 The Cell Danger Response: New Theory for Chronic Illnesses
The Cell Danger Response: New Theory for Chronic Illnesses
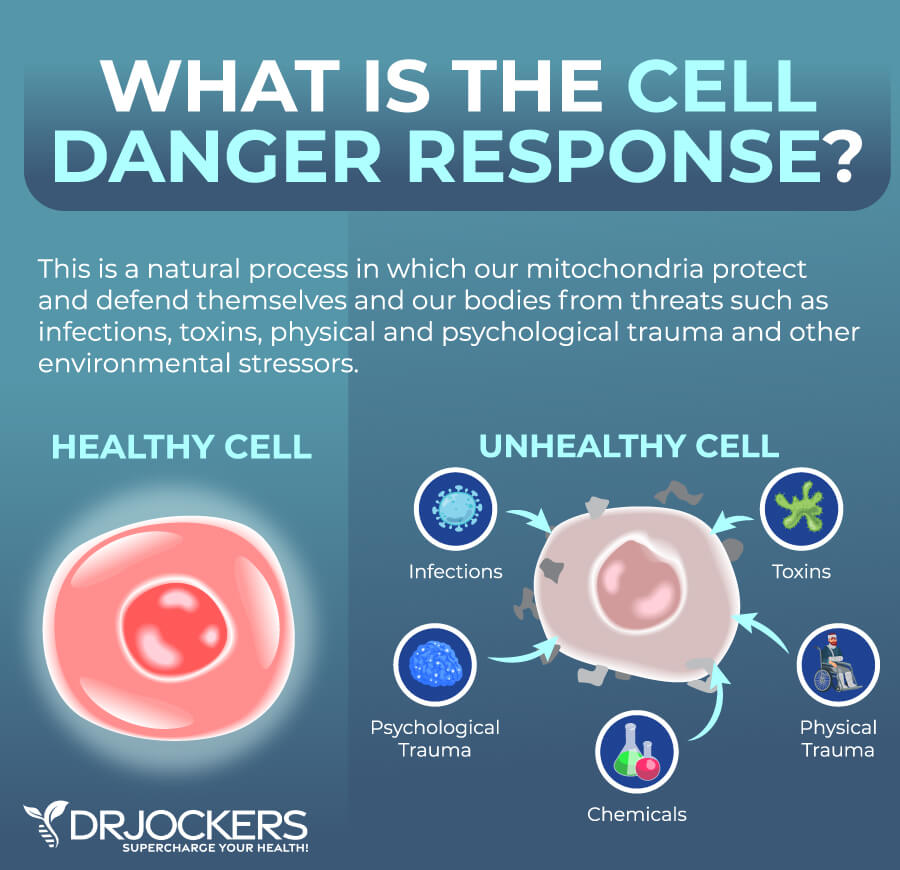
The cell danger response (CDR) is a new theory for chronic illnesses. It has been getting a lot of attention lately in functional medicine and holistic health. The CDR is part of your body’s natural response to cellular threatened danger. It may be triggered by biological stressors, chemical stressors, physical trauma, and psychological trauma.
Under normal circumstances, the CDR is an important part of your healing cycle. However, when ongoing triggers become overwhelming to your body, the CDR becomes ongoing as well and increases your risk of chronic symptoms and chronic illnesses.
In this article, you will learn what the cell danger response is. I will discuss the metabolic features of the cell danger response. You will learn about the factors that may trigger the cell danger response.
You will understand the 3 stages of the cell danger response. I will explain the connection between the cell danger response and chronic fatigue syndrome, hypothyroidism, metabolic disease, and neurological disease. I will also share how to address the cell danger response.
What Is the Cell Danger Response
The cell danger response (CDR) has been increasingly covered in functional medicine circles for good reason. A 2013 review published in Mitochondrion has described the CDR as a critical evolutionarily conserved metabolic response that is part of your body’s innate defense system (1).
It protects your individual cells from cellular threat, danger, and harm. Whether the threat is physical, biological, or chemical, if it goes beyond your cell’s natural capacity to ensure homeostasis, it triggers a CDR.
Your body is a complex system of individual cells that work together to form tissues, organs, and other systems in your body. Together, they create a complex organism that we call the human body. In this system, each cell works relentlessly to keep your body healthy.
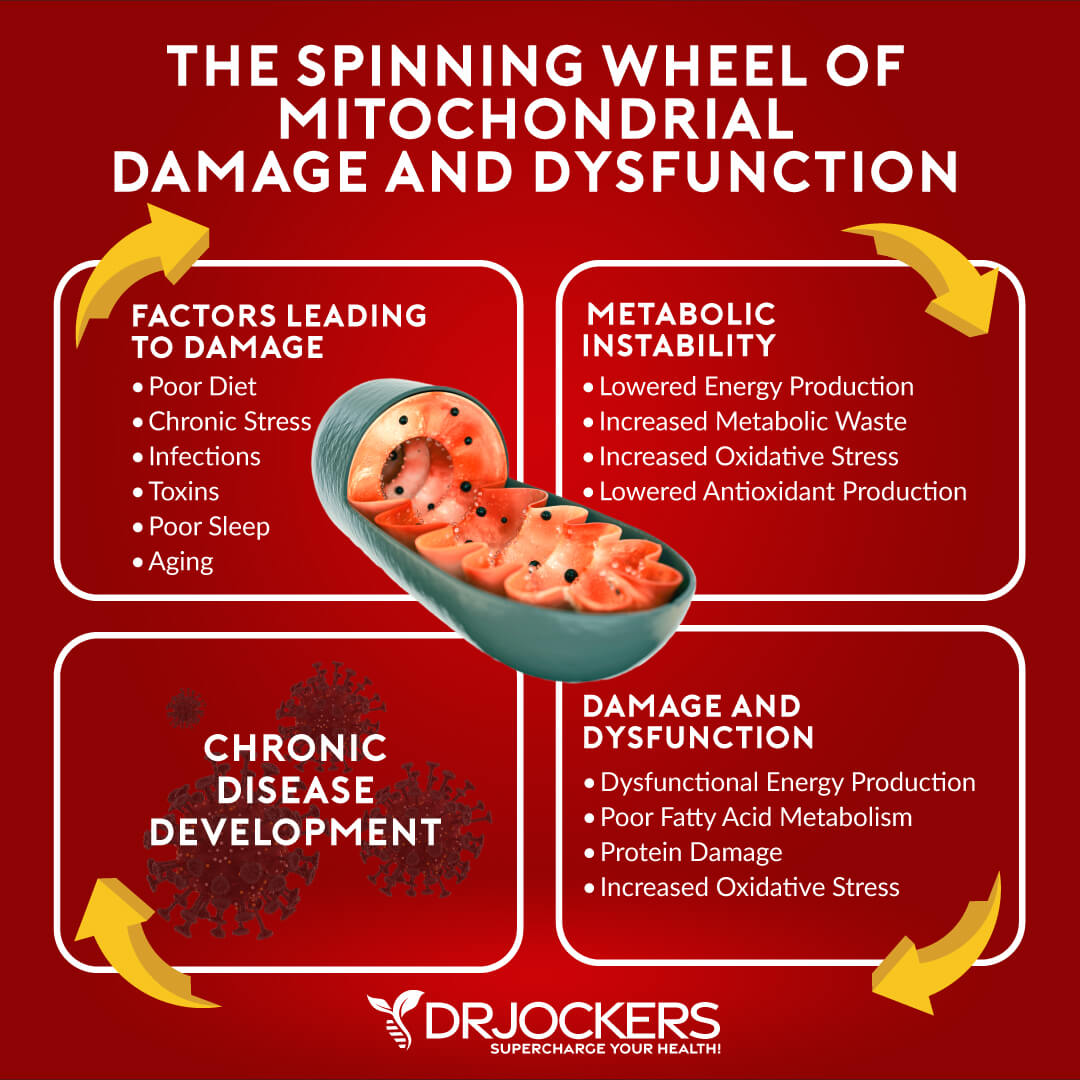
Each of your cells has several components. The most important component of your cells, and possibly your entire body, is the mitochondria. You may remember from school that the mitochondria are the powerhouse of your cells. It’s responsible for creating energy from the food you eat to fuel and energize your cells, tissues, and organs. Essentially, your mitochondria are essential for energy, function, and health.
