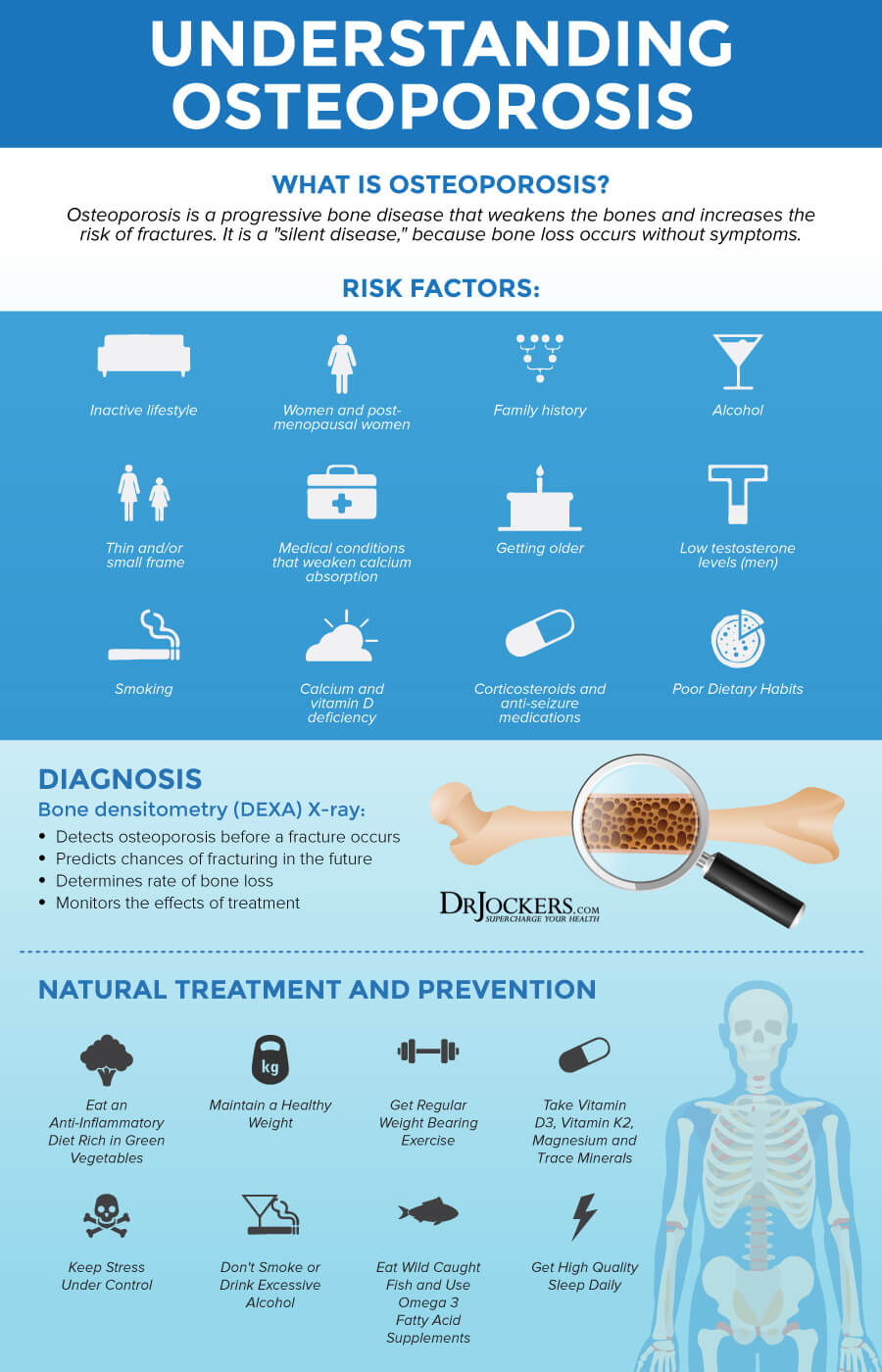
Osteoporosis: Symptoms, Causes and Natural Support Strategies
Our bones are living tissue made up of cells, blood vessels, proteins, vitamins, and minerals. Bones have many functions including providing structural support for the body and protection of vital organs. Bones also provide an environment for marrow and act as a storage area for minerals (1). Osteoporosis is a degenerative disease of the bones that interferes with the many vital functions they serve.
Our bodies are constantly in the process of bone-building and bone-breakdown. When this process is imbalanced, bones become weak. Depending on the amount of bone loss, a person can develop osteopenia or if more severe, osteoporosis. Around 10 million Americans have osteoporosis and about 44 million at least have low bone density.
This article will discuss the facts about osteopenia and osteoporosis, including characteristics, causes, complications, and the problems with conventional treatment options. I will then review my top natural support strategies to improve bone health.
Bone Regeneration
Bones grow continually from birth to the end of the teenage years, reaching a maximum strength (peak bone mass) and size in early adulthood. Once peak bone mass is reached, it is maintained by a process called remodeling. This is a continuous process in which old bone is removed (resorption) and new bone is created (formation).
The bone remodeling process revolves around two major cells, osteoblasts and osteoclasts. Osteoblasts build bone and act to increase bone mineralization. Osteoclasts work to break down bone tissue. These cells act in synergy to balance the bone building equation and effectively remodel healthier and stronger bone tissue. As we age, the rate of bone resorption is greater than the rate of bone formation and this results in thinning of the bones.

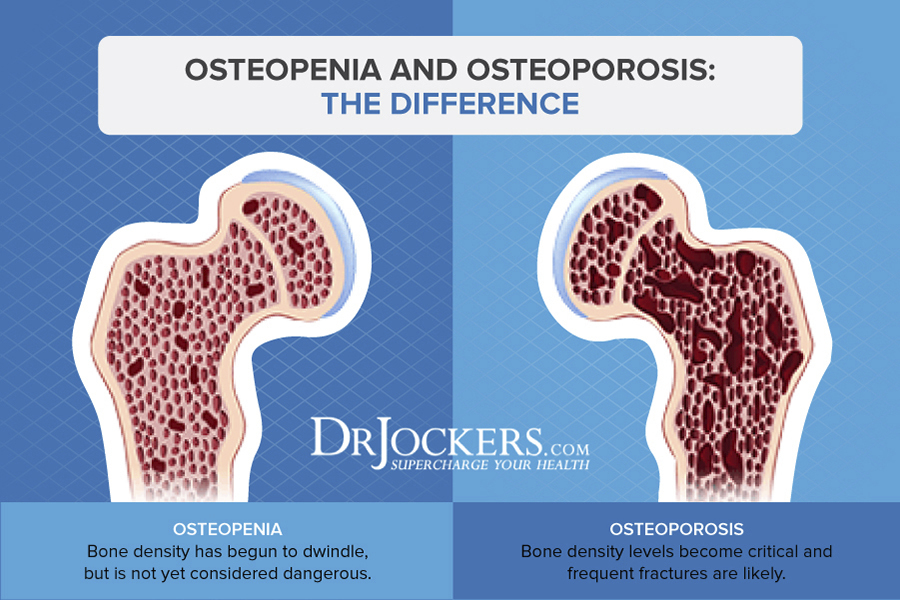
Characteristics of Osteopenia and Osteoporosis
Osteopenia and osteoporosis are conditions characterized by low bone density. Bone mineral density is the mineral concentration in the bones. Osteopenia and osteoporosis occur when bones become weak and lose minerals.
Osteoporosis means “porous bones”. It is a bone disease that occurs when the body loses too much bone, makes too little bone, or both (2). Osteoporotic bones have large holes and spaces and contain abnormal tissue structure. When bone density is not low enough to be classified as osteoporosis, but not high enough to be normal, it is classified as osteopenia.
