 Low Oxalate Diet: Overview, Best Foods, and How to Do It
Low Oxalate Diet: Overview, Best Foods, and How to Do It
We all have different bodies. While some foods are healthy for some people, they may cause symptoms of health issues in others. High oxalates foods are like that. Oxalates are naturally occurring compounds found in plants, animals, and humans.
Some of our healthiest foods, including many greens, vegetables, and fruits, are high in oxalates. Though for most people, oxalates don’t cause issues, for some, they can lead to chronic symptoms and health complications.
In this article, you will learn about oxalates. You will understand what oxalates are. You will understand the signs and symptoms of poor oxalate metabolism. I will go over the causes of poor oxalate metabolism. You will find a list of high oxalate foods and low oxalate foods. I will discuss how to follow a low oxalate diet. I will share my top strategies to reduce your oxalate levels.

What Are Oxalates?
Oxalates are naturally occurring compounds. They are found in plants, animals, and humans. Your body can naturally synthesize oxalates from various compounds, including excess vitamin C, fructose, and yeast. Certain nutrient deficiencies may also increase oxalate synthesis.
A 1984 study published in the Journal of Nutrition has found that a high sugar diet combined with low levels of vitamin B6 may increase oxalate synthesis (1). According to 1982 research published in the Journal of Urology, magnesium deficiency may increase calcium oxalate formation (2). A 1987 study published in the Annals Annals of Nutrition Metabolism has found that thiamine deficiency may also contribute to oxalate synthesis (3).
The problem is that too many oxalates and oxalate intolerance can lead to chronic inflammation and chronic symptoms in some people. Unfortunately, oxalates are found in high concentrations in some of the healthiest foods we have on the planet.
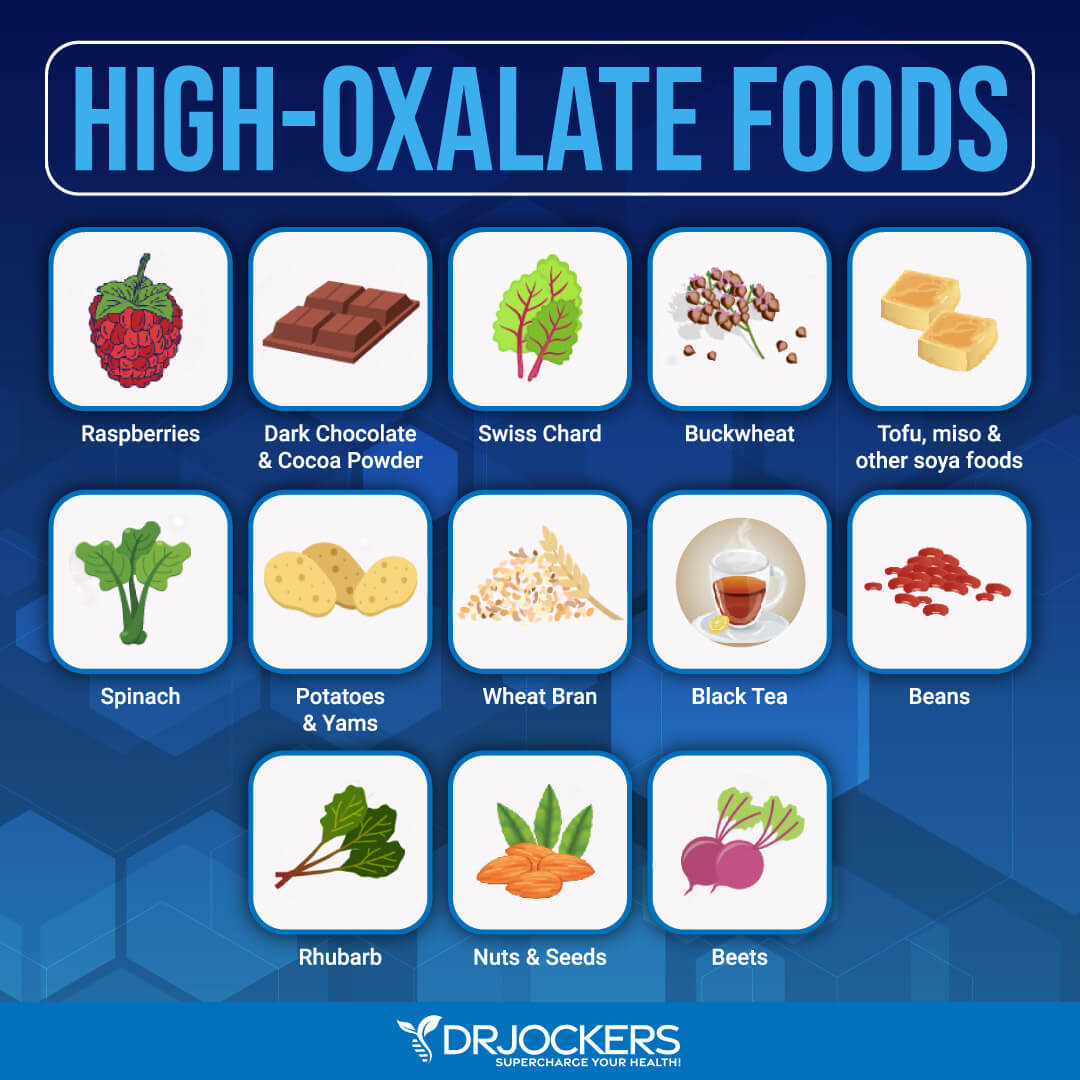
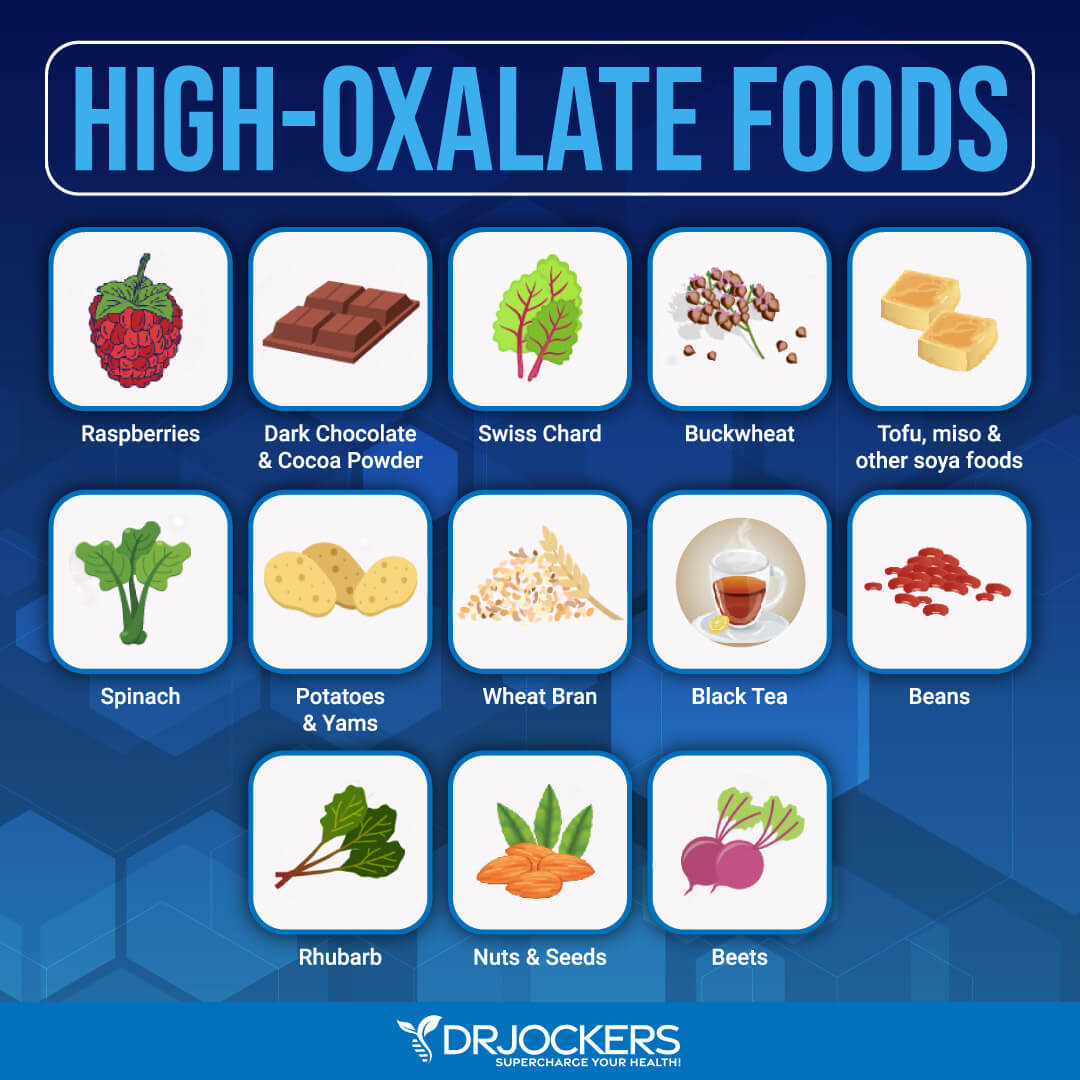
Though fruits are generally lower in oxalates, raspberries, and citrus, especially grapefruit, have high levels. In the vegetable world, beets, olives, spinach, yams, turnips, and rhubarb are among the top high-oxalate foods.
