 Celiac Disease: Causes, Symptoms, and Supportive Strategies
Celiac Disease: Causes, Symptoms, and Supportive Strategies
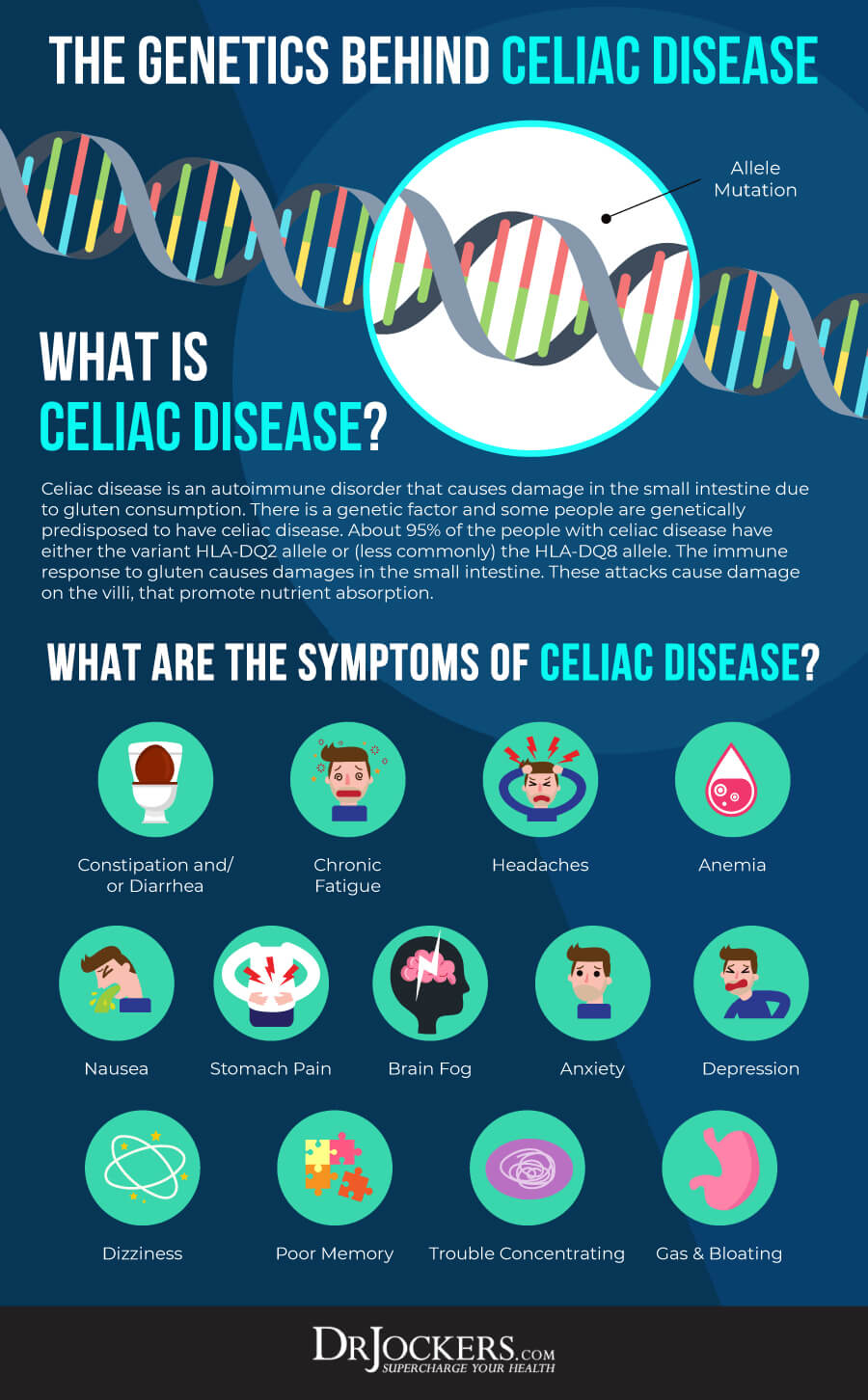
Celiac disease is an autoimmune inflammatory disease. This common condition affects around 1 in 100 people worldwide and is significantly increasing in prevalence. Celiac disease can develop at any age in genetically susceptible people.
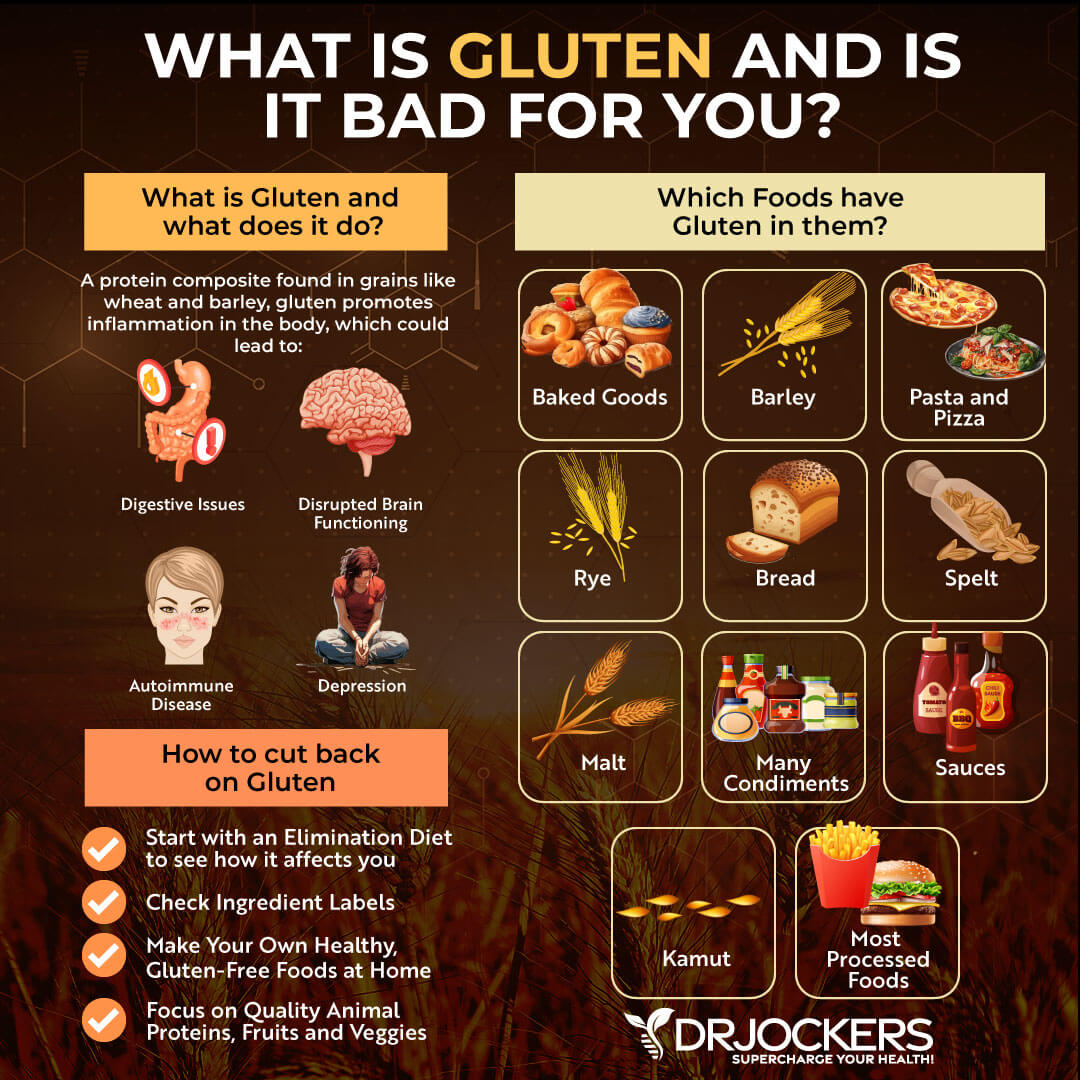
The immune system in people with celiac disease is abnormally sensitive to gluten. Gluten is a protein found in wheat, barley, and rye. When people with celiac disease consume gluten, this causes inflammation and intestinal damage. This can lead to a variety of symptoms and, in some cases, serious complications. Because these symptoms are common in other conditions, celiac disease often goes undiagnosed for many years.
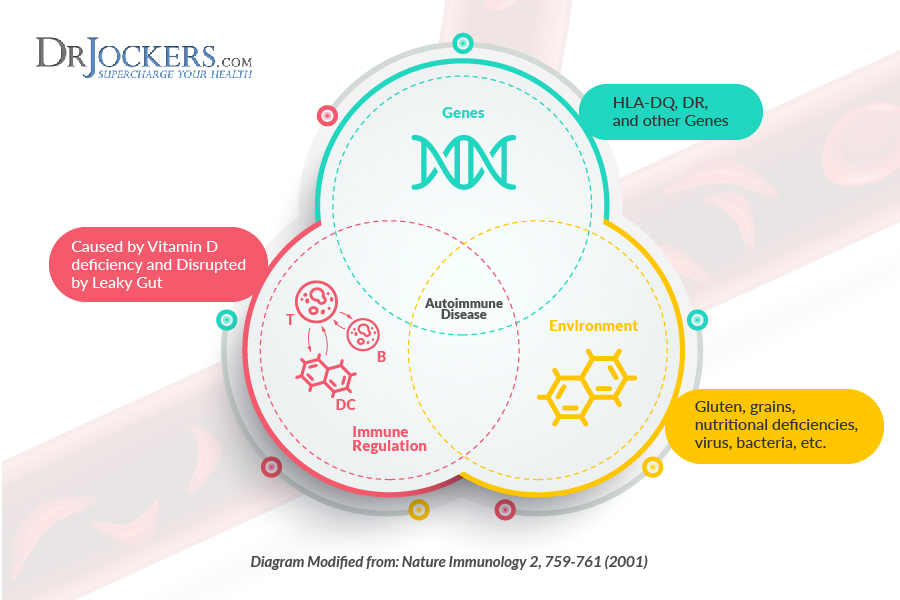
Genetics plays a major role in the development of celiac disease. However, the prevalence of celiac disease has increased significantly in recent decades. This has led researchers to look for environmental risk factors that increase the risk of developing celiac disease.
A strict gluten-free diet is critical for anyone with celiac disease. In addition to avoiding gluten, there are other supportive strategies. These natural strategies will be discussed in this article.
What is Celiac Disease?
