 Interstitial Cystitis: Symptoms, Causes, and Support Strategies
Interstitial Cystitis: Symptoms, Causes, and Support Strategies
Interstitial cystitis affects about 3 to 8 million women and 1 to 4 million men in the United States alone. It is a painful chronic condition that is characterized by pelvic pain, bladder discomfort, burning, stinging, an urgency to urinate, and painful urination. While there is no known cure for interstitial cystitis, there are several natural strategies that can reduce symptoms and improve the condition.
In this article, you will learn what interstitial cystitis is. I will explain its symptoms, risk factors, and causes. You will understand the difference between non-ulcerative and ulcerative interstitial cystitis. I will share my top natural strategies for interstitial cystitis to improve your health.
What Is Interstitial Cystitis
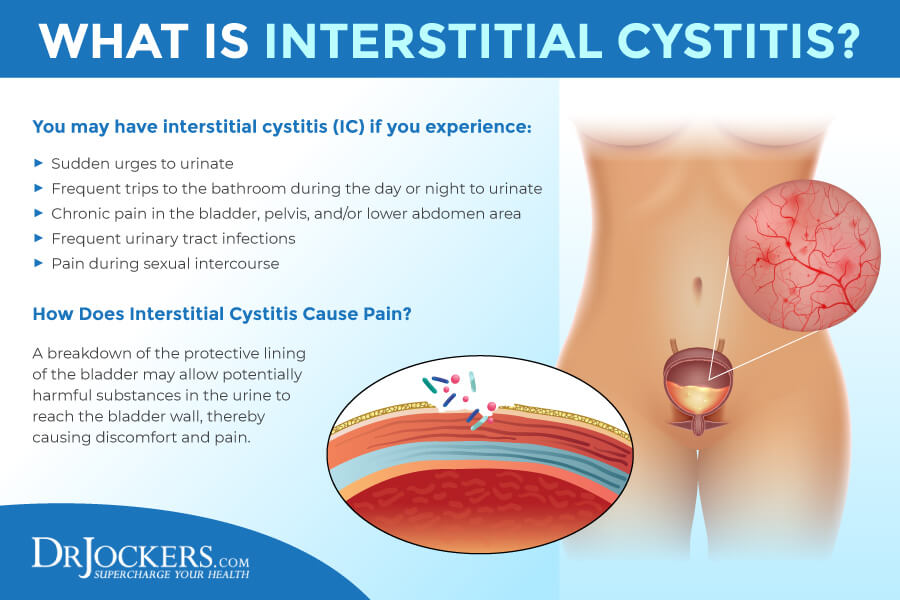
Interstitial cystitis (IC) is a chronic inflammatory pelvic condition. It is also referred to as painful bladder syndrome (PBS), bladder pain syndrome (BPS), and chronic pelvic pain (1). According to the Interstitial Cystitis Association, it affects about 3 to 8 million or 3 to 6 percent of women living in the United States (2). While it is more common in women, it can also affect men with about 1 to 4 million male sufferers in the US (2). The condition can be also diagnosed in children and many people with interstitial cystitis claim that their symptoms have already started in childhood (2).
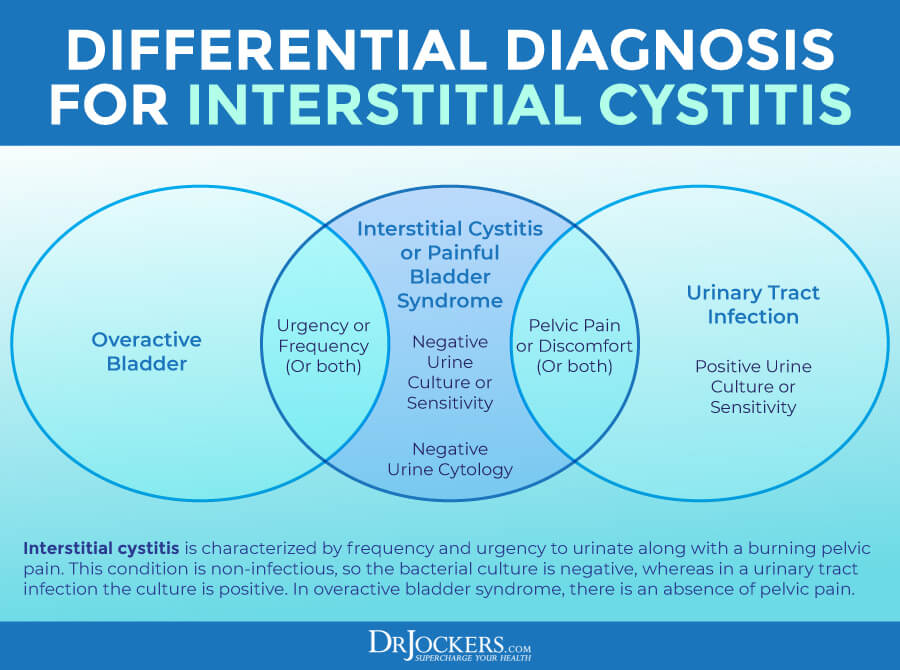
While some symptoms may be similar to urinary tract infections (UTIs) and other health issues, in interstitial cystitis, there is no infection present. In men, symptoms may be confused with chronic prostatitis which may result in the underdiagnosis of male cases.
Interstitial cystitis is a rather painful condition that in some cases can become debilitating. While it can cause severe pain and limitations impacting your quality of life, it is not considered a disability. It is a chronic condition that doesn’t have a currently known cure and treatment usually involves managing one’s symptoms long-term.
Major Symptoms of Interstitial Cystitis
Certain signs and symptoms of interstitial cystitis can be similar to or related to other conditions so before diagnosing interstitial cystitis, it is important to rule out acute infections or kidney stones and make sure one has experienced urinary and related pain for at least six weeks.
Symptoms of interstitial cystitis may vary from person to person. Some experience all or almost all symptoms while others only experience some. Some experience symptoms all the time, while others experience periods of flare-ups and remission. It is important that you visit a healthcare practitioner who can go over all your symptoms, health history, and do some relevant testing to rule out other issues and diagnose interstitial cystitis.
Common symptoms of interstitial cystitis may include (3):
- Bladder and pelvic pain or discomfort: It can spread to the lower back, urethra, or genitals. It can be severe, full, stabbing, or piercing.
- A frequent urge to urinate: The urgency is triggered by a pressure near the bladder. People with interstitial cystitis may have to urinate 40 to 60 times a day.
- Burning or stinging: People with interstitial cystitis often experience burning or stinging in their bladder, including during urination.
- Painful intercourse: Women may experience pain in the vagina, vulva, and behind their vagina, while men may experience pain in their penis, testicles, scrotum, and behind their scrotum.
- Pain while exercising: Many people find trouble exercising due to pain or the constant urgency to urinate.
- Sleep issues: Many people find it difficult to see because they have to get up to urinate all the time.
- Trouble performing daily activities: One’s everyday activities and regular life are often affected by pain, discomfort, and frequent urination.
- Chronic stress and mental health issues: Experiencing interstitial cystitis may increase chronic stress, emotional stress, anxiety, and depression.
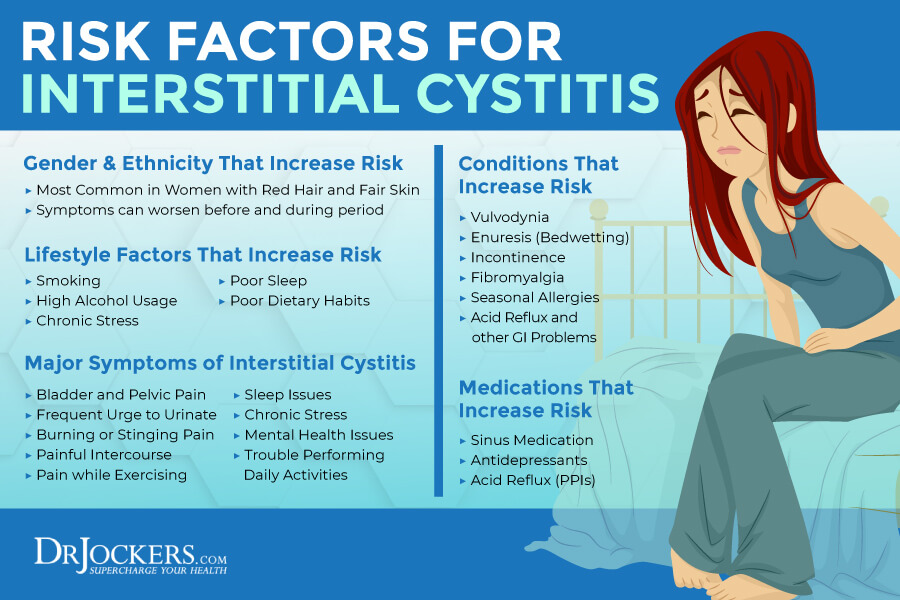
Risk Factors of Interstitial Cystitis
According to the Interstitial Cystitis Association, interstitial cystitis can affect anyone. Women and men are both affected, though the condition is somewhat more common among women (2, 4). It may affect people of all ages, including children, though it is usually diagnosed in one’s 30s or later. It may affect all races and ethnicities equally.
