 Prostate Cancer: Symptoms, Causes, and Support Strategies
Prostate Cancer: Symptoms, Causes, and Support Strategies
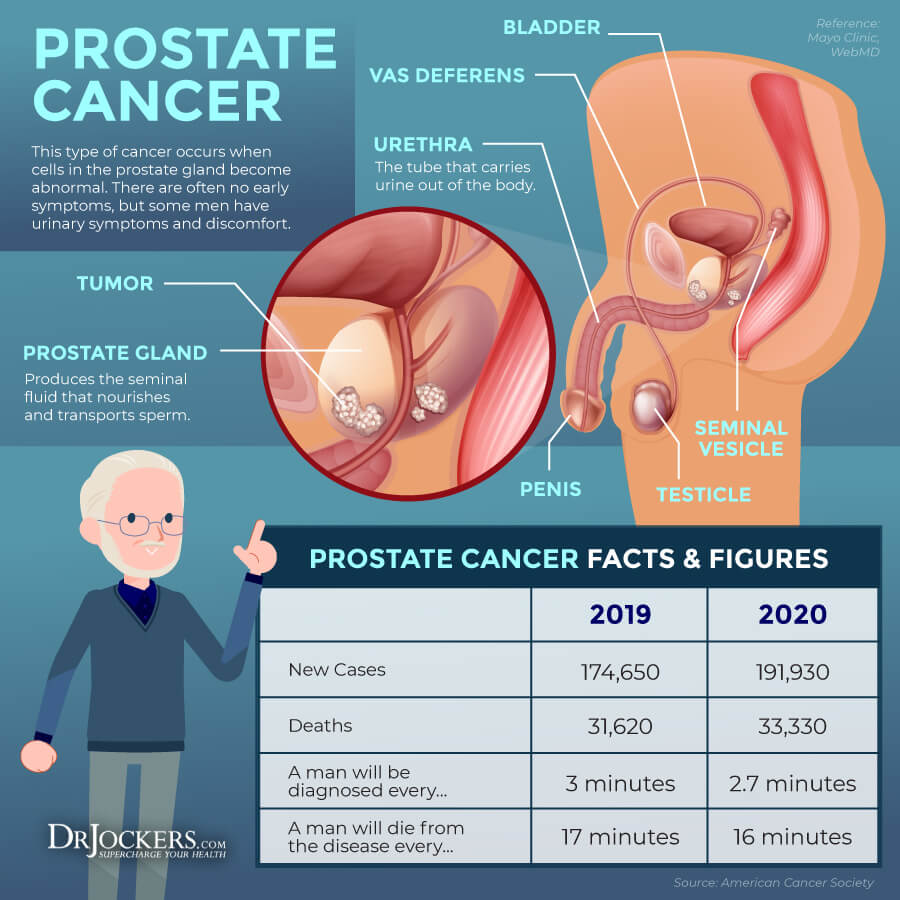
Prostate cancer is a form of cancer that affects the prostate gland in males. It will affect about 1 in 9 men during their life. While prostate cancer is highly treatable when caught early, there are still 34,130 new deaths a year from prostate cancer (1, 2, 3). As with other healthy issues I talk about, using natural support strategies, including diet, lifestyle, and supplementation methods may help to improve your health.
In this article, you will learn what prostate cancer is. I will go over the stages of prostate cancer. You will learn about its risk factors and top root causes. You will understand the symptoms of prostate cancer, how it’s diagnosed, and conventional treatment options. I will offer some functional lab analysis options that may help with diagnosis and identifying root causes and risk factors. I will share my top natural support strategies to improve your health.
What Is Prostate Cancer
Prostate cancer is a form of cancer that affects the prostate. The prostate is an organ that’s located below the bladder and in front of the rectum in males. The prostate serves a variety of functions, including making fluids that nourish and transport semen, facilitating urine control, and secreting a protein called prostate-specific antigen (PSA) that allows semen to stay in a liquid form (1, 2).
According to the American Cancer Society, there are about 248,530 new cases of prostate cancer and 34,130 new deaths from prostate cancer each year in the United States (3). It affects about 1 in 9 men at one point in their lives (3). While prostate cancer is highly treatable when caught early, it is still the second leading cancer-related cause of death, only preceded by lung cancer (3).
About 1 in 41 men will die because of prostate cancer, yet as of 2021, over 3.1 men in the US who have been diagnosed with prostate cancer at one point recovered and still alive today (3). Routine cancer screening, early detection, and lifestyle choice that reduce the risk of disease can help to reduce prostate cancer cases and increase the chance of recovery and survival.
Stages of Prostate Cancer
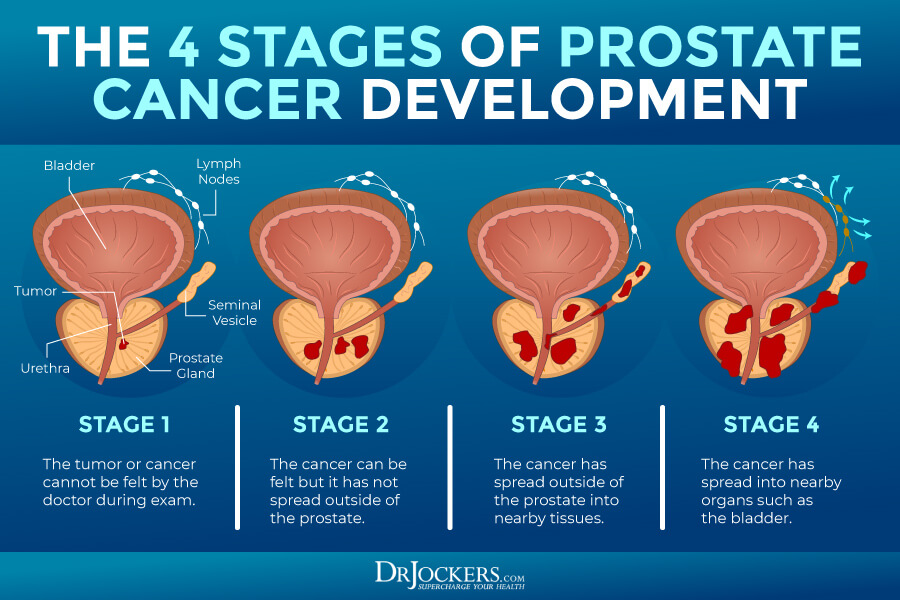
Caught in its early stages, prostate cancer is usually treatable with a high recovery rate. However, the chances of recovery become increasingly difficult as the diseases progress.
Stages of prostate cancer include (4):
Stage 0
At this stage, there are precancerous cells in the prostate gland, but they are slow-growing and only affect a small area.
Stage I
At stage 1, prostate cancer is localized. It can only be found in the prostate gland. It still only affects a smaller area or part of the prostate. It can be treated effectively at this stage.
Stage II
At this point, cancer is only found in the prostate with low to medium PSA levels. The cancer is relatively small with a risk of spreading and growing.
- Stage IIA: At this stage, the tumor is only on half of one side of the prostate or less and cannot be felt. Sometimes it’s a larger tumor but only in the prostate. The cancer cells are easily differentiated.
- Stage IIB: The tumor is still only located inside the prostate, but larger and with moderately differentiated cancer cells.
- Stage IIC: The tumor is still only located inside the prostate, but larger, can be felt, and with moderately or poorly differentiated cancer cells.
Stage III
At this stage, the cancer regional. It is growing and spreading. PSA levels are high.
- Stage IIIA: The cancer has spread to nearby tissues or the seminal vesicles.
- Stage IIIB: The tumor has spread outside to the bladder, rectum, or other outside structures.
- Stage IIIC: The tumor has spread outside the prostate gland to nearby structures and cancer cells are poorly differentiated.
Stage IV
The cancer is distant. It has spread to other organs even beyond nearby structures.
- Stage IVA: At this stage, the cancer has spread to regional lymph nodes.
- Stage IVB: At this advanced stage, the cancer has spread to more distant areas, including the distant lymph nodes, bones, lungs, or other areas of your body.
Risk Factors for Prostate Cancer
According to the American Cancer Society, risk factors for prostate cancer include (5):
- Family history: While prostate cancer can develop in men without a family history, men with a father, brother, or close male relative with prostate cancer may be more likely to develop the disease.
- Gene changes: Inherited genetic mutations may also increase the risk of prostate cancer, including BRCA1 and BRCA2 gene mutation and Lynch syndrome.
- Age: Age may be a risk factor for prostate cancer. While it’s rare under the age of 40, it is more common over the age of 50, and in 60 percent of cases, it occurs beyond age 65.
- Race and ethnicity: Black and white men may have a higher risk of prostate cancer, while it less common in Hispanic and Asian men.
While the following factors play a less clear role, according to the American Cancer Society, they may also pose a risk for prostate cancer (5):
- Diet: Consuming a lot of dairy products or too much calcium may increase the risk of prostate cancer.
- Obesity: Being highly overweight and obese may increase the risk of prostate cancer and may also increase the risk of a more aggressive and faster-growing form and death.
- Smoking: Smoking may slightly increase the risk of prostate cancer.
- Chemical exposures: Regular chemical exposures, for example in firefighters or exposure to Agent Orange, a chemical that was commonly utilized during the Vietnam War may increase the risk of prostate cancer.
- Inflammation of the prostate gland (prostatitis): While this link is not yet proven, prostatitis may increase the risk of prostate cancer.
- Sexually transmitted infections (STIs): Gonorrhea, chlamydia and other STIs may increase the risk of prostate cancer.
- Vasectomy: While vasectomy is a minor surgery that is used as a birth control option in some cases making men infertile, it may somewhat increase the risk of prostate cancer.

Root Causes of Prostate Cancer
Prostate cancer may develop for a variety of reasons. Here are the main root causes of prostate cancer:
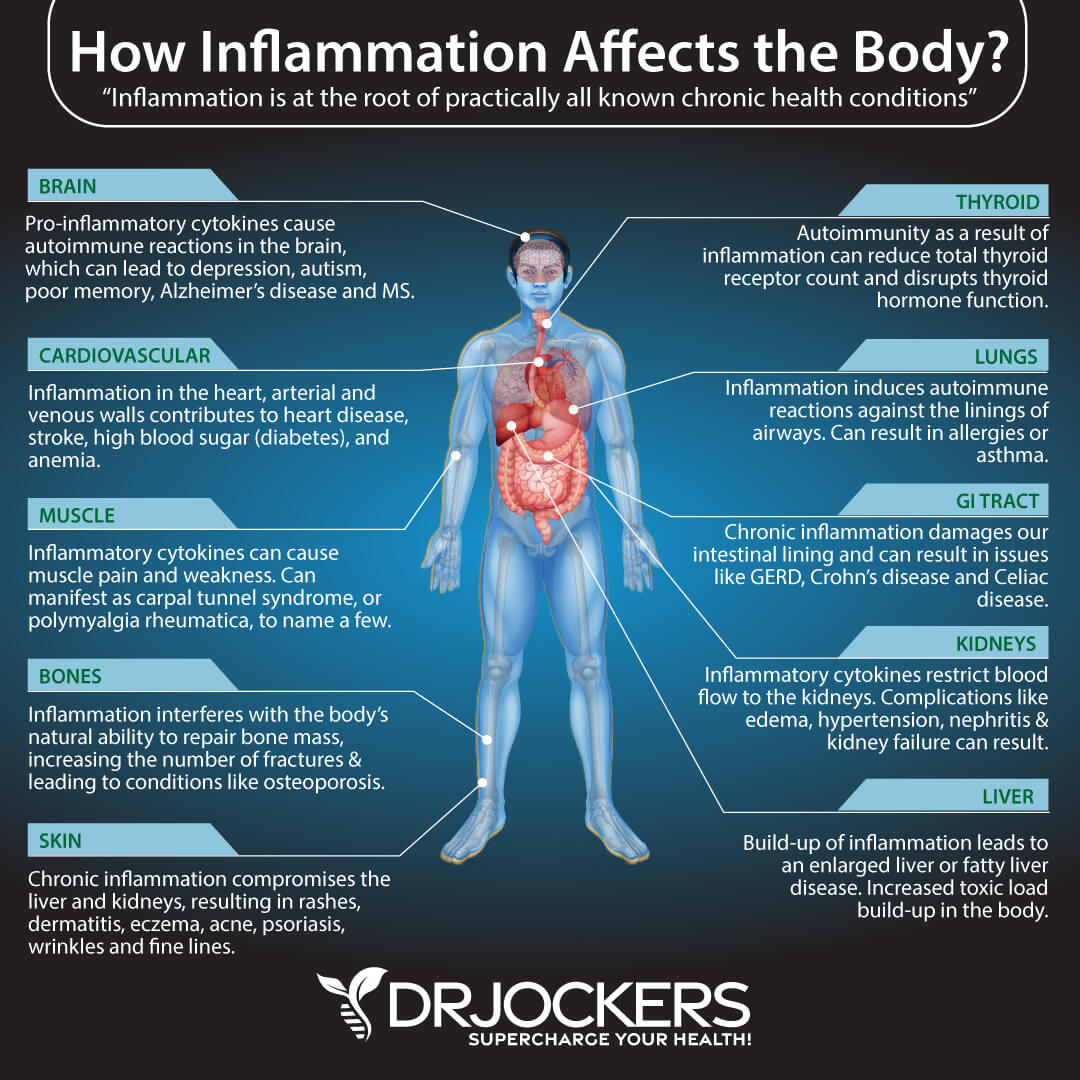
Chronic Inflammation
Chronic inflammation is one of the top root causes of most diseases, including most cancers. A 2014 review published in Histopathology has explained that about 20 percent of cancers are connected to chronic inflammatory conditions or diseases (6). They found that prostatitis (inflamed prostate) and prostate infections may both contribute to the development of prostate cancer.