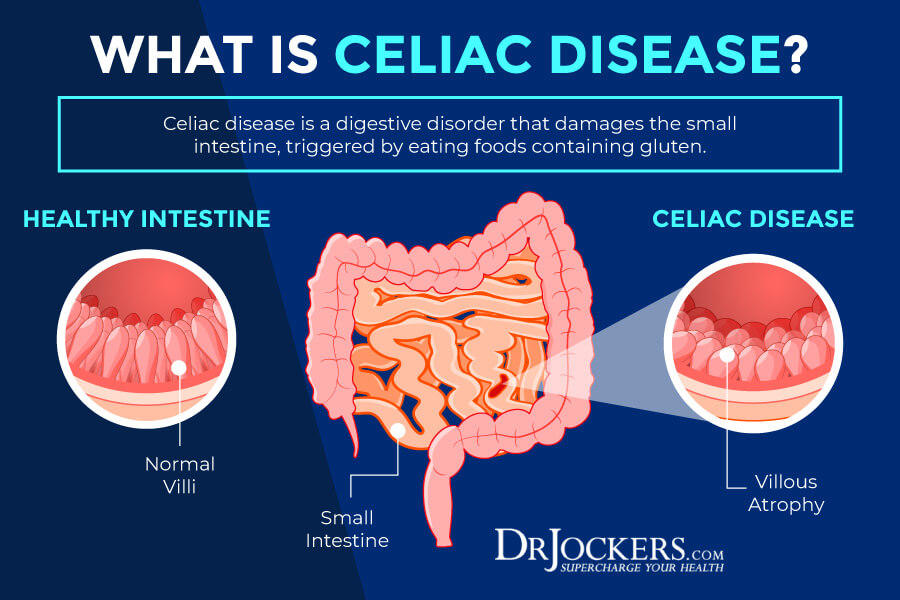
Celiac disease, also called celiac sprue, is an immune-mediated disorder triggered by an abnormal reaction to gluten (1). Gluten is a protein found naturally in wheat, barley, and rye. The two main proteins in gluten are gliadin and glutenin. The gut breaks down gliadin and glutenin proteins into smaller units, called peptides, polypeptides, or peptide chains.
Celiac disease is a common autoimmune condition, affecting at least 1% of the world’s population. It is characterized by the inappropriate activation of the immune system, causes inflammation that damages the body’s organs and tissues, and leads to numerous signs and symptoms.
The classic symptoms of celiac disease result from inflammation in the gastrointestinal tract. This inflammation damages the villi, which are small, finger-like projections that line the small intestine and provide a greatly increased surface area to absorb nutrients. In the disease, these villi become shortened and eventually flatten out.
Celiac disease can develop at any age and affects children and adults worldwide. Symptoms may appear as soon as a person starts eating foods that contain gluten. Gluten can even be found in the breast milk of mothers who eat gluten-containing foods.
Celiac disease tends to be more common in people who have a family member with celiac disease or dermatitis herpetiformis. It is also more common in people with the genetic disorders Down Syndrome and Turner Syndrome. Celiac is associated with other autoimmune conditions including type 1 diabetes, Addison’s disease, and autoimmune thyroid conditions.
Symptoms of Celiac Disease
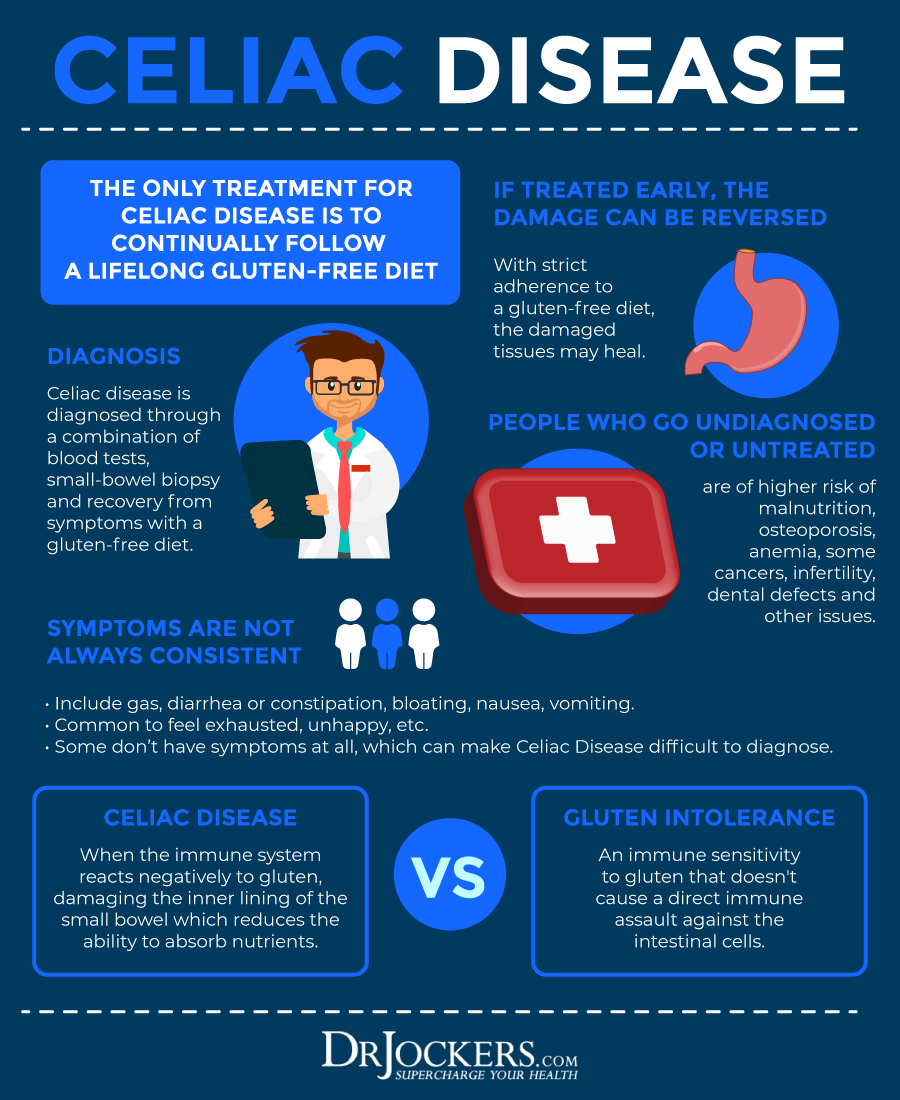
Celiac disease often goes undiagnosed because many of its signs and symptoms are nonspecific, which means they may occur in other disorders. Most people who have one or more of these nonspecific health problems do not have celiac disease. On average, a diagnosis of celiac disease is not made until 6 to 10 years after symptoms begin.
Symptoms range from mild to severe and differ in children and adults. The classic symptoms of the condition result from inflammation affecting the gastrointestinal tract.
- Diarrhea
- Nutrient deficiencies
- Fatigue
- Weight loss
- Bloating and gas
- Abdominal pain
- Nausea and vomiting
- Constipation
- Headaches
- Food intolerances
- Joint pain
Children are more likely than adults to have digestive problems. The most common symptoms in children with celiac disease include:
- Nausea and vomiting
- Chronic diarrhea
- Swollen belly
- Constipation
- Gas
- Pale, foul-smelling stools
Complications of Celiac Disease
Inflammation and poor nutrient absorption may lead to problems affecting many other organs and systems of the body in affected individuals. These health problems may include:
- Malnutrition
- Anemia (usually iron deficiency)
- Loss of bone density (osteoporosis) or softening of bone (osteomalacia)
- Itchy, blistery skin rash (dermatitis herpetiformis)
- Mouth ulcers
- Nervous system injury, including numbness and tingling in the feet and hands, cognitive impairment, problems with balance
- Joint pain
- Osteoporosis: low bone mineral density
- Defects in the enamel of the teeth
- Chronic fatigue
- Poor growth, or delayed puberty in children
- Failure to thrive in infants
- Infertility or repeated miscarriages
- Food intolerances (especially lactose)
- Neurological problems including ADHD, recurrent seizures (epilepsy), and migraine headaches
Inflammation associated with celiac disease may lead to an increased risk of developing certain gastrointestinal cancers such as cancers of the small intestine or esophagus. Liver diseases and lymphoma, a cancer of the part of the immune system that includes the gut (lymph system) are rare complications of celiac disease (1).
Types of Celiac Disease
There are different types of celiac disease (2). These include:
- Classic celiac disease: Inflammation in the GI tract leads to a variety of gastrointestinal symptoms.
- Neoclassic (atypical) celiac disease: A person has celiac disease with variant health problems but no gastrointestinal symptoms. This type may be more common than classic celiac disease.
- Silent celiac disease: A person has no symptoms but has immune proteins in their blood and inflammatory damage to their small intestine.
- Latent celiac disease: A person tests positive for celiac disease but there is no damage to villi that line the intestines.
- Refractory celiac disease (or refractory sprue): A person has trouble absorbing nutrients even when following a strict gluten-free diet because their intestines are severely damaged. IV nutrition may be necessary. Refractory sprue is characterized by chronic inflammation of the gastrointestinal tract, poor absorption of nutrients, and an increased risk of developing a type of cancer—T-cell lymphoma (cancer of the immune cells).
In addition to refractory celiac disease, there are other reasons people with celiac may not respond to a gluten-free diet. These include small intestinal bacterial overgrowth (SIBO), microscopic colitis, poor pancreas function, irritable bowel syndrome (IBS), and difficulty digesting sugars (lactose, sucrose, and fructose) (3).

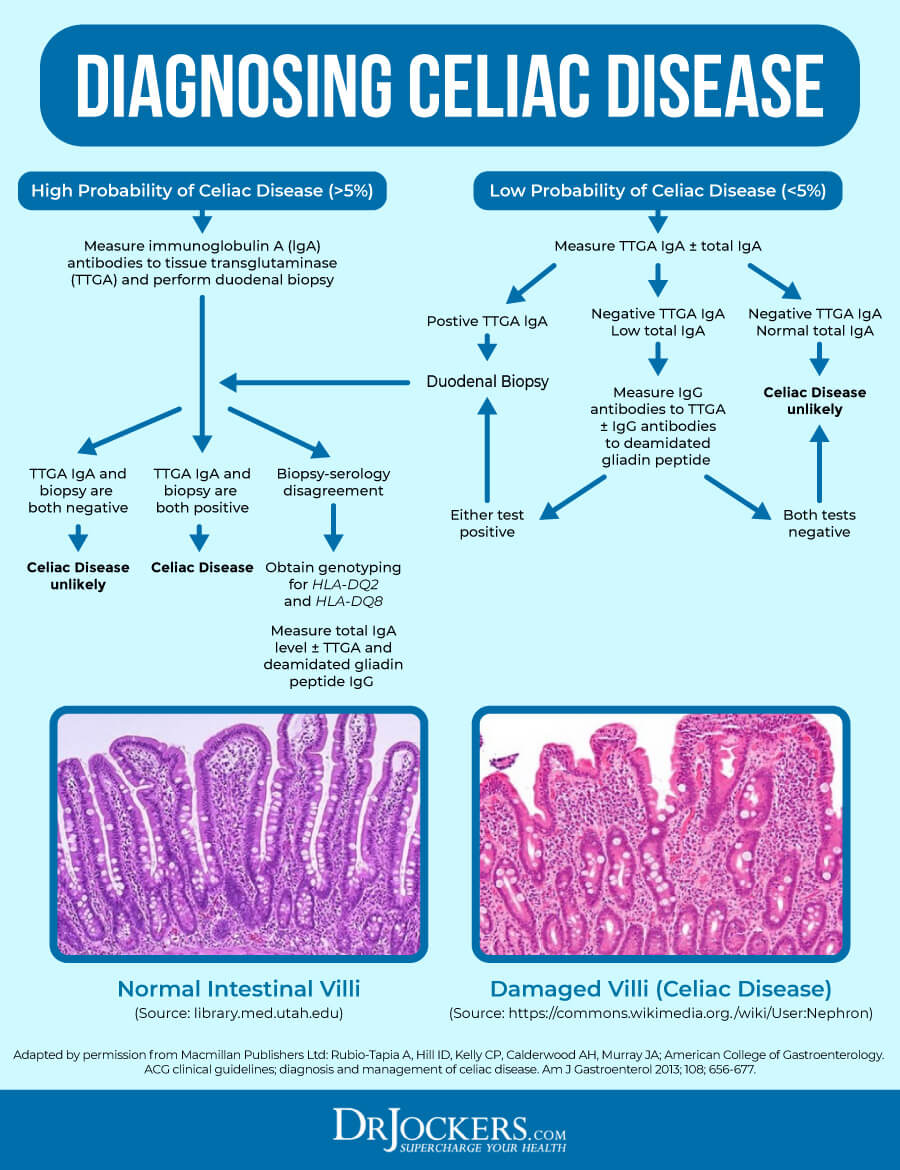
Diagnosing Celiac Disease
Celiac disease can be hard to diagnose. Symptoms often overlap with other conditions such as irritable bowel syndrome and food intolerances. Your doctor may diagnose you with a medical and family history, physical exam, and various tests.
