The AutoImmune Nutrition Plan:
How many times have you sought medical attention to improve a health problem you are facing only to walk out of the office with little indication of a possible diagnosis and a prescription sheet directing you to consume drugs only to treat your symptoms? A known 22 million people in the United States are affected by an autoimmune disease and millions are more likely to suffer unknowingly (6).
Now, what if that prescription sheet had a natural strategy for you to follow that could not only treat your symptoms but decrease the severity of your disease or disorder and possibly prevent further suffering? An autoimmune diet may be the answer you were originally seeking.
What is an Autoimmune Disease?
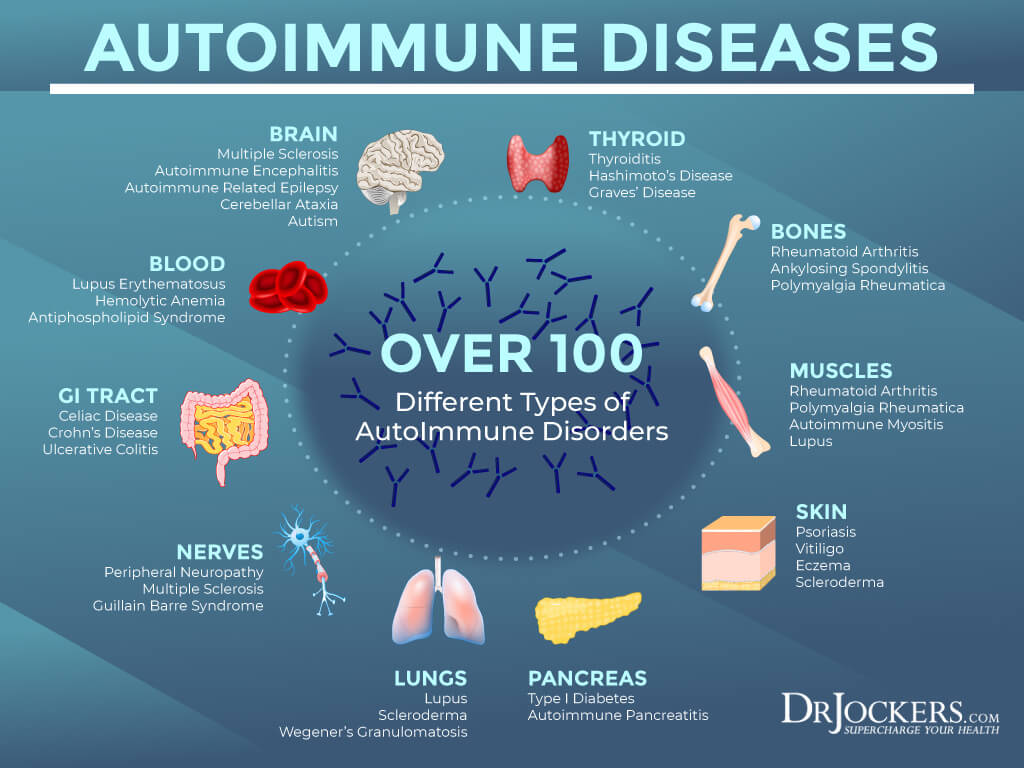
There are 80 known autoimmune diseases in which a broad range of symptoms can manifest in the body (6). In these cases, the immune system mistakenly attacks healthy tissue after a perceived threat from an otherwise normal food source. The most common food sensitives are gluten, dairy, eggs, and nuts (3, 15)
Many factors may trigger an individual’s immune system to function inappropriately such as infectious agents such as bacteria or viruses, genetics, and lifestyle factors. Although we are unable to change our genetic predisposition to autoimmune disease, we can change our lifestyle habits beginning with nutrition (6).
The Immune System
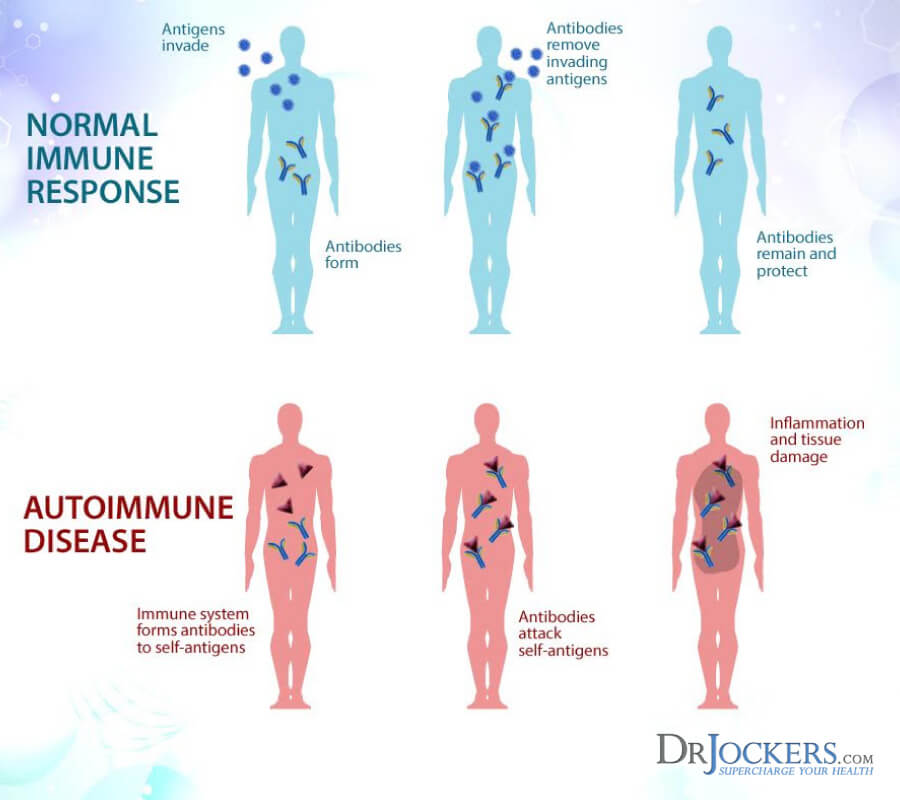
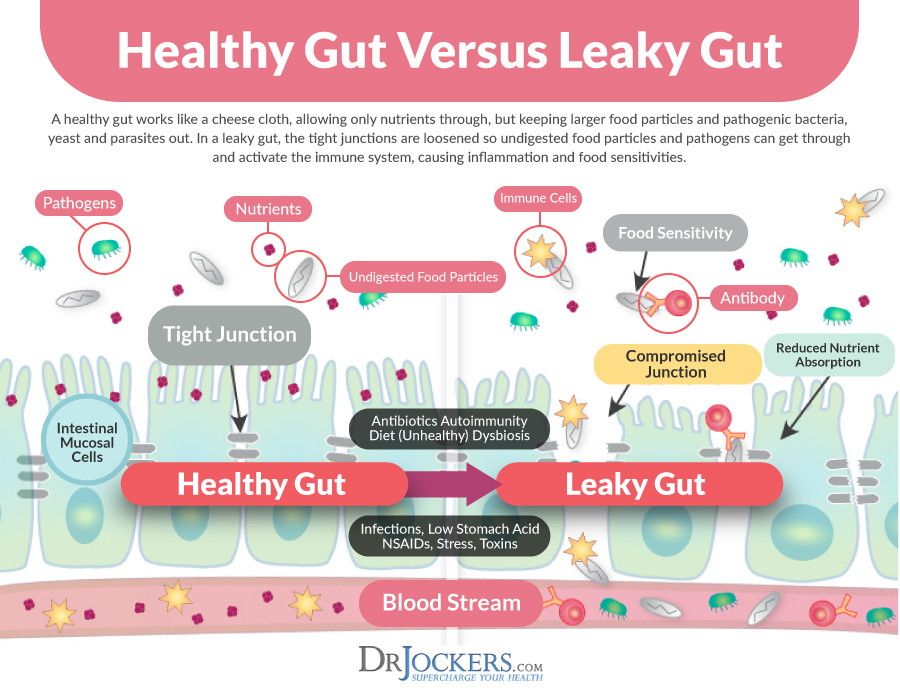
The human body is naturally designed to detect foreign agents in the body such as toxins or cancer cells. Antibodies are created to seek and destroy these harmful invaders flagged as potential threatening agents called antigens. Although these foreign antigens are looking to fit in, once the antibody recognizes them as invaders they alarm other cells to attack and remove the antigen immediately (2).
