 Varicose Veins: Symptoms, Causes, and Natural Support Strategies
Varicose Veins: Symptoms, Causes, and Natural Support Strategies
Painful, bluish-purple, swollen, and raised veins? Yes, I am talking about varicose veins, a common health issue that affects about a quarter of American adults, especially women. They may develop because of inflammation, obesity, aging, and other factors. Many people believe that they are a normal part of adulthood or aging, however, with the help of some natural support strategies you can reduce your risks and symptoms.
In this article, you will learn what varicose veins are. You will understand their symptoms, six stages, and risk factor. I will go over conventional treatment options for varicose veins. I will discuss the major causes of varicose veins. Finally, I will offer my top natural support strategies for varicose veins.
What Are Varicose Veins
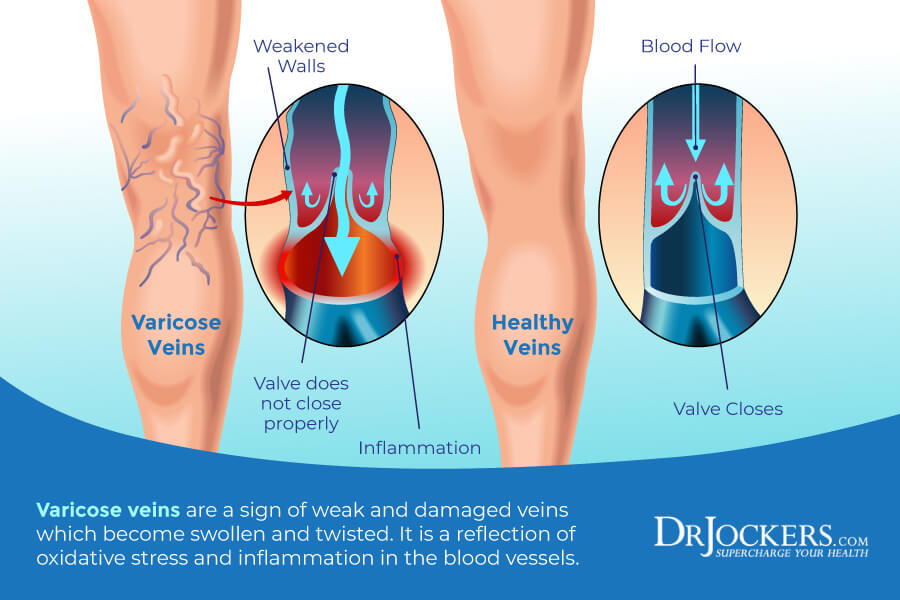
Varicose veins are also known as varicose or varicosities. They are twisted, large, swollen, and raised veins that are dilated and overfilled with blood. Varicose veins are bluish-purple or red in color and can be quite painful in some people (1).
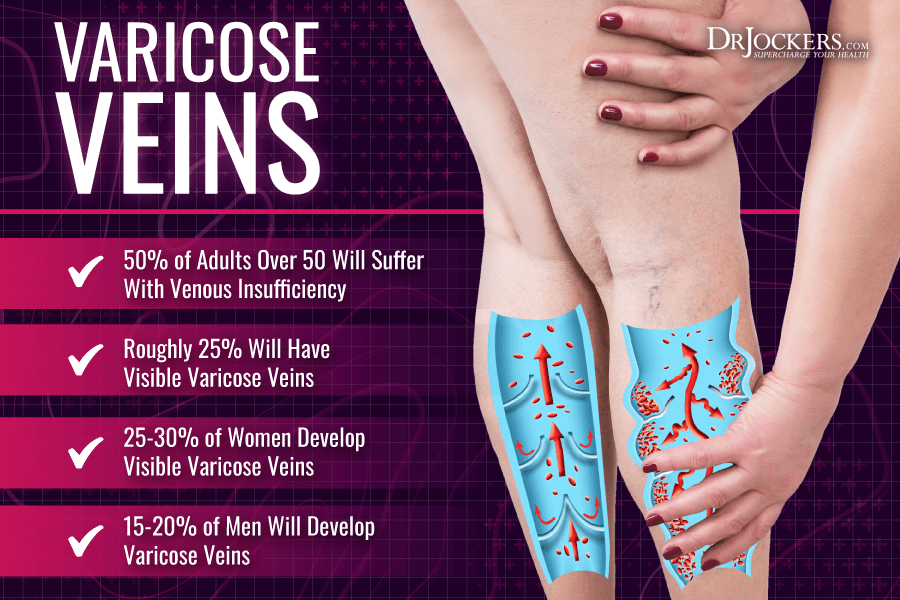
About 50 percent of adults develop some level of venous insufficiency with 25 percent of adults developing varicose veins at one point in their lives. They are particularly common in women.
While they are the most common in one’s legs, they can develop in other parts of your body. For example, hemorrhoids occur because of varicose in the rectum. They may develop in the esophagus, liver, or stomach. In men, they can also develop in the testicles potentially causing infertility (1).
Symptoms of Varicose Veins
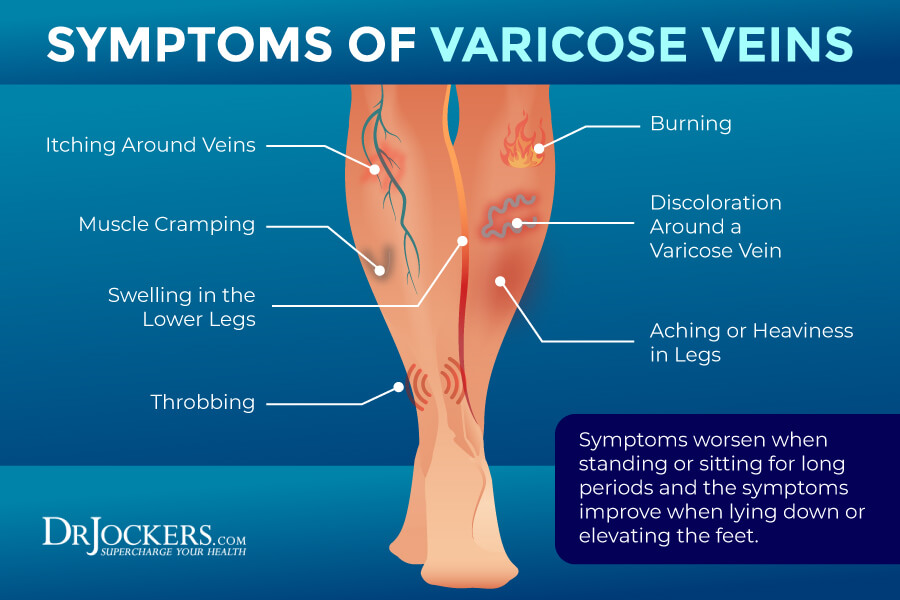
Symptoms of varicose veins may include (1):
- Bulging, bluish vein
- Enlarged veins
- Misshapen and highly visible veins
- Swelling
- Heaviness in the legs and feet
- Achiness and pain around or over the veins affected
- Increased symptoms when sitting or standing for a longer period of time
- Decreased symptoms when lying down or putting your feet up
- In severe cases, ulcers because of bleeding
Stages of Varicose Veins
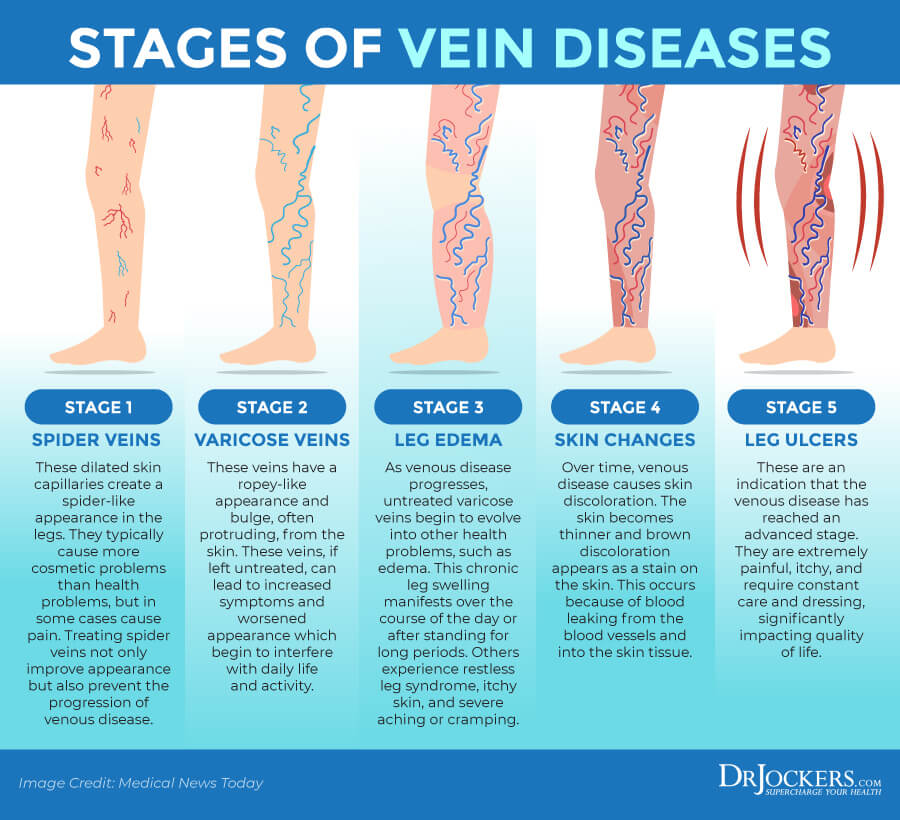
There are 6 stages of varicose vein depending on your symptoms and the progression of the condition:
Stage One – Spider Veins
Spider veins are smaller, reddish-purple veins. They usually appear on your legs, ankles, neck, face, or other areas of your body. While they may be the first stage of varicose veins, they are not always related to varicose veins. Spider veins are much more common in women than in men.
Stage Two – Enlarged, Ropy Varicose Veins
Stage two is characterized by swollen veins. You may experience numbness, burning, or itching around the veins or pain, weakness, or fatigue in the legs. In some people, this is the first stage as varicose veins are not always preceded by spider veins.
Stage Three – Edema Without Skin Changes
In this stage, you will notice swelling (edema) in your legs or ankles. This happens because of the circulatory system’s reduced ability to reabsorb fluid. Elevation of the legs may help to reduce symptoms or discomfort. In this stage, there are no visible skin changes.
