 Gastritis: Symptoms, Causes, and Support Strategies
Gastritis: Symptoms, Causes, and Support Strategies
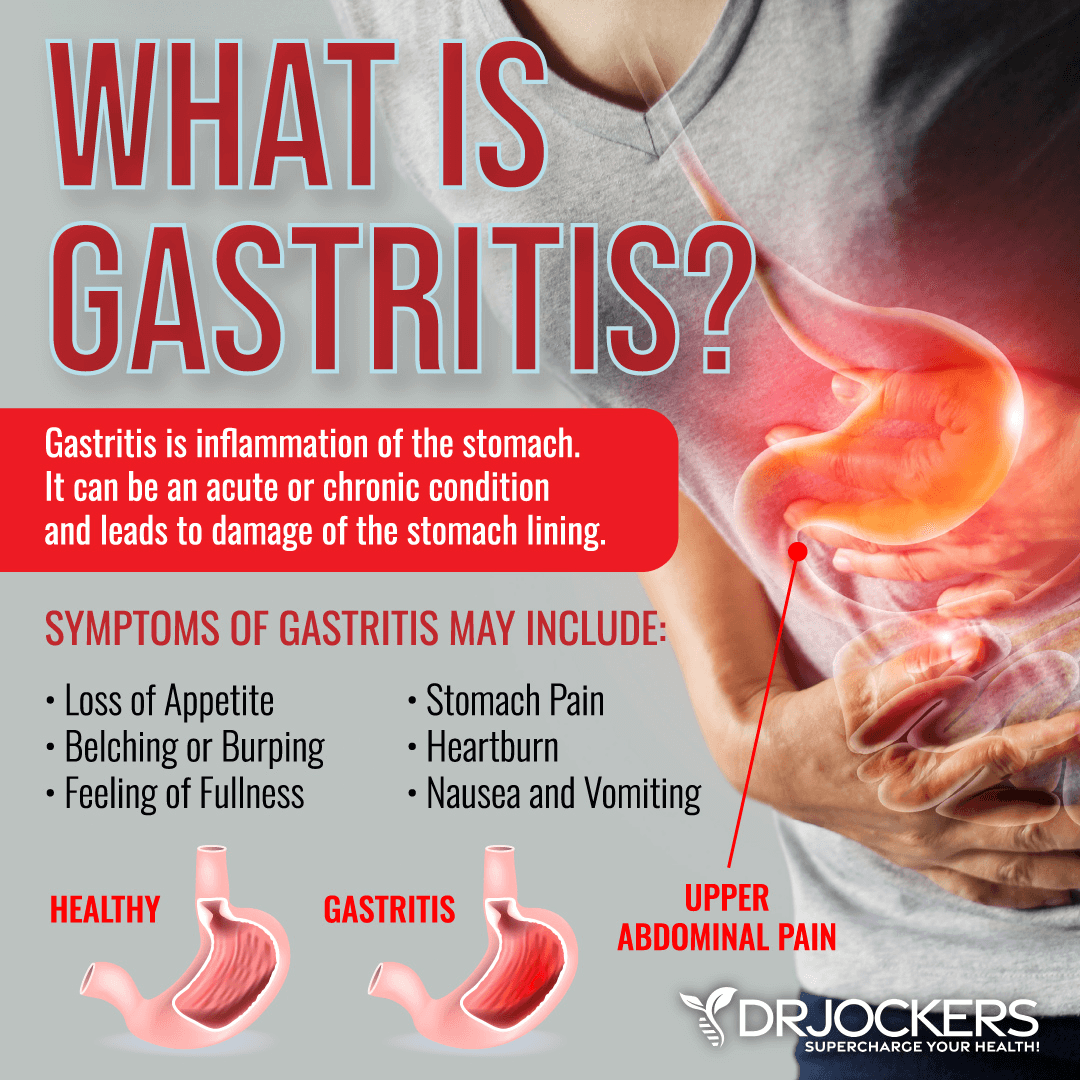
Gastritis is a gut condition characterized by inflammation of the stomach lining. Symptoms can be uncomfortable and can include abdominal pain, bloating, nausea, vomiting, feeling of fullness, loss of appetite, and weight loss. Untreated and serious chronic gastritis can lead to long-term damage and stomach ulcers. However, through a healthy diet and lifestyle, you can support your body and reduce your risks.
In this article, I will explain what gastritis is. You will learn about the signs and symptoms of gastritis. I will go over its three types of gastritis. You will understand the root causes of gastritis. You will learn about diagnosis and conventional treatment strategies. I will recommend some key lab analyses. Most importantly, I will offer some natural support strategies to support your body and improve your health.
What Is Gastritis
Gastritis is a gut health condition. It is an inflammation of the stomach lining that may develop because of chronic inflammation, an inflammatory diet, bacterial overgrowth, autoimmunity, certain medications, or other issues (1).
Gastritis can develop suddenly in an acute fashion. In these cases, they usually also resolve without treatment. Chronic gastritis, however, is a more serious and on-going issue. According to a 2015 study published in the Scandinavian Journal of Gastroenterology, over half of the world’s population is dealing with chronic gastritis (2). Chronic gastritis may cause various complications without treatment, including stomach ulcers and stomach cancer. However, as you will learn, gastritis is an avoidable and treatable condition.
Signs and Symptoms of Gastritis
At first, most people with gastritis are not experiencing any symptoms. Signs of indigestion may start to appear after a while.
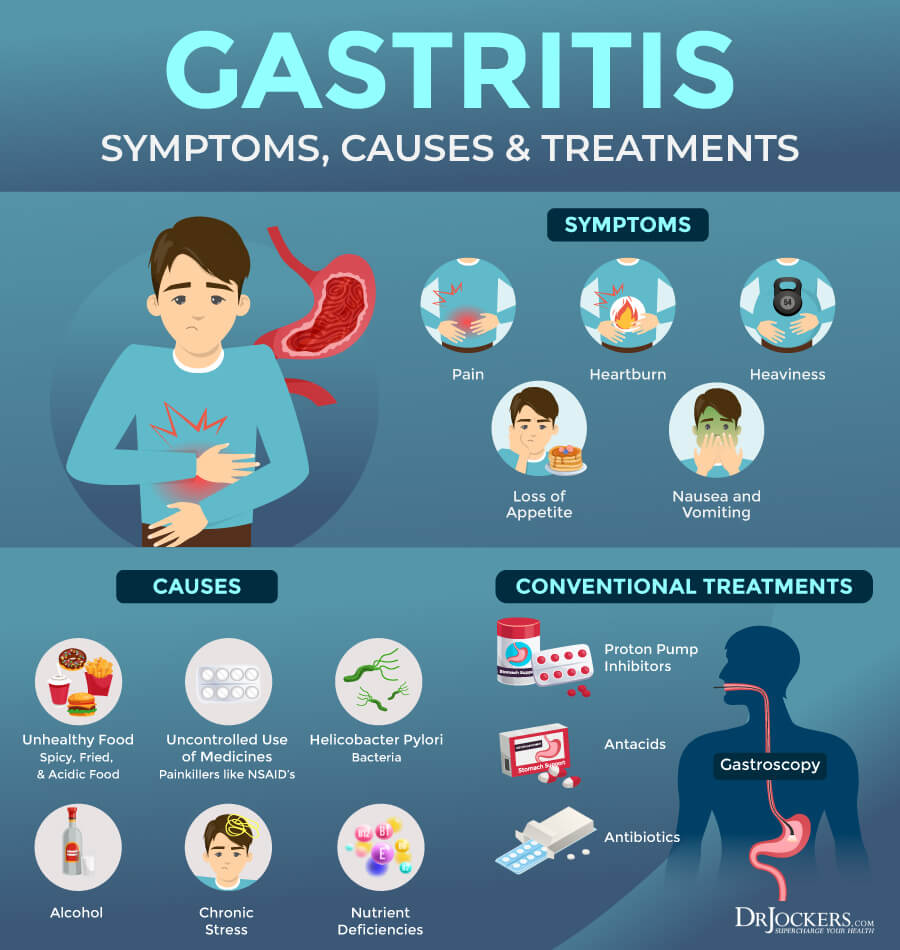
Symptoms of gastritis may include (3):
- Pain or discomfort in the upper abdomen
- Nausea
- Vomiting
- Experiencing fullness too early during a meal
- Experiencing fullness after a meal
- Loss of appetite
- Weight loss
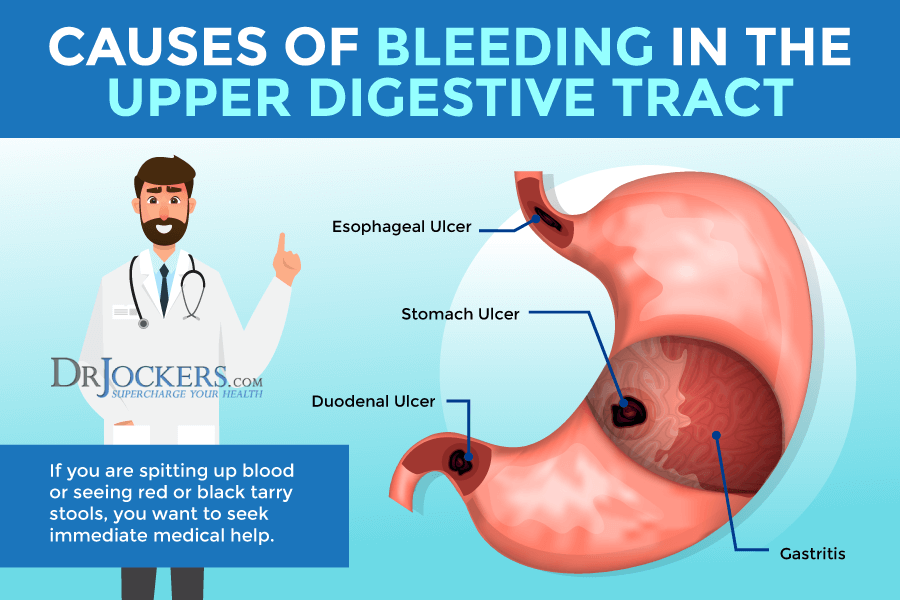
People with more serious cases of chronic gastritis can experience erosions, ulcers, or stomach bleeding. Bleeding in your stomach is a serious issue and you need to seek medical help right away.
Signs of stomach bleeding may include (3):
- Black or tarry stool
- Red or maroon blood in the stool
- Cramps, pain, or discomfort in the abdomen
- Feeling tired
- Shortness of breath or light-headedness
- Red blood in the stool
- Vomiting what looks like coffee grounds
Different Types of Gastritis
There are several different types of gastritis. While certain types are less common, the most common types of gastritis you need to know about include acute gastritis, chronic gastritis, and atrophic gastritis (4).
Acute Gastritis
As its name suggests, acute gastritis is an acute and sudden case of gastritis that develops quickly and lasts for a shorter period than other forms. However, the symptoms of acute gastritis are more clear and much more severe than in chronic gastritis. In some cases, symptoms of acute gastritis may come and go, and lifestyle factors can trigger episodes.