Grains, including oatmeal, whole wheat, brown rice, soy flour, buckwheat, and couscous, are high in oxalates. Meat alternatives, such as tofu, soy, and other vegetarian burgers, are also high in oxalates, so are almonds and most other nuts.
If you have issues with poor oxalate metabolism and oxalate intolerance, the excess oxalates found in food can aggravate your health issues. In this case, you may benefit from a low oxalate diet. You may learn about oxalate intolerance from this article.
Signs & Symptoms of Poor Oxalate Metabolism
Signs and symptoms of poor oxalate metabolism may include:
- Inflammation in joints causes muscle stiffness and pain.
- Kidney stones
- Urinary tract irritation, pain, or urgency to urinate.
- Vulvar pain (chronic irritation and pain of the female genitalia)
- Abdominal problems such as constipation or diarrhea
- Vitamin or mineral deficiency such as magnesium or vitamin B
- Lethargy or problems sleeping
- Histamine reactions such as hives
Health conditions associated with poor oxalate metabolism may include:
- Vulvar pain syndrome
- Cystic fibrosis
- Chronic obstructive pulmonary disease (COPD) or asthma
- Chronic kidney stones (medically termed nephrolithiasis)
- Thyroid disease or problems such as lupus, cirrhosis, or Wilson’s Syndrome
- Connective tissue disease
- Autism
- Autoimmune issues
- Irritable bowel syndrome (IBS)
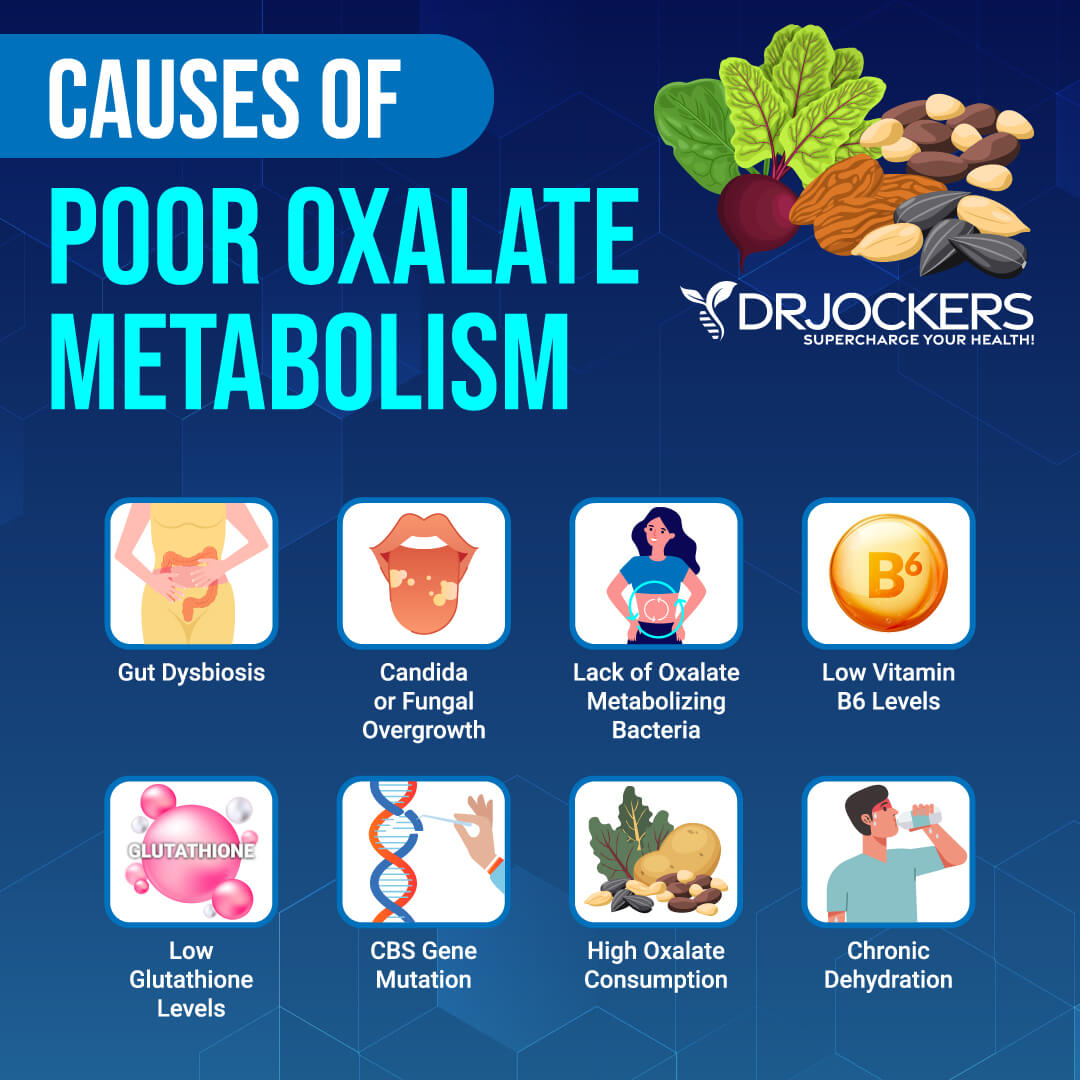
Causes of Poor Oxalate Metabolism
Poor oxalate metabolism can have several underlying causes, including gut dysbiosis, candida or fungal overgrowth, low vitamin B6 levels, low glutathione levels, CBS dysregulation, high oxalate consumption, low water intake, or dehydration. Let’s look at each of these factors one by one.
Gut Dysbiosis
Your gut is the home of trillions of microbes. Some of the bacteria in your gut are beneficial or ‘good’ that support your health. While others are harmful or ‘bad’ and can disrupt it. For gut and overall health, you need a nice balance of both, with more beneficial bacteria than bad ones.
