 Gut Mucosa: How to Strengthen Your SIgA Gut Immune System
Gut Mucosa: How to Strengthen Your SIgA Gut Immune System
The gut mucosa is a protective barrier that lines the digestive tract. It houses gut flora, aids in the absorption of nutrients, and protects us from pathogens, toxins, and dietary antigens.
As an integral part of our immune system, a healthy gut mucosa is key for overall health. When it is functioning properly, the gut mucosa stops microorganisms from passing through the gut lining while preserving the ability to absorb nutrients.
Secretory IgA is the main immunoglobulin produced by the gut mucosal immune system to help stop intruders from harming the body. Disruptions in our gut mucosa and low levels of SIgA can lead to infections, food sensitivities, gastrointestinal diseases, autoimmune conditions, and more.
To strengthen your SIgA gut immunity, it is important to eliminate factors that damage your gut mucosa and incorporate supportive strategies. This article will explain what the gut mucosa is, why it is important, and how to test your gut mucosa. I will also discuss the factors that damage your gut mucosa and strategies you can implement to support and strengthen your gut mucosa.
What is the Gut Mucosa?
The gastrointestinal tract is a tube-like structure that runs from the oral cavity to the anus. It is responsible for the digestion of food, absorption of nutrients, and elimination of unnecessary waste products.
The GI tract is continuously exposed to dietary antigens and toxins such as herbicides and pesticides. Bacterial and viral pathogens, including parasites, also enter the body through the GI tract.
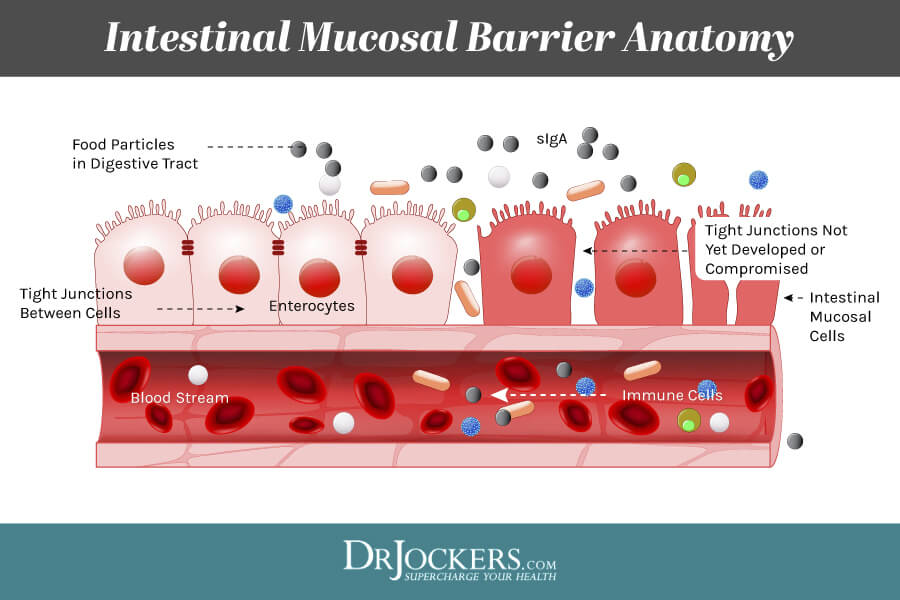
To protect the body from the constant onslaught of dietary antigens, toxins, and pathogens, the GI tract is covered by mucus (the gut mucosa). The gut mucosa is the innermost layer of the GI tract which surrounds the lumen, or open space within the tube. It has three layers:
- Epithelium (innermost layer): a single-cell layer lining the interior lumen of the gastrointestinal tract;
- Lamina propria: interstitial tissue with a rich vascular and lymphatic network and abundant lymphocytes; and,
- Muscularis mucosae: a thin layer of smooth muscle for local movement of the mucosa.
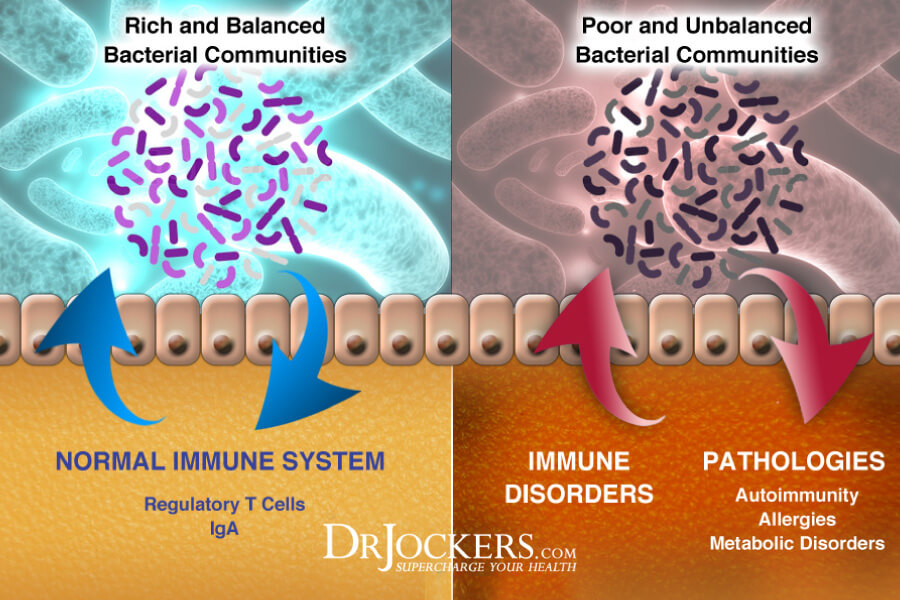
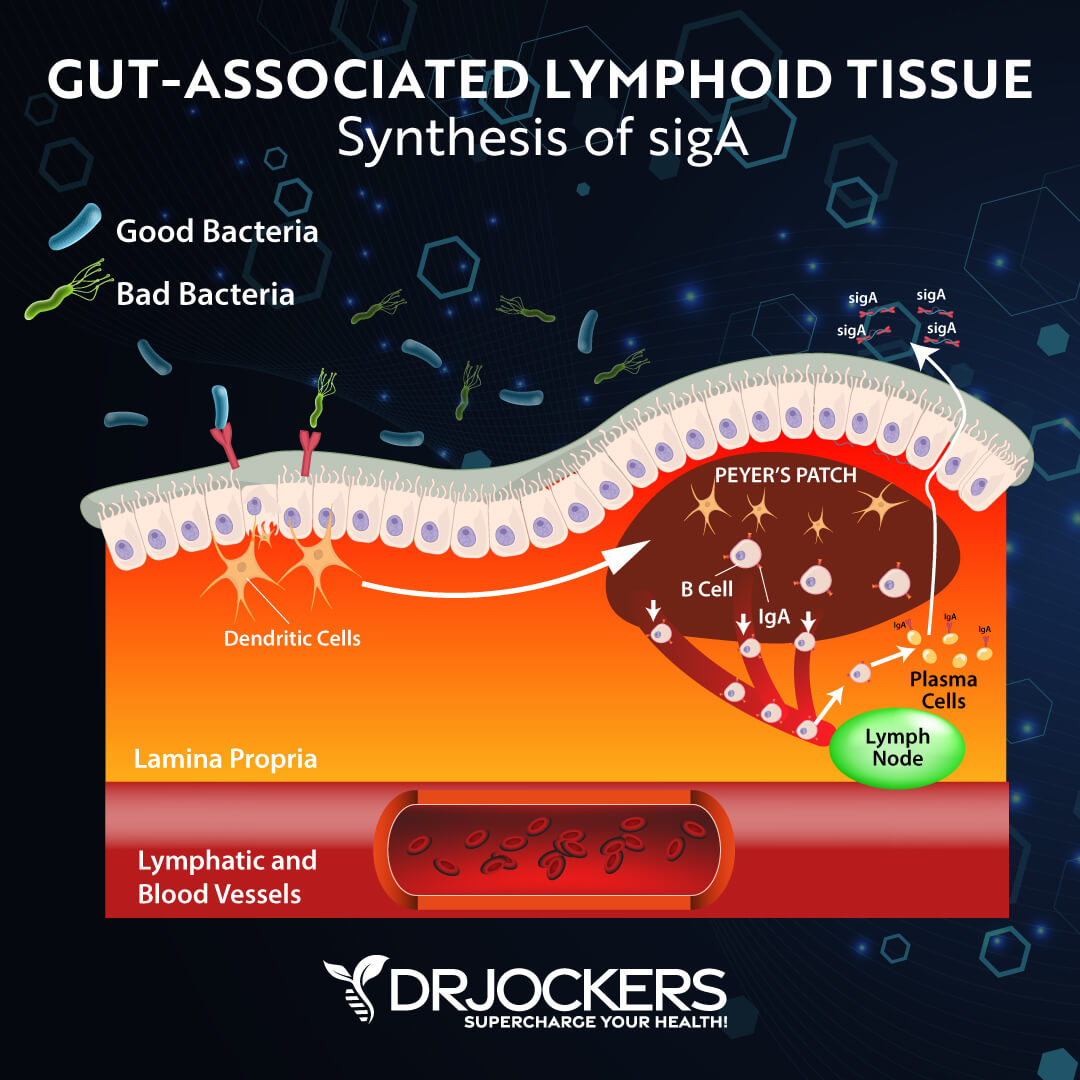
The gut mucosa contains gut-associated lymphoid tissues (GALT), secretory IgA (SIgA), antimicrobial peptides, mucosal membrane cells, cytokines, chemokines, and commensal bacteria (1). GALT represents almost 70% of your body’s entire immune system (2).
Gut Mucosa and sIgA
Immunoglobulin A, or sIgA in its secretory form, is the primary immunoglobulin in the intestinal mucosa. Immunoglobulins are proteins present in the serum and cells of the immune system which function as antibodies.
SIgA is the first line of defense in response to antigens, toxins, and pathogens in the GI and respiratory tracts. SIgA antibodies have been shown to establish and maintain healthy gut flora. Low SIgA levels are involved in allergy development and an increased risk of allergic manifestations in children. (1).