Stage Four – Skin Changes and Discoloration
At this stage, you will notice skin changes in both texture and color caused by poor circulation and congestion inside the veins. You may notice reddish-brown or white color in the legs and a leathery skin texture that can be brittle and more vulnerable to injury.
Stage Five – Skin Changes with Healed Ulceration
In stage five, you may experience scratches or injuries. While they can heal with the help of treatment, they often result in scarring.
Stage Six – Skin Changes with Active Ulceration
Stage six is the most serious stage when skin injuries and ulcers are resistant to treatment and leave the legs with bleeding, open, painful sores.
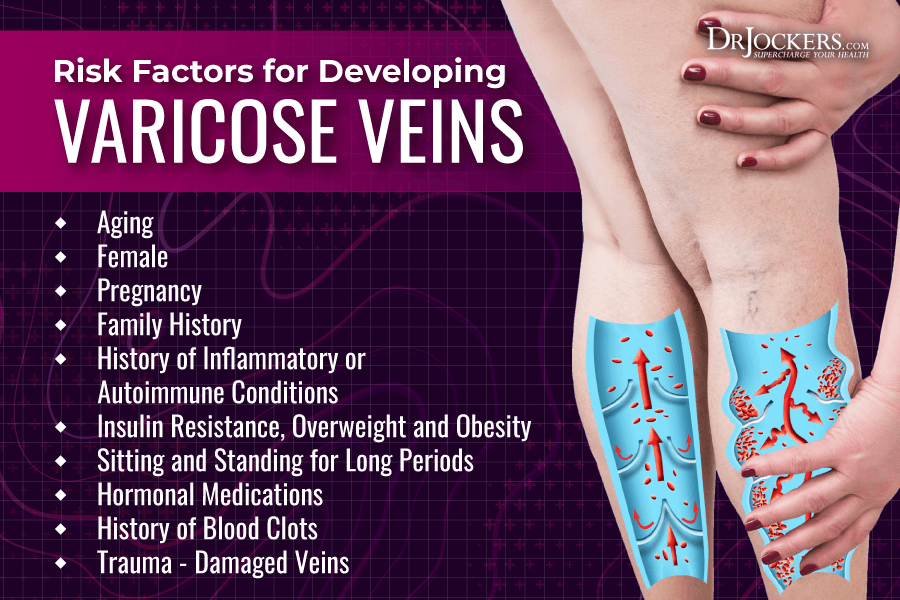
Risk Factors for Varicose Veins
Risk factors for varicose veins include (2):
- Age: Aging causes wear and tear on the valves inside the veins affecting blood flow and increasing the risk of varicose veins.
- Sex: Women are more likely to develop varicose veins due to hormonal changes during pregnancy or menopause and as a result of possible hormonal treatments.
- Pregnancy: Hormonal changes and increased blood volume during pregnancy may increase the risk of varicose veins.
- Family history: If others in your family had varicose veins, your risk of developing them is also higher.
- Obesity: Being overweight or obese puts extra pressure on the veins and can increase the risk of varicose veins.
- Sitting and standing for a long period of time: If you are sitting or standing for long periods in the same position, blood cannot flow properly and may increase your risk of varicose veins. Desk jobs can therefore increase your risk if you don’t get up to move and stretch regularly.
- Hormonal medications: Birth control pills, hormone replacement therapy, and other hormonal treatments may increase the risk of varicose veins.
- History of blood clots: A history of blood clots or deep vein thrombosis may increase the risk of varicose veins due to damaged valves or veins.
- Damaged veins: Damage to the veins caused by trauma can also increase the risk of varicose veins.
Conventional Treatments
Your doctor will likely recommend a few lifestyle changes, especially early in the disease, including avoiding sitting or standing for extended periods of time, exercising to increase circulation, and weight loss. Compression with the help of compression socks or stockings is often recommended (1).
When these non-invasive methods and lifestyle changes are not working, surgery is recommended. Vein ligation and stripping surgeries, cuts and removes varicose veins.
There are also other less invasive options available to block off the vein, including endoscopic vein surgery inserting a small lighted scope through a tiny incision, laser surgery using light, sclerotherapy using a liquid or foam chemical injection for larger veins, microsclerotherapy using a liquid chemical injection for smaller veins, or endovenous ablation using heat or radiofrequency. Check out the Denver Vein Specialist to learn more about the best options for your particular situation.
Later in this article, I will share my top non-invasive natural support strategies for varicose veins. But first, let’s go over their top causes.
Major Causes of Varicose Veins
Varicose veins may develop for a variety of reasons. Here are the most common major cause of varicose veins:
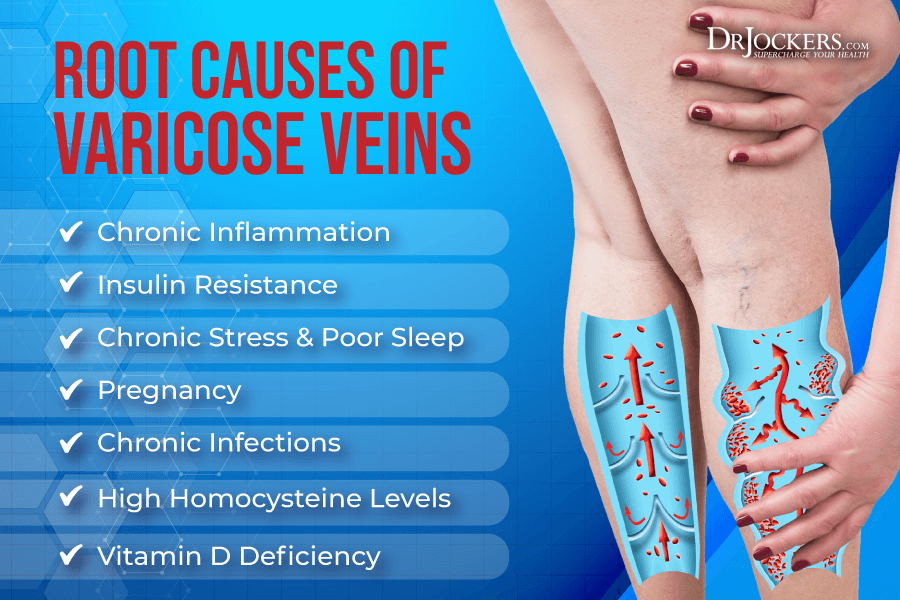
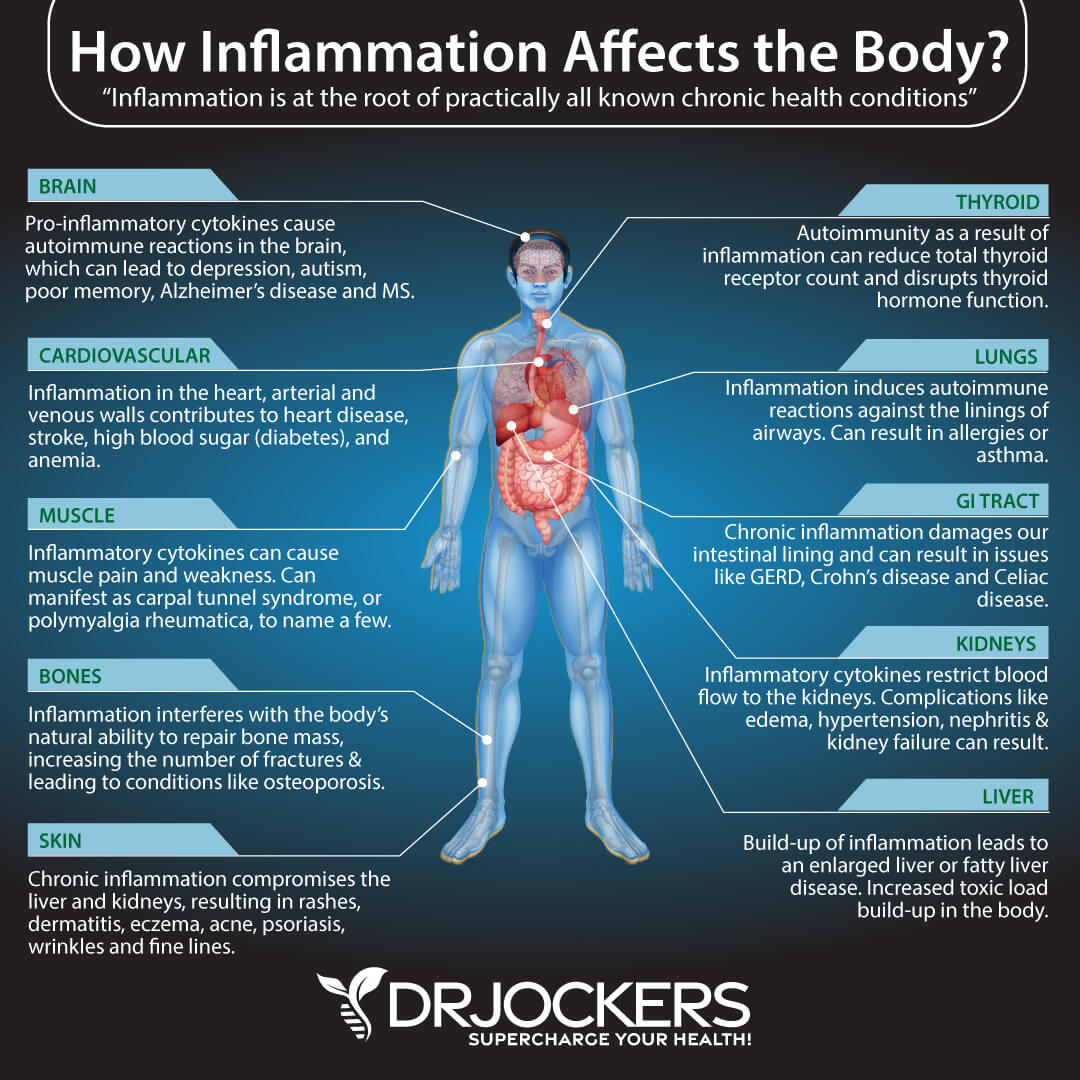
Chronic Inflammation
Chronic inflammation is the most common root cause of most chronic diseases and health problems. It’s no wonder that chronic inflammation plays a role in varicose veins as well. A 2016 study published in Clinical And Applied Thrombosis and Haemostasis looked at inflammatory biomarkers in patients with varicose veins and found that the group with varicose veins had significantly higher levels of inflammation than the control group (3).
