 COPD: Symptoms, Causes, and Support Strategies
COPD: Symptoms, Causes, and Support Strategies
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes breathing difficult. It causes coughing, shortness of breath, chest tightness, wheezing, and frequent infections. As a progressive disease, symptoms usually worsen over time making breathing, exercise, and daily tasks increasingly difficult. With appropriate lifestyle and dietary strategies, you can reduce your risks and the progression of the disease.
In this article, I will explain what COPD is. You will understand its signs and symptoms. I will explain the stages of COPD. I will go over the top risk factors and common root risk factors of COPD. You will understand how COPD is diagnosed and what are the conventional treatment options for the disease. I will share my top natural support strategies for COPD to support your health and improve your well-being.
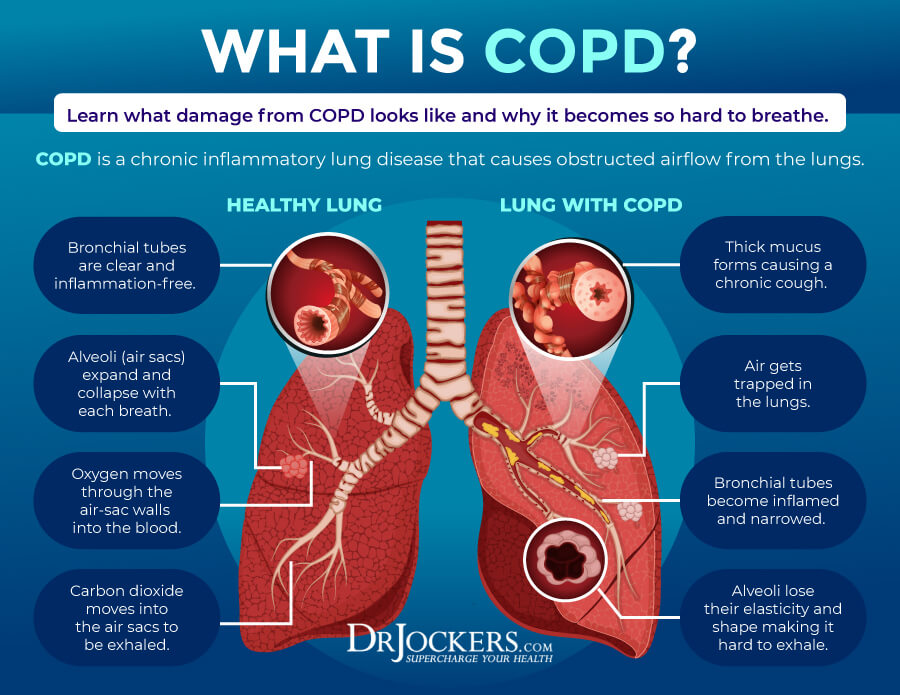
What Is COPD
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes breathing difficult. COPD can cause difficulty breathing, coughing with mucus, shortness of breath, wheezing, and chest tightness. Being a progressive disease, symptoms of COPD worsen over time.
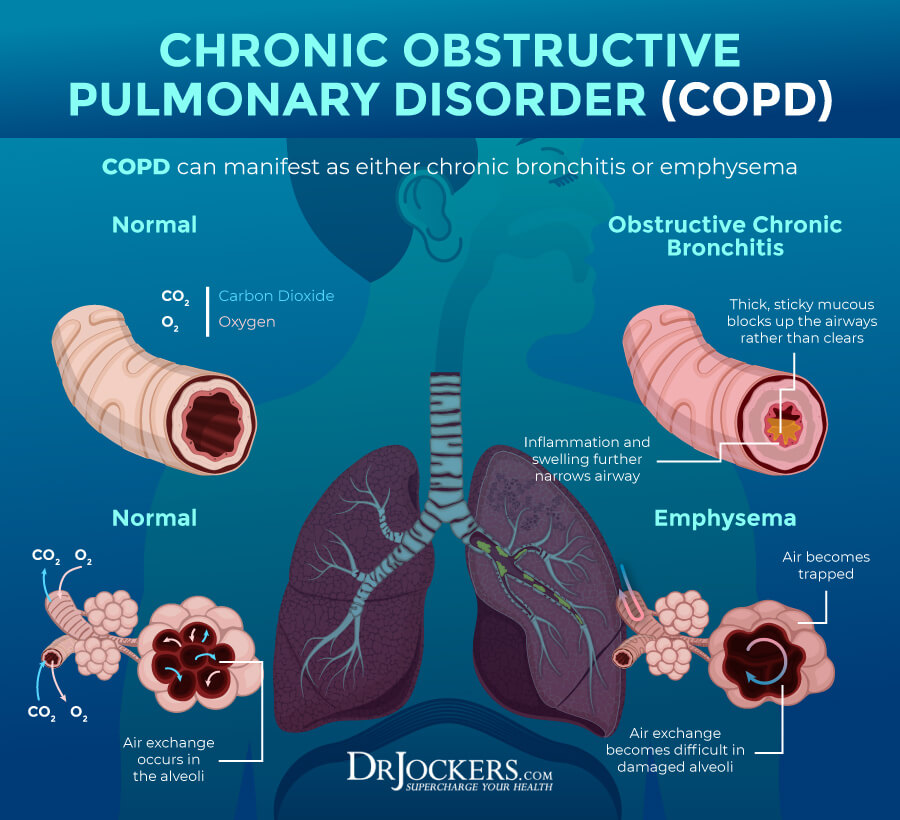
COPD is a group of progressive lung diseases with the two most common groups being emphysema and chronic bronchitis. Emphysema is a disease that slowly damages the air sacs in your lungs, preventing the outward flow of air and normal breathing. Chronic bronchitis is an inflammation and narrowing of your bronchial tubes, resulting in mucus buildup and difficulty breathing.
COPD affects about 30 million people in the United States alone. About half of these people are unaware of their condition (1). Early diagnosis and treatment of COPD, however, is critical. Untreated COPD leads to quicker progression of the disease and an increased risk of frequent and serious respiratory infections and heart problems.
While it is a very serious progressive condition, it can be prevented, and symptoms can be slowed down. Smoking cigarettes is one of the leading causes of the disease. According to the National Institute of Health, about 75 percent of people with COPD smoke or have smoked and only about 25 percent of people with COPD never smoked (2). Other than smoking, air pollution, dust, chemical fumes, and other lung irritants are among the top issues that contribute to COPD. Later in this article, I will go over some other risk factors that may increase your chances of developing COPD or worsen your symptoms.
Signs and Symptoms of COPD
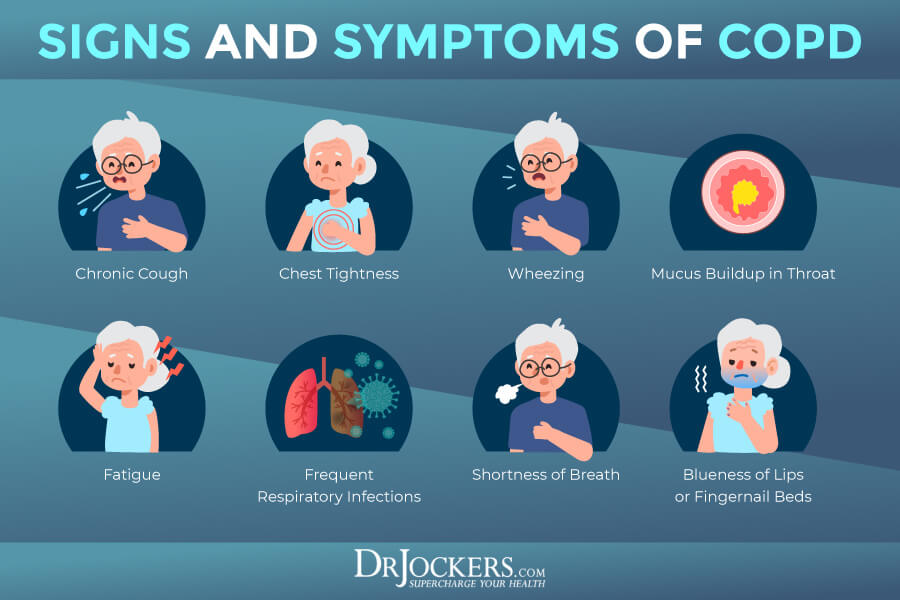
Since COPD is a progressive disease, it is not surprising that symptoms of COPD are progressive too. They may start with mild coughing or shortness of breath and then develop into more serious issues later as your lungs become more damaged.
Early signs and symptoms of COPD include (2):
- Recurrent mild cough
- Occasional shortness of breath, especially after exercising
- Needing to clear your throat, especially upon waking in the morning
- Subtle difficulties with certain activities, such as taking the stairs
Progressive signs and symptoms of COPD include (2):
- Shortness of breath after mild exercise, such as taking a flight of stairs or a walk
- Wheezing
- Chronic cough
- Needing to clear mucus
- Chest tightness
- Frequent respiratory infections
- Low energy
Late-stage signs and symptoms of COPD include (2):
- Fatigue
- Weight loss
- Swelling of ankles, feet, and legs
Stages of COPD
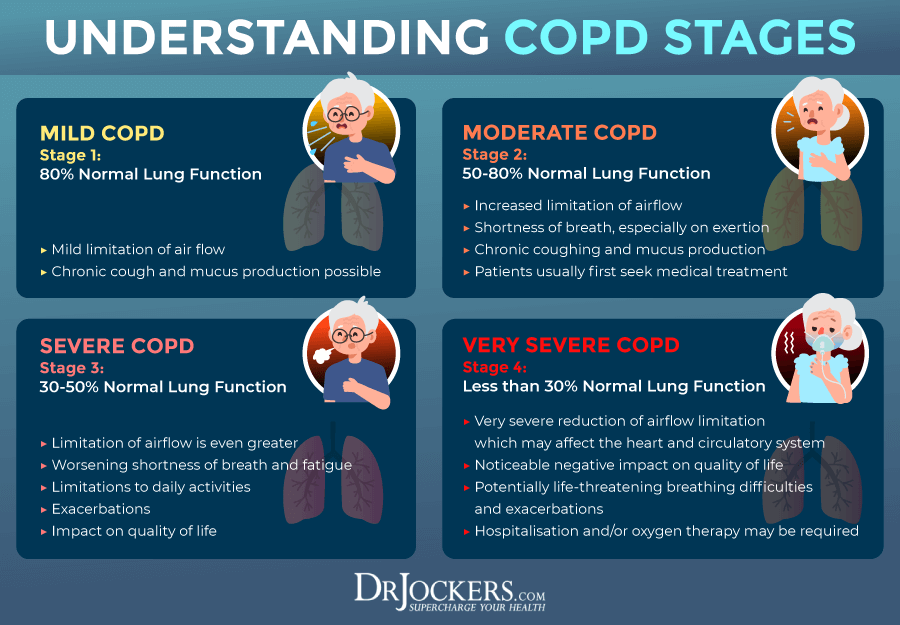
COPD is a progressive disease. There are 4 stages of COPD that help to understand the severity of the disease and to determine the right treatment option. To determine the stage of COPD, doctors use the GOLD Staging System or the BODE Index.
The GOLD Staging system looks at the forced expiratory volume in one second (FEV1) from a COPD pulmonary function test while the BODE Index referring to body mass, obstruction of airflow, dyspnea, and exercise capacity looks at these factors with the help of a 6-minute walk test, spirometry, gas diffusion testing, body plethysmography, and other tests (3).
The stages of COPD include:
- Stage 1: Stage 1 is the mild stage of COPD in which the FEV1 is around 80 percent or above. AT this stage, people often don’t realize that they have an issue. They may notice some coughing, phlegm, or difficulties breathing, especially during certain activities. Diagnosing COPD at this stage, however, is critical to take measurements to slow the progress of the disease (3).
- Stage 2: Stage 2 is also referred to as the moderate stage. FEV1 levels are between 50 and 80 percent of normal. At this stage, people will have more coughing, increased mucus, more breathing issues, and more limitations walking. Your doctor may prescribe bronchodilators and go to a pulmonary rehab program at this stage (3).
- Stage 3: Stage 3 is severe COPD with an FEV1 of 30 to 50 percent. At this stage, there is more coughing, increased mucus, even more difficulty breathing, and a significant decline in lung function. Many activities and even daily tasks become challenging. At this stage, doctors often prescribe corticosteroids for inflammation, inhalers for breathing, and an array of other therapies and medications depending on your situation (3).
- Stage 4: Stage for is the severe of end-stage COPD with an FEV1 lower than 30 percent of normal. This is the last stage of COPD. Symptoms become severe and breathing issues can become life-threatening. Many patients have trouble getting enough oxygen which can lead to hypoxia, hypoxia, cyanosis, and other health issues. Your doctor will likely recommend oxygen therapy at this stage to support breathing and helping you to get enough oxygen (3).
Risk Factors for COPD
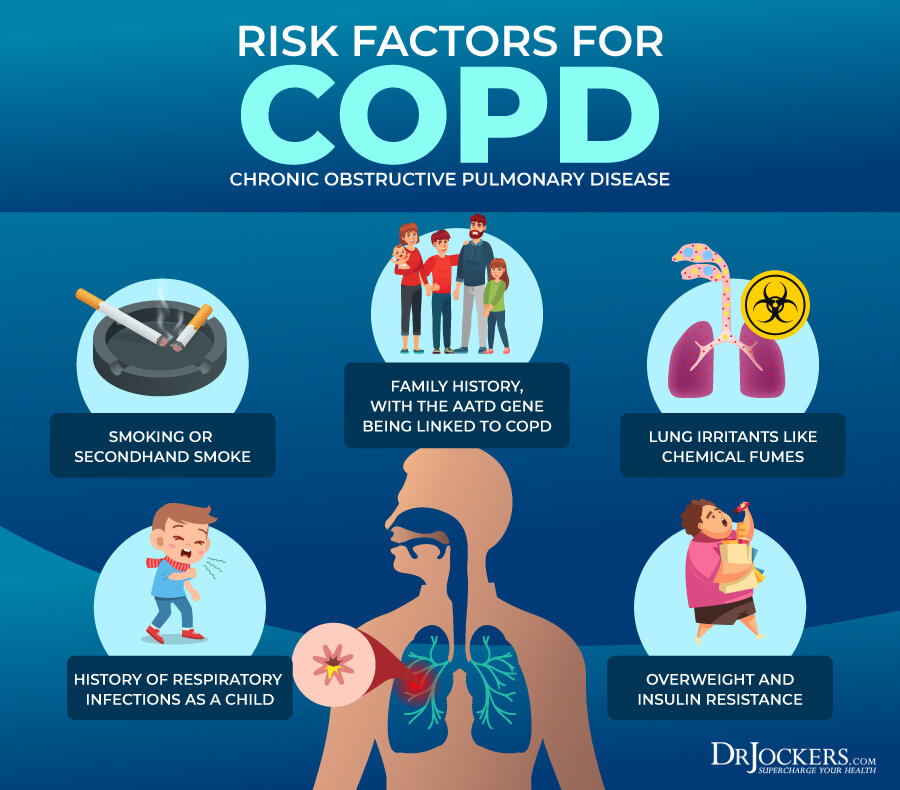
Considering that about 75 percent of people with COPD smoke or used to smoke, smoking cigarettes is one of the main risk factors for developing COPD (2). However, there are other risk factors that can contribute to the disease.
Risk factors for COPD include (2):
- Smoking
- Second-hand smoke
- Air pollution
- Chemical fumes
- Dust
- Other environmental lung irritants
- Family history
- Alpha-1 antitrypsin deficiency, a genetic condition that may be the cause of COPD in some rare cases
- Overweight and Insulin Resistance
Diagnosing COPD
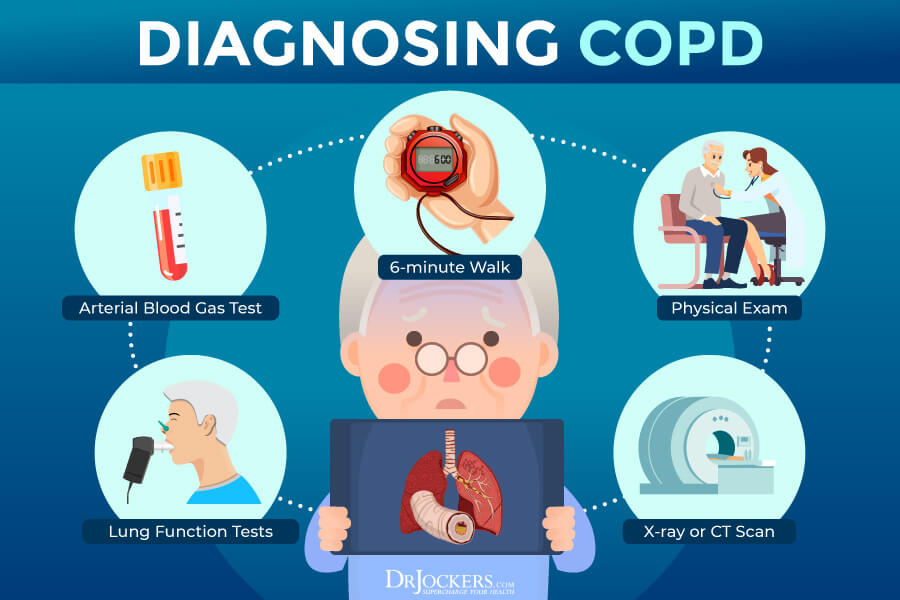
When diagnosing COPD, your doctor will first go over your medical and family history, signs and symptoms, and your risk factors, including if you are a smoker or if you’ve had contact with any lung irritants, including air pollution, chemical fumes, or second-hand smoke.
