 Epilepsy: Risk Factors and Natural Support Strategies
Epilepsy: Risk Factors and Natural Support Strategies
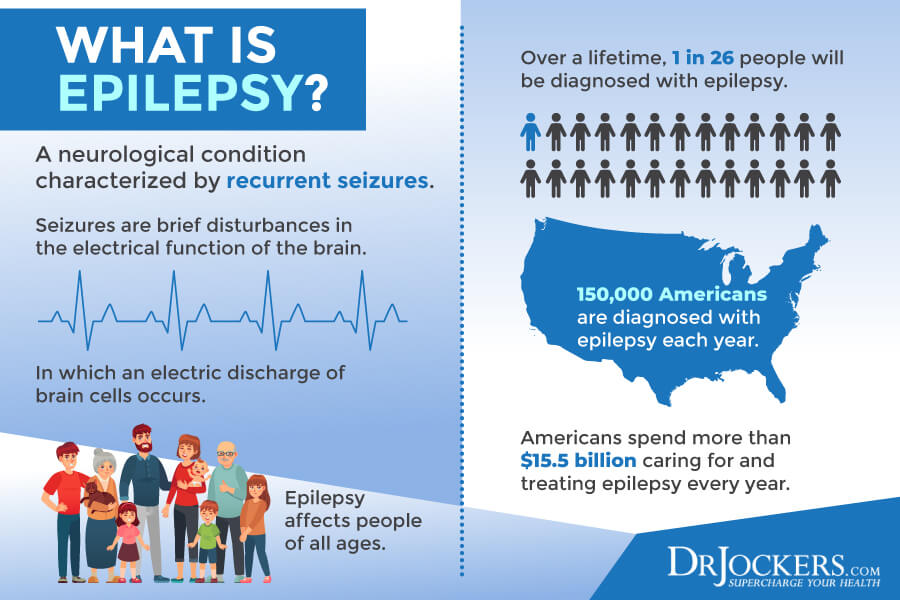
Epilepsy is a chronic health condition. It is a form of seizure disorder that’s characterized by recurrent, reflexive, or unprovoked seizures. Even though it’s a chronic disease, it is possible to manage the conditions, reduce or even eliminate seizures, and some people do completely recover. Natural dietary and lifestyle strategies can help you to reduce your risks and triggers for epileptic seizures.
In this article, you will learn what epilepsy is. You will understand the signs and symptoms of epilepsy. You will learn about the main types of epileptic seizures. You will understand the causes of epilepsy. I will discuss how epilepsy is diagnosed and the main conventional treatment options available to you. You will learn what to do if someone has a seizure. I will share my top natural support strategies for epilepsy to improve your health and well-being.
What Is Epilepsy
Epilepsy is a misunderstood condition as most people believe that epilepsy and seizures are the same. However, according to the Epilepsy Foundation, epilepsy and seizures are not the same things (1).
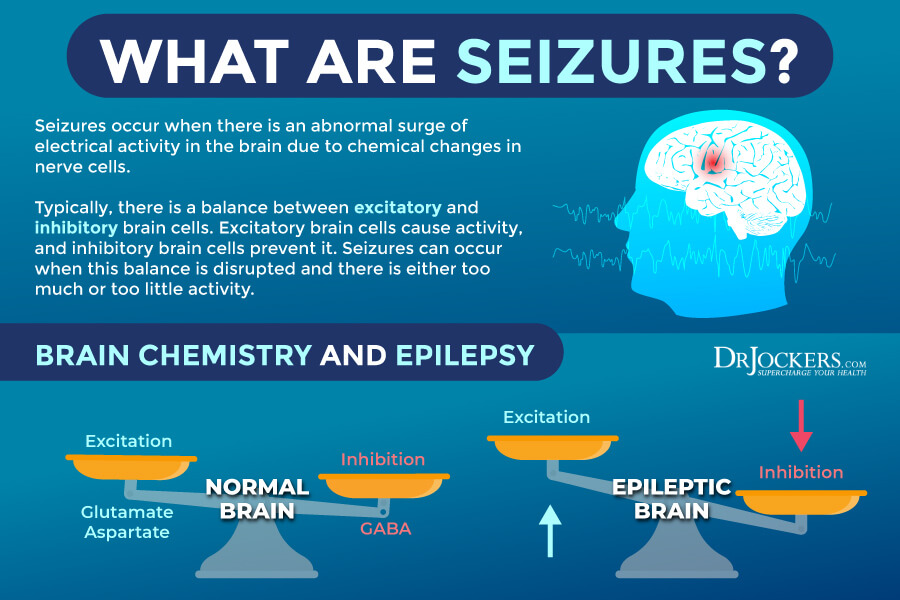
A seizure is one single neurological event characterized by an interruption of the electrical communication signals between your neurons in your brain. While seizures certainly affect your nervous system, they are one-time events.
Epilepsy, on the other hand, is a chronic disease characterized by recurrent and reflexive, or unprovoked, seizures. Epilepsy is just one form of seizure disorder. There are many different forms of seizures that fall under the umbrella of seizure disorder, including single seizure episodes and various types of epilepsy. Having one single seizure doesn’t necessarily mean that you have epilepsy, though it can be a warning sign.
Epilepsy is a chronic disease characterized by epileptic seizures and consequent neurobiological, psychological, cognitive, and social issues. Its definition and diagnostic criteria have evolved over the years. Today, someone is generally considered to have epilepsy if they have two or more unprovoked seizures within 24 hours.
While having one unprovoked seizure can increase the risk of another seizure within the ten years after the episode, an initial seizure usually doesn’t prompt an epilepsy diagnosis. Yet, some doctors still may assume an epilepsy diagnosis even when the patient doesn’t fit the criteria.
As the definition of epilepsy is evolving, some experts criticize the current criteria. They point out that the current definition ignores certain important aspects of epilepsy, including a possible genetic component and the fact that there are people who have recovered from the disease. Even though epilepsy is a chronic disease, some can overcome the condition. Some people may have age-dependent epilepsy syndrome that goes away once they pass a certain age. If someone is seizure-free for ten years after not taking seizure medications for at least five years, they will no longer be considered someone with epilepsy.
Signs & Symptoms of Epilepsy
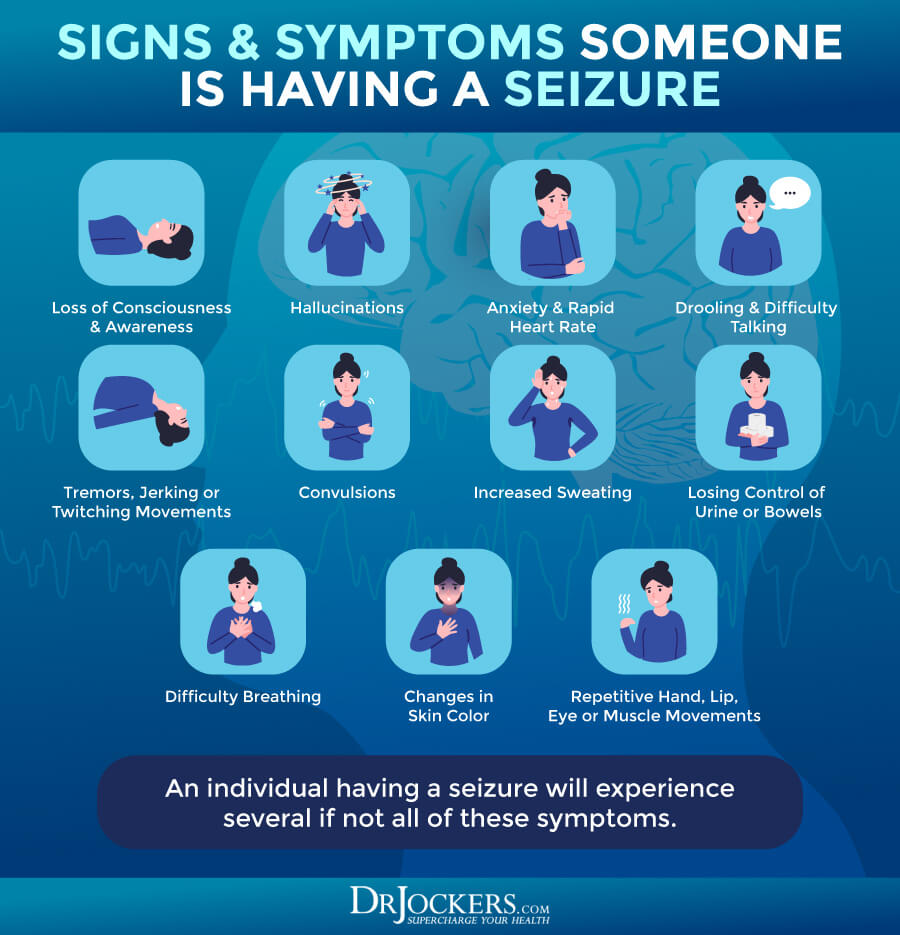
Signs and symptoms of epilepsy are not so clear-cut as there are different types of seizures that can differ in frequency and severity. Generally speaking, epileptic seizures are characterized by loss of muscle and motor control, shaking, convulsing, loss of awareness or consciousness, changes in mood, and issues with emotional regulation.
They may cause accidents, falls, mood changes, emotional complications. They may result in complications during pregnancy, lead to other secondary problems, or increase the risk of health issues.
Each seizure has its beginning, middle, and end characterized by different symptoms.
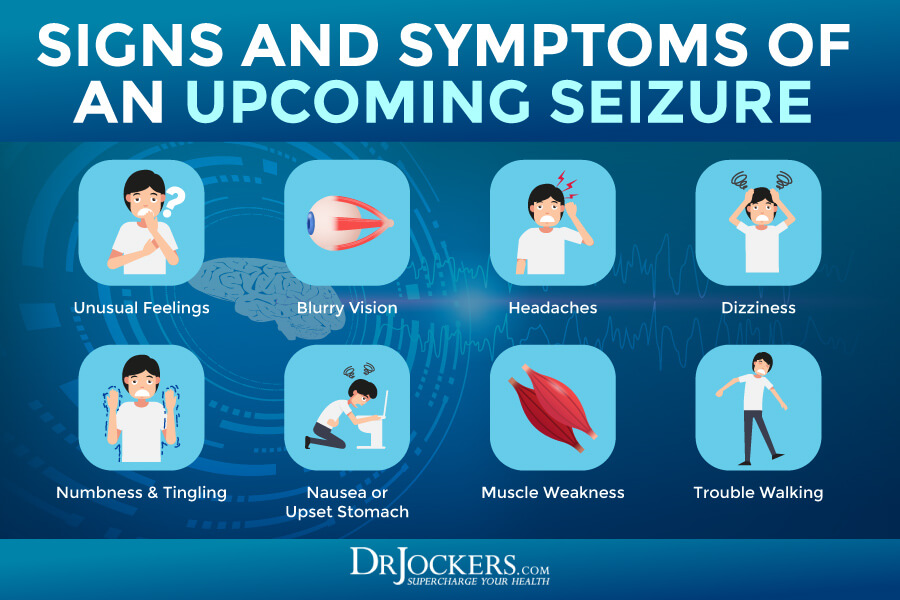
Signs and symptoms that may indicate the beginning stage of a seizure:
- Unusual feelings or changes in thoughts
- Visual loss or blurry vision
- Changes in sounds, tastes, or sights
- Headaches
- Dizziness or lightheadedness
- Tingling or numbness
- Nausea
- Upset stomach
Signs and symptoms of the middle stage of a seizure:
- Confusion, forgetfulness, or memory lapses
- Unconsciousness
- Loss of awareness
- Experiencing unusual smells, tastes, or sounds
- Blurry vision, flashing lights, or loss of vision
- Hallucinations
- Tingling, numbness, or feelings of electric shocks
- Anxiety, panic, racing heart, or mood changes
- Difficulty swallowing
- Drooling
- Difficulty talking
- Tremors, jerking, twitching, or other signs or lack of movement or muscle tone
- Repetitive hand, lip, eye, or other muscle movements
- Increased sweating
- Convulsion
- Losing control of urine or stool
- Difficulty breathing
- Changes in skin color
Signs and symptoms of the end stage of a seizure or after a seizure:
- Sleepiness
- Confusion or memory loss
- Lightheadedness, dizziness, or feeling fuzzy
- Difficulty talking, writing, or completing other tasks
- Sadness, feeling upset, anxiety, feeling scared, or other mood changes
- Headache
- Nausea
- Feeling thirsty
- Having to go to the bathroom urgently
- Cuts, bruises, head injury, broken bones, or other injuries due to a fall or other accident as a result of the seizure
Types of Epileptic Seizures
There are different types of epilepsy syndromes that may be differentiated based on (2):
- The type of seizures
- Causes of the seizures
- Factors that trigger the seizures
- The age of onset
- Inherited seizures or not and genetic information
- What parts of the brain involved during the seizures
- Severity of the seizures
- Frequency of the seizures
- Patterns shown on the electroencephalogram (EEG) during and between seizures, and findings on a brain magnetic resonance imagining (MRI) or computed tomography (CT) scan.
- Other disorders involved.
- Prospects of recovery or worsening
There are three main types of seizures: generalized onset seizures, focal onset seizures, and unknown onset seizures (2).