Mitochondria and the Cell Danger Response
Another job of your mitochondria is acting as energy sensors within your cells, as well as cellular defense agents. The goal of each cell is to maintain cellular homeostasis. Your mitochondria’s job is to provide enough energy necessary for this cellular balance.
If there is a significant drop in this energy and there isn’t enough energy to meet the minimum requirement for homeostasis, your mitochondria will recognize this energy drop as a threat to your health and balance. This perceived threat will force your mitochondria to change their primary function.
Instead of energy production and optimal cell metabolism, it will now focus on cellular defense. This is a major shift in cellular physiology. CDR refers to this switch from energy production and cell metabolism to cellular defense.
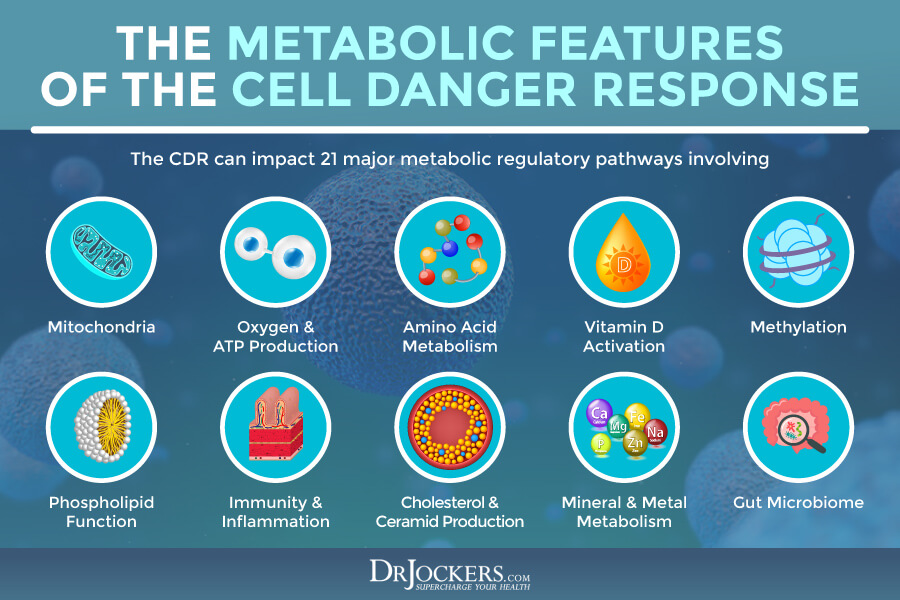
Metabolic Features of the Cell Danger Response
According to a 2013 review published in Mitochondrion, there are 21 points of metabolism that under normal circumstances are supporting health, polymer synthesis, renewal, and the decreased risk of health issues (1). However, if your cells encounter a virus, other microbial pathogens, or other potential offenders, your metabolism can move from health to inflammation, oxidizing conditions, monomer synthesis, and other issues as part of the CDR.
If these less favorable changes happen during the cell division process, inflammation may not occur. However, if there is significant cell damage or these changes occur in post-mitotic tissues with the reduced ability for growth, inflammation and other problems can occur.
The 21 metabolic features of the CDR response where problems can occur include (1):
- Mitochondria
- Oxygen
- ATP energy
- Cysteine and sulfur
- Vitamin D
- Vitamin B12 and folate metabolism
- S-adenosyl methionine (SAM)
- Ornithine
- Histidine
- Arginine
- Heme
- Phospholipids
- Tryptophan
- Lysine
- Cholesterol
- Vitamin B6
- Arachidonate
- Sphingosine
- Ceramide
- Metals
- Gut microbiome
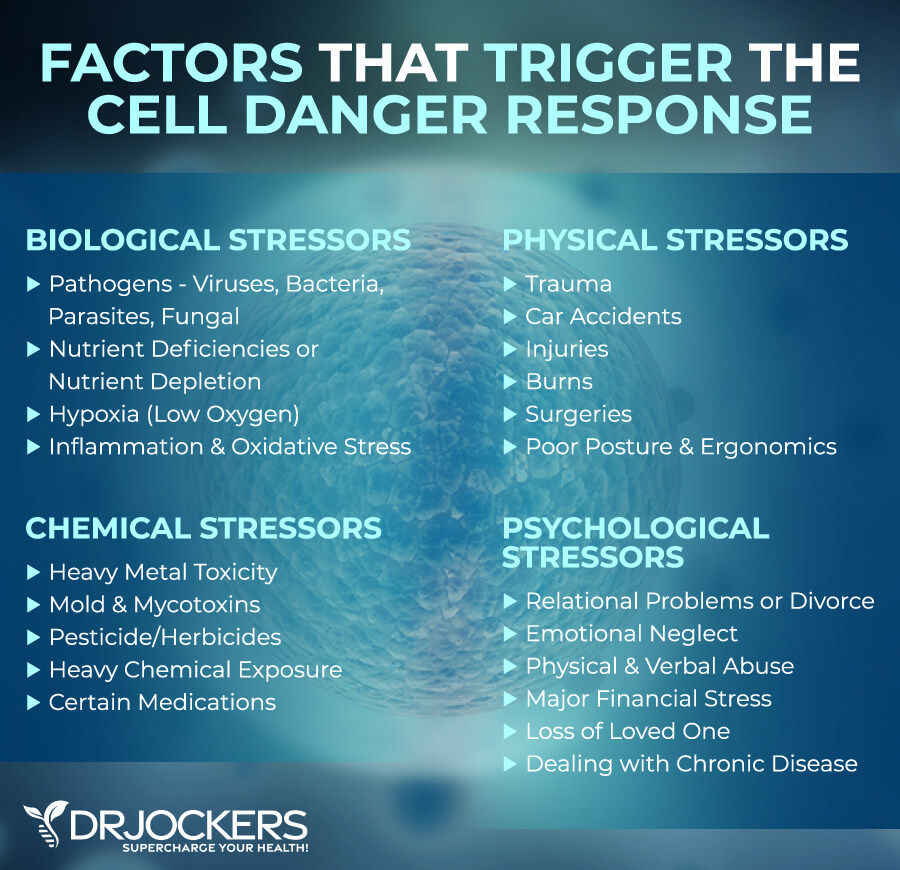
Factors That Trigger the Cell Danger Response
Anything that decreases cellular energy or increases cellular stress can potentially trigger a CDR. Factors that may trigger the CDR include:
- Biological stressors, such as viruses, bacteria, parasites, and fungi, as well as nutrient deficiency, nutrient depletion, hypoxia or low oxygen, inflammation, or oxidative stress
- Chemical stressors, such as heavy metal toxicity, chemical toxins, other toxins, and medications
- Physical stressors and trauma, such as accidents, injuries, burns, surgeries, and major infections
- Psychological stressors or trauma, such as divorce, loss of a loved one, emotional neglect, emotional abuse, major financial difficulties, and dealing with a chronic disease.