They will perform a physical exam and listen for abnormal chest sounds, wheezing, and other lung health issues. Other tests may include spirometry, an X-ray or CT scan, an arterial blood test, or other tests as needed (2). There is also a 6-minute walk test where the individual will walk for 6 minutes and then rate their level of fatigue, and this is often used as part of the COPD diagnosis.
COPD Conventional Treatments
There is currently no cure for COPD. Doctors recommend a variety of lifestyle strategies, medications, and other treatment options to reduce symptoms and help you stay active. The goal of the conventional treatment options is to reduce your symptoms, slow the progress of your COPD, improve function and exercise tolerance, prevent complications, treat any complications, and improve your overall well-being. Your doctor may recommend lifestyle changes, medication, pulmonary rehabilitation, oxygen therapy, or surgery depending on your symptoms and health (2).
Lifestyle Changes
Your doctor will recommend that you quit smoking and avoid second-hand smoke and other triggering lung irritants. Going to a support group for smokers may be recommended if you are struggling to quit on your own.
Your doctor may recommend strategies to keep you active, and you may work with a dietitian to develop an eating plan. Eating more frequent or smaller meals and resting before eating are often recommended for COPD patients (2).
Medication
Your doctor may prescribe bronchodilators, which help to relax the muscles around your airways to help you breathe more easily. Most bronchodilators are taken through an inhaler.
Depending on your stage, you may need to use this short-term or long-term. Your doctor may also prescribe a combination of bronchodilators and inhaled glucocorticosteroids to reduce inflammation, relieve breathing problems, and prevent flare-ups (2).
Pulmonary Rehabilitation
Pulmonary rehabilitation is often recommended. It may include an exercise program, nutritional strategies, psychological counseling, and disease management training. During your rehab, you will work with a team of doctors, nurses, respiratory therapists, exercise specialists, physical therapists, dietitians, and counselors, depending on your needs (2).
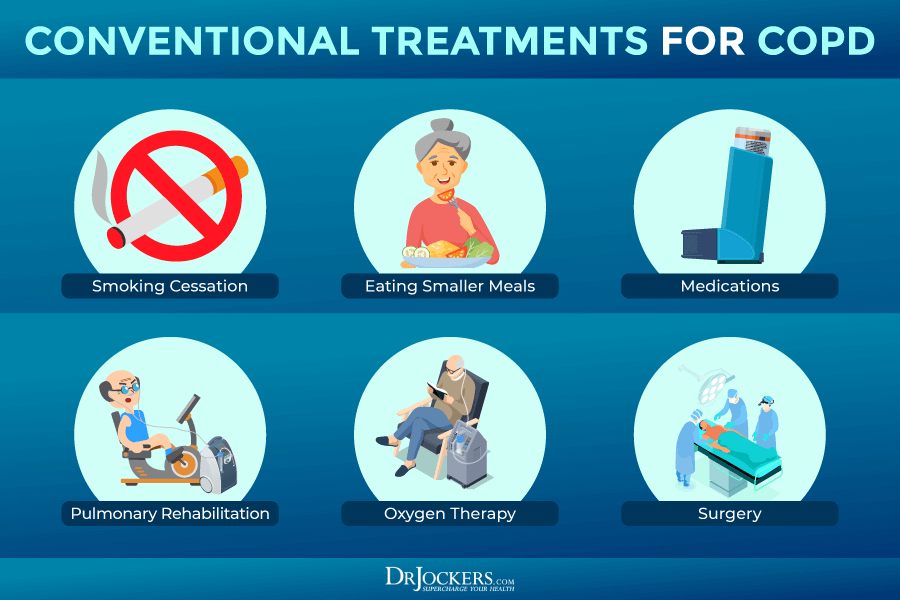
Oxygen Therapy
For people with severe COPD, oxygen therapy is often necessary to improve breathing, reduce symptoms, support sleep, reduce the risk of heart and other organ damage, and increase longevity. During this treatment, oxygen is delivered through nasal prongs or a mask (2).
Surgery
Surgery is recommended in certain severe cases of emphysema. Surgery options may include bullectomy, lung volume reduction surgery (LVRS), or a lung transplant. A bullectomy is performed to remove one or more large bullae from the lungs, which are air space formed when the air sacs are destroyed.
LVRS is performed to remove damaged lung tissue for better lung function. When a lung transplant is performed, doctors remove the damaged lung and replace it with a healthy lung from a donor. While a lung transplant can significantly improve one’s life, there are also a lot of risks, including infections and rejection of the new organ (2).
Root Cause Factors
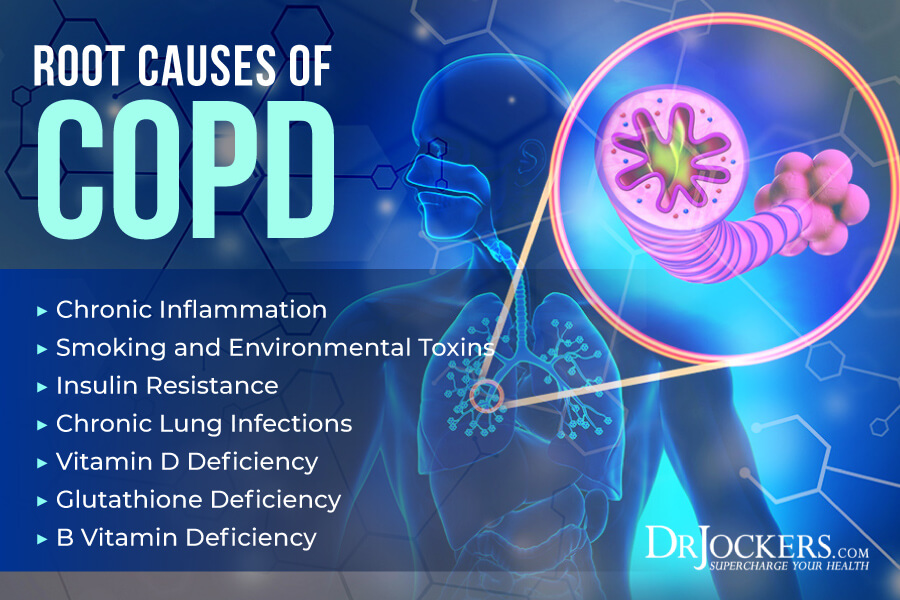
Now that you understand the most common risk factors of COPD, I want to go over the root cause factors of COPD that can further contribute to the development of the disease.
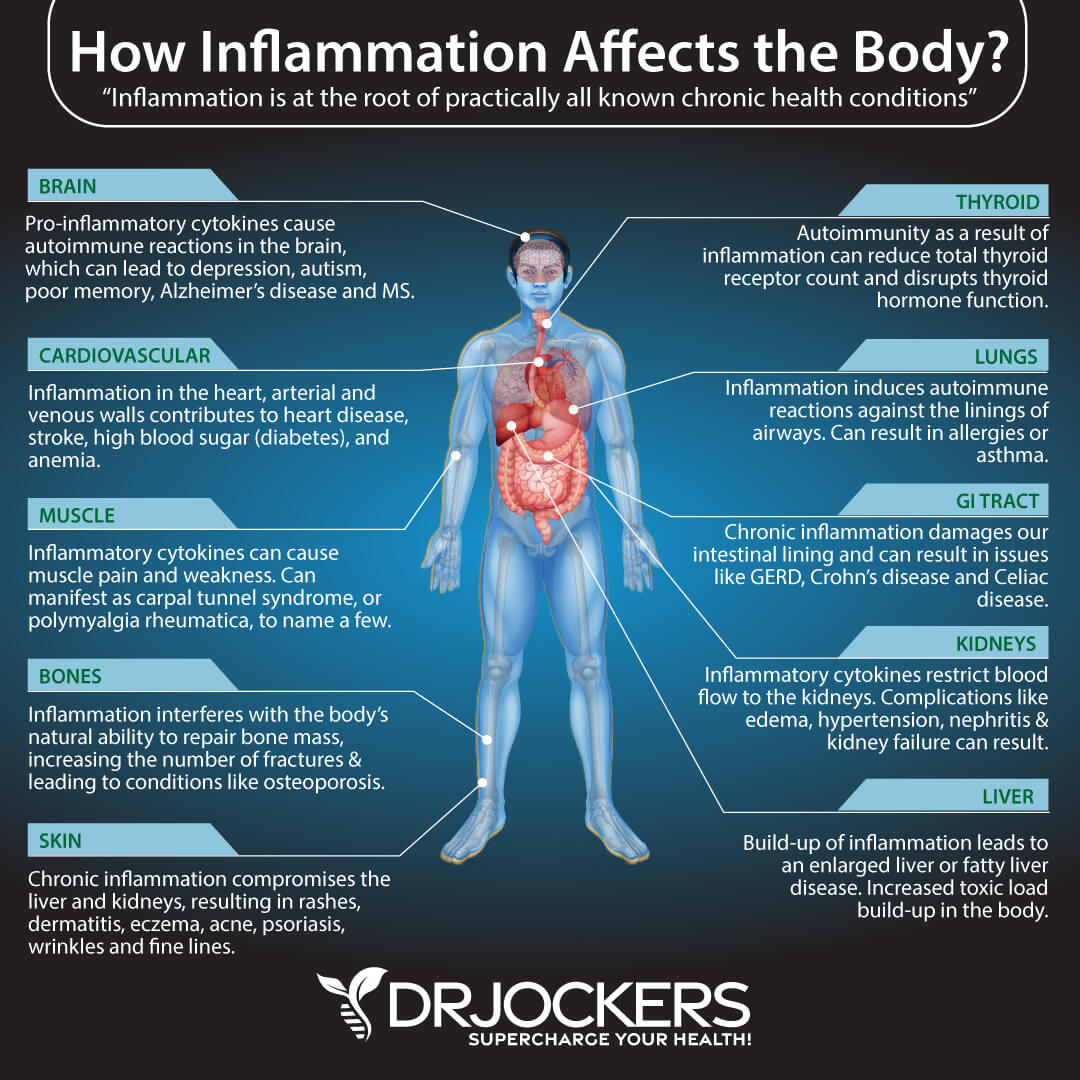
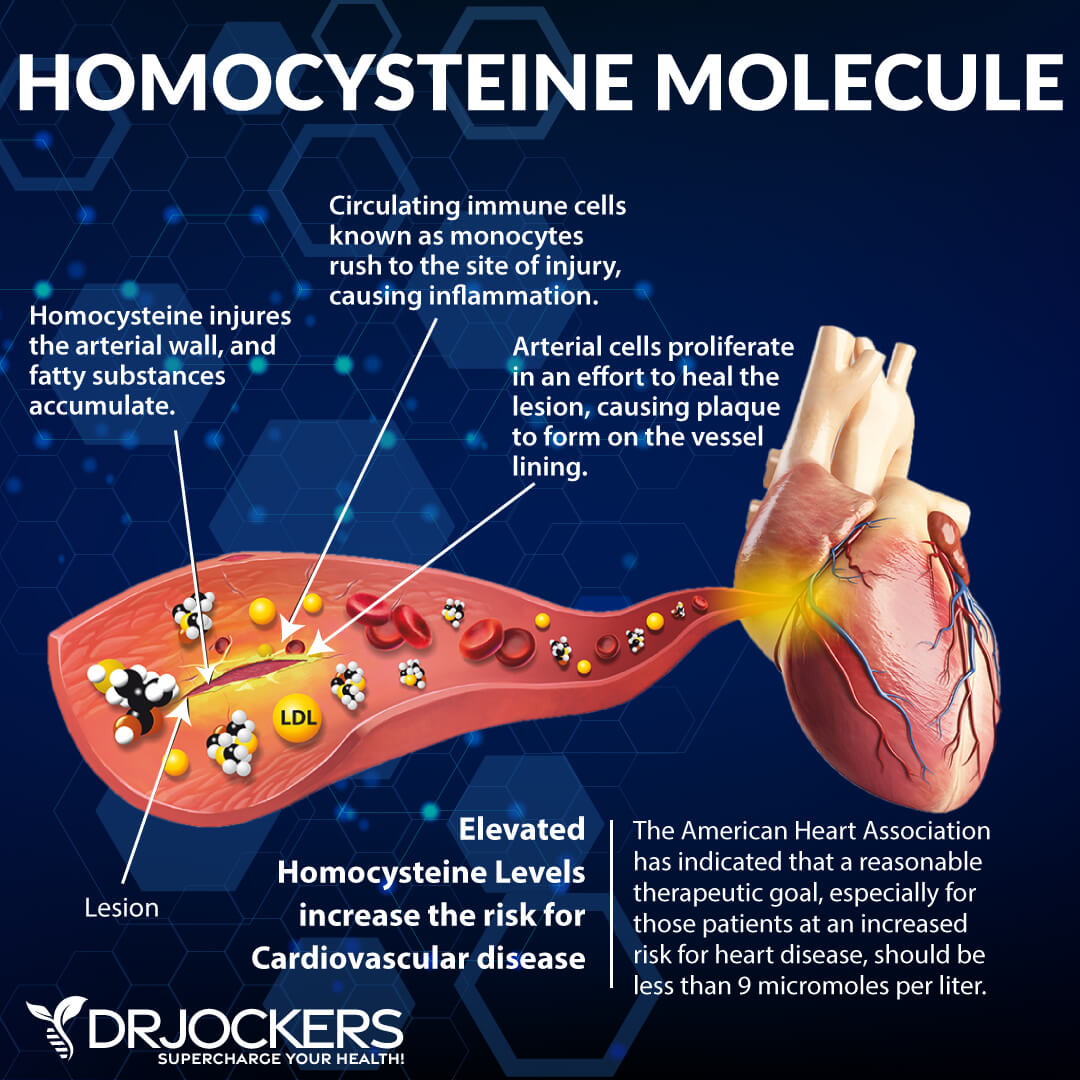
Chronic Inflammation
Chronic inflammation is one of the root causes of most diseases. This is not different for COPD either. According to a 2015 study published in Clinical and Translational Medicine, COPD is characterized by persistent lung inflammation, which can increase the risk of complications, lung cancer, heart disease, and stroke (4).
A 2012 study published in F1000 Medicine Reports discussed that lung inflammation plays a significant role in COPD and can increase symptoms and outcomes (5). It may develop because of acute and chronic effects of smoking, a poor lung microbiome, issues with innate immunity, autoimmunity, and nitric oxide. Researchers suggest that we must take inflammatory modulators into account when talking about the pathological processes of COPD.
Smoking and Environmental Toxins
We know that smoking cigarettes is the top contributing factor to COPD. About 75 percent of COPD patients are current or former smokers (2). However, lung irritants and environmental toxins play a role as well. Besides secondhand smoke, chemical fumes, dust, and air pollution, pesticides and herbicides may also contribute to the disease.
According to a 2013 study published in the International Journal of Environmental Research and Public Health, occupational pesticide exposure may impact respiratory health and increase the risk of COPD (6). A 2019 study published in the International Journal of Environmental Research and Public Health has found that herbicide exposure in veterans of the Vietnam War has increased spirometric pulmonary restriction associated with COPD (7).

