Systemic Lupus: Symptoms, Causes and Support Strategies
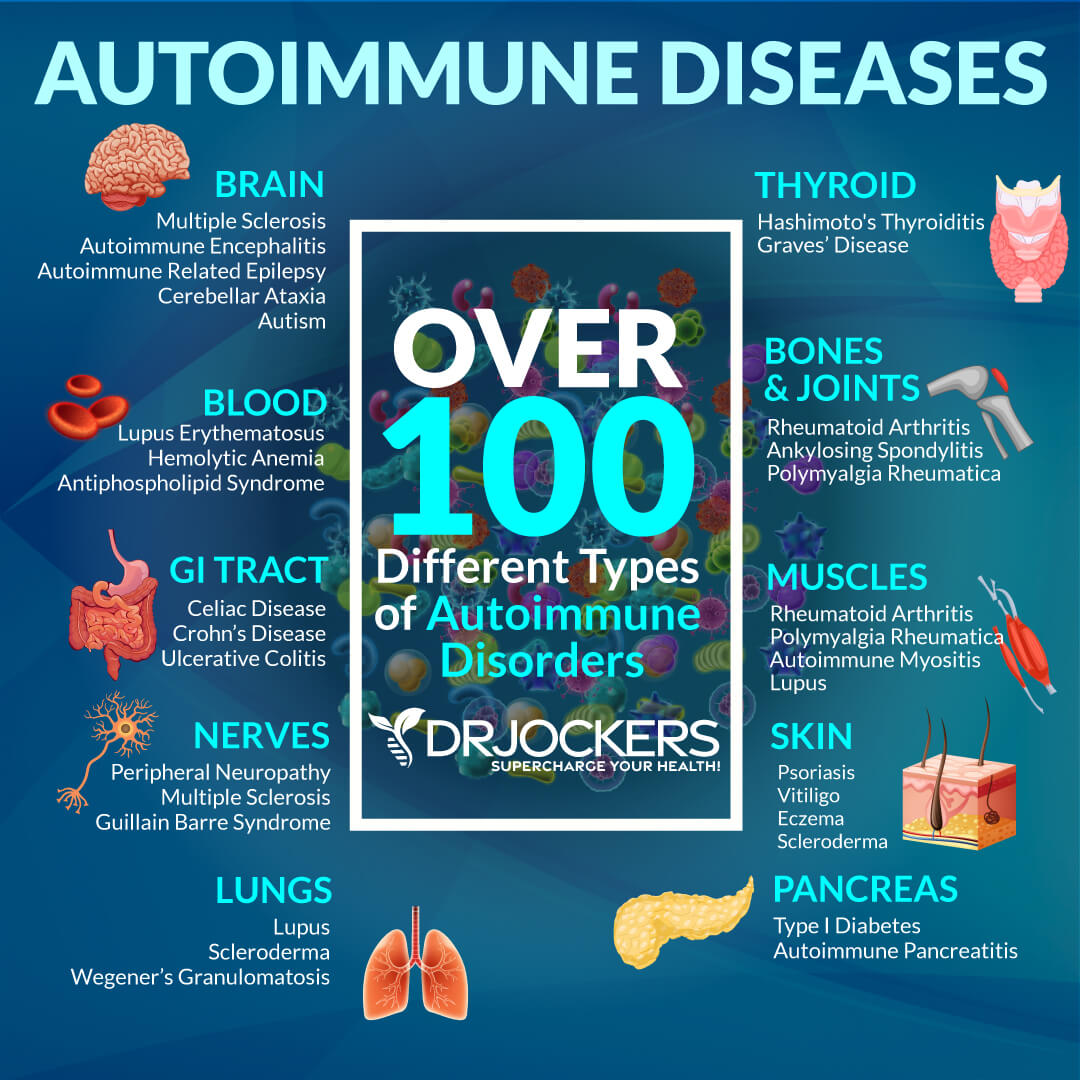
The inflammatory autoimmune disease that affects multiple organs and connective tissue in the body including the heart, brain, lungs, joints, blood vessels, skin and kidneys among others is called Systemic Lupus Erythematosus (SLE). Conventional medical treatment for lupus involves high dose corticosteroids which suppress the immune system and presents numerous other side effects.
This article will provide you with information on how to treat the inflammatory effects of autoimmune diseases such as lupus naturally. In addition, you will learn why it is important to avoid the dangers of immunosuppressant drug treatments, if possible, and address the root causes of the disorder. In this article, you will learn the most common symptoms and root cause factors for systemic lupus as well as natural support strategies.
Symptoms of Lupus:
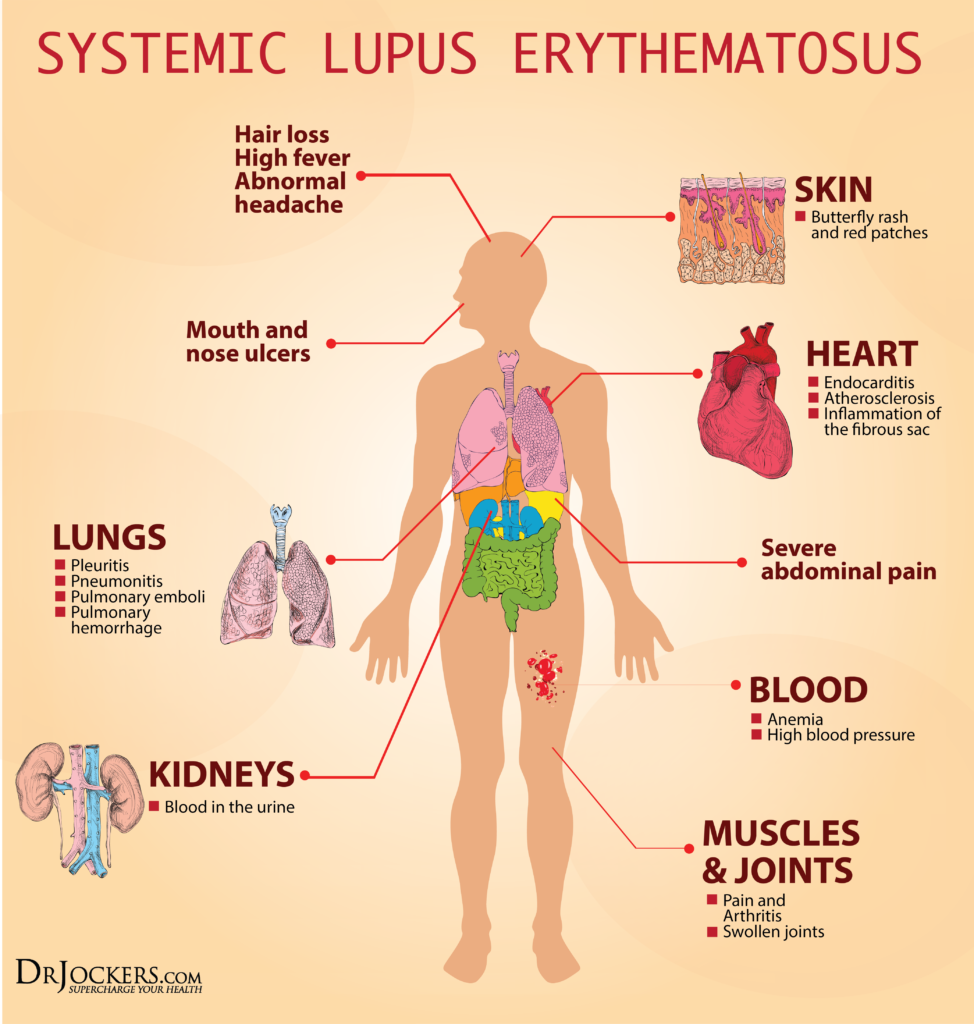
Skin lesions afflict 90% of individuals with lupus such as is evident by the butterfly-shaped rash present on an afflicted individual’s face (24). The rash covers the cheeks and the bridge of the nose. Common signs of lupus include arthritic changes, chronic fatigue, joint pain, headaches, mouth sores and reduced white blood cell count. (2)
Advanced neurodegenerative symptoms of the disease include memory loss, confusion, anxiety and depression. Lupus patients are also prone to cardiodegenerative symptoms including anemia, high blood pressure, heart disease, shortness of breath, seizures and stroke. (21)
SLE carries a wide range of clinical symptoms which can be mild or life threatening making diagnosis often a complicated and prolonged process.
Who Is Affected by Lupus?
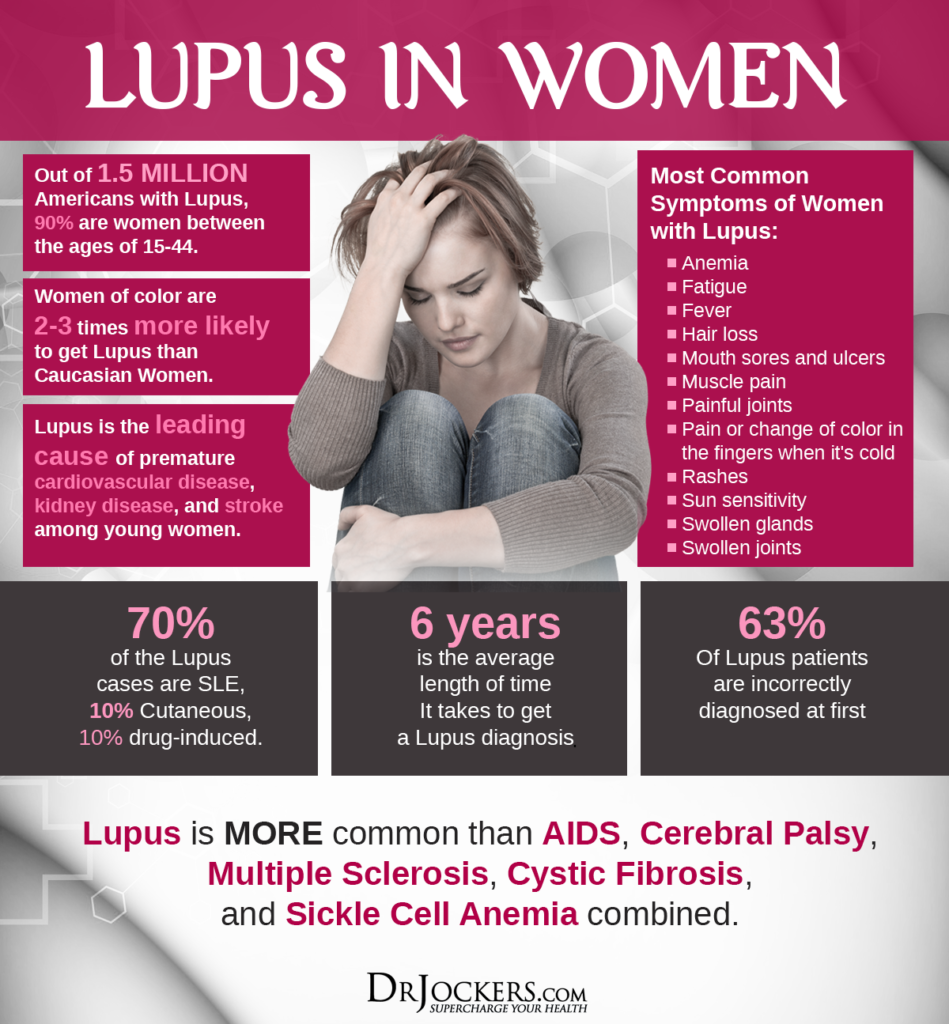
Sex matters in the risk of developing lupus as this chronic autoimmune disorder affects 9 women for every 1 man. Individuals at an increased risk for lupus also include individuals of Asian or African descent, individuals at reproductive ages between the late teens to early 40s and has the highest prevalence in Italy, Martinique, Spain and the British African-Caribbean population. (22)
Researchers hypothesize that factors which trigger the worsening effects of lupus are predominantly characterized by women’s hormones like estrogen and hormonal fluctuations caused from stress and pregnancy affecting the immune system (15). Individuals with a family history of an autoimmune disease have an increased risk of developing the disorder.
Environmental risk factors include those with increased exposure to toxins and poor diets. For example, a diet high in processed foods increases the inflammatory state of the body, increasing risk for autoimmune complications such as food allergies and gastrointestinal disturbances.
Boost Your Body’s Immunity:
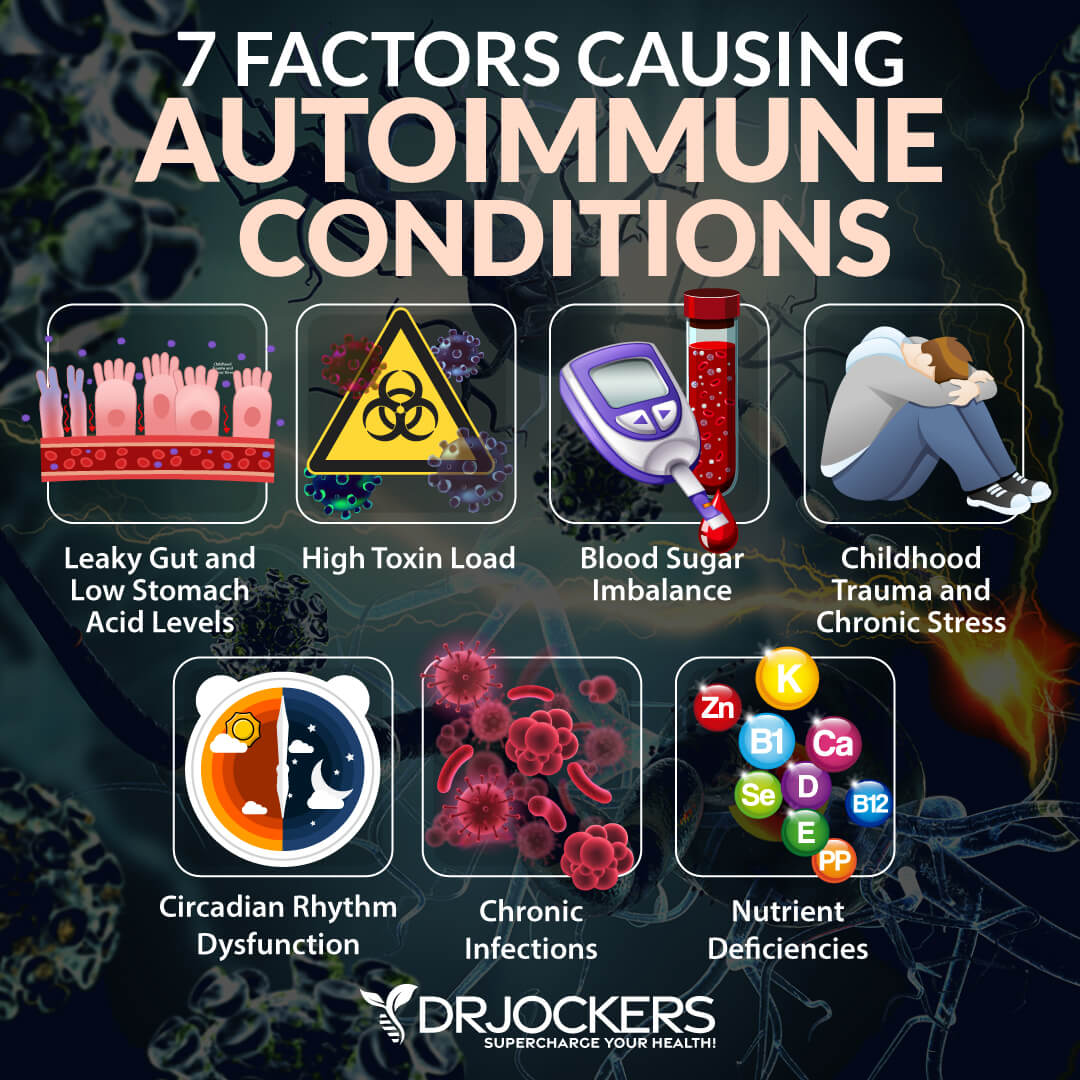
Restoring your body’s natural defenses to properly respond to a threat is crucial to overcoming chronic inflammatory disorders. People with such disorders have immune systems that are in a constant and overwhelming state of heightened reactivity which triggers inflammation. Here are 12 factors that you can address to better regulate immune function.