An increase in inflammatory pathways and inflammatory cytokines and chronic immune system issues may also contribute to the development of prostate cancer. Chronic inflammation often develops because of a poor, inflammatory diet high in processed foods and low in nutrients, so it’s not surprising that the researchers concluded that an anti-inflammatory, antioxidant-rich diet may reduce chronic inflammation and reduce the risk of prostate cancer.
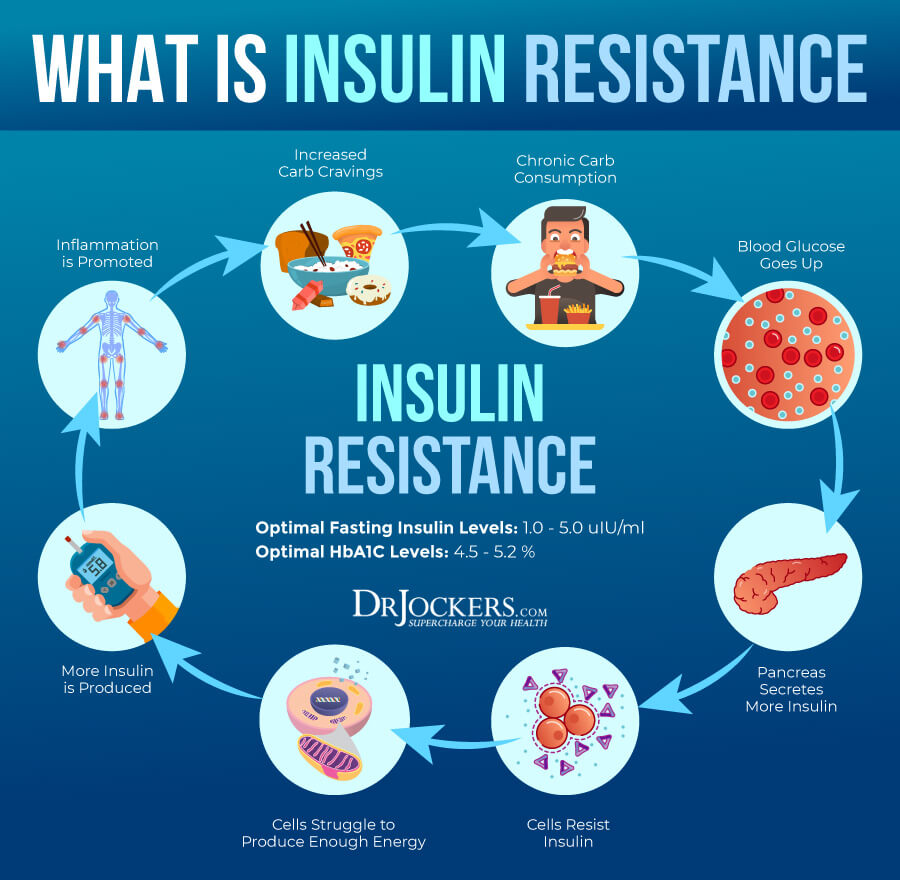
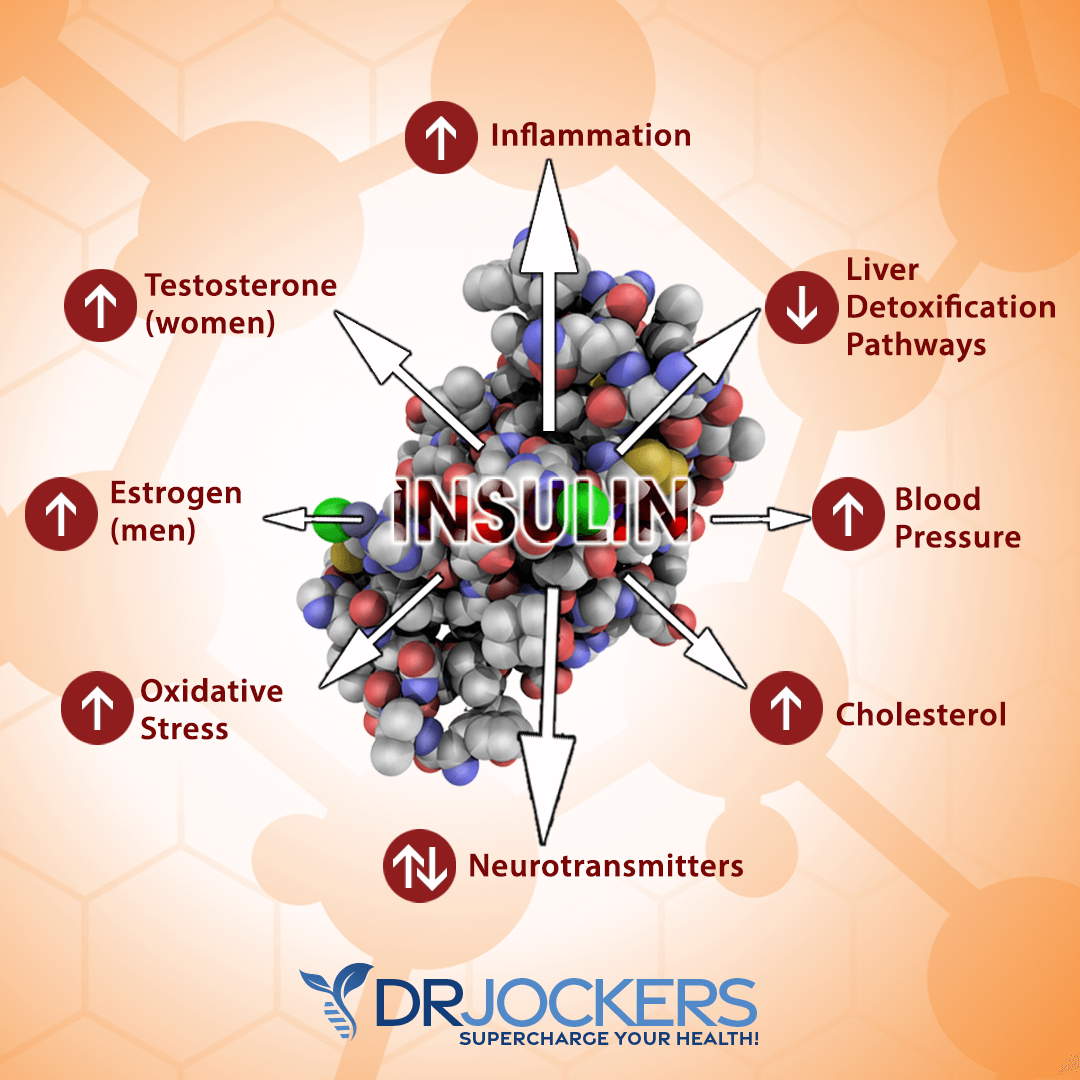
Insulin Resistance
Insulin resistance means that your body cannot respond to insulin well and is unable to break down all dietary glucose for energy effectively. Insulin resistance can not only lead to prediabetes and diabetes but prostate cancer as well.
A 2002 review published in Obesity Reviews has found that hyperinsulinemia and insulin resistance suppresses insulin-like growth factor-binding proteins 1 and 2 (IGFBP-1, IGFBP-2) and sex hormone-binding globulin (SHBG) while increasing insulin-like growth factor 1 (IGF-1) production, which can increase the risk of prostate cancer and other hormone-related cancer (7).
According to a 2003 study published in the Journal of National Cancer Institute, participants with insulin resistance had a higher risk of prostate cancer while those with higher insulin sensitivity had a lower risk of the disease (8). A 2018 review published in Obesity Reviews also agreed with these findings by discovering that hyperinsulinemia, insulin resistance, obesity, and metabolic diseases may also contribute to the development of prostate cancer and recommending that nutrition and exercise may both play a role in prevention (9).
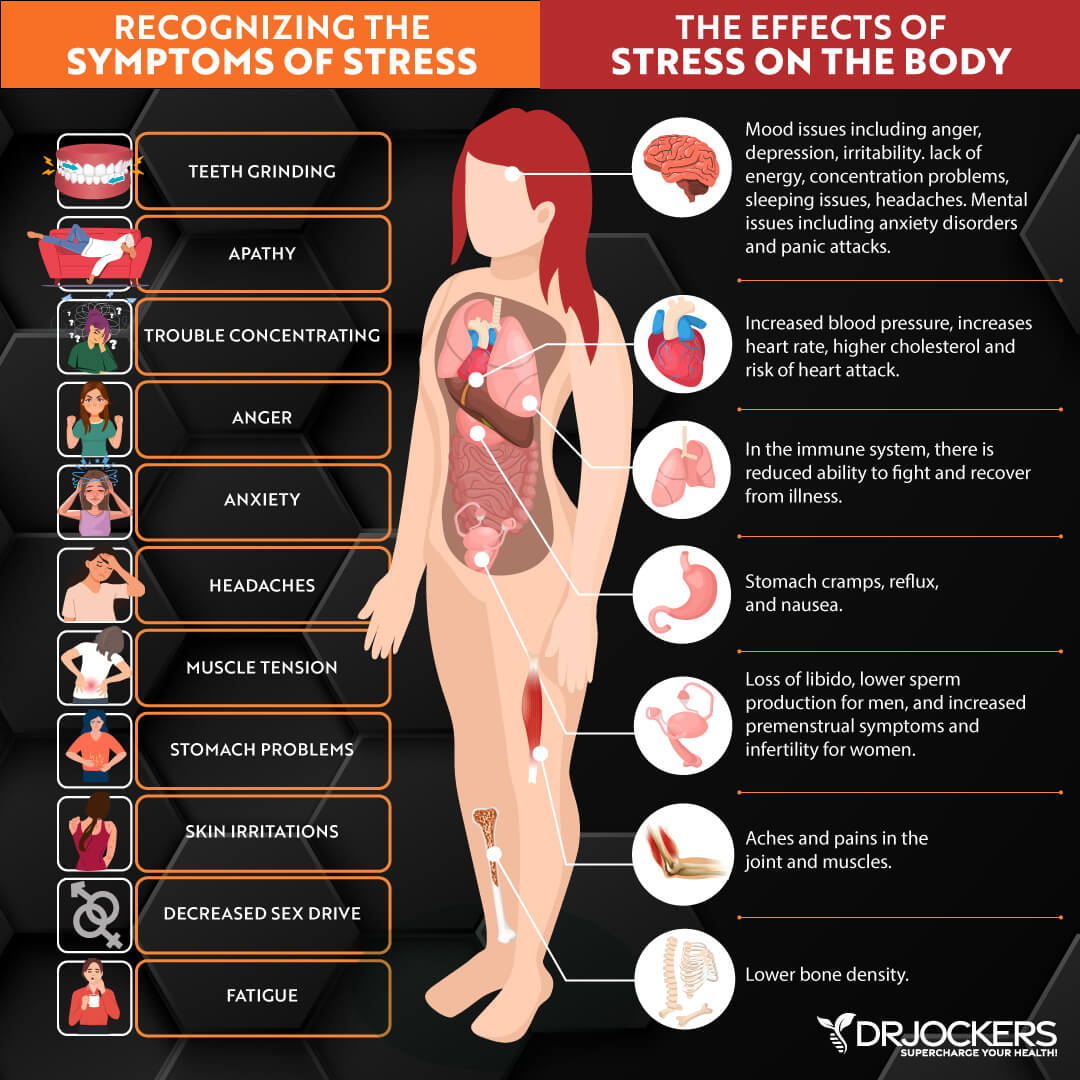
High Stress, Sedentary Lifestyle, & Poor Sleep
High stress, leading a sedentary lifestyle, and poor sleep all contribute to poor health, increased inflammation, and an increased risk of disease. A 2017 study on 1933 men published in Frontiers in Oncology has found that perceived work stress may increase the likelihood of prostate cancer in men under 65 (10).
According to a 2014 study published in Cancer Epidemiology Biomarkers Preview, sedentary occupations that involve a lot of sitting may increase the risk of prostate cancer by 27 to 30 percent (11). A 2013 study published in Cancer Epidemiology Biomarkers Preview has found that insomnia and other sleep disturbances may contribute to the development of prostate cancer in older men (12).