When the immune system confuses normal compounds with harmful antigens such as gluten, its defense mechanisms maintain the body in a chronic state of inflammation. A cascade of destructive physiological effects occurs which potentially leads to abnormal tissue growth or organ dysfunction (1).
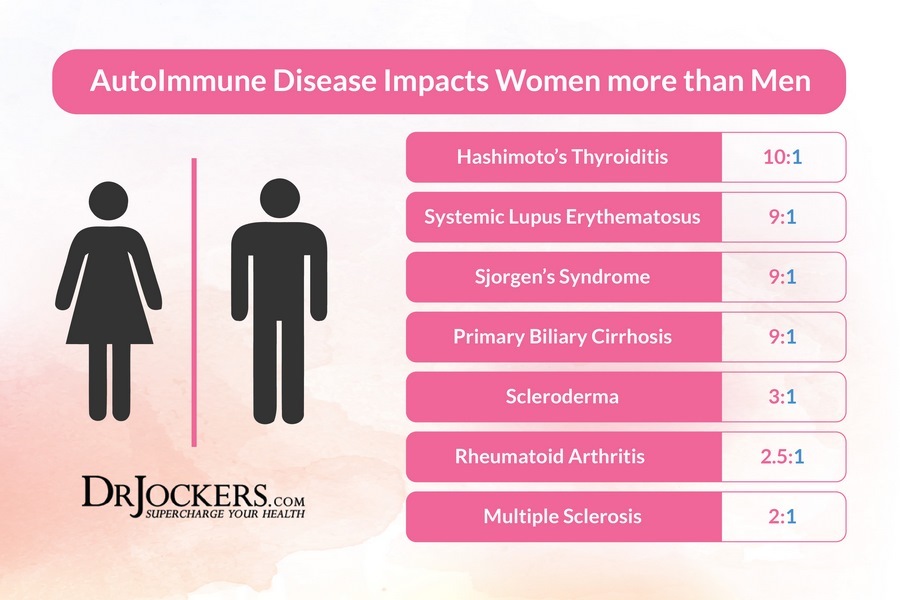
Common Autoimmune Disorders
The following is a list of common autoimmune diseases and autoimmune related disorders compiled by the National Institute of Health (1, 2). There are many others that are not listed. Chances are that you may suffer from one of the following disorders yourself or you know someone who does.
- Celiac disease
- Type 1 diabetes
- Addison’s disease
- Systemic lupus
- Multiple sclerosis
- Grave’s disease (Hyperthyroidism)
- Rheumatoid arthritis
- Hashimoto’s thyroiditis
- Psoriasis
- Sjogren’s Syndrome
- Ulcerative colitis
- Scleroderma
- Crohn’s disease
- Chronic Lyme Disease
Do You Have Any of These Symptoms?
Depending on the disease, symptoms of autoimmune dysfunction involve inflammation in the body that may manifest itself in a variety of ways. The most commonly affected organs and tissues include red blood cells, blood vessels, muscles, joints, endocrine glands (thyroid gland, ovaries, and testes for example), connective tissue (such as tendons and bone), and the skin. (2)
The following is a list of symptoms that may indicate your immune system is not functioning properly: (1, 2)
- Fatigue
- Reoccurring fever
- Joint pain and stiffness
- Skin rash
- Abdominal pain or discomfort perhaps associated with irritable bowel syndrome (IBS)
- Anemia or any known vitamin or mineral deficiency
- Mood changes
Heal with Dietary Lifestyle Changes
Many of these autoimmune complications are treated using immunosuppressive medications which can put the body at greater risk of harmful infections.
Fortunately, more evidence shows that dietary lifestyle changes can decrease the severity of these symptoms, halt the progression of disease and possibly prevent the problem from occurring from the start (1, 5).
