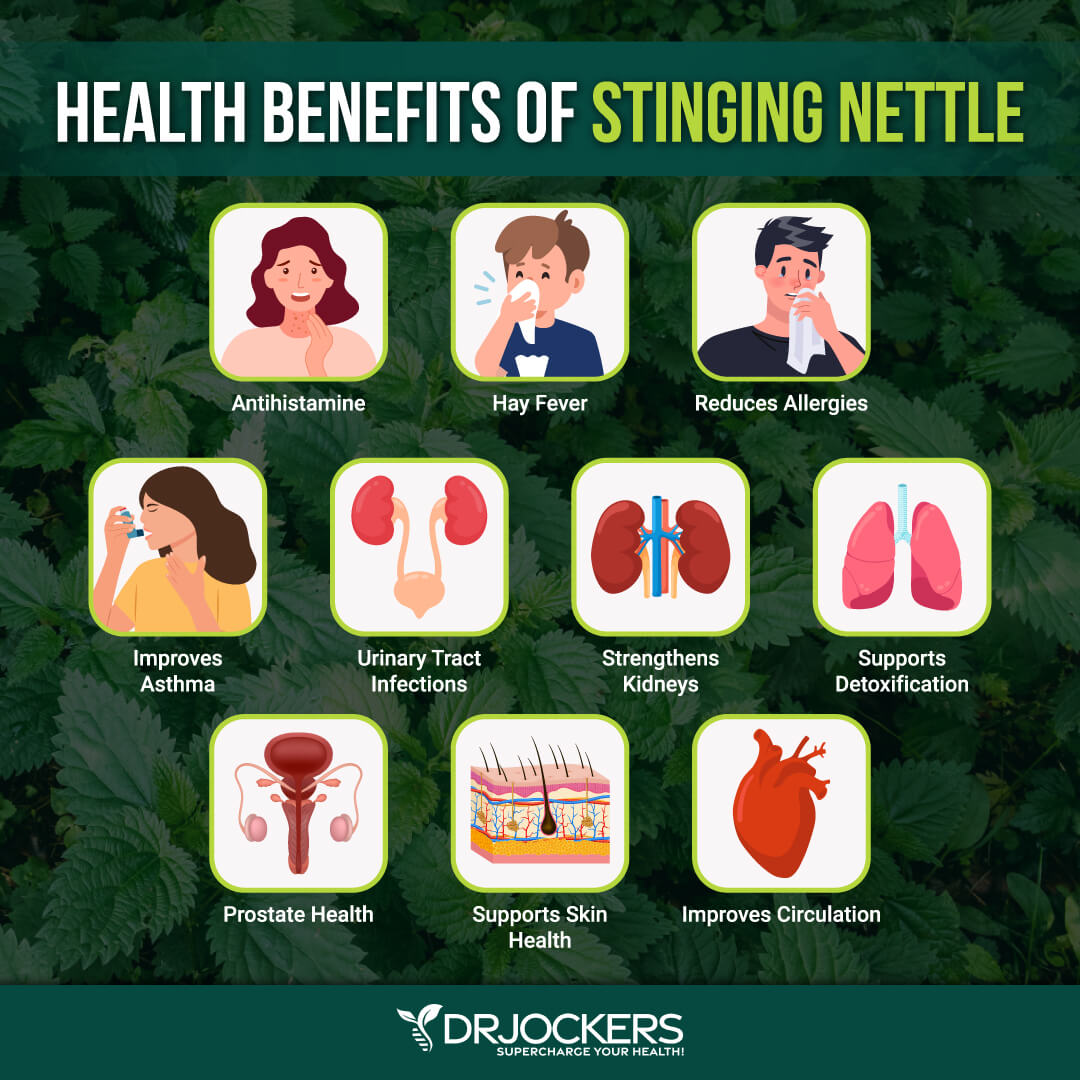
5. Stinging Nettle: Stinging nettle leaf has been found to regulate a variety of inflammatory activities associated with hyperimmune response, including mast-cell degranulation, prostaglandin formation, and histamine action (25, 26)
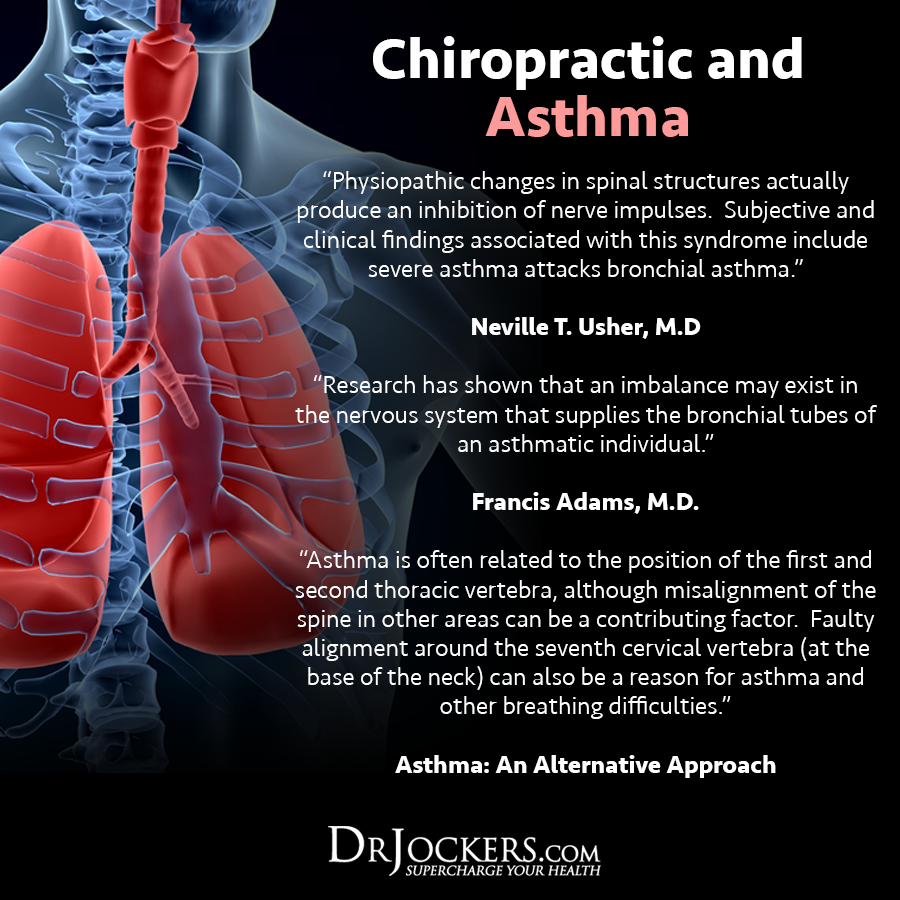
Chiropractic Care and Asthma:
Physical trauma to the upper cervical spine can impact the developing immune system of an infant or child. This form of trauma could include a slip or fall, a car accident, bad sleeping habits, or poor posture. This leads to an upper cervical (neck) subluxation that puts pressure on the brain stem.
Upper cervical subluxations lead to malcoordinated immunity, which can lead to asthmatic reactions in many individuals (27, 28, 29). Chiropractic adjustments help to restore normal motion to the spine and optimal function to the neurological system. This modulates the immune system and reduces inflammation throughout the body.
Respiratory Health Support Strategies:
Here is a list of action steps to take to begin the process of improving respiratory and immune health. These strategies are not currently FDA approved to prevent, mitigate, treat, or cure asthma and should not be confused as such.
This is not an exhaustive list, but it is the first few steps to take, and most people will see a significant improvement in overall respiratory health. You should always discuss any lifestyle change with your physician, and this is especially important if you are taking medications.
Change Your Diet:
Eating an anti-inflammatory diet rich in nutrient-dense foods is the best thing you can do to prevent chronic inflammatory conditions like asthma. First, eliminate all inflammatory foods, including refined sugar, gluten, refined oils, deep-fried and processed foods, conventional dairy, grain-fed meat and eggs, soda and sugary drinks, and foods to which you are sensitive.
Instead, it is important to eat an anti-inflammatory diet that is rich in nutrient dense vegetables, low glycemic index fruits, herbs, spices, healthy fats, grass-fed meat, and wild-caught fish. I also recommend a ketogenic approach for individuals with asthma. Getting into ketosis will enhance mitochondrial function and significantly reduce inflammation in the body.