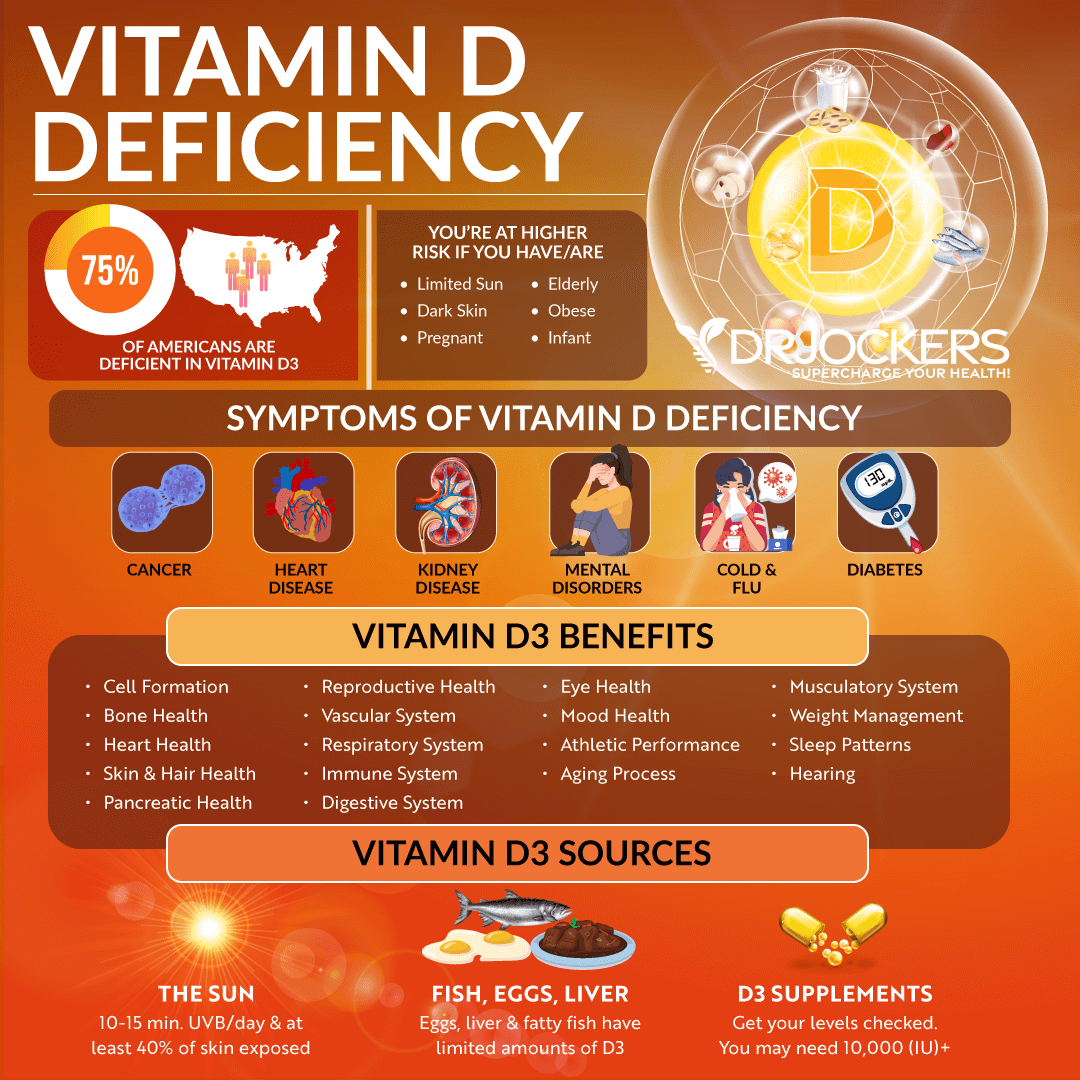
Vitamin D Deficiency
Vitamin D is one of the most important vitamins essential for immune, bone, muscle, brain, hormonal, and other areas of health. Vitamin D deficiency is incredibly common, and it is also linked to most chronic symptoms and health issues, including prostate cancer.
According to a 2009 study published in BJU International, vitamin D deficiency is very common among prostate cancer patients (13). About 18 percent of participants with prostate cancer were deficient in vitamin D while 50 percent had insufficient levels, only less than one-third at 32 percent had adequate levels of vitamin D. A 2018 study published in Endocrine Connections has found that higher vitamin D levels were linked to lower mortality rates in prostate cancer (14).
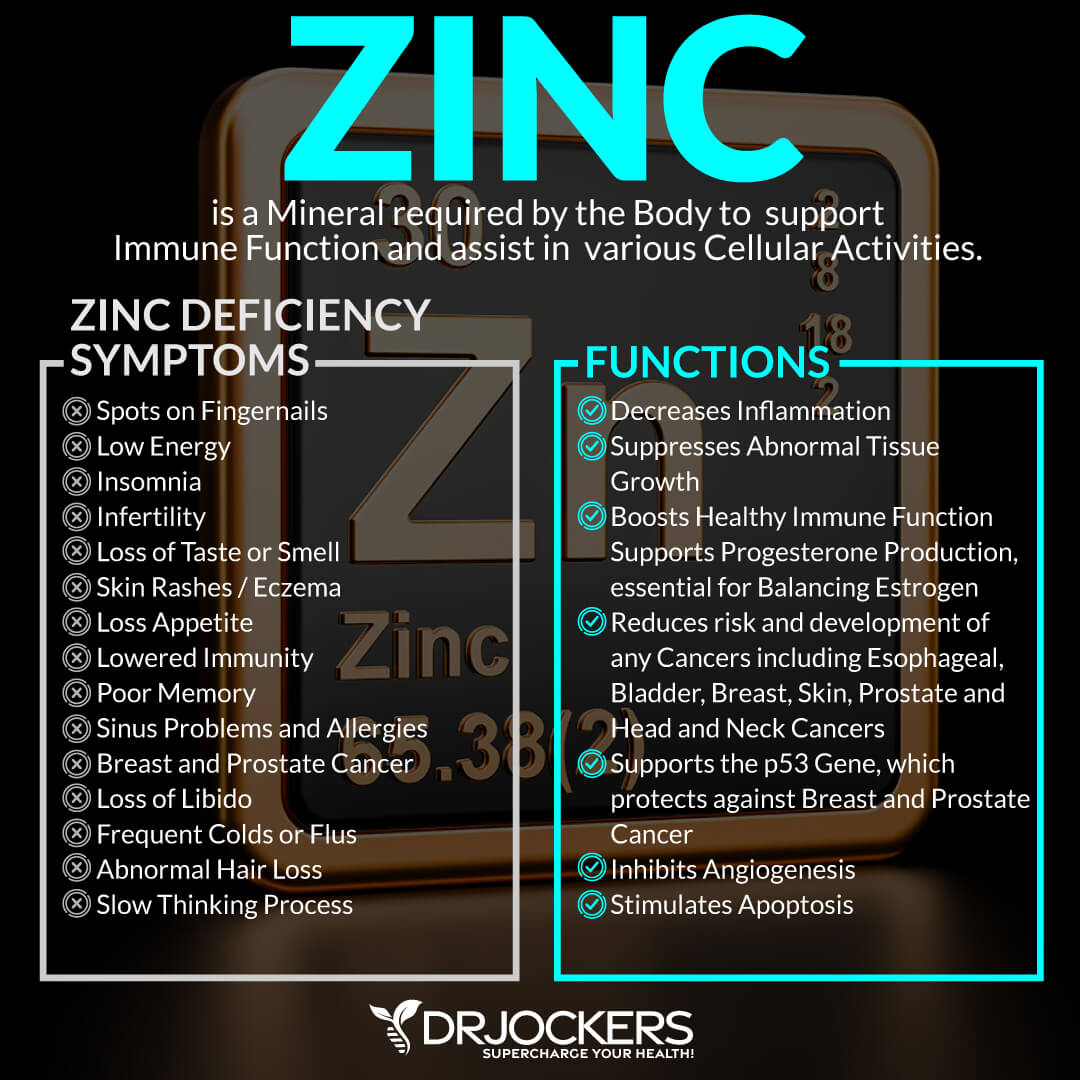
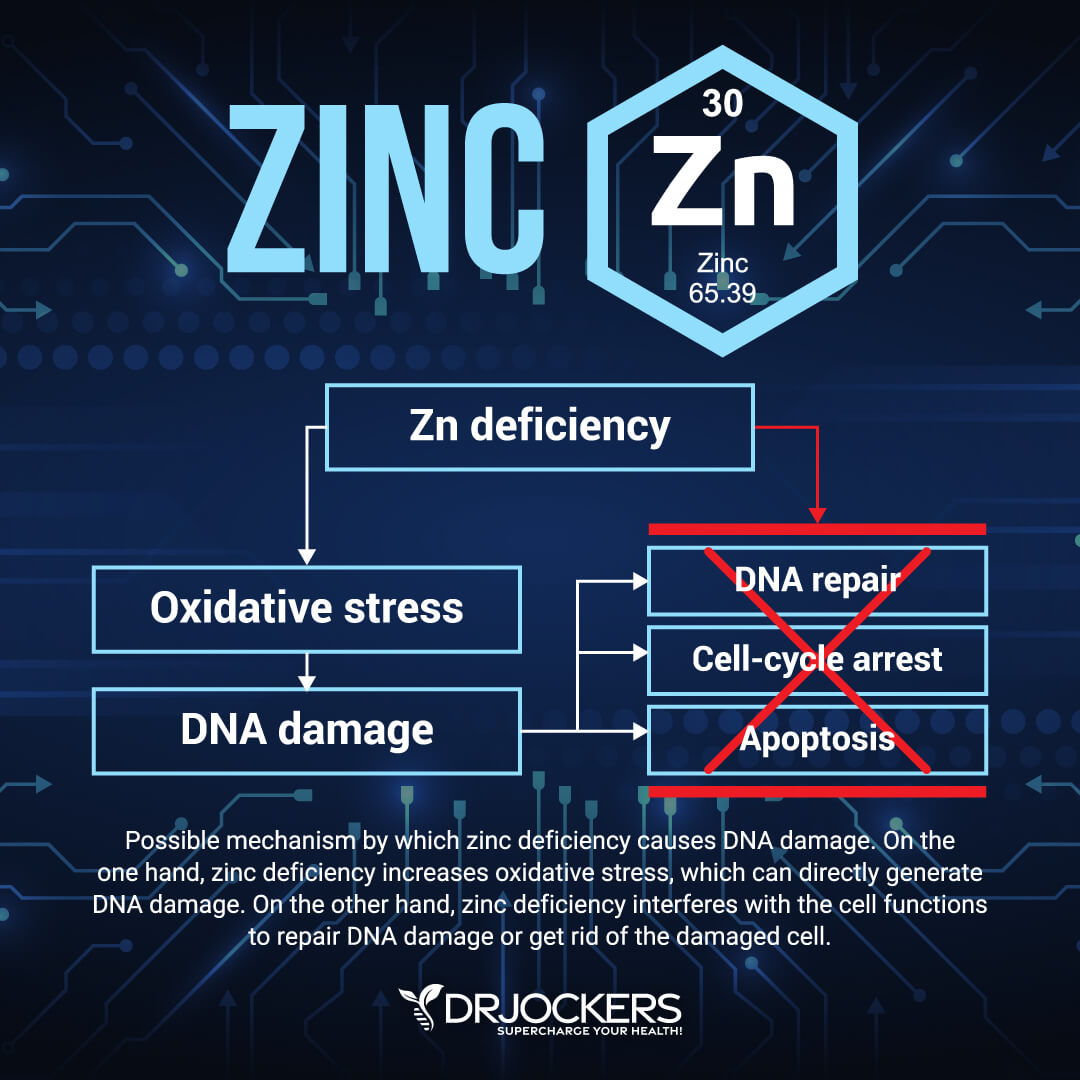
Zinc Deficiency and High Copper
Zinc and copper are two important minerals that may affect prostate cancer. According to a 2020 study published in Frontiers in Oncology, zinc deficiency may increase the likelihood of prostate cancer in those over age 50 (15).
On the other hand, a 2005 review published in Frontiers in Bioscience has found that increased levels of copper may increase the risk of cancer, including prostate, breast, and brain cancer (16).
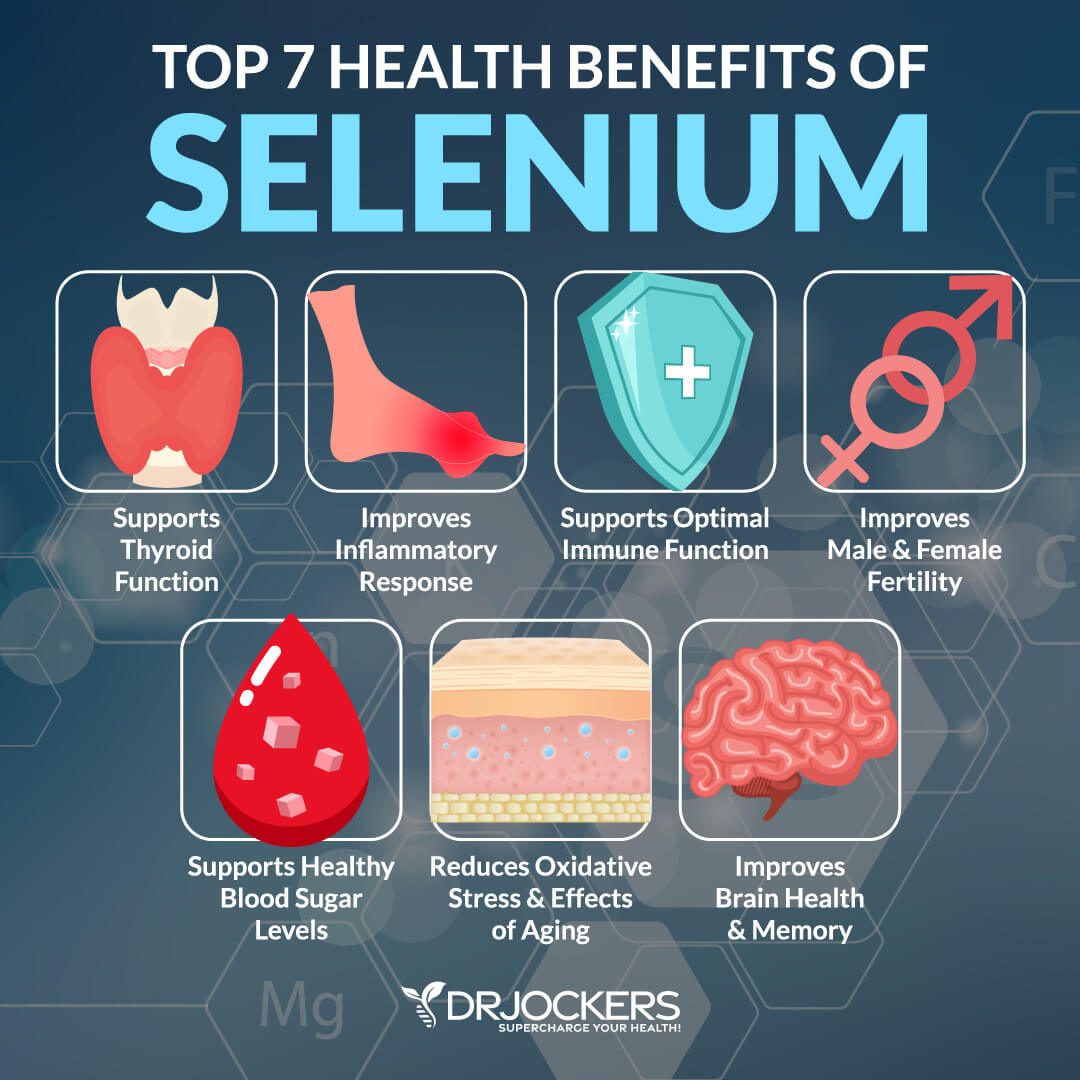
Selenium Deficiency
Selenium is an important mineral that helps to protect your immune health, metabolic function, heart health, and brain health, and lower oxidative stress and inflammation. Selenium is a key part of glutathione production and the antioxidant pathways that protect the cellular DNA.