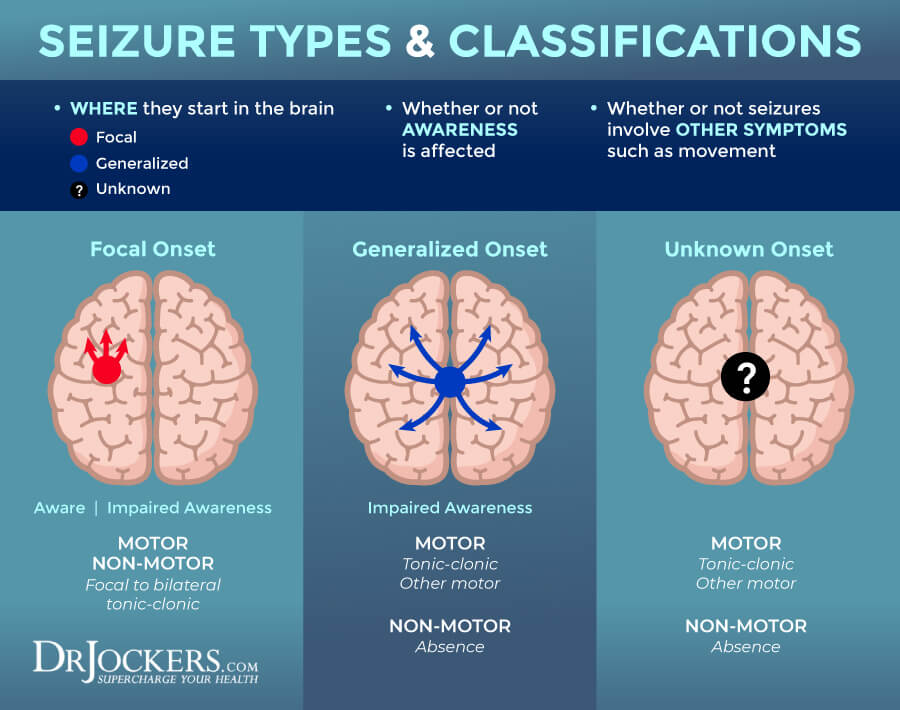
Generalized Onset Seizures
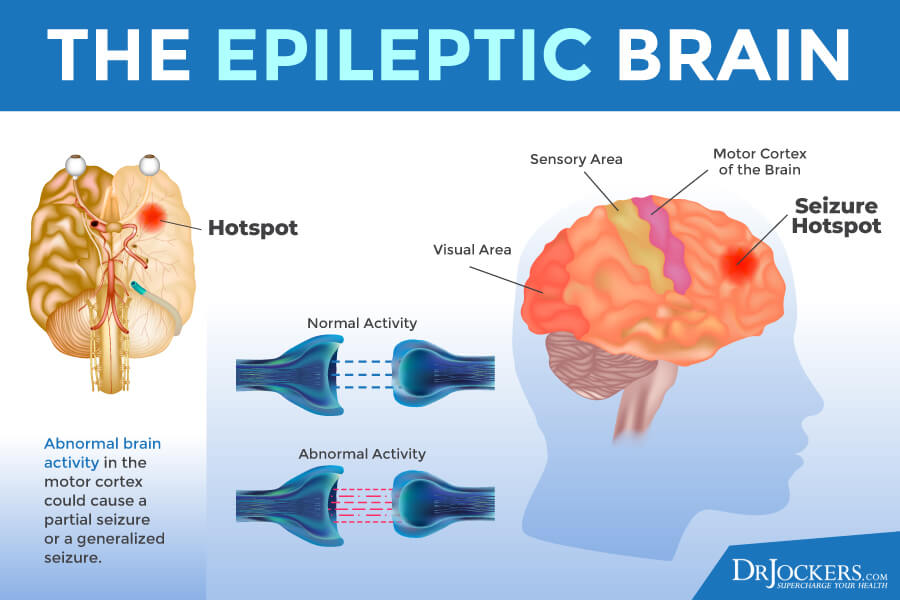
Generalized onset seizures are seizures that strike on either both sides of your brain or groups of cells located on both sides of your brain. This group of seizures includes tonic-clonic, absence, and atonic seizures among others (2).
Symptoms of generalized onset seizures may include (2):
- Motor symptoms, such as rhythmical jerking (clonic), muscle weakness or limp muscles (atonic), muscle twitching (myoclonus), tense or rigid muscles (tonic), or epileptic spasms
- Non-motor symptoms, including staring spells or brief twitches of the eyelids.
Focal Onset Seizures
Focal onset seizures are seizures that start in one area of the brain or in a group of cells on one side of your brain. During a focal onset aware seizure, you are both awake and aware during the seizure. This seizure may also be called a simple partial seizure. During a focal onset impaired awareness seizure, there is the confusion of impaired awareness during the seizure. This seizure may also be called a complex partial seizure (2).
Symptoms of focal onset seizures may include (2):
- Motor symptoms, such as rhythmical jerking (clonic), muscle weakness or limp muscles (atonic), muscle twitching (myoclonus), tense or rigid muscles (tonic), or epileptic spasms, and repeated automatic movements, including clapping, lip-smacking, chewing, rubbing of hands, or running
- Non-motor symptoms, such as changes in sensations, emotions, cognition, and autonomic functions, such as goosebumps, waves of cold or heat, gastrointestinal issues, or racing heart, or behavior arrest characterized by a lack of movement.
Unknown Onset Seizures
Unknown onset seizures describe seizures where the beginning of the seizure is unknown. They may occur at night or during other circumstances where there are no witnesses (2).
Symptoms of unknown onset seizures (2):
- Motor seizures with symptoms, including tonic-clonic or epileptic spasms
- Non-motor seizures with symptoms, including behavior arrests, staring, and not moving
Causes and Risk Factors for Epilepsy
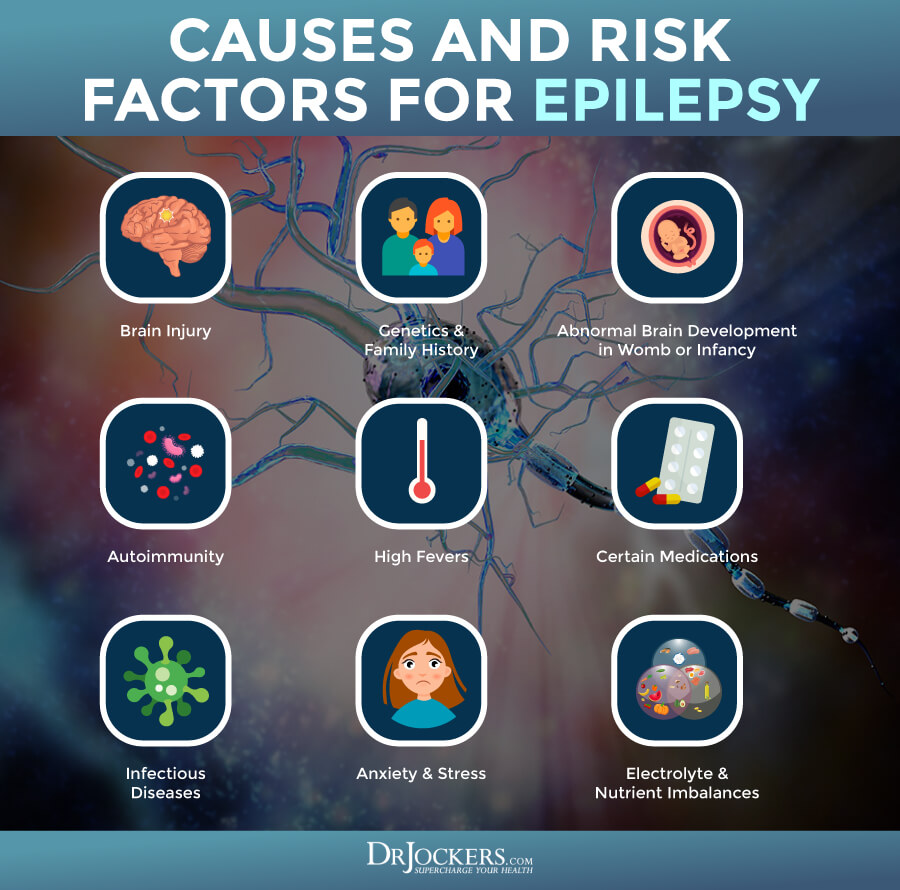
The exact cause of epilepsy in the majority of the cases is unknown. Though seizures and epilepsy may develop at any age, children and individuals over the age of 60 tend to be at higher risk than others.
Epileptic seizures tend to occur because of an interruption in the electrical activity somewhere in the central nervous system. Some of the following conditions and incidents may increase the risk or contribute to the development of epilepsy (4):
- Brain injury
- Tumors, dementia, strokes, and other brain conditions that cause brain damage
- Genetics
- Family history of seizures or epilepsy
- Abnormal brain development in the womb or during infancy due to poor nutrition during pregnancy, oxygen deficiency, infections in the mother or the child, cerebral palsy, or other issues.
- Infectious diseases that affect the brain, including meningitis, viral encephalitis, and AIDS
- Neurotransmitter imbalance or impairment in the brain channels for cellular communication
- Autoimmunity in autoimmune epilepsy (5)
- High fevers or certain medications may cause seizures, though they don’t necessarily lead to epileptic seizures or epilepsy
- Electrolyte imbalances and nutrient deficiencies
- Anxiety and stress
- Alcohol use and alcohol withdrawal
Diagnosing Epilepsy
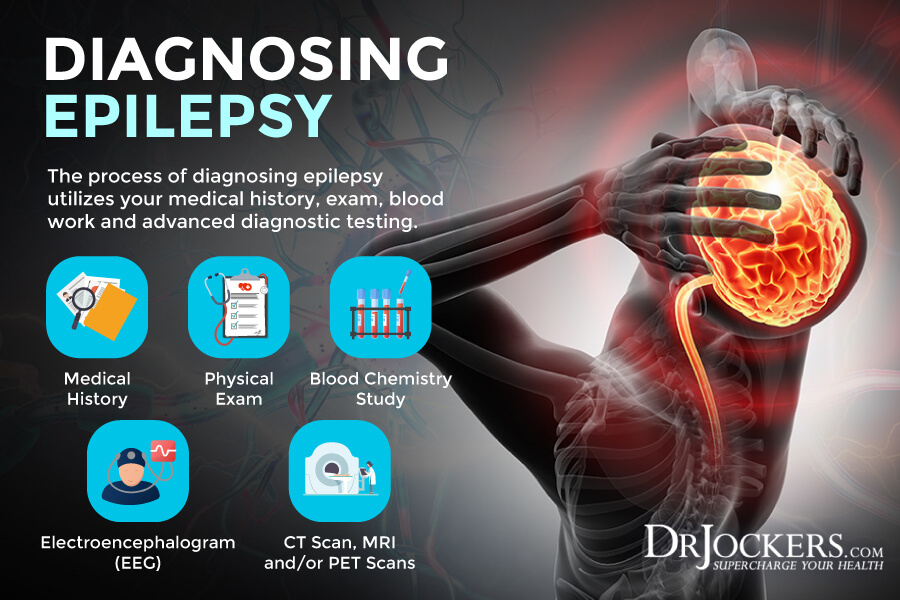
If you have experienced a seizure or several seizures, it is critical that you see a doctor urgently. Seizures can be a sign of some serious health issues. Getting the right diagnosis as soon as possible is the first step of getting appropriate treatment and moving towards recovery.
Your doctor will go over what happened and the circumstances of your seizure. They will go over your medical history, family history, and symptoms. After a physical, they will move onto a neurological examination to check your motor and mental functioning.
Before diagnosing epilepsy, your doctor has to rule out some other health issues that may also cause seizures. They will order a complete blood count, a blood chemistry test, and possibly some other blood test to look for and rule out problems related to:
- Signs of infectious diseases
- Liver and kidney functioning
- Blood glucose levels
The next step is usually an EEG, which is the most common test for diagnosing epilepsy. Your EEG technician will attach electrodes to your scalp to record electrical activity in your brain and possible seizures while performing certain tasks. In some cases, it may even be used during sleep. Don’t worry, it is a completely non-invasive and painless test.
Other than an EEG, you may need some imaging. CT scans, MRI scans, positron emission tomography (PET) scans, single-photon emission computerized tomography are used to find or rule out tumors and other abnormalities that may cause seizures. In most cases, epilepsy is diagnosed if you’ve had several seizures and your seizures occur for no apparent or reversible reason (6).
Conventional Treatments
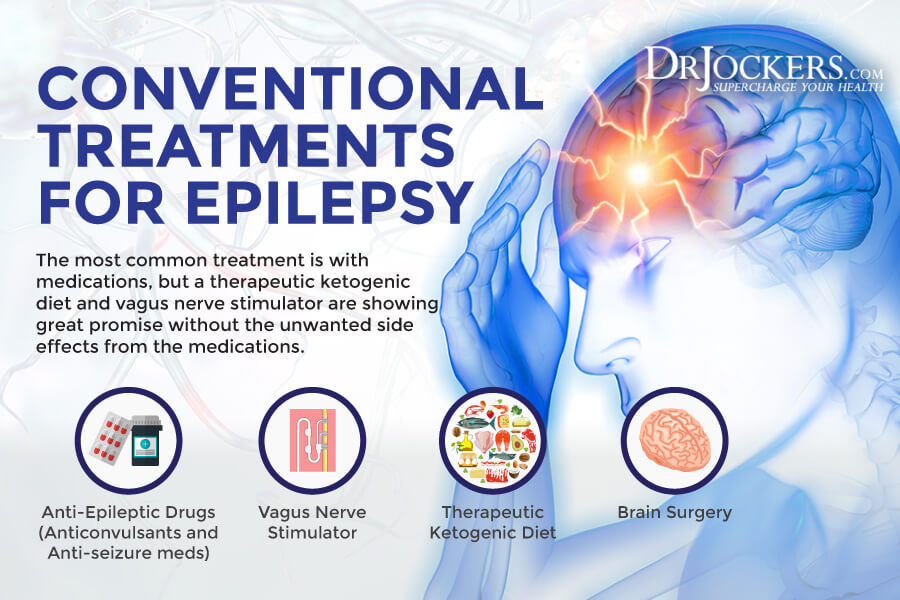
Your epilepsy treatment plan will greatly depend on your overall health, your symptoms, the severity of your symptoms, and how well you respond to certain methods of therapy. Research is ongoing and new methods may develop as we speak (7).