Chronic Gastritis
Unlike acute gastritis, chronic gastritis develops gradually and can result in long-term complications and health issues. Early on, people with chronic gastritis don’t notice any symptoms. It may take years until the inflammation gets so serious that you notice any concerning symptoms.
Chronic gastritis is characterized by the thinning of gastric mucosa, which can lead to the increase of inflammatory cells. This may not only worsen your gastritis but may also increase your risk of gastric cancer.
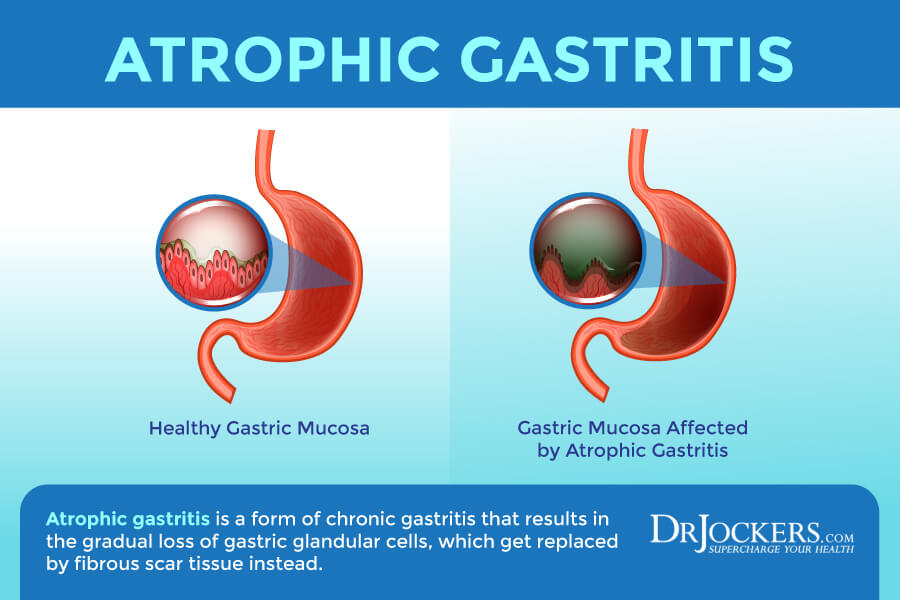
Atrophic Gastritis
Atrophic gastritis is a serious form of chronic gastritis that can result in the gradual loss of gastric glandular cells, which get replaced by fibrous scar tissue instead. If you have atrophic gastritis, as your gastric lining becomes more compromised, over time your risk of poor nutrient absorption and nutrient deficiencies increases.
Atrophic gastritis also increases your risk of autoimmune disorder reactions. It may also result in low gastric acid output and hypergastrinemia, which can increase your risk of both anemia and tumor growth.
Root Causes of Gastritis
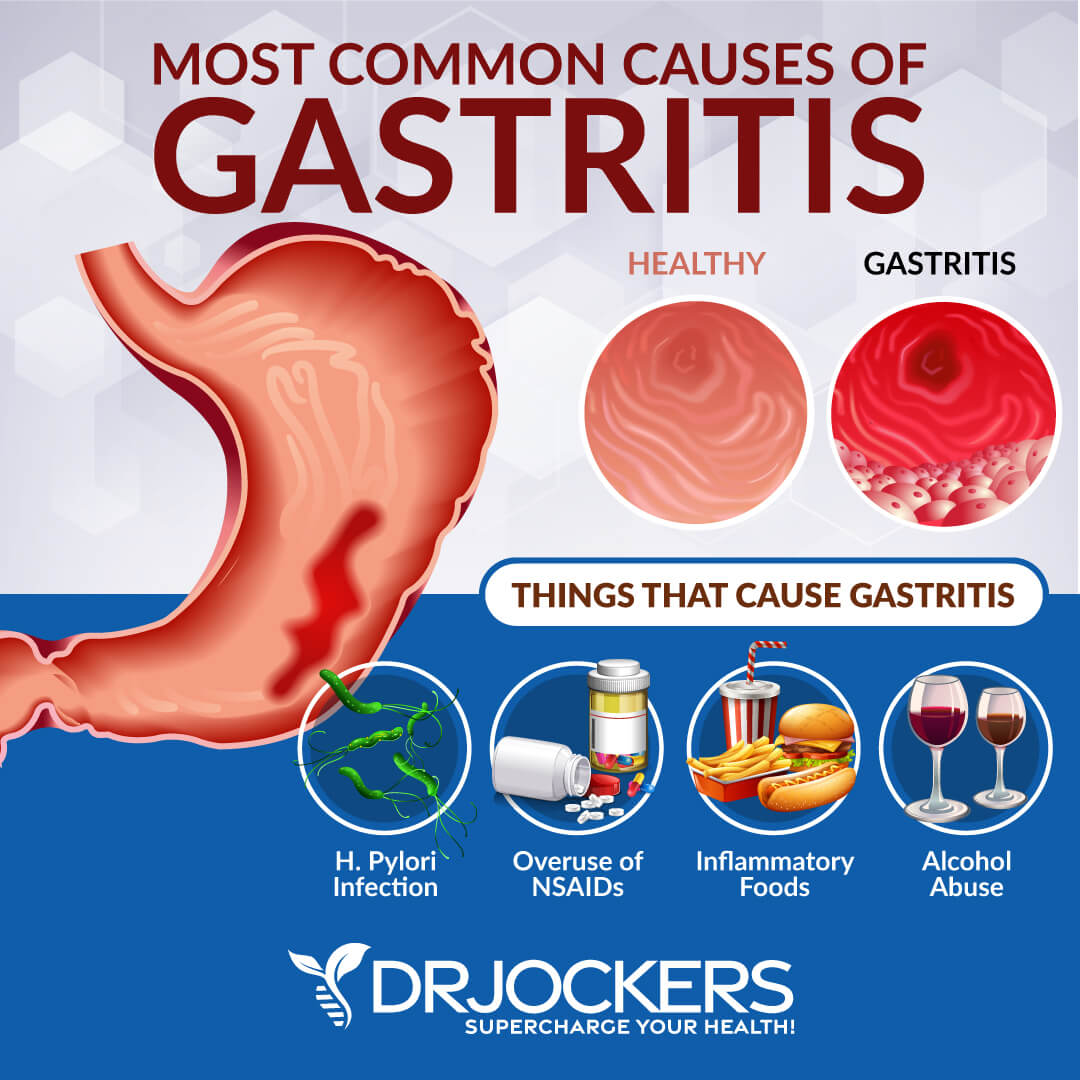
Gastritis may develop for a number of reasons, including health, dietary, lifestyle, and nutritional factors. Let’s look at the root causes of gastritis:
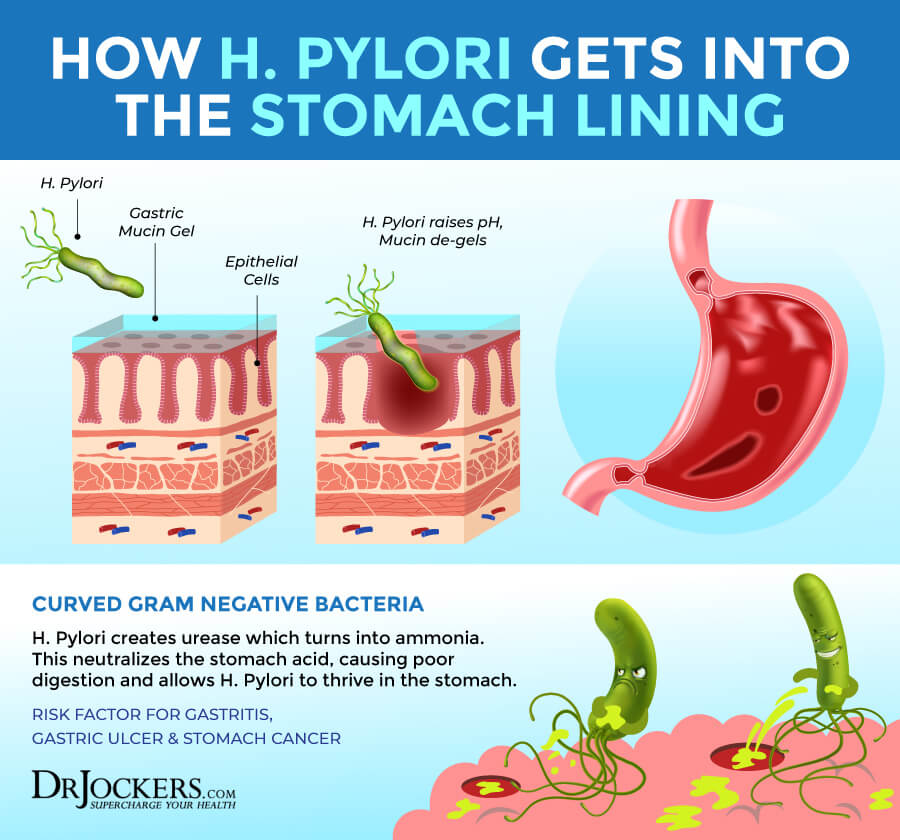
Chronic Infection
A 2003 review of Helicobacter pylori or H Pylori is the most common one that can cause gastritis (5). Having some H pylori in your system is okay, most people have them. However, when the bacteria starts to repopulate quickly, it can cause issues with the stomach lining, erosion, and stomach ulcers.
This often happens because of low immune function, too much stress, or a poor diet. H pylori infection can not only cause gastritis, but chronic gastritis can further increase h pylori overgrowth creating a vicious cycle.
