Crohn’s Disease: Symptoms, Causes, and Natural Support Strategies
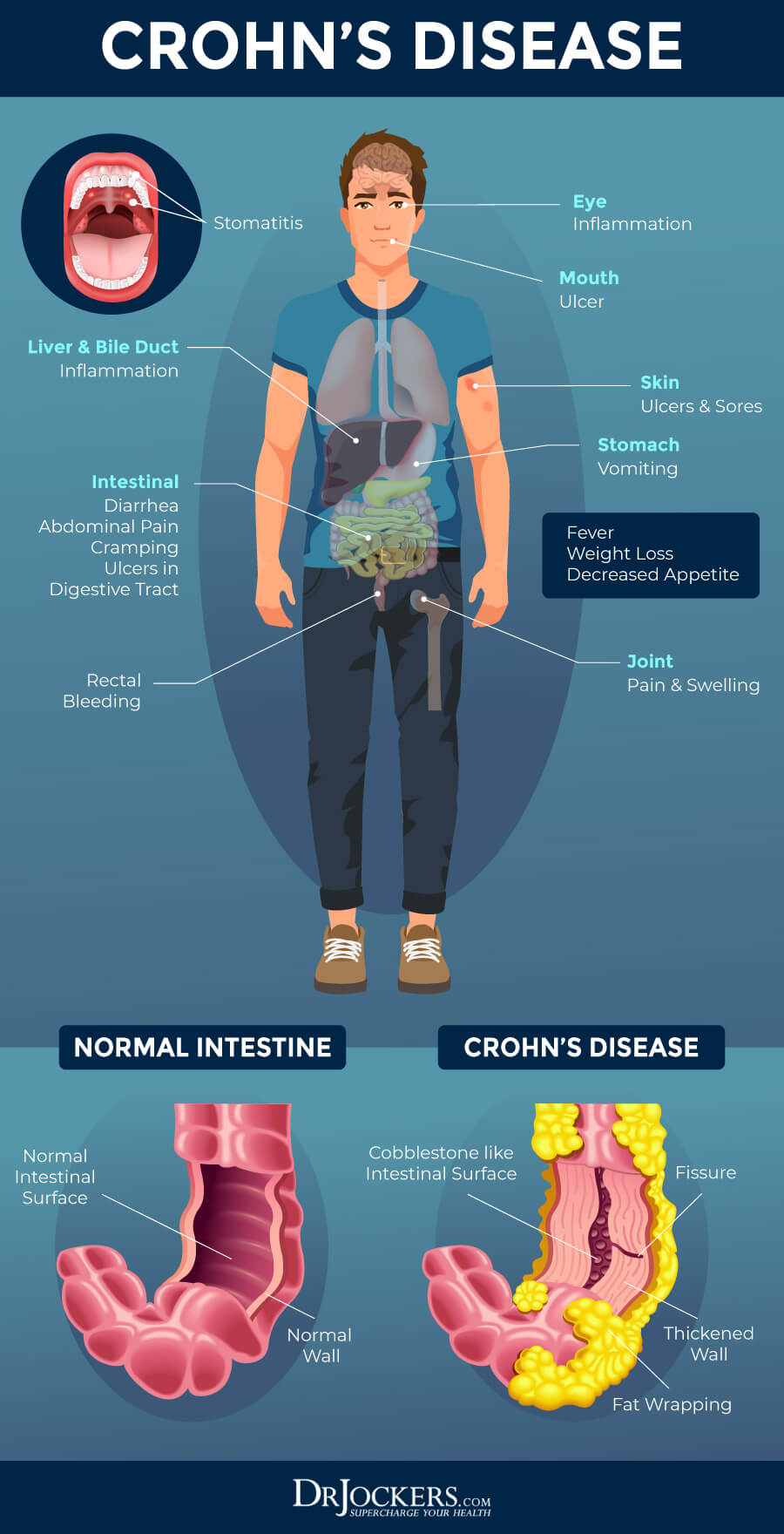
Crohn’s disease is an increasingly common inflammatory bowel disease. It can affect your small intestine and colon, but also other parts of your gastrointestinal tract. Symptoms of Crohn’s disease include diarrhea, abdominal cramping, fatigue, blood in the stool, weight loss, and more. While there is no cure for Crohn’s disease, there are some natural support strategies that can help to improve your gut health and symptoms.
In this article, you will learn what Crohn’s disease is. I will go over its symptoms and main causes. You will understand the potential risks and complications of Crohn’s disease. I will discuss my top digestive support strategies to improve your digestion and gut health.
You will learn more about testing for underlying issues related to Crohn’s disease and digestive health issues. I will discuss the benefits of working with a functional health coach if you have Crohn’s disease.

What Is Crohn’s Disease
Crohn’s disease is a form of inflammatory bowel disease (IBD). Another commonly known IBD is ulcerative colitis that you can learn more about in this article. Though Crohn’s disease tends to affect your small intestine and colon, it can also cause issues in any or all parts of your gastrointestinal (GI) tract from your mouth to your anus.
In some cases, Crohn’s disease can affect some parts of your GI tract, skip a section, then continue on in other parts.
It is an increasingly common condition that about 780,000 people deal with in the United Staes alone. Even though it affects so many people, Crohn’s disease is not fully understood and doesn’t have a known cure yet.
About 20 percent of people with Crohn’s disease also have at least one family member, a parent or a sibling, who also has the same disease. Symptoms can vary from mild to debilitating. Patients tend to experience periods of flares and remissions. Sometimes flares can lead to life-threatening complications (1).
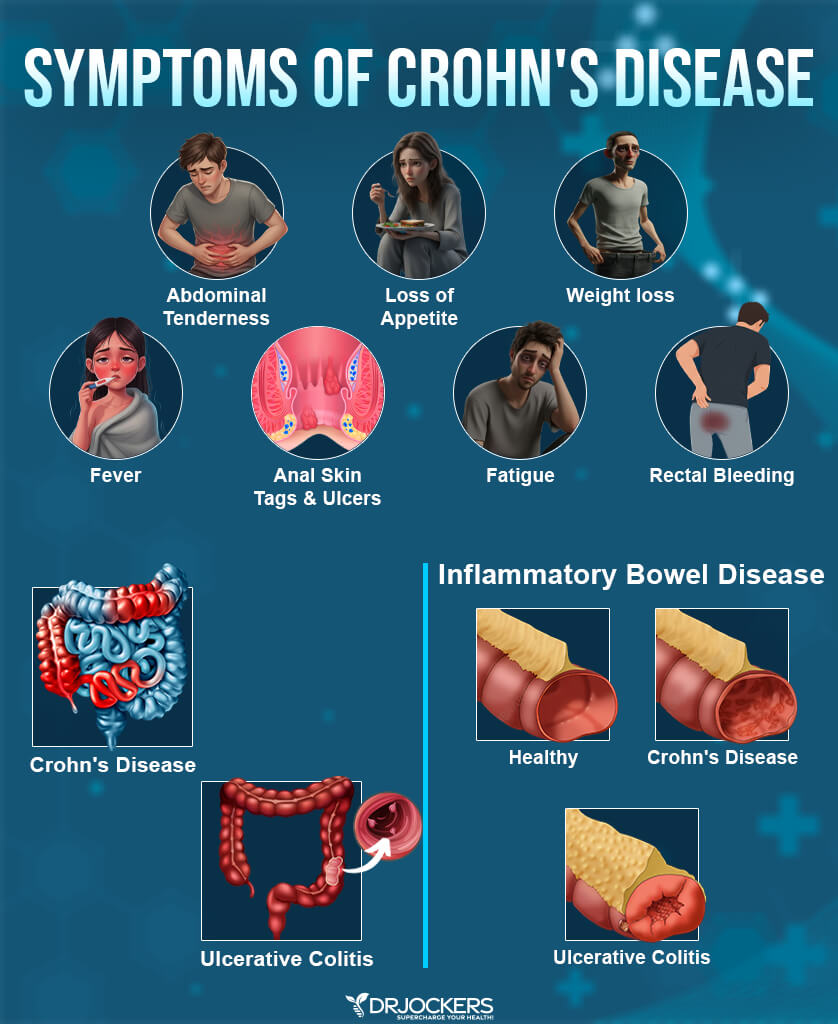
Symptoms of Crohn’s Disease
Symptoms of Crohn’s disease tend to develop gradually and may vary from person to person. Some people may mistake early symptoms with an upset stomach, food poisoning, or allergies, and it is important to visit a doctor if your symptoms persist for a diagnosis and to explore treatment options.