Antibody and genetic testing may be done to help diagnose celiac disease. Blood tests can show whether you have the antibodies that are common in celiac disease. They can also check for the gene variants associated with celiac. Having these variants alone is not enough to diagnose celiac disease because they also are common in people without the disease.
If blood tests suggest you have celiac disease, your doctor may do a biopsy to be sure. The doctor performs an upper GI endoscopy and takes a small piece of tissue from your small intestine.
Skin biopsies may be performed on people with dermatitis herpetiformis. A doctor examines the skin tissue and checks the tissue for antibodies common in celiac disease. If the skin tissue has the antibodies, a doctor will perform blood tests and/or a biopsy to confirm celiac disease.
For some people, a dentist may first identify possible celiac disease. Dental enamel defects, such as white, yellow, or brown spots on the teeth, are a problem for some people with celiac disease, especially children.
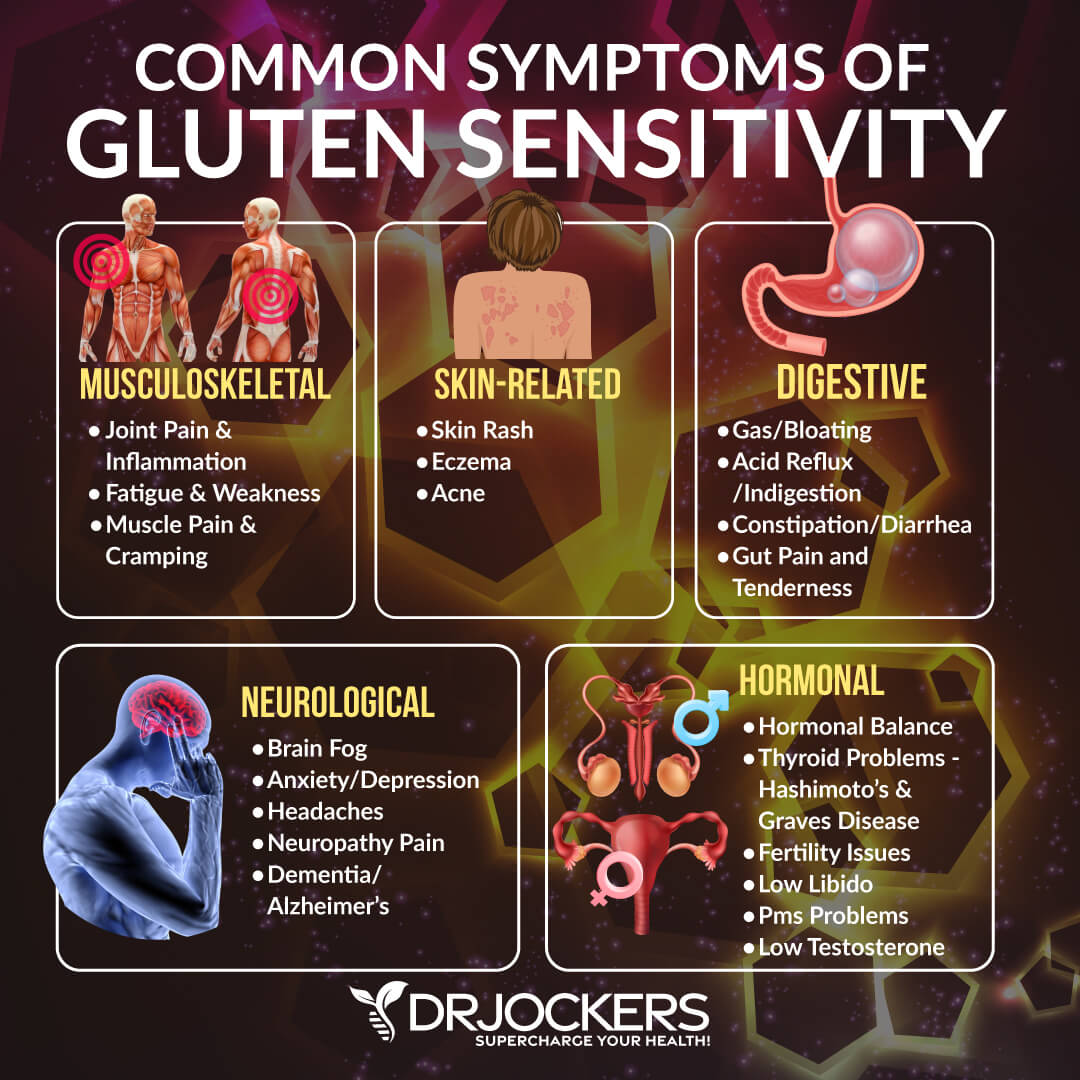
Gluten Sensitivity
You do not have to have celiac disease for gluten to be a problem for you. People with non-celiac gluten sensitivity experience the symptoms found in celiac disease even though they do not test positive for celiac disease.
The terms non-celiac gluten sensitivity (NCGS) and non-celiac wheat sensitivity (NCWS) are generally used to refer to this condition. As with celiac disease, individuals with NCGS have a systemic immune reaction and accompanying intestinal cell damage when exposed to gluten.
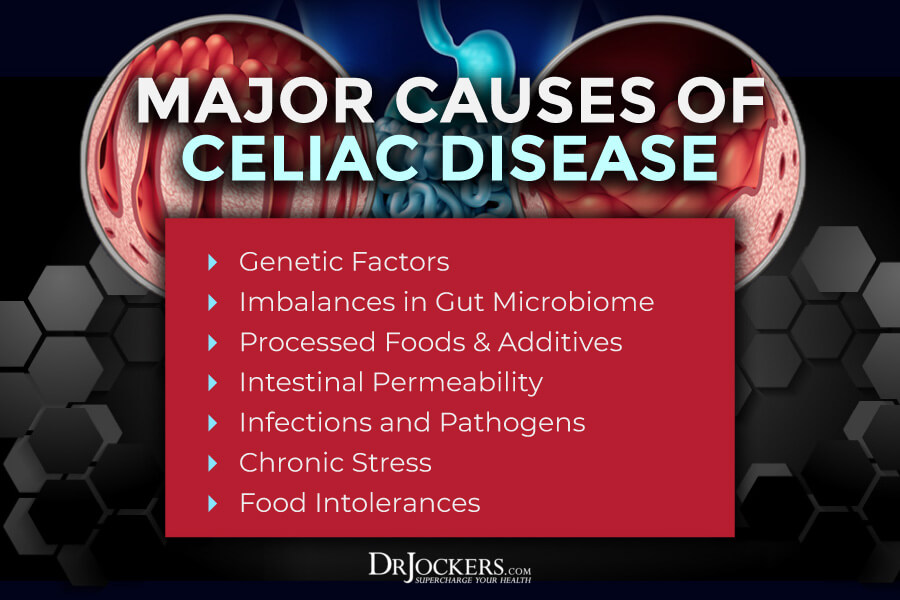
Major Causes of Celiac Disease
Celiac disease is a complex disorder. Almost all people with celiac disease have certain variants of particular genes. However, only 3 percent of individuals with these gene variants develop celiac.
Other factors also influence the development of celiac disease. Emerging research is looking at what environmental factors, other than gluten consumption, trigger this condition in genetically susceptible people.
The keystone of the development of celiac disease is an intestinal T-cell response brought about by gluten-derived peptides that can bind to certain genes. This T cell activation combined with genetic and/or environmental factors leads to immune intolerance to gluten, provokes intestinal permeability, and causes the vast symptoms of celiac disease.
1. Genetics
The risk of developing celiac disease is increased by certain genetic variants. The genes involved in celiac disease belong to a family of genes called the human leukocyte antigen (HLA) complex. The HLA complex helps the immune system distinguish the body’s own proteins from proteins made by foreign invaders such as viruses and bacteria.
More than 90% of people with celiac are human leukocyte antigen HLA-DQ2 positive and almost all of the rest carry HLA-DQ8 (4). These genetic variants seem to increase the risk of an inappropriate immune response to gliadin. However, these variants are also found in 30 percent of the general population, and only 3 percent of individuals with the gene variants develop celiac disease.
2. Imbalances in Gut Microbiome
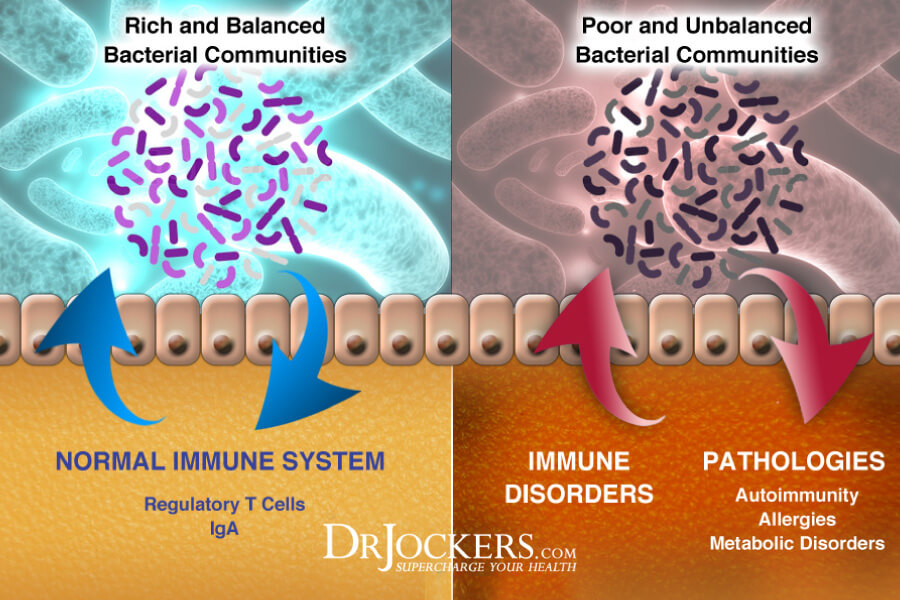
A healthy microbiome is necessary for normal immune development in the gut. The gut microbiome is made up of trillions of microorganisms. These microorganisms contribute to metabolic regulation and immune homeostasis.