A 2018 systematic review and meta-analysis has found that selenium may play a protective role in prostate health and deficiency in selenium may increase the risk of prostate cancer (17).
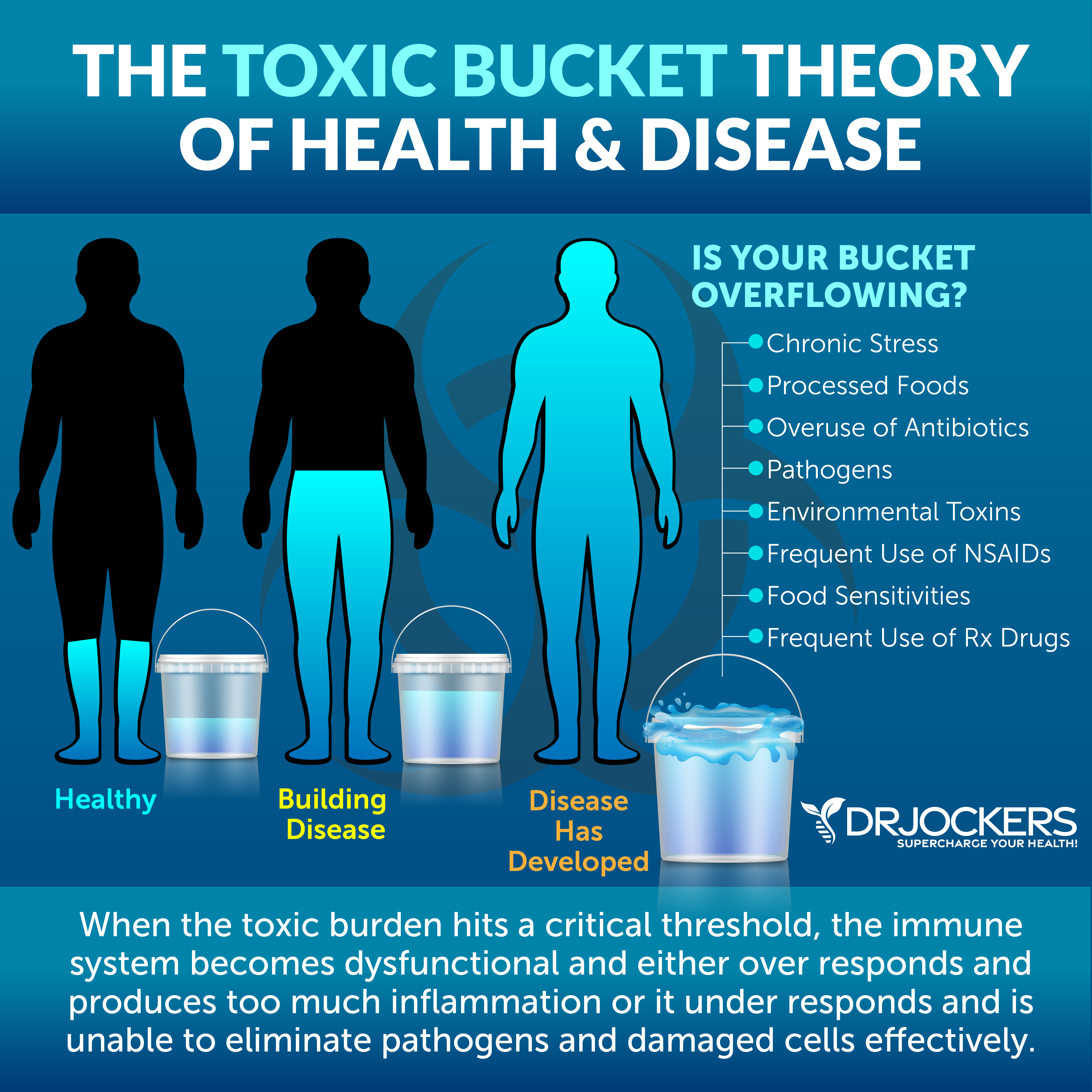
Heavy Toxic Load
Toxic exposure is problematic for your overall health. When it comes to prostate cancer, heavy metals pose the biggest problem. Heavy toxic load may increase the risk of prostate cancer. According to a 2008 study published in Cancer, exposure to Agent Orange during the Vietnam War might’ve increased the risk of prostate cancer in veterans (18).
A 2014 study published in Biological Trace Elements Research has found that increased cadmium levels in smokers may contribute to prostate cancer (19). A 2008 study published in Environmental Health Perspectives has found that inorganic arsenic exposure may increase the risk of prostate cancer (20).
According to a 2019 multiple metal analysis published Environmental Exposure, heavy metal serum levels may indicate risk of prostate cancer (21). A 2002 study published in Biomedical Environmental Sciences has found that environmental exposure to lead and thiobarbituric acid may increase the risk of prostate cancer (22).
According to a 2012 study published in the International Journal of Experimental Pathology, oral mercury exposure in rats may also increase the risk of prostate cancer (23). A 2018 and a 2020 study both published in Environmental Research have both found that phthalate exposure can contribute to the risk of prostate cancer (24, 25).
Diagnosis and Conventional Treatments
Before we get into the diagnosis of prostate cancer and conventional treatment options, let’s talk about the symptoms of prostate cancer first.
Signs and Symptoms of Prostate Cancer
Prostate cancer doesn’t always have any symptoms, especially early on, which makes regular screening very important. However, there are some signs and symptoms you have to be aware of and visit your healthcare professional if you experience them.
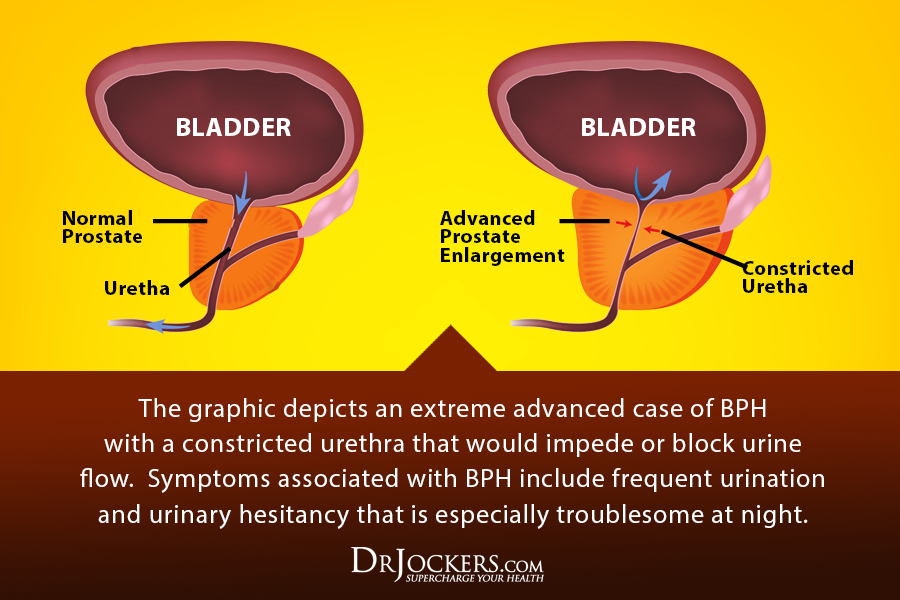
Possible signs and symptoms of prostate cancer may include (26):
- Urination issues, including a weak or slow urinary stream, frequent urination, or frequent urination at night
- Blood in the urine
- Blood in the semen
- Erectile dysfunction (ED)
- Pain in the hips, spine, back, or ribs
- Numbness or weakness in the feet or leg
- Loss of bladder or bowel control

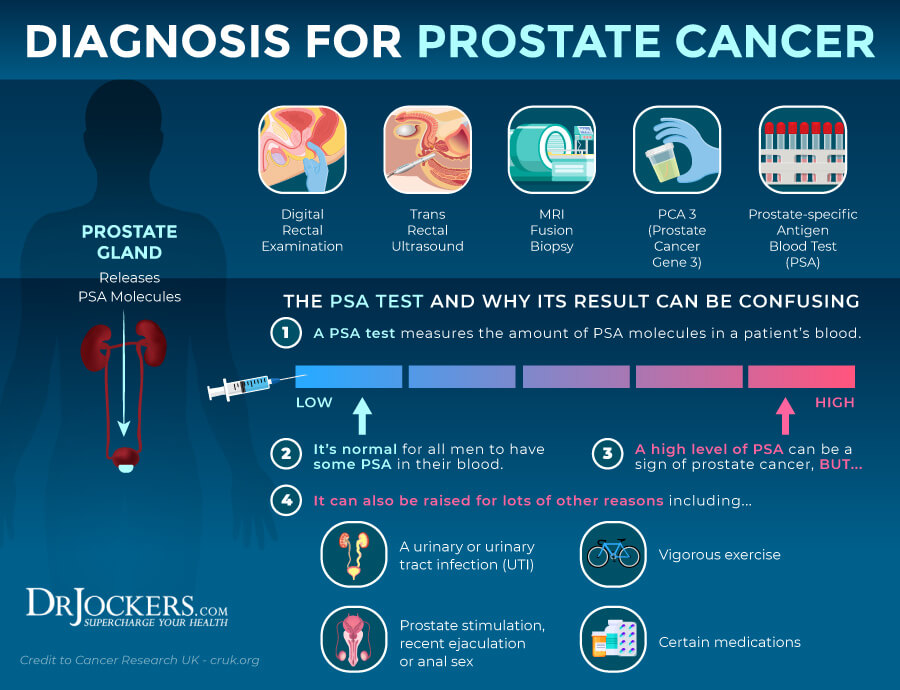
Diagnosis of Prostate Cancer
Screening for prostate cancer is important for early diagnosis. In most cases, prostate cancer is diagnosed with a prostate-specific antigen (PSA) blood test or a digital rectal exam (DRE), however, a biopsy is necessary for a final diagnosis (27).
At first, your doctor will go over your medical history, family history, risk factor, and symptoms and perform a physical exam. During the digital rectal exam, your doctor will insert a gloved, lubricated finger into your rectum to feel for any hard areas, bumps, or abnormalities (27).
Next, they will order a PSA blood test to look for abnormalities. The PSA blood test is usually used if you don’t have any symptoms as an early screening method. However, there are differences in normal results. Some doctors only ask for further testing at 4 ng/mL PSA in the blood or higher, while others recommend 2.5 or 3 ng/mL. About 1 in 4 men with a PSA between 4 and 10 have prostate cancer, however, in some cases, we may see prostate cancer even under 4 ng/mL. Having a PSA over 10 ng/mL suggests a 50 percent chance for prostate cancer (27).
If your PSA levels are abnormal, further screening tests will be ordered. Special PSA tests may include percent-free PSA, complexed PSA, Prostate Health Index (PHI), 4Kscore test, PSA density, specific PSA ranges. If the results are abnormal, your doctor may repeat the PSA test, may order a PSA biopsy and may order other cancer-related screening tests. A biopsy procedure takes a small sample of the prostate by a urologist to check for cancer. During the biopsy, your doctor may do a transrectal ultrasound (TRUS) or MRI, or a fusion of the two procedures to look at the health of the prostate. While this biopsy sounds scary, it doesn’t lead to more than a mild discomfort (27, 28).
The biopsy may lead to a positive for cancer diagnosis, a negative for cancer diagnosis, or a ‘suspicious’ diagnosis. Suspicious means that there is some abnormality that may or may not be cancer and further tests are needed. If you have a positive result, with the help of the Gleason score, your doctor will determine its grade level (27).
After a prostate cancer diagnosis, a variety of other tests may be used, including x-rays, CT scans, magnetic fields (MRI), or sound waves for imaging to determine the stage of cancer, look for complications, and help with certain treatment options and procedures (27).
Conventional Treatment for Prostate Cancer
Conventional treatment options for prostate cancer may depend on the stage and grade of your cancer, your age, overall health, in younger patients, the effects of the treatment on fertility, and the likelihood of a positive outcome.
