 The Appendix: How Important Is This Organ?
The Appendix: How Important Is This Organ?
You’ve probably heard about the appendix. Chances are, you know someone who had their appendix removed due to appendicitis. But what is the appendix anyway. Many believe it’s a useless organ. But is it really? It turns out the appendix is not useless but may play an important role in your microbiome health.
In this article, I want to talk about the appendix. You will learn what the appendix is and how the appendix functions. You learn about the connection between your microbiome and your appendix. You will learn how the appendix may reduce the risk of C diff infections.
You will learn about the signs and symptoms of appendicitis. You will understand the risk factors for appendicitis. I will go over the top root causes of gut inflammation. I will share the GI Map Test I recommend for gut testing. Finally, you will learn about the 5 R’s to healing gut inflammation.
What is the Appendix?
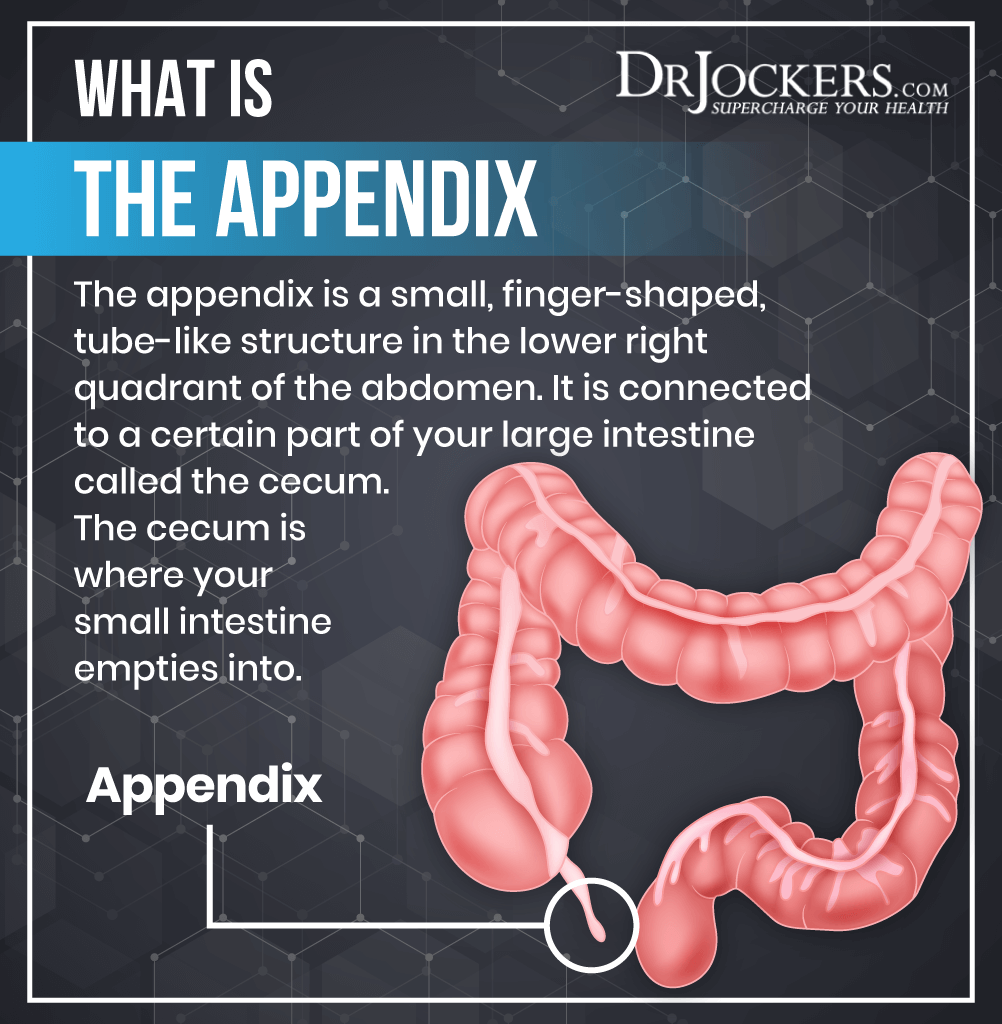
Your appendix is a small, finger-shaped, tube-like structure. It is connected to a certain part of your large intestine called the cecum. The cecum is where your small intestine empties into. The size of your appendix corresponds with the size of your colon and cecum. It looks like a small pouch right where your large intestine begins.
Your appendix can be found in the lower right portion of your abdomen. Doctors also refer to this section as McBurney’s point. If there is tenderness or pain when applying pressure to this point, your doctor may want to check for appendicitis, an inflammation of the appendix.
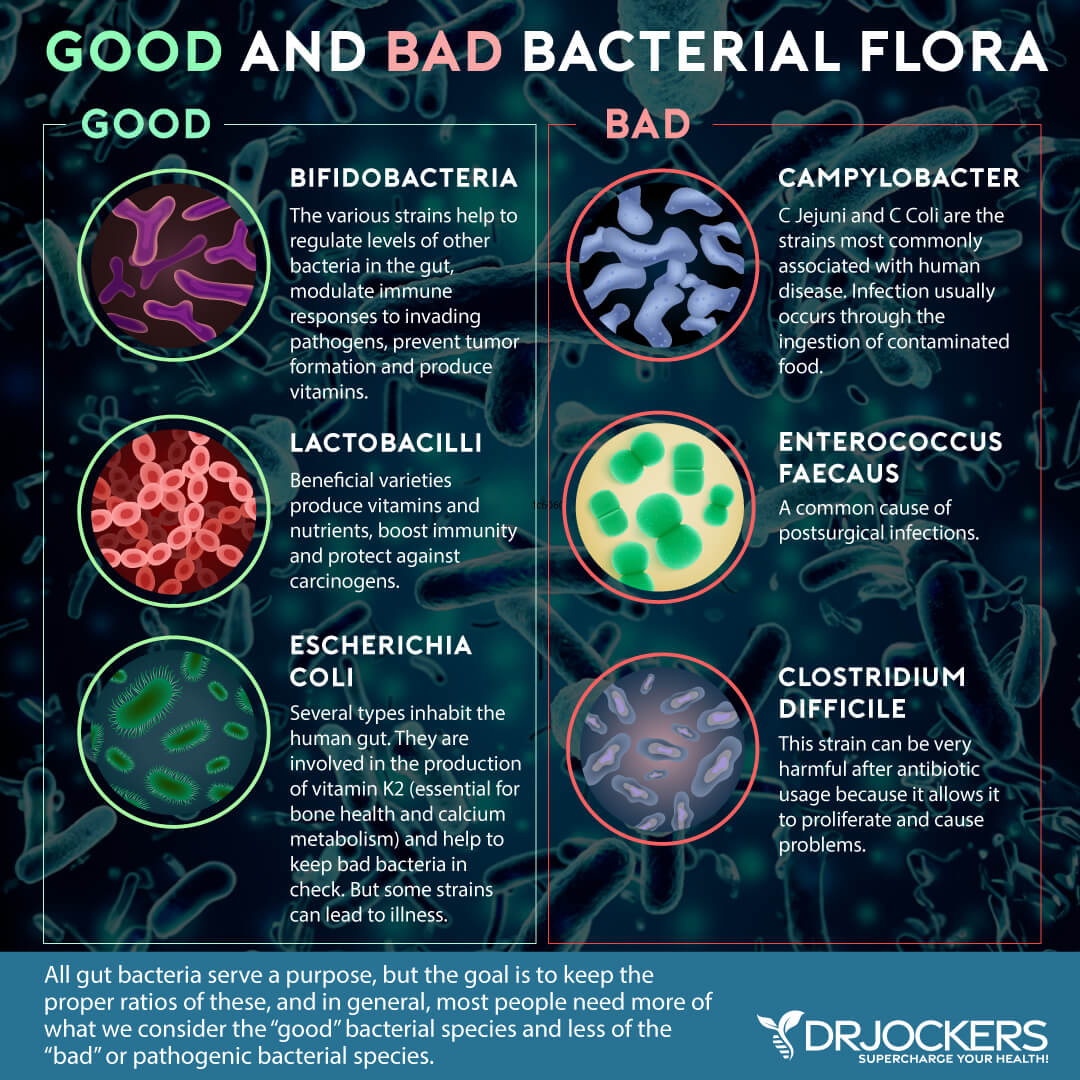
When doctors remove the appendix due to appendicitis, most people don’t suffer harm. For this reason, for the longest time, medical sciences considered the appendix to be an unnecessary ‘vestige’ organ that is simply an evolutionary holdover. Moreover, the appendix can’t move any waste or food through the intestinal tract, which also makes it seem unnecessary. However, as you will find in the next section, newer research is taking a different view on the appendix (1).
How The Appendix Functions
The appendix may not be as useless as once thought. What’s the function of the appendix, then? According to the National Cancer Institute Center for Cancer Research, the structure may indicate that it helps the movement and removal of waste from your gut (2). Other research also indicates that it may play a role in gut health.
A 2013 study published in Comptes Rendus Palevol has found that the appendix may play a role in microbiome balance and gut health (1). Researchers described the appendix as “a microbial safe-house under selection pressure from gastrointestinal pathogens potentially transmitted via a range of mechanisms rather than via a single mechanism dominated by a particular dietary or social factor” (1).
The Microbiome and the Appendix
A 2009 study published in the Journal of Evolutionary Biology has also looked at the evolutionary model of the appendix (3). They looked at the structure, function, and genetic composition of the appendix in various mammalian species over the past thousands of years and also the human appendix. The research shows that it’s not an accident that the appendix has been maintained through evolution in many mammalian species.