Certain lifestyle habits, including smoking, chronic stress, or a poor diet may trigger or worsen symptoms. Many women find that their symptoms are worse before and during their period. Certain medications, including antidepressants, acid reflux medication and sinus medications may also trigger symptoms of interstitial cystitis. People with interstitial cystitis commonly have other chronic symptoms or health conditions as well, including vulvodynia, enuresis (bedwetting), incontinence, fibromyalgia, allergies, acid reflux, or gastrointestinal problems.
Ulcerative vs Non-Ulcerative Interstitial Cystitis
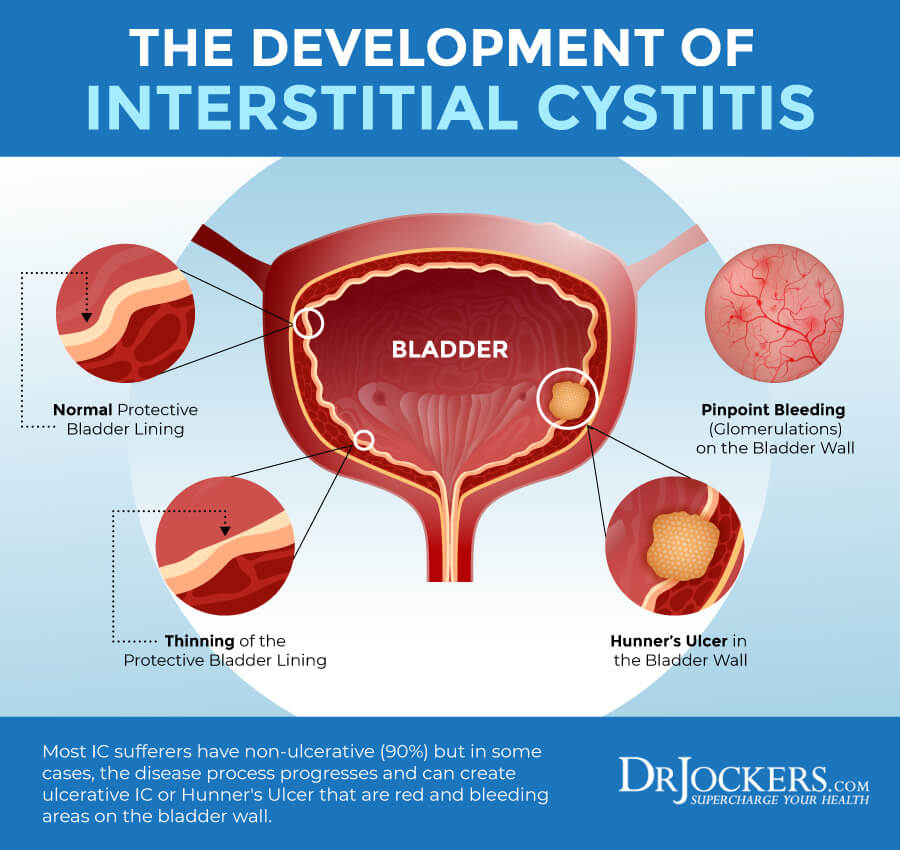
According to a 2011 study published in Urology, there are two subtypes of interstitial cystitis: ulcerative and non-ulcerative (5). They are not separate diseases but subtypes of the same one that shares some similarities and differences.
Non-ulcerative Interstitial Cystitis
According to the Interstitial Cystitis Association, about 90 percent of patients have non-ulcerative interstitial cystitis (1). This form is characterized by glomerulations or pinpoint hemorrhages on the bladder wall that are not specific for the condition and may present in other bladder inflammation as well.
Ulcerative Interstitial Cystitis
According to the Interstitial Cystitis Association, about 5 to 10 percent of patients have ulcerative interstitial cystitis (1). This form is characterized by patches called Hunner’s ulcers that are red and bleeding areas on the bladder wall.
End-Stage Interstitial Cystitis
End-stage interstitial cystitis is rare. It is diagnosed in about 5 percent of cases when someone has chronic and severe symptoms for at least two years. This form is characterized by a hardened bladder with ulcers and severe pain.
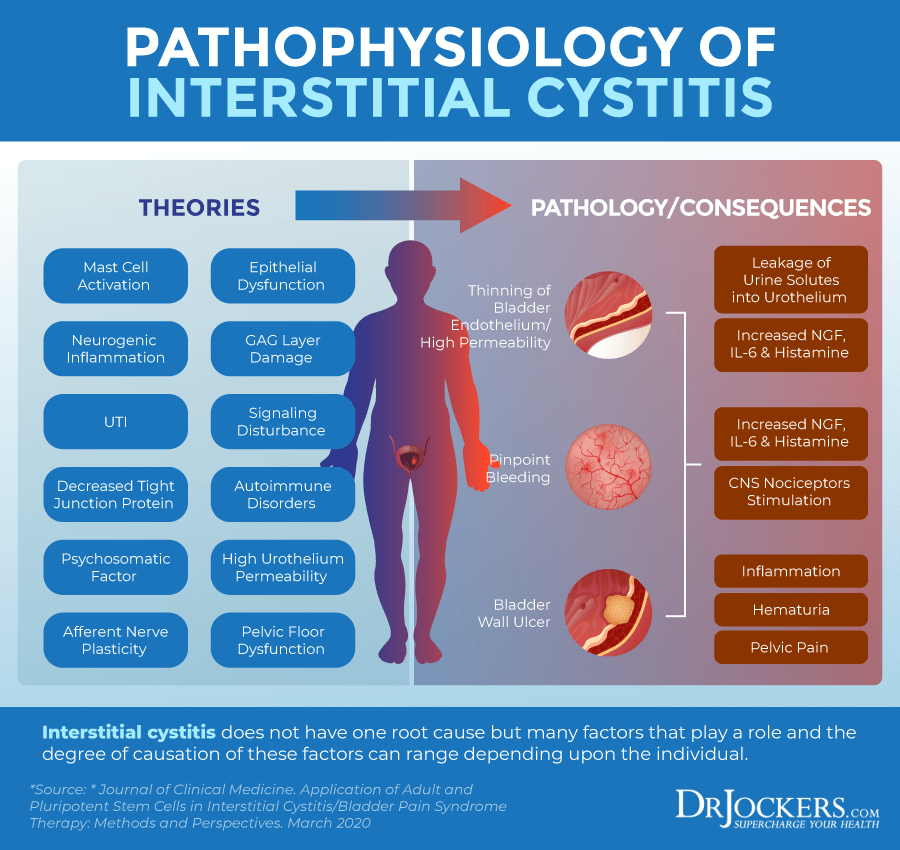
Causes of Interstitial Cystitis
While it is not clear what causes interstitial cystitis there are few issues that may contribute to the development of the condition. Potential causes of interstitial cystitis may include:
Bladder Tissue Damage
Bladder tissue damage may occur for a variety of reasons including bladder trauma and bladder overdistention. Bladder trauma or bladder injury is not common, however can occur from a pelvic fracture, piercing object, a blow, or other accident.
As described in a 2012 study published in Neurology and Urodynamics, acute prolonged bladder overdistension (ApBO) can happen because of an undetected, untreated, or inadequately treated acute retention which may develop due to prolonged childbirth, surgery, or regional anesthesia (6). Bladder tissue damage can lead to an increase in the risk of symptoms of interstitial cystitis.
