 Bile Acid Malabsorption: Symptoms & Solutions
Bile Acid Malabsorption: Symptoms & Solutions
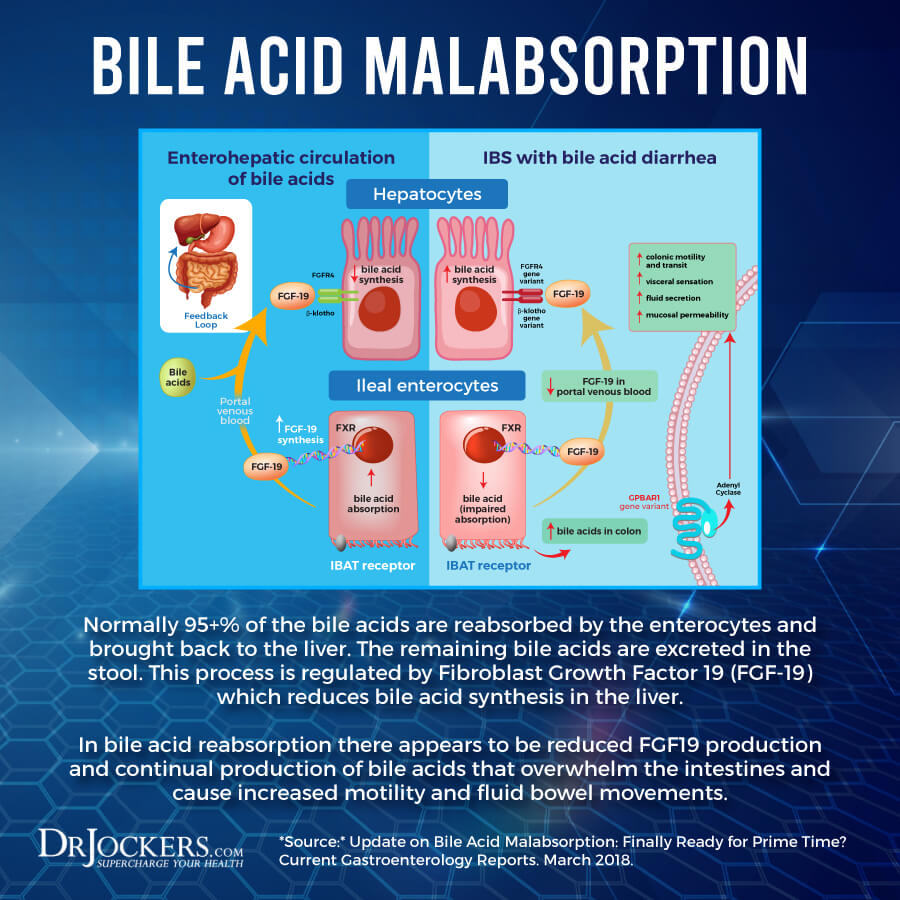
Bile is a green-ish brown liquid or digestive juice that emulsifies fats for your small intestine to absorb. It is essential for digestion and the absorption of nutrients. Bile acid malabsorption (BAM) is a health condition that you develop when your intestines are unable to absorb bile properly. Bile acid malabsorption leads to bile acid build-up which can cause watery diarrhea and other symptoms. Fortunately, with the help of some natural strategies, you can reduce your symptoms and improve your health.
Today, you will learn about bile acid malabsorption. I will explain what bile acid malabsorption is. You will understand the symptoms of bile acid malabsorption. I will discuss the risk factors for bile acid malabsorption. Finally, I will share my best strategies for bile acid malabsorption to improve your health and well-being.
What is Bile Acid Malabsorption
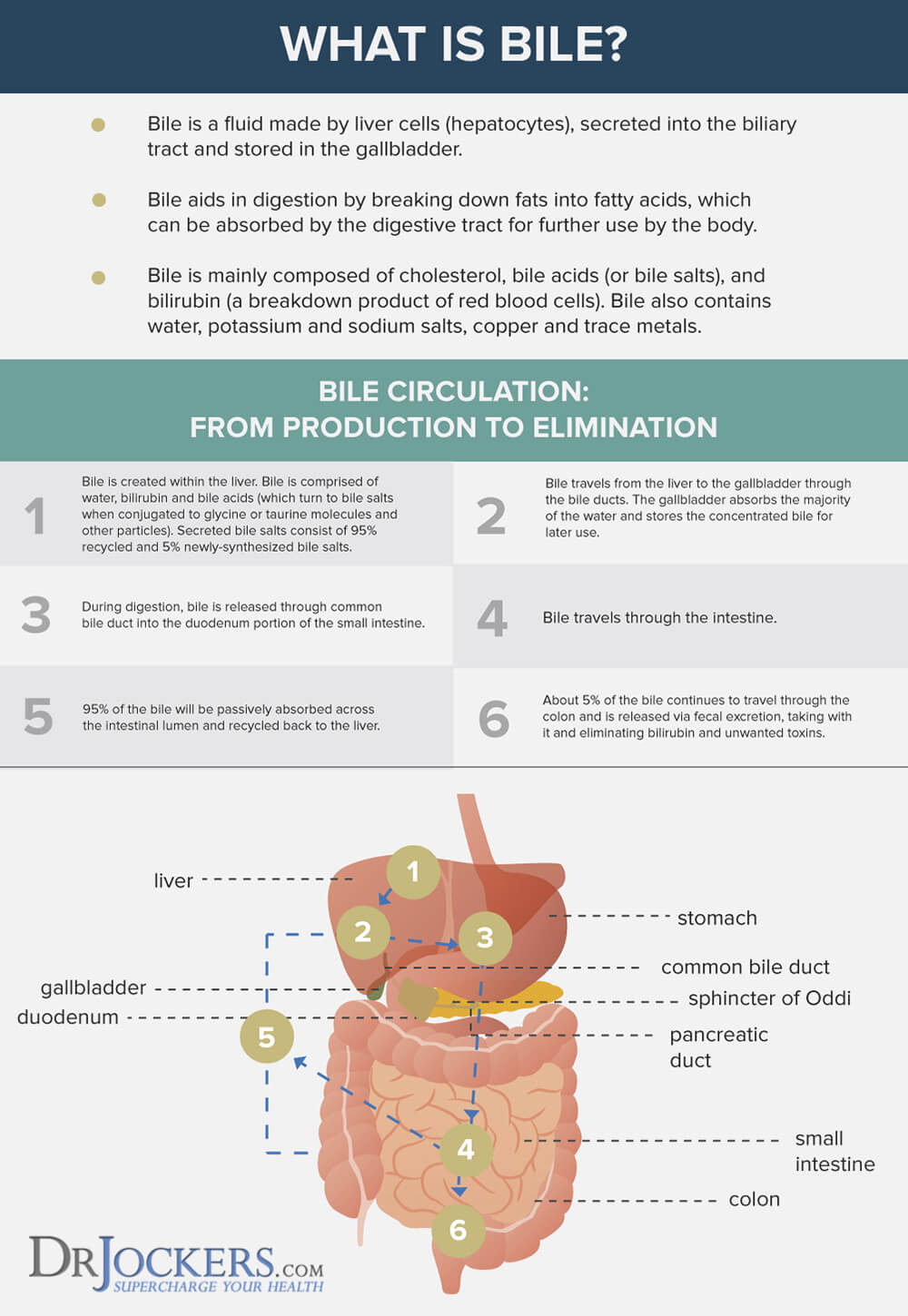
Bile is a green-ish brown liquid or digestive juice that emulsifies fats for your small intestine to absorb. It is made up of cholesterol, salts, and bilirubin. Your common bile duct transports bile from your life to your gallbladder to be stored until eating times. Eating food will urge your gallbladder to contact and release bile into your stomach to support the breakdown of food and nutrients.