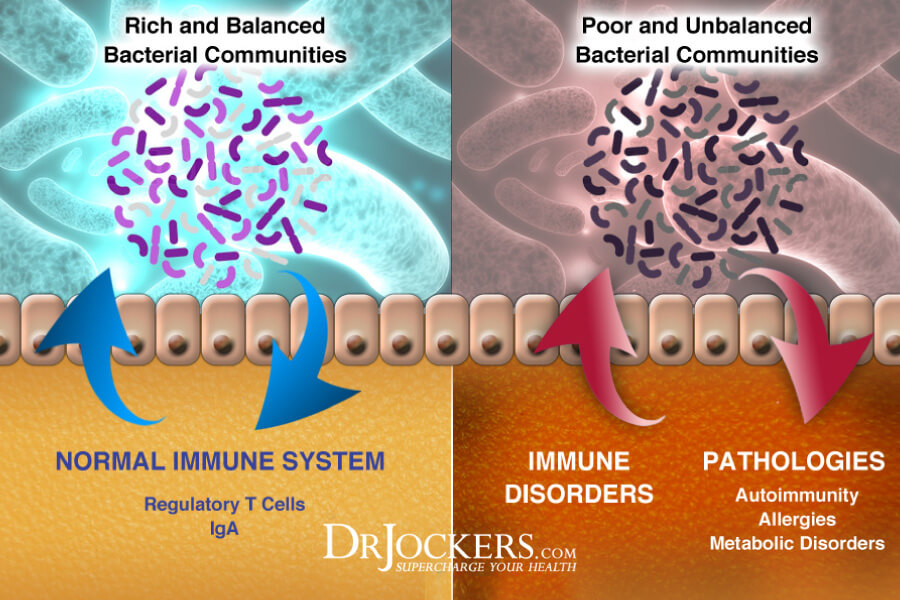
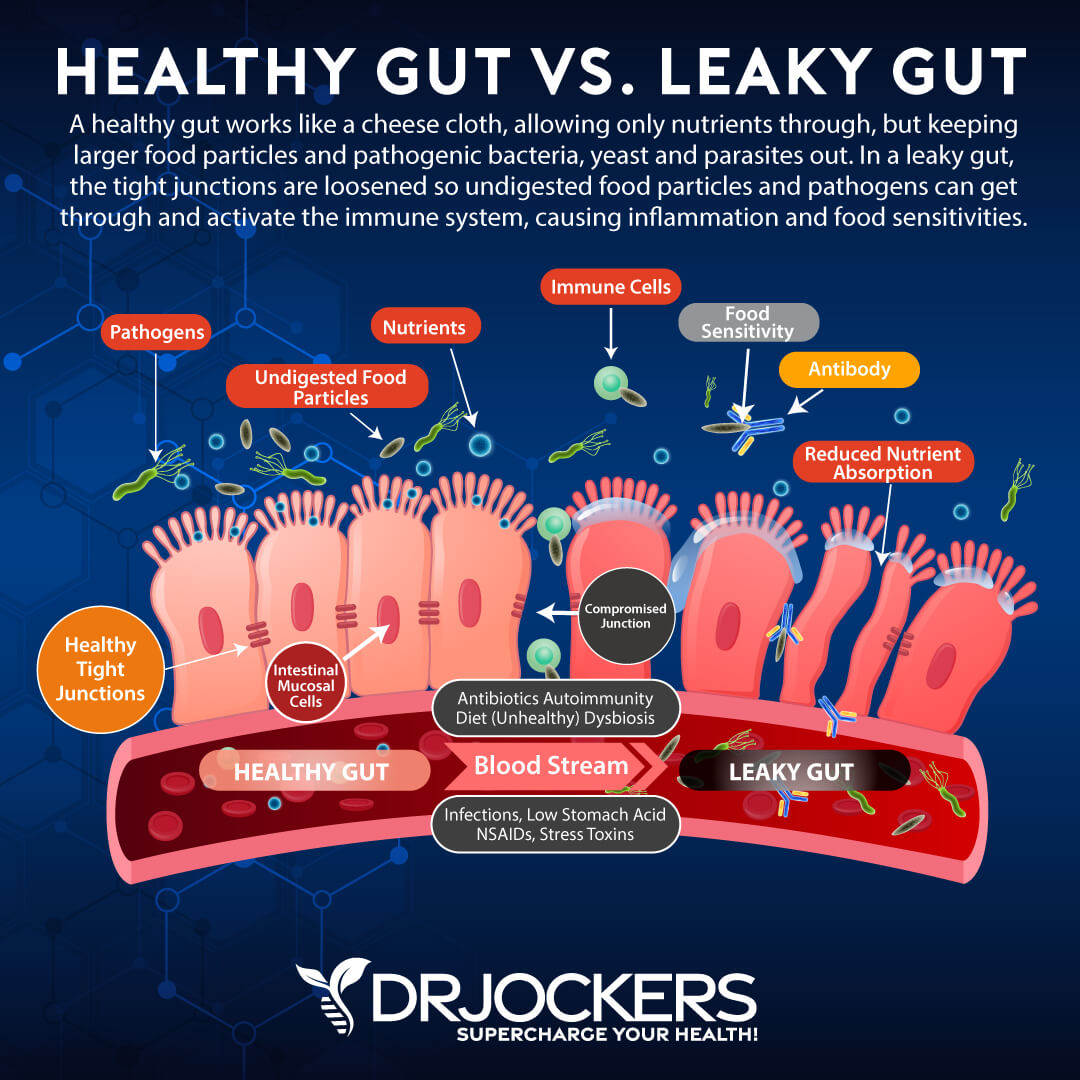
Gut Dysbiosis: This condition of the digestive tract is characterized by an imbalance of microbes, commonly an overgrowth of pathogenic bacteria. This imbalance results in chronic inflammation and can lead to leaky gut syndrome (5). In order to heal the immune system, optimizing gut health is key.
Methylation: Methylation is an important biological process in epigenetics. Methylation protects DNA, signals genes on and off and aids to detoxify cells of hazardous chemicals. Many people lack proper methylating abilities because of a specific genetic mutation that inhibits this function. Methylation is critical in boosting your body’s natural immune defenses because it also is used in regulating T cell function (6).
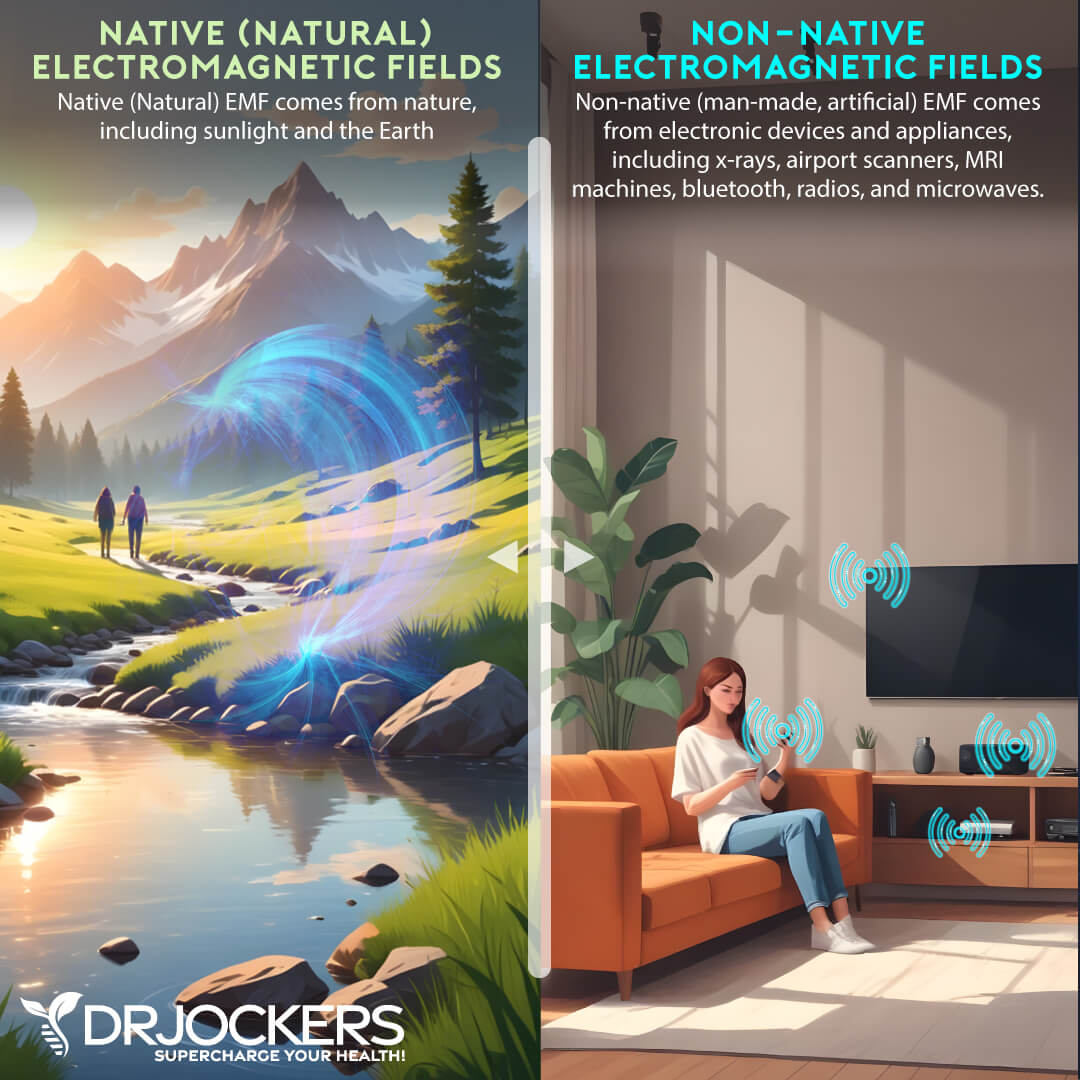
EMF Exposure: EMF exposure, or electromagnetic frequency, has been found to create immune system dysfunction. Exposure to EMF is thus associated with a higher risk of developing an autoimmune condition (7). Doing your best to reduce EMF exposure and getting grounded by going barefoot on grass, dirt or sand for at least 10 minutes each day can make a big difference.
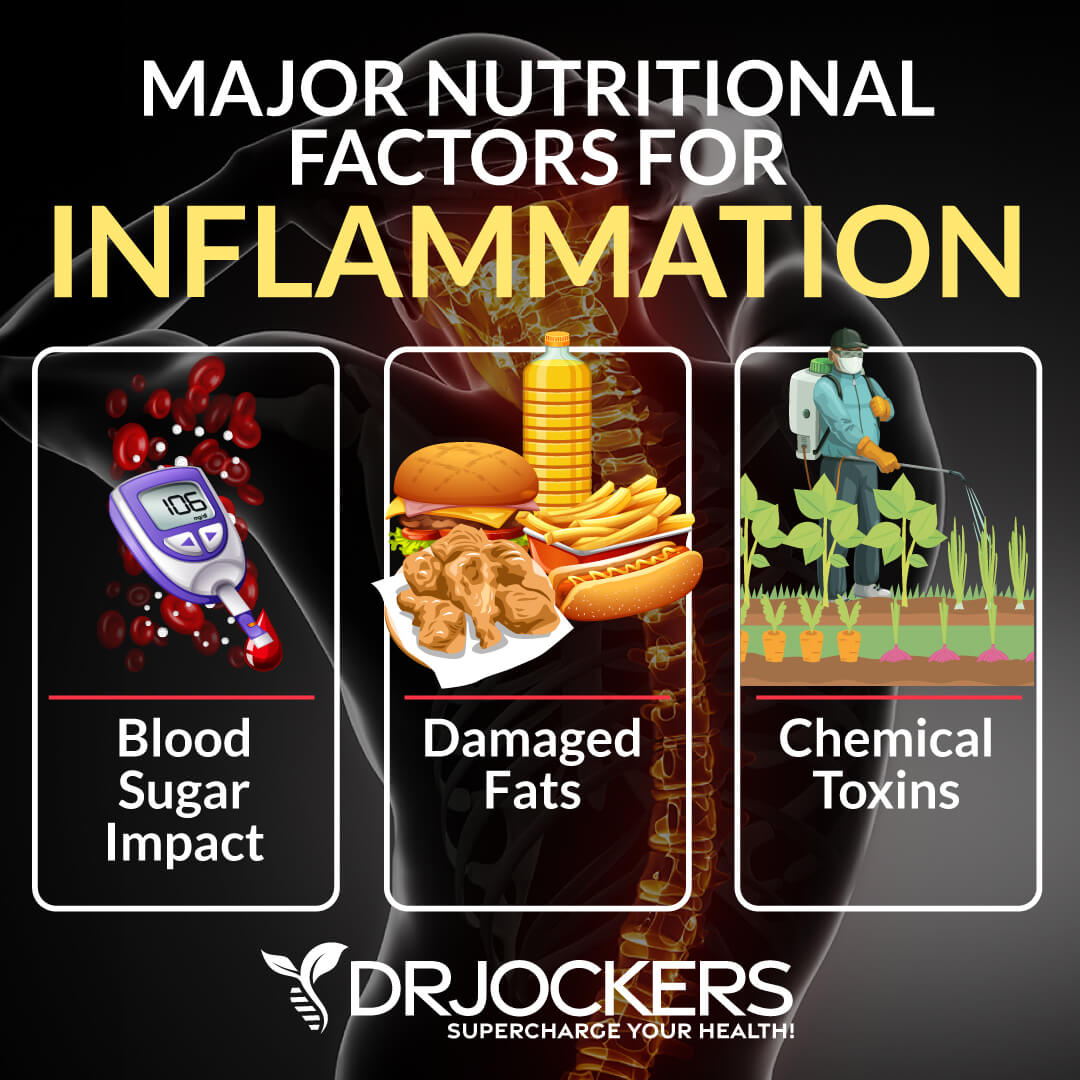
Poor Blood Sugar Regulation: Balancing blood sugar is essential for a healthy immune system. Unstable blood sugar levels promotes an increased response by the immune system working overtime to support the body’s energy needs causing altered signaling pathways and dysfunction.