Importance of the Gut Mucosa
The gut mucosa is critically important to our overall health. It is the main interface between the body and the outside world. The gut mucosa allows for the absorption of nutrients while being a barrier to pathogens, toxins, and dietary antigens. It maintains homeostasis (balance) in the GI tract.
The gut mucosal system is a vital part of our immune system. Intestinal immunomodulatory cells are located in the gut mucosa and are an intermediary by which the gut microbiota affects physiological and pathological properties. These cells control immune responses and reduce inflammation (3).
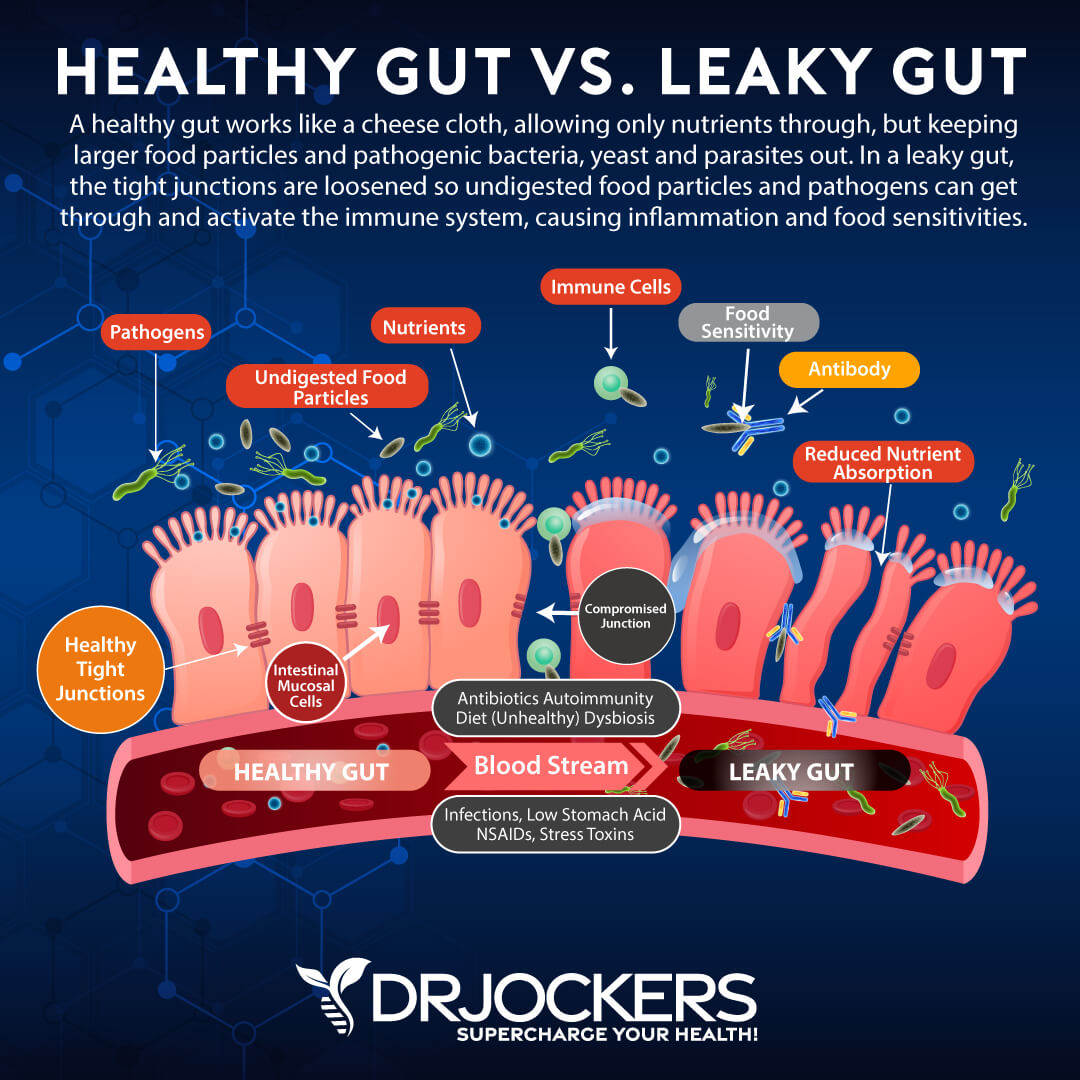
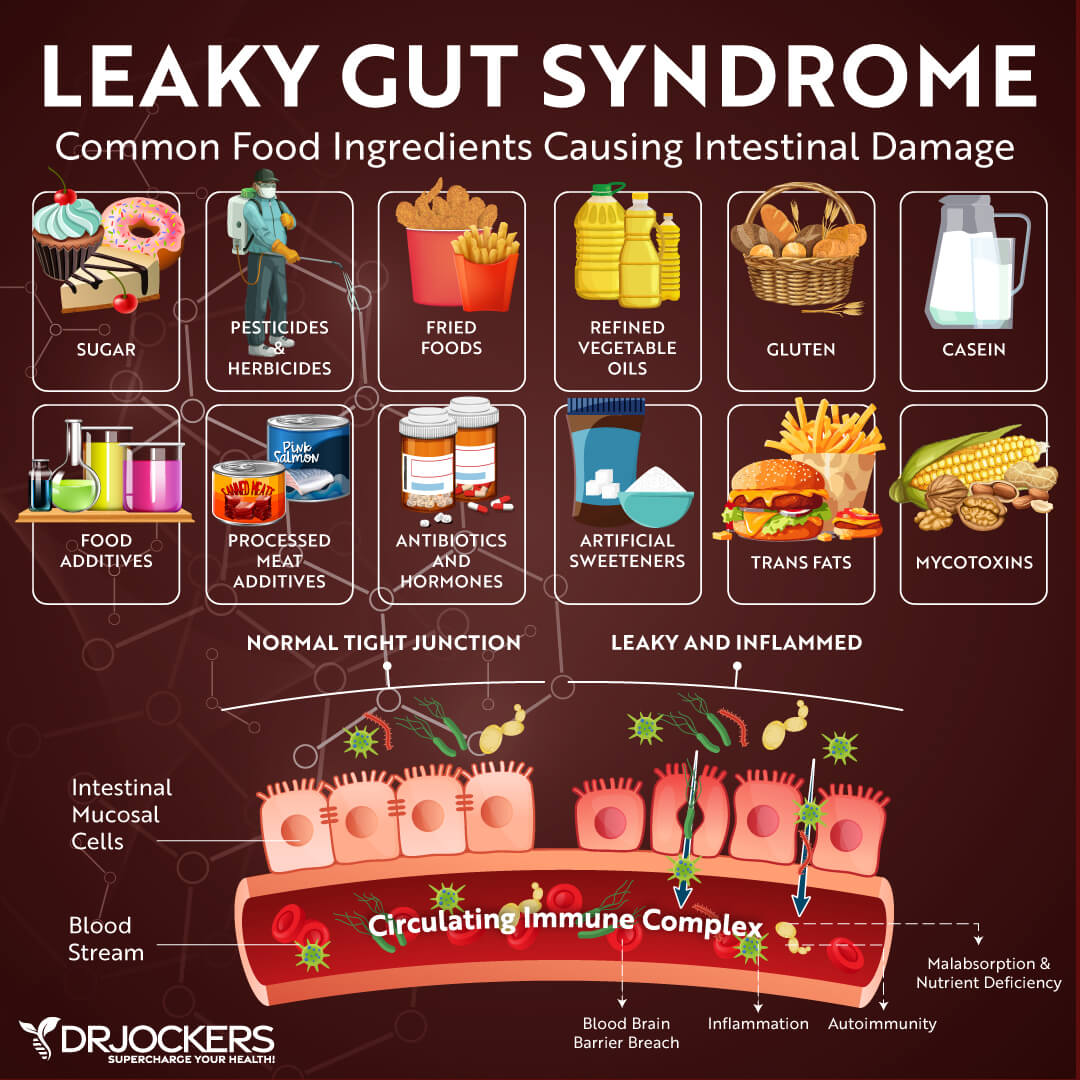
Disruption of the gut mucosa results in increased intestinal permeability (or leaky gut). Leaky gut syndrome is a condition in which the tight junctions in the gut lining become too large and abnormally permeable. Undigested food particles and toxins can pass through these holes in the intestinal wall and into the bloodstream. This causes the immune system to overreact and results in chronic inflammation.
A damaged gut mucosa and dysfunctional intestinal barrier can lead to many health problems. These include inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), gut infections, obesity, diabetes, celiac disease, food sensitivities and food allergies, and other health conditions (4, 5).
Testing the Integrity of the Gut Mucosa and SIgA Levels
The GI-MAP™ Stool Analysis Test is the most thorough stool test on the market. It is the only FDA-approved DNA test for gastrointestinal microbes and pathogens available.
The GI Map tests for imbalances in the gut microbiome, candida and other fungi, and parasites, including both protozoa and worms. This comprehensive stool test can reveal if you have H. pylori, viral pathogens, potential autoimmune triggers, and viruses, including cytomegalovirus and Epstein Barr virus.
GI Map reveals the integrity of your gut mucosa with digestion, gastrointestinal, and calprotectin (inflammation) markers. This test also measures SIgA levels. If SIgA levels are low, this indicates the gut immune system is suppressed. High fecal SIgA indicates an elevated immune response to antigens in the GI tract. For more information on the GI-MAP and how to order, go here.