Bile is critical for the digestion of fats and absorption of nutrients. Bile contains waste products that get removed through bowel movements. In your colon, remaining bile acids get reabsorbed so they can be used again. Poor bile acid absorption, poor bile flow, and other bile-related issues can lead to a variety of health problems.
Bile acid malabsorption (BAM) is a health condition that you develop when your intestines are unable to absorb bile as they should. Bile acid malabsorption leads to bile acid build-up in your colon which can lead to watery diarrhea and other issues. Bile acid malabsorption is often referred to as bile acid diarrhea (1, 2).
Symptoms of Bile Acid Malabsorption
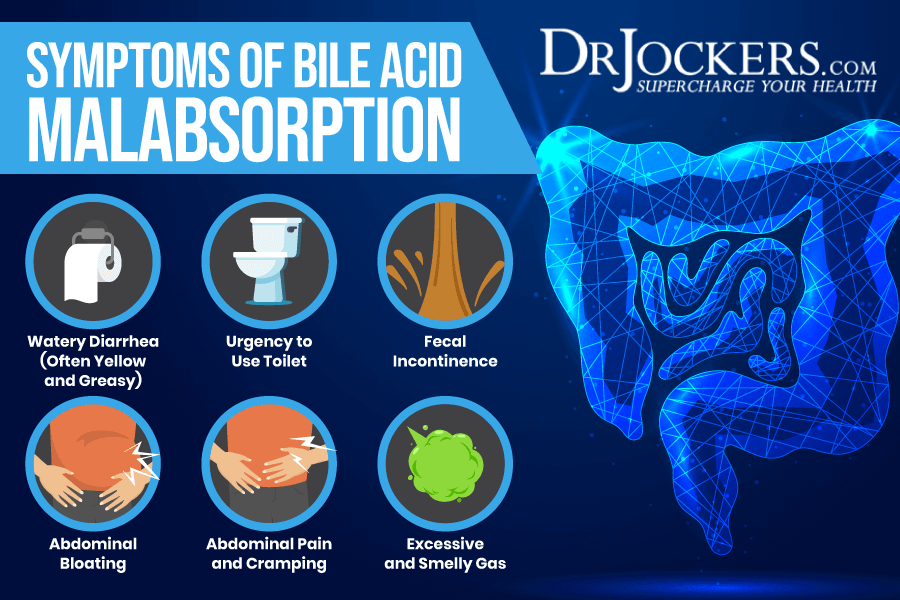
Due to the salt and water from bile acid building up in your colon and interfering with the formation of proper stool, the main symptom of bile acid malabsorption is diarrhea. If you have bile acid malabsorption, you may experience diarrhea daily, but maybe only occasionally. Other than diarrhea, you may experience other symptoms too.