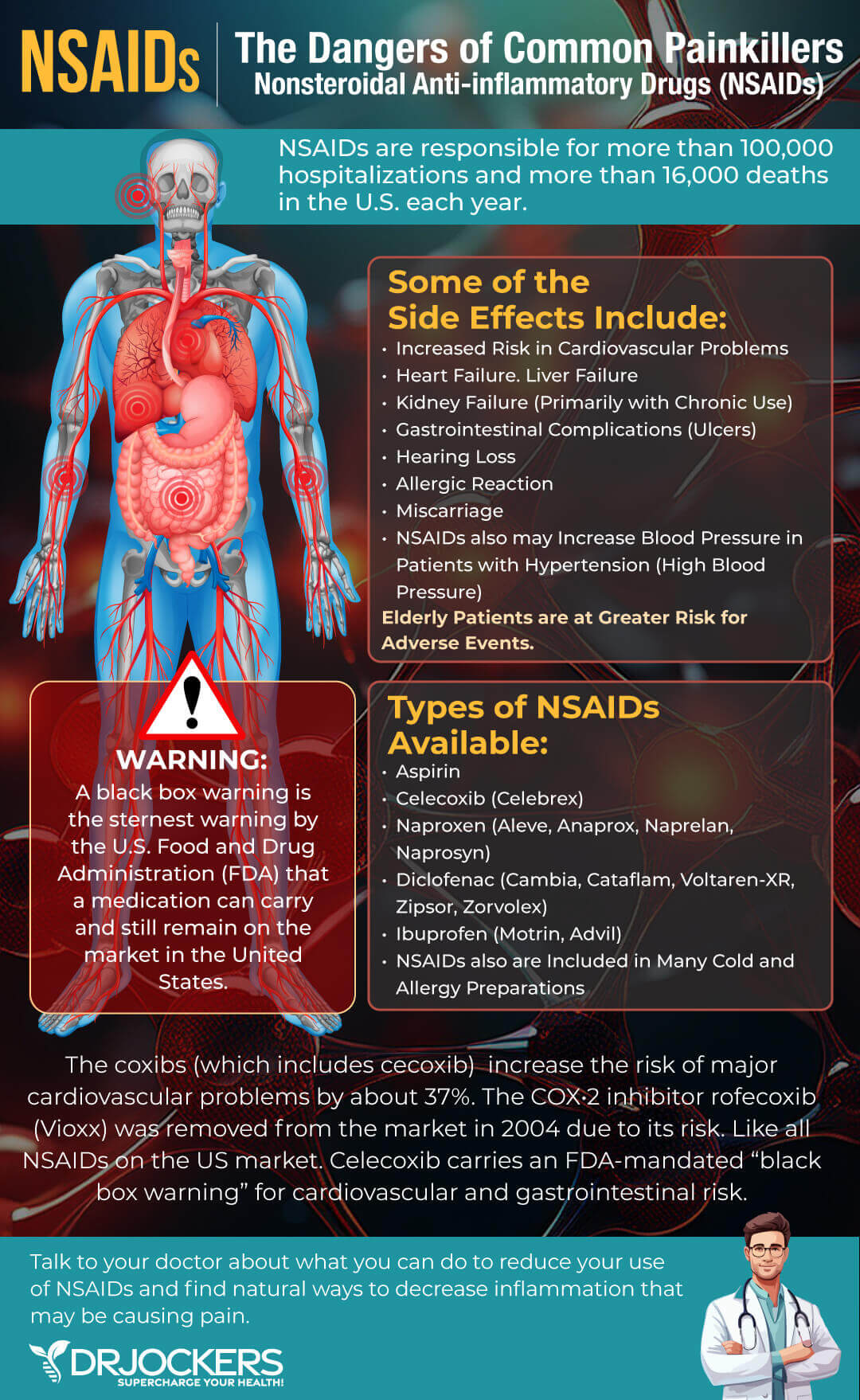
Overuse of NSAIDs
Reactive gastropathy is a form of gastropathy that develops because of the long-term use or overuse of medications and substances. They can irritate and damage the stomach lining, including non-steroidal anti-inflammatory drugs (NSAIDs), alcohol, and bile from bile reflux or bariatric surgery (3).
Using NSAIDs for pain is very common and some people use them on a regular or even on a daily basis. This can become a serious issue. According to a 2015 case study and review published in Drug, Healthcare and Patient Safety, the use of NSAIDs can lead to gastrointestinal injuries (6). In a 2000 study published in Baillieres Best Practice & Research, Clinical Gastroenterology has found that the overuse of NSAIDs can impair the gut barrier and reduce gastric mucosa, which can lead to gastritis, stomach ulcers, and stomach bleeding (7).
A 1992 study published in Agent Actions has explained that one of the biggest problems with NSAIDs is that they deplete glutathione levels, which can have detrimental effects on organ function (8). As a 2004 study published in Surgery explains, glutathione, an antioxidant is very important for the gut barrier function and integrity, and low levels can lead to all kinds of gut problems, including even a gut barrier failure (9).
Alcohol Abuse
Other than NSAIDs, alcohol is one of the major causes of reactive gastropathy that causes irritation to the stomach lining (3). Alcohol can cause irritation, damage, and inflammation of the stomach lining, impact gastric juices, cause gut health issues, and lead to gastritis and stomach ulcers.
A 2002 clinical trial published in the Annals of University Mariae Curie Sklodowska Medicine has found that chronic alcohol abuse can seriously impact the gastric and duodenal mucosa (10). Researchers observed atrophic gastritis in the group that was addicted to alcohol while the group that has never drank alcohol didn’t have gastritis.
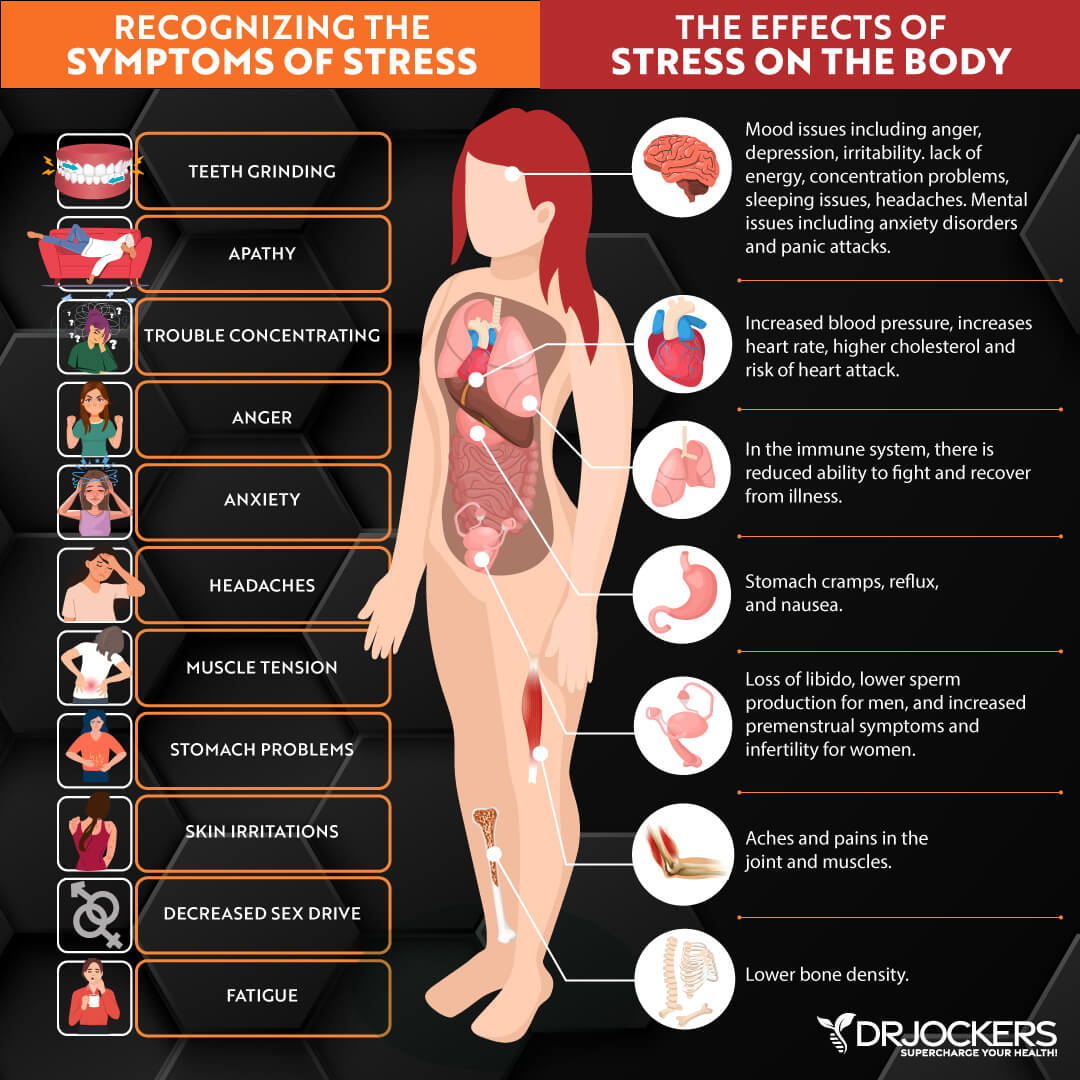
Chronic Stress
Chronic stress and high levels of stress can also lead to symptoms of gastritis. Unlike other forms of gastritis, stress-induced gastritis may not result in the inflammation of the stomach, but it can lead to gastritis-like symptoms, including the feeling of a full stomach, heartburn, and stomach pain.
Stress, anxiety, nervousness, and other emotional issues can lead to this problem. However, chronic stress can also impact your eating and lifestyle habits. For example, when stressed, you may be more likely to reach for inflammatory, sugary foods, drink alcohol, or take NSAIDs for stress-related pain and symptoms.
As a result, chronic stress can contribute to actual stomach inflammation and the development of gastritis. If gastritis is stress-induced, it is important to address emotional problems and stress levels during treatment (11).
Inflammatory Diet
Gastritis is an inflammatory condition so it’s not surprising that an inflammatory diet can bring upon and trigger symptoms. Certain inflammatory foods, including acidic, spicy, and hot foods, processed or packaged foods, alcohol, and caffeine can trigger inflammation and gastritis symptoms, while other foods, including high-fiber foods, antioxidant-rich food, electrolytes, and omega-3 fatty acids may help to reduce symptoms (12).
Eating disorders, especially ones that involve purging, such as bulimia nervosa, can also increase the risk of gastritis symptoms. Be sure to read down lower in the article for the best nutrition principles to follow.

