 Using Butyric Acid to Heal Leaky Gut and Improve the Microbiome
Using Butyric Acid to Heal Leaky Gut and Improve the Microbiome
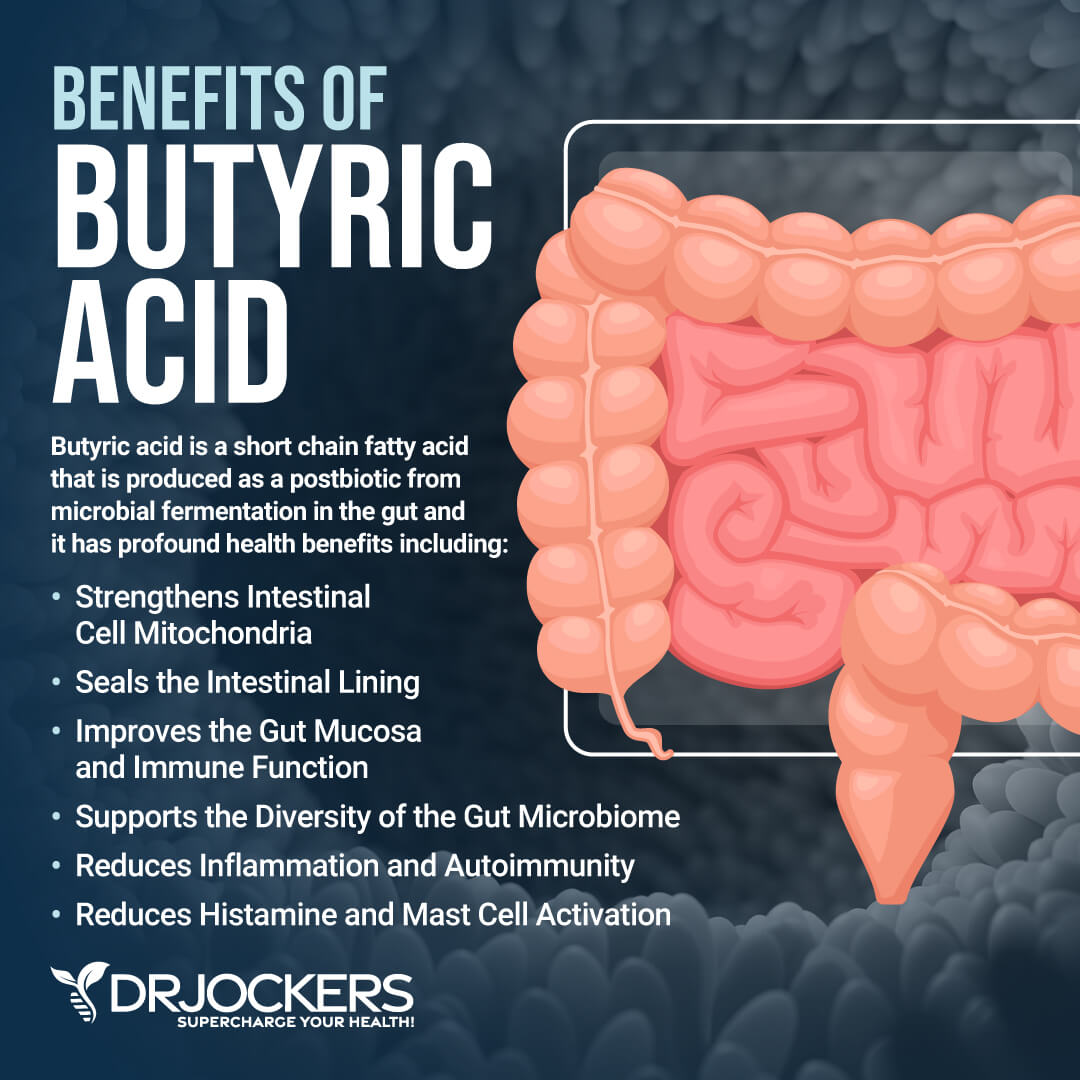
Butyric acid is a short-chain fatty acid (SCFA). It is made in your colon mainly through the fermentation of dietary fiber by beneficial gut bacteria.
Butyric acid has a lot of health benefits, including strengthening the intestinal cell mitochondria, sealing the intestinal lining, improving the gut mucosa, supporting immune function, supporting the diversity of the gut microbiome, reducing chronic inflammation, decreasing autoimmunity, reducing histamine levels, and decreasing mast cell activation. Improving butyric acid levels is important for improving leaky gut syndrome and gut dysbiosis.
In this article, you will learn about the problems with leaky gut and gut dysbiosis. I will go over the link between the cell danger response and leaky gut. You will learn about the connection between mitochondrial function and gut dysbiosis.
I will discuss the importance of probiotics. You will learn what butyric acid is. You will understand the benefits of butyric acid. You will learn what the butyric acid-producing bacteria are. Finally, I will share my best strategies on how to support your butyric acid levels naturally.
The Problem with Leaky Gut and Dysbiosis
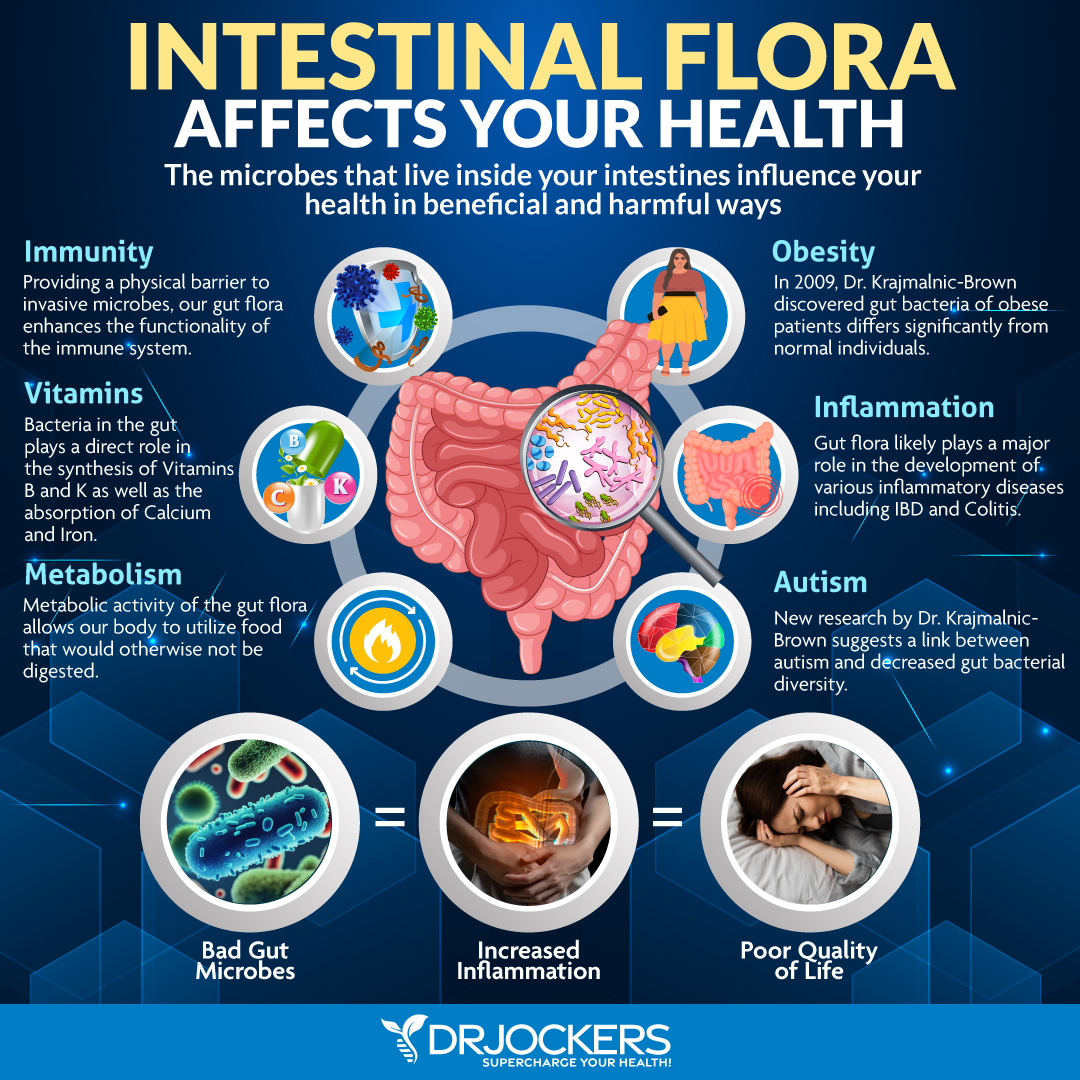
Your gut is home to trillions of microorganisms. Some of these bacteria are beneficial for your body, others are not so much. You need a healthy balance of good and bad bacteria, with more of the good guys, to maintain health.
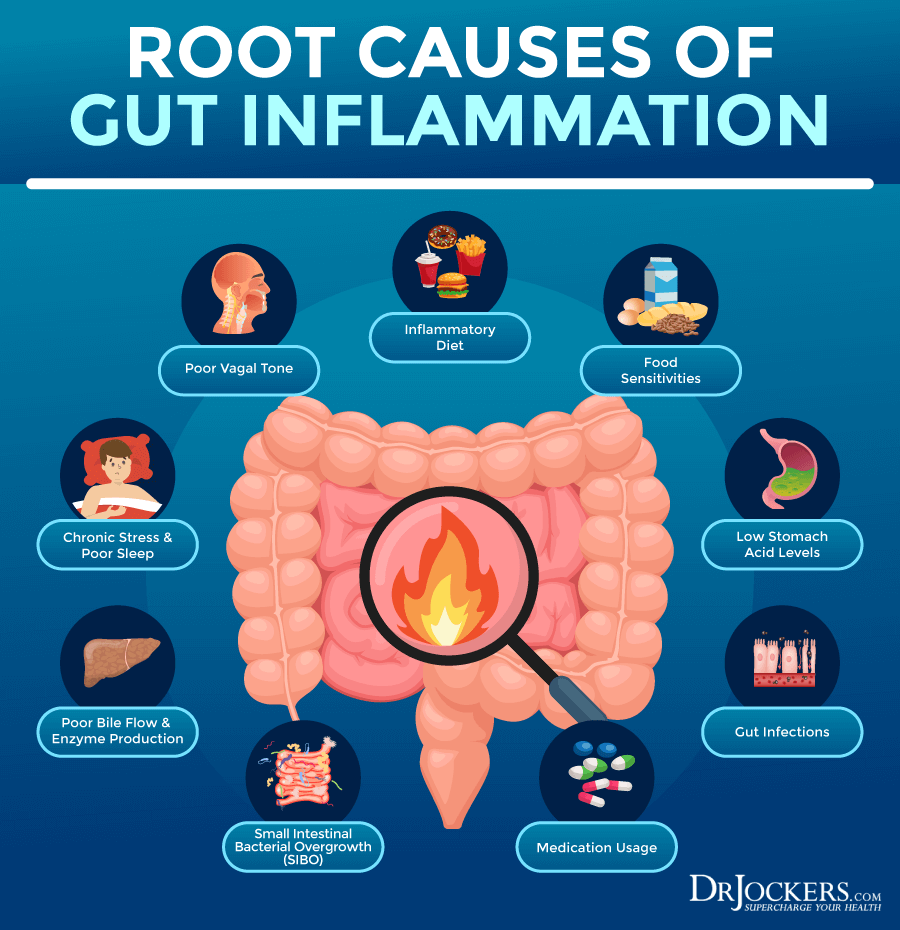
Unfortunately, a poor diet, environmental toxin exposure, stress, unhealthy lifestyle choices, antibiotics, other medication use, and other factors can result in gut microbiome imbalance, also called gut dysbiosis. Gut dysbiosis can increase the risk of chronic inflammation, chronic symptoms, and chronic health issues. It may also lead to leaky gut syndrome and related problems.