Mechanism of the CDR
Whenever your body encounters an infection, pathogen, or toxin, it will trigger a CDR. You may even notice that your body is experiencing a CDR. You may feel tired, depressed, or feverish. We often think that these symptoms are the problem. However, these symptoms are simply the natural result of your body’s natural defense mechanism trying to protect you from cellular threats, such as microorganisms or toxins.
Under normal circumstances, this response is short-lived. Within a few days or weeks, your body should recover from any infection, toxin exposure, or injury. The problem is that if this issue becomes ongoing, it can increase the risk of chronic illnesses.
According to a 2020 review published in Mitochondrion, chemical pollutants and toxins can decrease the CDR activation threshold. The review has found that ongoing CDR activation can interfere with healing and increase the risk of chronic health issues (2). Later in this article, you will learn how CDR may be related to ongoing health issues, such as chronic fatigue, thyroid problems, metabolic disease, and neurological diseases (1).

Stages of the Cell Danger Response
The 2013 review in Mitochondrion I’ve referred to earlier has outlined 3 energetically and metabolically distinct stages of the CDR (1). These 3 stages of the CDR are regulated by 3 quality control checkpoints, including CP1, CP2, and CP3. The completion of each stage works on a cell-by-cell basis instead of happening at the same time and within the same timeframe throughout your entire body.
Certain chemical signals and mitochondrial function will determine when each cell can enter the next stage to progress through a cellular healing cycle. Interruptions happening during each stage can disrupt the healing cycle and may increase your risk of chronic health issues (1).
A major problem happens when the cell gets stuck in one specific area of the healing cycle and is unable to move beyond this. This “frozen” CDR is unable to effectively adapt to the stressors of the environment and over time, this inability to adapt leads to disease.
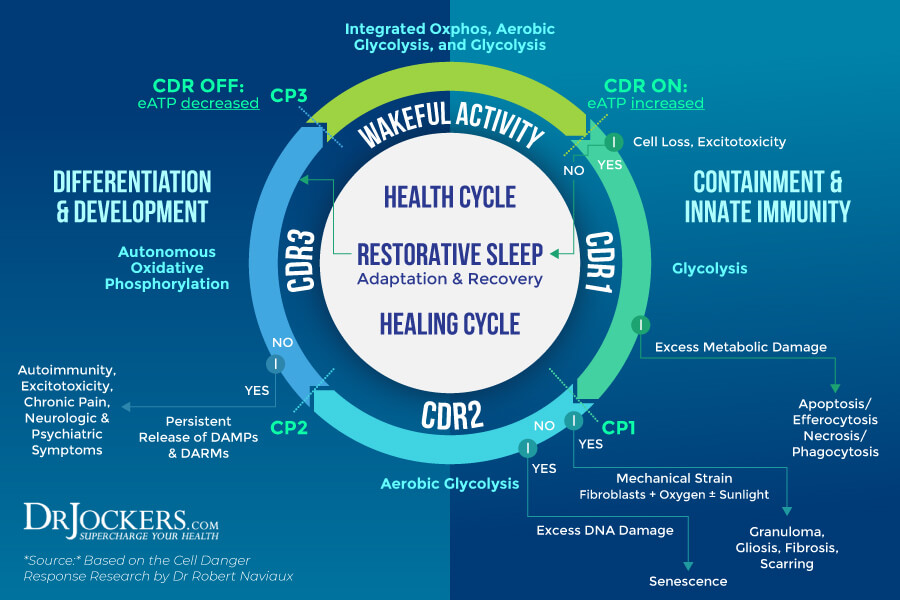
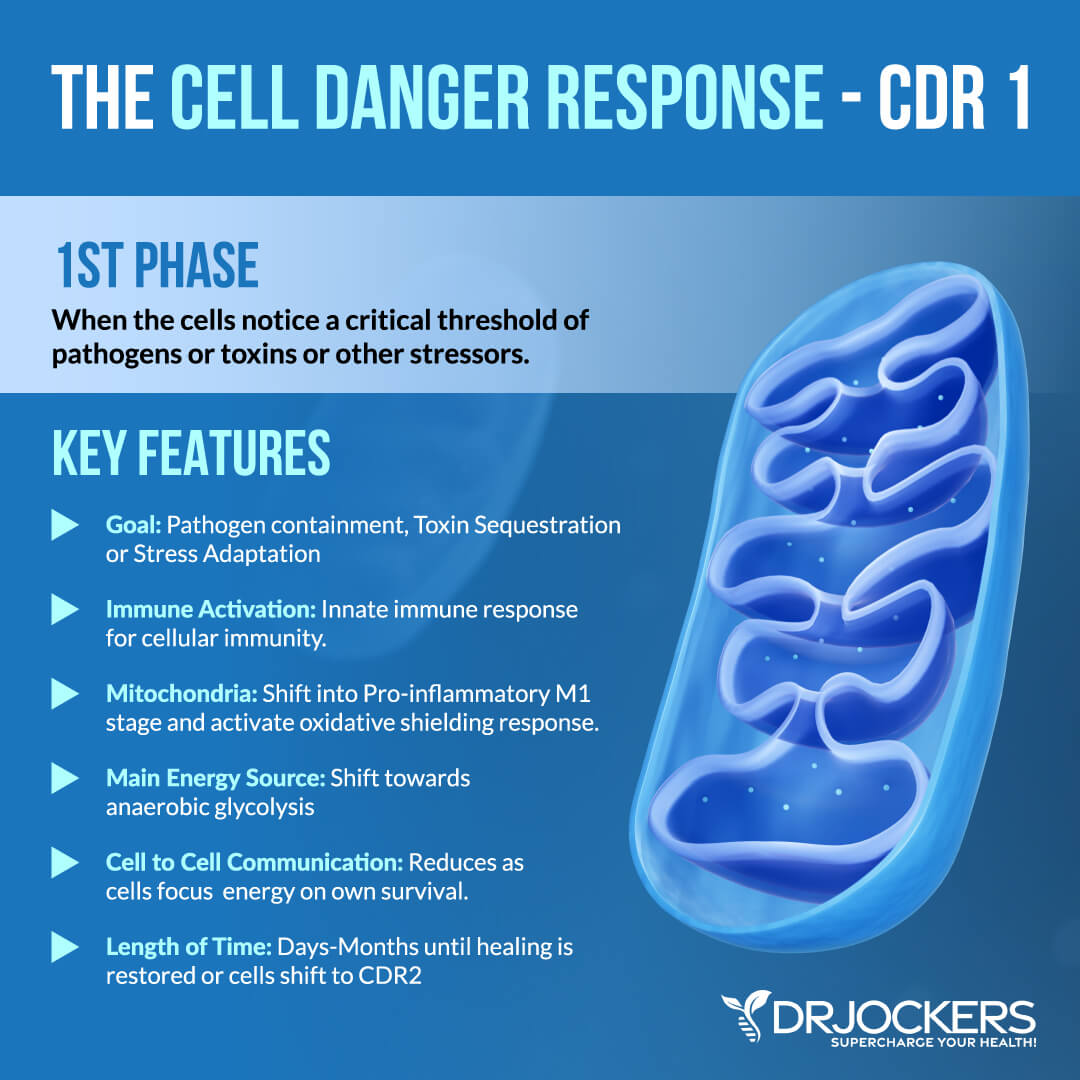
CDR1 — Glycolysis, M1 Mitochondria
CDR1 is the first stage of the CDR. This stage is responsible for activating your innate immunity. If your cells notice a pathogen, toxins, or another intruder though, they will activate your innate immune system to fight and remove the invader, do some damage control and containment as needed.
