 Lichen Planus: Symptoms, Causes & Support Strategies
Lichen Planus: Symptoms, Causes & Support Strategies
Lichen planus is an inflammatory autoimmune skin condition that can affect your mouth, genital regions, nails, scalp, and other areas. It can cause thin, white, and shiny skin, blisters, scabbing, redness, pain, itching, or discomfort. While there is no cure for lichen planus, you can reduce flare-ups and symptoms with the help of natural support strategies.
In this article, you will learn what lichen planus is. You will learn the four main types of lichen planus and what areas they may affect. You will understand its symptoms and main causes. I will go over conventional treatment methods. I will share my top natural support strategies and recommendations for lichen planus.
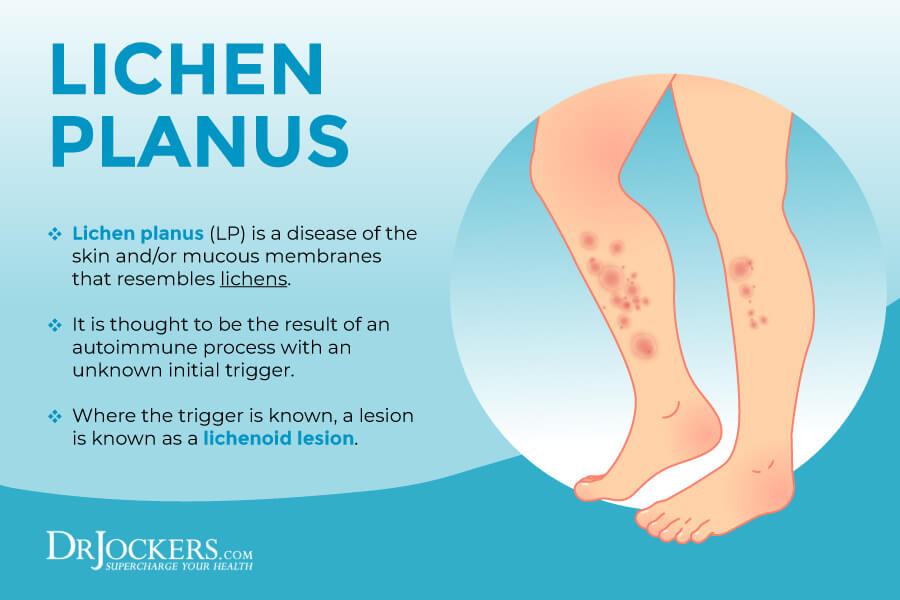
What Is Lichen Planus
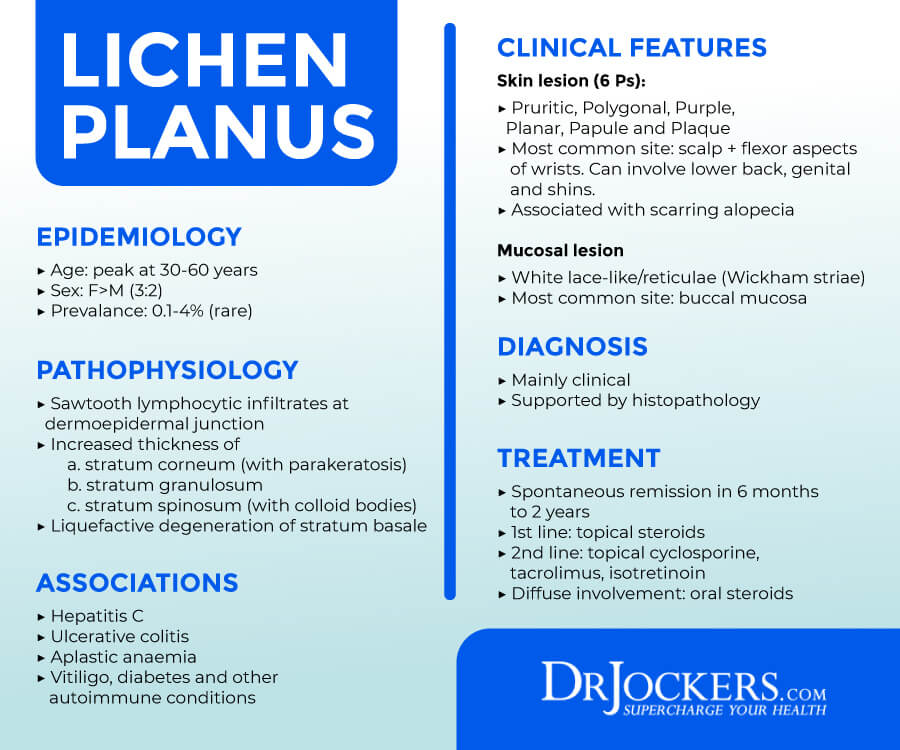
Lichen planus is an inflammatory skin condition that affects the skin or mucous membranes. According to a 2014 comprehensive review published in the Scientific World Journal, lichen planus is a T-cell mediated autoimmune disease with a chronic pattern (1). Lichen planus is also referred to as lichen sclerosus with a slight variation in that lichen planus more commonly affects the mucous membrane of the mouth and vagina as opposed to lichen sclerosus.
It usually appears in the genital or anal areas of your body but can affect any other region. It is the most common on the vulvas of women. Lichen planus is characterized by shiny white skin that’s thinner than normal. It may bruise or blister and in some cases may cause pain, itching, or discomfort.
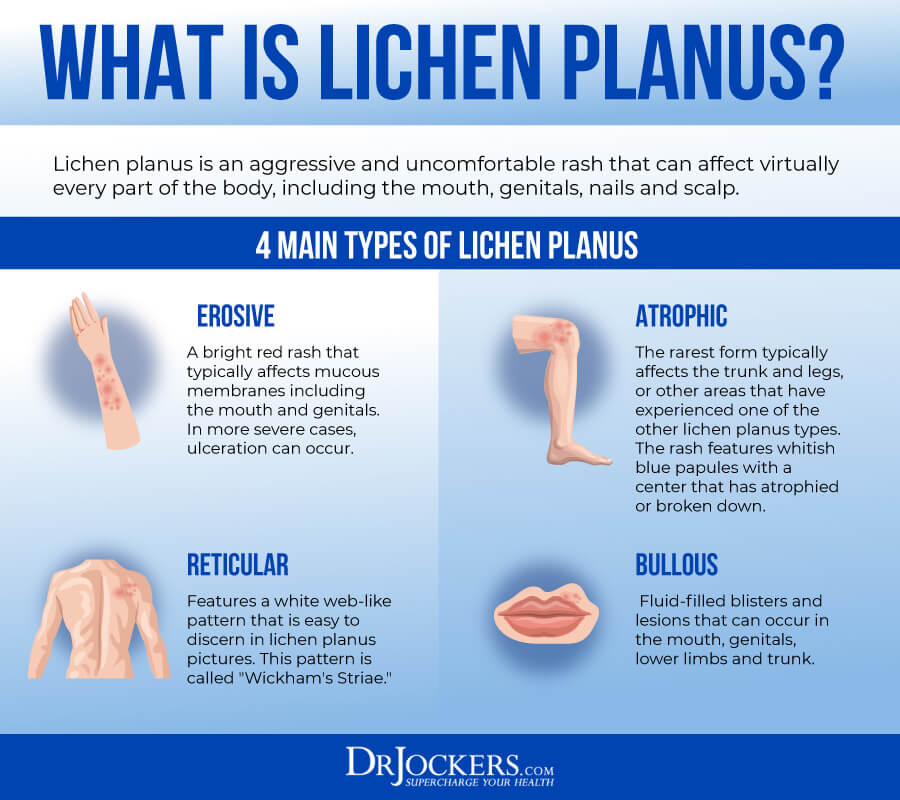
4 Main Types of Lichen Planus
There are 4 main types of lichen planus, including:
- Reticular: This type of lichen planus is characterized by a white web-like pattern also called “Wickham’s Striae”.
- Erosive: This form is a bright red rash that may cause ulceration and can appear on the mucous membranes of the genitals and mouth.
- Bullous: This form of lichen planus is characterized by fluid-filled blisters and lesions in the genitals, mouth, scalp, lower limbs, or trunk.
- Atrophic: This type of lichen planus is characterized by a rash with whitish-blue papules with an atrophied or broken down center on the legs or trunk. It may also affect other areas where previous outbreaks have occurred (2).
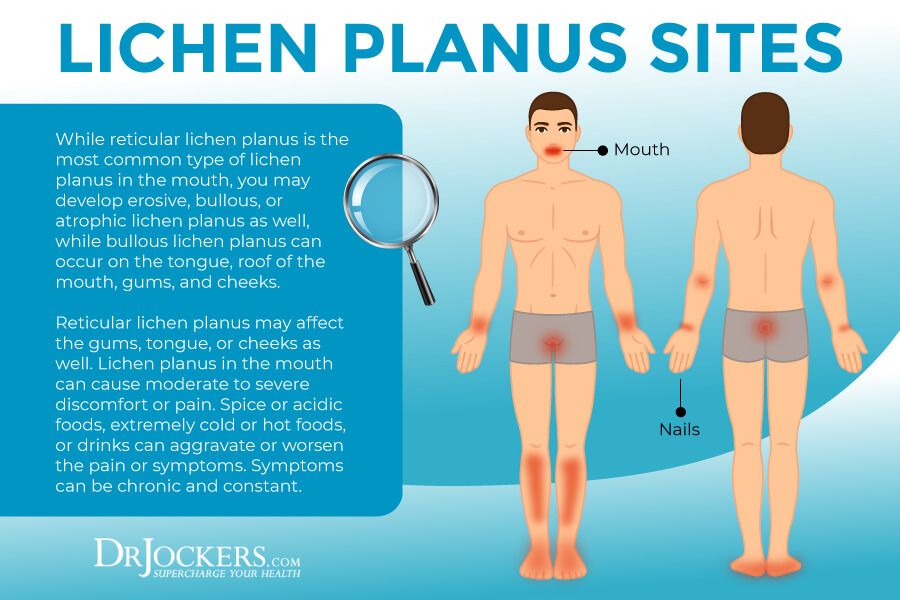
Regions Impacted by Lichen Planus
Lichen planus can affect a variety of areas of your body, including your mouth, genital regions, skin, and scalp.