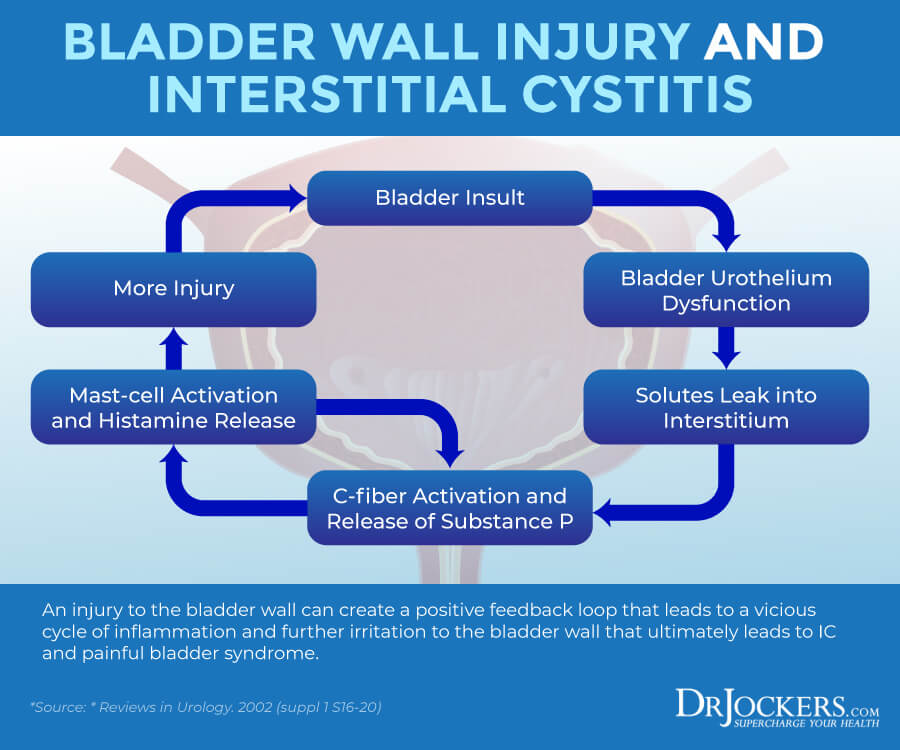
Pelvic Floor Dysfunction
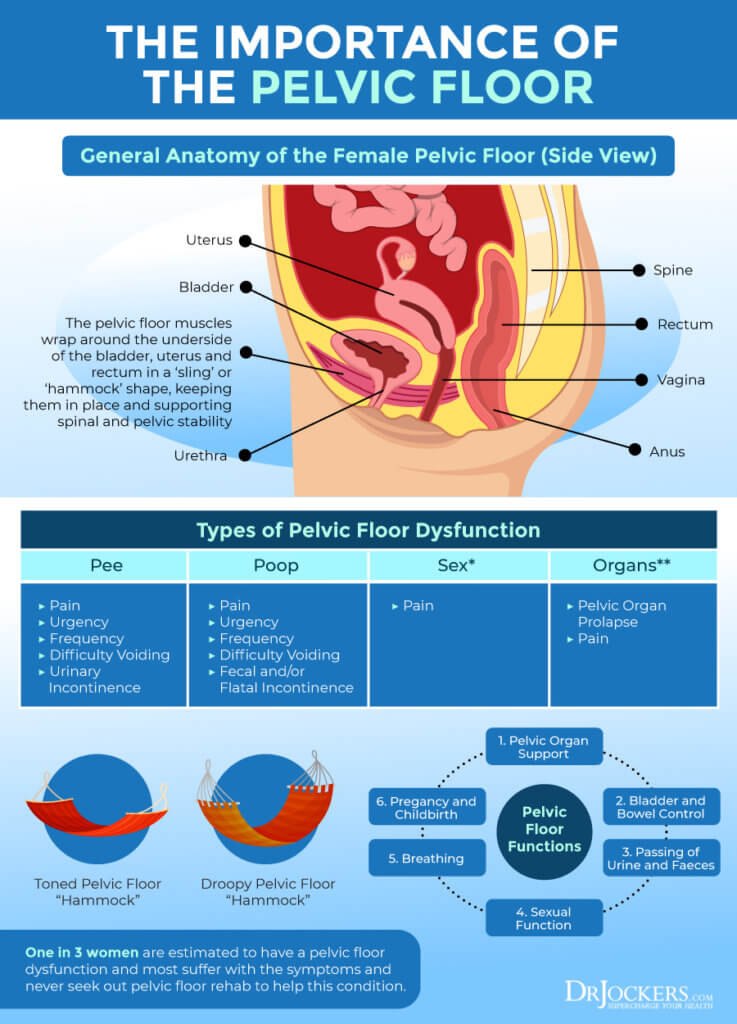
Your pelvic floor is a group of muscles that attach to your pelvic bone and sacrum and support your organs in your pelvis, including the bladder, uterus, prostate, and rectum, and also wrap around the urethra, rectum, and vagina. By contracting and relaxing, these muscles help to control bladder and bowel movements and in women also play part in sexual intercourse.
According to the Interstitial Cystitis Association, many people with interstitial cystitis also experience pelvic floor dysfunction that may result in problems around urination and painful sexual intercourse that are common symptoms of interstitial cystitis (7).
Autoimmune Issues
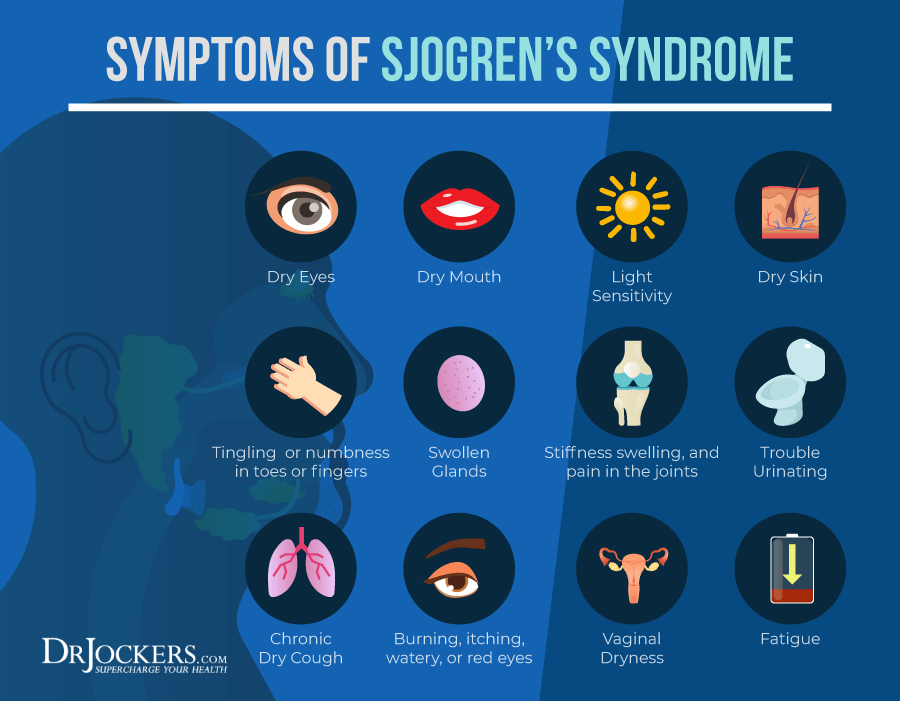
According to a 2007 study published in Nature Clinical Practice Urology, there may be a connection between autoimmune diseases and interstitial cystitis (8). People with interstitial cystitis commonly have an autoimmune condition or fibromyalgia as well. Indirect evidence suggests that interstitial cystitis may have an autoimmune nature.
The study found the strongest correlation between interstitial cystitis, Sjögren’s syndrome, autoantibodies to the muscarinic M3 receptor in Sjögren’s syndrome, however, more evidence is needed to fully understand the possible connection.
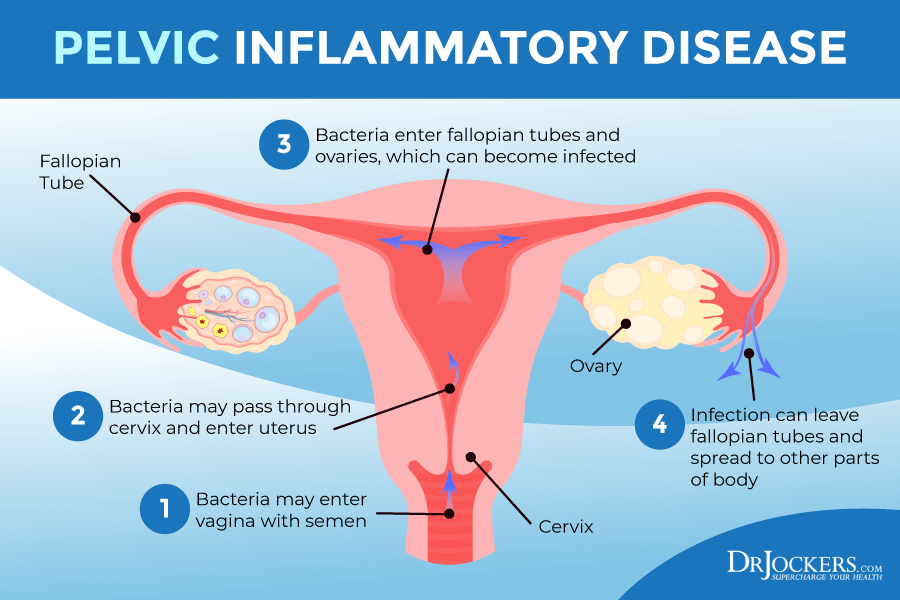
Pelvic Inflammatory Disease
Pelvic inflammatory disease may develop due to chlamydia and other sexually transmitted diseases. According to a 2015 study published in Medicine (Baltimore), there may be a connection between pelvic inflammatory disease (PID) and interstitial cystitis (9).
PID is associated with both inflammation and pelvic pain that may trigger further symptoms of interstitial cystitis. The study suggests that those with pelvic inflammatory disease should be evaluated for interstitial cystitis or vice-versa.
Neurogenic Inflammation & Spinal Cord Trauma
Neurogenic inflammation and spinal cord trauma may also cause interstitial cystitis. According to a 2018 study published in Seminars in Immunopathology, the nervous system may be an underlying issue in neurogenic inflammation in the pelvic viscera (10). Spinal cord trauma and neurogenic inflammation can cause both acute and chronic conditions related to the bladder wall.