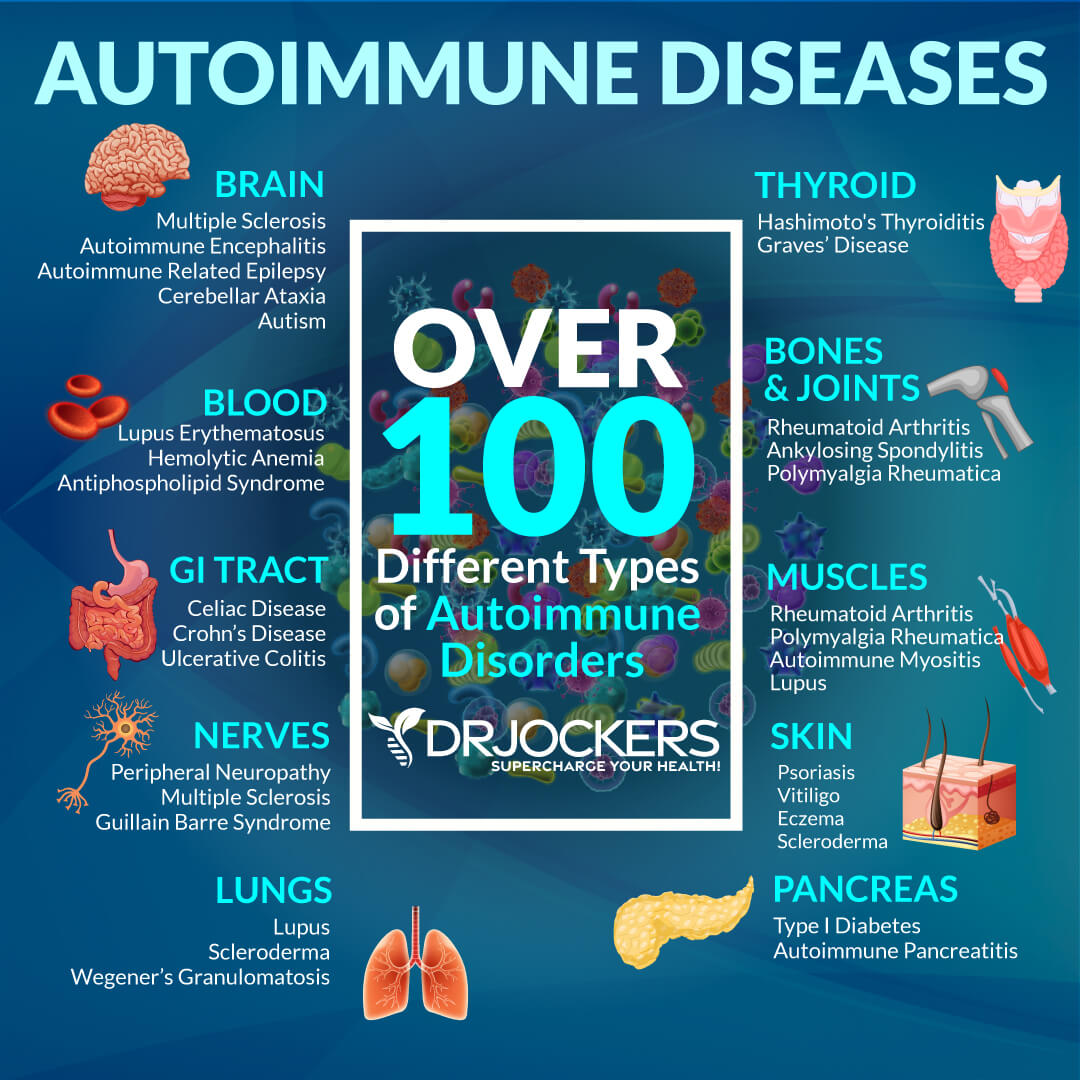
Autoimmunity
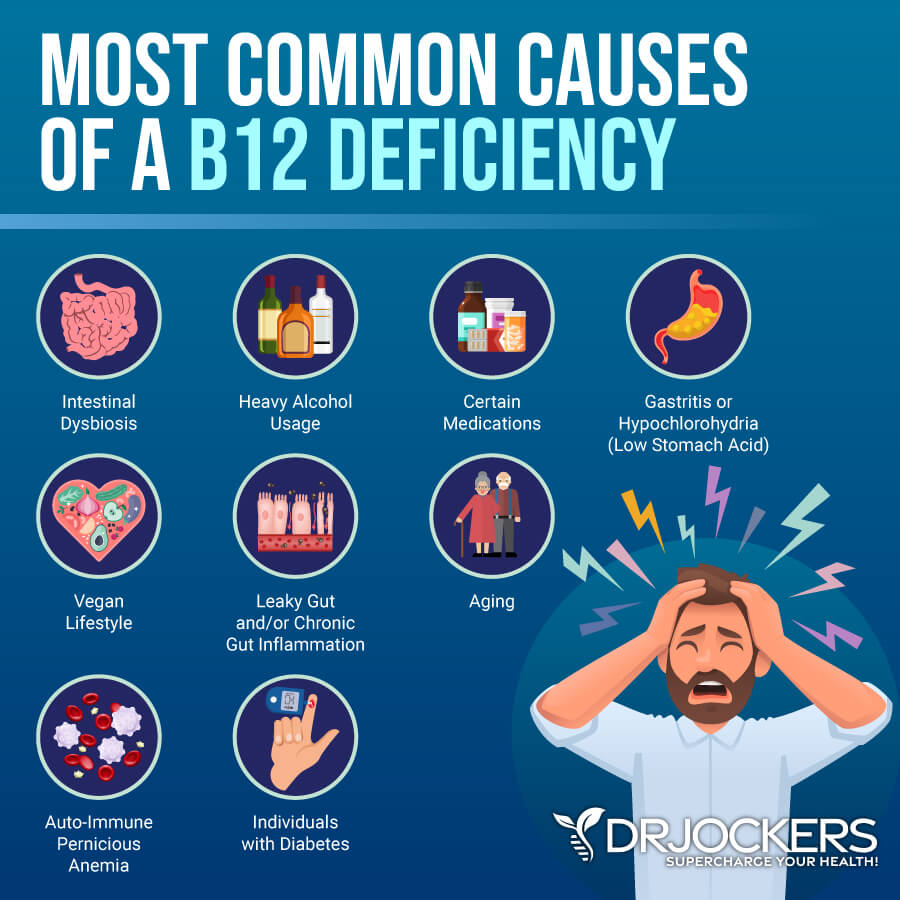
Autoimmune gastritis is a form of gastritis caused by an autoimmune reaction where your immune system attacks healthy cells in your stomach lining by mistake (3). According to a 2016 study published in Wiener Medizinische Wochenschrift (1946), autoimmune gastritis may be connected to a deficiency in vitamin B12 and iron (13).
Low vitamin B12 levels can result in pernicious anemia that can increase the reduction of the secretariat of gastric acid and absorption. While we don’t know what the exact cause of autoimmune gastritis is, however, it is more common in people with type 1 diabetes, autoimmune thyroiditis, Addison’s disease, vitiligo, and other autoimmune diseases.
Nutrient Deficiencies
Nutrient deficiencies, vitamin D, vitamin C, and zinc deficiencies, in particular, may also result in gastritis.
Vitamin D
Vitamin D is a very important vitamin for your muscle, bone, digestive, and immune health. A 2012 study published in the Clinical Reviews in Allergy and Immunology has found that vitamin D has anti-inflammatory and immune-regulatory properties (14). Since vitamin D affects the immune system deficiencies can increase autoimmunity and cause autoimmune gastritis.
A 2019 study published in Aging Clinical and Experimental Research has connected vitamin D deficiency to an increased risk of H pylori infection in older adults which is one of the main causes of the development of gastritis (15). A 2018 prospective study published in BMC Gastroenterology has also found that vitamin D deficiency is very common among chronic, autoimmune, and atrophic gastritis patients (16).

Vitamin C
Vitamin C is one of the most commonly known and most important vitamins for immune health. A 2012 historical review published in Digestive Diseases and Sciences has found ascorbic acid or vitamin C deficiency can increase the risk of H pylori infections and as a result, may increase the risk of gastritis and stomach ulcers (17).
A 2018 study published in Cureus, on the other hand, has found that vitamin C may be an effective prevention and therapeutic agent for H pylori overgrowth. Hence vitamin C may be helpful against H pylori-related gastritis (18).
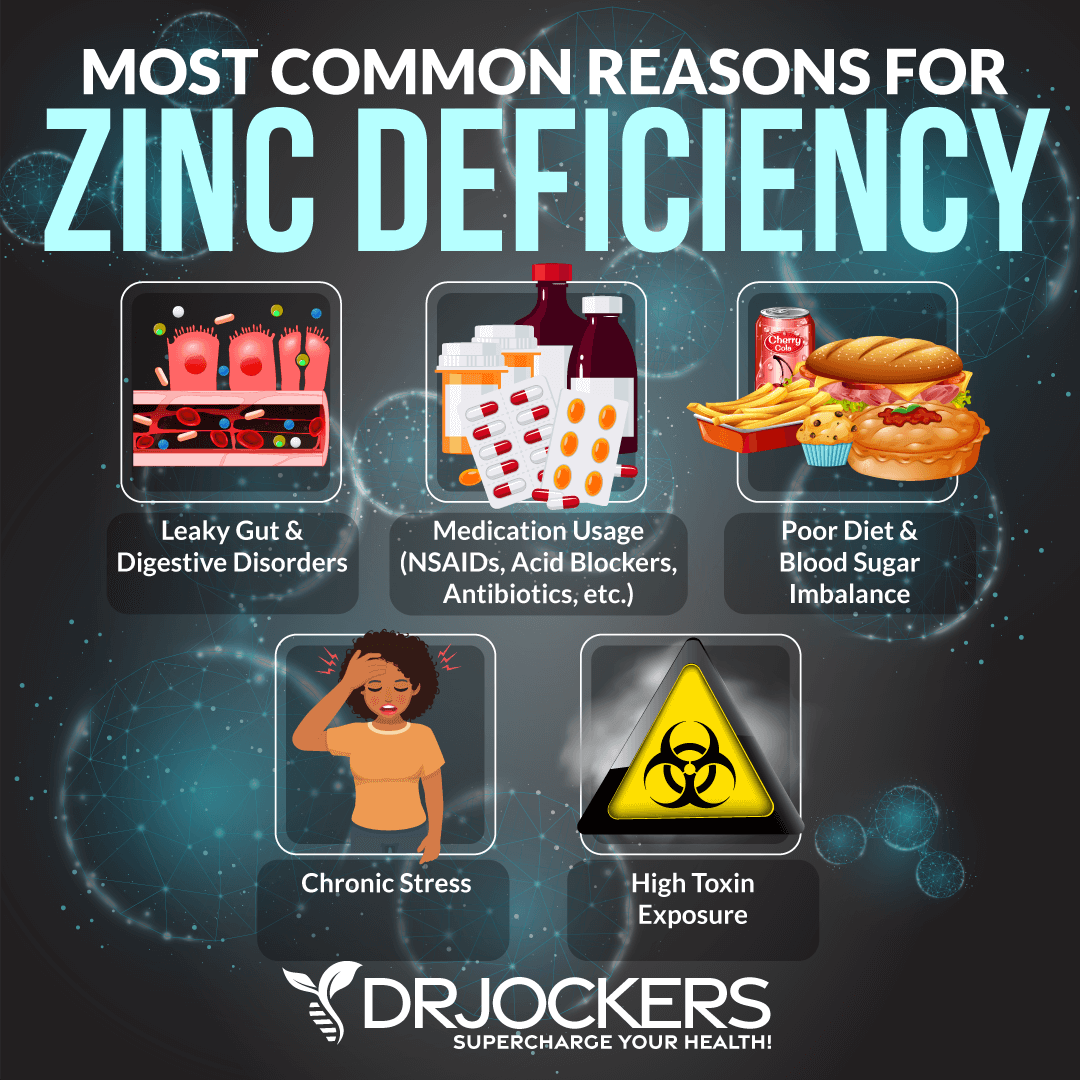
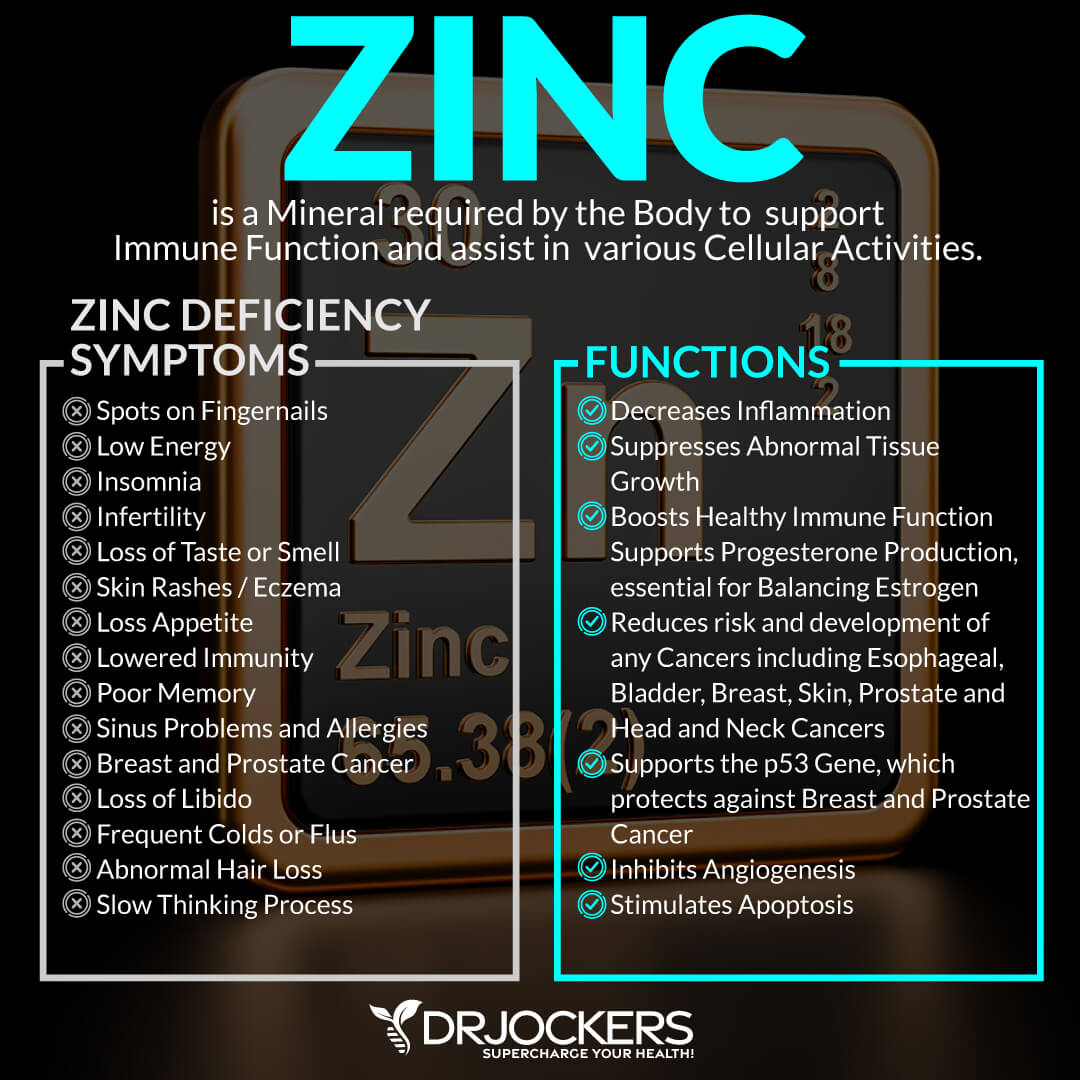
Zinc
Zinc is a critical vitamin for immune health and metabolic function. A 2007 study published in Helicobacter has found that zinc deficiency can impact the gastric mucosa and contribute to H pylori overgrowth (19).