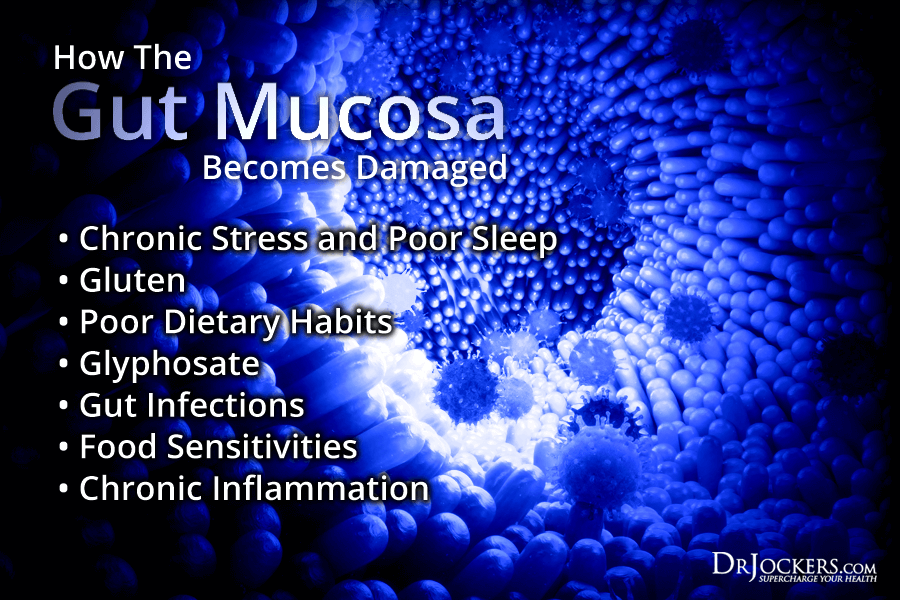 How the Gut Mucosa Becomes Damaged
How the Gut Mucosa Becomes Damaged
1. Chronic Stress and Sleep Deprivation
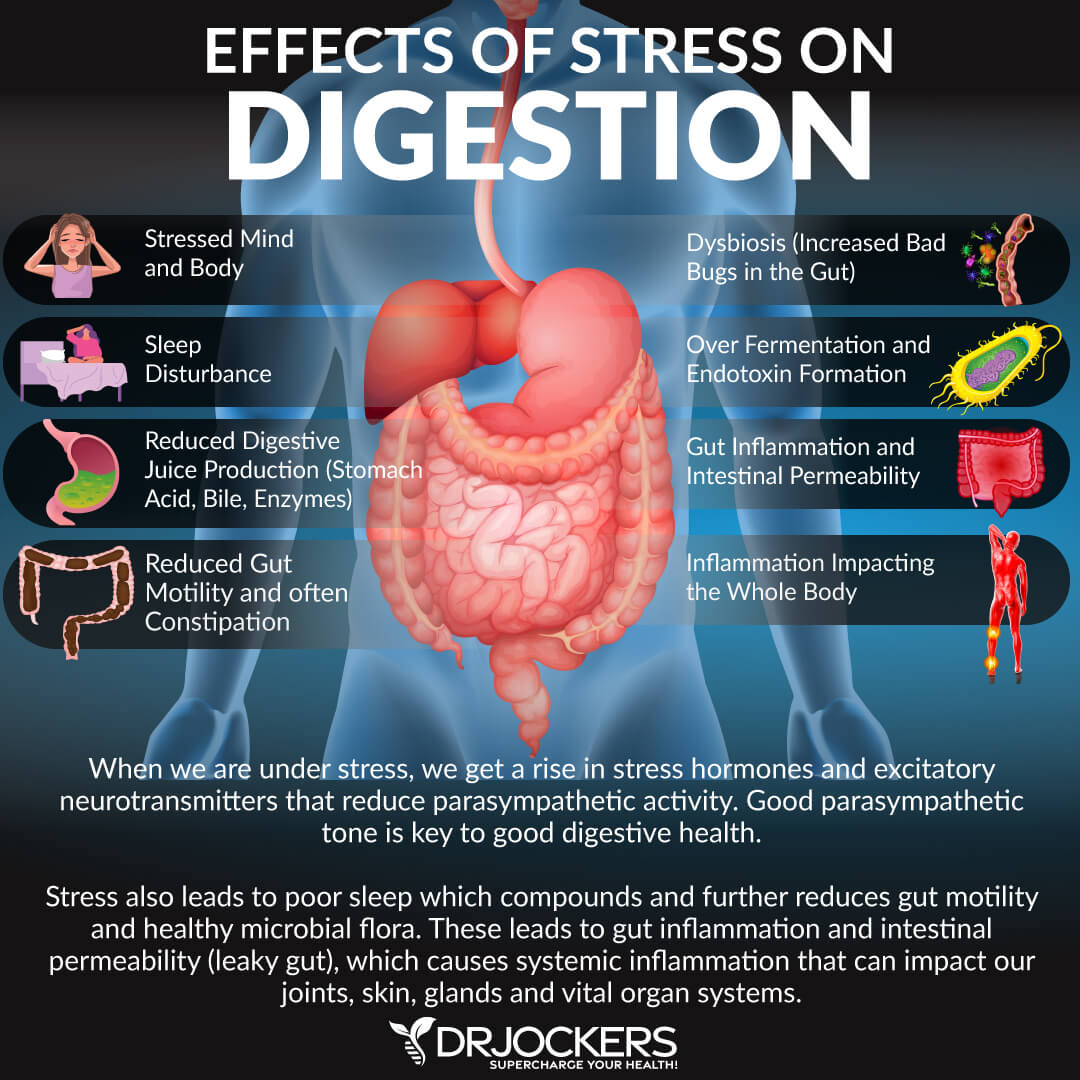
Chronic stress can damage the gut mucosa by modulating key inflammatory pathways (6). These pathways include oxidative stress, sympathetic activity, transcription factor nuclear factor kappa B (NF-kB), and pro-inflammatory cytokine production. Stress affects the gastrointestinal tract by decreasing mucosal blood flow and thereby compromising the integrity of the gut mucosal barrier.
Stress activates the “fight or flight” response in the central nervous system which can slow down or even stop the digestive process as the body diverts its energy to face the perceived threat. Chronic stress has been linked to numerous digestive disorders, including irritable bowel syndrome (IBS) (7).
Poor sleep habits also cause inflammation and damage the gut mucosa. Numerous studies on the effects of sleep loss have shown that mediators of inflammation are altered by sleep loss. Sleep loss induces a systemic, low-grade inflammation characterized by the release of several molecules, including cytokines and acute-phase proteins (8).
Sleep deficiencies cause blood sugar imbalances and increased cortisol secretion which cause more inflammation. Sleep deficiencies are linked to numerous health conditions, including high blood pressure, diabetes, and obesity.
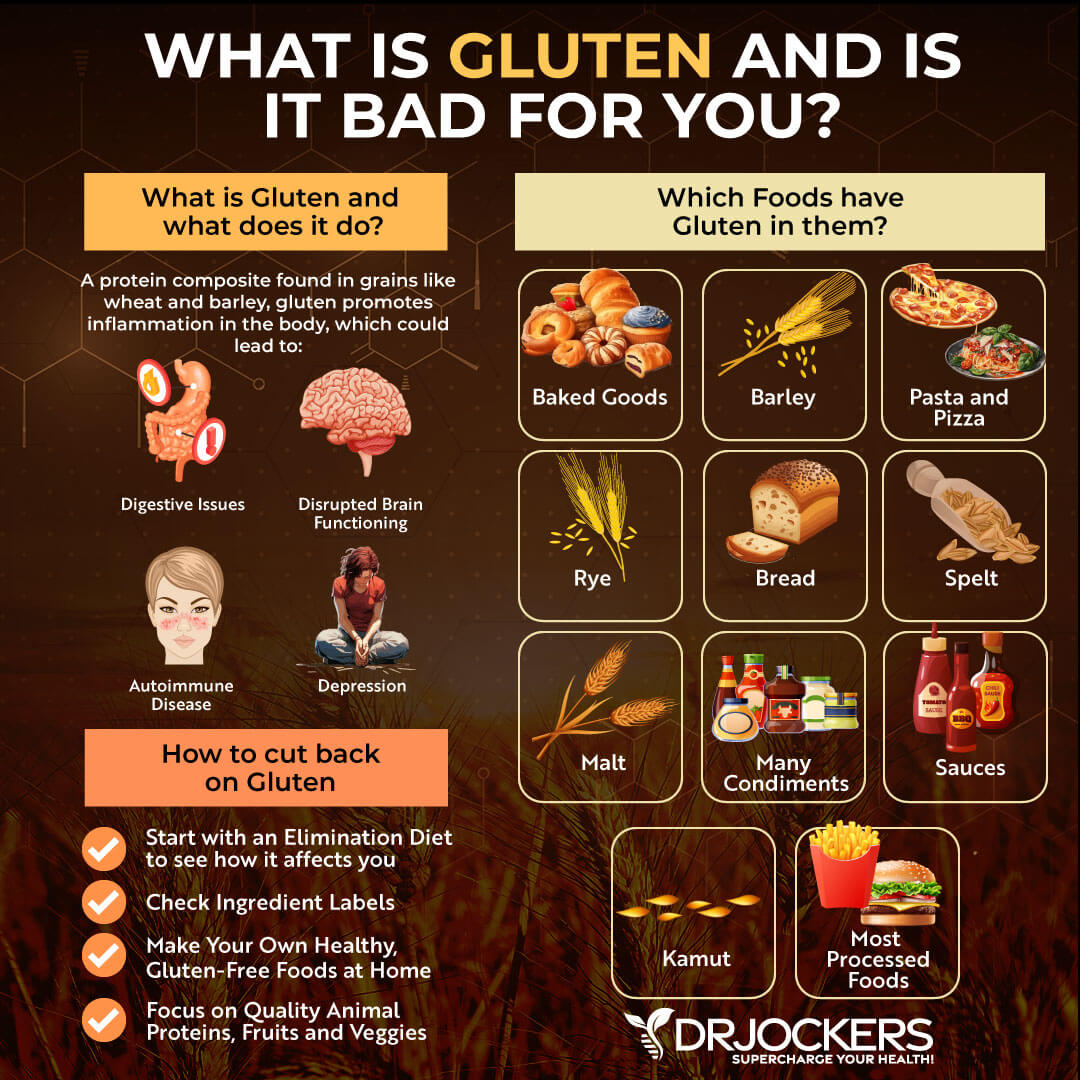
2. Gluten
Gluten is one of the most inflammatory foods you can consume. It damages the gut mucosa and creates holes in the tight junctions in the gut lining.