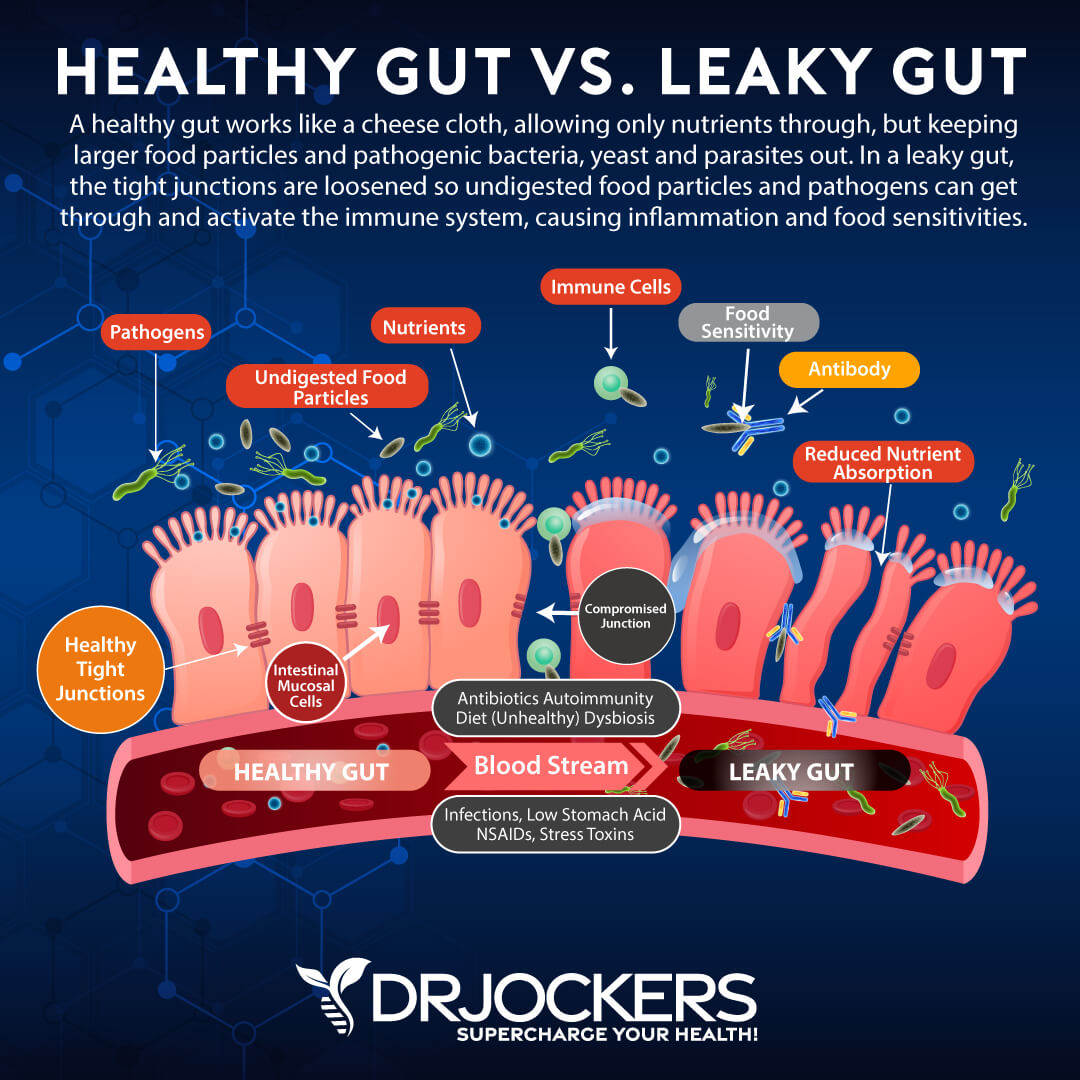
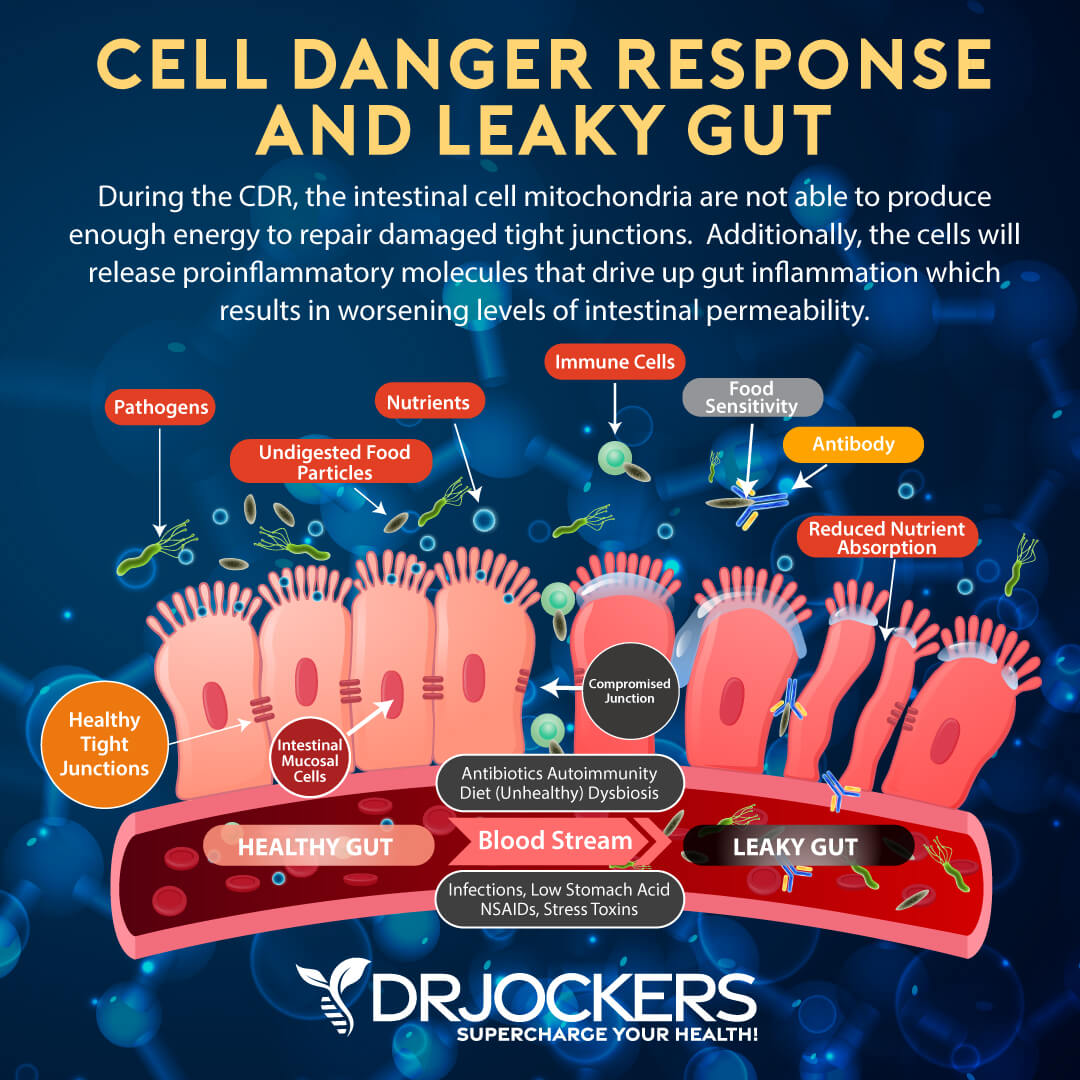
In a healthy body, your gut lining is healthy, it is naturally semi-permeable. This means that your gut lining allows important micronutrients to pass through tiny junctions or holes into your bloodstream.
We are talking about very small gateways that don’t allow microbes, toxins, and undigested food particles to get through to your bloodstream to keep your body healthy. These pathogens and harmful substances will be eliminated through urine and stool instead.
However, inflammatory foods, environmental toxins, chronic stress, gut dysbiosis, infections, and other factors may compromise your gut lining.
Leaky Gut and Chronic Inflammation
Over time these factors can seriously damage your gut lining and break apart these tiny passageways creating bigger holes. When bigger holes develop, your gut lining becomes permeable, and you develop leaky gut syndrome or intestinal permeability.
This means that microbes, toxins, undigested large food particles, and other pathogens can easily pass into your bloodstream and cause serious damage to your body.
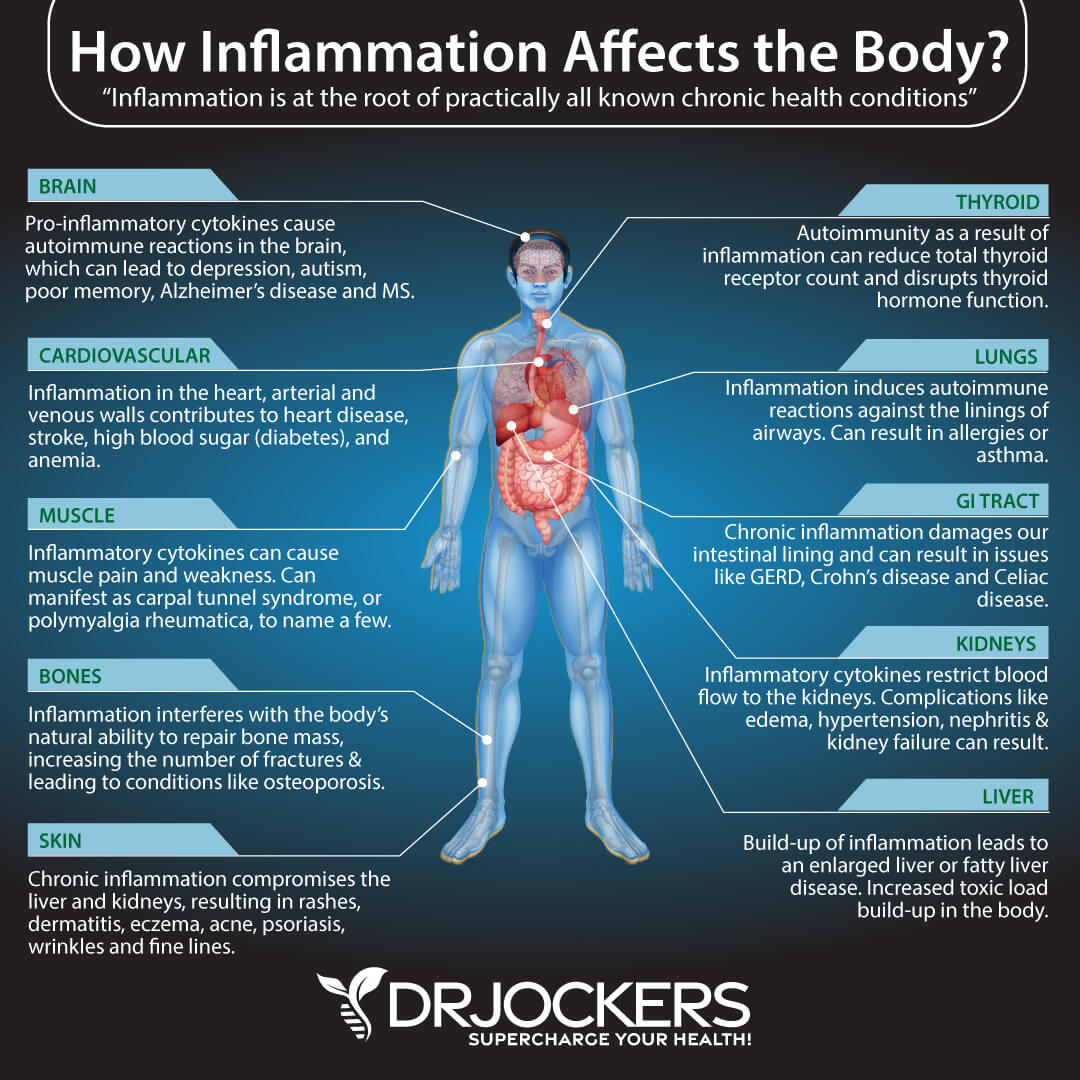
Leaky gut syndrome can increase chronic inflammation, compromise your immune system, and cause chronic health issues. It may result in an ongoing chronic immune response to these foreign substances, which increases the risk of chronic symptoms, autoimmunity, and other health problems.
According to a 2012 review published in Clinical Reviews in Allergy and Immunology and a 2017 review published in Frontiers in Immunology, leaky gut syndrome can increase the risk of intestinal permeability (1, 2).
A 2021 study published in PLoS One has found that leaky gut syndrome may also increase the risk of metabolic health issues (3). Thus, it’s critical that we take leaky gut syndrome and gut dysbiosis seriously to prevent and improve related health issues.
The Cell Danger Response and Leaky Gut
The cell danger response (CDR) is a relatively new theory to explain many chronic illnesses. A 2013 review published in Mitochondrion has explained the cell danger response as a critical evolutionarily conserved metabolic response that is part of your body’s innate defense system (4). It helps to protect your body from any cellular threat, danger, and harm, regardless of if the threat is physical, chemical, or biological. The CDR always aims to maintain homeostasis.
Your body is a very complex system. Cells, that form tissues, organs, and bodily systems, work together to keep your body healthy. While there are many important components in this system, your mitochondria are one of the key players. It is the powerhouse of your cells that creates fuel and energy for your cells, tissues, and organs to function. It’s critical for energy, function, survival, and health.
The mitochondria also serve as energy sensors and cellular defense agents in your cells to help maintain cellular balance and homeostasis. If there is a significant energy drop and the energy supplied is not enough to maintain homeostasis, the mitochondria will recognize this as a threat to balance.
As a response, it will turn its focus from energy production and cellular metabolism to cellular defense. The cell danger response essentially refers to this switch from energy production and cell metabolism to cellular defense.
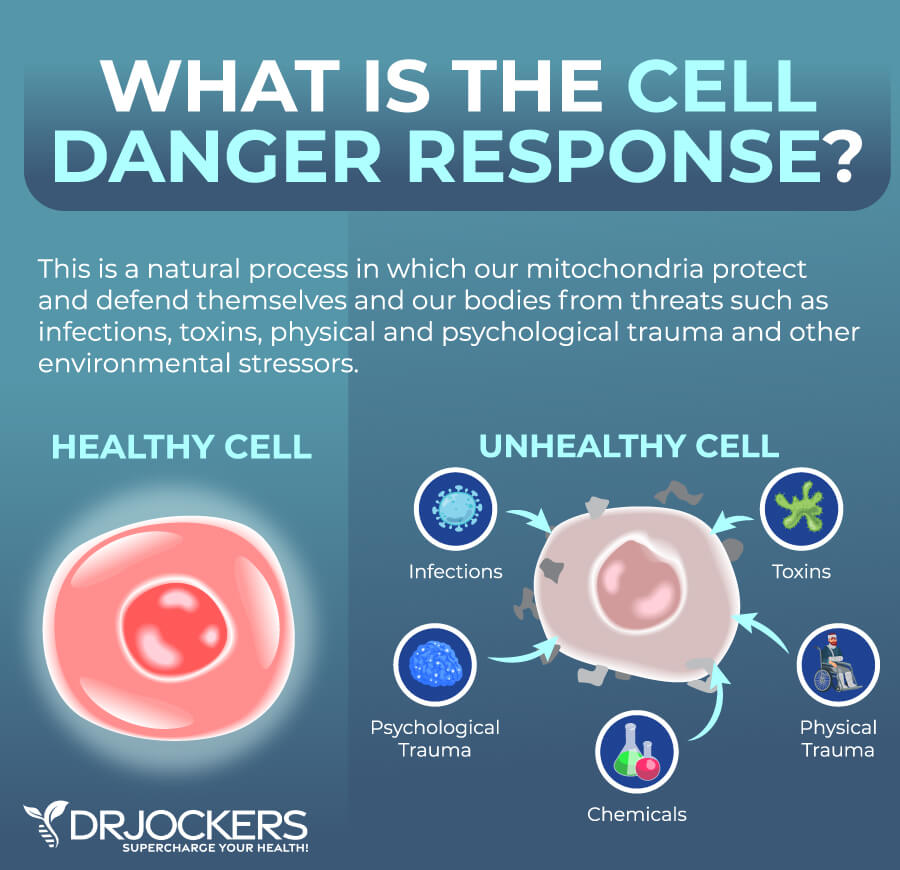
It may not be surprising to hear that the cell danger response and leaky gut syndrome are connected through the mechanism of defense, inflammation, and repair. As mentioned, the cell danger response gets activated if it senses a threat in the body.