The most common treatment options at this point include:
- Anti-epileptic drugs: Anti-epileptic drugs, including anticonvulsants and anti-seizure medications to reduce the number and frequency of your seizures. In some cases, these medications may completely eliminate seizures (7).
- Vagus nerve stimulator: A vagus nerve stimulator is a medical device that’s surgically placed under your skin on the chest. It uses electronic stimulation on the nerves that move through your neck to prevent seizures. A 2019 review published in Neurosurgery Clinics of North America has found that 50 percent of participants found a 50 percent reduction in seizures over a two-year period (8).
- Ketogenic diet: The ketogenic diet is a common treatment option for seizures. Over half of patients who don’t respond to anti-epileptic drugs see improvement from a high-fat, low-carbohydrate keto diet. A 2019 study published in Frontiers in Neuroscience has found that a ketogenic diet can be highly effective in both adults and children with seizures without major side effects (9).
- Brain surgery: Brain surgery is used in more severe cases. They remove or change a certain part of your brain where the seizures are happening (7).
What to Do If Someone Has a Seizure
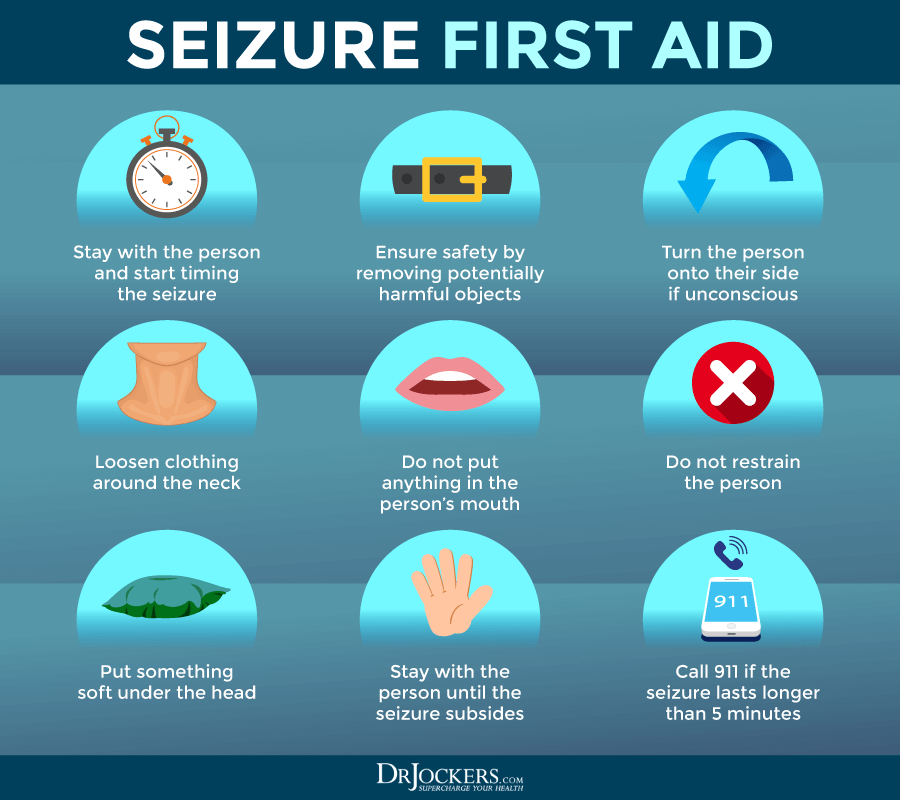
Witnessing someone having a seizure can be a scary experience. It is important that you do not panic and keep your cool.
If you see someone having a seizure (10):
- Only move them if they are in danger, for example, by a busy road or near a hot stove
- If they are on the ground, cushion their head
- Loosen any tight clothing around the neck, such a tie, scarf, collar, or turtle neck, to help them breathe
- If they have convulsions, turn them on their side to help them stoop
- If they are in a wheelchair, put on the breaks and keep the seatbelt on
- If they are in a wheelchair, make sure to support their head with a cushion but don’t move them
- Do not put your finger or anything else in their mouth
- Try to remember the start and the end time of the seizure
- Stay with the person and talk to them calmly during and after the seizure
- Make sure that they have no drink or food until they are completely recovered
Calling 911 is not always necessary. Not everyone needs to go to a hospital. Many people with epilepsy, especially with more regular seizures, wear a special bracelet or carry a card to inform people about their condition if they have a seizure (10).
Call 911 for an ambulance if (10):
- It’s their first seizure
- The seizure lasts longer than 5 minutes
- The person doesn’t regain full consciousness after the seizure
- The person has several seizures without regaining consciousness
- The person is seriously injured from a fall or other accident-related to the seizure
Try to take note of any information that may be useful to a doctor and the person with the seizure, including (10):
- What happened, and what were they doing before the seizure?
- Did they talk about any unusual smell, taste, or other sensation?
- Did their mood change suddenly before? For example, did they experience anxiety, anger, or excitement?
- How did you notice that they were having a seizure? Did they fall? Did their body move strangely? Did their eyes roll back or head turn? Did they make a strange noise?
- Was the seizure sudden without warning?
- Did they lose consciousness? Did you notice any altered awareness?
- Did their body stiffen? Did they jerk or twitch? What body parts had these reactions?
- Did they go pale, blue, or flushed, or did their color change in any other way? If yes, what parts (lips, face, hands, etc)?
- Did they bite their tongue?
Did you notice any changes in breathing? - Did they mumble?
- Did they lose control of their bladder or bowel movements?
- How long did the seizure last?
- How did they feel or act after the seizure?
- Did they need to go to sleep after the seizure, and for how long?
If your loved one has epilepsy, encourage them to keep a seizure diary to record all these helpful details of each seizure. It can help their doctor. If you have epilepsy yourself, I recommend keeping a seizure diary (10).
Natural Support Strategies for Epilepsy
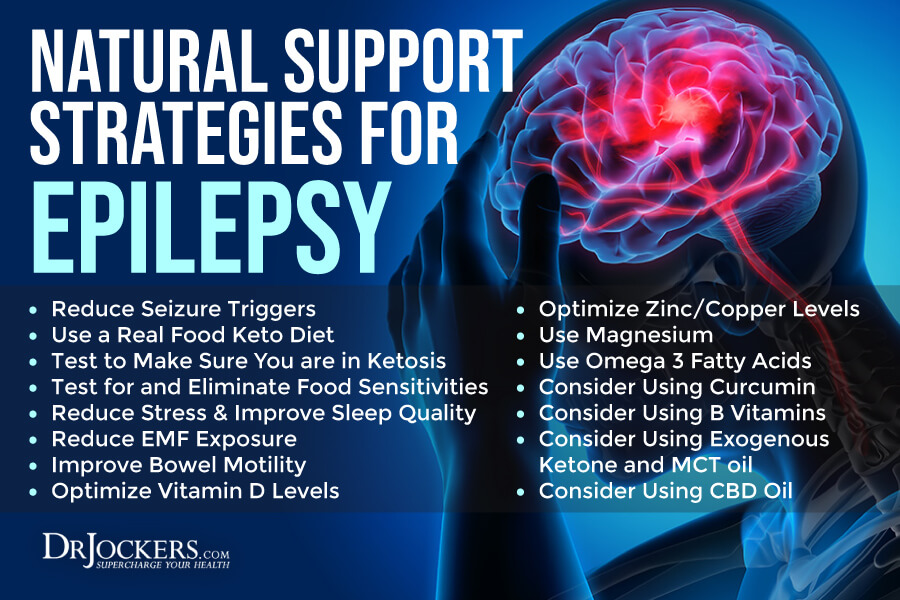
If you have epilepsy, there are a number of natural support strategies I recommend to reduce your seizures and improve your health.
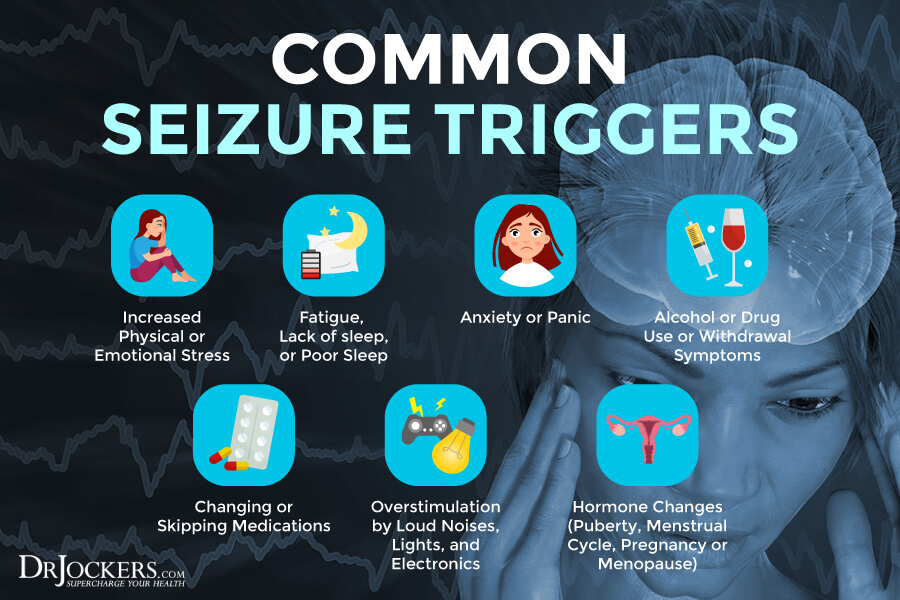
Reduce Seizure Triggers
Seizures can’t always be prevented. However, understanding, managing, reducing, or avoiding your triggers can significantly reduce your risks of having a seizure.
Common seizure triggers may include:
- Increased physical or emotional stress
- Fatigue, lack of sleep, or poor sleep
- Anxiety or panic
- Alcohol or drug use or withdrawal symptoms
- Changing or skipping medications, especially your anti-seizure prescription drugs
- Overstimulation by loud noises, lights, and electronics
- Hormonal imbalances and hormonal changes, especially during puberty, pregnancy, or menopause
To reduce your seizure triggers I recommend the following:
- Get regular sleep on a daily basis to reduce fatigue and stress.
- Reduce stress and stressors. Practice meditation, breathwork, visualization, relaxation strategies, gratitude, positive affirmations, prayer, and other strategies that may reduce stress, anxiety, and panic.
- Reduce or avoid alcohol and avoid illegal or not medically warranted prescription drug use.
- Make sure that you take your anti-seizure medication and other prescriptions as directed without skipping a dose or changing the schedule.
- Reduce the use of electronics, such as your phone, computer, television, and video games. Take breaks from your screen to lower mental strain.
- Improve your hormonal health and support transitional periods through a healthy diet and lifestyle. I recommend working with a functional medicine doctor. They can help you with some lab analysis to uncover hormonal issues and help you with a natural protocol to improve your hormonal health.
Get Into Ketosis
Believe it or not, the ketogenic it has been around and used for seizures by doctors since the 1920s. The ketogenic diet is a simple treatment approach since it only involves a dietary change. The keto diet is a high-fat, low-carb diet with carbohydrate levels very low at 5 to 10 percent, protein levels moderate at 30 to 35 percent, and fats high at 55 to 60 percent of your calories.
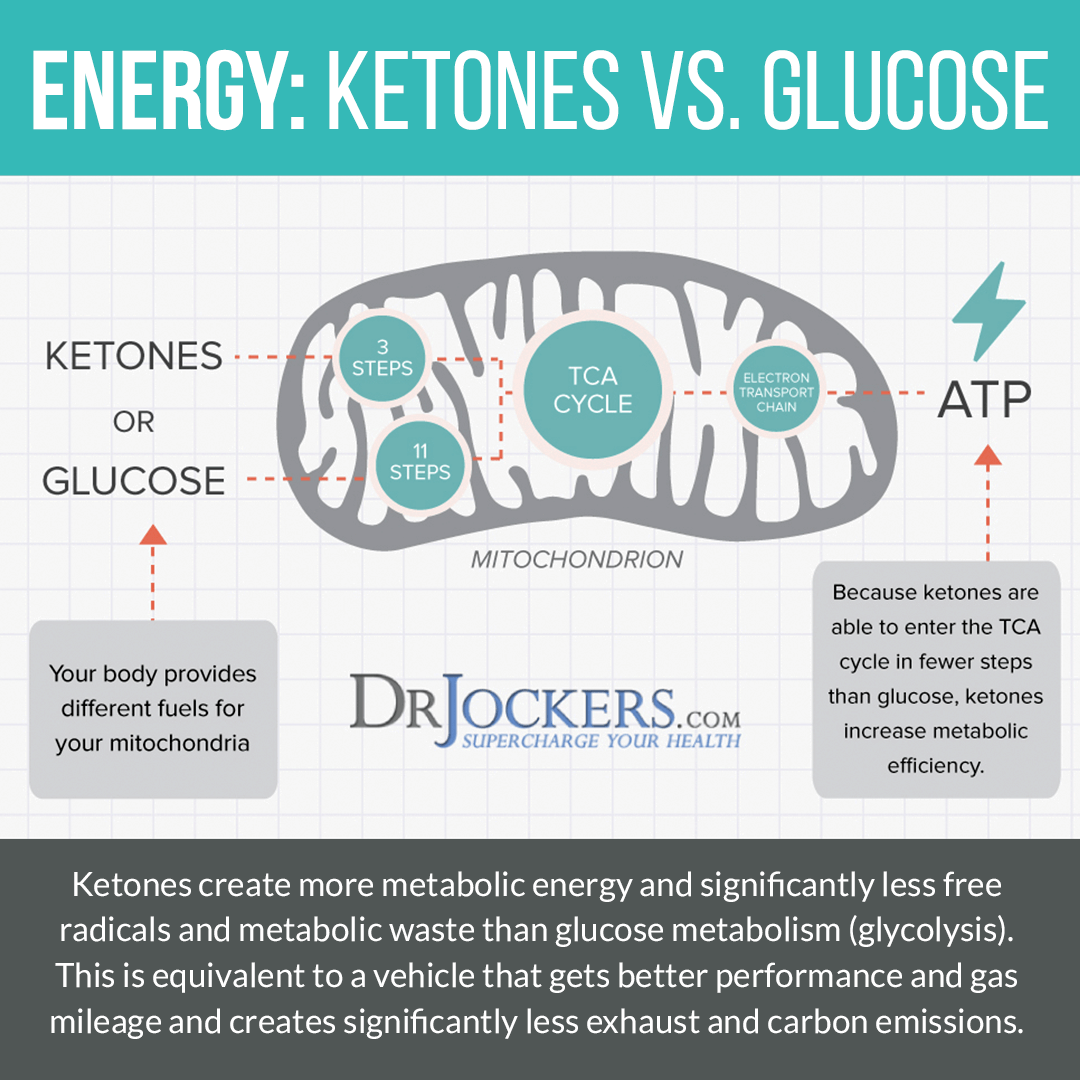
Usually, your body burns glucose for energy. When your body doesn’t have enough dietary glucose to burn for energy as a result of carbohydrate restriction, caloric restriction, or fasting, it will turn to fat for energy instead and starts to make ketones in the process. Ketosis has many health benefits, from reduced inflammation, increased insulin sensitivity, improved cellular renewal to a decreased risk of disease.