A 2014 study published in Phlebolymphology has also found a connection between inflammation, aging, chronic venous insufficiency (CVI), and varicose veins based on specimens from a group undergoing surgery for varicose veins and a control group (4).
Insulin Resistance
According to a 2010 study published in Cell Metabolism, insulin resistance can affect your vein and arterial health (5). Glucose built up in the blood can create numbness and affect blood flow in the veins and arteries causing damage in the nerves, veins, and causing swelling, burning, or pain.
According to a 2000 study published in the Journal of Clinical Investigation, being overweight or obese can increase insulin resistance, therefore affect the health of your veins and increase the risk of varicose veins (6).

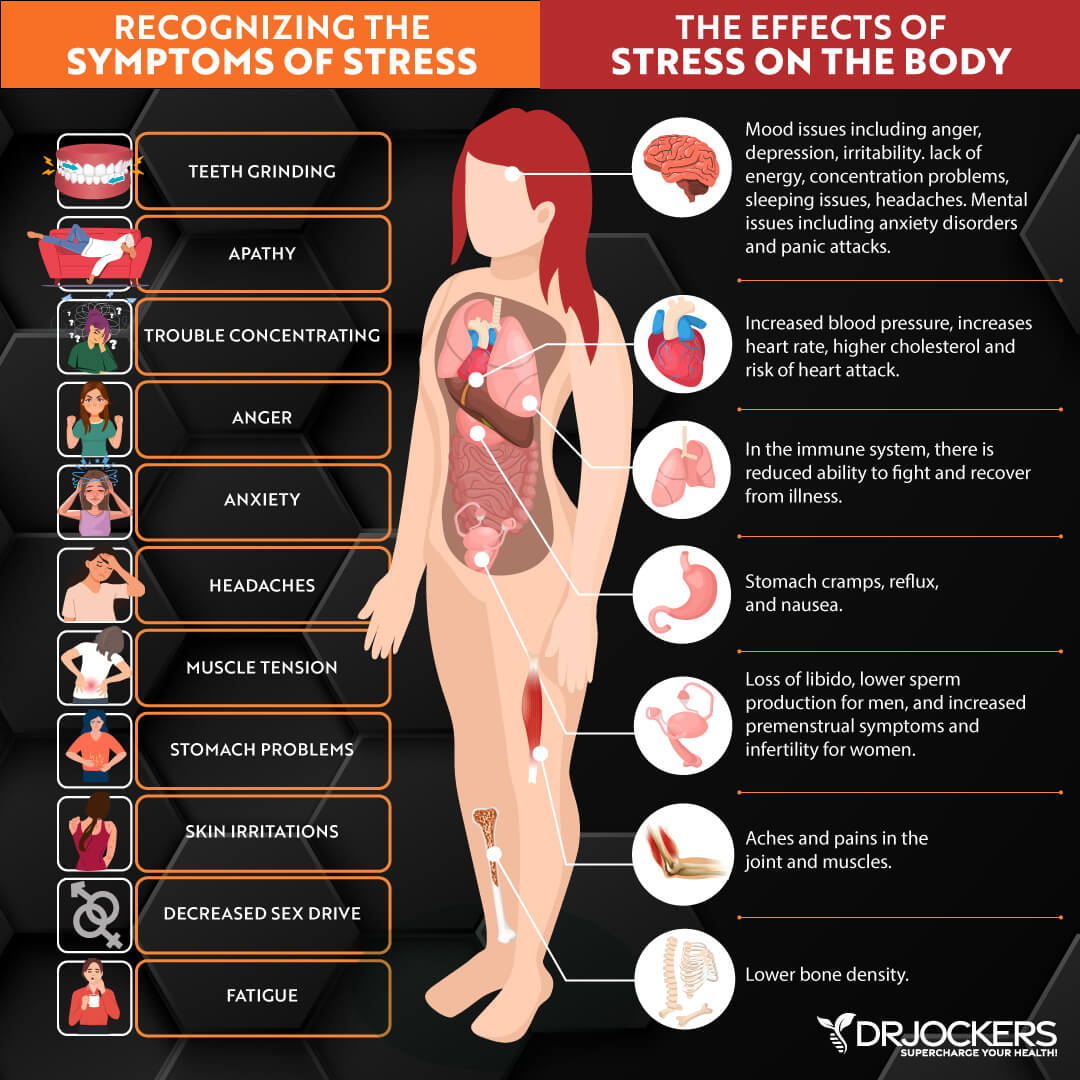
Chronic Stress & Poor Sleep
While chronic stress and poor sleep will not specifically cause varicose veins, chronic stress and poor sleep can add to the underlying problems, increase your risk, and increase your symptoms of varicose veins. Chronic stress and poor sleep can both increase chronic inflammation which is one of the top underlying risk factors for varicose veins (3, 4).
Chronic stress can also increase the risk of high blood pressure which can weaken your blood vessels and further increase your risk of varicose veins.
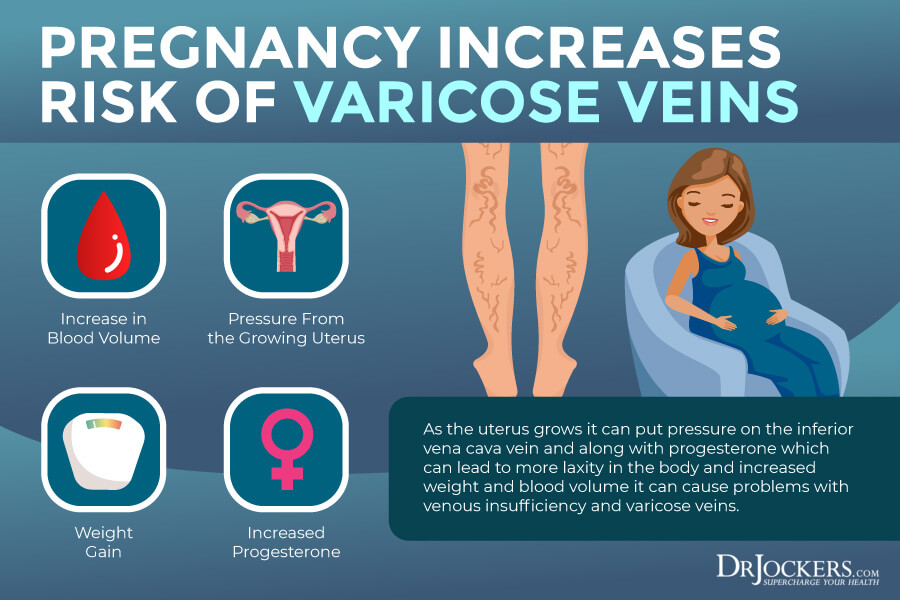
Pregnancy and Varicose Veins
Varicose veins are quite common during pregnancy and can develop any time during the course of the pregnancy. According to the American Pregnancy Association, during pregnancy, your hormones are changing, the blood volume increases, and the rate of the blood flow between the legs and the pelvis decreases, which can lead to varicose veins (7).
They state that exercise, elevating your legs, maternity supporting hosiery, sleeping on your left side, reducing sodium, and drinking plenty of water may reduce your risk during pregnancy.
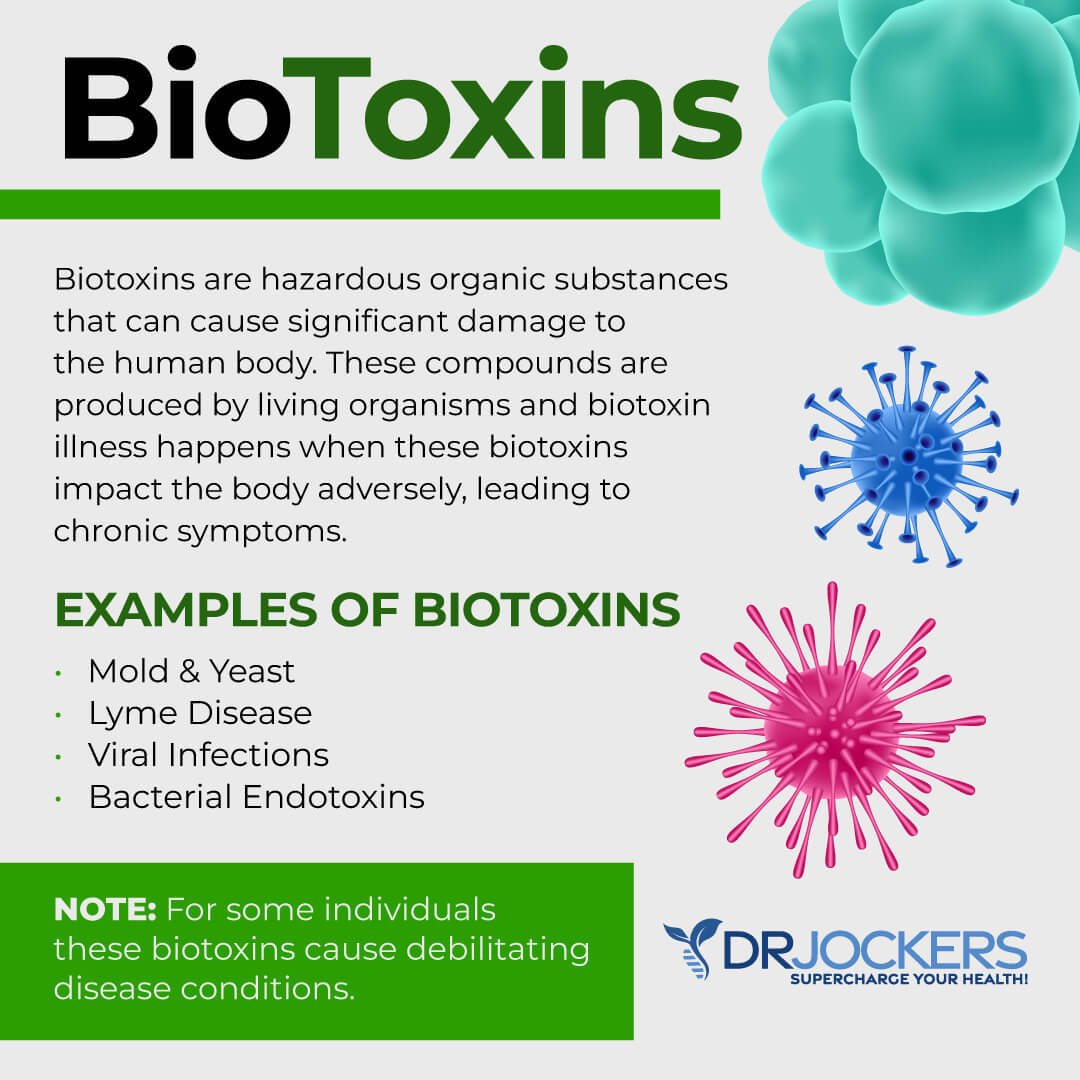
Chronic Infections
Chronic infections can also increase your risk of varicose veins. A 2016 study published in Cell Reports has found that Borrelia burgdorferi, a bacteria associated with Lyme disease, can migrate within the blood vessels causing inflammation and increasing the risk of varicose veins (8).