A 2012 randomized controlled trial published in the Asian Pacific Journal of Cancer Prevention has found that low serum zinc levels and H pylori overgrowth are common among gastritis patients compared to participants of the healthy control group (20).
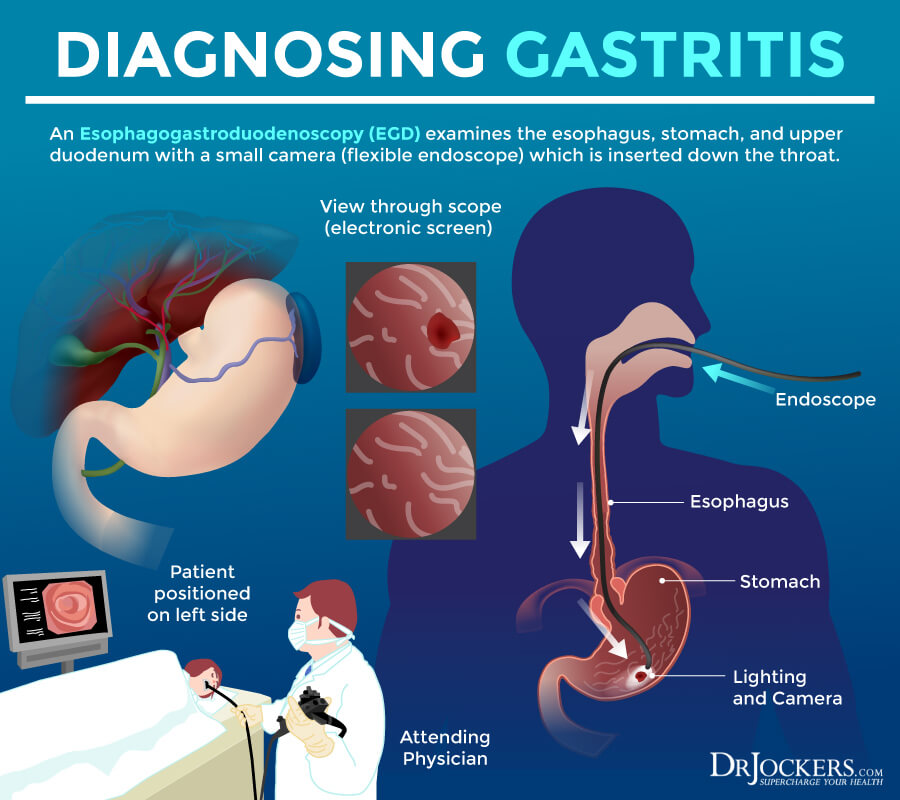
Diagnosis and Conventional Treatment
If you are experiencing symptoms of gastritis, your doctor will first go over your medical history, family history, symptoms, and the list of medications you are taking. Next, they will do a regular physical exam. To diagnose and confirm that you have gastritis and to identify the type, they may order a variety of tests including (1, 21):
- An upper gastrointestinal (GI) endoscopy to look at your esophagus, stomach, and duodenum.
- Various blood tests to check for causes of gastritis.
- A stool test to look for an H. pylori infection.
- A urea breath test to check for H. pylori infection.
- An upper gastrointestinal (GI) series that uses an x-ray and a chalky liquid called barium to look for signs of gastritis in your upper GI tract
Conventional treatment options for gastritis depend on the types of gastritis you have, your symptoms, and its causes. If your gastritis is connected to an H. pylori infection, your doctor may recommend two or more antibiotics, proton pump inhibitor (PPI) medications, and in certain cases, bismuth subsalicylate.
For acute gastritis, PPIs, H2 blockers, or sucralfate are often recommended to reduce stress gastritis. In other cases, such as autoimmune gastritis, iron, folate, and vitamin B12 may be recommended.
In some cases, non-steroidal anti-inflammatory drugs (NSAIDs) or ursodiol, a drug with bile acids may be prescribed. In some cases, dietary or lifestyle changes are recommended. For example, if Celiac disease or food allergies are identified as the underlying cause, you will have to avoid gluten and any identified food allergens (1, 22).
Key Labs to Analyze
As a functional medicine practitioner, I find it important that we look at certain key lab results to evaluate your risks and potential underlying causes of gastritis and other health issues. Understanding the full picture can help us to create the right plan to support your body. Here are the key labs I recommend for gastritis:
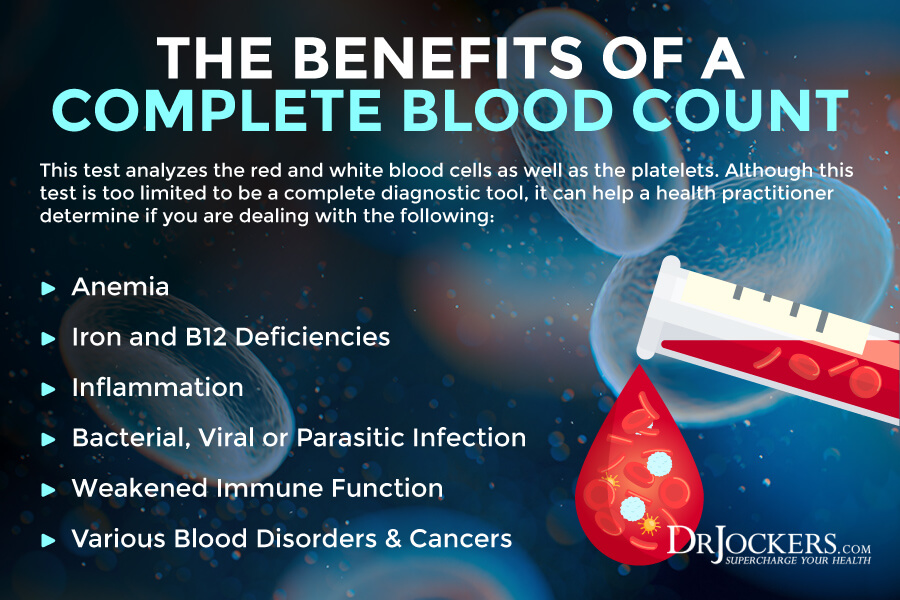
Complete Blood Count
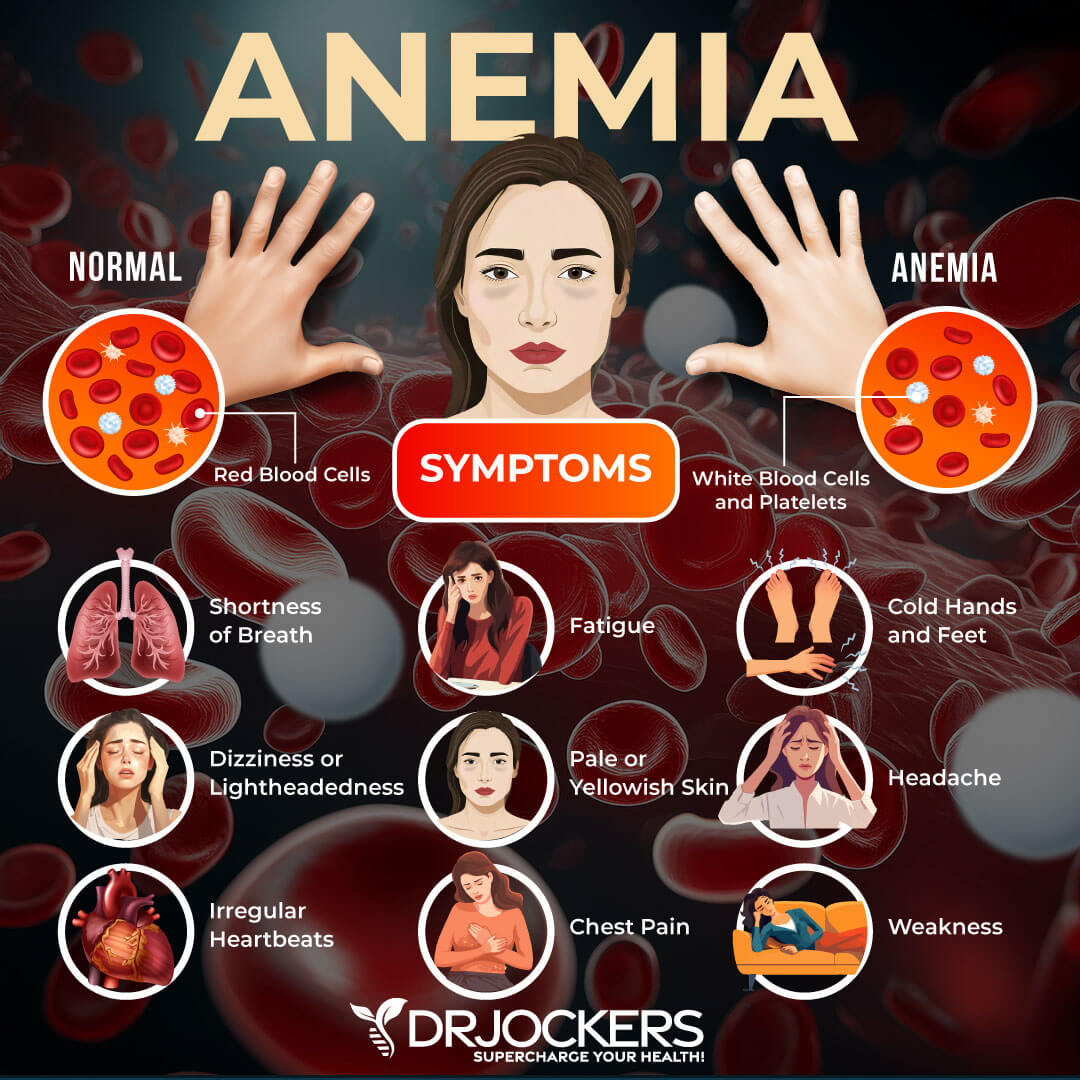
A complete blood count (CBC) is not just one test but a group of tests. It is used to evaluate the cells that circulate inside your blood, such as your red blood cells (RBCs), white blood cells (WBCs), and platelets (PLTs), and detect infections and inflammation.