Early and common symptoms of Crohn’s disease may include:
- Diarrhea
- Abdominal cramps
- Frequent need for bowel movements
- Feeling like your bowels aren’t empty after a bowel movement
- Blood in stool
- Weight loss
- Loss of appetite
- Fatigue
- Fever
In more severe cases of Crohn’s disease symptoms can progress and new symptoms may occur. Symptoms of more severe cases of Crohn’s disease may include:
- Ulcers anywhere between your mouth and your anus
- Perianal fistula causing pain and drainage near your anus
- Inflammation of your joint or skin
- Anemia and related shortness of breath
Major Causes of Crohn’s Disease
While we don’t know the exact etiology of Crohn’s disease, researchers believe that it is driven by genetic susceptibility and other internal and external factors. People with Crohn’s often have a parent or sibling with the same disease. While you can develop Crohn’s disease at any age, in most cases first symptoms occur before age 30.
Crohn’s disease tends to occur more frequently in industrialized countries pointing at our modern-day lifestyle choices and toxic environment. Here are the major causes of Crohn’s disease, including internal and external factors that may increase your risk:
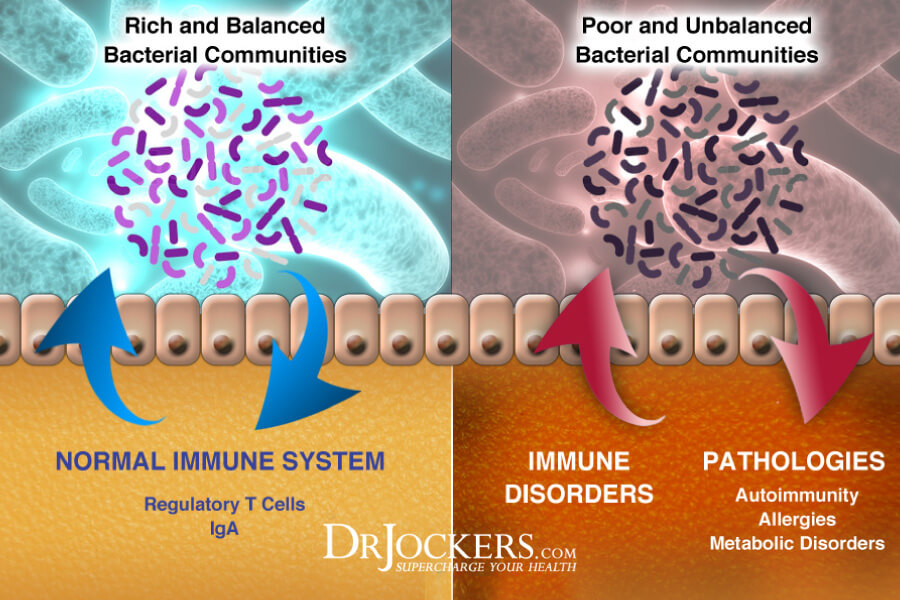
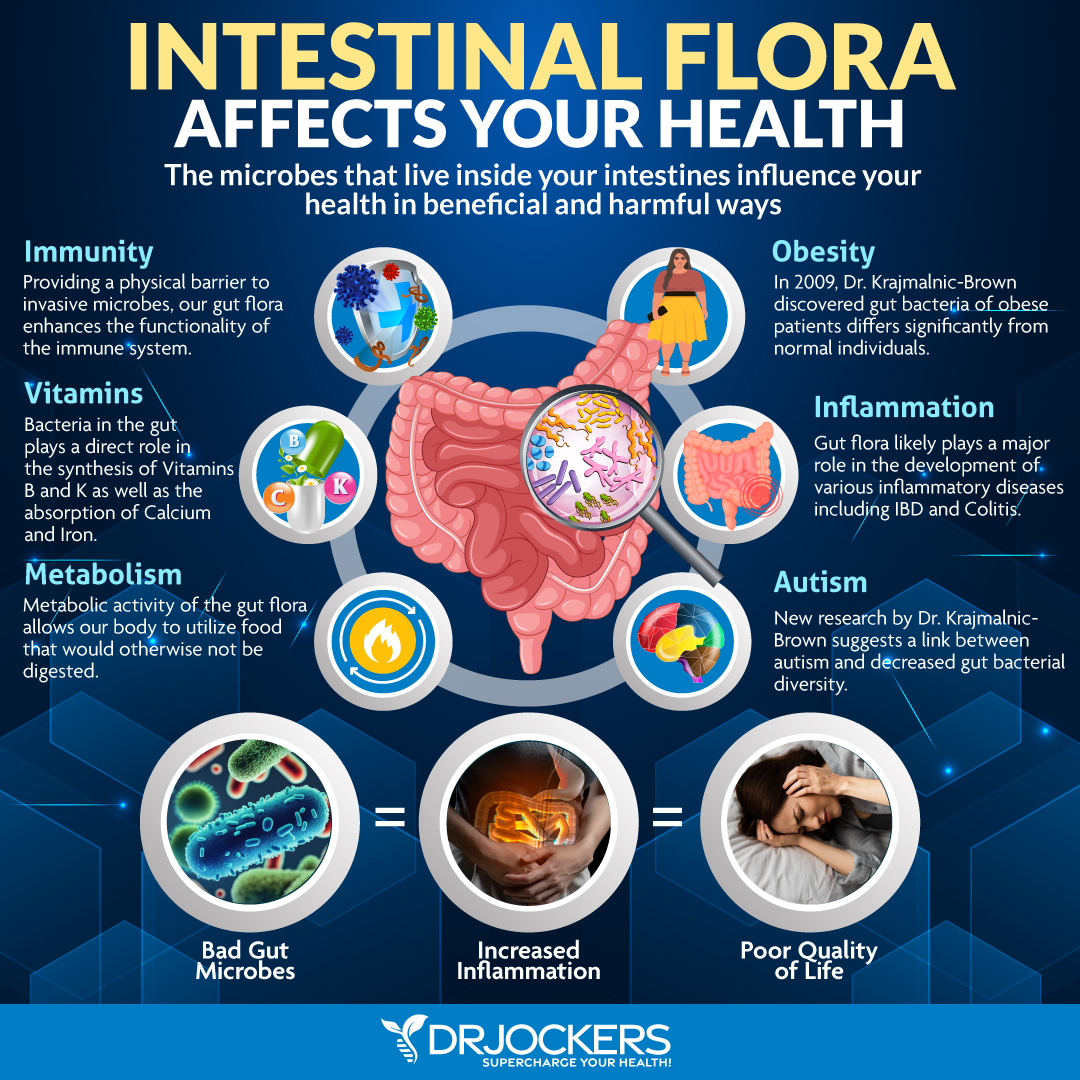
Imbalances in the Gut Microbiome
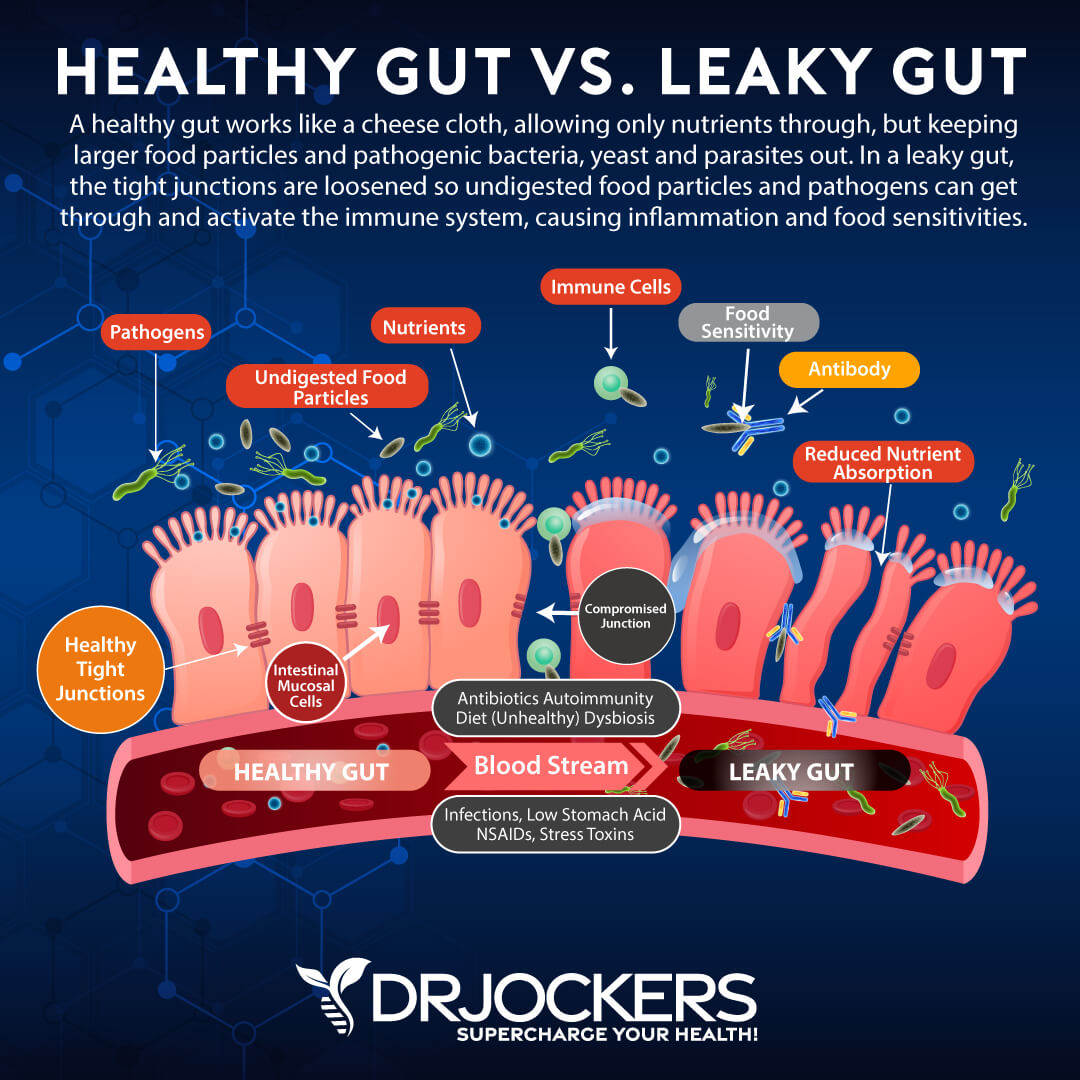
Your gut flora balance is absolutely critical for your digestive and overall health. Crohn’s disease involves a complex interaction between your gut, gut microbes, and immune system. According to a 2018 study, people with inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis have different and abnormal gut microbes (2).