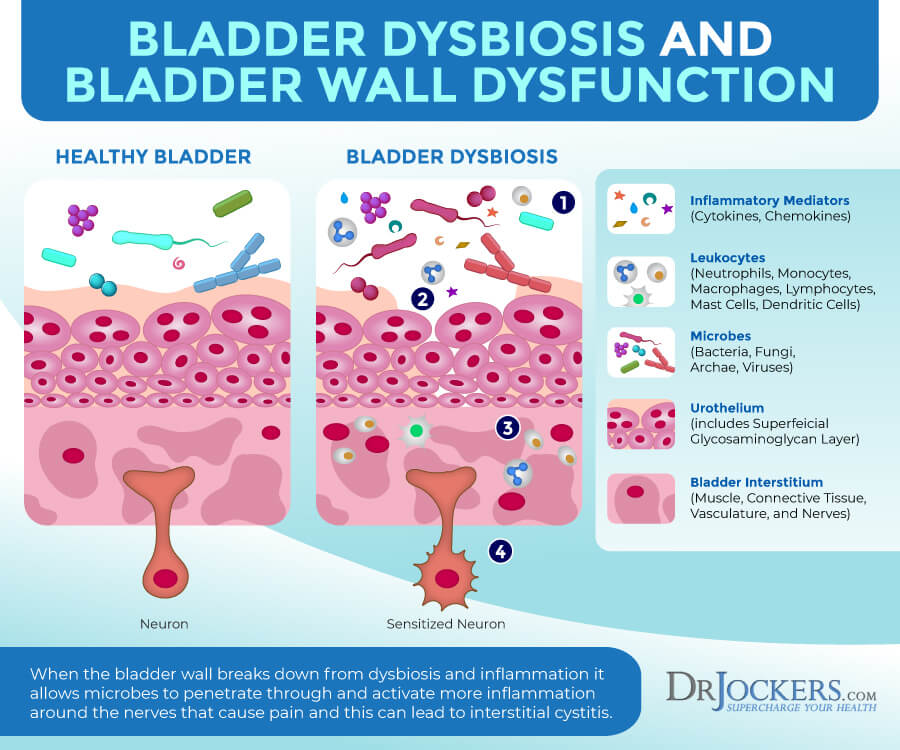
Vaginal and Urinary Dysbiosis
Having a healthy microbiome is important not only in the gut but the vaginal and bladder area. According to a 2019 culture-independent analysis of the female microbiota in interstitial cystitis published in the Journal of Clinical Medicine, urine microbiota may affect interstitial cystitis and bladder pain (11). The study looked at differences, including presence, diversity, and abundance in species and genus of bacterial and select fungal species of participants.
They found an overabundance of Lactobacillus gasseri and a lower prevalence of Corynebacterium in those with interstitial cystitis compared to the control group. The study suggests that further research is needed on the role of the vaginal and urinary microbiome in interstitial cystitis.
Natural Strategies to Support Interstitial Cystitis
Conventional treatment options for interstitial cystitis usually include medication, such as amitriptyline, pentosan polysulfate, hydroxyzine, cimetidine, gabapentin, prescription painkillers (opioid analgesics or codeine), and over-the-counter painkillers (ibuprofen, acetaminophen, or aspirin), physical therapy, bladder training, biofeedback, lifestyle changes, and biofeedback (12, 13).
Supporting your body with natural strategies may help your symptoms naturally within the need for medication or surgery. Here are the natural support strategies I recommend for interstitial cystitis:
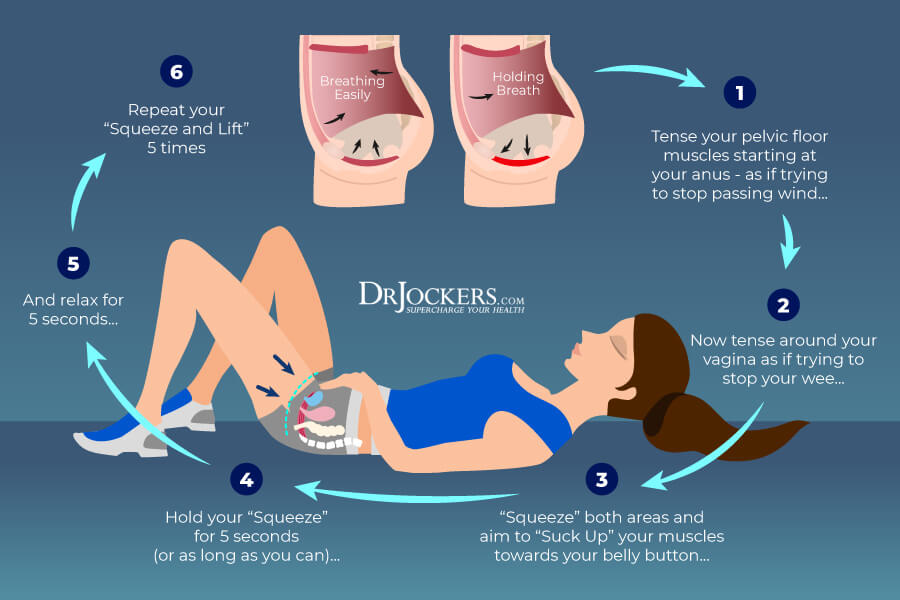
Pelvic Floor Rehab
Pelvic floor rehabilitation can be incredibly beneficial for those with interstitial cystitis. Working with a physical therapist can help you not only to stretch and release tight pelvic floor muscles but strengthen weak pelvic floor muscles to improve function. A 2012 randomized multicenter clinical trial published in the Journal of Urology has found that only 10 myofascial physical therapy sessions have helped 59 percent of participants with interstitial cystitis and improved their pain levels, sense of urgency, and frequency of urination (14).
Physical therapy can improve function, reduce muscle spasms, and improve a sense of control of the pelvic floor muscles and bladder function. According to a 2006 study published in Pain Medicine, internal and external neuromodulation can also help to improve the symptoms of interstitial cystitis, pelvic pain, pelvic floor dysfunction, sexual dysfunction, urinary retention, and lower bowel problems (15).
Reduce Stress & Improve Sleep
According to a 2002 review published in the Reviews in Urology, interstitial cystitis is a chronic illness that may affect or be triggered by someone’s psychological adjustment (16). Stress reduction and stress management are very important for helping with one’s ability to cope with illness and reduce depression and emotional distress associated with the condition. From a 2011 study published in Therapeutic Advances in Urology, we also know that inflammation plays a role in the condition and inflammation can be worsened by chronic stress and poor sleep (17).
Meditation, progressive muscle relaxation, deep breathing exercises, self-hypnosis, biofeedback, yoga, journaling, time in nature, exercise, regular ‘me-time’, and spending time with supportive people can help to reduce stress.
To improve your sleep, I recommend that you go to sleep and wake up around the same time every day, avoid stress, food, alcohol, caffeine, and electronics close to bedtime, and develop a calming evening routine that works for you. Healing baths, herbal teas, journaling, reading, stretching, and prayer are all helpful practices that support relaxation and sleep.

Interstitial Cystitis Anti-Inflammatory Diet
According to a 2011 study published in Therapeutic Advances in Urology, inflammation plays a role in interstitial cystitis (17). This inflammation may be triggered by an inflammatory diet. According to a 2008 study published in Female Urology, most patients with interstitial cystitis experienced increased symptoms because of certain foods (18).
A 1993 survey published in the Journal of Urology has found that coffee, tea, and spicy foods can be triggering (19). The US Department of Health and Human Services – National Institute of Diabetes and Digestive and Kidney Disease recommends avoiding coffee, soda, alcohol, caffeinated drinks, citrus juices and drinks, chocolate, hot and spicy foods, MSG, highly acidic foods, tomatoes, and artificial sweeteners as they may trigger symptoms (20).
Avoid refined sugar, refined oils, highly processed foods, artificial ingredients, deep-fried foods, and junk food. Eat an anti-inflammatory whole foods diet high in antioxidants by loading up on greens, vegetables, herbs, spices, sprouts, fermented foods, low-glycemic index fruits, nuts and seeds, healthy fats, such as coconut oil, avocados, organic butter and ghee, and clean protein, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild boar. Additionally, follow the recommendations outlined in the next three sections: reduce sugar, grains, bad fats, acidic foods, and arylalkylamine-containing foods.