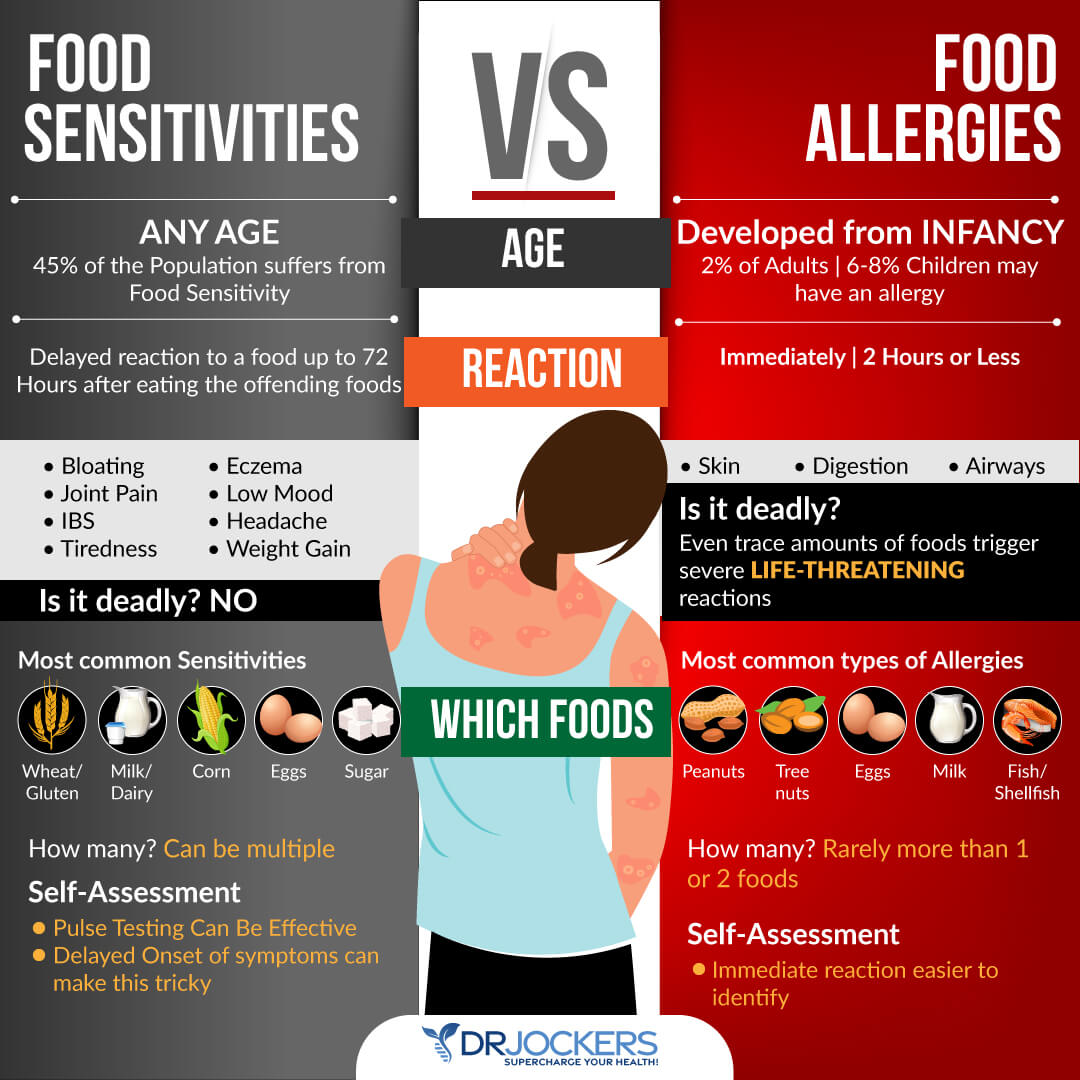
Test For Food Sensitivities:
Most people with chronic inflammatory conditions, such as asthm, have a leaky gut and food sensitivities. These sensitivities can be hard to pinpoint as they result in delayed symptoms that are not life threatening.
The most common food sensitivities include gluten, corn, dairy, soy, peanuts, and sugar. Some other potential food sensitivities to consider include all grains, eggs, nuts, seeds, and nightshade vegetables (tomatoes, potatoes, peppers, and eggplant).
