 Pollen Allergies: Symptoms & Natural Support Strategies
Pollen Allergies: Symptoms & Natural Support Strategies
Spring is here. If you are one of the millions dealing with pollen allergies, you know that it’s also allergy season. You may love the sunshine and the beauty of the flowering trees, but chances are, you could live without sneezing, runny nose, coughing, watery eyes, and other symptoms of pollen allergies.
I have good news for you. You don’t have to suffer from symptoms of pollen allergies this season. You can reduce your risk and symptoms of pollen allergies using some simple natural solutions.
In this article, I will explain what pollen allergies are, and what are their symptoms. You will understand how your immune system reacts to pollen and why you may develop pollen allergies. I will share my favorite natural support strategies to improve your pollen allergies this season.
What Are Pollen Allergies
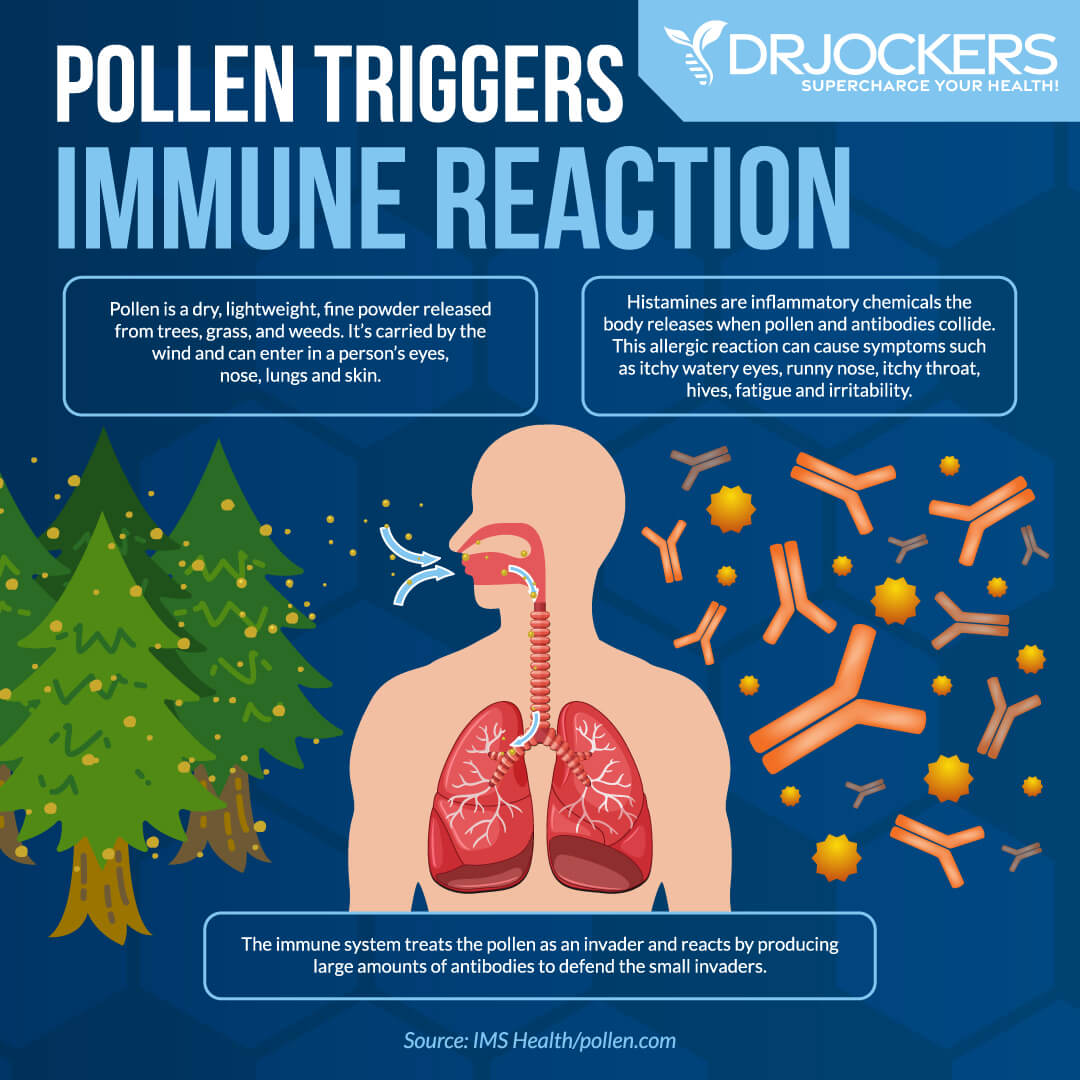
Pollen allergies are caused by pollen. Pollens are tiny, egg-shaped powdery grains that are released from flowering plants. Pollens are carried by the wind, bees, and other insects from one plant to another to serve their essential reproductive role. This is all amazing for our plants, however, when pollens are flying around the air, they can land in your eyes, nose, lungs, and skin. If you have pollen allergies, specific pollen can lead to a variety of allergic reactions (1).
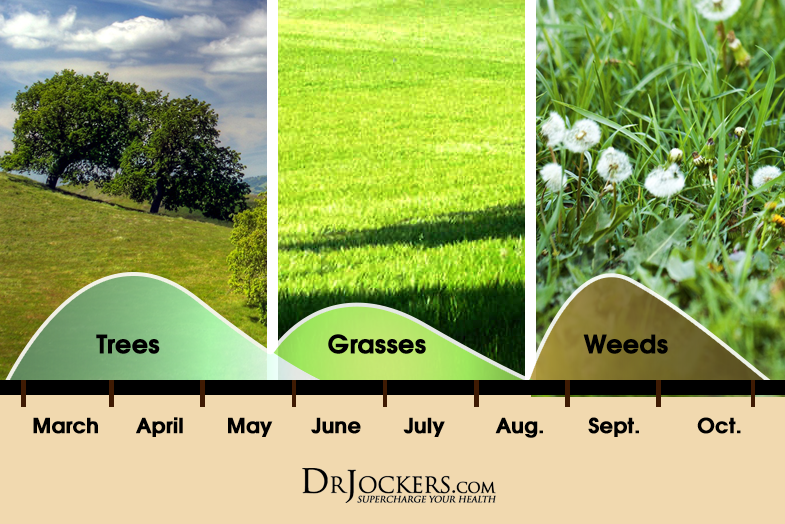
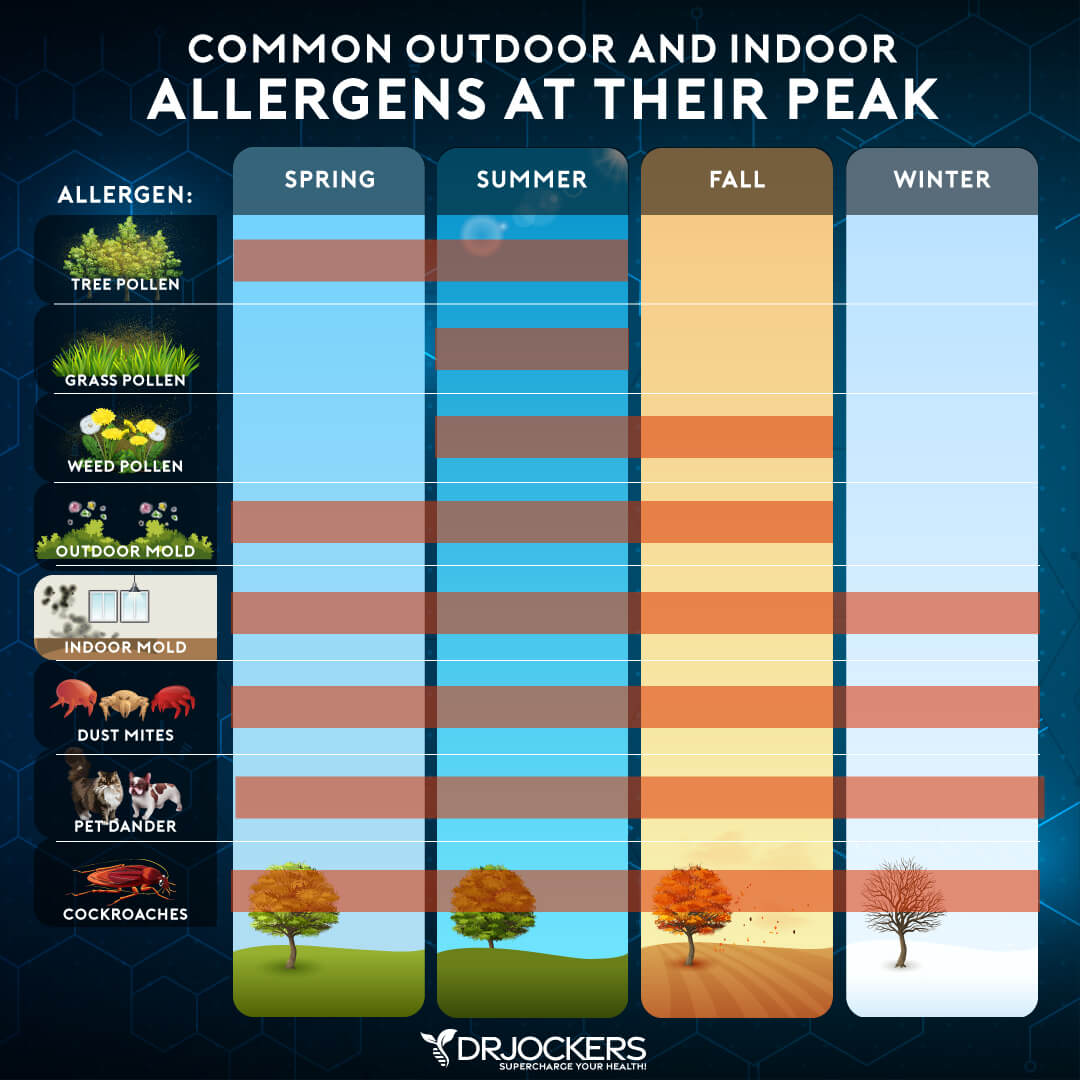
Since different plants flower at different times, depending on the type of pollen you are allergic to, you may be dealing with allergies during only a certain time of the spring or summer. Those with various pollen allergies may be experiencing symptoms throughout the entire spring and summer.