Gluten is a sticky protein found in grains such as wheat, rye, barley, and others. When we eat gluten, it is broken down into gliadin and glutenin. For people with gluten sensitivities, the GALT identifies gliadin as harmful and produces antibodies to attack it. This immune response creates inflammation throughout the body.
People with gluten sensitivities often experience digestive issues such as gas, bloating, indigestion, constipation, and other health issues. This article will give you more information on gluten and why it is so detrimental to our health.
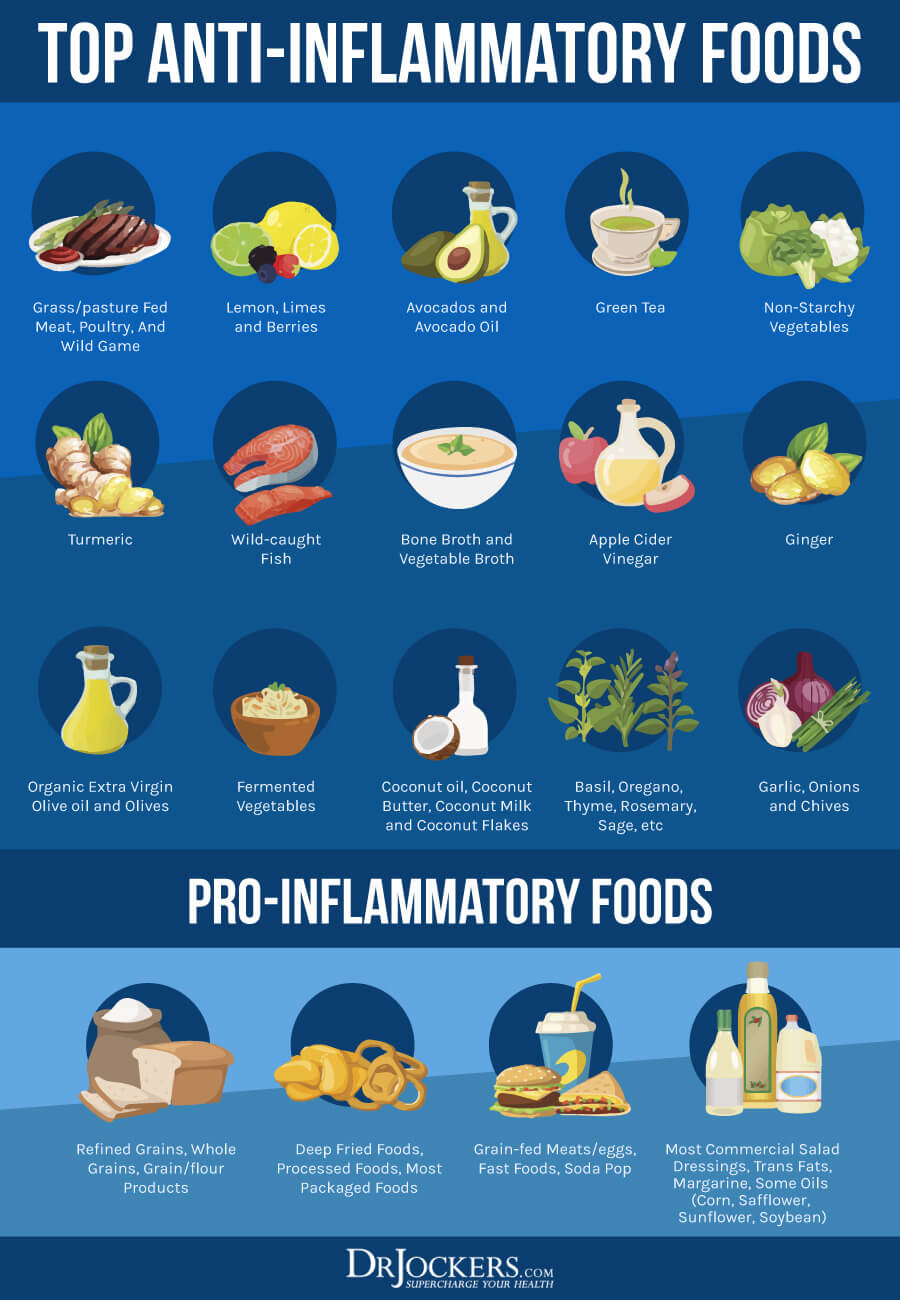
3. Poor Diet
One of the leading culprits that damage your gut mucosa is a poor diet. The foods we eat can either heal or harm our bodies.
Certain foods cause inflammation by triggering our immune system. Our immune system reacts to these foods with an excessive production of pro-inflammatory cytokines and a reduced production of anti-inflammatory cytokines (9).
Foods included in the Standard American Diet (SAD) diet are extremely inflammatory. The SAD diet relies heavily on refined sugars and starches, processed foods, and toxic fats such as trans-fats. This inflammatory diet is linked to a higher risk of cardiovascular disease, cancer, diabetes, and many other health conditions (10).
Many of the foods on the SAD diet contain high levels of advanced glycation end products (AGEs), or glycotoxins (11). AGEs are compounds that form within the body and also exist in foods. These compounds cause inflammation and oxidative stress, damaging the gut mucosa and tissue throughout the body.
4. Glyphosate
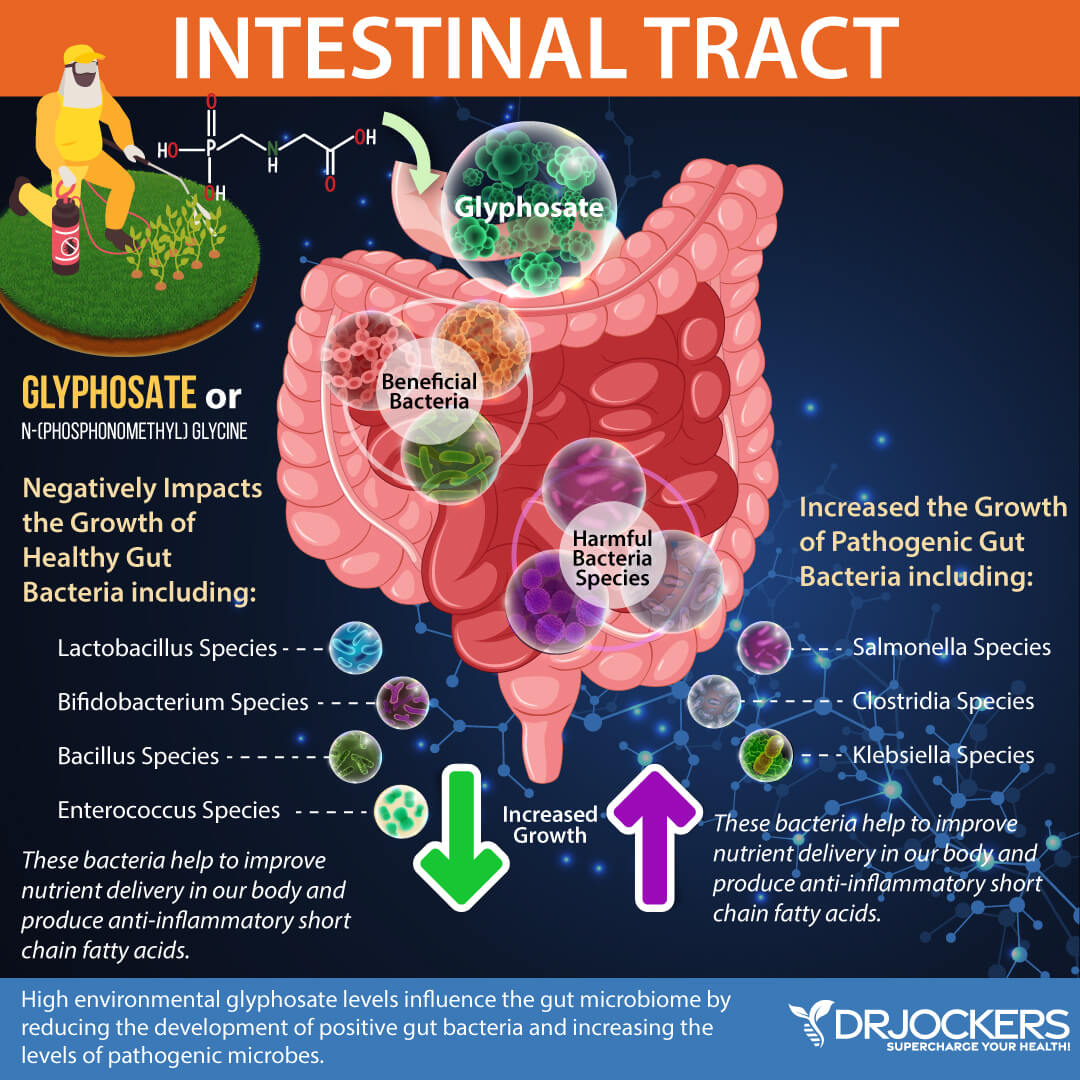
Glyphosate is an herbicide patented by Monsanto under the name “Roundup” (12). It has been approved since the 1970s as a weed killer to be applied to crops before and after planting and to control weeds in pastures and non-crop areas. Glyphosate is the most heavily applied herbicide in the world and often contaminates the water supply, precipitation, and air.
Monsanto genetically modified crops beginning in 1996 that are resistant to Roundup (“Roundup Ready”). Genetically modified foods (GMOs) along with grains, additives, vegetable oils, and many other foods contain glyphosate.
Glyphosate is extremely harmful to our health and has been linked to a number of health conditions, including cancer. Glyphosate damages the gut mucosa and kills beneficial gut bacteria, allowing for the overgrowth of pathogens. For more information on glyphosate and how to detox from this potent chemical, read this article.