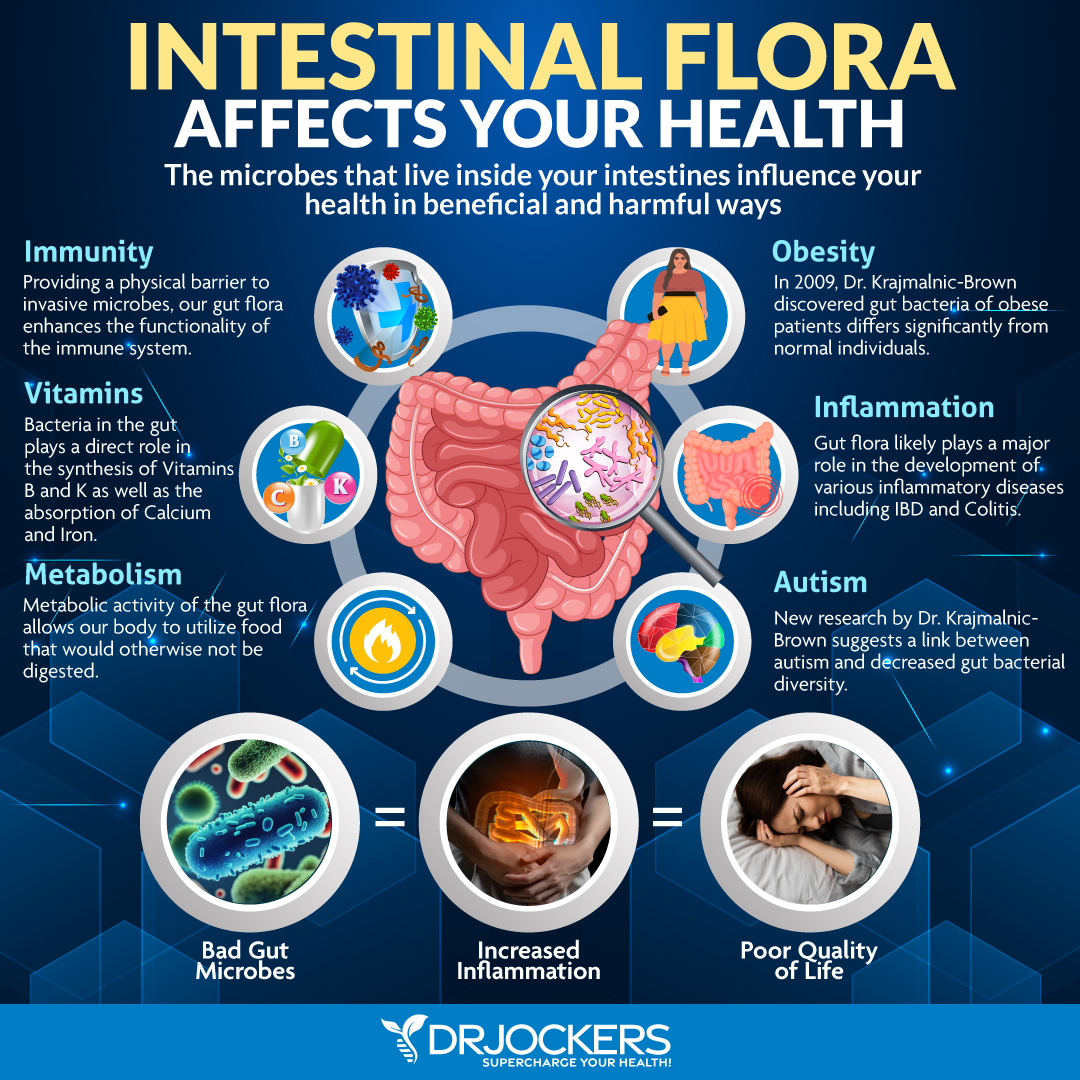
They came up with the theory that the appendix plays a role in gut immunity. It supports the symbiotic relationship between and the balance of beneficial and harmful microbes in your gut.
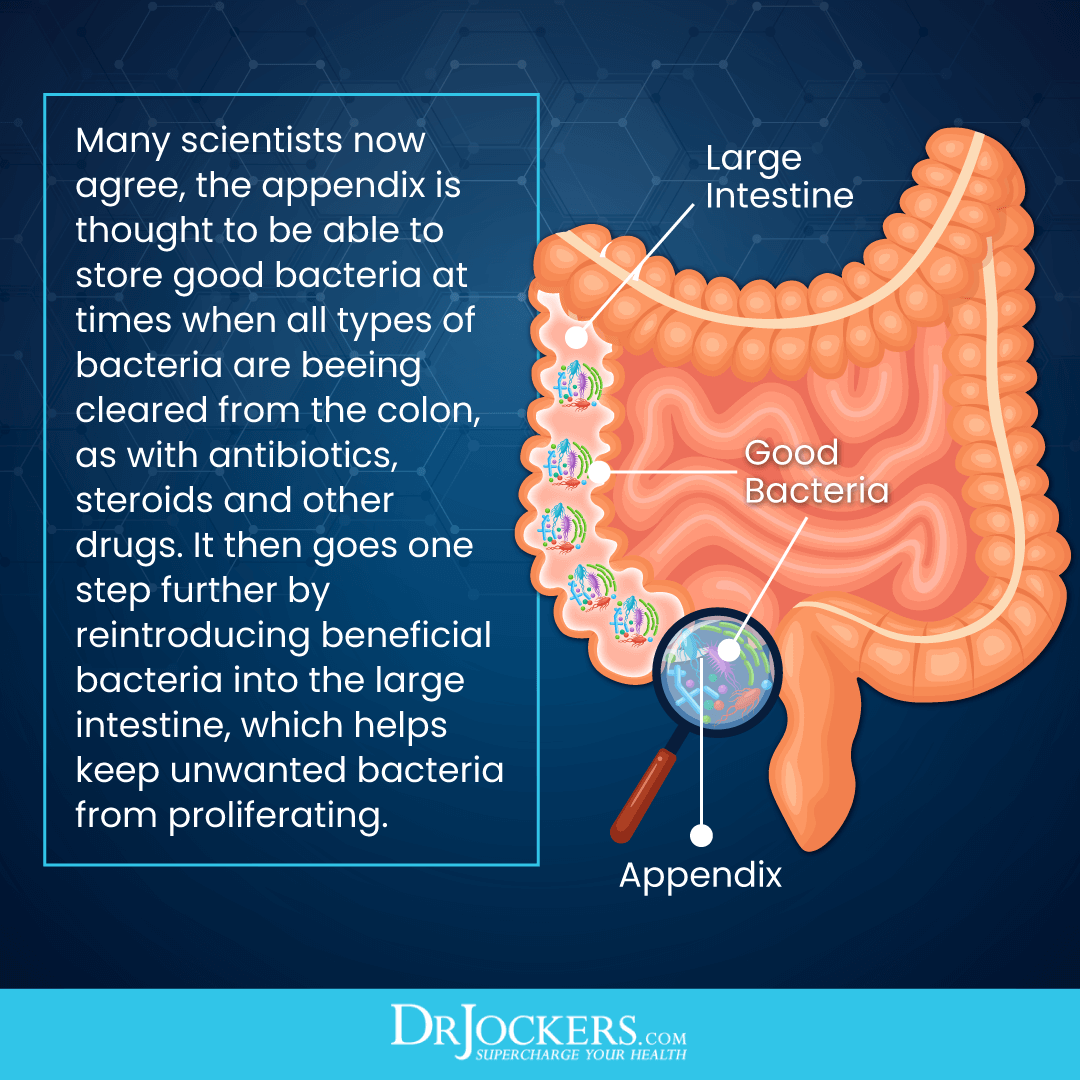
To support this balance, researchers believe that the appendix has evolved to serve as the storehouse of beneficial gut bacteria and support the microbiome during difficult times. This may be particularly helpful during infections that modern medicine can’t successfully address yet.
According to a 2007 study published in the Journal of Theoretical Biology, the appendix may play a role in the microbial balance of your gut (4). Dysentery, cholera, and other infections that truly distress the digestive system also eliminate good microbes.
In these situations, your appendix seems to step to your rescue to help the release of good bacteria to replenish your microbiome and reboot your gut. Considering that the appendix is found in the lower portion of the large intestine, where both microbes and food particles pass through, also supports the idea that the appendix may play a role in microbiome health.
The Appendix and C Diff Infections
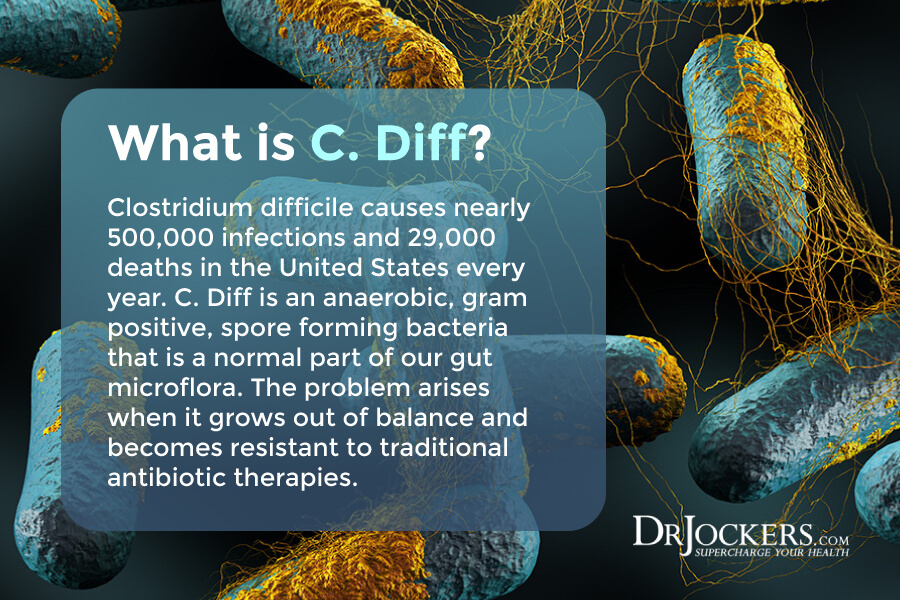
The appendix may also play a role in protecting you from Clostridium Difficile (C. diff) infection. C. diff is a bacteria that can lead to diarrhea and inflammation of the colon (colitis). According to a 2012 study published in Clinical Infectious Diseases, C. Diff infections are on the rise (5).
According to a 2011 study published in the Journal of Clinical Gastroenterology and Hepatology, the appendix may help to protect the body against C. diff (6). The study has found that recurrent C. diff infections (CDI) were 2.5 times higher in people without an appendix than in those with.
Researchers also found that the appendix is the home of many lymphatic follicles, which are generally not present in other parts of your intestines. The lymphatic follicles are also known as gut-associated lymphoid tissue (GALT), which play a critical role in your immune health. GALT contains B and T immune cells (lymphocytes), epithelial and intraepithelial lymphocytes, macrophages, and antigen-generating cells. These cells help to protect your body against pathogenic invaders.