Antibiotic overuse, a poor diet, chronic stress, environmental toxins, poor lifestyle choices, and other factors may throw this balance off, increasing the bad bugs in your gut. If your gut microbiome is out of balance and there are too many harmful bacteria, you have gut dysbiosis.
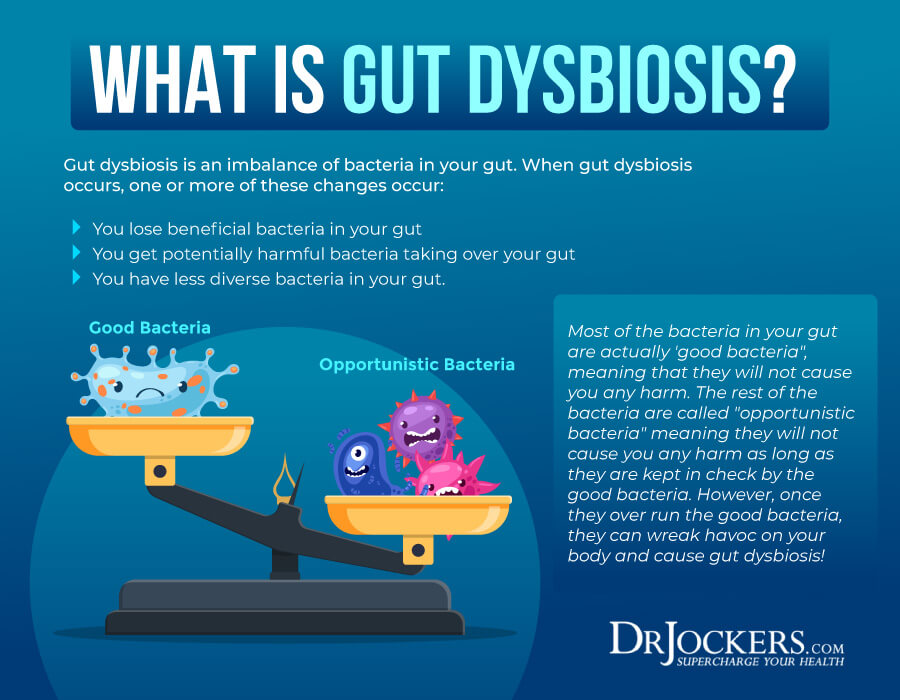
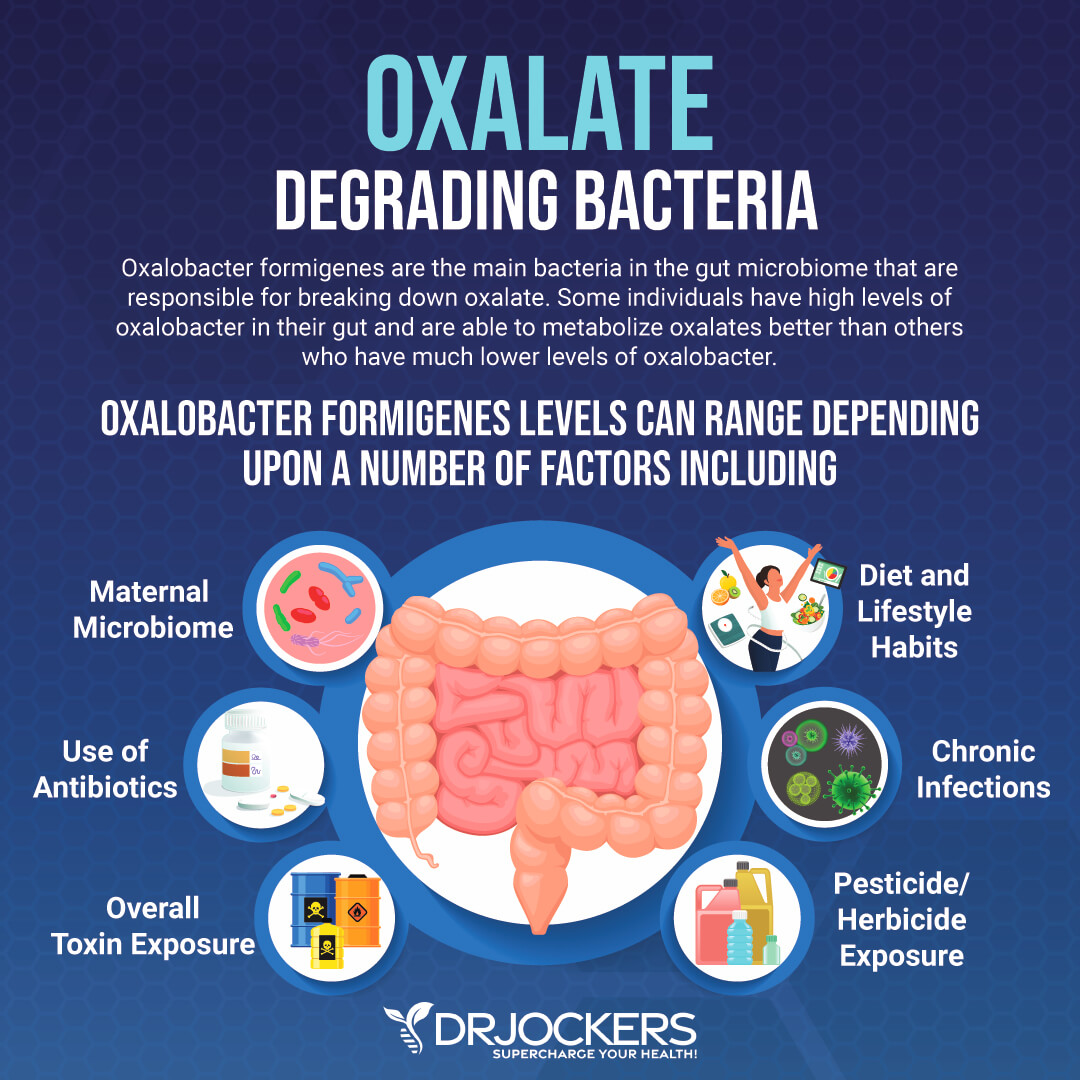
Gut dysbiosis may be characterized by low levels of good bacteria that help to reduce oxalate overload. Oxalobacter formigenes are bacteria in your intestines that are responsible for breaking down oxalate. A 2002 study published in Applied Environmental Microbiology has found that oxalobacter formigenes are characterized by oxalate-degrading characteristics and may reduce oxalate levels (4).
Another 2002 research published in European Urology has found that oxalobacter formigenes may play a role in reducing calcium oxalate stone disease (5). Other healthy bacteria that may help to break down oxalates include eubacterium, enterococcus faecalis, and lactobacillus acidophilus, and Bifidobacterium lactis (6). Low levels of these bacteria may lead to poor oxalate metabolism and oxalate-related issues.
Candida or Fungal Overgrowth
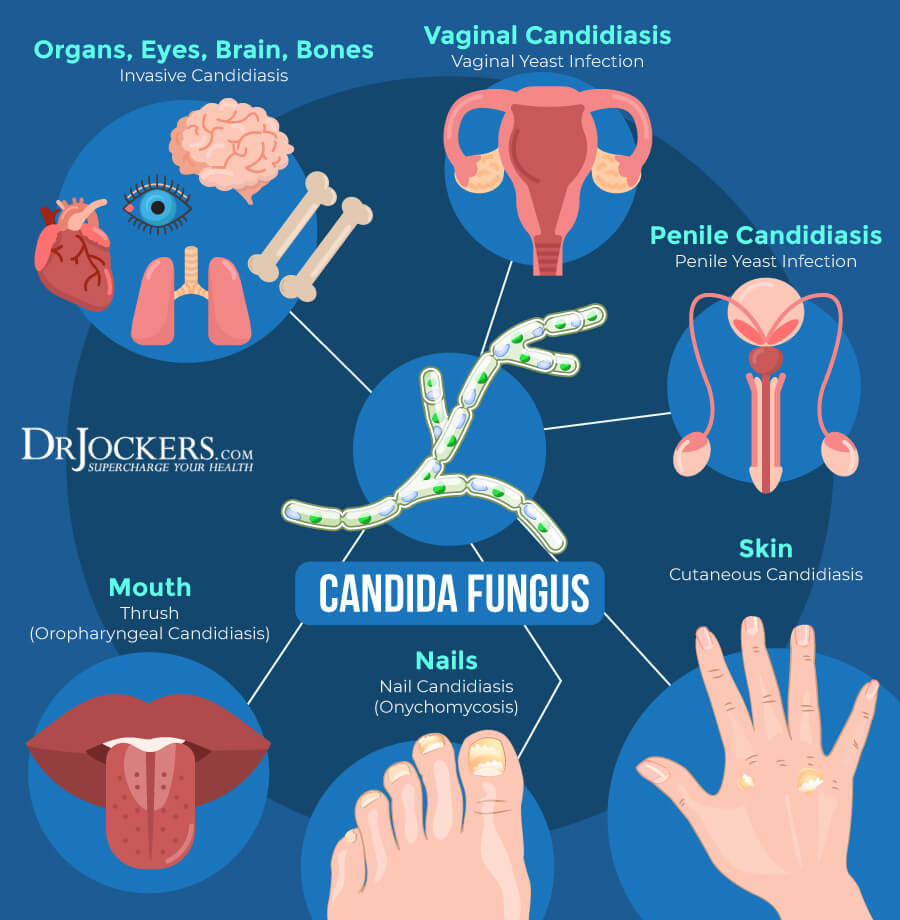
You may develop poor oxalate metabolism and oxalate-related health issues due to an underlying candida or fungal overgrowth. As you already know, your gut microbiome levels are directly related to your urine oxalate levels. It’s not only bad bacteria, but other pathogens, such as candida and other fungi can throw off your gut microbiome balance.
Candida albicans are a common fungus that occurs at small levels in the human body. Higher levels can lead to candida overgrowth and related health issues. Oxalate stones in the kidney are often surrounded by candida and fungi. Oxalate sensitivity is common in patients with candida overgrowth.
Yeast infections may also be linked to high oxalate levels. 2020 research published in the Journal de Micologie Medicale looked at 164 urine samples of 74 kidney stone patients and found 77 candida isolates (7). This suggests that candida may play a role in kidney stones and UTI, which can be characterized by high oxalate levels.