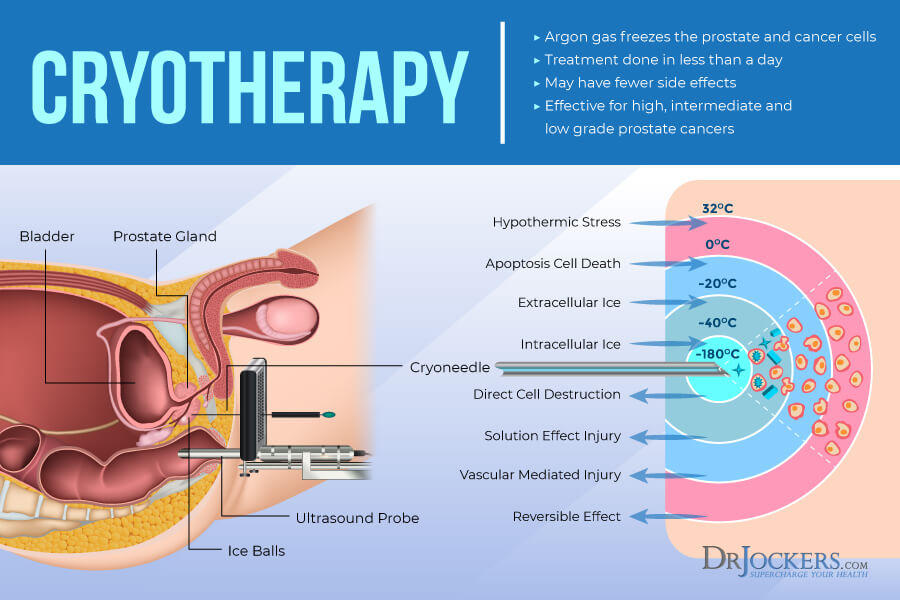
In the early stages, conventional treatment may mean monitoring PSA levels, surgery, radiation therapy, including brachytherapy and conformal radiation therapy. In more advanced stages, conventional treatment may include chemotherapy and hormonal therapy. Cryotherapy and high intensity focused ultrasound are new treatment options that may be used (29, 30).
Key Functional Labs to Look At
There are a variety of key functional lab markers we can look at to determine your risk and uncover underlying root causes of prostate cancer.
Inflammation
Since chronic inflammation is one of the root causes of prostate cancer, I recommend checking for inflammation markers (6). If you want to know more about the top 12 inflammatory lab markers than read this article.
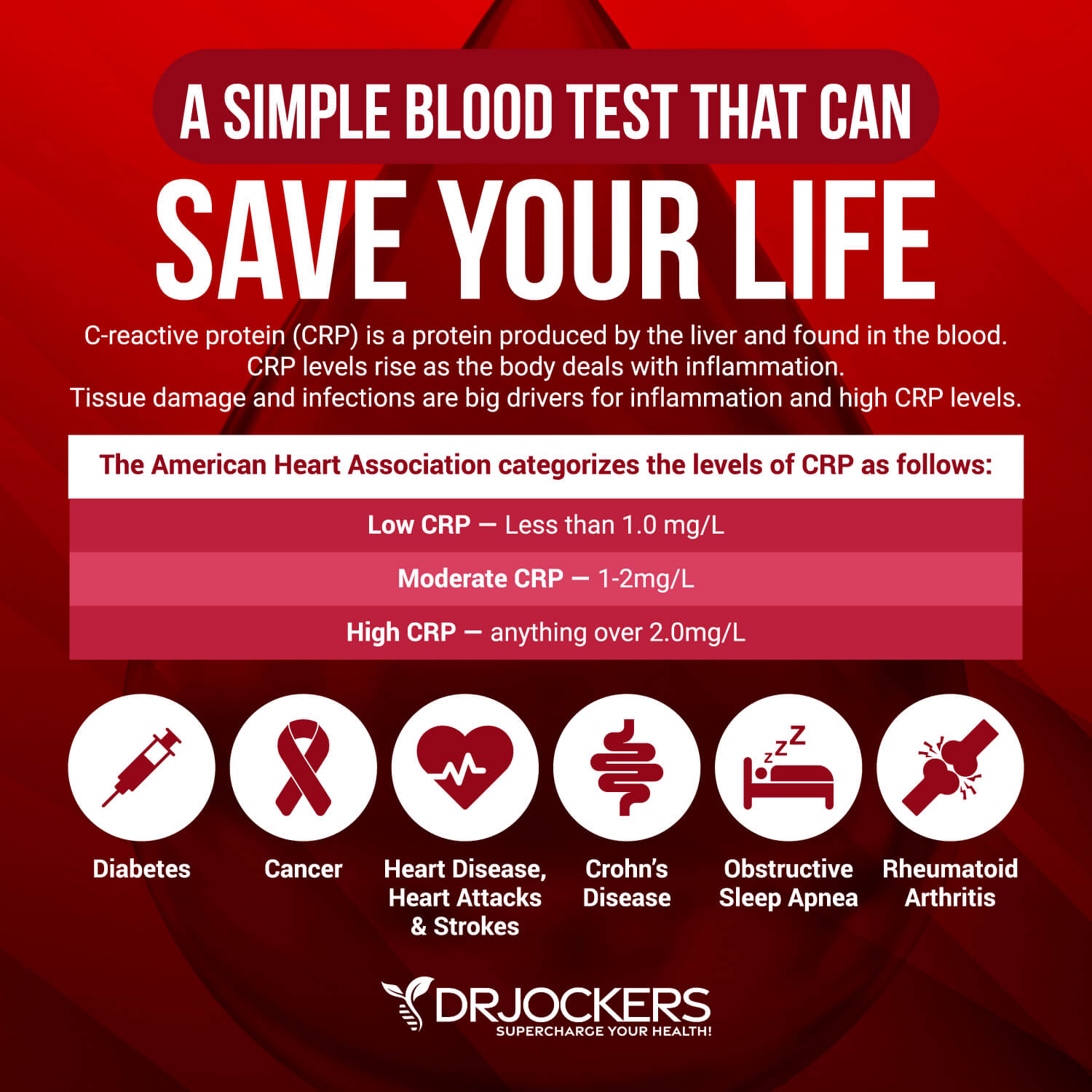
The C-Reactive Protein or CRP test measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L. When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
The C-Reactive Protein or CRP test measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L. When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
Lactate Dehydrogenase (LDH) is an enzyme found in all living cells. Elevated levels may indicate inflammation. Optimal levels are between 140-180. Levels over 180 indicate inflammation.
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer. The clinical range is 30 to 400 and the optimal range is 50 to 150 for males.
Insulin Resistance
Insulin resistance is another risk factor for prostate cancer, so I recommend testing for it (7, 8, 9).
Blood sugar imbalances may increase your risk of inflammation. Fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml and the optimal range is 1.0 – 5.0 uIU/ml.
Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6 while the optimal range is 4.5 – 5.2.
Your lipid profile may be another indication of inflammation and related issues, including cancer risk. Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal. For triglycerides, we are looking for an HDL ratio: 2:1 or less, 1:1 being optimal. Higher rates may indicate insulin resistance and inflammation. Optimal levels:
- VLDL cholesterol: The ideal range is 5 to 30 mg/dl.
- HDL cholesterol: The idea range is 55 to 80. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The ideal range is 40 to 80.
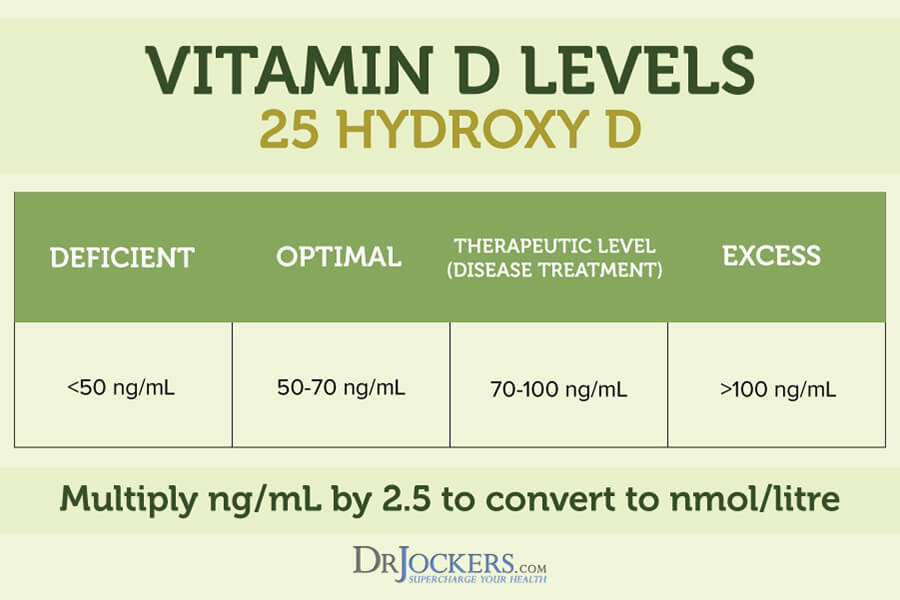
Vitamin D & Plasma Zinc
Vitamin D deficiency, high levels of zinc, low levels of copper, or a poor zinc-copper ratio may also increase your risk of prostate cancer (13, 14, 15, 16) so I recommend testing for these markers.
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. Normal levels of vitamin D are 50 nmol/L (20 ng/mL) or more, while optimal levels are over 75 nmol/L (30 ng/mL).
Zinc and copper compete against each other as antagonists to regulate physiological pathways. A proper balance between the two is essential for maintaining good health.
I recommend checking your plasma zinc and serum copper levels and their balance. The proper zinc-copper ratio should be 1:8, the normal range for zinc is 90 – 135µg/dL, and the serum copper ratio should be between 1 and 1.2.
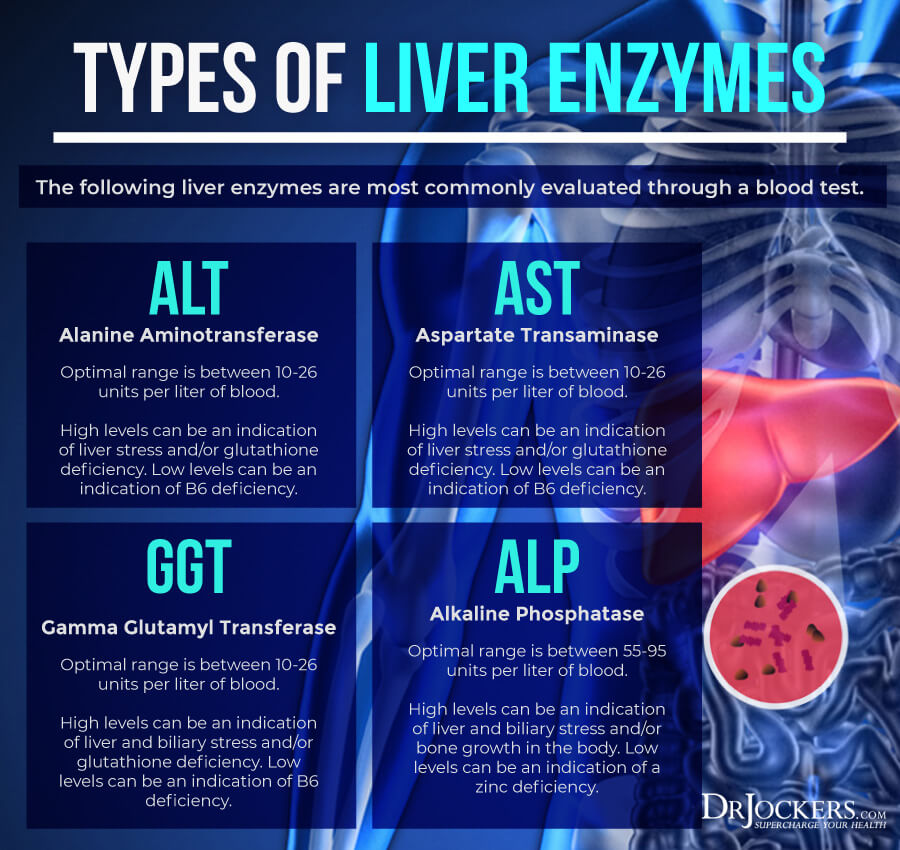
Liver Enzymes
Liver enzyme levels may also indicate inflammation. They may also indicate liver, gallbladder, bile, or kidney issues. Alkaline phosphatase is a liver enzyme that is made by the mucosal cells that line the bile system of the liver and helps normal bile flow. Elevated levels (over 95) may indicate inflammation and liver and gallbladder problems.
Alanine aminotransferase (AST) is a liver enzyme. Elevated levels may indicate inflammation. Normal levels are between 10 and 26 IU/L. Aspartate transaminase (ALT) is an enzyme present in the liver that spills out during times of increased liver stress. Elevated levels may indicate inflammation Normal levels are between 10 and 26 IU/L.
Gamma-Glutamyl Transpeptidase (GGT) is an enzyme in the liver, pancreas, and kidneys. Elevated levels may indicate inflammation and liver disease, usually due to alcoholism and/or sluggish gallbladder or gallstone obstruction. Normal levels are between 10 and 26 IU/L. Levels lower than 10 IU/L can be an indication of a vitamin B6 deficiency.