It can be helpful to do a 28-day elimination diet where you remove all of these and then slowly add them back in one at a time. You can also do both biofeedback and blood testing to determine what foods are causing stress in your system, and an elimination diet to test how you are responding to eliminating certain foods for periods of time. You can also
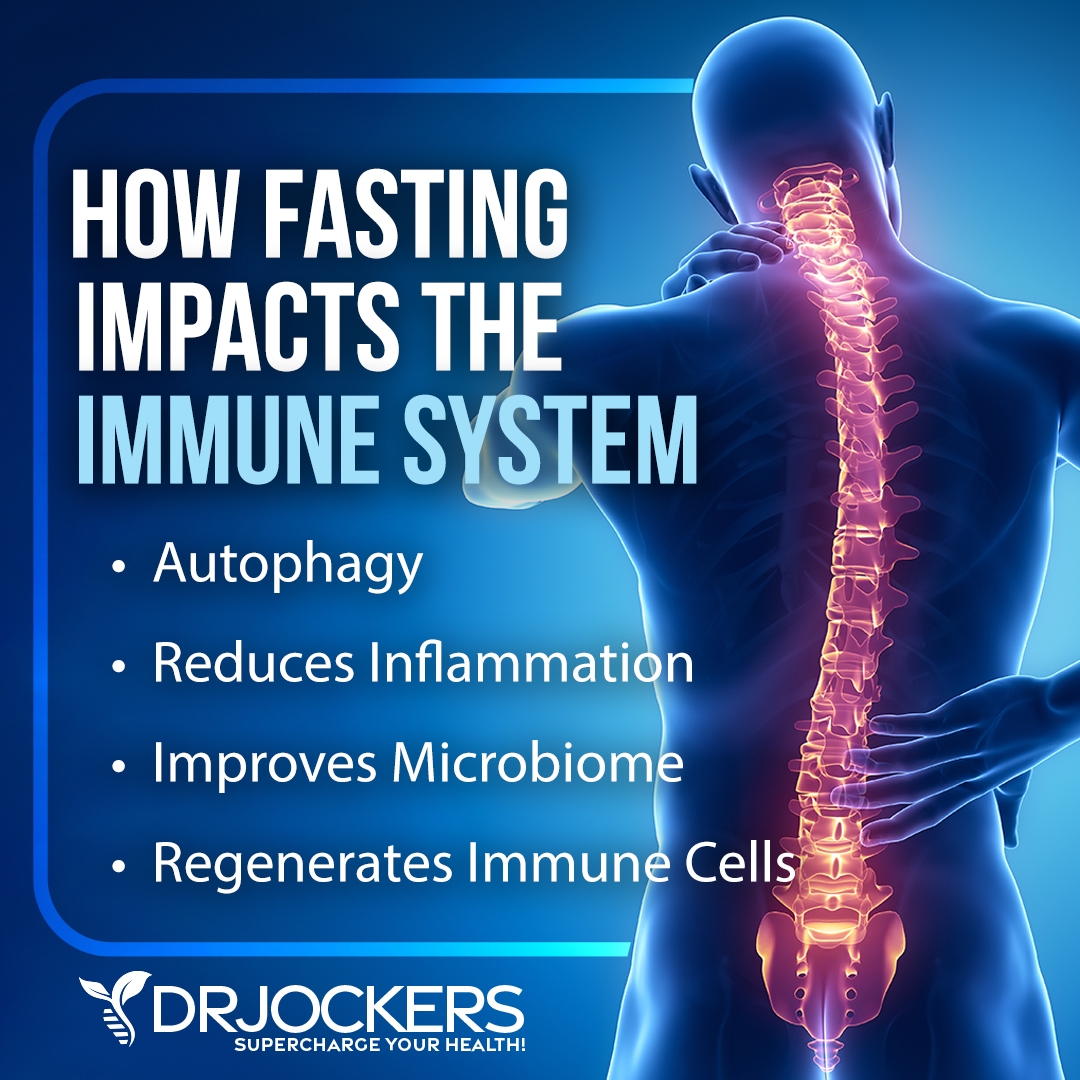
Intermittent Fasting:
Intermittent fasting is a form of fasting that cycles between not eating (fasting) and eating (feasting) over a period of time. The benefits of intermittent fasting include cellular repair, autophagy, immune regulation, inflammation levels, and insulin sensitivity.