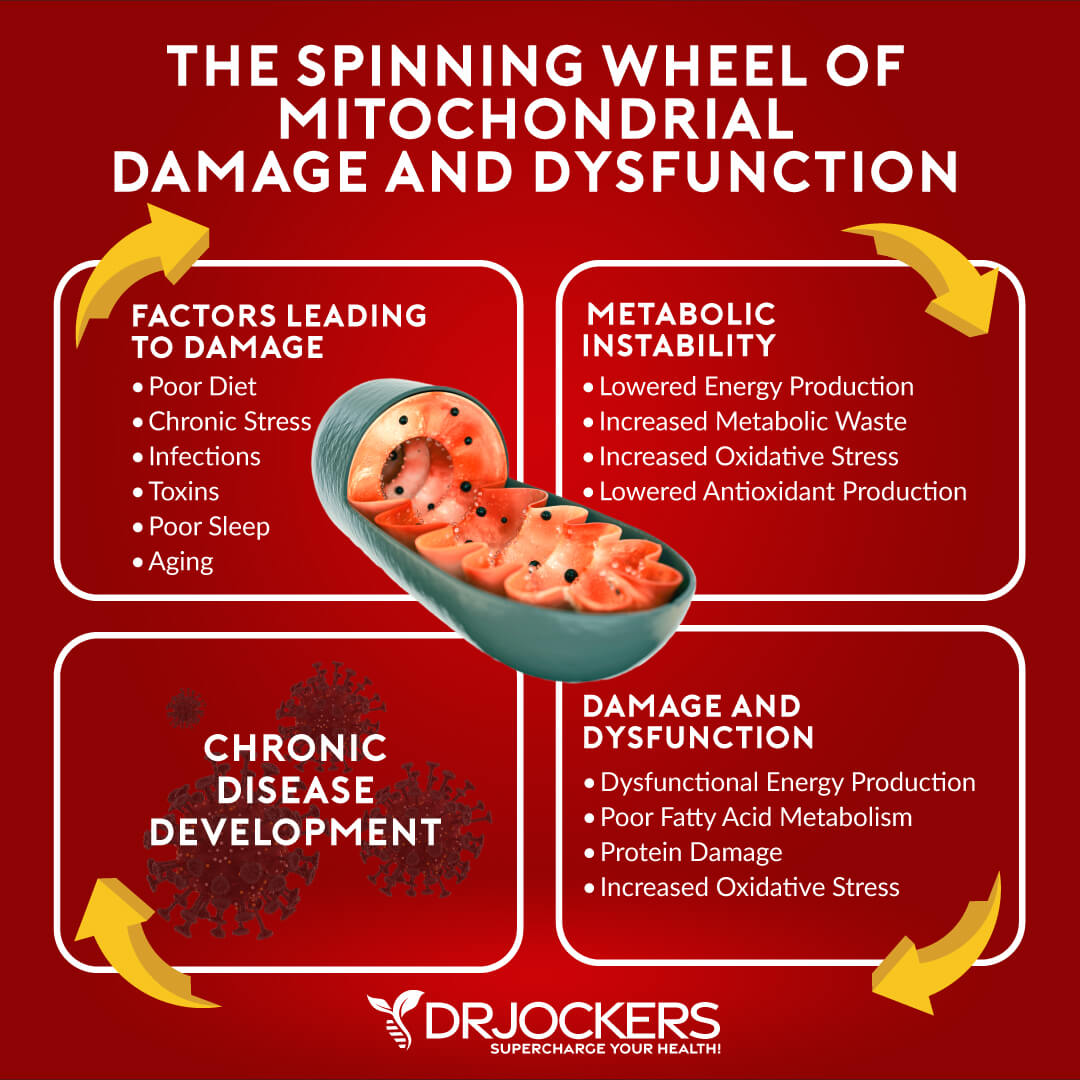
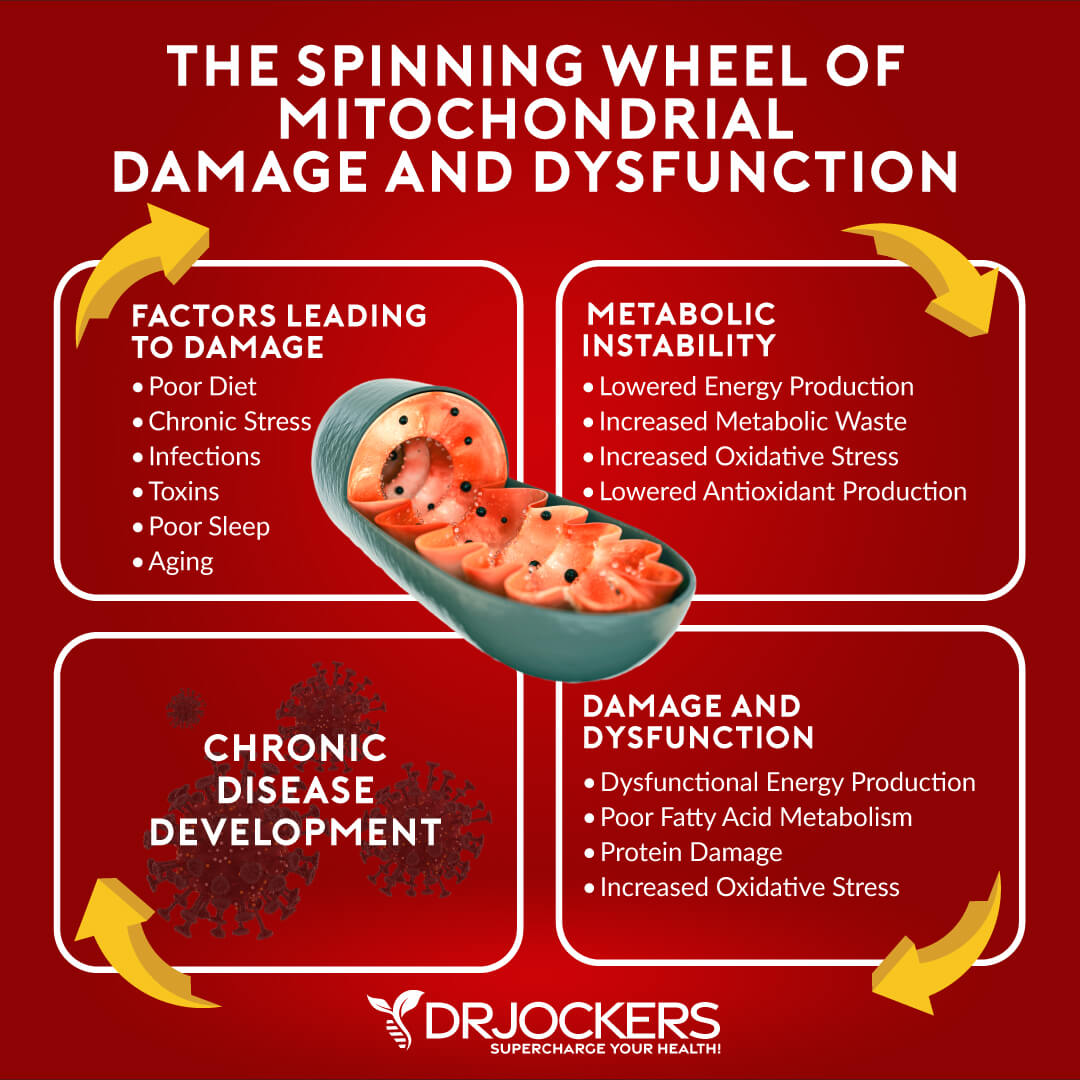
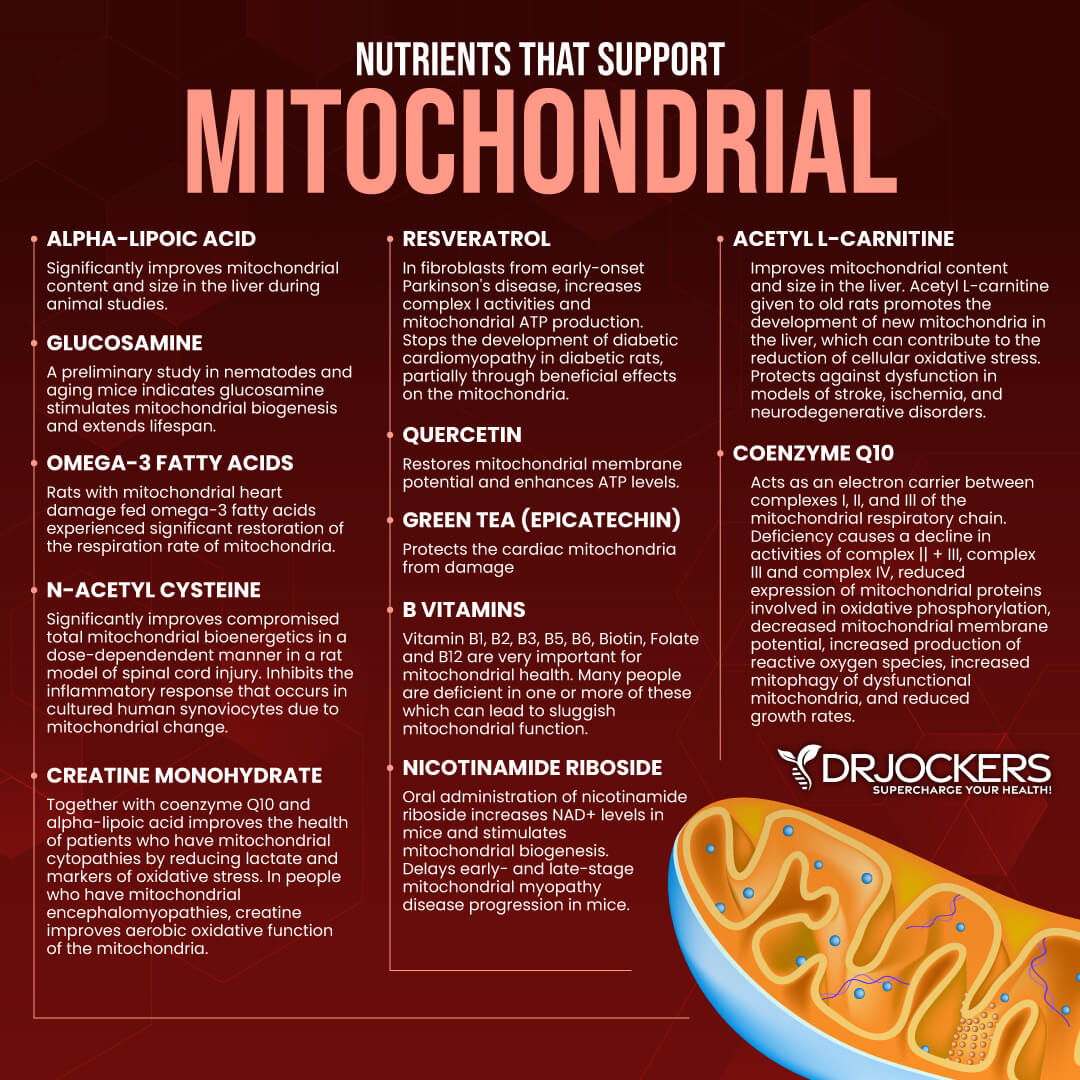
Mitochondrial Dysfunction: Mitochondria are energy producing “powerhouses” for each cell in the human body which are susceptible to high levels of oxidative stress daily. Abnormal mitochondria function is associated with increased free radical damage and oxidative stress.
This problem leads to an abnormal immune response. Most researchers agree that mitochondrial dysfunction is an abnormality that characterizes autoimmune diseases like multiple sclerosis (8).
Glutathione Deficiency: Glutathione is a master antioxidant present within every cell in the human body. Glutathione is needed to support white blood cell (WBC) function. WBCs are susceptible to high amounts of oxidative stress resulting from free radical damage every single second. A glutathione deficiency can exacerbate inflammatory levels and potentially lead to autoimmune conditions (9).