When under stress, during this stage, your mitochondria can change rapidly. Under healthy circumstances, your mitochondria are an anti-inflammatory M2 form of mitochondria responsible for nurturing your metabolic needs. Under stress, it will quickly transform into a pro-inflammatory M1 form of mitochondria to allow an oxidative shielding response for containment and damage control.
CDR1 reduces mitochondrial oxidative phosphorylation and supports glycolysis which can significantly decrease cell death. If no cells die during this stage, preconditioned cells can jump right into the last stage, CDR3.
During this stage, the cell-to-cell communication between neighboring cells also reduces or changes because each cell needs to focus on their own survival. The problem is that organ functions require cell-to-cell communication and coordination to achieve optimal health and function. The reduction in cell-to-cell communication can result in some loss of function during the early phases of inflammation and repair.
This may last for a few days, weeks, or even months into recovery depending on the cause of the problem. Eventually, as recovery occurs a metabolic shift can happen to move from glycolysis in stage 1 (CDR1) to aerobic glycolysis in stage 2 (CDR2) then oxidative phosphorylation in stage 3 (CDR3) (1).
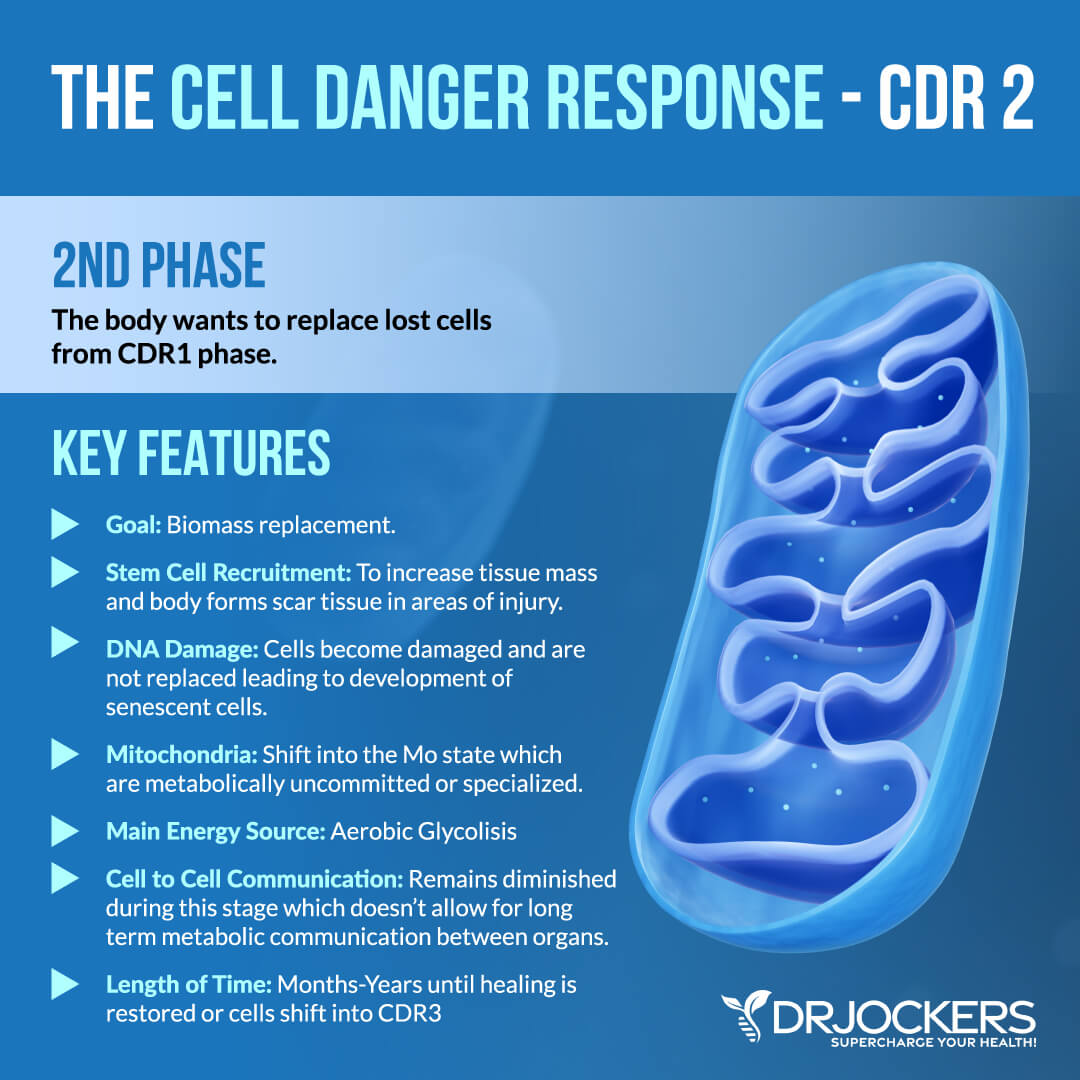
CDR2 — Aerobic Glycolysis, Mo Mitochondria
The goal of stage 2 of the CDR or CDR2 is biomass replacement. Each of your organs and tissues needs a certain number and diversity of differentiated cell types to function optimally. When this number or distribution changes and cells are lost, they need to be replaced with new and functional cells to restore health. During CDR1, your body’s focus was to clear infections, cleanse toxins, and repair initial injuries. Now, during CDR2, it’s time to replace lost but necessary cells.
To do this, your body recruits stem cells to restore needed biomass. Stem cells are your body’s raw material. They are not specialized cells that are located in all tissues throughout your life. When stem cells get activated, they become part of the cell cycle. The mitochondria in your stems cell and their daughter cells exist in a so-called Mo state. The Mo state refers to a youthful and metabolically uncommitted state. It means that they are not yet specialized. The Mo mitochondria at this stage can assist aerobic glycolysis necessary for rapid cellular growth.
CDR2 is a stage of regeneration in other ways as well. During this stage, your body also recruits fibroblasts and myofibroblasts to allow any areas of infection, damage, or injury to close off with scar tissue. This allows tissue regeneration and healing avoiding further issues.
During CDR2 the communication between cells is still not optimal. Your cells are constantly dividing, migrating, and growing. Due to these ongoing changes, they cannot create long-term metabolic cooperation. Once your cells stop growing and migrating, they will be ready to make long-term symbiotic relationships necessary for optimal health and protection for new exposure to similar danger. Once this cell cycle is over and cells are able to establish steady cell-to-cell relationships through gap junctions and other structural systems, your cells can move into stage 3 or CDR3 (1).