Symptoms of bile acid malabsorption may include:
- Watery diarrhea, usually yellow and greasy in appearance
- Urgency to use the toilet
- Needing to use the toilet frequently
- Fecal incontinence (inability to control bowel movement causing leakage of stool)
- Bloating
- Abdominal pain and cramping
- Excessive and smelly gas
Risk Factors for Bile Acid Malabsorption
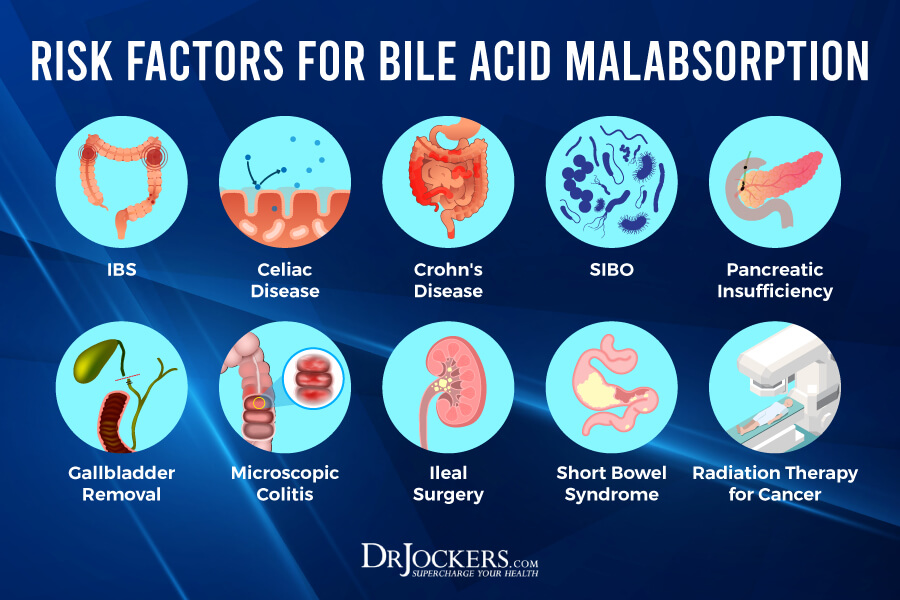
The cause of bile acid malabsorption is not always clear. These cases are called primary bile acid malabsorption where there isn’t a clear explanation for the condition. However, in most cases, bile acid malabsorption develops because of a symptom or complication of another condition. This is called secondary bile acid malabsorption.
According to a 2010 study published in the Royal College of Physicians, Clinical Medicine, about one-third of people with irritable bowel syndrome (IBS) have bile acid malabsorption (3). Other health issues may lead to bile acid malabsorption too.
Conditions that may increase the risk of bile acid malabsorption may include:
- IBS
- Celiac disease
- Crohn’s disease
- Small intestine diseases
- Small intestinal bacterial overgrowth (SIBO)
- Pancreatic insufficiency
- Other pancreatic diseases
- Gallbladder removal, or cholecystectomy
- Ileal disease
- Ileal surgery often used as a treatment for Crohn’s disease
- Microscopic colitis
- Short bowel syndrome, when a large portion of the small intestine has been removed
- Radiation therapy for cancer
Natural Strategies for Bile Acid Diarrhea
There are a number of natural strategies you can use for bile acid diarrhea to improve your symptoms and well-being. Here is what I recommend:
Avoid Food Allergens and Sensitivities
According to a 2015 study published in the World Journal of Gastroenterology, food allergies, food intolerances, and food sensitivities may play a role in functional gastrointestinal symptoms, IBS, and bile acid malabsorption (4). Avoiding food allergens, food intolerance, and food sensitivities may help to alleviate your symptoms.
Food allergies are different from food sensitivities. Food allergies cause an immediate reaction in your body. You may experience hives, difficulty breathing, puffiness, digestive issues, or other symptoms immediately after eating a food that you are allergic to. In some cases, these food allergy symptoms can be life-threatening when not addressed right away. Because of these immediate reactions, food allergies are easier to identify.
Food intolerances and food sensitivities, on the other hand, don’t cause an immediate reaction but cause issues over time. Food intolerances mean that your body is unable to digest a specific food or particle in a food, such as lactose or gluten.
Food sensitivities mean that your body has a reaction to food despite an obvious food allergy or specific food intolerance. You may eat food and only experience symptoms a few hours or even a few days later. When eating certain foods that you are sensitive to, you will experience chronic inflammation and chronic symptoms that you can’t seem to find a clear cause for.