According to a 2007 study published in the European Journal of VAscular and Endovascular Surgery, oral bacteria and chronic periodontal disease can increase the risk of varicose veins (9).
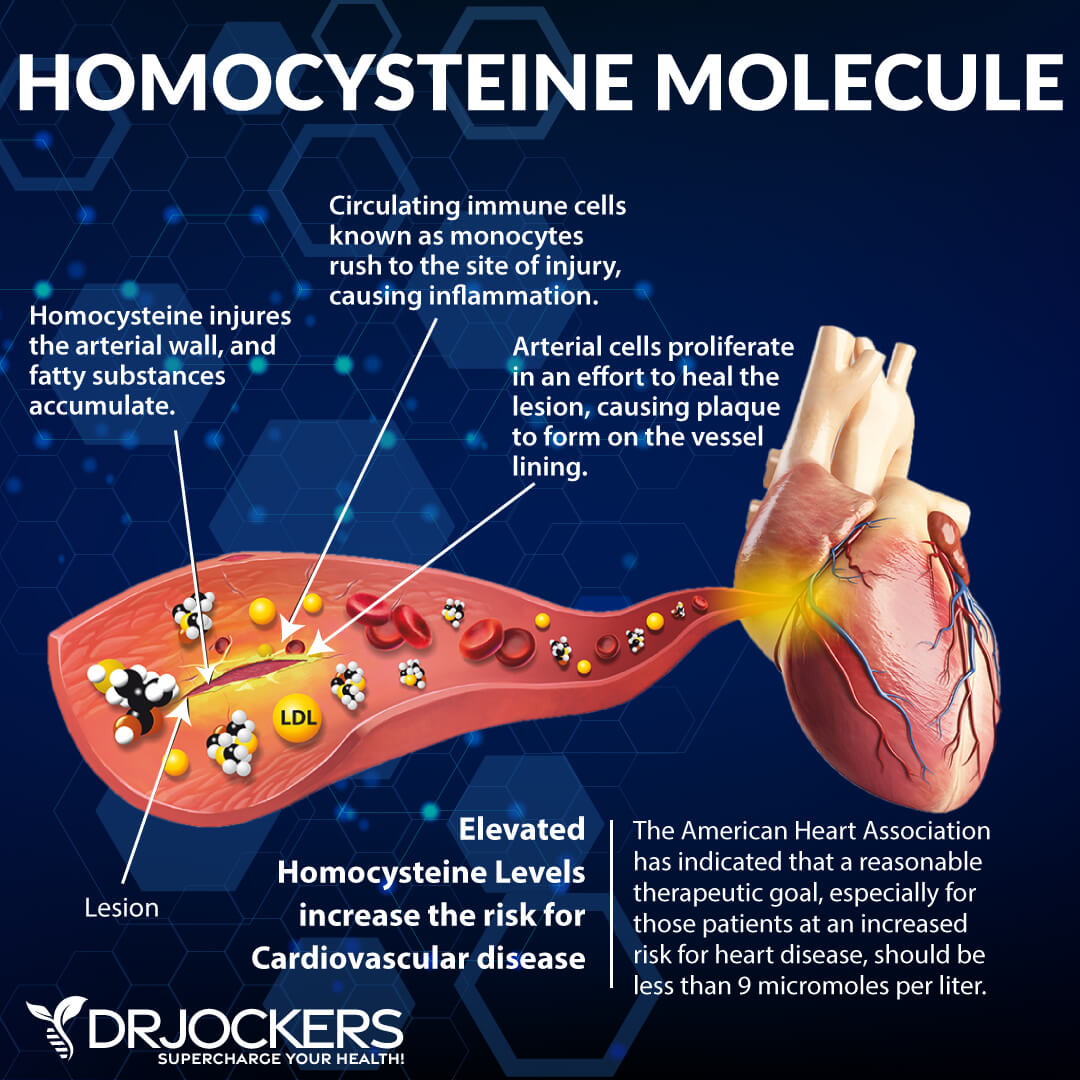
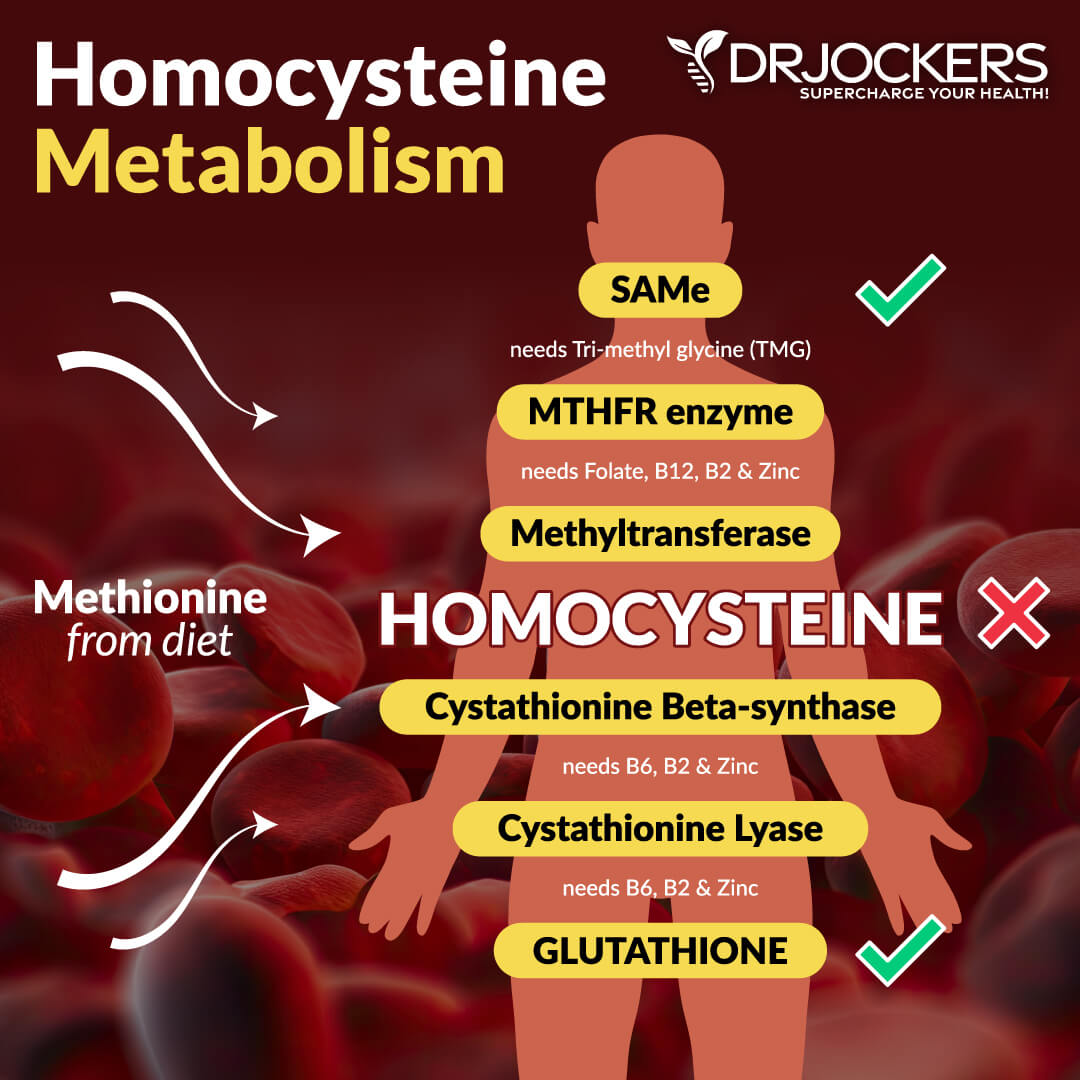
High Homocysteine and MTHFR
Homocysteine is an amino acid in your blood that is a good indicator of chronic inflammation and the risk of cardiovascular disease. According to a 2016 study published in Phlebology, increased serum homocysteine levels can be linked to primary chronic venous disease and varicose veins (10).
Methylenetetrahydrofolate reductase, or MTHFR, is an enzyme that helps to break down the amino acid homocysteine. According to a 2010 study published in Phlebology, MTHFR can be linked to deep vein thrombosis and vein health issues (11). According to a 2015 study published in EBioMedicine, changes in the MTHFR enzyme can lead to increased homocysteine levels and increased free radical damage and increase the risk and complications of varicose veins (12).