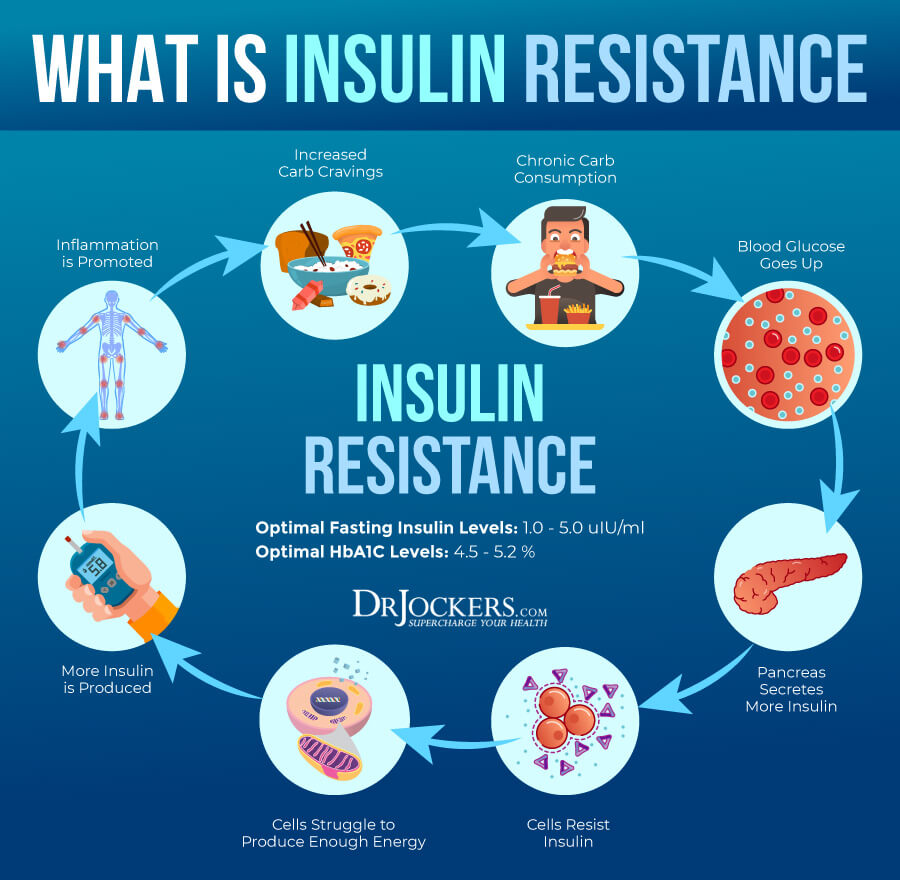
Insulin Resistance
Insulin resistance means that your body cannot respond to insulin well and is unable to properly deal with excess glucose in your blood. Insulin resistance increases the risk of prediabetes and diabetes, but also the risk of other health issues, including COPD. According to a 2018 study published in Endocrine, there may be a link between COPD and insulin resistance, as COPD is more common in people with diabetes or metabolic problems than in those without (8).
A 2015 study published in the Pakistani Journal of Medical Sciences has also found that the occurrence of insulin resistance is higher in COPD patients than in healthy subjects (9). A 2017 study published in PLoS One has found that smoking, insulin resistance, and vitamin D deficiency may all play a role in COPD (10).
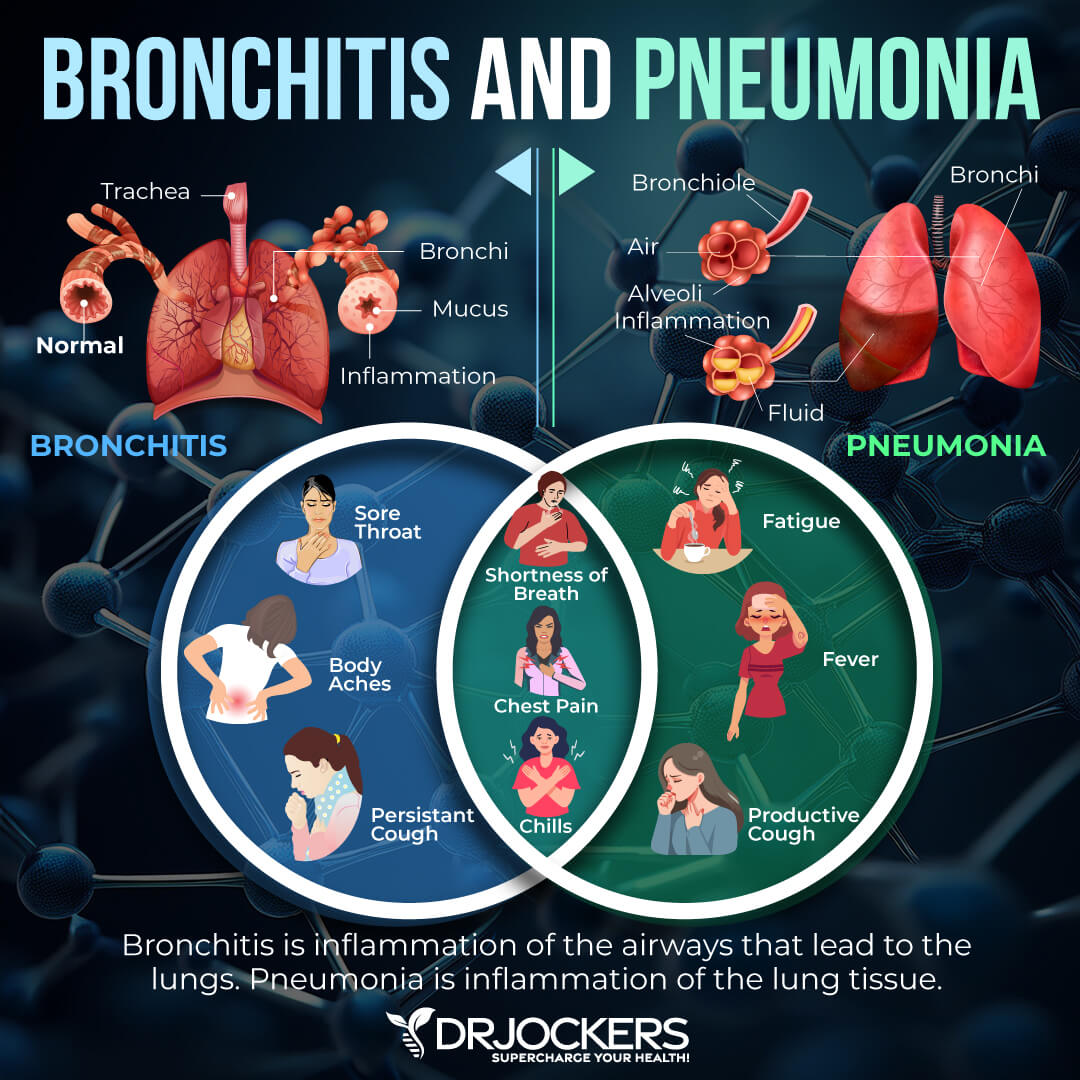
Chronic Lung Infections
Lung infections that cause scarring in the lungs can increase your risk of COPD or increase the progression and severity of the disease. According to 2009 research published in Pneumonologia i Alergologia Polska, COPD also increases the risk of lung infections that can worsen the disease (11).
Chronic lung infections that you need to be aware of may include chronic bronchitis, pneumonia, bronchiectasis-related pneumonia, cystic fibrosis-related pneumonia, and tuberculosis.
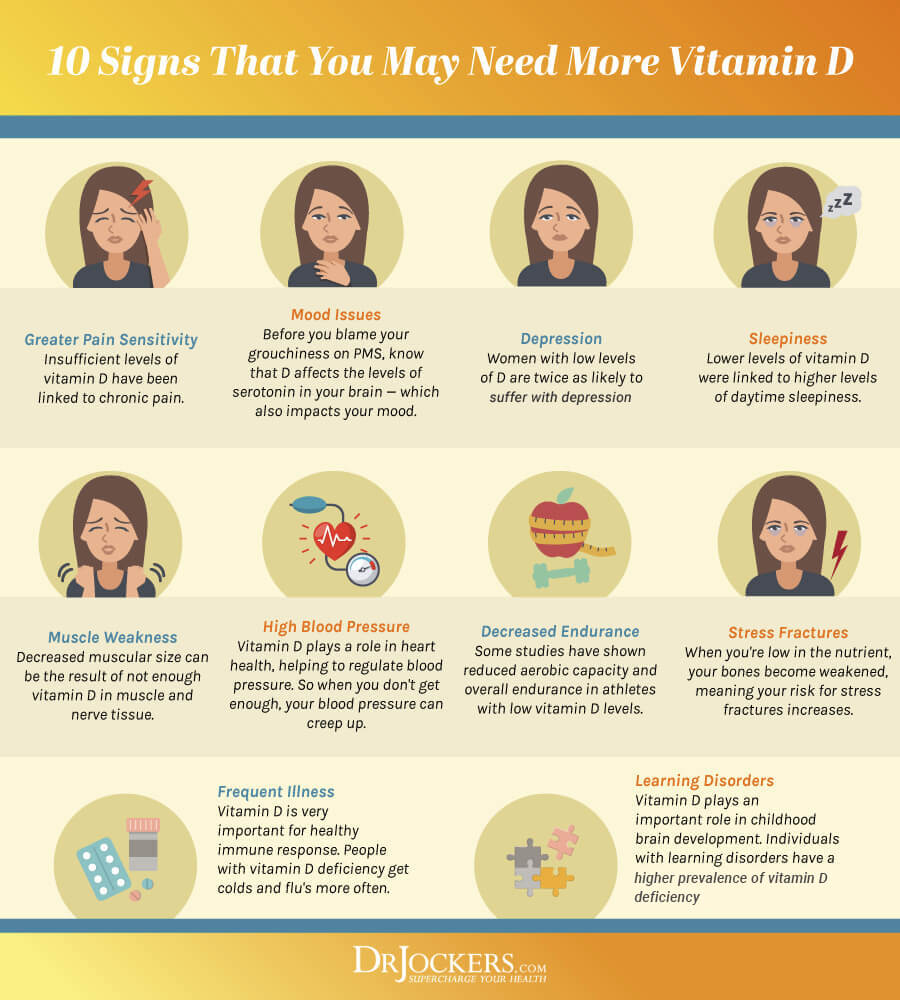
Vitamin D Deficiency
Vitamin D plays an important role in a variety of areas of your health, including your immune health and respiratory health. It is not surprising that vitamin D may play a role in COPD. According to a review published in the Clinical Respiratory Journal, vitamin D is associated with FEV1 decline and may contribute to COPD (12). A 2010 study published in Thorax found that vitamin D deficiency is highly prevalent in patients with COPD (13).
A 2011 study published in Vitamins and Hormones has also found that vitamin D deficiency plays a role in COPD by affecting the lung muscle tissue and increasing inflammation (14). According to a 2003 study published in the Journal of Allergy and Immunology, vitamin D modulates the Th1 and Th2 cytokine response and decreases issues with the airway and breathing (15).
A deficiency in vitamin D increases inflammation and immune health issues. Vitamin D helps to suppress proinflammatory cytokines and increase anti-inflammatory cytokines, which help to support the immune system. This can increase lung inflammation and the risk of COPD and complications.
Glutathione Deficiency
Glutathione is a powerful antioxidant found in plants, fungi, and animals, and helps to prevent damage to important cellular components and supports antioxidant levels. According to a 2010 study published in Cell Biochemistry and Function, glutathione deficiency may play a role in COPD as it can increase oxidation and inflammation (16).
They found that glutathione levels are generally lower in smokers and COPD patients. A 1999 review published in the American Journal of Physiology has also found that cigarette smoking may increase oxidative stress, deplete glutathione levels, and contribute to the pathogenesis of COPD (17).
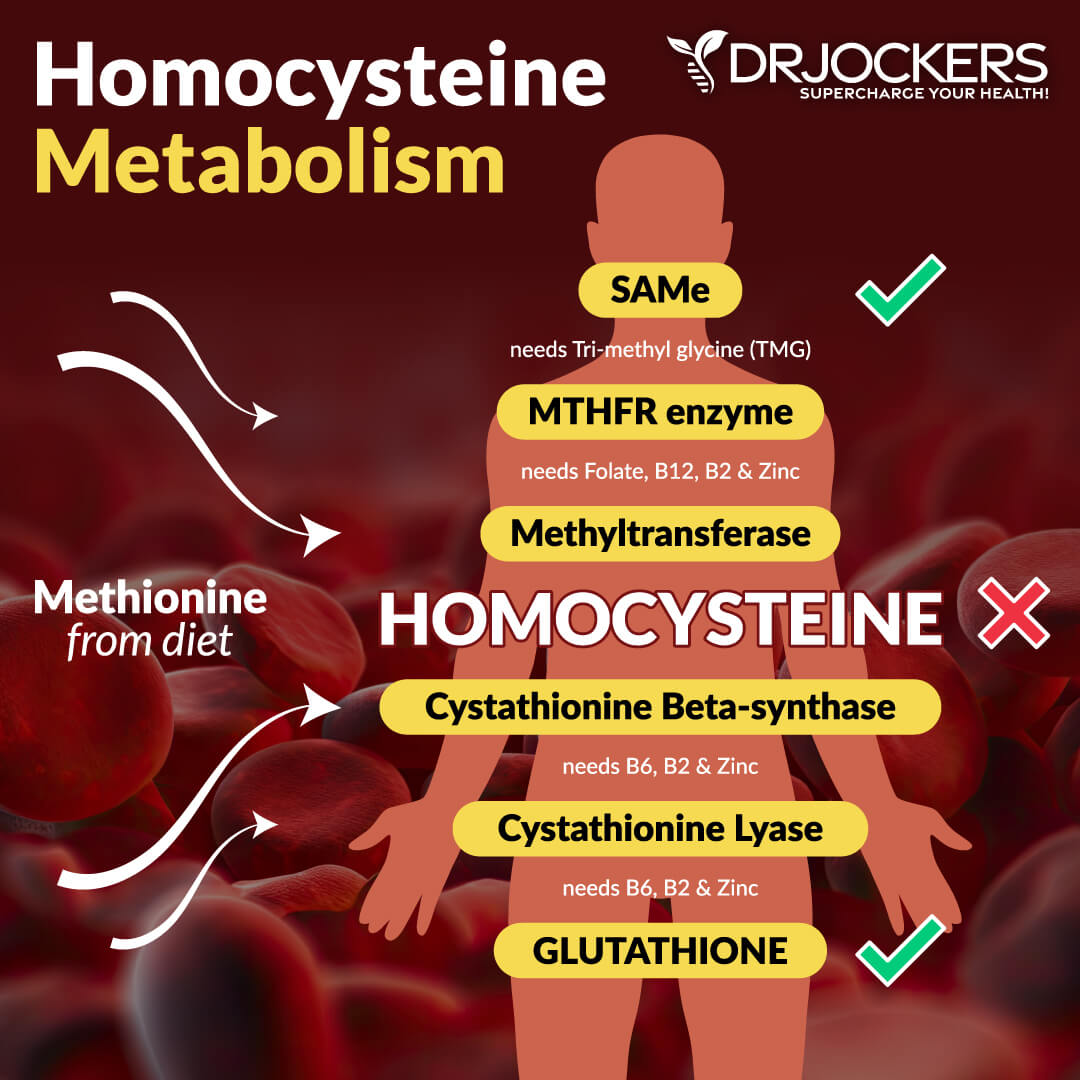
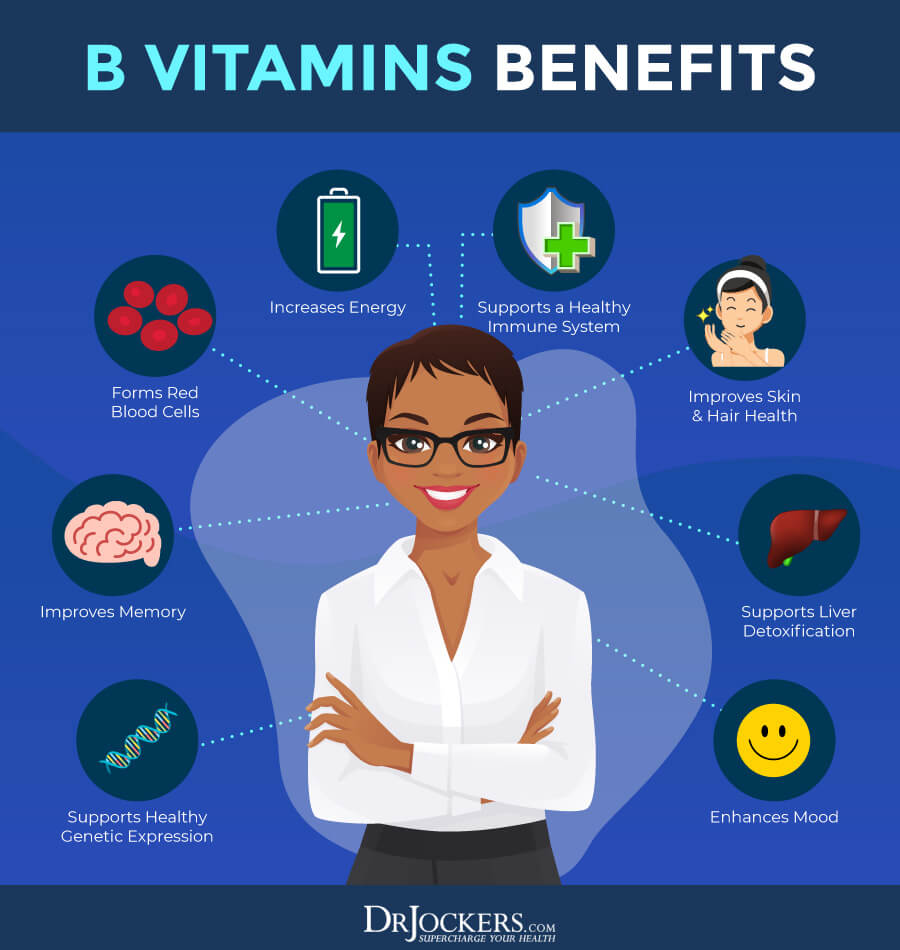
B Vitamin Deficiency
B vitamins are a group of vitamins that are important for a variety of aspects of your health, including cellular function, energy levels, and brain health. Low vitamin B levels, especially low folate levels, have been linked to COPD by recent research. A 2009 study published in Nutrition, Metabolism, and Cardiovascular Diseases (NMCD) has found that vitamin B deficiency and high homocysteine levels may increase the risk of COPD (18).