Oral
While reticular lichen planus is the most common type of lichen planus in the mouth, you may develop erosive, bullous, or atrophic lichen planus as well, while bullous lichen planus can occur on the tongue, roof of the mouth, gums, and cheeks.
Reticular lichen planus may affect the gums, tongue, or cheeks as well, Lichen planus in the mouth can cause moderate to severe discomfort or pain. Spice or acidic foods, extremely cold or hot foods, or drinks can aggravate or worsen the pain or symptoms. Symptoms can be chronic and constant.
Genital
Lichen planus can commonly occur in and around the genitals, including the glands or shaft of the penis, vulva, or vaginas. Even though it’s common for people with oral lichen planus to have symptoms in the genital region as well, a large number of cases go undiagnosed.
Nails & Scalp
Lichen planus may also occur on your fingernails, toenails, or scalp. For some people, it may only affect one or two nails, while for others it may affect many or all. It may lead to temporary or permanent nail damage. Lichen planus on the scalp can cause hair loss or alopecia (3).
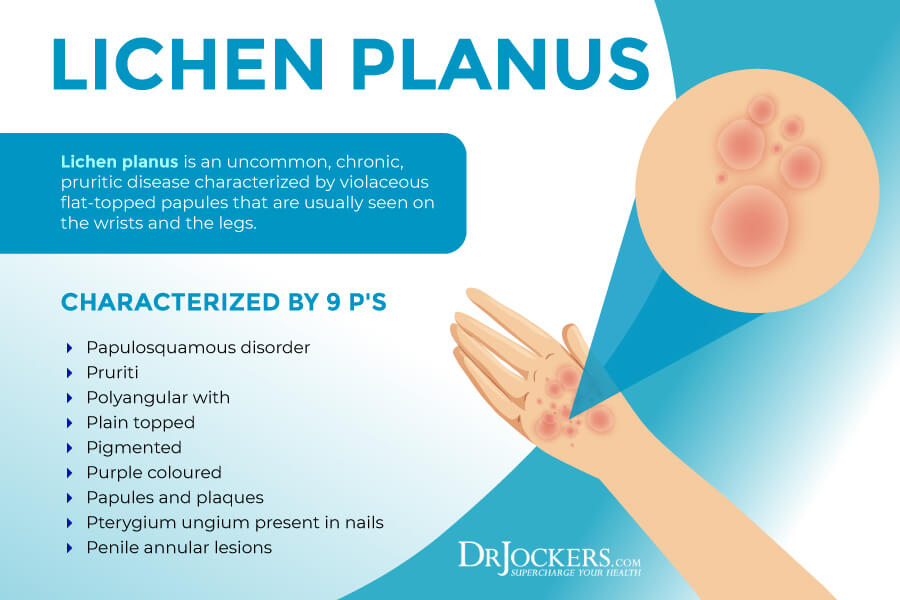
Signs & Symptoms of Lichen Planus
Lichen planus is usually distinguished and diagnoses by the six “Ps” that describe the shape and characteristics of lichen planus:
- Planar (flat-topped)
- Polyvagal
- Papules
- Plaques
- Purple
- Pruritic
Other signs and symptoms may include:
- Purplish-colored bumps or lesions
- Whitish-blue, fluid-filled blisters or lesions that burst open and scab over
- White web-like lines over red rashes or lesions
- Itching
- Wickham’s Striae in the mouth that causes burning and changes in taste
- White chalky nails with grooving, ridges, and splitting
- Rashes, itching, and pain on the scalp
- Vaginal discharge, burning, itching, or painful intercourse
- Lesions or blisters on the penis, itching, or painful intercourse
- An odd smell from the rash, even after cleaning it
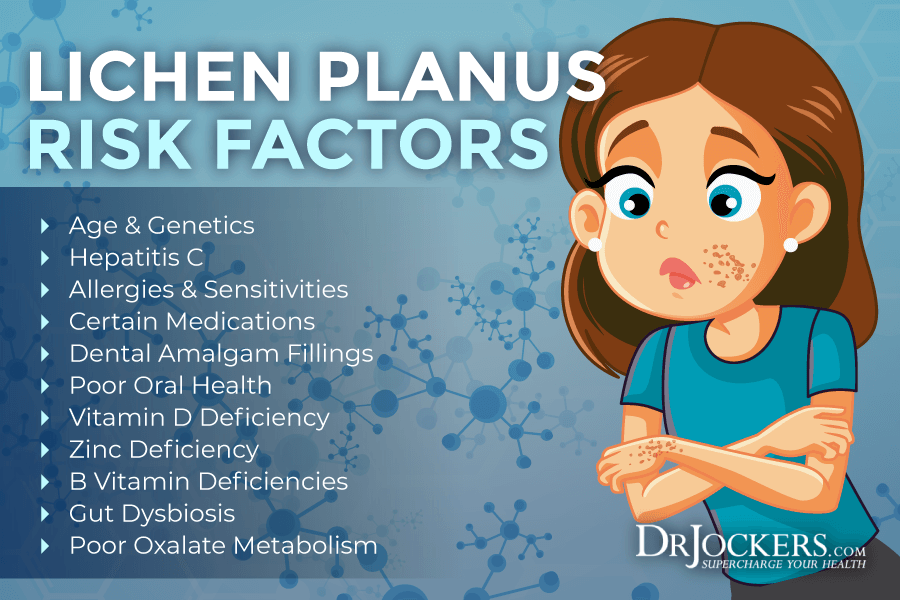
Lichen Planus Risk Factors
While there isn’t a single known cause of lichen planus, there are a variety of risk factors that may be involved in the development of the disease:
Age & Genetics
Lichen planus may affect any age group, however, according to a 2014 comprehensive review published in the Scientific World Journal, it is the most common among middle-aged adults (1). Women are slightly more common with roughly 3 women affected for every 2 men. Genetics may also play a role in the development of lichen planus. If you have immediate family members with lichen planus, it increases your risk of developing it as well.
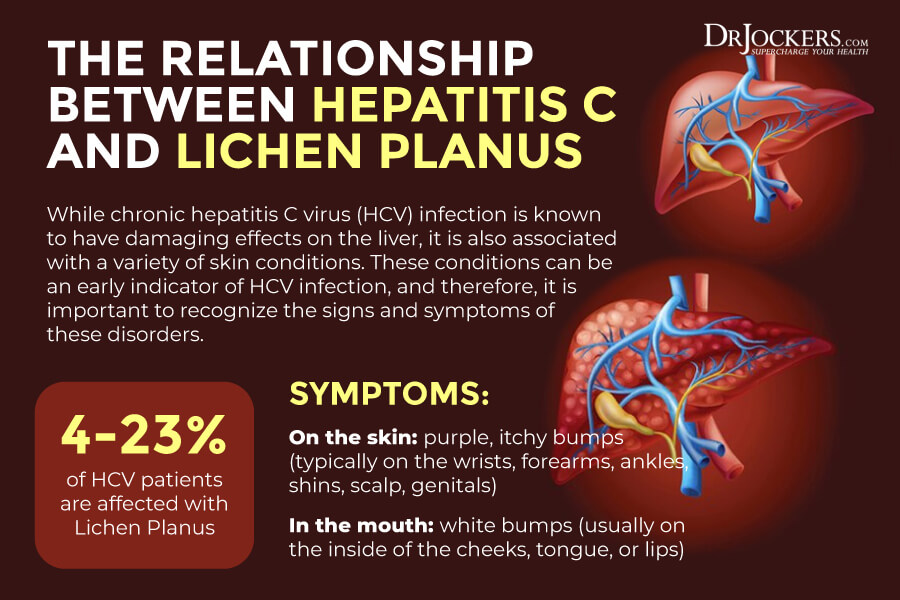
Hepatitis C
According to a 2009 meta-analysis published in the Archives of Dermatology, the hepatitis C infection is strongly associated with lichen planus (4). The meta-analysis examined 63 articles entailing 7 studies of various geographic regions.
Results suggest that the existence of the hepatitis C viral infection may indicate lichen planus while having lichen planus may also indicate a hepatitis C infection. Experts have found that roughly 4-23% of Hep C infected individuals also struggle with lichen planus.