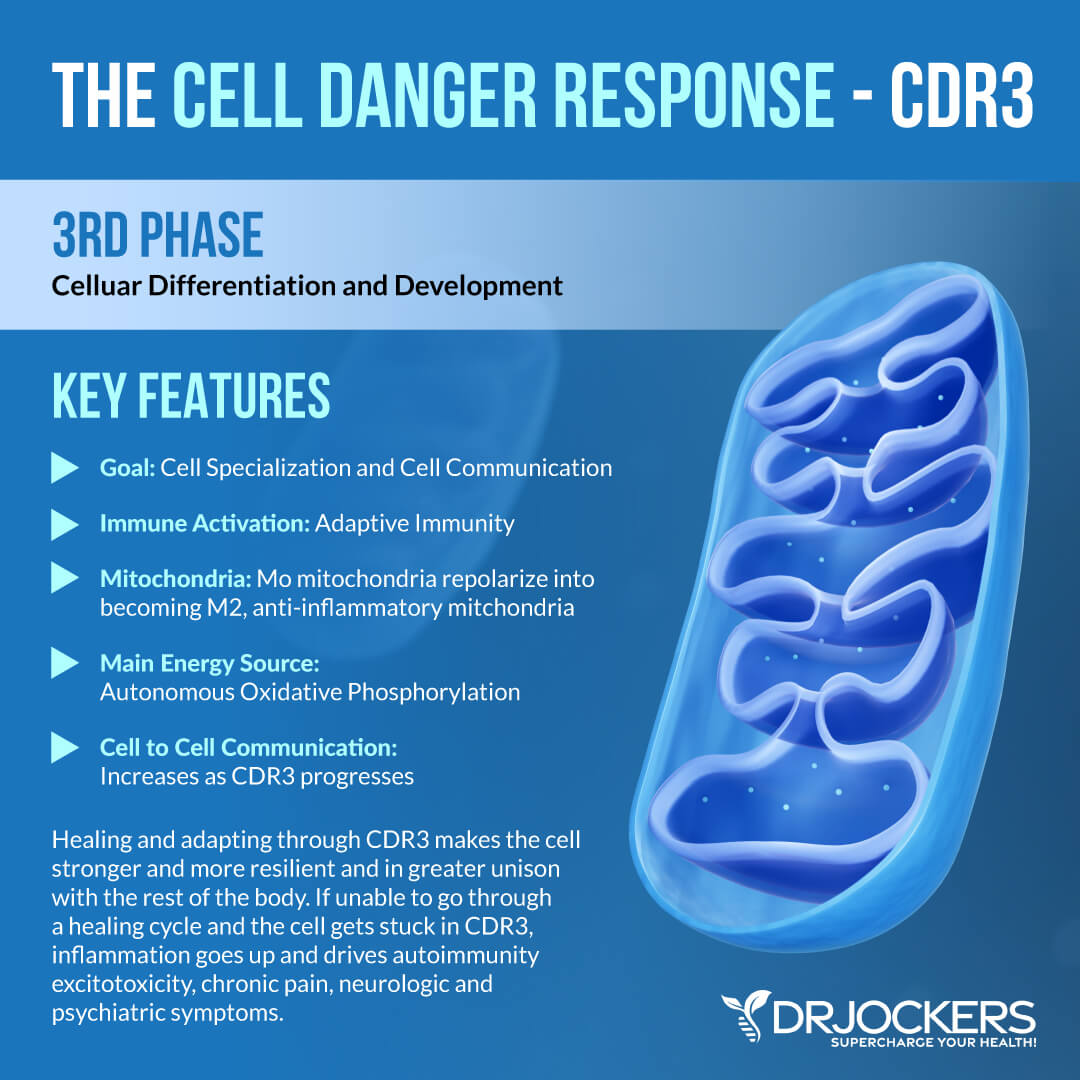
CDR3 — Cell Autonomous Oxphos, M2 Mitochondria
The goal of CDR3 is cellular differentiation, tissue remodeling, detoxification, adaptive immunity, metabolic memory, sensory modulation, pain modulation, and sleep. At this stage, your cells are done dividing and have developed strong cell-to-cell connections with neighboring cells.
Your new cells still have to receive metabolic instructions and learn a lot of things from older, existing, and neighboring cells to reach optimal function. They have to undergo some learning process when it comes to cell structure, cellular metabolism, and gene expression. They have to adapt to existing tissue conditions to fully integrate.
At this stage, Mo mitochondria can repolarize into becoming an M2, anti-inflammatory mitochondria. Access to nutrient and oxygen resources will be reestablished allowing the elimination of various metabolites and waste products as well through various capillaries and lymphatics. A normal mitochondrial network and a completely differentiated tissue function are also established at this stage.
By the end of CDR3, your cells will be able to re-create connections with your automatic nervous system and tissue lymphatics for optimal functions. The removal of metabolites and waste products through tissue-specific detoxification will allow better communication between your tissues and organs. The end of the CDR3 leads to improved baseline physiologic performance and an improved reserved capacity to deal with stress, injury, or illness (1).