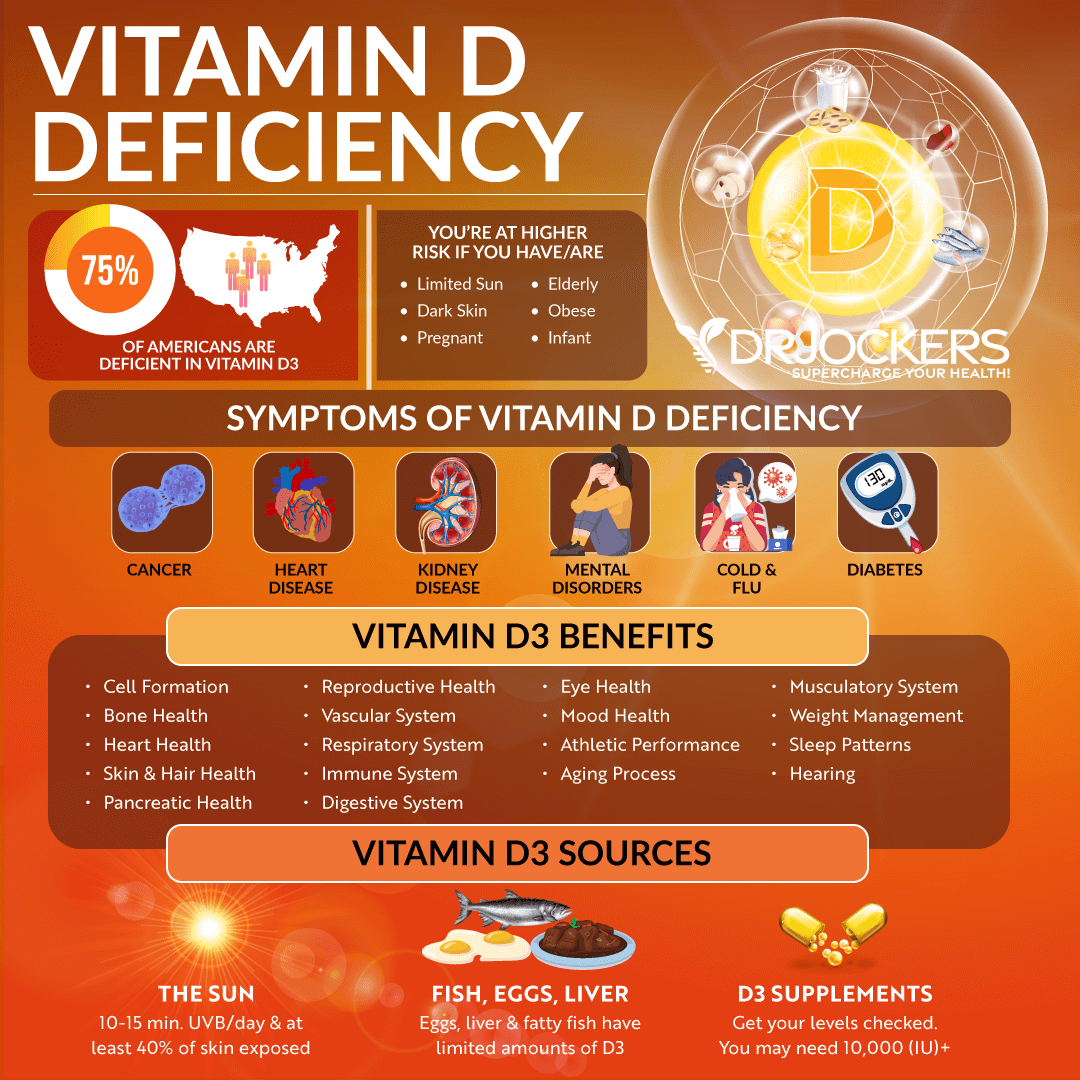
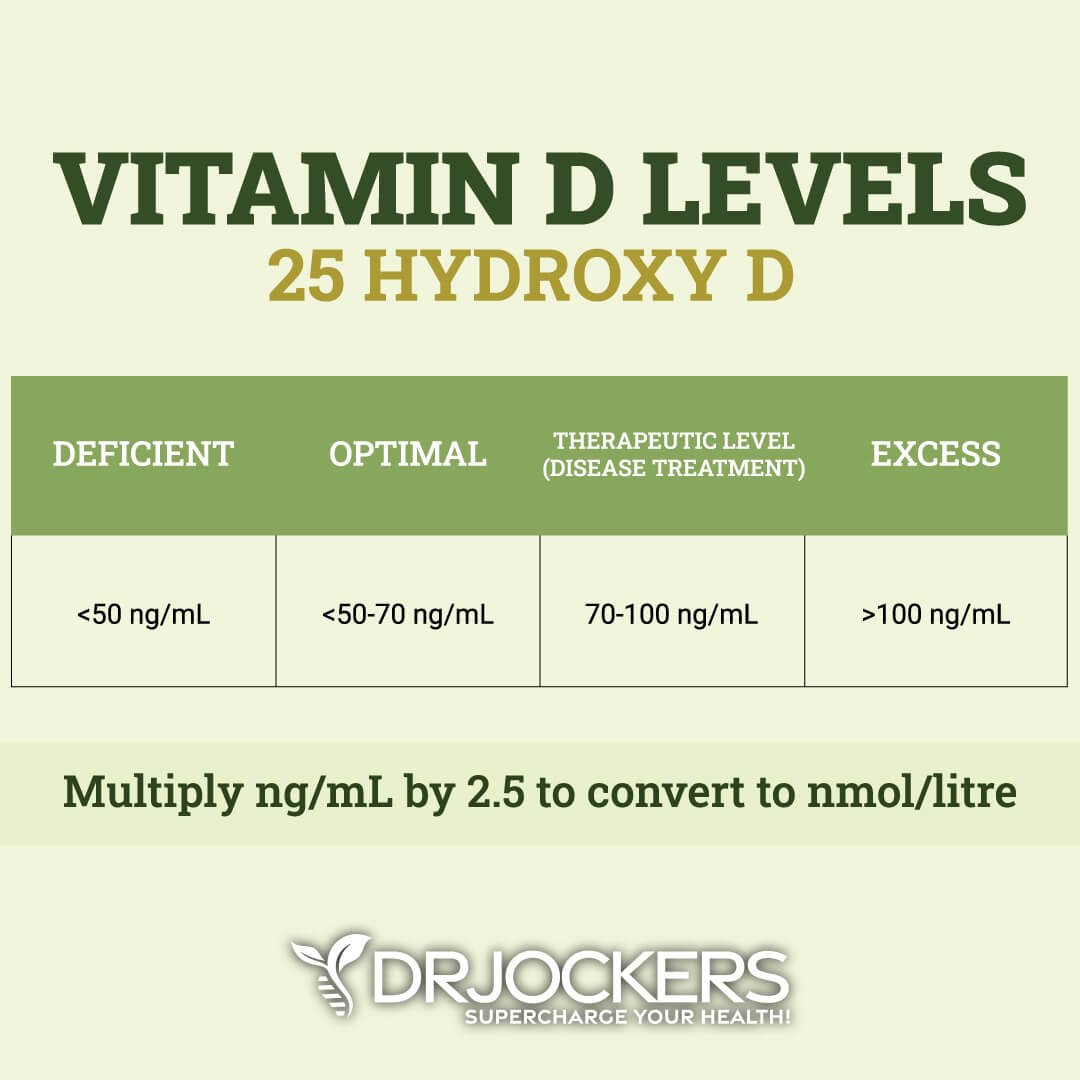
Low Vitamin D
Vitamin D is important for your immune, bone, muscle, and vascular health. Vitamin D helps your blood vessels to stay healthy and the blood flowing. Vitamin D helps to relax the blood vessels.
Deficiency in vitamin D causes the veins to struggle to do their job and can increase the risk of even health problems, including varicose veins. A 2015 study has found that vitamin D deficiency can increase the risk of lower-extremity deep vein thrombosis (13).
Natural Support Strategies for Varicose Veins
Natural support strategies for varicose veins address the major causes and the root issue of the condition. This information has been evaluated by the FDA and is for informational purposed only and does not replace the medical advice you get from your doctor. Here is what I recommend:
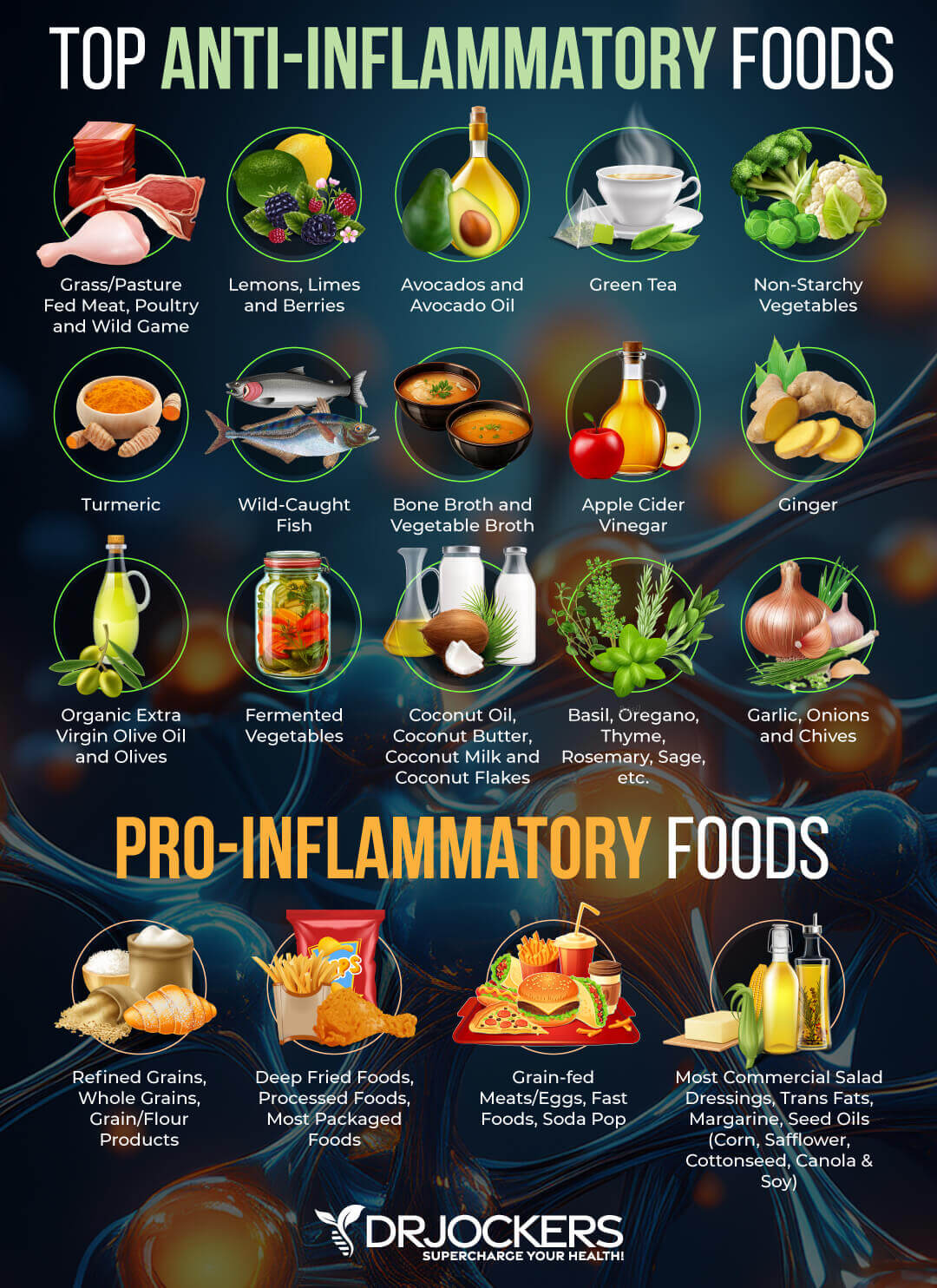
Anti-Inflammatory Nutrition Plan
Research studies have shown that chronic inflammation is one of the main underlying causes and risk factors of varicose veins (3, 4). An anti-inflammatory nutrition plan can help.