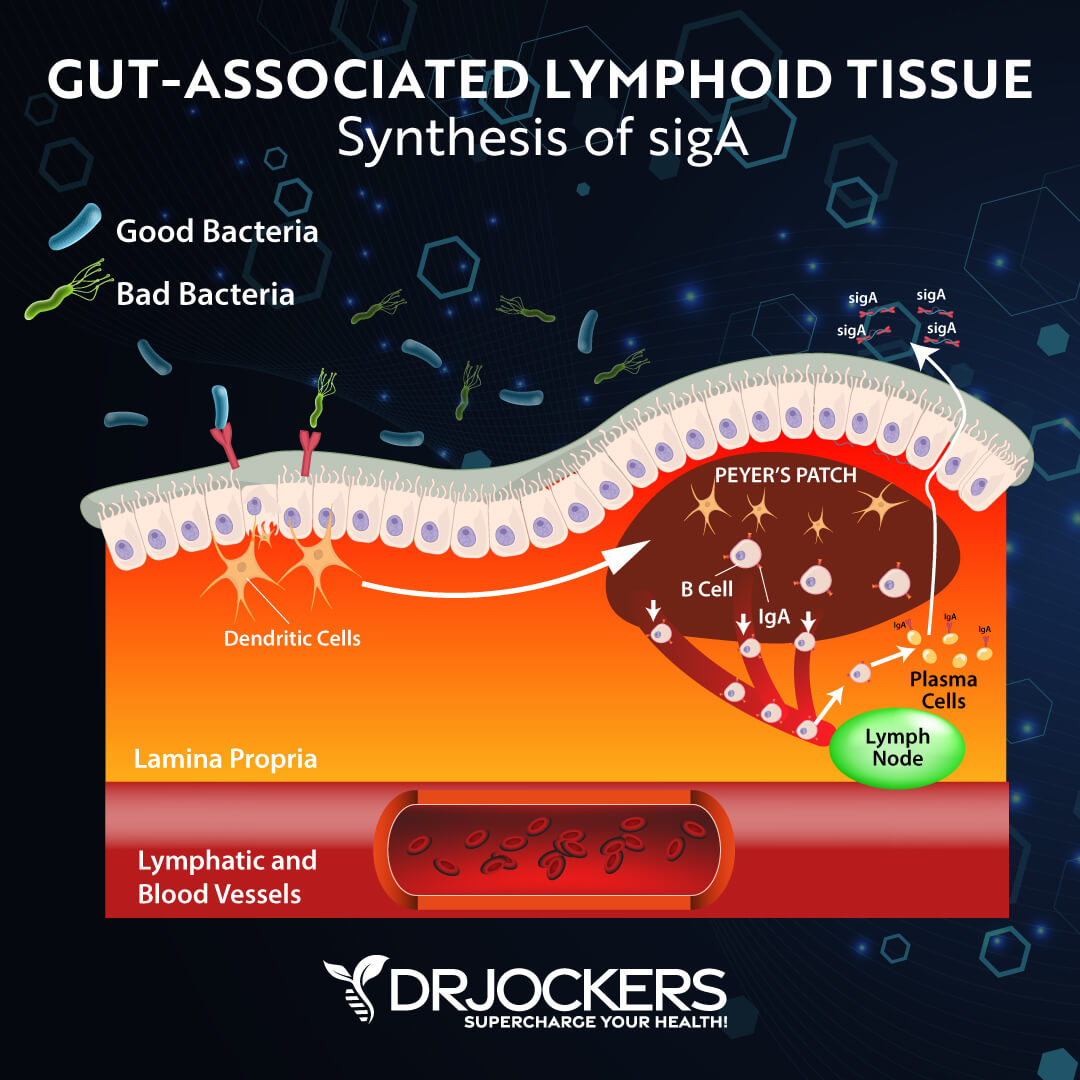
According to a 2016 study published in Clinical and Experimental Immunology, these and other structures suggest that the appendix may help to protect the body from serious infections (7). They do this by stopping invaders from proliferating the body but still allowing good microbes to enter and thrive in the gut.
Furthermore, the appendix has a higher concentration of immunoglobulin than your gut. This also supports the idea that your appendix may play a critical role in supporting the mucosal lining and reducing the risk of gut infections.
The appendix also has something called the appendiceal biofilm. If this biofilm starts to house pathogens, it can be a problem. But when beneficial microbes form biofilms, they can offer protection.
To keep your gut and appendix healthy, it’s important to keep pathogenic bacteria in check (8). An overuse of antibiotics, an inflammatory diet, environmental toxins, stress, and other factors can cause microbiome imbalance and gut health issues. Later in this article, I will offer some recommendations to keep gut inflammation at bay and support your gut and appendix health.
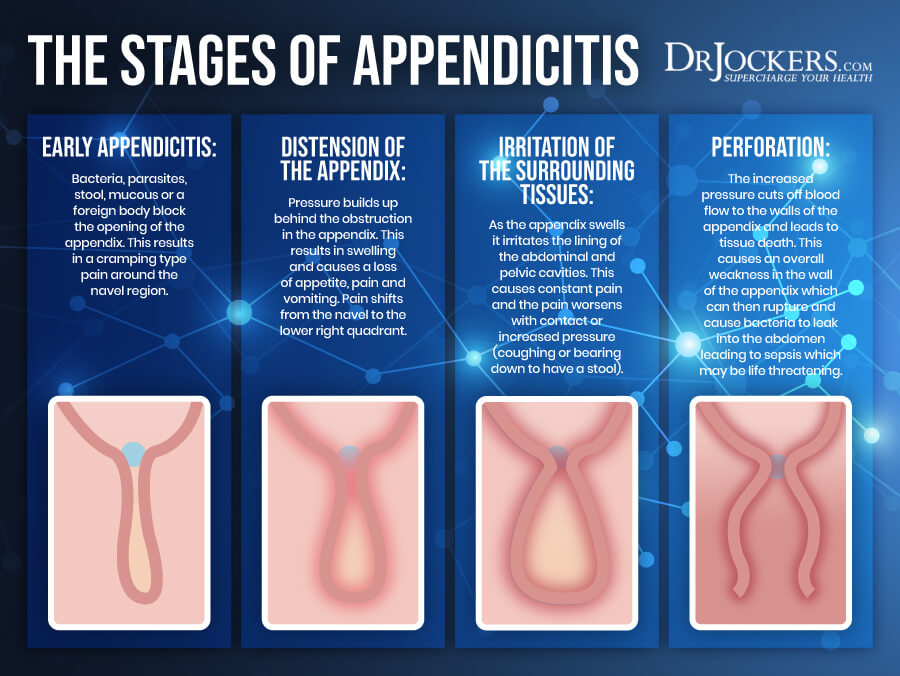
Signs & Symptoms of Appendicitis
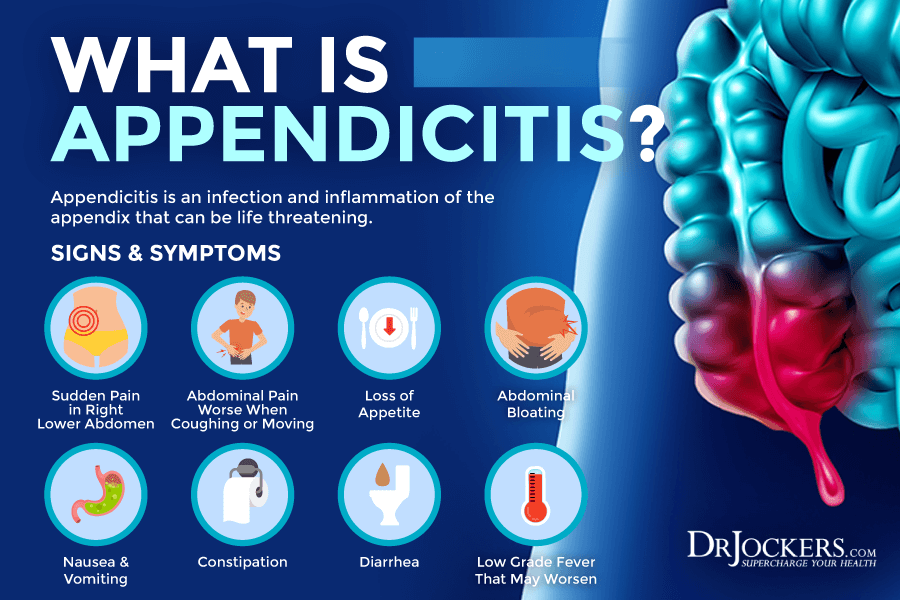
Signs and symptoms of appendicitis may include:
- A sudden pain that starts on the right side of your lower abdomen
- A sudden pain that starts around your belly button but moves to the lower right abdomen area
- Pain that feels worse when coughing, walking, or other movements
- Loss of appetite
- Abdominal bloating
- Nausea
- Vomiting
- Constipation
- Diarrhea
- Low-grade fever that may worsen
- Flatulence.
Risk Factors for Appendicitis
According to John Hopkins Medicine, about 1 in 1,000 people will be affected with appendicitis (9). In most cases, appendicitis occurs in people between the ages of 10 and 30. However, it can occur even if younger and older individuals (10).
Men have a higher risk of appendicitis. A family history of appendicitis can also increase your risk. In children, cystic fibrosis may also increase the risk of appendicitis (10, 11). A buildup of hardened stool, intestinal worms, enlarged lymphoid follicles, tumors, and traumatic injuries may increase the risk and lead to appendicitis.