The problem is that if the threat is chronic and the response becomes prolonged, it can turn into a problem and the cell danger response can become dysregulated, which may contribute to the development of chronic inflammation and chronic health issues.
As you know, leaky gut syndrome means that your gut lining is damaged, which can lead to chronic immune response and chronic inflammation. When pathogens pass through the intestinal barrier, it will activate your immune system, triggering the cell danger response.

Unfortunately, leaky gut syndrome is a chronic issue. This means a constant activation of the cell danger response which can prevent your cells from returning to normal function. Your body will be in a constant state of defense.
Moreover, when you are in the state of cell danger response, your cells may release various signaling molecules including adenosine triphosphate (ATP), cytokines, and other danger-associated molecular patterns (DAMPs). These molecules may negatively affect gut microbiome balance and further widen tight junctions on your gut lining. This ongoing cell danger response may worsen leaky gut syndrome.
However, a worsening leaky gut syndrome will trigger the cell danger response further. This can turn into a vicious cycle.
Ongoing leaky gut syndrome and persistent cell danger response will only feed chronic systemic inflammation increasing the risk of chronic health issues even further. To stop this cycle and restore balance in the immune system, we need to address both leaky gut syndrome and the cell danger response.
Reduced Mitochondrial Function and Gut Dysbiosis
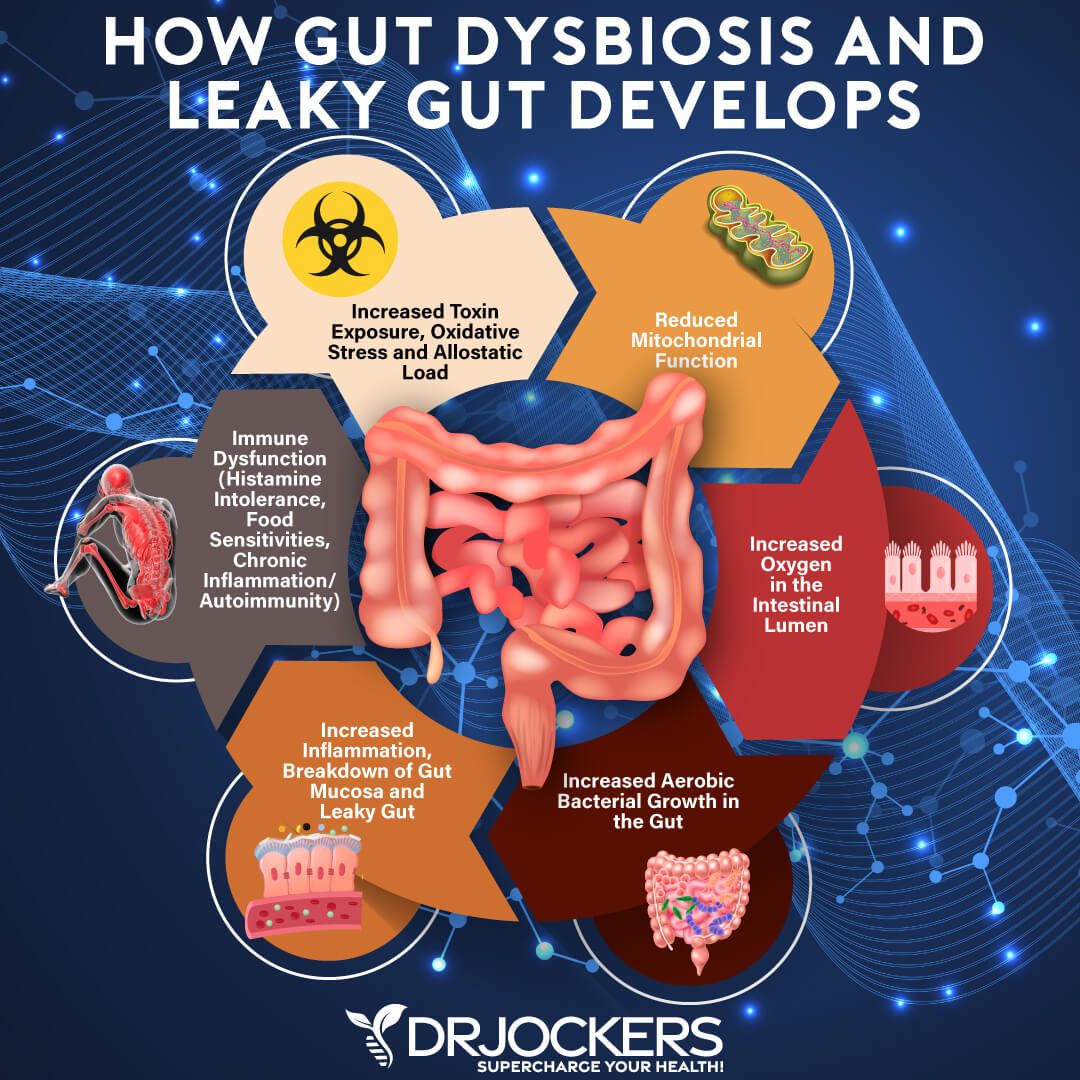
Reduced mitochondrial function and gut dysbiosis are also connected. The mitochondria play a vital role in maintaining cellular energy, regulating immune responses, and allowing healthy functioning.
If the mitochondria are impaired, it will impact the health and function of the cell. If these cells are located in the gut lining, they can compromise the integrity and health of the intestinal barrier, contribute to gut dysbiosis, and impact digestive function.
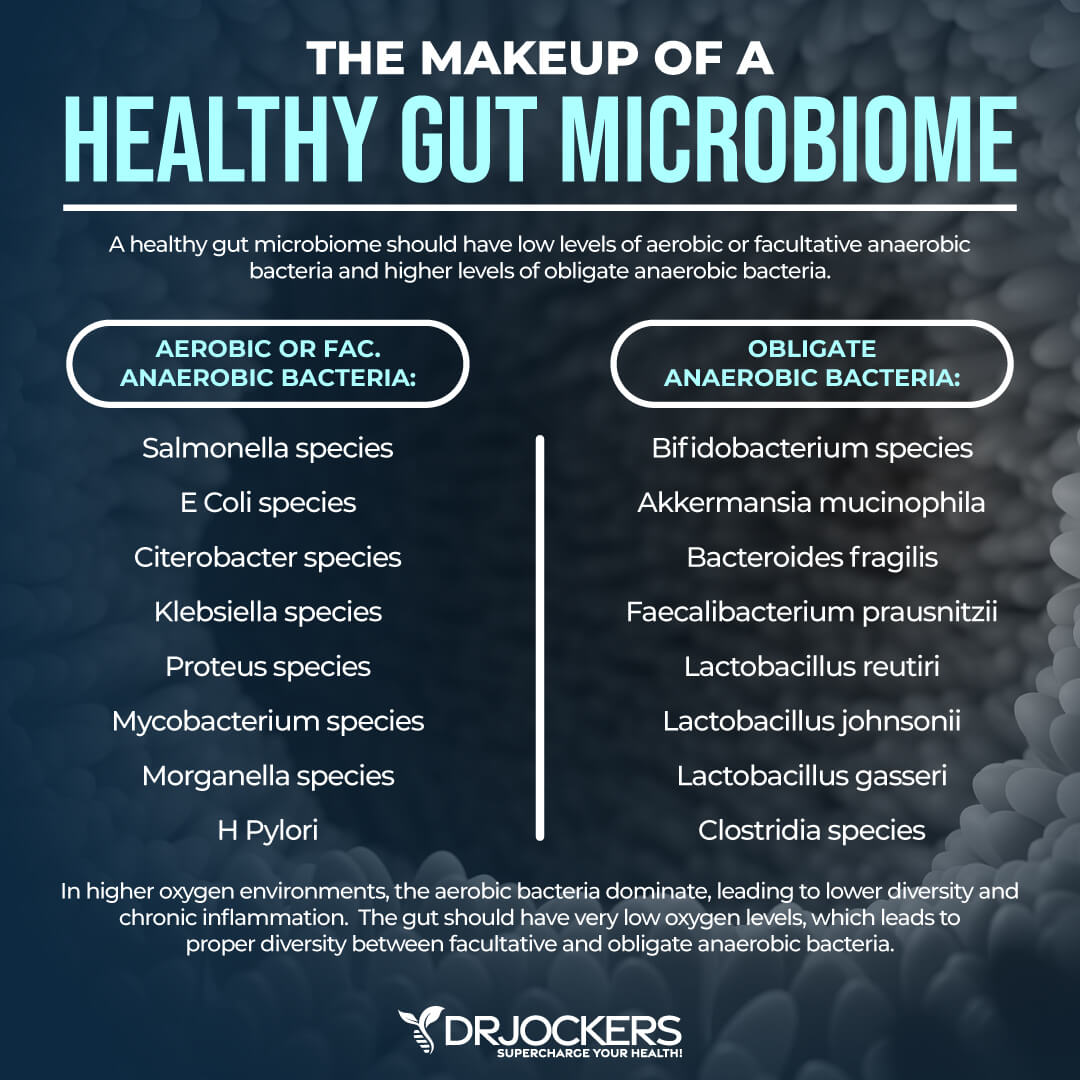
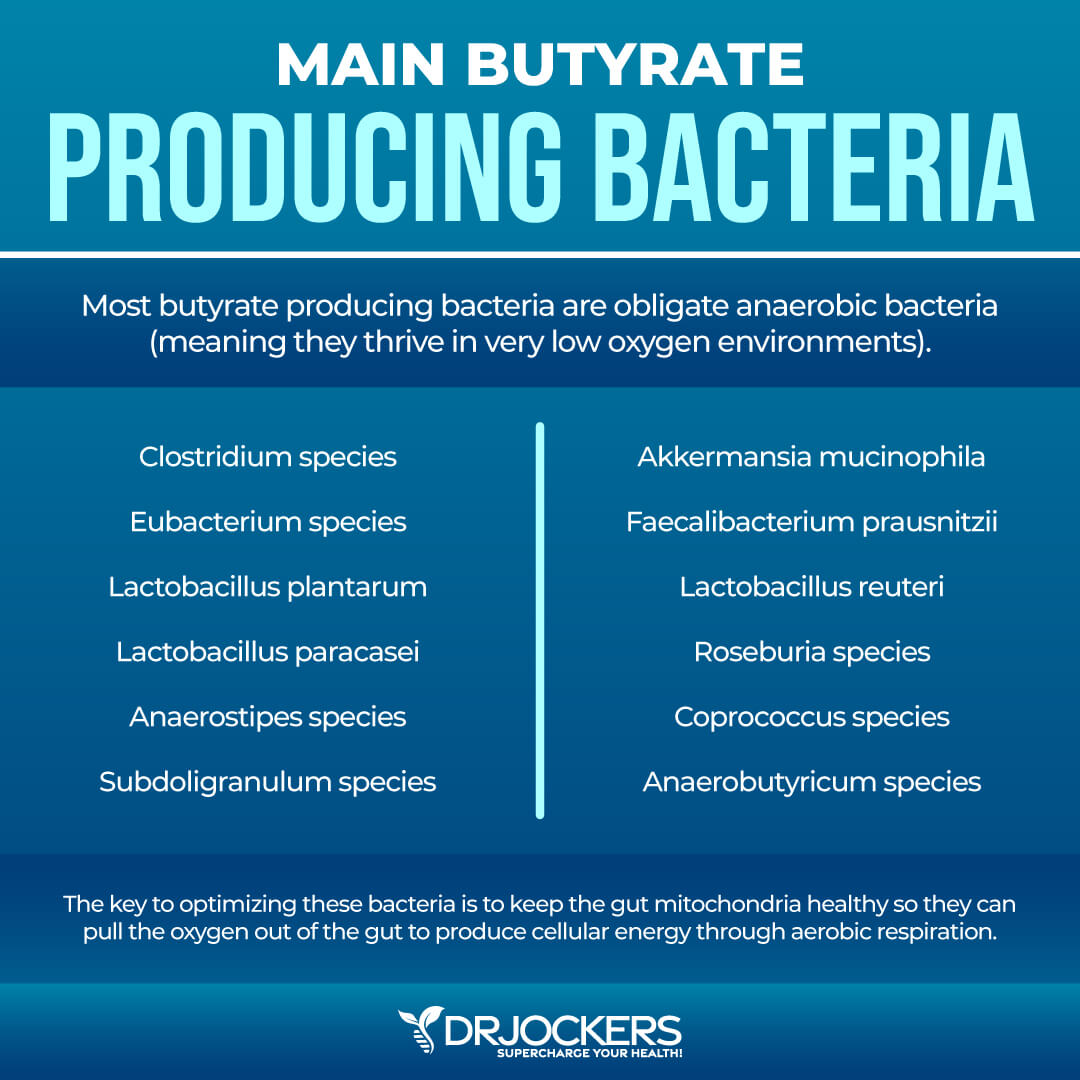
In gut dysbiosis, we see an overgrowth of pathogenic aerobic bacteria. In a normal gut flora, the gut microbiome is dominated by anaerobic bacteria. Anaerobic bacteria thrive in a low-oxygen environment of the healthy colon.
However, if there are gut microbiome imbalances and if the mitochondrial function is compromised and reduced, we can see an increase in oxygen levels in the gut tissues. This will allow aerobic or facultative anaerobic bacteria, including salmonella, E coli, Citerobacter, Klebsiella, Proteus, Campylobacter and Mycobacterium to grow and thrive.
These aerobic bacteria are pathogenic and carry the risk of various gastrointestinal issues, infections, acute and chronic inflammation, immune compromise, and autoimmunity. Some of these bacteria are specifically known as autoimmune triggers and histamine producers.