There is a strong correlation between gut microbiome imbalances and irritable bowel diseases. People with these gut problems gave fewer bacteria with anti-inflammatory properties and more bacteria with inflammatory properties. They also have a higher concentration of sulfate-reducing bacteria resulting in high metabolic production of hydrogen sulfide. Hydrogen sulfide is toxic to your intestinal epithelial cells and can lead to mucosal inflammation increases your risk of Crohn’s disease (3).
Crohn`s disease appears to be associated with anti-yeast antibodies (4, 5, 6). Mannon is a component of the yeast organism`s cell wall. Individuals with Crohn`s tend to have lower levels of lectin binding proteins that bind mannan and help expel it from the body.
Due to the lowered lectin levels and the insufficient innate immune system, individuals with Crohn`s very often develop anti-yeast antibodies. This overproduction of anti-yeast antibodies triggers an inflammatory response that damages the gut lining.
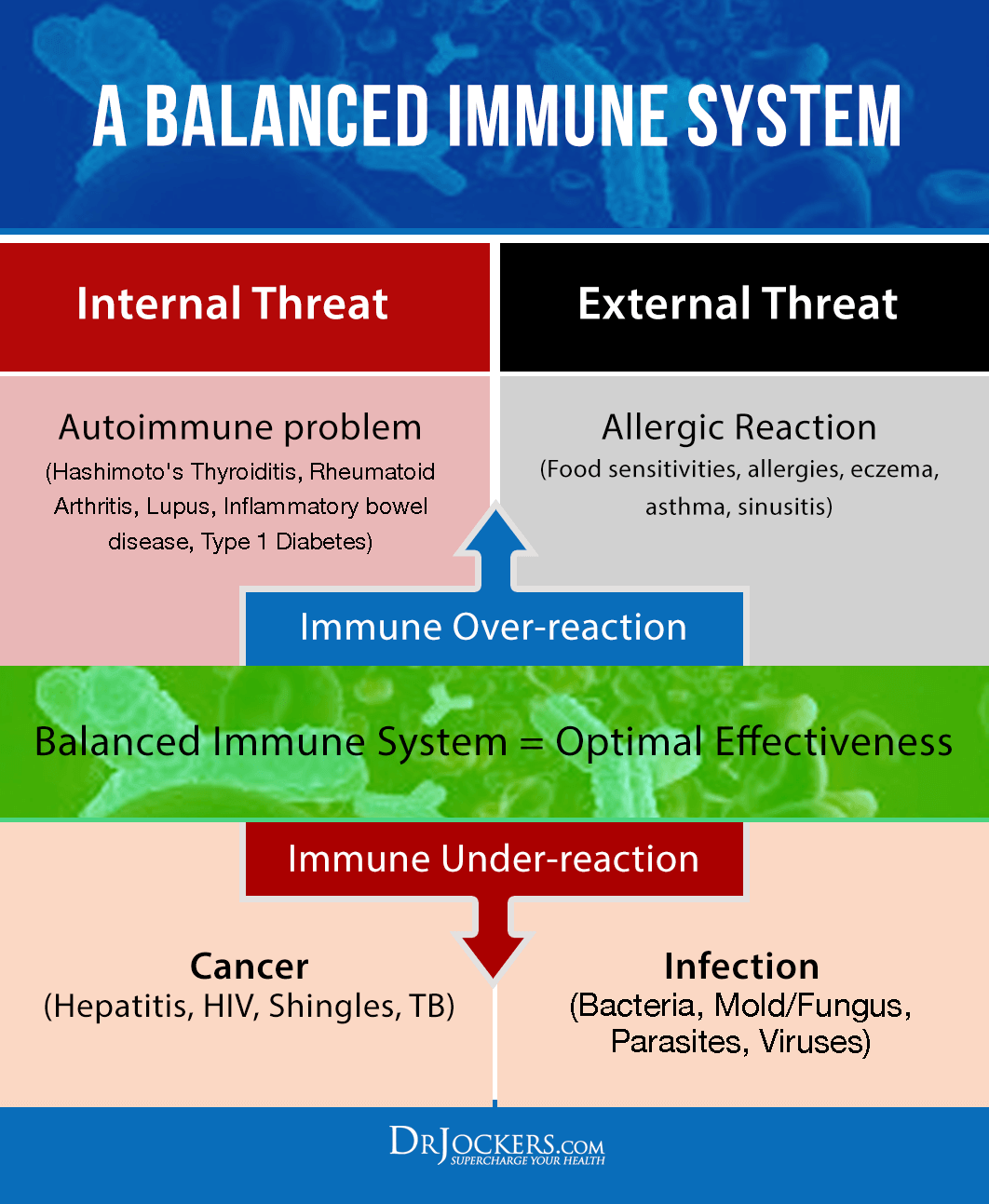
Overactive Immune System and Crohn’s Disease
The immune system is characterized by 2 major regions: Innate immunity and adaptive immunity. Innate immunity provides immediate defense against pathogens and is characterized by t-cell formation. Adaptive immunity is considered a `learned immunity` and is what provides long-lasting immune defense through antibody formation.
Researchers have shown that Crohn`s is an innate immune deficiency (7, 8, 9). Chronic inflammation with this disorder is caused by the adaptive immunity trying to compensate for the reduced function of the innate immune system.
One of your immune system’s roles is to protect your intestinal epithelial cells from dietary toxins and antigens. The problem that these very things can trigger and activate an immune response and increase inflammation. Crohn’s disease is an autoimmune or immune-mediated condition characterized by an overactive immune system and an abnormal immune reaction targeting your gut (10).