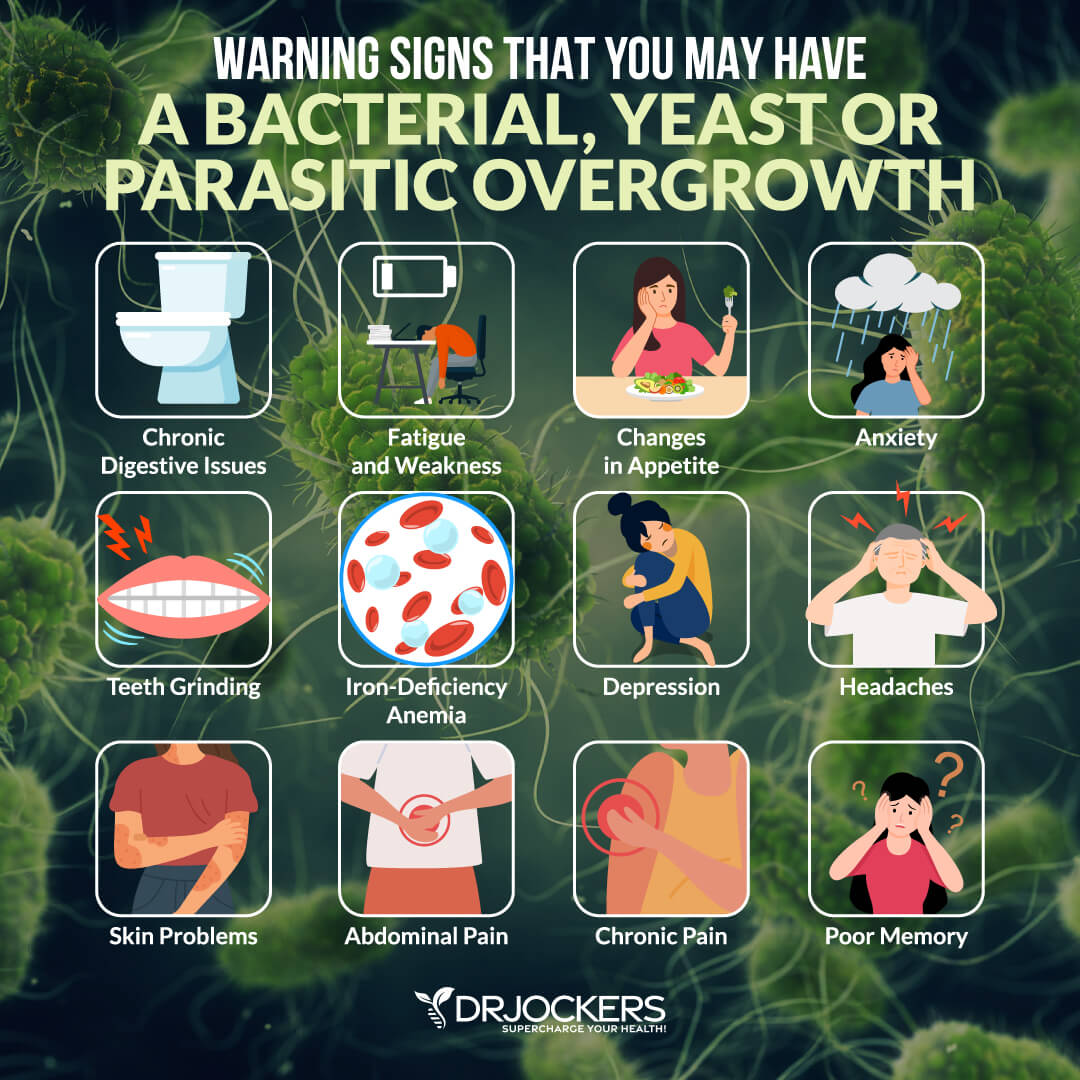
5. Gut Infections
The GI tract is a major entry point for pathogens. Gut infections result from a variety of pathogens such as bacteria, viruses, parasites, and fungi (13). Pathogens escape from our immune system by modulating, or regulating our immune response.
Infections can be present for many years, ranging from acute to chronic. Gut infections cause inflammation in our bodies and damage our gut mucosa.
6. Food Sensitivities
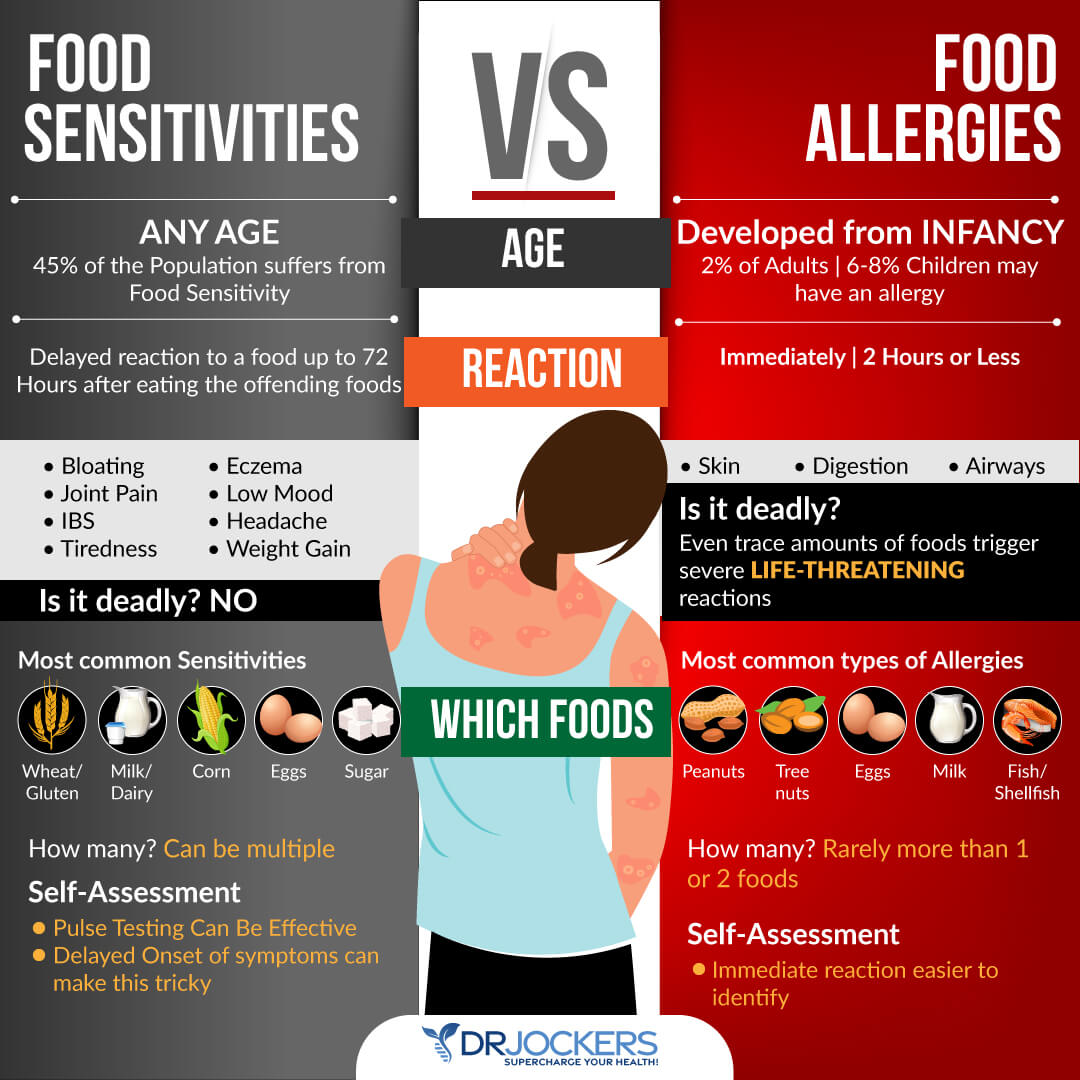
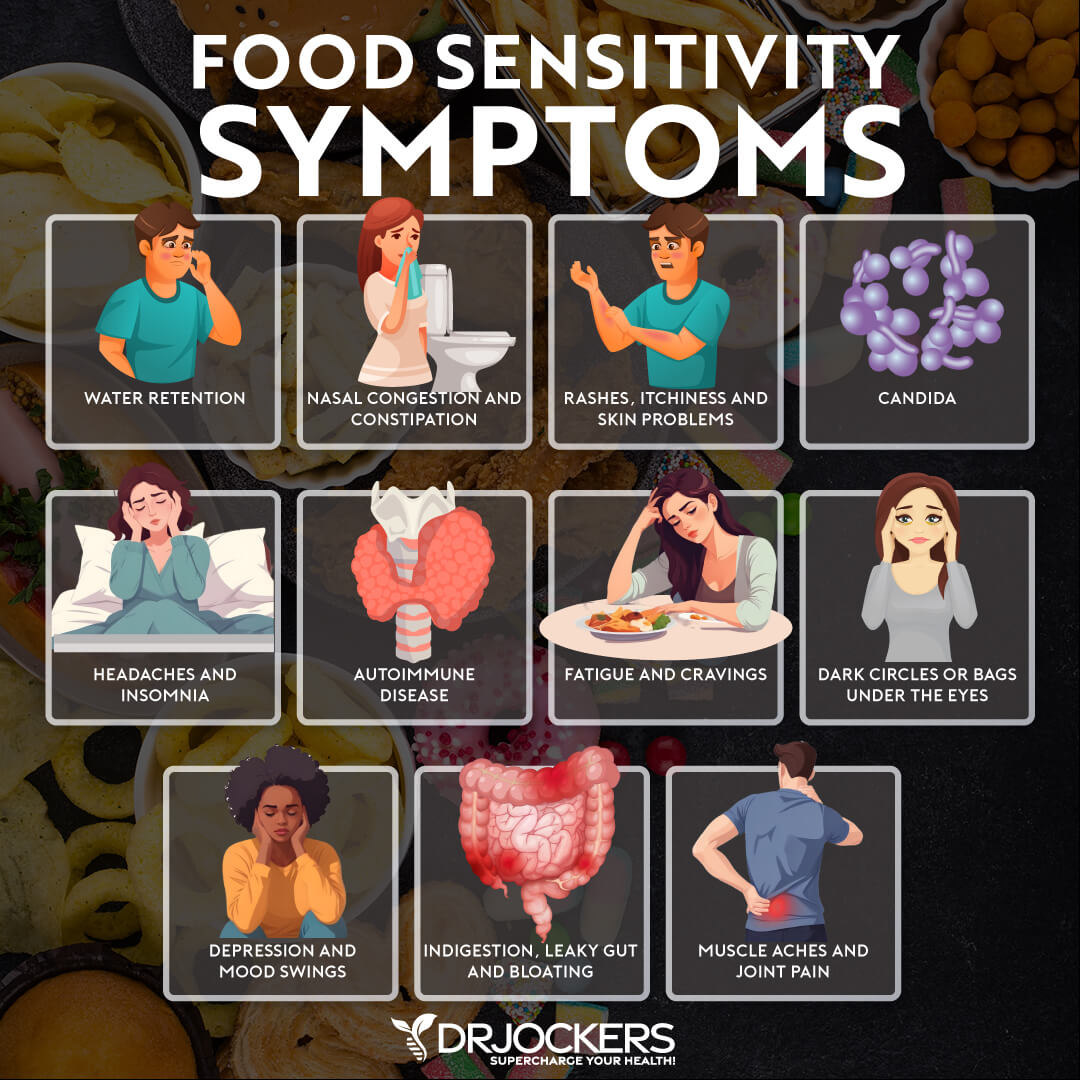
When you have food sensitivities, your body reacts to certain foods as a threat with an overactive immune response. Repeated exposure to problematic foods can damage the gut mucosa and result in chronic inflammation and other health problems. It is estimated that around 45% of individuals have food sensitivities.