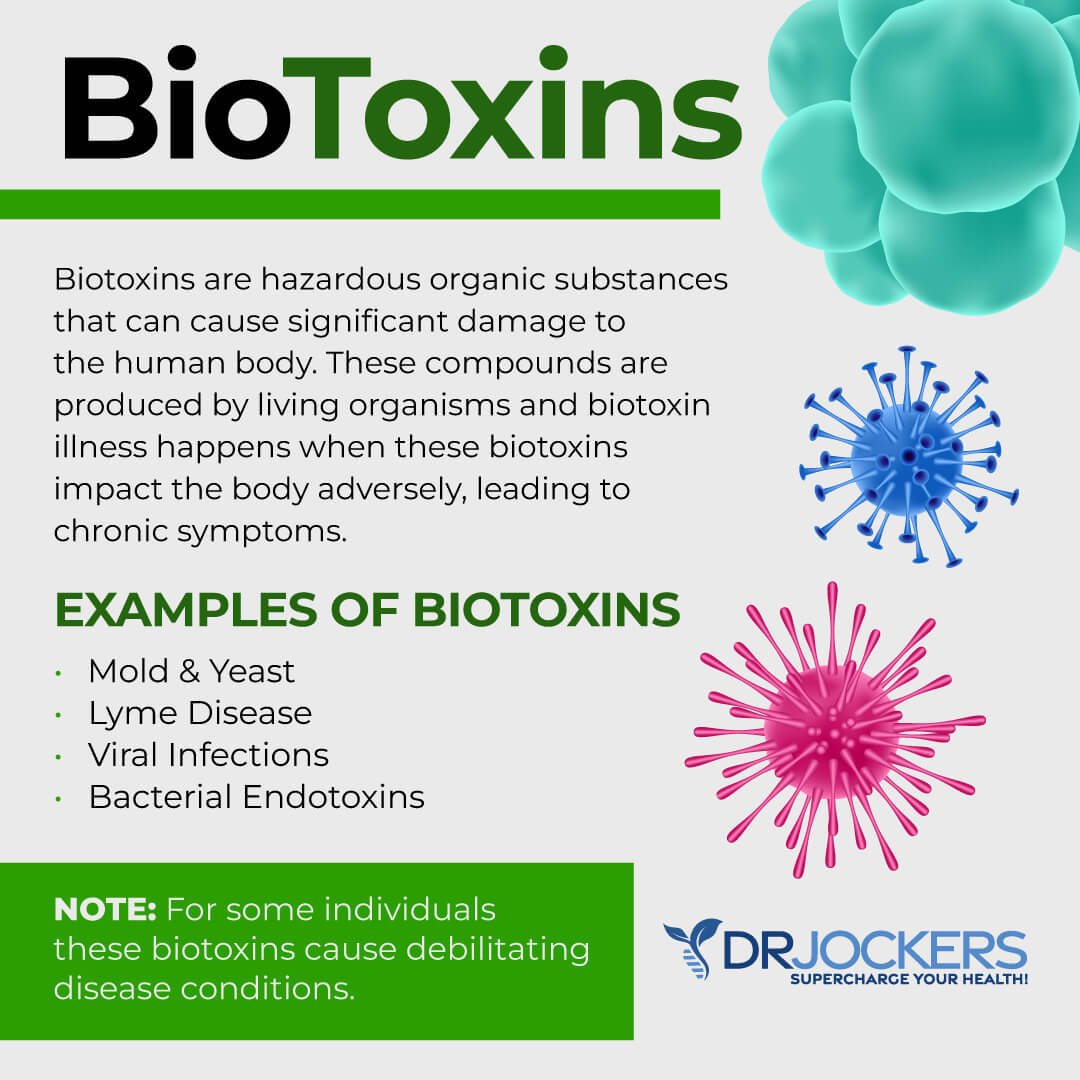
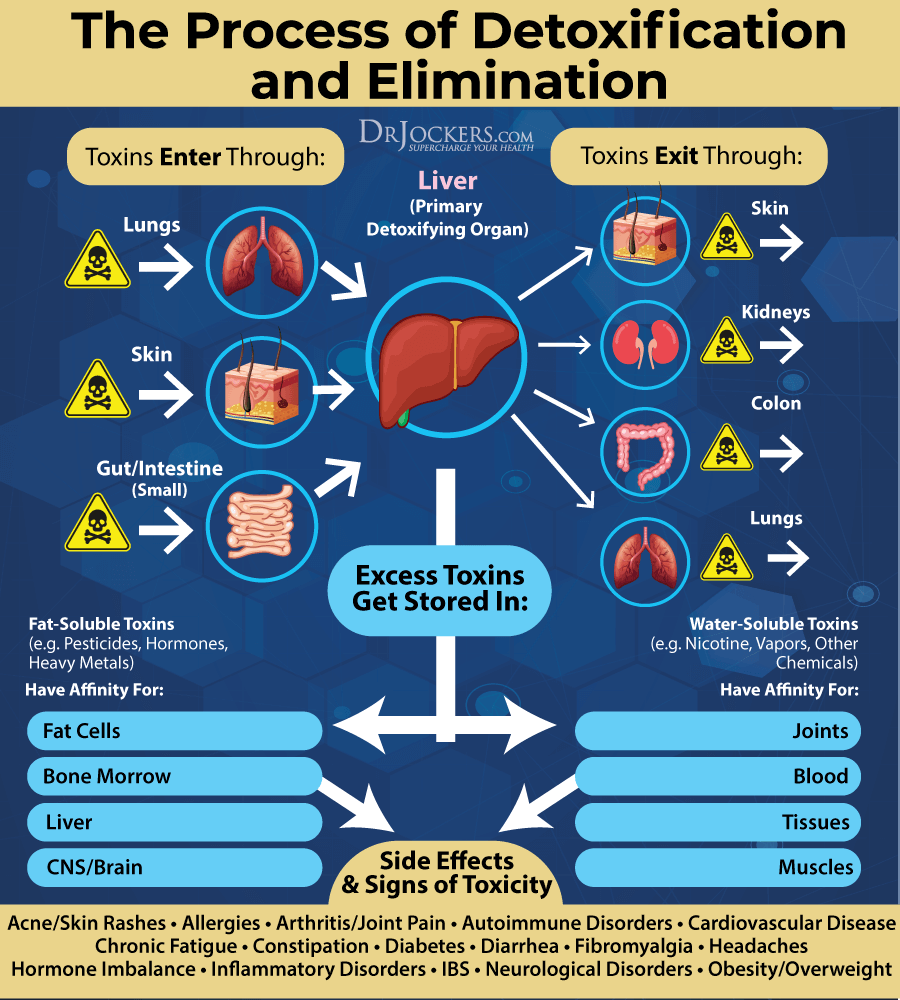
Environmental Toxins: Environmental toxins upset the gut microflora, reduce glutathione levels and trigger inflammatory activity in the body (10, 11, 12). The human body is regularly exposed to such toxic agents found in pesticides, herbicides, plasticizers, personal care products, and heavy metals as well as infectious microbes and biotoxins like mold which deplete glutathione levels.
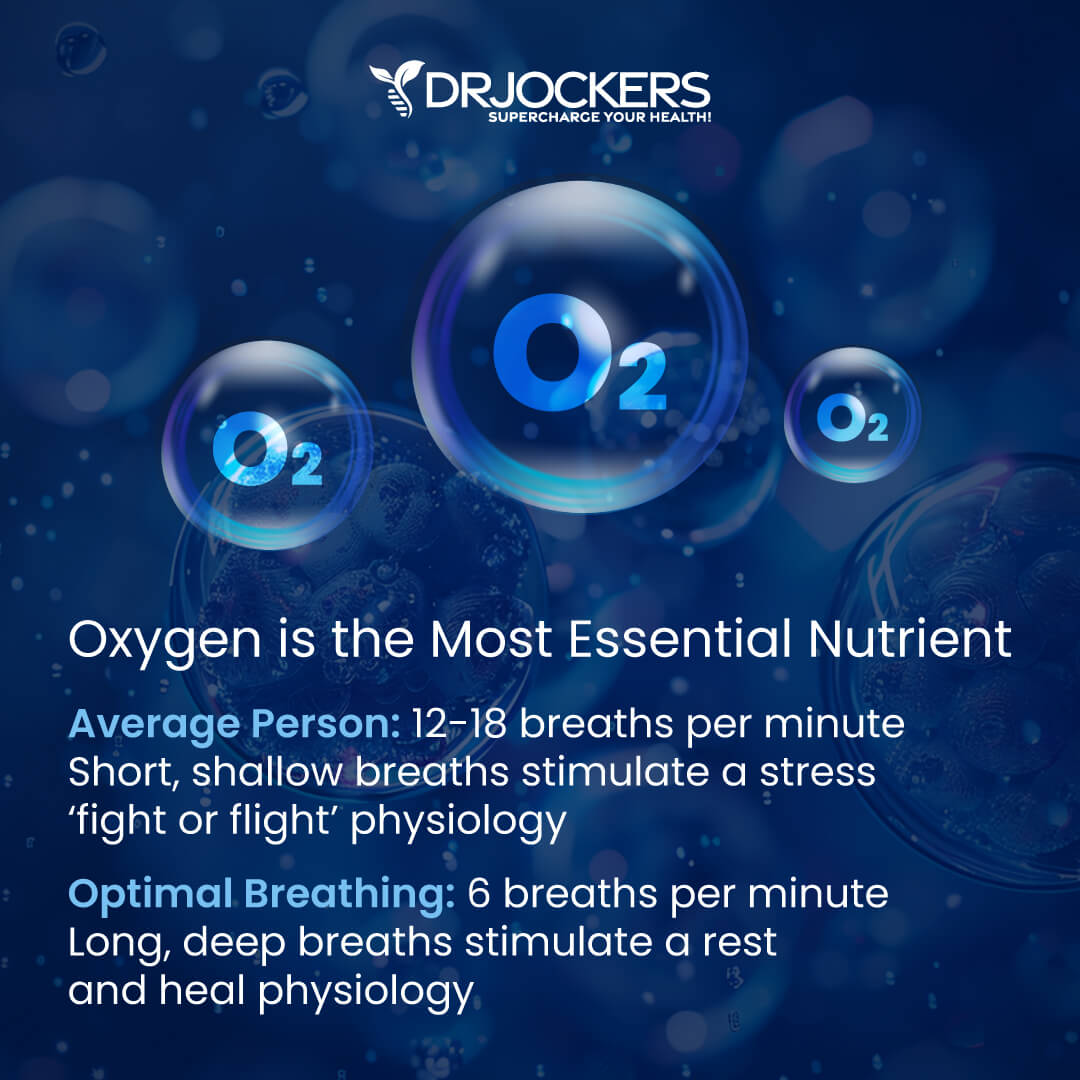
High Stress and Poor Breathing Habits: Mental and emotional stress elevates the production of stress hormones in the body. These hormones produce inflammatory effects. Coupled with short and shallow breathing habits throughout the day, these stressors induce mental and emotion stress at the physiological level (13).
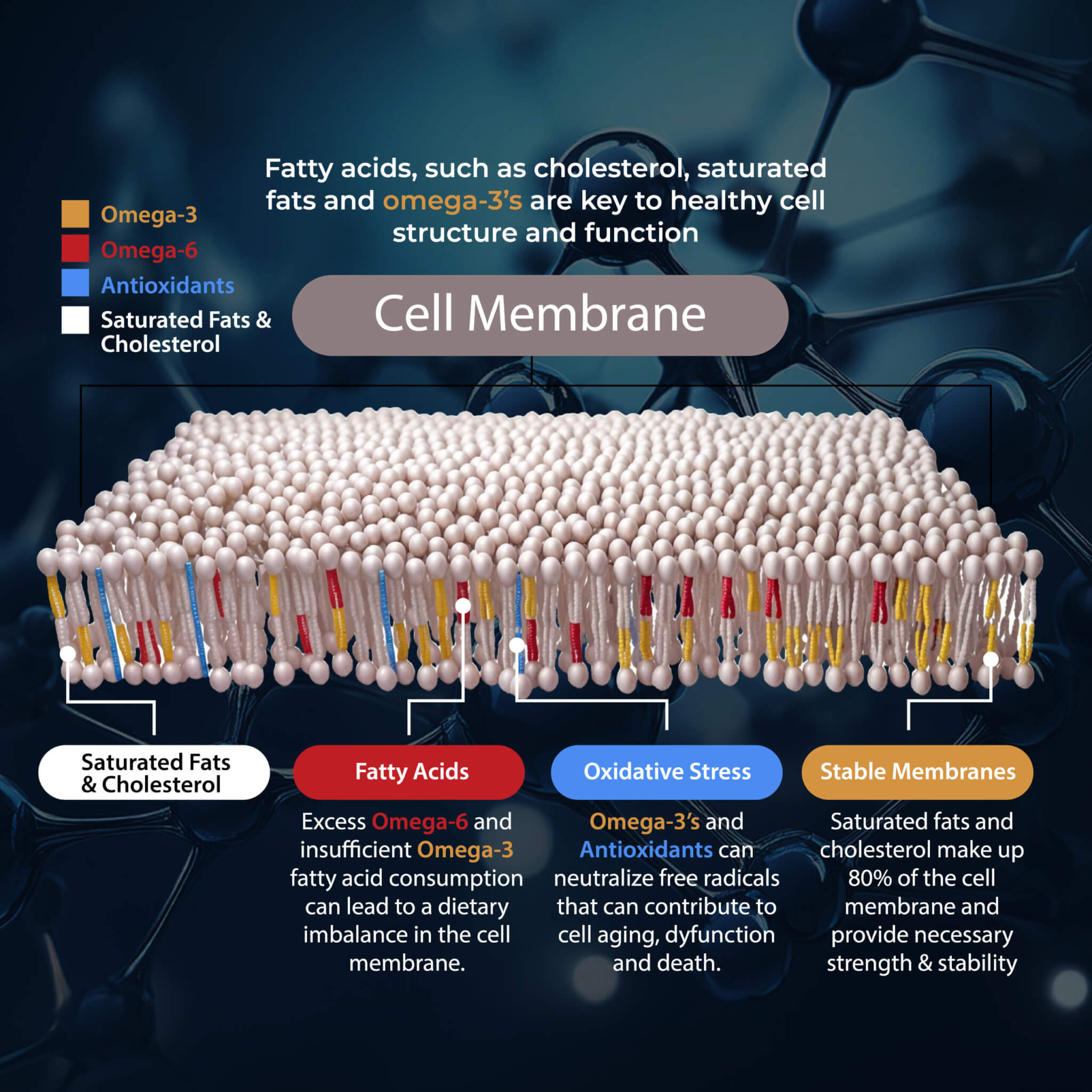
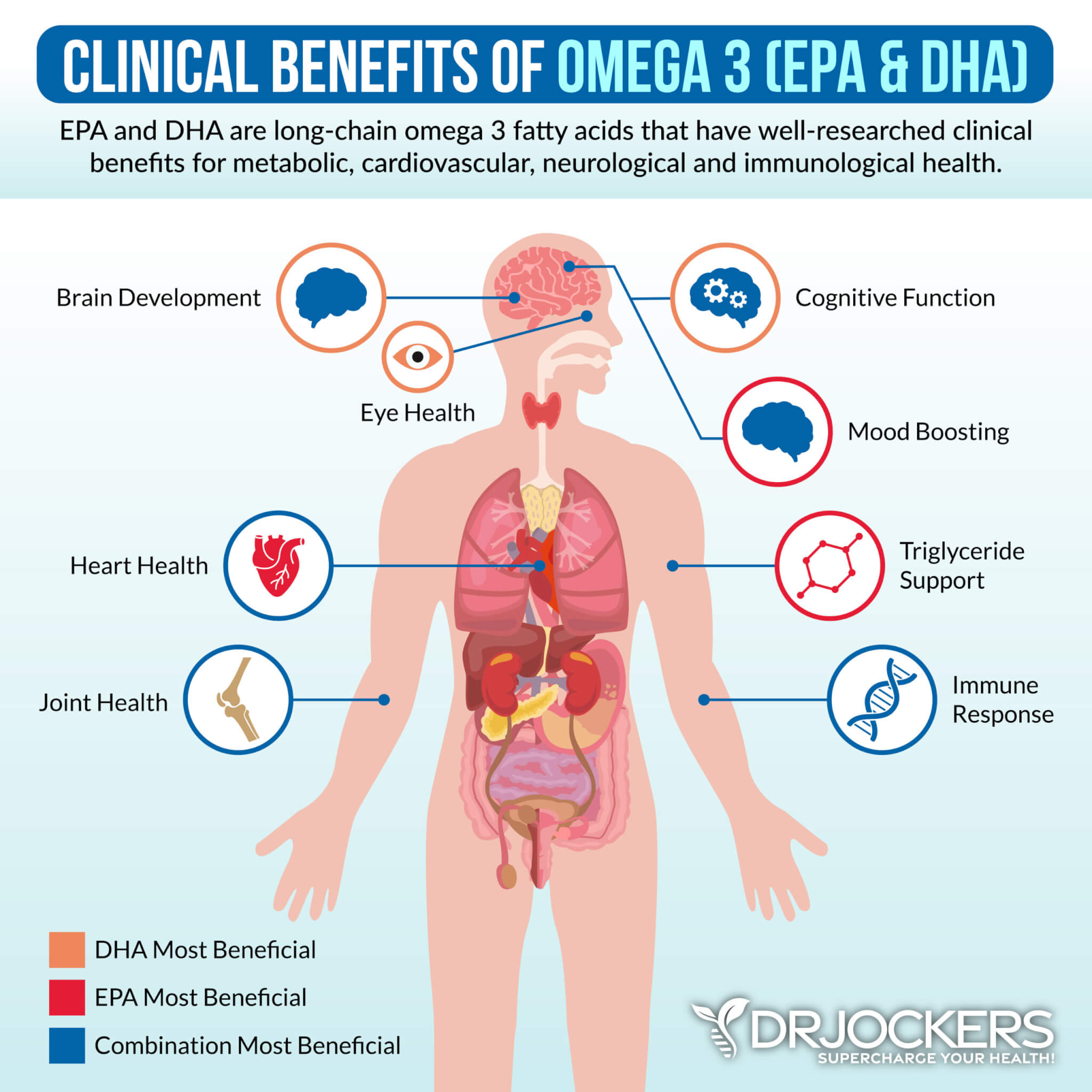
High Omega 6:3 Ratio: The ratio of omega 6 fatty acids to omega 3 fatty acids is critical in understanding chronic inflammation and autoimmunity (14). On average, most people have a higher concentration of omega 6 fats compared to omega 3 fats. The higher the concentration of omega 6 to omega 3 fats, the increased release of pro-inflammatory mediating prostaglandin molecules.