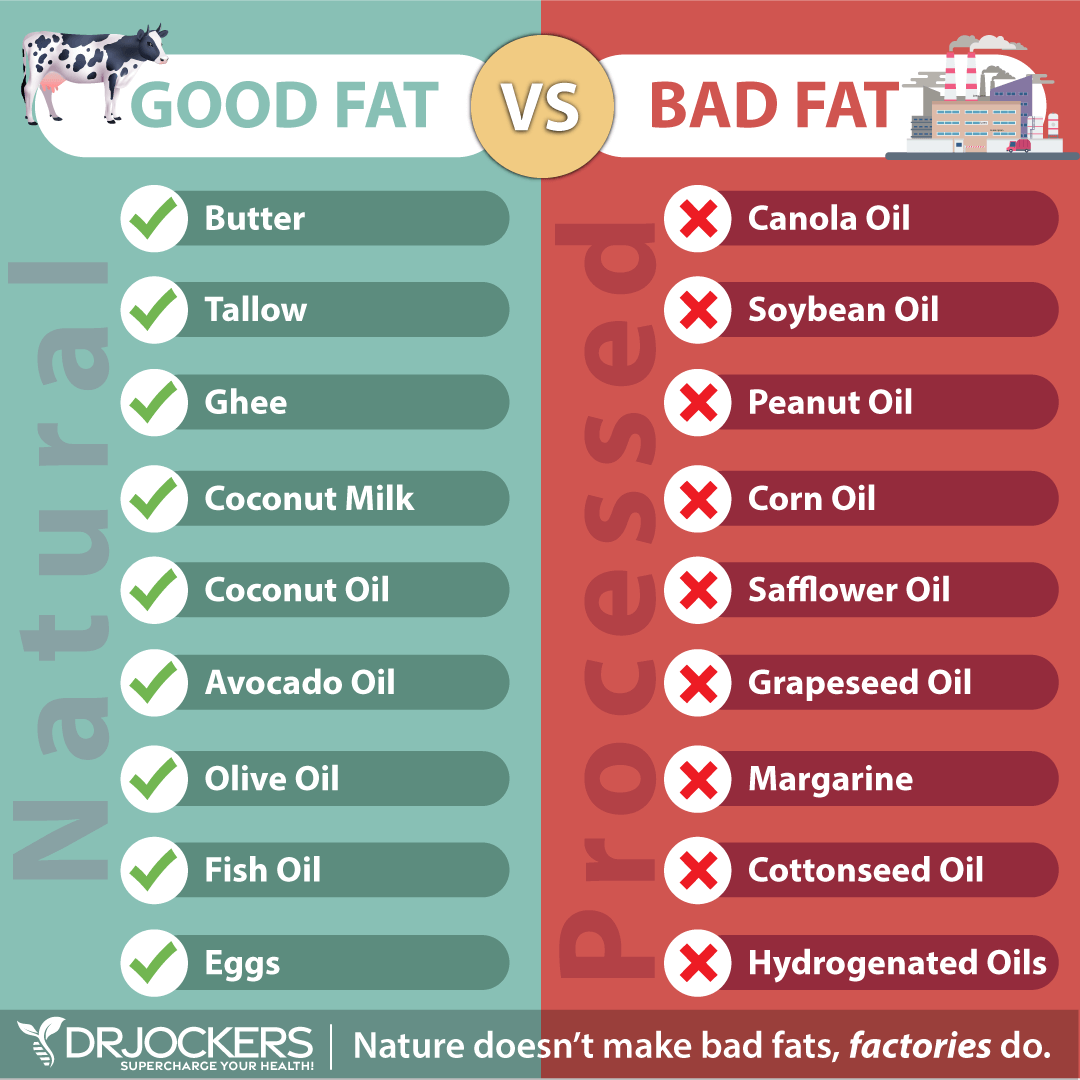
Reduce Sugar, Grains and Bad Fats
We know from research that interstitial cystitis is connected to inflammation and may be triggered by certain foods (17, 18). Sugar and bad fats can increase inflammation and trigger symptoms. I recommend that you remove refined sugar and grains from your diet
Reduce your overall carb intake and focus on a limited amount of low-glycemic index fruits and sweet vegetables, such as sweet potatoes, beets, carrots, and bell peppers instead. Remove refined oils, such as canola, corn, safflower, sunflower, and soybean oils, and margarine from your diet, including any deep-fried or processed foods using these oils.
Load up on healthy fats instead. Avocados, coconut oil, and coconut butter are great sources of healthy fats, so are grass-fed butter and ghee. Extra-virgin olive oil, coconut oil, butter, and lard are great oils and fats for cooking. Coconut oils, extra-virgin olive oil, avocado oil, and flaxseed oil are great for salad dressings.

Reduce Intake of Acidic Foods
Acidic foods can also be triggering for interstitial cystitis and avoiding them is also recommended by the US Department of Health and Human Services – National Institute of Diabetes and Digestive and Kidney Disease (17, 18, 20).
I recommend that you reduce your intake of acidic foods such as alcohol, apple juice, red and green apples, apricots, cantaloupe, carbonated drinks, chili/spicy foods, citrus fruits, coffee, cranberries, grapes, guava, lemon juice, nectarines, peaches, pineapple, plums, strawberries, tea, tomatoes, and vinegar.

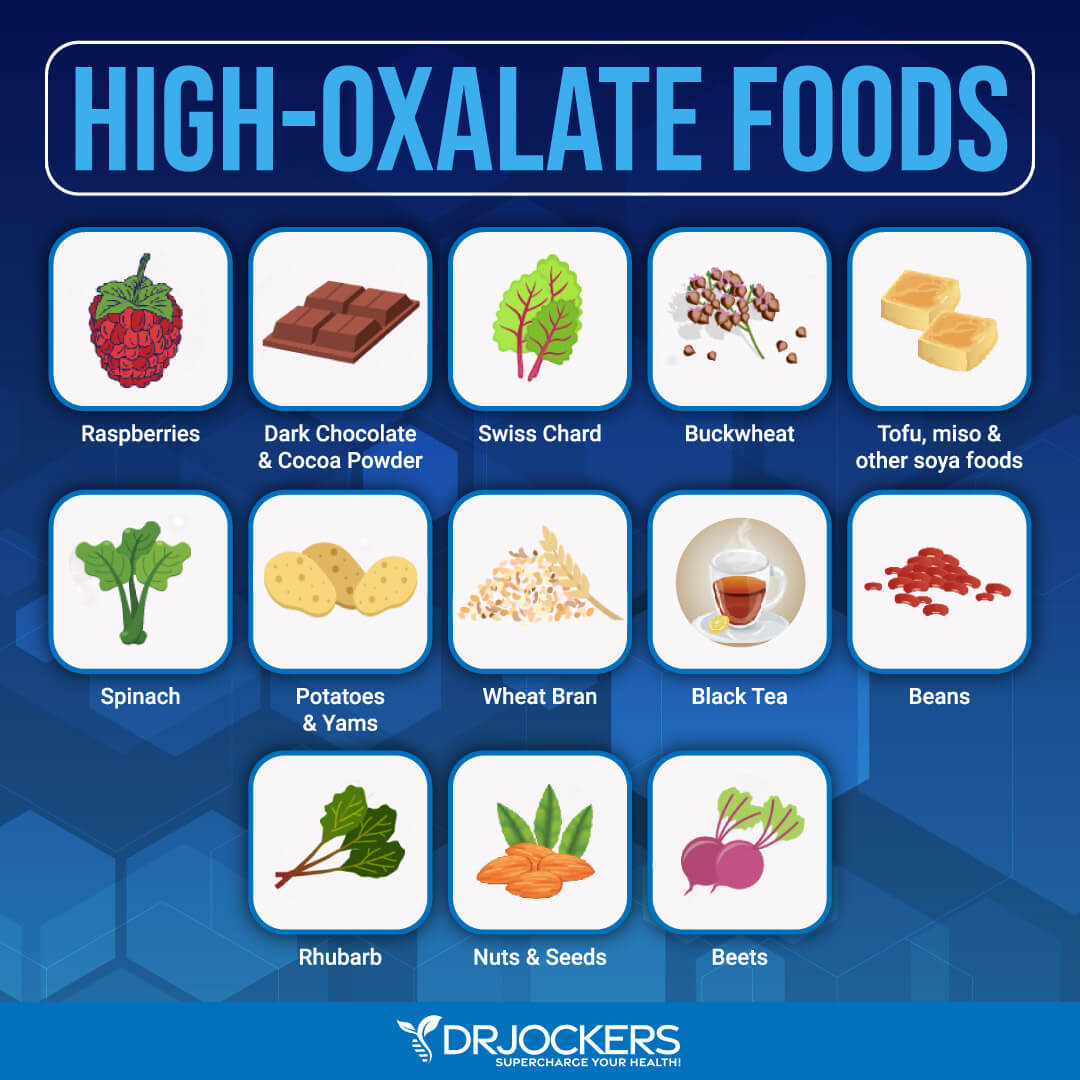
Reduce Intake of Oxalates and Arylalkylamines
Oxalates are naturally occurring molecules that are found in both humans and plants. In plants, oxalate helps to get rid of extra calcium. This also makes some plant foods high in oxalates. The problem is that too much oxalate in their diet can lead to various symptoms and health issues in humans.
Oxalates from certain plant foods travel through your intestinal tracts. They bind with magnesium, calcium, and potassium, which can lead to a build-up of minerals that needs to leave through urine and bowel movements.
No wonder that too many oxalates can lead to urinary issues, bladder pain, and kidney stones. According to a 1997 study published in the Amerian Journal of Obstetrics and Gynecology, excess oxalates, oxalate excretion can result in vulvar pain syndrome or vulvodynia which is often present alongside interstitial cystitis (25).

To reduce your oxalate levels, I recommend removing high-oxalate foods. High-oxalate foods include beets, spinach, celery, leeks, Swiss chards, potatoes, sweet potatoes, rhubarb, okra, figs, kiwis, berries, almonds, cashews, soy, soy products wheat germ, buckwheat, bran flakes, plantains, olives, tea, cocoa, cacao, and chocolate.
Arylalkylamines are chemical compounds made up of monoamine neurotransmitters and also found in some clinically and recreationally used drugs. They include tryptophan, tyrosine, tyramine, and phenylalanine. According to a 2015 study published in Translational Andrology and Urology, arylalkylamine-containing foods can be triggering for interstitial cystitis, and removing them should be part of an interstitial cystitis diet (21).
Arylalkylamine-containing foods that you should avoid include aspartame, banana, beer, brewer’s yeast, canned figs, champagne, cheeses, chicken liver, chocolate, corned beef, cranberries, fava beans, lima beans, marmite, mayonnaise, nuts, onions, pickled herring, pineapple, prunes, raisins, rye bread, saccharin, sour cream, soy sauce, wine, and yogurt.