When our gut lining is damaged, we can become sensitive to foods. Consuming these foods can make the gut more permeable and prevent the gut from healing and sealing. Food sensitivities inflame the gut lining, creating this cycle of gut permeability and more food sensitivities.
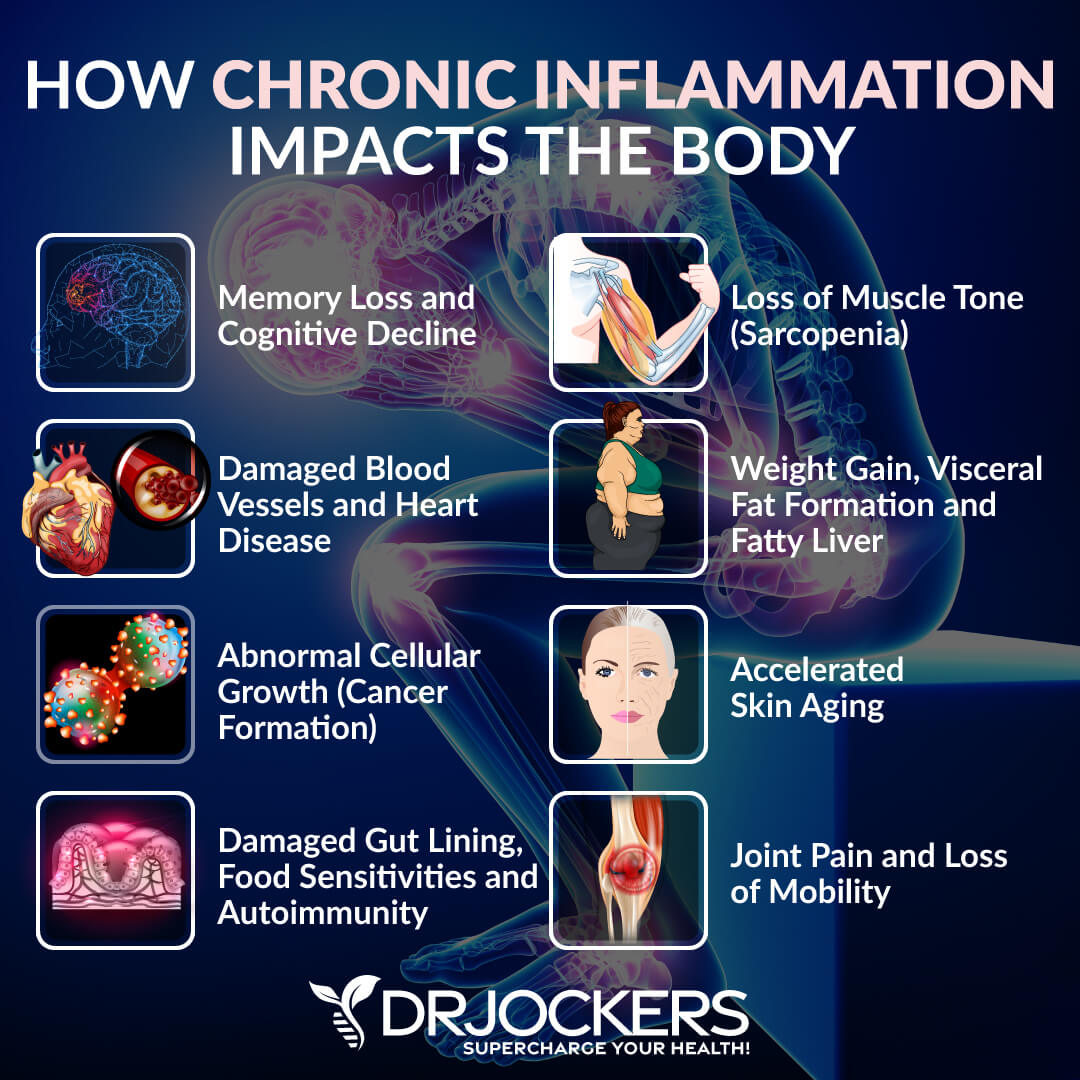
7. Chronic Inflammation
Inflammation is the body’s natural defense mechanism. It is your immune system’s response to cellular injury and involves the body’s white blood cells and the chemicals that they produce. Inflammation protects you from hostile microbes by eliminating toxic agents and repairing damaged tissue. In this way, inflammation is helpful.
Inflammation can be harmful when it is a low-grade, chronic inflammation. Chronic inflammation is systemic and can last for months or years. This inflammatory state is extremely detrimental to the gut mucosa and is associated with a wide range of health conditions.
Supporting the Gut Mucosa
1. Reduce Stress and Improve Sleep
Managing stress and getting adequate sleep is important for supporting the gut mucosa. Two of the most effective strategies to reduce stress and optimize sleep are implementing a healing diet and balancing your blood sugar levels.
Additional stress relieving techniques are grounding, deep breathing exercises, sunlight exposure, Epsom salt baths, and dry brushing. Supplementing with adaptogenic herbs, such as those in Cortisol Defense, may help your body resist and recover from everyday stress.
Strategies for better sleep are getting sunlight during the day, avoiding artificial light, blacking out your room with blackout curtains or using a sleep mask, and forming healthy sleep habits. It is important to turn off electronics, practice good hygiene, stretch, practice gratitude, journal, pray, and implement other healthy sleep habits. It is also important to be smart about caffeine intake by using it early in the day in small quantities and cycling on and off caffeine.
Magnesium is an important micronutrient that plays a critical role in stress and sleep. For additional sleep support, Brain Calm Magnesium may help the brain signal the body for sleep.

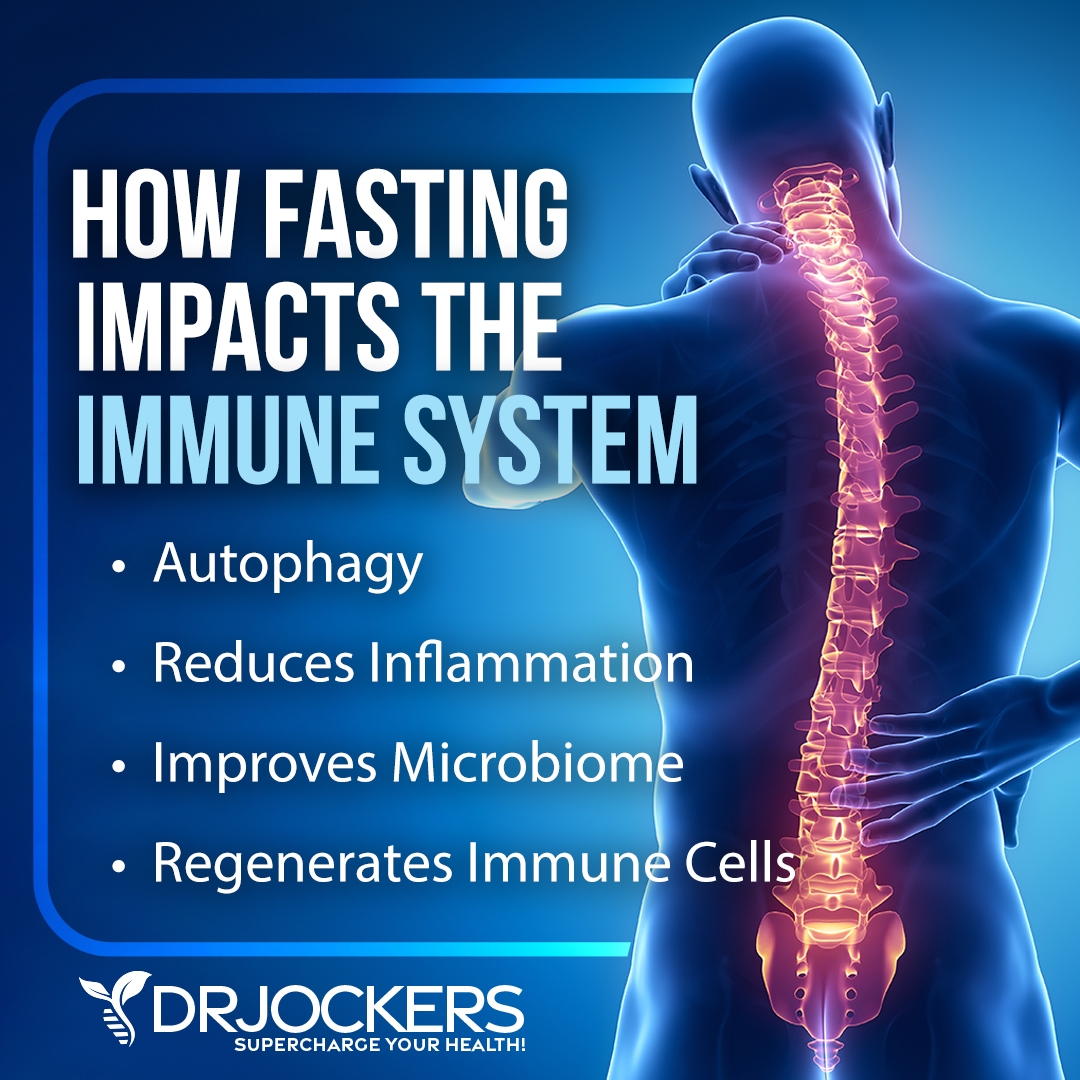
2. Fasting and Liquid Nutrition
Fasting and consuming liquid nutrition are fantastic strategies for supporting the gut mucosa. Digesting solid foods creates significant stress on the digestive system, irritates the gut lining, and leads to inflammatory processes.