It can look at the mean corpuscular volume (MVC) levels, which measure the size of your blood cells, and check for your mean corpuscular hemoglobin concentration (MCHC) to measure the average concentration of hemoglobin in your red blood cells. Doing a complete blood count, I am looking for signs of anemia, including iron-deficient anemia and pernicious anemia. Low RBC, Hbg, high or low MCV, or MCHC may indicate these issues.
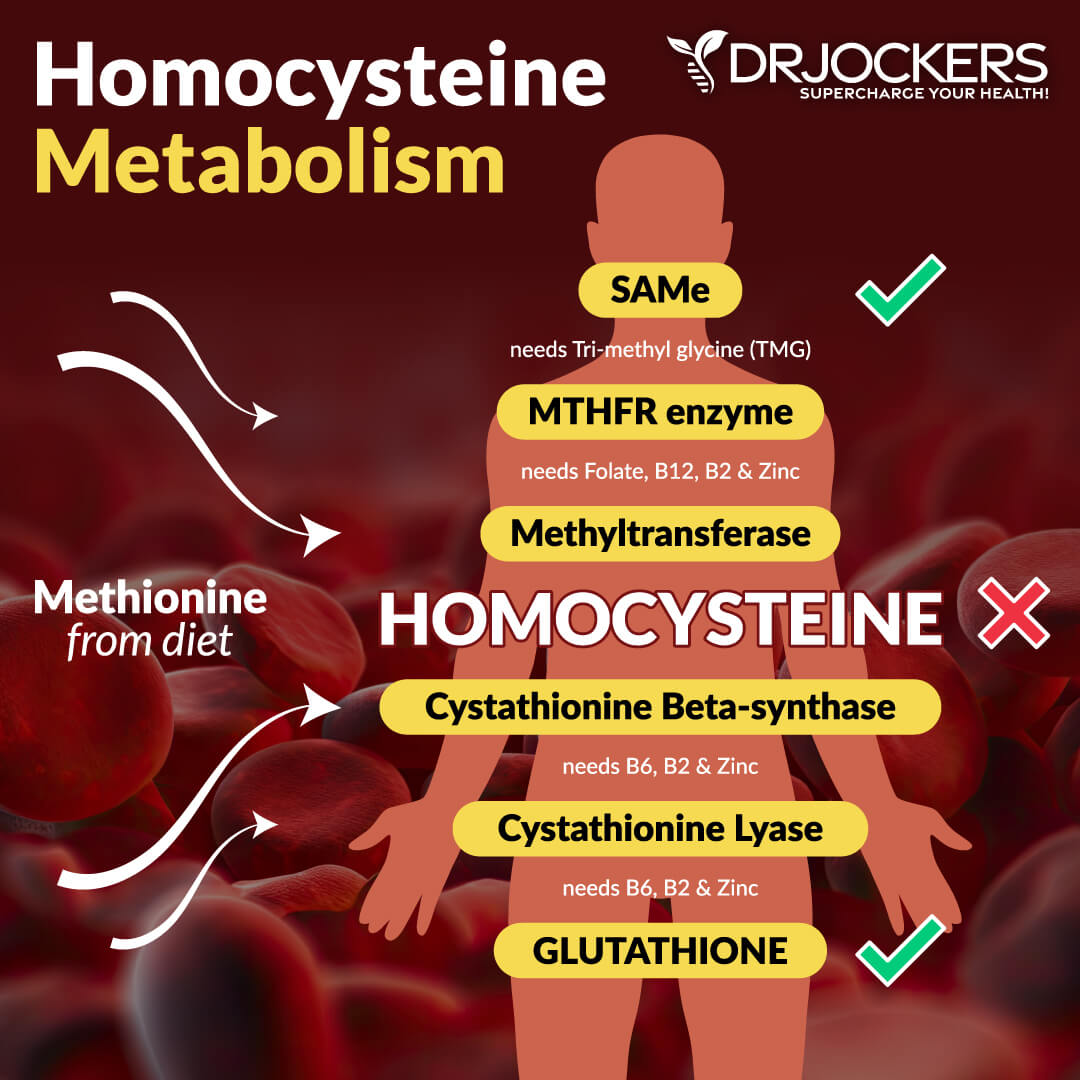
Serum B12 and Homocysteine
Vitamin B12 is a very common deficiency yet it is very important to keep your body’s nerves and your blood cells healthy. The ideal range is 800-1500pg/mL.
Homocysteine is a common amino acid in your blood that you mostly get from eating meat. Homocysteine is particularly a good marker for cardiovascular issues. The optimal range for homocysteine is between 6 and 9 umol/L. Some practitioners like to see it under 8 umol/L.
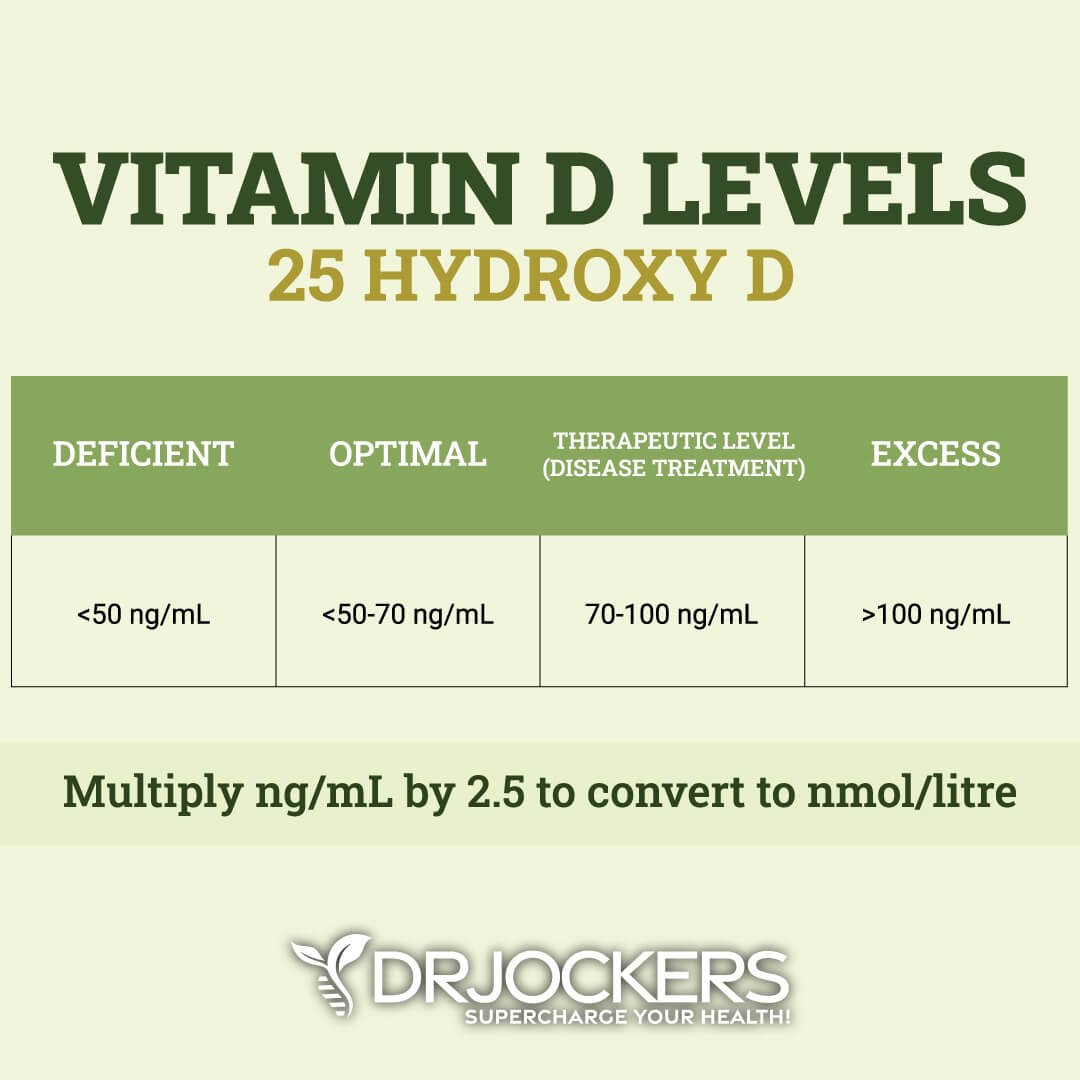
Vitamin D and Plasma Zinc
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. The ideal range of vitamin D is between 90-135 ug/dL.
Checking your plasma zinc levels is the best way to determine zinc levels in your body. Ideal plasma zinc levels are between 9 and 20 μmol.