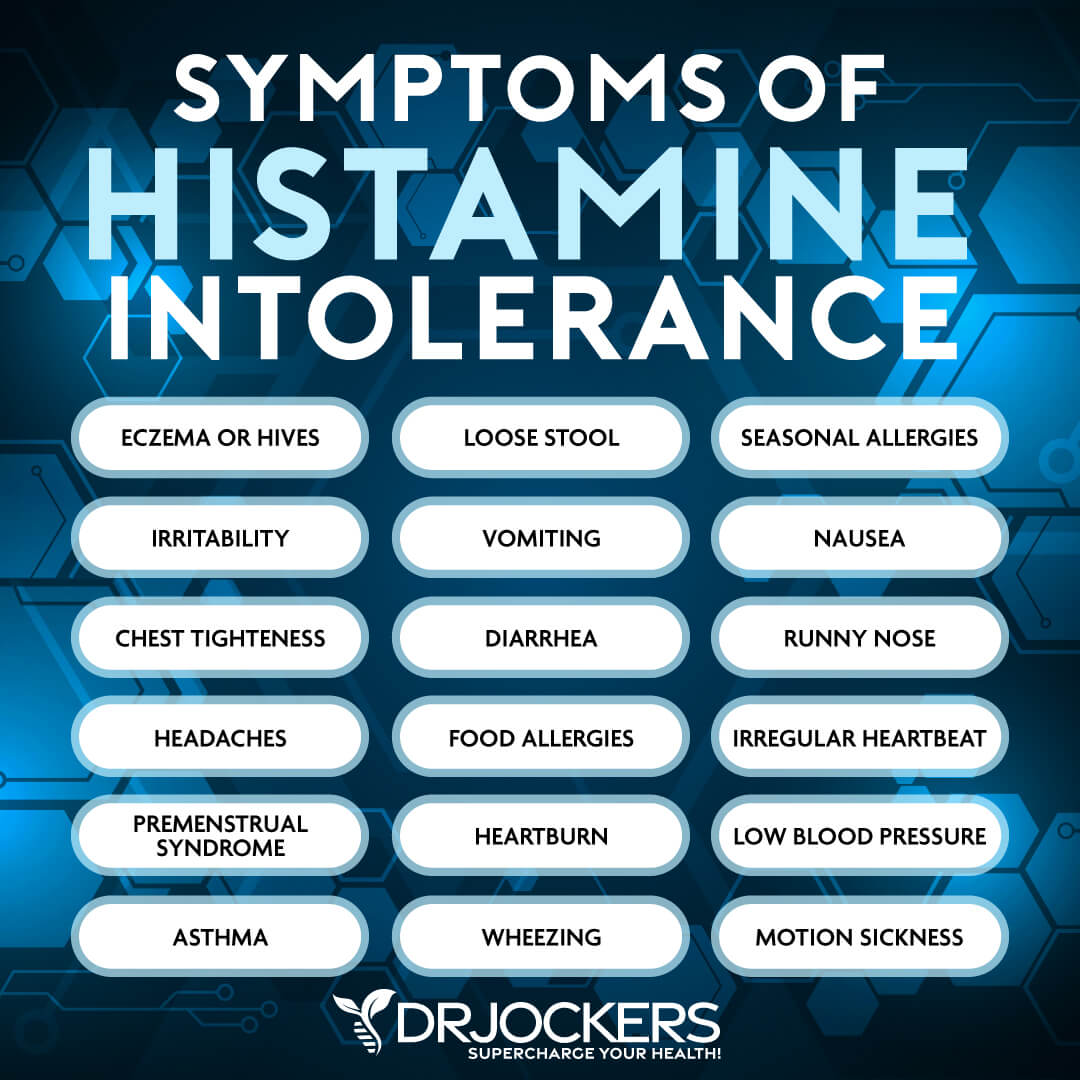
For example, Morganella spp is a gram-negative bacterium that may produce histamine. This can be an issue for those with histamine intolerance. High levels of this bacteria may also mean inflammation and may lead to diarrhea or SIBO. Klebsiella spp., Klebsiella pneumoniae is another gram-negative bacterium found in your oral cavity and respiratory system.
It can lead to abdominal pain, bloating, gas, diarrhea, or symptoms of inflammatory bowel disease. High levels may indicate gut inflammation. It may also release histamine which can be a problem for those with histamine intolerance (5).
Citrobacter spp and Citrobacter freundii are gram-negative bacteria. High levels may mean high inflammation in the gut and may be linked to rheumatoid arthritis. Fusobacterium spp is a gram-negative bacteria found in your mouth and intestines. High levels are associated with inflammation and autoimmunity (5). You can read more about specific bacteria that may trigger autoimmunity or histamine intolerance in this article.
In short, these aerobic bacteria can produce histamine and other inflammatory compounds. This may lead to an excessive immune response and increase pro-inflammatory cytokine levels.
Thus, people with poor mitochondrial function and related gut dysbiosis may experience poor regulation of the immune and inflammatory response and can experience chronic inflammation and immune system-related issues, such as autoimmunity.
Again, this can turn into a vicious cycle. Gut dysbiosis can increase bacterial overgrowth. Bacterial overgrowth can increase mitochondrial dysfunction and chronic inflammation.
This will further increase leaky gut syndrome, immune dysregulation, and autoimmunity, which will then only further contribute to gut dysbiosis. Thus, again, it’s critical that during treatment we focus both on mitochondrial function and gut health. Testing for gut dysbiosis and gut health issues is critical for identifying the right supplements and treatment approaches.
The Importance of Postbiotics?
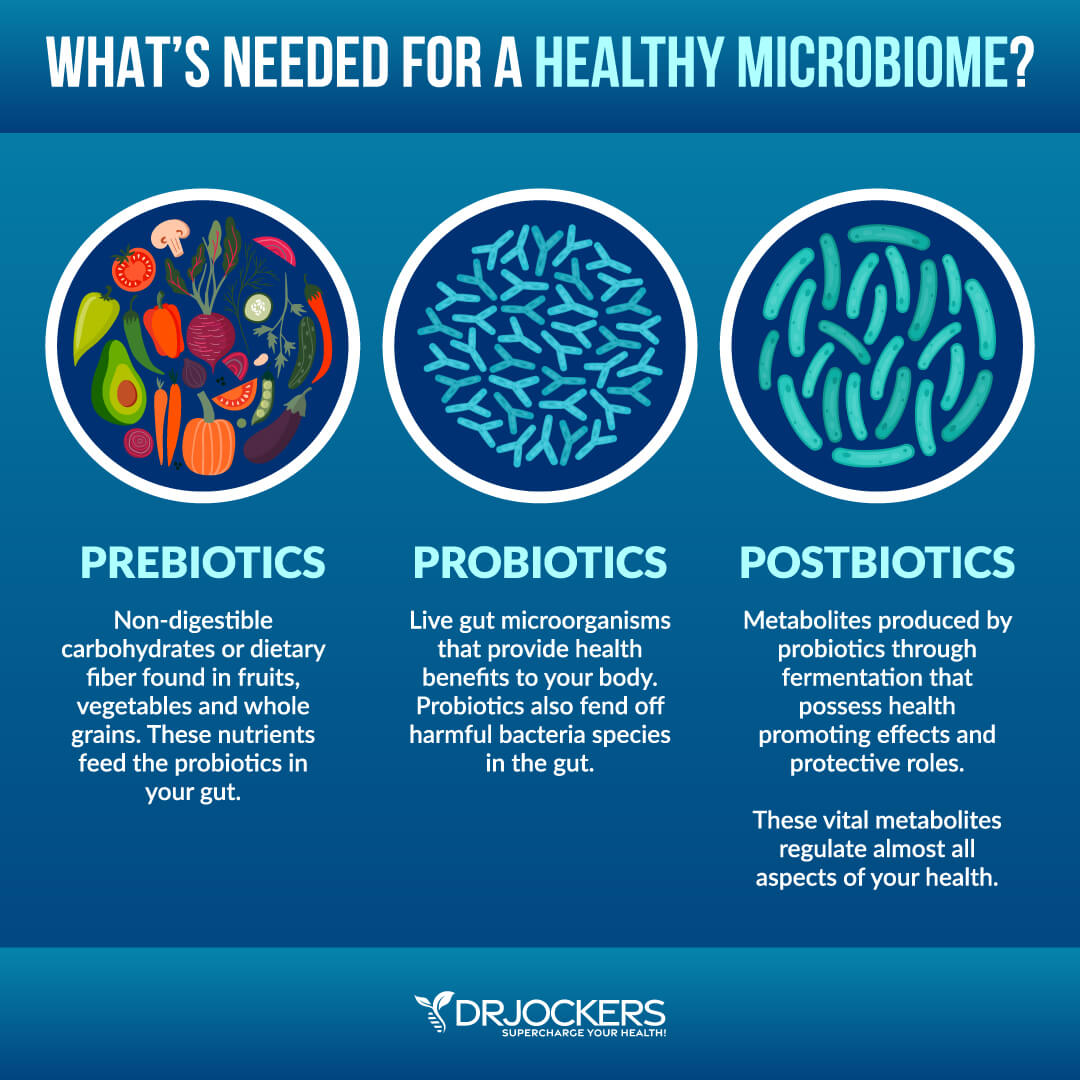
You’ve probably heard about probiotics and prebiotics. How about postbiotics though? Prebiotics are a type of non-digestible dietary fiber found in various plant-based foods, including asparagus, Jerusalem artichokes, apples, dandelion greens, onions, garlic, bananas, leeks, jicama root, and yacon root.
Prebiotics feed the friendly bacteria or probiotics in your gut. This helps to create a variety of important nutrients, including short-chain fatty acids such as butyrate, acetate, and propionate. This process supports a healthy gut microbiome.
Probiotics are healthy bacteria found in your gut. They offer various health benefits, including improved digestion, better immune function, healthier skin, improved mental and brain health, reduced inflammation, and lower risk of disease. Probiotic-rich foods and drinks include fermented vegetables, sauerkraut, kimchi, kefir, yogurt, tempeh, and kombucha. They also come from probiotic supplements.
Postbiotics are metabolites or byproducts of the fermentation process by probiotics in your gut. Probiotics feed on prebiotics and produce probiotics. The three are part of the same process. They complement each other and all play a critical role in your gut health.
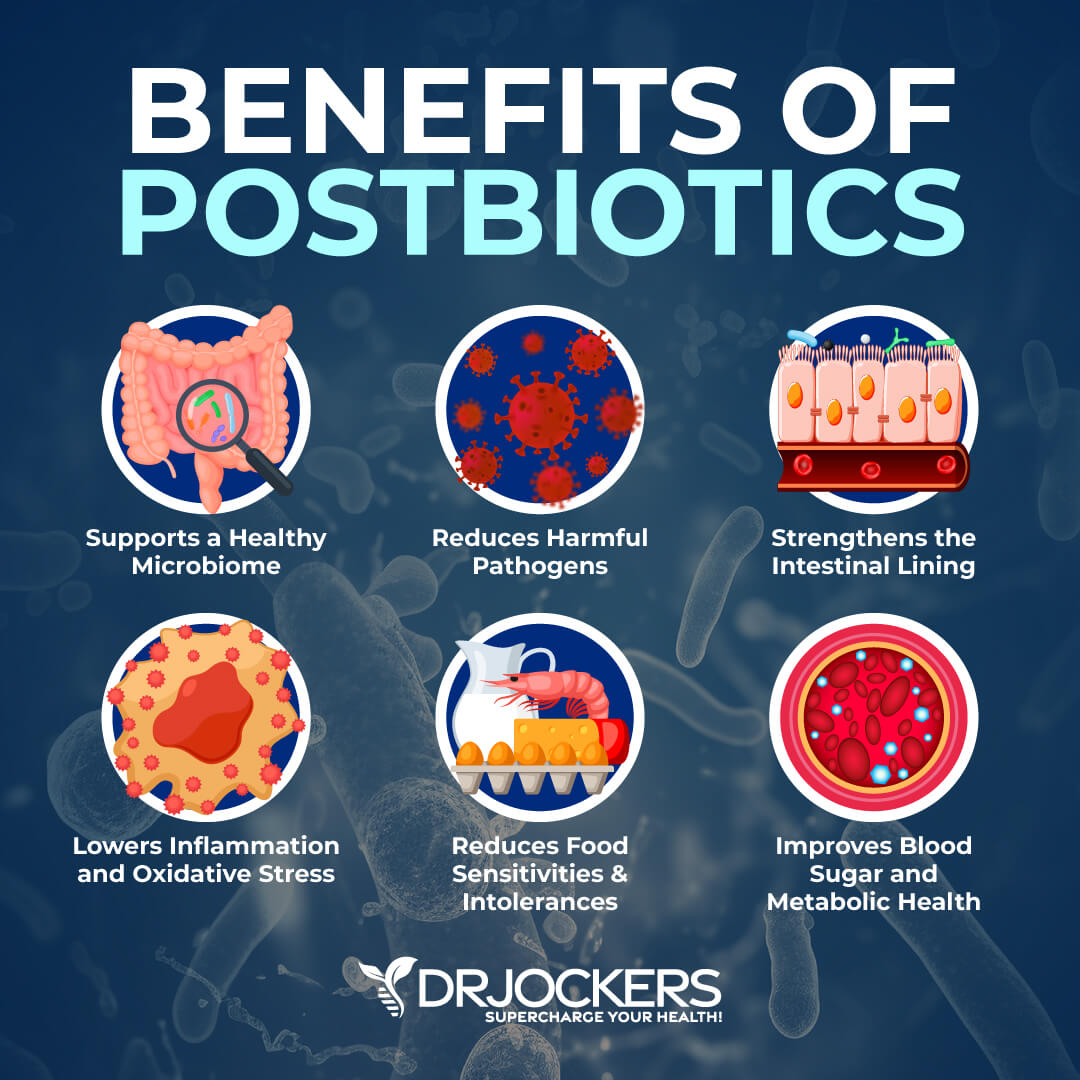
A 2020 study published in Nutrients has found that using postbiotics may be an effective strategy for improved gut health (6). Some of the health benefits people attribute to probiotics actually come from postbiotics.