Remove refined sugar, refined oils, conventionally raised animal products, artificial ingredients, highly processed foods, deep-fried foods, and junk foods. Keep your carb intake low, focusing on small amounts of low-glycemic index fruits and sweet vegetables while avoiding grains, refined sugar, and high glycemic index fruits.
Load up on antioxidant-rich and anti-inflammatory greens, vegetables, herbs, spices, and sprouts. Support your gut with fermented foods. Eat plenty of healthy fats, including avocados, coconut oil, coconut butter, coconut, nuts, seeds, organic butter and ghee, and fats from pasture-raised animal sources.
Enjoy clean protein, such as grass-fed beef, pasture-raised poultry and eggs, organ meats, wild-caught fish and seafood, and wild game. Eat organic whenever possible and available.
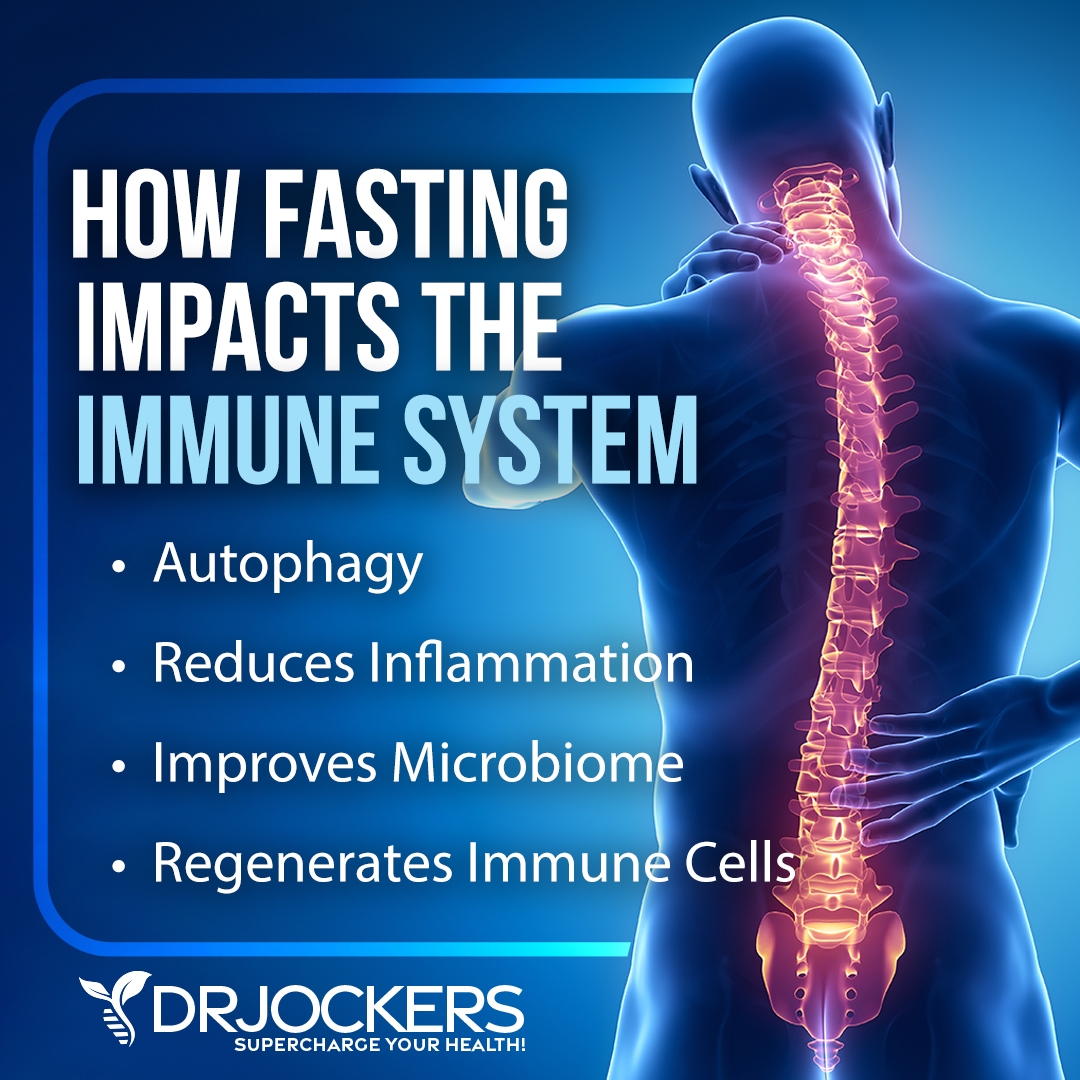
Intermittent Fasting
We know from research that chronic inflammation and insulin resistance can increase the risk of developing varicose veins (3, 4, 5, 6). Intermittent fasting can help with both. Intermittent fasting is a way of eating that cycles between periods of fasting (not eating) and feasting (eating) within a day.
According to a 2014 study published in the International Journal of Health Science (Qassim), intermittent fasting can reduce chronic inflammation, proinflammatory markers, and the risk of disease (14). According to a 2019 review and meta-analysis published in the Journal of Clinical Medicine, intermittent fasting can reduce insulin resistance and also lower body mass index (15). Since being overweight or obese are both risk factors for varicose veins, it is another risk factor intermittent fasting can potentially reduce.
If you are new to intermittent fasting, I recommend that you start with a Simple Fast, which involves 12 hours of fasting including your overnight sleep. Simply stop eating after dinner and don’t eat until breakfast 12 hours later. Increase your fasting window gradually.
Most people find that 16 hours of fasting brings them the most benefits, however, you may find that a slightly shorter or somewhat longer window works better for them. However, if you are currently pregnant, I don’t recommend intermittent fasting for varicose veins and you should focus on the other natural support strategies only.
Regular Movement and Exercise
Sitting or standing for an extended period of time can increase your risk and symptoms of varicose veins (2). Regular exercise can also help weight loss and weight management, reduce the risk of obesity, lower inflammation levels, keep stress levels down, and reduce insulin resistance, which are all risk factors for varicose veins (2, 3, 4, 5, 6).
If you have a desk job or have to sit or stand for extended periods of time, I recommend that you get up, move around, and stretch regularly. Even if you have to stay at your desk or workstation for a long period, make sure to change your position, shake out your legs, move a bit, and stretch regularly.
Stay active throughout the day by taking a short walk in the morning or at lunch, taking the stairs, walking or biking instead of driving whenever possible, dancing to your favorite song, and playing with your kids or pets. Exercise regularly at least 20 to 30 minutes 5 days a week mixing up cardiovascular exercise, strength- and resistance training, and low-impact workouts. Walking, biking, swimming, light jogs, leg lifts, trampoline workouts, or simply rocking your feet can help to move your legs and reduce varicose veins.

Compression Socks
Compression socks and stockings are often recommended for varicose veins, as well as to reduce the risk of deep vein thrombosis or swelling. According to a 2004 study published in Dermatologic Surgery, compression socks can reduce swelling of the legs (16).
During your sleep, laying in a horizontal position, your vein valves function better than when you’re sleeping or standing. This is the reason why you may feel better in the morning but experience more swelling or pain later in the day. Putting on your compression socks or stockings can support healthy blood circulation throughout the day and reduce pain, swelling, and other symptoms.
There are a variety of compression socks on the market. Depending on the stage of your varicose veins or symptoms, you can choose between mild, moderate, firm, and extra firm compression. To choose the right size, take measurements right in the morning before or right after you get out of your bed at the narrowest part of your ankles and widest part of your calves as your knees bend at a 90-degree angle.
If you need thigh-high stockings, make sure to also take measurements while standing on your thighs right under your buttocks and measure the length of your legs from your buttocks to the floor. If you are uncertain what size or kind of compression socks or stockings you need, talk to your healthcare provider, they can help.

Reduce Stress & Improve Sleep
Chronic stress and poor sleep can increase inflammation, weight gain, and insulin resistance, which are all risk factors for varicose veins (2, 3, 4, 5, 6). Hence reducing stress and improving sleep is critical. Reduce stressful situations as much as possible in your life. Learn to manage and respond to stress better.
Create positive mindset shifts throughout the day and look for opportunities to laugh. Practice meditation, breathwork, progressive relaxation strategies, visualization, journaling, gratitude, and prayer. Exercise regularly and spend time in nature. Seek a supportive community, spend time with friends and family, and also find daily ‘me-time’.
Support your circadian rhythms by going to bed and waking up around the same time each day. Develop a nighttime routine that relaxes and calms your body, mind, and soul. Avoid electronics, sugar, caffeine, food, and stress in the evening.
Try herbal tea, healing baths, and other calming activities, such as board games, coloring, reading, meditation, and prayer. Invest in comfortable pillows, bedding, and mattress, black-out curtains or eye masks, and anything that makes your bedroom a calm sanctuary.