The Timing of Pollen Allergies
Spring allergies tend to be caused by trees, most commonly by oak, olive, elm, birch, ash, hickory, poplar, sycamore, maple, cypress, and walnut trees. Depending on where you live, your spring allergies may already start winter time in the Southern region where trees may bloom earlier. In the Northern part of the country, you may not notice spring allergies until May or June.
Late spring or early summer pollen allergies are typically caused by grass pollen. As with spring allergies, your allergies may be dictated by where you live. Northern grasses are common in colder climates and include timothy, rye, orchard, sweet vernal, red top, and bluegrass. Southern grasses are present in warmer climates, with Bermuda grass being the major grass in this category.
Late summer and fall pollen allergies are usually caused by weed pollen. Again, these allergies may depend on your location. The most common weed pollen allergies in North America include ragweed, sagebrush, pigweed, tumbleweed (Russian thistle), and cocklebur. In certain areas of the world, some trees can pollinate in the fall as well.
Not All Seasonal Allergies Are Pollen Allergies
If you move across the country or travel to other states or countries, you may notice some allergies disappearing or new allergies appearing depending on the season and the type of plants and pollens in the area. You may learn more about seasonal allergies in this article.
Pollen can travel long distances and pollen levels may differ in various areas, time of the year, and daytime. They tend to be the highest between 5 am and 10 am or morning to mid-morning. Remember, some allergies are not caused by pollen, but by indoor molds, dust mites, pet dander, or cockroaches, so it is very important you understand the cause of your allergies in order to prevent them.
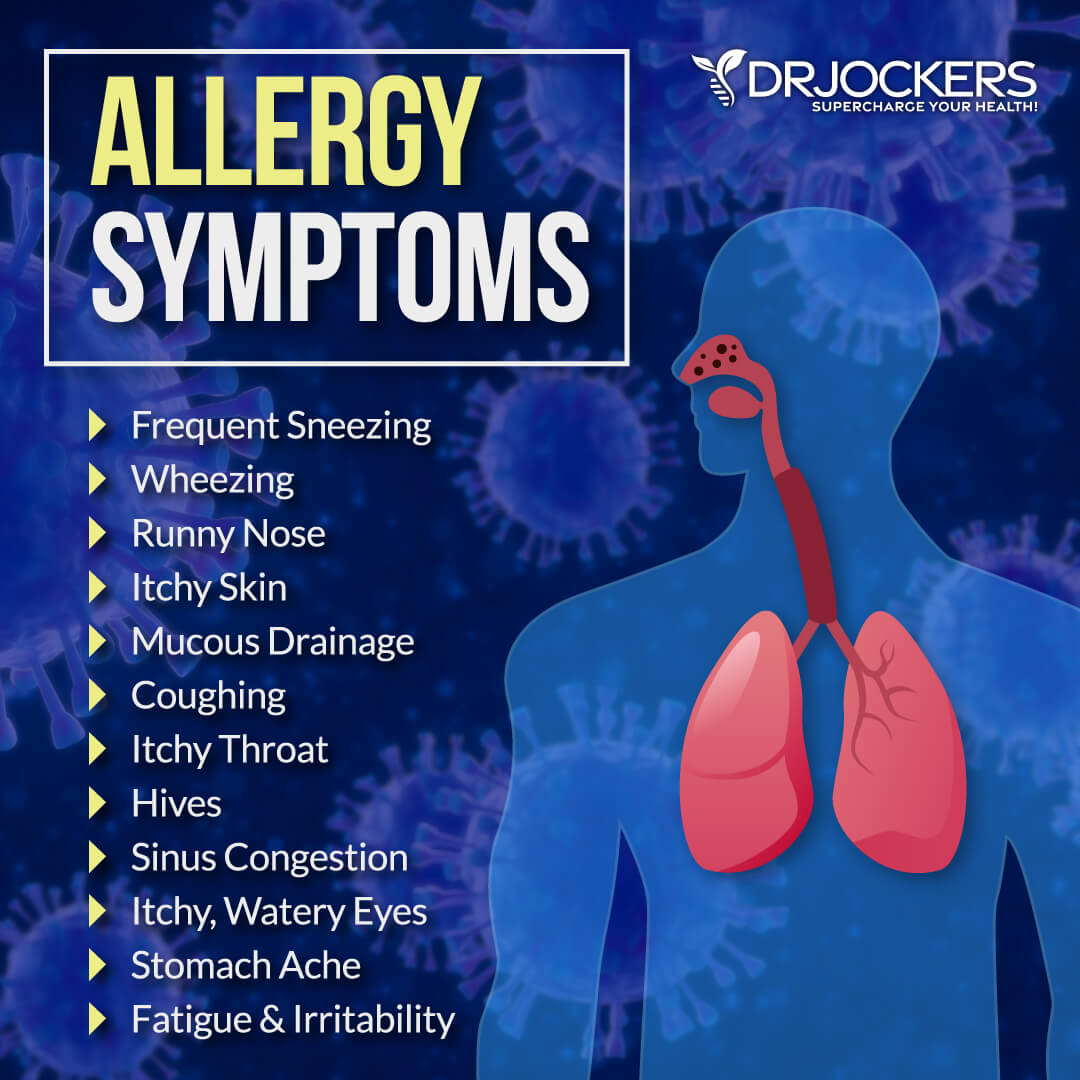
Symptoms of Pollen Allergies
While some of the most common issues pollen allergies cause are sneezing, runny nose, and coughing, they may lead to a variety of other symptoms. Symptoms of pollen allergies may include:
- Sneezing
- Runny nose
- Mucous drainage
- Sinus congestion
- Coughing
- Itchy or watery eyes
- Red eyes
- Itchy throat
- Wheezing
- Hives
- Stomach aches
- Fatigue
- Irritability
- Itchy skin
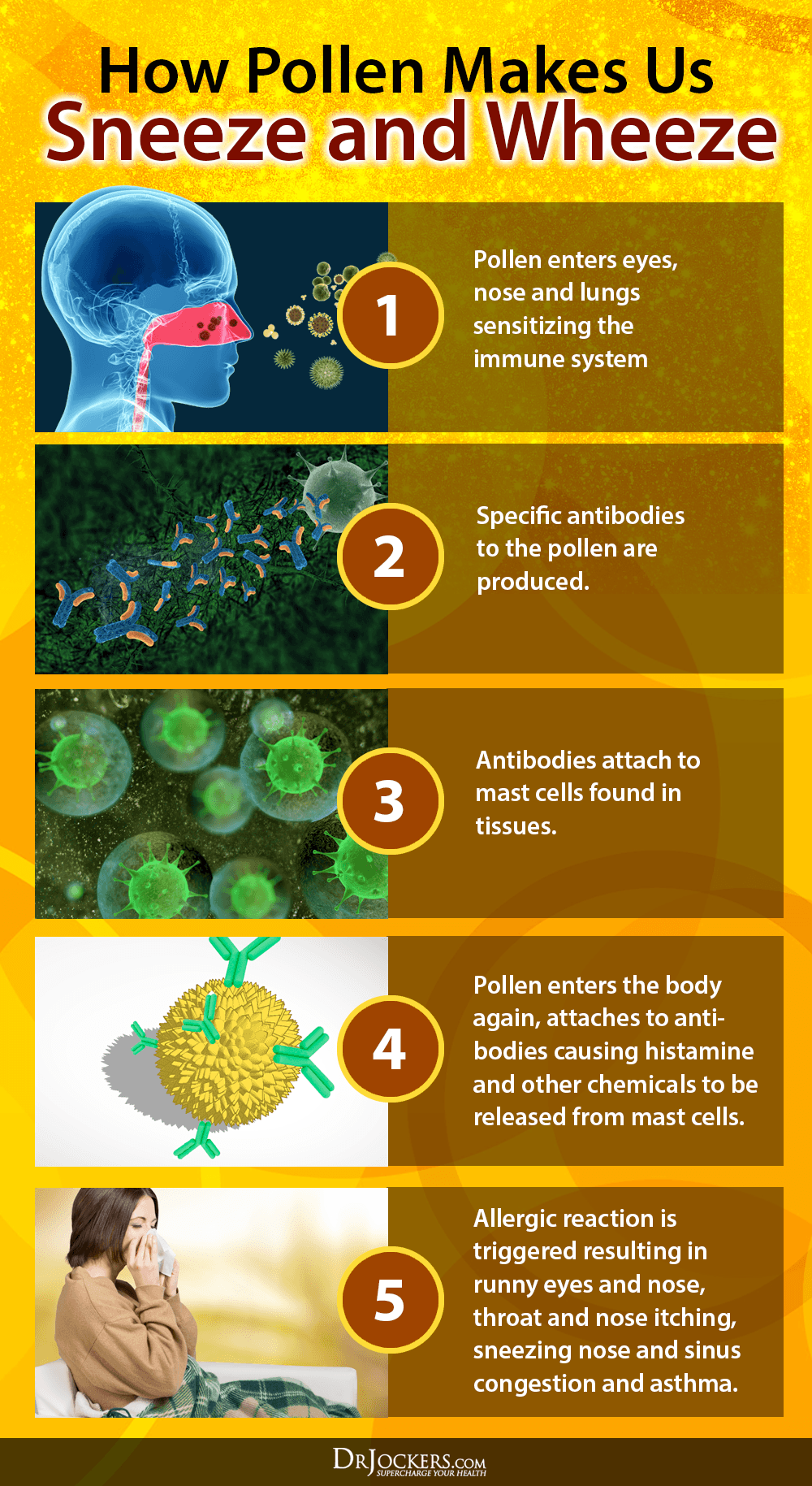
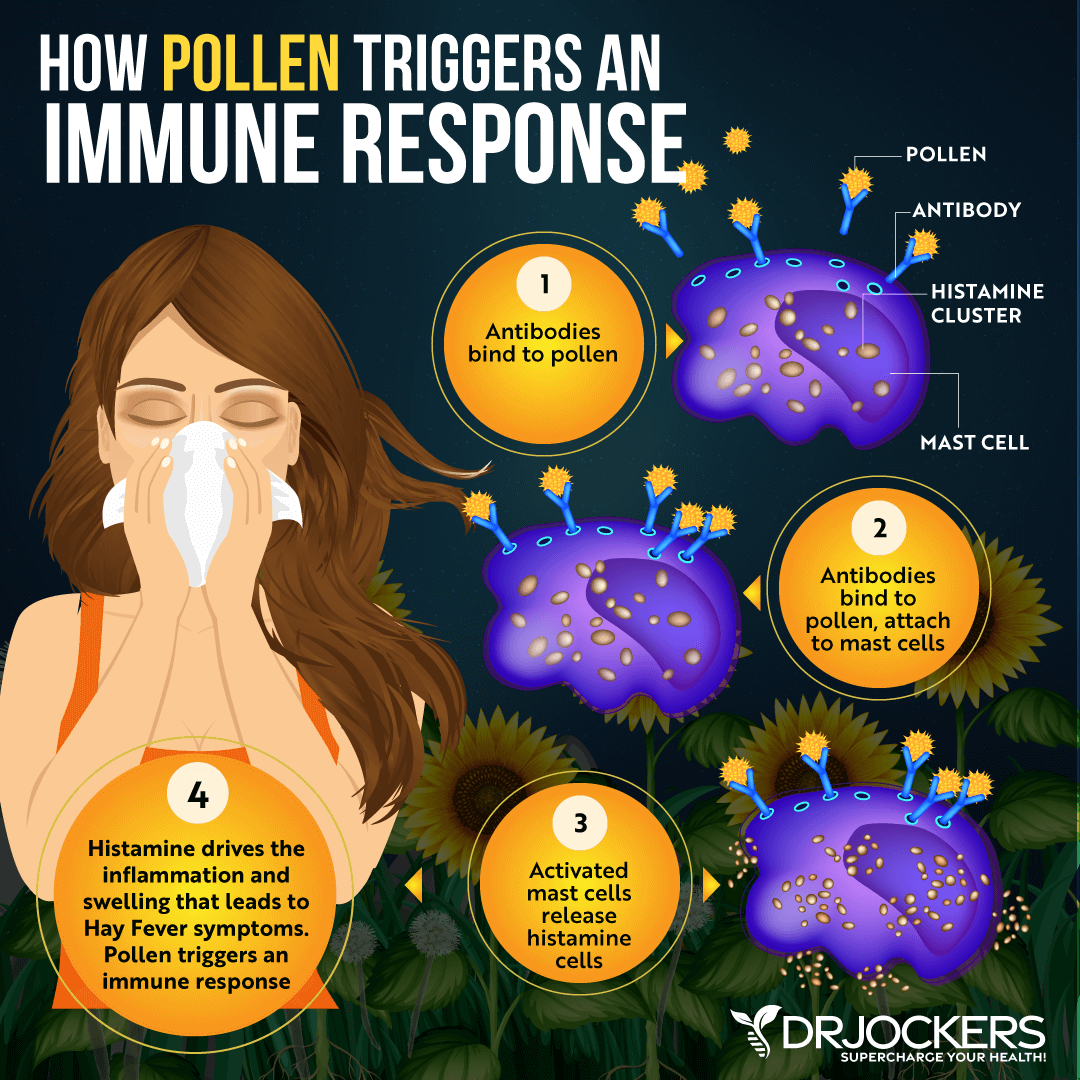
How The Immune System Reacts to Pollen Allergies
Your pollen allergies have everything to do with your immune system. When your immune system is mal coordinated, it may result in pollen or other allergies. This can happen from any major bodily stressor that interferes with the healthy function or natural maturity of your immune system.
For example, if you have experienced environmental challenges in early life, your body may not be able to develop a natural immune response to certain pollen or other things which makes you prone to allergic reactions. However, if you experience an immune insult later in life, it may wreak havoc in your immune system, and lead to allergic reactions later in life.