Natural Support Strategies
Reducing inflammation, balancing your blood sugar, improving your vitamin and mineral levels, and other factors play a role when it comes to reducing your risk of any disease and supporting recovery. You can support your health naturally through a variety of dietary and lifestyle strategies and smart supplementation.
While these strategies are not FDA approved to prevent, mitigate, treat or cure prostate cancer, there is data that suggests they are very helpful. Please discuss these with your physician or health care practitioner.
Anti-Inflammatory Nutrition Plan
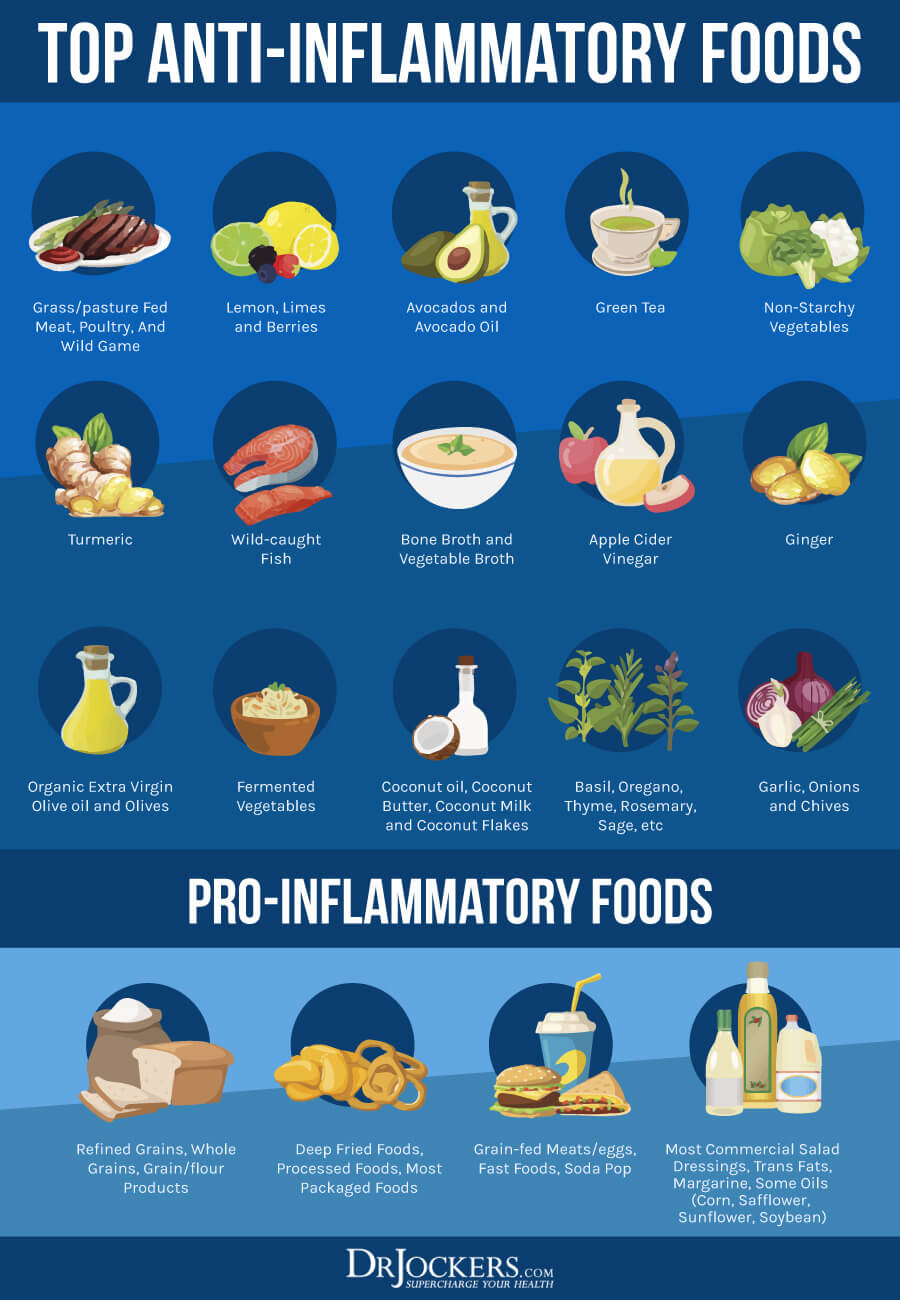
A 2014 review published in Histopathology has found that chronic inflammation may be one of the underlying causes of prostate cancer and an anti-inflammatory and antioxidant-rich diet may help (6). Remove inflammatory foods from your diet, including refined sugar, refined oils, conventional dairy, conventionally raised and processed animal products, gluten, artificial ingredients, highly processed foods, deep-fried foods, and junk food.
Fuel your body with plenty of greens, vegetables, herbs, spices, fermented foods, low glycemic index fruits, healthy fats, and clean animal protein, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
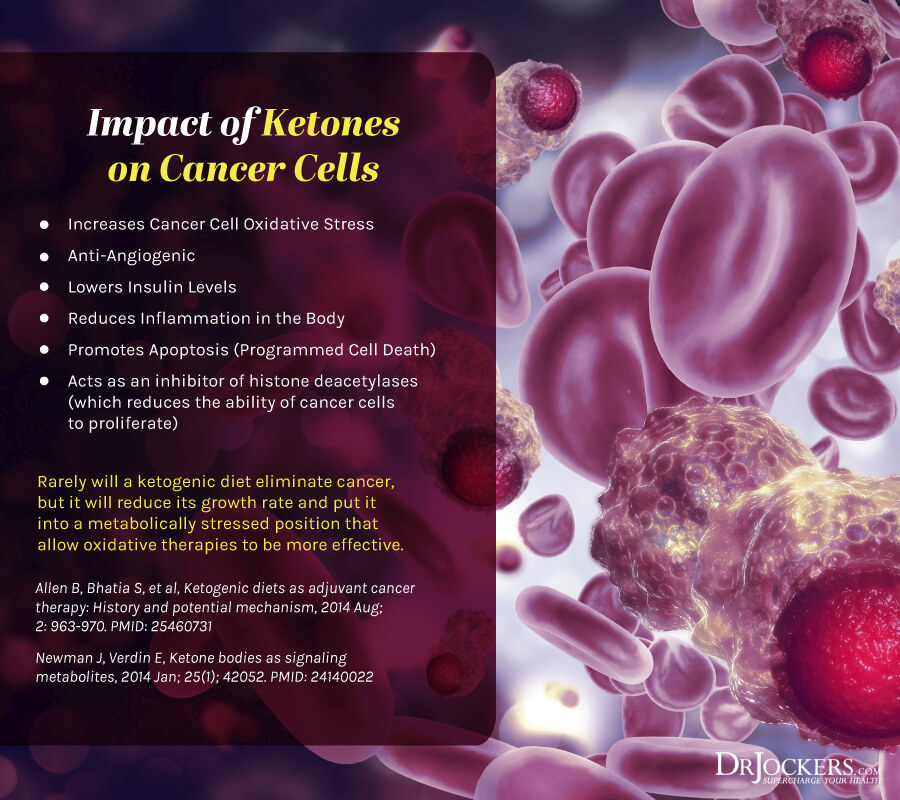
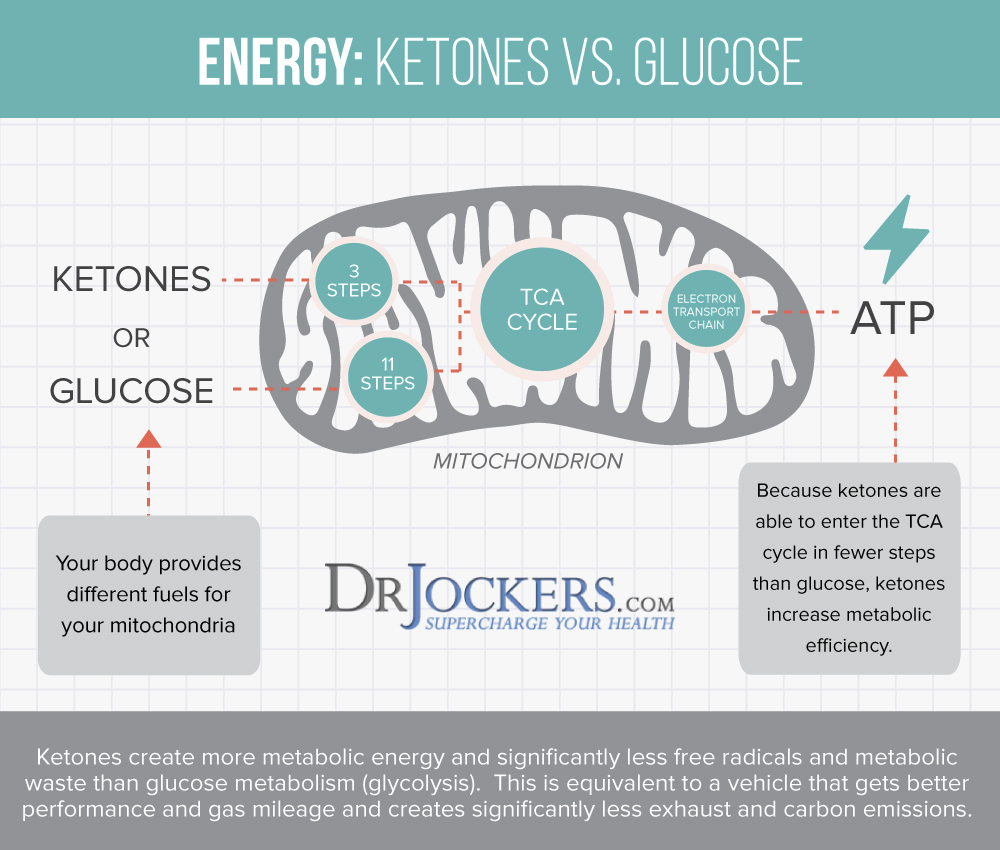
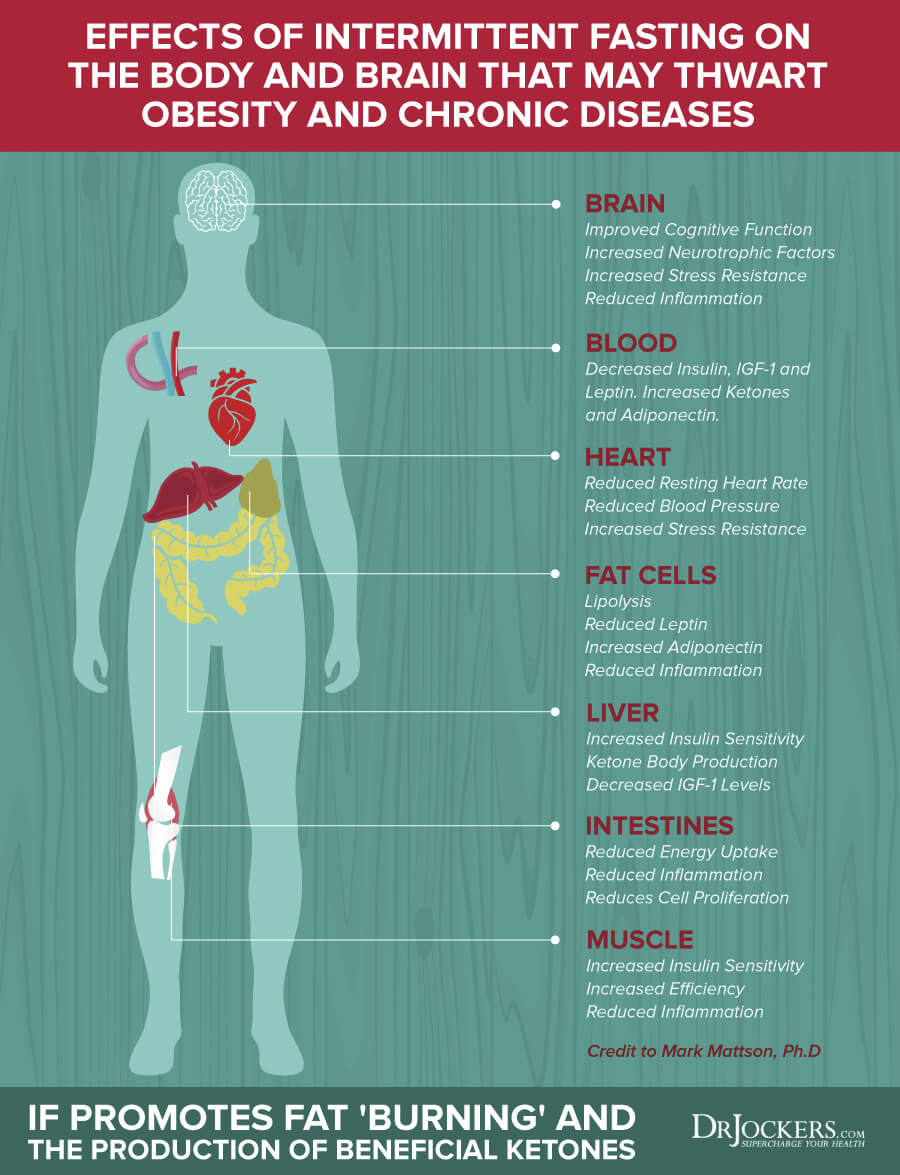
Get Into Ketosis
Usually, your body burns glucose for energy. When your body doesn’t have enough dietary glucose to burn for energy as a result of carbohydrate restriction, caloric restriction, or fasting, it will turn to fat for energy instead and starts to make ketones in the process. Ketosis has many health benefits from reduced inflammation, increased insulin sensitivity, improved cellular renewal to a decreased risk of disease.