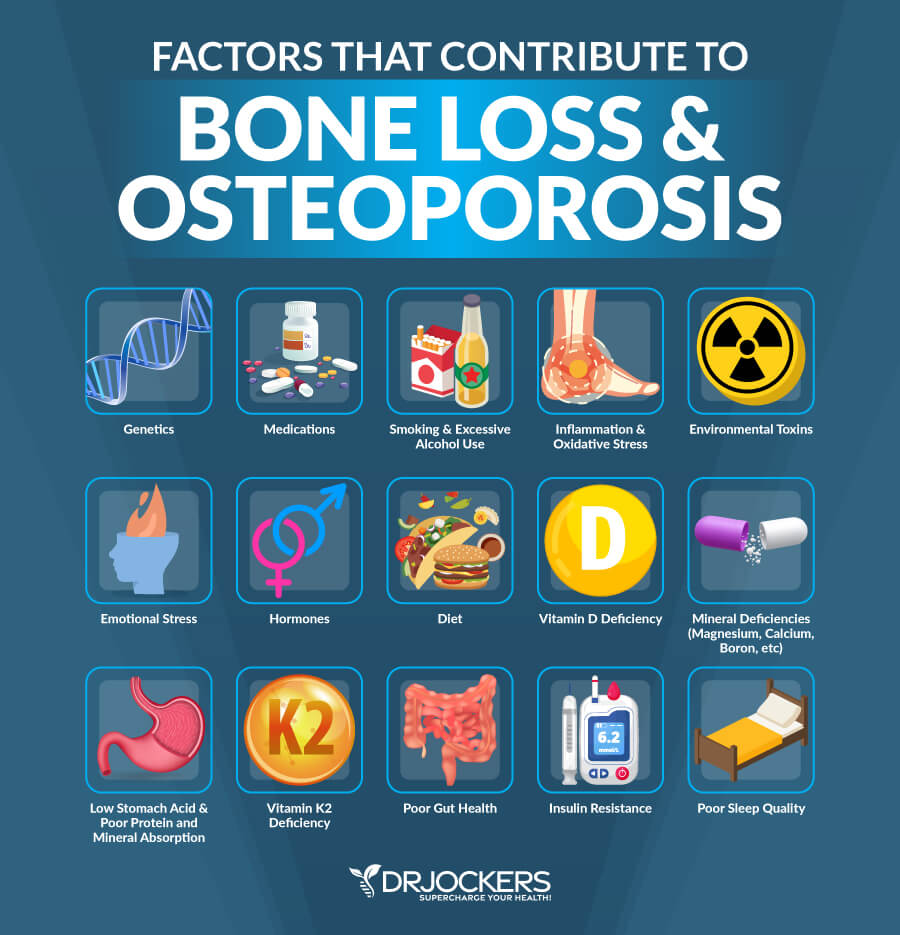
Causes and Risk Factors of Osteoporosis
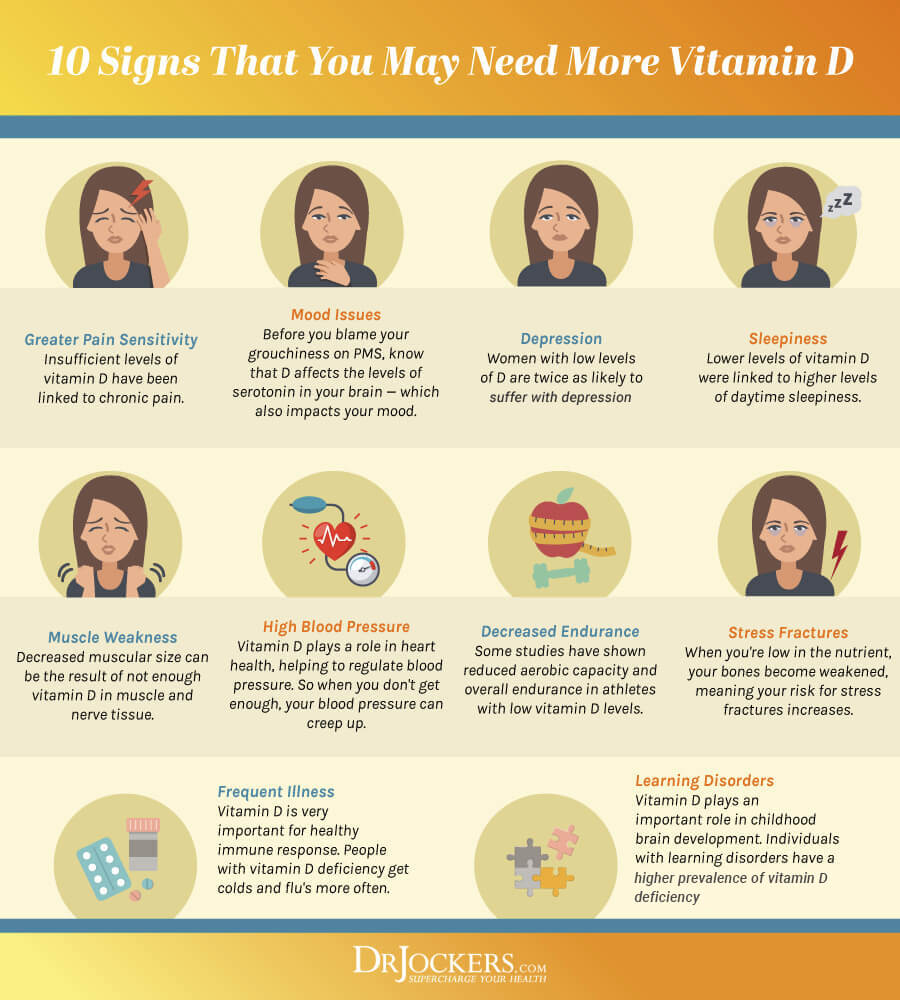
There are many factors which can cause a higher rate of bone remodeling and lead to a more rapid loss of bone mass and more fragile bones. The main causes of osteopenia and osteoporosis are inactivity, aging, hormonal imbalances, long-term use of certain medications, steroid use, low vitamin D levels, emotional stress, and nutritional deficiencies.
Certain health conditions increase the likelihood of bone loss, including autoimmune disorders (rheumatoid arthritis, lupus, multiple sclerosis, and ankylosing spondylitis). Digestive and gastrointestinal disorders such as celiac disease, inflammatory bowel disease, and weight loss surgery, may also lead to osteoporosis. Other conditions associated with osteoporosis are cancer, blood disorders, neurological disorders, bone marrow and blood disorders, endocrine and hormonal disorders, and certain other diseases and conditions. Depression and eating disorders also increase the likelihood of osteopenia or osteoporosis.
Osteopenia and osteoporosis are more common in women who naturally have lower bone density, but men may also develop the condition. Men and women over the age of 60 are at higher risk than younger people.