Low Vitamin B6 Levels
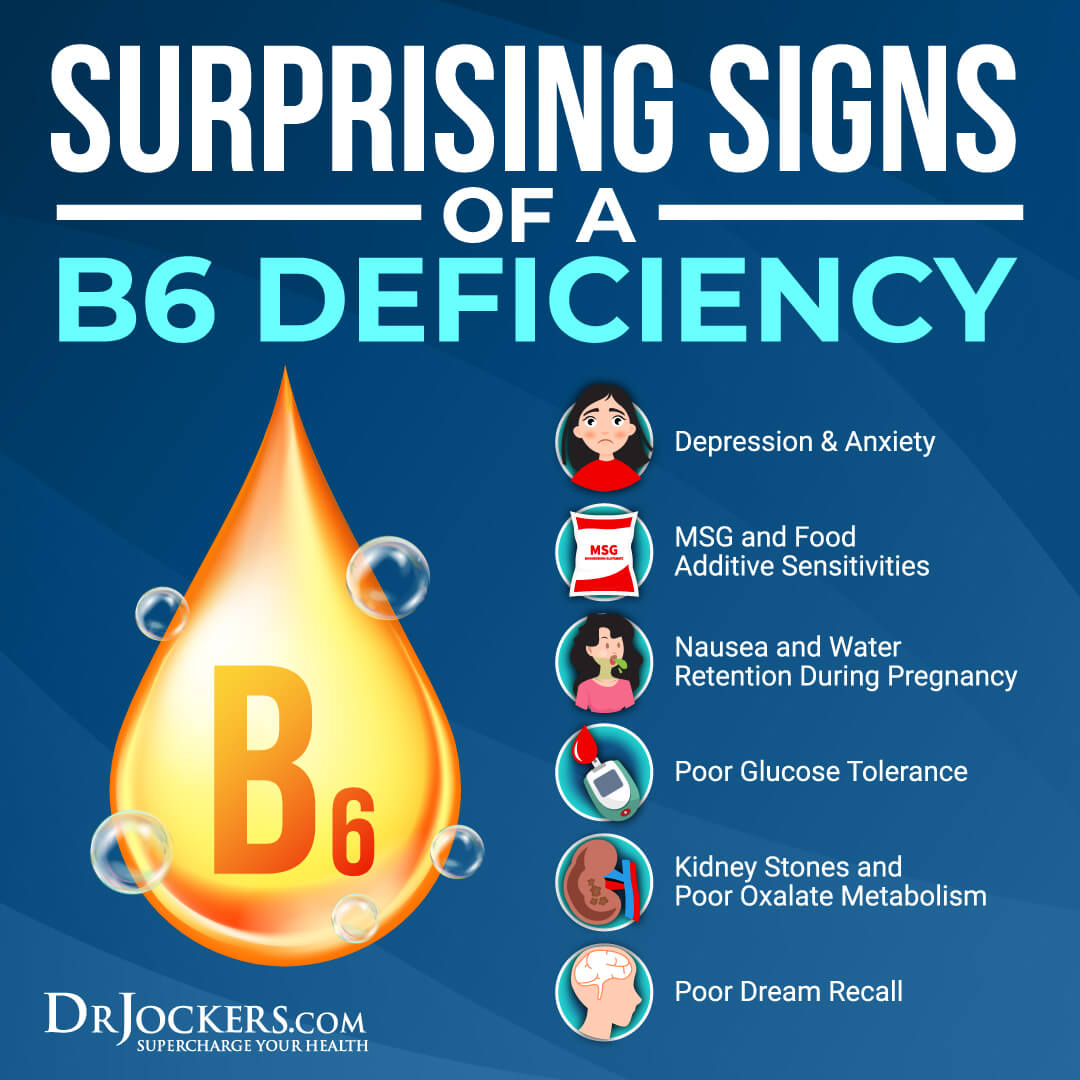
Vitamin B6 is critical for your immune, brain, and nervous system health. As mentioned earlier, vitamin B6 deficiency may lower your body’s ability to adequately methylate and support proper oxalate synthesis. It is critical for the Citric Acid Cycle.
Poor methylation can lead to oxalate buildup, and oxalates may also interrupt methylation. A 1984 study published in the Journal of Nutrition has found that a high-sugar diet combined with low levels of vitamin B6 may increase oxalate synthesis (1).
According to a 2022 review published in Frontiers in Nutrition and Food Science Technology, vitamin B6 is also an essential nutrient for your gut lining (8). Thus, low vitamin B6 levels may lead to gut inflammation, leaky gut syndrome, and gut microbiome imbalance, increasing poor oxalate metabolism. It may also contribute to fat malabsorption issues, which in cystic fibrosis patients may further aggravate gut inflammation and increase kidney stones (9, 10).
Low Glutathione Levels
Glutathione is a powerful antioxidant that is critical for gut health, insulin sensitivity, and the reduced risk of disease. Low glutathione levels may increase oxalate issues. According to a 1998 study published in Molecular and Cellular Biochemistry, glutathione plays a role in mitochondrial health in the kidneys and hyperoxaluria (11).
It’s not only vitamin B6 and good methylation but also glutathione that’s necessary for oxalate metabolism in the Citric Acid Cycle. Glutathione may protect B vitamins from toxins in the methylation cycle.
According to 2004 research published in Chemical Research in Toxicology, glutathione is critical for protecting vitamin B12 from xenobiotics (12). Low glutathione levels may result in the inefficiency of methylation. Poor methylation and poor vitamin B6 levels may lead to oxalate issues.

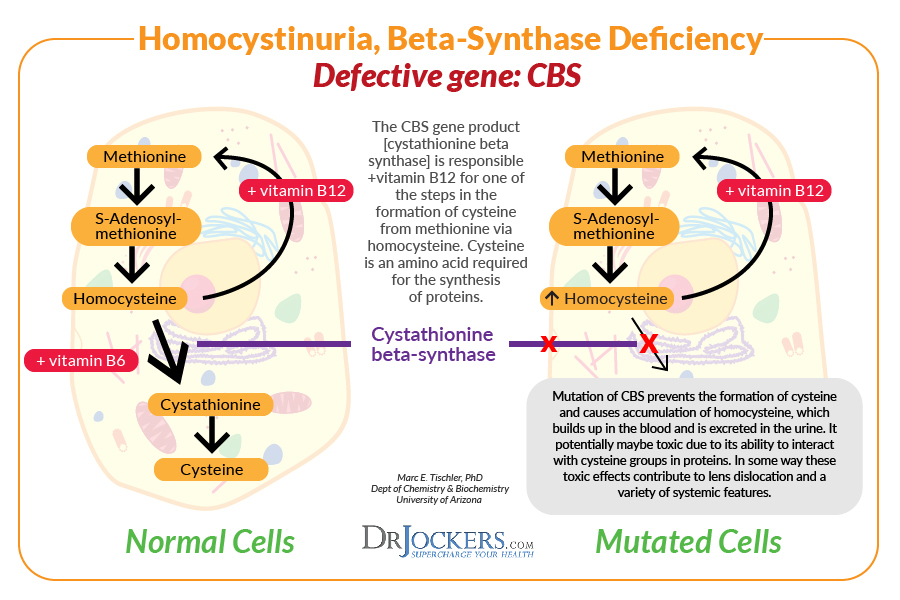
CBS Gene Dysregulation
The Cystathionine Beta Synthase or CBS gene plays a role in creating an enzyme called cystathionine beta-synthase, which is responsible for using vitamin B6 to convert the amino acids, homocysteine and serine to cystathionine. After this, another enzyme makes the amino acid cysteine from cystathionine.
Cysteine is then used to build proteins or is broken down and removed through urine. The CBS pathway is a sulfuration pathway that plays a role in glutathione production and detoxification.
CBS gene dysregulation may happen due to genetic expression or environmental upregulation from a yeast infection or other health issues. CBS gene dysregulation may result in oxalate formation because it needs vitamin B6 and its role in glutathione formation.
According to a 2018 study published in Molecular Genetics and Genomic Research, CBS mutations may help to predict B6-responsiveness in homocystinuria (13). Moreover, when the CBS pathway is impaired, and not enough glutathione is made, it may increase oxalate levels.
High Oxalate Consumption
High oxalate consumption or a high-oxalate diet may also lead to poor oxalate metabolism-related issues and high oxalate levels. A healthy body with enough oxalate-degrading bacteria and without other health issues contributing to poor oxalate metabolism should handle high oxalate foods.
However, people who are dealing with gut dysbiosis, candida or fungal overgrowth, CBS gene mutation, nutrient deficiencies, kidney or liver problems, or even chronic stress may have difficulties breaking down and eliminating oxalates properly.
If you are one of these people, a high oxalate diet may lead to chronic symptoms and oxalate-related health issues. For example, according to a 2020 review published in Nutrients, a high oxalate diet may increase kidney issues (14).
Low Water Intake and Dehydration
Finally, low water intake and dehydration may also contribute to high oxalate levels. Dehydration may increase the formation of calcium oxalate stones. Calcium and oxalates both play a role in the development of kidney stones.
If you don’t drink enough water, they may bind together in the kidneys instead of your digestive tract. If you are dehydrated and there isn’t enough liquid in your urine, oxalates, and calcium can build up and form kidney stones.
The stones may also pass the kidneys and get stuck in your ureters or urethra. According to a 2020 review published in the Turkish Journal of Urology, proper hydration may help to prevent kidney stone disease (15).