The ketogenic diet is a great way to get into ketosis, which may help to improve your health. A 2019 study published in Current Opinions in Oncology has found that diet may play a role in the risk and progression of prostate cancer and following a low-carbohydrate or ketogenic diet may help weight loss and metabolic markers that may reduce the risk of the disease (31).
A 2010 study published in Cancer Prevention Research has also examined the role of a low-carbohydrate diet in prostate cancer and has found that consuming less than 20 percent of carbohydrates offers benefits for the disease (32).
Real Food Keto Diet:
To follow the ketogenic diet, keep your carbohydrate levels very low at 5 to 10 percent, your protein levels moderate at 20 to 30 percent, and your fats high at 65 to 70 percent of your calories. Make sure to eat an anti-inflammatory diet with nutrient-dense whole foods as described above, instead of only focusing on your macronutrient ratios through fatty junk food.
Most of your diet should be made up of healthy fats, including avocados, coconut oil, coconut butter, coconuts, avocado oil, extra-virgin olive oil, pasture-raised butter and ghee, flax seeds, hemp seeds, chia seeds, pumpkin seeds, other seeds, olives, nuts, and any fats from clean animal foods, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game. To learn more, read this article about a real food keto diet.
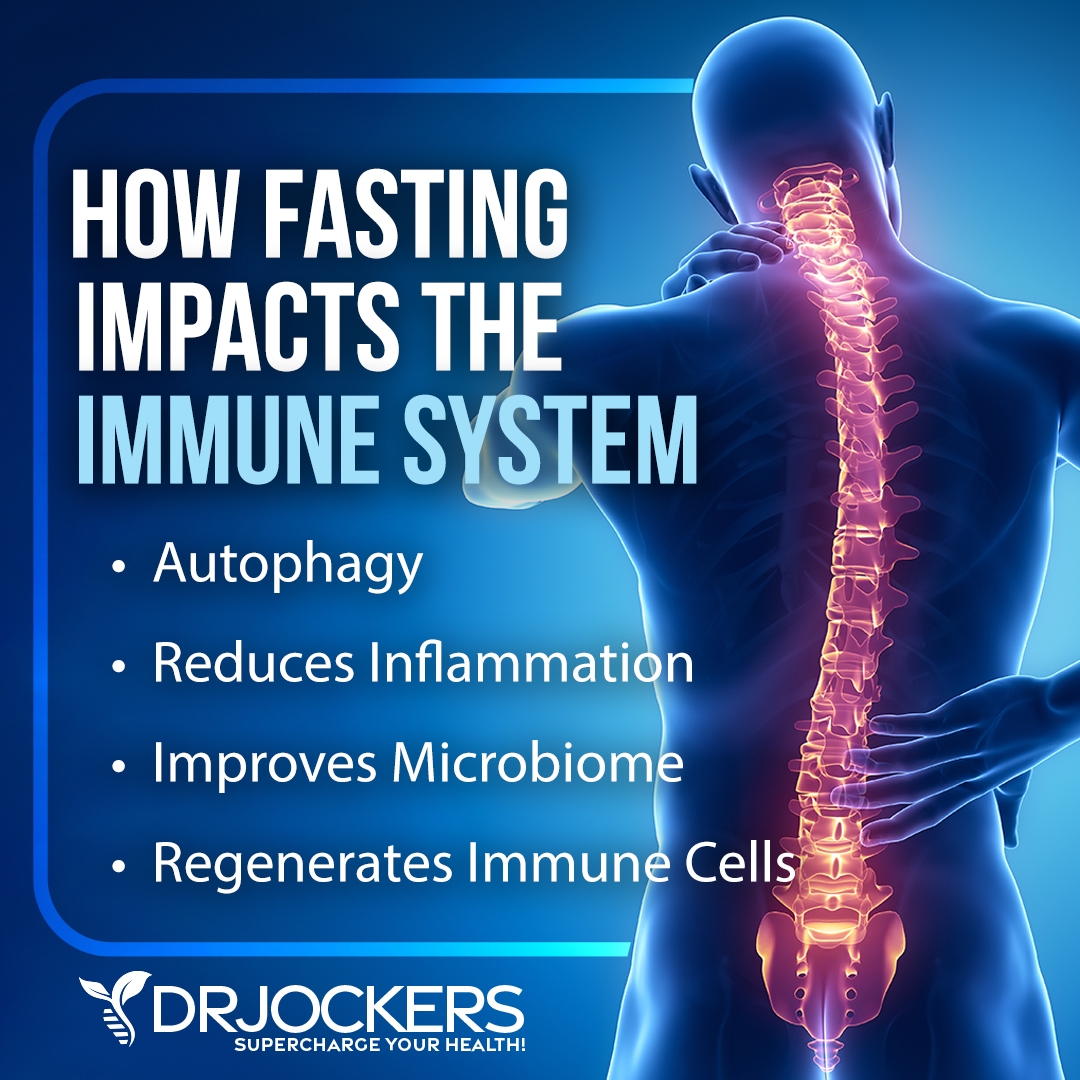
Intermittent Fasting
Fasting is another great way to get into ketosis and support a ketogenic, anti-inflammatory diet. Fasting offers many other health benefits, including for cancer. According to a 2018 study published in the National Reviews Cancer, fasting may support cancer treatment methods without serious risks or side effects (33). There are a variety of ways to fast.
Intermittent fasting is a way of eating that cycles between periods of fasting and periods of eating within one day. If you are new to intermittent fasting, you may start with the Simple Fast that involves 12 hours of fasting including your overnight sleep.
You may start your fast after dinner and don’t eat for 12 hours until breakfast. During your eating window, focus on a nutrient-dense, anti-inflammatory, and ketogenic diet to meet your nutrient and caloric needs. Gradually increase your fasting window until you reach your sweet spot. Most people do the best with a 16-hour fasting window using the 16:8 method.
Partial Fasting:
If you are ready to challenge yourself but not quite ready to go completely without food, you may try a partial fast. Partial fasts usually involve a strategy that focuses on liquids or caloric reduction. You may trial a liquid partial fast. Green Juice Fasting focuses on green juices, while Bone Broth Fasts focus on drinking bone broth for a few days.
You may try the Fasting Mimicking Diet® or FMD®, which is a partial fasting plan that is high in nutrients, low in protein, and low in carbohydrates. On Day 1, restrict your calories to 1,100 calories a day. 500 of these calories should come from complex carbohydrates and 500 from healthy fast. About 100 calories or 25 grams of plant-based proteins are also allowed, mainly from nuts. On Days 2 to 5, your calories are restricted to 800 calories only with 400 calories from complex carbs and 400 calories from healthy fats.
You may also turn to a Fat or Keto Fast or the Daniel Fast. The Fat or Keto Fast focuses on eating 500 to 1000 calories a day with 90 percent of those calories coming from healthy fats. The Daniel Fast is a Biblical fast focusing on a plant-based, vegetarian diet for 21 days.
If you are ready and doing well on longer intermittent fasting or partial fasting strategies, you may try an extended fast. During an extended fast or water fast, you are only drinking non-caloric drinks, including purified water and may herbal tea for a day or several days. This strategy is only for those who are experienced in fasting. You may learn about all these fasting methods by searching my website.
Regular Movement and Exercise
A 2018 review published in Obesity Reviews has found that along with diet, exercise may play a role in prevention (9). I recommend that you move your body daily and exercise regularly. Start your day with a bit of stretching, a short walk, or yoga.
Make sure to stay active throughout the day by taking the stairs, getting up to stretch, shaking out your body, taking a midday stroll, playing with your kids or pets, dancing to your favorite song, and walking or biking instead of driving whenever possible. At the end of the day, you may try a fun dance session, an evening walk, yoga, or some stretching.
Exercise regularly, at least 20 to 30 minutes a day 5 days a week. Mix up cardiovascular exercises, such as brisk walking, hiking, jogging, biking, swimming, dancing, or trampoline workouts, strength and resistance training, such as weight lifting, bodyweight workouts, resistance band exercises, kettlebell training, CrossFit, or TRX, and low-impact activities, such as yoga, pilates, or Barre workouts. High-intensity interval training (HIIT) is a smart way to get your cardio, strength workout, and resistance workout in within a short yet effective session.

Reduce Stress and Prioritize Good Sleep
A 2017 study on 1933 men published in Frontiers in Oncology has found that stress may increase the risk of prostate cancer, while a 2013 study published in Cancer Epidemiology Biomarkers Preview has found that insomnia and other sleep disturbances may contribute to the development of prostate cancer (10, 11, 12). Reducing your stress levels and prioritizing sleep is important for your health.
Reduce stressful activities and interaction with people who bring you down as much as possible. Seek relaxing and uplifting activities and interactions. Learn to deal with stress better. Seek a supportive community and spend time with supportive people. Make sure you have a daily designated ‘me-time’ no matter how short it may be. Try practicing meditation, breathwork, guided relaxation, visualization exercises, progressive muscle relaxation, journaling, gratitude, and prayer.
To improve your sleep, aim to go to bed and wake up every day around the same time to support your circadian rhythms. Avoid electronics, food, sugar, caffeine, alcohol, and stress in the evening before bed. Seek relaxing activities and meaningful connections. Try taking a healing bath, drinking herbal tea, and using some calm essential oils.
Make sure that your bedroom is a calming and safe sanctuary. Leave any arguments out of your bedroom and commit to never go to bed angry. Having a gratitude practice with your spouse before sleep is a nice idea. You may practice the same with your children as well. Invest in blackout curtains or an eye mask, comfortable pillows and bedding, and a supportive mattress.

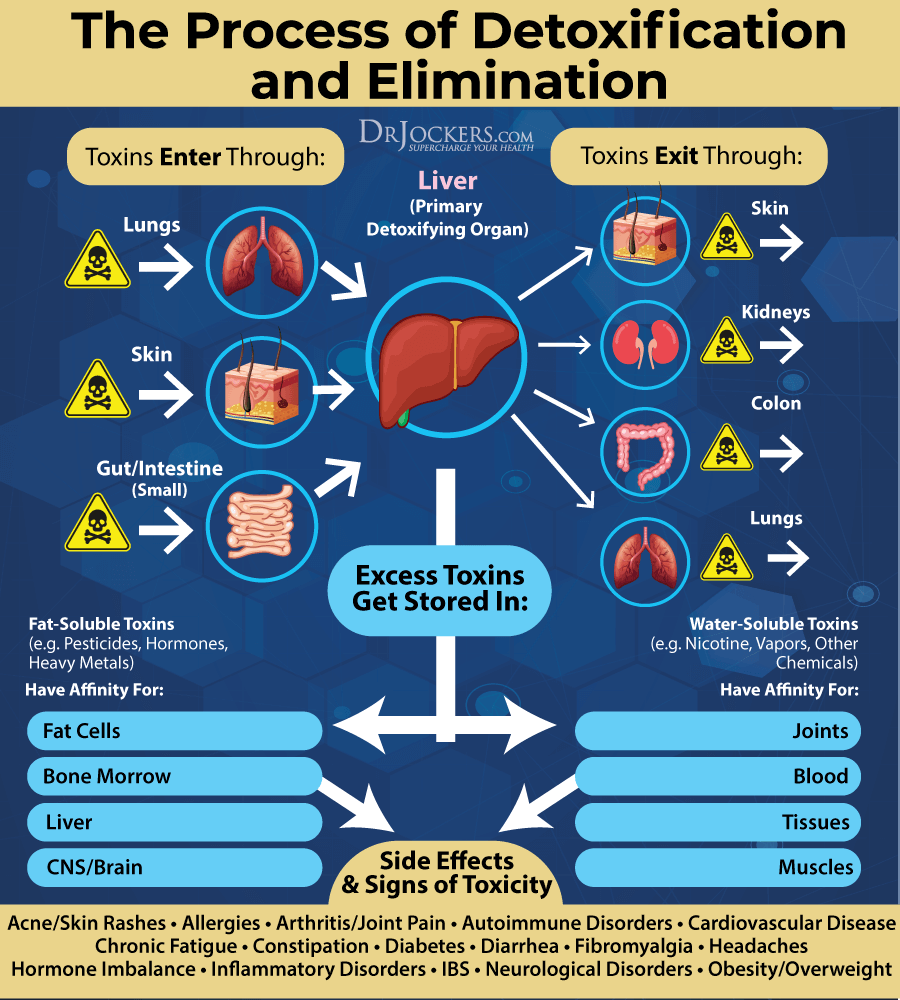
Open up Detoxification Pathways
We know from research that heavy metal toxicity may increase your risk and progression of prostate cancer (18, 19, 20, 21, 22, 23, 24, 25). Opening up your detoxification pathways is very important. Support your digestion, absorption, and elimination pathways through a healthy diet.
Support detoxification through the skin by sweating through exercise and infrared sauna use. Make sure that your amalgam mercury fillings are all removed at a biological dentist.
Try activated coconut charcoal that binds to heavy metals and toxins, supports the elimination of these toxins and reduces oxidative stress and inflammation. I also recommend Bioactive carbons derived from multiple sources of humic acid, fulvic acid, and humic acid that supports the removal of heavy metals and other toxins and improves detoxification pathways. I recommend working with a functional health practitioner that can help you with specific heavy metal detox supplements and other supplementation for detoxifying from other toxins or infections.