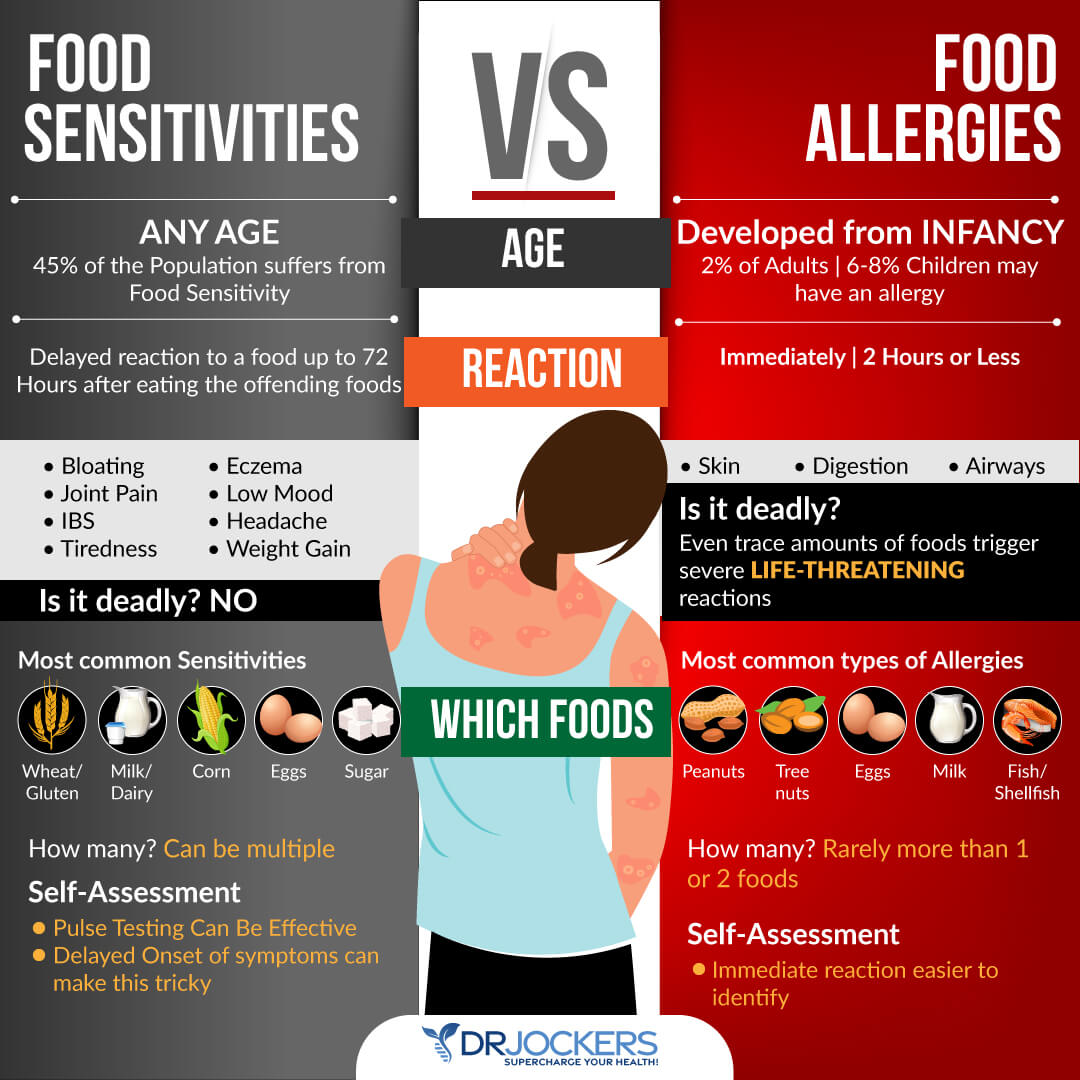
Common food sensitivities include gluten, sugar, soy, corn, shellfish, peanuts, and dairy. Spicy foods, caffeine, coffee, chocolate, acidic foods, carbonated drinks, and high-histamine foods are also common foods that may trigger gastrointestinal symptoms. However, you may find that you have issues with certain other foods.
There are various food allergy and food sensitivity blood tests out there. However, false results are common and these tests can’t check for every single potential food. To figure out your personal food triggers, I recommend a combination of an elimination diet, pulse test, and muscle response testing.
If you find any food sensitivities, remove these foods from your diet. Please note that food sensitivities can change over time. Testing for sensitivities regularly, once a year or if new symptoms pop up is critical for your health.
As you repair your body with a healthy diet and lifestyle, certain food sensitivities may also disappear and you may eventually be able to reintroduce some foods again. However, I recommend that you continue to avoid refined sugar, gluten, conventional dairy, food additives, and artificial ingredients.

Avoid Processed Vegetable Oils
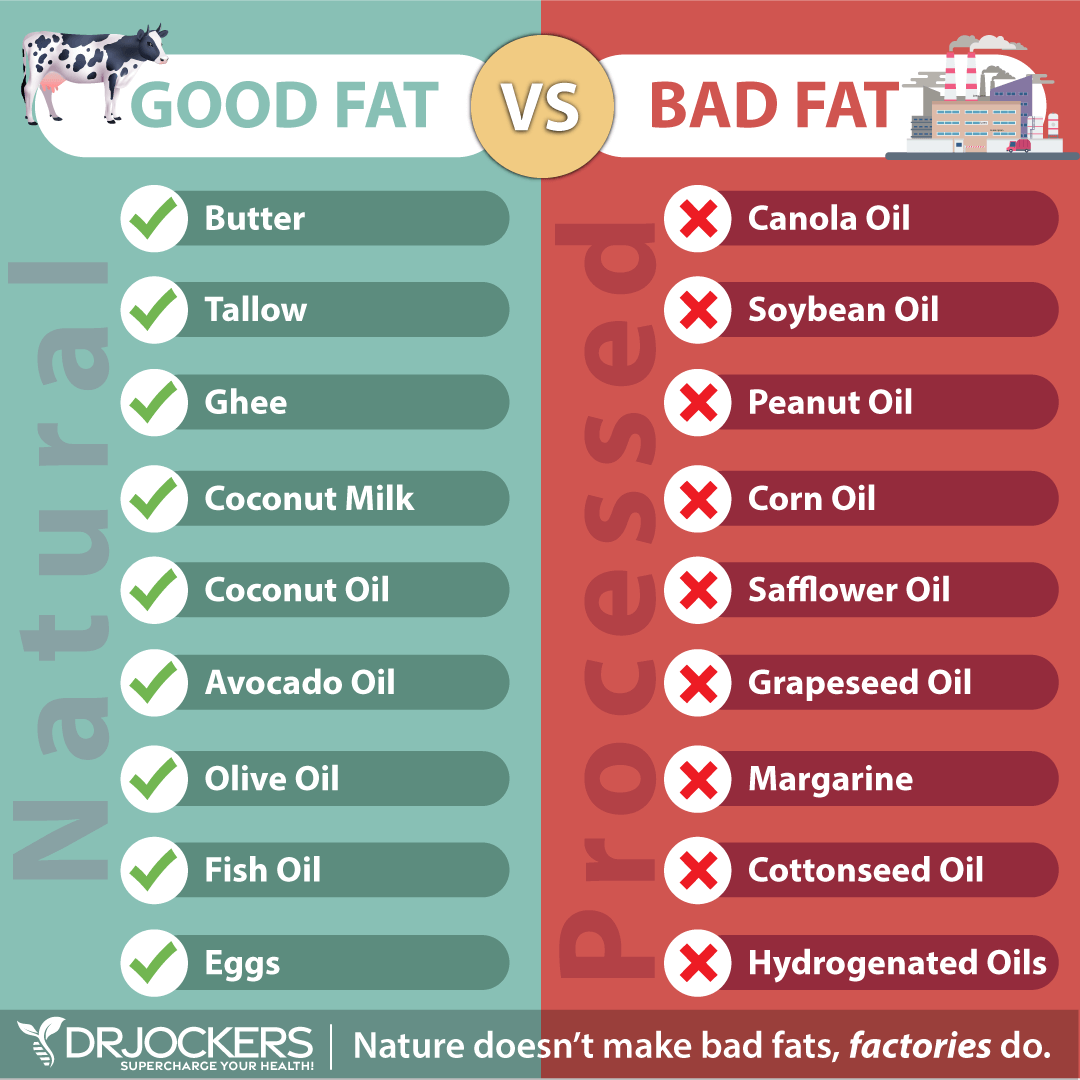
According to a 2019 study published in Nutrients, following a higher-fat diet may increase the risk of more bile acids in the stool compared to a lower-fat diet (5). Consuming too much processed vegetable oils may be a particular problem. Refined vegetable oils or industrial seed oils are highly processed oils extracted from corn, soybeans, safflower seeds, rapeseed (for canola oil), and cotton seeds.
Unfortunately, these processed vegetable oils are high in inflammatory omega-6 fatty acids and low in anti-inflammatory omega-3 fatty acids. They may increase the risk of inflammation and related disease.
According to a 2009 study published in the Journal of Lipid Research, pro-inflammatory polyunsaturated fatty acids can increase symptoms of IBS which, as you know, may also lead to bile acid malabsorption (6). They are also highly unstable, often genetically modified (GMO), and often full of unhealthy additives.