Ketosis and the keto diet also help reducing seizures, in fact, as I mentioned, it was one of the first things doctors recommended it for. When you are experiencing ketosis and your body uses fat for energy, neurons in your brain seem to start working and communicating differently. This may help to control and reduce your seizures.
Using the ketogenic diet is a popular and common approach for children, especially for those who take multiple antiepileptic drugs. A 2010 study published in the Canadian Family Physician has found the ketogenic diet is highly effective for children with epilepsy (11).
However, it is also an effective option for adults. A 2019 review published in Neurosurgery Clinics of North America has found that 50 percent of participants found a 50 percent reduction in seizures over a two-year period (8). A 2019 review published in Nutrients has found that the ketogenic diet may be effective for drug-resistant epilepsy (12).
It seems like that beyond altering your brain and neuron health, the keto diet also supports your gut microbiome, which may play a role in reducing symptoms. This is particularly important for those who have taken excessive doses of antibiotics that can lead to microbiome imbalance. The ketogenic diet can help to replenish good bacteria and improve balance. As you know, your gut and brain are closely connected and a healthy gut flora balance can support healthy brain function and neuron communication (8, 12).
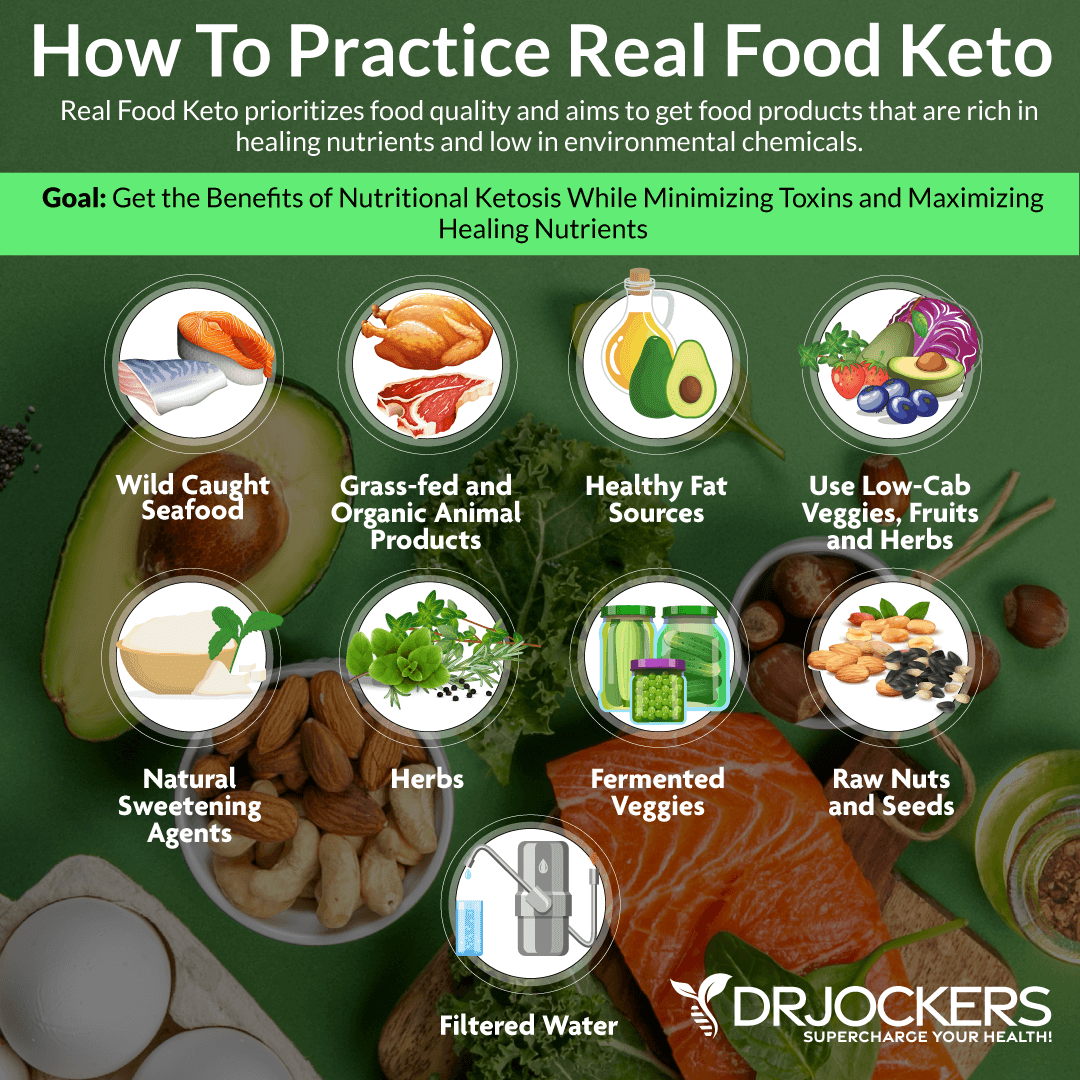
Use a Real Food Keto Diet
If you are following a ketogenic diet, it is crucial that you follow a real food keto diet. Keeping to your micronutrient ratios, keeping your fats at very high, carbs at very low, and protein at moderate levels, is critical for achieving ketosis. However, loading up on high-fat, low-carb, keto-friendly, such as low-nutrient junk foods, such as a burger with cheese without the bun, chicken deep-fried in refined oil, processed or canned meat, or diet sodas, may be convenient and keto-approved but can be detrimental to your health.
Real food micronutrients, such as vitamins and minerals are just as critical as your macronutrient ratios. Following an anti-inflammatory nutrition plan that supports your gut flora and brain health is not negotiable.
Follow an anti-inflammatory, real food ketogenic diet rich in greens, vegetables, herbs, spices, fermented foods, low glycemic index fruits, healthy fats, such as coconut oil, MCT oil, organic grass-fed butter or ghee, avocados, nuts, and seeds, and clean animal protein, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
Most of your diet should be abundant in healthy fats, including avocados, coconut oil, coconut butter, coconuts, avocado oil, extra-virgin olive oil, pasture-raised butter and ghee, lard, flax seeds, hemp seeds, chia seeds, pumpkin seeds, other seeds, olives, nuts, and any fats from clean animal foods, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
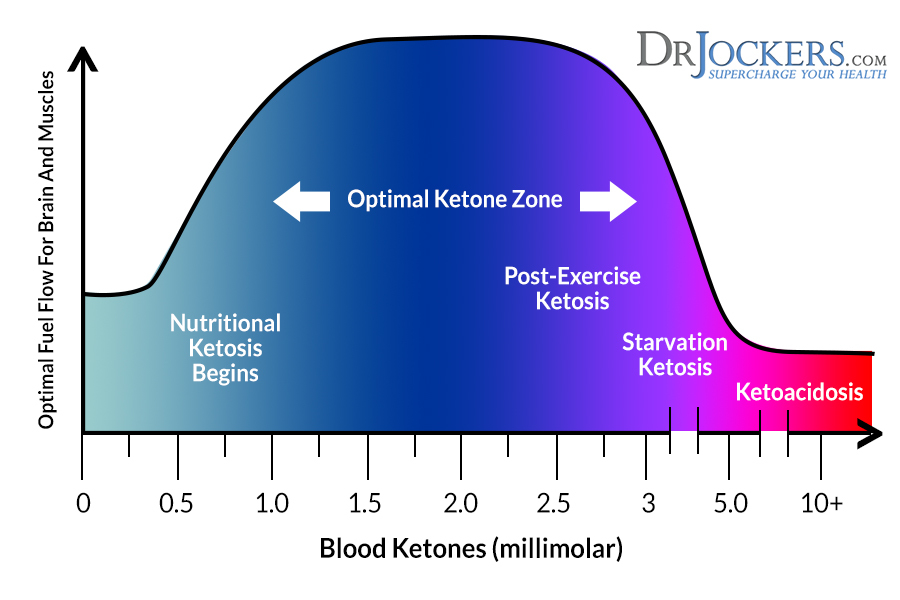
Test to Make Sure You Are in Ketosis
If you have epilepsy and following a ketogenic diet, you want to make sure that it’s working. More specifically, you want to make sure that you have achieved ketosis or a ketogenic state when your body is effectively burning fat for fuel.
I recommend that you test to make sure that you are in ketosis using an at-home strip test or a urine test. Working with a dietitian or functional health practitioner may be beneficial. They can help you to make sure that your transition to this new way of eating goes smoothly and that you successfully get into ketosis.
Blood measurement for the ketone Beta Hydroxybutyrate or BHB is considered the most accurate depiction of the ketogenic state. This is performed in a similar fashion to blood sugar testing.
Many of the blood glucose monitors on the market also have the ability to read blood ketones. Using a different type of testing strip, all you have to do is prick your finger, collect a small sample of blood, and place it into the monitor for a quick ketone measurement.
The monitor I usually recommend is the Keto Mojo monitor.
The ranges you are looking for here are as follows:
Very Low Ketone Levels: Less than 0.5 mmol/L
Mild Ketosis: 0.6-1.5 mmol/L
Optimal Ketosis: 1.6-3.0 mmol/L
Very High Ketone Levels: Greater than 3.0 mmol/L
Although mild ketosis can be achieved rather quickly, it can take up to 2-3 weeks to enter an optimized ketogenic state (2).
The only downside with blood ketone measurement is that the testing strips generally run for about $4 per strip. To perform daily ketone measurements using this method you would be looking at around $120 per month on just testing strips!
Test for and Eliminate Food Sensitivities
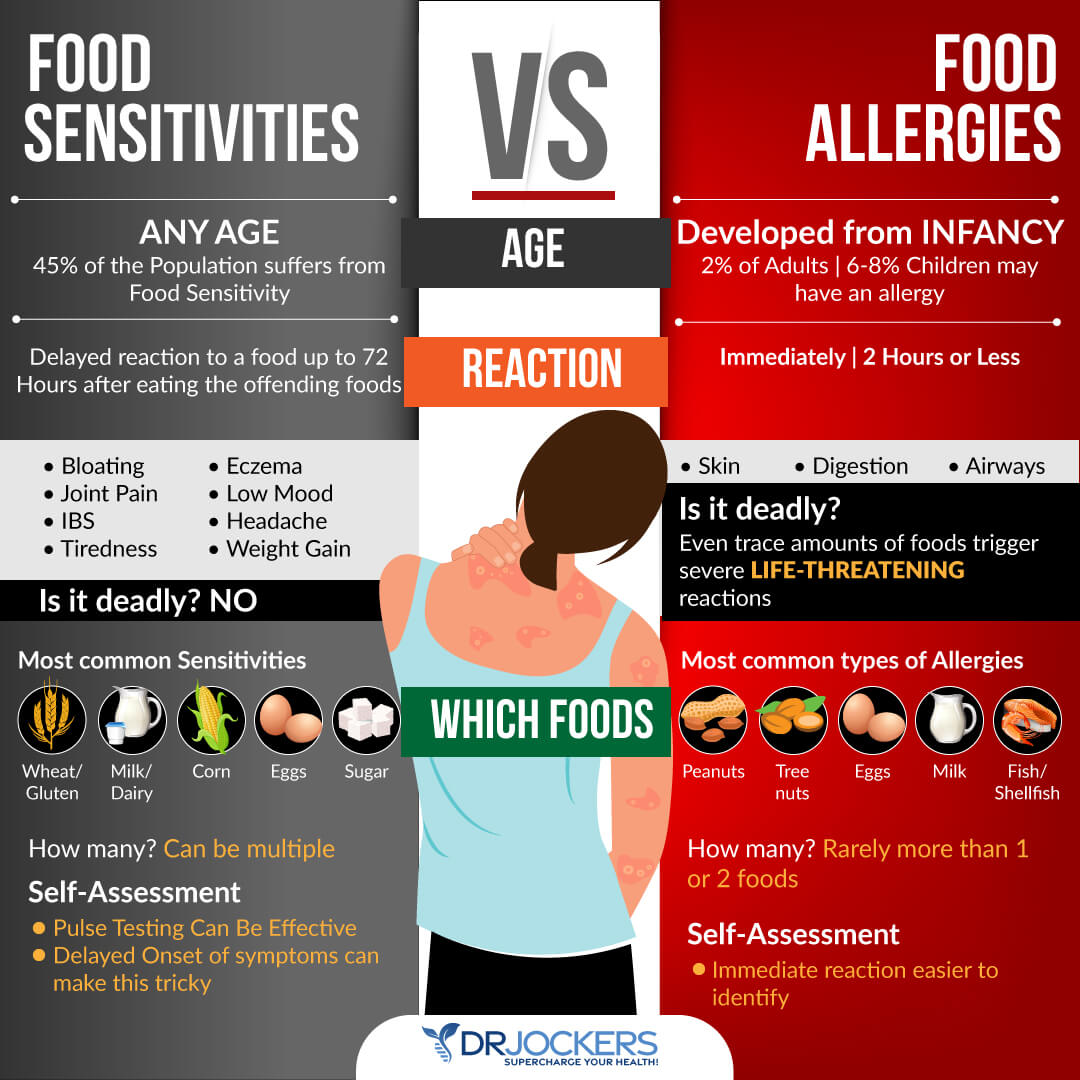
Food sensitivities can be triggering for seizures. Food sensitivities are different from food allergies. Food allergies cause an immediate reaction in your body, including hives, puffiness, digestive issues, difficulty breathing, or other symptoms after consuming a certain food. Food sensitivities, on the other hand, don’t lead to an immediate reaction. Instead, they cause issues over time.