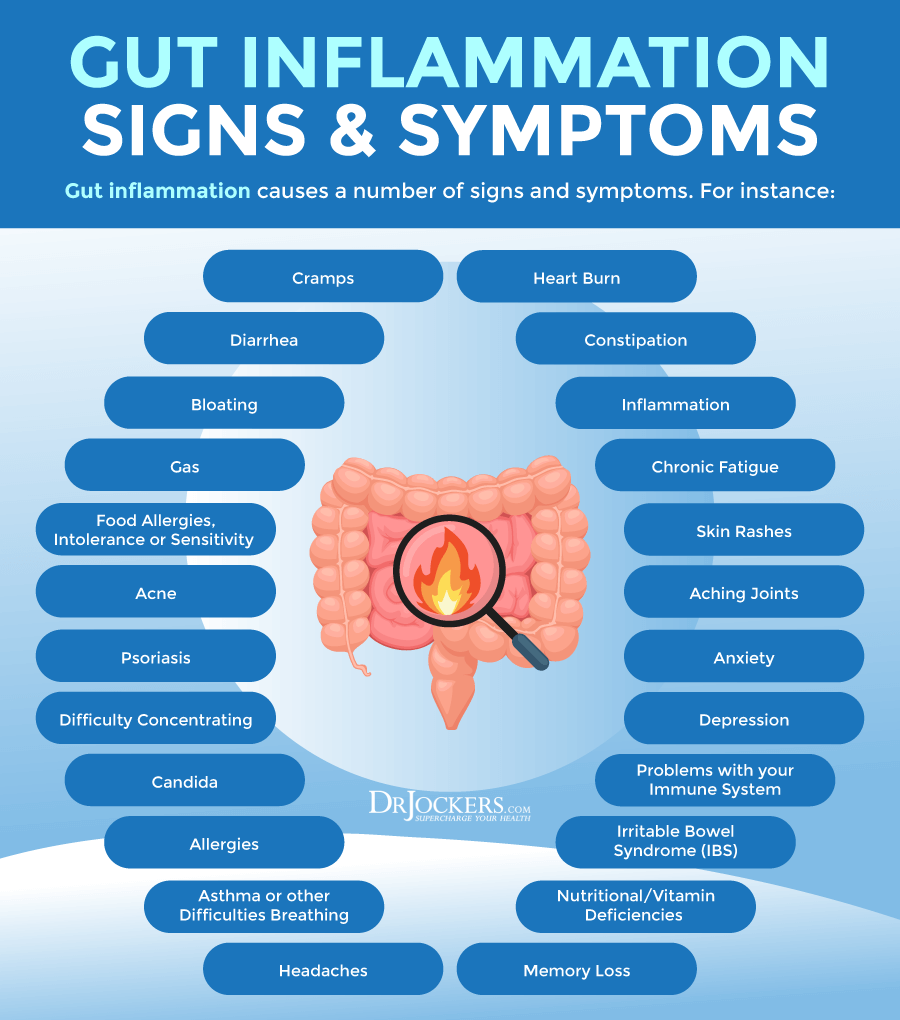
Root Causes of Gut Inflammation
You may develop gut inflammation for a variety of reasons. The root causes of gut inflammation may include the following.
Inflammatory Diet
An inflammatory diet is one of the most common root causes of chronic inflammation and gut inflammation. An inflammatory diet is high in refined sugar, refined oil, artificial ingredients, additives, gluten, processed foods, and junk food and low in greens, vegetables, herbs, spices, fermented foods, fruits, healthy fats, and clean animal-based protein.
A 2021 study published in BMJ has found that dietary factors may increase the risk for gut inflammation (12). Researchers looked at 173 dietary factors in 1425 people. They divided the participants into four groups, including those with Crohn’s disease, ulcerative colitis, irritable bowel syndrome (IBS), and without gut health issues.
According to the results, following a diet high in processed foods, processed sugar, alcohol, and processed animal foods were linked to increased intestinal inflammatory markers, gut inflammation, and gut microbiome imbalance.
A whole food anti-inflammatory diet with lots of omega-3 fatty acids, vegetables, legumes, and fish, on the other hand, showed a potential to decrease intestinal inflammatory markers and lower the risk of gut inflammation and related health conditions.

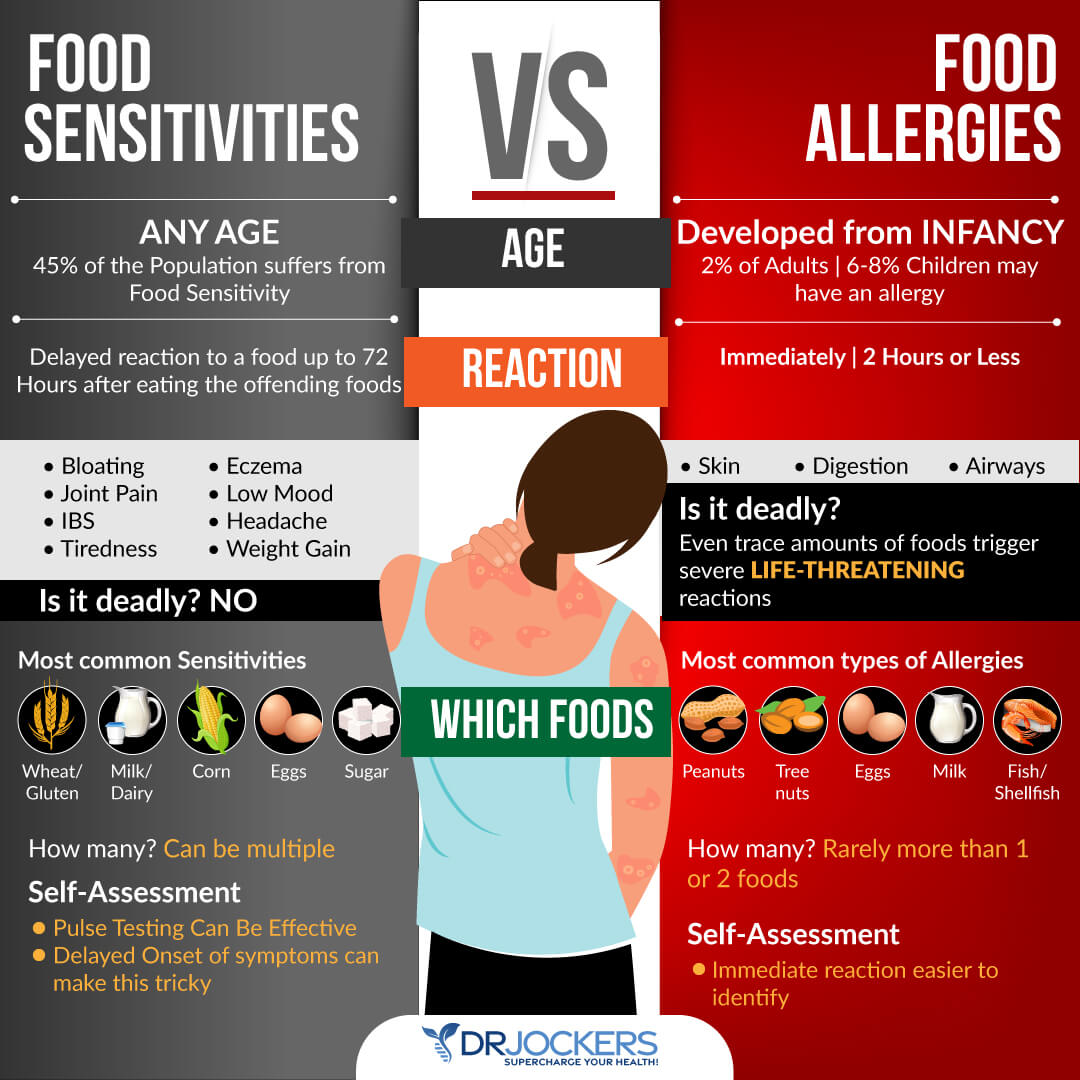
Food Sensitivities
Food sensitivities may also increase your risk of gut inflammation. Unlike food allergies, food sensitivities don’t cause immediate symptoms. Instead, they lead to a delayed and milder response.
Chronic symptoms of food sensitivities often occur several days after consuming a certain food. You may experience symptoms, like digestive issues, headaches, skin issues, or fatigue, hours or even days after eating a certain food without even realizing the culprit.
Common food sensitivities include gluten, dairy, sugar, corn, soy, legumes, shellfish, and eggs. However, you may be experiencing food sensitivities to other, less common foods. Gluten, however, is one of the most common culprits behind gut inflammation.
According to a 2016 study published in Tissue Barrier, gluten triggers the release of zonulin, which is a protein that causes the breakdown of tight protein junctions between intestinal epithelial cells (13). This can lead to gut inflammation and leaky gut syndrome. According to a 2019 study published in the International Journal of Molecular Sciences, gluten may also cause the activation of your mast cells, which release histamine, increasing the risk of gut inflammation (14).