Omega-3 Fats Decrease Inflammation
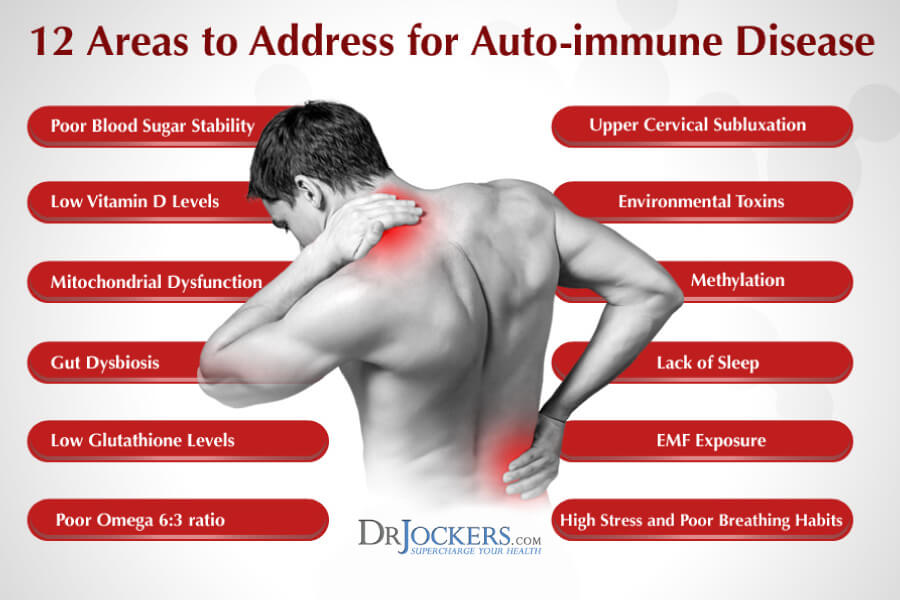
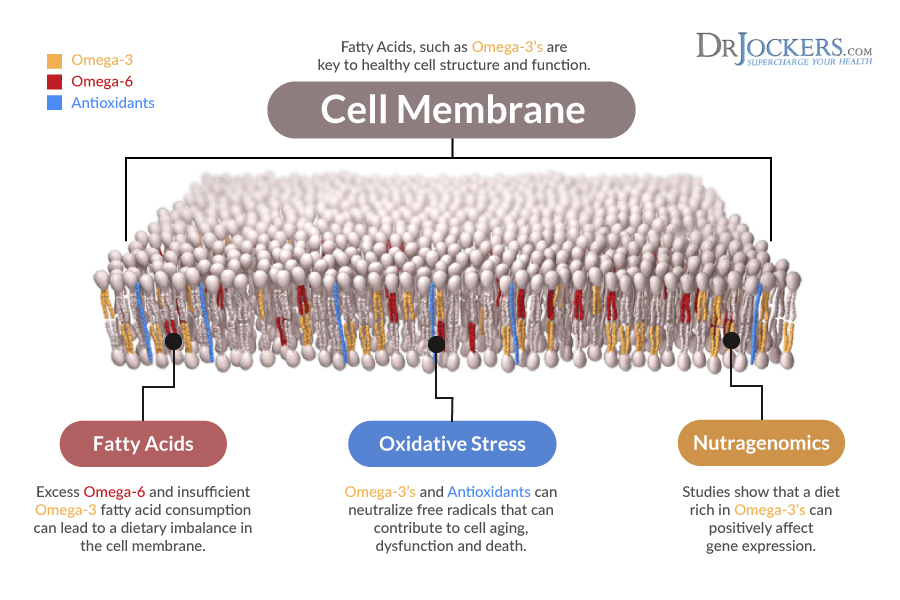
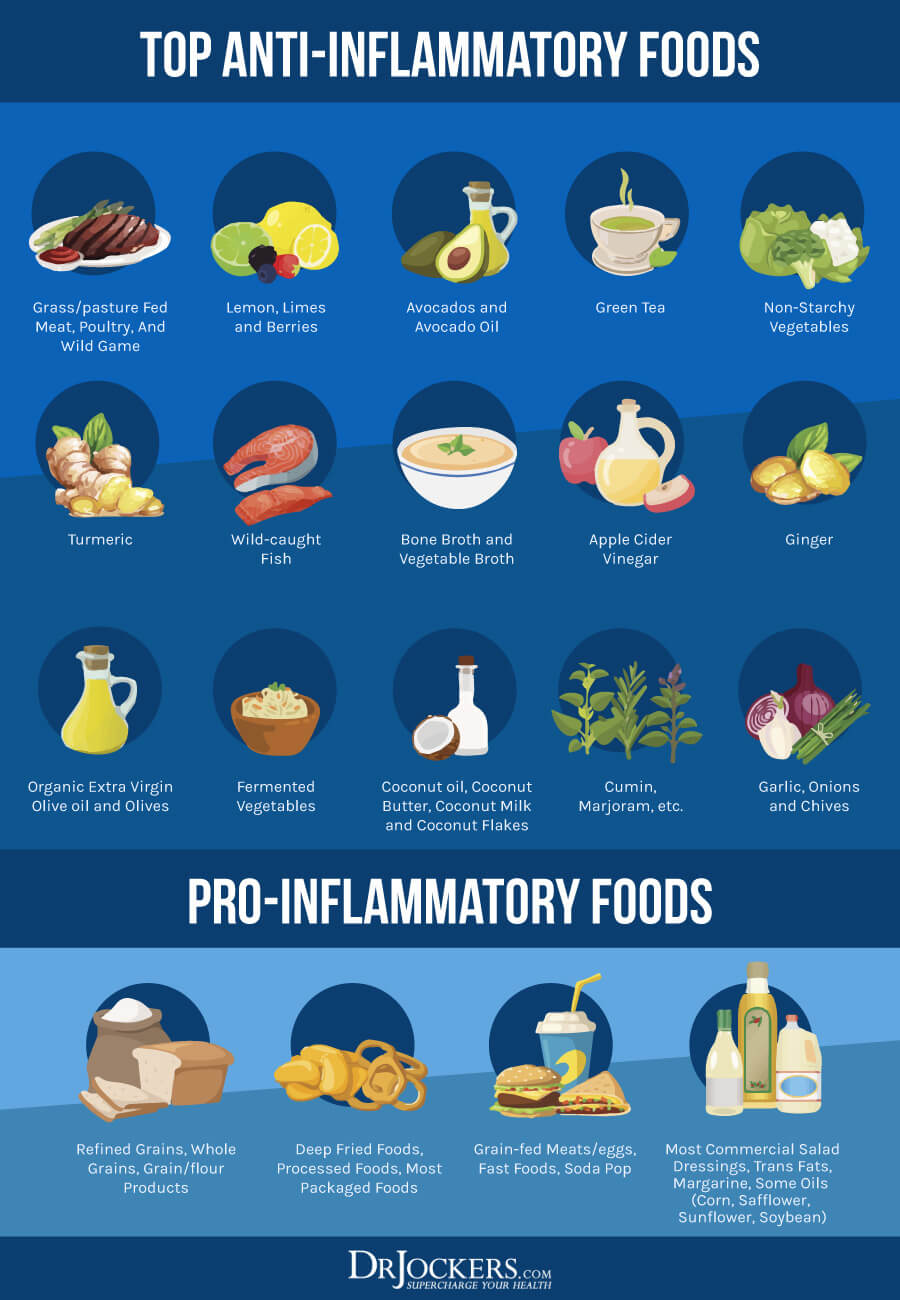
The average American diet today consists of an unbalanced proportion of omega-3 fatty acids to omega-6 fatty acids. Ideally, the human body requires omega-3 fatty acids in greater concentration because they produce anti-inflammatory effects. Although omega-6 fatty acids are necessary, a higher concentration of omega-6 fatty acids in our diet from processed foods, and high amounts of vegetable oils is associated with an increase in molecules which trigger inflammation. (1, 7)
Individuals with different autoimmune diseases have shown a significant improvement in their symptoms while taking fish oil supplements. Patients with rheumatoid arthritis showed a 73% decrease in their drug treatment use and 60% of patients who had Crohn’s disease experienced a decrease in their relapse rate. (11)
Fatty acids are attributed to decreasing immune mediated inflammation. Fatty acids suppress antibodies that alarm the immune system for defense and improve the signaling pathways of cells that cause inflammation.