Sleep Deprivation: Up to 80% of lupus patients are not receiving enough sleep and suffer from chronic fatigue (23). Poor sleeping habits promotes immune dysfunction and chronic inflammation. Adequate sleeping habits are essential to melatonin secretion responsible for reducing inflammation and tissue repair (15).
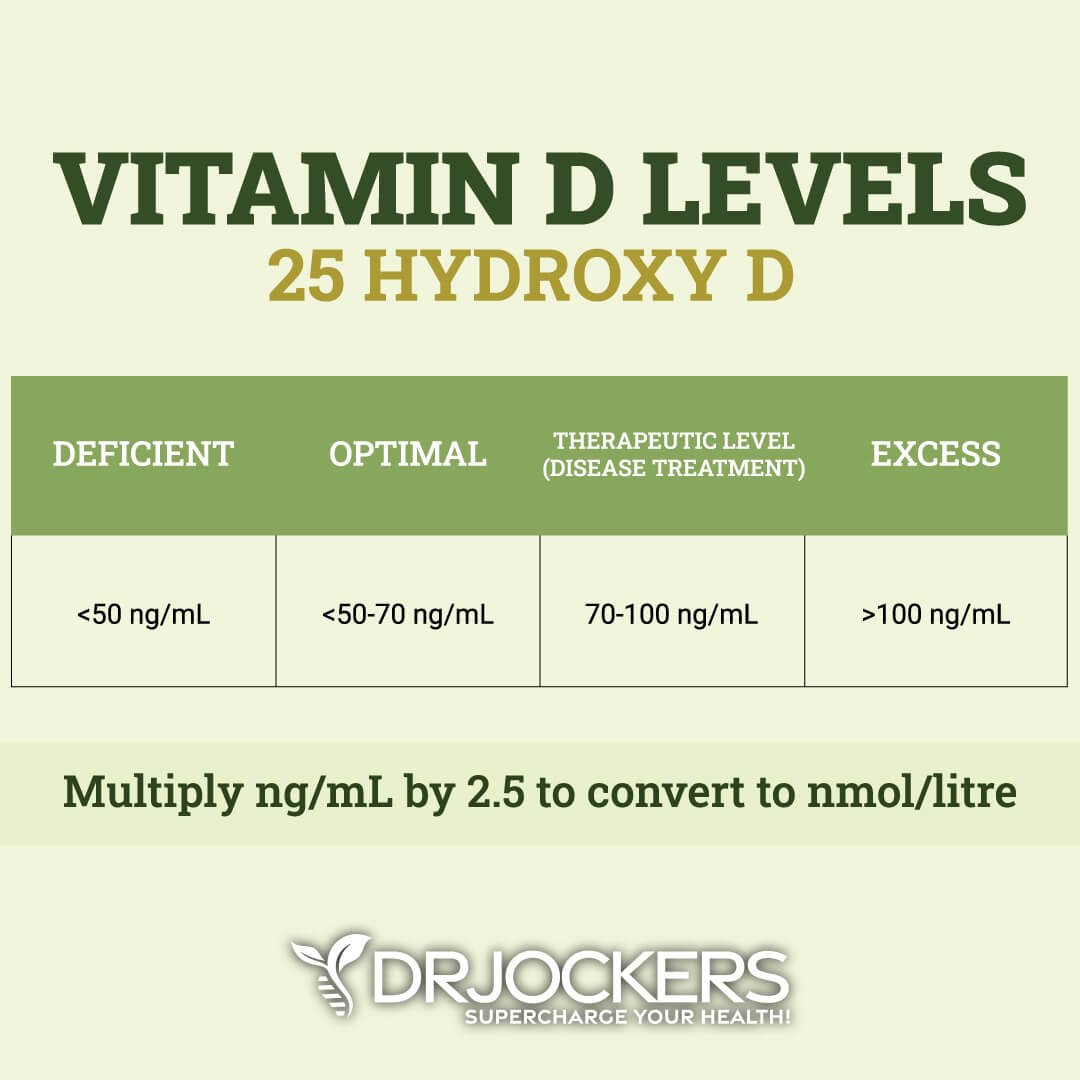
Vitamin D Deficiency: People who are deficient in vitamin D (have levels lower than 40 ng/ml) are significantly more likely to develop chronic inflammation and autoimmunity (16).
Upper Cervical Subluxation: The occiput which is the bottom of the skull and the atlas, the first bone, both play a key role in the information coordinated between the brain and immune system. Subluxation at this joint creates a rotation to the top of the spinal cord resulting in compression and increased inflammation in the body (17).
The Microbiome and Lupus:
The gut plays a major role in the health of the immune system because it supports nutrient absorption and detoxification. More than 1000 unique species of bacteria make up the gut microbiome. An overgrowth and depletion of certain bacteria is evident in individuals with lupus. Researchers have found that individuals with low levels of beneficial Lactobacilli and bifidobacterium and increased levels of the butyrate producing Lachnospiraceae were present in the early onset of lupus development (4).
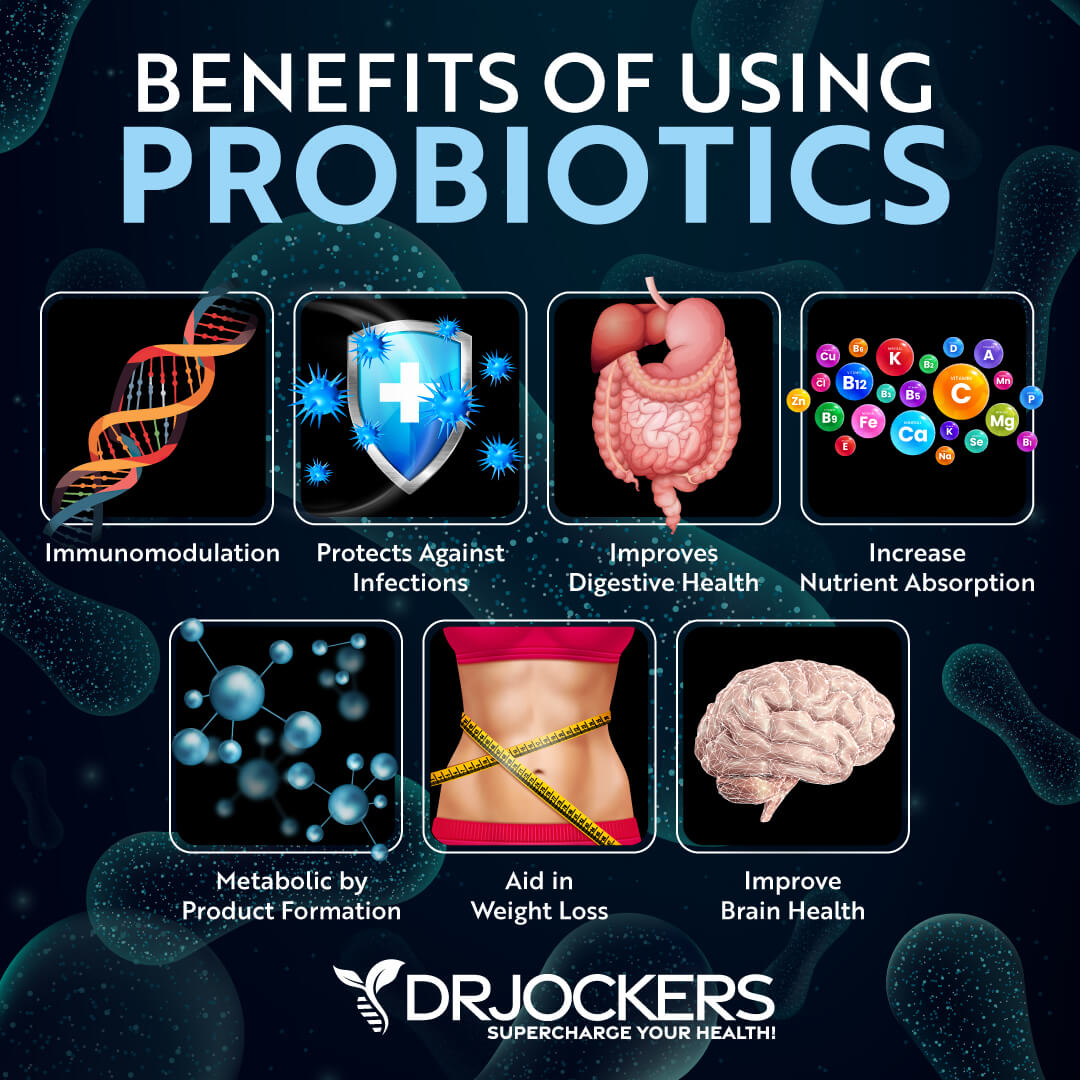
Individuals with lupus are recommended to take a daily probiotic and consume probiotic rich foods. Adding healthy probiotics rich in Lactobacillaceae bacteria can exhibit anti-inflammatory effects by suppressing pro-inflammatory T cells and interleukins and stimulating Treg cells to regulate immune cell homeostasis. (4)
Raw and organic vegetables are also an excellent choice to heal gut issues. Avoiding unnecessary toxins is required to balance gut flora, improve digestive motility, remove toxins and reduce inflammation. Raw vegetables improves homeostasis by promoting an alkaline environment that is not susceptible to disease.
Prescription Drugs Influence Microbiome:
Unfortunately, many prescription medications used to manage lupus symptoms include immunosuppressive drugs which can increase the microbial imbalance in the gut. Drugs like Cytoxan (cyclophosphamide) and Rheumatrex (methotrexate) suppress inflammation by reducing the body’s own ability to fight off infection.
Steroidal drugs cause a variety of side effects which can also upset the microbiome and have damaging effects comparable to antibiotics. In fact, researchers have found that certain drugs promote a bacterial environment within the gut that despite not being classified as pathogenic, can still promote arthritic symptoms in autoimmune diseases (3). Individuals genetically predisposed to lupus are also more likely to harbor commensal gut bacteria which promote autoimmunity (19).
Anti-Inflammatory Diet and Lifestyle:
A lifestyle supplemented with anti-inflammatory foods and exercise can help to naturally treat lupus. Poor digestion resulting from a diet with reactive and inflammatory foods puts the body in a hyperimmune state that is highly reactive. Such a disruption can further create hormonal upset, toxicity and essentially a weakened immune system.