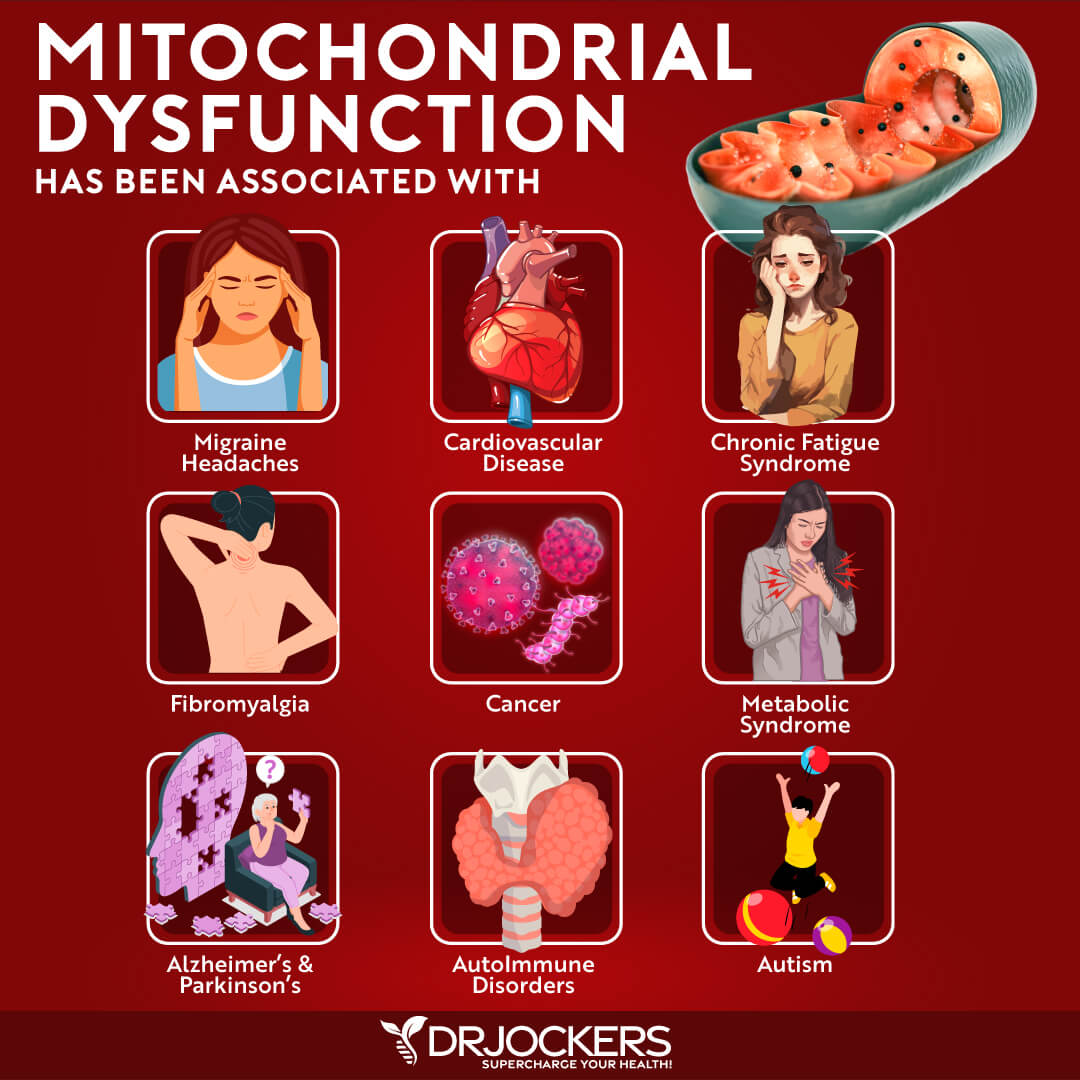
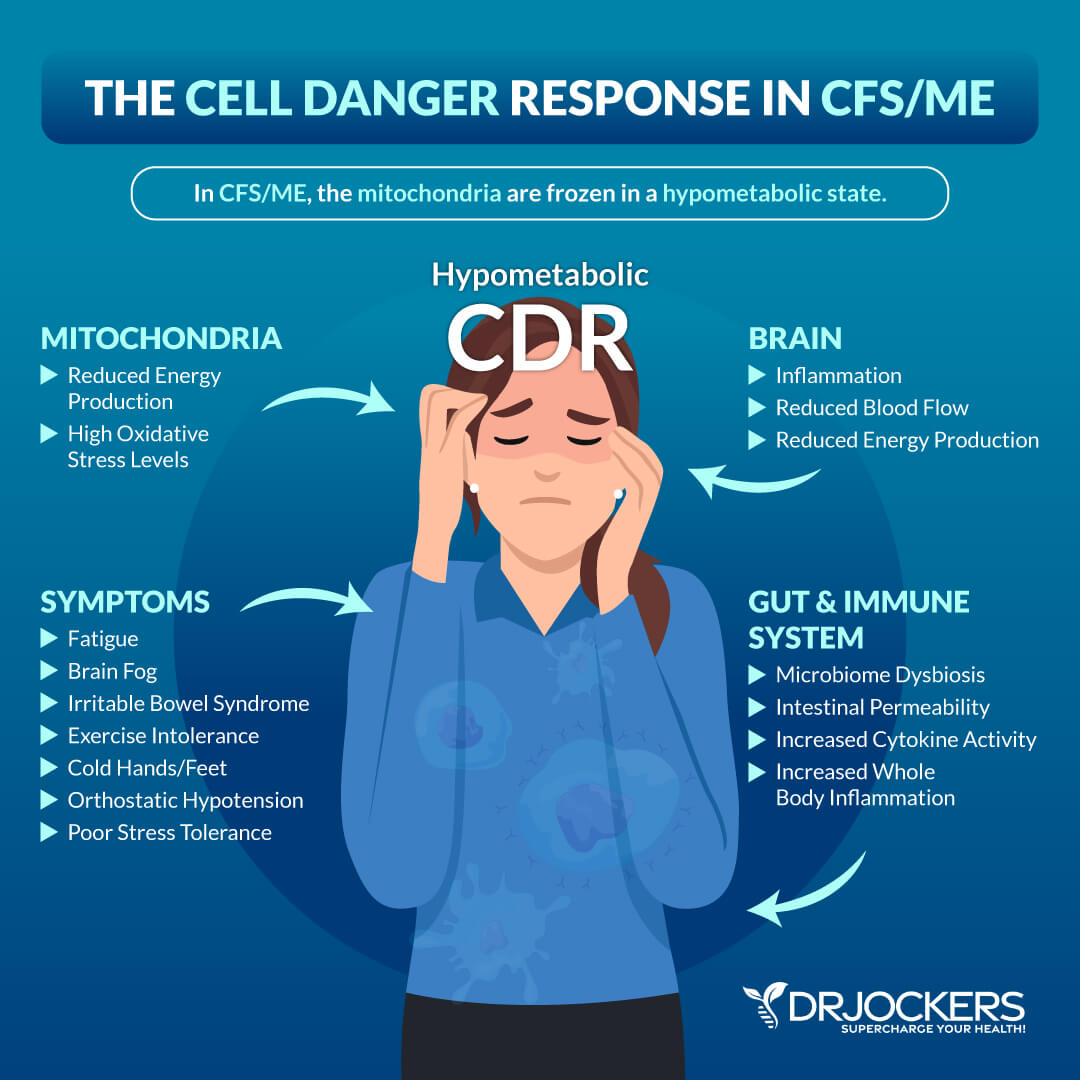
CDR and Chronic Fatigue Syndrome
Chronic fatigue syndrome (CFS) is also called myalgic encephalomyelitis (ME) is a chronic illness that’s widespread across your body affecting many areas of your health. It may cause chronic fatigue, muscle pain, tender lymph nodes, headaches, brain fog, concentration troubles, and other issues.
According to a 2016 study published in the Proceedings of the National Academy of Sciences, CFS is a state of hypometabolic function characterized by prolonged CDR (3). Hypometabolic refers to an abnormal reduction of metabolic functions.
CFS may be triggered by various infections, toxins, physical trauma, or psychological traumas. You may notice that these triggers are the very same triggers of the CDR. In the case of CDR, these environmental triggers can result in hypometabolic CDR.
A hypometabolic state will lead to a fight, flight, or freeze stress response, which when prolonged can increase the risk of disease. This ongoing state of threat can become overwhelming to the body leading to an ongoing survival-based CDR causing the chronic symptoms of CFS.
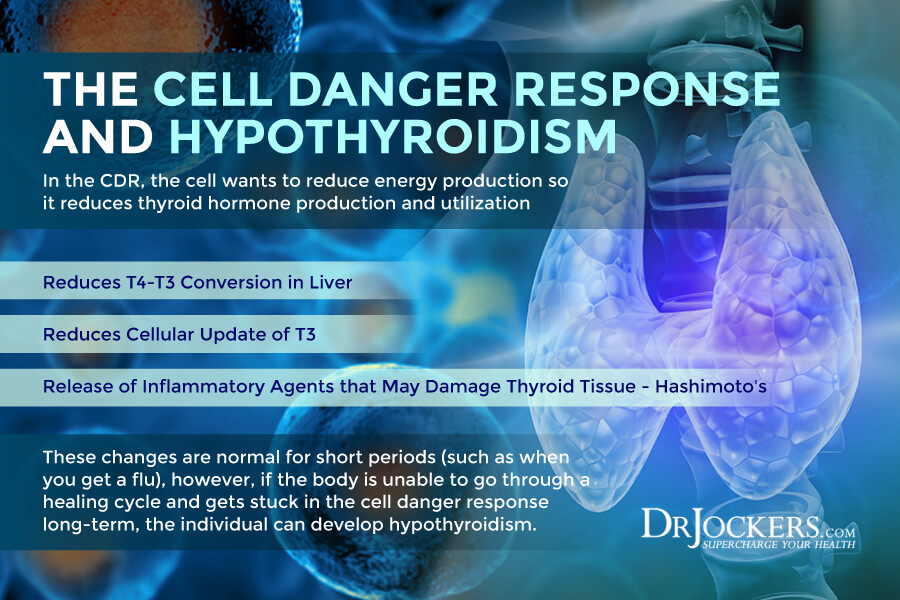
CDR and Hypothyroidism
The CDR can also affect and change cellular thyroid physiology as well by decreasing thyroid hormone transportation and deactivating thyroid hormones. A 2020 study published in the Journal of Clinical Endocrinology and Metabolism has found that cell stress can affect thyroid health (4).