Dysbiosis is the imbalance of protective and pathogenic microbes in the gut. Intestinal dysbiosis is linked to celiac disease (5). Children with active celiac disease typically have different “microbial signatures” in their microbiomes and greater dysbiosis (6).
Numerous studies have shown that antibiotic use early in life is associated with celiac disease (6). Antibiotics negatively impact the gut microbiome and can lead to dysbiosis. In addition to dysbiosis, antibiotic exposure in the first year of life has been shown to cause reduced fecal microbial diversity and early onset of the condition.
3. Processed Food and Additives
The production of autoantibodies is an important feature of many autoimmune diseases. In celiac disease, there is a significantly enhanced autoantibody response to the transglutaminase 2 (TG2) enzyme (or tissue transglutaminase (tTG)) (7). A heavily used food additive microbial transglutaminase (mTG) is in the same family as tTG and imitates tTG functionally (8).
mTG is an enzyme used as a protein glue in processed foods. It is regularly used as a food glue in meat, fish, seafood, milk and dairy, sweet foods, and bakery products. The enzyme is used in gluten-free products to improve the texture.
mTG increases intestinal permeability, suppresses the gut mucosa, stimulates bacterial growth, and augments the uptake of gliadin peptide. Exposure to mTG is associated with celiac disease.

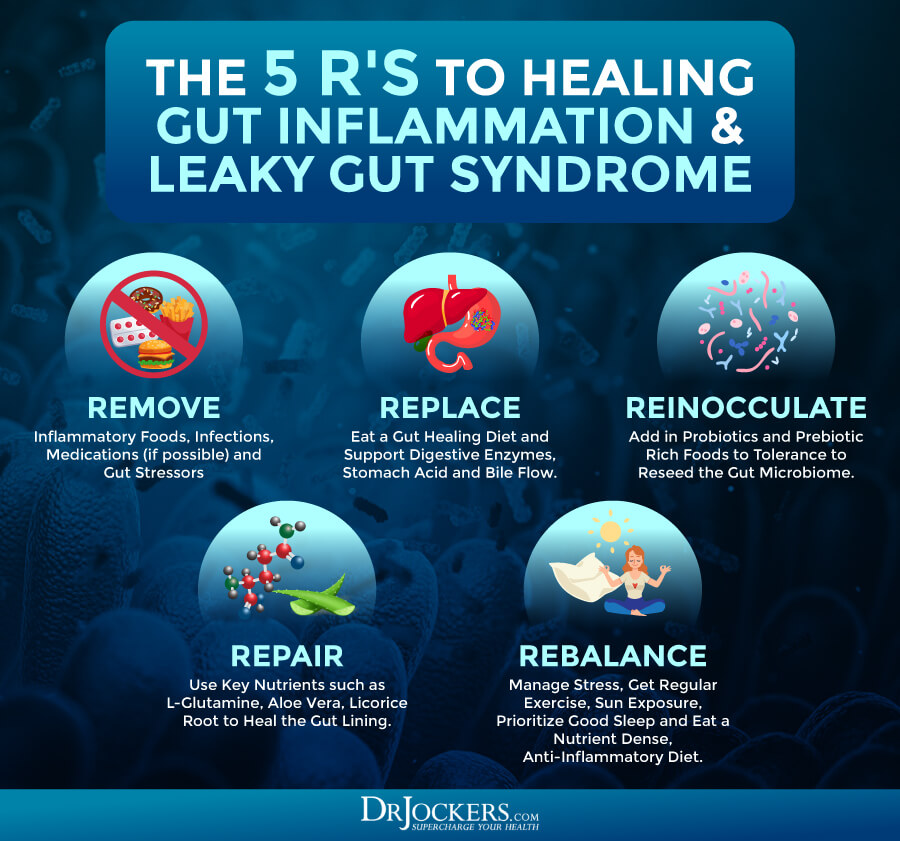
4. Intestinal Permeability
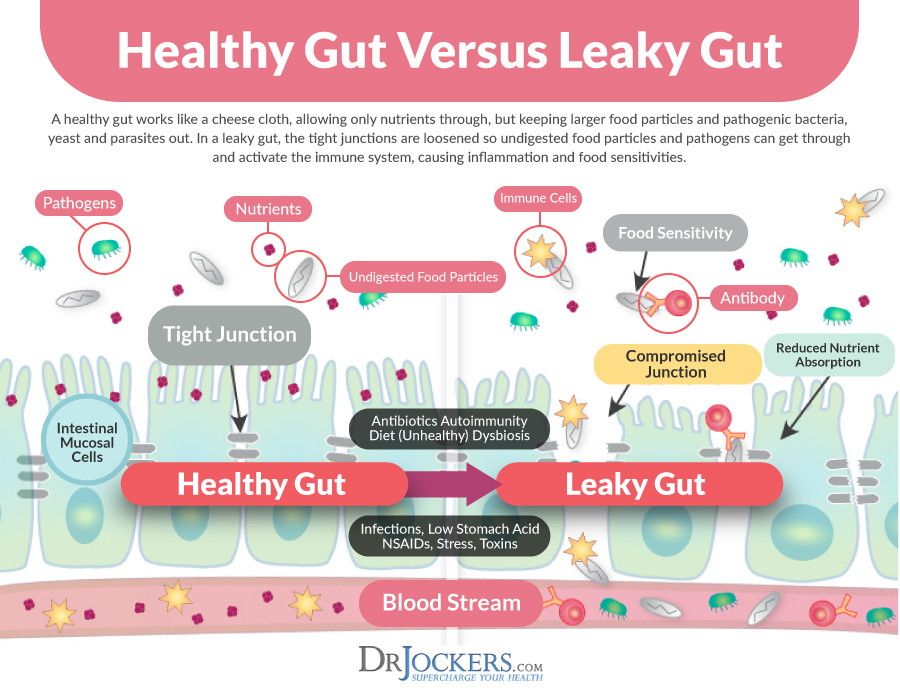
The gastrointestinal tract consists of an enormous surface area with essential roles in the body. The intestinal lining is designed to efficiently absorb nutrients, water, and electrolytes from food.
At the same time, it provides a tight barrier against harmful substances such as pathogens and protects against a reaction to harmless compounds. When this intestinal barrier is dysfunctional or compromised, it can play a role in a number of common disorders (9).
Intestinal permeability (or leaky gut syndrome) is a condition in which the tight junctions in the gut lining become too large and abnormally permeable. Individuals with celiac disease have abnormally loose tight junctions and increased intestinal permeability. Increased intestinal permeability may be a risk factor for developing celiac and/or a consequence of the immune reaction to gluten (9).