When we fast or use liquid nutrition, our bodies can conserve the energy used in digesting, processing, and assimilating solid foods. Instead, the body can use this energy for healing and detoxification.
Intermittent Fasting
Intermittent fasting, or time-restricted eating, is eating foods within a certain window of time each day. It is divided into the building or feeding window when you consume food and the fasting or cleansing window when you are going without food. The best way to start fasting is by doing a simple fast, consuming only water for the 12 hours between dinner and breakfast.
Extended Fasting
Extended fasting is fasting for over 48 hours. There are greater benefits to extending the fast beyond intermittent fasting. With extended fasting, your body can heal and repair cells, tissues, and organs and a higher and deeper level. This is one of the most powerful healing tools you can utilize for a quick health transformation. For more information on extended fasting and how to break an extended fast, check out this article.
3. Anti-Inflammatory Diet
One of the best strategies for supporting the gut mucosa is to consume an anti-inflammatory diet. This healing diet removes foods that cause inflammation and damage the gut lining. It includes organic, non-GMO vegetables, fruits, healthy fats, and clean protein.
Foods to Avoid
The most important foods to avoid are refined sugars, processed foods, vegetable oils, meat and dairy from conventionally-raised animals, and farmed fish. These foods contain chemicals, trans-fats, and other toxic ingredients that are highly inflammatory, create extra acidity in the tissues, and damage the gut mucosa.
Foods to Include
An anti-inflammatory, gut-healing diet includes whole, unprocessed foods. This diet consists of clean protein, organic vegetables and fruits, and healthy fats. Clean protein sources are grass-fed meats, pasture-raised, organic chicken and eggs, and wild-caught fish.
Vegetables and fruits are high in anti-inflammatory antioxidants and phytonutrients which are great for gut and overall health. You should also include plenty of healing herbs.
Healthy fats are found in coconut, olives, avocados, and their oils and in grass-fed butter and ghee. These healthy fats are an efficient source of fuel to reduce inflammation and support the gut mucosa.
4. Eliminate Gut Infections
It is important to take steps to eliminate gut infections. Having an overgrowth of opportunistic bacteria, viruses, or parasites creates toxicity and inflammation. Reducing the microbial load in the gut is important for reestablishing a healthy microbial balance and strengthening the gut mucosa.
A fantastic supplement to include in an antimicrobial protocol is GI Clear. GI Clear is a blend of botanical extracts with antimicrobial properties. These herbs help to reduce pathogenic bacteria, yeast, and parasites which create infections in your gut.
5. Reduce Gut Mucosa Inflammation
There are numerous strategies you can incorporate to reduce gut inflammation. These strategies include intermittent fasting, liquid nutrition, and targeted supplementation. For more information on using fasting and liquid nutrition to heal leaky gut and effective supplements, read this article.
It is also critical to identify and remove food sensitivities to reduce gut inflammation. Food sensitivities can be hard to identify because symptoms of food sensitivities are usually delayed up to 72 hours after consuming the offending food.
The gold standard test for food sensitivities is the Cyrex Array 10-90X. This test is a multiple food and chemical immune reactivity screen using the ELISA method. There are 10 advanced technologies used in the Cyrex Array 10-90X. For information about different methods of testing for food sensitivities, check out this article.
Key Supplements to Support the Gut Mucosa
Here are the top 5 supplements that can improve the health of your gut mucosa and sIgA levels. The number one supplement I use to improve the immune tolerance of the gut is Mega Mucosa as that is the most specific supplement for this.
However, there are many other tools to improve the health of the gut mucosa including things like collagen, ashwagandha, L-glutamine, bioflavonoids, quercetin, probiotics, and herbs like turmeric and ginger. I would recommend bringing a few of these into your supplement protocol if you want to improve your gut health and immune system.
1. Mega Mucosa
A fantastic product for strengthening the gut mucosa is MegaMucosa. MegaMucosa helps to heal and seal a damaged gut lining. It is the first complete mucosal support supplement formulated to rebuild a healthy mucosal barrier.
MegaMucosa contains dairy-free immunoglobulins to support a healthy immune response in the mucosa and increase SIgA levels. It also contains four key amino acids and citrus polyphenols which support microbial diversity and alleviate barrier dysfunction.

2. Gut Healing Protein