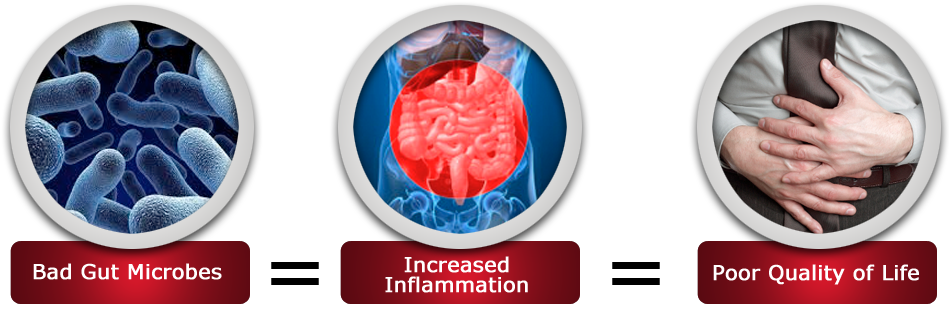
Promote Gut Health
The gastrointestinal tract contains the greatest concentration of immune cells in the body and maybe the activation site of fighter cells known as T-cells (9). Diets associated with chronic inflammation of the gut are therefore at a greater increase of developing an autoimmune disease.
Increased intestinal permeability allows food allergens to pass through the intestinal wall stimulating the production of antibodies. As you now know, specific antibodies seek to destroy the foreign invader by releasing fighter T-cells which cause chronic inflammation of the intestines. These fighter cells are also released into neighboring tissue and the bloodstream. As a consequence, the entire body is susceptible to an immune response resulting in fatigue, muscle stiffness, and skin reactions. (10)
The result of a chronic autoimmune response and decreased gut health increases the susceptibility of individuals to develop more than one type of autoimmune disease. Researchers found that 30% of patients with celiac disease also suffered from another autoimmune disease or autoimmune related problem such as irritable bowel syndrome (IBS) (10).
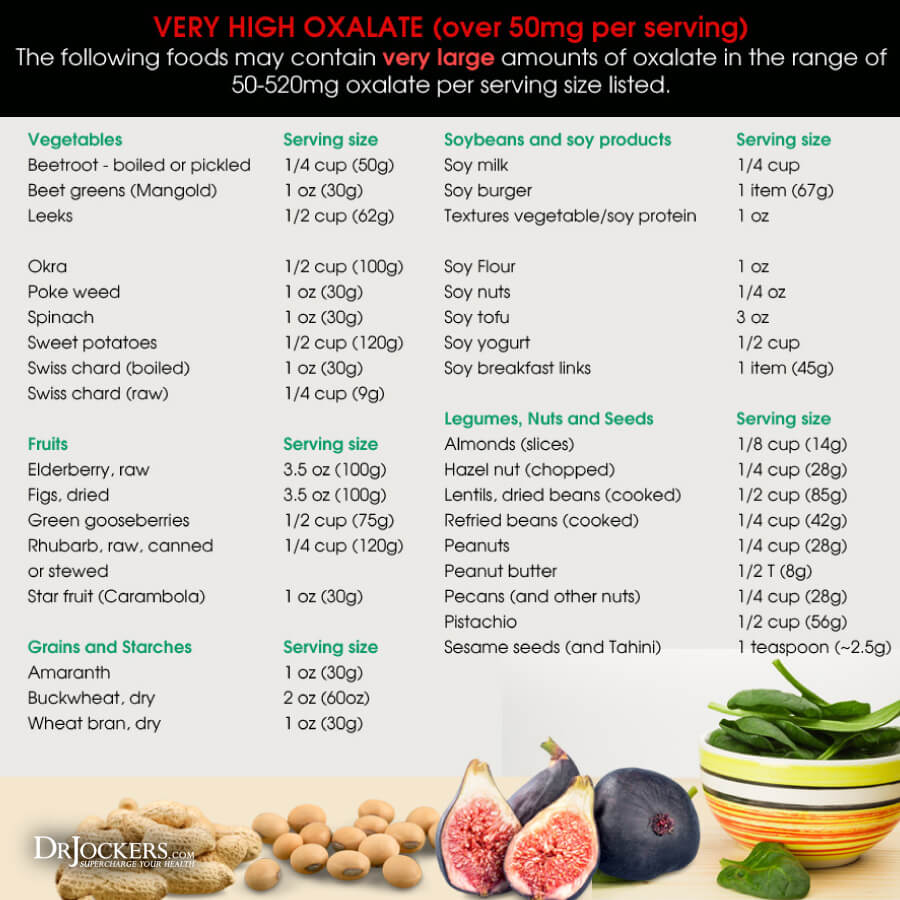
Oxalates and Autoimmunity:
If you are experiencing symptom flare ups with no known reason, oxalates may be a source of inflammation for you. Detecting if oxalates may be triggering an autoimmune response in your body can help you heal sooner.
Oxalates are naturally occurring compounds in nature found in many protein alternatives such as soy as well as grains, nuts, and some fruits and vegetables. Although some of these foods can be excellent additions to a healthy diet, an unhealthy gut can lead to chronic inflammation, nutrient deficiency, and oxidative stress, and damage to the body. (12)
Antioxidants Reduce Inflammation:
Theoretically, increased antioxidants can decrease oxidative stress which promotes tissue damage and therefore directly correlate to reducing inflammation, chronic illness, and autoimmune disease (8). One study found that diets supplemented with antioxidants and lower in total fat and caloric intake delayed the onset of Lupus symptoms by stimulating a healthy immune system (6).
Antioxidants protect the brain from oxidative stress known to cause aging and the loss of cognitive function (3). The healthy maintenance of the gut and mind interaction is crucial to healthy aging and vitality.
Vitamins which act as antioxidants have anti-inflammatory properties inhibiting cytokine activity in autoimmune diseases which signal cells for an inflammatory response. Many herbs high in antioxidants such as curcumin derived from turmeric have been shown to exhibit similar anti-inflammatory control as do synthetic drugs such as aspirin. (1)
B Vitamins and Methylation:
Folate, B-6 and B-12 have antioxidant properties. Vitamin B-6 has specifically been shown to inhibit macrophages from engulfing foreign matter associated with autoimmune diseases (1). Vitamin B-6 deficiency is also positively correlated with increased sensitivity to oxalates in food (12). (7)
Individuals with MTHFR gene mutations have a lowered ability to produce the key antioxidant glutathione. Glutathione is critical for detoxification and immune modulation. These individuals are at a much greater risk for developing autoimmune or chronic inflammatory diseases (17).
They need extra methylation support nutrients such as methyl-folate, methyl-B12, zinc, magnesium, riboflavin, and B6 (18).