Postbiotics offer many benefits, including improved digestive health and better immune function. Postbiotics can improve your gut microbiome, reduce infections and bacterial overgrowth, and improve the intestinal lining.
According to a 2014 review published in Current Opinions in Biotechnology, postbiotics from your diet may strengthen your intestinal microbiome (7). A 2020 review published in Nutrients has also noted the potential benefits of postbiotics for your microbiome health (8).
A 2020 systematic review published in Nutrients has found that supplementing with postbiotics may help to reduce the risk and support the treatment of diarrhea, laryngitis, and pharyngitis in children (9). A 2011 study published in Digestive Disease has found that postbiotics may help to reduce diarrhea associated with irritable bowel syndrome (IBS) (10).
According to a 2019 article published in the Journal of Nutrition, postbiotics may be the key to reducing the risk of leaky gut (11). A 2020 review published in Nutrients has also found that postbiotics may help to support the integrity of the intestinal barrier (8). A 2018 review has found that butyrate may offer therapeutic benefits for inflammatory bowel diseases (IBDs) (12).
A 2021 study published in Frontiers in Veterinary Science has found that probiotics from Lactobacillus Plantarum, a probiotic strain, may offer anti-inflammatory and antioxidant properties (13). According to a 2021 review published in Critical Reviews in Food Science and Nutrition, postbiotics may improve immune tolerance and offer a new strategy for food allergies and intolerances (14).
According to a 2014 review published in Gut, butyric and other short-chain fatty acid postbiotics may support the gut microbiome and may help to reduce diabetes and metabolic syndrome (15).
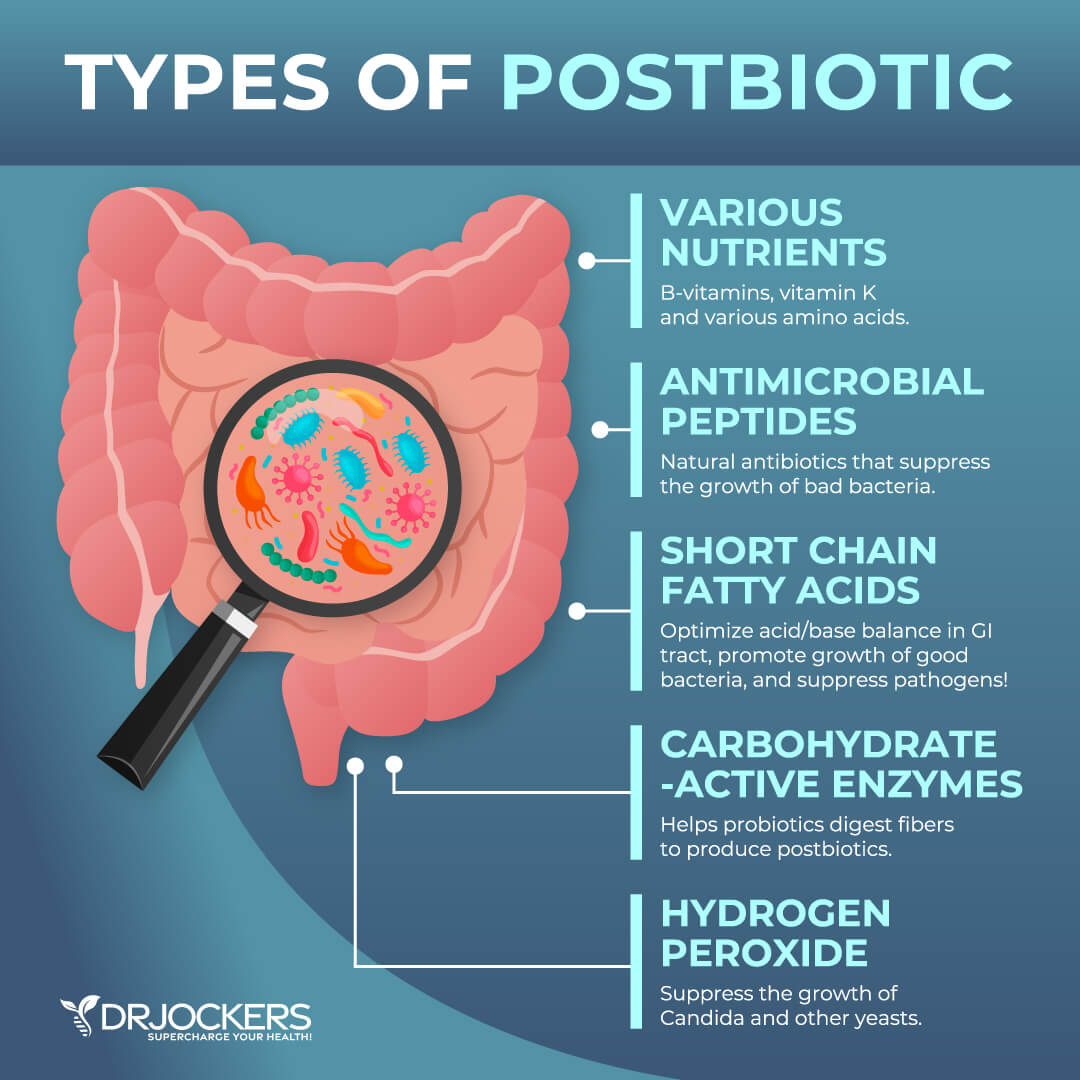
Types of Postbiotics Include:
- Short-chain fatty acids
- Enzymes
- Lipopolysaccharides
- Exopolysaccharides
- Bacterial lysates which are from a mix of bacterial components
- Cell wall fragments
- Cell-free supernatants made by bacteria and yeast
- Vitamins, amino acids, and other metabolites
Good Sources of Postbiotics Include:
- Apple cider vinegar
- Fermented vegetables
- Kefir
- Kombucha
- Postbiotic supplements
What is Butyric Acid?
Butyric acid is a short-chain fatty acid (SCFA) (16, 17). It is made in your colon mainly through the fermentation of dietary fiber by beneficial gut bacteria, particularly members of the Firmicutes phylum, such as Clostridium and Faecalibacterium prausnitzii.
Butyric acid plays a critical role in gut health and metabolic function. It is the main energy source for colonocytes, which are the cells in the lining of your colon. This means they support the integrity and function of the intestinal lining and gut barrier.
By supporting the gut lining, it can help to prevent or improve leaky gut syndrome, thus reducing the risk of related chronic inflammation, autoimmunity, and health issues.
We will get into the specific benefits of butyric acid in the next section, but in short, it offers anti-inflammatory benefits. It may help to regulate the immune system by decreasing the production of pro-inflammatory cytokines, supporting the release of anti-inflammatory molecules, and aiding immune cell health. It may play a role in metabolic health and reducing autoimmune and gut health issues.
Benefits of Butyric Acid
Let’s look at the potential health benefits of butyric acid in detail.
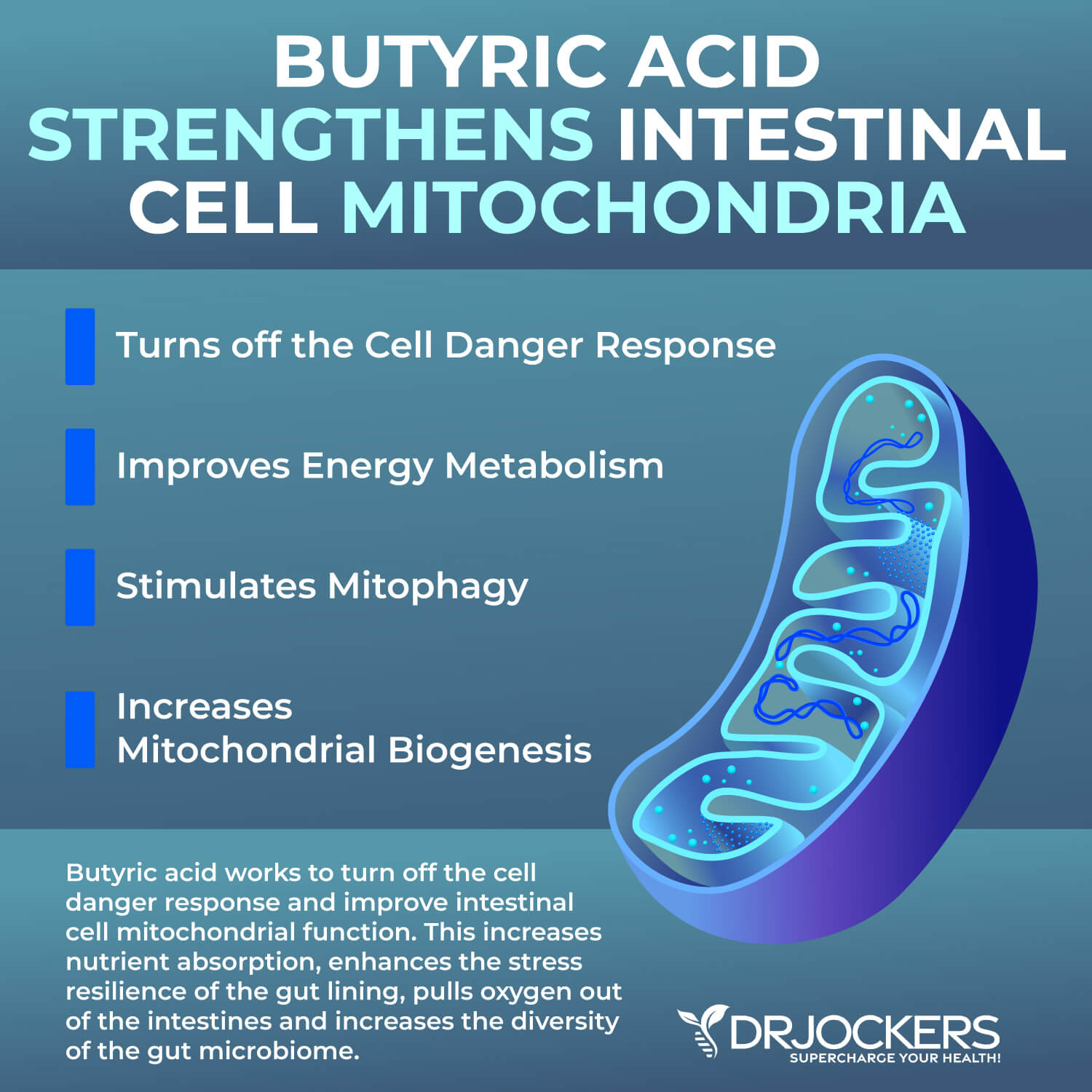
Strengthens Intestinal Cell Mitochondria
One of the major functions of butyric acid is to strengthen the intestinal cell mitochondria, which is critical for both energy production and cellular function. A 2023 study published in the International Journal of Molecular Sciences has found that butyrate is a key regulator in the mitochondrial function of glomerular endothelial cells (18).
A 2020 study published in Oxidative Medicine and Cellular Longevity has also found that butyrate may help to improve mitochondrial energy metabolism (19). A 2011 study published in Cell Metabolism has found that butyrate may improve energy metabolism and autophagy in the colon (20).
The mitochondria rely on a variety of sources of fuel. Butyric acid can serve as an energy substrate for colonocytes, which are cells lining the colon. By acting as a fuel source, butyric acid can improve mitochondrial function which can increase energy metabolism, resulting in better integrity and function of the intestinal barrier.
Butyric acid may also help complete the cell danger response. It can also increase the expression of PGC-1 α mRNA, which regulates mitochondrial biogenesis to improve mitochondrial biogenesis, which is the process of new mitochondria being created. New, healthy mitochondria can improve the capacity of your intestinal cells to make energy.
This is especially important at times when your body is experiencing stress and damage. Improved mitochondrial function can also improve nutrient absorption which can help to repair damaged tissue. Moreover, improving mitochondrial health in the intestinal cells can improve balance in the gut and reduce the risk of leaky gut syndrome and other gut health issues.
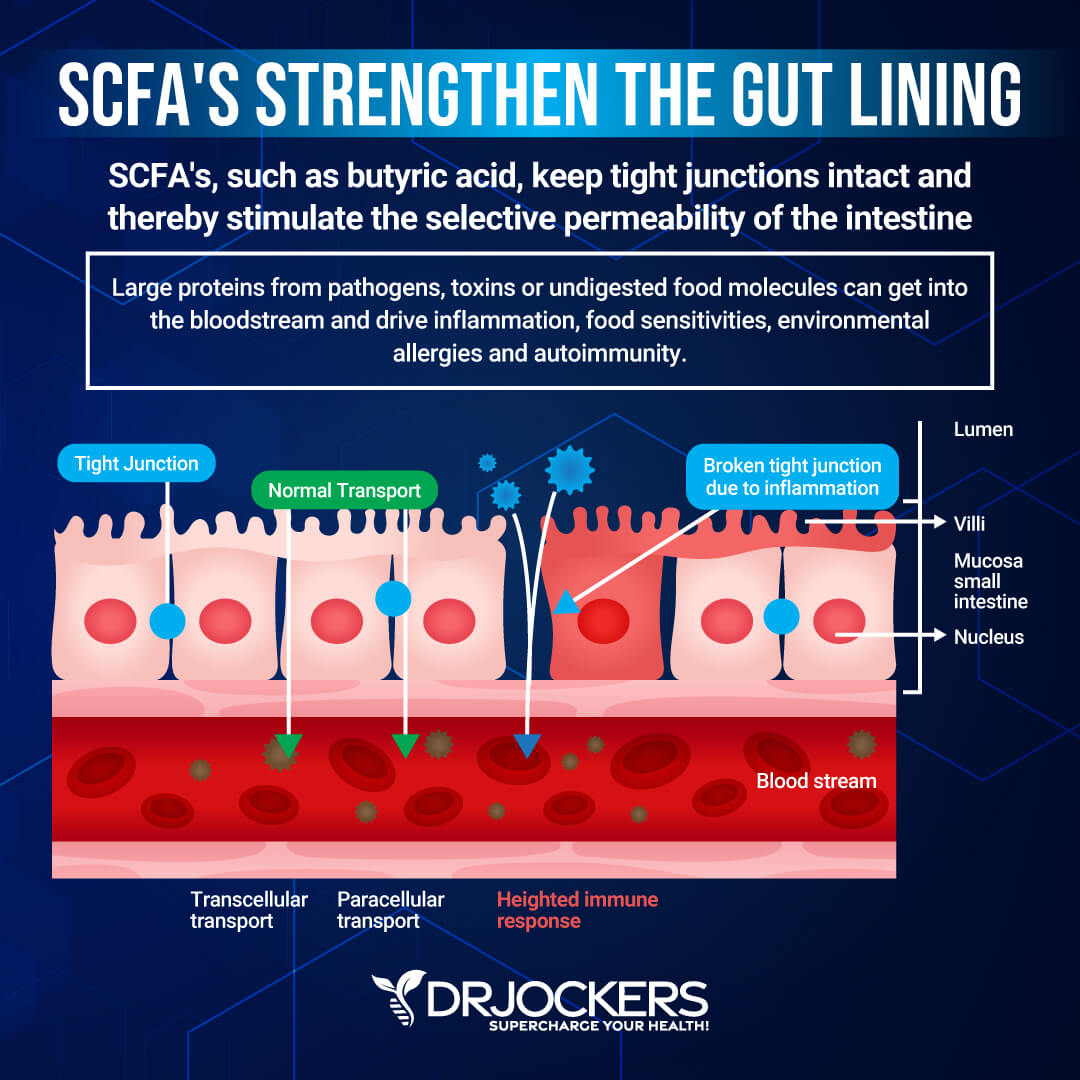
Seals the Intestinal Lining
Butyric acid also has an important role in the intestinal lining, particularly sealing the intestinal lining, promoting the function of the tight junctions of the gut lining, and maintaining the integrity of the intestinal lining.