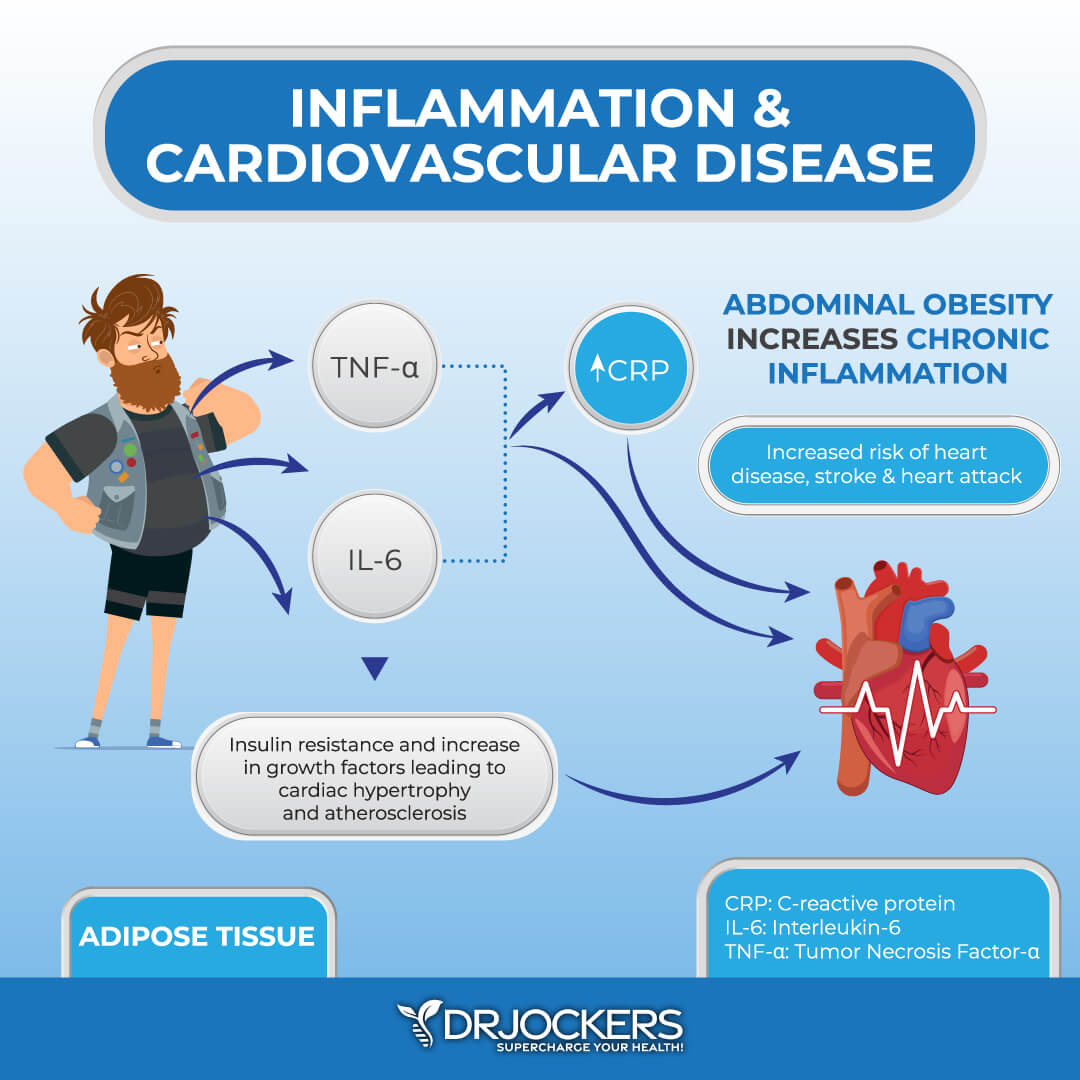
Women are more likely to have osteopenia or osteoporosis because reproductive hormones, especially estrogen, can affect bone mass. Estrogen helps activate vitamin D3’s calcium absorbing properties. When levels of estrogen drop (usually after menopause), this increases osteoclastic activity (3). Low estrogen also increases IL-6, an immune factor that triggers inflammatory damage to bone tissue (4). This combination can dramatically and negatively affect bone tissue health.
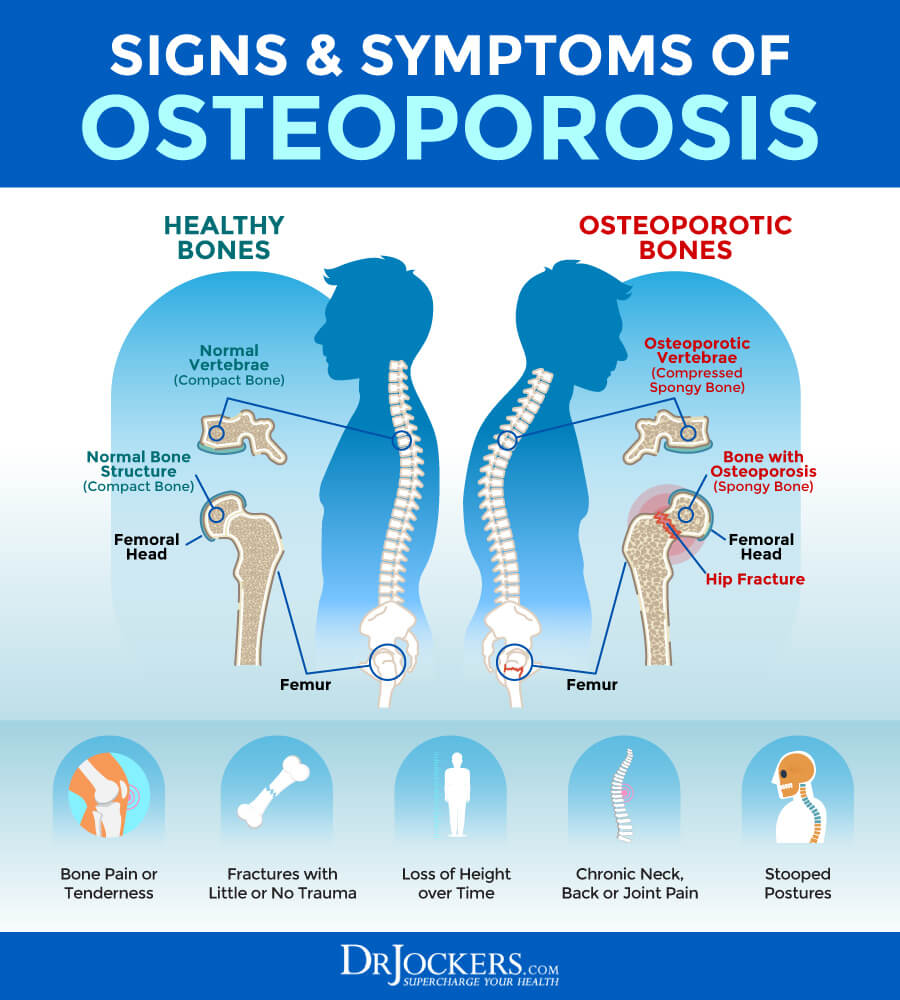
Signs and Symptoms of Osteoporosis
Osteoporosis is often referred to as “the silent disease” because most people are not aware they have osteopenia or osteoporosis until they break a bone. Bone loss is gradual and painless, and there are usually no symptoms to indicate a person is developing osteoporosis.
A person with osteoporosis may notice they are getting shorter or their spine curving. Elevated parathyroid hormone (PTH) is a major factor in these conditions. This hormone is raised by deficiencies of vitamin D or calcium or by excess phosphorus.
Hip fractures may be the most serious complication of osteoporosis. One in two women and one in four men over age 50 will break a bone due to osteoporosis (5). Twenty-four percent of hip fracture patients over 50 die in the year following the fracture. One quarter of hip fracture patients end up in nursing homes and half never regain previous function.
Diagnosis and Conventional Treatments
Diagnosis of osteopenia or osteoporosis is done by measuring bone mineral density. Traditional X-rays cannot measure bone density. The most commonly used test for measuring bone mineral density is DXA (dual-energy X-ray absorptiometry). It is used to measure spine and hip bone density to assess the risk of osteoporosis.
To diagnose osteoporosis or osteopenia, a person’s bone mineral density deviation from healthy young adults (T-score) is calculated. A person is diagnosed with osteopenia if their T-score is lower than -1 and greater than -2.5 and osteoporosis if the T-score is -2.5 or lower.
