 High Fasting Blood Sugar on Keto?
High Fasting Blood Sugar on Keto?
The more I coach people through a ketogenic lifestyle, the more I become familiar with small nuances that can affect different people’s experiences. For example, there are a number of people who experience high fasting blood sugar upon waking in the morning. These individuals would express that they were following a ketogenic diet and were in a fasted state so it doesn’t make sense to have elevated blood sugar.
What you are going to find out in this article is that this effect may actually be much more normal than you think. In fact, it may not even be an issue. That being said, for some people, it may actually be a sign of something undesirable going on with their metabolism. This article will help you troubleshoot what is likely to be causing your high fasting blood sugar.
Pathologic Insulin Resistance
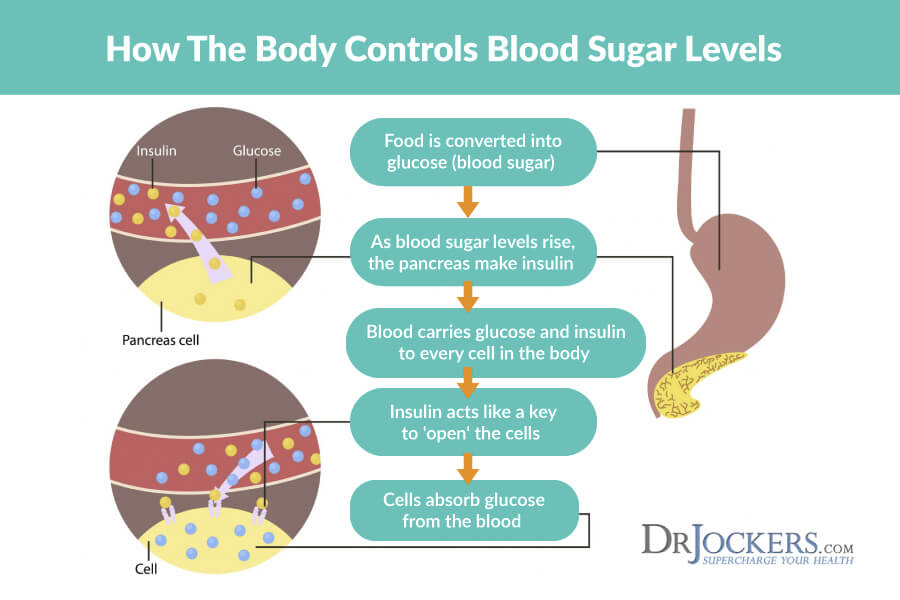
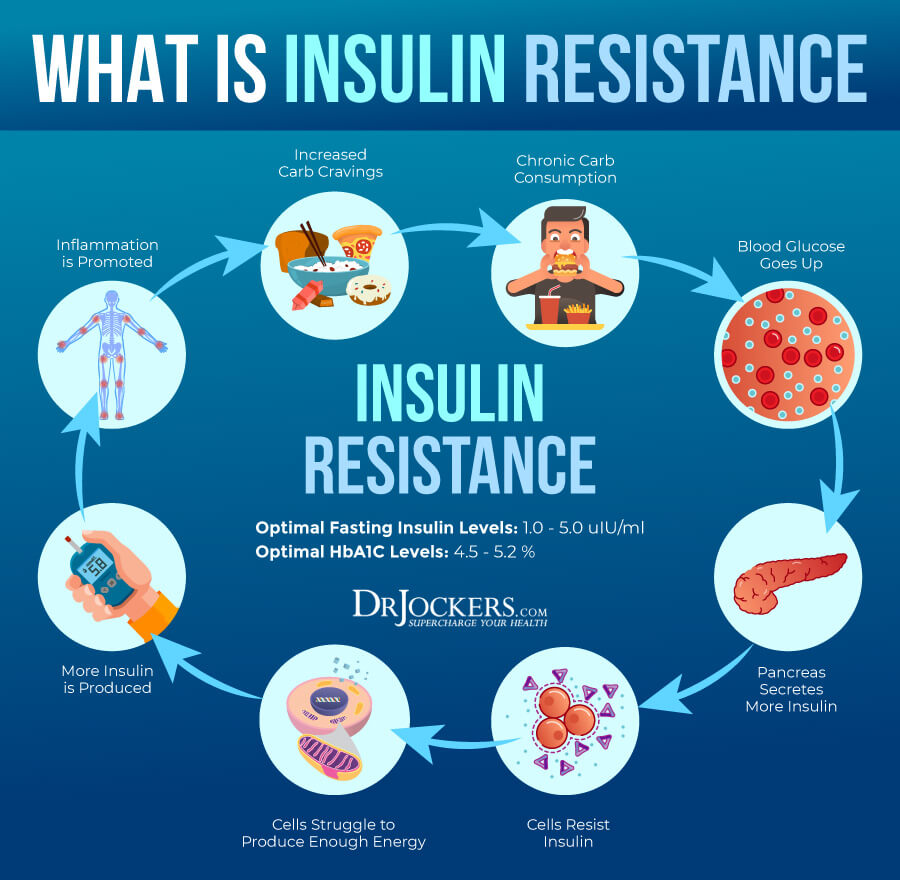
When someone has elevated fasting blood sugar and is NOT following a ketogenic lifestyle, it is likely that they are suffering from insulin resistance. Insulin resistance is characteristic of pre-diabetes and diabetes, as well as metabolic syndrome. This is when your cells stop listening to insulin’s signals to let glucose into the cell and instead allow glucose to continue circulating in the blood.
This is often due to a high sugar diet that constantly bombards insulin receptors to the point where they become desensitized. Think “Little Boy Who Cried Wolf”, but with your cells. This is called pathologic insulin resistance as it is considered a disorder and increases your risk of many different diseases.
Dawn Phenomenon and Somogyi Effect
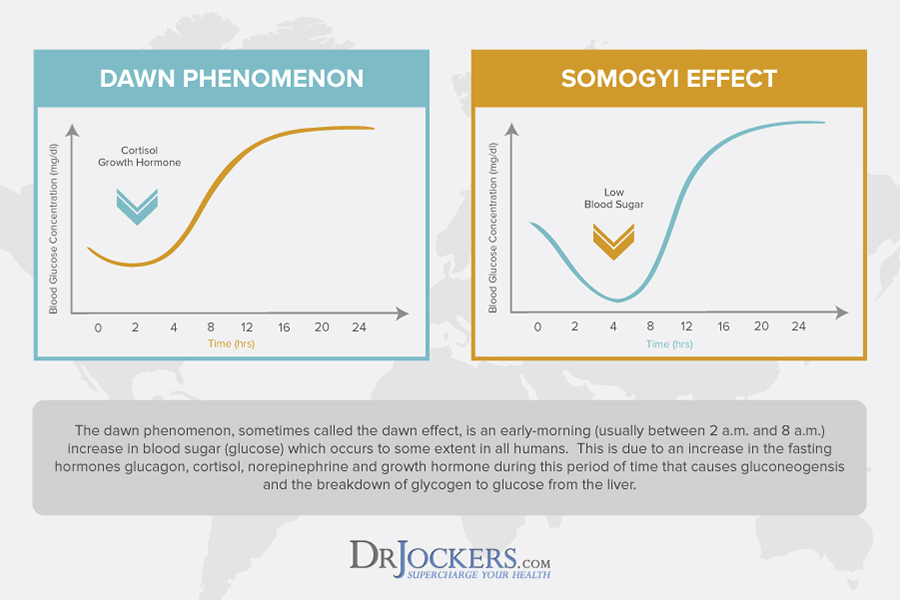
In diabetics, there are 2 common ways that high fasting morning blood sugar arises. The first reason is the “Dawn Phenomenon” and this impacts individuals who are following a ketogenic lifestyle as well. Overnight as we sleep between the hours of 2-8 AM a slurry of hormones including cortisol, growth hormone, adrenaline, and glucagon all begin to rise.