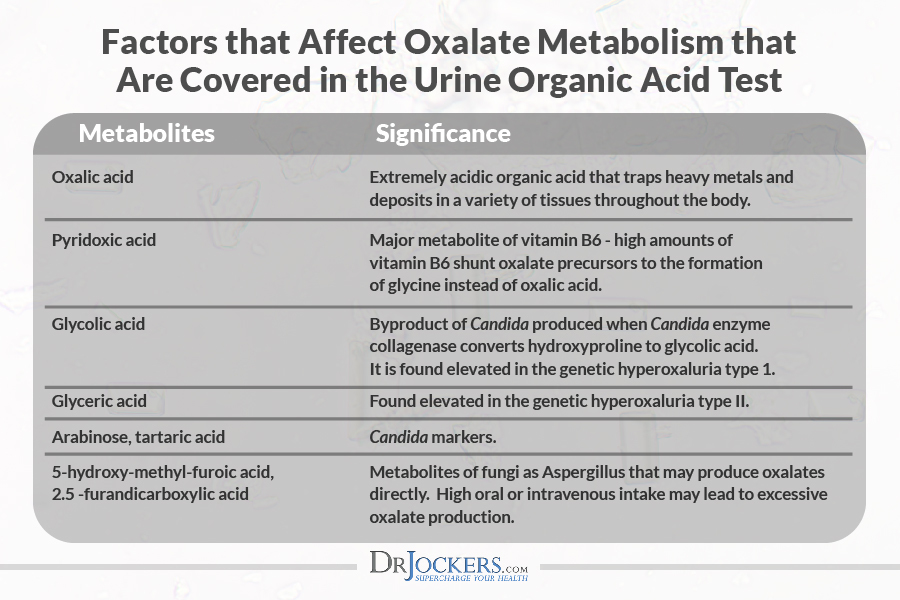
Testing For Oxalate Metabolism:
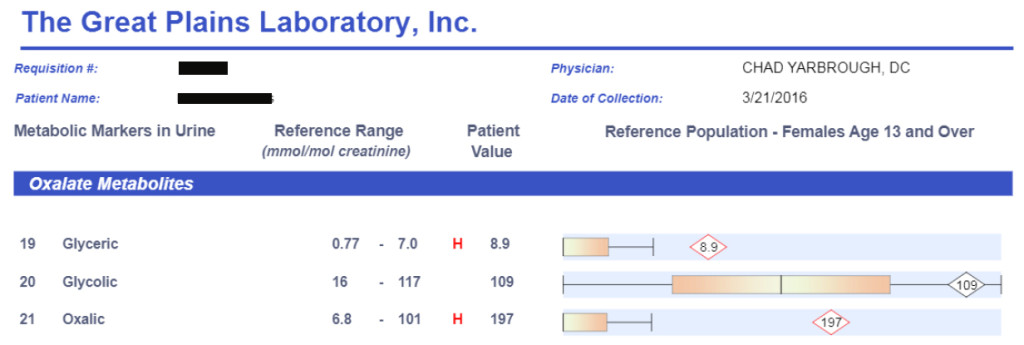
Clinically, I use the Great Plains Laboratory organic acid test to determine if someone has elevated oxalates in their system. This is a simple urine test done in the comfort of your own home.
When I see elevated oxalic acid with elevated glyceric or glycolic acid it is usually a sign of a genetic hyperoxaluria. When oxalic acid is elevated without an elevation in glyceric or glycolic acid it is typically related to Candida Albicans overgrowth or a very high vitamin C intake.
This test also lets me analyze for vitamin B6 deficiencies and for Candida overgrowth which are both major causes of hyperoxaluria. From a functional nutrition and natural medicine perspective this test helps me to determine the cause and best diet and treatment for this condition.
High Oxalate Foods
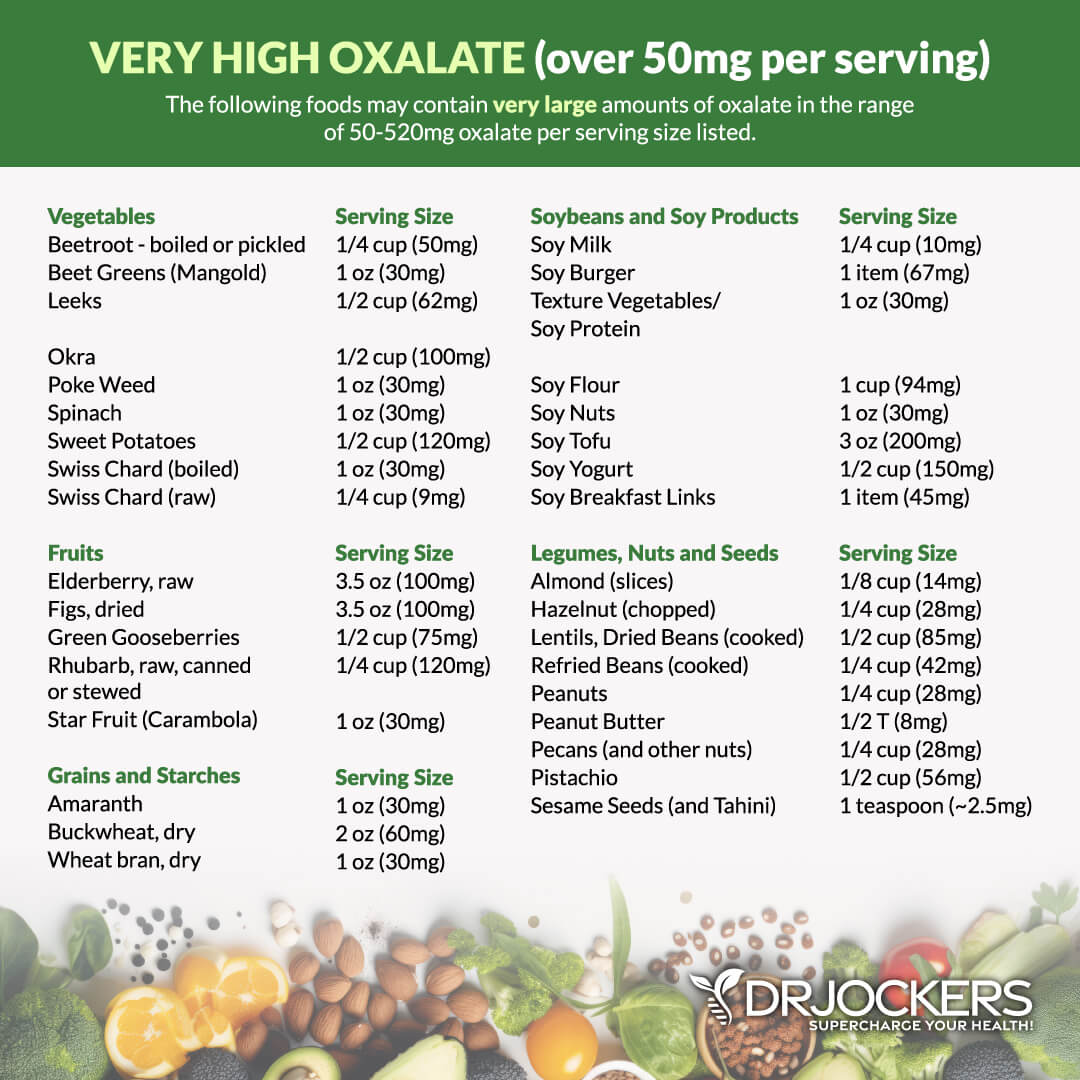
High oxalate foods that should be limited on a low oxalate diet include:
Some fruits:
- Berries
- Kiwis
- Figs
- Raspberries
- Oranges
- Grapefruit
- Purple grapes
Some vegetables:
- Spinach
- Swiss chard
- Rhubarb
- Okra
- Celery
- Beets
- Potatoes
- Leeks
- Turnip
- Yam
- Okras
- Carrots
- Plantains
- Sweet potatoes
- Olives
Some nuts and seeds:
- Almonds
- Cashew
- Peanuts
- Walnuts
- Pistachio
- Macadamia
- Sunflower seeds
- Pumpkin seeds
Soy products
- Soybeans
- Soy burgers
- Tofu
Some grains:
- Wheat germ
- Quinoa
- Bran flakes
- Buckwheat
- Couscous
Some drinks:
- Hot chocolate
- Chocolate milk
- Tea
Chocolate products:
- Cacao
- Cocoa
- Chocolate
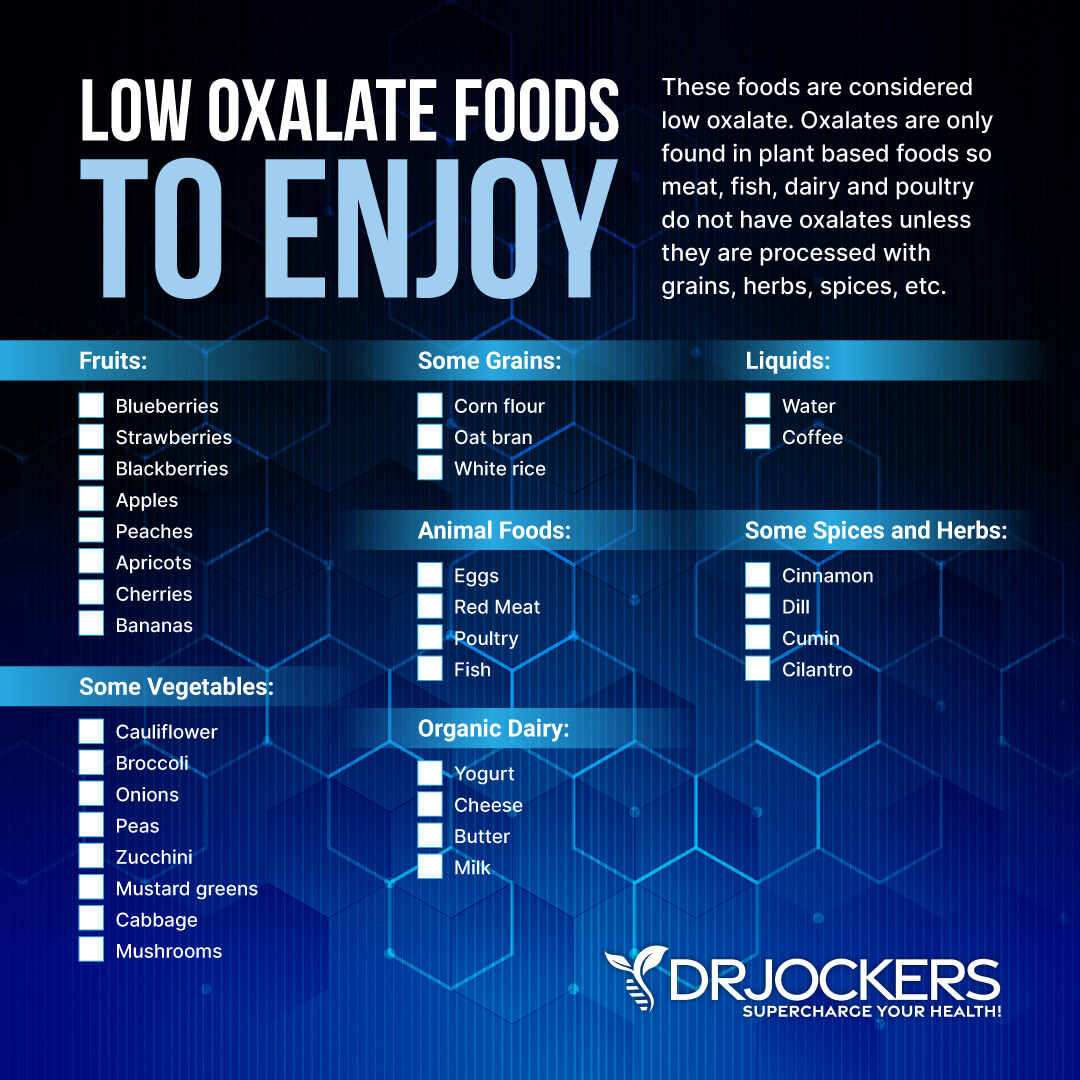
Low Oxalate Foods
Low oxalate foods to be used on a low oxalate diet include:
Some Fruits:
- Blueberries
- Strawberries
- Blackberries
- Apples
- Peaches
- Apricots
- Cherries
- Bananas
Some Vegetables:
- Cauliflower
- Broccoli
- Onions
- Peas
- Zucchini
- Mustard greens
- Cabbage
- Mushrooms
Some Grains:
- Corn flour
- Oat bran
- White rice
Animal Foods:
- Eggs
- Meat
- Poultry
- Fish
Organic Dairy:
- Yogurt
- Cheese
- Butter
- Milk
Liquids:
- Water
- Coffee
Some Spices and Herbs:
- Cinnamon
- Dill
- Cumin
- Cilantro
How to Follow a Low Oxalate Diet
Following a low oxalate diet may help if you have poor oxalate metabolism related issues or high oxalate levels. Reduce or avoid the consumption of high oxalate foods and focus on low oxalate foods instead, as listed in the earlier section.