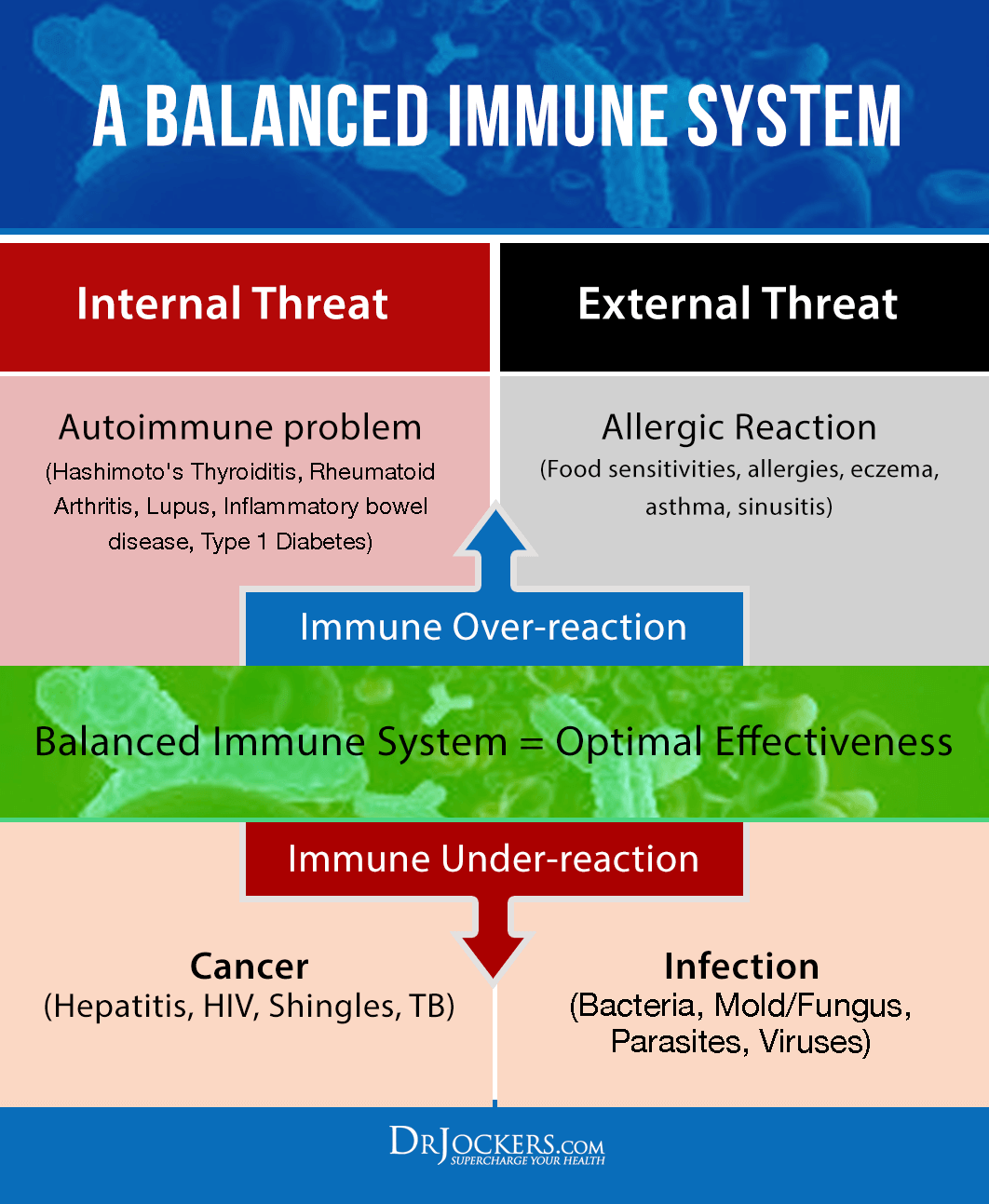
A Balanced Immune Response Is Key
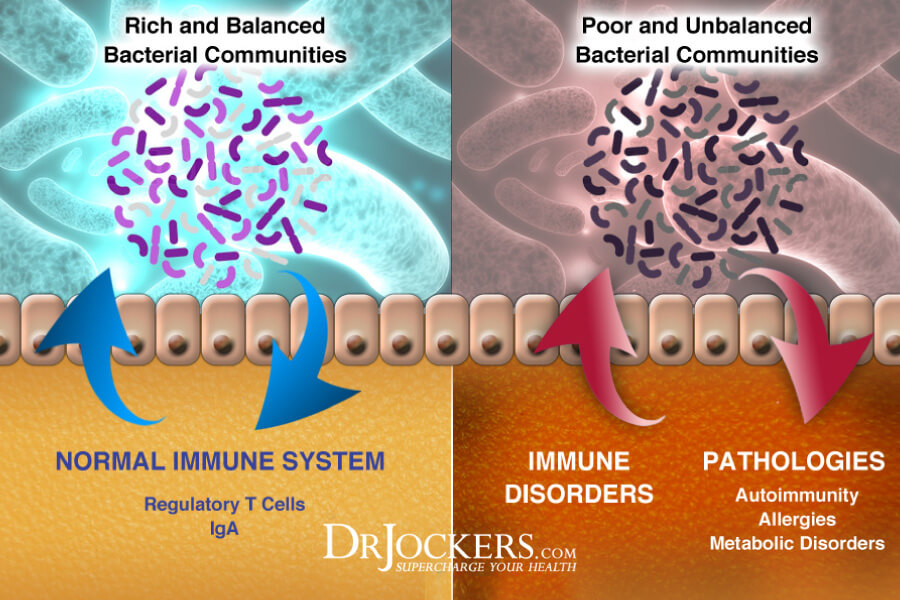
Even though most people don’t connect gut health to allergies, the most common issue that can increase your symptoms or make you prone to allergies is altered and unbalanced gut flora. Your gut microbiome is responsible for 70 percent of your body’s innate immune response and allows your body to differentiate between safe environmental particles, including pollen, weed, and dust, and unsafe environmental particles, including bad bacteria, viruses, and unhealthy yeast.
When your gut flora is altered early in life, it can lead to an immune malcoordination and an oversensitivity to safe environmental particles. This may not only increase your risk of pollen and other seasonal allergies, but also increase your risk of asthma, autoimmune conditions, and chronic inflammation (2, 3, 4, 5, 6, 7).
While many people with pollen allergies have had allergies since childhood or teenage years, it is certainly possible to develop pollen allergies later in life or experience worsened symptoms as you grow older. It is also possible to reduce your symptoms and even eliminate your pollen allergies through proper immune support.
Natural Solutions to Pollen Allergies
If you have been dealing with pollen allergies, I have good news for you. There are many people who have been able to reduce or even eliminate the symptoms of pollen allergies without medication.
Your lifestyle plays an enormous role in the way your immune system acts and responds to the environment. Certain lifestyle practices will help to balance the immune response and dampen allergy like responses. These natural support strategies are not FDA-approved to prevent, mitigate, treat, or cure allergies, however, many people have seen helpful results by following them.
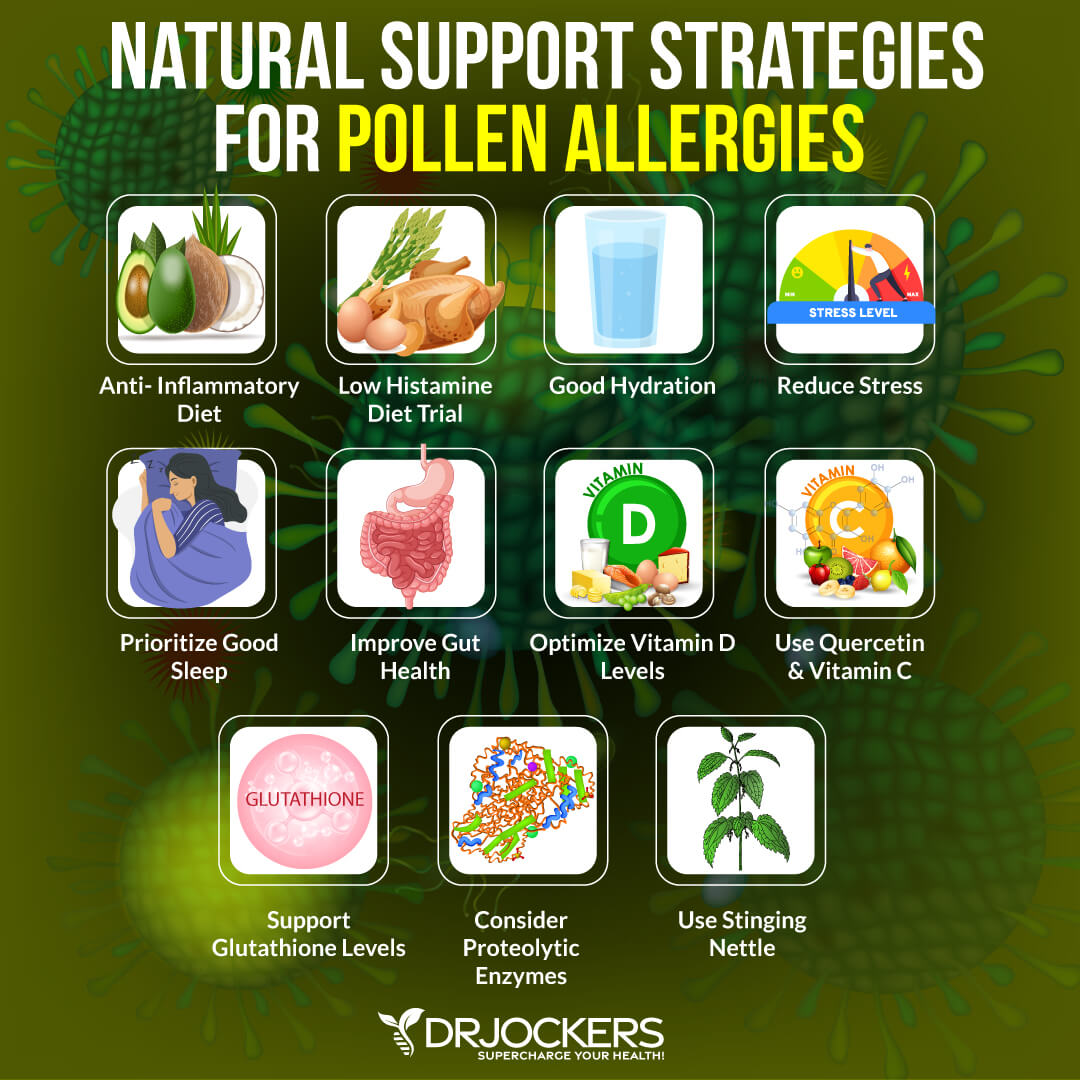
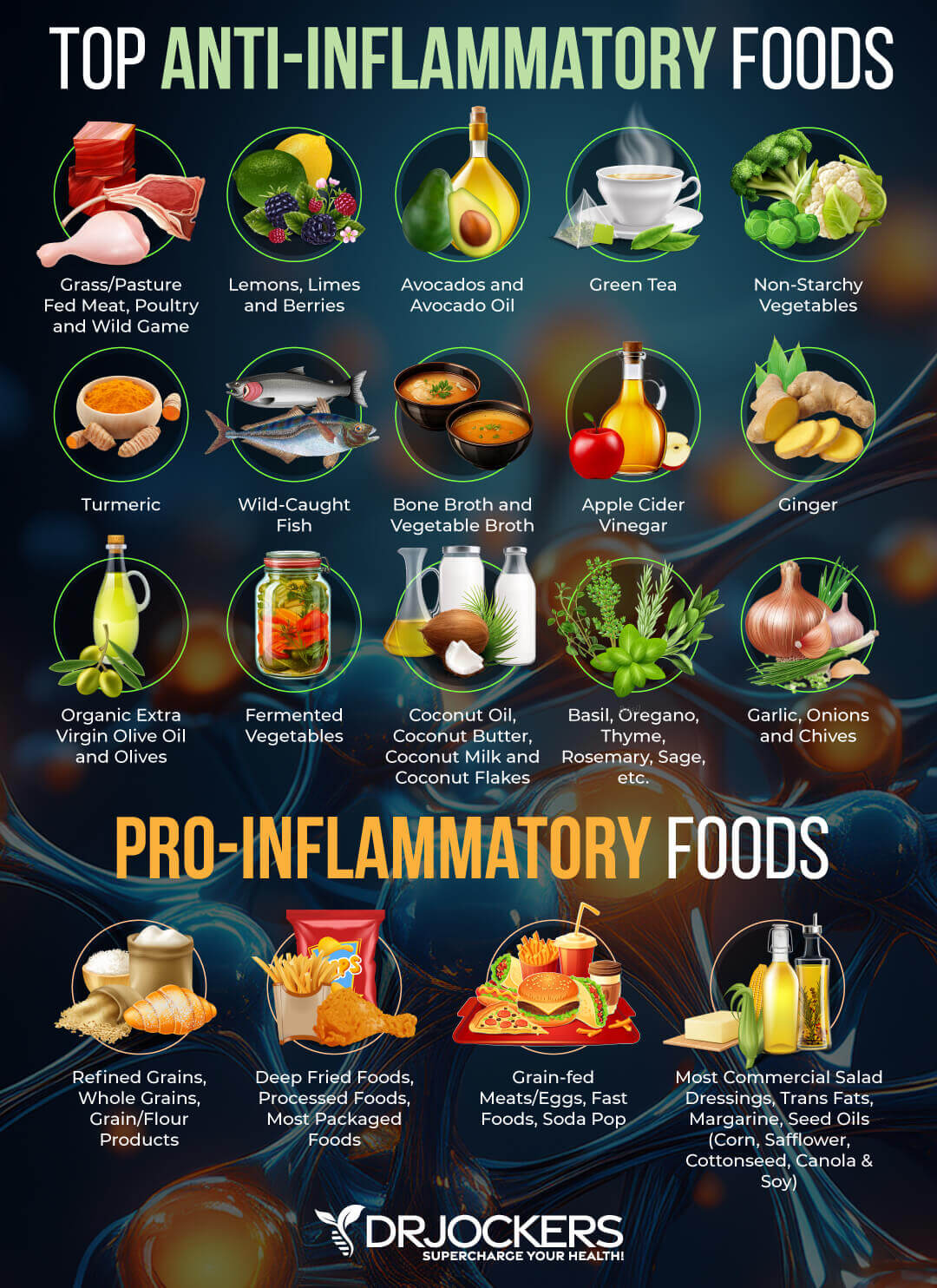
Anti-Inflammatory Diet
You may be wondering what your diet has to do with allergies caused by pollen. The truth is that your diet has to do with everything that happens in your body. Eating an inflammatory diet high in sugar, simple carbs, refined oil, conventional dairy, gluten, processed food, junk food, and artificial ingredients increases inflammation in your body. An inflammatory diet, especially when high in dairy and gluten, may also increase mucus production and sinus issues. An inflammatory diet also compromises your gut flora further increasing your risk and symptoms of pollen allergies (8).