These hormones cause a gluconeogenesis effect where the liver and muscles break down their stored sugar (glycogen) to increase circulating blood sugar. This helps us have energy and mental arousal in the morning. This is a normal physiological response and it is normal for keto dieters to have slightly higher fasting blood sugar…although it shouldn’t be too high and you can mitigate this with the strategies discussed further on in this article.
Diabetics who are also taking exogenous insulin can also have something called the somogyi effect where they shoot too much insulin before bed and have a blood sugar crash, followed by a huge increase in stress hormones that dramatically increases blood sugar through gluconeogenesis. This is obviously not an issue unless you are a type I or type II diabetic taking prescription insulin.
Adaptive Glucose Refusal
When someone is following a ketogenic lifestyle and is in a fasted state, it is typical that blood sugar levels will be relatively low and stable. However, in some individuals, it is possible to have temporary elevations in fasting blood sugar. More often than not, this occurs in the morning when the individual is in a fasted state.
When you are sleeping your body is very active cleaning out the brain and rebalancing hormones. Sometime in the morning between 4-8 AM, the body releases cortisol, epinephrine, growth hormone, and glucagon. These hormones all have the effect of increasing blood sugar to wake you up. These hormones may also be released in response to a significant drop in blood sugar during sleep (1).
The difference in those who are following a ketogenic lifestyle is that if they are well keto-adapted, then their cells may refuse to burn that sugar for energy. This will naturally make fasting blood sugar levels seem elevated.
Instead of sugar not being able to get into the cells due to insulin resistance, the cells are simply refusing to burn sugar because they would prefer the ketones already being used. In this case, elevated fasting blood sugar is less of a concern.
Where Does This Blood Sugar Come From?
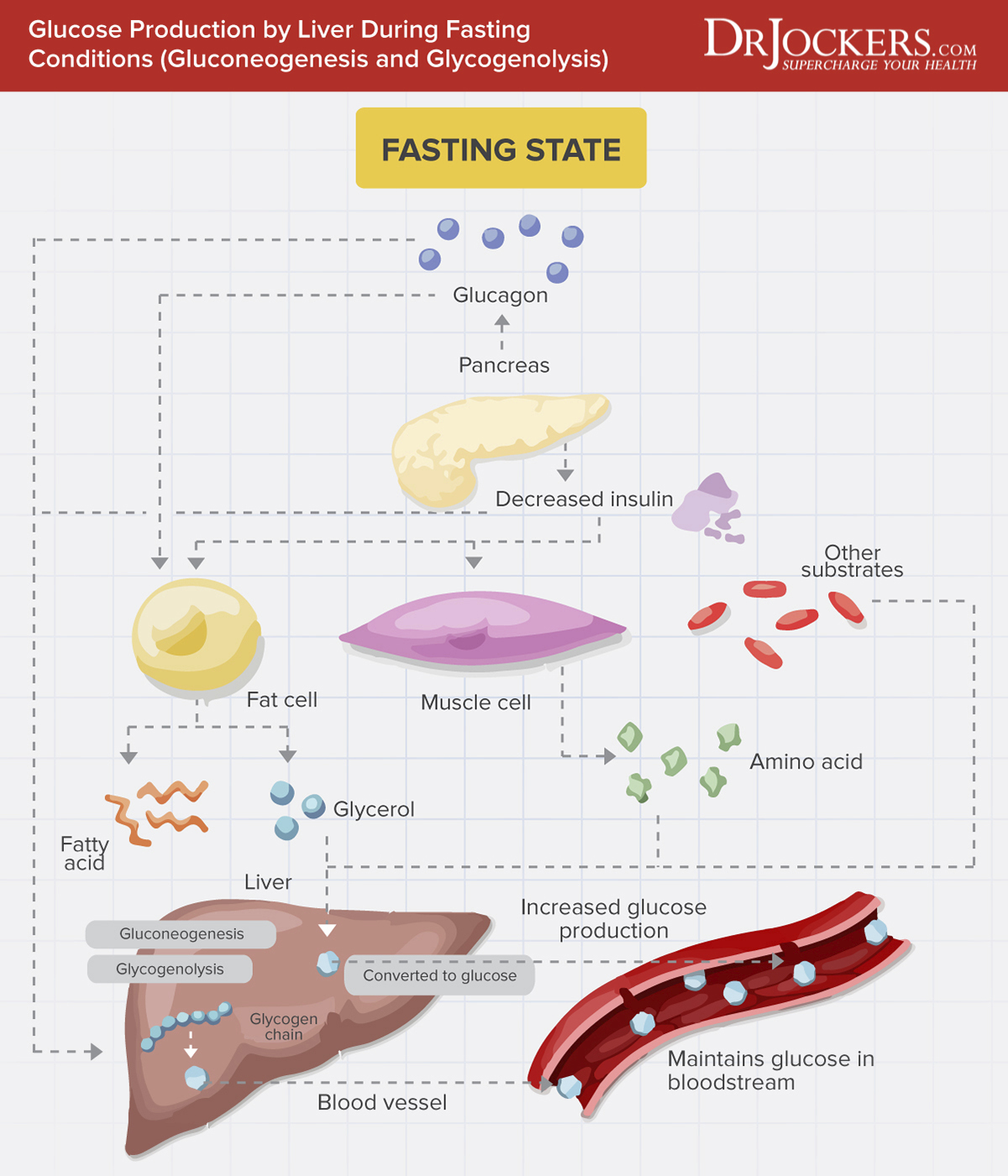
You may be wondering how your fasting blood sugar can become elevated if you have only been consuming high-fat meals and very little carbs. Well, your body has a built-in mechanism to create its own glucose. This is because there is a small proportion of the body that can only burn sugar as an energy source.
While the rest of the body’s cells are burning ketones for energy, your body will actually use amino acids, lactic acid, and glycerol to manufacture the necessary sugar for those cells. This process is called gluconeogenesis. Additionally, the body will store a small supply of glucose in the liver and muscles in the form of glycogen.
This is why some people are able to stay in ketosis for long periods of time with no consequences, they are still getting all the sugar they need! Some people do seem to do better with a cyclical ketogenic diet, however.

