Vitiligo: Symptoms, Causes, and Support Strategies
Vitiligo: Symptoms, Causes, and Support Strategies
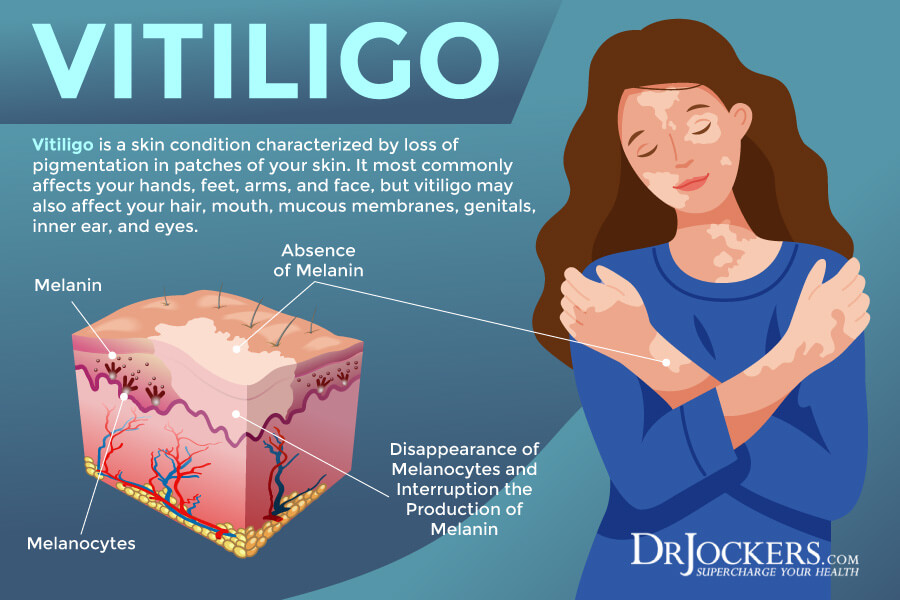
Vitiligo is a skin condition characterized by loss of pigmentation in patches of your skin. It most commonly affects your hands, feet, arms, and face, but vitiligo may also affect your hair, mouth, mucous membranes, genitals, inner ear, and eyes. While vitiligo may affect anyone of any age, sex, or ethnicity, certain factors may increase your risk. While conventional strategies for vitiligo tend to use creams, medication, surgery, and coverage, there are some natural support strategies for vitiligo that can improve your health and well-being.
In this article, you will learn what vitiligo is. You will understand the major symptoms of vitiligo. I will go over the main risk factors for vitiligo. I will explain the pathogenesis of vitiligo. You will understand the diagnosis and conventional treatment options for vitiligo. I will detail the major root causes of vitiligo. I will also offer my top natural support strategies for vitiligo.
What Is Vitiligo
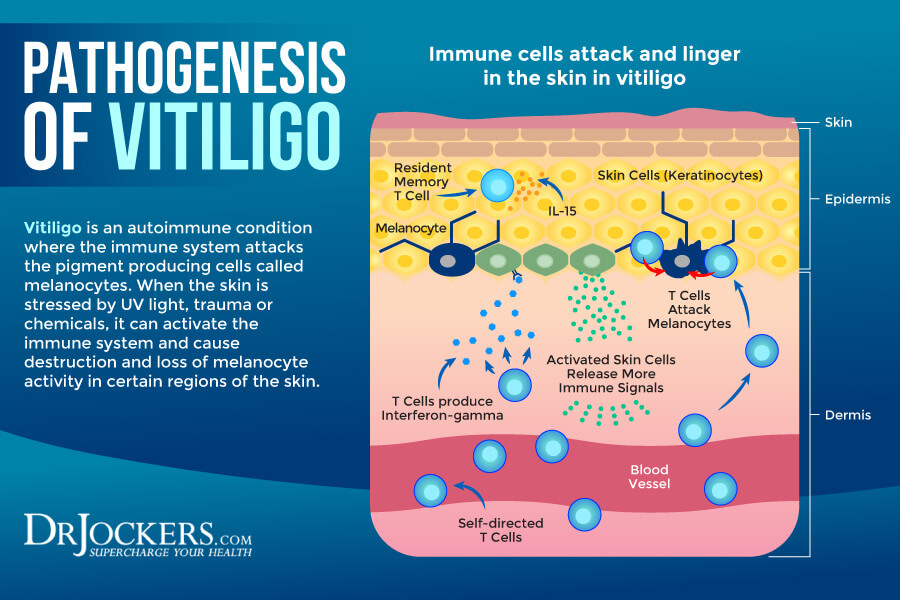
According to the American Osteopathic College of Dermatology, about 1 percent of the world’s population has vitiligo (1). Vitiligo is an autoimmune skin condition characterized by patches of skin that lose their pigmentation due to melanocyte loss. The melanocytes are pigment-producing cells that get attacked and destroyed, causing them not to be able to produce melanin or skin pigment. As a result, the skin will lose color and become white instead.
Vitiligo may affect the skin, eyes, inner ear, mucous membranes, and hair. Most common affected areas include your hands, feet, arms, face, genitals, nostrils, mouth, mucous membranes, ear, and back of the eye. It may also affect your hair and cause white or grey hair.
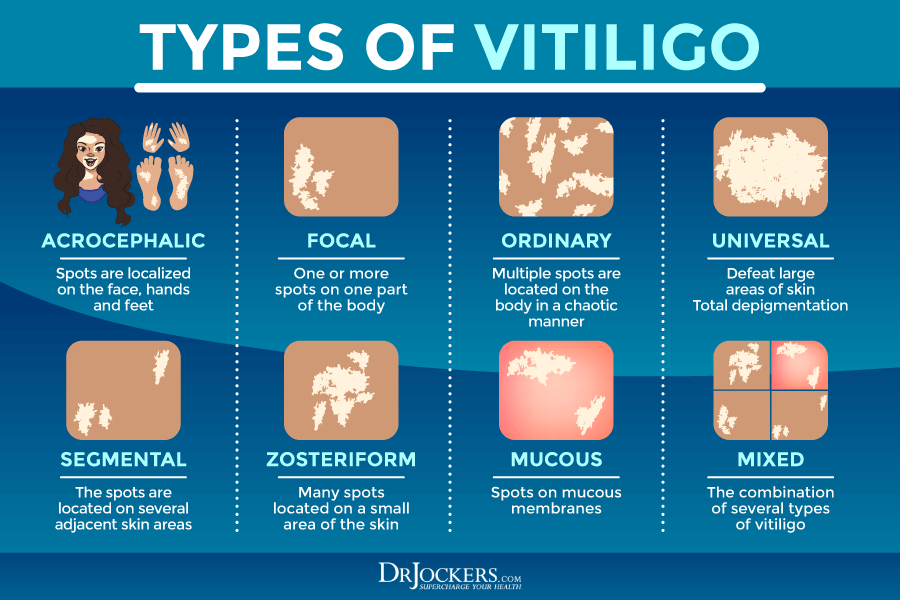
Vitiligo may affect all ages, both sexes, and any ethnicities. The most common type is Vitiligo Vulgaris or common vitiligo. However, other types include linear, trichome, segmental, and inflammatory vitiligo. Vitiligo is not contagious and is generally considered to be an autoimmune condition.
Major Symptoms of Vitiligo
Major symptoms of vitiligo may include (2):
- Patches of the skin losing color or turning white, usually on the hands, feet, arms, or face
- Patches of hair, including hair on the head, eyelashes, eyebrows, and beard turning grey or white early
- Loss of color the inside of your mouth or nose
- Change of color of the retina of the eyes
- Inflammation of the ears or eyes and related hearing or vision problems
Risk Factors of Vitiligo
Vitiligo may affect anyone, including all ethnicities, sexes, and ages. In most people, vitiligo shows up before the age 20.
The causes of vitiligo are unclear but a few factors may increase your risk, including (3):
- Family members with vitiligo
- Having family members with or personally dealing with certain autoimmune disorders, including type 1 diabetes, thyroid issues, scleroderma, alopecia areata, psoriasis, Addison’s disease, and rheumatoid arthritis.
- Being under 20
- Environmental triggers, including sunburn or skin injuries
- Genetic factors with over 50 genes linked to a risk for vitiligo
- High level of stress

Pathogenesis of Vitiligo
Vitiligo tends to start out with only one or a few small white patches of skin. Over time this gradually will spread over the body. This can take several months or longer. In most cases, vitiligo affects the hands, feet, forearms, arms, and face. These are the areas where the first patches usually appear. They may eventually spread to the nose, moist inner lining of your mouth, genitals, rectal area, inner ears, and eyes.
Larger patches usually stay where they are for years. However, they may widen and spread over time. Smaller molecules tend to shift, change, and spread over time. Symptoms may vary from patient to patient. Some experience fewer and smaller depigmented areas, while others may notice a more widespread loss of skin pigmentation. The spread and severity of vitiligo may determine your treatment options and their success.
Diagnosis and Conventional Treatment Options
During your first doctor’s visit, your medical professional will go over your medical and health history, family history, and symptoms. They will perform a physical exam and may order some labs.
They may use an ultraviolet lamp called the Wood’s lamp to detect patches of vertigo and make sure it’s not mistaken with some other skin condition. They may send a sample of skin for biopsy. They may order some blood tests to look for anemia, diabetes, thyroid issues, and other problems that may be related to vitiligo.
Conventional treatment protocols may very much depend on the type of vitiligo, its severity, the location and size of the patches, the number of patches and how widespread they are, and how they respond to various treatment options. Conventional treatment options may include (1):
- Prescription topical creams, including corticosteroids, may help to return the color of the skin and allow small growth.
- Oral medications, including steroids and antibiotics to reduce vitiligo
- Psoralen and ultraviolet A (PUVA) therapy is a combination of a psoralen pill or cream and UVA light to restore your skin color.
- Narrow UVB light as an alternative to PUVA therapy with less side effects and as a home treatment option.
- Excimer laser treatment to improve small patches over a four-month period used 2 to 3 times a week.
- Depigmentation for people with widespread vitiligo affects 50 percent of their skin to fade the remaining areas to match the affected skin.
- Skin grafting is a surgical option for those who have had no new or worsening patches for at least 12 months, which removes and transfers pigmented skin to depigmented areas.
- Melanocyte transplants, another surgical option for those who have had no new or worsening patches for at least 12 months which removes melanocytes, grow them in a lab, then transplant them to depigmented areas.
- Micropigmentation, another surgical option for those who have had no new or worsening patches for at least 12 months, tattooing pigment into the skin.
- Sunscreen to reduce sun exposure and to keep the skin even and reduce damage.
- Cosmetics, including self-tanning lotions and make-up, to cover affected areas.
- Therapy, counseling, or psychiatric medication to reduce negative mental health effects and improve your quality of life.