As you know, keeping these tight junctions on the intestinal lining tight and small is critical. If they become too large, you develop leaky gut syndrome, and toxins and pathogens will be able to pass into your bloodstream.
A 2023 study published in Frontiers in Microbiology has found that butyric acid may help to maintain gut barrier integrity by regulating Claudin-1 and synaptopodin expression (21). Butyric acid can help your body make proteins, including claudins and occludins, which can help to seal and tighten these junctions. This will help to keep the intestinal barrier semi-permeable so only nutrients but not pathogens and toxins can pass through.
According to this 2023 study published in Frontiers in Microbiology, butyric acid can also reduce pro-inflammatory cytokine production offering anti-inflammatory effects and immune-modulating benefits (21). This can help to further protect the gut lining and reduce the risk of developing leaky gut syndrome, inflammatory bowel disease (IBD), and other autoimmune conditions.
Butyric acid may also help the repair and regeneration of your intestinal cells, which can help to improve leaky gut syndrome. A 2023 study published in Clinical Nutrition has found that butyric acid may be a good option for improving gastrointestinal disorders partly because it can help to maintain the gut barrier and reduce inflammation (22).
Improves the Gut Mucosa and Immune Function
Butyric acid can also help to improve the gut mucosa and immune function. Since the gut mucosa is critical for protecting you from harmful pathogens and supporting nutrient absorption and digestion, it’s critical to keep it healthy. Butyric acid helps to improve the gut mucosa by promoting the growth and repair of your epithelial cells, which are cells that line your gastrointestinal tract.
By supporting the production of mucus, butyric acid can help to strengthen the gut mucosa and gut barrier, which can protect you from leaky gut syndrome, gut health issues, and autoimmunity. According to a 2011 article published in the World Journal of Gastroenterology, butyric acid may help to improve impaired intestinal inflamed mucosa in IBD (23).
Moreover, according to a 2021 study published in the Journal of Inflammation Research, butyric acid may help to maintain immune homeostasis (24). Butyric acid can modulate immune cells, like T cells and macrophages, in the gut to improve immune function.
It may reduce pro-inflammatory cytokines and increase anti-inflammatory molecules. Thus, it may reduce increased immune activation and the risk of chronic inflammation and autoimmunity.
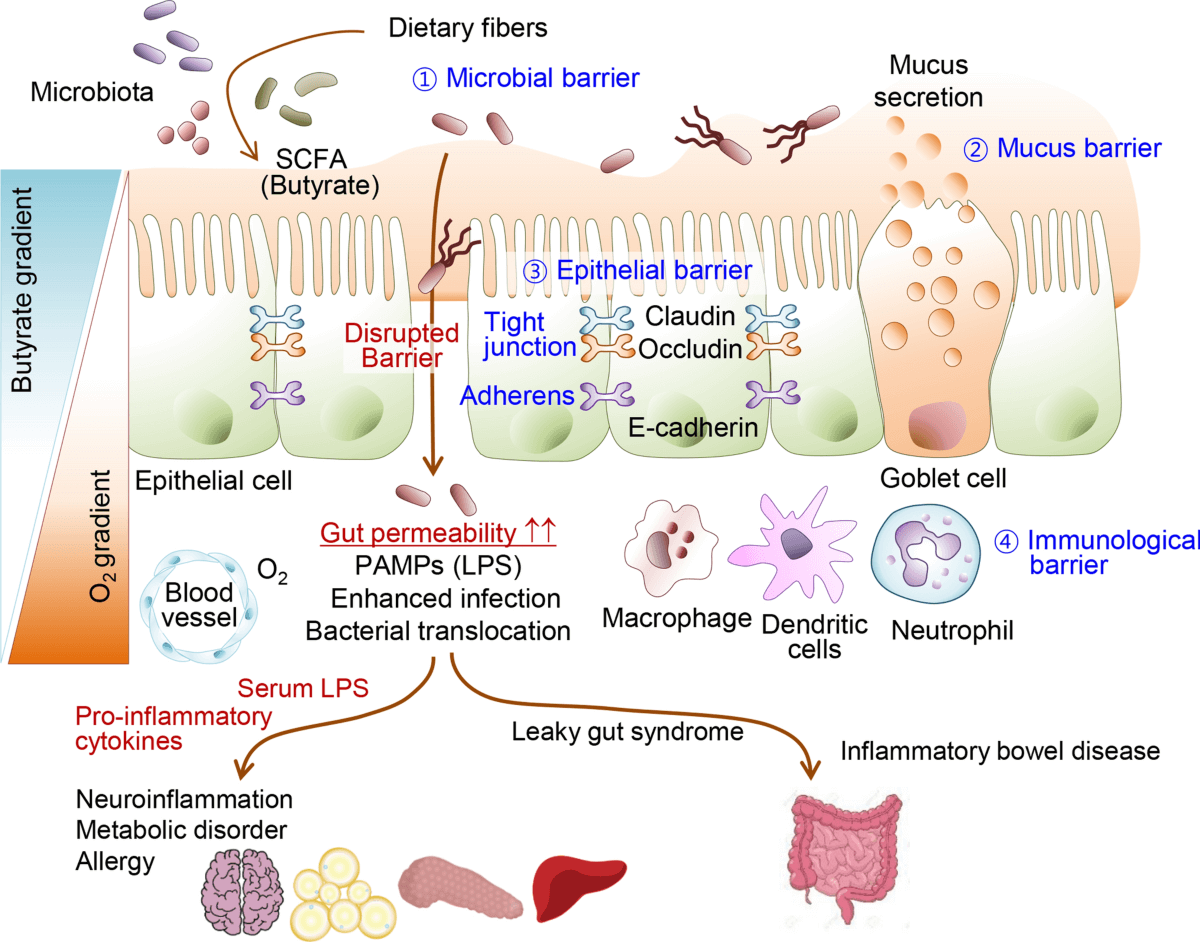
Supports the Diversity of the Gut Microbiome
A 2023 study published in Clinical Nutrition has found that butyric acid may be a good option for improving gastrointestinal disorders partly because it can improve gut microbiome health (22). Gut microbiome balance is critical for your gut health, metabolic function, and overall health.
Butyric acid also has an essential role in supporting the diversity of your gut microbiome. Butyric acid is a byproduct of fermentation of dietary fiber by beneficial bacteria.
This means it can ensure a good environment for the growth of beneficial gut bacteria. It may also reduce the pH of the gut making it more difficult for harmful bacteria to grow but easier for the proliferation of the beneficial bacteria, including Bifidobacteria and Lactobacilli.
The study found that it improves the diversity of the gut microbiome by pulling more oxygen out of the intestinal lumen for mitochondrial respiration, which reduces the aerobic bacteria and enhances the anaerobic bacteria diversity. It can also help your gut to break down dietary fiber easier.
This can improve microbial balance in the gut, a diverse gut flora, support immune regulation, improve digestion, and protect you from pathogens. Butyric acid can also increase resilience against gut dysbiosis, leaky gut syndrome, inflammatory bowel disease, gut health issues, metabolic disease, and autoimmunity through these actions.
Reduces Inflammation and Autoimmunity
Butyric acid may also help to reduce inflammation and autoimmunity. It helps to modulate immune responses and support a balanced immune environment. One of the key parts of this process is reducing pro-inflammatory cytokines, such as TNF-α, IL-6, and IL-1β.
Increased inflammatory cytokines often characterize chronic inflammatory and autoimmune conditions, including IBD. Suppressing their activity may help to lower chronic inflammation and support the recovery of damaged tissues.
Butyric acid also helps the production of regulatory T cells or Tregs, which are needed for controlling immune responses. This can help to improve immune tolerance and reduce the risk of autoimmunity. As 2023 research published in Fermentation explains, it also helps to improve T helper or Th cell balance by changing the immune response from pro-inflammatory Th1 and Th17 to anti-inflammatory Th2 and Treg profile (25).
According to a 2020 study published in Ebiomedicine, butyric acid in the gut can autoimmune responses by supporting the differentiation of follicular regulatory T cells (26). While Th1 and Th17 cells are linked to inflammatory and autoimmune activities, Th2 and Tregs may help to support immune regulation.
By balancing Th cells, butyric acid can reduce the risk of chronic inflammation and autoimmune conditions and support homeostasis and health instead. According to a 2024 study published in Biomedicines, butyric acid may help to reduce autoimmune rheumatic diseases (27).
Reduces Histamine and Mast Cell Activation
Finally, butyric acid may help to reduce histamine levels and mast cell inflammation. Your mast cells play a critical role in inflammatory and allergic responses.
When they become activated from an allergen, toxin, infection, stress, or other factors, they release histamine and other inflammatory chemicals. Dysregulation or overactivation of your mast cells and high histamine levels from histamine intolerance can increase chronic inflammation, chronic symptoms, gut health issues, and other health problems.
According to a 2020 study published in Allergy, butyric acid may reduce mast cell activation (28). Butyric acid may help to regulate mast cell activity by lowering pro-inflammatory cytokine release.
It may also help to stabilize the mast cell membranes. This can reduce degranulation and histamine release, which can calm the immune system, reduce mast cell activation issues, and lower histamine intolerance.
By supporting the gut, butyric acid can also decrease excess mast cell activation in the gut, which is the home of many gut cells. This can reduce gut inflammation and improve gut microbiome balance which may lower the risk of chronic inflammation and chronic health issues.
What are the Butyric Acid Producing Bacteria?
The main bacteria that make butyric acid is the Firmicutes phylum including Clostridium species and some of the lactobacillus strains (21, 29). Other main butyric acid producers include Faecalibacterium, Blautia, and Roseburia (30).
Ruminoccocus, Eubacterium, Butyrivibrio, and Anaerostipes can also make butyric acid and there is a variety of bacteria that can also produce butyric acid to a certain level (31).
How to Support Butyric Acid Levels
So, what can you do to support butyric acid levels?
Address Factors Causing Cell Danger Response
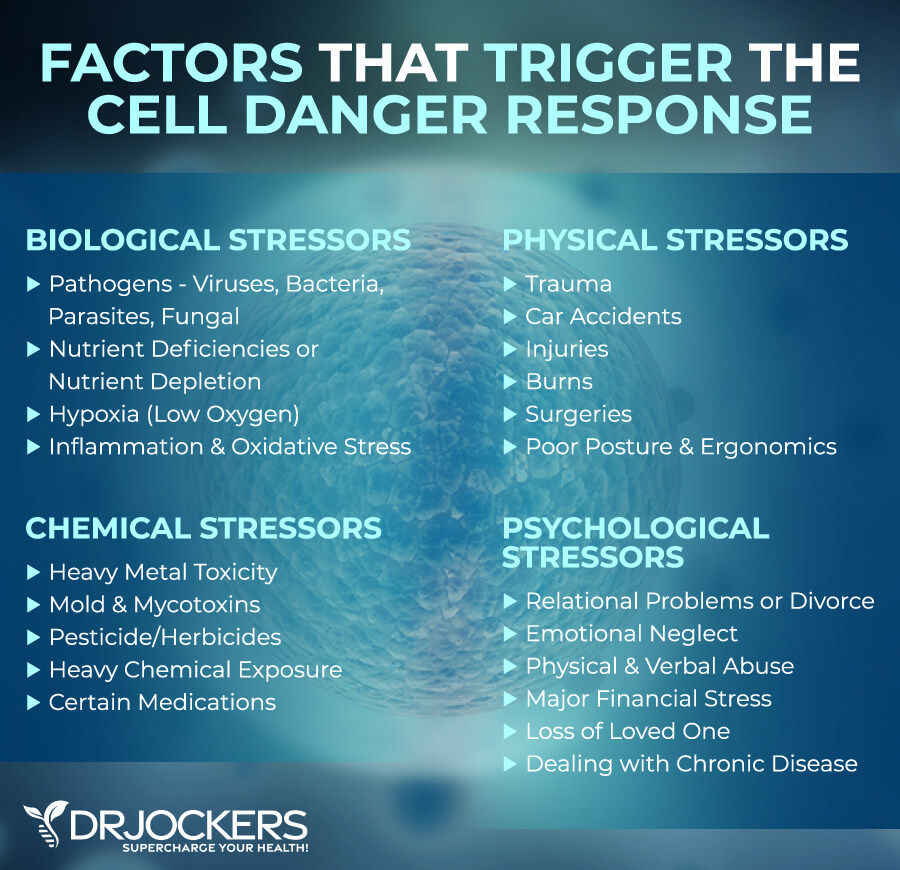
The first thing I recommend is to address any factors that could be causing the cell danger response. Anything that decreases cellular energy or increases cellular stress can potentially trigger a cell danger response. Factors that may trigger or cause the cell danger response include:
- Biological stressors, such as viruses, bacteria, parasites, and fungi, as well as nutrient deficiency, nutrient depletion, poor diet, hypoxia or low oxygen, inflammation, oxidative stress, or circadian rhythm dysfunction
- Chemical stressors, such as heavy metal toxicity, chemical toxins, other toxins, and medications
- Physical stressors and trauma, such as accidents, injuries, burns, surgeries, and major infections
- Psychological stressors or trauma, such as divorce, loss of a loved one, emotional neglect, emotional abuse, major financial difficulties, and dealing with a chronic disease
So, what does this mean? Consider any factors that may be involved. Get tested for any microbial or pathogenic overgrowth or infection and inflammation from a functional medicine doctor and address it through diet and supplementation.