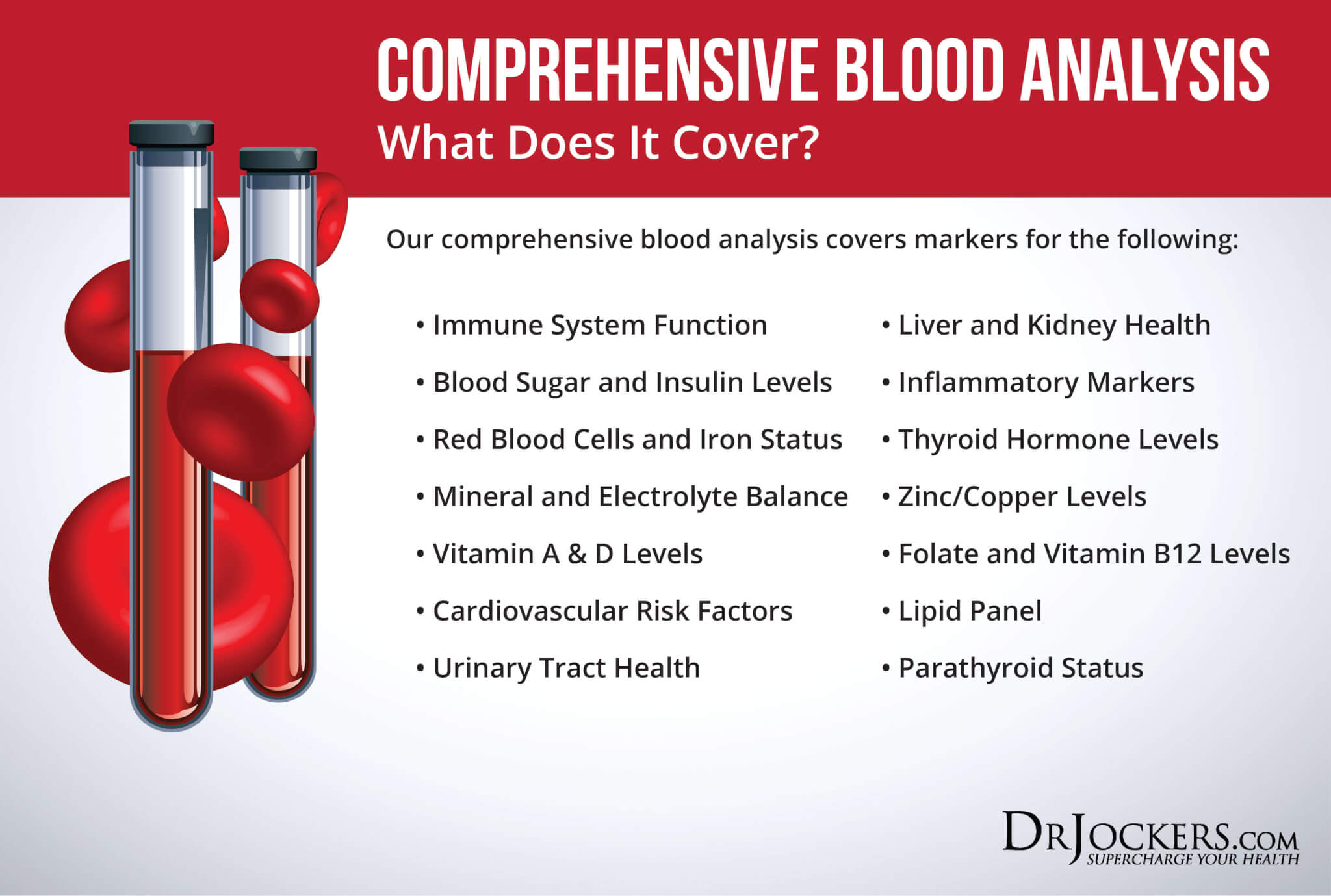
Measuring Blood Sugar Balance
So, as you can see, it is not as simple as looking at a single isolated blood sugar value when determining if your elevated fasting blood sugar is a reason for concern. If your blood sugar is a concern to you, there are a number of other values that are actually much more helpful. These include:
Fasting Insulin: A high fasting insulin will be a sign of insulin resistance, especially accompanied by an elevated blood sugar
Hemoglobin A1C (Hb A1C): Gives insight into blood sugar balance over the last 3 months, an elevated value would signify poor blood sugar control and potentially diabetic conditions
C-Reactive Protein: An inflammatory marker highly correlated with blood sugar, an elevated value would signify poor blood sugar balance as well as a potential increased risk of several chronic diseases (heart disease, arthritis, psychological disorders, IBS, etc.)
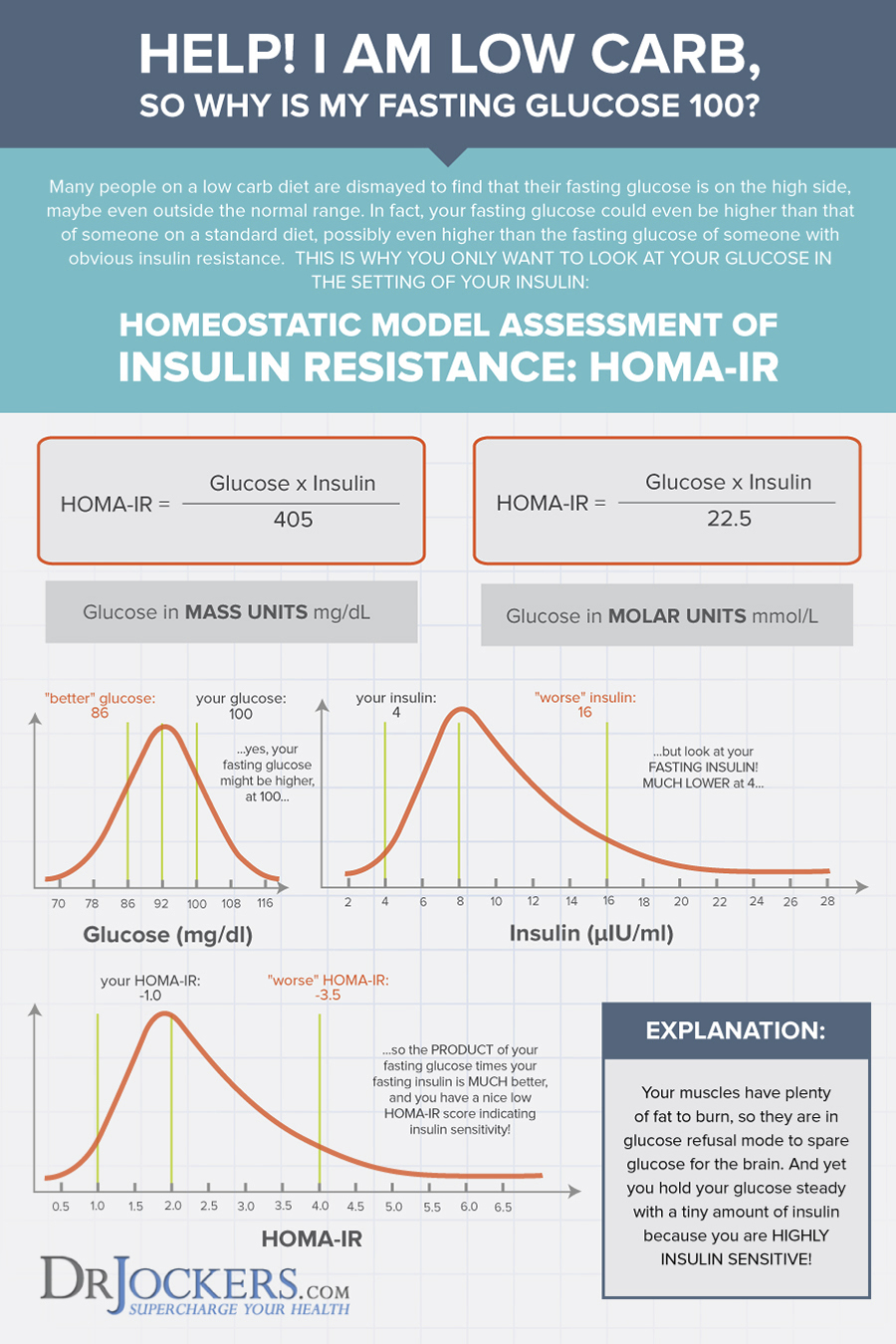
HOMA-IR: This is a key measurement for understanding insulin resistance. HOMA-IR is actually a simple equation that multiplies fasting glucose (in mg/dL) by fasting insulin (in μIU/mL). This total is then divided by 405. The following ranges are then compared:
Less than 1 = Optimal Insulin Sensitivity
Above 1.9 = Early stage insulin resistance
Greater than 2.9 = Significant Insulin Resistance
Essentially, HOMA-IR looks at the relationship between insulin and glucose in your body rather than each as a separate value. I learned about the HOMA-IR and got the ideas for this graphic below from our friends at Heads Up Health.
Other Factors Affecting High Blood Sugar
In addition to the normal cycle that occurs before waking up, there are a number of other factors that may be influencing fasting blood sugar. After considering the tests above, the following factors should be considered and addressed for optimal blood sugar balance.

Cortisol
If you are under a high amount of stress or are having HPA axis dysfunction, then uncontrolled cortisol secretion could be causing high fasting blood sugar levels. This is because cortisol quickly stimulates the release of glycogen stores to prepare the body for an immediate stressor and increased physical demand.
If you are constantly stimulating cortisol throughout the day due to your stressful lifestyle, then this will likely cause a blood sugar rollercoaster and elevated blood sugar at times.