5. Infections and Pathogens
As an autoimmune, or immune-mediated condition, celiac disease involves an overactive immune response to gluten. Pathogens and infections trigger and activate an immune response creating inflammation as a protective mechanism.
Childhood infections are associated with celiac disease in a number of studies (6). This may be due to the inflammatory response to the infections increasing the risk for autoimmunity or through increased antibiotic exposure.
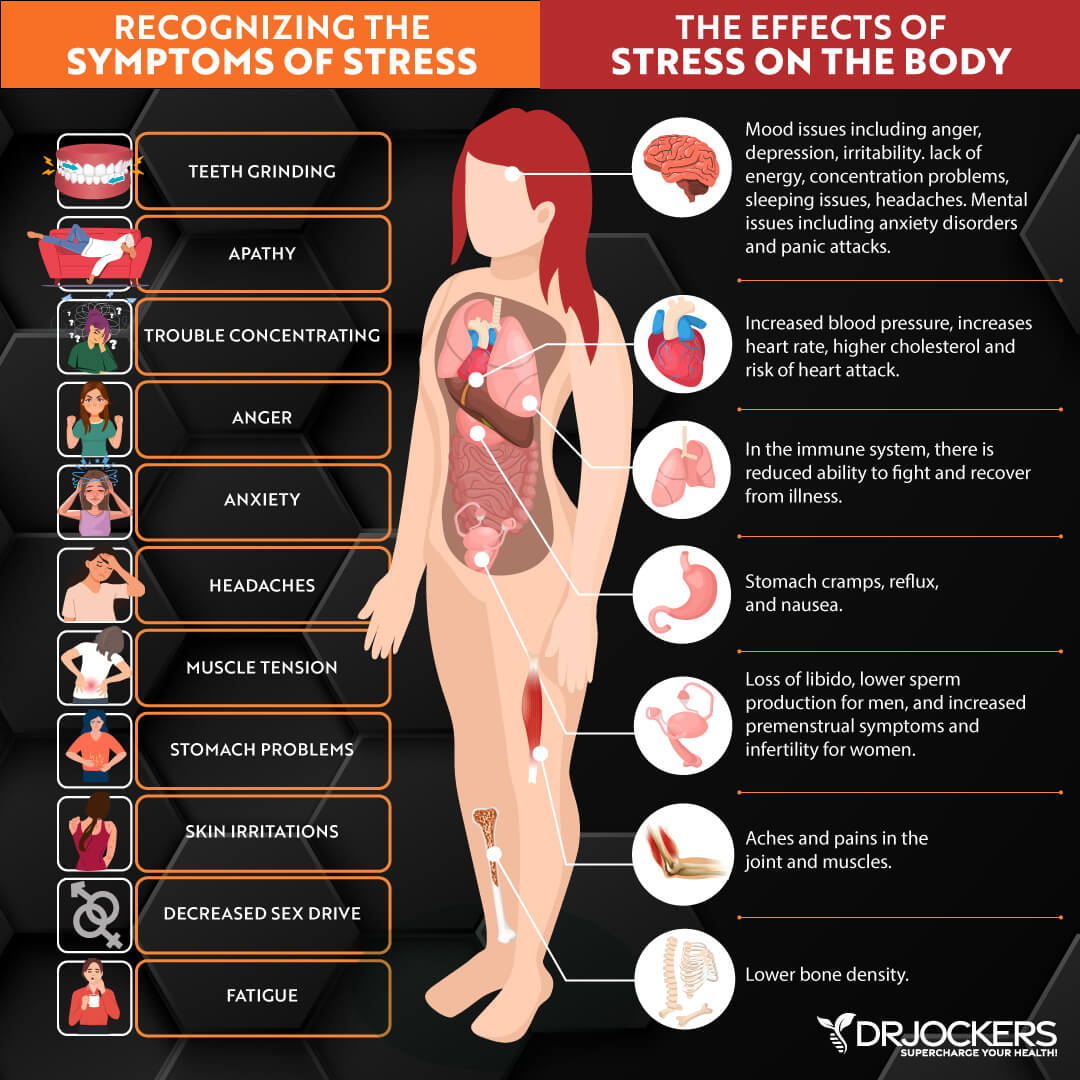
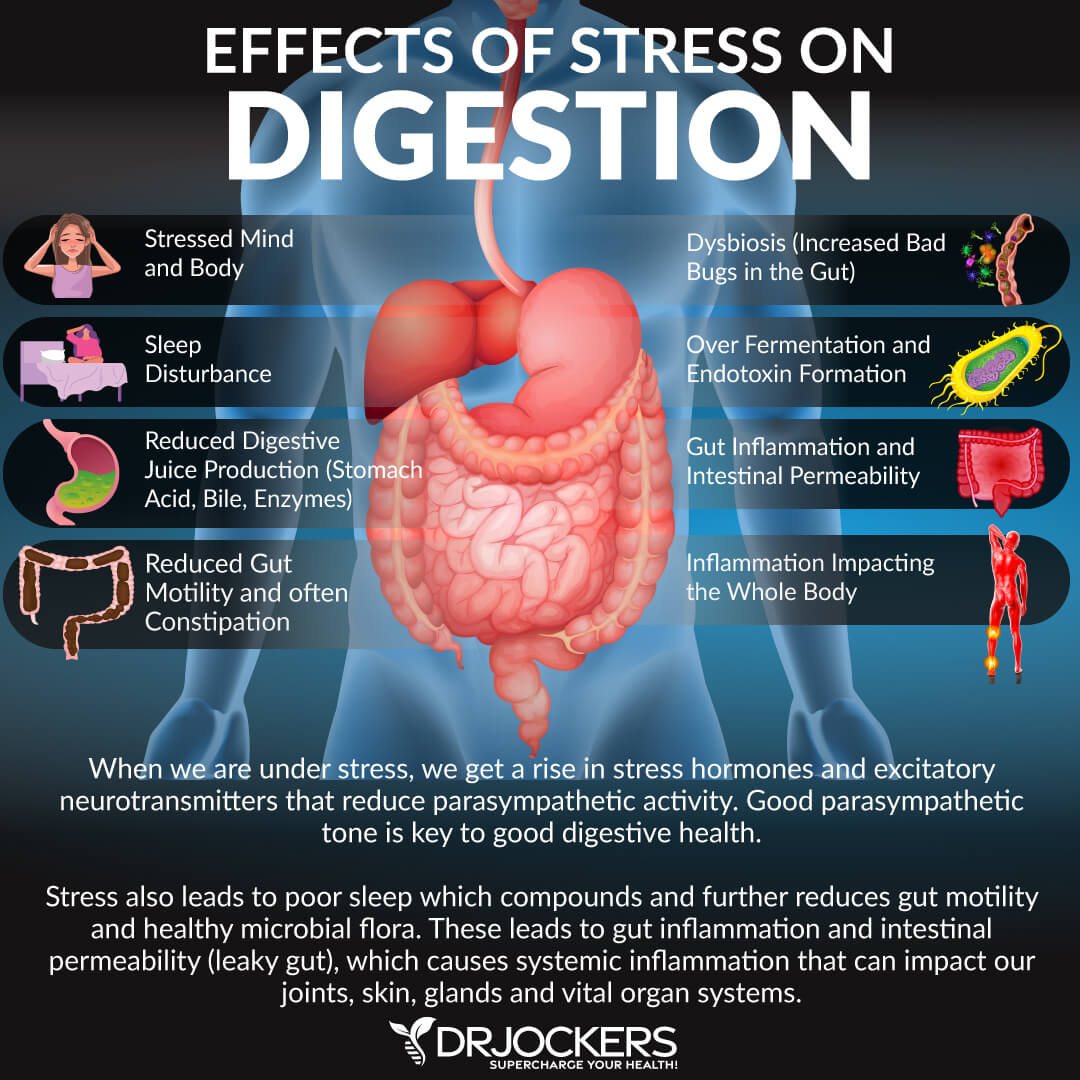
6. Chronic Stress
Celiac disease can become active after stressful events such as surgery, pregnancy, childbirth, or severe emotional stress (3). Psychological and physical stressors affect gut function and gut-brain interactions.
Stress can damage the gut by modulating key inflammatory pathways. This can alter the gut microbiome, increase intestinal permeability, and compromise the integrity of the gut mucosal barrier. These factors are associated with many different autoimmune conditions.
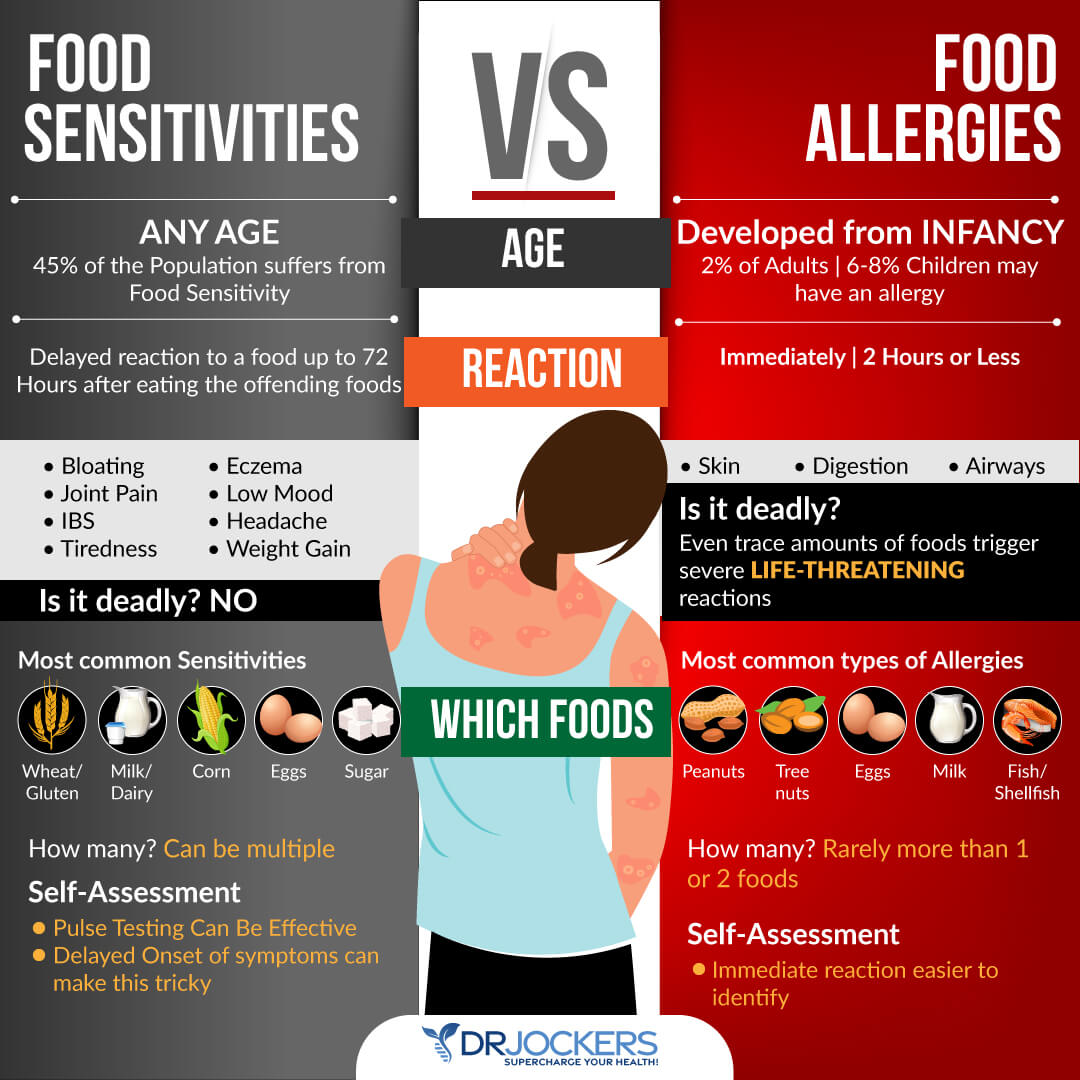
7. Food Intolerances
When a person has a food sensitivity or intolerance, consuming these foods may cause an overactive immune response. Repeated exposure to these foods inflames the gut lining causing intestinal permeability and digestive problems.
People with celiac disease are more likely to be sensitive or intolerant to other foods, including cow’s milk (6). The inflammatory reaction to milk protein in people with celiac disease exposure mimics the effect of gluten. This is seen with skim or low-fat milk which has more of dairy protein than whole milk.
Supportive Strategies for Celiac Disease
Avoiding gluten is critical for anyone with celiac. Foods contain gluten, as well as other products such as personal care products. In addition to eliminating gluten, there are other supportive strategies to help the body. While these strategies are not FDA-approved to prevent, mitigate, treat, or cure celiac disease, they may be helpful for people with digestive health issues.
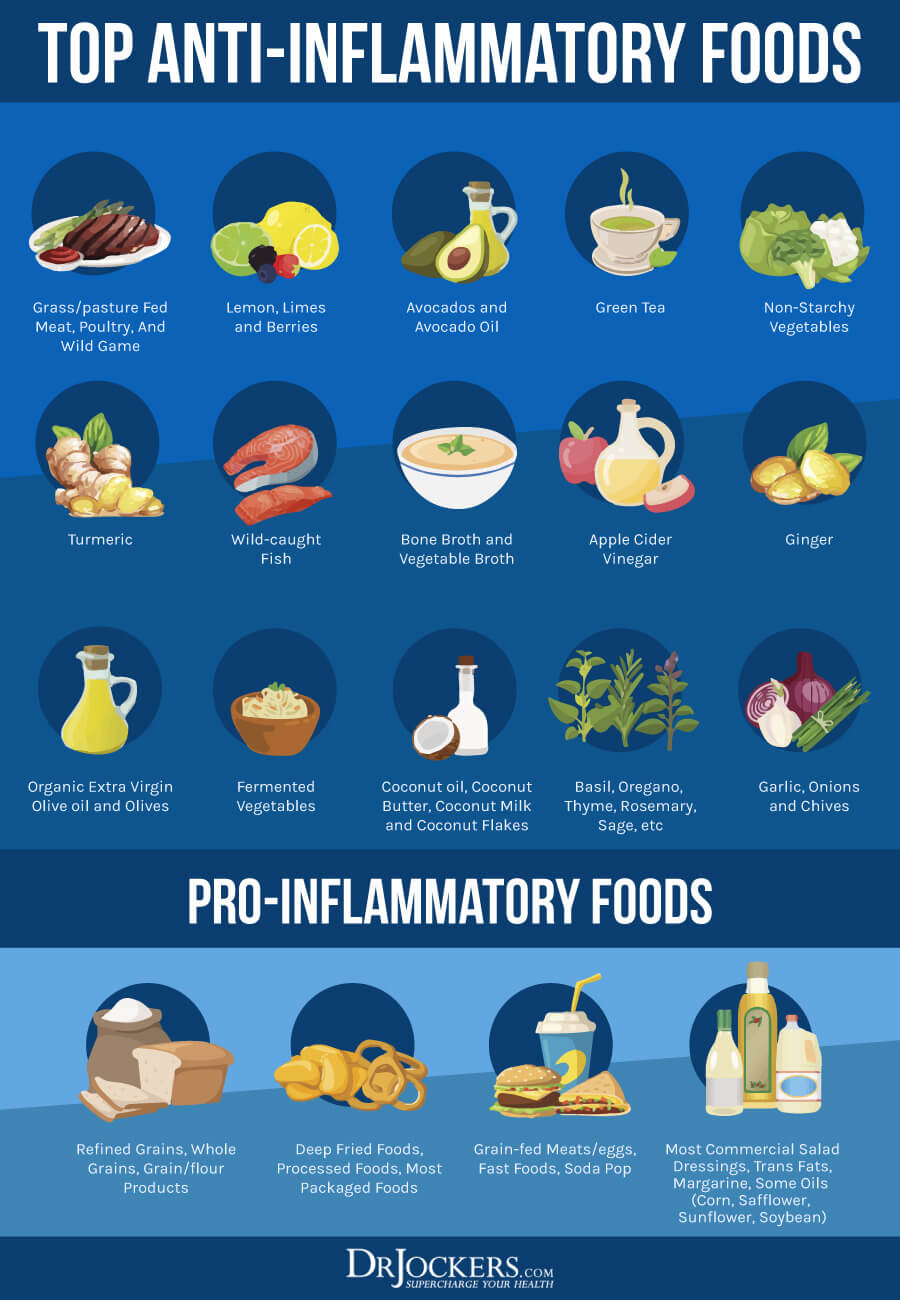
1. Anti-Inflammatory Nutrition Plan
Celiac disease is an inflammatory disease. One of the most effective strategies for healing is to follow an anti-inflammatory nutrition plan. You should remove foods that promote inflammation and replace them with anti-inflammatory healing foods.