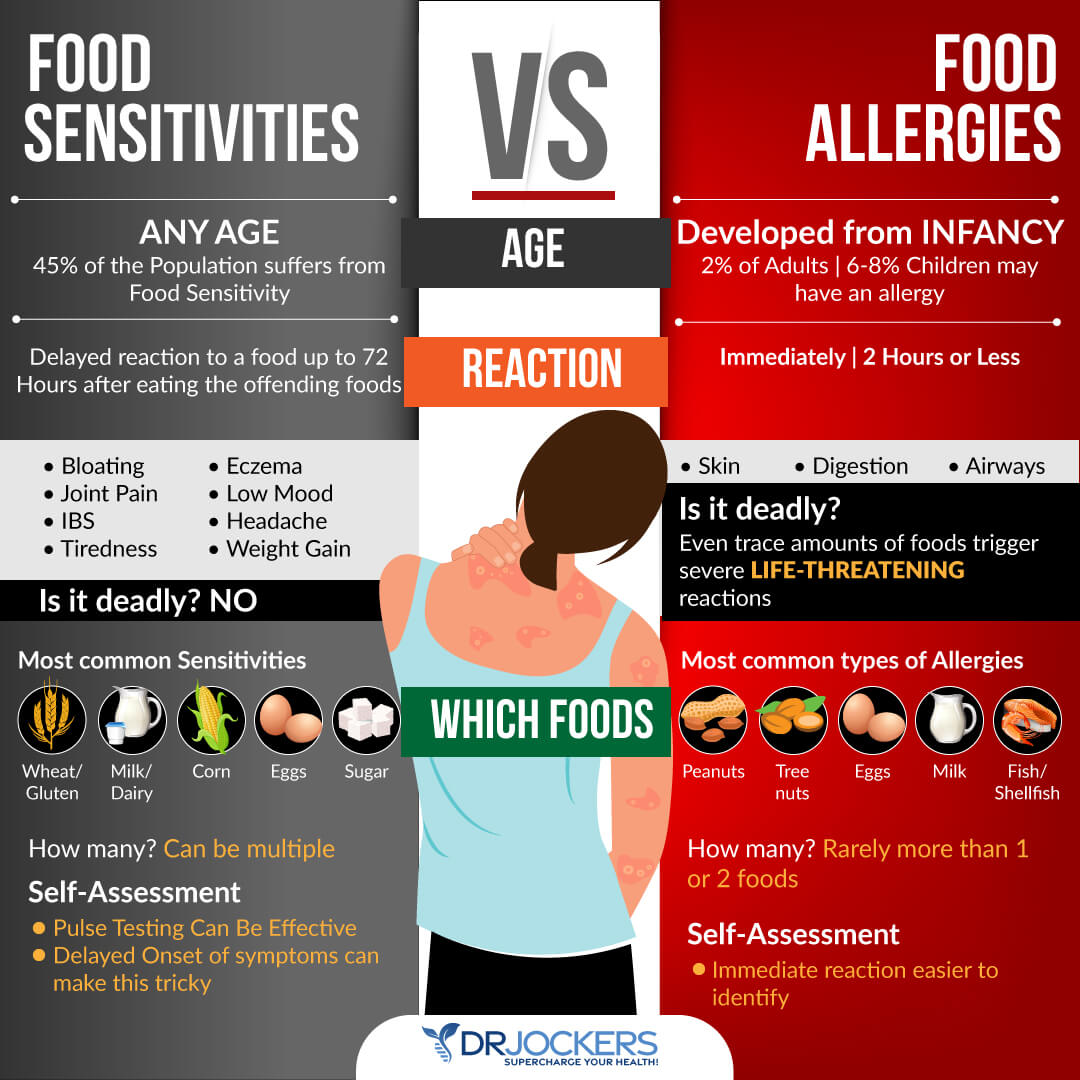
Inflammatory foods, foods that you are sensitive to, toxins, and pathogens can lead to this overactive immune response. Food sensitivities are often the main culprit.
Common food sensitivities that are associated with Crohn’s and other gut health issues include gluten, dairy, soy, corn, nuts, eggs, and nightshades; however, you may be sensitive to less common foods. Repeated exposure to foods that you are sensitive to can increase inflammation, the risk of leaky gut syndrome, and gut health issues. To learn more about food sensitivities and food sensitivity testing, I recommend reading this article.
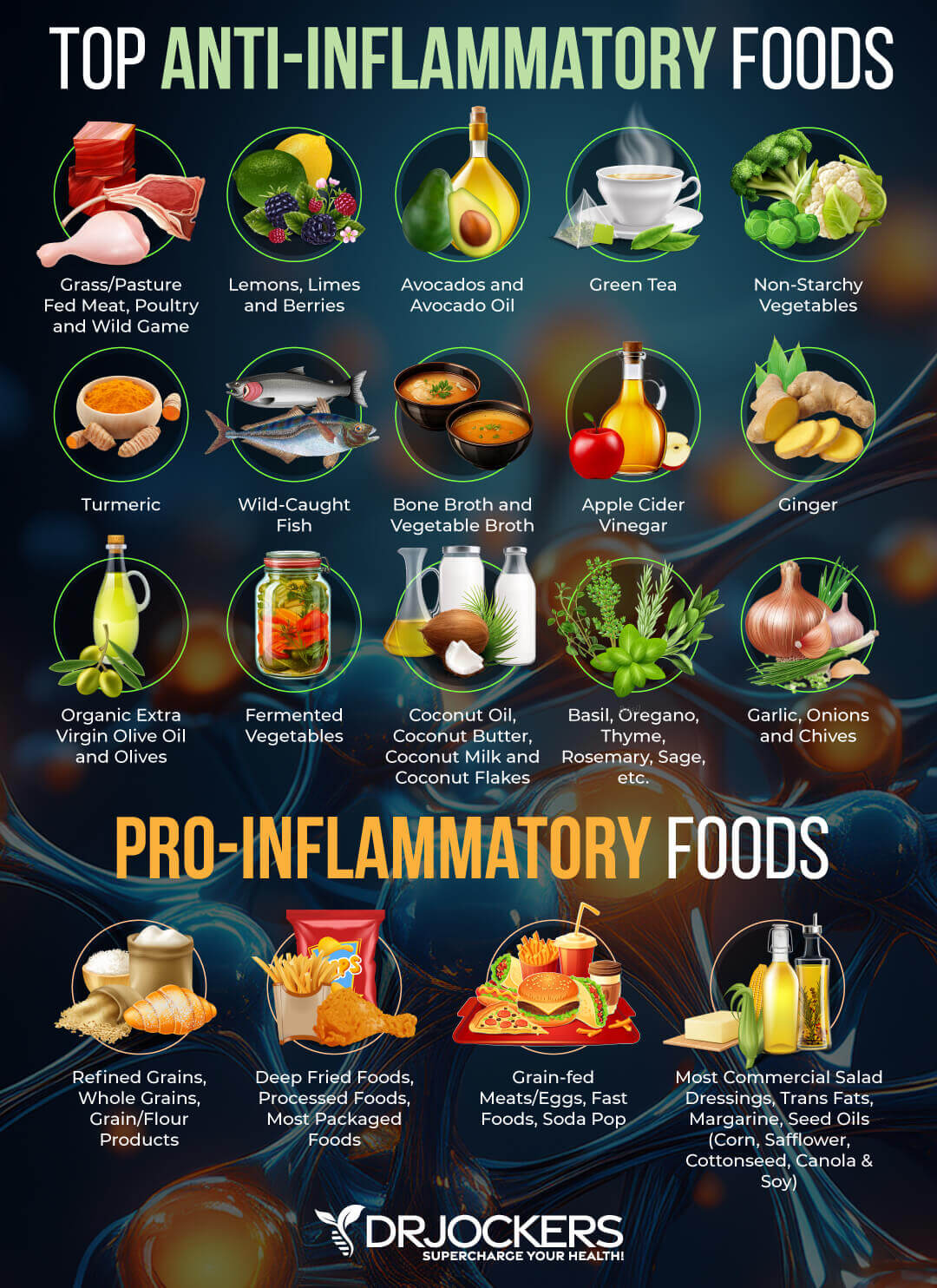
Poor Diet
Your diet plays a major role in your gut health. Eating an inflammatory diet high in processed foods, refined sugar, refined carbs, refined oil, artificial ingredients, factory-farmed meat, farmed fish, and deep-fried junk food can increase your risk of developing Crohn’s disease.
These foods increase the production of pro-inflammatory cytokines, reduce the production of anti-inflammatory cytokines, increase inflammation, and compromise your immune system (11).