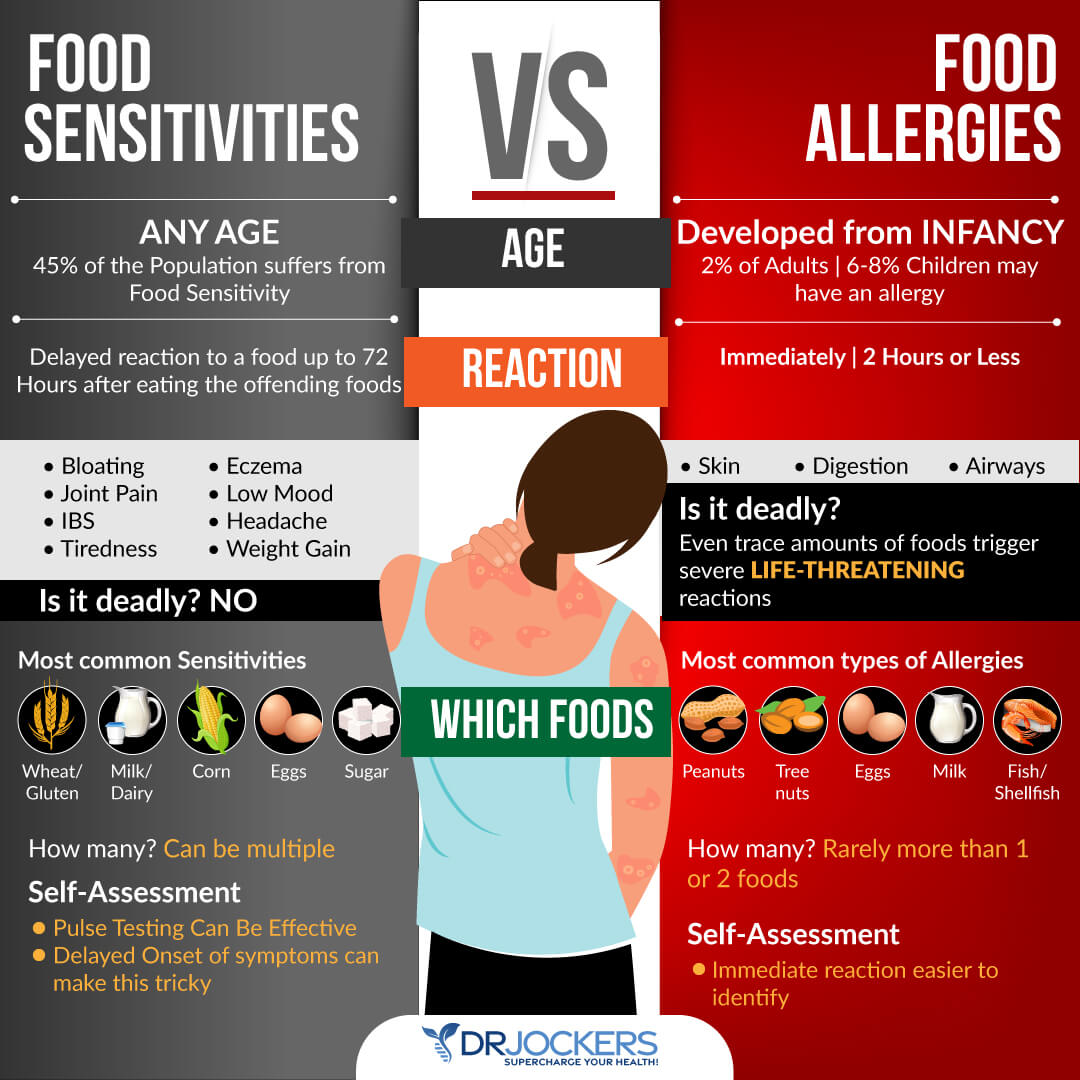
Some of the risk factors for lupus include a diet limited in adequate nutrients, food allergies and sensitivities, and gastrointestinal disturbances which may manifest as leaky gut syndrome. Individuals with lupus should consider regular low-intensity exercise to reduce symptoms such as depression, fatigue and improve cardiovascular fitness and overall health.
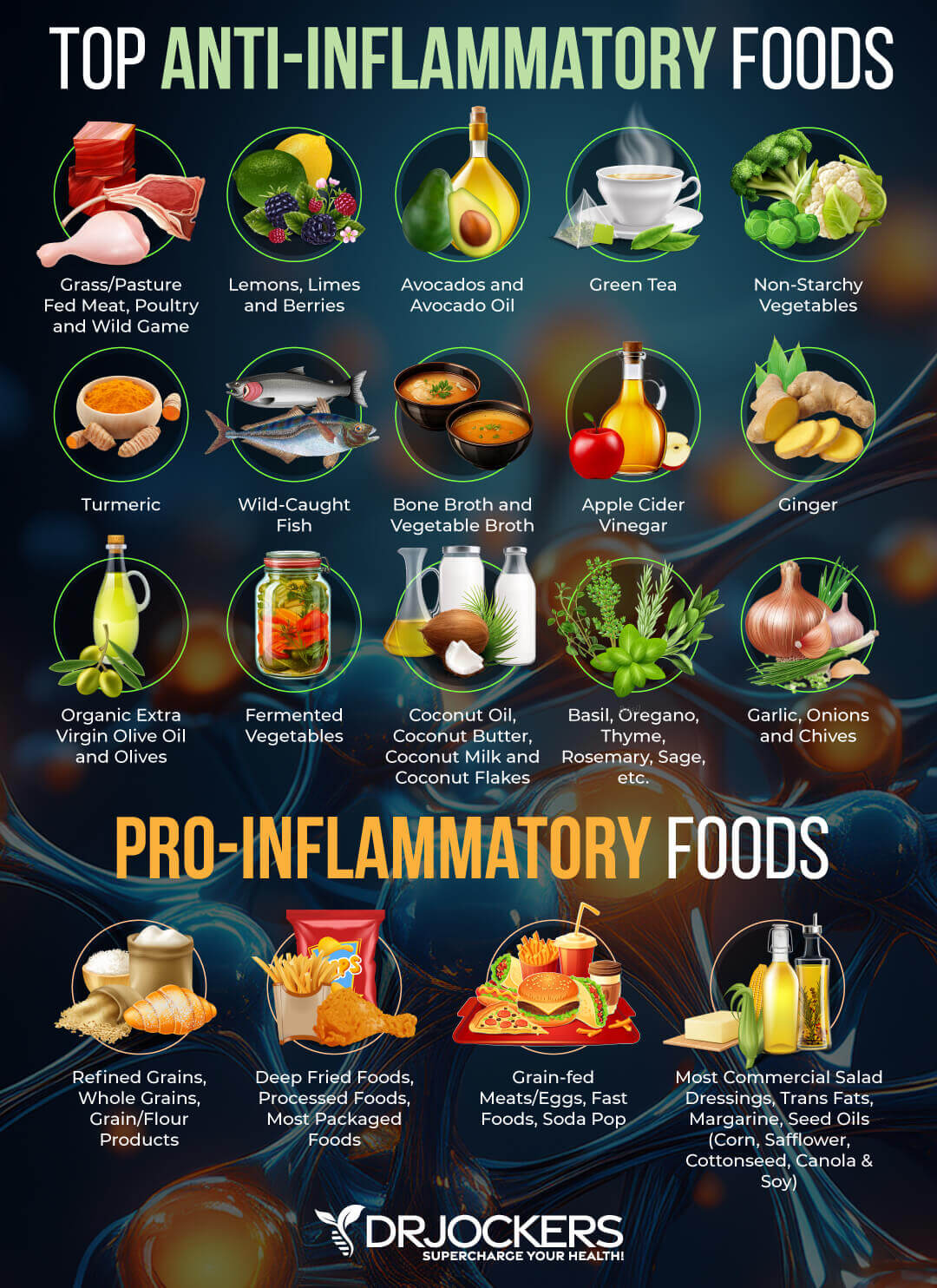
Treat lupus symptoms naturally by consuming a diet full of anti-inflammatory foods and healthy fats such as coconut oil, avocados, olives, vegetables, herbs and wild caught fish like salmon and sardines. Supplements to consider in the treatment of lupus include vitamin D, fish oil, b vitamins and probiotics. (1)
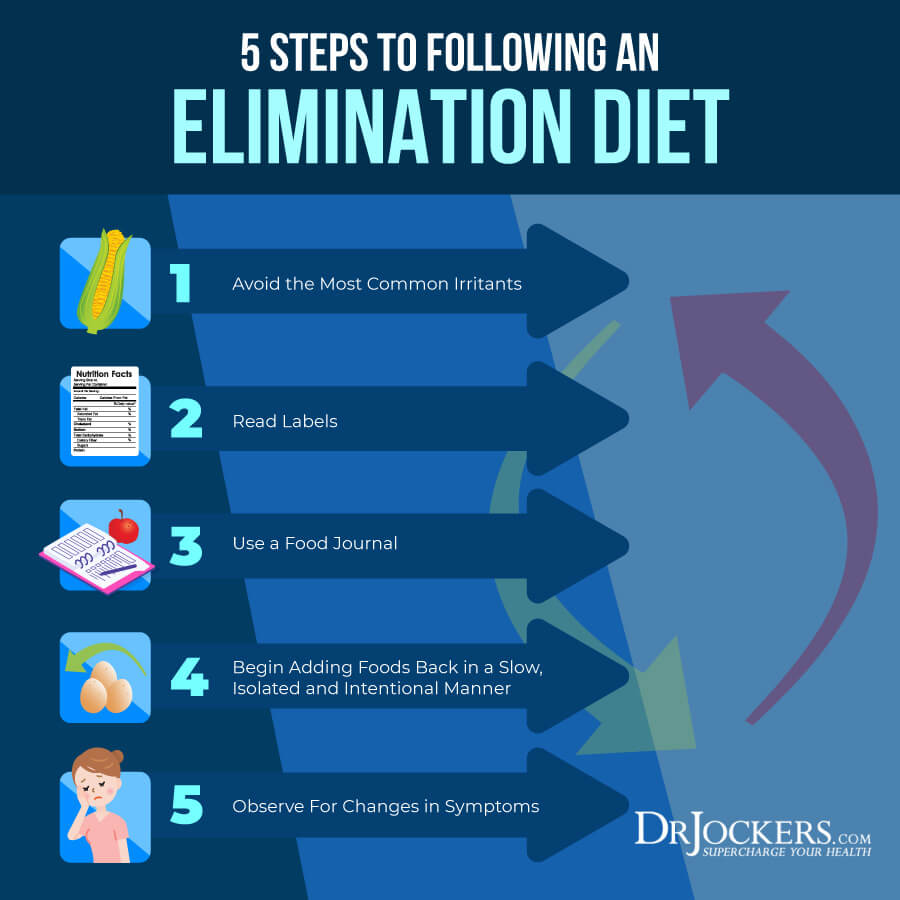
One of the best approaches for individuals with lupus is to follow an elimination diet where you eliminate the most common food irritants and any other suspicious foods for a few weeks and then slowly and intentionally add them back in in order to see if they trigger an inflammatory reaction. This article goes into more detail on this.
Foods and Activities to Avoid:
People with lupus should avoid foods hard to digest such as gluten and legumes. Foods which can increase inflammation in the body such as sugar, trans-fat, alcohol and caffeine should also be limited if not avoided. To reduce symptoms of lupus it is beneficial to consume 1 to 2 cups of bone broth daily.
Individuals with lupus should limit exposure to the sun as ultraviolet rays can trigger an autoimmune reaction. They should still aim to get 15 minutes of quality sunshine daily as that level is very beneficial for the immune system. However, try to avoid more than 30 minutes of direct sunshine as this can cause skin inflammation and a butterfly rash reaction for individuals with lupus.
Incorporating certain foods into your diet is an excellent way to improve the moisture of your skin. Healing foods that provide relief from dry and irritated skin from the inside out include coconut oil, avocado, green tea, cucumbers and omega 3 rich walnuts, almonds and flaxseeds. Patients who smoke are strongly advised to quit as this habit increases the strain on the cardiovascular system and can exacerbate symptoms of lupus. (1)
One supplement that can be very helpful for individuals with lupus is a good quality bone broth or collagen protein which provides key amino acids that support the gut and the tissues that are most commonly affected by lupus.
Mitochondrial Dysfunction and Lupus:
Mitochondria are present within each cell to supply the body’s energy demand. These powerhouse organelles are major sites of oxidative stress due to the high production of reactive oxygen species ROS (reactive oxygen species) and RNS (reactive nitrogen species). Each promotes free radical damage and further oxidative damage to cells and tissue resulting in chronic inflammation and autoimmune symptoms.
Prolonged increased stress to cells depletes the body’s biological abilities to protect against oxidative damage. Mitochondrial dysfunction in lupus patients is associated with reduced glutathione and SOD (superoxide dismutase) levels as well as abnormal energy production. (20)
Natural Support Strategies for Healthy Inflammation
Here are the best action steps to get started with on your journey to improve your inflammatory response. These strategies are not at this time FDA approved to prevent, mitigate, treat or cure systemic lupus and should not be confused as such. You should always consult with your physician before stopping or changing medications or taking on new health strategies.
Additionally, you should be working with a functional health practitioner to help guide you through these strategies. This is not an exhaustive list and there are other natural therapeutic strategies that I and functional health practitioners will utilize to help individuals with rheumatoid arthritis.
Anti-Inflammatory Diet
Good nutrition is always important for any health condition. There are foods that can cause inflammation and intestinal permeability, both of which contribute to various health problems.
An anti-inflammatory, healing diet removes foods that cause inflammation and damage the gut lining. Instead, your diet should include organic, non-GMO vegetables, fruits, healthy fats, and clean protein. This will help to reduce inflammation, stabilize your blood sugar, reduce your toxic load, and support healthy blood pH levels.
Many people with Lupus have nutrient deficiencies. An anti-inflammatory healing diet is nutrient dense and will help to supply your body with the nutrients it needs.

Foods to Avoid with Lupus
It is important to avoid highly inflammatory foods. Pro-inflammatory foods include:
- Refined sugars and grains (and any foods that are easily metabolized into sugar)
- Conventionally raised meat and dairy products
- Gluten-containing foods
- Farmed fish
- Processed foods
- Highly processed vegetable and seed oils, such as canola, grapeseed, and safflower
- Foods with additives and preservatives

Foods to Include
The foods you should be eating on an anti-inflammatory, healing diet are whole, unprocessed foods. Choose grass-fed and pasture-raised meats and wild-caught fish. Include a variety of low to moderate carbohydrate, lower glycemic, colorful vegetables and fruits for their abundant antioxidants and phytonutrients. Plentiful amounts of herbs are a powerful addition to a healing diet.
Healthy fats are a very important part of a healing diet. Healthy fats are found in coconut, olives, avocados, and their oils and in grass-fed butter and ghee.
Omega-3 fatty acids and conjugated linoleic acid (CLA) found in wild caught salmon and grass-fed beef and dairy are fats with many health benefits. These healthy fats are an efficient source of fuel for the body to combat inflammation.
Test For Food Sensitivities:
Most people with autoimmune conditions have leaky gut and food sensitivities. These sensitivities can be hard to pinpoint as they result in delayed symptoms that are not life threatening.
The most common food sensitivities include gluten, corn, dairy, soy, peanuts and sugar. Some other potential food sensitivities to consider include all grains, eggs, nuts, seeds and nightshade vegetables (tomatoes, potatoes, peppers and eggplant).
It can be helpful to do a 28-day elimination diet where you remove all of these and then slowly add these back in one at a time. You can also do both biofeedback and blood testing to determine what foods are causing stress in your system and an elimination diet to test how you are responding to eliminating certain foods for periods of time. You can also
Intermittent Fasting:
Intermittent fasting is a form of fasting cycles between not eating (fasting) and eating (feasting) over a period of time. The benefits of intermittent fasting benefits include cellular repair, autophagy, immune regulation, inflammation levels, and insulin sensitivity.