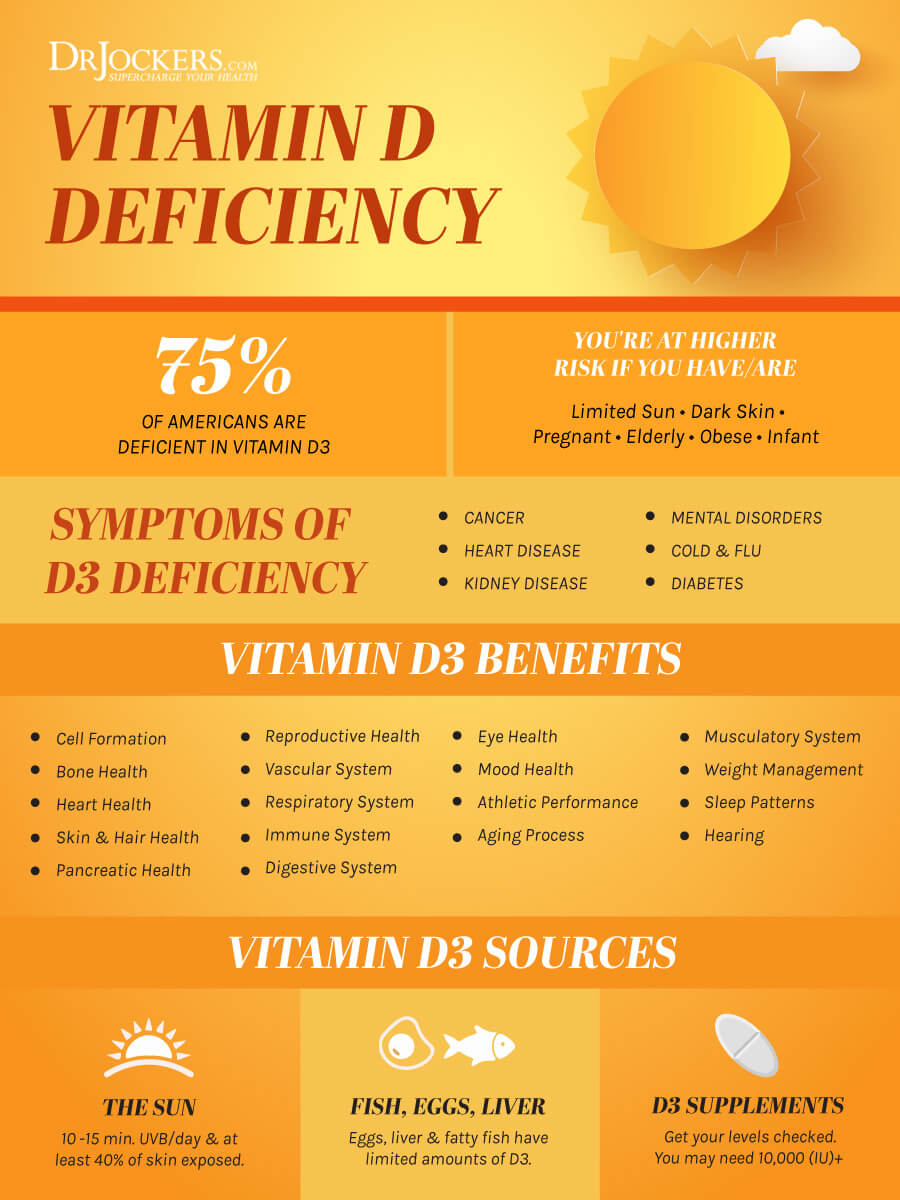
Vitamin D
Vitamin D3 plays a critical role in the development, coordination, and control of the immune system. Individuals with vitamin D3 deficiencies are at a much greater risk for the development of an auto-immune disease or chronic inflammatory disease. Supplementing to boost vitamin D3 levels can be very effective in reducing inflammation (19).
Studies have found that biologically active vitamin D is linked to a decreased risk of type-1 diabetes in which the pancreas does not produce insulin. Sunshine is a natural source of vitamin D. People in geographical locations that see fewer hours of sunshine have higher rates of type-1 diabetes (9).
Choose the Right Proteins
Proteins break down into amino acids and their sequence can promote inflammation. Researchers are beginning to find that although such triggers as gluten cause an autoimmune response in people with celiac disease or gluten sensitivity, it is the chain of amino acids that are contained in the gluten that damage the small intestine (9, 10).
Wheat, soy, and milk have all been associated with promoting type-1 diabetes due to how the body perceives the protein contained in these common food allergens. Countries that consume refined wheat flour as a major food source found that there is a higher incidence of type-1 diabetes. (9)
Opt instead for organic, pasture-raised meats such as turkey and lamb and wild-caught fish high in omega-3 fatty acids like Alaskan salmon.
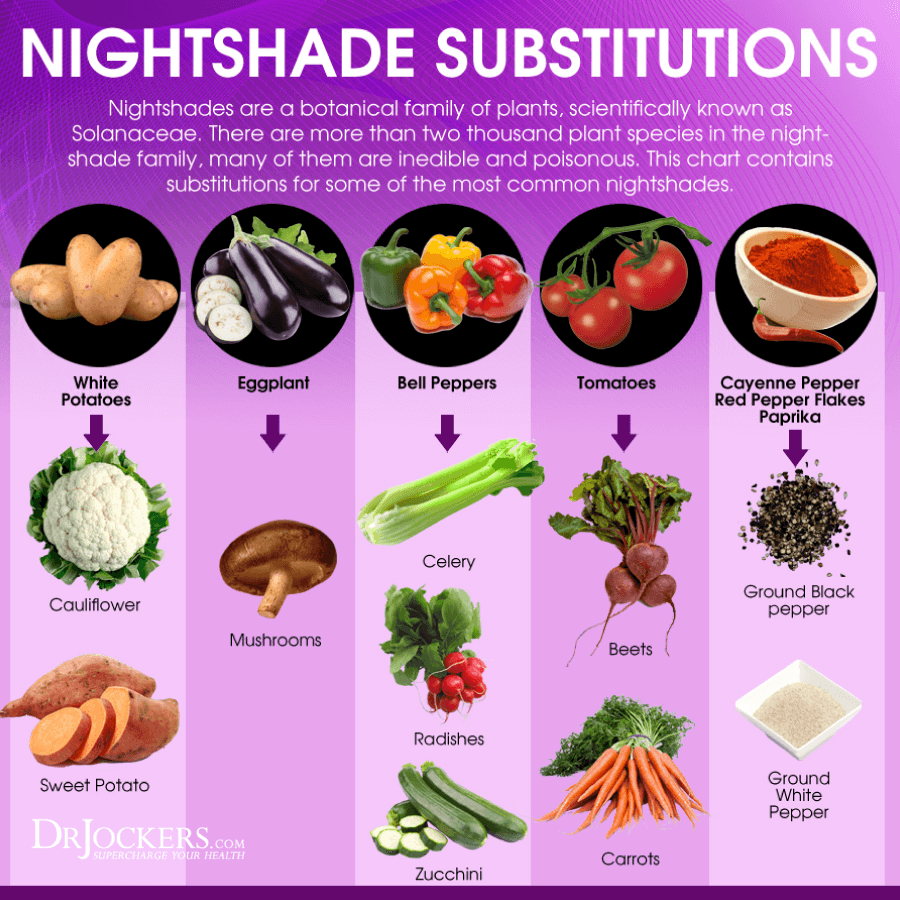
Avoid Nightshades
Avoiding nightshade vegetables such as tomato, white potato, and any pepper variety can help to improve an unhealthy autoimmune response. Nightshades can increase calcium deposits in tissue which causes chronic inflammation leading to a cascading effect of adverse health consequences.
Damage to the kidney and liver can trigger autoimmune diseases such as rheumatoid arthritis and diabetes. (13, 14) Not everyone responds negatively to nightshades, however, many individuals with auto-immunity struggle with these foods.