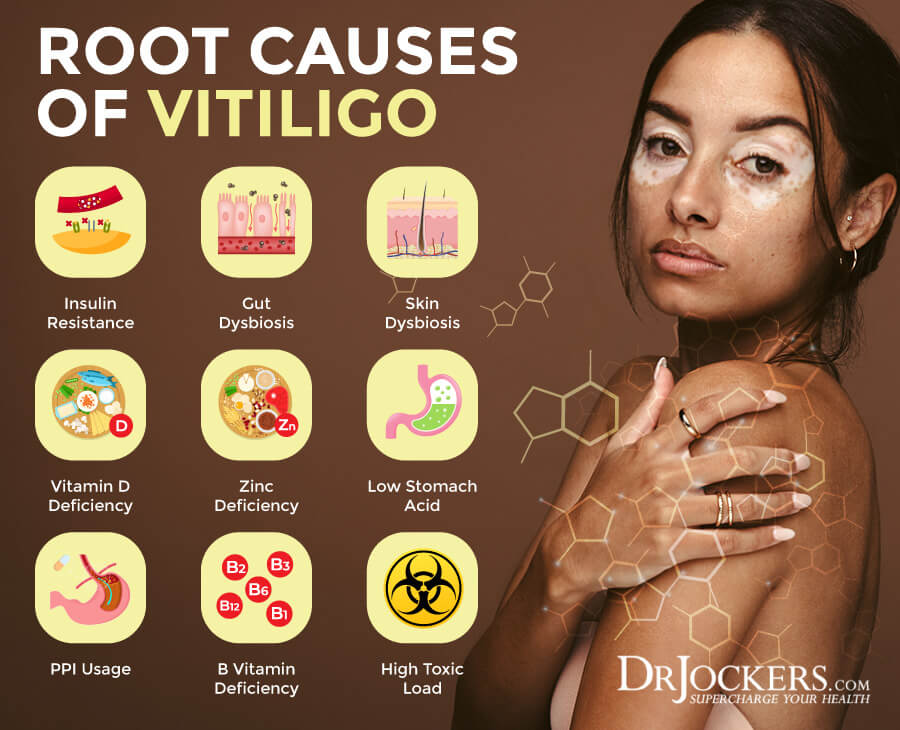
Root Causes of Vitiligo
Understanding the risk factors for vitiligo is not enough. There are certain root cause factors that may or may not directly cause vitiligo but can compromise your health, increase your risk, and contribute to or worsen the condition. Here is what you need to know:
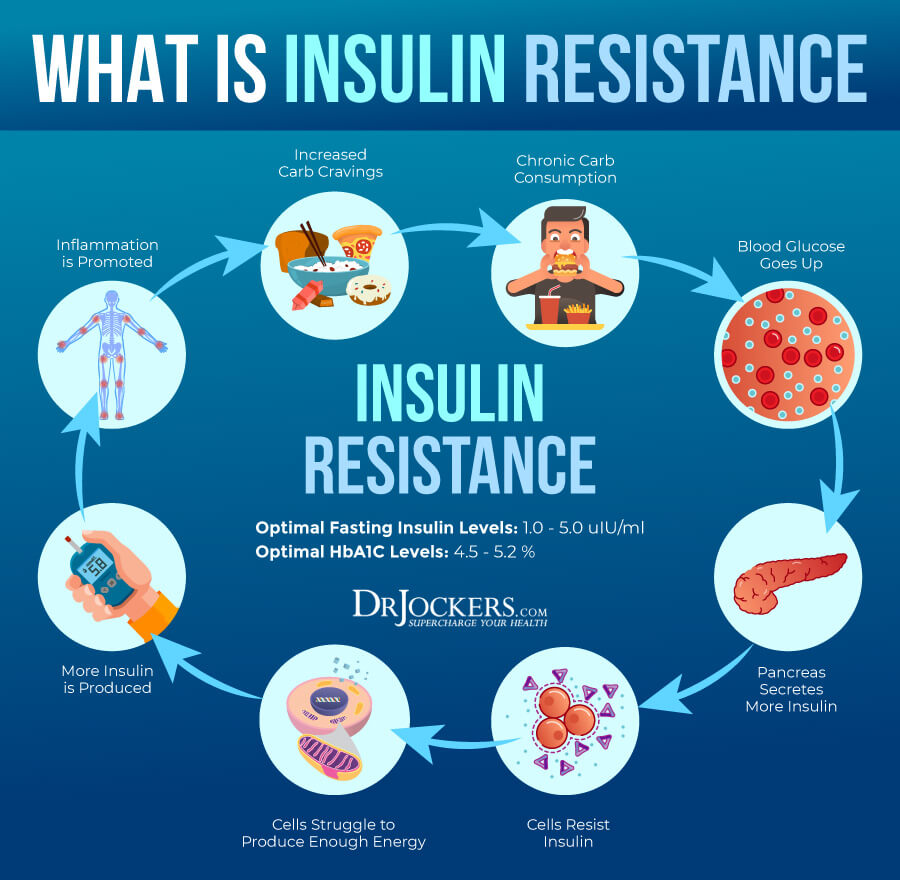
Insulin Resistance
Insulin resistance is a condition in which your body is unable to respond to insulin well and can’t use glucose for energy as it should. As a result, your pancreas will end up making more insulin to keep up, which over time will lead to increased blood glucose levels as well. Insulin resistance can lead to blood sugar fluctuations, prediabetes, and type 2 diabetes. It may also increase the risk of various other health issues, including vitiligo and other health issues.
A 2015 study published in the Scientific World Journal has found a link between insulin resistance and various skin conditions, including psoriasis, acne, and vitiligo (5). A 2017case-control study published in the Balkan Medical Journal has also found a higher incidence of metabolic syndrome in patients with vitiligo (4).
A 2011 study published in Acta Dermatology and Venereology has looked at the fasting blood samples, insulin, C-peptide, glucose, total cholesterol, triglyceride, low-density lipoprotein-cholesterol (LDL-C), and high-density lipoprotein-cholesterol (HDL-C) of 96 patients, 57 with vitiligo and 39 control group and found a link between insulin resistance and vitiligo (6). Patients with vitiligo were more likely to be insulin resistant, had higher insulin levels,c-peptide levels, LDL/HDL ratio, and lower HDL-C levels.

Gut Dysbiosis
Your gut is the home of 100 trillion bacteria. Some of these bacteria are harmful; others are beneficial. These bacteria need to live in balance to create health and homeostasis in your body.
If your microbiome becomes out of balance and you have too many bad or harmful gut bacteria and too few goods or beneficial bacteria, you develop gut dysbiosis. Gut dysbiosis can affect your entire body, including your skin. Gut dysbiosis may contribute to the development of vitiligo.
A 2020 animal study published in The Journal of Investigative Dermatology has found that gut dysbiosis but not skin dysbiosis may be linked to the development of vitiligo (7). A 2020 study published in Frontiers in Microbiology has looked at 30 patients with vitiligo and 30 without vitiligo found that gut dysbiosis was more common in those with vitiligo and may be linked to vitiligo (8). The two bacteria that seemed to be the most problematic were Corynebacterium 1 and Psychrobacter.
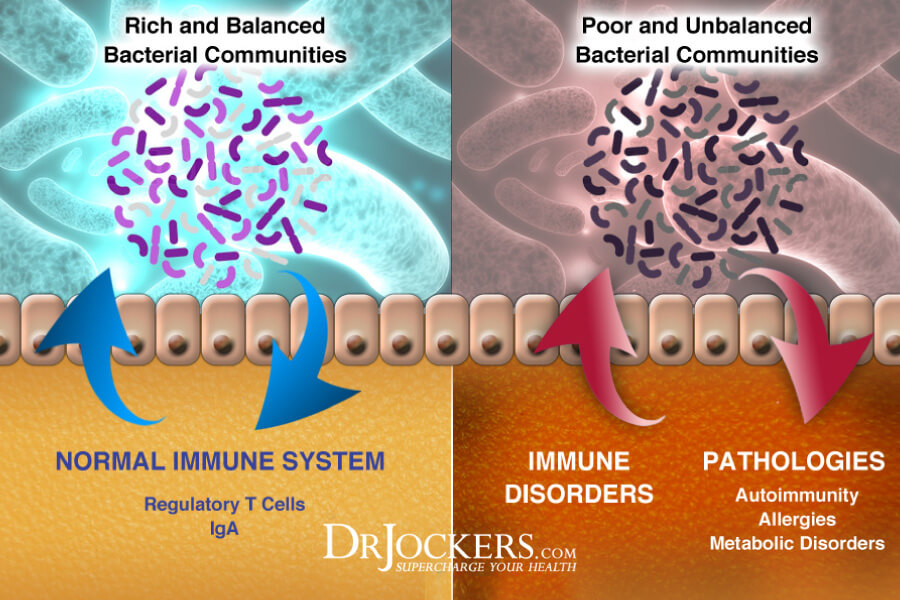
Skin Dysbiosis
Just like your gut, your skin also has its own microbiome with 1.5 trillion bacteria, including beneficial and harmful ones. Just like in your gut, there needs to be balanced. If there is an imbalance and you develop skin dysbiosis, it may increase your risk of various skin problems, including vitiligo.
A 2016 review published in Science Reports has found that skin dysbiosis may play a role in vitiligo (9). They also found that the skin microbial profiles of lesion and non-lesion vitiligo patients were different. However, both are dominated by four phyla, at about 85 percent, including Actinobacteria, Proteobacteria, Firmicutes, and Bacteroidetes. The phylum Actinobacteria was more than 45 percent abundant in both groups. Other major bacteria found include Corynebacterium, Staphylococcus, Propionibacterium, Micrococcus, Kocuria, Acinetobacter, Streptococcus, and Paracoccus.
A 2021 study published in the Journal of Investigative Dermatology has found that both skin and gut dysbiosis can contribute to immune and mitochondrial changes in patients with vitiligo (10). Researchers have found that vitiligo patients had depleted levels of α- and β-diversity between samples with decreased richness and distribution of species.
They also had depletion of two beneficial bacteria, including, Bifidobacterium and Bacteroides but had too many harmful bacteria, such as Proteobacteria and Streptococcus, and too much Mycoplasma, and mtDNA increasing stress markers and contributing to poor immune markers.

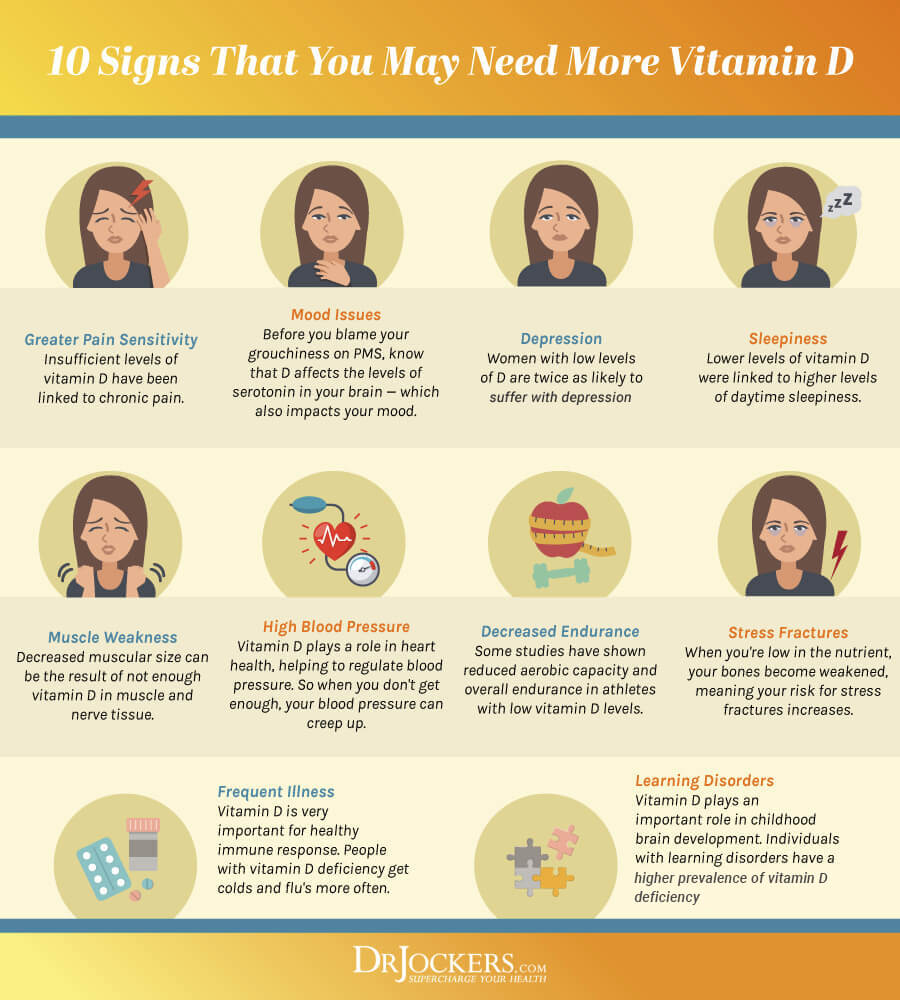
Vitamin D Deficiency
Vitamin and mineral deficiencies can pose a serious health risk. Vitamin D is a critical vitamin for your immune, bone, muscle, brain, and overall health. Research has shown that vitamin D deficiency may also play a role in vitiligo. A 2013 review published in the Indian Journal of Dermatology, Venereology, and Leprology has found that vitamin D deficiency is common and may play a role in vitiligo (11).
A 2013 clinical trial published in Photodermatology, Photoimmunology, and Photomedicine has found that out of 40 vitiligo patients, 39 were deficient in vitamin D, versus only 5 out of 20 patients without vitiligo and autoimmunity had vitamin D deficiency (12). This shows that while vitamin D deficiency may be common in the general population, it is much more common in those with vitiligo and autoimmunity.
A 2013 case-control published in the Indian Journal of Dermatology has found similar results (13). About 40 percent of patients with vitiligo had insufficient levels of vitamin D, and 26.7 percent were deficient. 96.7 percent of the control participants without vitiligo have normal vitamin D levels.