It also helps to lower the risk of developing autoimmune and chronic inflammatory conditions such as Lupus. Going 16–18 hours between dinner and breakfast is one of the best ways to improve mitochondrial production. Your body improves energy efficiency by increasing and strengthening the mitochondria during periods of fasting. Consume your meals in a 6-8 hour window such as 11am–7pm or 12–6pm.
When you do this, you enhance cellular healing and joint cell regeneration. Fasting also helps enhance regulatory T cells which calm the immune system and keep inflammation under control (18). To learn more about the benefits of intermittent fasting and best intermittent fasting practices, I recommend this article.
Reduce Stress:
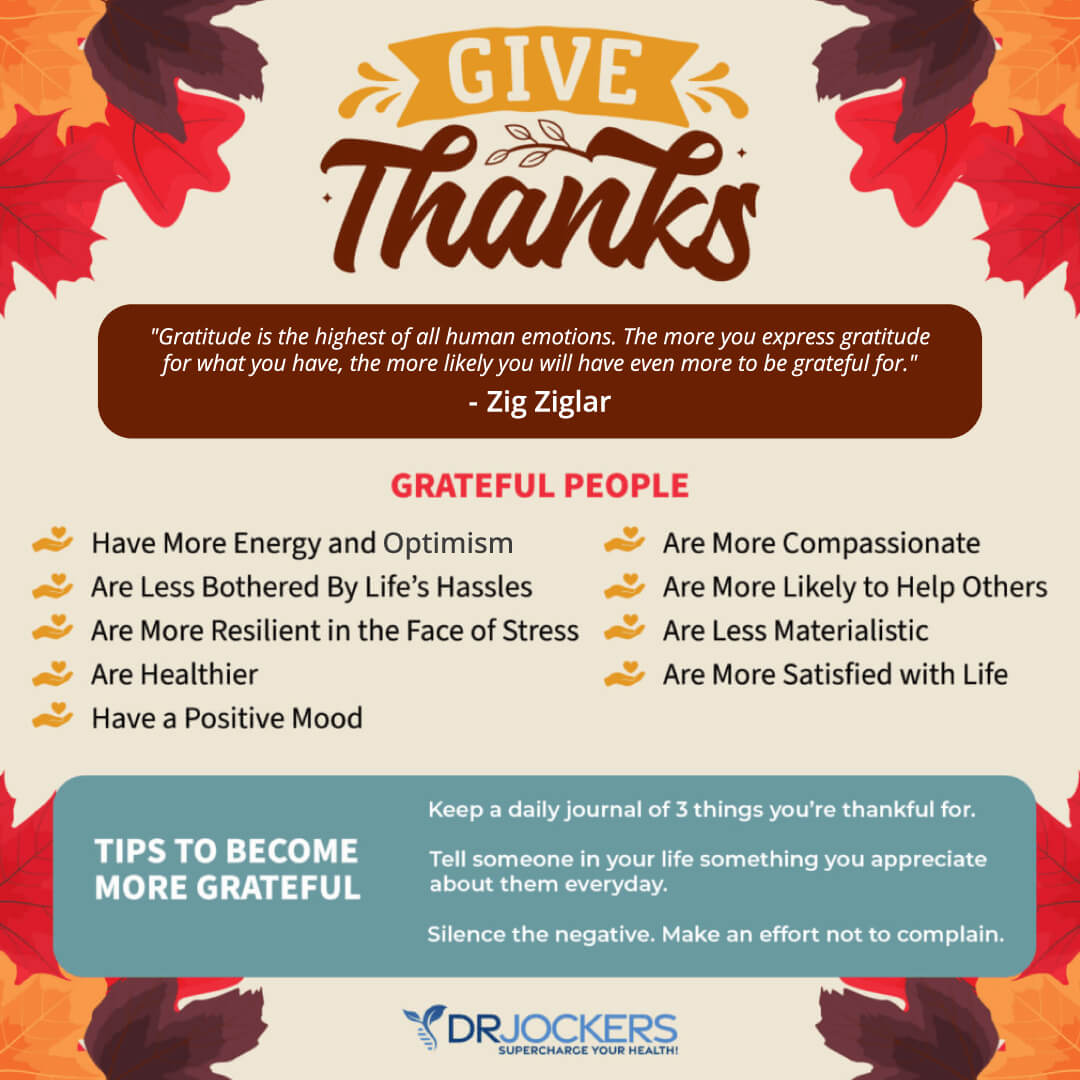
Reducing stress is a critical for reducing inflammation and improving immune health. I recommend that you reduce stressors from your life as much as possible. Turn off the news, and only look at it once a day or a few times a week for a specific period. Reduce your social media use and time on the internet.
Avoid people and situations that bring you down. Surround yourself with loving and uplifting people. Engage in uplifting and relaxation-promoting activities. Read, try some arts and crafts, play cards or board games, sing, and dance.
Spend time in nature and do some grounding walking barefoot on grass. Practice daily gratitude and try positive affirmations. Practice self-love and laugh with friends and family. Meditate, pray, journal, and try daily breathing exercises. Be grateful and smile more.
Improve Your Sleep:
Prioritizing good sleep is just as important as reducing your stress levels. Develop a regular schedule going to bed and getting up at the same time every day to support your circadian rhythms.
Avoid electronics, sugar, caffeine, heavy foods, and stress close to the bed. Engage in relaxing activities, including stretching, relaxing baths, meditation, and prayer. Make sure that you have a supporting bed, pillow, and bedding, and sleep in a dark calming room.

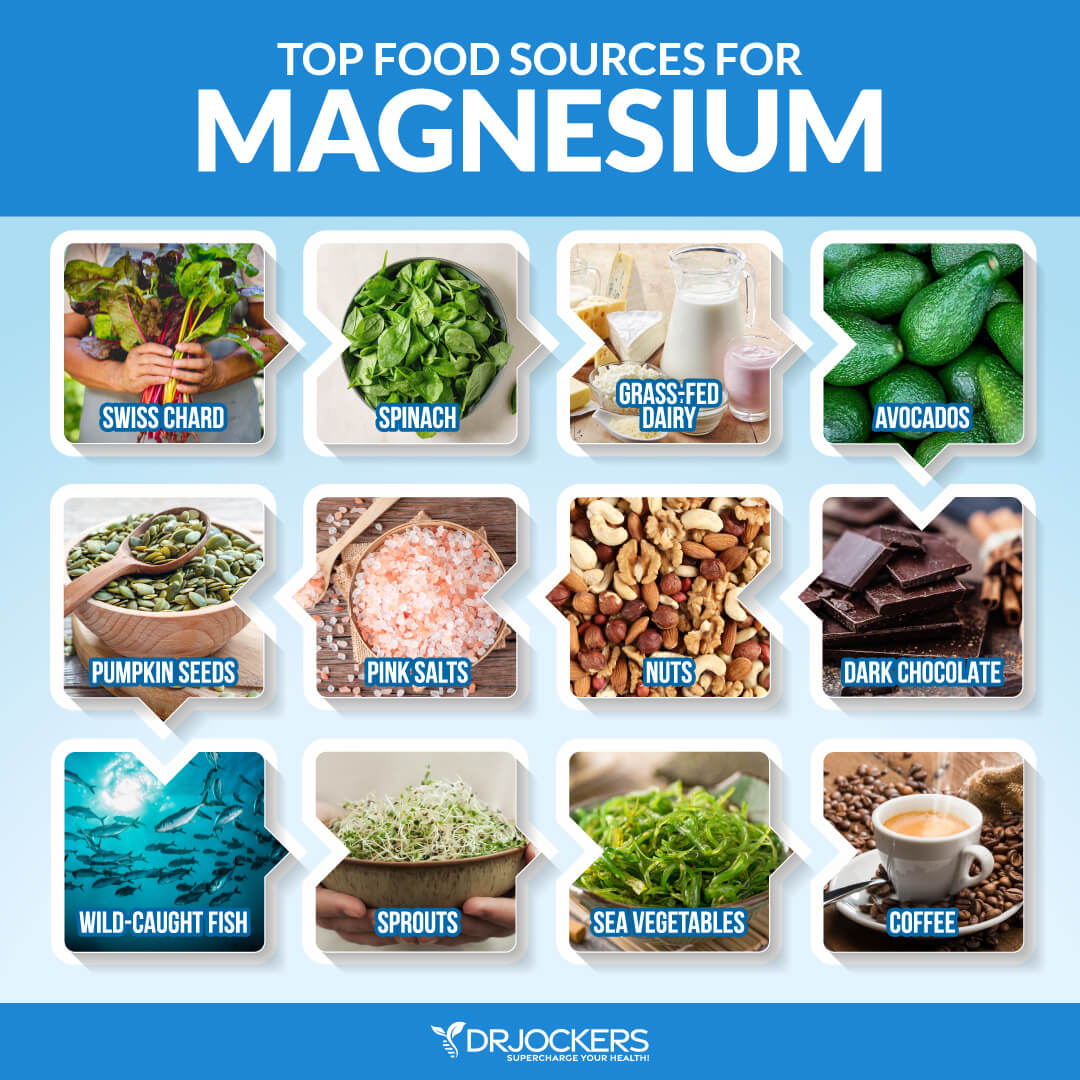
Include Magnesium & B Vitamin Rich Foods:
Magnesium helps to improve blood sugar signaling patterns and improves mitochondrial health. The best magnesium and B vitamin rich foods include dark green leafy veggies, avocados, grass-fed animal products, raw cacao and pumpkin seeds.
You can also do Epsom salt baths to support your magnesium levels. It would also be wise to supplement with a good magnesium and B complex supplement. Look for magnesium L-threonate which is the best form of magnesium for crossing the blood brain barrier.
When it comes to B vitamins, it is best to look for one with pre-activated forms such as methyl-folate, methyl-cobalamin (B12), Pyridoxal-5-Phosphate form of B6, and Riboflavin-5-phosphate form of vitamin B2. The methyl groups are in the active form and will be better utilized by the body.
Focus on Deep Breathing:
Improving your posture, seeing a high-quality chiropractor and optimizing your breathing patterns is highly recommended. Taking time to slow down your breathing and take long-deep breaths for a few minutes every hour will help reduce the sympathetic, fight or flight part of the nervous system.
The better we breathe, the better we will heal and the more blood flow we will get, and the better our immune and inflammatory health will be. Follow these tips here to improve your breathing patterns.
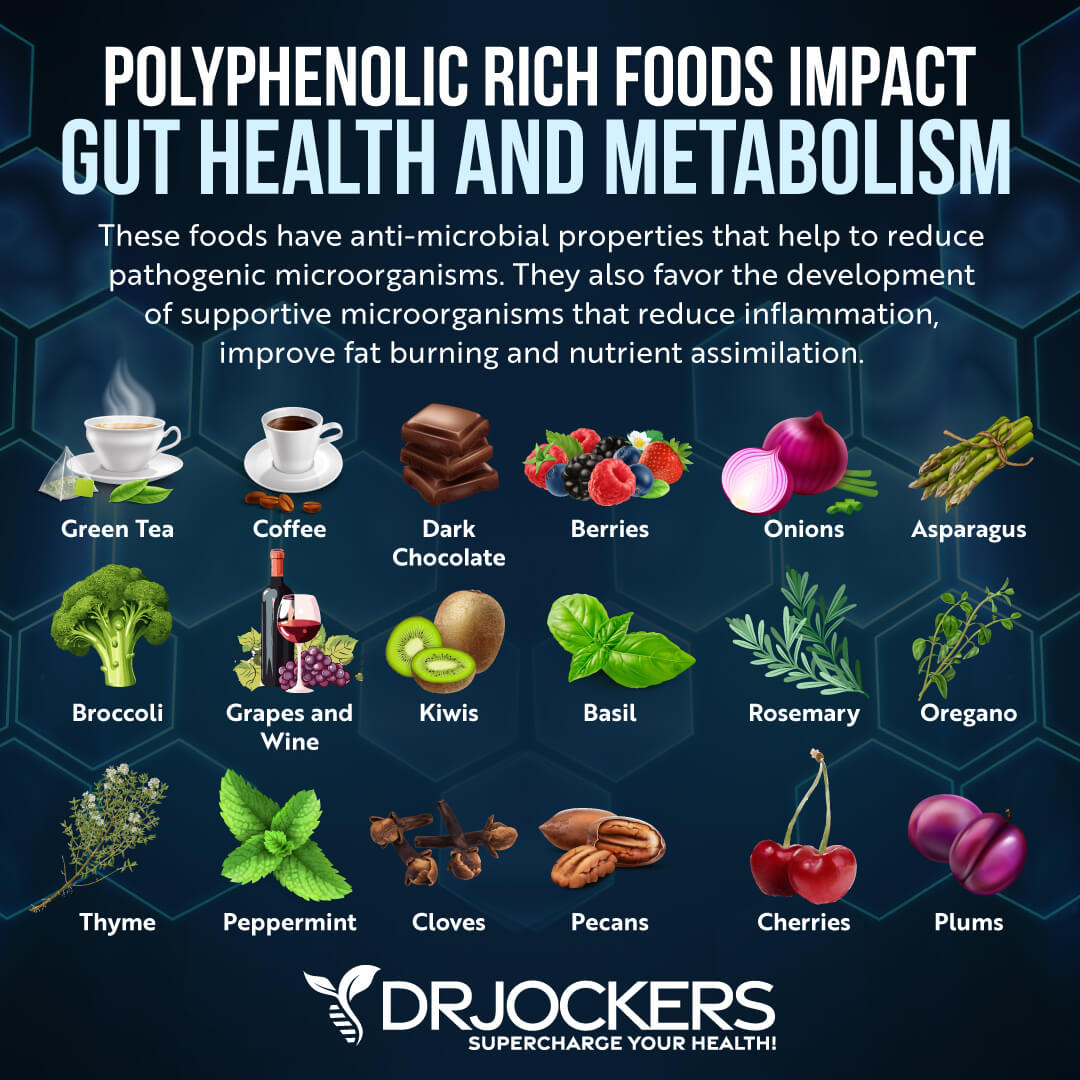
Use Antioxidant Rich Herbs:
Carminatives are herbs that help to improve digestive health by reducing pathogens in the gut, stimulating the production of stomach acid, bile and pancreatic enzymes and modulating the gut microbiome.
Examples of these herbs include turmeric, ginger, oregano, garlic, basil, thyme and rosemary. These herbs help to improve digestion, reduce inflammation and support a healthy brain. There are a number of ways to use these that I discuss in the following image. I like putting the herbs on foods, using herbal teas, fermented foods and essential oils.