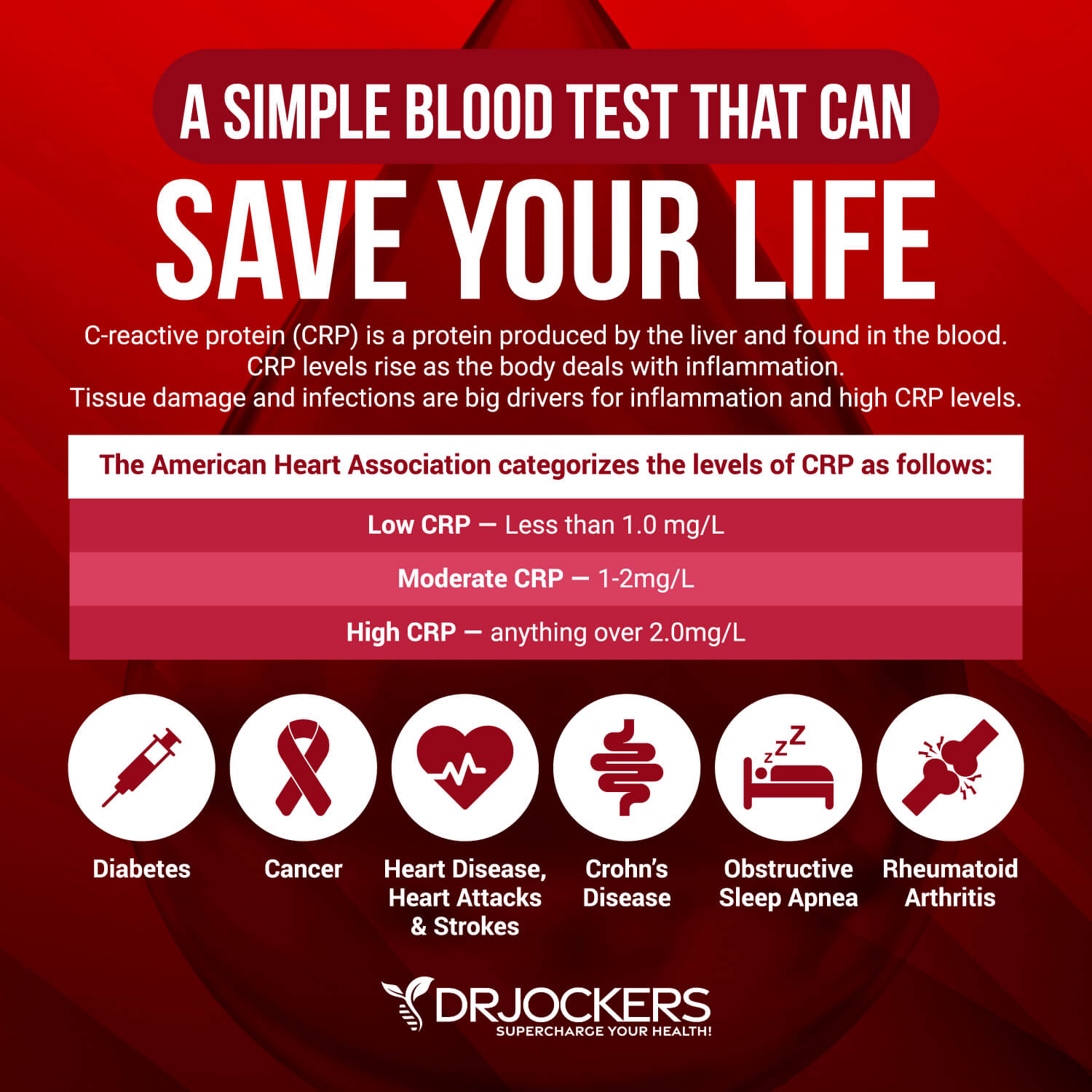
C Reactive Protein (Hs-CRP)
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L.
When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions. Ideally, we want to see the CRP levels as low as possible, certainly under 1 mg/L and more like .01 mg/L.
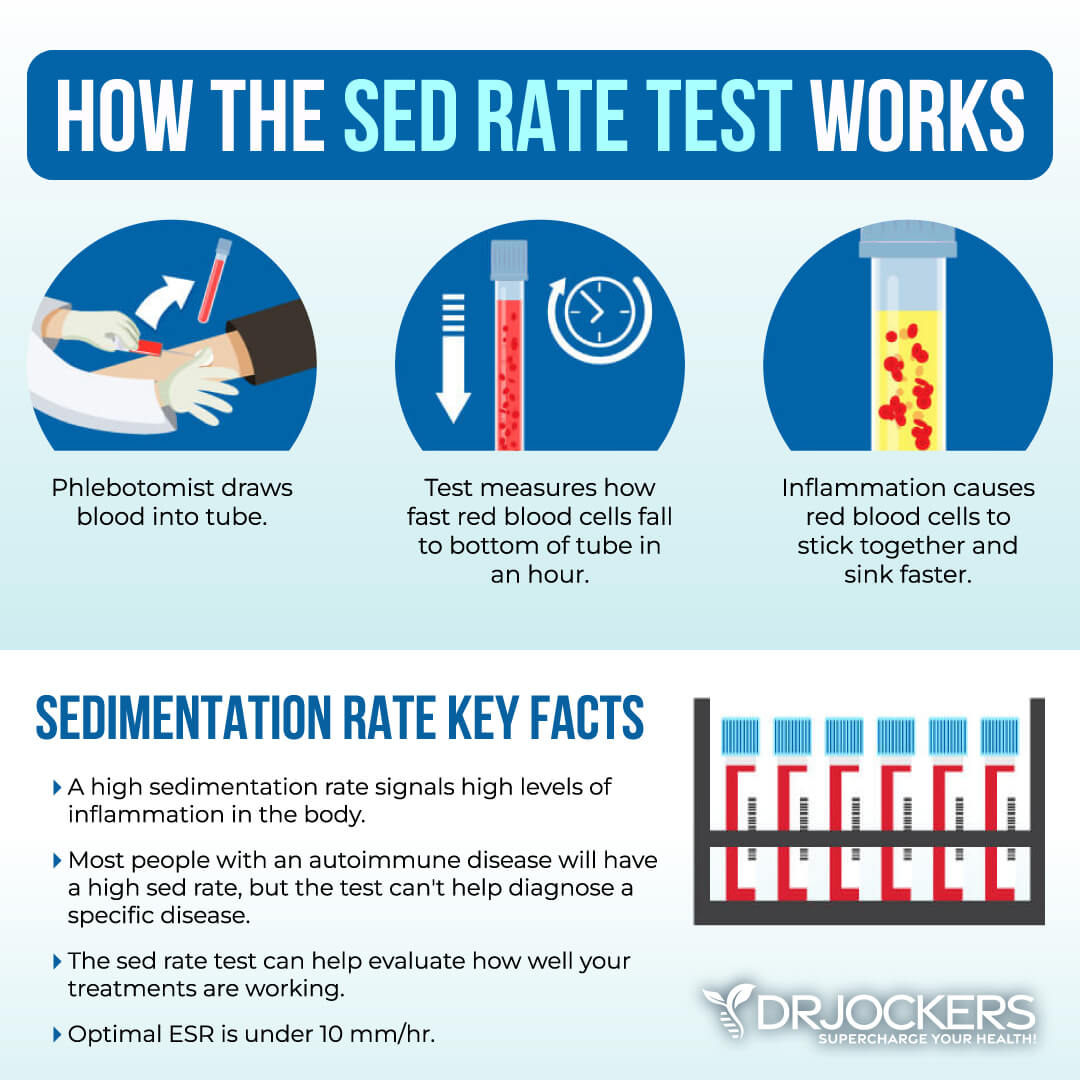
ESR
The erythrocyte sedimentation rate (ESR) is a common hematology test to look for inflammation It refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Optimal ESR rates for women under 50 are between 0 and 20 mm/hr, men under 50 are between 0 and 15 mm/hr, women over 50 are between 0 and 30 mm/hr, men over 50 are between 0 and 20 mm/hr, and children between 0 and 10 mm/hr.
You can also look at platelets as a measurement tool for inflammation and the stickiness of blood. Platelets elevated above 250 is a sign of inflammation. The sweet spot for platelets is between 175 and 250. Below 175, immune function and blood clotting are compromised; the same is true for levels above 250.
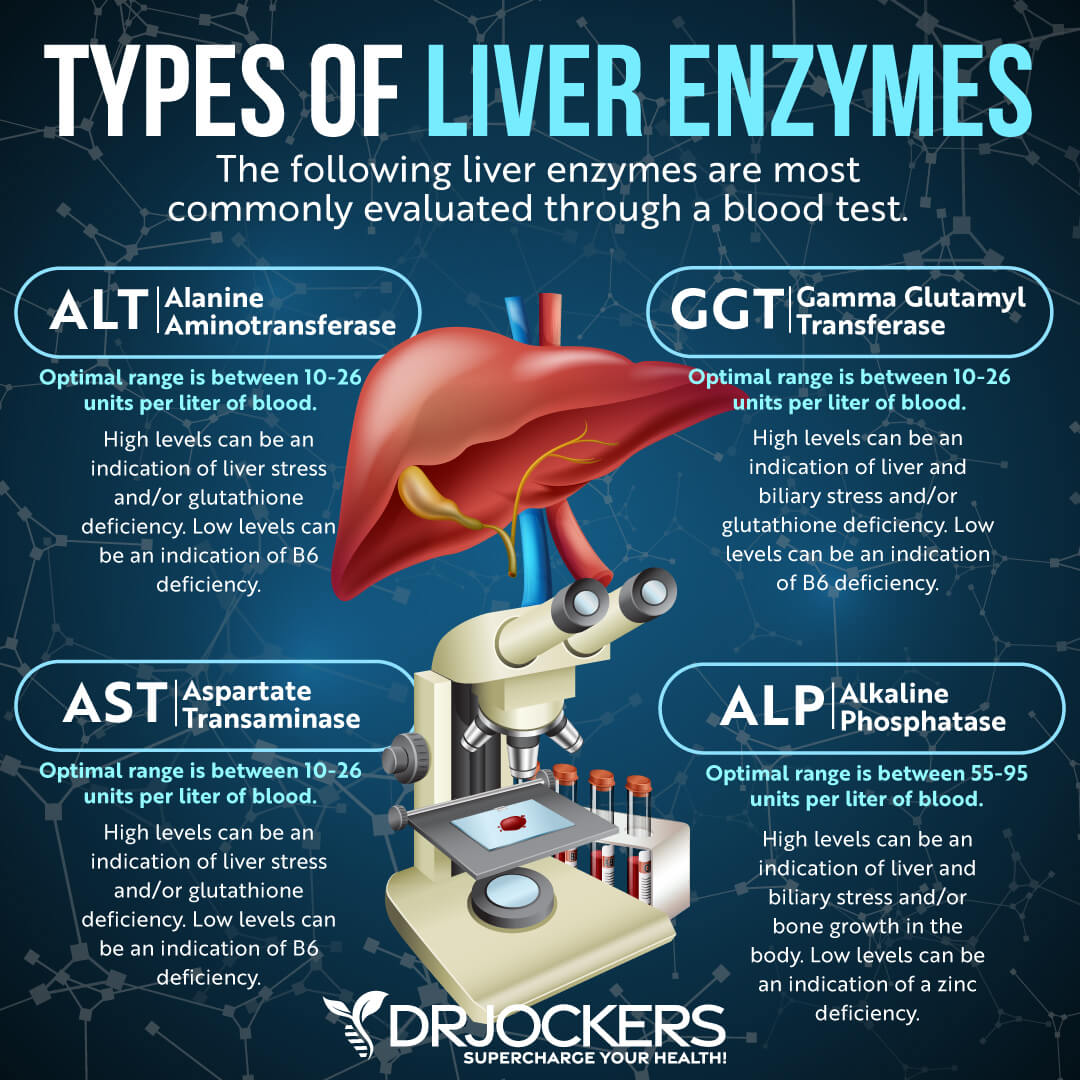
Liver Enzymes
Liver enzyme levels are often high in gastritis, especially associated with NSAID or alcohol abuse. Liver enzyme levels may also indicate inflammation, as well as liver, gallbladder, bile, or kidney issues. Elevated levels (over 95) may indicate inflammation and liver and gallbladder problems.