If you are consuming any high oxalate foods, such as cruciferous vegetables or leafy greens, make sure you cook them, as cooking can help to break down oxalates. Soaking nuts, seeds, and beans may also help to remove oxalates from these foods.
Oxalate dumping refers to what happens when your cells ‘dump’ oxalate from your body after starting a low oxalate diet. If this happens too quickly, you may experience symptoms related to oxalate dumping, including rashes, hives, pain with urination, grainy stools, moodiness, and irritability. To avoid this, I recommend a gradual 10 to 20 percent reduction of oxalate in a week.

Strategies to Reduce Oxalate Levels
So, how can you reduce your oxalate levels? Here is what I recommend.
Limit High Oxalate Foods
One of the easiest ways to reduce your oxalate levels is to limit your consumption of high oxalate foods. Use the list in the earlier section and limit or avoid those foods.
Researching and following a low oxalate diet is one of the first steps you should take when it comes to reducing oxalate induced inflammatory issues. Depending on your issues, this may be temporary or may be critical for the long term.
Cook Higher Oxalate Foods
As I mentioned earlier, cooking higher oxalate foods may help to reduce oxalate levels. A 2005 study published in the Journal of Agriculture and Food Chemistry has analyzed and compared nine different types of raw and cooked foods for oxalate content (16).
They found that boiling was the most effective at 30 to 87 percent of oxalate reduction. Steaming led to 5 to 53 percent reduction. Baking was also tested for potatoes, and it didn’t lead to any oxalate loss.
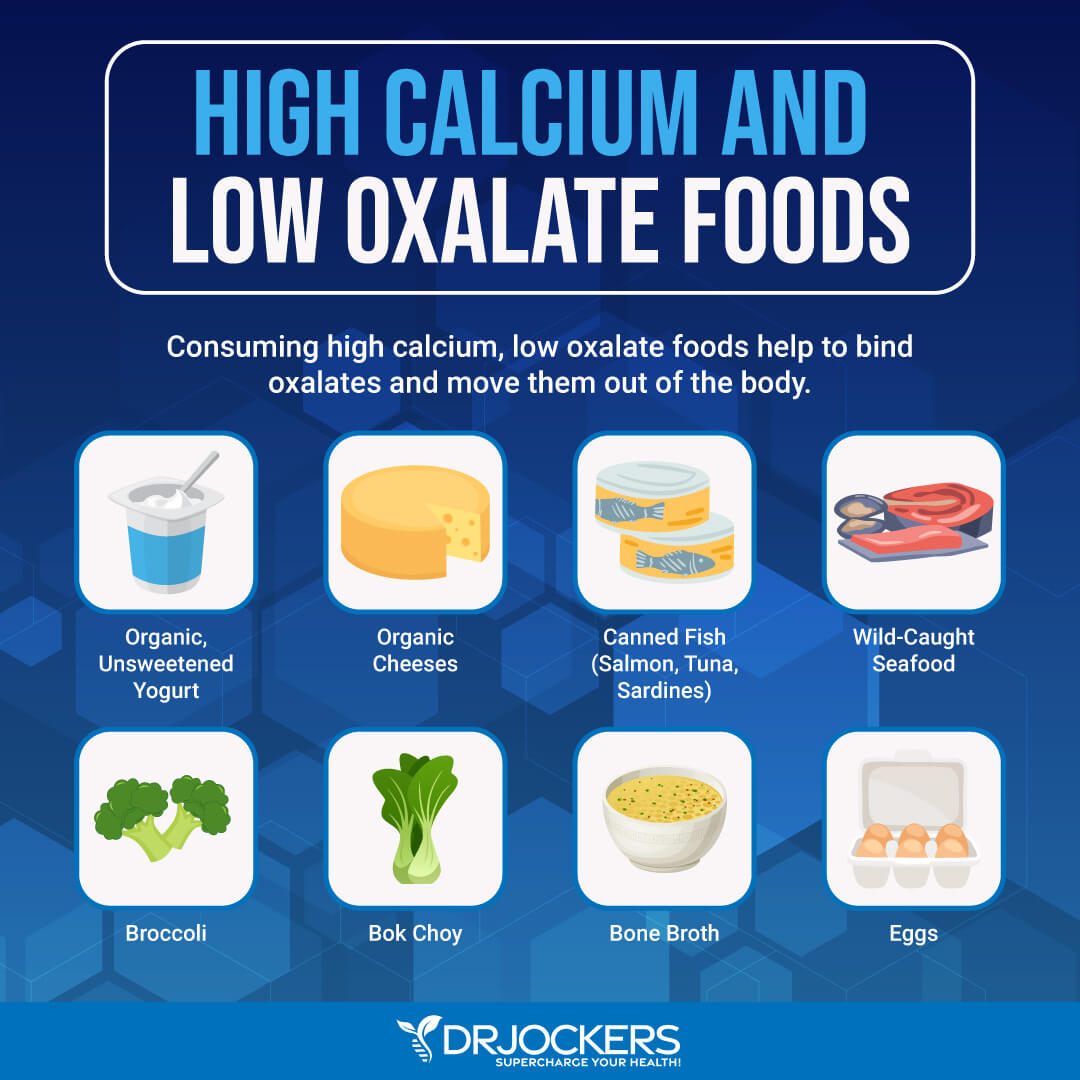
Consume High Calcium, Low Oxalate Foods
Calcium binds to oxalates and helps move them out of the body. If you are dehydrated, however, it can cause kidney stones. I recommend staying well hydrated and consuming low oxalate, high calcium foods. The best combination is high calcium foods that are also high in magnesium and low in oxalates and low in sugar.
For example, organic unsweetened yogurt, cheese, canned fish, broccoli, and bok choy are good options for foods that. Combine high calcium/magnesium foods with low oxalate foods using the list from earlier.