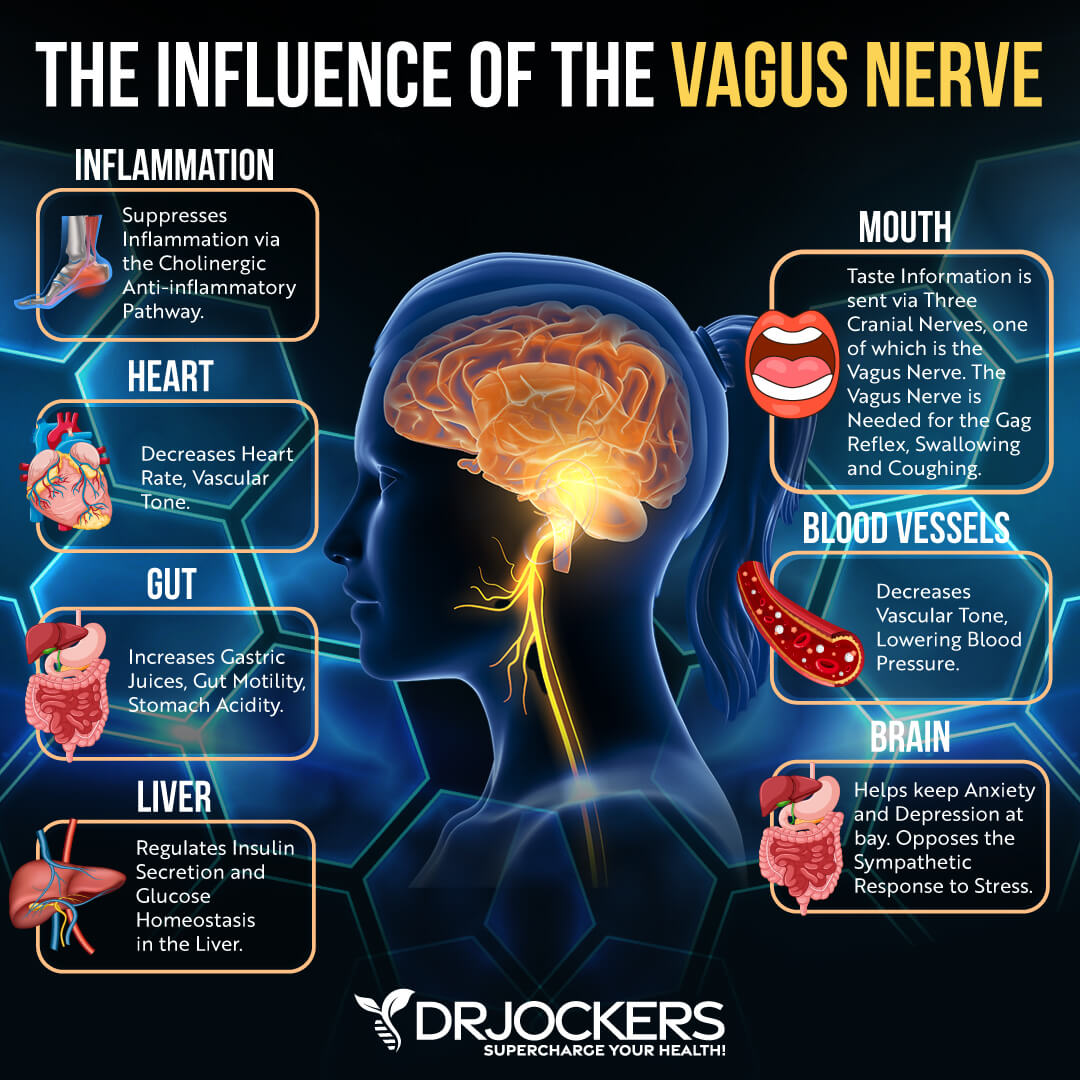
Poor Vagal Tone
Your vagus nerve is the tenth cranial nerve. It is your body’s major parasympathetic nerve. It allows your body to slow your heart rate, control gag reflex, allow involuntary constriction and relaxation of the muscles of your gut, control sweating, regulate blood pressure, and control vascular tone. Vagal tone refers to the activity of the vagus nerve.
Excessive vagus nerve function may result in a variety of nervous system issues. For example, it is commonly found in dysautonomias, such as postural orthostatic tachycardia syndrome (POTS). Vagus nerve stimulation may lead to sudden stress, gastrointestinal symptoms, sudden blood pressure drop, and slow heart rate.
Poor vagal tone may also cause mental and emotional health issues, including anxiety, panic attacks, and depression. It may also play a role in a variety of health issues, including migraines, headaches, tinnitus, hypertension, fibromyalgia, weight problems, and inflammatory issues.
Your vagal tone is closely connected to your gut health. Poor vagal tone and vagus nerve health may increase the risk of gut inflammation and gut health problems. Your brain and gut are connected through nerve activity, and your vagus nerve is one of the main nerves in charge of this.
Stress can interrupt proper signaling from your vagus nerve. This may result in gastrointestinal symptoms. According to a 2014 study published in PLoS One, conditions, including IBS and Crohn’s disease, that are characterized by gut inflammation tend to be characterized by reduced vagus nerve function and poor vagal tone (15).
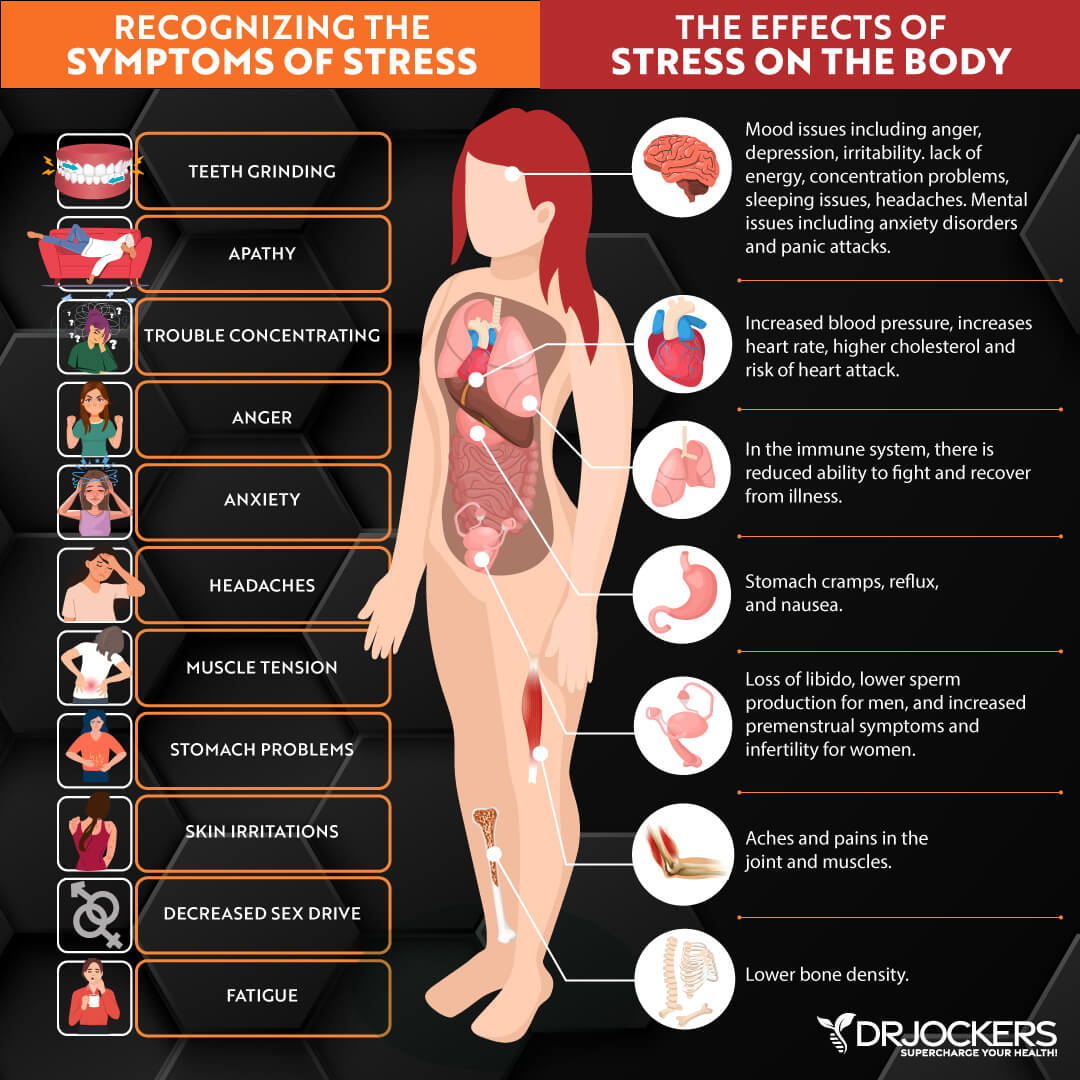
Chronic Stress & Poor Sleep
Chronic stress and poor sleep are two major lifestyle factors that can increase chronic inflammation, chronic stress, and chronic symptoms. They both can play a serious role in the increased risk of gut inflammation. According to a 2017 study published in Oxidative Medicine and Cellular Longevity, leading a sedentary lifestyle may increase inflammatory molecules in the gut (16).
Exercise, on the other hand, may improve the gut microbiome and gut inflammation levels. According to a 2015 review published in Exercise Immunology Reviews, exercise may improve the gut microbiome and gut health (17).
According to a 2018 study published in Frontiers in Microbiology, a disruption of the body’s natural circadian rhythm or sleep-wake cycle can throw off gut microbiome health, increase the growth of inflammatory gut bacteria, discourage the growth of beneficial gut bacteria, and increase the risk of leaky gut syndrome (18).
A 2016 study published in Molecular Metabolism has found that only two nights of poor, short sleep can increase pro-inflammatory gut bacteria growth (19). A 2009 study published in Sleep Medicine has found that poor sleep and sleep deprivation can worsen gut inflammation and interfere with recovery from gut inflammation related to colitis (20).
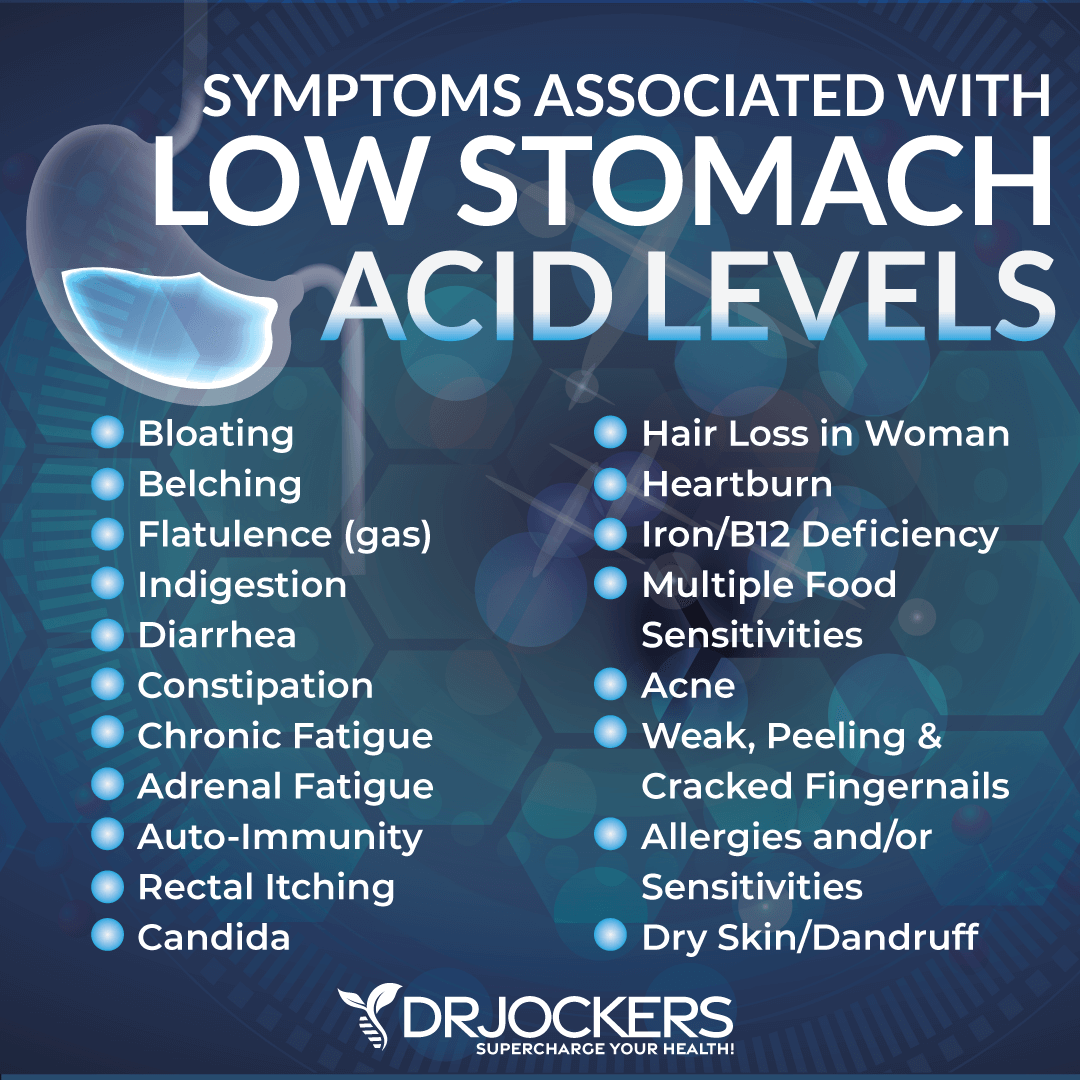
Low Stomach Acid Levels & Digestive Juice Production
Stomach acid helps to kill microbes and supports digestion. If you have low stomach acid levels and your body can’t make enough, it can cause microbial overgrowth, poor digestion, acid reflux, gut inflammation, and other gut health issues.