A 2016 meta-analysis published in Photodermatology, Photoimmunology, and Photomedicine has found similar results regarding the incidence of vitamin D deficiency in vitiligo (14). Researchers looked at 383 articles identifying 17 qualifying studies and 7 studies for random-effects with data of 1200 patients. They found a significant relationship between vitamin D deficiency and vitiligo. However, vitamin D deficiency causes vitiligo needs more research evidence.
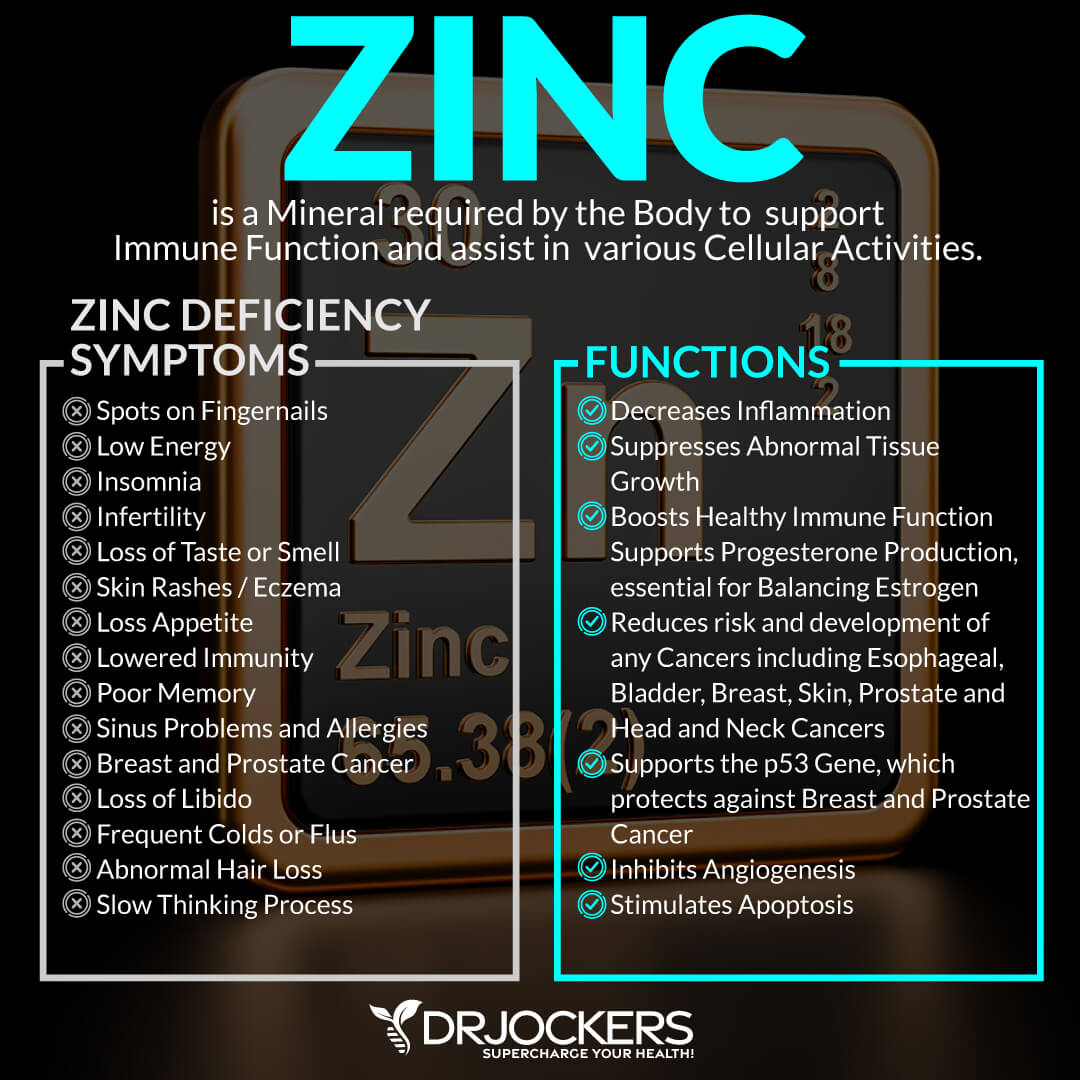
Zinc Deficiency
Zinc is a very important mineral for your immune health, yet, deficiencies are common. Research suggests that zinc deficiency may be linked to vitiligo. A 2017 study published in Advances in Dermatology and Allergology has found a significant link between vitiligo and zinc levels (15). Patients with vitiligo are more likely to have low zinc levels.
A 2018 case-control study published in the Indian Journal of Dermatology has also found that zinc deficiency is common in people with vitiligo (16). They found that low zinc levels were correlated with the duration of the disease. A 2020 study published in the Journal of Clinical and Aesthetic Dermatology has found that low zinc levels may be linked to inflammation in vitiligo (17). Researchers recommended that zinc supplementation may be beneficial for those with vertigo.
Low Stomach Acid & PPI Usage
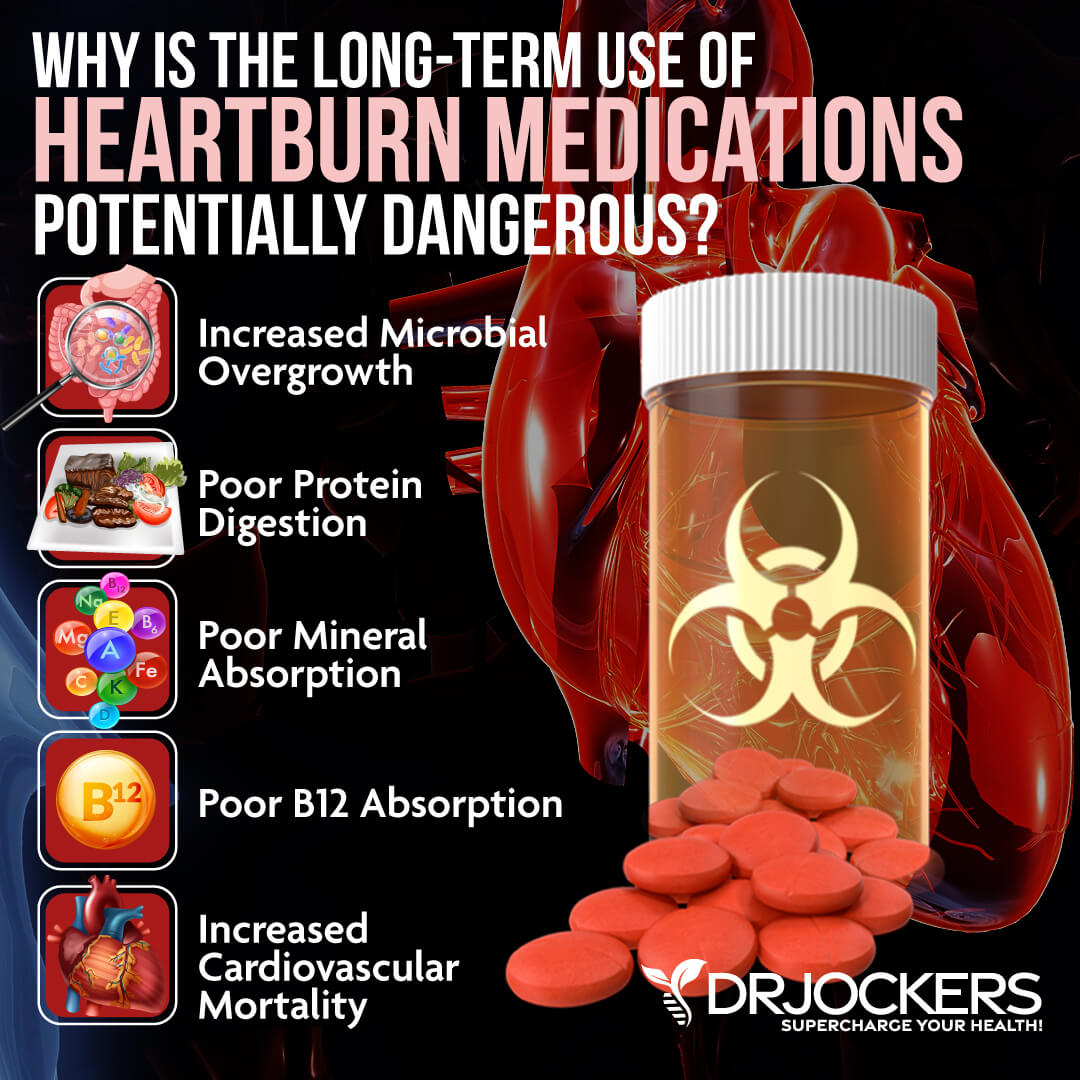
A 1986 study published in Digestions has found a link between autoimmune gastritis and vitiligo (18). A 2017 study published in the Journal of Case Reports has also found a link between autoimmune gastritis, pernicious anemia, and vitiligo (19).
Unfortunately, proton inhibitors (PPIs) are commonly used for gastritis and other gastrointestinal issues. The problem is that these problems are actually caused by low stomach acid instead of too much and PPIs end up causing problems instead of improvements.
Not surprisingly, a 2013 study published in the Journal of the European Academy of Dermatology and Venereology has found that in some cases PPIs may be the possible cause of vitiligo (20).
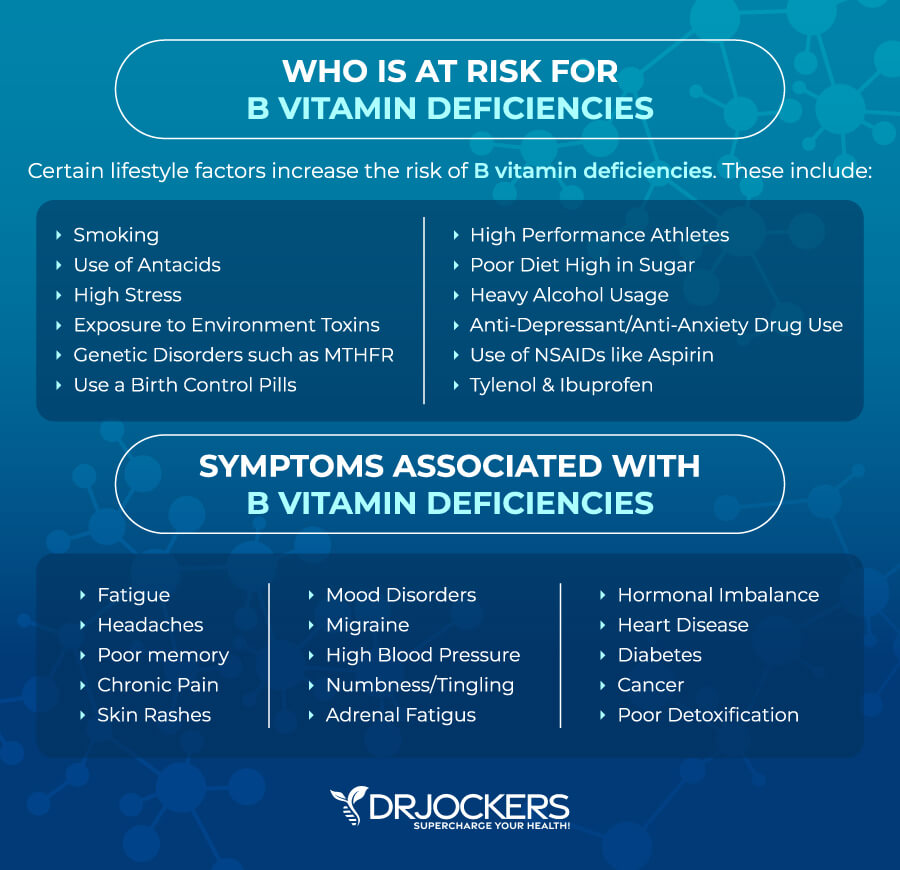
B Vitamin Deficiency
B vitamins are a group of very important vitamins. They are needed for your brain, mental health, nerve function, energy levels, cellular health, and, yes, skin health. Deficiencies in B vitamins, in vitamin B12 and folate, in particular, may increase your risk or worsen your vitiligo.
A 2012 study published in Clinical Experiments in Dermatology has found that deficiencies in vitamin B12 and folic acid levels may be linked to vitiligo (21). A 2018 systematic review and meta-analysis published in the Journal of the American Academy of Dermatology has found that low vitamin B12 and folate, and higher serum homocysteine levels are common in those with vitiligo (22).