Reducing your stress load and using other strategies to balance your cortisol levels will be an important step in ensuring this is not the cause of elevated blood sugar. For specific strategies on how to balance your cortisol, here is a great article: 7 Ways to Balance Cortisol Levels
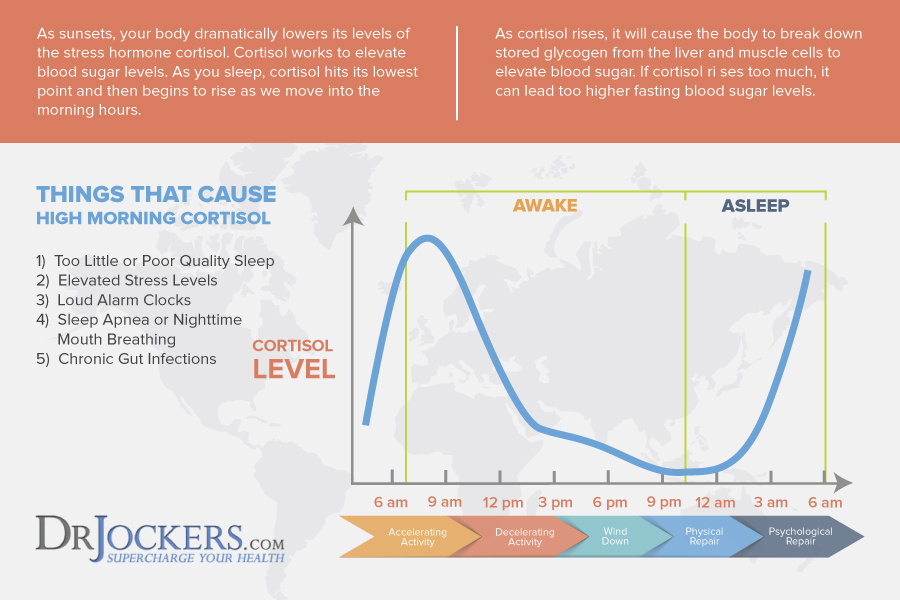
Sleep
Just one night of poor sleep can be a cause for elevated fasting blood sugar the next morning. In fact, poor sleep alone may be responsible for blood sugar readings that mimic those of pre-diabetic conditions (2). Not surprisingly, those who consistently get poor sleep seem to also have higher instances of diabetes (3).
I have a great article titled 7 Lifestyle Strategies for Better Sleep that can be helpful for troubleshooting any sleep issues you are having.
Another common sleep issue that I have seen is mouth breathing and sleep apnea. Mouth breathing and sleep apnea are associated with an increased stress response and poor oxygenation of tissues which can create stress responses and throw off blood sugar. Taking steps to ensure you are breathing through your nose and that your airways remain open throughout the night will be incredibly important.
Using a bit of micro pore tape at night to hold the mouth closed can help to facilitate more restorative nostril breathing. These SomniFix Sleep Strips recently came out and they are excellent.
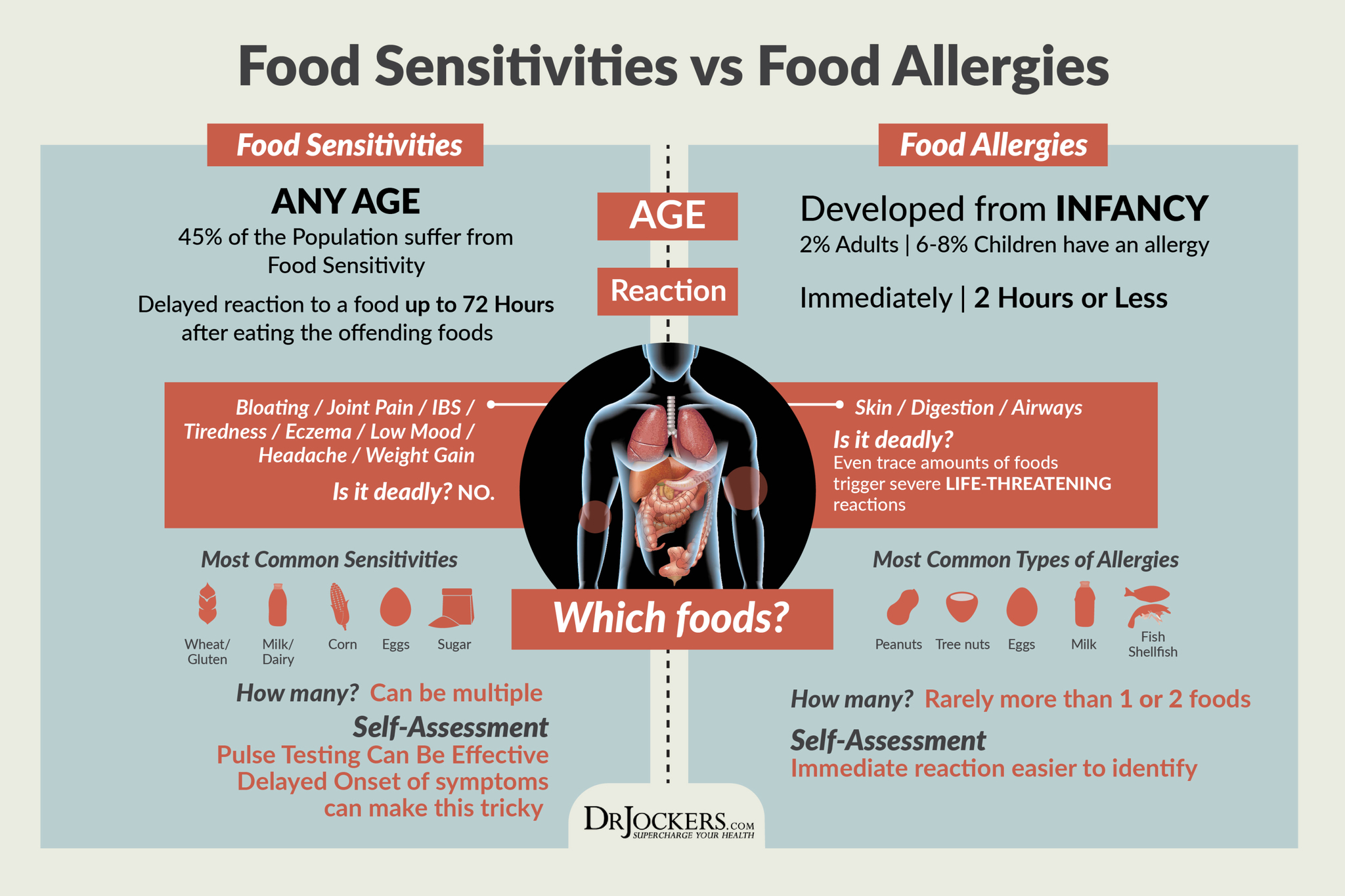
Food Sensitivities
A food sensitivity is a low-grade immune response to a particular food. These immune responses may be impossible to feel as they are occurring, however over time they can become an internal stressor on the body and stimulate cortisol, leading to elevated blood sugar.
Each individual will tend to have their own unique food sensitivities, however, common sensitivities include: grains (including wheat), cow’s milk, eggs, fish, soy, nuts, and seeds.
One way to find your food sensitivities is to have them tested through functional lab work. A simple and inexpensive way to test for your unique food sensitivities is to perform the pulse biofeedback test as outlined in this article.
Controlling for Monitor Accuracy
Oftentimes I have seen that certain blood sugar monitors can have off readings every now and then. If you have an elevated reading that seems unexpected, take the same measure 2 more times and average the values, oftentimes an elevated reading can be a monitor malfunction.
Other things to consider are any kind of residues that are present on the surface that you tested. For example, if you recently held a piece of fruit or used a product that contained sugar (soaps, artificially scented products, etc.) then this can also throw off your monitor.
Make sure you wash the testing area thoroughly before testing and take multiple readings to ensure accuracy.
Monitoring both ketones and fasting blood sugar can be extremely helpful as well. This is because if your ketones are elevated at the same time as a slightly elevated blood sugar reading, this is a good gauge that you are still in ketosis. As I described above, this scenario may be more likely to be adaptive glucose refusal. My favorite 2-in-one monitor is the Keto Mojo.