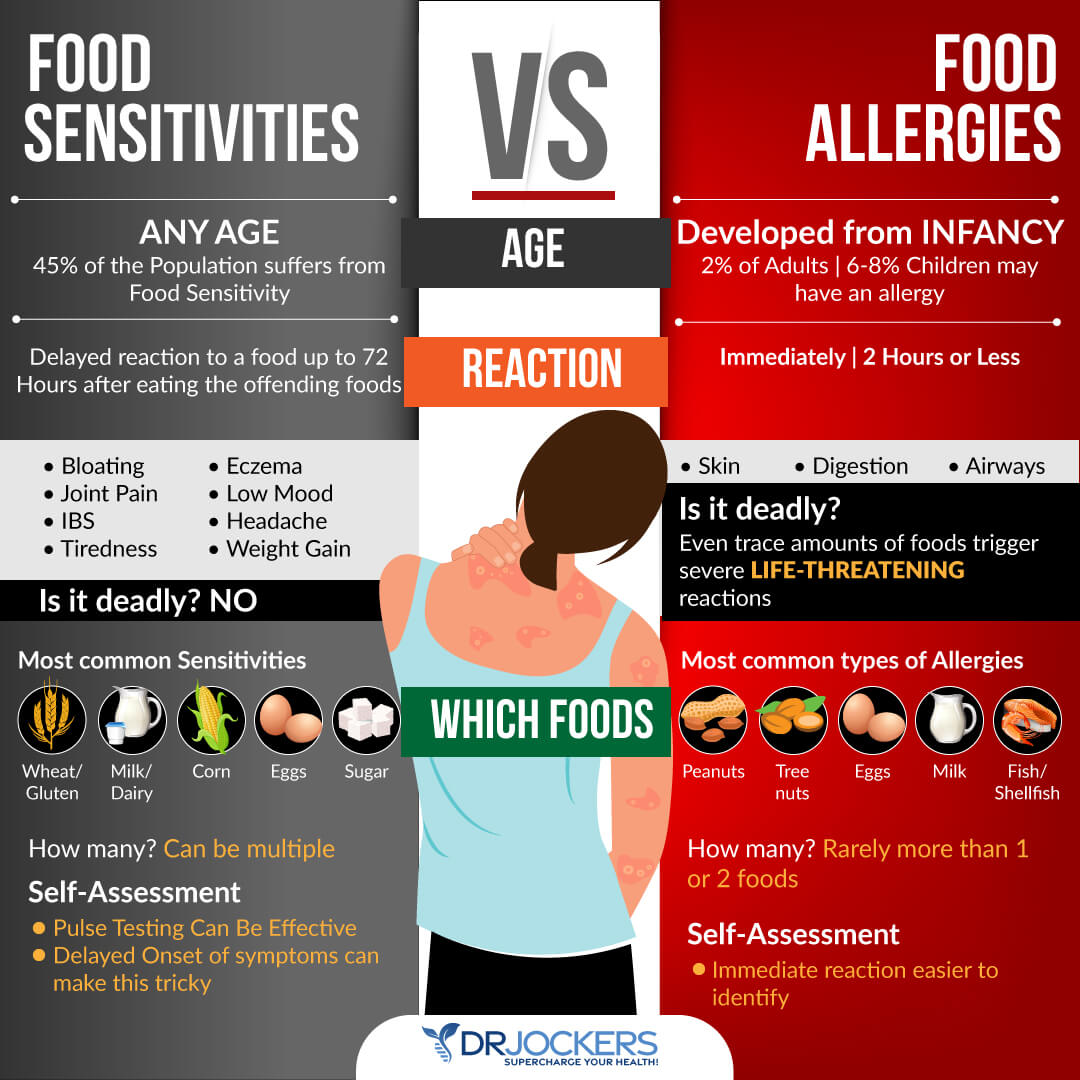
Allergens & Sensitivities
Allergies and sensitivities may also play a role in lichen planus. This includes both environmental allergens to things like pollen, weeds and mold as well as food allergies and sensitivities.
A 2010 study published in the Journal of the Royal Society of Medicine – Short Reports has found an association between lichen planus in the genital region and gluten sensitivity (5). Other common food sensitivities that may contribute to inflammatory and autoimmune conditions like lichen planus include sugar, dairy, eggs, nuts, soy, and legumes.
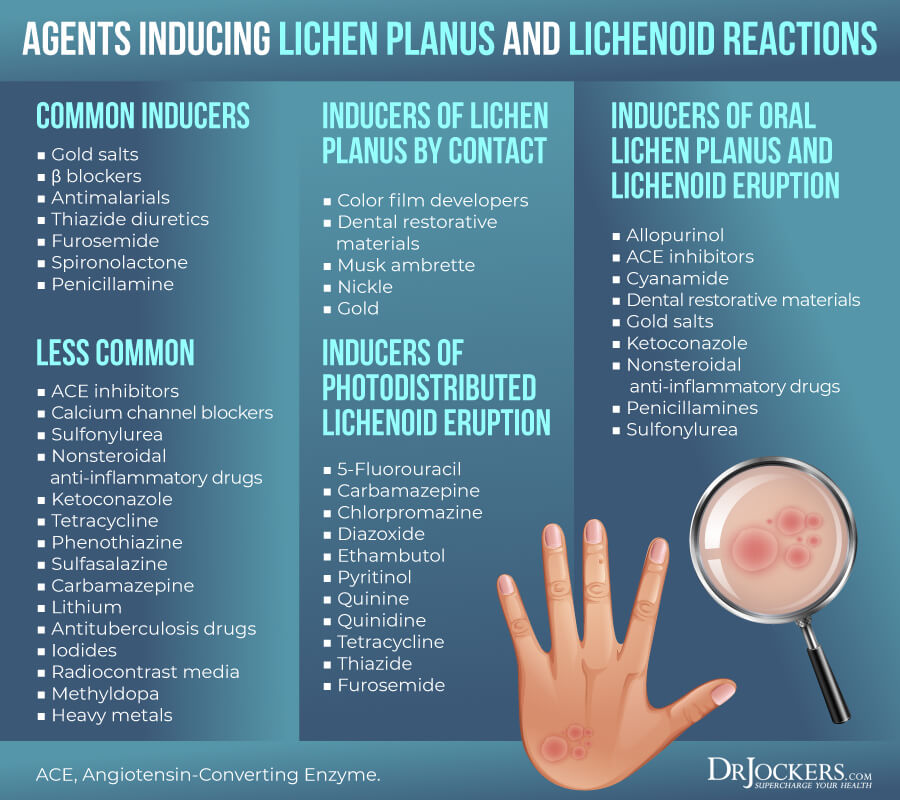
Medications
Certain medications may also increase your risk of lichen planus. Medications that may trigger symptoms are called lichenoid drugs.
Medications that may trigger the disease and symptoms include drugs that contain arsenic, bismuth, gold, or quinidine, including antibiotics, diuretics, malaria drugs, diabetes medications, high blood pressure medications, and medications for heart disease.