To lower your risk and improve your symptoms of pollen allergies, I recommend a nutrient-dense anti-inflammatory diet. Eliminate inflammatory foods, such as sugar, refined oil, conventional dairy, gluten, conventional animal products, and any processed or junk food.
Eat nutrient-dense anti-inflammatory foods, including leafy greens, such as kale, spinach, collard greens, and chard, vegetables, such as cucumber, celery, and asparagus, low glycemic index fruits, such as lemon, lime, and berries, herbs and spices, such as turmeric, ginger, mint, rosemary, and oregano, healthy fats, such as avocado, coconut oil, extra virgin olive oil, and organic butter or ghee, clean protein, such as pasture-raised beef, free-range poultry and eggs, wild-caught seafood, and fermented foods, such as sauerkraut, kimchi, and kefir.
Consider Low Histamine Foods
Histamine is an important neurotransmitter and immune messenger molecule. It is essential for your body’s healthy functioning. It is involved in processes involving hydrochloric acid secretion for digestion, triaging water reserves to key areas of the body and the inflammatory response, and communicating with your brain. Histamine receptors are found all over your body, including your smooth muscle and endothelial cells, intestines, and central nervous system.
While histamine is essential and plays a very important role in your health, it is important to have enough but not too much histamine. Histamine intolerance means that your body has too much histamine. Too much histamine is never a good thing. In fact, it can lead to a variety of mild to severe symptoms and serious health issues.
Under normal circumstances, your body releases specific enzymes to break down histamine build-up. However, when you have too much histamine, your body won’t be able to keep up and won’t be able to break down all the excess histamine completely.
Histamine intolerance can affect your entire body, including your lungs, gut, brain, heart, and hormones. It can lead to a variety of issues, including digestive problems, sleep disturbances, bladder problems, anxiety, headaches, and skin problems. Pollen and seasonal allergies are some of the signs of histamine intolerance (9, 10, 11, 12, 13, 14).