A 2008 study published in Infection and Immunology has found that low stomach acid may contribute to the increased risk of bacterial pathogen overgrowth, gut infections, and, consequently, gut inflammation (21).
Bile is a greenish-brown liquid primarily made of cholesterol, bile salts, and bilirubin, made in your gallbladder. It helps your body digest fats but is also important in other areas of digestion and health. Pancreatic enzymes are secreted by your pancreas to break down fats, protein, and carbohydrates.
Problems with both bile flow and pancreatic enzyme production can increase your risk of gut inflammation. According to a 2018 study published in the Annals of Gastroenterology, poor bile flow can increase the risk of inflammatory bowel disease (IBD) (22). According to a 2018 review published in the Journal of Clinical Medical Research, pancreatic dysfunction may be linked to IBDs (23).
Gut Infections
Gut infections, including H Pylori, parasites, yeast, bacterial, and viral infections, can all increase your risk of gut inflammation. According to a 2019 study published in FEBS Open Biology, H Pylori infection may lead to pro-inflammatory bacteria growth in the gut (24).
This can increase gut inflammation. According to a 2018 study published in Frontiers in Immunology, viral infections, including respiratory viral infections and secondary bacterial pneumonia, can also modify the gut microbiome and lead to gut inflammation (25).
A 2019 study published in Peer Journal has found that parasitic infections may interfere with gut microbiome balance, increasing the risk of gut inflammation (26). According to a 2019 randomized control trial published in Digestive Diseases and Sciences, even a short, acute bout of food poisoning can trigger gut inflammation, inflammatory autoantibody production, and symptoms of IBS (27).
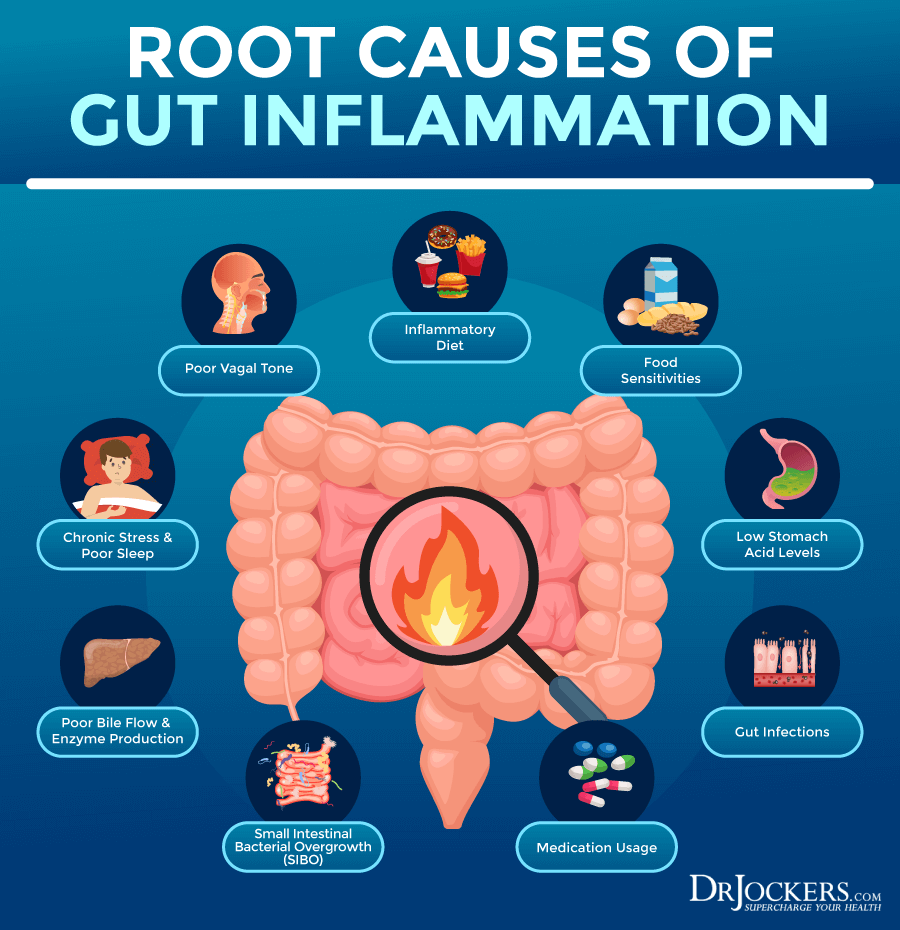
SIBO
As the name suggests, small intestinal bacterial overgrowth (SIBO) is bacterial overgrowth in your small intestines. Symptoms of SIBO may include abdominal pain, bloating, constipation, diarrhea, fatigue, malnutrition, food sensitivities, and a list of other chronic issues. Chronic gut inflammation is often an underlying issue caused by or causing these symptoms of SIBO.
A 2007 review published in Gastroenterology and Hepatology, the excess bacteria in SIBO may trigger an intestinal inflammatory response and cause gut inflammation (28). This may lead to even further microbial imbalance and bad bacterial overgrowth. This can then result in a vicious cycle of SIBO, gut infections, gut inflammation, and chronic gut health issues.
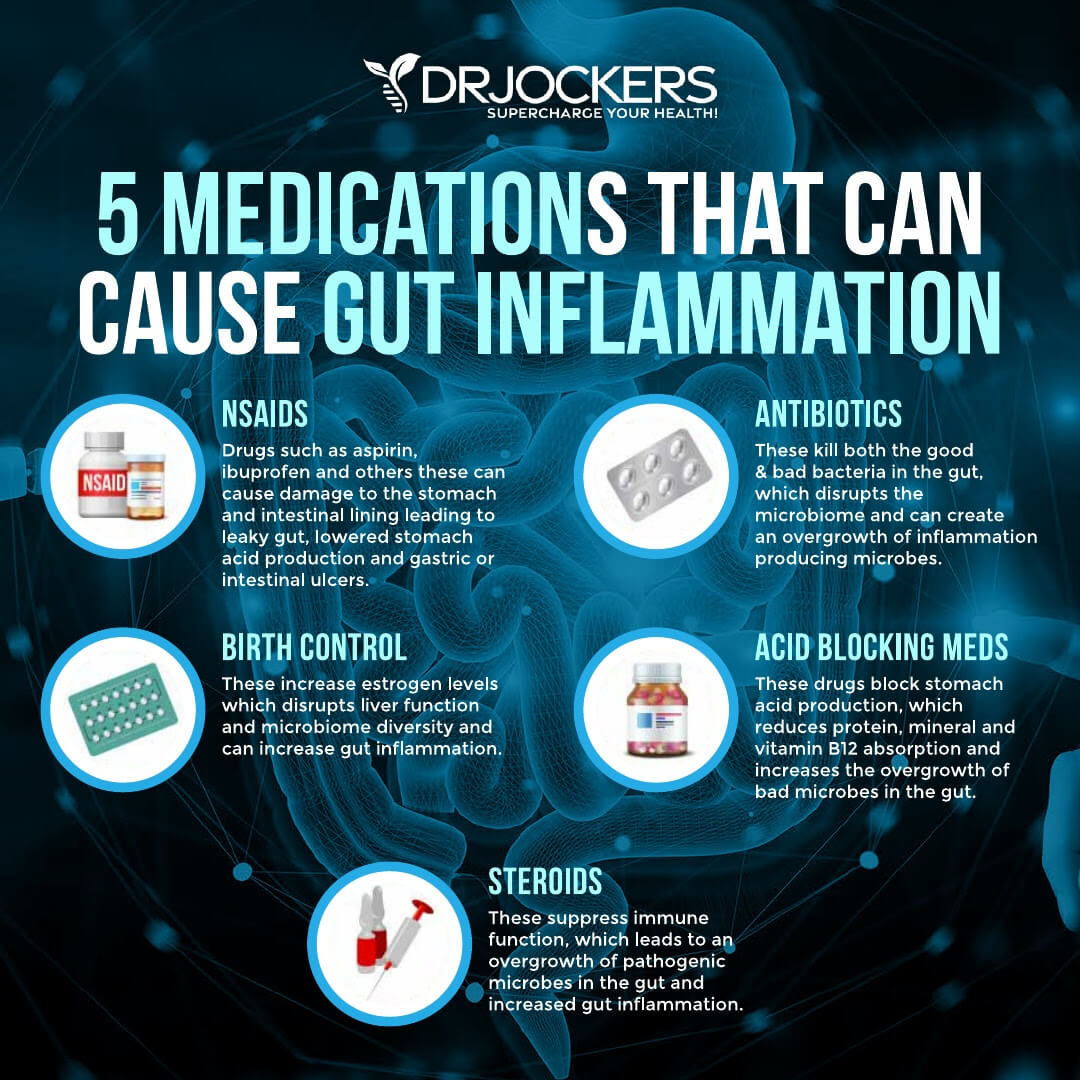
Medications
Finally, the use and overuse of certain medications can increase your risk of gut inflammation and related gut health issues. Some of these medications include antibiotics, proton pump inhibitors (PPIs), selective serotonin reuptake inhibitors (SSRIs), non-steroidal anti-inflammatory drugs (NSAIDs), and oral contraceptives.