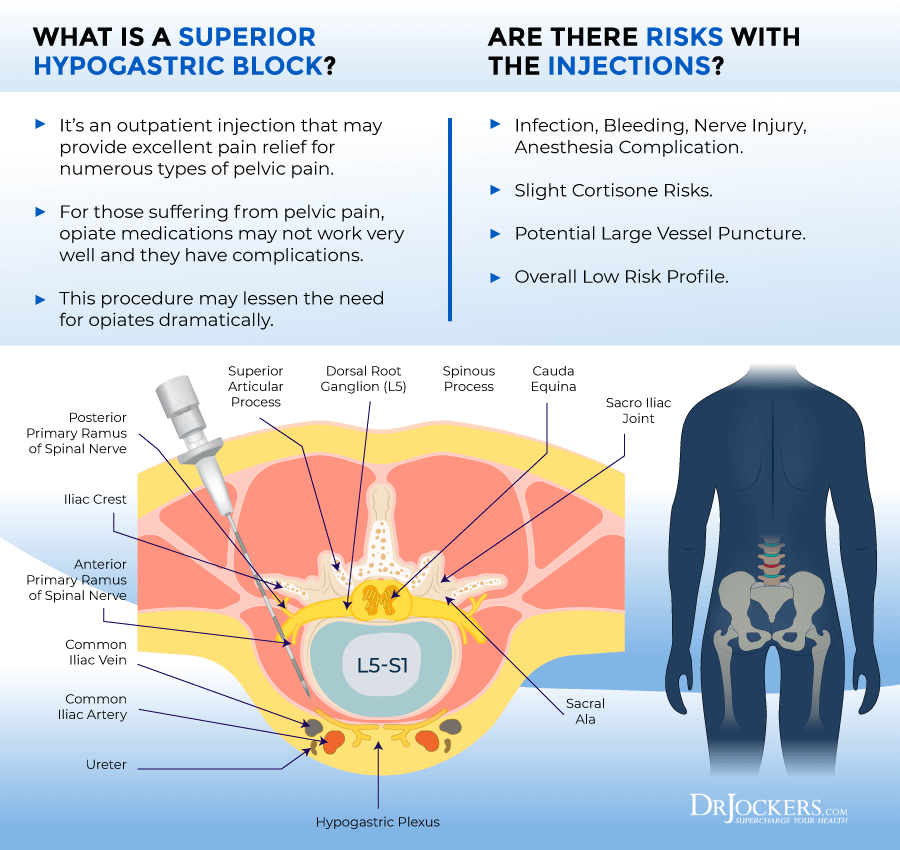
Consider a Hypogastric Plexus Block
Hypogastric plexus blocks are injections that are used for interstitial cystitis and pelvic pain to relieve pain. According to a 2015 study published in the Journal of Japan Society of Pain Physicians, hypogastric plexus block may help to successfully treat interstitial cystitis (22).
During the procedure, you’d ask to lie in prone position pillows under your lower belly while x-rays are taken of your L5-S1 with a fluoroscope. You would be mildly sedated to feel calm. After cleansing and numbing the area, your doctors would guide a needle to the superior hypogastric plexus with fluoroscopy. Alcohol or phenol is also used to kill the nerves responsible for the pain. Relief may last for weeks, months, or years, depending on your case.
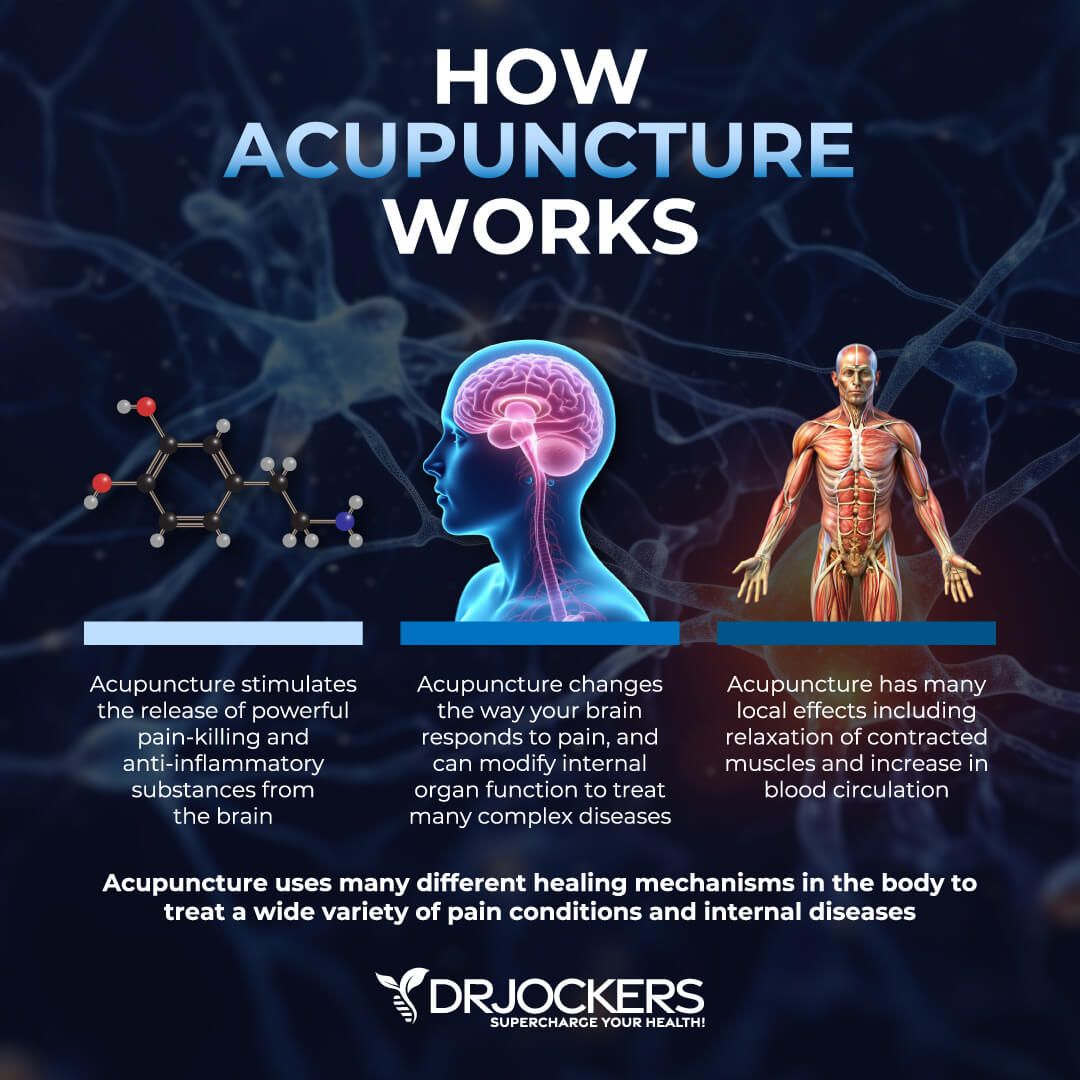
Acupuncture
Acupuncture is a form of alternative medicine that’s part of traditional Chinese medicine and works with your body’s so-called meridians and acupoints. It helps to stimulate and rebalance energy flow in the body and improve your overall health as a result.
According to a 2002 review published in the Reviews in Urology, acupuncture may help to improve interstitial cystitis (16). Researchers have found the only 6 to 8 weeks of acupuncture twice a week helped to relieve symptoms of interstitial cystitis in participants, in most cases by over 50 percent.
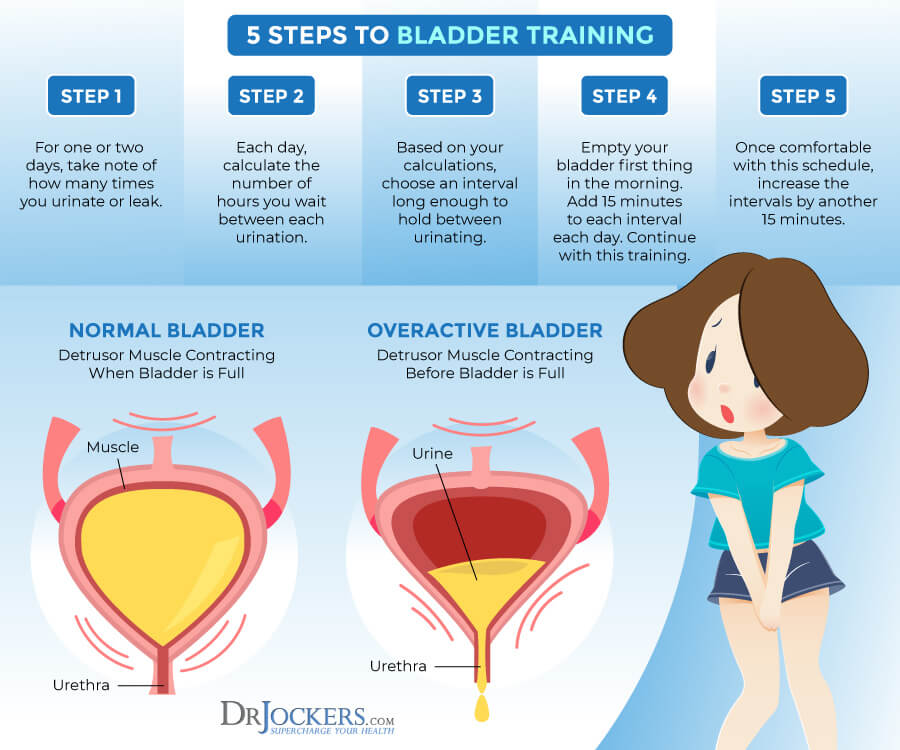
Bladder Training and Urinary Alkalization
The same 2002 review published in the Reviews in Urology has found that bladder training may also support patients of interstitial cystitis (16). Bladder training involves stopping the urge to urinate to reduce frequency and urgency. Researchers found that only 15 to 30 minutes of bladder training for 3 to 4 weeks helped to reduce the frequency, nocturia, and urgency in 71 percent of participants.