According to a 2010 study published in the Asian Pacific Journal of Clinical Nutrition, low folate levels may be linked to low lung function, breathlessness, and COPD (19). A 2020 nationwide population-based survey published in Nutrients has found that high folate levels are linked to better lung function in male COPD participants who smoke (20).
Key Lab Markers to Consider
If you have or at risk of COPD, I recommend that we look at several key lab markers that can indicate underlying levels of inflammation. You can read more about these lab markers in this article.
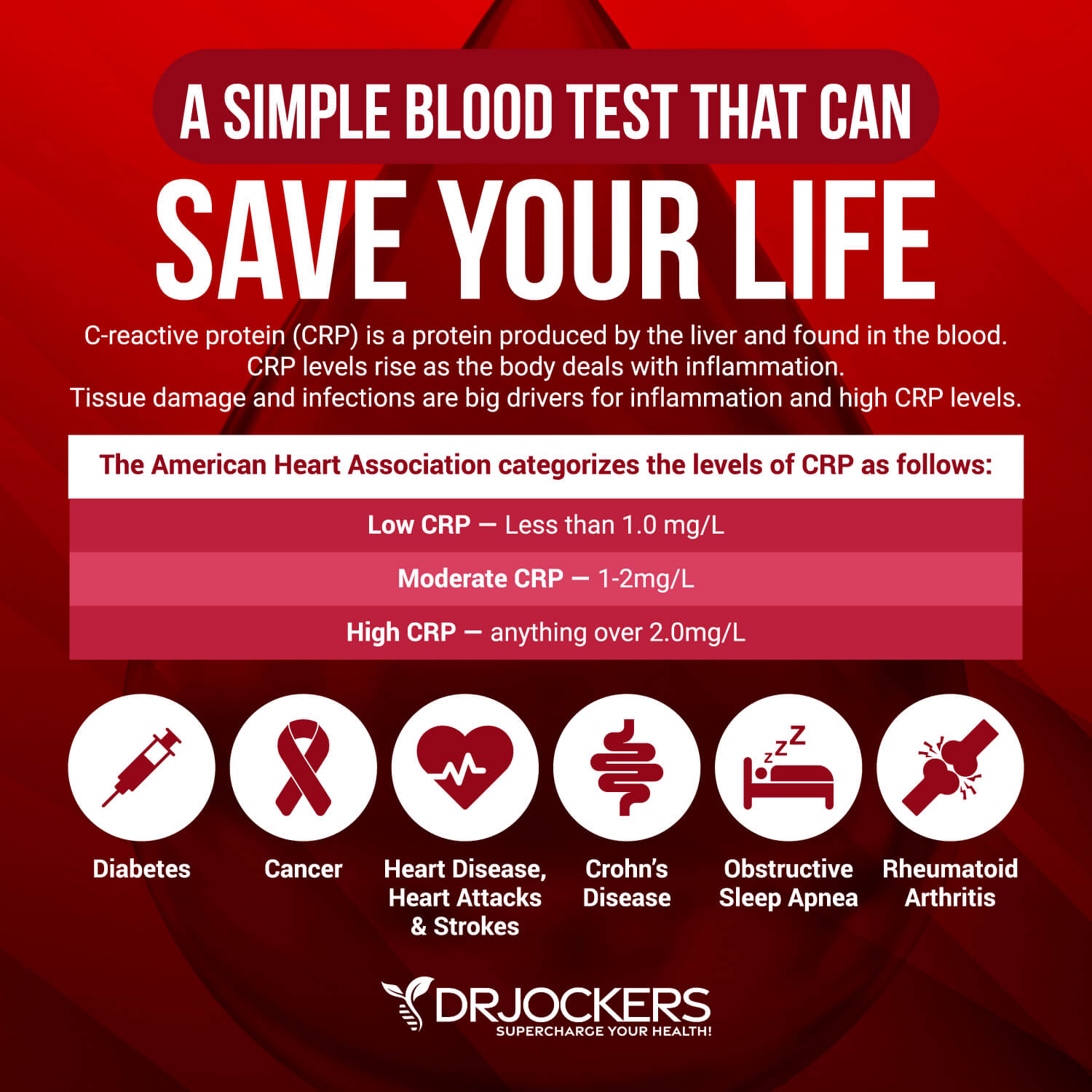
Hs-CRP
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L, while the optimal range is 0 to 1 mg/L.
When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions. Ideally, we want to see the CRP levels as low as possible, certainly under 1 mg/L and more like .01 mg/L.
HbA1C
Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months, making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6, while the optimal range is 4.5 – 5.2.
Fasting Insulin
In addition to testing your HbA1C levels, I recommend checking your fasting insulin levels. Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml, and the optimal range is 1.0 – 5.0 uIU/ml.
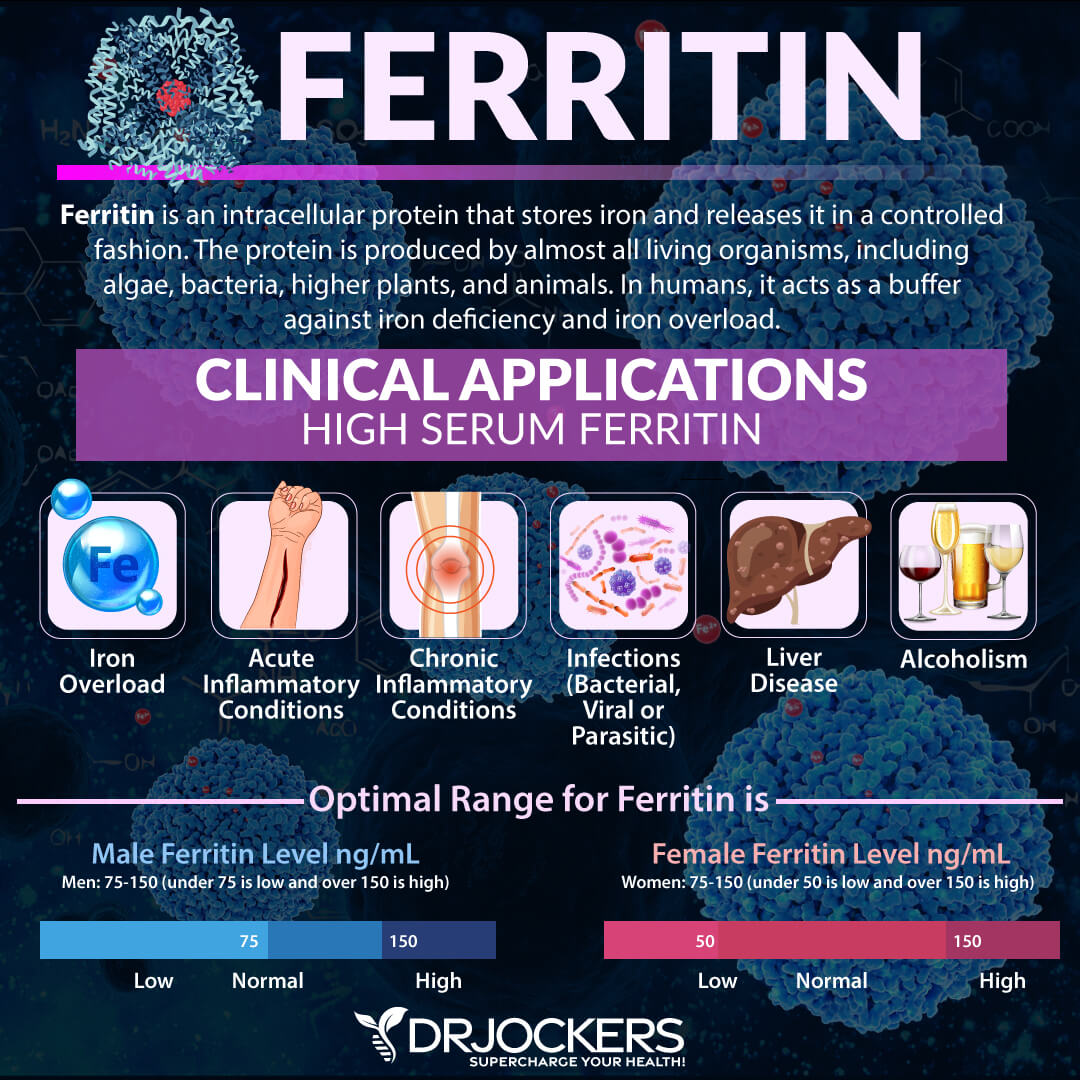
Serum Ferritin
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer. The optimal range is 30 to 400, and the optimal range is 50 to 150 for females and 75 to 150 for males.
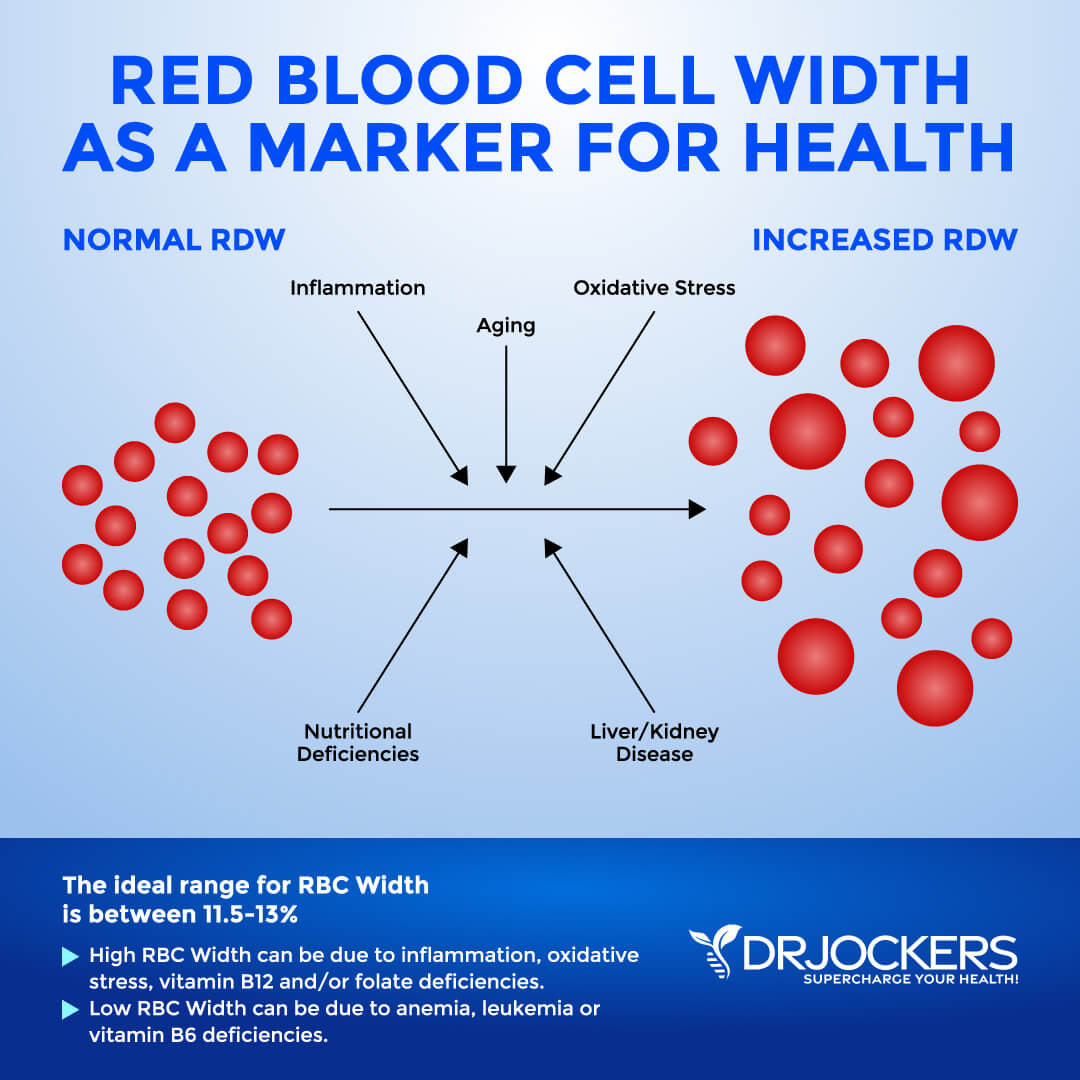
Red Blood Cell Width
The size of your blood cells has to do with maturation and also depends on methylating agents, such as folate and vitamin B12. Red Blood Cell Distribution (RDW) markers are a great way to detect underlying inflammation in your body.
The clinical range is between 12.3 and 15.4 percent, while the optimal range is 11.5 and 13 percent. When this level is above 13 percent, it may be a sign that inflammation has impacted the development of the red blood cell.
Homocysteine
Homocysteine is a common amino acid in your blood that you mostly get from eating meat. Homocysteine is a particularly good marker for cardiovascular issues. The optimal range for homocysteine is between 6 and 9 umol/L. Some practitioners like to see it under 8 umol/L.
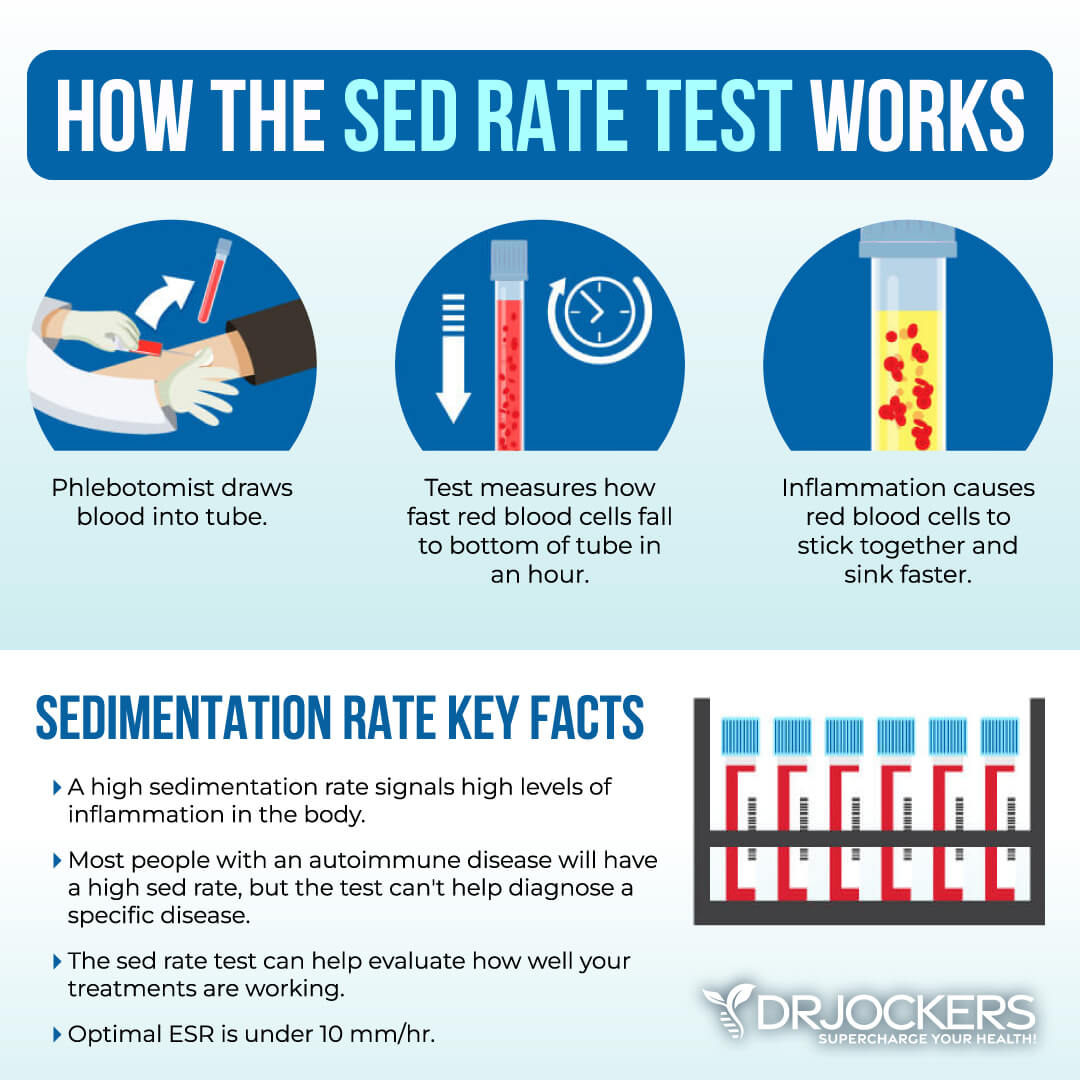
ESR
The erythrocyte sedimentation rate (ESR) is a common hematology test to look for inflammation. It refers to the rate at which your red blood cells in anticoagulated whole blood settle in a standardized tube over a period of one hour. Optimal ESR rates are between 0 and 10 mm/hr. Anything above 20 mm/hr is an indication of inflammation impacting the body.