Antibiotics are designed to fight bacterial infections. Though using antibiotics is sometimes necessary and can even be lifesaving, in our modern world, antibiotics are overprescribed and overused. Unfortunately, antibiotics can seriously disrupt your gut microbiome balance and even cause antibiotic resistance.
According to a 2018 study published in Yonsei Medical Journal, antibiotics not only clean out harmful microbes but can also destroy beneficial gut bacteria leading to gut flora imbalance and the risk of gut inflammation (29). According to a 2015 study published in PLoS One, antibiotics can increase the risk of leaky gut syndrome and gut inflammation (30).
According to a 2019 study published in Scientific Reports, long-term PPI use for heartburn may also reduce beneficial, anti-inflammatory gut bacteria and increase harmful bacteria overgrowth and gut inflammation (31). According to a 2019 study published in Peer Journal, SSRIs may also increase the risk of gut dysbiosis and inflammation (32).
According to a 2015 study published in Clinical Microbial Infections, NSAIDs may also interfere with gut microbiome balance and increase the risk of gut inflammation (33). Moreover, according to a 2016 study published in Gastroenterology, the long-term use of oral contraceptives may also increase the risk of gut inflammation and complications in Crohn’s disease (34).
GI MAP Testing
I recommend using gut testing to look at markers of gut inflammation, gut microbiome imbalances, and root causes of gut health issues. My favorite test to look at your gut health and identify bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora, potential autoimmune triggers, and all intestinal health markers is the GI Map Stool Analysis.
This is the best and most comprehensive gut test I have found, and it helps me tremendously to identify the root cause of my patient’s health issues and help them to repair their body and regain their health naturally.
Most medically trained conventional GI doctors to pay little to no attention to diet and lifestyle factors and their impact on your gut health. They look at drugs and surgeries as the first step in addressing digestive problems instead of as the very last resort.
While many natural and holistic health doctors offer probiotics and herbs to improve your gut microbiome, without proper testing, they can’t know if these suggestions are truly the right ones and won’t be able to see the actual effects of these probiotics and herbs on one’s unique terrain and the gut microbiome.
The GI Map Stool Analysis is a comprehensive stool test that looks at all major factors of your gut health and helps us identify what compounds will work best for eliminating the various pathogenic microorganisms that may be causing your symptoms. This takes the guesswork out of the process and also helps to see your true progress.
I have found that the GI map is the most thorough stool test with actionable biomarkers. There are other complex stool tests that may give some interesting information, but often not clinically relevant ones. Other tests may also show false negatives or are more confusing to understand. This test offers everything that I, as a natural health doctor, need to see to make good clinical decisions and offer a treatment protocol that can help to improve your gut microbiome and your overall health.
As a natural health doctor, I believe that your recovery and health are a collaborative effort between us. It is important that you understand how each test works and why I recommend certain natural support strategies. Today, I want to discuss everything the GI Map Stool Analysis has to offer and how to interpret this test.
The 5 R’s to Healing Gut Inflammation
To reduce the risk of and heal gut inflammation, I recommend that you follow the 5 R’s to healing gut inflammation:
Remove
Remove any inflammatory foods, infections, unnecessary medication, and gut stressors from your life. Remove refined sugar, refined oils, additives, artificial ingredients, deep-fried food, junk food, overly processed food, sugary drinks, and sodas. Remove and address food sensitivities.
Get tested for gut and other chronic infections and address them through supplementation and diet. If you are on any medication, check with your doctor, and remove them if possible. Choose natural options whenever you can. Reduce chronic stress, environmental toxins, and other factors that can affect your gut health.
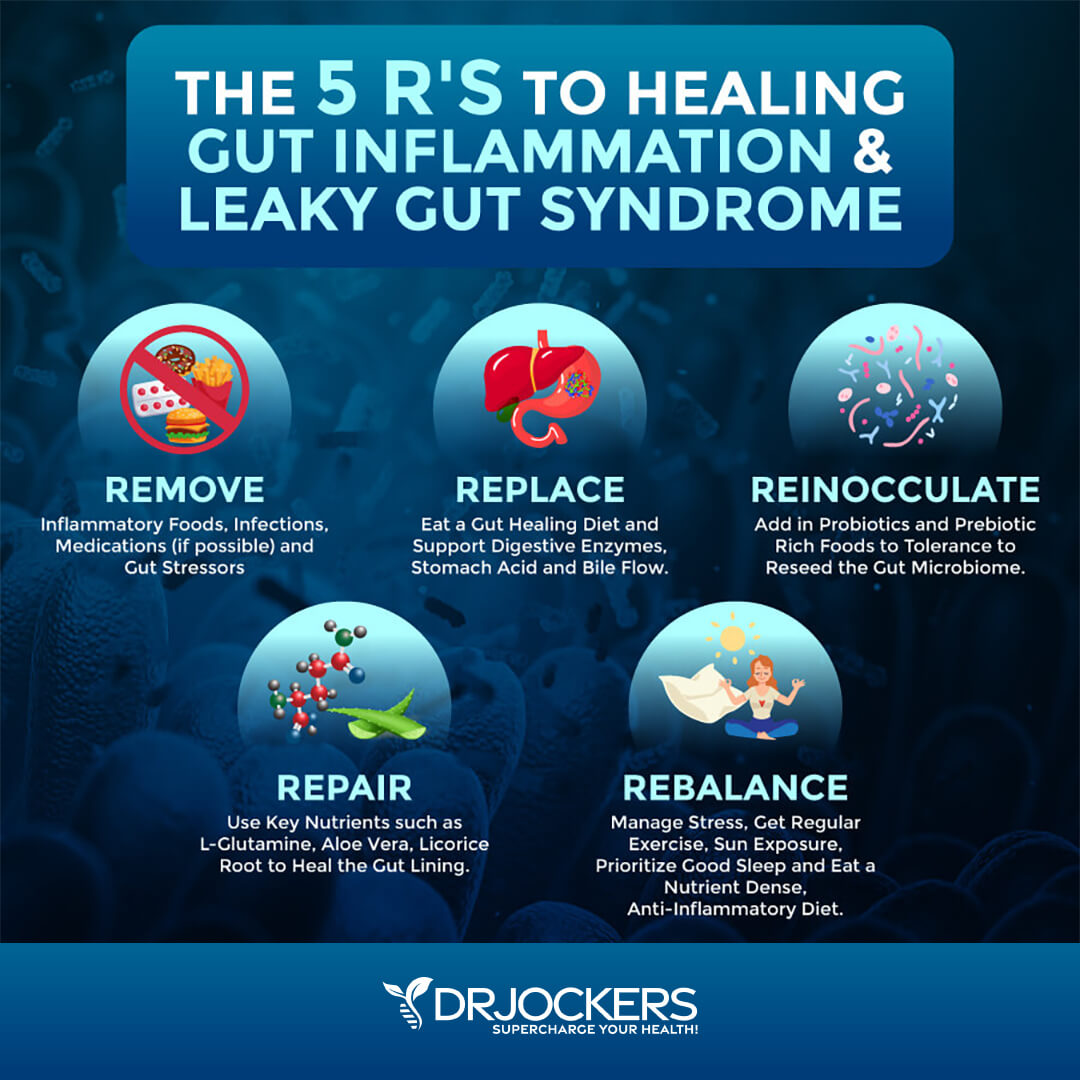
Replace
These harmful things with beneficial things. Eat a gut-healing, anti-inflammatory diet. You may try a prebiotic-rich, low-FODMAP, semi-elemental, or elemental diet, depending on your needs. You may learn more about these gut-friendly dietary strategies from this article.