I recommend avoiding processed vegetable oils. If you are cooking with oils, I recommend extra virgin olive oil, virgin coconut oil, grass-fed butter and ghee, grass-fed beef tallow. You may learn about the healthiest cooking oil recommendations by reading this article.
Eat Low-Moderate Fat, High Protein Diet
A higher-fat diet may increase the risk of more bile acids in the stool compared to a lower-fat diet (5). According to a 2015 study published in Clinical Medicine (London) following a low-fat diet may be beneficial for those with bile acid malabsorption and diarrhea-prone IBS (7).
If you have bile acid malabsorption, I recommend following a low-moderate fat and high protein diet. Your fat sources should come from healthy fats, including avocados, coconut oil, olives, extra virgin olive oil, grass-fed butter, ghee, beef tallow, nuts, and seeds. Keep your fats on the lower or moderate sides.
Eat plenty of healthy protein from animal sources, including grass-fed beef, pasture-raised poultry and eggs, wild-caught fish and seafood, and wild game. Some with bile acid malabsorption do well with greens and other vegetables while others do not.
The same can be said with fruit and fermented foods so try small amounts and see how you tolerate them. Root vegetables such as carrots, beets and sweet potatoes are usually well tolerated when cooked and soft.
White and brown rice and gluten-free oats tend to be well tolerated by people with bile acid malabsorption and can help to reduce the fluid level in the bowel movements. These are foods you can try out and see if you tolerate well. I would recommend adding in collagen or bone broth protein into your grains to increase the protein levels if you are consuming them without other forms of protein.
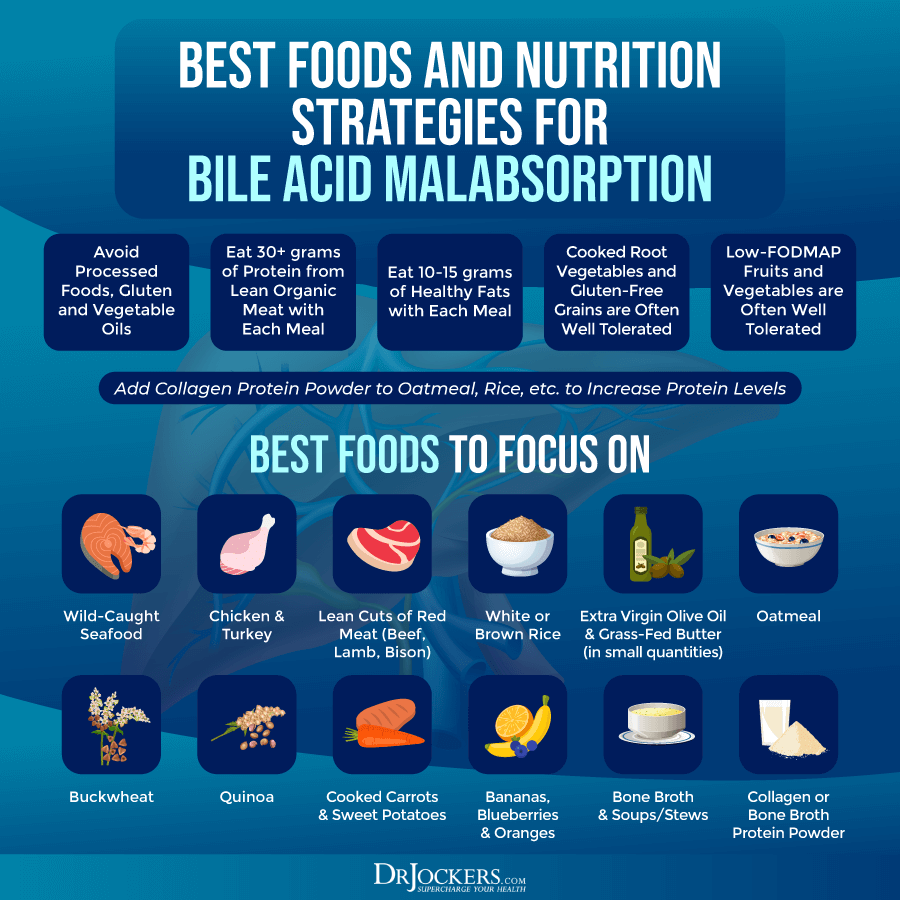
Use a Low-FODMAP Diet
FODMAP stands for Fermentable, Oligo, Di-, and Monosaccharides, and Polyols. A low-FODMAP diet is a diet low in FODMAP foods. A low-FODMAP diet is commonly used for SIBO, because higher FODMAP foods, such as beans, grains, cruciferous veggies, and many fruits tend to increase SIBO symptoms, including abdominal bloating. It is also often used for other digestive symptoms and gastrointestinal health issues. It may be helpful for bile acid malabsorption too.