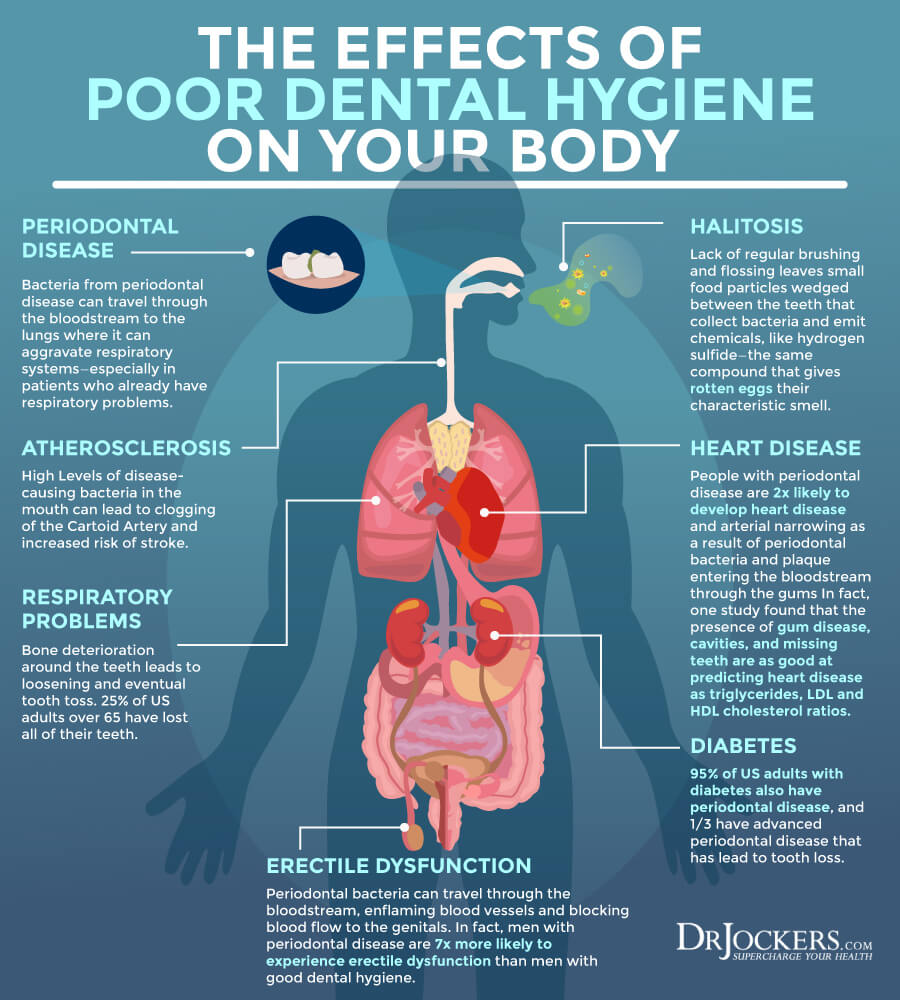
Holistic Oral Health
Chronic periodontal disease and oral health issues can increase your risks of varicose veins (9). I recommend a holistic oral health practice. Starting your day with 20 minutes of oil pulling by swishing coconut oil around your mouth can help to reduce bad bacteria, pull out toxins, and improve oral health.
Use organic, natural, and fluoride-free toothpaste and dental products. Use plastic-free toothbrushes, such as bamboo toothbrushes. Visit a holistic dentist who can help to remove any amalgam fillings and take care of any dental problems with adding toxicity to your body.
They can recommend specific holistic oral health protocols that may help your specific issues. You can look for a holistic dentist in your area on IAOMT.org
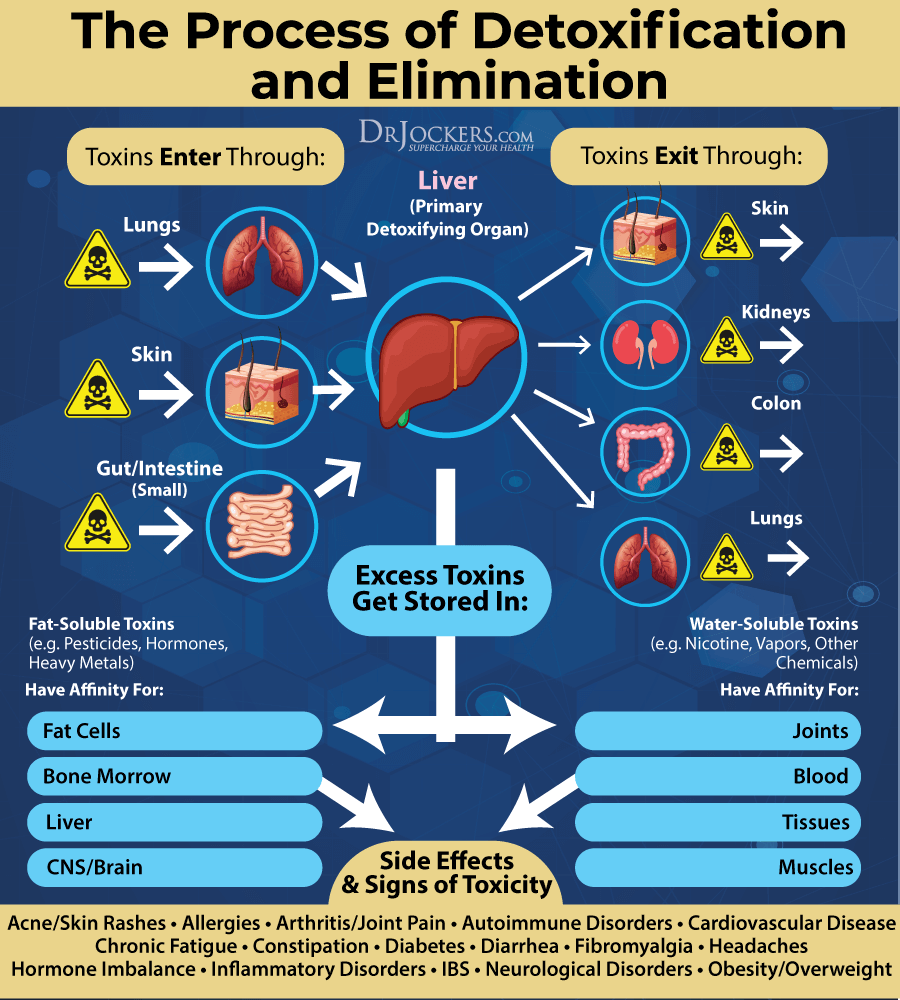
Improve Detoxification
Chronic infections, chronic inflammation, and toxic exposure can increase your risks and symptoms of varicose veins making detoxification incredibly important (8, 9). Oil pulling in the morning is one important way to pull out toxins from your body. Exercising and using an infrared sauna regularly can increase detoxification through sweating. Dry brushing daily before your shower can remove dead skin cells, increase lymphatic flow, and support detoxification.
Eating an anti-inflammatory diet can improve your gut health and support detoxification. Bioactive carbon and activated coconut charcoal can both help to remove toxins from your gut. Working with a functional medicine practitioner like myself and my team can help to identify your personal issues. They can recommend specific supplements and dietary strategies that can address your personal issues.
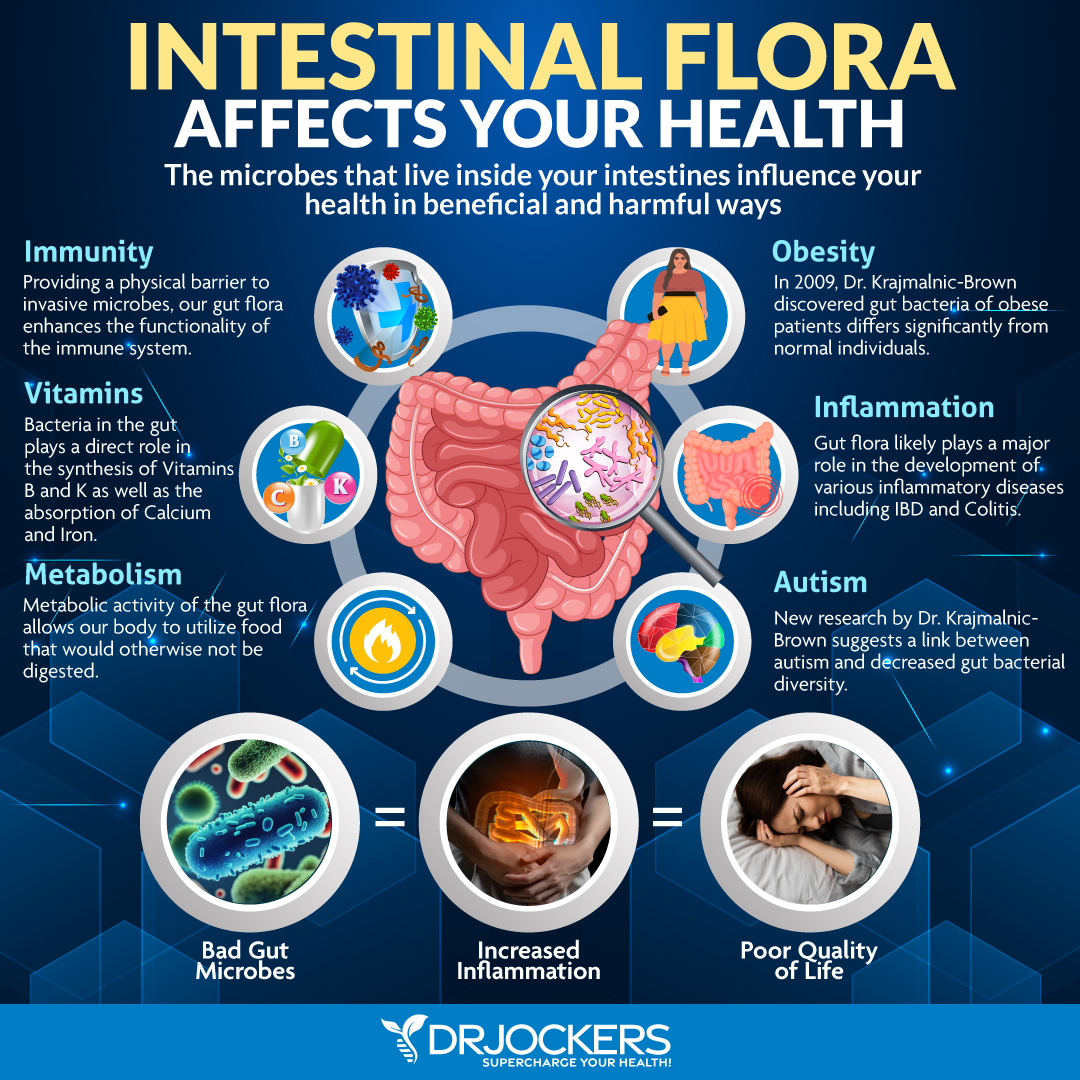
Support Gut Health
Chronic infections, chronic inflammation, obesity, and insulin resistance can all increase your risk of varicose veins all of which are connected to your gut health (2, 3, 4, 5, 6, 8, 9). Supporting your gut health through a gut-friendly, anti-inflammatory diet is critical.
Eat plenty of prebiotic-rich foods, such as Jerusalem artichokes, onions, garlic, asparagus, leeks, and jicama roots, and probiotic-rich fermented foods, such as sauerkraut, kimchi, fermented vegetables, kefir, and kombucha. Take a daily dose of probiotic supplement. Take digestive enzymes before meals to support your digestion. Work with a functional medicine practitioner to uncover and address any underlying gut health issues.
Key Nutrients for Varicose Veins
There are certain vitamins and key nutrients that can play a role in your natural support protocol for varicose veins.
B Vitamins
Homocysteine levels and MTHFR function are connected to the development of varicose veins (10, 11, 12). According to a 2016 study published in Nutrients, B vitamins, specifically vitamin B6, B12, folate, and riboflavin can help to lower homocysteine levels (17).