As we know, cell stress can cause CDR. Symptoms of hypothyroidism can often be induced or worsened by the CDR.
The CDR can affect thyroid function in various ways. For one, thyroid hormone transport depends on cellular energy. If the cell is under stress, it causes decreased cellular energy as well, which will lower thyroid hormone transport. This will result in fewer T3 and T4 thyroid hormones entering your cells and making it to the thyroid receptor, which may lead to symptoms of hypothyroidism.
The CDR will also cause the release of inflammatory chemicals which can deactivate T3 and T4 hormones inside your cells. The CDR will also trigger the release of some release signaling molecules (DAMPs and PAMPs) into your bloodstream to help your body fight various pathogens or toxins. However, your thyroid is very sensitive to these molecules triggering thyroid self-destruction. This may lead to an autoimmune response resulting in Hashimoto’s thyroiditis.
As with all of these chronic health conditions I am discussing in this article, CDR becomes problematic for your thyroid if it becomes chronic. Ongoing CDR can impact cellular energy, cause thyroid hormone deactivation, and increase chronic hypothyroid symptoms.
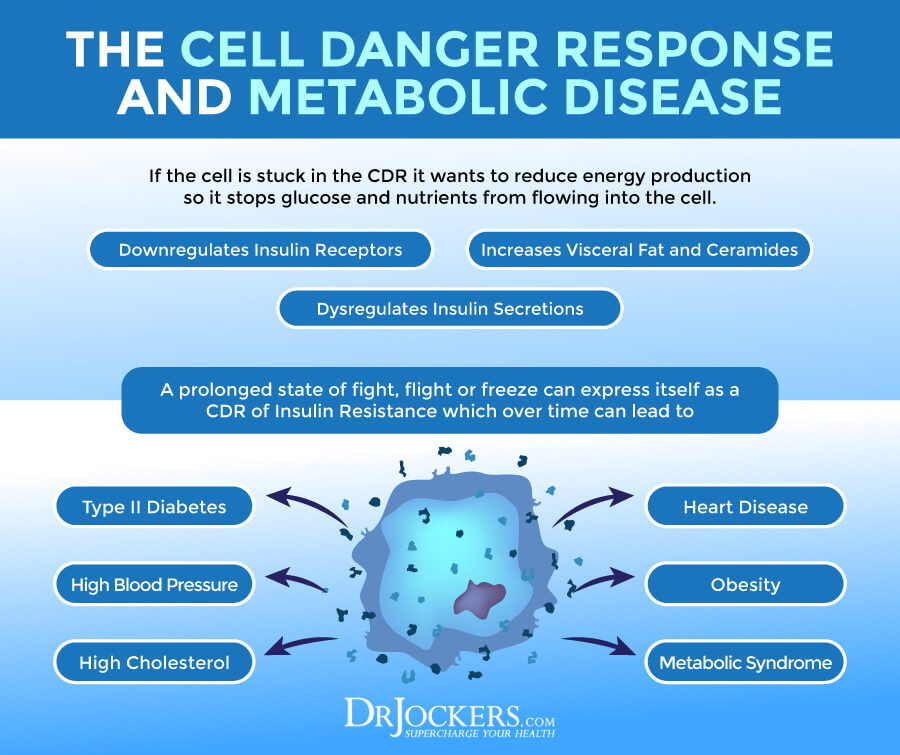
CDR and Metabolic Diseases
CDR can trigger metabolic diseases. When your body encounters some stress, your sympathetic nervous system, as a part of the CDR, will respond with a fight or flight response to allow escape, safety, and overcoming danger.
In other situations, your body responds with a freeze response, which means shutting down energy for surviving the overwhelming threat. When your body becomes overwhelmed with ongoing perceived threats, CDR becomes chronic, increasing the risk of chronic health issues.
When your body is stuck in a chronic flight or fight response and persistent CDR, it can affect your insulin and blood sugar levels. Insulin is an important hormone that allows glucose to be used for energy and to enter your cells to be used for energy later.
It depends on each situation how your body uses glucose. If you are eating a meal under safe circumstances, your body will allow insulin to rise and store sugar for later. However, when your body perceives danger, it will act otherwise.
Under danger, your body may end up reducing insulin production to prevent glucose from entering your cells, it may cause glucose to stay outside your bloodstream, it may release stored glucose without needing it, and it may even start to make glucose from other molecules.
This prolonged fight or flight response associated with ongoing CDR can increase blood glucose levels and increase the risk of insulin resistance, type 2 diabetes, metabolic syndrome, obesity, high cholesterol, hypertension, and heart disease.
A 2015 study published in Current Problems in Pediatrics and Adolescent Health Care has followed pregnant women starting during World War II during a time of famine and found that prenatal stress had increased their chance of insulin resistance and metabolic disease (5). Thus, being overweight or inactive is not always the cause or only cause of metabolic disease, but it can be chronic stress and ongoing CDR.
A 2019 study published in PLOS ONE has also found that insulin resistance may be an overlooked characteristic of chronic pain syndromes like fibromyalgia (6). Fibromyalgia is a condition that just like CFS, is characterized by a CDR stuck in fight or flight mode.
Most practitioners believe that type 2 diabetes occurs because your body is overwhelmed by glucose. However, it may also be the result of an ongoing CDR and the fight, flight, or freeze response.
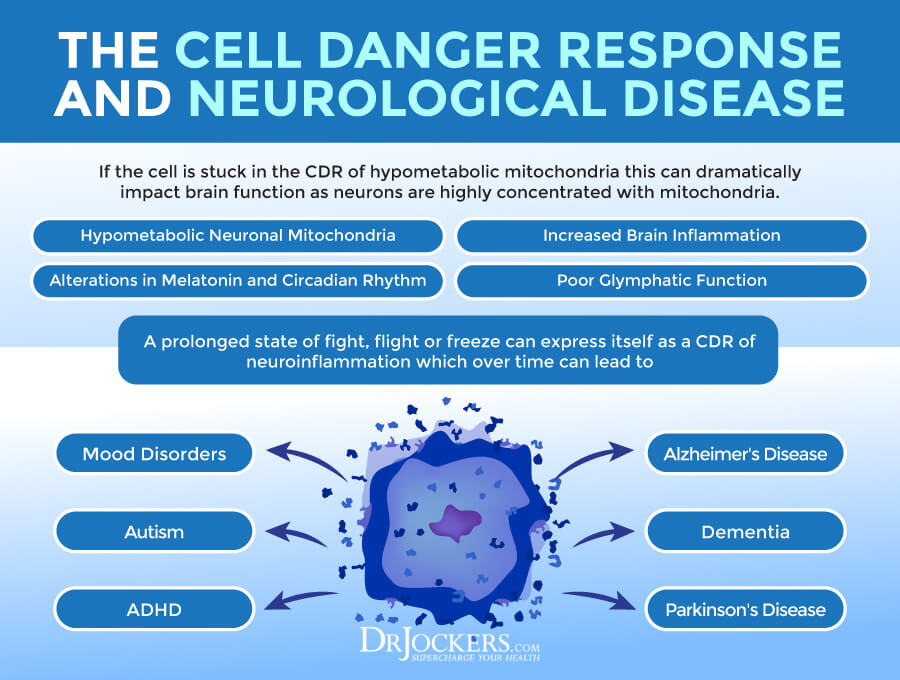
CDR and Neurological Disease
Considering the CDR’s involvement in the fight, flight, and freeze response, you may not be surprised that it may also be connected to mental health and neurological issues, including PTSD, bipolar disorder, anxiety, obsessive-compulsive disorder (OCD), autism, and neurodegenerative diseases, such as Alzheimer’s or Parkinson’s disease.