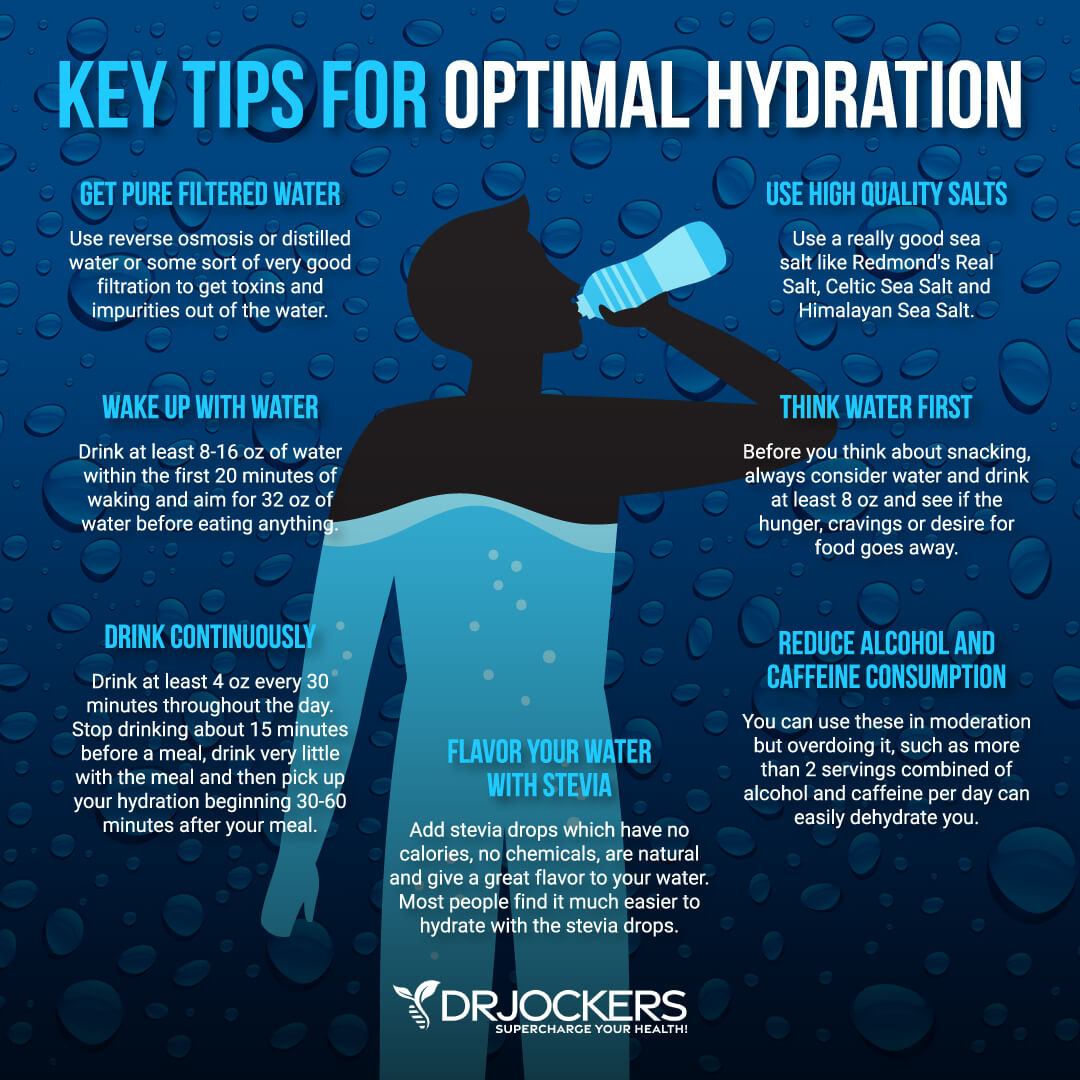
Good Hydration
Since dehydration may lead to high oxalate levels and kidney stones, I recommend hydrating your body appropriately. Start your day with 16 to 32 oz of water.
You may add some lemon or low oxalate fruits or herbs for taste. Drink a glass of water every hour after. Consume hydrating low oxalate fruits and vegetables.
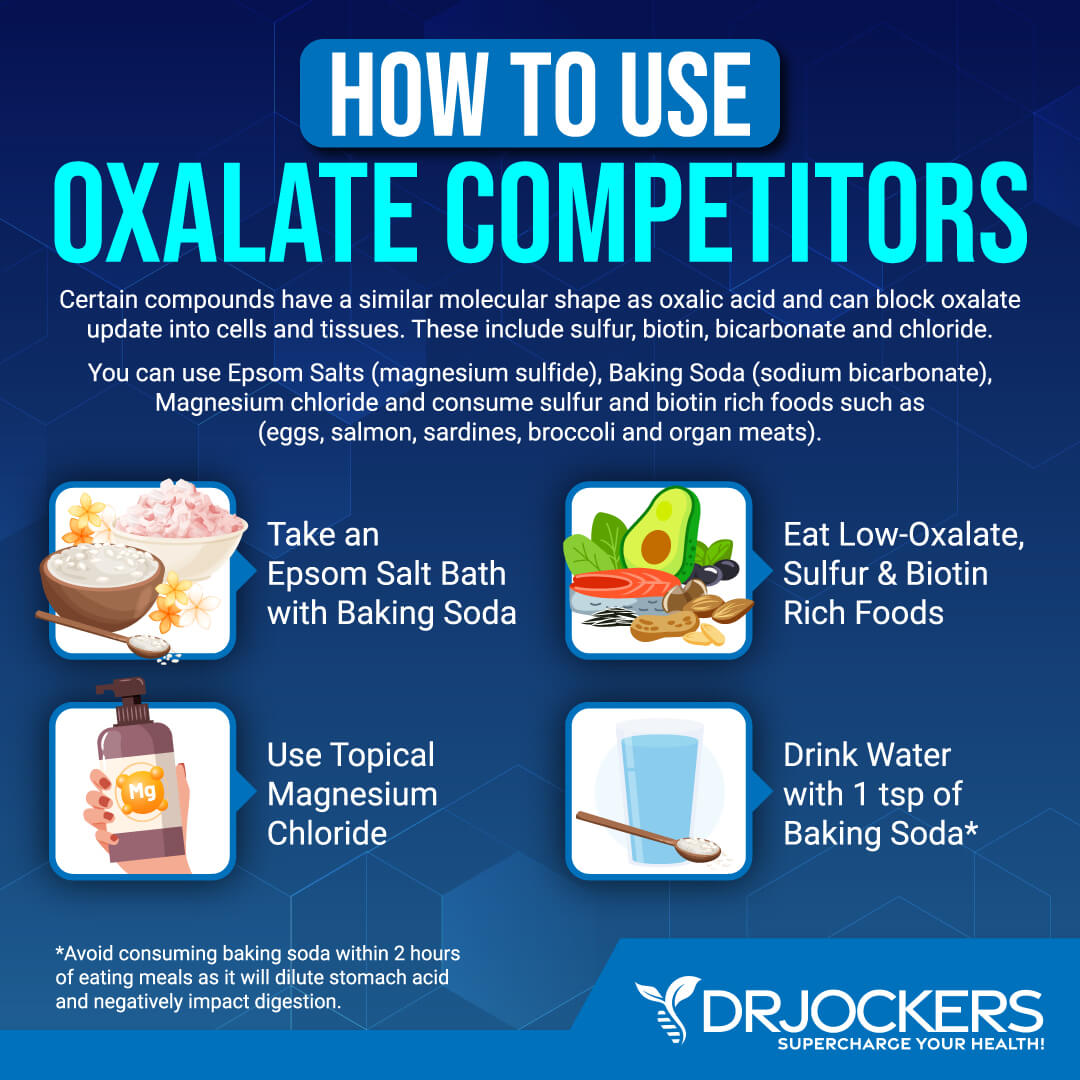
Use Oxalate Competitors
You may also add some oxalate competitor compounds to your diet and lifestyle. These oxalate competitors, including sulfur, biotin, bicarbonate, and chloride, have a similar molecular shape to oxalic acid.
Thus, they may take over and use the pathways normally oxalic acid would move into your cell. This can crowd out oxalates and reduce its impact on cellular levels. Taking a bath with Epsom salt, magnesium chloride, or soda bicarbonate may be the easiest way to use oxalate competitors. Taking biotin or eating biotin-rich foods may also help.