Testing for Food Sensitivities:
Do you suffer from a chronic autoimmune disease or condition that inhibits you from living an optimal lifestyle? Testing for sensitivities to any known food allergens by using the following biofeedback test or more extensive blood work.
Food sensitivities differ from food allergies in that food allergies are an IgE antibody reactions that are immediate and often life-threatening reactions. Food sensitivities are an IgG antibody reaction that is delayed and causes subtler imbalances in the body. Both of these create inflammation, with food allergies creating a highly acute inflammatory attack while food sensitivities cause the low-grade, chronic inflammation that is characteristic of autoimmune conditions.
While food allergies are typically known early in life, it is the food sensitivities that most people never think about. You can do an analysis with both at home biofeedback testing and blood testing to discover any hidden food sensitivities you may have.
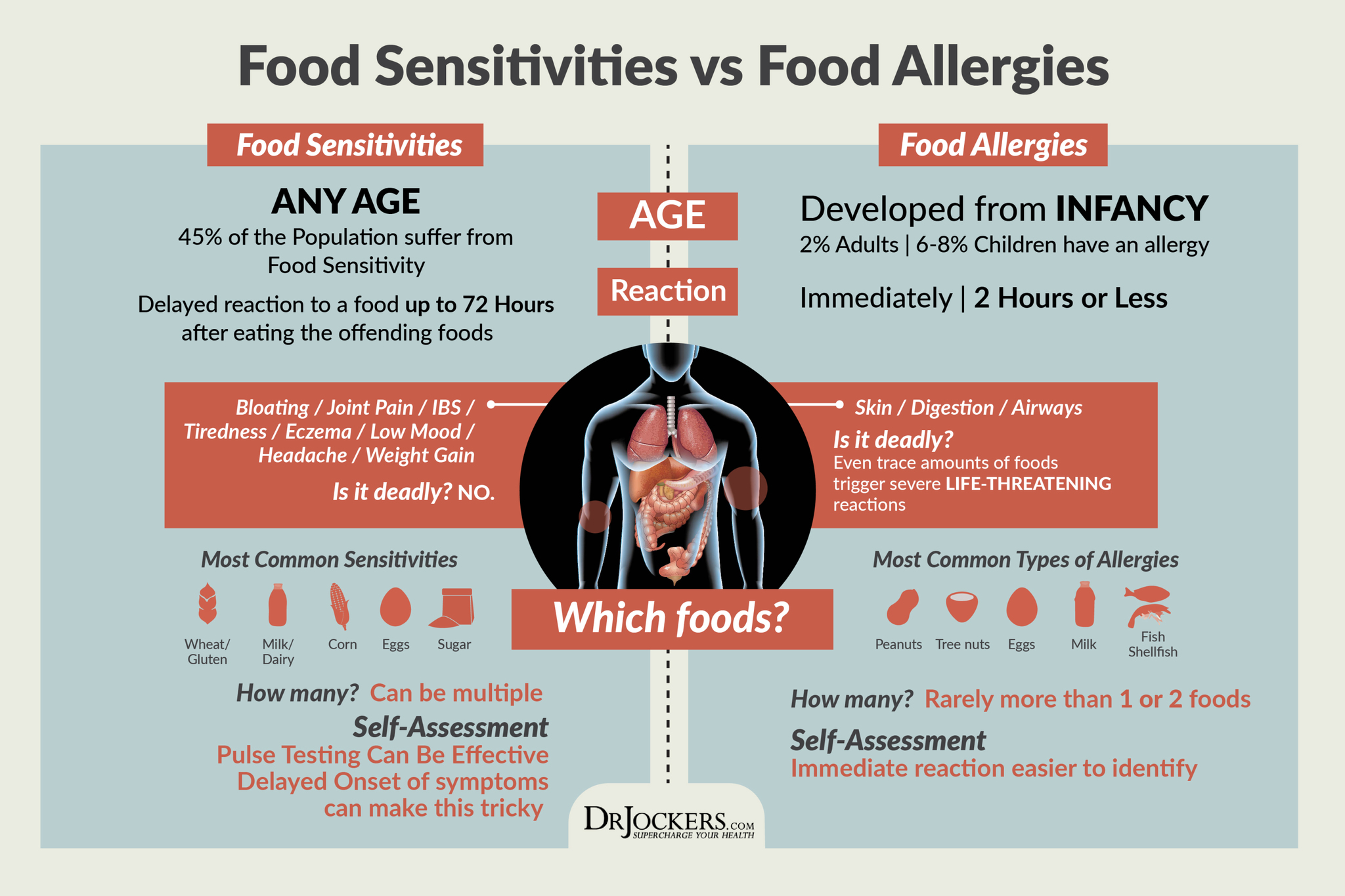
Biofeedback Test
Come to a relaxing state lying down in an environment where there are no factors that may contribute to increasing your heart rate. After a few minutes, determine your resting pulse. Take a food allergen in question such as a peanut and place it on your tongue letting it remain there for approximately 20 seconds. Follow up by counting your resting pulse a second time. (16)
Negative Response: You may have no sensitivity to the specific nut you tested if your heart rate does not increase more than 1 bpm.
Gray Area Response: Your resting pulse increases by 2 or 3 bpm and further testing should be completed.
Positive Response: Heart rate increases by more than 4 bpm and you have identified a source of food sensitivity or intolerance.
You can find more information on biofeedback sensitivity training here. You may decide to receive more objective testing in order to determine more definitive conclusions. Allergy tests are available as well as blood tests which detect the number of antibodies and different types of proteins representative of a malfunctioning autoimmune response.
Autoimmune Diet Plan
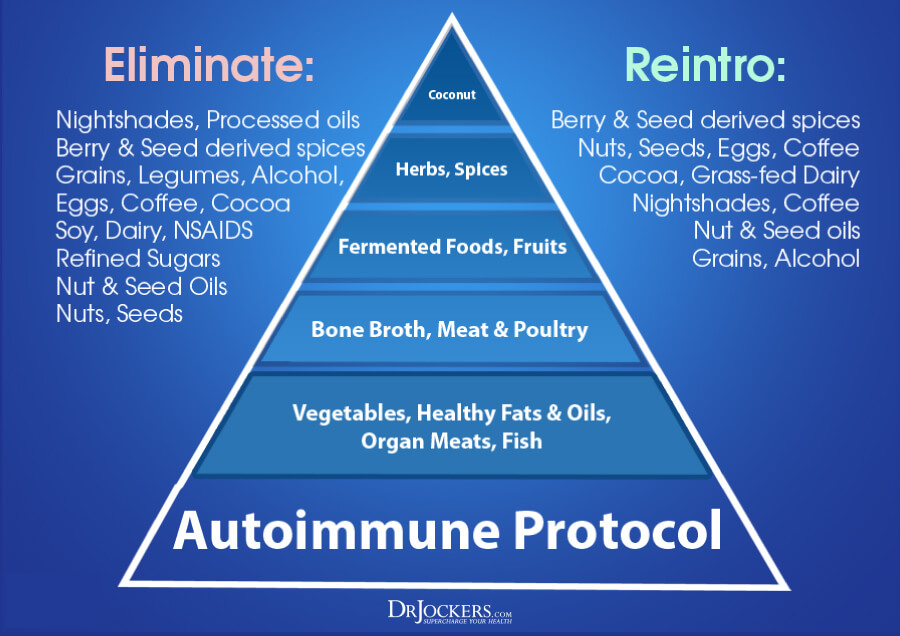
To get started on an autoimmune diet plan, download the shopping guide here (4). Following the diet for 90 days is crucial in resetting your body’s immune response.