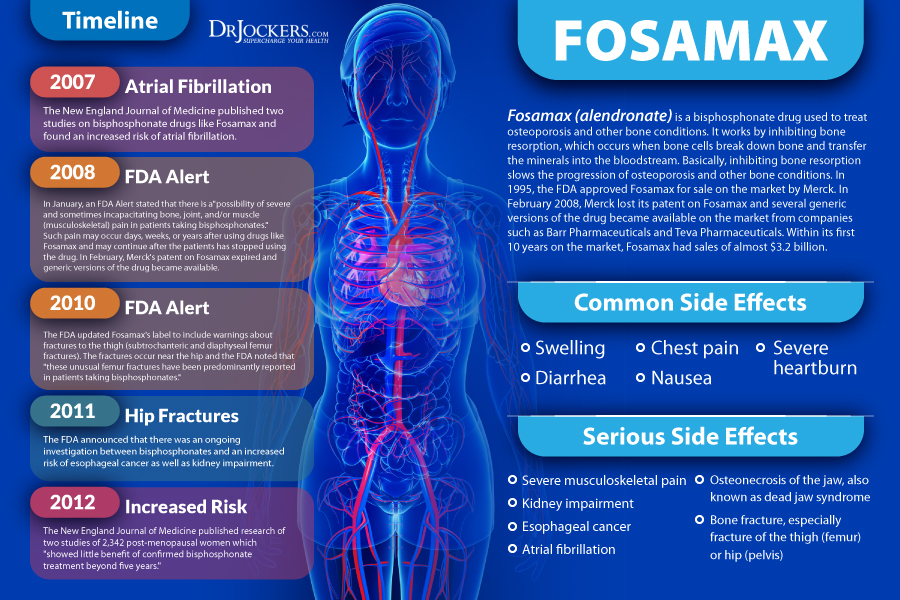
Classic mediations to treat osteoporosis are called bisphosphonates. Fosamax (alendronate sodium) and related drugs are commonly prescribed by doctors. These drugs are designed to destroy osteoclasts and slow down the body’s process of breaking down bone.
While these drugs may improve bone density, research shows that they decrease the necessary collagenous flexibility necessary for adequate bone strength (6). Very dense bone created by destroying osteoclasts (bone-degrading cells) may be far more brittle than less dense bone where there is healthy turnover of the osteoclasts and osteoblasts (bone-building cells). This reduced osteoclastic activity creates rigid bones that are prone to fracture.
These drugs also have dangerous side effects. The most common side effects are gastrointestinal issues and esophageal irritation. Other serious side effects include kidney impairment, atrial fibrillation, bone fracture, osteonecrosis of the jaw, and esophageal cancer.
10 Natural Strategies to Prevent and Treat Osteoporosis
There are many safe and effective natural strategies to reduce the risk of fracture, support healthy bone mineral density, bone strength and structural integrity.
These strategies include nutrition, exercise, stress reduction, and key supplements. These strategies I discuss are not at this time FDA approved to prevent, mitigate, treat or cure osteoporosis and shouldn’t be confused as such. However, they are important for the health of your bones and overall body.

Anti-Inflammatory Healing Diet
One of the best strategies for preventing and treating osteopenia and osteoporosis is to consume an anti-inflammatory, healing diet. You should include foods that naturally boost bone density.
A healing diet removes foods that cause inflammation and includes organic, non-GMO vegetables, fruits, healthy fats and clean protein. A healing diet reduces inflammation, stabilizes blood sugar, reduces toxic load, provides necessary nutrients, and supports healthy blood pH levels.
 Food to Avoid
Food to Avoid
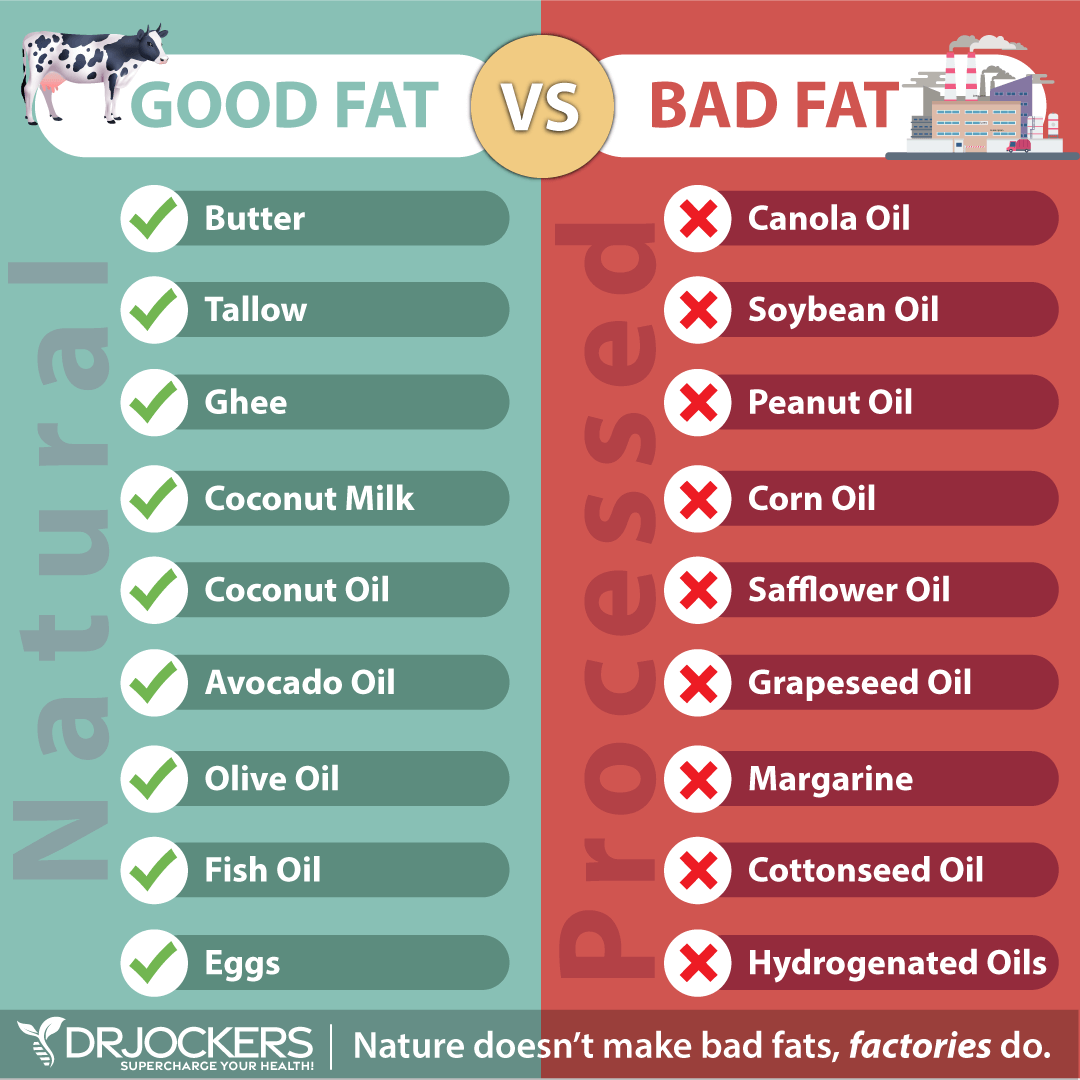
Osteoporosis is associated with inflammation in the bones, so it is critical to avoid highly inflammatory foods. Highly inflammatory foods are refined sugars and grains, and any foods that are easily metabolized into sugar (high glycemic foods). These foods upregulate inflammation and create extra acidity in the tissues.
It is important to avoid sodas. In addition to sugar, most sodas have a high phosphoric acid content which can remove calcium from the bones. Drinks and foods with high levels of caffeine can also interfere with calcium absorption.
Meat and dairy from conventionally raised animals, farmed fish, processed foods and highly processed vegetable oils, such as canola, peanut, cottonseed, soy and safflower, promote inflammation and should be eliminated. Processed foods and meats contain a high amount of sugar and chemicals that may result in bone loss.