Improve Vitamin D Levels
Studies have shown that vitamin D deficiency can increase your risk of prostate cancer (13, 14). To improve your vitamin D levels, it is important that you spend time outside in the sun daily. However, with our indoor lifestyle and many of us experiencing cloudy, gloomy, rainy, or snowy weather a large part of the year, sunshine is usually not enough for optimizing your vitamin D levels.
Eating foods rich in vitamin D, such as fatty fish, liver, and egg yolks, is important, but not enough. Daily supplementation is important. Using only vitamin D supplements is not enough, however, you also need vitamin K2 for proper absorption and calcium utilization. This is why, I recommend a daily Vitamin D3/K2 supplement to optimize vitamin D levels.
Typically taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for diseases like prostate cancer is going to be between 70-100 ng/ml.
Improve Zinc and Selenium Levels
We know from research that poor zinc and selenium levels may increase the risk of prostate cancer (15, 16, 17). Food sources of zinc include meat, shellfish, nuts, seeds, and legumes. However, a daily intake of a zinc supplement is critical for optimal levels.
On the other hand, selenium supplementation is rarely essential. You can easily meet your daily needs by eating two Brazil nuts a day, a nut that’s incredibly high in selenium. Other foods that are rich in selenium include beef, poultry, eggs, shellfish, yogurt, sunflower seeds, spinach, mushrooms, lentils, cashews, and bananas. Usually dietary sources of selenium is enough, however, you may consult with a functional health practitioner to see if you need to supplement.

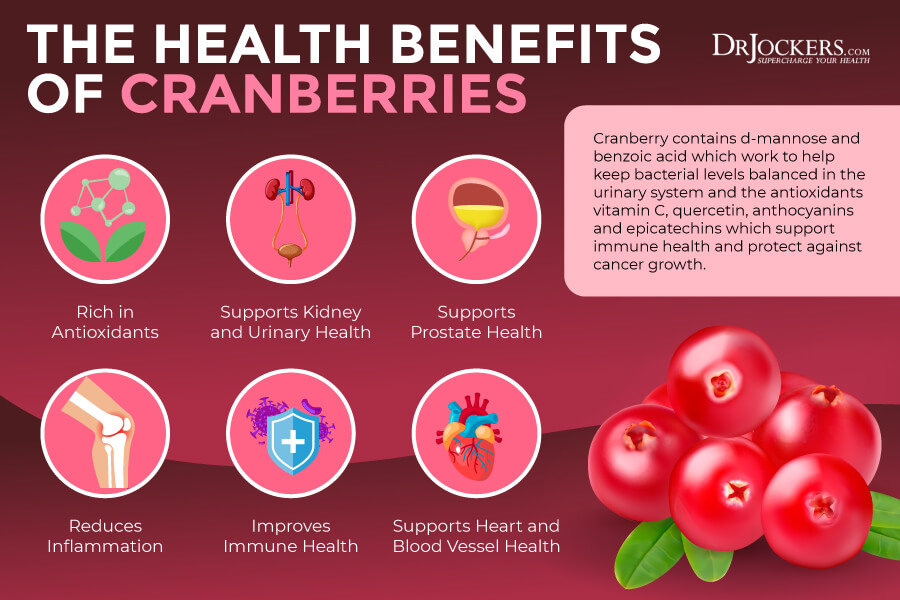
Consider Using Cranberry
Using cranberry may be a fantastic natural support idea. According to a 2016 randomized controlled trial published in the Biomedical Papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia, using cranberry supplementation before radical prostatectomy may offer some benefits for prostate cancer patients by reducing PSA and other prostate cancer markers (34).
You may benefit from consuming cranberry juice and taking cranberry supplements. You may find prostate protection supplements that include cranberries as an agent supporting prostate health and urinary function.
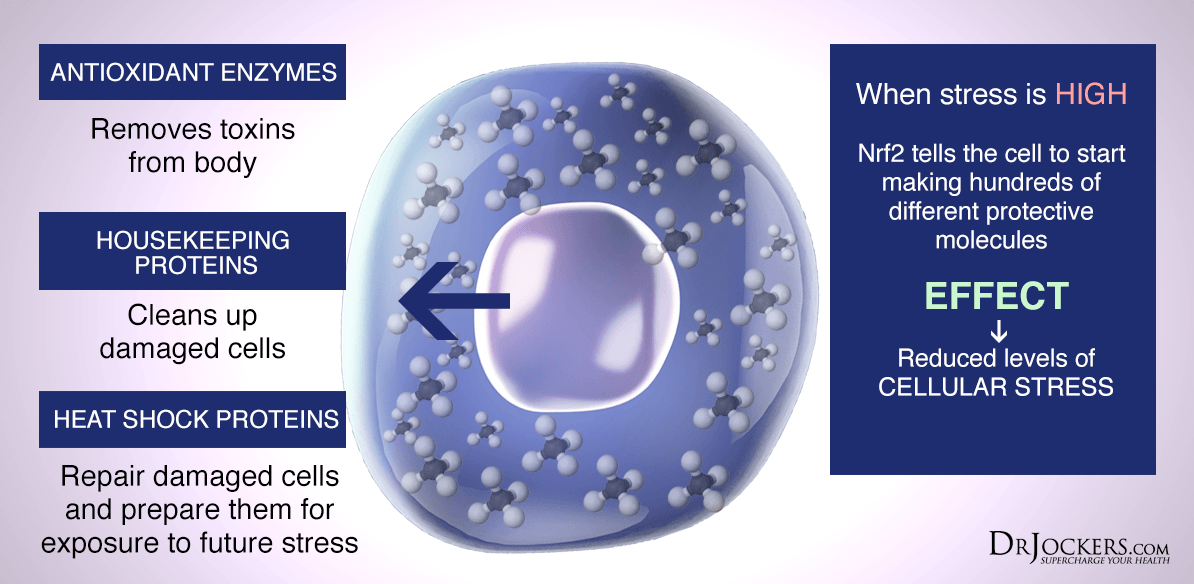
Consider Using Curcumin, Quercetin, and Resveratrol
Research has shown that chronic inflammation is one of the main root causes of prostate cancer and reducing inflammation through an anti-inflammatory diet and herbs may help (6). Curcumin is the active compound of one of the most well-researched anti-inflammatory spices, turmeric.
Quercetin is a plant flavonoid that works well together with resveratrol, a plant compound and antioxidant found in red wine, grapes, and berries. They both offer anti-inflammatory benefits.
A 2019 randomized, double-blind, placebo-controlled trial published in Prostate has found that the oral intake of curcumin may offer anti-cancer benefits in prostate cancer (35). A 2020 study published in Cancers (Basel) has found that using the combination of quercetin and resveratrol may benefit prostate cancer management (36).
These compounds all help to activate the NrF2 antioxidant response element within the cells that protect cells from oxidative stress. I recommend supplementing with all these compounds. You can find some high-quality supplements for inflammation defense that include all there, curcumin, quercetin, and resveratrol, and possibly some other anti-inflammatory herbs.
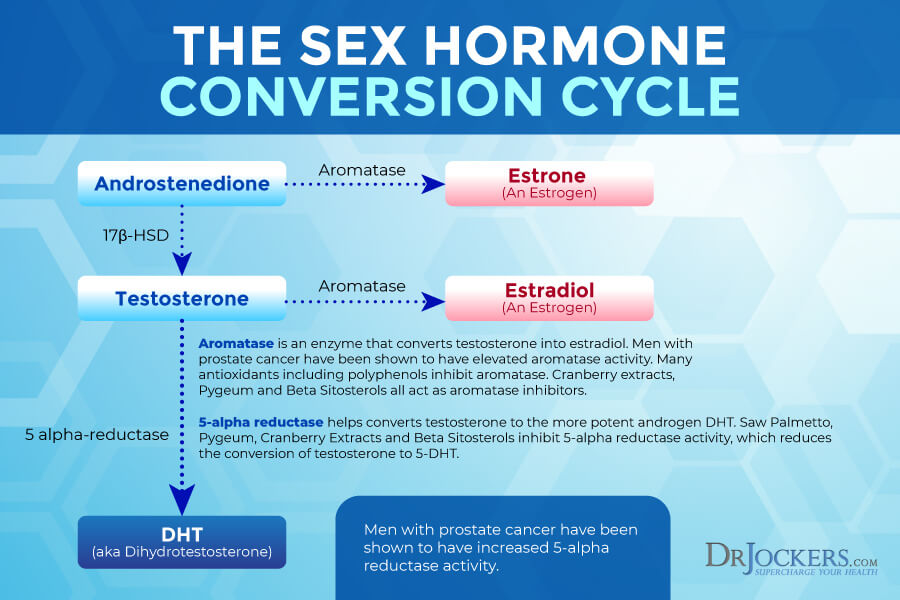
Consider Using Saw Palmetto, Pygeum, and Beta-Sitosterol
Saw palmetto is a form of palm commonly used as a supplement for a variety of benefits, especially for men, including improved prostate function, better urinary health, reduced inflammation, improved testosterone levels, and reduced hair loss. According to a 2007 study published in the International Journal of Oncology, saw palmetto may benefit prostate cancer (37).
Pygeum is an herbal extract from an African cherry tree offering various health benefits, including reduced inflammation and improved urinary health. A 2007 study published in Endocrine has found that phytosterol pygeum may help to reduce the risk and help the treatment of prostate cancer (38).
Beta-sitosterols are a plant substance that may help to improve cholesterol levels. According to a 2000 review published in Cochrane Database of Systematic Reviews, beta-sitosterols may reduce the symptoms of benign prostatic hyperplasia (39).
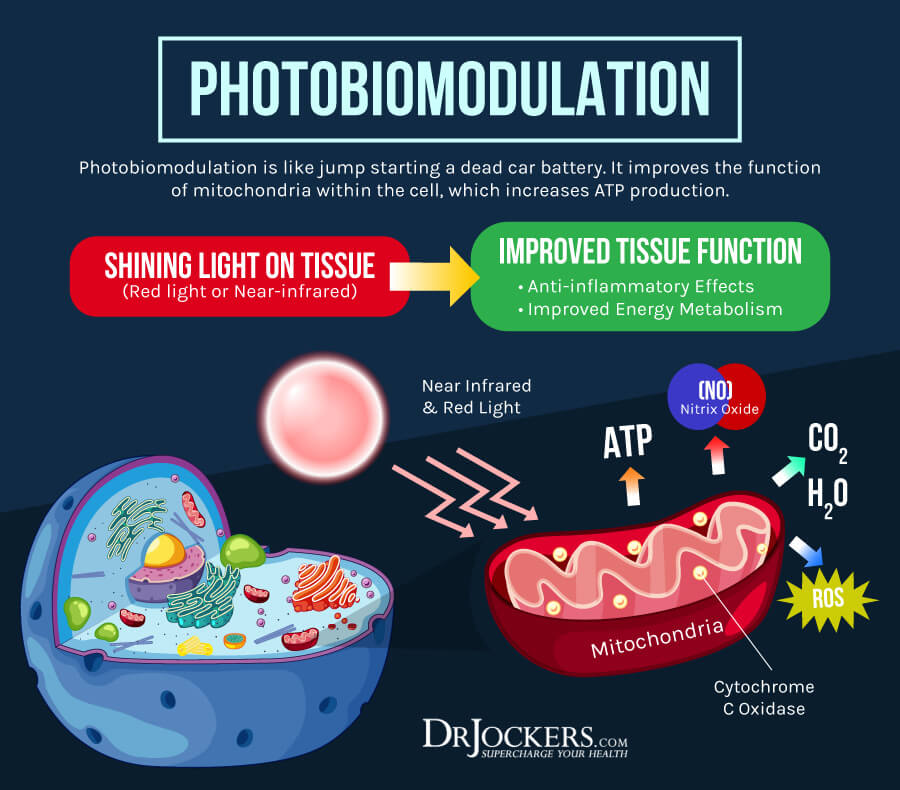
Consider Using Red Light Therapy
Red light therapy (RLT) is a powerful therapeutic technique and an alternative healing method. It uses red low-level wavelengths of light for a variety of therapeutic purposes, including reduced inflammation, better sleep, and more energy. According to a 1985 in-vitro study published in the Journal of Urology, photodynamic therapy may be a beneficial treatment method for prostate cancer (40). A 2012 preliminary animal study published in Photomedicine and Laser Surgery has found that red light therapy for 37 days has reduced tumor growth in 330 measured tumors (41).
You can use red light therapy at home. There are some high-quality, affordable, and small red-light therapy devices on the market. Using red light therapy is simple. It can become a relaxing self-care routine. Remove your clothes leaving only your undergarments, such as underwear and socks on. Sit or stand 4 to 6 inches from your red light therapy device.
Start with 1 to 2 minutes at first, but gradually increase the time and treat each affected area for 5 to 15 minutes. You may also use a full-body red light therapy device for 12 to 20 minutes (6 to 10 minutes on each side). Use your red light therapy device 4 to 10 times a week allowing at least 6 hours between sessions.
Final Thoughts
Prostate cancer is a form of cancer that affects the prostate gland. There are about 248,530 new cases of prostate cancer each year. When caught early, the chances of successful treatment is high, however, screening and prevention is important for reducing your risk and increasing the chance of a positive outcome (1, 2, 3).
I recommend that you follow my natural support strategies for prostate cancer, including my dietary and lifestyle recommendations and supplementations I outlined to support your health and improve your well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



You are inspirational Dr Jockers. I long for the day when I see doctors properly trained AND treating the patient holistically And in his or her patient’s best interests. They have lost their way and could take not just a leaf out of your NMD training and values. Your leadership in functional medicine is to be applauded. Thank you!