According to a 2012 study published in Gut, a low-FODMAP diet may help to improve functional gastrointestinal symptoms, such as diarrhea (8). According to a 2016 review published in F1000 Research, a low-FODMAP diet may be beneficial for IBS (9). Since bile acid malabsorption is incredibly common in IBS patients, a low-FODMAP diet may help (3).
I recommend that you try a 2 week trial on a low-FODMAP diet. If you are not improving add back FODMAPs and see if you feel better or worse. If you are improving on a low-FODMAP diet or your symptoms worsen after adding FODMAPs back to your diet, you may benefit from following a low-FODMAP diet for longer-term until your body repairs itself.
Low-FODMAP vegetables include carrots, green beans, arugula, mint, basil, pepper, olive, pumpkin, tomato, potatoes, sweet potatoes, cucumber, zucchini, Swiss chards, lettuce, radishes, parsnip, sprouts, kale, and collard greens.
Low-FODMAP fruits include lemon, lime, kiwi, grapes, papayas, strawberries, raspberries, blueberries, melon, pineapples, and tangerines. Other low-FODMAP foods include egg, meats, fish, brazil nuts, chestnuts, butter, bone broth, seafood, quinoa, millet, rice, walnuts, and pinenuts. To learn more about the low-FODMAP diet, I recommend this article.

Use Digestive Enzymes
Digestive enzymes may help to reduce symptoms of diarrhea and IBS, which are often connected to bile acid malabsorption. According to a 2011 study published in Frontline Gastroenterology, digestive enzymes may be helpful for those who experience diarrhea after meals (10).
A 2011 study published in the European Review for Medical and Pharmacological Sciences has found that using digestive enzymes may reduce symptoms of IBS, including abdominal pain, diarrhea, gas, and bloating (11). I recommend Super Dzyme.

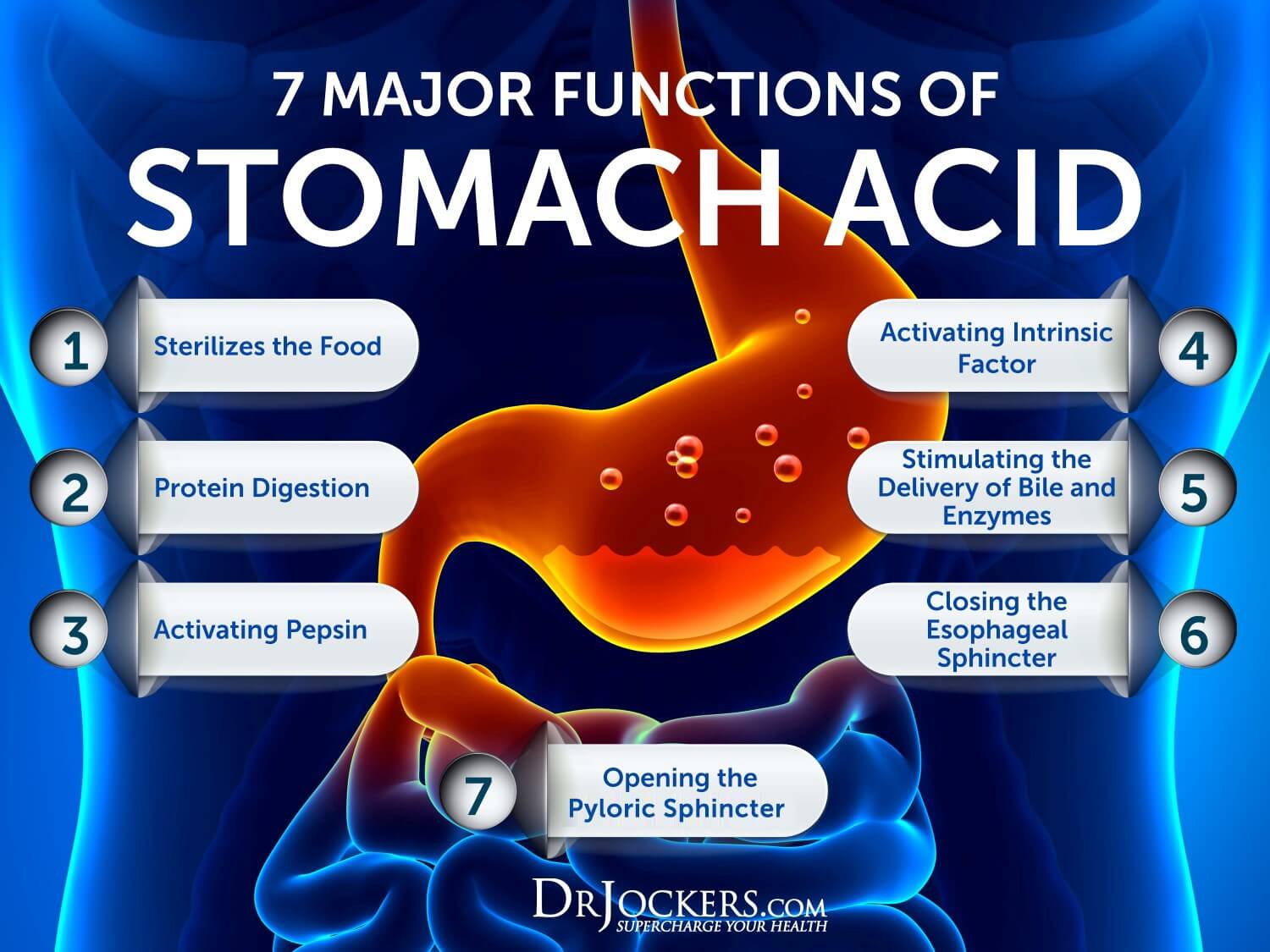
Support Stomach Acid Levels
Poor stomach acid is a common culprit behind digestive issues and gut health symptoms. A 2010 study published in the World Journal of Gastroenterology has found overlap and connection between gastroesophageal reflux disease and IBS (12).
According to the results of a 1986 study published in the Journal of the American Geriatrics Society and a 2004 study published in the American Journal of Medicine, a common root cause of gastroesophageal reflux is poor stomach acid production (13, 14).
Improving your stomach acid may not only improve acid reflux but also IBS and related bile acid malabsorption. You may benefit from supporting your stomach acid levels. To improve your stomach acid levels, I recommend the following:
- Use Liquid Nutrition Throughout the Day: Try to make sure that at least half of your meals are in a liquid form such as a protein shake or green smoothie. Protein shakes are pre-metabolized and very easy to digest and do not depend upon HCL production. If you have low HCL it may be helpful to drink one to two protein shakes daily to support amino acid absorption, reduce extra stress on your digestion, and support healthy stomach acid levels