Foods to Include
The foods you should be eating on an anti-inflammatory, healing diet are whole, unprocessed foods. Choose grass-fed, pasture-raised, wild-caught meats and fish. Enjoy a variety of lower carbohydrate, low glycemic, colorful vegetable and fruits for their abundant antioxidants and phytonutrients. Plentiful amounts of herbs are also wonderful to use on a healing diet.
There are many low to medium glycemic vegetables including cruciferous vegetables, leeks, shallots, cucumbers, asparagus, and leafy greens. Low glycemic fruits include berries, lemons and limes, grapefruit, and granny smith apples.
Healthy fats are a very important part of a healing diet. Healthy fats are found in coconut, olives, avocados, and their oils and in grass-fed butter and ghee. Omega-3 fatty acids and conjugated linoleic acid (CLA) found in wild caught salmon and grass-fed beef and dairy are fats with many bone health benefits. These healthy fats are an efficient source of fuel for the body to combat inflammation and maintain bone strength.
Foods to Boost Bone Density
Along with a healing diet, it is important to include foods that can boost bone density. Raw cultured dairy such as kefir, yogurt, and raw cheese contain calcium, magnesium, vitamins D and K, and phosphorus, all of which help build strong bones.
Sea vegetables and green leafy vegetables also contain vitamins and minerals that are critical for bone formation and bone strength. Foods rich in omega-3 fats such as wild-caught salmon and sardines, walnuts, and certain seeds help reduce inflammation. Additionally, osteoporosis may be related to an acidic body environment so including alkaline foods like fruits and vegetables can promote a more alkaline environment.

Improve Mineral Absorption
A sufficient intake of minerals is essential for many bodily functions and systems, including healthy bones. Bones are made up of calcium, phosphorus, sodium and other minerals.
Absorption of minerals is critical to maintaining bone strength. Many people do not produce enough stomach acid to properly absorb minerals and other nutrients. A digestive enzyme with stomach acid support can be helpful.
You will also want to consume trace mineral rich foods that you can read about in the image below. Be sure to take a few deep breaths and reduce stress levels before your meals in order to help activate stomach acid so you can digest and absorb the minerals effectively.

Weight Bearing Exercise
Exercise is critical for both maintaining bone health and preventing fractures. Weight bearing exercise has been shown to have positive effects on bone loss by increasing bone formation and decreasing bone reabsorption (7).
Most people think of weight bearing exercise as lifting weights. Actually, weight bearing exercise is any exercise that requires your bones and muscles to support your body weight. Examples are running, walking, dancing, and tennis. It is important to do weight bearing exercises at least 3-4 times per week for 30-60 minutes per time. It is also helpful to weight train three times a week for at least 30 minutes.
Incorporating balance exercises, such as Tai Chi, to your exercise regimen is important for reducing the overall risk of falling and being injured.

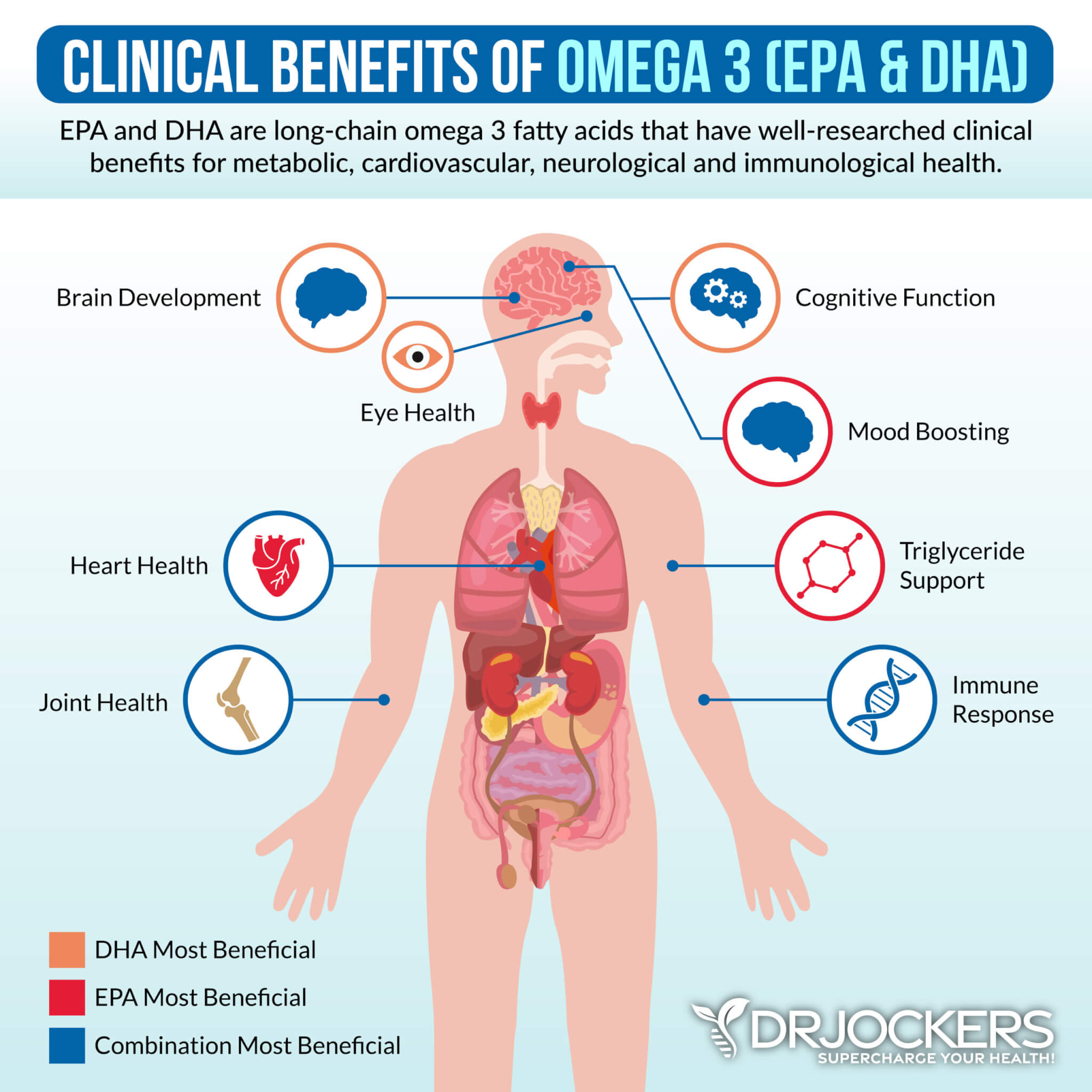
Omega-3 Fatty Acids
Osteoporosis is associated with inflammation in the bones. Omega-3 fatty acids help to support a healthy inflammatory process and provide building blocks for healthy bone tissue and hormones that regulate bone tissue formation.
Omega-3 fatty acids are essential fats that are found in fatty fish such as wild-caught salmon and sardines, grass-fed meats, pasture-raised eggs, nuts (especially walnuts), and seeds (flax, hemp, pumpkin and chia seeds). Omega-3 fatty acids have wide-ranging health benefits.
Plant based omega 3’s such as flax oil only contain the small chain omega 3 called ALA and do not have any DHA. It is very hard for our body to convert ALA into DHA so it is best to get a high-quality fish or krill oil that is rich in EPA and DHA. You want to find a brand that is molecularly distilled to take out any heavy metals and other unwanted contaminants.
Be sure to discuss with your physician before using as fish oils have a blood thinning affect and can be contraindicated if you are on blood thinning medications.
Calcium
Calcium is a major building block of bone tissue. In fact, 99% of our body’s calcium stores are housed in our bones. Consuming optimal amounts of calcium from food or supplementation is critical to prevent and treat osteoporosis.