Trigger Foods for Crohn’s Disease
There are certain foods that may trigger or worsen your symptoms of Crohn’s disease. Foods that may trigger your symptoms of Crohn’s disease include:
- Alcohol
- Caffeine
- Carbonated beverages
- Refined sugars
- Dairy products
- Raw vegetables
- Dried beans, peas, legumes
- Dried fruits and berries
- Fruits with pulp or seeds
- Sulfur or sulfate-containing foods
- High fiber foods
- Spicy foods (including hot sauces)
- Nuts and crunchy nut butter
- Seeds
- Popcorn
- Sorbitol (in many sugar-free gums and candies)

Chronic Stress
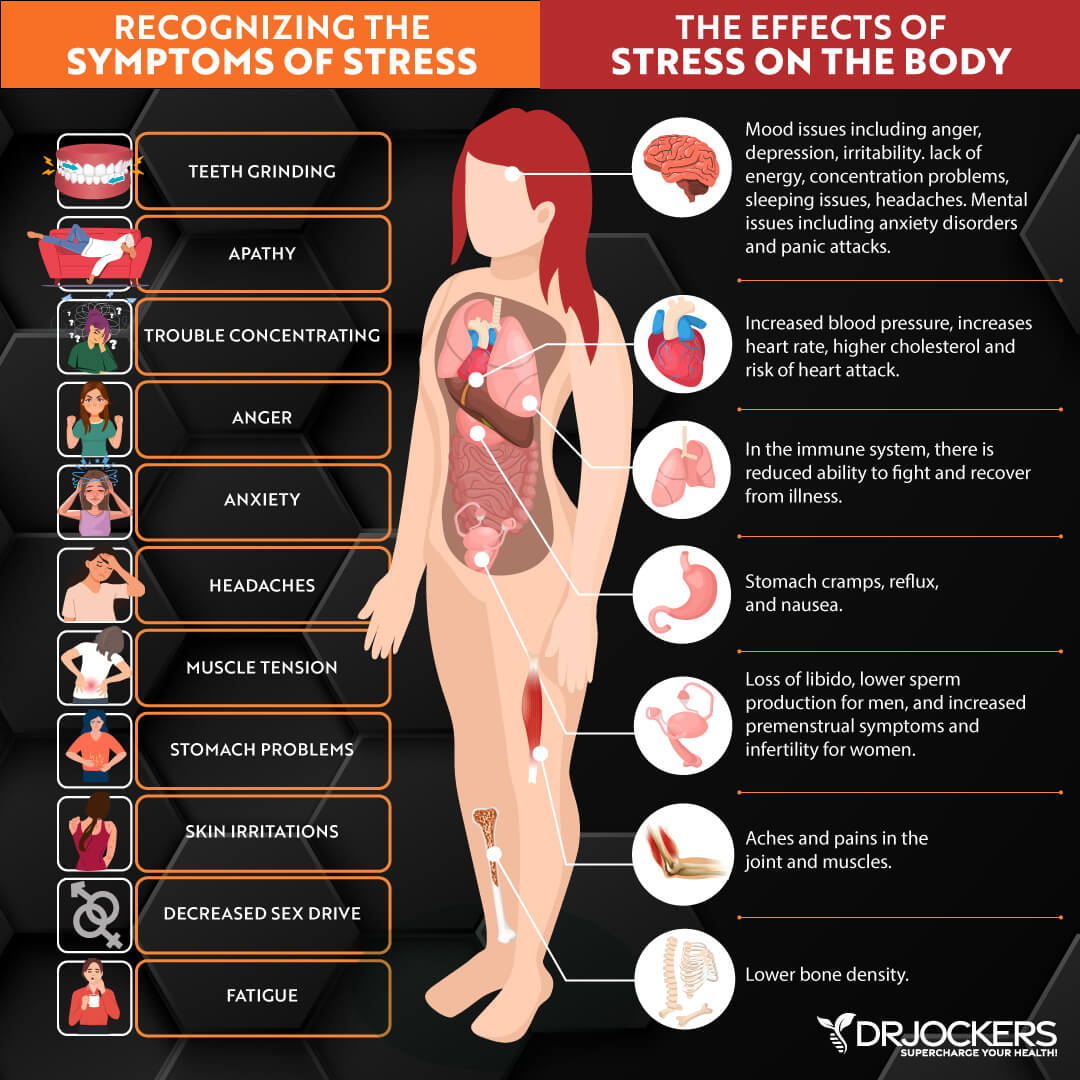
According to 2019 research, irritable bowel diseases, such as Crohn’s disease are associated with chronic stress. Both physiological and chronic stress can have a negative impact on your gut function and the close connection and interaction between your gut and brain.
Stress can increase and activate inflammatory pathways, decrease mucosal flow, and damage the mucosal barrier. Chronic psychological stress can also lead to poor sleep which can stimulate the production of pro-inflammatory cytokines increasing your risk of altered gut microbiota, leaky gut syndrome, and gut health issues (12).
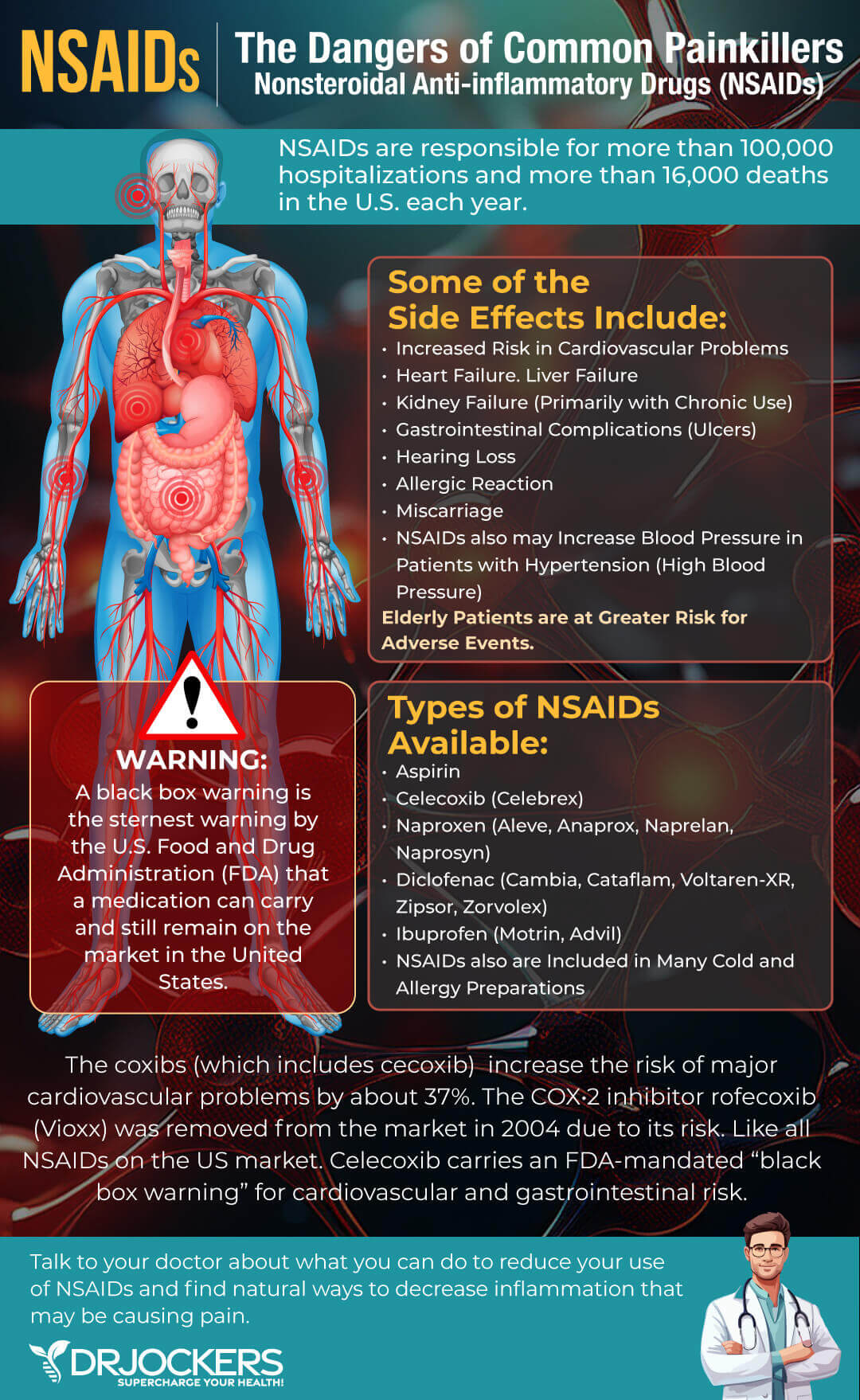
Certain Medication
Anti-inflammatory drugs, antibiotics, oral contraceptives, and non-steroidal anti-inflammatory drugs (NSAIDs) can increase your risk of Crohn’s disease. The problem is that some of these drugs are used for the conventional treatment of Crohn’s yet long-term may become problematic.
According to 2017 research, long-term exposure to antibiotics can negatively affect your gut microbiome and intestinal immune system and increase your risk of inflammatory bowel diseases (13).
Complications of Crohn’s Disease
There are serious risks and complications associated with Crohn’s disease especially when left untreated. Some complications that may occur:
- Bowel obstruction
- Fistulas
- Ulcers
- Anal fissure
- Malnutrition
- Colon cancer
- Other health problems
Medications used for Crohn’s disease also present a risk as they lower your immune system function and may increase your risk of cancer and infections. Corticosteroids are also associated with increased risk of glaucoma, cataracts, diabetes, high blood pressure, bone fractures, and osteoporosis.