Ground Your Body:
In our society we are surrounded by toxic electromagnetic frequency’s (EMF’s). These EMF’s increase stress and inflammation within the body and can be a trigger for autoimmune activity for some individuals.
By going outside daily and walking barefoot on grass, dirt or sand you absorb natural EMFs from the ground that balance your electrical rhythms. Follow the steps in this article here.

Supplement With Omega 3’s:
Omega 3 fatty acids and in particular the long chain variety EPA and DHA are critical for stabilizing blood sugar, reducing inflammation and autoimmunity improving joint health. Consume grass-fed meat, grass-fed butter, wild-caught fish, seafood and spirulina to get it in your diet.
Plant based omega 3’s such as flax oil only contain the small chain omega 3 called ALA and do not have any DHA. It is very hard for our body to convert ALA into DHA so it is best to get a high-quality fish or krill oil that is rich in EPA and DHA. You want to find a brand that is molecularly distilled to take out any heavy metals and other unwanted contaminants.
Be sure to discuss with your physician before using as fish oils have a blood thinning affect and can be contraindicated if you are on blood thinning medications.
Improve Your Mitochondria:
The mitochondria are the energy powerhouses of every cell. When someone has an autoimmune disorder, it is a clinical sign that they have dysfunctional activity going on in the mitochondria.
Support your mitochondria with clinical doses of CoQ10, L-carnitine, N-acetyl cysteine, creatine monohydrate, B vitamins, magnesium, alpha lipoic acid and D-ribose. You can find mitochondrial support supplements that have most if not all of these key nutrients.
Optimize Your Vitamin D:
Low vitamin D3 is associated with chronic inflammation and autoimmune conditions. Vitamin D is arguably one of the most powerful nutrients responsible for modulating and coordinating the immune system.
In autoimmune disease, the immune system has a hard time differentiating self from non-self (foreign invaders). Vitamin D helps the immune system make this important distinction, which reduces autoimmune disease formation (25). Vitamin D also helps to modulate the immune system to reduce inflammation throughout the body (26).
Support Gut Health
In order to reduce inflammation and autoimmunity, you have to repair and heal your intestinal lining. I recommend eating a gut friendly diet that works best for your body type. For some individuals with RA, a low oxalate diet is very helpful.
Consuming liquid nutrition for is great for stimulating the digestive process, increasing nutrient absorption, and improving gut health. Liquid nutrition does not require as much energy to digest, so your body can focus on healing and repair. You can combine liquid nutrition with fasting strategies for quicker healing.
Using a good quality bone broth collagen in a shake or smoothie is a great way to include liquid nutrition in your diet. Collagen contains amino acids, including glycine and glutamine, which are essential for healing leaky gut. These amino acids seal the holes in the gut by healing damaged cells and building new tissue. Collagen also makes up the villi, small finger-like structures on the intestinal wall and assists with water absorption in the intestines.
Additionally, I recommend taking a daily probiotic supplement. Probiotics helps to optimize your gut health and improve your nutrient absorption while reducing gut related inflammation. When gut inflammation goes down it also reduces inflammatory mediators that impact joint health.
Reduce Toxin Exposure
Reducing your toxic exposure is critical for improving liver function and reducing inflammation. Buy organic food as much as possible. Stop using conventional beauty, body, and household products, and replace them with organic, natural, or homemade alternatives.
Use glass, stainless steel, wood, and bamboo products instead of plastic. Spend time in nature and breathe in the fresh air. Use a good indoor air filtration system. Make sure that you drink clean, toxin-free water by using a high-quality reverse osmosis system. Add a slice of lime and pinch of salt for some extra flavor, electrolytes and antioxidants.
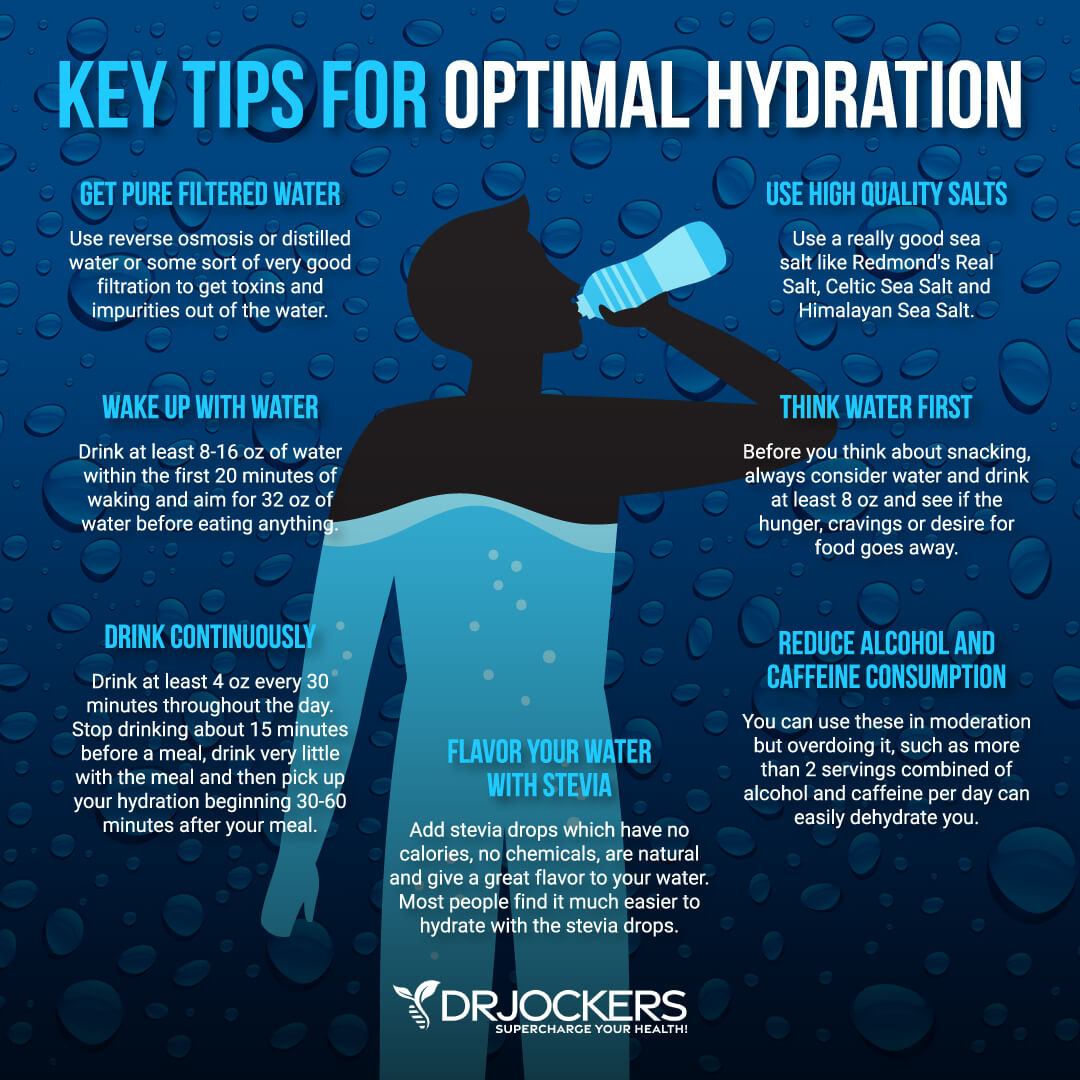
Support Detoxification Pathways
It is not enough to put good things into your body, you have to make sure that the bad things come out as well. Drink plenty of water to support detoxification through sweating and urine. Support your detoxification pathways to protect your body from brain inflammation.
I recommend using infrared saunas to promote detoxification through sweating. Try rebounding and dry-skin brushing to support your lymphatic pathways. Support two major detoxifying organs, your kidneys and liver with herbs like milk thistle, parsley, dandelion and bioactive carbons which can penetrate and remove toxins from deep within the tissues and cells.
Final Thoughts
Rheumatoid arthritis is a serious issue that affects millions of people around the world. The symptoms of RA include joint pain, impaired joint function, fever, weight loss, anemia and fatigue. To protect yourself from chronic inflammatory and autoimmune conditions, follow the recommendations in this article. You may notice improvements in your pain, energy and overall health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



This was an informative well put article
Thanks for reading Grace!
My niece suffers with lupus the reason for my research…
Can you recommend an all-in-one supplement for people with SLE, or can you tell me dosages for each supplement? I’ve been suffering with headaches for over 2 years and all I can do is eat ibuprofen like candy for relief, which I know will cause future scary effects. It’s the only thing that works, even after having 2 MRIs and nothing being found.
Hey Erica, Unfortunately there is no all-in-one supplement for this. It comes down to using lifestyle and dietary strategies along with targeted supplementation depending on each person’s particular situation. If you would like help putting together a comprehensive plan or some more specific guidance on supplements, feel free to send an email to michael@drjockers.com
Hi good evening,
My sister has been diagnosed with SLE and recently experienced continuous seizures. She is hospitalized and in the ICU.
The seizure is in control but her response to the doctors while not being sedated. I am hoping if you can advise on how I can assist her on this matter.
Thank you
A ketogenic diet and Magnesium supplementation may be helpful here: https://store.drjockers.com/products/brain-calm-magnesium
As rheumatologist taking care of lupus patients I try to cover all areas of well being – not just the physical part.
Your tips are important for a healthier lifestyle – I think it is a bit misleading saying we can heal lupus Naturally. Unfortunately we can’t, and patients and family should be aware of that.
So: healthy lifestyle and diet, vitamin D, above all stop smoking…but then trust your referral Rheumatologist: he/she is in charge to take care of you. And will do in the best way , using necessary drugs and doing the possible to taper them safely when appropriate.
Dr Mariele Gatto
Unit of rheumatology
University of Padova
Italy
Thank you for your valuable input Mariele!
Dr.Jockers,is it possible to heal lupus naturally? Please let me know…why the above doc saying something different?I’m confuse..
Dr. Brooke Goldner. Look her up.
Thanks for sharing!
I’ve stumbled upon this page after my mother’s co-worker died of heart attack – lupus complication, at the age of about 50. This information is of course helpful, however as good as it is, from my point of view it should focus much more on eliminating the real cause of lupus and almost every other chronic disease – which is internal toxicity.
And what is the best toxicity elimination – fasting, especially water or even dry fasting. Fasting, coupled with good diet can create “miracles” and free from disease even people suffering for their entire lives – it all comes to perseverance, desire and willingness to make some radical changes in their lives in order to be free of lupus or any other disease.
I doubt that 16 hours of daily intermittent fasts even for years can completely cure patients, only to alleviate the symptoms.
However, this article is still much better than many I’ve read before!
Dr. Jockers,
HELP please! I have years of unanswered health problems. Onset of a migraine 6 years ago that lasted 4 days turned my life into a nightmare. I’m pretty much home bound , severe chronic pain, seizures out of control , essential tremors, internal vibrations, fibromyalgia chronic fatigue, severe body pain neuropathy , Periodic paralysis, H2 histamine levels out of control, abdominal pain constant, blood in urine and kidney issues, Burning sensation throughout my extremities , opcitipcal neuralgia, colitis , Auto immune disease, severe head pain, muscle and joint pain, body fatigue , hair loss , Chills, hard to breathe, food sensitivity and rash on face now! I’ve been on so many antibiotics, steroids, I am now going to get blood work for lupus. There is so much more my body is just shutting down and the doctors seem to be a loss and I’m losing hope. I have sensitivity to medication and foods.
I was perfectly normal one day and the next day my world came to an end it feels like!
If you would like to privately inbox me if you can help me or give me guidance I would greatly appreciate it .
I cannot been the only one out there suffering like this. I need help !
I’m only 50.
Thank you, Teresa
Sorry for the typos and miss spelling! It’s 4 am and I did not proof read. I just went to typing and text talking. You get my point either way. I really need medical help, changes, perhaps something that they maybe over looking ?
Hi, Teresa,
I’m not Dr. Jockers, but I think I may be able to give you some advice.
Only fasting can probably save you! – try water, and if that doesn’t help – dry fasting. Don’t be afraid of it, it’s the most ancient, natural and effect way to get rid of health issues, coupled with moderate exercise(walking) it can make miracles. Just try it, you have nothing to lose.
Hello, i have a question regarding fasting. I’ve been diagnosed with lupus, but i have no many complications (overall i can keep on living my life normally). Anyway, my reumathologist has told me not to use hormonal contraceptives because of estrogen. If i start a 16:8 IF won’t it mess with my hormones? Thanks.
Hey, i just want you to see this article. Is pretty much a spanish translation of your work. I trust yours is the original because it contains references and his doesn’t. https://temassobresalud.com/lupus-eritematoso-sistemico/
I was diagnosed with skin lupus in 2007. I for the last year and a half had a breakout that won’t go away. My diet is very good don’t eat junk. I take vitamin D, magnesium, vitamin C, B12, and bone broth everyday. My lupus doctor put me on a med that made me vomit every time I took it. Am on plaquenil 2 a day. Am at the end of my rope. What can I do?
Brenda Morris
Hey Brenda, you may need a more in-depth autoimmune protocol. I would take a look at your food sensitivities, gut analysis (GI MAP), and an Organic Acids Test. Otherwise I would say try to implement the strategies in the article as closely as possible. For one on one coaching advice you can reach out to michael@drjockers.com
Dr. Kickers
Thank you for getting back to me. I am going to do your one on one. But what can I do to naturally suppress my immune system to get this out break under control?
Thank you
Brenda Morris
Control sources of inflammation by following the strategies in this article. Beta-Glucan can be very helpful as well.
Hi Dr. Jockers,
Thank you for this in-depth article! I know you can’t promise results and every body is so different, but how long being on an AIP diet and working on healing your gut does it take for your body’s symptoms to go back down? I understand that normal or healed may take years, but how about just relief right away? Thanks!
Hey Marlana, this highly depends on the individual. Sometimes within a week and sometimes several!
There are only a few types of lupus that can go away permanently, Medication induced and pregnancy induced. All other types your stuck with. Lupus never goes away. There are NO magical cures for this. Only thing to do is to eat right, take your meds, live a healthy life.
Yes that is true that there is no medical or magical cure. However, it is possible to put the symptoms into remission.
I know you can’t promise results and every body is so different, but how long being on an AIP diet and working on healing your gut does it take for your body’s symptoms to go back down?
It is different for each person, but many people feel significantly better in 4-6 weeks.
The article mentions garlic, but aren’t Lupus patients are supposed to avoid anything that stimulates the immune system?
Garlic won’t stimulate the immune system enough to activate autoimmunity. It will help to balance the immune system and bring down autoimmunity.