Calcium is best obtained from foods in your diet. Dairy products (preferably raw, grass-fed, organic dairy products) are the most readily available sources of calcium. Dairy products also contain protein and other micronutrients important for bone health. Other calcium rich foods include fish with soft, edible bones (such as sardines), green vegetables (broccoli, curly kale and bok choy), and nuts (Brazil nuts and almonds).
If you are unable to get enough in your diet, supplementing with calcium citrate can be effective. Excess phosphorus inhibits calcium absorption and may aggravate a dietary deficiency. Excessive caffeine and salt can also increase calcium loss from the body.
It is also important to note that calcium deposition in the body works in tandem with Vitamin D, Vitamin K, and magnesium. In fact, most people actually don’t need much calcium and should focus on getting plenty of these other nutrients.

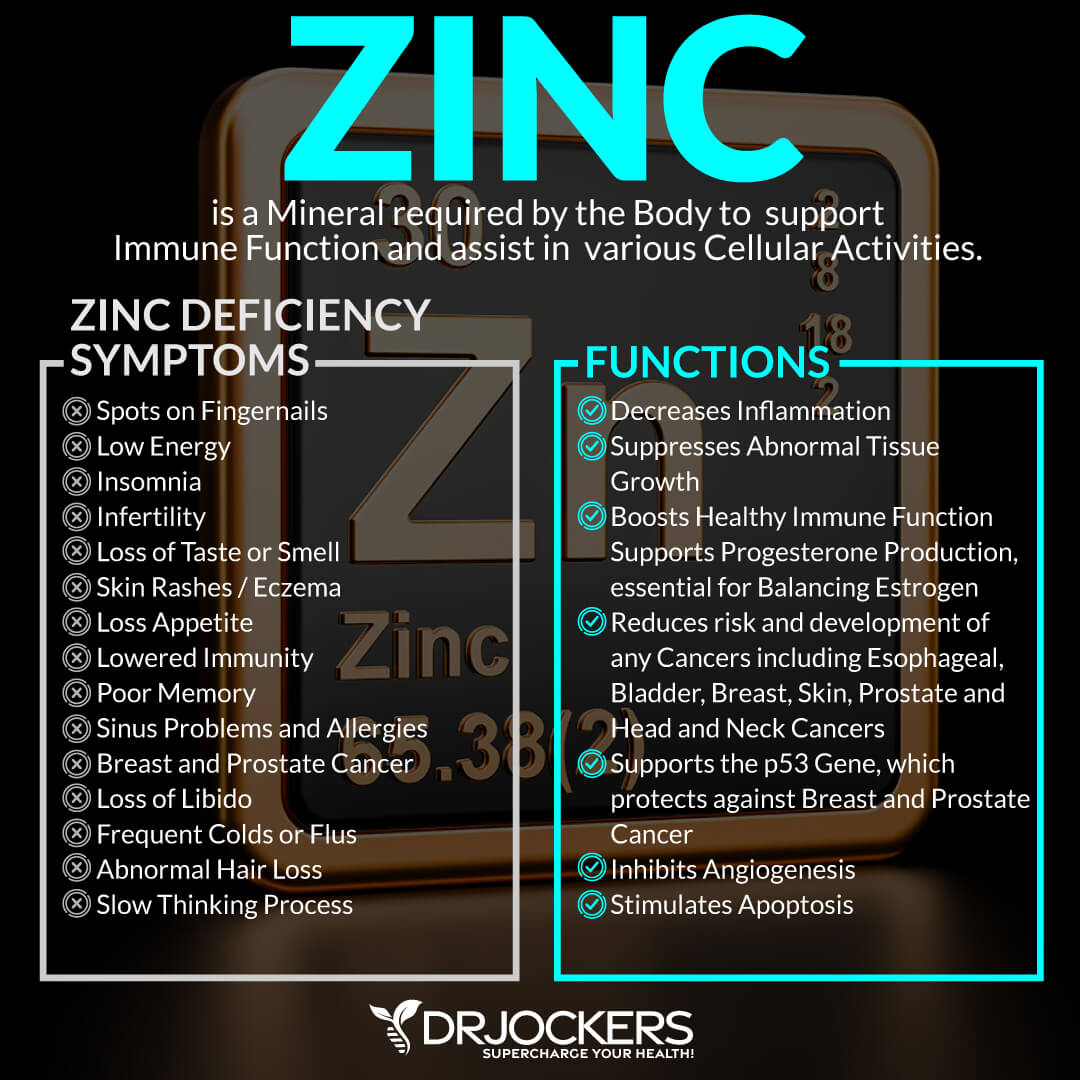
Zinc and Magnesium
Including optimal amounts of zinc and magnesium in your diet is important for improving your overall health. Both zinc and magnesium are important for bone health and for supporting the immune system.
Zinc is a mineral required for bone tissue renewal and mineralization. Foods high in zinc include pasture-raised chicken and eggs, grass-fed beef and dairy, spinach, and wild-caught salmon. Nuts and seeds such as cashews, almonds, pumpkin seeds, and watermelon seeds are also high in zinc. It is best to soak or sprout nuts and seeds to reduce the level of phytic acids.
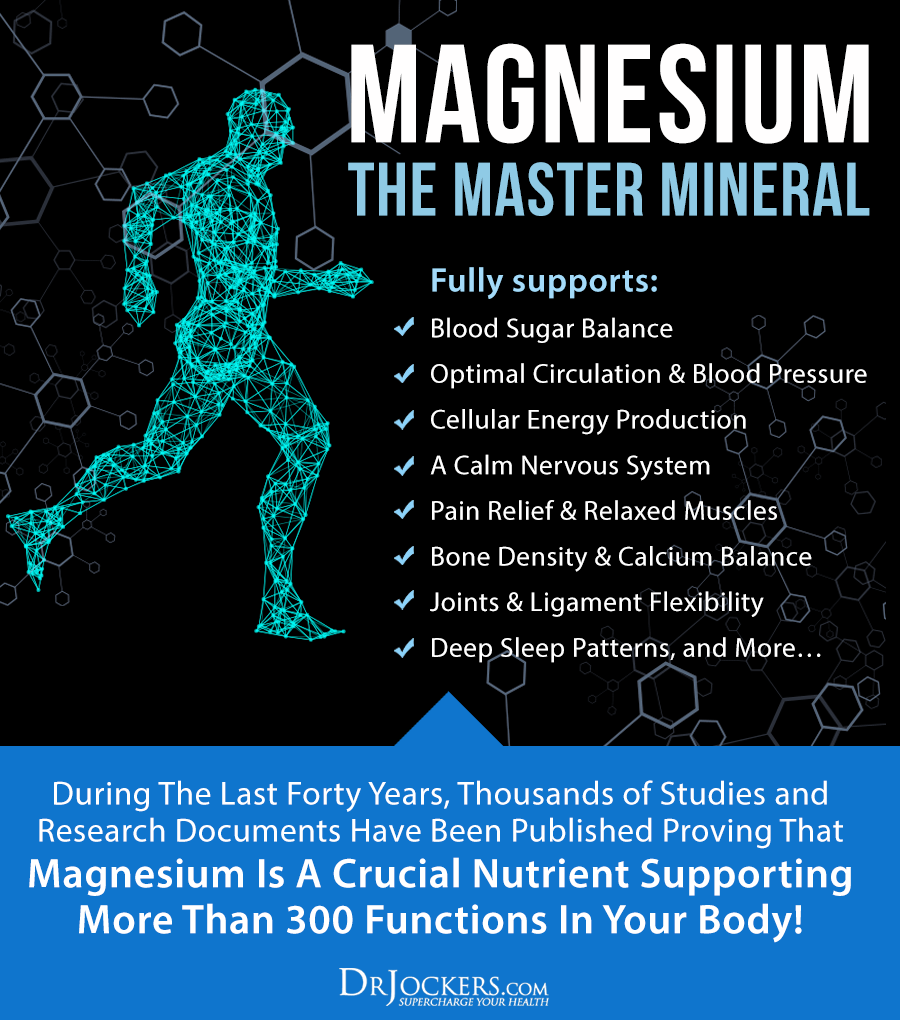
Magnesium is a crucial nutrient that supports over 300 physiological processes or functions in the body. It is referred to as the “master mineral” and plays an important role in forming bone. Magnesium is critical to all aspects of vitamin D and calcium metabolism.