- Use Ginger: Ginger is one of the best things for improving digestive juices. I recommend drinking 2 to 3 cups of ginger tea each day, you can put ginger essential oil in water (2 to 3 drops in 8 oz of water), juice a ½ inch of fresh ginger root in a green juice each day and use ground ginger on your foods. You can also add fermented ginger to your diet which is common in Asian dishes such as kimchi. Since spicy foods can be triggering for silent reflux, make sure that it is not triggering for you. If it is, focus on the other steps.
- Super Hydrate Outside of Meal Times: Good hydration can help activate bowel motility and push contents through the digestive system which will reduce microbial fermentation and toxicity in the body. This can help to support your stomach acid levels.
- Drink Very Little With Meat Containing Meals: When you are eating meat or any sort of heavier food, you should stop drinking water or other liquids at least 30 minutes before the meal, except if you need to take a supplement with 2 ounces of water. Holding off water during these meals will reduce any potential dilution of the gastric juices and allow for better digestion.
- Hold Off On Water After a Meal: To allow for optimal digestion, I also recommend not drinking water or other liquids until at least 30 minutes after a meal. This allows for proper stomach acid activity, sterilization, and protein metabolism.
- Use Lemon and Apple Cider Vinegar: Squeezing fresh lemon or using lemon juice or apple cider vinegar on your meat and vegetables helps to pre-metabolize the food and support better digestion and nutrient absorption. You can either marinate foods in a lemon or ACV base or just add them as a dressing right before you consume them. Again, make sure that apple cider vinegar is not triggering your silent reflux symptoms and if it is, focus on my other recommendations.
- Eat Protein Foods at the Beginning of the Meal: The stomach will begin churning out its stomach acid when you begin eating, especially when you are consuming protein. While it’s culturally common to a salad before their protein dish, this is not great for your HCL production. It is a much better idea to eat your protein with the salad or vegetables instead of after.
- Use Fermented Veggies: Fermented foods such as sauerkraut, kimchi, pickles, pickled ginger, and other fermented vegetables all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions I recommend using one of these with all of your heavier meals and especially any meal with protein.
- Use Fermented Drinks: Fermented drinks such as apple cider vinegar, coconut kefir, and kombucha offer antimicrobial benefits and help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Keeping H Pylori levels down is critical for the body to be able to produce enough stomach acid.
- Eat Your Largest Meal When You Are Most Relaxed: Your body needs to activate the parasympathetic nervous system to produce enough stomach acids. If you are busy and on the go, you will be in fight or flight sympathetic mode. If you struggle with low stomach acid, this fight or flight state is not going to allow your body to produce anywhere near enough. Relaxing before the meal is important to improve stomach acid production.