Address any environmental toxin overload. This includes reducing toxin exposure and detoxification. Follow a healthy diet and use supplementation to improve any nutritional deficiencies. Seek treatment for any injuries or similar physical issues.
Work through emotional trauma and stressors. You may benefit from working with a therapist, coach, or spiritual counselor. Meditation, mindfulness, journaling, yoga, and other strategies may also help to reduce stress.
Follow an Anti-Inflammatory Nutrition Plan
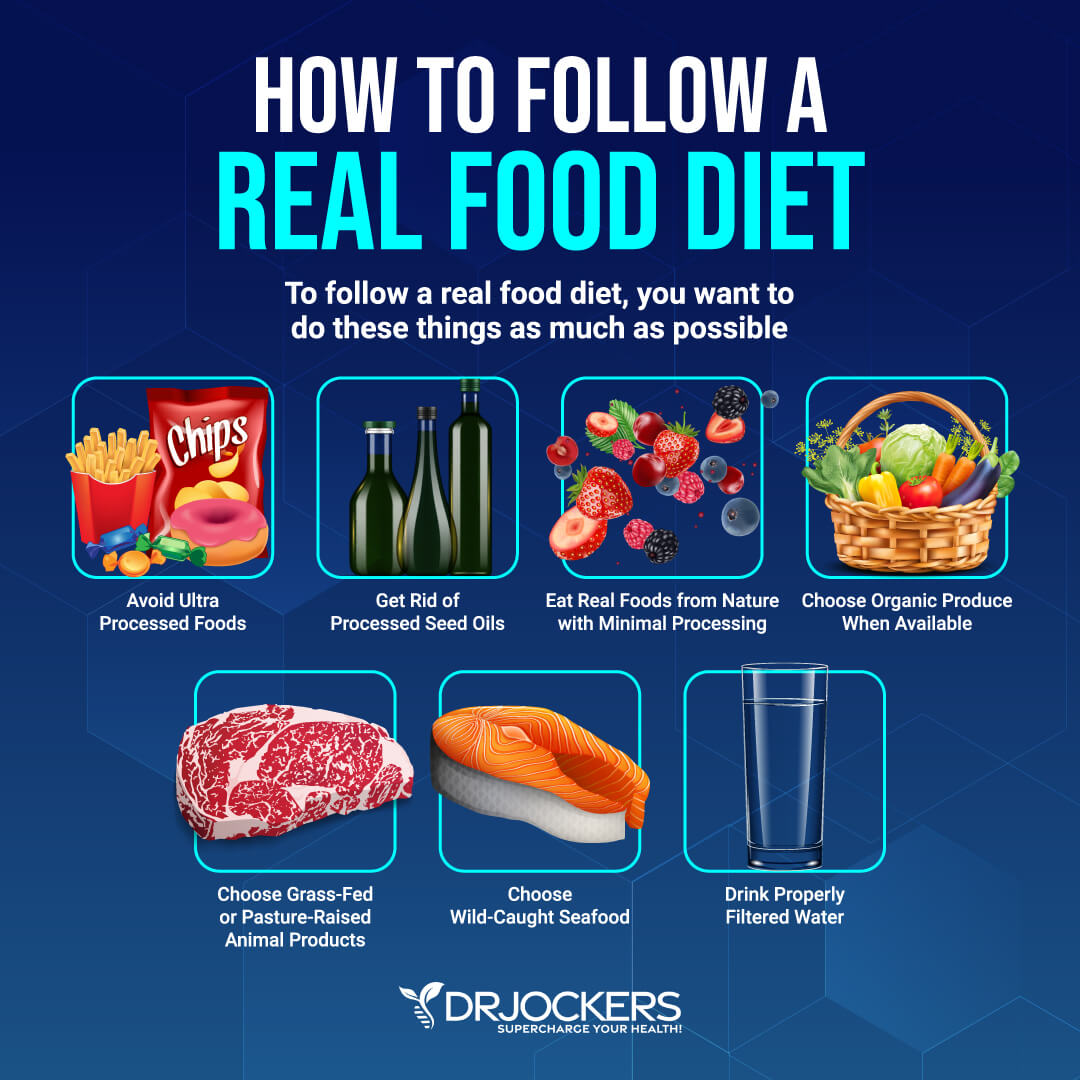
The next thing I recommend to support butyric acid levels is following an anti-inflammatory nutrition plan. Remove any inflammatory foods. This includes refined sugar, refined oil, artificial ingredients, sugary drinks and sodas, junk food, deep-fried food, additives, and ultra-processed food, as well as food sensitivities and food allergies.
Opt for anti-inflammatory, nutrient-dense real food instead. Eat lots of greens, vegetables, herbs, sprouts, fermented food, fruits, seeds, grass-fed beef, pasture-raised eggs and poultry, wild-caught fish and seafood, and wild game. Eat lots of healthy fats, such as avocados, coconut oil, coconut meat, olives, extra virgin olive oil, and animal fats.
Choose organic whenever possible and keep in mind the Dirty Dozen and Clean Fifteen list. Hydrate your body well with purified water and herbal tea.
Find Your Fiber and FODMAP Threshold
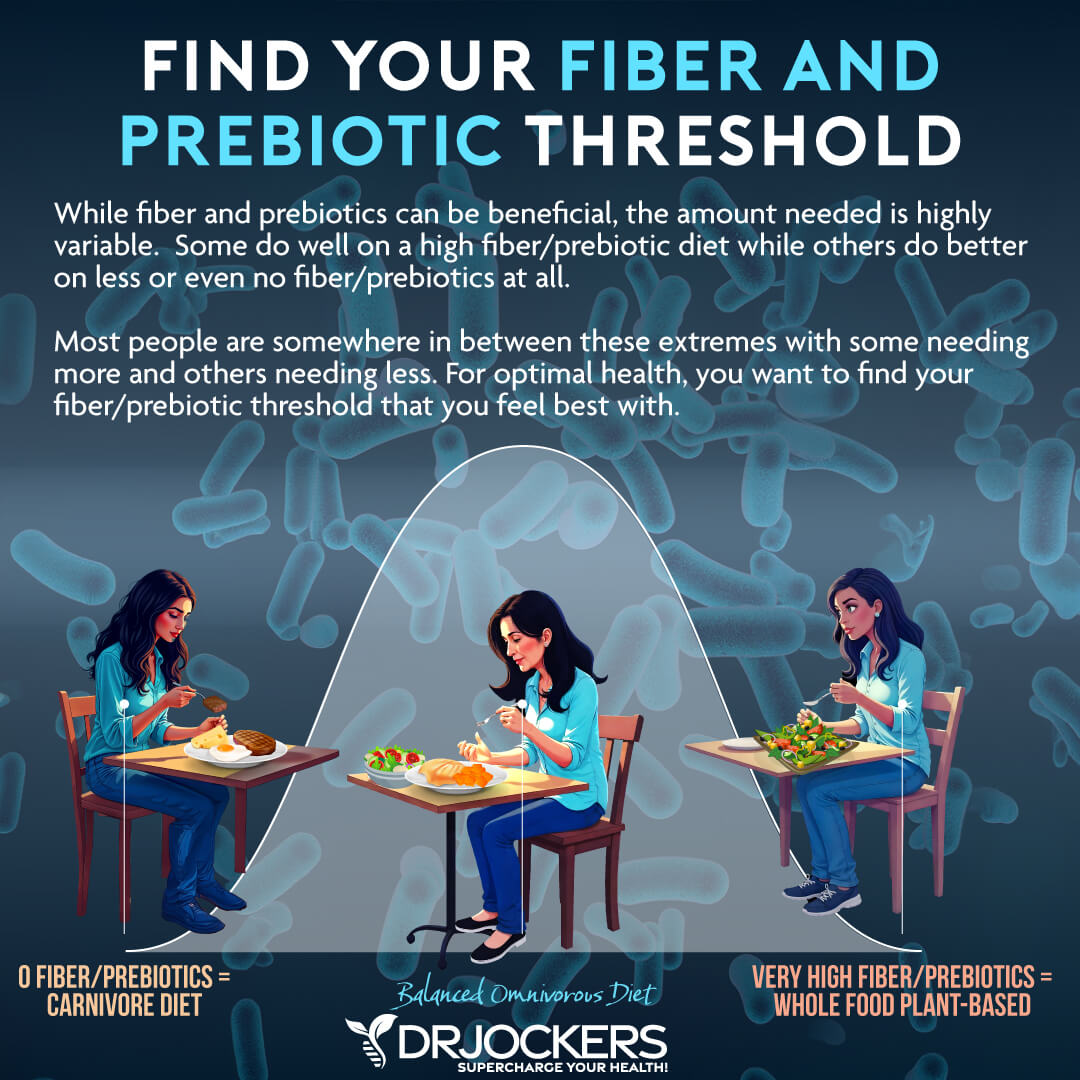
You may also benefit from finding the right fiber intake and FODMAP threshold for your body to support butyric acid levels. While fibers are good for your health, not everyone tolerates them the same.
The same goes for FODMAPs which cause issues for some but less so for others. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. They are types of short-chain carbohydrates that act as prebiotic foods for the gut bacteria that are poorly absorbed in the small intestine, and found in a variety of foods, including certain fruits, vegetables, dairy products, grains, and sweeteners.
Just think about a bell curve with fiber and FODMAPs. Some people do well with a higher fiber and FODMAP diet, such as plant-based diets while others do well with low or almost no fiber, such as a low-FODMAP or carnivore diet. Most people do well with moderate amounts, which is in the middle of the bell curve, and include a healthy whole food-based diet with fiber.
This can take a bit of experimentation. It may be best to begin with a low-fiber and low-FODMAP diet and see how you’re doing. Slowly increase your fiber and FODMAP intake and pay attention to your body’s messages. Back off if you experience symptoms and stay at your sweet spot.
Consider Practicing Intermittent Fasting
Intermittent fasting is a dietary strategy that cycles between a period of not eating (fasting) and a period of eating (feasting), Practicing intermittent fasting can improve intestinal healing. It takes off mechanical pressure from the intestinal lining and allows time and rest to heal. Your gut lining only takes 4 to 5 days to change so the change can be actually very quick compared to let’s say a bone or joint injury.
Intermittent fasting also helps to balance and regulate the immune system by increasing T regulatory cells and decreasing inflammatory cytokines. This can reduce systemic inflammation and inflammatory issues.
Intermittent fasting can also improve the gut microbiome. It can improve the gut microbiome diversity and increase beneficial bacteria. It also increases short-chain fatty acid, including butyric acid levels.
When you look at the gut microbiome, you will see primary feeders that are on the top of the intestinal mucosa, which is the primary area of your immune system. There are also secondary feeders inside the intestinal mucosa which can actually eat the mucosa which helps to create postbiotics.
One of these is Akkermansia Mucinophilia. It does this by starving the primary feeders and supporting the secondary feeders. Eating all the time can actually reduce secondary feeders which can lead to issues.