Foods that cause inflammation and damage the gut include:
- Sugar
- Refined carbohydrates (white flour, white rice, white potatoes)
- Conventionally raised meat and dairy
- Farm-raised fish
- Processed foods, including meats
- Trans fats (partially hydrogenated oils)
- Monosodium Glutamate (MSG) and other food additives and preservatives
- Highly processed vegetable and seed oils, such as canola, corn, sunflower, peanut, grapeseed, cottonseed, and safflower
- Artificial sweeteners
You should replace these pro-inflammatory foods with whole, unprocessed foods including grass-fed, pastured organic meats and eggs, wild-caught salmon, organic vegetables, and healthy fats. Hypoallergenic brown rice or pea proteins can be used as well as bone broth from clean-sourced animals.
Healthy fats are found in coconut, olives, avocados, and their oils, and in grass-fed butter and ghee. Pumpkin, flax, hemp, and chia seeds, and borage, hemp, or flax oils are additional sources of good fats. Healthy fats are an efficient source of fuel for the body to combat inflammation.
Include foods rich in anthocyanins. Anthocyanins are flavonoids that are responsible for the dark pigments in fruits and vegetables. They have anti-inflammatory, antioxidant, anti-microbial, and immunomodulatory properties. Anthocyanins protect against inflammation and increase gut permeability. This can be very beneficial for individuals with celiac disease.
2. Autoimmune Elimination Diet
While controversial, studies show that celiac disease is associated with other systemic autoimmune diseases. For example, the prevalence of celiac disease (immune reaction to gluten) is significantly higher in people with Sjogren’s (10). Following an autoimmune elimination diet may be very helpful for individuals with celiac.
To implement an autoimmune elimination diet, you should avoid gluten and the most common allergenic/sensitive foods which may be contributing to or causing a negative reaction and inflammation. These include dairy, eggs, peanuts, tree nuts, soy, fish, and shellfish. Many people are also sensitive to nightshade vegetables (tomatoes, potatoes, eggplant, bell peppers), corn, legumes, and all grains.
The elimination period is around 6 weeks. After the elimination period, you slowly reintroduce foods, one at a time, noting any reactions and symptoms you may experience. It is important to keep a journal during the entire process to document how you are feeling as you eliminate and reintroduce the foods.
Food sensitivities can be hard to identify. This is because symptoms of food sensitivities are usually delayed up to 72 hours after consuming the offending food. For information about different methods of testing for food sensitivities, check out this article.

3. Support Gut Health
Celiac disease involves inflammation throughout the gastrointestinal system. Reducing stress on the gut with easy to digest foods and liquid nutrition can be very effective. Foods that are easy to digest include bone broth, soups, and cooked vegetables.
Consuming liquid nutrition is great for stimulating the digestive process, increasing nutrient absorption, and improving gut health. Liquid nutrition does not require as much energy to digest, so your body can focus on healing and repair. You can combine liquid nutrition with fasting strategies for quicker healing.
A great healing strategy for people with celiac disease is to consume collagen. Collagen makes up the villi, small finger-like structures on the intestinal wall, and assists with water absorption in the intestines. These villi are damaged in people with celiac disease. It is important to note that collagen is not FDA-approved to prevent, mitigate, treat, or cure any medical conditions.
4. Repair and Strengthen the Gut Lining
The gut mucosa covers the intestinal surface providing a physical barrier against pathogens. Supplementing with colostrum or a bovine-serum immunoglobulin (BSI) blend that supports gut barrier function, improves immunity, and decreases inflammation in the gut. These immunoglobulins also bind to environmental toxins, neutralize pathogens, and aid digestion.
To help soothe an irritated gut lining and reduce inflammation, you should consider adding nutrients such as the amino acid l-glutamine, the antioxidant quercetin, aloe vera, curcumin, omega-3, EGCG, arabinogalactan, and licorice. This combination may be very effective for improving the healing process of the gut lining.
5. Avoid Hidden Sources of Gluten
There are many foods that contain gluten in hidden and unexpected ways. If a product does not have the “certified gluten-free” label, it is important to read the ingredients. Remember a product may say “wheat-free” but still contain spelt, rye, or barley-based ingredients that are not gluten-free.
Common foods that contain gluten are pasta, breads, crackers, baked goods, flour tortillas, beer, cereal, and granola. Gluten-containing grains may also be used in energy bars, soups, sauces, and more. When eating at a restaurant, be careful of batter containing wheat flour or cross-contact with gluten-containing foods (such as in a fryer, toaster, or cutting board).
Certain medications (prescription and over-the-counter) and supplements contain gluten so be sure to check the label or ask the pharmacist. Personal care products such as lip glosses, cosmetics, skin and hair products, and toothpaste and mouthwash may contain gluten. Additionally, children’s modeling dough, such as Play-Doh, often contains gluten.
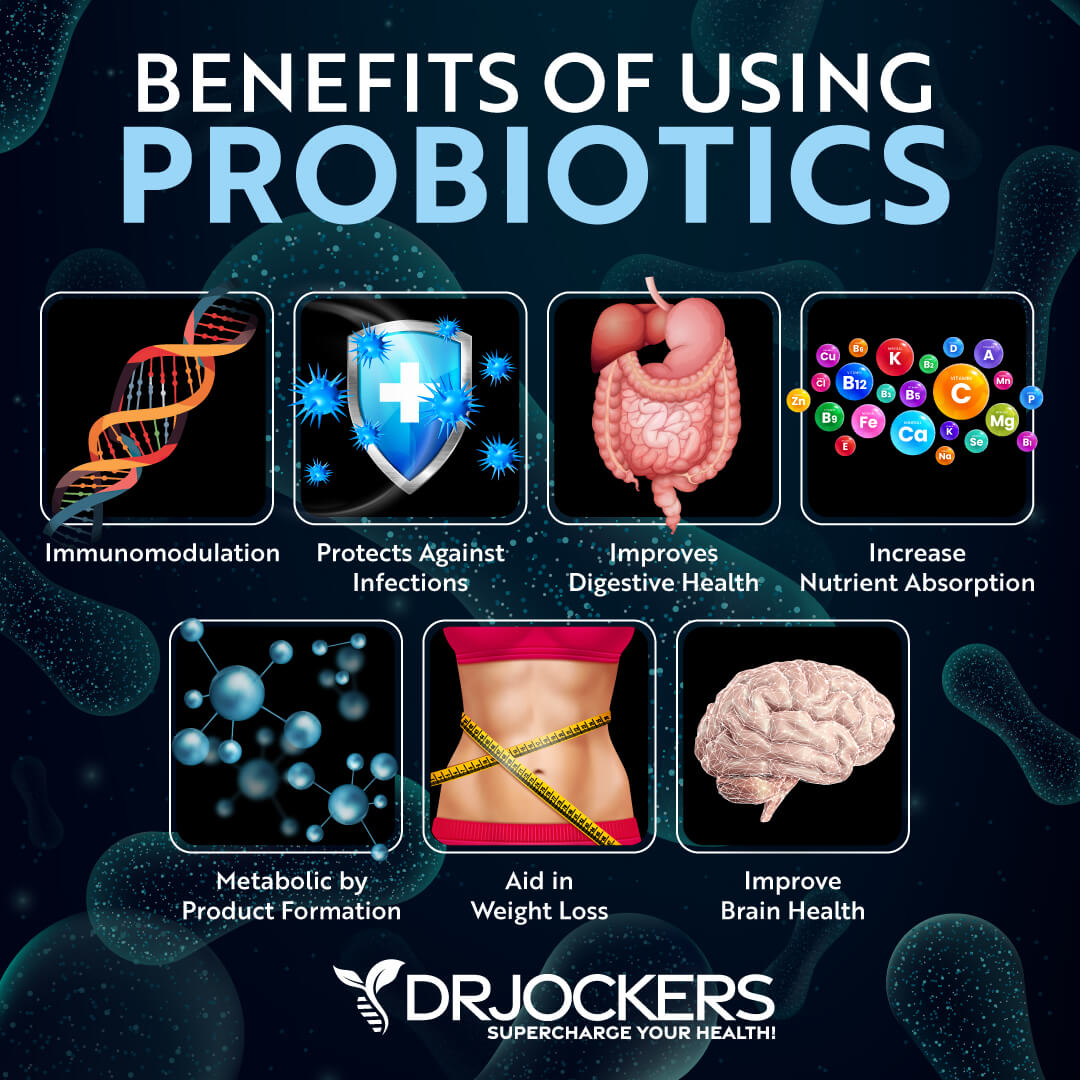
6. Balance Gut Microbiome
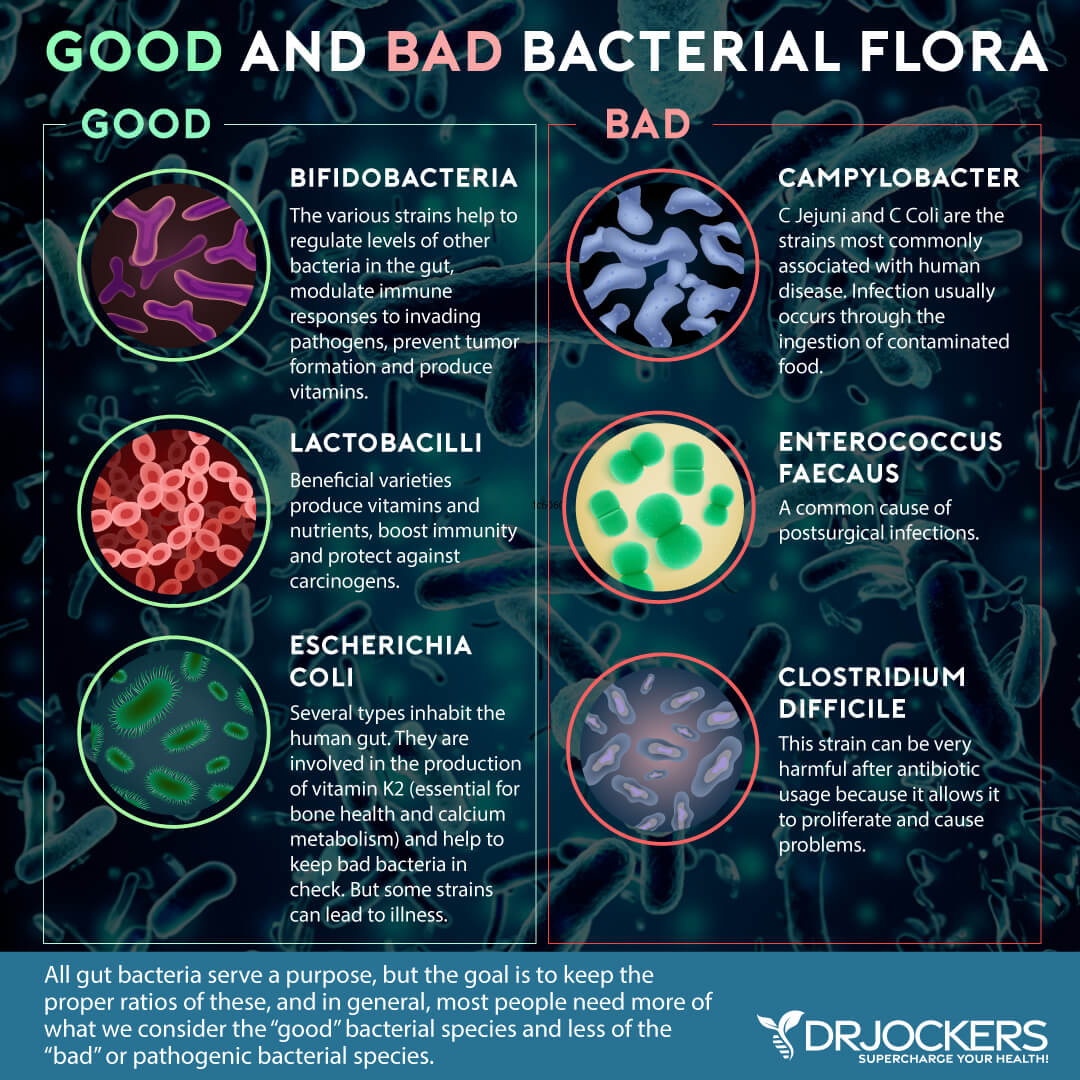
Improving the microbial balance in your gut is very important for anyone with celiac disease. Probiotics are beneficial microorganisms (bacteria and yeasts) that are similar to the microorganisms that naturally live in our bodies.