Digestive Health Support Strategies
Conventional treatment strategies of Crohn’s disease involve dietary changes, anti-inflammatory medication, antibiotics, steroids, immunomodulators, and biologic therapies. In up to 75 percent of cases, people with Crohn’s disease also require surgery. The good news is that if you have Crohn’s disease you can employ some digestive health support strategies to support your body and digestion naturally.
Fortunately, alternative natural strategies, including dietary changes and targeted supplementation, may improve digestive health and improve the inflammatory response. While none of these strategies are FDA approved to prevent, mitigate, treat, or cure Crohn’s disease many people have benefited greatly from implementing them. Here is what I recommend to support your digestive health (14):
Anti-Inflammatory Nutrition Plan
Considering that Crohn’s disease is an inflammatory disease, following an anti-inflammatory nutrition plan is critical. Remove inflammatory foods, including refined sugar, refined carbs, refined oil, gluten, factory-farmed animal products, processed foods, junk foods, and food sensitivities.
Focus on organic greens, vegetables, herbs, spices, low glycemic index fruits, healthy fats, pasture-raised beef, grass-fed poultry and eggs, and wild-caught fish. To learn more about the anti-inflammatory nutrient plan I recommend, read this article.
Consider a Low-FODMAP Diet Trial
A low-FODMAP diet consists in the global restriction of all fermentable carbohydrates that is commonly used for the treatment of irritable bowel diseases, such as Crohn’s disease and ulcerative colitis. According to a 2020 randomized trial, a low-FODMAP diet may decrease inflammation and improve the microbiome of those with inflammatory bowel disease.
According to a 2018 meta-analysis and systemic review, a low-FODMAP diet may be beneficial for those with inflammatory bowel disease. I recommend that you consider a low-FODMAP diet trial for 2 to 6 weeks to see if your symptoms improve (15, 16). Read this article to learn more about a low-FODMAP diet and how to put it into action.

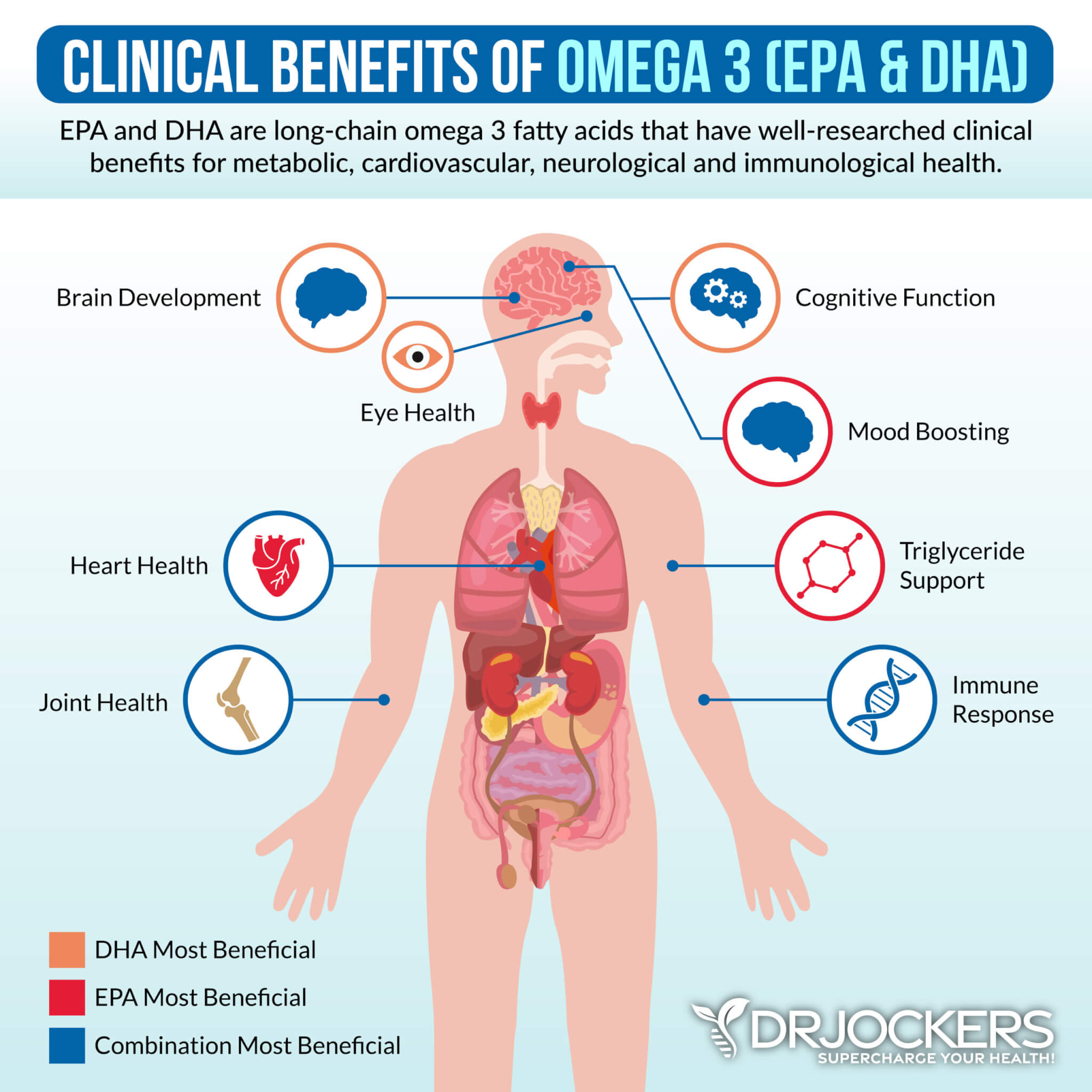
Omega-3 Fatty Acids
2019 research has shown that omega-3 fatty acids in fish oil may benefit irritable bowel diseases. Omega-3 fatty acids have anti-inflammatory properties. They may help to lower inflammation and aid remission.
Omega-3 fatty acids are found in fatty fish, such as salmon and sardines, nuts, especially walnuts, seeds, such as flax, hemp, chia, and pumpkin seeds, grass-fed meats, and pasture-raised eggs. Since meeting your needs alone with food can be difficult, especially if you are already dealing with inflammation and gut health issues, omega-3 supplementation with high-quality fish oil is important (17).
Identify and Remove Food Triggers
Crohn’s disease may be triggered by a variety of foods. It is important that you identify and remove your food sensitivities and food triggers.
Since triggering food sensitivities often lead to delayed symptoms up to 72 hours after eating, discovering them can be tricky. Follow my tips on testing for and identifying food sensitivities explained in this article.
Support the Gut Mucosa
Crohn’s disease involves the inflammation of your gut mucosal layer, therefore your recovery has to involve reducing this inflammation and supporting your gut health through nutrition, fasting, and targeted supplementation. I recommend consuming liquid nutrition to stimulate your digestion and improve absorption.
I also recommend combining this with fasting strategies to improve recovery. Drinking bone broth collagen is a great way to help to seal the holes on your damaged gut lining and support your intestinal wall’s health and function.
Key Supplements for Gut Mucosa
For mucosal support, I also like herbs and nutrients like aloe vera, licorice root, vitamin C, colostrum and dairy-free, bovine serum-derived (BSD) immunoglobulin concentrate. These all act to support gut barrier function, improve immunity, and decrease inflammation in the gut.