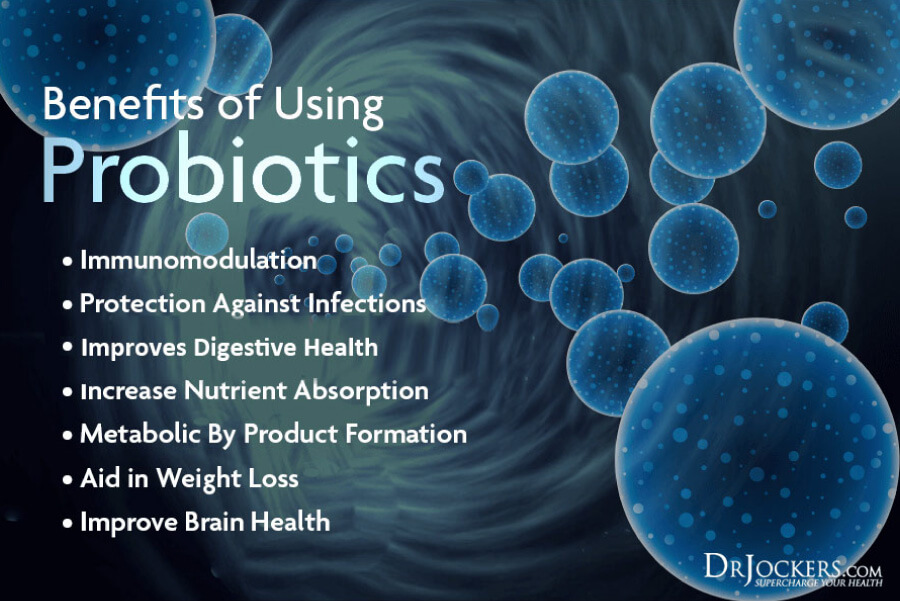
Use Powerful Probiotics
Probiotics are incredibly important for your gut health and digestion. If you are dealing with any sort of digestive symptoms, probiotics are likely beneficial for you. Probiotics are beneficial microorganisms in your gut. They are the gut bacteria that help to create balance in your gut microbiome.
If there are too many bad bugs but too few beneficial bacteria in your gut, it leads to gut dysbiosis and gut health issues, including IBS, Crohn’s disease, and other problems that may increase your risk of bile acid malabsorption. Probiotics help to create gut flora balance and support gut health.
Probiotic-rich foods include sauerkrauts, fermented herbs, kimchi, kefir, kombucha, and yogurt. However, eating probiotic-rich foods is not enough to support your gut flora, especially if you are dealing with gut microbiome imbalance and all kinds of chronic gut health issues.
Probiotics may help to improve bile acid malabsorption and other gut health issues. According to a 2021 study published in the Proceedings of the National Academy of Sciences, probiotics may help to manipulate bile acid to create better gut health (15).
If you are dealing with chronic gut health problems, including diarrhea from bile acid malabsorption, you may benefit from using some powerful probiotics with 100 billion CFUs. I recommend using Probiocharge 100 Billion.
Support Liver Function
Liver function is closely connected to bile acid absorption. I recommend using some foods and herbs that support liver health.
Some of the top foods and herbs that support your liver include cruciferous vegetables, such as broccoli, cauliflower, Brussel’s sprouts, cabbage, collard greens, and cabbage, sulfur-rich foods, including cruciferous vegetables, garlic, online, and egg yolk, beets, citrus, leafy greens, berries, and fruits rich in vitamin C, including citrus, strawberries, kiwi, pineapple, broccoli, and bell pepper, avocados, olive oil, and certain herbs, including milk thistle, dill, caraway, and turmeric (16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28).
I also recommend taking Advanced TUDCA. This blend of tauroursodeoxycholic acid (TUDCA), BioActive Carbon, N-acetyl cysteine (NAC), and melatonin combines Carbon Technology’s proprietary blend of fulvic acids and polysaccharides that support cellular repair and the body’s natural ability to detoxify. With a low pH, Carbon Technology also helps protect ingredients from being digested by stomach acid, so that they remain intact as they enter the desired location in the body.
Carbon Technology also boosts TUDCA’s ability and efficacy to work systemically throughout the body while melatonin serves as a driver to help deliver the product into target areas, particularly at the liver; however, in this formulation, melatonin will not cause sleepiness. Finally, NAC helps further the body’s natural detoxification efforts and replenish glutathione levels.
Use a Strong Bile Acid Binder
Binders are various substances that ‘bind’ to toxins by either trapping them or attracting them through a negative charge in your body then helping them remove them through bowel movements. Binders are very important for detoxification.
Binders are various substances that ‘bind’ to toxins by either trapping them or attracting them through a negative charge in your body then helping them remove them through bowel movements.
It is great for binding with mold mycotoxins, pesticides, and some drugs, but doesn’t work well for heavy metals. Activated charcoal can also adsorb bile acid and cholesterol. According to a 1980 study published in Lipids, activated charcoal may help to remove bile salts (29). If you have bile acid malabsorption, I recommend using this Activated Charcoal.
Consider GI MAP Test
I recommend a GI Map Stool Analysis to look for gut infections, steatocrit levels, and beta glucuronidase levels. The GI Map Stool Analysis is the best comprehensive stool test I’ve found and recommend to my patients. It looks at all major factors of your gut health and helps us figure out the root causes of your issues and find the best treatment strategies.
This takes the guesswork out of the process and also helps to see your true progress. This test offers everything that I, as a natural health and functional medicine doctor, need to see to make good clinical decisions and offer a treatment protocol that can help to improve your gut microbiome and your overall health.
Final Thoughts
Bile acid malabsorption is a health condition that you develop when your intestines are unable to absorb bile properly. Bile acid malabsorption leads to bile acid build-up which can cause watery diarrhea and other symptoms. I recommend that you follow my strategies for bile acid malabsorption to improve your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and thrive in life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!