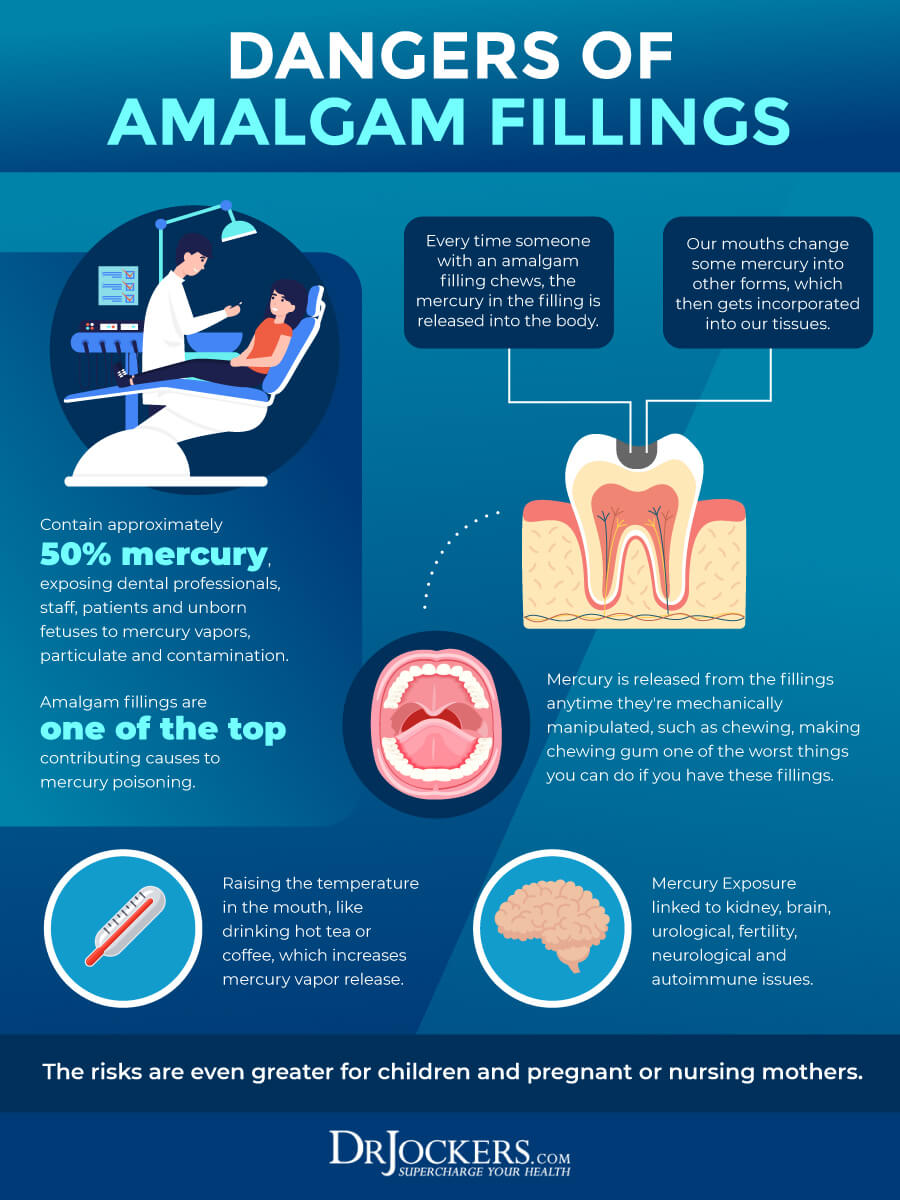
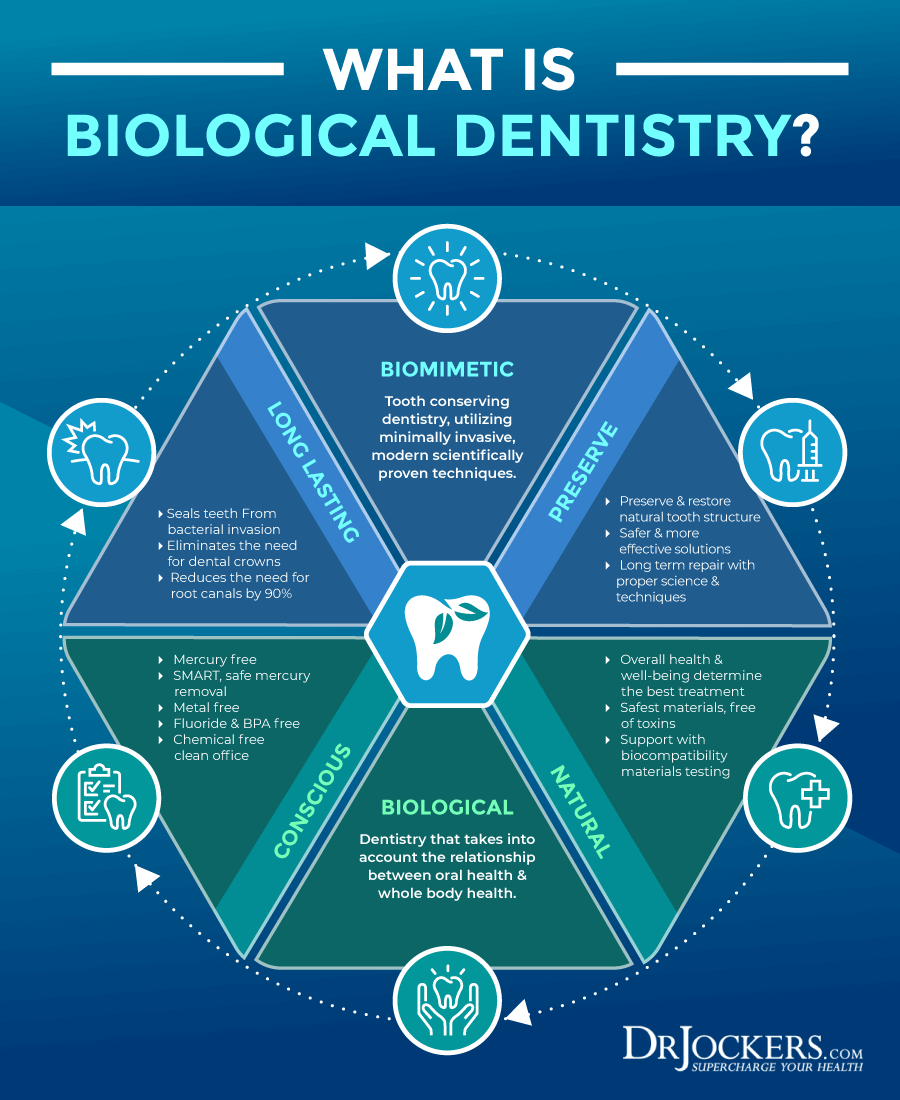
Dental Amalgam Fillings
Dental amalgam fillings are very toxic to the body and can lead to a variety of health issues. While they are used increasingly less today, they were very common in the past and many people walk around with old amalgam fillings in their mouth.
Root canals and amalgam used for root canals can also be incredibly harmful to your health. According to a 2012 review published in the Journal of Biomedicine and Biotechnology, amalgam fillings include mercury that may lead to lesions associated with lichen planus (6).
Poor Oral Health
Since one of the most common areas you may develop lichen planus, oral health is particularly important. Bacteria and yeast overgrowth can lead to a variety of health issues.
According to a 2020 study published in BMC Microbiology, a poor oral microbiome can play an important role in the development of diseases in the mouth (7). The study has found an association between oral dysbiosis and the development of oral lichen planus. Root canals can be a source of chronic oral infections that can trigger autoimmune conditions. Read about the issue with root canals in this article.

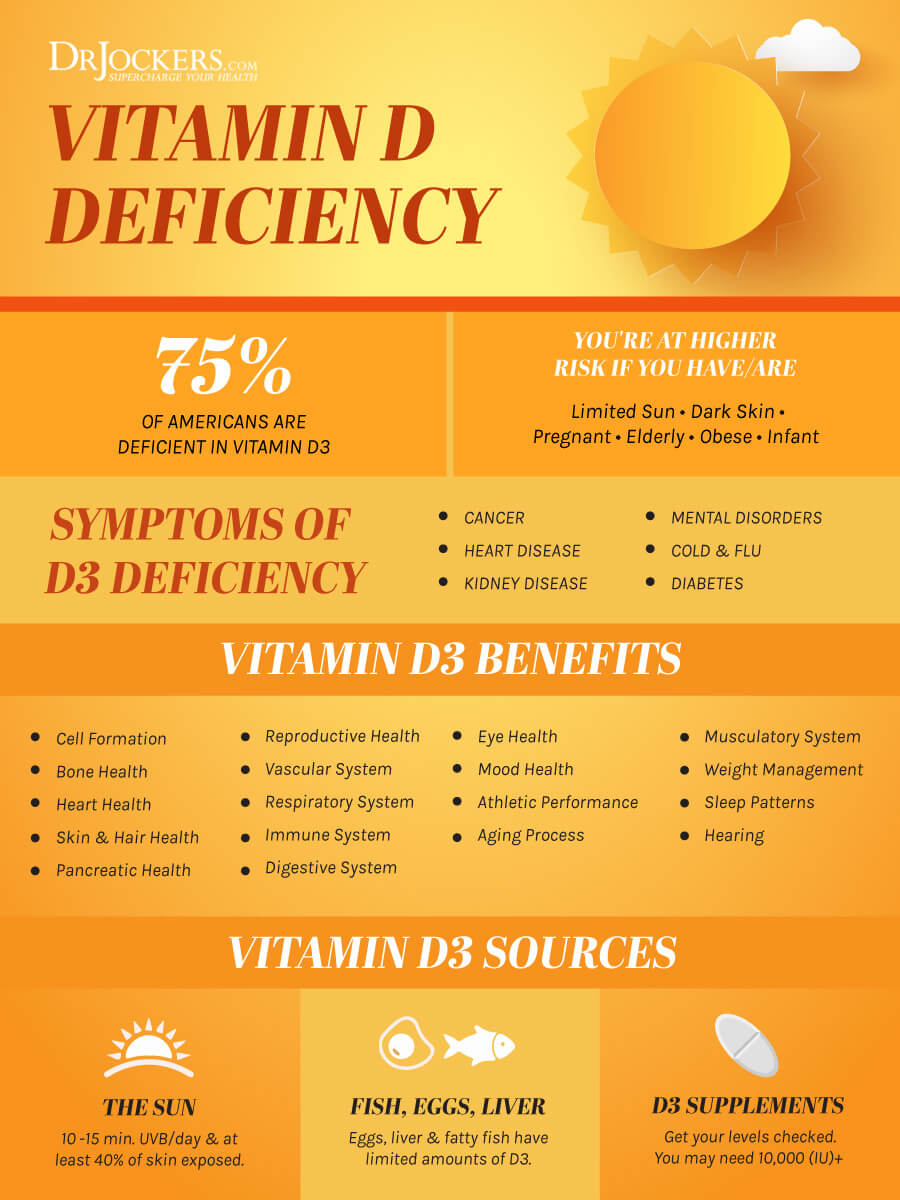
Vitamin D Deficiency
As a 2011 article published in the Journal of Investigative Medicine, vitamin D can modulate T cell immune responses and deficiencies have been associated with autoimmune disorders (8). A 2018 study published in the Turkije Klinikleri Journal of Dermatology has found that vitamin D levels were significantly lower in patients with lichen planus than in those without (9).
A 2018 study has found downregulation of expression of the vitamin D receptor in oral lichen planus (17). The study has also demonstrated that lipopolysaccharide (LPS) is responsible for this downregulation. A 2020 study published in BMC Oral Health has also found that vitamin D receptor genetic polymorphisms and lower vitamin D levels may be linked to oral lichen planus susceptibility (10).