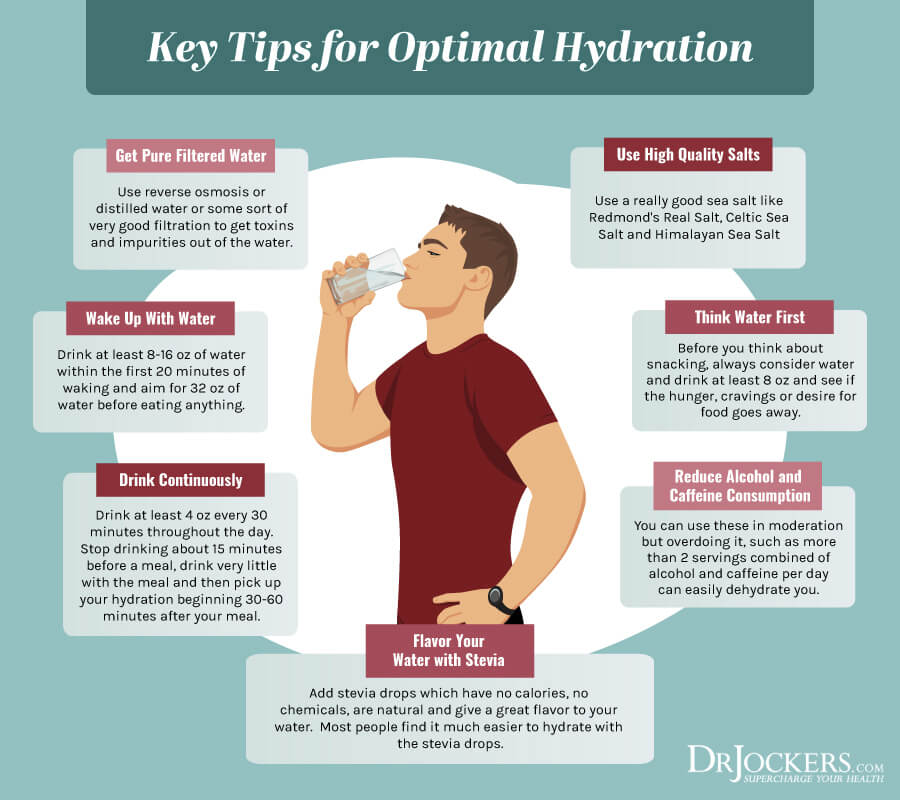
Hydration
Your level of hydration is going to have an impact on the concentration of things that are dissolved in your blood, including glucose. This means that a high blood glucose could simply be due to dehydration. To address this matter, simply follow these guidelines for daily water consumption:
At least half of your body weight in lbs. should be consumed in ounces of water per day. Ideally, this would even reach your full body weight.
Start your day with what I call super hydration. Before consuming your first bite of food, drink 16-32 oz. of water to hydrate your body, flush out your system, and stimulate a bowel movement. If you are someone who does intermittent fasting, feel free to increase this amount.
I often recommend that those who fast until noon or later consume around a gallon of liquids in the form of water, organic broths, herbal teas, and coffee.
Additional Strategies to Balance Blood Sugar
Blood sugar balance is critical for optimal health. Along with addressing the factors discussed above, the following are additional strategies to ensure you maintain stable blood sugar.
Many of these strategies are simple to incorporate into your daily and weekly schedule.
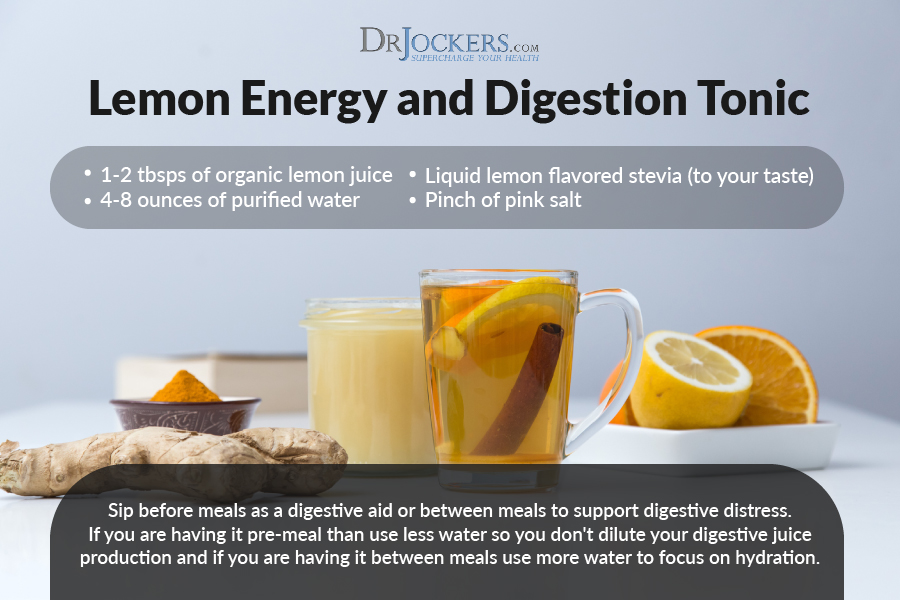
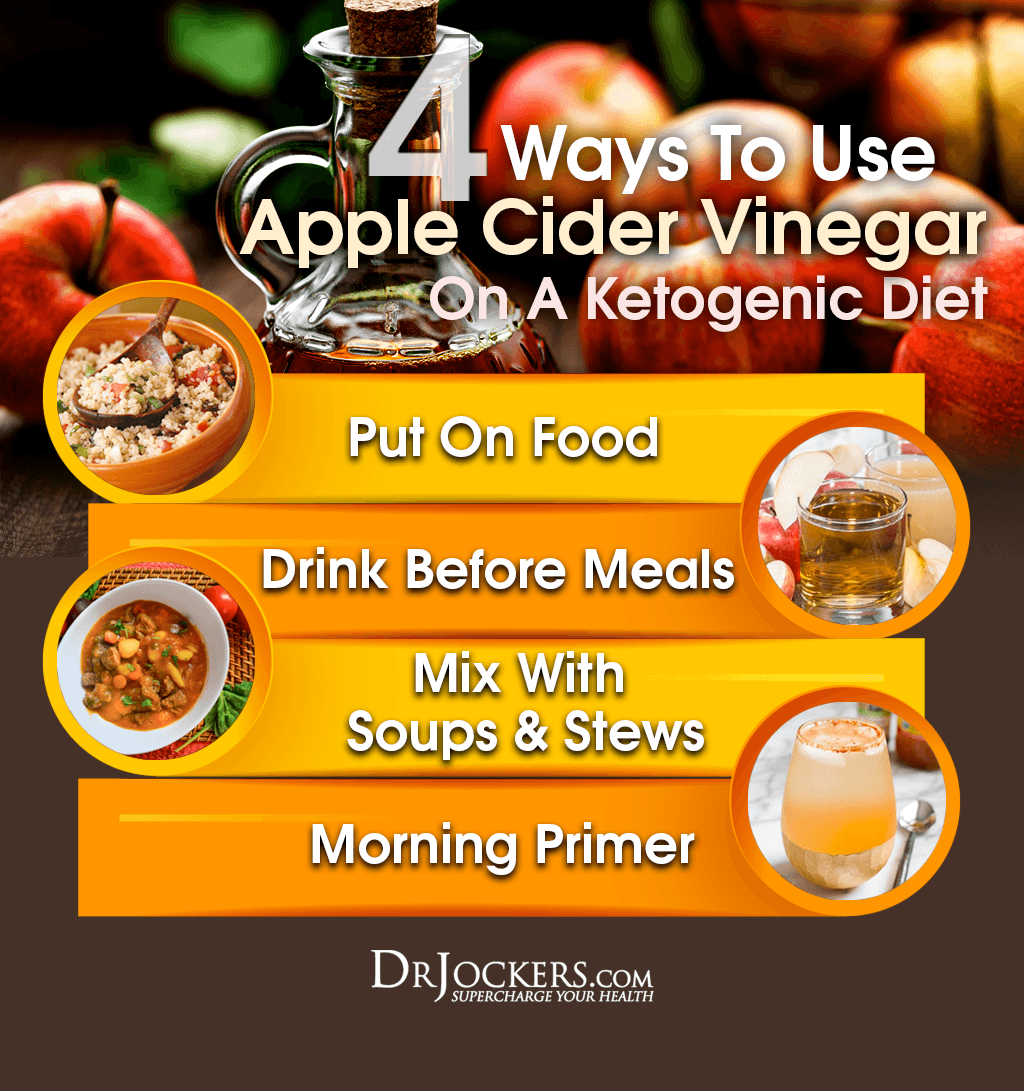
Apple Cider Vinegar or Lemon
The naturally occurring acids found in apple cider vinegar and citrus fruits, namely acetic and citric acids, are a cheap and powerful way to balance blood sugar (4, 5). One of the most effective ways to use these is to simply add them to your food and water.