The diet eliminates nightshade vegetables, dairy, eggs, chocolate, nuts, and caffeine sources such as coffee and chocolate. It is high in low-glycemic fruits, organic vegetables, organic, grass-fed, and pasture-raised protein sources, wild-caught fish, fermented foods, and healthy fats.
You can also sign up for aip meal plans or autoimmune protocol diet plans to ease your transfer to a healthy diet that supports your body when dealing with an autoimmune disease.
Pork and shellfish are eliminated because they are one of the most highly toxic foods you can consume. Pigs and shellfish are scavengers and pollutants containing heavy metals and toxins which are easily absorbed along with the animal’s hormones.
People exposed to toxins such as coal miners have an increased risk of developing an autoimmune disease such as rheumatoid arthritis by a minimum of three times the normal expectancy (6).
A Lifelong Commitment
Resetting your autoimmune system can leave you with phenomenal physical results. Preventing flare ups of symptoms from reoccurring following a strict 30-90 day autoimmune diet regimen requires a change in lifestyle.
Although you may be able to slowly reintroduce limited quantities of inflammatory foods back into your diet, maintaining a healthy gut can prevent the severity of an autoimmune response. Be vigilant for the initial period and then slowly reintroduce the fringe foods (nuts, seeds, eggs, cocoa, coffee, nightshades, legumes, etc.) back in.
I typically recommend adding one fringe food every 3 days while you analyze how your body is responding to that individual food. If you notice more inflammatory symptoms such as pain, headaches, fatigue, acne, eczema, allergies, or clearing your throat a lot then it is a sign you are not tolerating that food, and it should be eliminated for another 90 days before reintroducing it in the same manner.
 Lifestyle Tips
Lifestyle Tips
The following tips can decrease the severity of symptoms if you have an autoimmune disease, prevent an unhealthy autoimmune response, or stop the progression of an autoimmune condition. (1, 2, 3, 9, 10)
- Breastfeeding is recommended to introduce foods to babies while they are developing an immune system and prevent an autoimmune response later in life.
- Practice stress reduction: and yes, laughing amongst friends counts.
- Exercise decreases cortisol levels and helps to balance hormones.
- Avoid unnecessary use of antibiotics. Antibiotics deplete the healthy bacteria in your gastrointestinal tract leaving you at risk for harmful pathogens.
- Detox the body of toxins and chemicals from non-food sources such as skin and hair care products. Your skin is a sponge, and your body does not need any additional pollutants.
AutoImmune Nutritional Tips:
- Switch to organic teas such as green tea or herbal teas instead of coffee.
- Commit to taking a probiotic and prebiotic daily to promote healthy gut microflora
- Eliminate refined sugars which cause inflammation and increase the variety of fruits and vegetables to aid in detoxifying the body of irritants.
- Replace industrialized vegetable oils with organic, cold-pressed coconut oil or extra virgin olive oil to supplement your diet with healthy fats.
- Avoid any food source that does not come from nature such as artificial sweeteners, synthetic food dyes, and preservatives.
- Buy organic. Chemical toxins such as pesticide residue destroy the healthy microflora of the gut thereby creating an environment susceptible to an unhealthy autoimmune response.
- Drink purified water to avoid contaminants such as heavy metals and chemicals.
Why suffer any longer? Are you ready for a lifestyle change and a healthier you? Commit now to heal your body for better health and happiness.






Hello Dr David
Mind blowing information on Autoimmune problems and it’s possible management. Great!!!!!!!
In a typical patient one should remove all the nuts or should eliminate like peanut, almonds, pistachio etc. Please suggest then what other nuts, legumes as well as seeds one can eat?
With regards,
Dr Prakash
Dr Prakash,
Everyone is different and some will be able to handle certain nuts and seeds while others will not. Typically, I will have the client stick to only flax seeds, chia seeds and pumpkin seeds in the beginning phase – 30 days. Then they can do food sensitivity biofeedback testing to see what else they can tolerate.
Hi Doc,
I am also one of those who are suffering from autoimmune disease. But story is a little bit a roller coasters from Day 1 I had the confirmation. Back in my country, I went to Rhuematologist and presented my symptoms without blood test yet, He diagnosed me having SLE-that was 2013. From then on I am
Already occupied that I do really have and been taking Plaquinel and steriods intermittently, a trial
From Imuran(which i couldn’t tolerate the adverse effect so i decided to stop).However, when we moved here in the US in 2017, i seek another advice from Rheumatologist, we ran some test coz i am not really comvinced that i have SLE based on the symptoms i am experiencing. We found out that i have “mixed connectibe tissue disease”accdg to my MD,its a rare type of autoimmune diease that its symptoms is a combinations of
All types of autoimmunes.
So, based on the test, i am not
Positive in sLe, i have hashimoto, i have fibromyalgia but never positibe from RA, i have skin scaling and redness at times but never been positive from Psoriasis. We
Continue my Plaquenil plus steriods at low dose 2.5 whenever i cant tolerate the flare and have to taper down slowly. i have been struggling with my dietary plan since the beginning.
I hope you could help me. Thanks a lot-kitty
So sorry to hear that! Be sure to follow what you read here and also in this article: https://drjockers.com/heal-autoimmune-disease/
Thanks Dr David
Deeply appreciative for this comprehensive guide! Any advice for dietary or supplement changes to increase adrenal function?
I had a Lupus diagnosis in 2010. 2014, Lupus Nephritis. I’ve been on high to lose dose Prednisone since 2010.
Thank you!
So sorry to hear about this. I would highly recommend following this autoimmune nutrition plan and taking some adrenal support supplements such as Adapt-Strong that I have in my online store. I also have a whole Adrenal Support program you can find here https://store.drjockers.com/collections/dr-jockers-products/products/adrenal-support-pack?variant=2476746369
Can auto iimmune diease such as hashimoto ever be cured or only ever managed with this auto immune diet?
Hey Annette – yes the AutoImmune nutrition plan is the foundation for healing autoimmune conditions such as Hashimoto’s. It is not a “cure” as that would imply that the condition would never return. If you come off the nutrition plan and live a stressful, unhealthy lifestyle the condition will come back. However, the condition can be put into remission, even permanently can be done through diet and healthy lifestyle practices. Here is a helpful article on hypothyroidism: https://drjockers.com/18-strategies-to-beat-hypothyroidism-naturally/
Good Afternoon Dr. Jockers,
I have several Auto-Immune conditions (MS, Hypo-Thyroid, Reynards, Interstitial Cystitis). I believe I have one more, but I can’t think of it right now. Clearly brain fog as well as Sleep deficient. Dark bags under my eyes etc. Almost all of these have been diagnosed 6-7 years ago and I am now about to turn 52 this February.