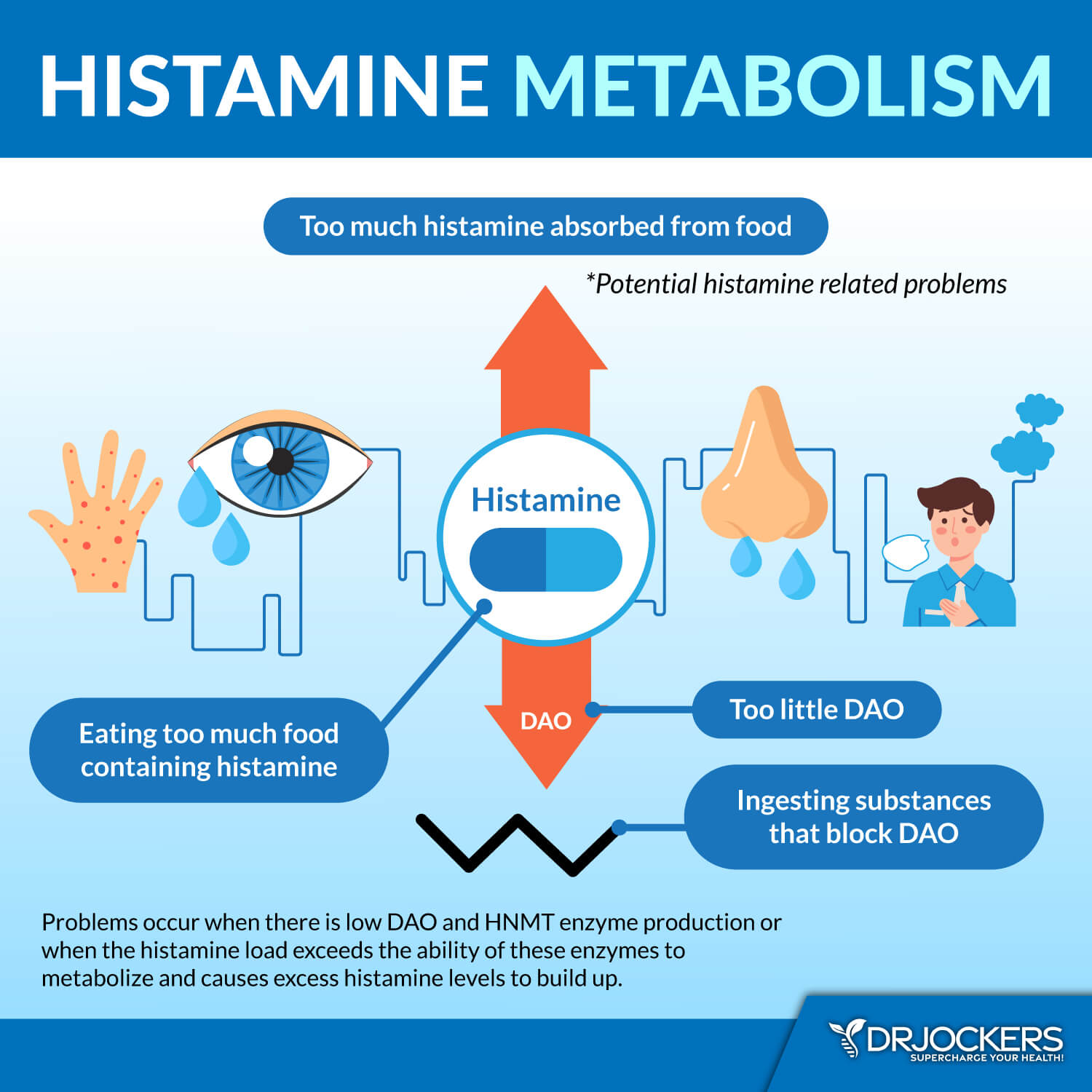
Try a Low Histamine Diet Trial
To reduce histamine intolerance and consequent pollen allergies, I recommend that you remove or reduce high-histamine foods, including cured meat, dried fruit, sour food, vinegar-containing food, aged cheese, nuts, high-histamine vegetables (eg. tomatoes, spinach, eggplant), and smoked fish.
I also recommend avoiding histamine-releasing food, including bananas, chocolate, avocado, tomatoes, shellfish, strawberries, cow’s milk, preservatives, and dyes. Focus on low-histamine foods instead, including artichoke, beets, bok choy, broccoli, carrots, cauliflower, cucumber, collard green, jicama, kale, leek, lettuce, onion, swiss chard, zucchini, leafy herbs, coconut oil, ghee, grass-fed butter, apples, blackberries, blueberries, cherries, pears, pasture-raised beef, grass-fed poultry and wild-caught fish.
You can try reducing your consumption of these foods for a week or two and see if you notice an improvement in your pollen allergies. If so, you have issues with histamine and should consider lower histamine on a more regular basis. To learn more about histamine intolerance, I recommend reading this article.

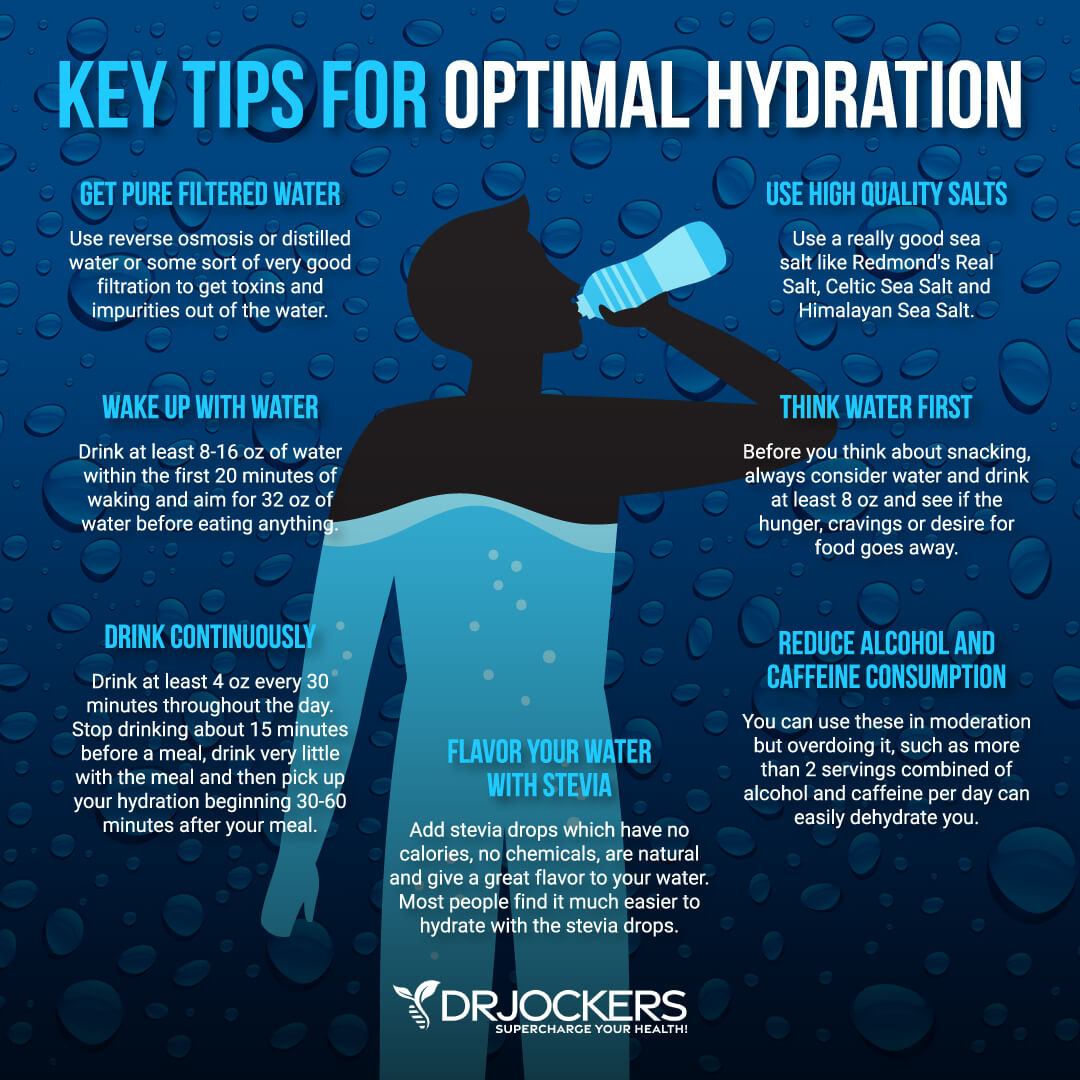
Good Hydration
Water is key to your health. A fetus develops within a water-bound environment inside the amniotic sac and a baby’s water-rationing system takes effect quickly after birth to avoid dehydration. Histamine helps to redistribute water inside your body to keep you hydrated and healthy. It helps to make sure that your vital organs receive enough water to maintain optimal functioning.
If you are chronically dehydrated, histamine has to withdraw water from major regions of your vital organs to send it to your vital organs to sustain life and function. This chronic dehydration can lead to excessive histamine activity and histamine intolerance. As you’ve already learned, histamine intolerance can lead to a variety of symptoms including pollen allergies and related symptoms, such as congestion, sneezing, fatigue, pain, watery eyes, and coughing (15, 16, 17, 18).
To keep your body healthy and reduce symptoms of pollen allergies, it is important that you stay hydrated. I recommend that you use a reverse osmosis system to avoid toxicity from tap water. Avoid plastic water bottles, and use glasses, glass bottles, stainless steel bottles, and mason jars instead. Start your day with 32 oz of fresh clean water.
You may add some lemon or apple cider vinegar for an extra boost of alkalinity and digestion support. Drink regularly throughout the day, about 4 oz every 30 minutes or so. Make sure to drink green juices, herbal tea, and green smoothies, and eat hydrating fruits and veggies throughout the day in addition to water. To learn more about the connection between hydration, allergies, and asthma, I recommend this article.