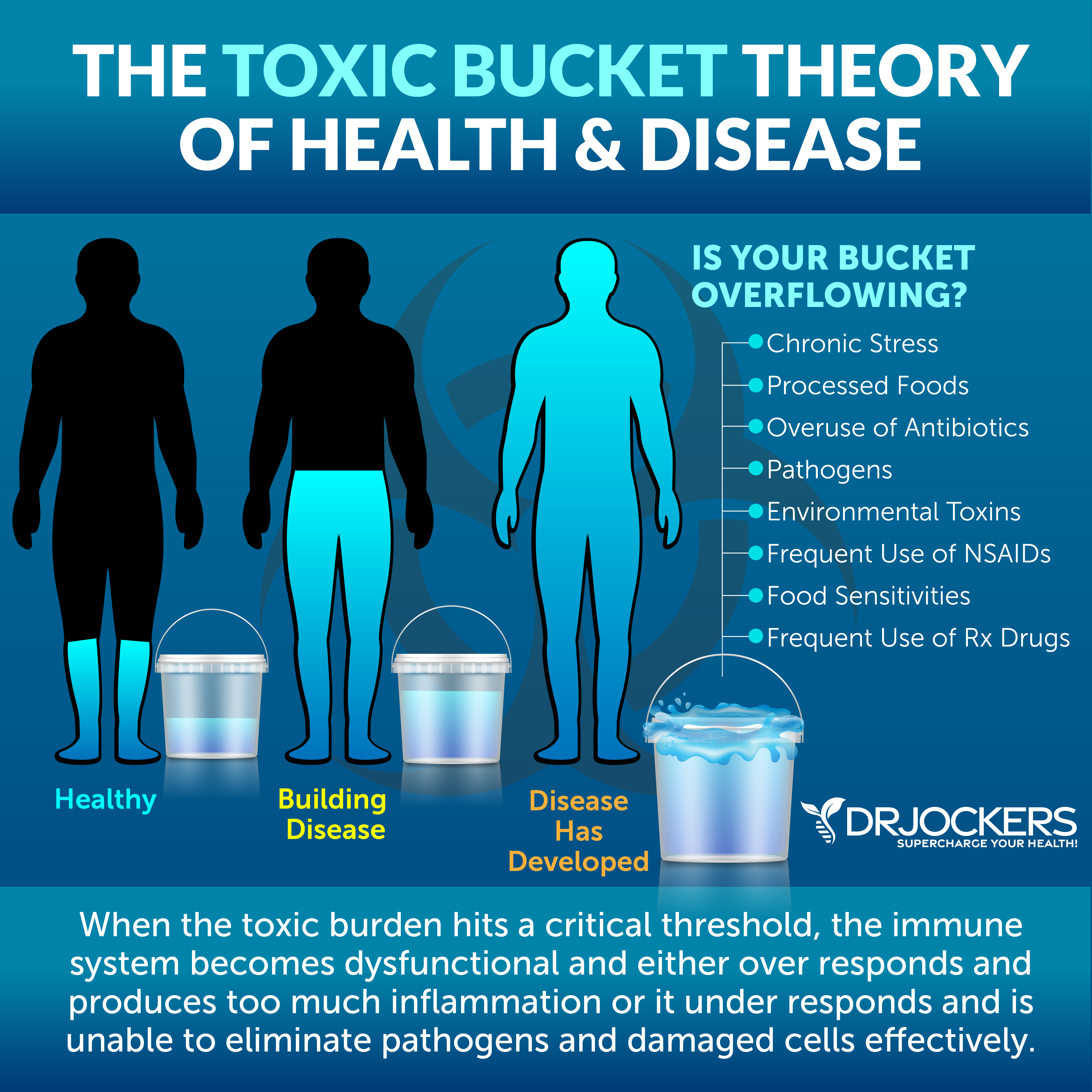
High Toxic Load
Unfortunately, toxins are all around us. There is air pollution, pesticides in non-organic food, chemicals and toxins in our conventional cleaning, hygiene, body, and beauty products, toxins in our tap water, toxins in our plastics, and so on. While it’s impossible to completely avoid them, you have to lower your toxin load as much as possible. A high toxin load, especially mercury, lead, and cadmium, may increase your risk and worsen vitiligo.
A 2011 study published in the Journal of Cutaneous Medicine and Surgery has found higher mercury levels may contribute to vitiligo (23). A 2021 study published in The Science of the Total Environment has found that higher mercury, lead, and cadmium levels in the blood of patients with vitiligo and psoriasis (24). They also found that there may be a link between these higher levels and the diet of these patients.
Key Functional Labs
There are a number of key functional labs I like to look at when testing for issues with skin inflammation, autoimmunity and underlying root causes. Here is what I recommend:
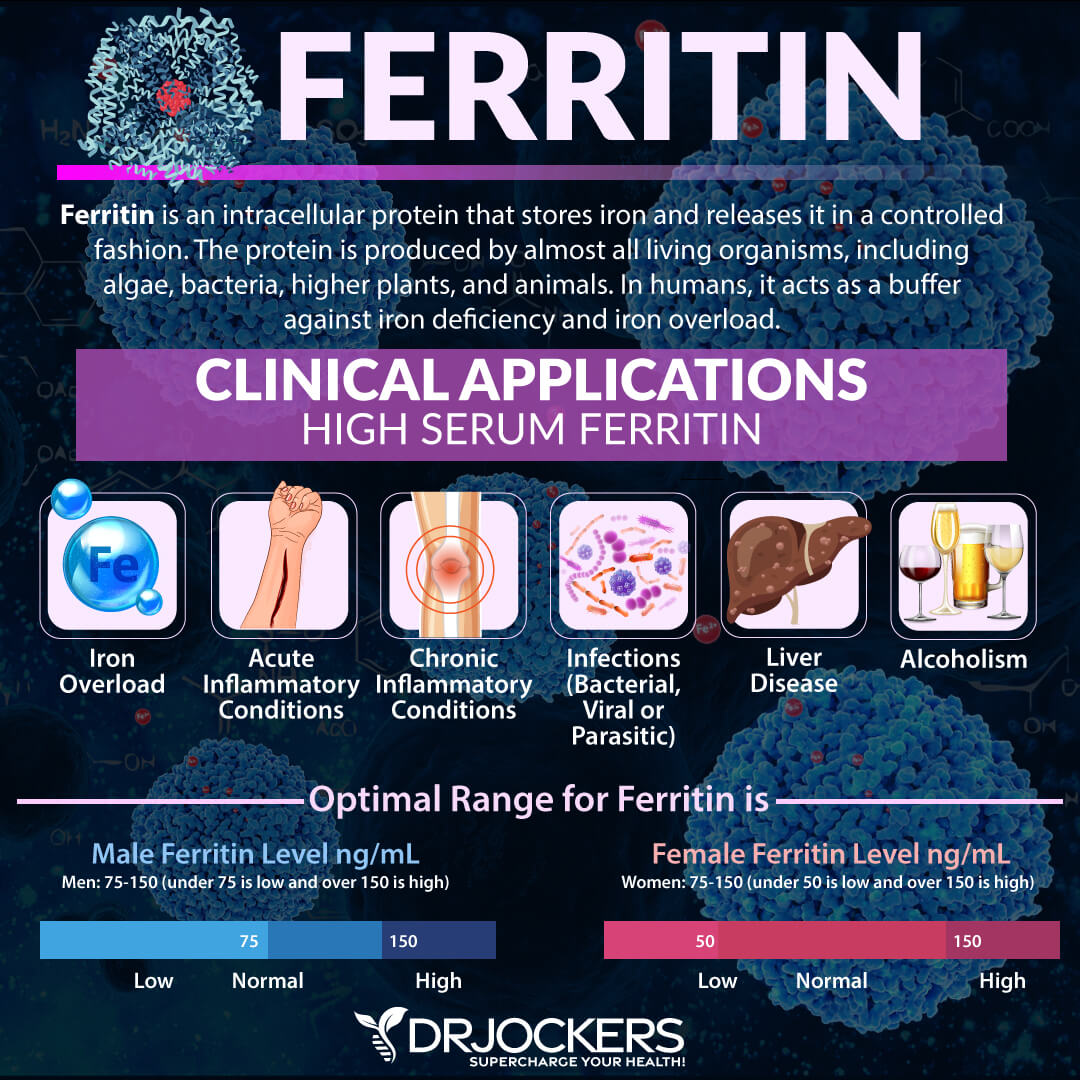
Inflammation: Hs-CRP, ESR, LDH & Serum Ferritin
For inflammation, I recommend a C-Reactive Protein or CRP test, erythrocyte sedimentation rate (ESR) test, Lactate Dehydrogenase (LDH) test, and serum ferritin levels.
The Hs-CRP test measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L. When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
ESR refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Optimal ESR rates are between 0 and 10 mm/hr.
LDH is an enzyme found in all living cells. Elevated levels may indicate inflammation. Optimal levels are between 140-180. Levels over 180 indicate inflammation and levels under 140 indicate reactive hypoglycemia.
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer. The clinical range is 30 to 400, and the optimal range is 50 to 150 for females and 75 to 150 for males. You can learn more about the best lab markers for inflammation in this article here.
Insulin Resistance: Fasting Insulin, HbA1C, Lipid Profile
For insulin resistance, I recommend looking at your fasting insulin, hemoglobin A1C (HbA1C) levels, and lipid profile.
Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml, and the optimal range is 1.0 – 6.0 uIU/ml. Anything above 6 indicates insulin resistance and especially if it is above 10.
Your HbA1C levels measure your average blood sugar over the past 2 to 3 months. Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months, making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6, while the optimal range is 4.5 – 5.2.
Your lipid paneer may be another indication of inflammation and related issues, such as clogged arteries and cardiovascular issues, as well as insulin resistance. We are looking for low HDL or high triglycerides as a sign of insulin resistance. Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal.
Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal. We are also looking at a triglyceride: HDL ratio of 2:1 or less, 1:1 being optimal. Higher rates may indicate insulin resistance and inflammation. Optimal levels:
- HDL cholesterol: The idea range is 55 to 80. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The ideal range is 40 to 80.
Vitamin A, Vitamin D, Plasma Zinc: Serum Copper Ratio
Vitamin A is essential for your immune system, eye health, bone health, and skin health. Normal serum vitamin A levels are between 35–60 ug/dL.
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. Normal levels of vitamin D are between 50-100 ng/mL.
Checking your plasma zinc levels is the best way to determine zinc levels in your body. Ideal plasma zinc levels are between 90–135 ug/dL and for serum copper it should be 70–110 ug/dL. Zinc and copper compete against each other as antagonists to regulate physiological pathways.
A proper balance between the two is essential for maintaining good health. I recommend checking your plasma zinc and serum copper levels and their balance. The proper zinc:copper ratio should be between 1–1.2.