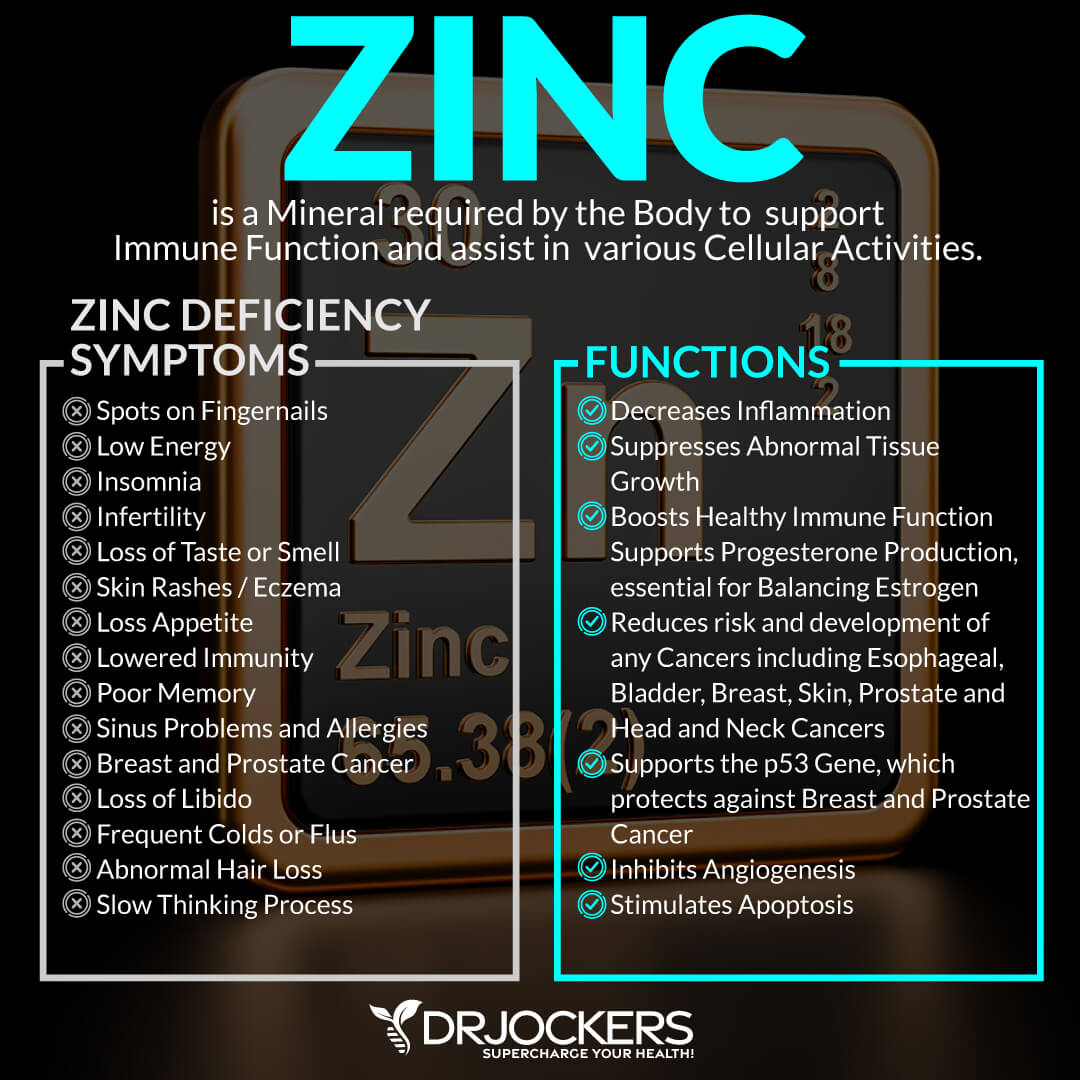
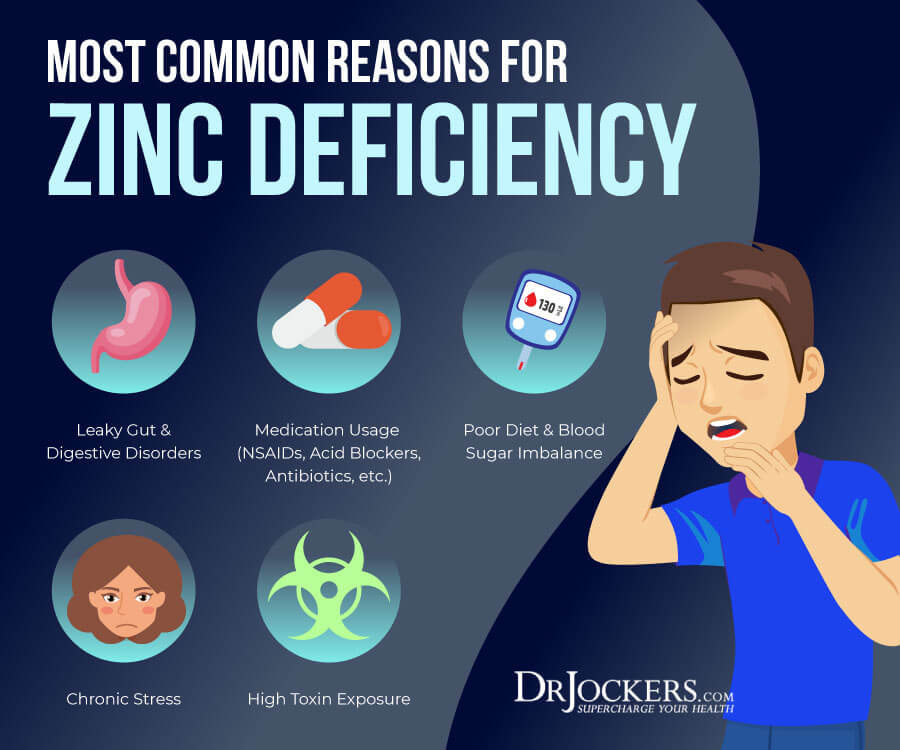
Zinc Deficiency
According to a 2017 article published in Nutrients, zinc is a gatekeeper to your immune system (11). It has anti-inflammatory and antioxidant benefits and is essential for homeostasis in the body. Deficiencies can impact your immune function. A 2008 study published in Molecular Medicine has found that zinc deficiency can impact the growth and function of T and B cells and T cell immunity (12).
A 2016 study published in Medicina Oral, Patologica Oral Y Ciruga Bucal has found that zinc deficiency is common in oral mucosal diseases, including oral lichen planus (13). A 2014 study published in the Journal of Dentistry – Shiraz University of Medical Sciences has also found lower zinc serum levels in the group with oral lichen planus than in the control group (14).
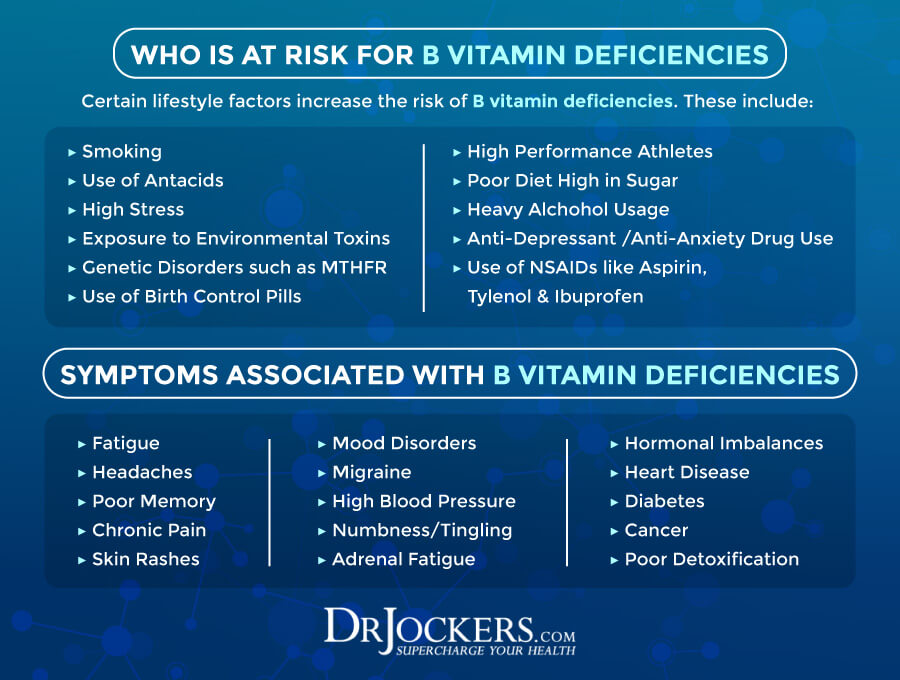
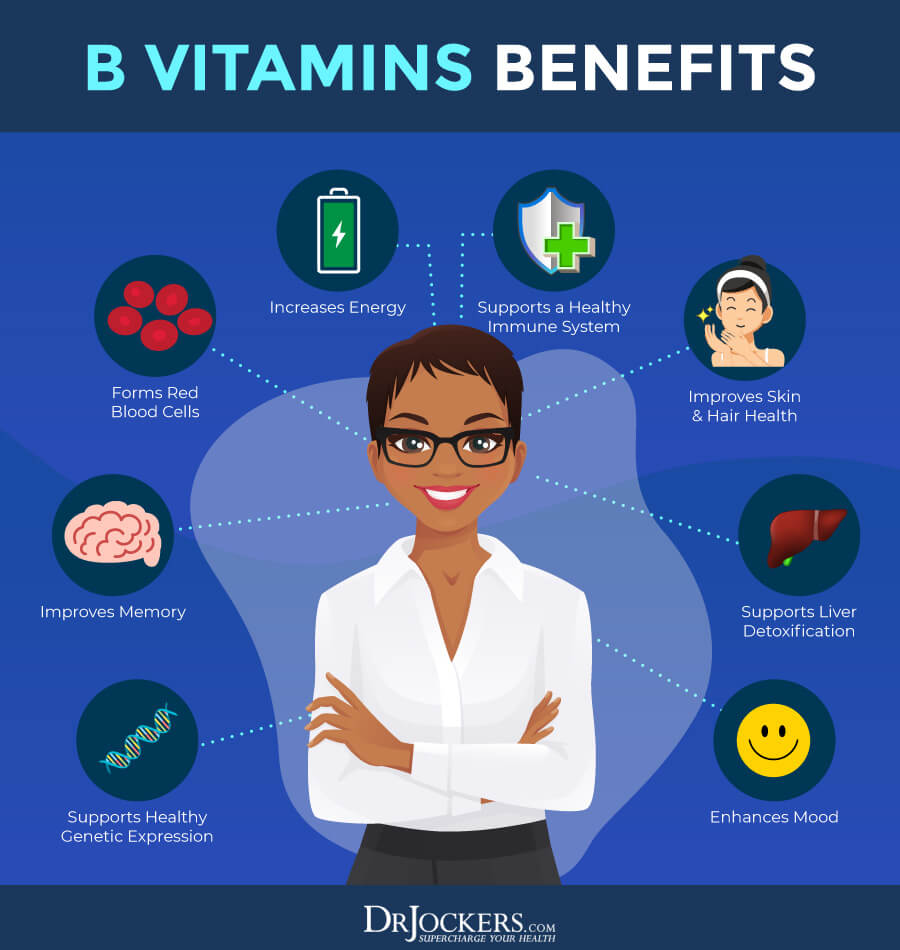
B Vitamin Deficiencies
B vitamins are also essential for your immune and overall health. A 2015 study published in the Journal of Formosan Medicinal Association has found a strong connection between low B12 and low folate levels and oral lichen planus (15).