Reduce Stress & Prioritize Good Sleep
Chronic stress and poor quality of sleep can increase inflammation in your body and compromise gut health. When you are under stress, your body also releases histamine to protect your body. However, when you are under chronic stress and your body is fatigued from low-quality or little sleep, your body will release too much histamine. As you know, too much histamine is not good for your body and can lead to a variety of issues, including allergies (19).
To reduce pollen allergies, I recommend that you take charge of your stress levels and sleep habits. Try meditation, breathwork, guided relaxation exercising, grounding, time in nature, journaling, positive affirmations, mindset shifts, gratitude practice, and prayer to reduce stress.
Spend time with loving family members, supportive friends, uplifting people, and friendly pets. If you need help with transforming negative thoughts into positive ones, develop positive coping strategies and mindset shifts, or simply want to talk things out, you may reach out to a therapist, life coach, or spiritual counselor.
Make sure to go to bed and wake up around the same time every day. Develop a nighttime routine that works for you. You may want to play board games or other games with your family, color, read, listen to calming music, meditate, stretch, and sip on herbal tea while staying away from electronics for the last hours of the day. Invest in a comfortable bed, bedding, and pillows. You may want to try a salt lamp or essential oils to create an extra feeling of calm and relaxation.

Improve Gut Health
An alteration of your gut microbiota can have serious consequences on your overall health. It can lead to chronic inflammation and impact your immune response. It may increase allergic response, and lead to symptoms of allergies even when coming in contact with otherwise safe particles from pollen or weed. Eating an inflammatory diet, taking antibiotics, environmental toxins, and stress can all impact your good health and lead to allergies (20).
To improve your gut health, I recommend that you eat an anti-inflammatory gut-friendly diet, reduce environmental toxicity by using natural and organic products, not smoking, and spending time in nature, and reduce stress.
Probiotics also play an important role in your gut microbiome and immune coordination. Probiotics can be very effective in reducing allergy symptoms. I recommend that you take MegaSporebiotic probiotics to optimize your gut health and improve your immune health (21).
Optimize Vitamin D Levels
Vitamin D is critical for your immune system. Low levels of vitamin D are associated with chronic inflammation and a risk of developing allergies. While getting sun exposure on a regular basis is essential for your vitamin D levels, it is difficult to meet your needs, especially when working indoors or living in a colder climate.
To optimize your vitamin D levels, I recommend 1,000 I of vitamin D3 with 4.5 mcg of K2 per 25 lbs. of body weight daily. Vitamin D3/K2 is a potent supplement that can help to optimize your vitamin D levels when taken daily (22).

Use Quercetin & Vitamin C
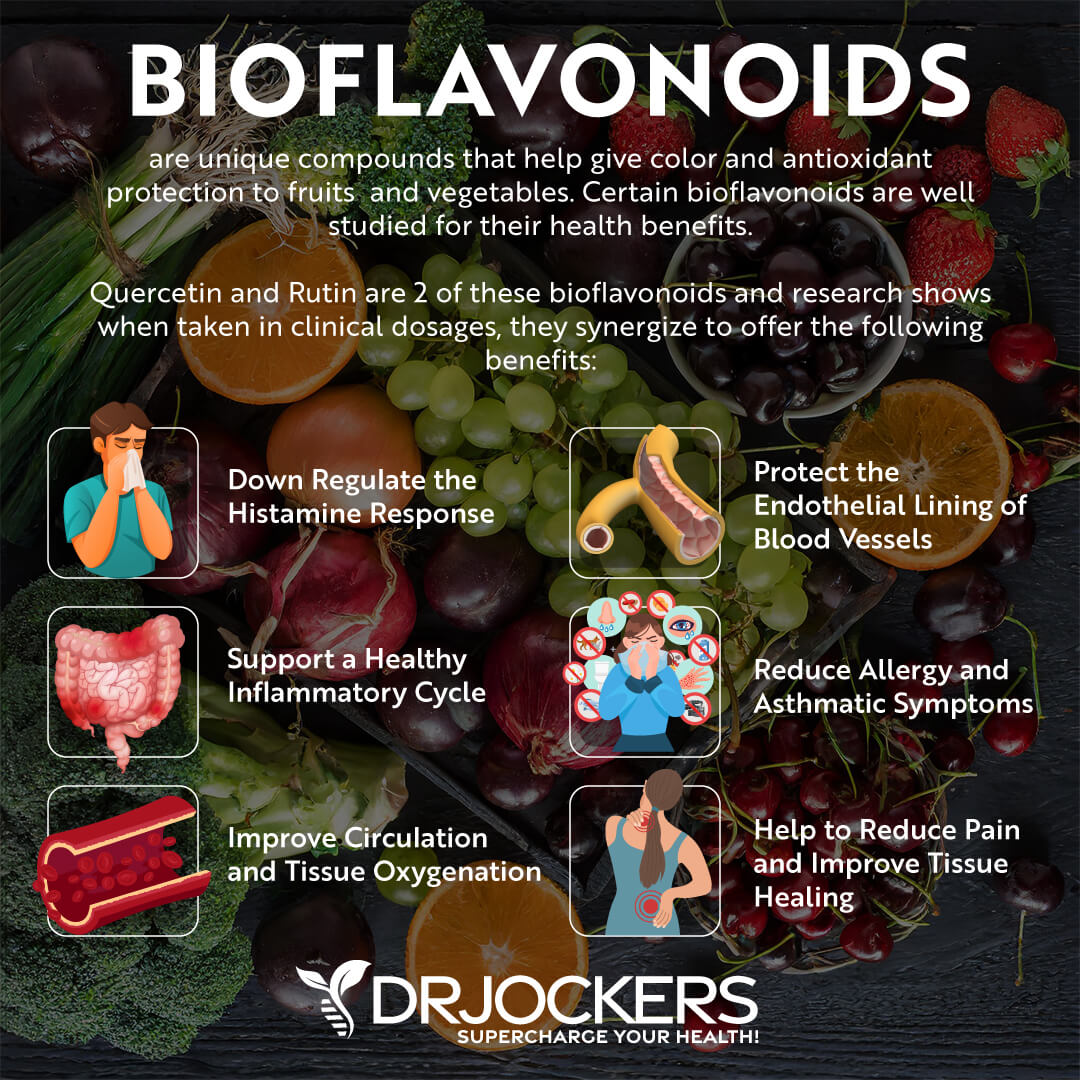
Taking quercetin and vitamin C can significantly improve your immune response to allergens. Quercetin and other active bioflavonoids, such as dihydroquercetin (DHQ) and rutin help to modulate an exaggerated immune response.
Vitamin C and other bioflavonoids like quercetin are fantastic for immune system support and decreasing histamine reactions. This is why I recommend Allergy Support, a potent supplement powered by Vitamin C, quercetin, and other bioflavonoids to improve your immune response (23, 24).
Support Glutathione Levels
Glutathione is a powerful antioxidant in plants, animals, fungi, and some bacteria. It helps your body’s natural antioxidant response. It can also help to improve the inflammation response, decrease oxidative stress, and lower the risk of seasonal allergies.
You can upregulate your glutathione levels by supplementing with N-Acetyl Cysteine, Alpha Lipoic Acid, selenium, milk thistle, resveratrol, and curcumin. It may also help to decrease symptoms of pollen allergies. I recommend Super Glutathione for pollen allergy support (25).