When you eat a food that you are sensitive to, you may only experience symptoms a few hours or days later and inflammation and internal damage may also occur over a period of weeks, months, or even years. This damage may lead to gut or brain health or other issues that may trigger epilepsy.
Testing for food sensitivities and removing them is critical. The most common food sensitivities include gluten, dairy, soy, corn, peanuts, tree nuts, shellfish, and eggs. However, it is important that you find out what food sensitivities you have. Some people are sensitive to foods that are less common. There are various blood tests that can help identify food sensitivities. These tests may be a good start, however, they don’t test for every food and false results can also happen. Additionally to these tests, I also recommend that you try an elimination diet, pulse test, or muscle response testing.
Once you find your sensitivities, it is important that you immediately remove them from your diet. Since food sensitivities can change over time, I recommend that you test for them regularly, at least once a year, or if new symptoms occur. However, I recommend eliminating refined sugar, gluten, and conventional dairy completely for life.
Reduce Stress & Improve Sleep Quality
Reducing stress and improving your sleep quality may help to reduce your seizure triggers. I recommend that you reduce activities, situations, and interactions with people that stress you out. I also recommend that you practice meditation, breathwork, guided muscle relaxation strategies, visualization, gratitude, journaling, prayer, positive affirmations, and positive mindset shifts.
These strategies can help you lower your stress levels and manage stress better. Spending time in nature and exercise can also help to lower stress. You may also benefit from working with a therapist, counselor, spiritual counselor, or life coach to improve your anxiety and emotional stress.
I recommend that you go to sleep around the same time and wake up around the same time every day. This supports your natural circadian rhythms or sleep-wake cycle. Aim to sleep 7 to 9 hours a night. Avoid sugar, caffeine, heavy food, and alcohol late afternoon, in the evening, and late at night. Avoid electronics at least two hours before going to bed.
Choose calming and relaxing activities, such as calm conversations, crossword puzzles, coloring, journaling, reading, taking a healing bath, meditation, and sipping on herbal tea. Make sure that your bedroom is a safe and calm sanctuary. Salt lamps or relaxing essential oils, such as lavender may help. Invest in a supportive mattress, bedding, and pillows, and blackout curtains or an eye mask to enhance your sleep.

Reduce EMF Exposure
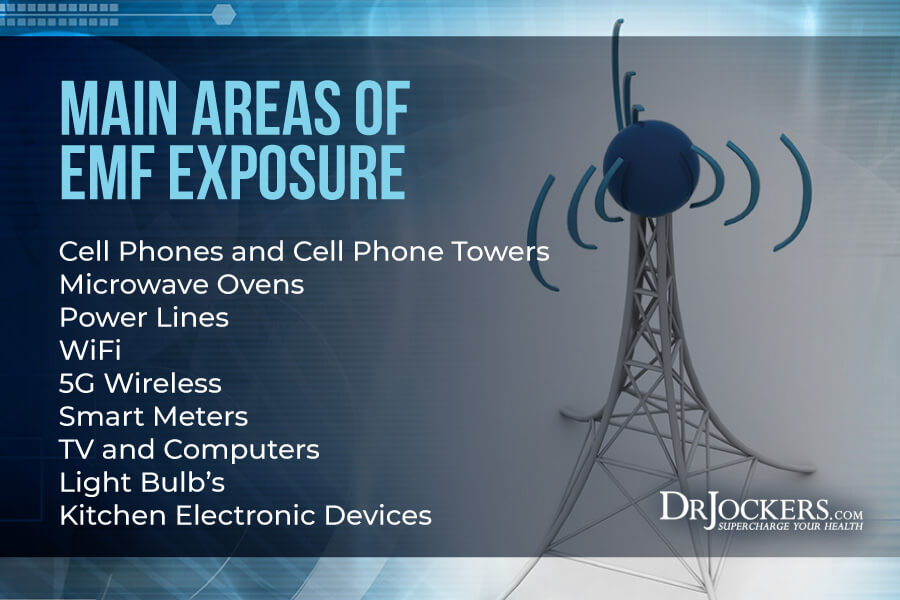
Electric and magnetic fields (EMFs) are invisible areas of energy. You may also hear EMFs being referred to as radiation. They are related to the use of electrical power, as well as various forms of lighting, including man-made and natural lighting.
EMFs can be grouped into two main categories based on their frequency: ionizing and non-ionizing radiation. Ionizing radiation is a high-level radiation that may be much more harmful to your body. Non-ionizing radiation is low-level radiation that includes appliances and tools that are thought to be relatively harmless to people.
However, it seems that long-term, regular exposure to low-level radiation can also lead to a variety of issues, including headaches, fatigue, blood sugar changes, hormonal changes, dizziness, irritability, anxiety, depression, and in some, even seizures.
A 2013 animal study published in Medical Science Monitor Basic Research has found that electromagnetic exposure has lead to seizures in mice (13). The higher the exposure was, the higher their chance was for severe seizure. Results suggest that acute electromagnetic exposure may increase the risk of epileptic seizures in humans as well.
A 2020 review published in Acta Epileptologia has also found that electromagnetic activity may be an environmental factor in epilepsy (14). They may also result in episodic seizures in non-epileptic patients. Some studies speculate that electromagnetic activity, such as geomagnetic activity, may play a role in sudden unexpected death in epilepsy (SUDEP). Other studies have found that exposure to GSM electromagnetic fields of cell phones may affect the frontal and temporal alpha rhythms of people. They found that those with epilepsy are more sensitive to GSM fields and their neuron activity may be affected by these electromagnetic fields.
On the other hand, electromagnetic fields may be used in the diagnosis and treatment of epilepsy. For example, rTMS, low-level artificial field exposure has shown a reduction in symptoms of patients with epilepsy. More research is needed to fully understand the role of electromagnetic fields (14).
Non-Ionizing Radiation Includes:
- Microwave ovens
- Cell phones
- Computers
- Tablets
- Wireless (WiFi) routers
- Bluetooth devices
- Power lines
- House energy meters
- MRIs
Ionizing Radiation Includes:
- Ultraviolet lights
- X-rays
Reduce Your Daily EMF Exposure Levels
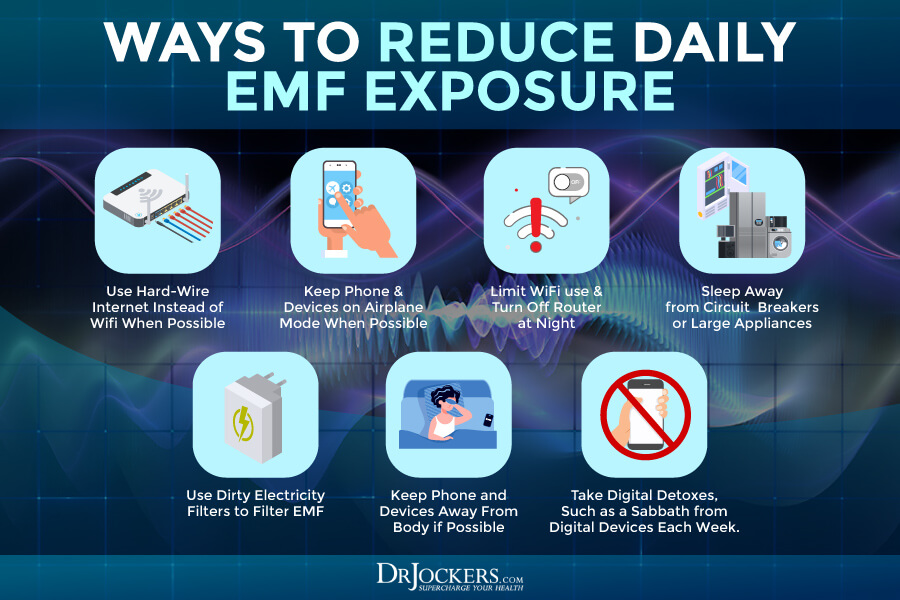
Follow the following steps to lower your EMF exposure throughout your day:
- Keep your phone, other devices, and appliances off or on airplane mode as much as you are able to.
- Use hard-wire internet connections instead of WiFi whenever it’s possible.
- Limit your WiFi use to the necessary minimum.
- Turn off your WiFi router at night and whenever you are not using it.
- Use hard-wire computer peripherals instead of wireless or Bluetooth connections whenever possible.
- Make sure that the electrical wiring of your home is done properly.
- Keep your electronic devices, such as your cell phones, computers, and tablets as far from your body as possible. For example, you may want to use headphones while talking on the phone. Turn off and put your devices down when not in use instead of keeping them in your pocket or on your lap.
- Keep your cell phone and other devices out of your bedroom.
- Sleep away from any circuit breakers or large appliances that may be running overnight.
- Use dirty electricity filters to filter out dirty electricity.
- Choose landlines or face-to-face contact whenever possible.
- Minimalize your use of cell phones, computers, and other digital devices. Take regular digital detoxes. For example, taking Sundays offline may be a great idea.
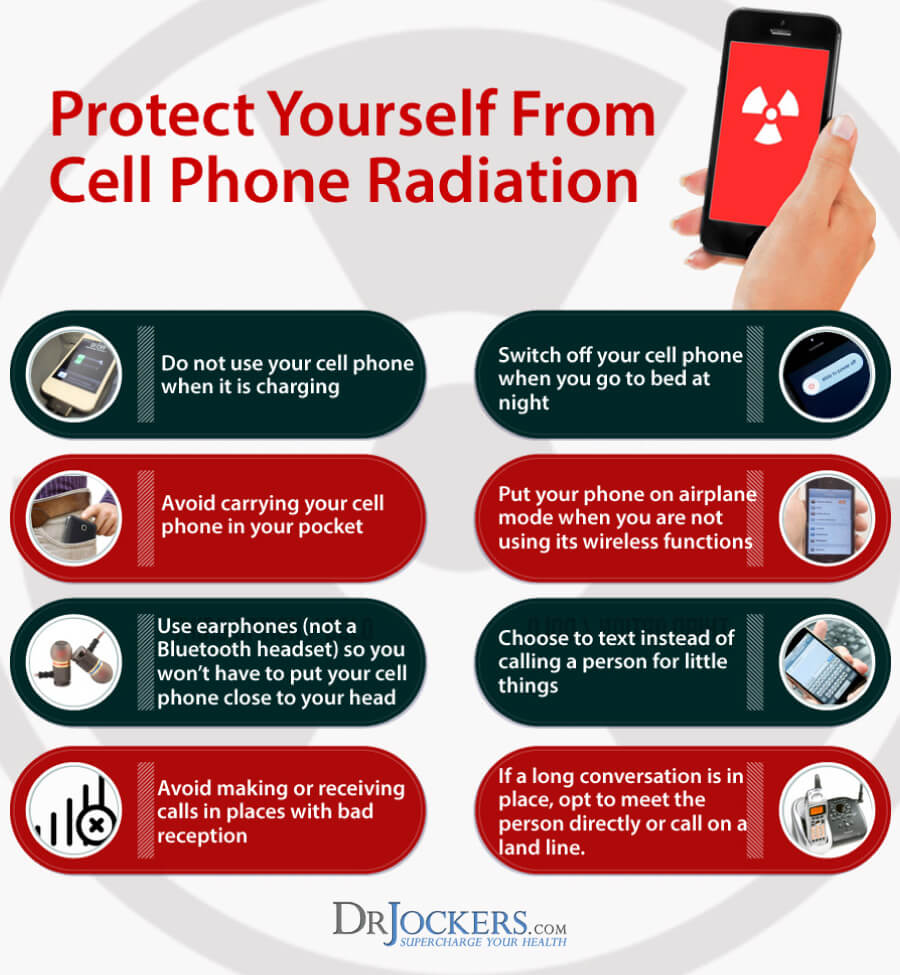
Protect Yourself From Cell Phone Radiation
While cell phones can certainly be handy, it is also important to protect yourself from cell phone radiation. Here are some strategies that can help you reduce your risks from cell phone radiation.
- Do not use your cell phone when it is charging.
- Switch off your cell phone when you go to bed at night.