Probiotics work through different mechanisms to support gut health and downregulate the effects of bacteria in initiating and sustaining an intestinal inflammatory response. Studies show that probiotics may be helpful for celiac disease (5).
There are 4 main categories of probiotics: food based (lactobacillus and Bifidobacterium), spore-forming soil based (bacillus strains), probiotic yeast (S boulardii), and combination probiotics that have all these strains. If your gut is very sensitive, you can try one of these categories at a time and experiment with small dosages and gradually increasing dosages to find what works best for you.
7. Reduce Stress and Improve Sleep
Chronic stress and lack of sleep may contribute to the development and worsen symptoms of celiac disease. To help manage stress and improve sleep, it is critical to follow an anti-inflammatory diet and balance your blood sugar levels. Additional stress relieving techniques are grounding, deep breathing exercises, sunlight exposure, Epsom salt baths, and dry brushing.
Strategies for better sleep are getting sunlight during the day, avoiding artificial light and EMFs, blacking out your room with blackout curtains or using a sleep mask, and being smart about caffeine intake. It is also helpful to turn off electronics, practice good hygiene, stretch, practice gratitude, journal, pray, and implement other healthy sleep habits.
Supplementing with adaptogenic herbs such as ashwagandha, holy basil, rhodiola, and ginseng can be very helpful in balancing stress hormones. Most individuals with Celiac need more magnesium and that plays an important role in reducing anxiety and improving sleep quality.

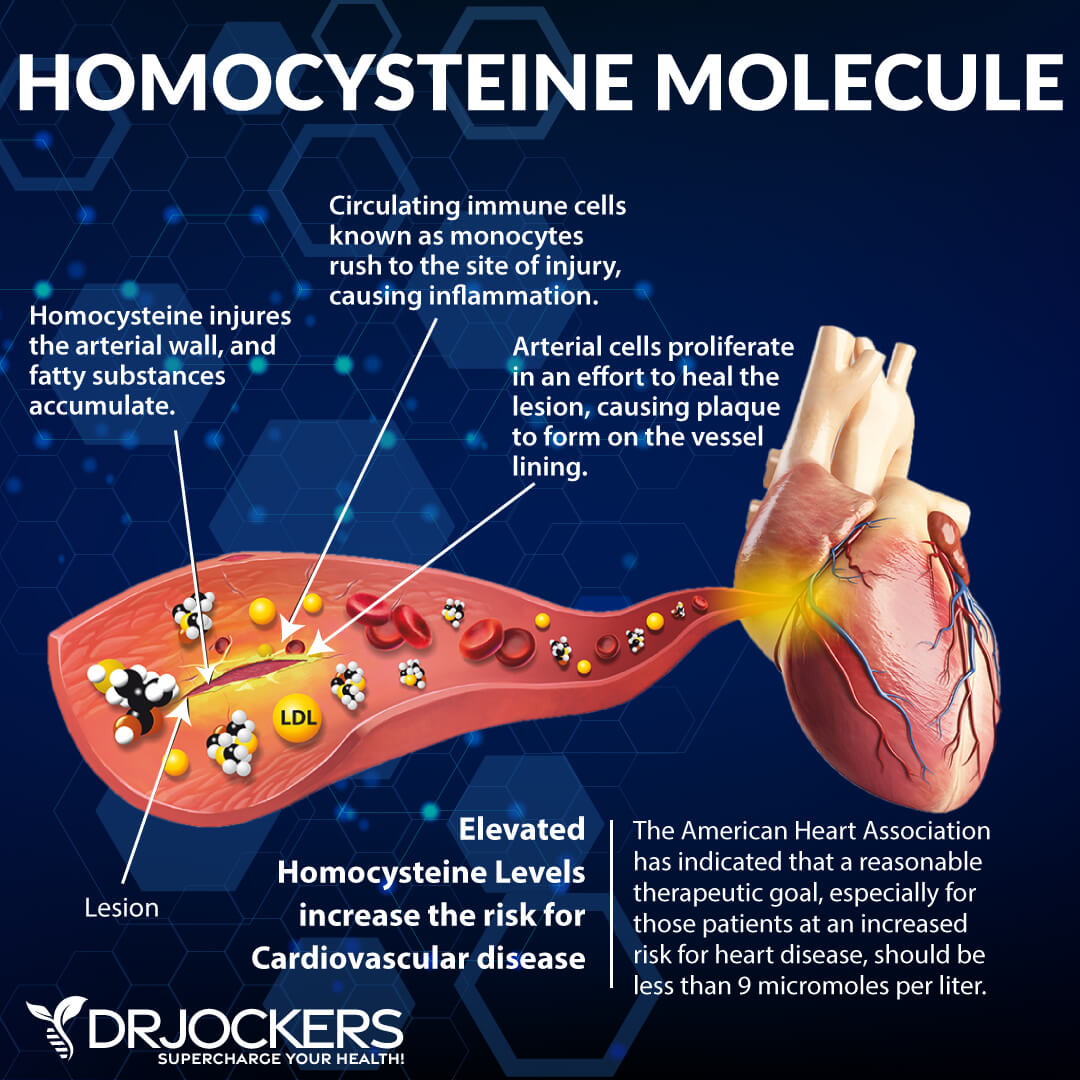
8. Monitor Homocysteine Levels
People with celiac disease have a higher risk of venous thromboembolism and vascular disorders (12). A high level of homocysteine is a risk factor for these chronic diseases.
Homocysteine is an inflammatory amino acid that is produced as a byproduct of protein metabolism. It is metabolized in the body through remethylation and transsulfuration. Proper levels of methylated vitamins B2, B6, B12, folate, and magnesium help to prevent homocysteine from building up in the body.
Vitamin B12 works with folate and its metabolites to change homocysteine into the non-toxic amino acid methionine. Providing proper methylation support can help to reduce homocysteine to a safe level.
9. Reduce Oxalates
Hyperoxaluria occurs when there is too much oxalate in the urine. There are two forms of hyperoxaluria, primary and secondary. Secondary hyperoxaluria is linked to celiac disease (12).
Secondary hyperoxaluria results from increased intestinal absorption of dietary oxalates. Foods rich in oxalates include spinach, beets, chocolate, peanuts, sweet potatoes, wheat bran, tea, berries, and nuts (cashews, pecans, and almonds). These foods are very healthy for most people, but for people with celiac disease, they can be problematic.
Normally, oxalates within food combine with calcium making it difficult to absorb. In people with fat malabsorption, the fat binds to calcium, increasing the amount of free oxalate available for absorption. Celiac disease causes fat malabsorption, so more oxalates are absorbed in people with this condition.
High oxalates can cause oxidative damage, inflammation, and pain. In the gastrointestinal tract, high oxalates may significantly reduce the absorption of essential minerals such as calcium, magnesium, zinc, and more. Mineral deficiencies are common in people with celiac disease. Reducing these inflammatory oxalates helps to heal the gut and reduce yeast and dysbiosis. For more information on a low oxalate diet, read this article.