It has also found a link between low iron and hemoglobin and high homocysteine levels and oral lichen planus. A 2020 cross-sectional study published in the Journal of Oral, Biological, and Craniofacial Research has found reduced levels of vitamin B12 in symptomatic oral lichen planus (16).
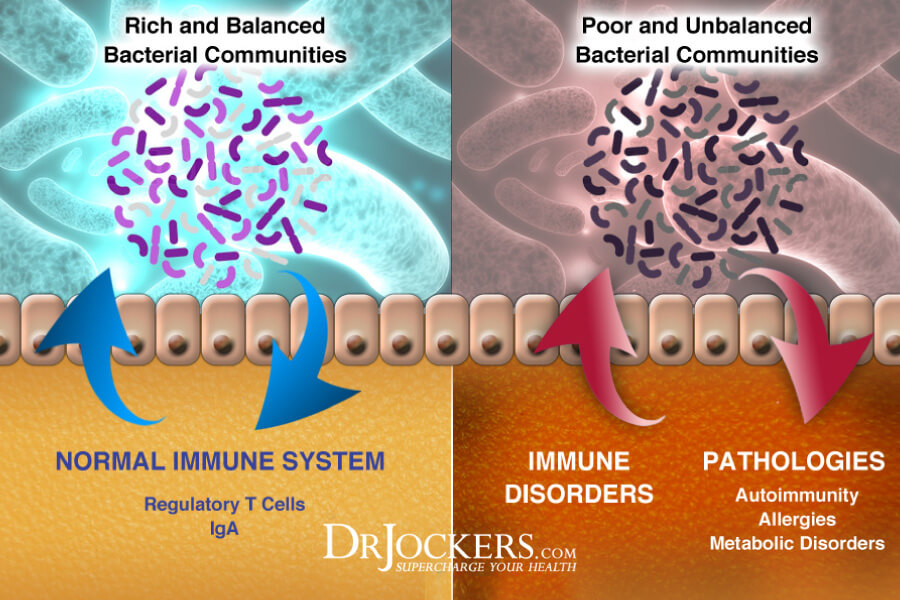
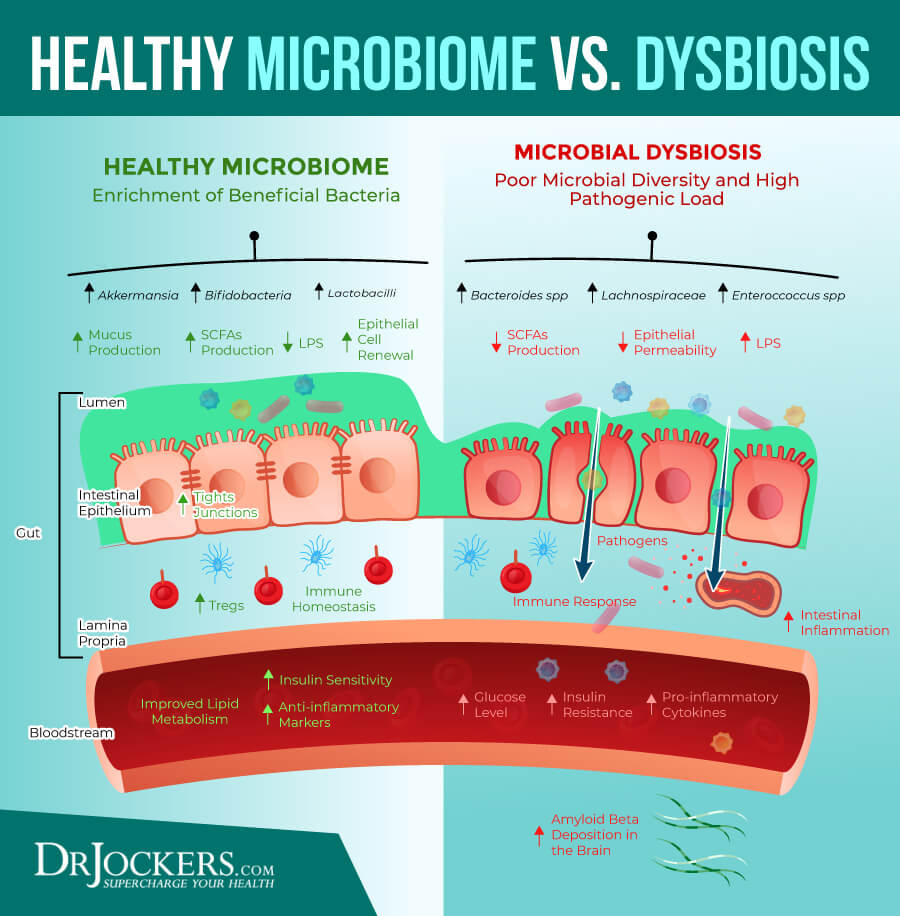
Gut Dysbiosis
Gut microbiome balance and your gut health play an important role in your immune health, skin health, and the development of autoimmune diseases. A 2017 study published in the Frontiers of Immunology has found a connection between leaky gut syndrome and autoimmune diseases (18).
A 2019 study published in Microorganisms has found a link between microbiome health and the risk of developing an immune-mediated skin disease, like lichen planus (19). A 2011 study published in the International Journal of Oral Sciences has also found a connection between microbiome shifts on oral lichen planus (20).
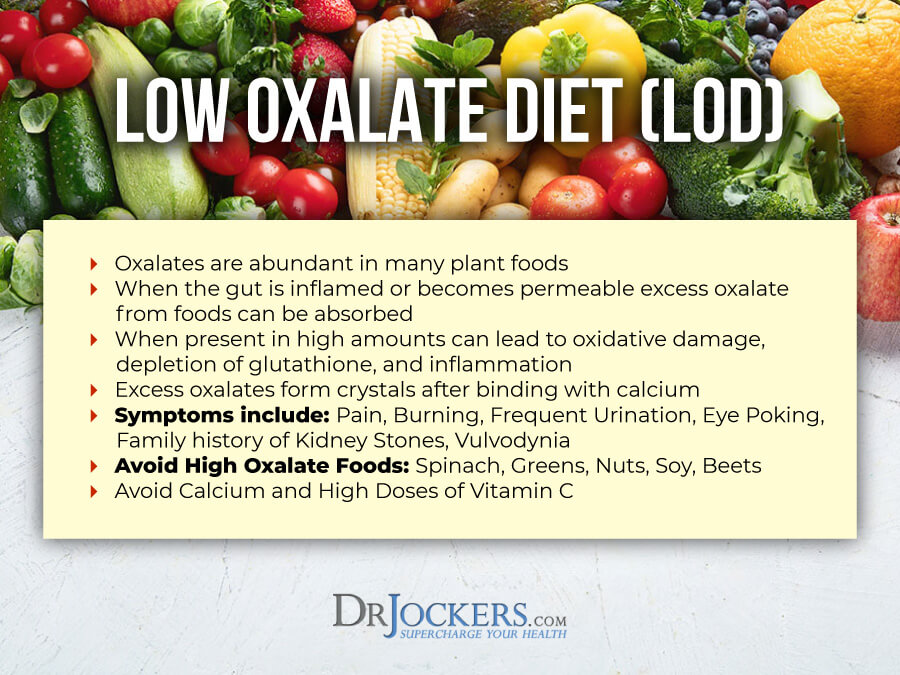
Poor Oxalate Metabolism
Oxalates are naturally occurring molecules found in a variety of plant foods. Too much oxalate and poor oxalate metabolism can lead to a variety of issues, including kidney stones. A 2016 study published in the International Brazilian Journal of Urology has found that patients with lichen planus are also prone to urolithiasis (21).