- Avoid carrying your cell phone in your pocket.
- Put your cell phone on airplane mode when you are not using its wireless functions.
- Use earphones (not a Bluetooth headset) so you don’t have to put your cell phone close to your head.
- Choose to text instead of calling a person for little things.
- Avoid making or receiving calls in places with bad reception.
- If a long conversation is in place, opt to meet in person directly or call on a landline.
- Try an anti-radiation safe sleeve.
Improve Bowel Motility
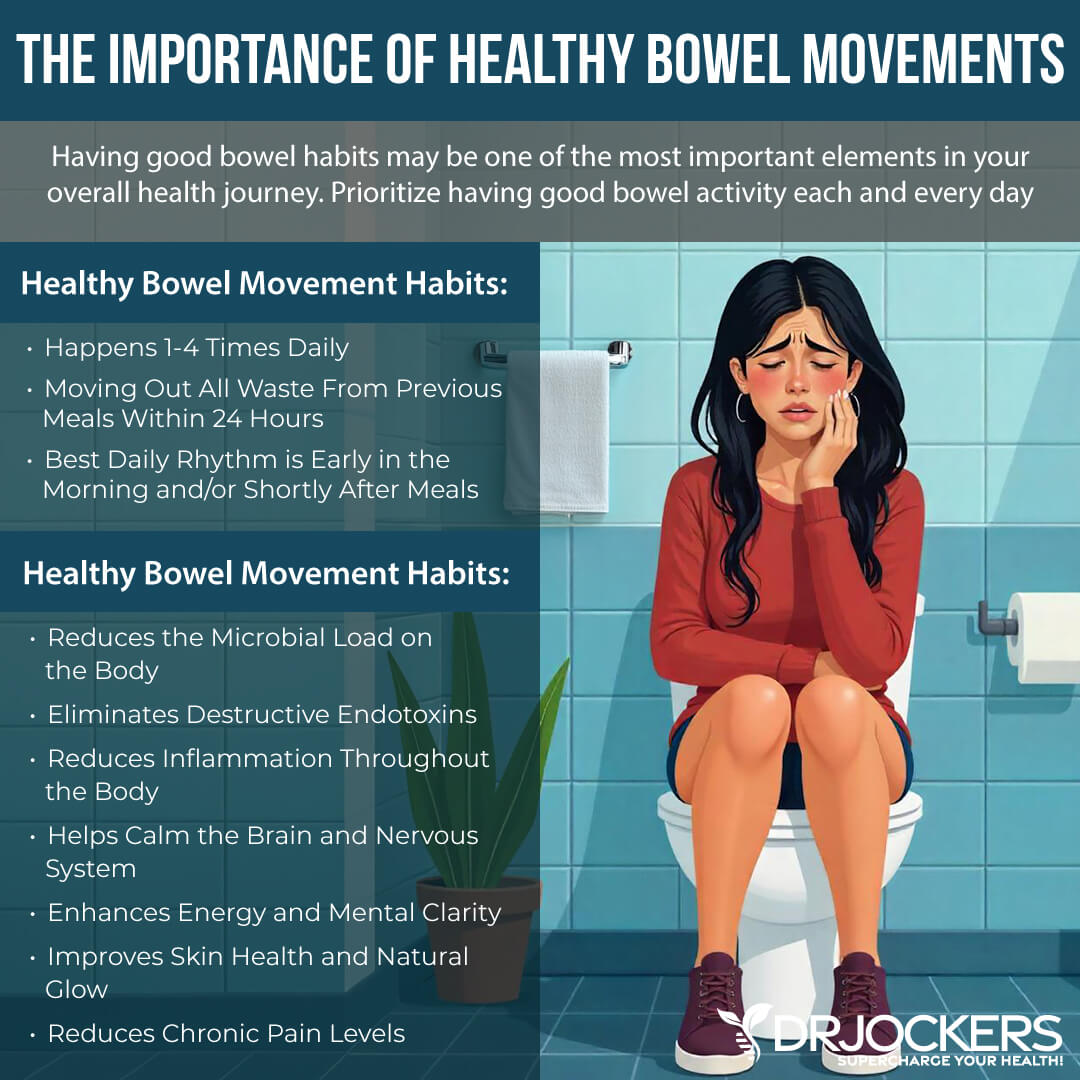
We already discussed how microbiome imbalance can affect your neurological and brain health and increase the risk of seizures (8, 12). But other gut health issues and poor bowel motility may play a role as well. A 2015 population-based study published in Medicine (Baltimore) has followed 32,122 patients with irritable bowel syndrome (IBS) and 63,295 control participants without IBS for 11 years (15). They found that irritable bowel syndrome (IBS) can increase the risk of epilepsy.
A 2015 animal study published in Epilepsy Behavior has found that constipation can also increase the risk of seizures (16). The problem is that anti-convulsant medications for epilepsy can increase the risk of constipation. Improving and supporting your bowel motility is critical for reducing your risks.
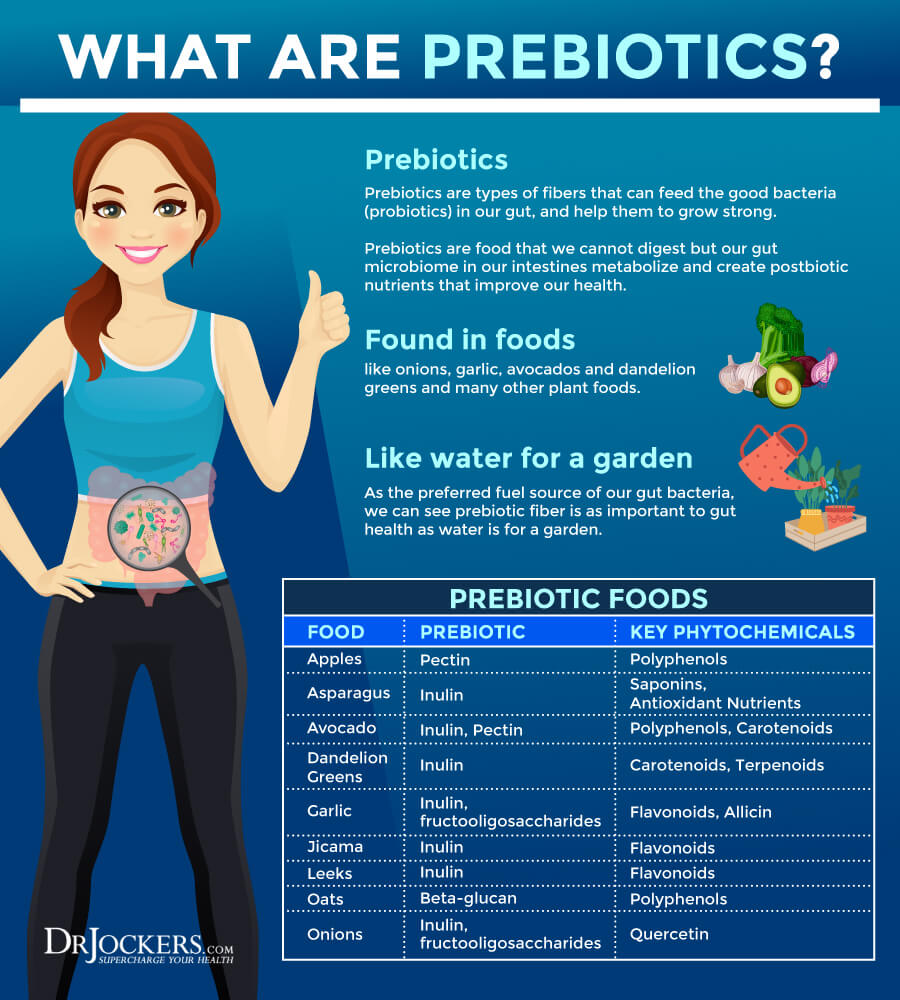
I recommend improving your bowel motility to support your digestion. Increasing your fiber intake is a common piece of advice for improving bowel motility. However, not everyone’s body deals with extra prebiotics and fiber well. For some people, prebiotics and fiber are very helpful for digestion.
For others, they may lead to problems, and too much can cause diarrhea or constipation. For example, if you are on a LOW-FODMAP diet for another health condition, prebiotics and fiber are not right for you. If you are following a carnivore diet or close to it, prebiotics is also not right for you. Know your body and experiment to find what works best for you. If prebiotics and fiber are triggering, reduce the amount of back off completely.
Proper hydration and electrolyte balance are critical for healthy bowel motility. Begin your day with 32 oz. of water. Drink regularly throughout the day, at least ten glasses a day or more if you are working out a lot, sweating, sick, or simply thirsty. Feeling thirsty means that you are already dehydrated. You can prevent this by drinking regularly. To support electrolyte balance, you may add a pinch of salt to your water, eat mineral-rich vegetables, and try an electrolyte balance powder.
Taking magnesium supplements can also support bowel motility and smooth bowel movements. You may also benefit from a magnesium and oxygen-based colon cleanser. It improves bowel motility, prevents and relieves constipation, improves your microbiome balance, and removes toxins from your colon.
Supporting your vagal nerve activity can also help to improve your bowel motility and digestion. Strategies that may improve your vagal tone include practicing gratitude and laughter, getting good sleep, meditation, prayer, deep breathing, stimulating your palatal muscles, social connections, cold exposure, exercise and movement, and following an anti-inflammatory nutrition plan.
Optimize Vitamin D Levels
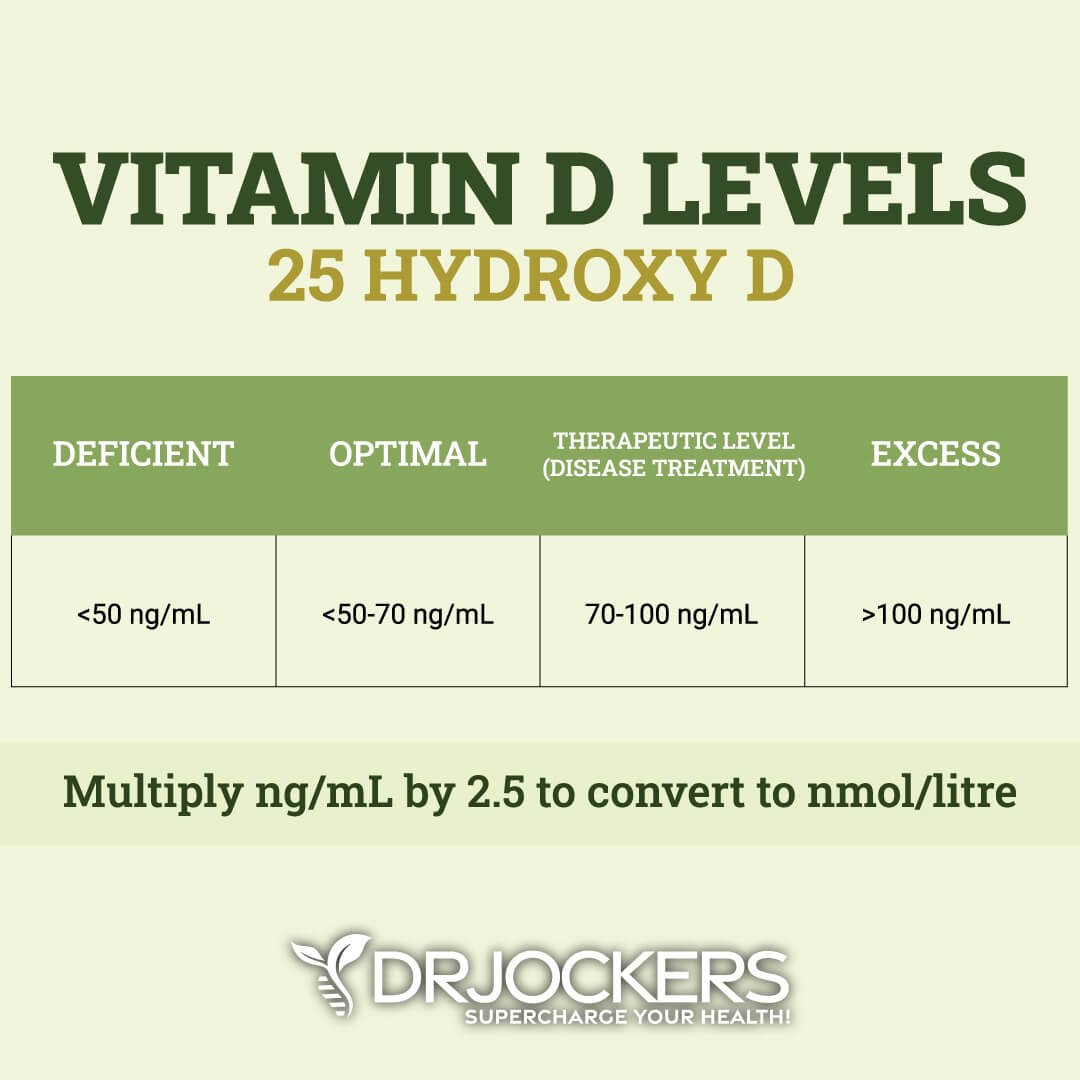
Vitamin D is essential for your muscle, bone, brain, neurological, mental, immune, and gut health. Unfortunately, most of the population is deficient in it, which can lead to serious problems, including an increased risk of seizures.
A 2012 study published in Epilepsy Behavior has found that correcting vitamin D deficiencies may help to control seizures in epilepsy (17). A 2014 follow-up study published in the International Journal of Neuroscience has discussed that vitamin D deficiency may increase the risk of epilepsy and other neurological health issues, such as Alzheimer’s and Parkinson’s disease (18). Vitamin D supplementation may help. A 2019 clinical trial published in Medicine (Baltimore) has found that vitamin D supplementation may help to reduce the risk of vitamin D deficiency and improve the condition of children with epilepsy (19).