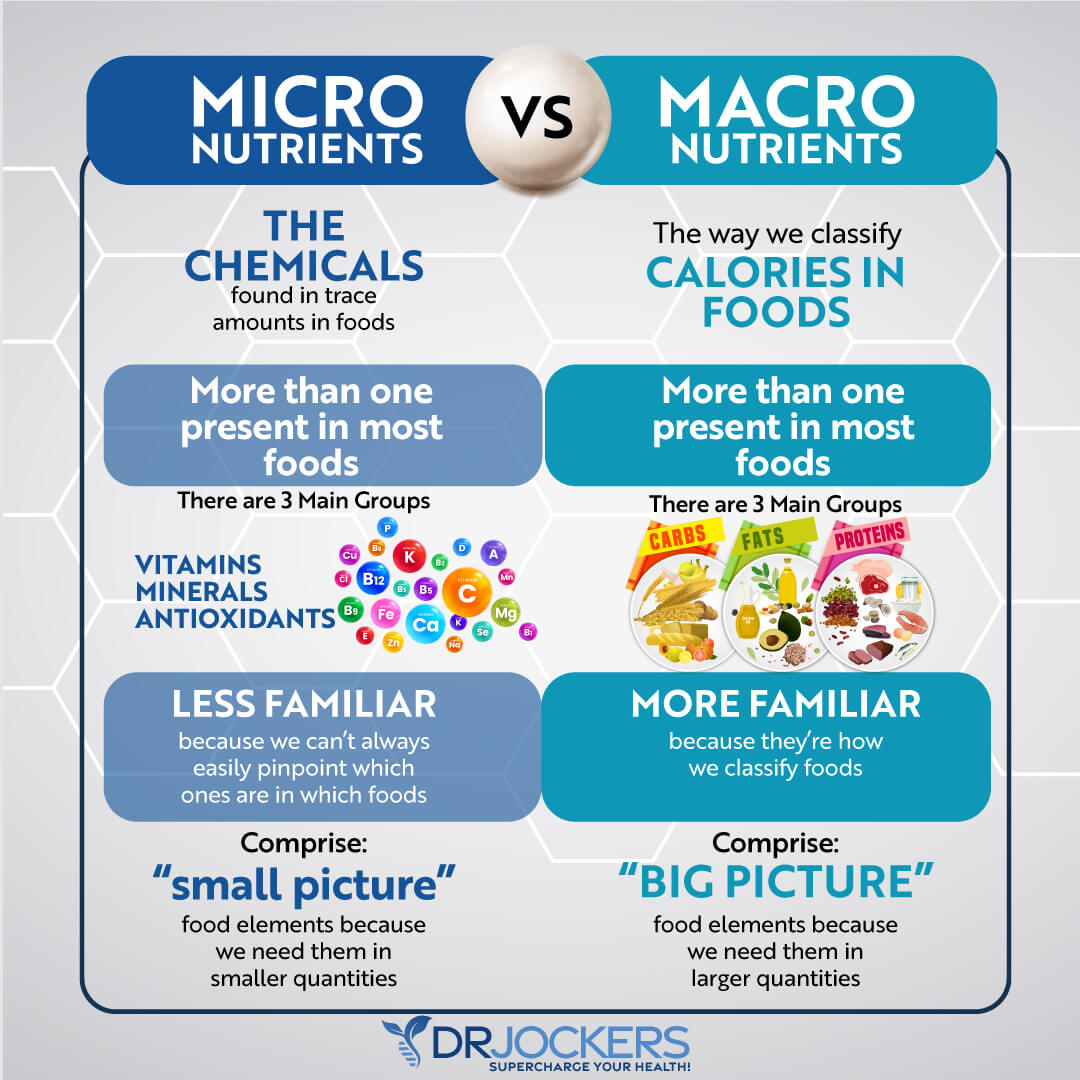
10. Optimize Micronutrient Levels
Nutrient deficiencies are common in people with celiac disease. Damage to the small intestines leads to poor absorption of fatty acids, transferrin, glucose, electrolytes, vitamins, and minerals (2).
Vitamins, minerals, antioxidants, and amino acids are all micronutrients. They play a central role in metabolism and the maintenance of tissue function. The micronutrients iron, folate, vitamins B6 and B12, vitamin D, copper, and zinc are commonly deficient in people with celiac disease (13).
Testing for nutrient deficiencies may be very helpful for anyone with celiac disease. The SpectraCell Micronutrient Test measures functional deficiencies of micronutrients at the cellular level giving a comprehensive nutritional analysis. This extensive test assesses how well the body utilizes 33 vitamins, minerals, amino and fatty acids, antioxidants, and metabolites. Once any micronutrient deficiencies are identified, an individual can use targeted supplementation to optimize their levels.
Additional Testing
GI Map Stool Analysis
The GI-MAP™ Stool Analysis Test is a stool test that gives a thorough picture of overall gut health. It is an FDA-approved DNA test that shows gastrointestinal microbes and pathogens (viruses, bacteria, parasites), imbalances in the gut microbiome, potential autoimmune triggers, and more.
The GI Map measures the immune response in the gut with Secretory IgA levels, including anti-gliadin SIgA. Immunoglobulin A is the primary immunoglobulin in the intestinal mucosa. Low SIgA levels indicate that the gut immune system is suppressed. High levels indicate an elevated immune response to antigens in the GI tract. The presence of fecal anti-gliadin antibodies can indicate an immune response in the gut to gluten.
The GI Map also reveals the integrity of your gut mucosa with digestion, gastrointestinal, and other intestinal health markers. This is an important test for anyone with celiac disease. For more information on the GI-MAP and how to order, go here.
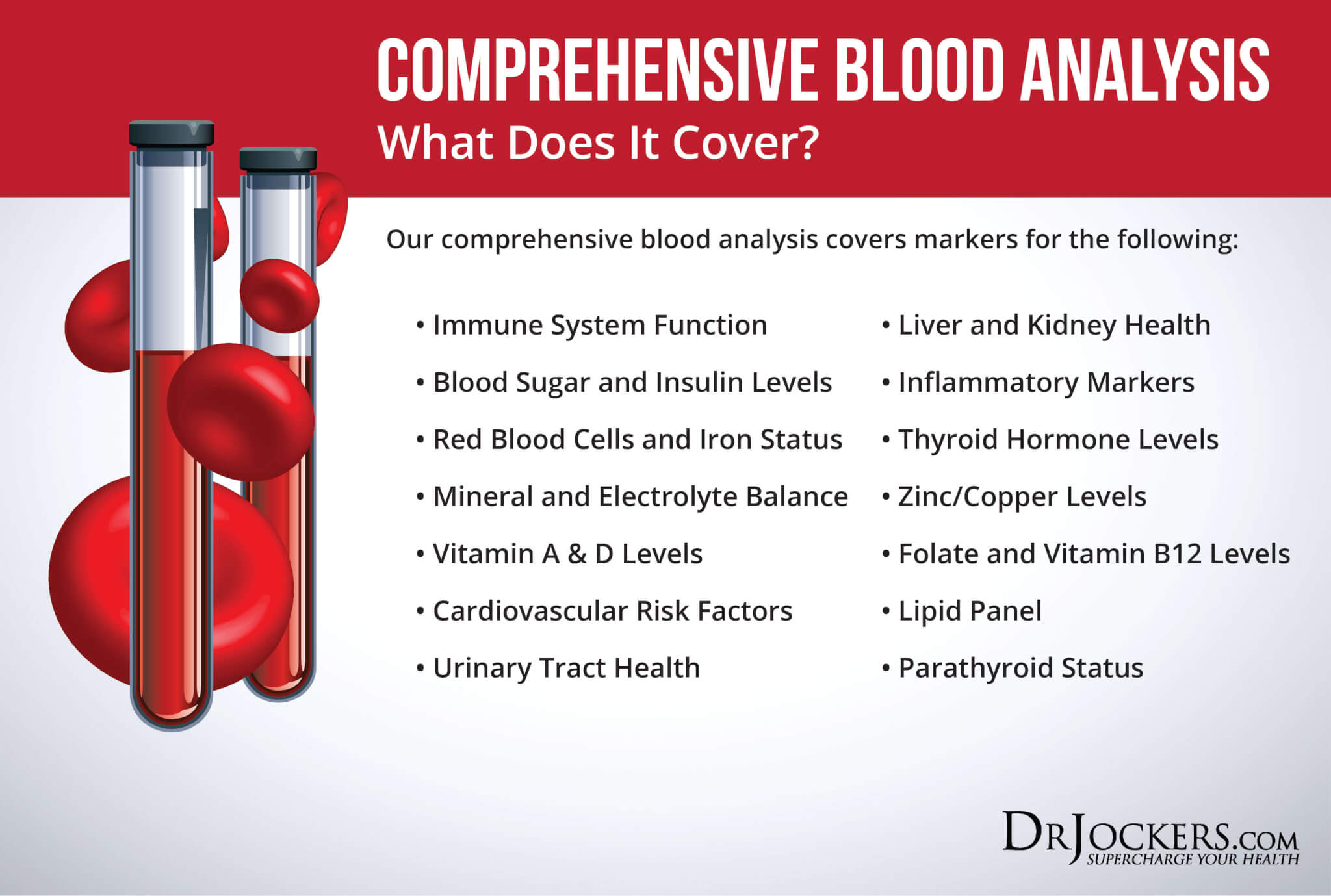
Comprehensive Blood Analysis
It can be helpful for anyone with celiac to monitor levels of inflammation, nutrient deficiencies, homocysteine, and other markers with a thorough blood test. One of the most comprehensive blood tests available is the Comprehensive Blood Analysis.
The Comprehensive Blood Analysis includes markers of immune system function and inflammation such as a high sensitivity C-Reactive Protein (hs-CRP), Red Blood Cell Width (RBCW), ferritin, and erythrocyte sedimentation rate (ESR). It measures fasting glucose, hemoglobin A1c, and homocysteine levels.
This test will show whether thyroid antibodies are present which may indicate an autoimmune thyroid condition. Autoimmune thyroid conditions are associated with celiac disease. The comprehensive blood analysis also measures several vitamin and mineral levels including vitamins B12, A, and D, folate, zinc, copper, and iron. These nutrients may be low in people with celiac disease.
Conclusion
Celiac disease is an immune-mediated systemic disorder triggered by the ingestion of gluten in genetically predisposed individuals. It is characterized by inflammation in the small intestines.
Avoiding all sources of gluten and other hard to digest foods is critical. Other strategies that may be helpful include following an anti-inflammatory, autoimmune elimination diet, reducing oxalates in the diet, optimizing micronutrient levels, and monitoring homocysteine levels.
It is also important to work on gut health by reducing stress on the gut, healing and repairing the gut lining, and balancing the microbiome. Addressing excess stress and prioritizing sleep may also be helpful. You should also monitor the condition with stool and blood tests to measure inflammation, nutrient deficiencies, and gut health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Through DrJockers.com, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and thrive in life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




In 4 Intestinal Permeability, second paragraph.
This statement seems wrong: Individuals with Celiac disease have abnormally tight junctions and increased intestinal permeability. The text also says the tight junctions in the gut lining become too large and abnormally permeable. These two statements seem to be at odds with one another.
Yes those can be written better and we will look at them. Tight junctions refers to the way the intestinal cells are packed together.
My sister is down syndrome and is 52 she was a high functioning downs lived independantly with 24 hour support.she started loose weight a few years ago investigated on numerous occassions and found nothing.End of 2020 i asked dr to test for celiac n appently test came back very unlikely so im told.Various stages in her live shed been celiac.Last year she stopped walking talking not eating all in same day and w were told expect the worse she was then moved to a pallative care home.Fortunetly shes still here today.for a year care home have given her celiac food and only now has she been putting weight on.Her bloods show an overload of iron but on a scan it shows no problems only marks on spleen and cyst on pancreas n slight hardening on 1 of lung wich all confused about but is not well enough to undergo further investigations.In about march i red up on some drinks which i needed by privately for celiacs high in calorie but full of goodness since these and gluten free diet she has started regaining weight
Sorry to hear about this! Glad she is doing better. Reach out to our functional health coaches to get her set up on a personalized plan to heal. https://drjockers.leadpages.co/long-distance-coaching-dr-jockers/