Vinegar and lemon juice go great in many different dishes as a marinade, a dressing, or simply drizzled over top. I will often sprinkle these over a good grass-fed steak or salad to help assist in digestion and absorption as well.
Putting lemon juice and a bit of stevia in your water is another great refreshment to have throughout the day to satisfy your sweet tooth and stabilize blood sugar at the same time.
Prolonged Fasting
Fasting is one of the quickest and most effective strategies for restoring blood sugar balance and possibly improving fasting blood sugar. This is because it provides a rest for insulin receptors and allows for a deeper state of ketosis.
While performing an intermittent fast every day can be helpful, I will often recommend performing a 24-48 hour fast once per week to kick the benefits of fasting to the next level.
A common eating schedule I see a lot of success with is where one consumes a ketogenic style meal plan from Monday to Saturday, consumes a higher carb meal on Saturday night, and follows that up with a 24 hour fast from Saturday dinner to Sunday dinner.

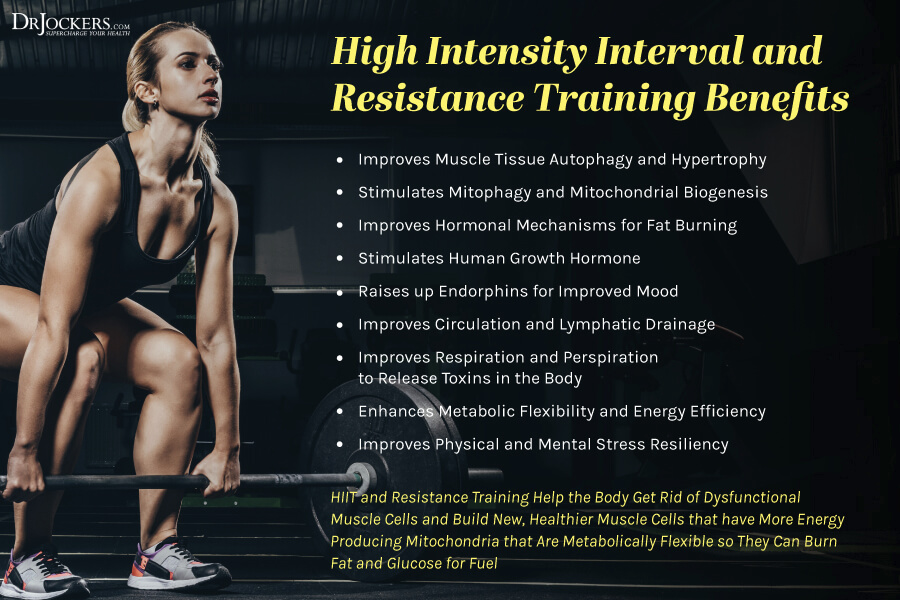
High Intensity Exercise
Getting your blood pumping with some high-intensity exercise 2-4 times per week can have a powerful impact on your blood sugar balance. This is because when placed under a high demand, your muscles will rapidly burn up any available sugar available, improving insulin sensitivity in the process (6).
Another helpful strategy if you tend to have elevated blood sugar after meals is to take a light 10-minute walk. The muscle activity may activate a glucose transporter named GLUT 4 which will help ensure excess blood sugar is stored in the muscle tissues (7). Over time, remaining physically active may improve fasting blood sugar levels.
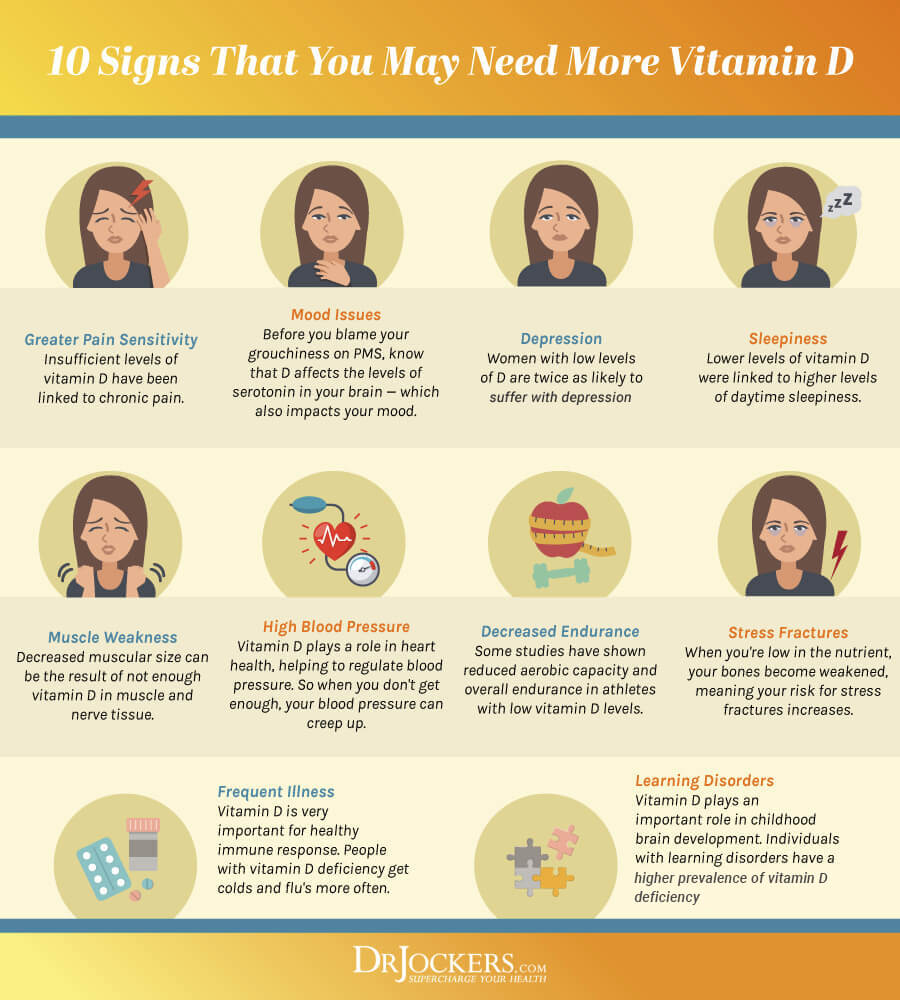
Improve Vitamin D Levels
A commonly overlooked aspect of blood sugar control is Vitamin D levels. Low Vitamin D levels are commonly associated with poor blood sugar control. It appears that supplementation with a high-quality Vitamin D supplement may help with elevated blood sugar in some individuals (8).
Increasing your exposure to the sun is also helpful for improving Vitamin D levels. Ideally, you would want your Vitamin D levels to fall between 60-100 ng/ml. In my experience, most individuals are well below this range unless they have taken active steps to improve their levels.
Assess Thyroid Health
The thyroid is the master controller of the metabolism. The way your brain and thyroid communicate to determine the expression of your thyroid hormones ultimately dictates your ability to burn fat and stabilize blood sugar to a large extent.
There are many different factors that can influence your thyroid hormones including stress levels, liver health, nutrition, and paradoxically, blood sugar.
If you have poor blood sugar control and chronically elevated insulin levels, this will likely place stress on the liver. The liver has the important job of assisting the conversion of the inactive thyroid hormone (T4) into its active form, T3. If this function is inhibited and the metabolism slows, burning and balancing blood sugar becomes more difficult. It then becomes apparent how this can turn into a vicious cycle.