The top food sources of magnesium are leafy greens such as Swiss chard and spinach, sea vegetables, sprouts, and avocados. Grass-fed dairy and wild-caught fish are rich in magnesium. Pumpkin seeds, nuts, dark chocolate, and coffee are also good sources of magnesium.
Vitamins D and K2
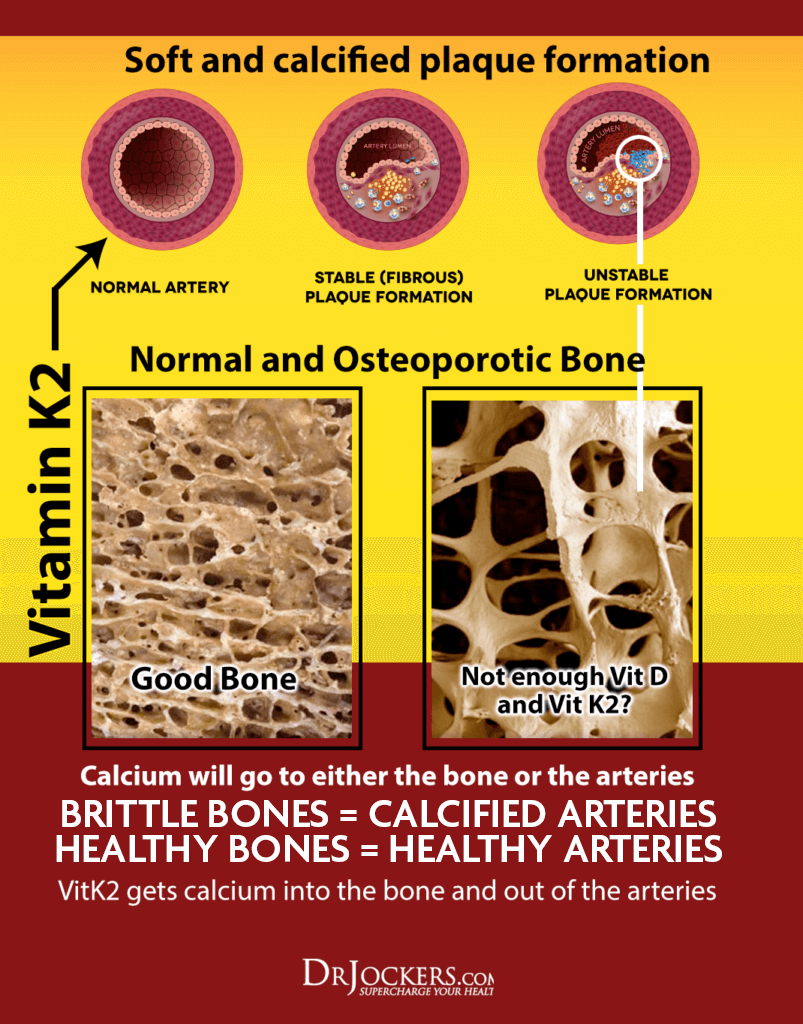
Vitamin D3 and vitamin K2 work synergistically to promote bone health and reduce the incidences of fractures (8). These nutrients work together to help guide calcium into the bone tissue and prevent it from accumulating in places such as the arteries.
Vitamin D3 is important for calcium absorption. D3 is the biologically active form of vitamin D. It is more potent in raising and maintaining vitamin D concentrations than D2.
Vitamin D3 is created in your skin in response to sun exposure. Aim to get 15-20 minutes of sun exposure daily.
There are numerous animal-based food sources of vitamin D3. Whole food sources of vitamin D are much healthier options than foods fortified with vitamin D. The best dietary sources of vitamin D are wild-caught salmon and fatty fish, cod liver oil, grass-fed butter and raw cheese, egg yolks, mushrooms, and beef liver.
Vitamin K2 is an important nutrient that plays a role in many bone metabolism. Getting enough vitamin K in your diet is key to maintaining healthy bones and protecting against fractures (9).
Vitamin K2 is needed to form a bone-building protein called osteocalcin (10). Osteocalcin is a necessary protein for maintaining calcium homeostasis in bone tissue. It works with osteoblast cells to build healthy bone tissue. When we are deficient in vitamin K2, osteocalcin production is inhibited which reduces calcium flow into bone tissue. This can lead to osteopenia and osteoporosis.
Foods rich in vitamin K2 are meat, dairy, fermented foods, and natto. Vitamin K2 is also produced by the beneficial bacterial in your gut.
The combination of vitamins D3 and K2 enhances osteocalcin accumulation in bone cells greater than either nutrient alone. Increased osteocalcin formation significantly improves bone mineral density. D3 and K2 also work together to increase Matrix GLA protein (MGP), which protects blood vessels from calcification.
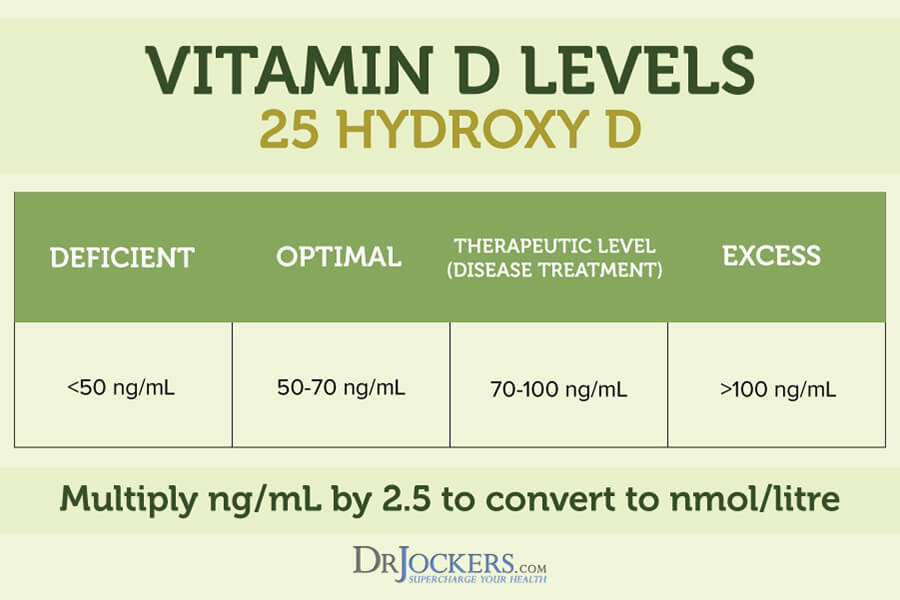
The adequate range for vitamin D3 levels is between 50-80 ng/ml and optimal may even bu up closer to about 100 ng/ml. It is important to keep vitamins D3 and K2 in balance. A great way to ensure balance is by taking a Vitamin D2/K2 supplement. To obtain these amounts through supplementation, I use the following formula:
- To boost D3/K2 levels: 2,000 IU of vitamin D3 (400 mcg of vitamin K2) for every 25 pounds of body weight. This typically will add 15-20 IU to your blood D3 levels each month. If your levels are 20, supplementing vitamin D using this formula for three months should get the level up to 80. I always recommend that you test your D3 levels to be sure.