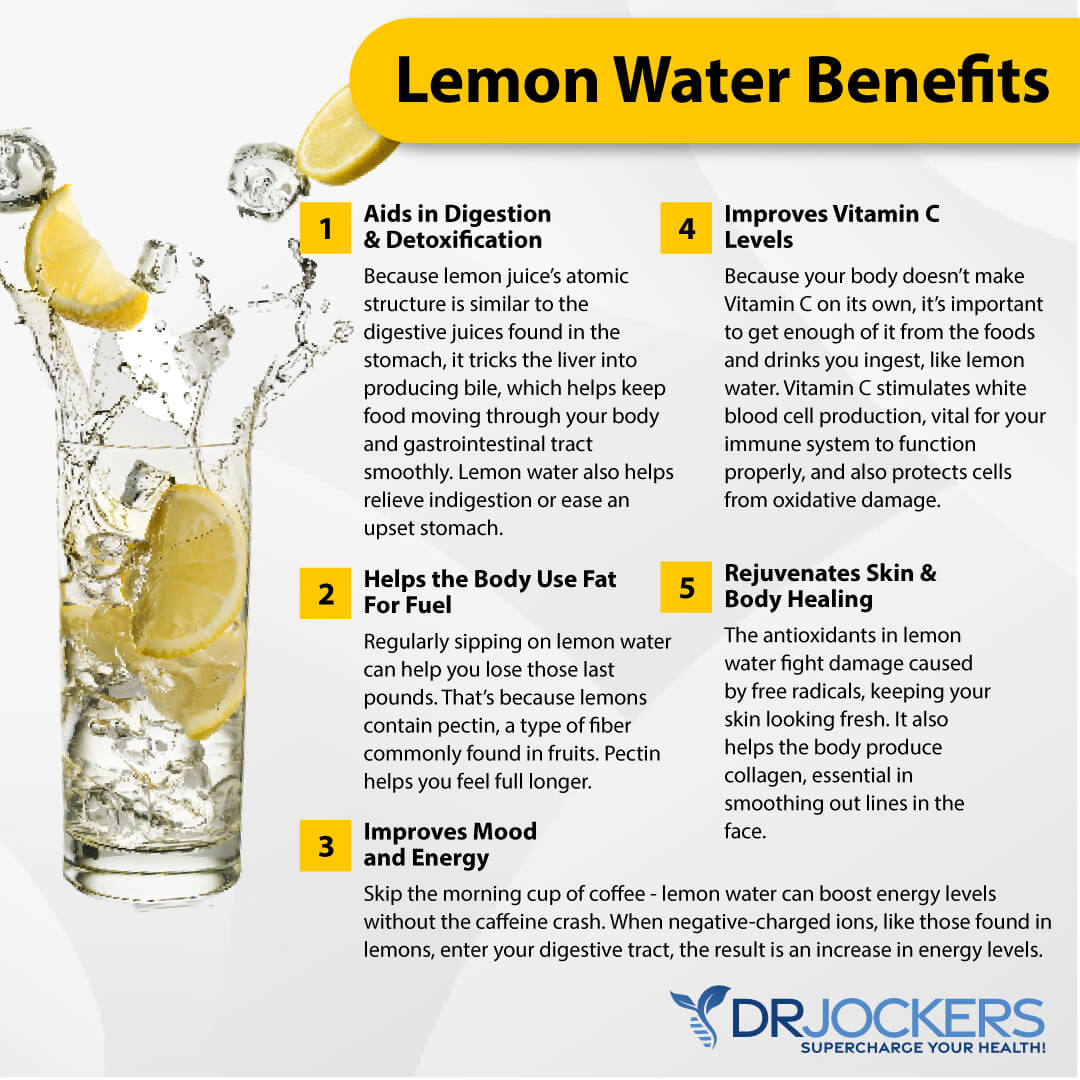
Use Lemon Juice
Fresh lemon juice is not only great for your immune health but may help to reduce your oxalate levels as well. A 2021 study published in E Clinical Medicine has found that using fresh lemon juice of 60 ml twice a day may help with recurrent stones in patients with calcium oxalate nephrolithiasis (17). They followed patients for two years.
Within those two years, 21 of 100 patients using lemon juice and 32 of 103 controls not drinking lemon juice had a stone recurrence. However, many patients reduced their intake of lemon juice over the course of the study. Patients drinking lemon juice had significantly better results.
Researchers found that lemon juice may be a safe way to reduce kidney stones. If you have poor oxalate metabolism-related issues or high oxalate levels, I recommend drinking lemon juice daily. You can mix it with your water in the morning and mid-day.
Optimize Vitamin B6 Levels
Vitamin B6 deficiency may increase your risk of high oxalate levels (1, 8, 9, 10). Optimizing your vitamin B6 levels may help.
Low oxalate foods rich in vitamin B6 include beef liver, chicken liver, beef, salmon, tuna, and eggs. I also recommend supplementing with methylated vitamin B6 or a vitamin B complex. I recommend B Strong as a B complex.
Take a Good Quality Probiotic
Gut dysbiosis may be among the underlying driving forces of high oxalate levels (4, 5, 6). Taking care of your gut flora with a healthy diet is important but not enough.
Using a good quality probiotic supplement may help. I recommend using Ultimate Probiotic. Take 2 capsules daily, 20 minutes before your first meal, with water or as recommended by your healthcare provider.
 Take Citrate Salts
Take Citrate Salts
You may also benefit from taking calcium citrate or magnesium or potassium citrate. According to a 1997 clinical trial published in the Journal of Urology, potassium-magnesium citrate helped to reduce recurrent calcium oxalate stones and using it for up to 3 years may decrease the risk of recurrence by 85 percent (18).
A 2014 study published in the Korean Journal of Urology has found that using magnesium citrate along with vitamin B6 may decrease recurrent calcium oxalate and phosphate stones (19).
Moreover, bedrest and microgravity may increase the risk of kidney stones. A 2007 study published in the Journal of Urology has found that potassium-magnesium citrate has helped to reduce the risk of kidney stones during 5 weeks of bed rest (20). They used 42 mEq potassium, 21 mEq magnesium, and 63 mEq citrate a day in 20 subjects.
I recommend using Mg-K Citrate. Mg-K Citrate™ provides two intracellular cations that are vital to maintaining healthy muscle contractility, nerve conduction, and blood pressure levels already within the normal range. These minerals help maintain healthy electrolyte and acid-base balance and support kidney health and function.
Take one capsule one to two times daily with meals or as directed by your healthcare practitioner. Consult your healthcare practitioner prior to use.
Take Activated Charcoal or a GI Binder
Finally, since gut microbiome imbalance, candida and fungal overgrowth, dietary excess oxalate, and other issues can contribute to high oxalate levels, you may benefit from taking activated charcoal or a GI binder to support detoxification and gut health. I recommend GI Detox+.
G.I. Detox+ is formulated to provide broader activity than a single-ingredient product. Zeolite clay, activated charcoal, and MMST silica, plus apple pectin, humic and fulvic acids, and aloe vera. Binding and detoxification agents have long been used in traditional medicine and supported by modern research.
This product includes zeolite clay, activated charcoal, aloe vera (organic) gel, apple pectin, silica, and humic powder. It is a great agent for detoxification, cleansing, gut health, bloating, gas, mental clarity, and comfortable cleansing. Use 1 capsule on an empty stomach with a full glass of water or as directed by a healthcare professional. Take 1 hour apart from other medications and supplements.
Final Thoughts
Oxalates are naturally occurring compounds found in plants, animals, and humans. Some of our healthiest foods, including many greens, vegetables, and fruits, are high in oxalates. Though for most people, oxalates don’t cause issues, for some, they can lead to chronic symptoms and health complications.
If you are experiencing symptoms related to poor oxalate metabolism and high oxalate levels, I recommend following the tips in this article on a low oxalate diet and reducing high oxalate levels to improve your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!






Dr J …,is there a specific stool test that tests for all those important oxalate processing strains ? Then why not probiotic enemas along with oral dosing of them to try to replace/re-seed them ?
Thanks
I wish I had this information a few years ago when I went crazy-KETO and majored on all the healthy foods you recommended that turned out to be oxalate-dense. You can add plantar fasciitis to the list of oxalate ailments, as that is where all that inflammation settled in my body. After a year of reducing oxalates and supplementing with the good things you talk about in this article, I am finally able to walk most days without pain in my feet. Staying healthy at 70 is such a balancing act! Thank you for the info you provide & for acknowledging that our healing ultimately comes from the Giver of Life, Almighty God.
Your articles are always fantastic and they remind me of the adage that a doctor is a teacher.
Other doctors that push antibiotics(A) as candy create untold problems that the general public is unaware of, such as the destruction of Oxalobacter formigenes(OF). It is said that just two courses of A will eliminate these friendly bacteria; thus subjecting many of their patients to the issues you have presented. Without the benefit of OF, I support my weaker secondary system of dealing with oxalates by consuming magnesium citrate with meals and then I can consume all those nutritious foods that are high in oxalates.
A question: In my case it is not just “excess vitamin C”, but all ascorbic acid turns to oxalates (OAT). I am seriously deficient in vitamin C (OAT) and utilize about a dozen different ways to obtain the vitamin without much success. Am I just producing a lot of oxalates? Are there any possible ways around this? Thanks for any suggestions.
I didn’t follow up on this link, but nevertheless I thought it might be interesting; https://pubmed.ncbi.nlm.nih.gov/19507407/
Hi RichV, thanks for posting that link. They state that hyperoxaluria is a prominent risk factor for kidney stones; whlle that is true for the general populace, there are those of us that do not maintain the acidic condition required for stone formation. Without that ubiquitous acidic state, our bodies are not receptive to viruses and hyperoxaluria is not a prominent risk factor for kidney stones.
Nevertheless, hyperoxaluria is not a healthy state for anyone and should be mitagated in some way.
You list broccoli and cauliflower as low oxalate foods but then say to cook cruciferous vegetables to lower the oxalates. But cruciferous foods are the brassica family: kale, broccoli, cauliflower, cabbage. So that’s confusing. Also, FYI, I never heard of oxalates until I was 70. That was just last year, when I read the clue to a problem that developed in 2022, of needing to get up to the bathroom 90 minutes after falling asleep, regardless of what I had to drink. I figured out last year this problem corresponded to high oxalate levels, verified by a lab test. The problem began in a certain week of 2022, which I later learned my husband had his second cvd shot.
Thanks Doc. I was drawn to read your article because of how you are extremly detailed in your articles and videos. I have finally found out how to fix my CAC. I had tests done +20 years ago and no one could tell me how to correct it.
This article comes at a perfect time for me. L4L5 spondy. Im super active but this pain is unbearable. I consider myself a high pain tolerate person until this experience. Greatful for your time here, Sir.