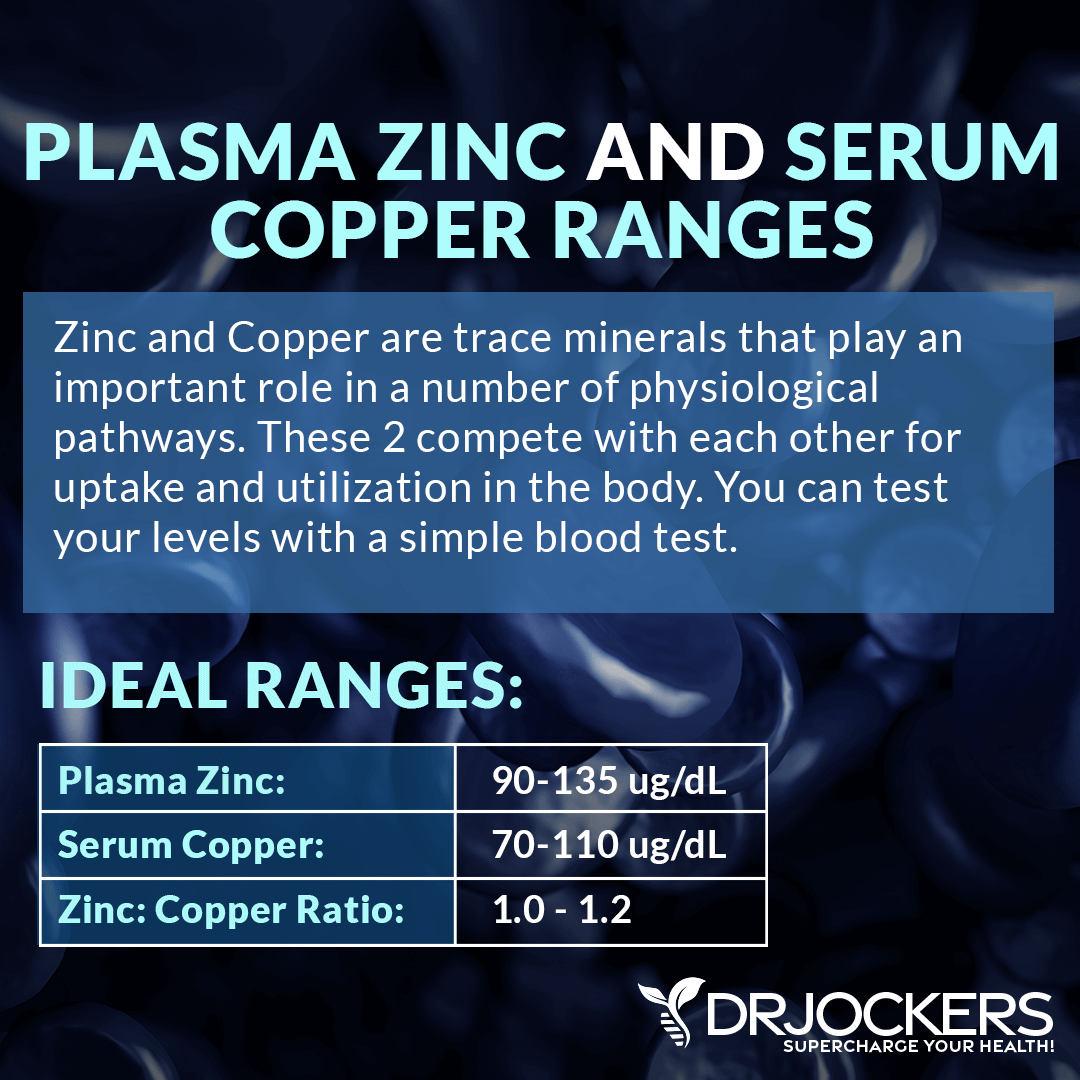
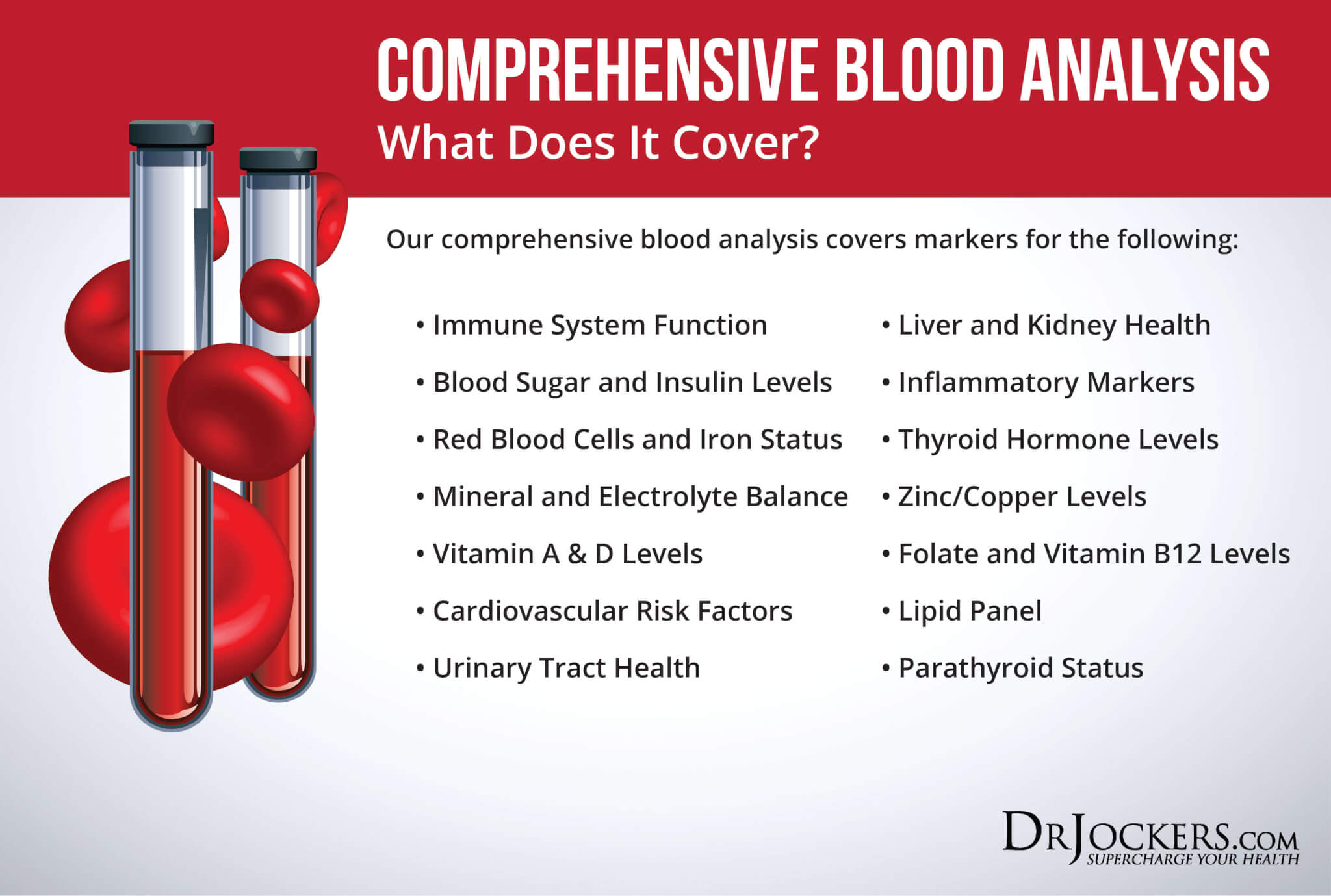
To test all these, I recommend the Comprehensive Blood Analysis (CBA). This is the most detailed blood test that looks at all of these markers of inflammation. This test is more sophisticated than most conventional doctors are able to order.
It examines all parameters for inflammation, blood sugar levels, thyroid function, zinc and copper ratio, vitamin A and D levels, a complete metabolic panel, complete blood count, liver function, nutrient deficiencies, and more. I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your inflammation levels and progress.
Natural Strategies to Support Vitiligo
As you can see, conventional treatment options for vitiligo include creams, medications, surgeries, and covering the affected area. Fortunately, there are some natural strategies to support vitiligo as well. Here is what I recommend:
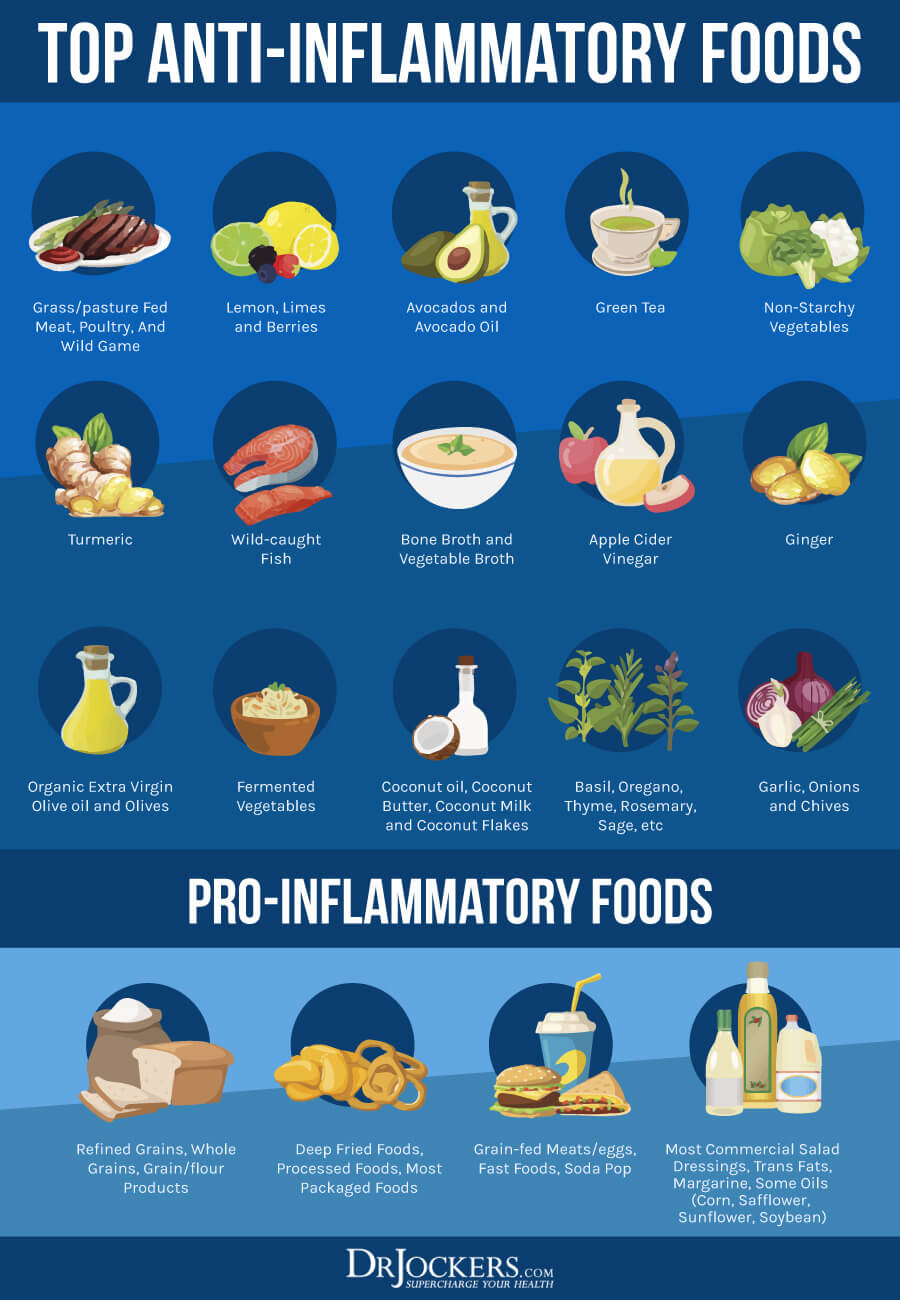
Anti-Inflammatory Nutrition Plan
A 2016 review published in Immunology Reviews has found that innate inflammation and cellular stress both play a role in the development of vitiligo, an autoimmune skin condition (24). Following an anti-inflammatory nutrition plan is one of the best ways to reduce chronic inflammation and related health issues.
A 2017 review published in Dermatology Clinics has found that diet may play a role in the outcome of vitiligo (25). Researchers found that gluten may trigger vitiligo. They also found that a nutritious diet along with vitamins, minerals, and botanicals may help.
I recommend removing all inflammatory foods, including refined sugar, refined oil, gluten, conventional dairy, processed and canned meat, additives, artificial ingredients, non-organic produce with pesticides or hormones, junk food, and highly processed foods. Since cancer feeds on sugar, eating a low carbohydrate diet is critical. If you are looking for sweetness, choose low-glycemic index, high-antioxidant berries instead of high-glycemic index foods.
Follow an anti-inflammatory nutrition plan with plenty of greens, vegetables, herbs, spices, fermented foods, grass-fed meat and butter, pasture-raised poultry and eggs, organ meats, wild-caught fish, and wild game. Eat plenty of healthy fats, including omega-3-rich fish and seafood, nuts and seeds, avocados, grass-fed butter and ghee, olives, and coconut oil. Use anti-inflammatory and antioxidant-rich herbs and spices n your cooking, including turmeric, ginger, cinnamon, basil, rosemary, dill, cloves, cayenne pepper, black pepper, onion, and garlic.