It also helps to lower the risk of developing autoimmune and chronic inflammatory conditions such as asthma (30). Going 16–18 hours between dinner and breakfast is one of the best ways to improve mitochondrial production.
Your body improves energy efficiency by increasing and strengthening the mitochondria during periods of fasting. Consume your meals in a 6–8-hour window, such as 11 AM–7 PM or 12–6 PM.
When you do this, you enhance cellular healing and respiratory function. To learn more about the benefits of intermittent fasting and best intermittent fasting practices, I recommend this article.
Optimize Your Vitamin D3 Levels:
Vitamin D is more of a hormone than it is a vitamin. Hormones interact with cells directly to elicit specific biological processes. Low vitamin D3 is associated with chronic inflammation and autoimmune conditions. Vitamin D is arguably one of the most powerful nutrients responsible for modulating and coordinating the immune system.
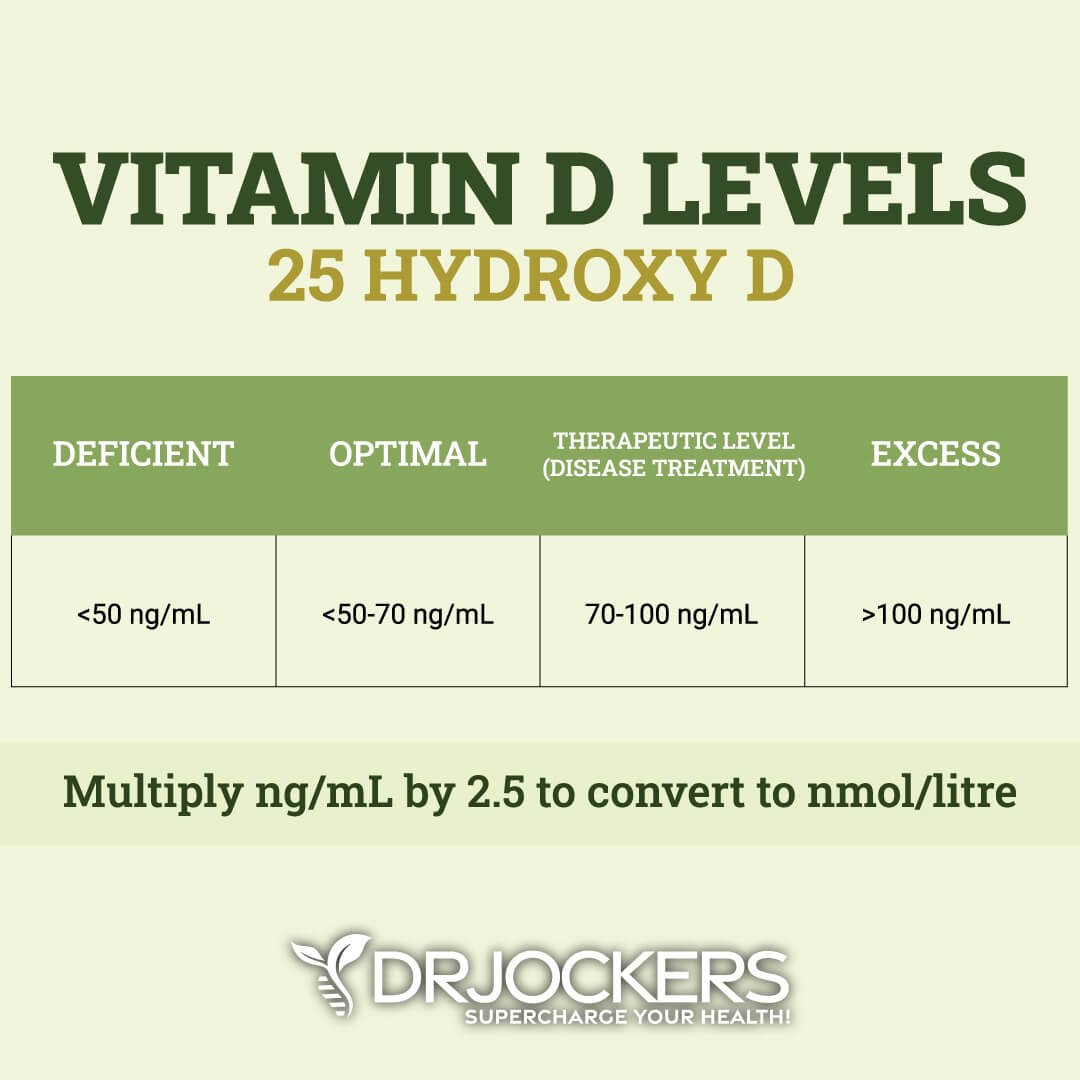
Sunshine is the best way to get enough vitamin D; however, our indoor lifestyle and in some places, cold climate and cloudy weather, make it practically impossible to meet all your requirements. Taking a good quality vitamin D3 supplement on a regular basis and testing your 25-OH vitamin D3 levels a few times a year to make sure it is in the optimal 50-100 ng/mL range is recommended.