My go-to product for anyone dealing with digestive issues or a leaky gut is Gut Healing Protein. This fabulous protein powder is a critical part of any gut-healing protocol. It provides high-quality hypoallergenic amino acids and powerful antioxidants to strengthen the gut mucosa and improve liver function.
Gut Healing Protein is a comprehensive dietary supplement that supports GI function and balanced detoxification. It contains bioflavonoids, ginger, turmeric, MSM, watercress, green tea extract, and a full methylated multivitamin and 26 grams of protein without any sugar or stevia.
3. Organic Bone Broth Collagen
One of the top supplements for supporting the gut mucosa is Bone Broth Collagen. The amino acids in collagen, including glycine and glutamine, are essential for healing the protective lining of the gastrointestinal tract. These amino acids seal the holes in the gut by healing damaged cells and building new tissue. Collagen also makes up the villi, small finger-like structures on the intestinal wall, and assists with water absorption in the intestines.
In addition to healing and strengthening the gut mucosa, collagen has many other health benefits. Organic Bone Broth Collagen is certified organic and has 13 grams of whole-food collagen protein from real bone broth. It also contains ashwagandha to support the stress response.
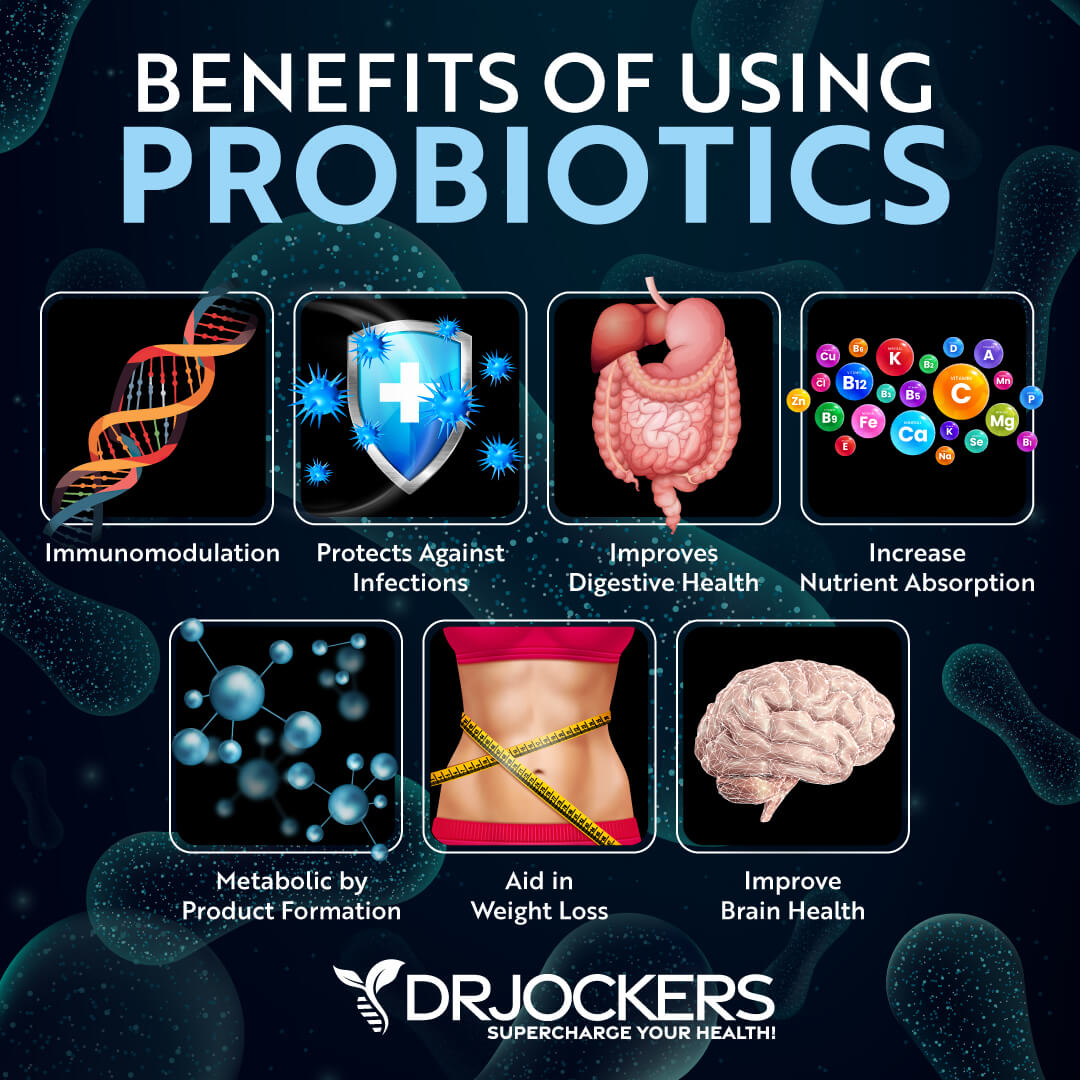
4. Probiotics
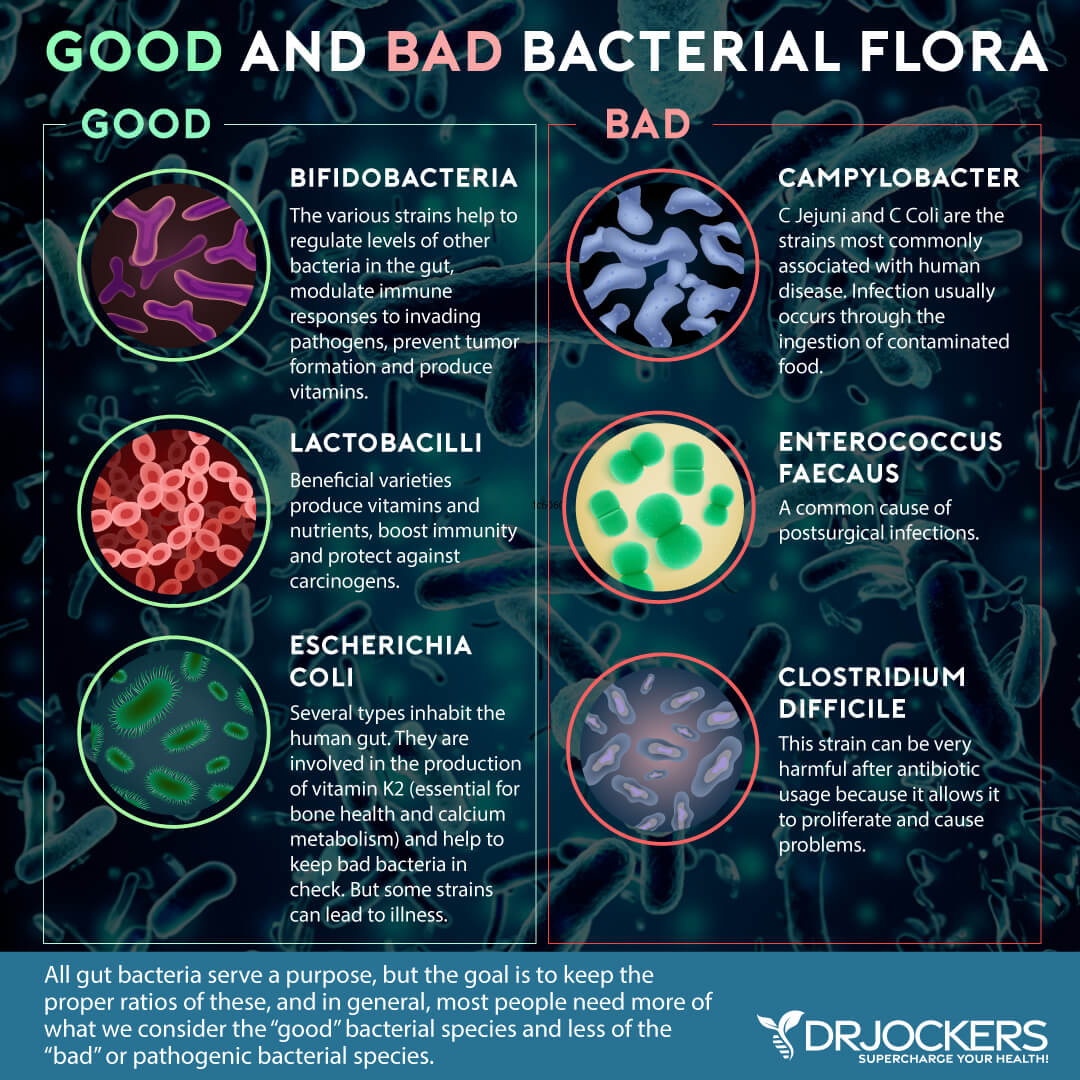
Probiotics are beneficial microorganisms (bacteria and yeasts) that keep your gut and body healthy. They are similar to the microorganisms that naturally live in our bodies.
Probiotics support the gut mucosa in many ways:
- Probiotics act as a physical barrier to incoming pathogens by lining the digestive tract.
- Probiotics enhance mucous production to protect against invasive bacteria.
- Probiotics stimulate the production of antimicrobial compounds – they cause the mucosal immune system to secrete protective immunoglobulins such as secretory IgA and protective defensins and bacteriocins into the lumen; and,
- Probiotics make the mucosal immune system more anti-inflammatory (14).
There are 4 main categories of probiotics: food-based, spore-forming soil-based, probiotic yeast, and combination probiotics. If you are struggling with digestive issues, a good strategy is to try one probiotic from each category for a short time to determine which is most beneficial. You should also rotate probiotics to keep the microbiome adapting. For information on the benefits and categories of probiotics along with suggested protocols, read this article.
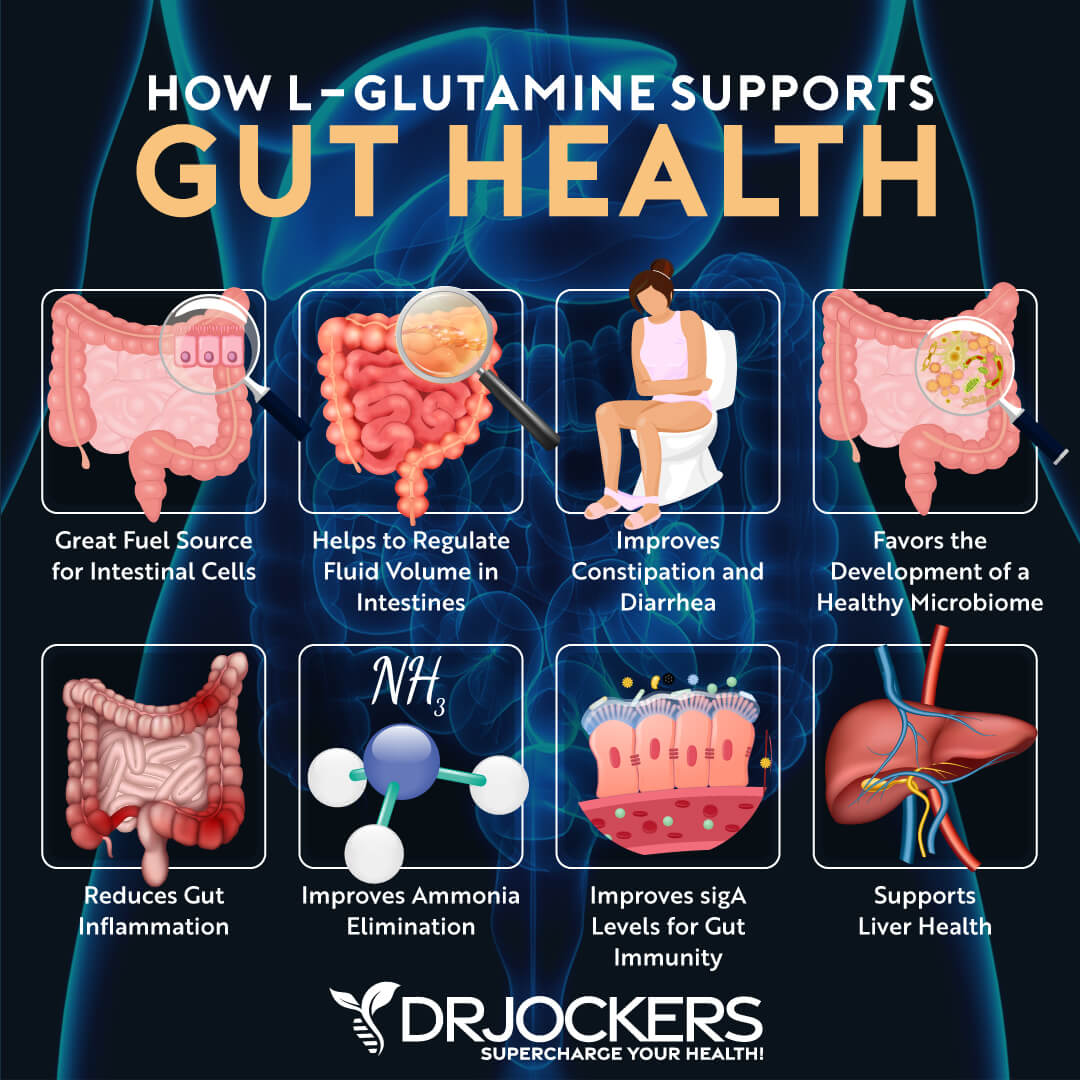
5. L-Glutamine
Glutamine is an amino acid that plays a vital role in many bodily functions including gut, immune, and many other functions in the body. Glutamine is the primary source of amino acids for the gut mucosa.
Glutamine has been shown to improve intestinal barrier function and a lack of glutamine can increase permeability (5). Supplementing with L-Glutamine can help to heal intestinal permeability, improve digestion and nutrient absorption, regulate bowel motility, and improve the balance of your gut microflora.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!







My daughter has a rhuematoid factor blood test for IgA greater than 500. Does this mean her IgA in her gut is too much or too little causing her arthritis? Thank you
Hi Laurie, I am sorry to hear that your daughter is struggling with this! I would highly recommend that you consult with a functional health practitioner who can look at all of her lab results to interpret and create a customized plan for reducing inflammation!
Can your products be given to an 18mth old child with leaky gut/food allergies/eczema?
Hello Debra, this is a great question, we do have some products from BioRay that are specifically formulated for children. This is a key one here that we use with young children https://store.drjockers.com/products/ndf-belly-balance
My daughter is 11 years old and has selective IgA deficiency. What product(s) can she use (that are ok for children)
Sorry to hear this Jennifer, I would highly recommend she get started on the Gut Defense here: https://store.drjockers.com/products/mega-igg2000
Have her take 1 scoop – 2x daily. Also, have her take the Mega IgG: 2 caps – 2x daily: https://store.drjockers.com/products/mega-igg2000
Dr. Jockers can you provide testimonials of people that have healed the subject matter of your blog post?
I have yet find one testimonial from someone who has achieved success that relates to your blog post .
I’ve been working hard getting low secretory IGA back again using colostrum and all of the supplements mentioned above. I’ve worked with a couple different natural path. I see no improvement. The testimonials that I do find from the naturopath team are very vague they don’t specify what the person was challenged with and what they did to get better. Thank you