I recommend that you eat plenty of foods high in B vitamins, such liver, meat, eggs, leafy greens, and seeds, and also take daily vitamin B complex supplements. Since many people have issues with methylation, make sure to get a pre-methylated supplement.
Vitamin D
Research has shown that vitamin D deficiency can increase the risk of varicose veins (13). To optimize your vitamin D levels, it is important that you spend time in the sun daily whenever it’s possible and eat foods rich in vitamin D, such as organ meat, eggs, and fatty fish.
However, it’s challenging for most people to meet vitamin D needs through food and sunshine alone, so I recommend a daily Vitamin D/K2 supplement. Vitamin K2 helps the absorption of vitamin D.
Typically taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml.
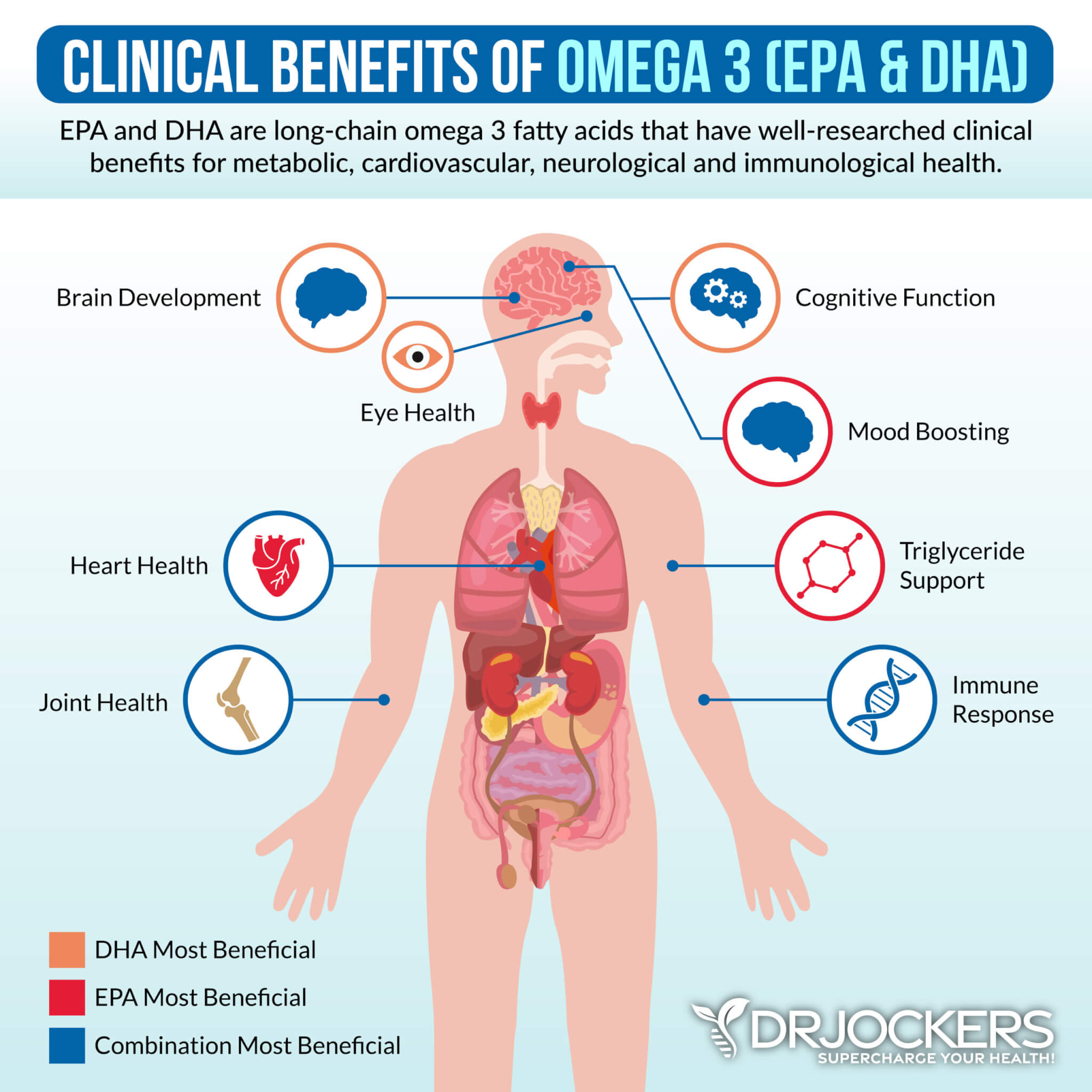
Omega-3 Fatty Acids
Omega-3 fatty acids are healthy fats that are known to help to reduce chronic inflammation. According to a 2016 study published in Nutrition, Metabolism, and Cardiovascular Diseases, omega-fatty acids can improve vascular health (18).
According to a 2017 study published in Prostaglandins and Other Lipid Mediators, omega-3 fatty acids can help to reduce inflammation and vascular tone and improve vein health (19). I recommend that you eat plenty of omega-3-rich foods, such as wild-caught fish and seafood, algae, flax seeds, chia seeds, and hemp seeds. Additionally, taking omega-3 fish oil supplements daily can be very beneficial.
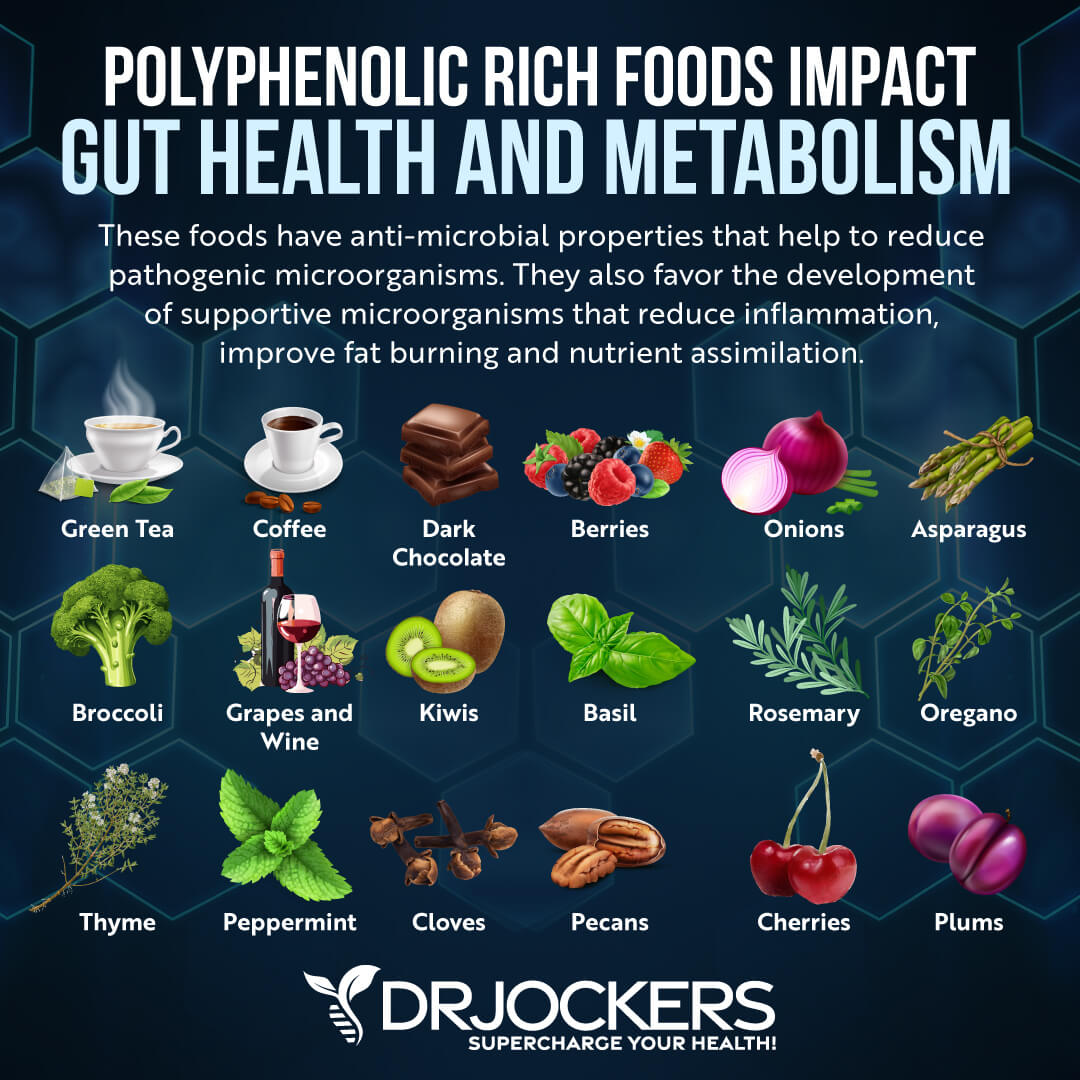
Dietary Polyphenols
Polyphenols are naturally occurring organic compounds in many plant foods that offer an array of health benefits, including reduced inflammation and chronic symptoms. A 2019 study published in Nutrients has found that dietary polyphenols can improve the gut microbiome and reduce arterial stiffness (20). A 2013 controlled clinical trial published in the Journal of Science and Food Agriculture, grape seed extracts can help to reduce swelling in the legs caused by prolonged sitting (21).
A 2014 study published in the International Journal of Angiology has found that pycnogenol in pine bark can improve chronic venous insufficiency and improve vein health (22). According to a 2019 review published in the International Journal of Molecular Science, resveratrol also supports the vascular system by reducing inflammation and oxidative stress (23).
According to a 2019 study published in Evidence Based Complementary and Alternative Medicine, curcumin can also support the health of your veins (24). You can find all these herbal compounds in supplements. I highly recommend that you add them to your daily routine to reduce inflammation and support vein health.
Final Thoughts on Varicose Veins
Varicose veins are a common health concern characterized by painful, bluish-purple, swollen, and raised veins. Even though they are common, you don’t have to suffer from them. Try my top natural support strategies for varicose veins to support your health and improve your well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



Do you know of any stories of people being able to eliminate current varicose veins once they made changes to their lifestyle? I would love to know if that’s possible. I currently have varicose veins. Two days a month they are painful but mostly I don’t like how they look. Over the last years I have made many of these lifestyle changes you suggest but my veins are still there. Perhaps they lifestyle changes have kept them from getting worse but I really want to eliminate them. I think I am only in stage two. Thanks.
Yes many people do see results with healthy lifestyle principles improving varicose veins.