Support Gut Health
Your respiratory system and gut are closely connected, and supporting your gut is important for preventing and reducing respiratory problems. Make sure gut-friendly, anti-inflammatory, and nutrient-dense diet abundant in veggies, healthy fats, clean protein, and probiotic-rich foods, such as sauerkraut, kimchi, and kefir.
Additionally, I recommend taking a daily probiotic supplement. Probiotics help to optimize your gut health and improve your nutrient absorption while reducing gut related inflammation. When gut inflammation goes down, it also reduces inflammatory mediators in the lungs.
Focus on Deep Breathing:
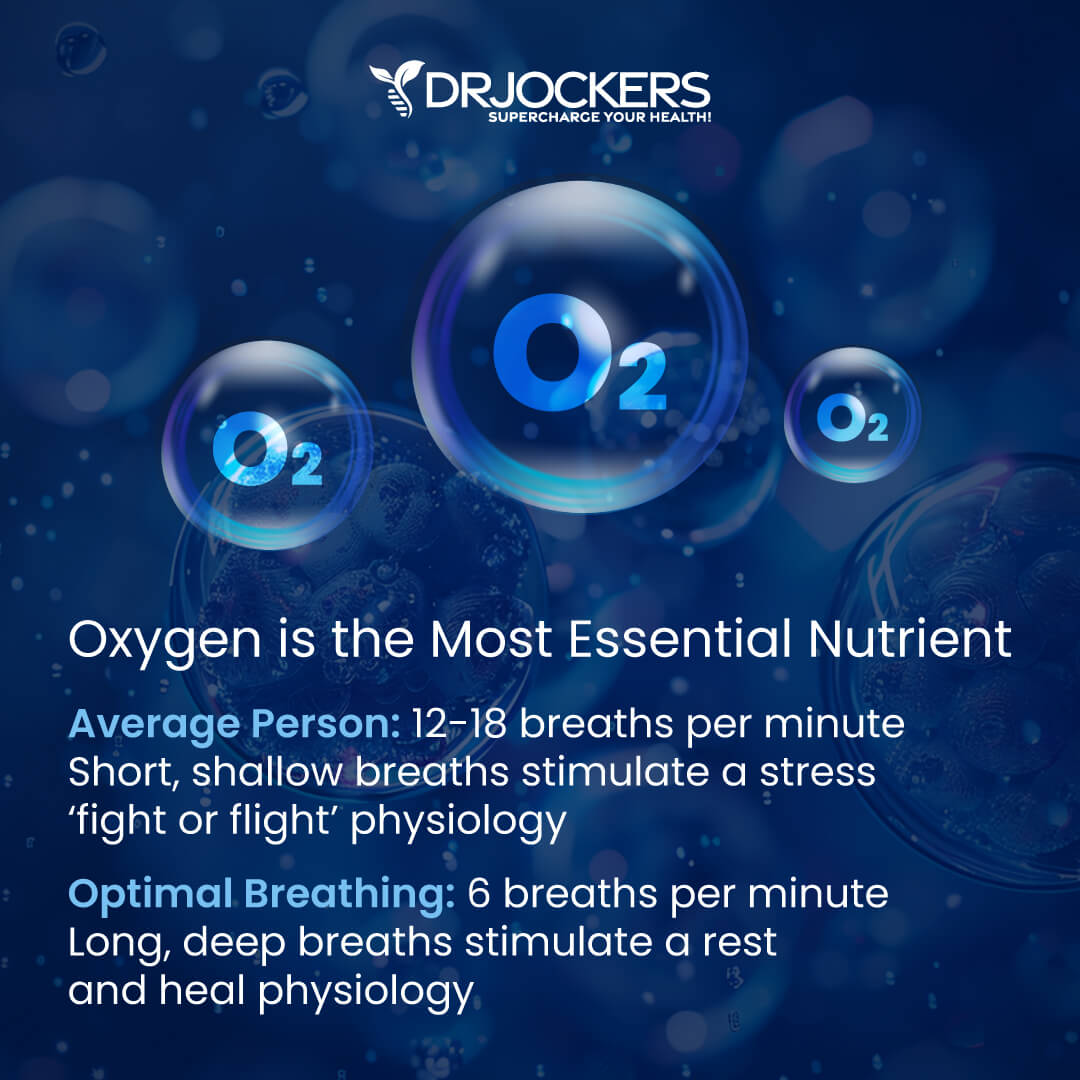
Improving your posture, seeing a high-quality chiropractor, and optimizing your breathing patterns are highly recommended. Taking time to slow down your breathing and take long-deep breaths for a few minutes every hour will help reduce the sympathetic, fight or flight part of the nervous system.
The better we breathe, the better we will heal, the more blood flow we will get, and the better our immune and inflammatory health will be. Follow these tips here to improve your breathing patterns.
Reduce Stress:
Reducing stress is critical for reducing inflammation and improving respiratory health. Most people with asthma notice a significant worsening of symptoms when they are under a lot of stress.
I recommend that you reduce stressors in your life as much as possible. Turn off the news and only look at it once a day or a few times a week for a specific period. Reduce your social media use and time on the internet.
Avoid people and situations that bring you down. Surround yourself with loving and uplifting people. Engage in uplifting and relaxation-promoting activities. Read, try some arts and crafts, play cards or board games, sing, and dance.
Spend time in nature and do some grounding walking barefoot on grass. Practice daily gratitude and try positive affirmations. Practice self-love and laugh with friends and family. Meditate, pray, journal, and try daily breathwork. Be grateful and smile more.
Improve Your Sleep:
Prioritizing good sleep is just as important as reducing your stress levels. The better you sleep, the less you provoke inflammation in your respiratory pathways. Many people with asthma have noted that they have worsening symptoms on days after they sleep poorly.
Develop a regular schedule for going to bed and getting up at the same time every day to support your circadian rhythms. Avoid electronics, sugar, caffeine, heavy foods, and stress close to the bed. Engage in relaxing activities, including stretching, relaxing baths, meditation, and prayer. Make sure that you have a supporting bed, pillow, and bedding, and sleep in a dark, calming room.

Supplement With Omega-3s:
Omega-3 fatty acids, and in particular the long chain variety EPA and DHA, are critical for stabilizing blood sugar, reducing inflammation and improving respiratory health (29). Consume grass-fed meat, grass-fed butter, wild-caught fish, and spirulina to get it in your diet.
Plant-based omega-3, such as flax oil, only contains the small chain omega 3 called ALA and does not have any DHA. It is very hard for our body to convert ALA into DHA, so it is best to get a high-quality fish or krill oil that is rich in EPA and DHA. You want to find a brand that is molecularly distilled to take out any heavy metals and other unwanted contaminants.
Be sure to discuss with your physician before using, as fish oils have a blood thinning effect and can be contraindicated if you are on blood thinning medications.
Final Thoughts
Asthma is a serious, chronic inflammatory issue that affects millions of people around the world. It happens when the immune system within the respiratory system gets over activated. The symptoms of asthma include difficulty breathing, chest pain, cough, and wheezing. Follow the strategies in this article to help support a healthy immune, respiratory, and inflammatory process.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




Typically, lol, how long til improvement such as eczema etc, is seen following these measures? Will allergies heal or would these same recommendations for diet be necessary for maintenance? Can you get enough omega 3’s through food, which ones, or is supplimentation needed?