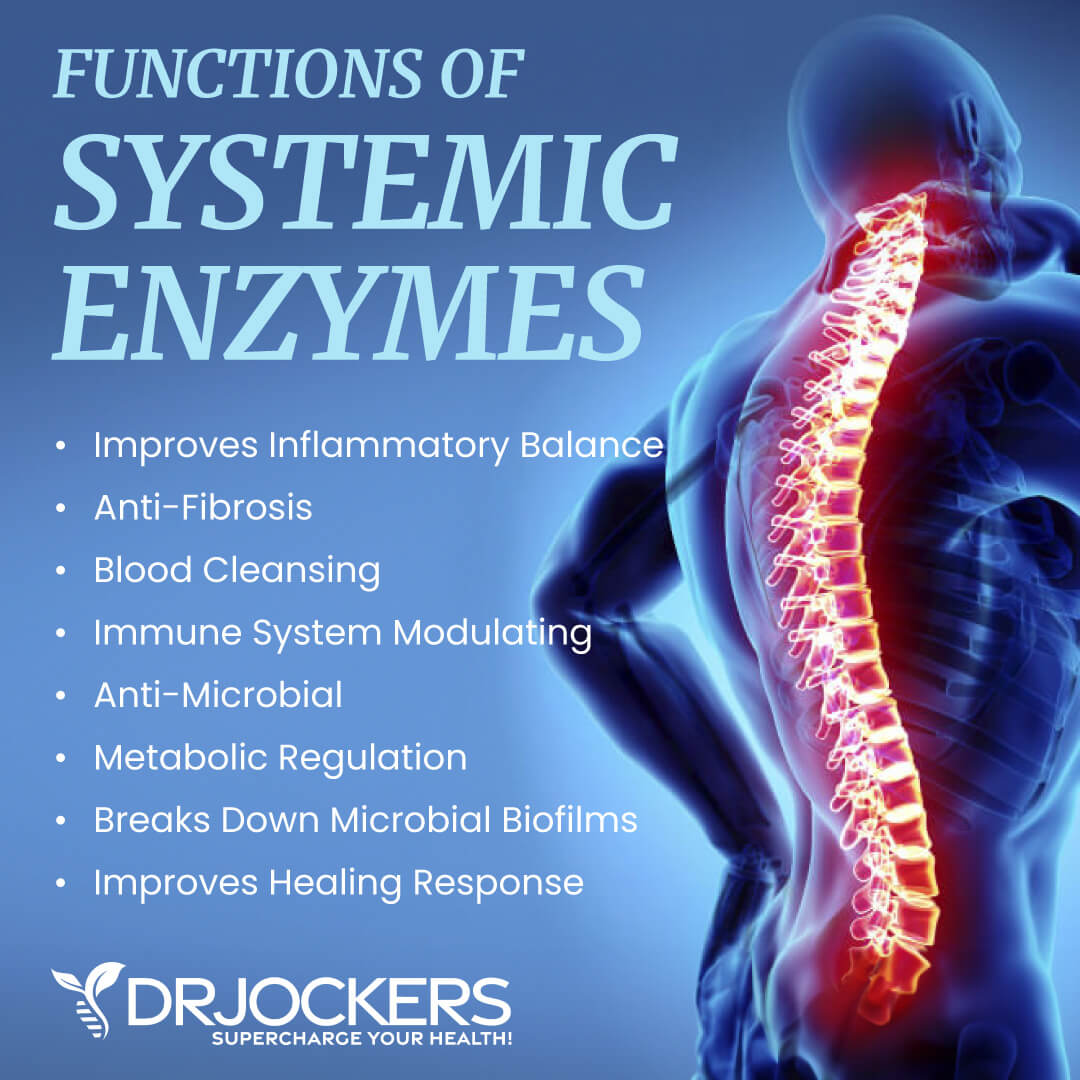
Consider Proteolytic Enzymes
Proteolytic enzymes help to catalyze proteolysis, the breakdown of proteins. They help to stimulate immune activity and optimize your immune system function by promoting healthy gut bacteria and a healthy gut flora balance.
As a result, they may also support immune health and allergy-like symptoms. For microbiome health, reducing oxidative stress, and immune support, I recommend taking Proteo Enzymes (26).
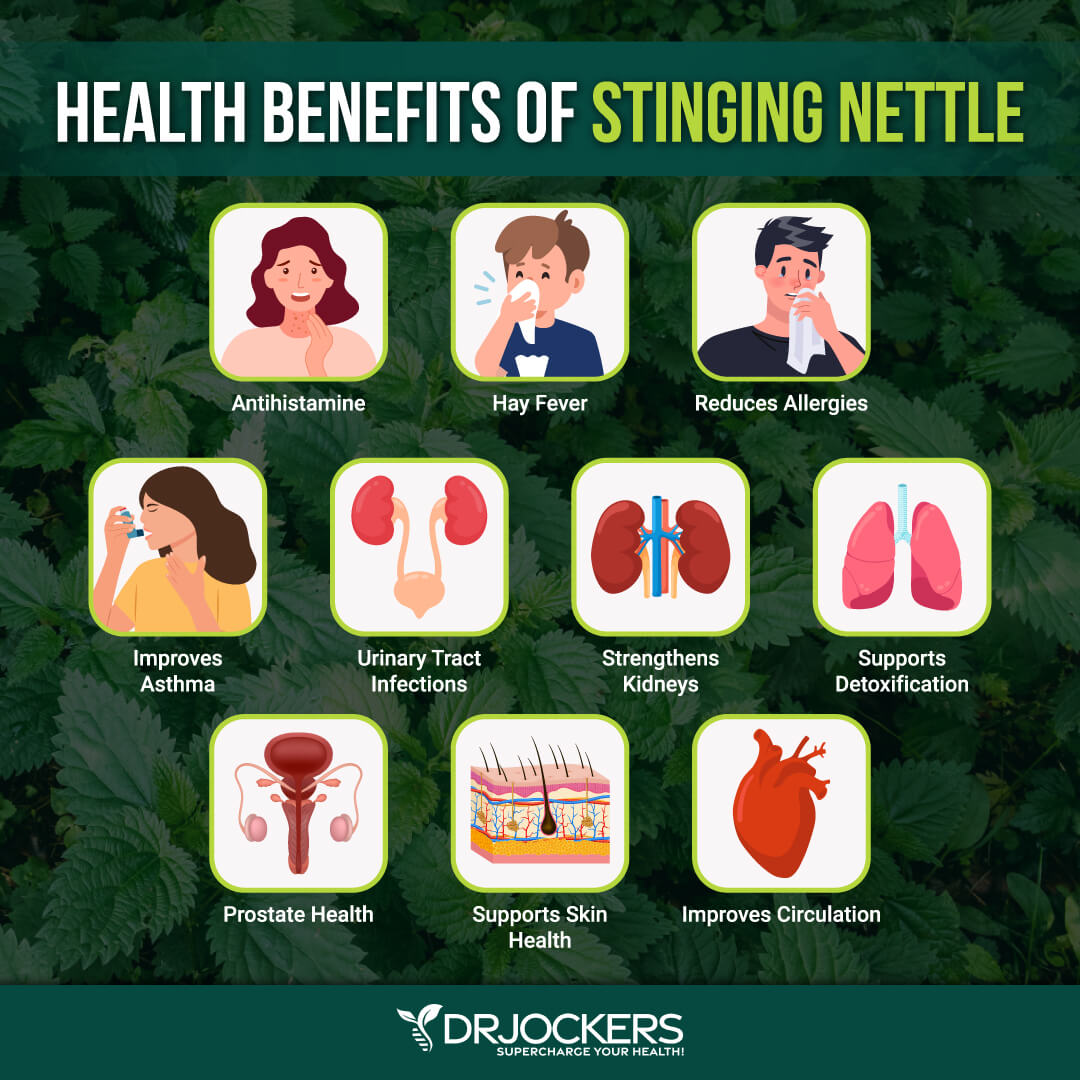
Use Stinging Nettle
Stinging nettle is a plant native to Europe but can be also found in North America and New Zealand. Stinging nettle leaf has been found to help regulate inflammatory activities and hyperimmune responses related to histamine intolerance, mast-cell degranulation, and prostaglandin formation.
Research has shown that it may help to improve symptoms associated with seasonal allergies. This is why I recommend Allergy Defense, a supplement made with stinging nettle and other immune-boosting nutrients that help support allergy sufferers (27, 28).
Consider Allergy Defense
For pollen allergies and seasonal allergies, I recommend Allergy Defense. This supplement is made with vitamin C, bioflavonoids, such as Quercetin, dihydroquercetin (DHQ) and rutin, FlavitPURE™, nettle leaf extract, the proteolytic enzyme from pineapple called bromelain, and N-Acetyl-Cysteine (NAC).
This product contains anti-histamine compounds, proteolytic enzymes, and glutathione supporting agents making it a powerful defense against pollen and other seasonal allergies. This product works to help moderate unpleasant immune reactions and improve the health of those with pollen allergies. Take 1-2 capsules, 2 times daily for optimal results.
Final Thoughts on Pollen Allergies
Pollen allergies are quite common in the spring, summer, and early fall. Symptoms of pollen allergies may include sneezing, runny nose, congestion, coughing, itchiness, watery and red eyes, and more.
If you have been dealing with pollen allergies, it is important to take action to improve your health. Follow the natural support strategies for pollen allergies to improve your immune response and experience better overall health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.

Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




Can you do an article on primary Lympedema – born with it , not puberty onset, menopause onset or not just cancer created , when lymph nodes are damaged?
Yes we may consider that down the road! Praying for you!
Hello. I purchased gut healthy protein shake recently; however, I don’t see the Ingredient list anywhere on the container and the taste leaves much in the desirable department 😉 lol
It is on the side of the container and you can also find it here: https://store.drjockers.com/products/gi-cleanse-protein