You can also look at platelets as a measurement tool of inflammation and the stickiness of blood. Platelets elevated above 250 is a sign of inflammation. The sweet spot for platelets is between 175 and 250. Below 175, immune function and blood clotting are compromised; the same is true for levels above 250.
LDH
Lactate Dehydrogenase (LDH) is an enzyme found in all living cells. Its job is to help support energy production in the lactate and pyruvate cycle of glycolysis. Elevated levels may indicate inflammation. Optimal levels are between 140-180. Levels over 180 indicate inflammation.
Neutrophil-Lymphocyte Ratio
Neutrophil-Lymphocyte Ratio (NLR) is a measure of stress and inflammation that may affect your health. NLR is usually measured with the absolute count, and we want to see it at roughly 1.2-2.0. If you see that the number of neutrophils is more than twice the number of lymphocytes, it is a sign of chronic inflammation.
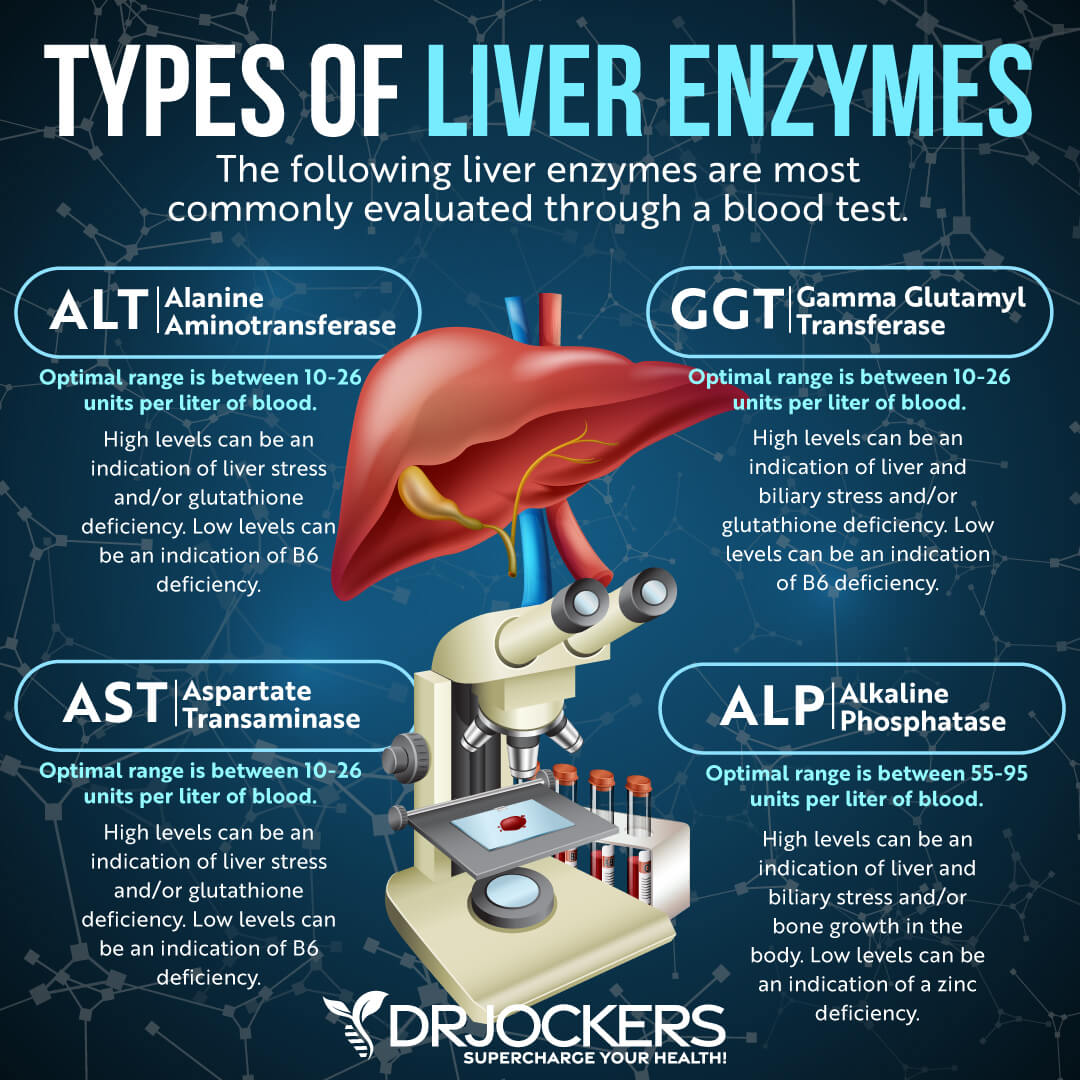
Liver Enzymes
Liver enzyme levels may also indicate inflammation, as well as liver, gallbladder, bile, or kidney issues. Elevated levels (over 95) may indicate inflammation and liver and gallbladder problems.
Alanine aminotransferase (ALT) is a liver enzyme. Elevated levels may indicate inflammation. Normal levels are between 10 and 26 IU/L.
Aspartate transaminase (AST) is an enzyme present in the liver that spills out during times of increased liver stress. Elevated levels may indicate inflammation. Normal levels are between 10 and 26 IU/L.
Gamma-Glutamyl Transpeptidase (GGT) is an enzyme in the liver, pancreas, and kidneys. Elevated levels may indicate inflammation and liver disease, usually due to alcoholism and/or sluggish gallbladder or gallstone obstruction. Normal levels are between 10 and 26 IU/L. Levels lower than 10 IU/L can be an indication of a vitamin B6 deficiency.
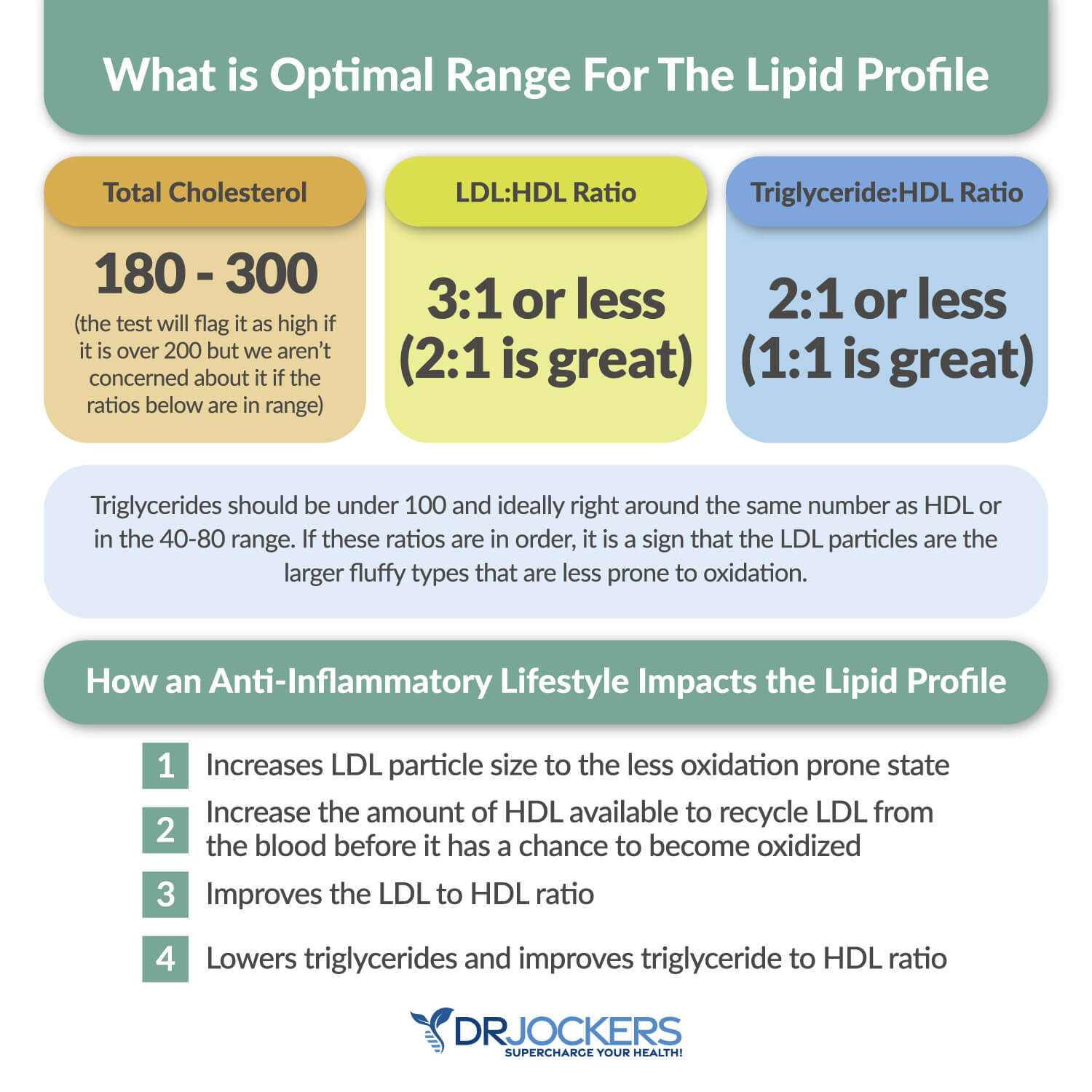
Lipid Panel
Your lipid panel may be another indication of inflammation and related issues, such as clogged arteries and cardiovascular issues. Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal. As we analyze triglycerides, we want them to be under 100, and we are looking for the Tri: HDL ratio to be 2:1 or less, 1:1 being optimal. Higher rates may indicate insulin resistance and inflammation. Optimal levels:
- VLDL cholesterol: The ideal range is 5 to 30 mg/dl.
- HDL cholesterol: The ideal range is 55 to 80. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The ideal range is 40 to 80.
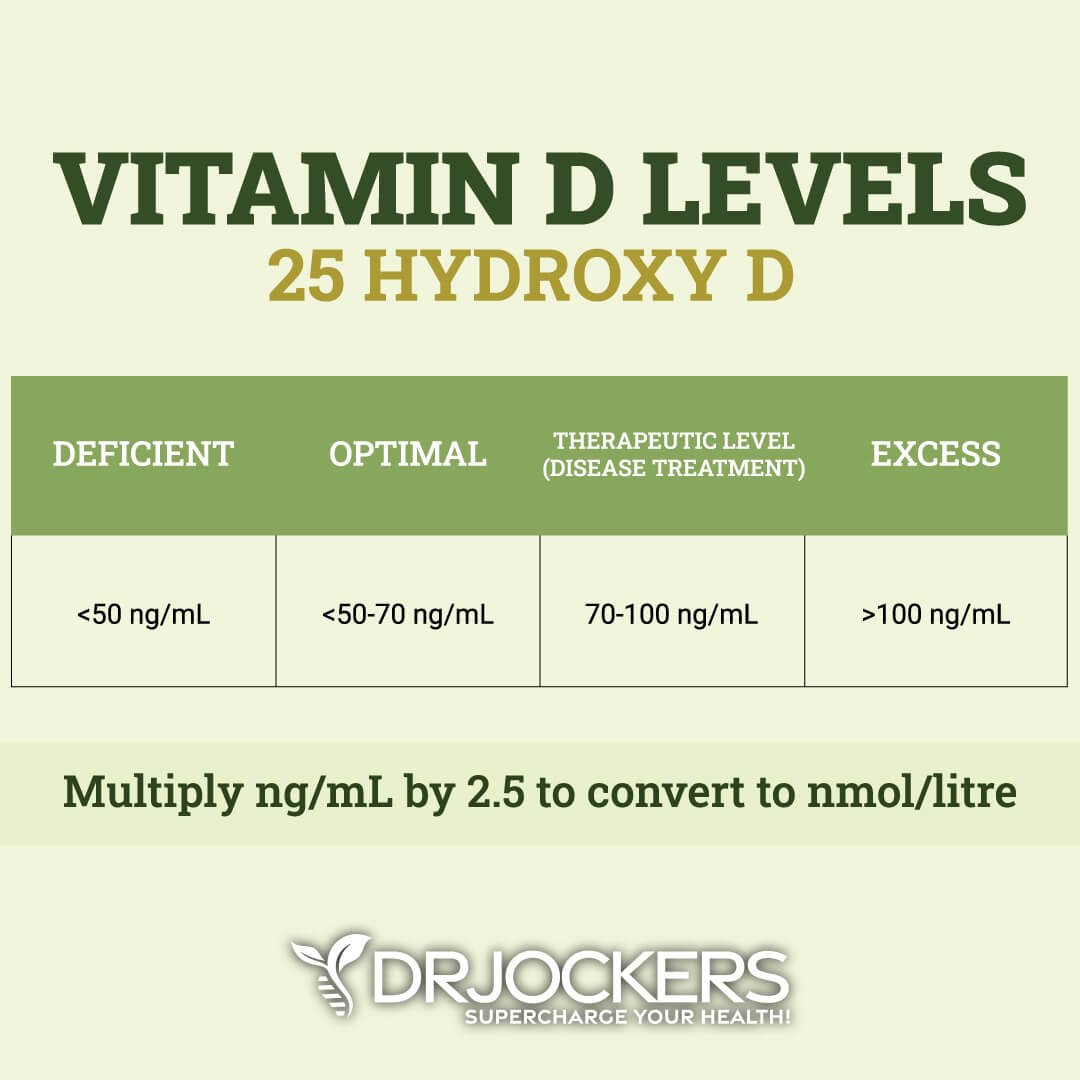
Vitamin D3
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. Optimal healthy levels of vitamin D are between 50 ng/mL and 70 ng/mL, while therapeutic levels are over 70 ng/mL up to 100 ng/mL.