They also found the pelvic floor muscle exercises combined with relaxation tapes lead to an improvement in 98 percent of patients. Additionally, to bladder training, a 2013 study published in the International Journal of Urology has found that urinary alkalization can improve pain and sleep in interstitial cystitis (23).
Biofeedback and Electrical Stimulation
The same 2002 review published in the Reviews in Urology has found that biofeedback and electrical stimulation can improve symptoms of interstitial cystitis (16). Researchers found that only 6 weeks of biofeedback and electrical stimulus can improve interstitial cystitis when used in combination with physical therapy or a home exercise program for pelvic floor function.
It can improve pain, voiding and bowel, function, sexual function, and quality of life.
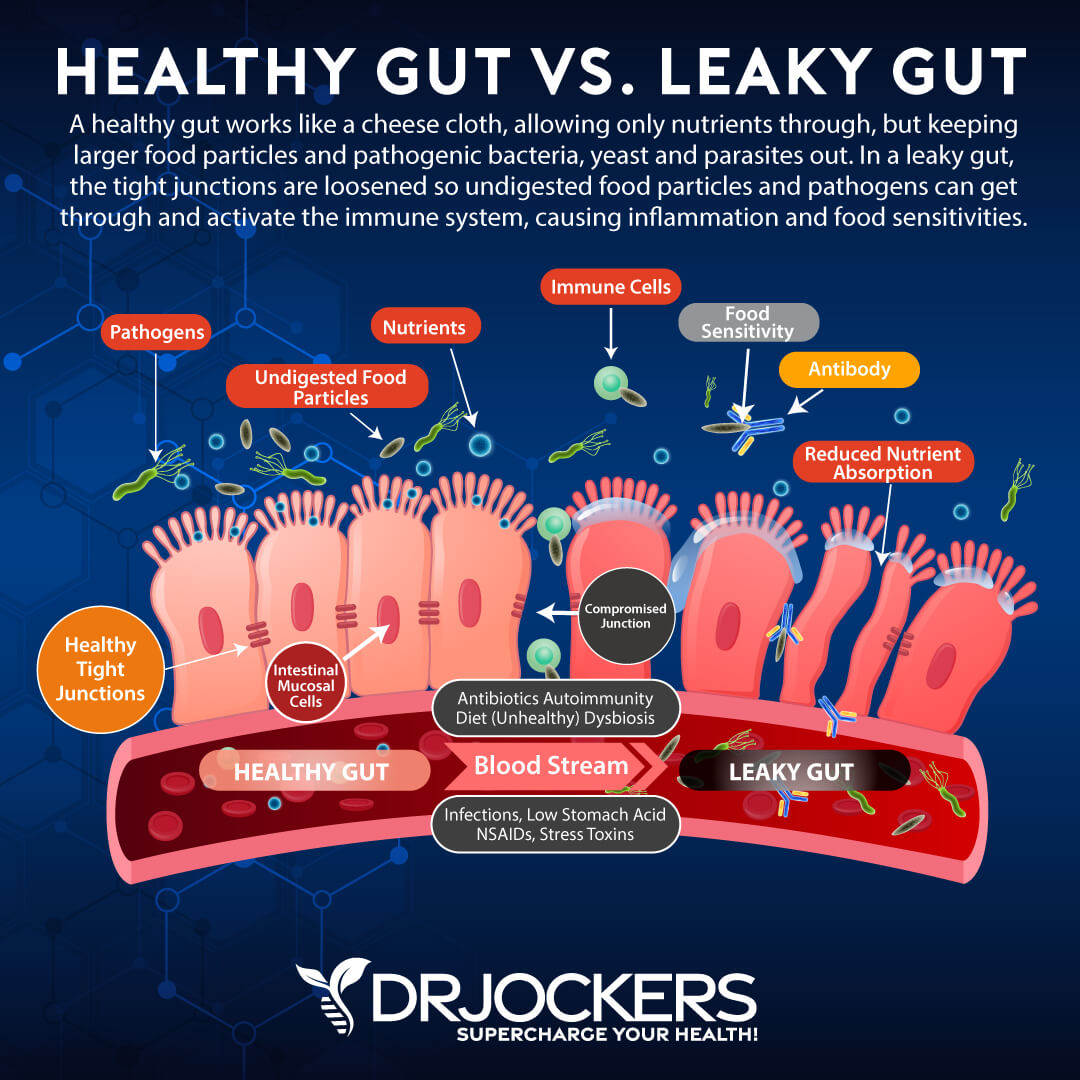
Support Gut and Microbiome Health
According to a 2019 pilot cross-sectional study published in Frontiers in Cellular and Infection Microbiology, vaginal and urinary microbiome can be linked to interstitial cystitis (24). However, your vaginal and urinary microbiome health is also affected by your gut microbiome.
Gut microbiome imbalance and gut health issues can increase inflammation, pain, and chronic health issues. We also know from a 2007 study published in Nature Clinical Practice Urology that there may be a connection between autoimmune diseases and interstitial cystitis, and autoimmune diseases are closely connected to gut health and gut microbiome balance (8).
To improve your gut microbiome, it is important that you follow an anti-inflammatory diet and lead a healthy lifestyle. Eating prebiotic-rich foods, such as Jerusalem artichokes, leeks, asparagus, and dandelion greens, and probiotic-rich fermented foods, such as sauerkraut, kimchi, kombucha, and kefir can be helpful.
Additionally, I recommend a daily probiotic supplement. You may also want to work with a functional health practitioner and get some gut stool testing done to identify and address potential underlying gut infections.
Use Nutraceuticals
Nutraceuticals are products that are derived from foods and can improve your health. The same 2002 review published in the Reviews in Urology has found that nutraceutical improves symptoms of interstitial cystitis, including bladder irritation and pain (16).
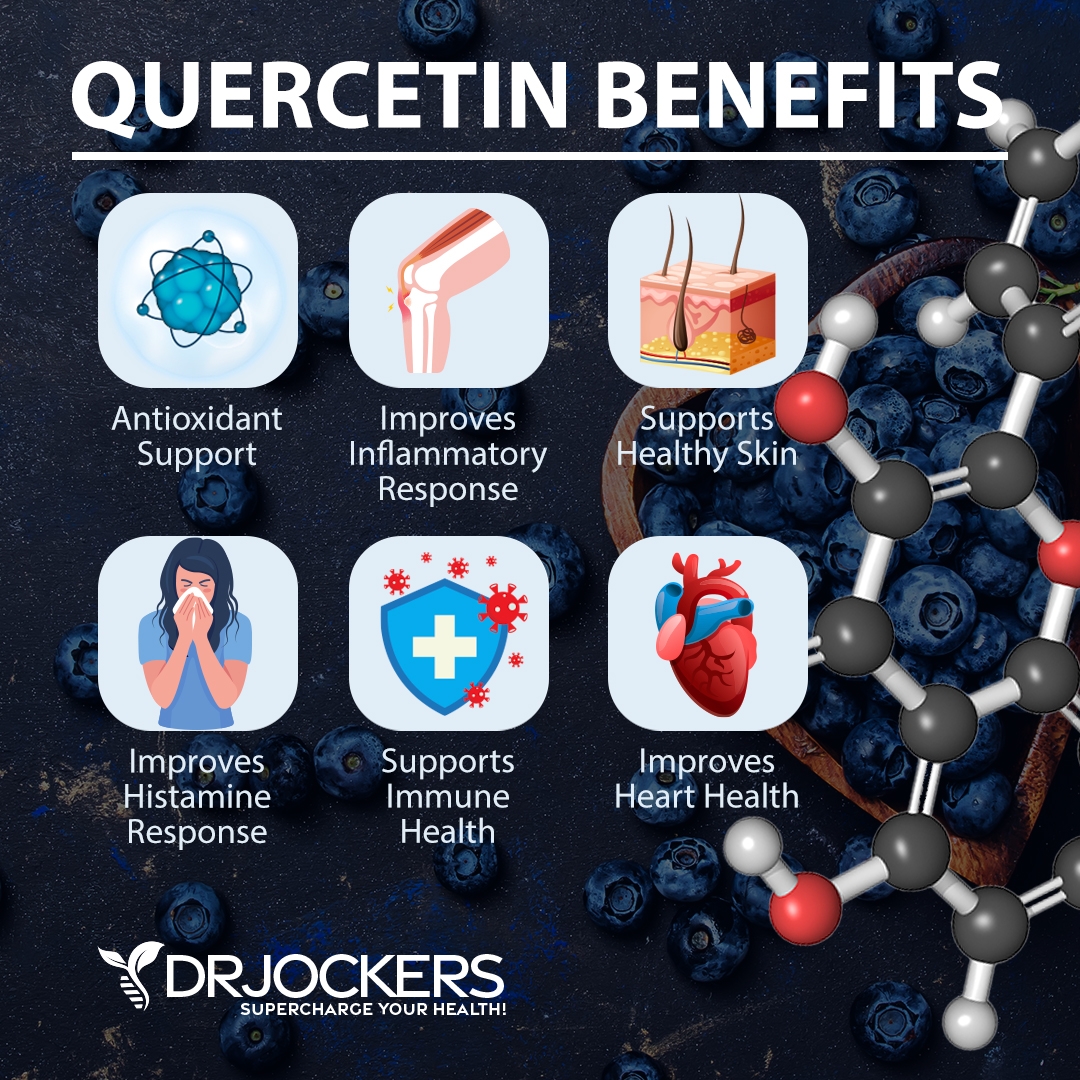
Quercetin and Bioflavonoids
The review has found that the bioflavonoid quercetin can inhibit histamine release, lower inflammation, and offer antioxidant benefits (16). Researchers found that 500 mg of quercetin taken twice a day for 4 weeks was able to significantly decrease pain and symptoms.