The risk for this issue may be reduced with a low-oxalate diet. A 2008 study published in the Journal of Reproductive Medicine has found that dietary changes, such as eating a low-oxalate diet may help adult-onset vulvodynia, which can develop in women with lichen planus (22). You can test your oxalate levels through an Organic Acid Test here
Conventional Treatments
If you think that you have lichen planus, it is important that you visit your doctor for the correct diagnosis. They will do some tests to rule out other issues, including hepatitis C and allergies in the case of oral lichen planus.
There is no cure for lichen planus. In some cases, symptoms can go away on their own, how treatment may be required. Conventional treatments of lichen planus may include:
- Topical, oral, or injection corticosteroids for inflammation
- Antihistamines for inflammation, itching, pain, and discomforts
- Immunosuppressant medications
- Acne medications
- Pain medications
- Mouthwash with lidocaine
- Photochemotherapy light treatment (PUVA)

Natural Support Strategies
If you are dealing with lichen planus, there are some natural support strategies that may benefit you. Here is what I recommend to improve your health:
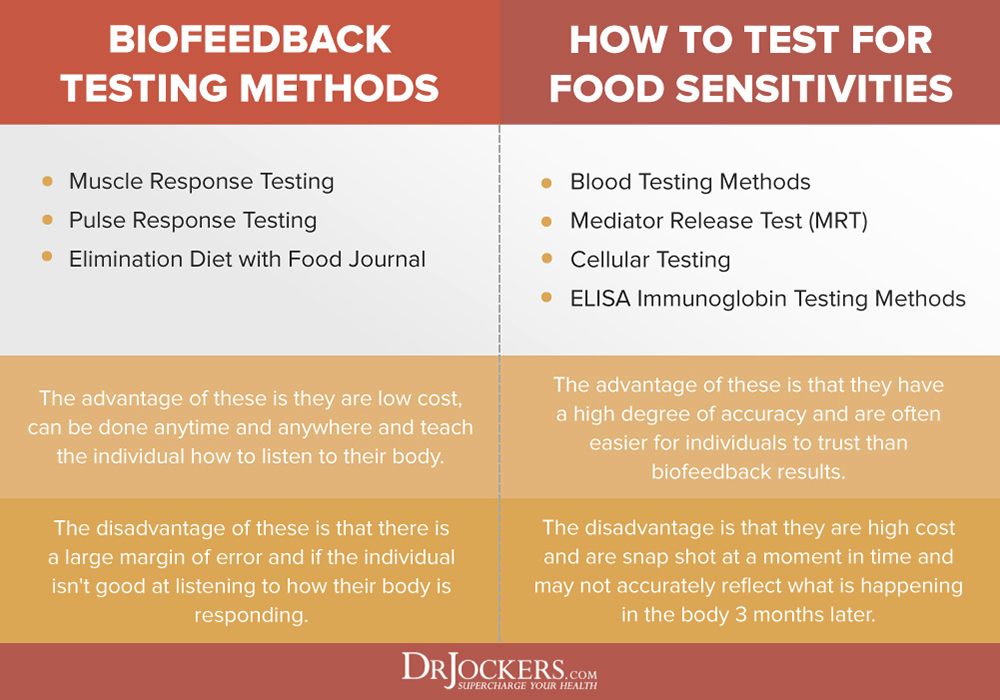
Test for Food Sensitivities
Food sensitivities and allergies can increase your risk and symptoms of lichen planus (5). Common food sensitivities include gluten, sugar, peanut, nuts, legumes, soy, dairy, and eggs. Identifying your food sensitivities is critical. While there are a variety of blood tests available to identify your food sensitivities, there is a risk for false positives and false negatives and they don’t test for all foods, I recommend other alternatives instead or additionally.
I recommend trying pulse testing or muscle testing as functional testing methods. You may also try an elimination diet by eliminating potential culprits for a month and re-introducing them one by one watching your symptoms disappearing or returning. If you find any food sensitivities, remove them from your diet.
Since food sensitivities can change over time, I recommend that you repeat testing once a year or if your symptoms return. I recommend reading this article to learn about both biofeedback testing and clinical lab testing options for food sensitivities.
Consider a Low-Oxalate Nutrition Plan
Following a low-oxalate nutrition plan may help to reduce symptoms and complications of lichen planus (22). High-oxalate foods include spinach, dried fruit, rhubarb, rice bran, bran flakes, brown rice flour, almonds, cashew, peanuts canned pineapples, beets, potatoes, sweet potatoes, swiss chard, turnips, peanut butter, cacao, chocolate, berries, kiwi, figs, purple grapes, okra, leeks, celery, plantain, olives, buckwheat, quinoa, and tea.
I recommend that you reduce your consumption of high-oxalate foods for about a month and see if your symptoms improve. Slowly introduce each oxalate food one by one to see if your symptoms return. If you notice your symptoms returning, a low-oxalate diet may be beneficial for your long-term.
You can also improve your B6 levels and use a potassium-magnesium citrate supplement to help bind oxalates and remove them. You can learn more about oxalates in this article here.

Reduce Stress & Improve Sleep
According to a 2008 review published in Autoimmunity Reviews, chronic stress can trigger autoimmune diseases, including lichen planus (23). Chronic stress can interfere with the quality of sleep and poor sleep can increase chronic stress feeding into a vicious cycle and further triggering autoimmune symptoms.
Reducing your stress levels and improving your sleep is critical for your well-being. I recommend that you practice meditation, breathwork, relaxation strategies, guided visualization, gratitude, prayer, and journaling. Spend time in nature. Spend time with supportive and uplifting people but also delegate some quality ‘me-time’.
Make sure to sleep 7 to 9 hours a night. Develop a nighttime routine that helps you relax at night. Avoid electronics, eating, and stress before bed, and choose relaxing activities, like reading, coloring, writing, taking relaxing baths, and drinking herbal tea.

Embrace Biological Dentistry
Since poor oral health and toxic amalgam fillings can both play a role in lichen planus, I recommend that you take care of your oral health and embrace biological dentistry (6, 7). Removing amalgam fillings at a regular dentist can be dangerous since drilling them out will spread mercury and increase toxic effects.
A biological dentist can help to safely remove amalgam fillings, root canals, and cavitations. They can help to address current dental issues without the use of amalgam or other harmful practices and recommend natural and safe dental hygiene methods.
Heal the Microbiome
Your microbiome and gut health can influence the symptoms of lichen planus (18, 19, 20). I recommend that you eat an anti-inflammatory, gut-friendly diet rich in greens, vegetables, herbs, spices, sprouts, low-glycemic index fruits, healthy fats, and clean protein from pasture-raised, grass-fed, and organic animal sources.
Find the right diet that works for you body. Some people need a low-FODMAP or low prebiotic diet while others need more prebiotic and probiotic rich foods to see improvement. Prebiotic-rich foods include garlic, onion, leeks, Jerusalem artichokes, jicama, chicory roots, dandelion greens, asparagus, and apples.
Probiotic-rich foods include sauerkraut, fermented vegetables, kimchi, kefir, yogurt, and kombucha. Take a daily dose of probiotic supplement. Improve your stomach acid levels by taking betaine hydrochloride (HCl) and digestive enzymes.