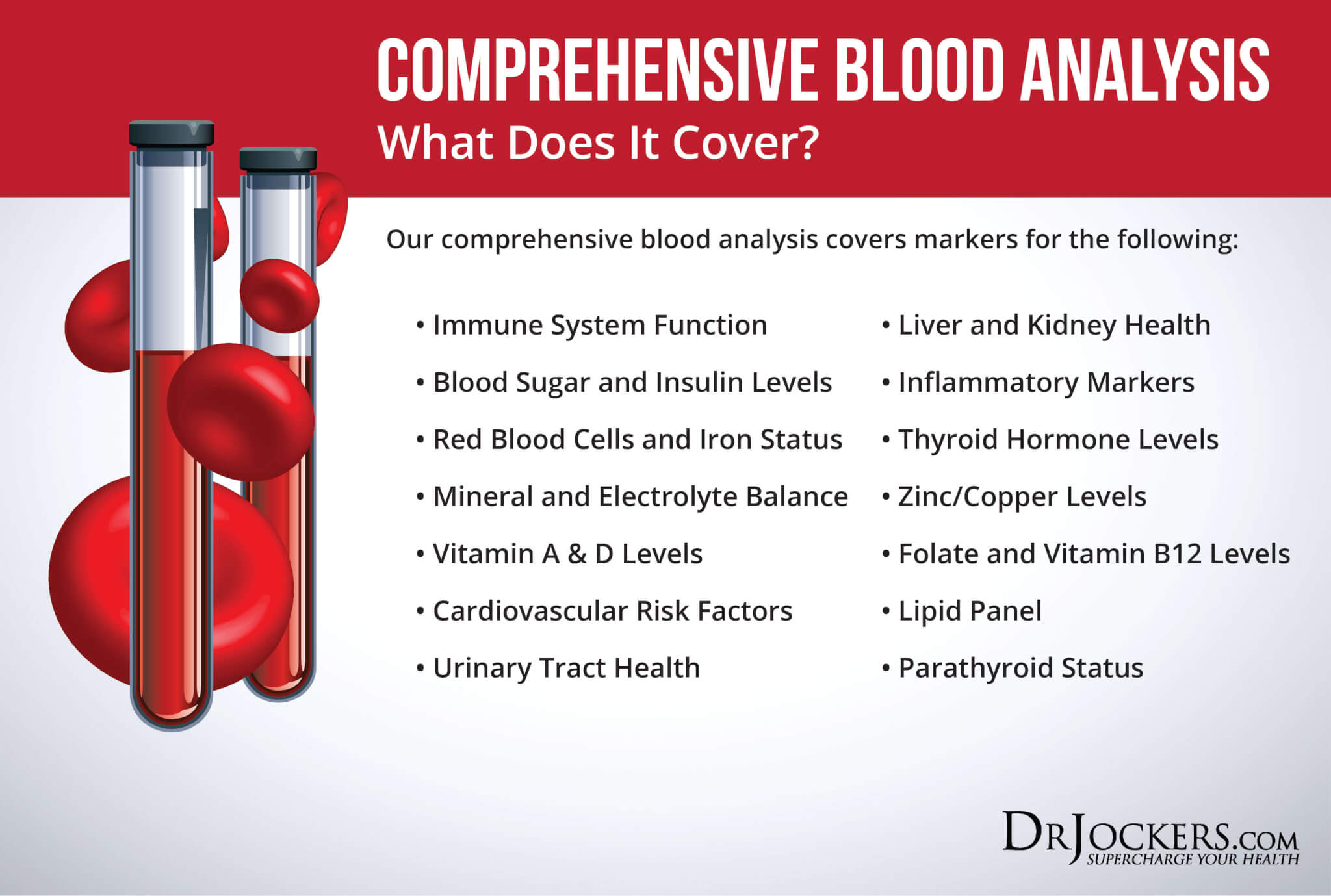
Comprehensive Blood Analysis
To check for these health markers, I recommend a Comprehensive Blood Analysis (CBA). This is the most detailed blood test that looks at all of these markers of inflammation.
This test is more sophisticated than most conventional doctors are able to order. It examines all parameters for inflammation, blood sugar levels, thyroid function, zinc and copper ratio, vitamin A and D levels, a complete metabolic panel, complete blood count, liver function, nutrient deficiencies, and more.
Natural Support Strategies for COPD
Your diet and lifestyle matter. How you treat your body and what you put into it can either support or damage your health, including your lung health.
This information has not been evaluated by the FDA and is not approved to prevent, treat, or cure any health condition. This is for informational purposed only and does not replace the medical advice you get from your doctor. These are the natural support strategies I recommend for COPD:
Reduce Exposure to Environmental Toxins
Environmental toxins, including cigarette smoke, secondhand smoke, chemical fumes, dust, air pollution, pesticides, and herbicides, can increase your risk of COPD (2, 6,7). It’s not surprising that I recommend reducing your exposure to environmental toxins.
Considering that the majority of COPD patients are smokers or former smokers, it is critical that you stop smoking as soon as possible. If you have difficulty quitting on your own, I recommend that you work with a therapist or join a support group.
It is important that you also avoid second-hand smoke. If there are smokers in your family or among your friends, urge them to quit. If someone is smoking around you, step away or ask them not to smoke or to move further away from you.
If you are working around chemical fumes, industrial pesticides or herbicides, or other pollutants, wear protective gear, and look for a safer job if possible. Reduce environmental toxins in your indoor air by using a HEPA filter at home and in your office.
Vacuum and clean your home regularly to reduce dust and allergens. Check for home and remove any indoor mold. Have indoor plants to improve your air quality, and spend plenty of time in nature to get fresh air.
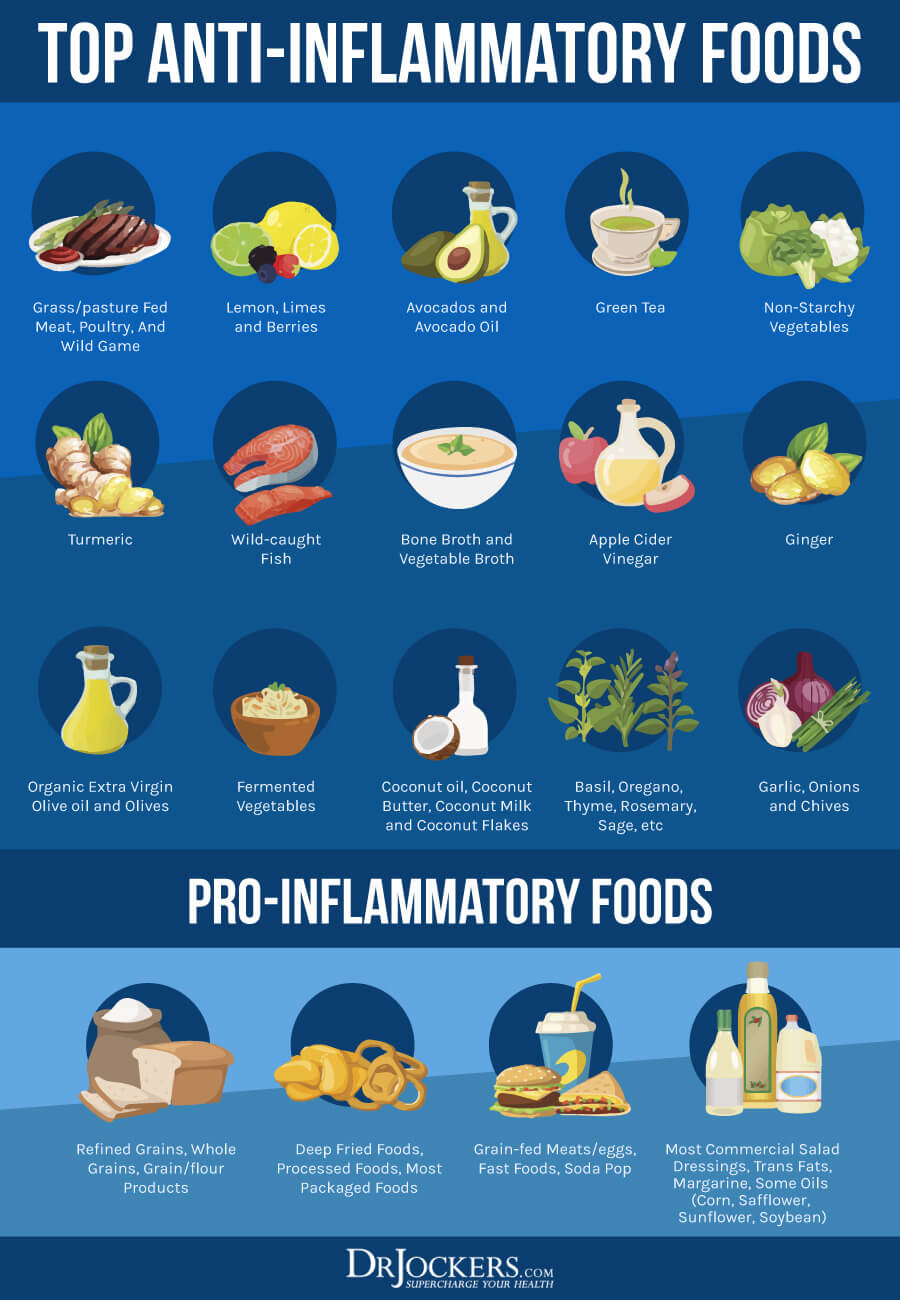
Anti-Inflammatory Nutrition Plan
Research studies have shown that chronic inflammation plays a role in the development and progression of COPD (4, 5). According to the American Lung Association, the right mix of nutrients can make breathing easier (21). Metabolism is the process of creating fuel from food.
Your body processes food and oxygen into energy and carbon dioxide. Processing carbohydrates for fuel produces the most carbon dioxide, while metabolizing fats creates the least, which means that eating a higher-fat and lower-carbohydrate diet can be easier for people with COPD.
A 2015 review published in the Journal of Translational International Medicine has found that a diet low in nutrients may increase the risk of a negative outcome and morbidity in COPD, while meeting your nutrient needs and improving muscle strength and exercise tolerance can help (22). To start, remove all inflammatory foods, including refined sugar, refined oil, artificial ingredients, deep-fried foods, junk food, and highly processed foods.
I recommend that you fuel your body with greens, vegetables, low glycemic index fruits, herbs, spices, fermented foods, nuts, seeds, and high-quality animal proteins, such as grass-fed beef, pasture-raised poultry, and eggs, wild-caught fish, and wild game.
Focus on healthy fats, such as avocados, coconut oil, olives, pasture-raised butter and ghee, and extra-virgin olive oil, while eating moderate levels of clean protein and low amounts of healthy carbohydrates, such as sweet potatoes, beets, carrots, and berries.
Intermittent Fasting
The Lung Health Institute recommends fasting for COPD patients because it may help to support their immune system, remove damaged cells, reduce excess body fat, and lower inflammation (24). A 2015 review published in the Journal of Nutrition, Fasting, and Health has also found though the evidence is not clear and more research is needed, some research suggests that intermittent fasting may help the symptoms of COPD (25).
When practicing intermittent fasting, you cycle between periods of fasting and periods reserved for meals during a day. If you are new to intermittent fasting, start with a 12-hour fasting window, practicing the Simple Fast. Stop eating after dinner and don’t eat until breakfast, 12 hours later.
Gradually increase your fasting window by pushing your breakfast to a later time. Most people feel the best when practicing fasting for 16 hours using the 16:8 method; however, you may thrive with a slightly shorter or longer fasting window.
Women may benefit from Crescendo fasting. You can find information about the best intermittent fasting strategies by searching my website or reading my book, The Fasting Transformation.

Reduce Stress and Improve Sleep
Chronic inflammation plays a role in the development and progression of COPD (4, 5). Since chronic stress and poor sleep can increase chronic inflammation, poor immunity, and the increased risk of symptom flares, reducing your stress and improving your sleep is important. I recommend that you practice meditation, daily gratitude, breathwork, journaling, relaxing exercises, and prayer to reduce your stress levels.
Avoid stress as much as possible. For example, stop scrolling through the news all day; it is enough to check it once a day. Spending time in nature, connecting with friends, family, and your community, and delegating daily ‘me-time’ are all important for stress reduction.
Commit to going to bed and waking up around the same time every day. It helps to support your natural sleep cycle. Avoid sugar, caffeine, alcohol, heavy foods, electronics, and stress close to bedtime. Engage in relaxing activities, such as board games, coloring, taking a bath, reading a book, having a relaxed conversation, meditation, or prayer. Make sure that you have comfortable pillows and bedding and a supportive bed.

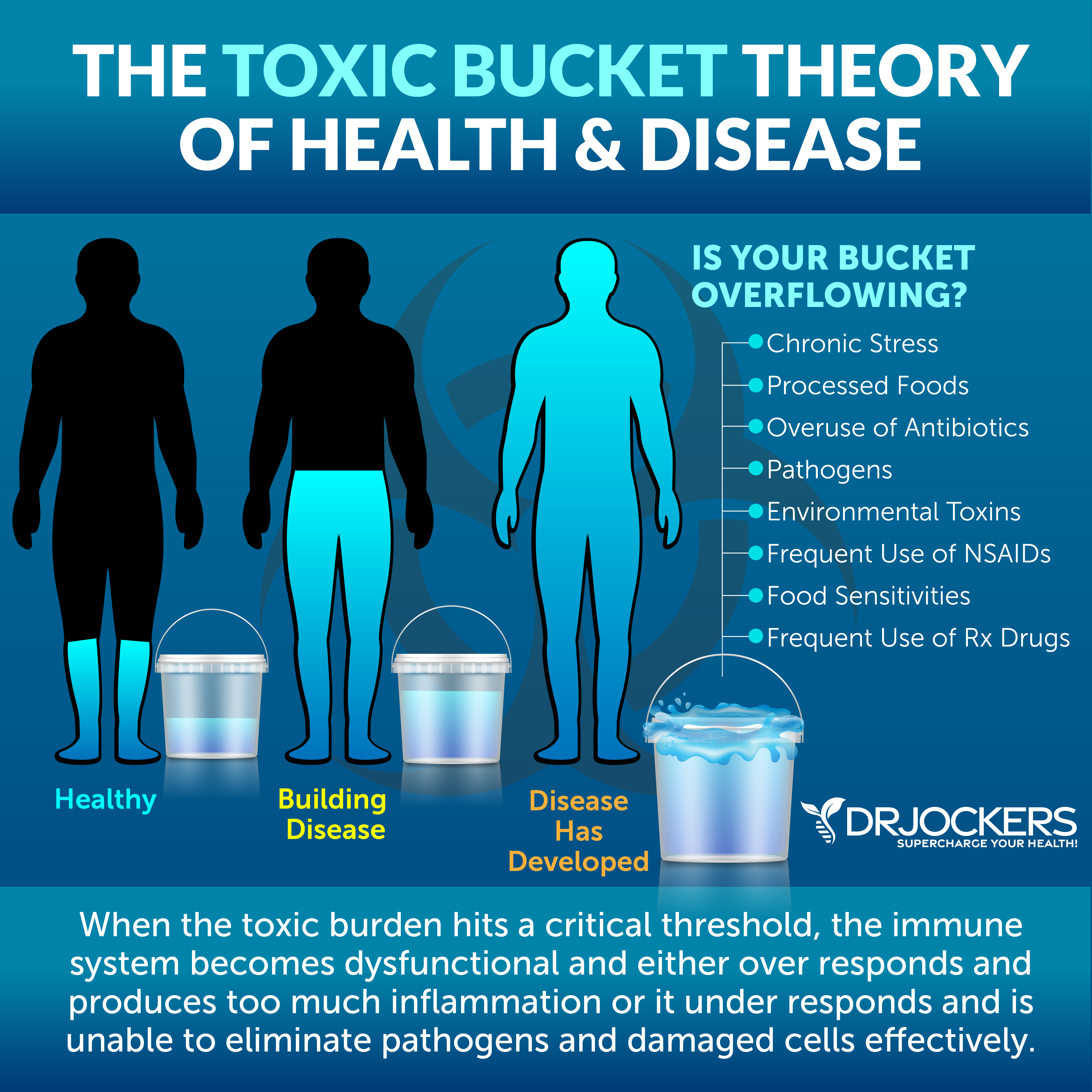
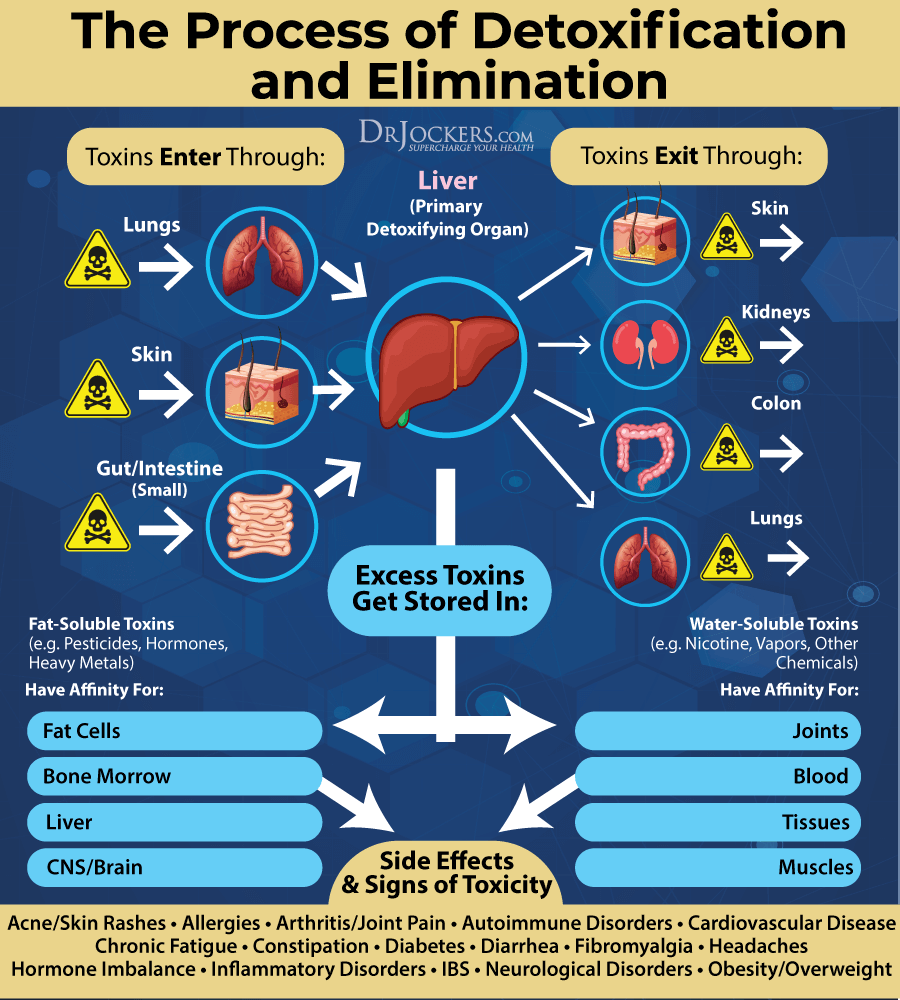
Improve Detoxification Pathways
Environmental toxins, including cigarette smoke, secondhand smoke, chemical fumes, dust, air pollution, pesticides, and herbicides, can increase your risk of COPD, while inflammatory foods and dietary toxins can increase inflammation and contribute to your symptoms (2, 6,7).