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need to supplement to optimize their vitamin D levels. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
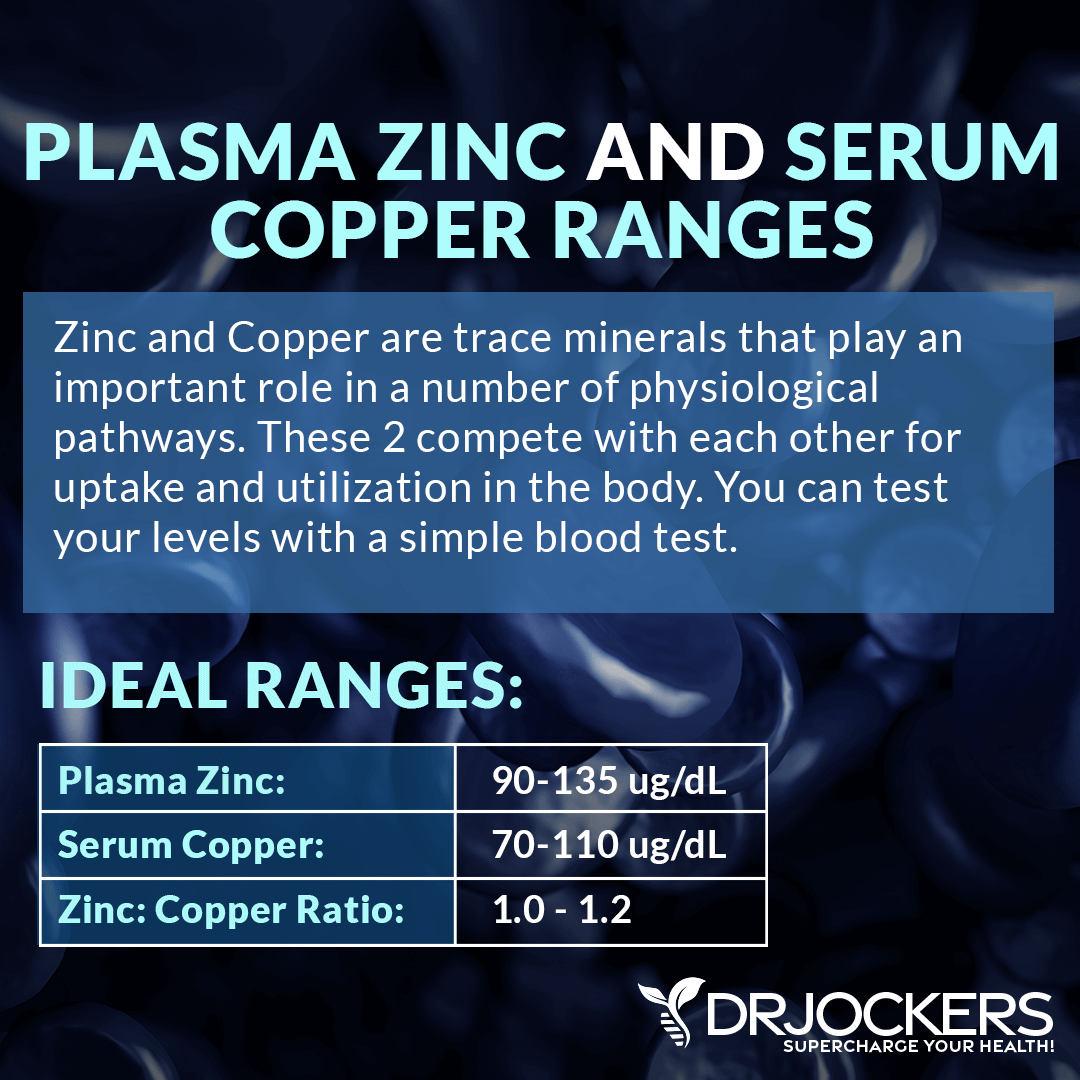
Optimize Zinc/Copper Levels
Zinc is a critical mineral for your immune system and copper is important for your nerve, immune, and bone health. Zinc deficiencies and poor zinc/copper balance may play a role in epilepsy. A 2015 study published in Neurosciences (Riyadh) has found that serum zinc levels tend to be lower in children with epilepsy treated with anti-seizure medication (20).
Rebalancing their zinc and copper levels is critical. A 2019 study published in Pharmacology and Therapeutics has found that poor zinc signaling can increase the risk of seizure in epilepsy while proper levels can have positive effects (21).
Zinc and copper compete against each other as antagonists to regulate physiological pathways. A healthy balance between these two minerals is critical for your health. I recommend checking your plasma zinc and serum copper levels and their balance. This should help you with a dietary and supplement strategy to improve your levels.
Your dietary choices can improve your copper/zinc ratio. Zinc-rich foods include grass-fed lean meat, pasture-raised poultry, nuts, seeds, oysters, peas, and chickpeas. Foods that are good sources of copper include oysters, leafy green, shitake mushrooms, liver, lobsters, nuts, and seeds. Additionally, I recommend that you take a high-quality zinc supplement. If you find that your copper levels are off, you can take a chelated copper supplement or a zinc supplement with copper to support a healthy copper/zinc ratio.
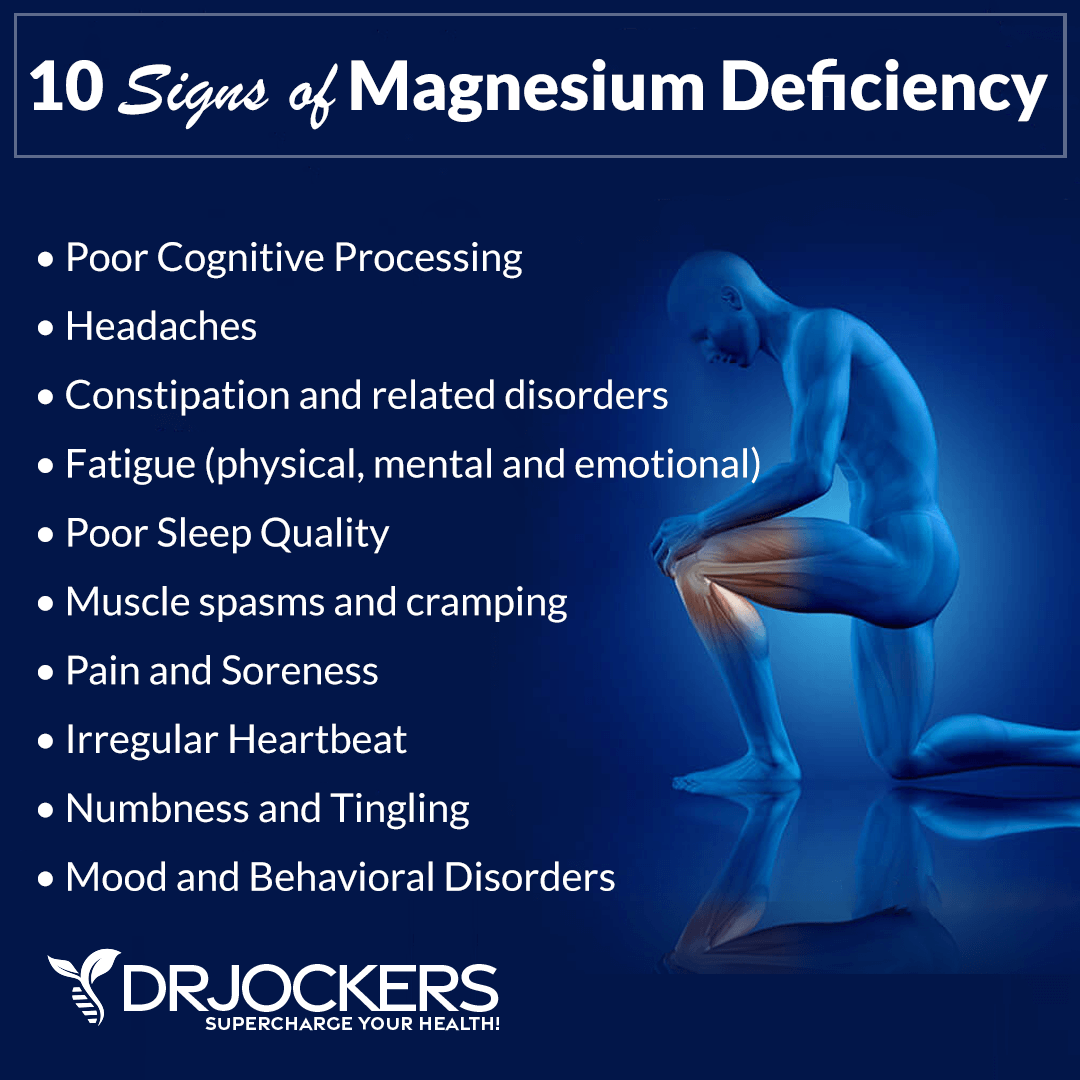
Use Magnesium
Magnesium is an important mineral for many areas of your health, including lowering inflammation, decreasing muscle tension, improving blood sugar levels, supporting healthy blood pressure levels, and more. It may play a role in epilepsy as well.
A 2018 study published in Nutrition has found that a dietary intake of magnesium can decrease the risk of epilepsy in middle-aged and older adults (22). A 2012 review published in Epilepsy Research has found that magnesium is a potential modulator for seizure activity and magnesium may help to reduce epileptic seizures (23). The review recommends that magnesium supplementation is considered a treatment option for epilepsy.
I recommend eating foods rich in magnesium, including greens, nuts, and seeds. However, it is difficult to meet your needs through food alone, so I recommend daily supplementation with a high-quality magnesium supplement.
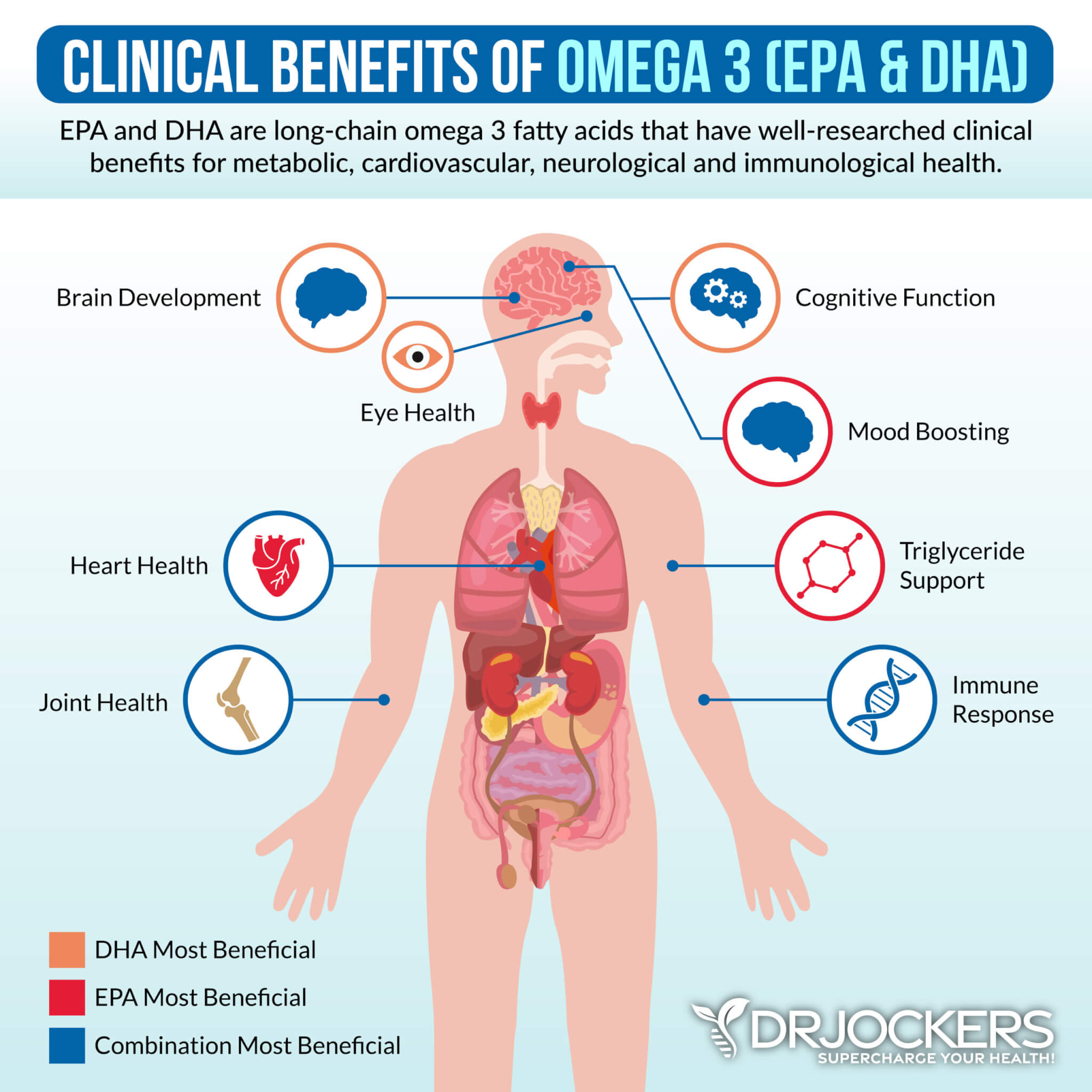
Use Omega-3 Fatty Acids
Omega-3 fatty acids are anti-inflammatory fatty acids that play a role in reducing inflammation, pain, various symptoms, and the risk of disease in your body. They are also important for those with seizures and epilepsy. A 2004 study published in Seizure has found that a deficiency in omega-3 fatty acids may increase the risk of seizures and SUDEP (24).