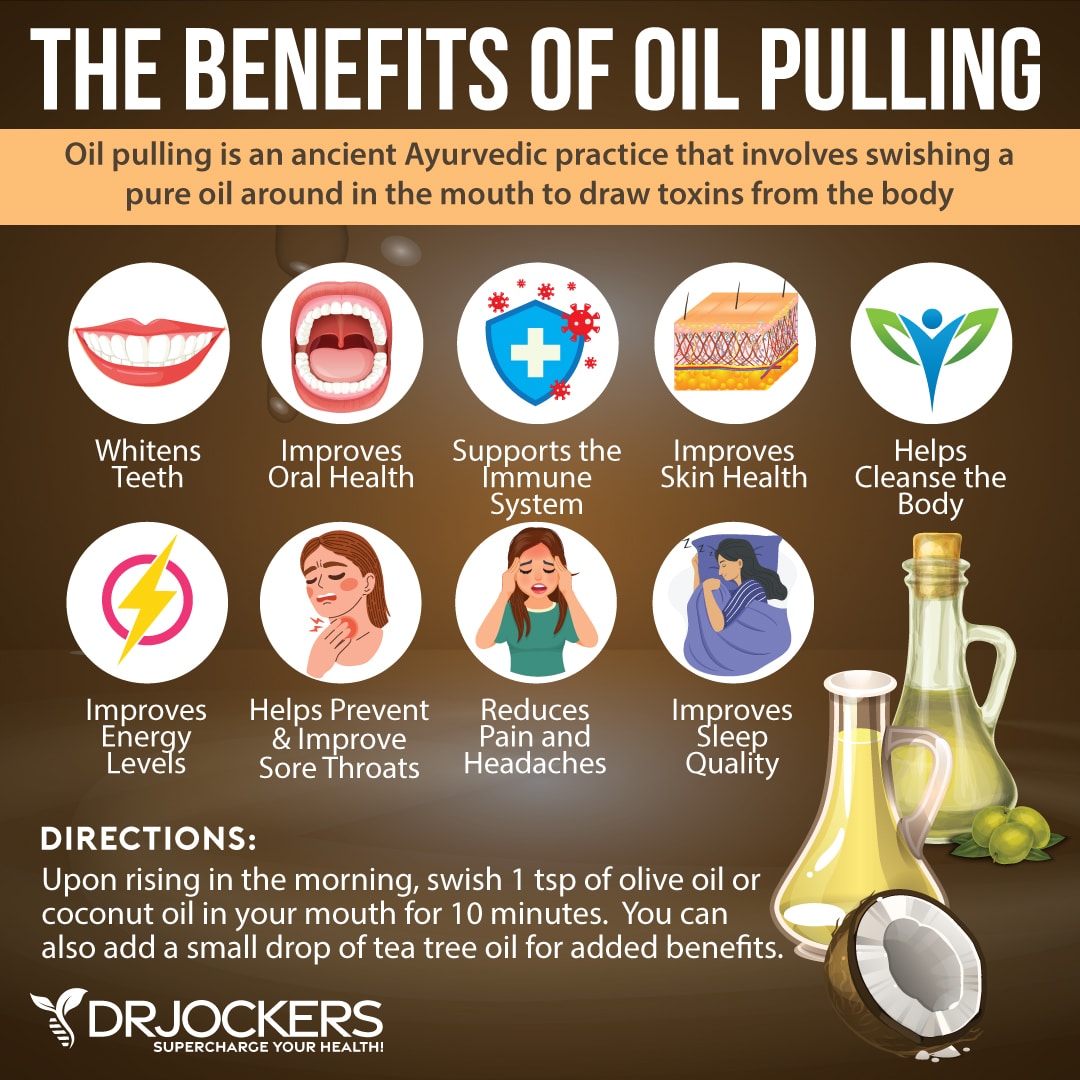
Oil Pulling
Oil pulling can help to improve your dental and oral health to avoid oral health issues and amalgam fillings that may trigger lichen planus in the mouth (6, 7). It helps to pull out toxins, remove bacteria and yeast, and reduce plaques. I recommend that you start every day with oil pulling.
Swish around a tablespoon of coconut or olive oil in your mouth for about 20 minutes. Spit it out and brush your teeth thoroughly. Use a different toothbrush at night or other times of the day. The time you spend oil polling may be a great opportunity for meditation, journaling, or stretching.
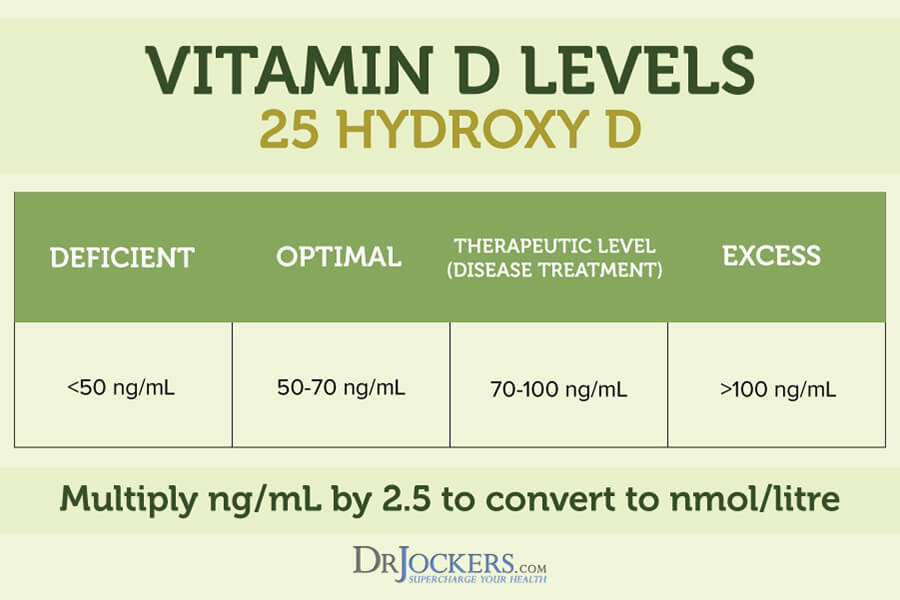
Sun Exposure & Vitamin D Supplementation
Vitamin D deficiency can increase the risk of lichen planus (17). I recommend that you spend at least 15 minutes outside in the sun every day if possible. Eat plenty of foods that are rich in vitamin D, including fatty fish, liver, liver oil, egg yolks, and mushrooms.
Unfortunately, diet and sun exposure is not enough to meet all your vitamin D needs, so I recommend a daily vitamin D supplement as well with roughly 1,000 IU of vitamin D for every 25 lbs of body weight daily. You should get your 25-OH Vitamin D levels tested at least twice each year and aim to get your levels between 70-100 ng/ml for the best therapeutic benefits.
Zinc Supplementation
Zinc deficiency can trigger autoimmunity and lichen sclerosus (11, 12, 13,14). According to a 2019 study published in the Indian Dermatology Online Journal, taking 50 milligrams of zinc can be an effective treatment option for symptomatic lichen sclerosus (24).
I recommend taking a high-quality zinc supplement daily. Additionally, eat foods that are rich in zinc, including crab, lobster, shellfish, seeds, kale, and legumes.
B Vitamins
Vitamin B deficiencies, especially low vitamin B12 and folate, can trigger and worsen lichen planus (15, 16). I recommend that you eat plenty of foods that are rich in B vitamins, including leafy greens, salmon, liver, organ meat, beef, oysters, clams, muscles, and sunflower seeds. Additionally, take a daily dose of vitamin 12 and a vitamin B complex supplement.
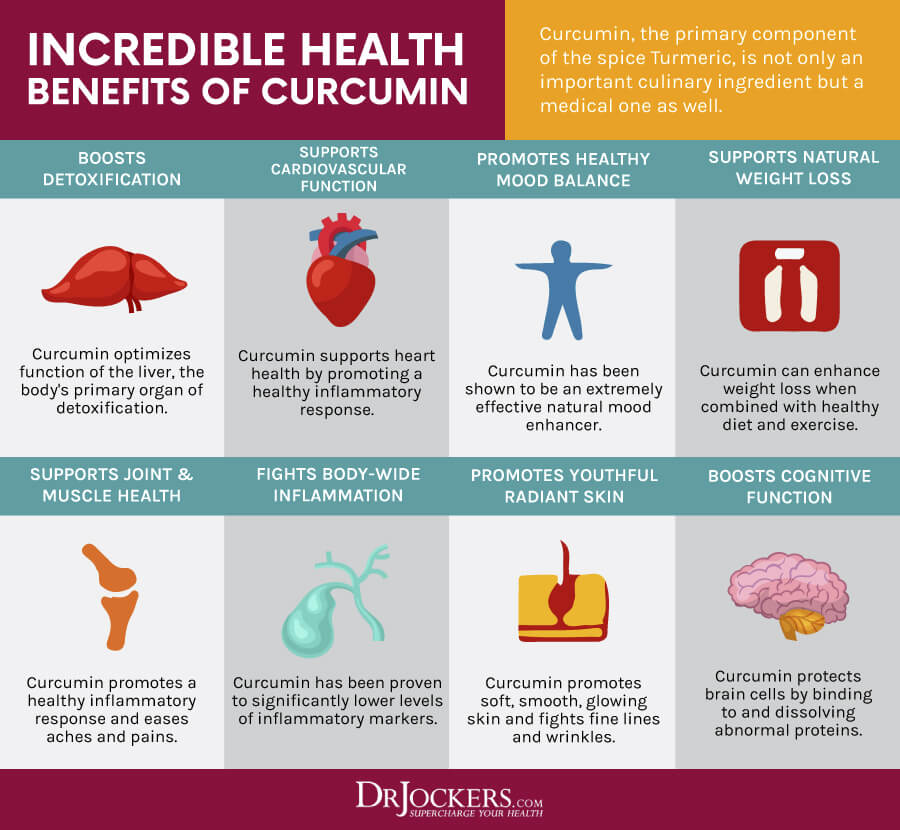
Use Turmeric
According to a 2019 systematic review published in Oral Diseases, through oral curcumin trials found no significant difference, an observational extension study found that curcumin therapy may be safe and may show some potential for the treatment of lichen planus (25).
A 2018 systematic review published in the Journal of Dermatology Treatment, curcumin may be safe and may help to reduce symptoms of oral lichen planus along with corticosteroids (26). I recommend adding turmeric to your smoothies, dips, dressings, soups, curries, dishes, and salads, and taking a high-quality daily turmeric/curcumin supplement.
Final Thoughts
Lichen planus is an inflammatory autoimmune skin condition that can cause thin, white, and shiny skin, blisters, scabbing, redness, pain, itching, or discomfort. It may affect your mouth, genital regions, nails, and scalp, but also any other areas of your body. Follow my top natural support strategies and recommendations for lichen planus to improve your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. We do offer long-distance functional health coaching programs with our world class team of health coaches. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and thrive in life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!