Improving your detoxification pathways is very important. Support your digestion, absorption, and elimination pathways through a healthy diet. Drink plenty of clean, purified water to improve detoxification through urine and sweating.
Support detoxification through the skin by sweating through exercise and using an infrared sauna regularly. Spend plenty of time in nature and improve your indoor air quality by using a HEPA filter to support your lungs in receiving clean air and releasing toxins.
I recommend activated coconut charcoal that binds to toxins in your body. It supports the elimination of these toxins and lowers inflammation and oxidative stress.
Try bioactive carbons derived from multiple sources of humic acid, fulvic acid, and humic acid that support the removal of heavy metals and other toxins and improve detoxification pathways. I recommend working with a functional health practitioner who can help you with specific heavy metal detox supplements and other supplementation for detoxifying from other toxins or infections.
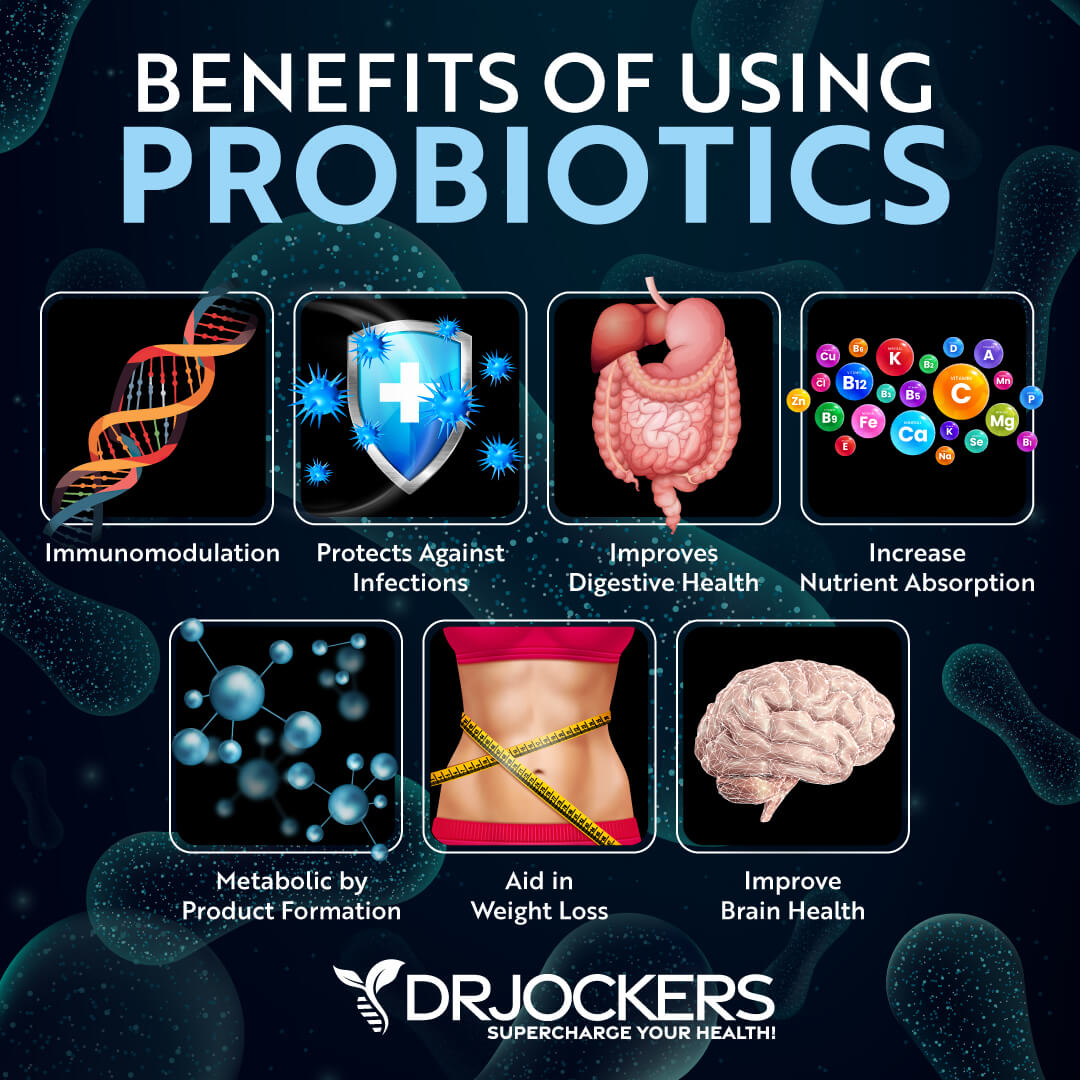
Support Gut Health and Use Probiotics
A 2018 study published in Frontiers in Microbiology has found that your gut and lung health are connected (26). This phenomenon can be described as the gut-lung axis. Gut dysbiosis has been connected to a variety of lung health issues, including allergies, asthma, and cystic fibrosis. Poor gut health can also increase inflammation, lower immune health, and increase the risk of respiratory conditions, infections, and lung inflammation.
Improving your gut health with probiotics can also improve your lung health. A 2020 animal study published in PLoS One has found that probiotics can reduce inflammation in bronchial cells in smoke-induced COPD (27). A 2020 study published in Nutrition Research Reviews has found that oral and nasal probiotics can improve COPD, allergies, and asthma (28).
I recommend that you eat probiotic-rich fermented foods, including kimchi, sauerkraut, fermented vegetables, coconut kefir, and kombucha. Additionally, I recommend a high-quality daily probiotic supplement and a probiotic throat spray.
Optimize Vitamin D Levels
Research has shown that vitamin D deficiency can contribute to COPD, so optimizing your vitamin D levels is important (12, 13, 14, 15). A 2019 meta-analysis and systematic review published in Thorax and a 2017 study published in the Pakistani Journal of Medical Science have both found that vitamin D supplementation may help to prevent the worsening of COPD symptoms (29, 30). A 2020 study published in the Annals of Palliative Medicine has also found that vitamin D may benefit the treatment of COPD (31).
I recommend that you spend time outside in the sun to get some vitamin D and eat foods that are rich in vitamin D, such as fatty fish, liver, and egg yolk. However, this is not enough to meet all your needs, so I recommend that you supplement with vitamin D daily.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml.
Support B Vitamin Levels
B vitamin deficiencies, especially folate deficiencies, seem to correlate with COPD symptoms, and supporting your vitamin B levels may help your condition (18, 19, 20). I recommend that you eat plenty of foods that are rich in B vitamins, including pasture-raised eggs and poultry, organ meats, such as liver and kidney, grass-fed beef, wild-caught fish, shellfish, beets, avocados, dark green vegetables, such as kale and spinach, and citrus.
To ensure that your B vitamin levels are optimal, I recommend that you take a high-quality B vitamin complex supplement daily. Since many people have methylation issues and have difficulty with absorption, make sure you select a methylated form of B vitamin supplements.
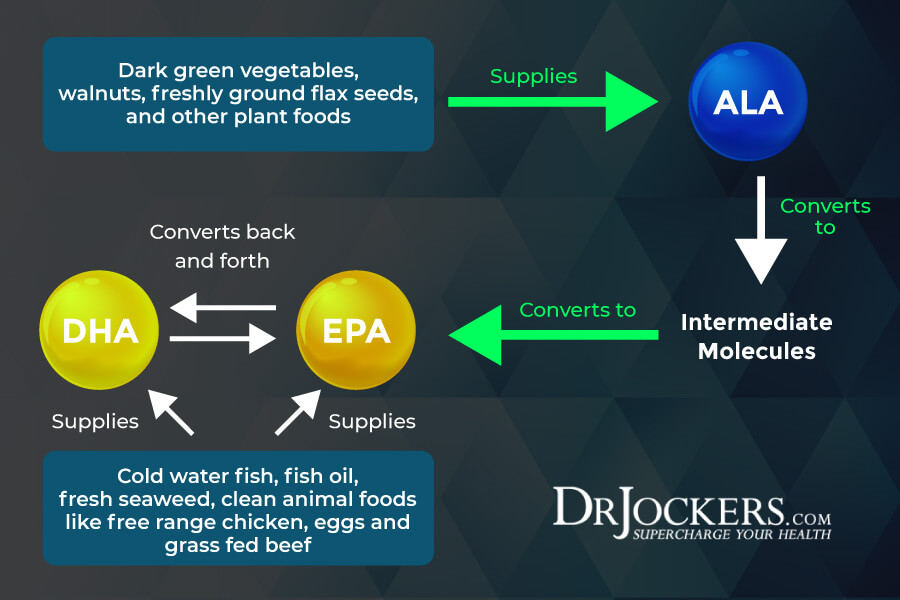
Use Omega-3 Fatty Acids
Chronic inflammation plays a role in the development and progression of COPD, and improving your anti-inflammatory omega-3 fatty acid levels may help (4, 5). A 2008 study published in Chest has found that omega-3 fatty acid supplementation may improve inflammatory markers in COPD patients (32).
A 2019 study published in Respiratory Medicine has found that the intake of omega-3 and omega-6 fatty acids and the balance between the two can impact COPD morbidity (33). The study has found that too many omega-6 fatty acids can be highly problematic and even detrimental, while a high intake of omega-3 fatty acids can be helpful.
I recommend that you eat plenty of foods that are rich in omega-3 fatty acids, including wild-caught fish, seafood, algae, hemp seeds, chia seeds, and flax seeds. To support your omega-3 levels and reduce inflammation, I recommend that you take a high-quality omega-3 fish oil supplement as well.
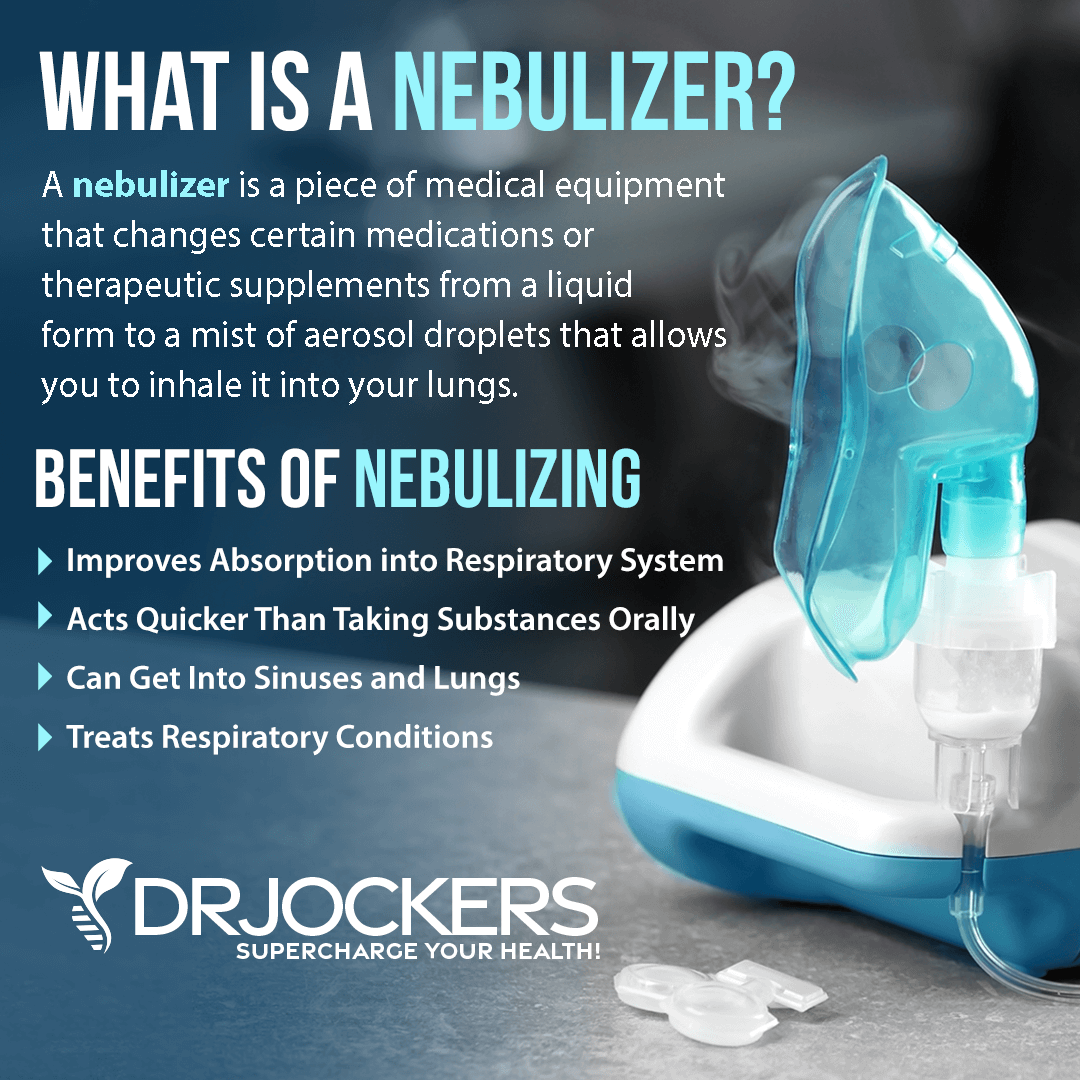
Nebulize NAC or Glutathione
Research has shown that glutathione deficiencies can affect COPD symptoms and outcomes (16, 17). Nebulizing with glutathione and N-acetyl cysteine (NAC) can be helpful. NAC is an essential amino acid that is important for the production of glutathione.
A 2000 case study published in Alternative Medicine Reviews has found that nebulizing with glutathione can support the treatment of emphysema and COPD (34). A 2019 study published in the European Respiratory Journal has found that NAC used through inhalation or orally can help COPD patients (35).
Diffuse Essential Oils
Diffusing essential oils may also help to improve your breathing and symptoms. A 2009 placebo-controlled double-blind trial published in Respiratory Research has found that eucalyptus oil can reduce the worsening of symptoms in COPD patients (36). A 2017 animal study published in Scientific Reports has found that essential oils may reduce acute airway inflammation (37).
According to a 2015 review published in Flavour and Fragrance Journal, essential oils may play a role in reducing inflammation in bacterial respiratory infections (38). A 2009 study published in the European Journal of Medical Research has found that essential oils can offer anti-inflammatory benefits in COPD patients (39).
The essential oils I recommend for lung and respiratory health include eucalyptus oil, lavender oil, bergamot oil, sweet orange oil, frankincense oil, and myrrh oil. However, certain oils may be triggering for some people, so it’s important that you try them for a short time at first to see how your body reacts.
Use high-quality essential oils. Diffuse them in well-ventilated places for no more than 60 minutes at a time.

Improve Antioxidant Levels
Improving your antioxidant levels may also be beneficial for people with COPD. There are a variety of antioxidants I recommend.
Vitamin C
Vitamin C is possibly the most well-known vitamin that we all take when we are feeling under the weather. According to a 2012 study published in the International Journal of Chronic Obstructive Pulmonary Disease, vitamin C may help to provide protection against COPD (40).
I recommend that you eat foods rich in vitamin C, including citrus, strawberries, black currants, Brussels sprouts, pepper, and broccoli. Additionally, I recommend that you supplement with vitamin C daily.