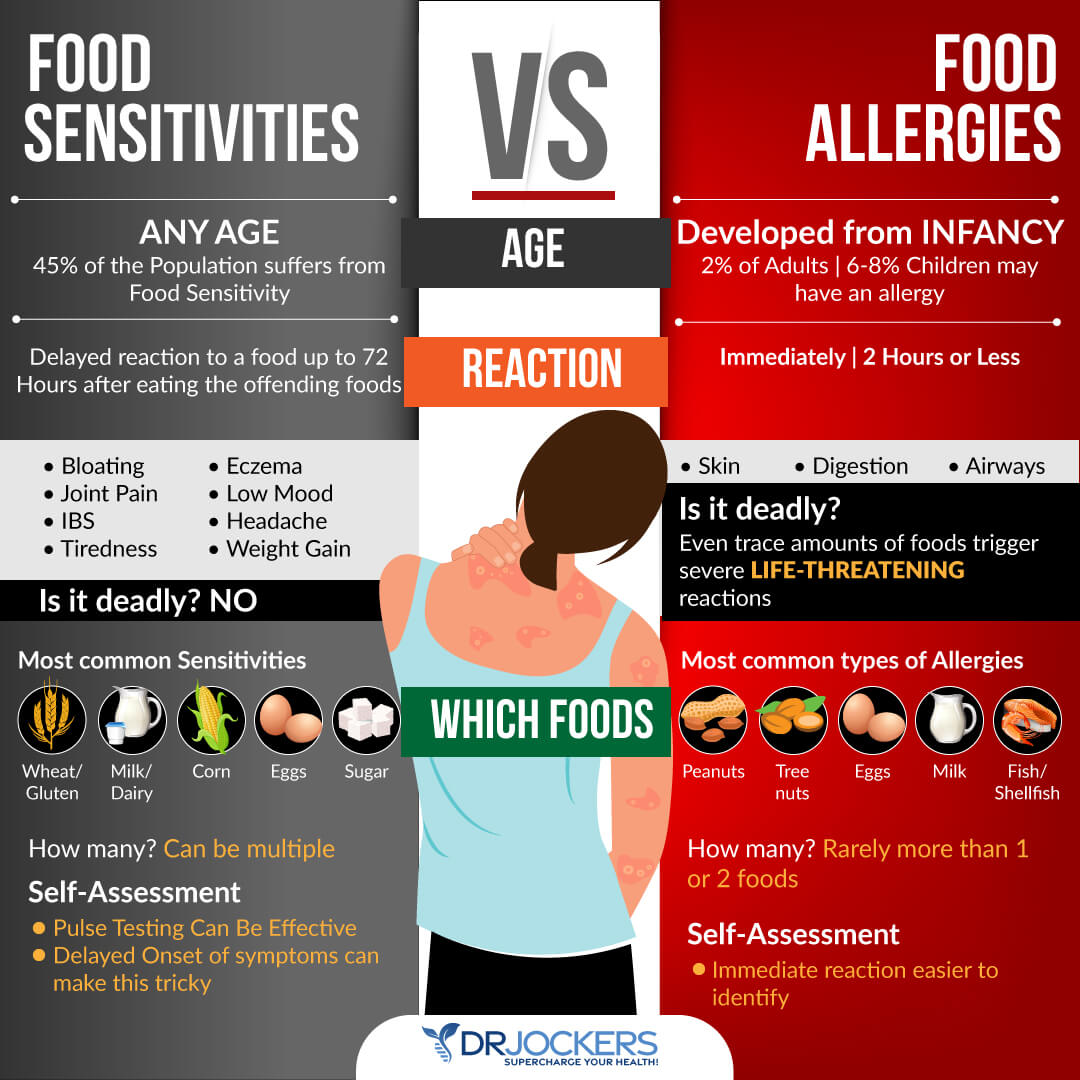
Avoid Food Sensitivities
Food sensitivities and intolerances may cause chronic inflammation and trigger various symptoms and health issues, including vitiligo. For example, a 2017 review published in Dermatology Clinics has found that gluten may trigger vitiligo (25). A 2013 review published in the International Journal of Preventative Medicine has found that celiac antibodies were more prevalent in vitiligo patients than in the non-vitiligo group (26). This may also indicate that gluten may be a problem in vitiligo.
Of course, it may not only be gluten. Other food sensitivities can also increase inflammation and trigger or worsen vitiligo. A 2018 study published in Autoimmune Reviews has shown that food intolerances are commonly seen in autoimmune patients, gluten, casein, cow’s milk, egg white, gliadin, rice, ad wheat being the most common culprits (27).
There are various blood tests to identify food sensitivities. However, these tests only look for certain common sensitivities, and false results are not unusual. Blood tests may be a great first step, but you may need to dig deeper to identify your own sensitivities. I recommend that you first identify your personal food sensitivities with the combination of some blood tests, pulse testing, and an elimination diet. You can learn about these strategies on my website, just use the search bar.
Once you have identified your triggers, remove them from your diet. Since gluten seems to be connected to vitiligo and is highly inflammatory, I recommend removing it regardless of your food sensitivity results. Since food sensitivities can change over time, I recommend testing yearly or if you notice new symptoms.
Intermittent Fasting
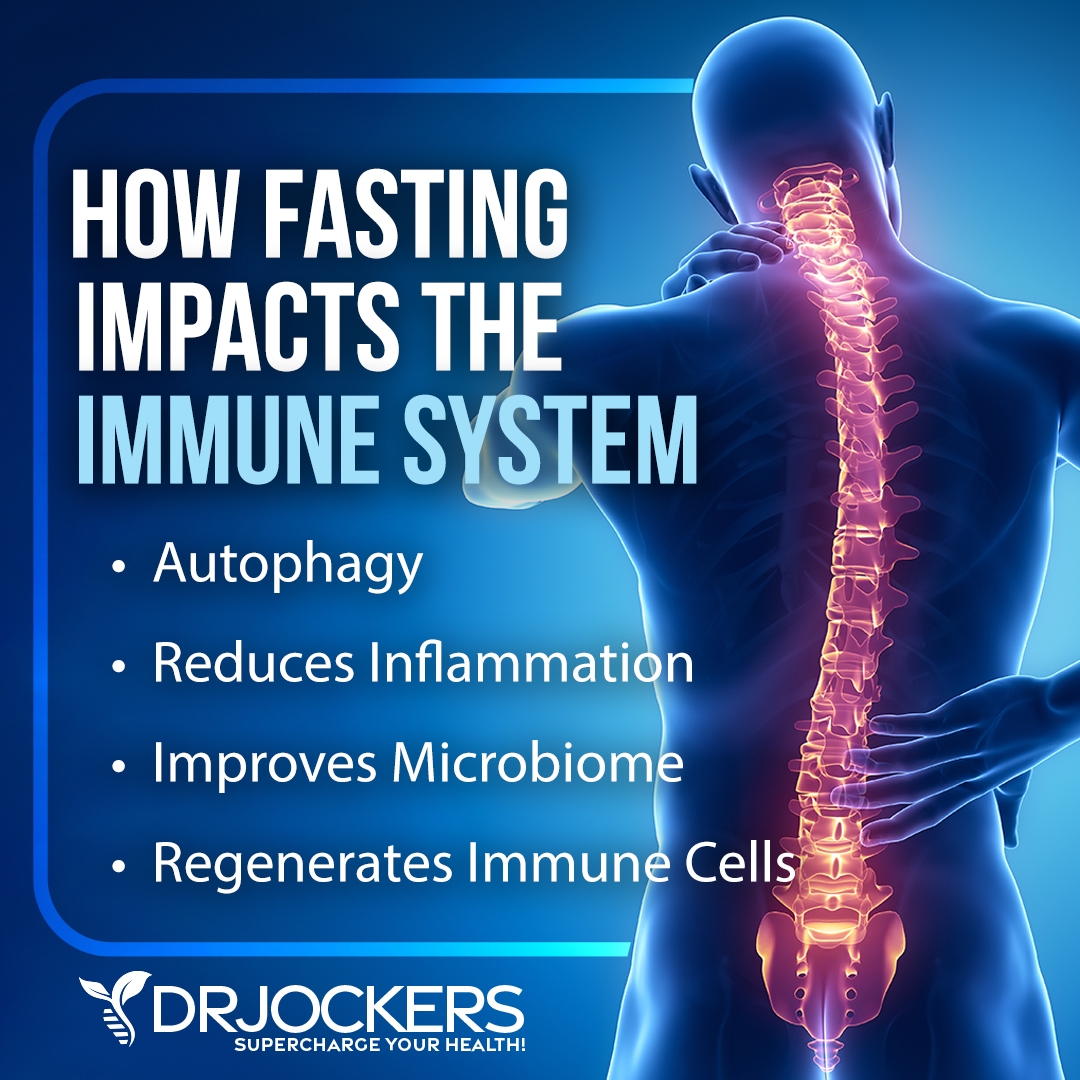
As you’ve learned, according to research, insulin resistance and gut dysbiosis can both increase the risk or worsen vitiligo (5, 4, 6, 7, 8). Intermittent fasting may help to reduce these factors. Intermittent fasting is a form of fasting that cycles between periods of fasting (not eating) and feasting (eating) within one day. It offers a number of benefits, including better insulin sensitivity, improved gut health, and cellular regeneration.
A 2019 systematic review and meta-analysis published in the Journal of Clinical Medicine has found that intermittent fasting may reduce insulin resistance, improve glucose metabolism, and reduce body mass index (28). A 2020 study published in BMC Microbiology has found that 16 to 20 hours of daily intermittent fasting can significantly improve the gut microbiome (29). A 2018 review published in Nutrients has also found that Ramadan fasting, a form of intermittent fasting, may improve skin anatomy, improve various skin conditions, including vitiligo, and support skin renewal (30).
If you are new to intermittent fasting, start with 12 hours of fasting, including your overnight sleep. Then, gradually increase your fasting period over time. Most people feel the best with 16 hours of fasting a day. However, you may feel your best with a slightly longer or shorter fasting window. You can learn more about intermittent fasting and the best intermittent fasting strategies by searching my website.
Reduce Stress & Improve Sleep
A 2021 research published in the Journal of American Academy of Dermatology has discussed that stress can trigger the onset and also affect the progression of the disease (31). A 2021 study published in Middle Eastern Current Psychiatry has found that stress, anxiety, and depression are very common in vitiligo (32). This means that stress can not only trigger or worsen vitiligo, but experiencing vitiligo itself can also increase stress, anxiety, and depression and lead to a poorer quality of life.
Poor sleep and sleep troubles can lead to chronic stress, but stress and mental health issues due to vitiligo can also increase sleep issues. A 2021 study published in Clinical, Cosmetic, and Investigative Dermatology has found that insomnia is highly prevalent in vitiligo patients (34). 49.9 percent of the 409 participants with vitiligo reported insomnia and 59.9 percent of them develop insomnia as a direct result of vitiligo.
The study looked at the factors that may contribute to vitiligo-related insomnia. It turns out that the visibility and severity of the disease, as well as the choice of treatment, may play a role. Researchers have found that having vitiligo symptoms on the face or the neck, having a more advanced case of vitiligo, and using corticosteroids for vitiligo treatment all increased the chance of developing insomnia due to vitiligo.
Reducing stress and improving your sleep are both critical for reducing your risks and managing your symptoms. To reduce stress, I recommend practicing meditation, breathwork, muscle relaxation strategies, guided visualizations, positive affirmatios, gratitude, journaling and prayer. Spend time in nature. Seek support and uplifting activities with friends and family. Have some dedicated me-time as well. If you are experiencing depression or anxiety, you may benefit from support from a therapist, counselor, life coach, or spiritual counselor.
Make sure to sleep 7 to 9 hours a night. To improve your sleep, I recommend that you develop a relaxing bedtime routine that works for you. Turn down electronics and avoid sugar, heavy foods, and alcohol several hours before going to sleep. Reading, crossword puzzles, journaling, listening to calming music, and meditation are beneficial and relaxing ideas to calm your mind and get ready for sleep. Follow a regular sleep schedule that supports your body’s natural sleep rhythms. Invest in a supportive bed and comfortable bedding and pillows.