Omega-3 fatty supplementation may help. A 2005 randomized trial published in Epilepsy Behavior has found that omega-3 fatty acids may benefit those with chronic epilepsy (25). Researchers found that supplementation with omega-3 for only 6 weeks reduced the frequency of seizures in participants. A 2018 randomized, double-blind placebo-controlled trial published in Epilepsy Behavior has also found that omega-3 supplementation, more specifically, using both eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), has helped to improve and reduce the frequency of seizures in drug-resistant epilepsy (26).
I recommend consuming foods rich in omega-3 fatty acids, such as algae, wild-caught fish and seafood, chia seeds, hemp seeds, and flax seeds. Additionally, I recommend taking a high-quality omega-3 fish oil supplement daily.
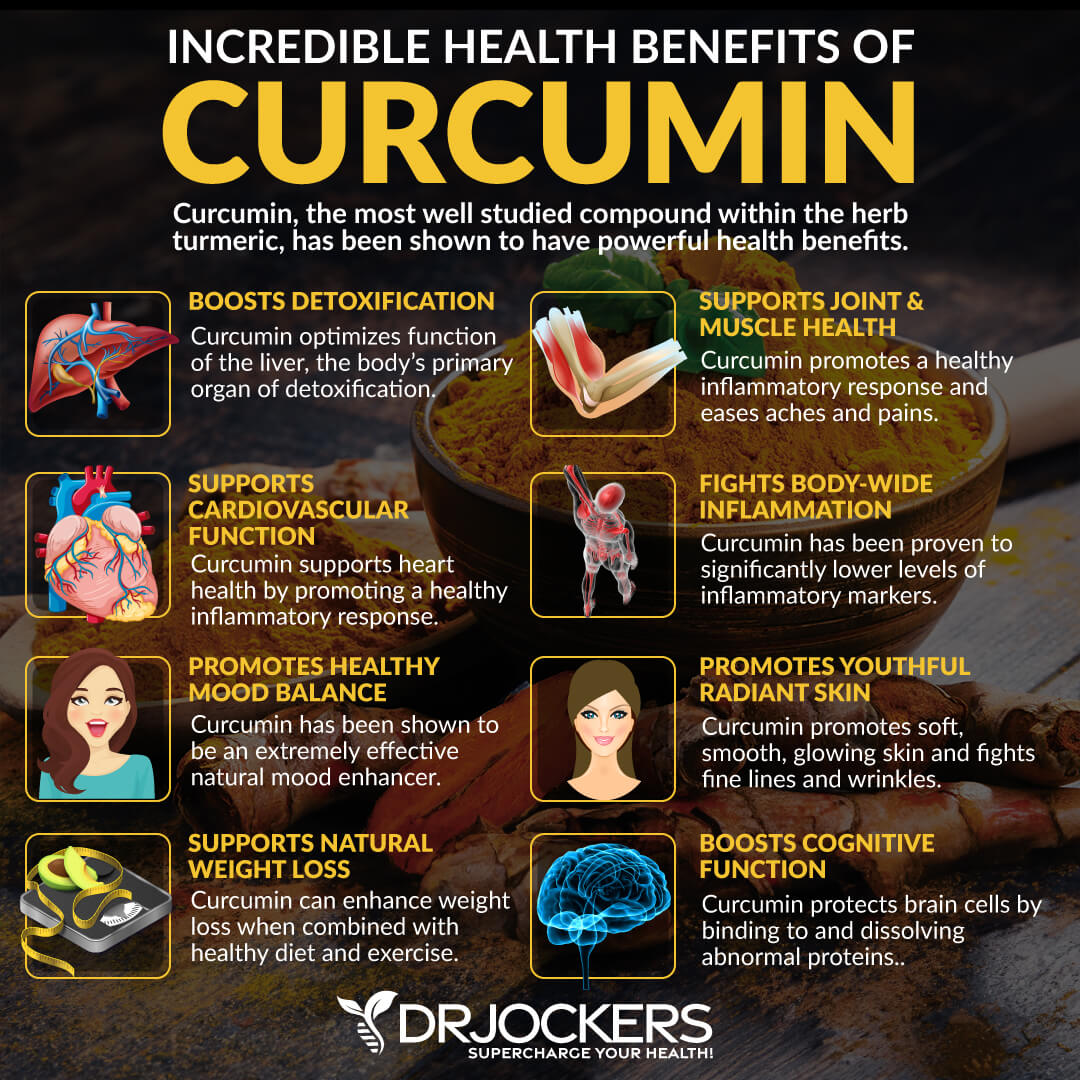
Consider Using Curcumin
Curcumin is the active compound of one of the most research anti-inflammatory herbs, turmeric. Due to its anti-inflammatory and pain-relieving benefits, curcumin may be a great option for seizures and epilepsy.
A 2017 experimental review published in Reviews in Clinical Medicine has found that curcumin supplementation may help to improve epilepsy and could be part of a long-term therapy (27). A 2018 review published in Phytotherapy Research has also found that curcumin may help to reduce spontaneous seizures due to its anti-inflammatory and antioxidant benefits (28). A 2018 study published in Science Reports has also found that curcumin offers anti-seizure benefits and may help to support the treatment of epilepsy (29).
I recommend adding turmeric to your curries, soups, vegetable dishes, dressings, sauces, juices, and smoothies. I also recommend daily supplementation with a high-quality curcumin supplement.
Consider Using B Vitamins
B vitamins are important for brain function, mental health, cell metabolism, immune function, and many other areas of your health. Healthy levels are critical for people with epilepsy. Anticonvulsant medications can reduce vitamin B levels. According to a 2011 study published in Annals in Neurology, anti-epileptic drugs can deplete vitamin B12 and folate levels which can increase the risk of complications (30).
A 2016 study published in Biomedical Reports has found that by interacting with vitamin B12 and folate, anti-epileptic drugs can increase the risk of strokes (31). A 2017 study published in the European Reviews in Medical Pharmacology has found that vitamin B supplementation can help the treatment of epilepsy after a stroke (32).
I recommend that you eat foods that are rich in B vitamins on a regular basis. These foods include grass-fed meat, pasture-raised eggs, grass-fed or fermented raw dairy if you can tolerate it, dark leafy greens, sunflower seeds, almonds, avocados, and citrus.
I also recommend that you supplement with vitamin B12 and a high-quality B complex vitamin daily. Make sure that you are using a methylated form of B vitamin supplement to ensure proper absorption. Choosing a liquid form of vitamin may also help absorption.

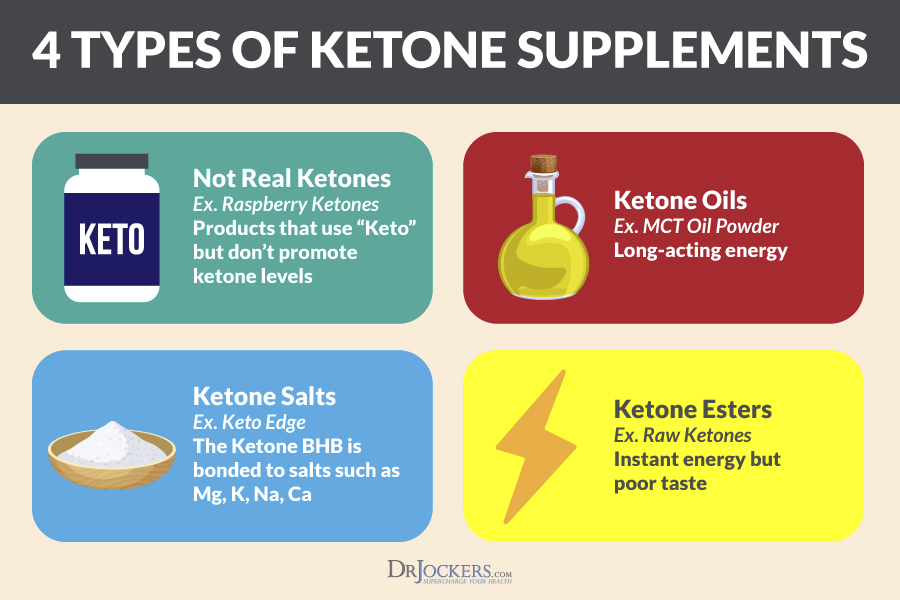
Consider Using Exogenous Ketone and MCT Oil
As you know, following a ketogenic diet and getting into ketosis can help to reduce epileptic seizures and improve epilepsy (8, 11, 12). Exogenous ketones and MCT oil can help with this. Exogenous ketones can help to put your body into ketosis even without a ketogenic diet and can support a ketogenic diet. Medium-chain triglycerides (MCT) oil is a great tool that supports ketosis and a ketogenic diet.
A 2019 study published in Frontiers in Neuroscience has found that using exogenous ketones can help to induce ketosis and improve seizure disorders and epilepsy (33). A 2013 study published in Neuropharmacology has found that MCT oil can support a ketogenic diet and help to control seizures (33). A 2013 study published in Case Reports in Neurological Medicine has also noted seizure reduction after four tablespoons of MCT oil twice a day (34).
I recommend taking pure C8 MCT oil. It is the purest and the most effective form of MCT oil. You can add it to your coffee, tea, or just take it as is. I recommend starting out slow with 1 tablespoon the most at first and see how you feel. Taking too much can cause stomach upset or diarrhea, so it’s all about finding your saturating point and the most effective dose for your body.
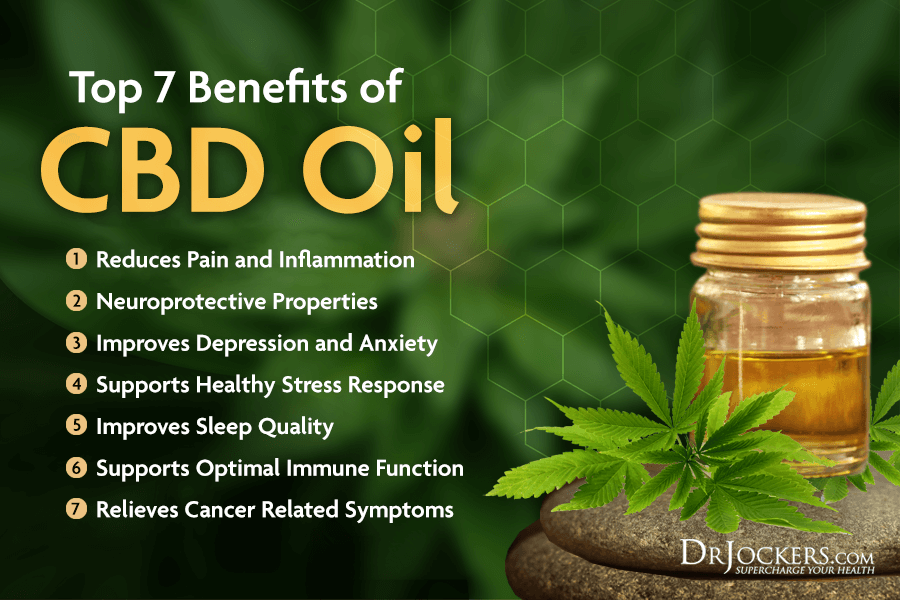
Consider Using CBD Oil
Cannabidiol, or CBD, is just one of the over one hundred cannabinoids, or chemical compounds found in cannabis plants, including marijuana and hemp. Hemp is a strain of the plant Cannabis sativa that can be used to make clothing, paper, textile, and other products.
The two primary and commonly know cannabinoids are CBD and tetrahydrocannabinol (THC). THC is a psychoactive compound that is responsible for the feeling of ‘being high’ when smoking or consuming marijuana. CBD, on the other hand, is not psychoactive. CBD doesn’t make you high and it’s a great option for people who desire pain or symptoms relief but are not looking for mind-altering effects from THC. CBD is safe and natural offering a great alternative for those who are looking to avoid side effects from pharmaceutical drugs.
CBD offers many health benefits, including reduced pain, inflammation, stress, anxiety, depression, and better sleep, brain function, and immune health. It may also benefits those with seizures. A 2015 study published in Neurotherapeutics has found that is a safe, well-tolerated therapeutic agent that may help to reduce seizures in people with epilepsy (36). A 2019 review published in Molecules has found that CBD may offer anti-seizure, neuroprotective, anti-inflammatory, antioxidant, anti-psychotic, and antidepressant benefits and may benefit those with treatment-resistant severe epilepsy (37).
I recommend trying CBD to see if it benefits your condition. There are different forms of CBD oils on the market, including oils, tinctures, capsules, pills, vapors, edibles, lotions, and creams. Oils and tinctures are placed under your tongue and offer more rapid benefits than pills, capsules, or edibles. However, you may prefer capsules or pills for their convenience.
Edibles may also be convenient, however, always read the ingredients. Many edible CBDs, like gummies, are high in sugar or other refined ingredients that I don’t recommend. While vaping offers the most rapid release, I don’t recommend it because vaping may affect your lung tissue. Lotions and creams usually offer a lower dose of CBD, however, they are a great idea if you have muscle tension and pain.
Finding what dose works for you takes time. It depends on the individual. Read the directions on the box and start with a lower dose at first. Increase it gradually until you find what works for you best.
Final Thoughts
Epilepsy is a chronic seizure disorder that’s characterized by recurrent, reflexive, or unprovoked seizures. Even though it’s a chronic disease, it is possible to manage the conditions, reduce or even eliminate seizures. Some people can completely recover from epilepsy.
Natural support strategies, including nutrition, lifestyle strategies, and supplementation may benefit your condition and reduce your risks and triggers. I recommend that you follow my natural support strategies for epilepsy to improve your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. We do offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



VERY INFORMATIVE, APPLICATIONAL