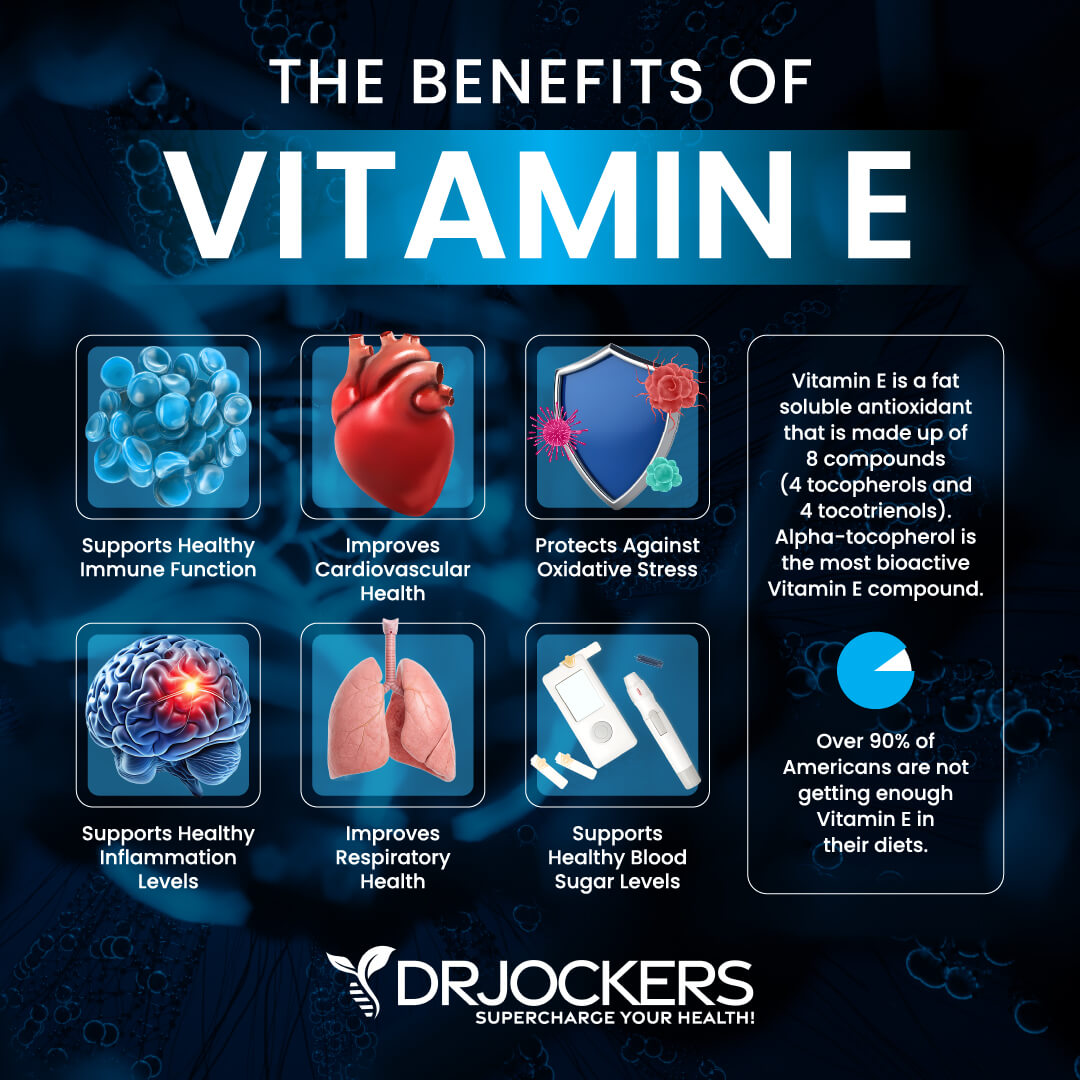
Vitamin E
Vitamin E is another important vitamin. According to a 2011 randomized controlled trial published in Thorax, taking vitamin E can reduce the risk and symptoms of chronic lung disease, like COPD (41).
I recommend eating foods that are rich in vitamin E, including sunflower seeds, almonds, beet greens, collard greens, spinach, and red bell pepper, as well as supplementing with vitamin E.
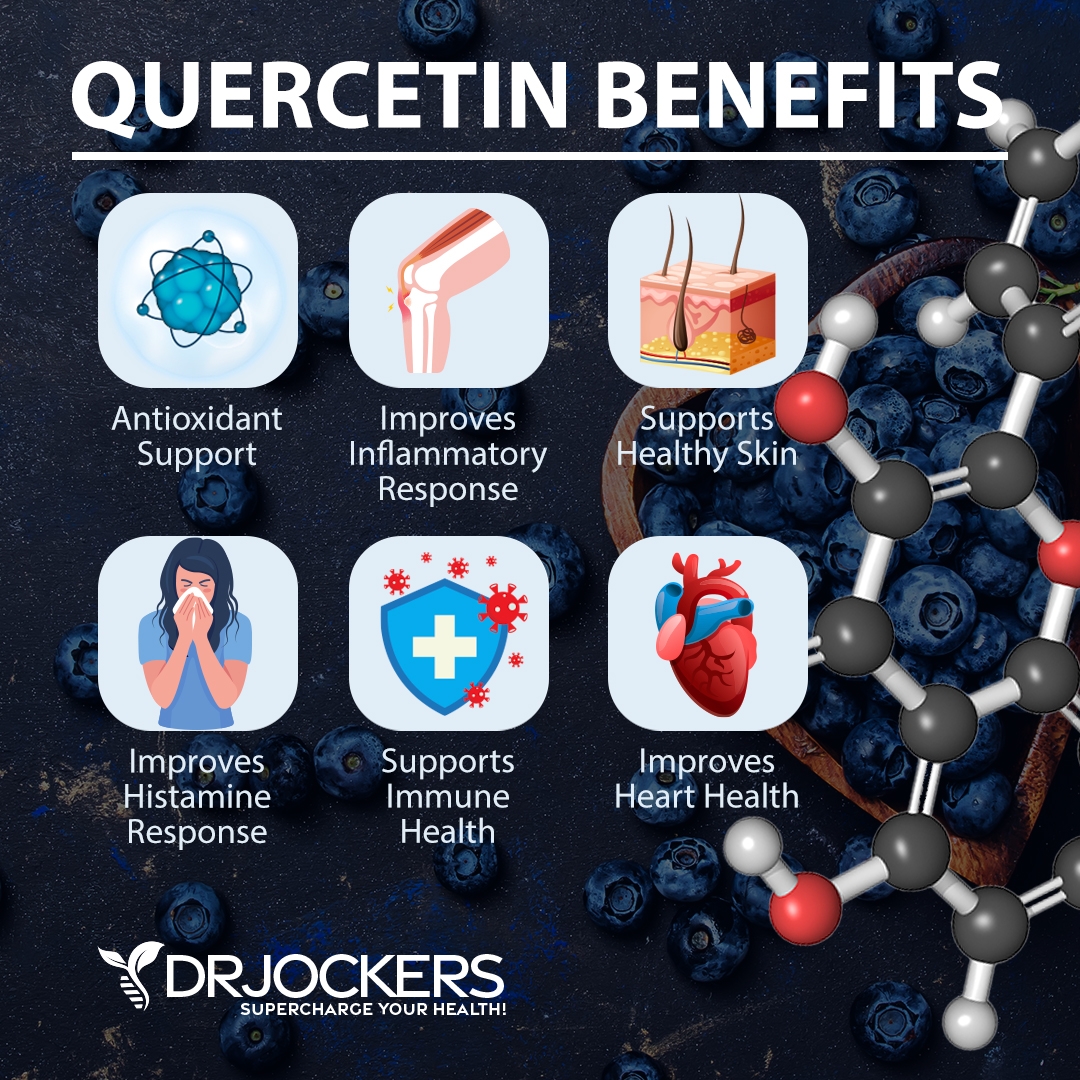
Quercetin
Quercetin is an antioxidant and flavanol found in many plants. According to a 2018 animal study published in PLoS One, quercetin may be beneficial for reducing the progression of COPD (42). I recommend daily supplementation with quercetin.
I recommend that you include plenty of quercetin-rich foods in your diet, including black currants, cherries, blueberries, black plums, cranberries, apples, grapes, sage, broccoli, olive oil, pepper, kale, romaine lettuce, red leaf lettuce, raw red onions, snap peas, cabbage, raw asparagus, sprouts, and herbs.
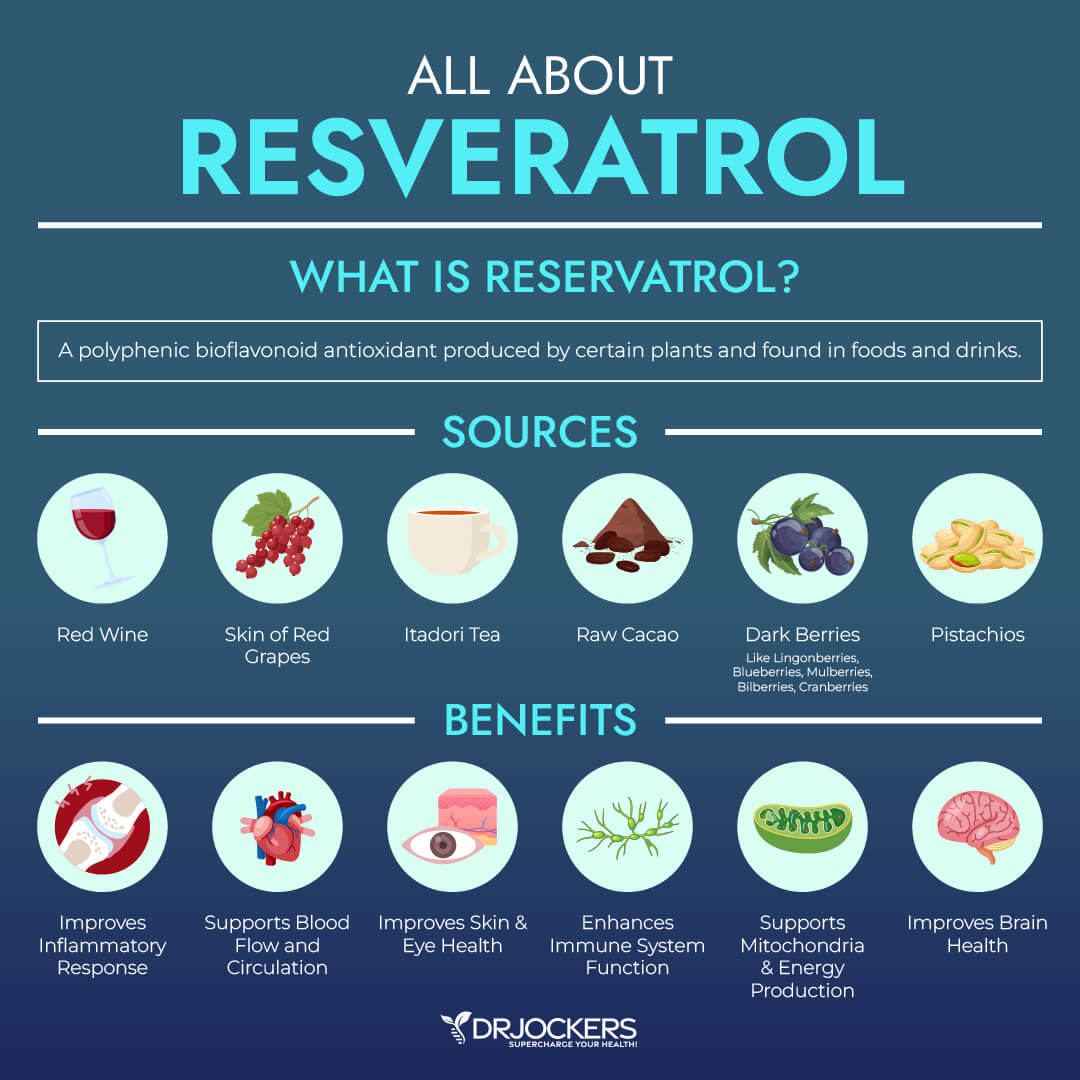
Resveratrol
Resveratrol is a powerful antioxidant found in the skin of grapes, berries, and red wine. It greatly complements the benefits of quercetin. According to a 2017 study published in Molecules, resveratrol may help to reduce inflammation and oxidative stress in COPD (43).
You may include more resveratrol-rich foods in your diet, including grapes, cranberries, blueberries, other berries, pistachios, and cacao. I recommend daily supplementation with resveratrol.
You may also find some supplements that include both quercetin and resveratrol and some supplements for inflammation defense with curcumin, resveratrol, and quercetin. Since these three antioxidants work well together, you may benefit from a supplement that includes all three.
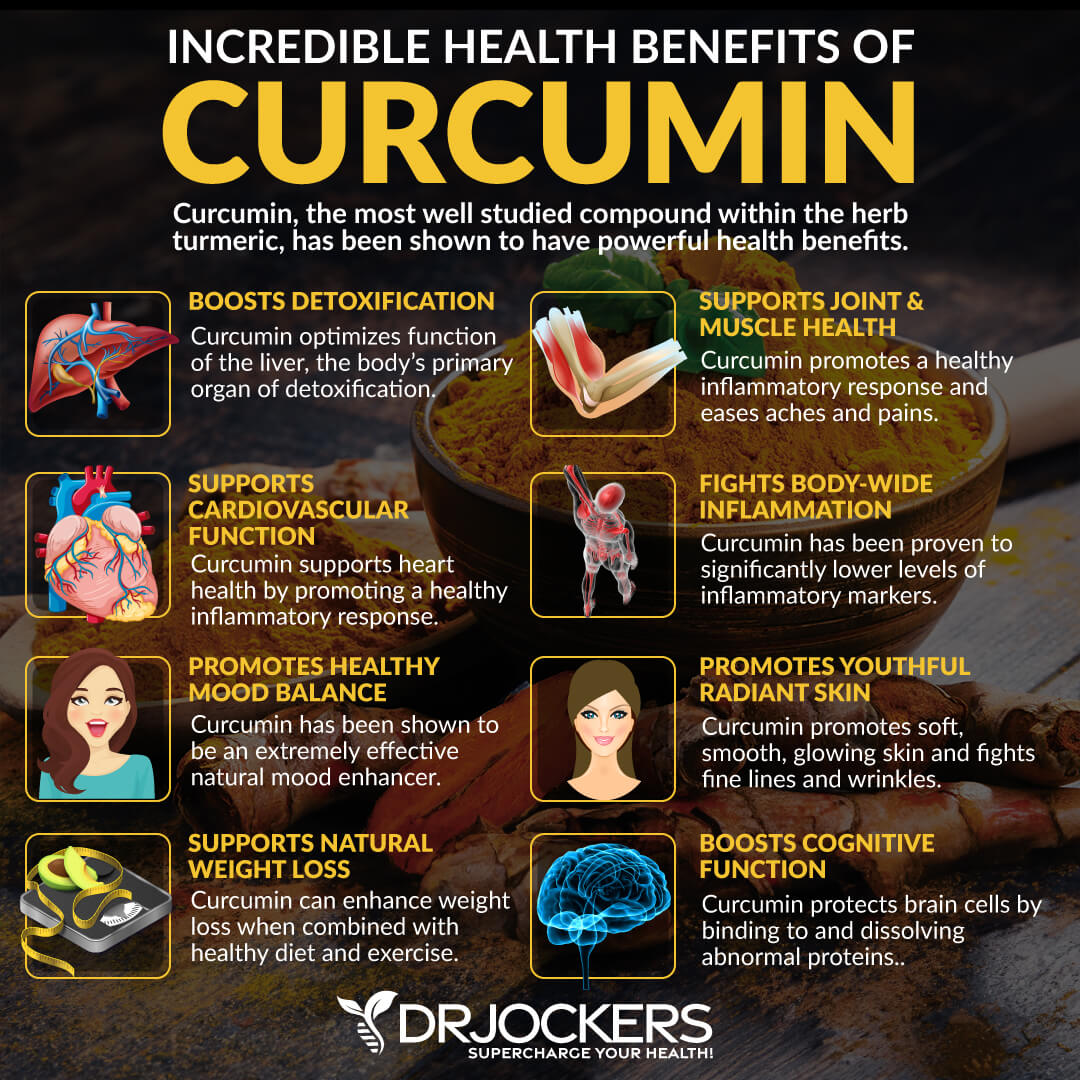
Curcumin
Curcumin is the active ingredient of the spice turmeric. It offers science-backed anti-inflammatory and pain-relieving benefits. According to a 2019 animal study published in the International Journal of Medical Research, curcumin may help to stimulate autophagy and cellular renewal in COPD (44).
You may add turmeric to your dishes, soups, salads, dressings, smoothies, and juices. I also recommend that you supplement with curcumin. Choose a high-quality curcumin/turmeric supplement. You may also find some great supplements for inflammation defense with curcumin, resveratrol, and quercetin in them, since these three antioxidants complement each other.
Final Thoughts
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes breathing difficult. As a progressive disease, symptoms usually worsen over time, making breathing, exercise, and daily tasks increasingly difficult; however, with the appropriate lifestyle and dietary strategies, you can reduce your risk and support your lung health. Follow my top natural support strategies for COPD to support your health and improve your well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.

Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




I feel truly blessed to have been cured of my COPD. It wasn’t an easy journey, but healing did happen. At one point, my condition was really critical, and I didn’t think I’d come out of it, until I found a helping hand. What symptoms are you experiencing? Do you think we might have had similar ones? I’d really like to hear your story.