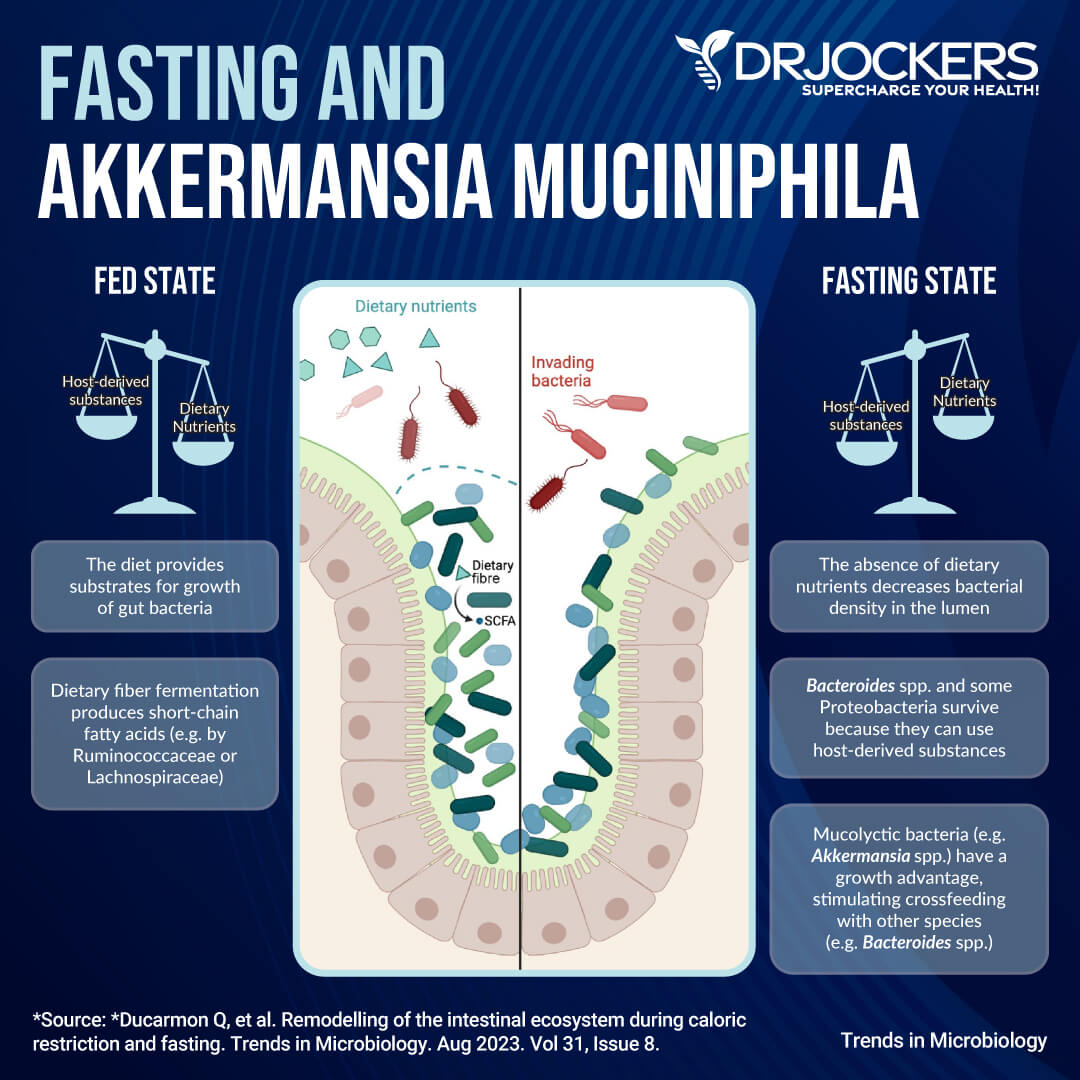
Moreover, intermittent fasting can also stimulate intestinal cell mitophagy which can help to improve leaky gut syndrome. It can increase intestinal cell resilience as well.
The most popular way of intermittent fasting is a 16-hour fasting window and an 8-hour eating window. It’s called the 16:8 fast. But you may notice that you do the best with a slightly shorter or slightly longer fasting period. During your fasting window, you can’t consume any food or calories, only water, herbal tea, and in some cases, coffee. During the eating window, you want to meet all your nutrient needs into 2 or 3 meals, with no snacking.
Start out with a Simple Fast, a 12-hour eating window. Keeping the 12-hour fasting window is simple. If you finish dinner at 6 PM, you can eat again at 6 AM. With a 7 PM dinner, you are ready for your first meal at 7 am. Once you are comfortable with this, increase your fasting window gradually to 14, 16, and even 18 hours.
You don’t have to practice this every day unless you want to. You may benefit from 2 to 3 fasting days a week. I recommend 16:8 (16 hours fasting, 8 hours of eating) or 18:6 (18 hours fasting, 6 hours of eating) a few times a week and 14:10 (14 hours fasting, 10 hours of eating) at the minimum. You may learn more about intermittent fasting from this article.
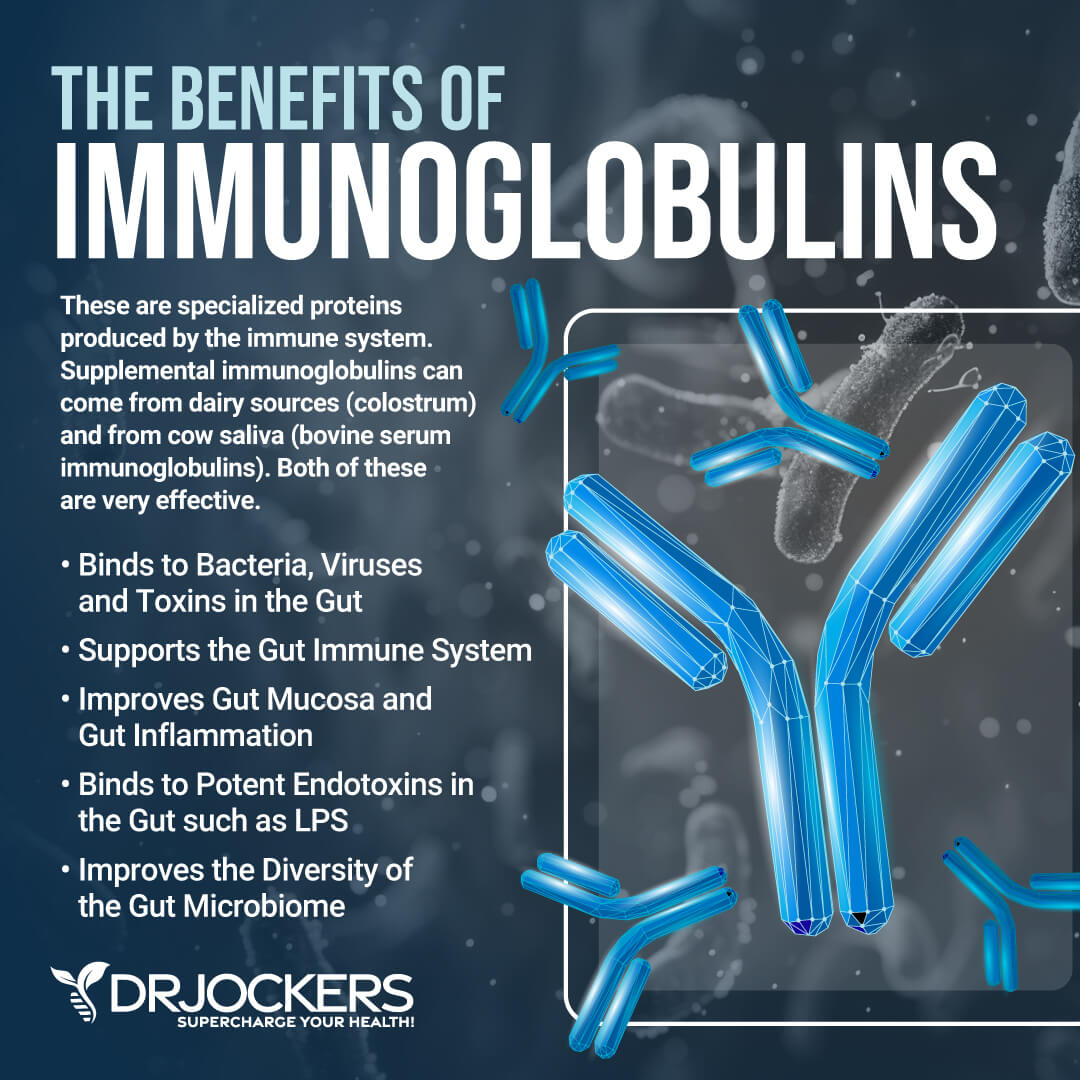
Consider Using Immunoglobulins
Finally, I recommend using some immunoglobulins. Immunoglobulins, commonly known as antibodies, are specialized proteins produced by the immune system. They are designed to identify and neutralize foreign invaders like bacteria, viruses, and toxins.
They are a critical part of the adaptive immune response. They allow the body to recognize and remember pathogens. Immunoglobulins are produced by B cells and plasma cells in response to the presence of antigens.
A 2024 article published in Nutrients has found that serum-derived bovine immunoglobulin may help to reduce inflammation and improve gut barrier integrity (32). Using immunoglobulins may help to improve butyric acid levels by allowing the gut to neutralize pathogens and decrease gut inflammation more effectively. IgA is an immunoglobulin that may be great for improving mucosal immunity, creating a balanced gut microbiome, reducing gut inflammation, and supporting gut health.
Consider Using Supplemental Butyrate
You may also want to consider using supplemental butyrate. Oral butyrate supplements can be absorbed by your small intestine and also enter your bloodstream.
They may offer anti-inflammatory benefits. However, since your small intestine doesn’t use butyrate well, the benefits may be more apparent in the large intestine versus the small one. By being absorbed in the bloodstream, it can offer anti-inflammatory benefits to various organs.
Still, the best way to benefit from butyric acid is from your microbiome which makes it in your large intestine. Supplementation is an extra step that doesn’t replace the recommendation I just shared earlier to help your body make more butyric acid.
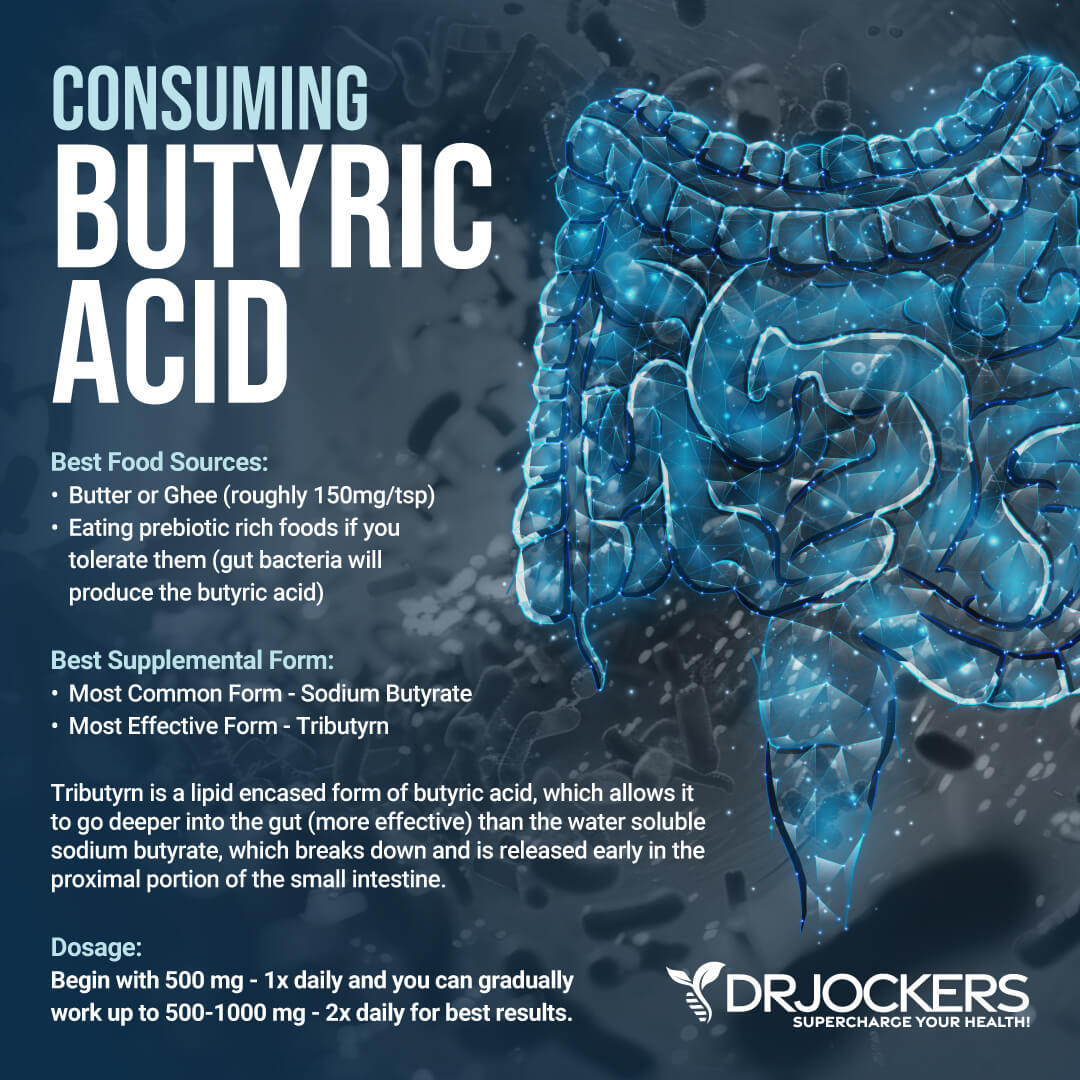
Introducing Tributyrn-X
I recommend using Tributryn-X. If you need support for a dysfunctional immune system, leaky gut, chronic inflammation in the digestive tract, food sensitivities, bloating, or digestive discomfort then your body deserves to try this supplement. It’s the most advanced formula on the market. It’s great for gut health.
Many clinicians we know use around 1,500 mg a day. And in certain cases, higher amounts than that. However, EVERYONE should start slowly with one capsule a day 500mg, as each person’s gut integrity, motility, and microbiome are different.
Each person’s effective dose can also be influenced by alcohol consumption, tobacco consumption, fat mass levels, speed of digestion (too fast might need more, too slow might need less), and other variables. This means you start with 1 soft gel a day and may take 1-3 gel capsules per day of Tributyrin-X or more as directed by your health provider.

Introducing Mega IgG
I also recommend using Mega IgG. Immunoglobulin G (IgG) is the most abundant antibody in the system and can be found in blood and extracellular fluid, allowing it to control infections in the body. IgG antibodies can bind a variety of pathogens, including bacteria, viruses, and fungi, as well as their toxic by-products.
Binding these toxins will neutralize them and allow the immune system to safely remove them from the body. This supplement may help to maintain the gut barrier function and can also support your H Pylori protocol. It helps support the H. Pylori protocol and helps maintain the gut barrier function.
Unlike other milk-derived immunoglobulins on the market, Mega IgG2000 is derived from bovine serum, making it lactose-free, casein-free, and β-lactoglobulin-free. Take 1 scoop daily with or without food or as directed by your healthcare practitioner. Mix powder into 16 oz. of cold water or liquid of your choice. Stir for 20 seconds. For children under the age of 2, please consult your healthcare practitioner. Drink plenty of fluids
Final Thoughts
Butyric acid is a short-chain fatty acid (SCFA). It is made in your colon mainly through the fermentation of dietary fiber by beneficial gut bacteria. Improving butyric acid levels is important for improving leaky gut syndrome and gut dysbiosis. I recommend following my best strategies on how to support your butyric acid levels naturally to improve leaky gut, gut microbiome health, and gut health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!