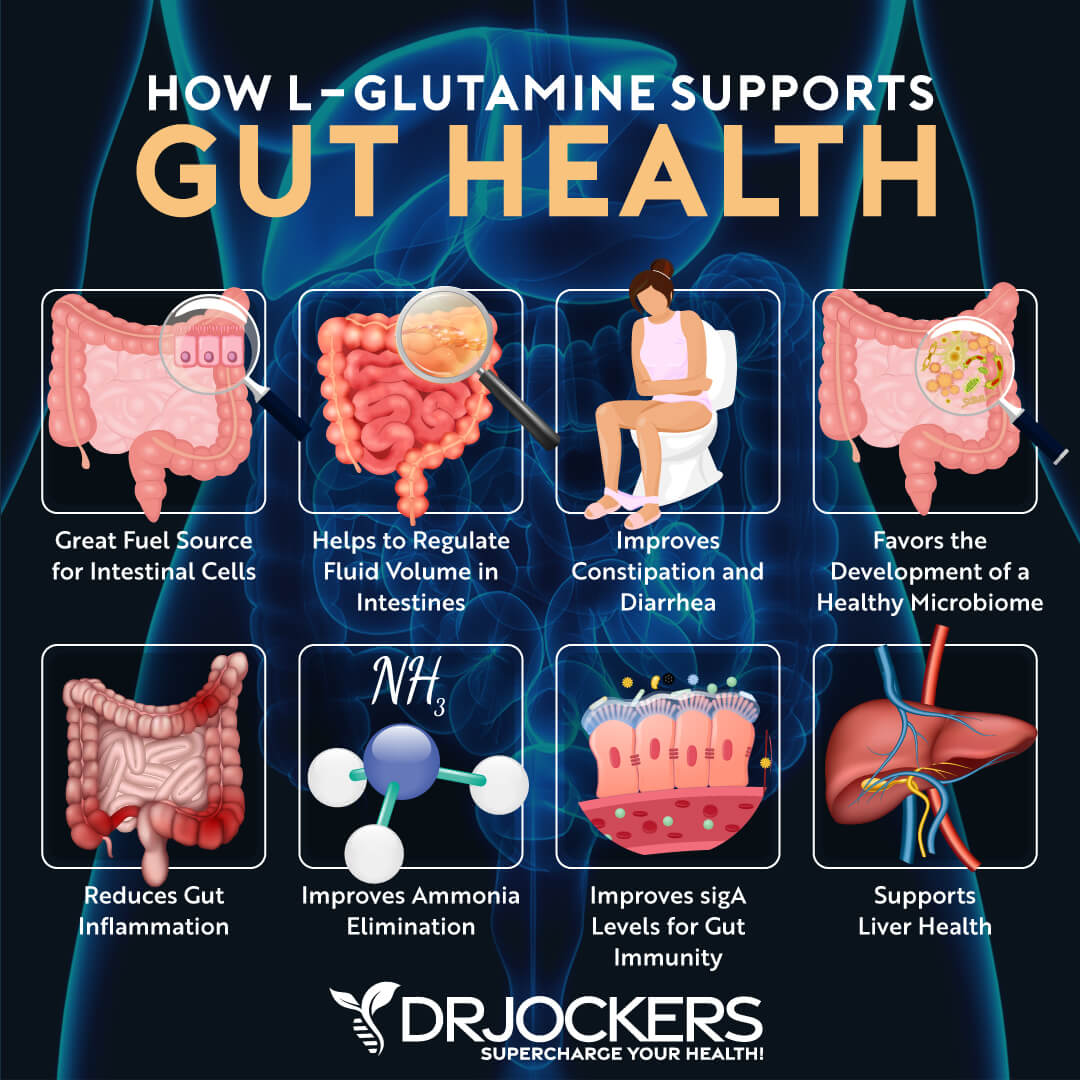
The immunoglobulins in colostrum and BSED immunoglobulin concentrate work to bind to environmental toxins, neutralizes pathogens, and improve gut mucosal immunoglobulin sIgA levels. Using L-glutamine supplements can help to repair leaky gut and soothes and protects the gut mucosa as this is the primary amino acid that strengthens the intestinal lining.
Balance the Gut Microbiome
Improving the microbial balance in your gut is very important to heal from Crohn’s disease. Probiotics play a very important role in the management of this condition. Probiotics are beneficial microorganisms (bacteria and yeasts) that are similar to the microorganisms that naturally live in our bodies.
Probiotics work through different mechanisms to support gut health and downregulate the effects of bacteria in initiating and sustaining an intestinal inflammatory response. To learn more about different forms of probiotic supplements, I recommend reading this article.
Reduce Stress and Improve Sleep
Reducing stress and improving sleep is critical for improving your gut health and reducing inflammation in your gut. I recommend practicing meditation, grounding, breathwork, dry brushing, journaling, yoga, and prayer.
Sunlight exposure, regular exercise, and dry brushing are also great ideas. Avoid electronics, food, and stress close to bedtime. Develop an evening routine that relaxes your body and calms your mind. Make sure that you get 7 to 9 hours of quality sleep each night.

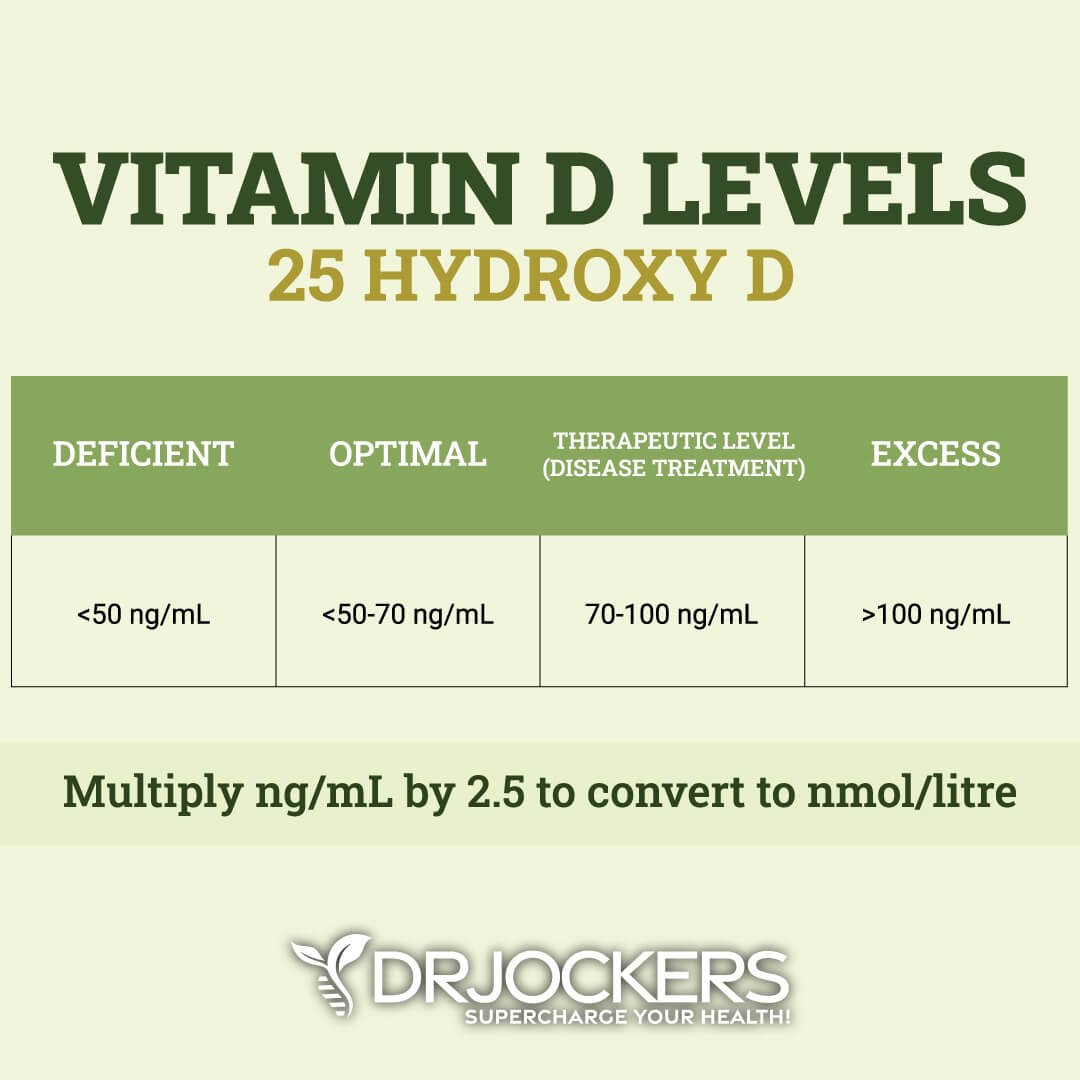
Optimize Vitamin D Levels
Vitamin D is critical for immune regulation. It is an immunomodulator. Research has linked vitamin D deficiencies to immune-mediated disorders, such as chronic infections and autoimmune diseases, as well as inflammatory bowel disease.
Spending time on the sun is important for optimizing your vitamin D levels. However, due to our indoor lifestyle, gloomy days, and darker months, it is impossible to meet your needs through the sun alone. This is why I recommend supplementing with high-quality vitamin D3 together with vitamin K2, which helps absorption (18, 19).
The ideal range for vitamin D3 levels is between 50-80 ng/ml. To maintain optimal levels, you can use a high-quality supplement and take around 1,000 IU’s per 25lbs of body weight. I recommend finding a D3 that also has vitamin K2 in it as well and get your vitamin D3 (25-OH) tested once or twice a year to make sure you know your levels.