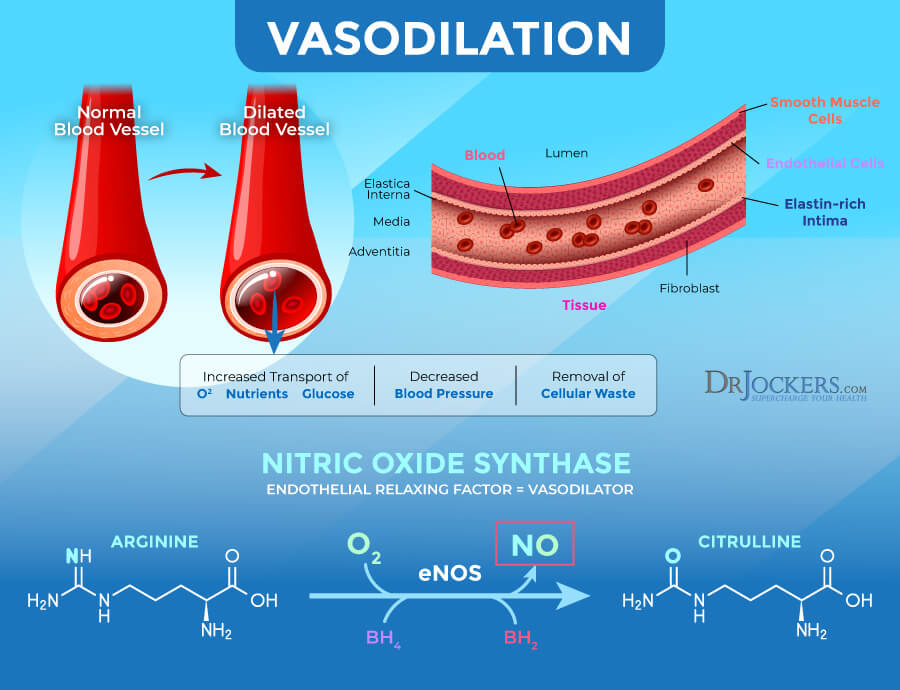
L-Arginine
The review explained that L-arginine is an amino acid that can help nitric oxide (NO) production (16). NO is a precursor of nitric oxide synthase (NOS), both of which helps to relax muscles, support immune health, offer antibacterial benefits, and support hormone release.
Researchers found that 1.5 g of L-arginine a day taken for 6 months improved pain, frequency, nocturia, and urinary issues. The thought on this is that the increased NO helps improve blood flow and healing of the bladder wall.
Mucopolysaccharides
The review has found that mucopolysaccharides, including hyaluronic acid, chondroitin sulfate, aloe vera can help patients with interstitial cystitis (16). Researchers found that they can reduce pain and urgency associated with the condition.
Researchers found that 40 mg of hyaluronic acid over 12 weeks, 80 mg of chondroitin sulfate over 4 weeks, or 600 mg of aloe vera capsule for 3 months all made an improvement in symptoms.

Calcium Glycerophosphate
According to the review, calcium glycerophosphate can help to reduce symptoms of interstitial cystitis in participants who ingested foods that trigger symptoms of the conditions, such as coffee or chocolate (16).
Using a food diary to track symptoms, researchers have found the 0.66 gm of calcium glycerophosphate has helped to improve symptoms and reduce flairs over a 4-week period.
Magnesium-Potassium Citrate
According to a 2013 study published in the International Journal of Urology, urine alkalization therapy with citrates improved hypersensitive bladder syndromes (26). Researchers looked at the urinary frequency, urine pH, and pain levels at each voiding of 76 patients and notice a decrease in micturitions per day, increase in urine pH, and decrease in pain.
Results suggest that magnesium-potassium citrate may help to reduce the symptoms of interstitial cystitis and other bladder or urinary issues.
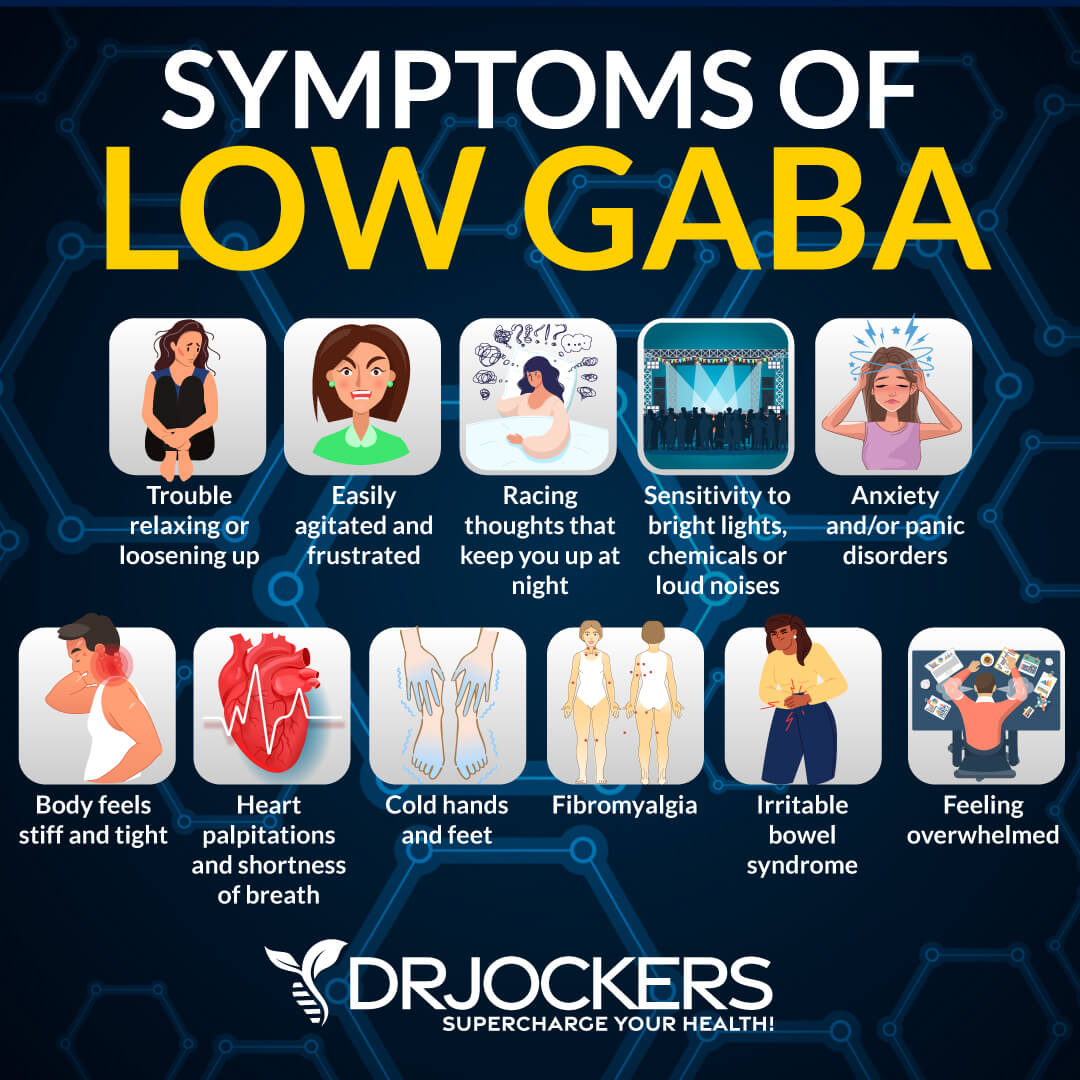
GABA
Gamma-aminobutyric acid (GABA) is an amino acid that serves as a neurotransmitter in your brain. Due to the GABA receptors in the bladder, GABA can have a pain-reducing effect in interstitial cystitis.
According to a 2015 study published in the British Journal of Pharmacology, the GABA receptor may help to improve overactive bladder, bladder pain, as well as pain in gastrointestinal issues (27).
Final Thoughts
Interstitial cystitis is a painful chronic condition that is characterized by pelvic pain, bladder discomforts, burning, stinging, an urgency to urinate, and painful urination. While there is no known cure for interstitial cystitis, there are several natural strategies that can improve the condition. Follow my top natural strategies for interstitial cystitis to improve your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. We do offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!