Luckily, your thyroid status can be easily tested along with several other markers mentioned in this article (Vitamin D, fasting blood glucose, fasting insulin, HbA1C, and CRP). In fact, all of these markers can be found in one lab, our Comprehensive Blood Analysis.
Conclusion
High fasting blood sugar on a ketogenic diet may not be of huge concern. In fact, it may be a sign that your body is adapting well to burning fat for fuel!
To be sure that you are not having other complications, additional measures of blood sugar balance are mentioned in this article including HOMA-IR, HbA1C, and CRP.
Finally, using additional strategies to balance blood sugar as mentioned above is a great way to ensure your fat burning engines stay primed. If you are looking for a more detailed fat-burning, keto meal plan and recipes then check our complete Navigating the Ketogenic Diet program here:



How can I safely intermittent fast when having HPA Axis dysfunction and hypothyroidism and seemingly, blood sugar issues though I do not consume any sugar? There seems to be such a fine line with how long I fast and just how bad my body might feel ( ice cold hands, white noise and ringing pressure in my ears and head mostly). If it were not for these symptoms, I would easily do 20/4 or 24hours fasts to ultimately heal my body. My intention is to do just that and I would love any suggestions on how to titrate up in my fasting windows without stressing my body. Thanks for much, for your site, your videos and for listening right now!
Amanda
Hey Amanda, check this out! https://drjockers.com/best-intermittent-fasting-strategies/
Thank you ! Though I’ve read and reread that great article, I always skipped the simple and cycle fast options. I dove right in at 16/8. And to think I considered myself a patient person! Thank you for slowing me down to be more safe and realistic!
Very informative article. Thank you. I have been doing fairly strict keto with a 16 hour fast every day for 3 months. I have lost 25 pounds but my fasting morning glucose has been high. I have been prediabetic in the past but sugars never higher than 100. Now they are 130-140! I haven’t checked glucose later in the day, just want to know how concerned to be. I will definitely have my doctor order those tests to mentioned. Will also try the lemon water at night.
Hey Amy! There could be a few reasons for this. Running some more of these tests will help get a better idea of what is going on!
See above post
Is it possible that apple cider vingegar could actually cause too low blood sugar and possibly stimulate a “rebound” gluconeogenesis/higher blood sugar after the initial drop?
I have not seen this happen Jim!
Thank you for the post. Are there any long term studies or data on the high and increasing FPG in people on keto diet? That’s, will FPG continue to rise with time and convert to frank DM in few years?
No this does not happen Hisham
I was not diabetic before starting keto over a year ago although my alc was 5.5. Now that I’ve been keto, if I even have a bite of anything high carb, even a sweet potato my blood sugar will spike to over 160. I did not have this issue before going keto . What would be the cause of this? Thanks
This is a normal response if it is within 1 hour of eating as your body is so used to burning fat for fuel, the key is to test after 2-3 hours and it should be at 100 or lower.
My friend said she did keto for a few weeks and gained 20 lbs. What could cause that? (She is usually in a high stress situation.)
That seems like an embellishment, but she may have gained a few pounds and this article would explain why https://drjockers.com/weight-loss-hacks/
Been Keto adapted for several months, been noticing an odd pattern. I intermittent fast on a 16/8 pattern and before I break the fast, here is what I see:
1. FBG around 99, ketones at 0.8 at waking
2. Fasting (nothing but black coffee, tea, water), my BG steadily rises to 110ish as the day progresses. Ketones decline down to about 0.3 as the fasting day progresses.
3. I’ve been testing the impact of single foods – 1 hr and 2 hr post meal BG and Ketones. Only eat that one food and monitor for 2 hours after fasting.
4. If I eat carrots or green banana (two of my tests), my BG goes down to 90ish immediately. Not up, but down. Ketones increase at the same time.
5. BG slowly rises back to the 110ish level, ketones increase.
I can replicate this by eating a good carb at any time (green banana, carrots, yam/sweet potato) all day long. Eat carb, BG lowers significantly and ketones increase.
Yesterday I did a carnivore fast (meat only, no carbs) and saw the same behavior, note I had some wine the night before which always lowers my morning BG (another mystery).
Morning BG 91/Ketones 1.0
Break-fast at noon (meat only) BG 95/Ketone 0.6
4pm (no more food) BG 100, Ketone 1.0
5pm (no food) BG 101, Ketone 1.6
eat green banana
6pm BG 93, Ketone 1.7
7pm BG 101, Ketone 1.3
eat cauliflower mash – immediate BG 91
8pm BG 100, Ketone 0.6
9pm BG 94
next AM
FBG 99,Ketone 0.8
9am BG 108, Ketone 0.4
11am BG 107, Ketone 0.3 (nothing but black coffee all morning
Any idea what is going on? This seems contrary to my understanding of insulin/carb behavior.
That is interesting that would happen. My guess is that you have very good insulin sensitivity but are overproducing cortisol when you are fasting. When you eat carbs, it calms the stress hormones and your body is very good at getting those carbs into the cells so you don’t produce enough insulin to drive down ketones.
I noticed a small editing/typo error and am pointing it out in case you would like to correct it. In the third bubble in the diagram “How Body Controls Blood Sugar Levels,” it says “Blood caries glucose and insulin…” instead of saying “Blood carries glucose…” I’m not complaining, just trying to be helpful!
Thanks for all the great info. I listened to many of the talks from the Fasting Transformation Summit and have learned a lot and been inspired to change some of my eating habits.
With gratitude, Paula
Thanks for letting us know Paula, we will update that image!
If you are having dawn phenomenon while doing an extended fast, what do you recommend to stop that BG rise without breaking the fast?
ACV/lemon juice in water or tea? Coconut oil? Bone broth? Or, something else?
I would recommend deep breathing and possibly mouth taping at night!
Hi Doc,, your article is really helpful in clearing many aspects in this regard.
I am diabetic for last 20 years, was taking metformin and glimepride as medication, now with the help of weight loss and ketosis i am now without medication.
The problem i am facing with blood sugar is that as soon as it goes down to 120mg/dl at any time of the day with exercise or diet, it jumps up again.
Your advise is needed in regards to how i can decrease this limit of 120mg/dl
Great to hear that Doomham! I would be sure to incorporate intermittent fasting strategies to further lower your blood sugar and improve insulin sensitivity: https://drjockers.com/best-intermittent-fasting-strategies/
Hi! I have some questions about my blood glucose readings. I’ve been doing strict keto for a little over a month. I’m not diabetic or pre diabetic. My fasting blood glucose in the morning is usually in the 90’s and typically goes down to the 80’s and 70’s throughout the day. My ketone levels are usually around 1.5 with the higher blood glucose in the am and go up to sometimes 3.0 as my blood sugar goes down. Could the higher blood glucose in the am just be from the dawn phenomenon?
Yes the higher morning blood glucose is very normal and associated with higher morning cortisol.
Hi, I have been strict Keto for six weeks. I lost 8 pounds the first
4-5 weeks and am normally in ketosis ( 1.6 to 2.1) but FBS stays consistently between 107-116. I keep my carbs under 20 most days. Please help – what could be wrong?
Yes this could be due to higher morning cortisol. I wouldn’t be overly concerned but follow the suggestions I listed in the article.
Dr Jockers, first thank you for all your info & support. I often visit your site. I been doing keto / IF beautifully for the last 5 month due to insulin resistance/ skin inflammation/ mental fog/fatigue. All my blood work number gotten better my morning fbg is at around 80 and IF have provided pretty skin and better all my functions. 3 weeks ago during a weekend conference I was deprived sleep, feel stressed, during the last day of the conference my morning fbg got up to 120-130 and when i eat it does go lower but then it will go back up because the my liver is make it’s own glycogen . Since then i have try everything to bring it down like sleep more, relaxe to supposely to lower my cortisol. It has not worked. I eat less then 10 carbs a day. There is probably Dawn effect/ or glucose sparing. However the part that is concerning is that I am losing my hair, skin is inflamed, hot flashes while on these high bg numbers. For the 5 month on keto I have nice numbers like bg at 80-90, ketones 1.5-3.0
Now I have 120 morning fbg, during the day 100-120. Ketone down to 0.3-to 0.5.