When the CDR gets stuck in a state of increased energy, it will result in increased heart rate, adrenaline, cortisol, blood pressure, and inflammation. This may cause you to feel wired and make it difficult to relax, calm down, connect with yourself, or connect with other people.
A 2013 review published in Mitochondrion has described these conditions as CDR3 disorders (1). It also explained that autism, Alzheimer’s disease, bipolar disorder, Parkinson’s disease, and schizophrenia doesn’t only affect the brain and cause neurological symptoms, but may also result in whole-body metabolic abnormalities that can show up on blood and urine tests.
A 2014 study published in Biogerontology has also found that cancer, which is a CDR2-related disease, may also increase the risk of Alzheimer’s disease (7). Furthermore, CDR can also disrupt gut health, which according to a 2017 review published in Clinics and Practice on the gut-brain axis, can affect the brain, neurological, and mental health (8).
A 2017 study published in the Annals of Clinical Translation and Neurology has discussed that a drug named suramin may help to improve CDR (9). This medication has been around for about a hundred years originally to treat African sleeping sickness. The authors describe that it may also help to improve cell dysfunction in autism spectrum disorder. They explain that the neurons in autism have little channels that allow the ATP produced by the mitochondria to flow out into the surrounding place.
When this ATP attaches to the receptors on the cell’s surface, it will trigger a CDR. Neurons go into survival mode resulting in symptoms. However, suramin is able to block these channels. ATP cannot escape, the CDR is blocked, and neurons and cells can continue functioning normally.
This study was rather small with only 5 subjects to prove the benefits of suramin for autism. However, it demonstrates how CDR may be responsible for some symptoms of autism and how blocking CDR may help to reduce or eliminate these symptoms.
Addressing the Cell Danger Response
So how do you address the cell danger response? Great question! As you’ve learned, the CDR may be triggered by biological, chemical, physical, or environmental stressors, including viruses or other pathogens, nutrient deficiency, chemical toxins, heavy metal, accidents, burns, other physical trauma, and psychological trauma.
To address the CDR and improve your symptoms and health issues, it is important that you first understand the root of these biological, chemical, physical, and psychological stressors triggering an ongoing CDR and related health issues. Once you understand the root causes of the problem, you can put your body into a healing state.
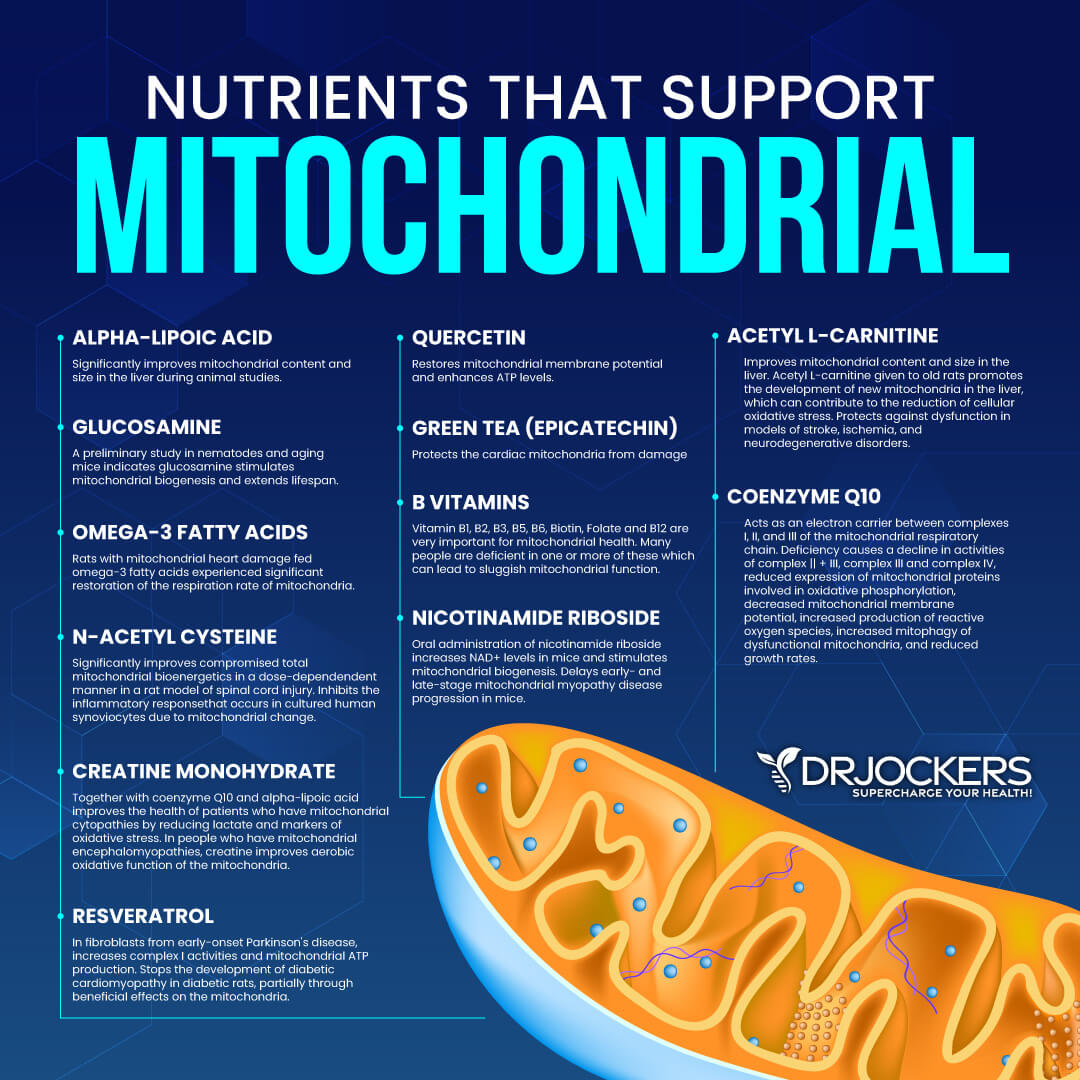
You can support your mitochondrial health and healing through an anti-inflammatory, nutrient-dense nutrition plan, regular exercise, reduced stress, improved sleep, intermittent or extended fasting, red light therapy, and various mitochondria-supporting nutrients. To learn more about how to support healing and mitochondrial health, I recommend reading this article.
Final Thoughts
The cell danger response is part of your body’s natural response to cellular threatened danger. It may be triggered by biological stressors, chemical stressors, physical trauma, and psychological trauma.
It is an important part of your healing cycle. However, when chronic triggers become overwhelming to your body, the CDR becomes ongoing and increases your risk of chronic symptoms and chronic illnesses. To address the CDR, I recommend that you follow my tips to support your mitochondria or make an appointment with us.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



Thank you so much for your godly knowledge and wisdom in the true science that God gives us. We are a blessing.
Thanks so much for all your support Aimee! Blessings to you!