I was interested in starting your program, but wasn’t sure what I should start first. I have traveled to other countries, so wasn’t sure if I should do a parasite cleanse first before starting the Auto-Immune Elimination Diet plan, etc. If you have any thoughts on what I should do that would be great. Currently, I have been controlling my M.S. via Diet, Supplements, and Exercise and no prescription medication. I am on Armor Thyroid. Lots of B Vitamins, D, etc. and practice a Gluten Free Diet.
Thank you for all this great information on your site. Now I am ready to move to the next step.
Blessings
HI Dr. Jockers, I always love your comprehensive and detailed articles. Thanks for sharing this wonderful information. I was just wondering if this diet plan will work for someone with Vitiligo, since its also termed under an Autoimmune disorder?. Also are there any other recommendations or information you could share pertaining to Vitiligo.
Thanks
I have few patches on my beard it’s due to alopecia areata autoimmune ,I am too much worried,how it will recover and how many it take to recover
Sorry to hear about this Smeet! I would highly encourage you to begin following this sort of nutrition plan.
I thought it was interesting reading through this article and seeing the many ways autoimmune treatments can be done naturally. The article also states that many people suffer from autoimmune diseases unknowingly. What signs should I look for to identify and autoimmune disease? I suspect my son my be allergic to gluten.
Sorry to hear about this John. Here is a helpful article for you: https://drjockers.com/5-steps-to-heal-autoimmune-disease/
Great article. Valuable tips.
Thank you Minash!
Hello! I have an 8 year old son with alopecia universalis. Autoimmune hair loss. What is your advice for someone so young? Thank you in advance!
Hey Kristy, Sorry to hear about this! You may want to try an elimination diet to try and calm his autoimmunity. Email nutrition@drjockers.com for some deeper guidance on this!
Blessings!
Thank you! I sent an e-mail! Have you helped people with this condition before?
This is a wonderful article with so much information. My mother who was previously an “energizer bunny” has had several issues recently.
She has had Pernicious Anemia for the last 20 years or so. She also has Osteoporosis. Her stomach has always been sensitive, but had to have her gallbladder removed about 4 months ago. She had developed a rash, which at first the Dermatologist thought was Scabies, but when it didn’t clear up and blisters developed, a skin biopsy was performed and she has been diagnosed with Bullous Pemphigoid. I’m very worried about her as this is a serious autoimmune disease.
Besides a gluten free diet, are there supplements that can help her?
Hey Ilene, so sorry to hear about this. It’s not just gluten but all common food sensitivities. An autoimmune elimination diet would be helpful: https://drjockers.com/autoimmune-elimination-program/
As for supplements, I go into that here: https://drjockers.com/5-nutrients-heal-autoimmune-disease/
Is this a good choice for allergies and asthma? I get a skin rash and also have problems around my eyes.
What about the high histamine foods on this diet?
Hey Pat! Yes, allergies are an Auto-immune response. Anything you can do to re-coordinate the immune system can be very helpful. If you react to high histamine foods you will definitely want to avoid those for the time being and possibly look at lab markers for histamine intolerance.
I really enjoyed the infographics on your article. It really helped to see a diagram of what you were explaining. Really great information.
I have not eaten any gluten, soy, corn, nuts, nightshade, for a very long time, Years. I was eating a small amount of grains, such as millet and brown rice, and eggs once or twice a week, and I gave them up, thinking that my digestive issues and dry eyes would get better, but things are getting worse. I was drinking two cups of coffee per week, so I thought I would give that up for one month to see if it was the culprit, but it was not, I did not feel any better. A stool test came back that I have candida, one of the commensal bacteria was high, and Secretory IgA is low. I was surprised I have candida because I have no cravings at all. I don’t like sweets, and I go out my way to avoid sugar, bread, or pasta. I don’t miss or want these foods. I even follow a low oxalate diet. So I am not sure why I have all these problems. Could it be old age?
It is hard to say without more information. There could be several factors contributing to this. You may consider working with on our health coaches on this. We do have a great candida product: https://store.drjockers.com/products/copy-of-candida-combat2
I live in California and am dealing with possible chronic pancreatitis. I had my gall bladder removed in 2010 but my digestion has been poor since. For awhile taking betaine HCL felt like a cure. Since May I’ve been taking Digest Gold and Lypo gold with every meal, and none of my meals have over 10 to 11 g of fat. I have lost over 30 pounds since May and I’m worried about losing more. I was able to have low-fat milk and tested negative for gluten intolerance so I tried to eat healthy whole-grain bread every morning with powdered peanut butter. I was taking in an average of 1600 cal a day and no more than 45 g of fat a day but I’m still not gaining weight. Clearly something isn’t working I don’t know where to start is there a way to get help for coaching from your team if I don’t live in Georgia? All doctors do is throw medicine at you and send you on your way and you get worse.
Hey Heidi! Yes, my team does consultations over Skype or phone! You can email michael@drjockers.com to get started!
Do you think that biofilms play a role in autoimmune diseases?
Hey Brie, moreso the underlying pathogens that are creating the biofilms and causing a chronic inflammatory response! Both need to be addressed for sure.
I’ve been diagnosed with graves disease a few months ago.
But , I have finally discovered, that I have had auto immune problems for close to 5 years!
Had hasimotto disease, rumitoid arthritis, eczema, psoriasis, polyrhumatica…
I am lost, and dont know how to proceed.
I have read so many different things from different sites, on what to eat, etc.
I will not take the meds from endocrinologist, I want to do this naturally.
Please help me begin, the correct way.
Thank you so much , marie
Hey Marie! Sorry to hear about this, here is a good place to start: https://drjockers.com/7-factors-causing-autoimmune-conditions/
You can also reach out to Michae, our functional diagnostic nutrition practitioner who would be happy to put together a plan for you! His email is michael@drjockers.com
I have recently been diagnosed with lichen sclerosus and don’t know where to start. I also have IBS. Can you help?
Thank you.
Thank you for all that you do to bring improved quality of life to all, Dr. Jockers! I have difficulty digesting animal proteins and even plant-sourced fats. My list of food sensitivities is growing and so is my list of autoimmune issues. Would it suffice to begin with your auto immune protocol, or should I schedule an appointment with you or one of your nutrition coaches? I have been gluten, dairy, soy, tomato free for at least 10 years now. I’m having a lot of discomfort in my stomach/intestines area as well as burning pain in my back. Some days it’s a little more than I can handle. Thank you for your direction/guidance.
Sorry to hear about this Gloria! I would recommend beginning the autoimmune diet and also scheduling a consult with one of our health coaches so they can customize a specific plan for you. https://drjockers.com/long-distance-coaching/
Hello
I have Litchen Sclerosus and struggling, please help in any possible way . Any feedback will be appreciated.
Agnes
Sorry to hear this Agnes. Here is a helpful article: https://drjockers.com/autoimmune-disease/