Before these number went up. My fast insulin was at 7 fasting glucose 90.
I think I need to go back to my doctor ask for another test right now. My question is if I cycle in more carb may increase more inflammation. Or how do I reset my body, almost as if it got stuck on stress train and don’t know how to get off the train I am so confused on what my body is doing. Would really appreciate any suggestion!
Sorry to hear this! I would recommend reading this article: https://drjockers.com/hair-loss-keto/
Thanks for a great article! I little background. Have been a type 2 for about 13 years. I have been using Metformin, glimpizide, and about 20 units of Levimir before bedtime. I know that it is very difficult to loose weight when you have a high insulin level. So I started a keto diet about 6 weeks ago. My blood sugar came down nicely, so I slowly eliminated the glimpizide and Levimir after the first month. The good thing is so far I have lost 15 pounds(now at 205 want to go to 170) My issue/concern is my blood sugars are averaging 155 when I wake up. Later before dinner when I test it is 140(average about 12 grams of carbs, many times I skip breakfast and lunch). After dinner(15-20 grams) it goes back to the 160’s. I am only taking Metformin in the morning and before dinner. Feeling a little discouraged. Do you think it needs to take more time to get my blood sugars lower? When I test for Ketones, it is usually shows a small/low reading. My other thought is am I insulin resistant, and possibly not producing enough of insulin as well? I had pancreatitis about the same time as I was diagnosed with D2, dont know if it was coincidence or part of the cause. Appreciate any input you might have. My doctor is a bit of “old school” so she does not get the new thinking on this.
Hey Steve, great news about dropping the weight. If you are very insulin resistant it is going to take you longer to keto adapt. While I cannot give you specific advice, one good strategy I have seen with many insulin resistant type II diabetics is only consuming 1 meal a day (ketogenic based with less than 20 total carbs) within a 1 hour eating window and doing intermittent fasting for 23 hours each day and drink a lot of water and take a bit of salts during that time period. Most see really good results over time with this strategy. Remember, this is not specific advice, just sharing an observation. Be sure to discuss with your doctor.
Thank you!
I’m pre-diabetic and have been keto for 10 months. I typically do the 16/8 IF. I definitely suffer from the Dawn effect- my FBG is usually around 110 in the morning when it was under 100 before bed. My question is, how can fasting be good for me if raises my FGB? If my blood glucose is lower and more stable when I’m not fasting then shouldn’t I avoid it? The way I see it, more time I spend with a blood glucose level over 100, the higher my A1C will be, right? My A1C was 5.5 after 3 months of keto. I started IF after that and now my A1C is 5.7. I really want to control this naturally without drugs.
There are a lot of great benefits to fasting, but yes, you need to get your blood sugar down and ketones up. It dosn’t appear that you have ever spent a lot of time in true nutritional ketosis. You most likely have high cortisol isssues and may need to eat 3 keto meals a day at first and focus on getting exercise, deep breathing and good sleep. Here is a helpful article: https://drjockers.com/7-ways-balance-cortisol-levels/
Fasting bs 300 I am following a strict keto diet and Dr wants me to do a sliding scale insulin before each meal also my A-1 C was over 12. I don’t know what to do a couple of years ago I was on insulin long and short acting and also pills when I went first time on keto gradually was able to get off all the medications I’m afraid to start back on anything
Sorry to hear that! You may have autoimmune diabetes where you are not producing insulin. Be sure to get tested!
I need some advice, type 2, NAFL, HBP, 270lb, 50 yr, 6ft male. I take no meds except for blood pressure linsopril. I have been on Keto around 20 grams per day for about 5 years since diagnosed with type 2. My normal morning/fasting blood sugar used to be 100-120 range. This year at some point my morning Blood sugar went up to around 130-150. Stays more on the 140-150 side. No change in diet except maybe more calories. My blood sugar seems to go down through out the day. Down to maybe 120 or lower by bedtime. I’ve tried intermittent fasting, for about a week no change in morning BS. Tried daily shots of ACV after every meal, seem to have an effect post meal, but no change on morning blood sugar. I’ve tried restricting calories, that did lower my blood sugar for a few days then it spikes back up. It takes about two days to see an effect, it drops to 130’s on the 3rd day, and then 120’s the next. But it will shoot back up to the 140’s maybe the next. I’m going nuts trying to understand what’s going on. I have a VA doctor they don’t really understand the keto / low carb diet. I really don’t want to take insulin or meds if I can avoid it. Thanks
Hello Michael, it sounds like there is most likely an autoimmune condition going on, I would recommend working with a functional health coach to get to the root cause of this. https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
I need some help, please; I am following a low carb diet since a while now, and I notice that lately, my fasting glucose is higher than before, Around 100. Also, my ketones levels more than 1, which concerns me because I do go out of ketosis and also add carbs, but my ketones are usually high. I am interment fast at least five times a week. I don’t eat junk food, gluten or vegetable oils. I often exercise and have low stress levels. What is going on :(?
I did a blood test, and my results are:
HOMA-IR 1,62
HbA1c ( HPLC) 5.1%
HbA1c (IFCC) 32 mmol/mol HB
CPR <5
Glucose 94
Cholesterol 209
Triglycerides 67
HDL 75
LDL 121
sd-LDL 20,3
Homocysteine 12 ( I do take B complex vitamins, and it was 7.9 five months ago)
Vitamin D 70 ( 5 months ago was 110, and I did not change my supplementation of vitamin D with K and A)
Help what should do? Why I am insulin’s resistant when I do all the right things it is frustrating.
Hello Sol, there is nothing bad about these numbers other than the homocysteine. I would look to take a specific homocysteine reducing supplement to optimize that here: https://store.drjockers.com/products/homocysteine-support
This is my second time doing the keto diet and I wouldn’t describe myself as a “beginner”. Last time, I did keto for 8 months and became fat adapted and I adjusted to the diet easily. The first round was successful and I was able to keep the weight off. But now I want to do it again and lose more fat. However, this time around, I’m struggling to maintain ketosis over night and I can’t figure out why. I will go to bed well into ketosis, but 2-3 hours after waking (fasted) my blood glucose is up and ketone production is down, and I’ll be well out of ketosis. I started the diet a week ago and was in ketosis in less than 48 hours. I have yet to maintain ketosis over night since I’ve started. I’ve been doing 16:8 IF but yesterday I did 18:6 and this morning my glucose levels are even higher than the other days (about 100 mg/dL). I’ve been eating 25g or less of carbs daily. I was reading about cortisol levels in your article as well as in a previous comment, is it possible jumping straight into keto and fasting all at once, is causing me to have cortisol issues? I do have chronic anxiety issues, but I’m medicated for that. I can’t decided what to try next; stop the IF or drop my carbs to 20g? Any suggestions?
Hello Rachel, these are great questions. I would recommend working with a functional health coach to help customize the best plan for you: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
I recently switched to a Keto diet. My body went into ketosis fast! I have a healthy BMI and A1C of 4.6, and fasting glucose numbers are all in normal range. I like to check randomly at times after a mild case of GDM with a pregnancy to see how my body is doing (I’ve never had high numbers after delivery and GDM was diet controlled).
I decided to do a “test” the other day (after about 4 weeks of being in ketosis) to see how my blood glucose would react. After a 90 blood sugar reading (a few hours after a 5 g carb snack) I drank 8 oz of juice (28 g carbs, 0g proteins). My 1 hour bg was within normal range, but I spiked to 155 bg at the 2 hour, then back to 112 bg at 3 hour. Was the spike due to leaving ketosis or is this a cause for concern of insulin resistance?
It sounds like the release of sugar was somewhat slow but hit at 2 hour range and then your body produced insulin to bring it back down. If you have a healthy BMI, low A1C of 4.6 and low fasting glucose, then most likely you are very insulin sensitive. I would get a fasting insulin level to make sure it is under 6 next time you get labs run.