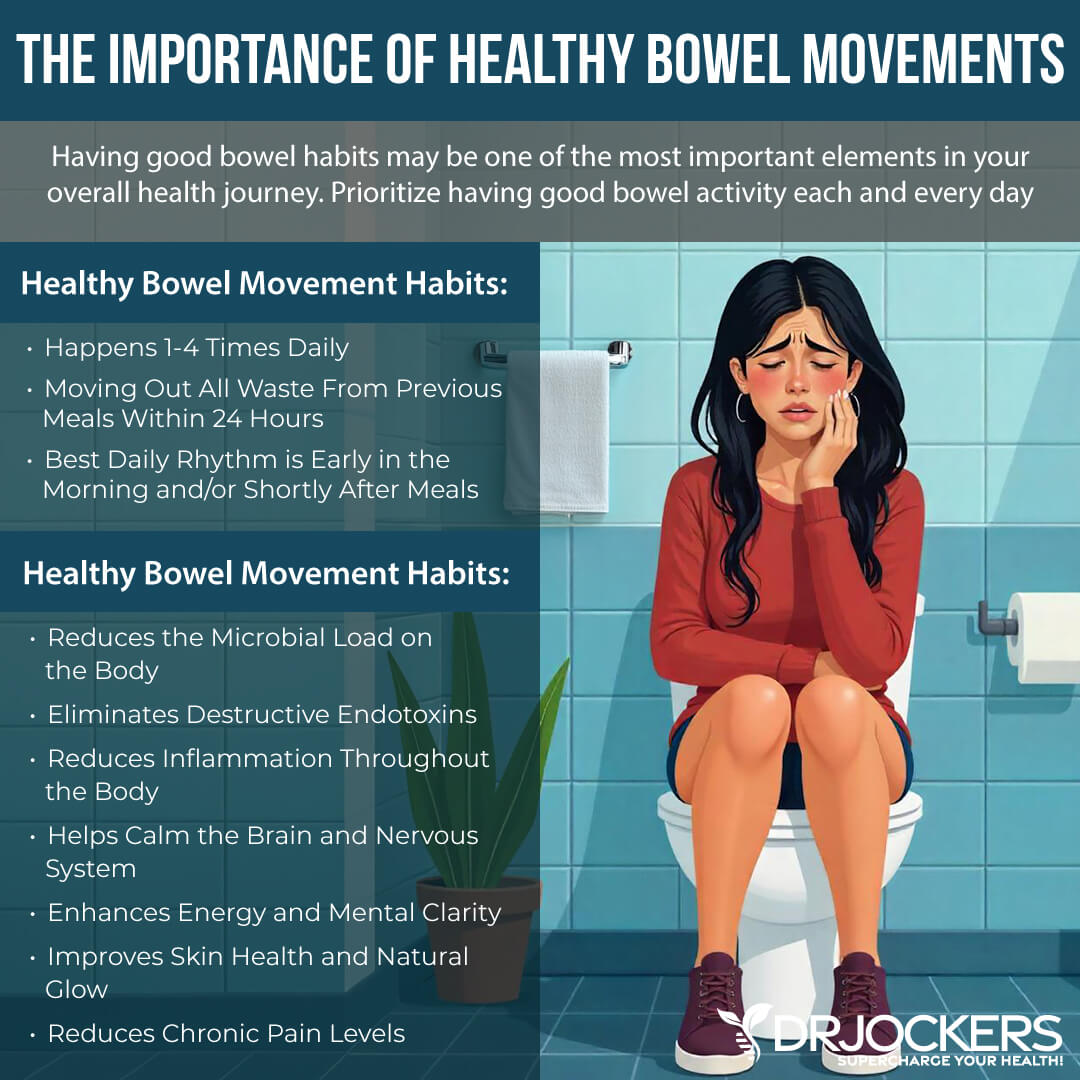
Support your gut health with digestive enzymes, such as Super D-Zyme to support your digestion. Support stomach acid and bile flow. You may support healthy stomach acid levels by using liquid nutrition throughout the day, using ginger, apple cider vinegar, and lemon, hydrating well outside of meals but avoiding drinking right before, during, and after meals, starting your meals with protein, consuming your largest meals when the most relaxed, and using fermented food and drinks.
If you have low stomach acid, using an HCL supplement, such as Super Digest HCL can be helpful. For GI mucosal membrane health, I recommend GI Clear. If you have trouble with elimination and have constipation, a supplement like Bowel Mover can help until your body recovers enough and regains its normal rhythms of elimination.
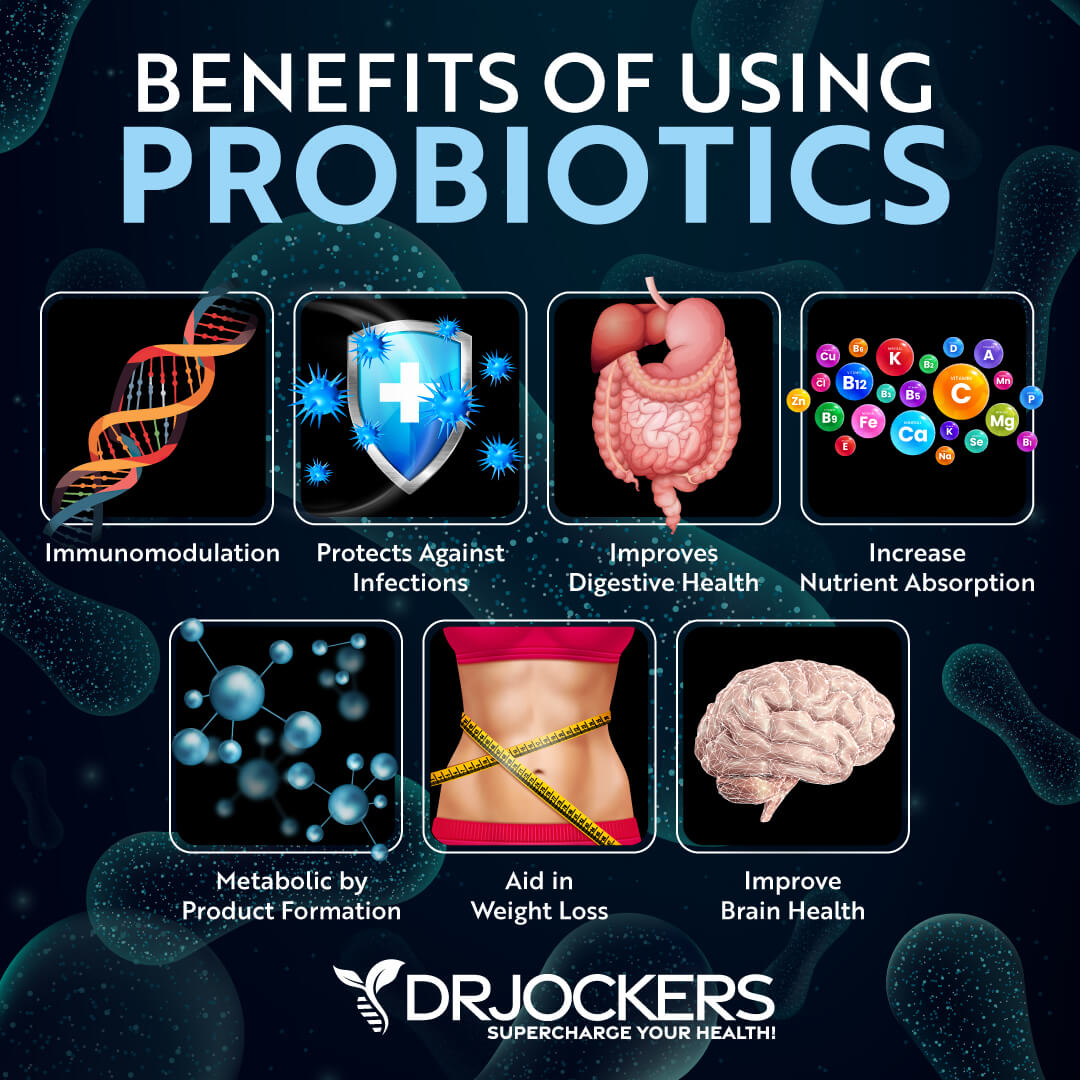
Reinocculate
Reinocculate your gut microbiome with prebiotic and probiotic-rich foods and probiotics. Prebiotic-rich foods include Jerusalem artichokes, leek, onion, garlic, asparagus, dandelion, chicory greens, jicama, apples, and bananas. However, prebiotic-rich foods are not right for everyone. Some people find too many prebiotics in their diet are triggering for them.
If you notice digestive complaints from a prebiotic-rich diet, back off. If you are following a low-FODMAP or carnivore diet, you shouldn’t follow a prebiotic-rich diet either. Unless you are on these diets or find prebiotics triggering, I recommend eating prebiotic-rich foods.
I recommend that you include probiotic-rich foods in your diet, including sauerkraut, kimchi, fermented vegetables, coconut kefir, pickles, and kombucha. I recommend that you also take a daily probiotic supplement, such as ProbioCharge.
If you have SIBO, I recommend soil-based probiotics, such as SBO Probiotics, because some bacteria in other probiotics can be triggering for SIBO. You can learn more about how to select the best probiotic supplements and how to rotate various types of probiotics in this article.
Repair
Repair your gut lining and gut health with L-glutamine, aloe vera, licorice, and other herbal supplements. According to a 2012 study published in the Journal of Epithelial Biology and Pharmacology, l-glutamine plays an important role in the gut barrier function, gut mucosal health, metabolism, and the reduction of gut inflammation (35).
A 2021 study published in Evidence-Based Complementary and Alternative Medicine has found that aloe vera may have anti-inflammatory and antioxidant benefits for colitis (36). A 2017 study published in Pharmaceutical Biology has found that licorice may also have anti-inflammatory benefits (37). To lower gut inflammation and protect your gut, I recommend taking a daily L-glutamine supplement.
Rebalance
Rebalance your gut flora. Reduce your stress levels. Practicing meditation, gratitude, mindfulness, guided relaxation, and prayer can help you to learn how to respond to stress better and lower your stress levels. Journaling, positive mindset shifts and positive affirmations can also help. Exercise, grounding, and time spent in nature are also great ways to calm your mind and reduce stress.
Get regular exercise. Move your body throughout the day every day. Exercise at least 20 to 30 minutes five days a week. Use a combination of strength and resistance training, cardiovascular, and low-impact exercise. Get outside to move or exercise whenever you can. Get daily sun exposure for optimal vitamin D levels.
Prioritize good sleep. Going to be and waking up around the same time helps to support your body’s natural circadian rhythms. Avoid electronics, sugar, caffeine, heavy foods, and stress in the evening. Choosing calming activities instead, such as reading, coloring, taking a healing bath, sipping on herbal tea, crossword puzzles, journaling, and having good conversations. Ensure that your bed, mattress, bedding, and pillow are supportive and comfortable.
Follow a nutrient-dense, anti-inflammatory diet. Eat plenty of greens, vegetables, herbs, spices, fermented food, low-glycemic index fruits, grass-fed beef, pasture-raised poultry and eggs, wild-caught fish and seafood, and wild game. Focus on healthy fats, such as avocados, coconut oil, olives, extra virgin olive oil, organic butter and ghee, and far from clean animal sources.
To learn more strategies for improving gut inflammation and supporting your gut, I recommend that you read this article about gut inflammation.
Final Thoughts
Doctors used to believe that the appendix was a useless organ. It turns out the appendix plays an important role in microbiome health, gut health, and reducing the risk of C diff infections. To reduce your risk and improve gut inflammation and support your gut health, I recommend that you follow the 5 R’s to healing gut inflammation.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
 Inflammation Crushing Ebundle
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!





This is a great article… but what about if you have already had the appendix removed? What now? – Husband had his appendix removed as a child. Now he has IBS & diverticulitis. Also contracted C-Diff in the hospital. So how does he now balance all that flora without his appendix?
Sorry to hear that! Here is a helpful article for you: https://drjockers.com/gut-inflammation/