Testing for Underlying Causes of Crohn’s Disease
There are certain tests that I recommend to look for underlying causes of Crohn’s disease and other gut health issues to help your recovery. Here is what I recommend:
GI Map Stool Analysis
I recommend the GI-Map Stool Analysis test. It is an FDA-approved DNA test for gastrointestinal microbes and pathogens that also included calprotectin, a reliable marker for mucosal inflammation in Crohn’s disease. It measures your gut microbiome, and able to detect candida, fungi, and bacterial overgrowth, viruses, and parasites that may lead to Crohn’s disease and other gut health and inflammatory issues (20).
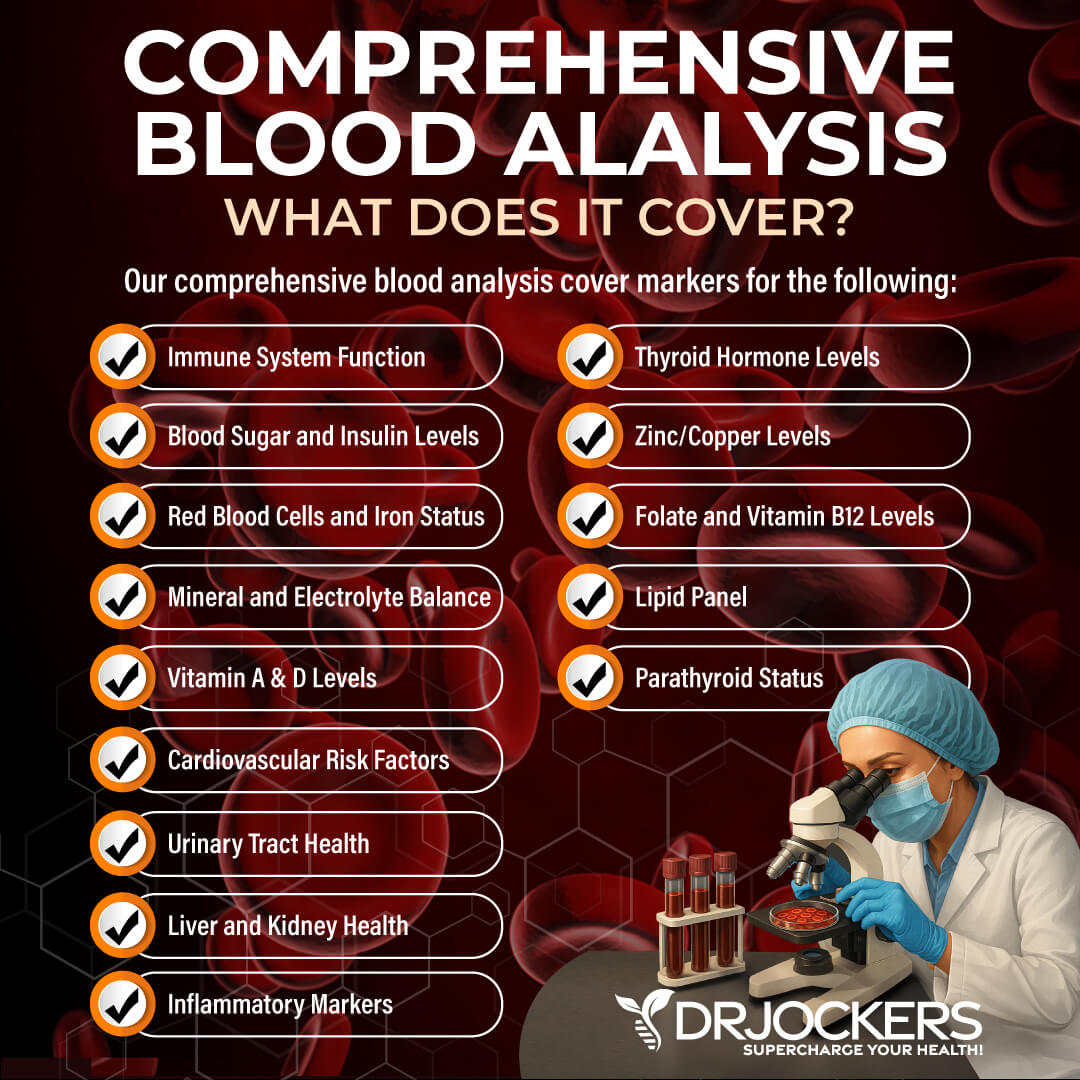
Comprehensive Blood Analysis
A blood test may help diagnose Crohn’s disease. Indications of Crohn’s include anemia, inflammation, and low albumin or protein. These tests are included in the Comprehensive Blood Analysis.
The C-Reactive Protein (CRP) test is a blood test used to assess levels of inflammation in the body. CRP is a protein produced in the liver. It is an acute phase reactant, which means it increases or decreases in concentration with inflammation or trauma.
CRP is useful in diagnosing and monitoring chronic inflammatory conditions such as ulcerative colitis. Other tests that measure or indicate inflammation are the Red Blood Cell Width (RBCW), ferritin, and erythrocyte sedimentation rate (ESR).
The Comprehensive Blood Analysis also measures vitamin D, zinc, and iron. Suboptimal levels of these micronutrients are associated with an increased risk of inflammatory bowel diseases. In fact, low vitamin D status is a biomarker for disease activity and a predictor of poor clinical outcomes in IBD patients (21).
Consider Working with a Functional Health Coach
Crohn’s disease is an inflammatory bowel disease that affects 780,000 people in our country. It comes with uncomfortable symptoms and serious complications. The good news is that you can support your gut with some digestive support strategies naturally. Follow my tips to improve your gut health, repair your body, and regain your vitality.
The functional nutrition and functional medicine approach look at the body as a summation of systems rather than overly specific mechanisms. A functional health coach is able to offer a truly holistic approach and support for your health. They can help to run and analyze specific labs.
They can also guide you with an anti-inflammatory autoimmune dietary plan, suggest beneficial supplements, and coach you along the way serving as your guide, support, and personal cheerleader that empowers you to create the healthiest version of yourself.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



I would like to talk to Dr.Jockers about doing a mutually beneficially television infomercial. If he can contact me, Clarence Martin, at 678-266-8778 I would love to discuss some options.
MAP can’t possibly cause Crohn’s disesae. Here’s why.1) Long-term anti-mycobacterial protocols have failed to produce a cure for anyone with CD. A few people have been put into remission for a year or so, but that’s hardly news. Myoconda (an antibiotic protocol consisting of three anti-mycobacterial drugs) has been a complete failure. Surely we would have seen some modicum of success in more than an anecdotal number of cases if anti-mycobacterial drugs were going to work.2) The absolute contraindication for use of TNF-alpha drugs is tuberculosis. Other contraindications include infection. If Crohn’s were caused by MAP, people would get worse when they were given TNF drugs, not better. Moreover, there is (to the best of my knowledge) not a single case of an individual who has died of fulminant MAP infection as a result of being given TNF drugs. (For that matter, if the pro-MAP crowd could give me a single case of MAP being attributed as the cause of death in a Crohn’s patient, I would be very interested.)It is unfortunate that MAP continues to distract researchers. It should have been disproven long ago. I have no doubt that MAP persists in the gut of a sizable proportion of Crohnies, probably because the damage that has been done to the gut provides a suitable environment for the organism. But the meta-studies have shown repeatedly the correlation between MAP and Crohn’s isn’t a very good one- certainly far from absolute.
in 2012 I was diagnosed with crohn’s disease. I had gotten in a car wreck and cracked one of my teeth. I went to the dentist and he fixed it but ended up in the hospital losing weight like crazy. P.Taking Remicade and steroids thank God came out of it. I felt like I had toxins in my body and found the doctor to run a nutrient and toxic element test. Well my suspicions were true and I was full of mercury aluminum and cadmium. I have had over 8 caps put on my teeth and my dentist just left the mercury in and put Miracle mix over the top. I have four teeth exposed to with Mercury in them and leak between 2 and 20 micrograms a day. I got off the Remicade and went on a ketogenic diet and my health improve dramatically. I ended up cracking another tooth and had a very close to a biological dentist fix it but still I ended up in the hospital. I just want people to know that almost every person that I know that has either Crohn’s disease or ulcerative colitis has a mouth full of mercury. The Mercury leaks out and gases and you swallow your saliva goes down and creates dysbiosis in your gut is inflamed your whole digestive tract. Please check to see if you have mercury toxicity for Crohn’s . If you do have amalgam fillings make sure you go to a certified biological dentist to use as a rubber Dam in your mouth and all the proper procedures to keep Mercury out of your body. God bless.
Wow that’s interesting I just had my new dentist take out all my silver fillings and the ended up in the hospital for colitis none infectious. Inflammation pattern on the CT suggests chron’s.