BJ, these are impossible questions to answer without understanding a health history and knowing what health challenges are present. However, the nutrition plan should be followed as closely as possible for life to avoid food sensitivities and environmental toxins.
Yes, you can get a lot of omega 3’s from wild caught fish, sea vegetable, grass-fed beef and flax/chia seeds. But you need to stay away from omega-6 fats from refined oils, nuts and commercial meats as well.
I have COPD and am looking for information to improve my abilities and have limited funds to work with. Can you recommend any place that may be helpful in healing and gaining some more abilities.
Thank you for this article and look forward to your answer.
Hey Andrew, so sorry to hear about your health issues. There is tons of free information, recipes, shopping plans, etc on this site that you can take advantage of as well as low-cost, high quality supplements. Wishing you all the best! Blessings!
I am surprised there is no mention of MSM supplementation in this article. After reading Dr. Jockers’ “The Health Benefits of MSM”, I started supplementing 2 grams MSM, 2-3 times daily. For the first time in 15 years, I have survived February-March pollen season in Phoenix, AZ with absolutely zero asthma/allergy symptoms. In the past I have had to rely on Albuterol, Benadryl, Sudafed, Mucinex, and various prescription nasal sprays just to get through the season. I have seen references claiming 60-70% of asthmatics are completely relieved of symptoms through MSM supplementation. It definitely seems to be a life changer for me.
That is great to hear Galen! Yes getting more sulfur containing amino acids boosts up glutathione which can be huge for asthmatics!!
Poor Micah is18 months old..he gurgles all night to the point of vomiting..he coughs constantly but cannot seem to get it up until he vomits..
his breathing sounds horrbile at night.A friend suggested I get some L Glutamine and Bromelaine , which I did..but I don’t know what dose to give him..The doctor says it is upper respiratory and nothing an antibiotic will help with. His nose runs all the time
I have been sick for 4 days myself and wonder is Micah contagious.I am keeping 5 other kids here for DSS
Hey Joyce, I’m so sorry to hear about this! I would recommend finding a Pediatric Chiropractor in your area: https://icpa4kids.com/index.php
Thank you so much for taking the time to reply…A Chiropractor for congestion and runny nose?..could you tell me the thought proccess behind that?
Micah saw 3 doctors this week Pediatrician, ENT, Allergist, in that order..he got 40 pricks 🙁 daily… Claritin, Qvar , Nasonex, Nasal saline at night) rescue..for cough Pro Air…(man that stuff works nicely and quick) albuterol nebulizer …also as needed
allergies to dust mites, mold, pollen, Timothy Grass -which we have a yard full of..:(…
no significant change yet..but back in 6 weeks and if no better ..beck to ENT to research deeper nasal activity
Hey Joyce, chiropractic adjustments have been shown to improve these symptoms. Additionally, you may be able to find one who is qualified in natural medicine who can give you some ways to improve your son’s immune defenses against these things so he is not as reactive. I hope this is helpful!
Blessings!
Dr Jockers, got issues with asthma, rheumatoid arthritis, HP, High Cholesterol levels and bad allergies. Been on medication since 2012, no feeling OK. Please help I live in Zambia, Chingola CopperBelt.
What can I use and to get the remedies. Please help me…..
Christine
So sorry to hear that! Be sure to follow the recommendations in the article and here is another good one: https://drjockers.com/beat-rheumatoid-arthritis-naturally/
Hi Dr. J.
Although my doctor has a hard time believing me, I believe that I contracted Asthma at the age of 42 from using snorkeling equipment that wasn’t cleaned before it was given to me. The mouth piece was full of thick mucus when I put in in my mouth. That same night I developed a bad bronchiole cough that lasted for weeks, and mild asthma started after that. It is now 10 years later and I still use asthma medication daily to control the symptoms. Is there anything that I can do to cure myself.
Sorry to hear that! I would be sure to follow the 10 steps I laid out in this article. Blessings!
Love the article!
How could you rid the bad bugs that asthmatics seems to have in their lungs that you mentioned. Would a normal oral probiotic help that? I’d imagine it wouldn’t.
My son is 6 with year round allergies that sometimes turn into asthmatic flares but has a very clean diet and takes d hist jr daily.
Yes an oral probiotic is helpful and also improving indoor air with an air purifier and plants can be helpful!