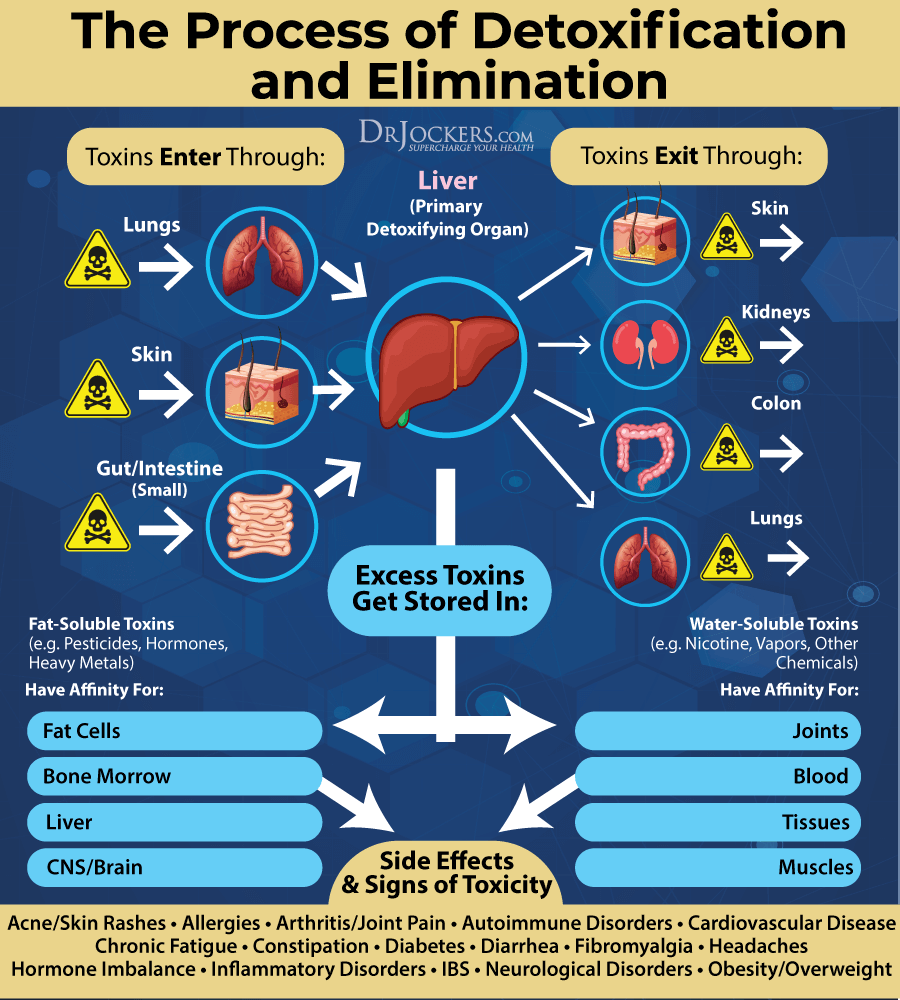
Open Up Detoxification Pathways
Research has shown that A high toxin load, especially mercury, lead, and cadmium, may increase your risk and worsen vitiligo (23, 24). A high toxin load may also increase the risk of chronic inflammation, insulin resistance, gut dysbiosis, and autoimmunity, all of which may contribute to vitiligo. Reducing your toxin load and opening up your detoxification pathways may reduce your risks and support your health.
Choose organic food and organic, natural products, and reduce any other exposure to chemicals or toxins. If you have any mercury amalgam fillings, root canals or dental cavitation’s, visit a biological dentist to safely remove them. Use a high-quality indoor air filtration and water filtration system to improve the air you breathe in and the water you drink. Avoid smoking and second-hand smoke. Spend time in nature to breathe in the fresh air.
Use activated coconut charcoal to remove toxins from your intestinal tract. Follow an antioxidant-rich, anti-inflammatory nutrition plan and take high-quality probiotics and to improve your body’s ability to fight toxins and to support elimination. Drink lots of water to support detoxification through sweating and urine.
Try infrared saunas to promote detoxification through sweating. Practice rebounding and dry-skin brushing to support your lymphatic pathways. Support your two major detoxifying organs, your kidneys and liver, with kidney and liver support supplements.
Regular Sun Exposure & Optimize Vitamin D Levels
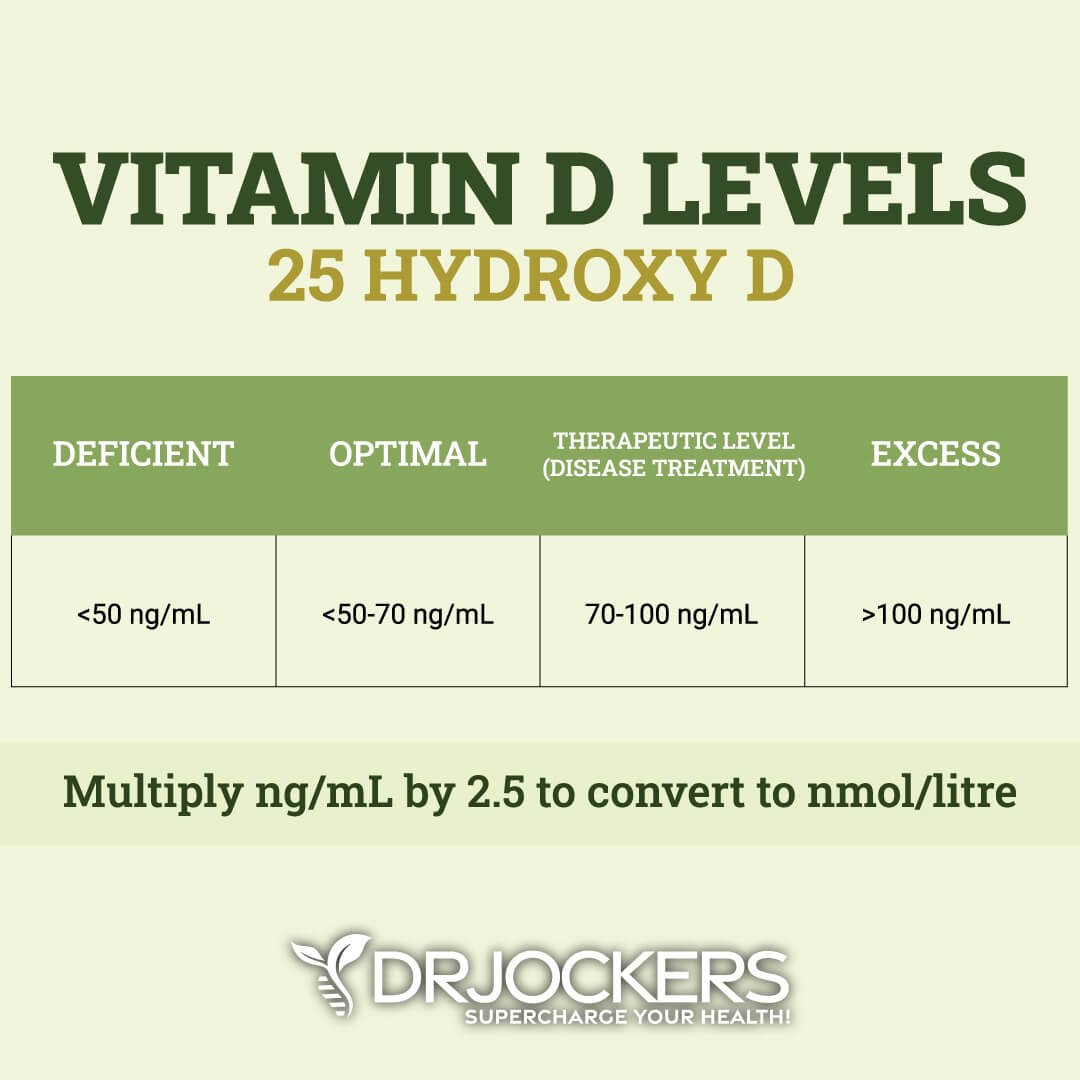
Research has shown that vitamin D deficiency is common in and may be linked to vitiligo (11, 12, 13, 14). Optimizing your vitamin D levels may help. A 2020 study published in the International Journal of Vitamin and Nutrition Research has found that supplementing with vitamin D may have therapeutic benefits for people with vitiligo (35).
To improve your vitamin D levels, I recommend time outside in the sun every day. Unfortunately, it may not be possible on gloomy days or if you live in Northern states or colder countries to meet your daily sunshine requirements. Our indoor lifestyle may also compromise our ability to get as much sun as our ancestors did.
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need supplements to optimize their vitamin D levels. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
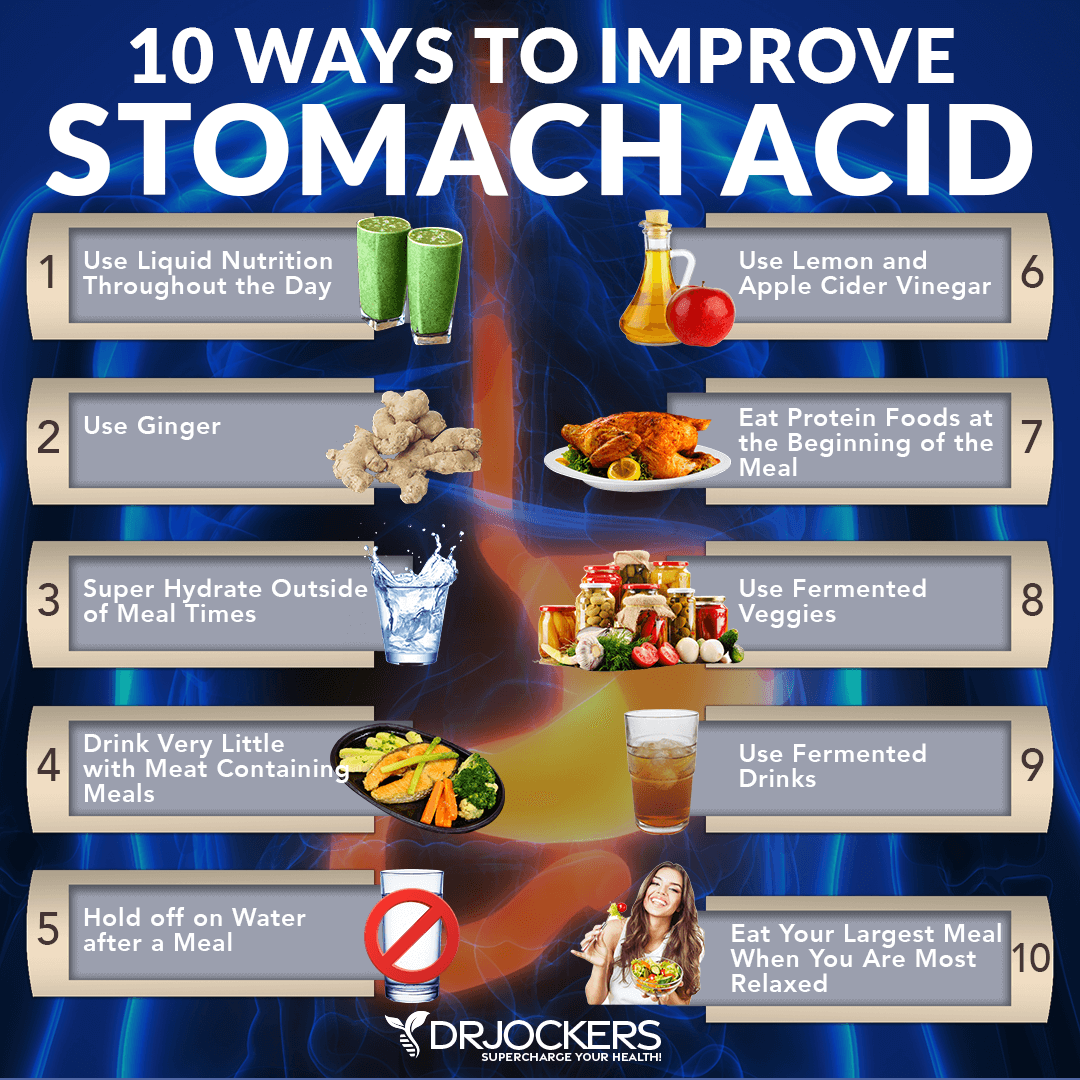
Improve Stomach Acid Levels & Gut Health
Research has shown that low stomach acid levels and poor gut health may be linked to vitiligo (7, 8, 18, 19, 20). Improving your stomach acid levels and gut health is critical for your overall health and may be beneficial for vitiligo.
Eating an anti-inflammatory and gut-friendly diet is the first step. You may benefit from liquid nutrition until your stomach acid levels and gut health improves. Try to make sure that at least half of your meals are in a liquid form, such as a protein shake or green smoothie. Protein shakes are pre-metabolized and very easy to digest and do not depend upon HCL production. If you have low HCL, it may be helpful to drink one to two protein shakes daily to support amino acid absorption, reduce extra stress on your digestion, and support healthy stomach acid levels.
Start your meals with protein first. While it’s culturally common to have a salad before their protein dish, this is not great for your HCL production. It is a much better idea to eat your protein with the salad or vegetables instead of after. Eat your largest meals when you are the most relaxed.
Your body needs to activate the parasympathetic nervous system to produce enough stomach acids. If you are busy and on the go, you will be in fight or flight sympathetic mode. If you struggle with low stomach acid, this fight or flight state will not allow your body to produce anywhere near enough. Relaxing before the meal is important to improve stomach acid production.