- For maintenance: 1,000 IU of vitamin D3 (200 mcg of vitamin K2) for every 25 pounds of body weight Again, be sure to test to make sure!
This supplement is not at this time FDA approved to prevent, mitigate, treat or cure osteoporosis and it shouldn’t be confused as such.
Maintain a Healthy Weight
Being overweight or obese can contribute to a number of health issues. Obesity causes hormonal imbalances which contribute to bone loss. Being an unhealthy weight also makes it more difficult to exercise and be active.
Many people are unable to maintain a healthy weight despite exercise and dieting. This is due to insulin resistance. Weight gain, particularly abdominal fat, is a classic sign of insulin resistance and chronic inflammation. Following the healing diet outlined above is a powerful way to reduce inflammation and balance hormones.
Other steps to maintain a healthy weight include healing gut dysbiosis and balancing the gut microbiome. Optimal vitamin D3 levels are also critical for maintaining a healthy weight. Low levels of vitamin D3 are associated with cellular inflammation and weight loss resistance (11).
High intensity exercise and restful sleep are also important for maintaining a healthy weight. High intensity exercises should be done in sequence, for short time periods with little rest between sets, and incorporating full body movements such as squats and push-ups. High intensity exercise increases fat-burning, anti-aging hormones for the next 36 hours.
Along with the high intensity exercise, it is critical to optimize your sleep. You should sleep 7-8 hours a night with as much sleep before midnight as possible. Rest is anti-inflammatory, regulates gut health, and balances hormones, all of which can help maintain a healthy weight.
Stress Reduction
There is a relationship between stress and osteoporosis (12). Increased stress hormones wreak havoc on the body including the bones. Stress induces physiological changes leading to osteoporosis. Stress also induces behaviors that may lead to osteoporosis such as distorted eating patterns, drinking alcohol, lack of exercise, and poor sleep habits.
Additionally, osteoporosis can lead to stress due to the anxiety, depression, and social isolation that can accompany osteoporosis. It is critical to take steps to reduce stress and lower elevated cortisol levels daily.
Following the healing diet and balancing your blood sugar levels are two effective strategies for reducing stress on the body. Other powerful techniques are grounding, deep breathing exercises, sunlight exposure, Epsom salt baths, and dry brushing. Practice these stress reduction strategies daily to reduce stress and protect your bones from the detrimental effects of stress.

Melatonin
Melatonin is a hormone produced by the body that regulates circadian rhythm. As we age, our melatonin levels decrease which may lead to imbalanced bone remodeling.
Recent studies have shown that melatonin may have a positive effect on the skeleton. Melatonin was shown to increase bone mineral density after one year of treatment in a study of postmenopausal women with osteopenia (13).
Melatonin can be taken as a supplement; however it is possible to promote your body won ability to make it as necessary. The best way to support your own production is to try and control your light exposure to match sunrise and sunset.
If possible, wake up in the morning and watch the sunrise to help set your circadian rhythm for the day, this only takes 5-15 minutes. Next, it is critical to control exposure to blue-lit devices (phones, TV, computers, etc.) immediately upon waking or 2-4 hours before bed as it is overly stimulating to the body.
Conclusion
Osteoporosis and osteopenia are conditions characterized by bone loss or lower bone mineral density resulting in weak and fragile bones. Osteopenia is the precursor to osteoporosis. Common drugs used to treat osteoporosis have dangerous side effects.
Individuals with osteoporosis or osteopenia are usually unaware of their condition until a fracture occurs. Osteoporosis and osteopenia are associated with chronic inflammation, vitamin and mineral deficiencies, aging, inactivity, hormonal imbalances and a number of other conditions.
There are many natural ways to support and improve bone health. One of the most effective remedies is eating an anti-inflammatory healing diet including foods that naturally boost bone density. It is also important to include abundant foods with the key bone-building nutrients, calcium, vitamin D3, vitamin K2, zinc, magnesium, and Omega-3 fatty acids.
Ensuring mineral absorption is key to maintaining healthy bones. Performing weight-bearing exercise, practicing stress reduction techniques, and maintaining a healthy weight are also great strategies to support your overall health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!
Sources for this Article Include:
1. Introduction to Bone Biology: All About our Bones, International Osteoporosis Foundation: Link here
2. What is Osteoporosis and What Causes It? National Osteoporosis Foundation: Link here
3. Kameda T, Mano J, et al., Estrogen Inhibits Bone Resorption by Directly Inducing Apoptosis of the Bone-reabsorbing Osteoclasts, 1997 Aug18; 186(4): 489-495. PMID: 2199029
4. Stein B, Yang MX, Repression of the interleukin-6 promoter by estrogen receptor is mediated by NF-kappa B and C/EBP beta, 1995 Sep; 15(9): 4971-9. PMID: 7651415
5. Osteoporosis Fast Facts, National Osteoporosis Foundation: Link here
6. Meier RP, Perneger TV, et al., Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. 2012 Jun 25; 172(12): 930-6. PMID: 22732749
7. Peppone LJ, Mustian KM, et al., Effects of a structured weight-bearing exercise program on bone metabolism among breast cancer survivors: a feasibility trial. 2010 Jun; 10(3): 224-9. PMID: 20497921
8. Hosol T, Absolute risk for fracture and WHO guideline. Pharmacological intervention to prevent osteoporotic fractures in the elderly. 2007 Jul; 17(7): 1098-104. PMID: 17607078
9. Cheung AM, Tile L, Vitamin K supplementation in postmenopausal women with osteopenia (ECKO trial): a randomized controlled trial. 2008 Oct 14; 5(10: e196. PMID: 18922041
10. Koshihara Y, Hoshi K, Vitamin K2 enhances osteocalcin accumulation in the extracellular matrix of human osteoblasts in vitro. 1997 Mar; 12(3): 431-8. PMID: 9076586
11. Reyman M, Verrjin Struart AA, Vitamin D deficiency in childhood obesity is associated with high levels of circulating inflammatory mediators, and low insulin sensitivity. 2014 Jan: 38(1): 46-52. PMID: 23736361
12. Kumano H, Osteoporosis and stress. 2005 Sep; 15(9): 1544-7. PMID: 16137956
13. Amstrup AK, Sikjaer T, Melatonin improves bone mineral density at the femoral neck in postmenopausal women with osteopenia: a randomized controlled trial. 2015 Sep; 59(2): 221-9. PMID: 26036434




Is your product available in India
Insult to injury…broke my hipbone over the holidays, and the future looks bleak. From adrenal fatigue to this. You say many die a year later. This is not very encouraging. What are they dying from: another fall?
You say that 24% of hip fracture patients over 50 die the yr after fracture…1/4 of patients end up in nursing homes…and half never regain full function. This is all so very negative and am wondering why you included this to scare people:-((
I am 73 and recently had a hip repair with pin implants…scared s…less!!
No, we aren’t trying to scare people. Just writing about the facts of this disorder. We are focused on providing natural strategies in the article!
DEXA bone density is an obsolete paradigm used to sell pills that does not correlate with fracture risk. A much better measure is bone strength. The FRAX score incorporates many variables that, together, much more accurately measure bone strength.
Thanks for sharing!
So many studies now showing that the use of Vitamin D3 supplementation (even at low levels of 400 IU’s) is decreasing bone mineral density and putting people at risk of osteoporosis. It’s unknown whether d3/k2 was used in these studies. Whats your view on this?
More of a response than simply using k2 with d3 would be appreciated. Thanks
Yes any sort of D3 supplementation will help. But taking it with K2 is more helpful. https://pubmed.ncbi.nlm.nih.gov/11180916/
Didnt really answer the question. Plenty of more recent D3 studies showing supplementation may accelerate bone mineral loss. Whats your view on this?
Hi, AJ. Can you provide links to some of these studies, please?