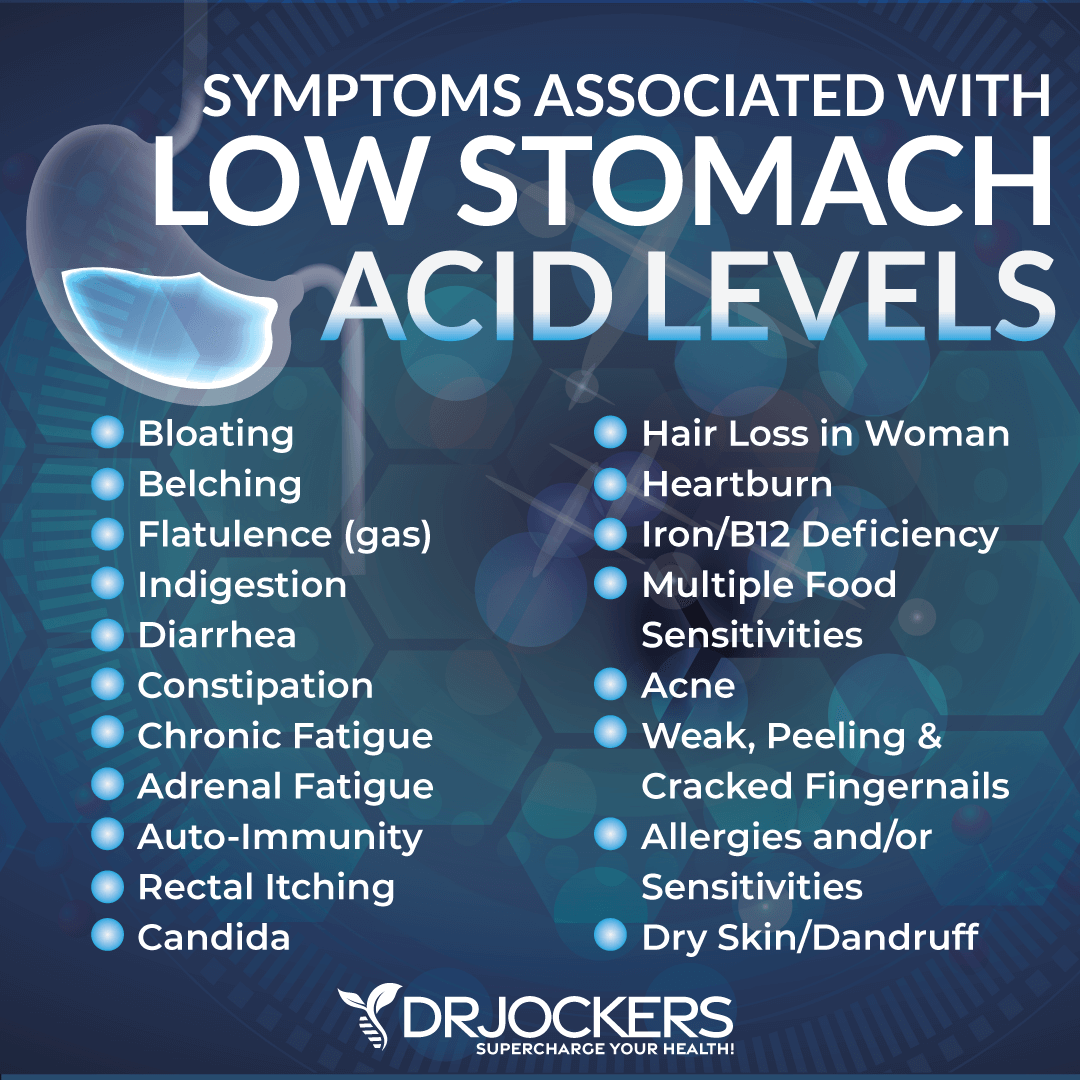
Add fermented foods, such as sauerkraut, kimchi, pickles, pickled ginger, and other fermented vegetables that all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions. I also recommend fermented drinks, such as apple cider vinegar, coconut kefir, and kombucha with anti-microbial benefits to help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Additionally, take daily probiotic supplements to support your microbiome health, digestive enzymes to support digestion, and a supplement with betaine hydrochloric acid to support stomach acid production and bile flow.
Eat slowly and chew your food well. Hydrate well throughout the day between meals to help activate bowel motility and push contents through the digestive system, which will reduce microbial fermentation and toxicity in the body.
However, stop drinking water or other liquids at least 30 minutes before the meal, except if you need to take a supplement with 2 ounces of water and don’t drink water or other liquids until at least 30 minutes after a meal. This allows for proper stomach acid activity, sterilization, and protein metabolism.
For better digestion and improved stomach acid levels, I recommend using ginger in your meals and adding ginger to your tea. Ginger is one of the best things for improving digestive juices. I recommend drinking 2 to 3 cups of ginger tea each day.
You can put ginger essential oil in water (2 to 3 drops in 8 oz of water), juice a ½ inch of fresh ginger root in a green juice each day, and use ground ginger on your foods. You can also add fermented ginger to your diet, which is common in Asian dishes such as kimchi.
Optimize Zinc, B12 & Folate Levels
Zinc, vitamin B, and folate deficiencies are common in people with vitiligo and may be linked to the disease (15, 16, 17, 21, 22). A 2020 patient-controlled prospective study published in Dermatologic Therapies has found that zinc may have therapeutic benefits for those with vitiligo (36). A 1997 study published in Acta Dermato-Vermatologica has found that vitamin B12, folate, and sun exposure may help to improve vitiligo (37).
Zinc-rich foods I recommend adding to your diet include grass-fed meat, pasture-raised poultry, nuts, seeds, oysters, peas, and chickpeas. Additionally, I recommend that you take a high-quality zinc supplement. I also recommend consuming foods rich in B vitamins, including liver, meat, seafood, poultry, leafy greens, and seeds. Additionally, I recommend taking a daily high-quality B-12 and B complex supplement.

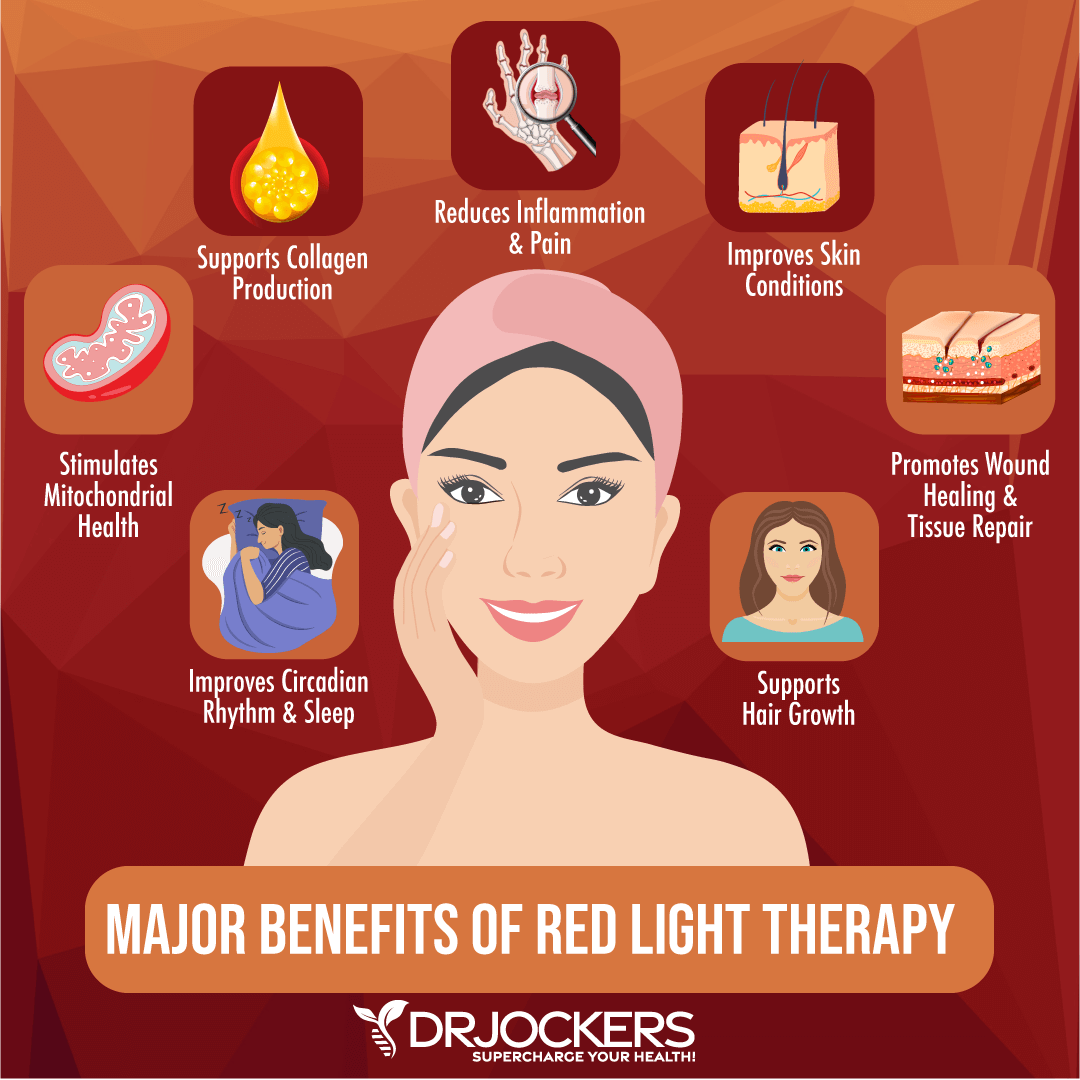
Consider Phototherapy
You may also benefit from phototherapy. A 2017 systematic review and meta-analysis published in JAMA Dermatology has found that phototherapy may benefit vitiligo (38). Researchers looked at the benefits of both narrowband UV-B (NBUVB) phototherapy and undergoing psoralen-UV-A (PUVA) phototherapy and both showed at least mild improvements.
A 2019 review published in Experimental Dermatology has found that photobiomodulation (PBM) therapy which uses an “exposure of biological tissues to low-level laser light (coherent light) or light-emitting diodes (LEDs; noncoherent lights)” may benefit repigmentation of vitiligo (39).
A 2013 study published in Seminars in Cutaneous Medicine and Surgery has found that low-level laser light therapy may benefit vitiligo and other skin disorders (40). A 2014 controlled trial published in Photomedicine and Laser Surgery has found that red and near-infrared light therapy may benefit your skin health (41). There is also an ongoing clinical trial at the University of British Columbia that is looking at the benefits and effectiveness of red light therapy for vitiligo (42).
Red light therapy is a powerful therapeutic technique and an alternative healing method. It uses red low-level wavelengths of light for a variety of therapeutic purposes, including wound healing, scars, and other skin issues, inflammation, pain, hair growth, and sleep quality.
The best part is that it’s accessible, and you can use it from the comfort of your home. You can find more information on red light therapy and red-light therapy for skin health, specifically on my website.
Consider Using Antioxidant Herbs and Compounds
You may also benefit from using antioxidant herbs and compounds for vitiligo. A 2021 review in Dermatology Reports has discussed how oxidative stress may play a role in vitiligo and what strategies may help (43). Along with finding that phototherapy, vitamin D, and zinc may help, they also found that those with vitiligo may benefit from antioxidants for anti-inflammatory, immune-protecting, and free-radical-reducing benefits.
Researchers found that green tea may be beneficial for vitiligo due to its anti-inflammatory, antioxidant, and immunomodulatory properties. They found that you may also benefit from alpha-lipoic acid for its antioxidant benefits at 50 mg twice a day orally. Researchers found that Polypodium leucotomos, a tropical fern, may be beneficial due to their antioxidant and immunomodulator properties.
They also found that ginkgo biloba, which is an important part of traditional Chinese medicine, may also offer therapeutic benefits for vitiligo. Lastly, they found that flavonoids, a plant compound found in blueberries other berries, tea, onions, bananas, all citrus fruits, cacao, dark chocolate, red cabbage, kale, arugula, and other plant foods, may also benefit. You may benefit from using these antioxidant herbs and compounds in your diet and as supplements.

Final Thoughts
Vitiligo is a skin condition characterized by loss of pigmentation in patches of your skin. Vitiligo most commonly affects your hands, feet, arms, and face. However, it may also affect your hair, mouth, mucous membranes, genitals, inner ear, and eyes.
Conventional strategies for vitiligo tend to use creams, medication, surgery, and coverage, which are not without risks and side effects. The good news is that there are some natural support strategies for vitiligo that can improve your health and well-being. I recommend that you try my natural support strategies for vitiligo.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!