Alanine aminotransferase (ALT) is a liver enzyme. Elevated levels may indicate inflammation. Normal levels are between 10 and 26 IU/L.
Aspartate transaminase (AST) is an enzyme present in the liver that spills out during times of increased liver stress. Elevated levels may indicate inflammation Normal levels are between 10 and 26 IU/L.
Gamma-Glutamyl Transpeptidase (GGT) is an enzyme in the liver, pancreas, and kidneys. Elevated levels may indicate inflammation and liver disease, usually due to alcoholism and/or sluggish gallbladder or gallstone obstruction. Normal levels are between 10 and 26 IU/L. Levels lower than 10 IU/L can be an indication of a vitamin B6 deficiency.
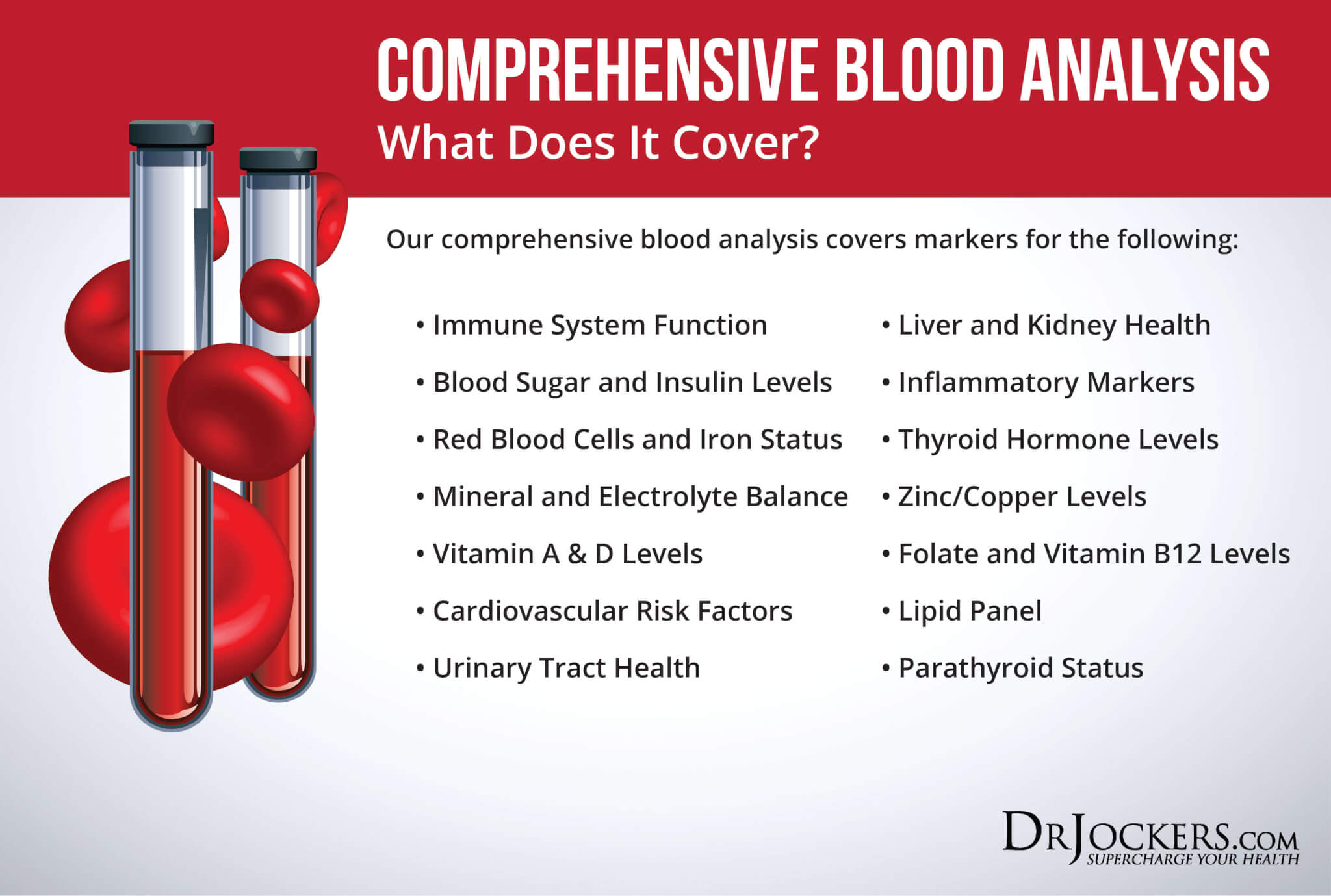
Comprehensive Blood Analysis
To check for these health markers, I recommend a Comprehensive Blood Analysis (CBA). This is the most detailed blood test that looks at all of these markers of inflammation.
This test is more sophisticated than most conventional doctors are able to order. It examines all parameters for inflammation, blood sugar levels, thyroid function, zinc and copper ratio, vitamin A and D levels, a complete metabolic panel, complete blood count, liver function, nutrient deficiencies, and more.
Natural Support Strategies
If you have or are at risk of gastritis, there are a number of natural support strategies you can try. Here is what I recommend to improve your health and well-being:
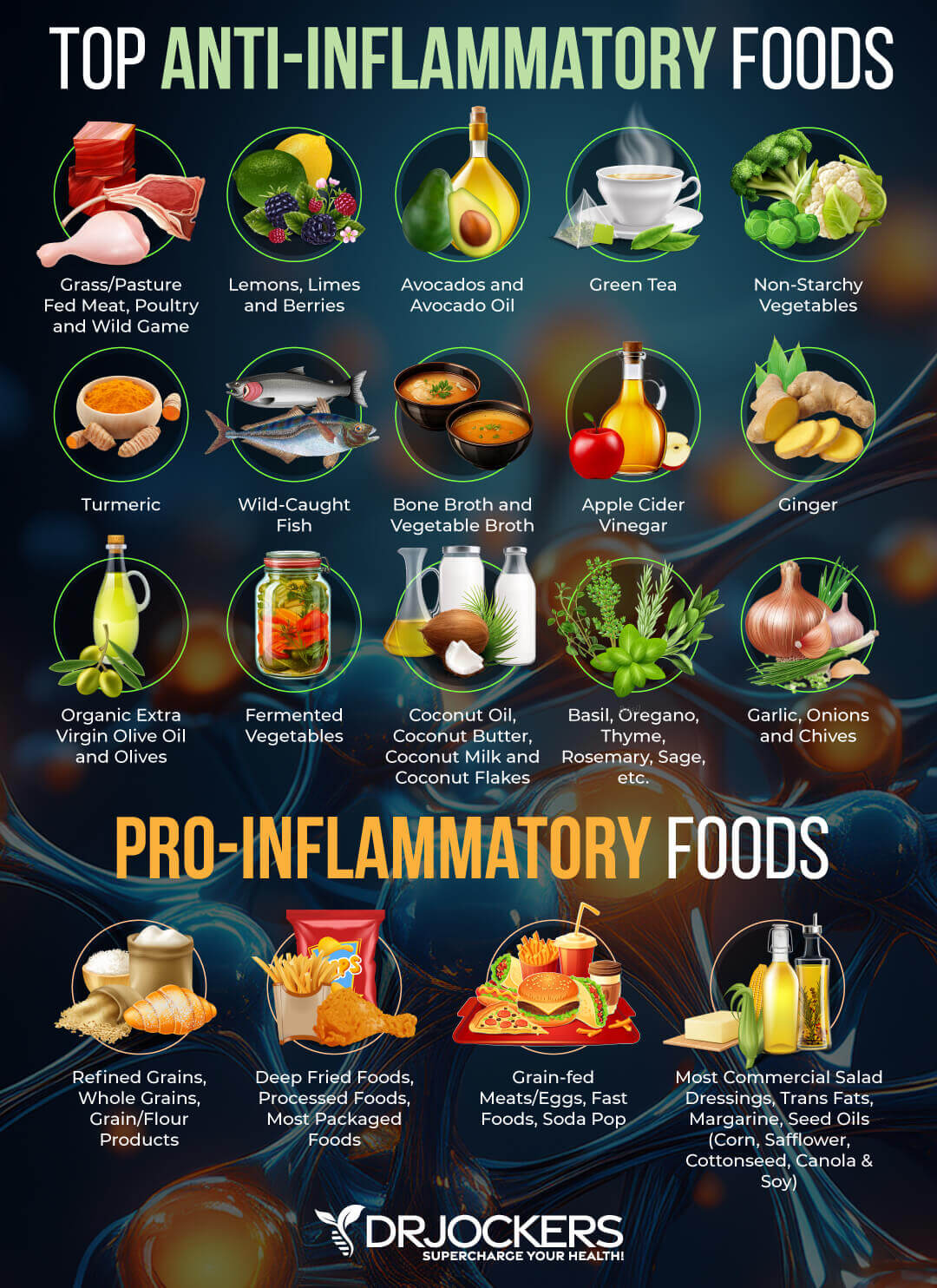
Anti-Inflammatory Nutrition Plan
Gastritis is an inflammatory condition and following an anti-inflammatory nutrition plan can help. Certain inflammatory foods, including acidic, spicy, and hot foods, processed or packaged foods, alcohol, and caffeine can trigger inflammation and gastritis symptoms, while other foods, including high-fiber foods, antioxidant-rich food, electrolytes, and omega-3 fatty acids may help to reduce symptoms (12).
Remove any foods that may be triggering, including acidic, spicy, hot, processed, and packaged foods. Remove other inflammatory foods, such as refined sugar, refined oil, deep-fried foods, conventional dairy, processed meat, gluten, and artificial ingredients.
Load up on antioxidant-rich foods, including greens, vegetables, herbs, low-glycemic index fruits, and healthy fats such as avocados and olive oil. Get quality protein from grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
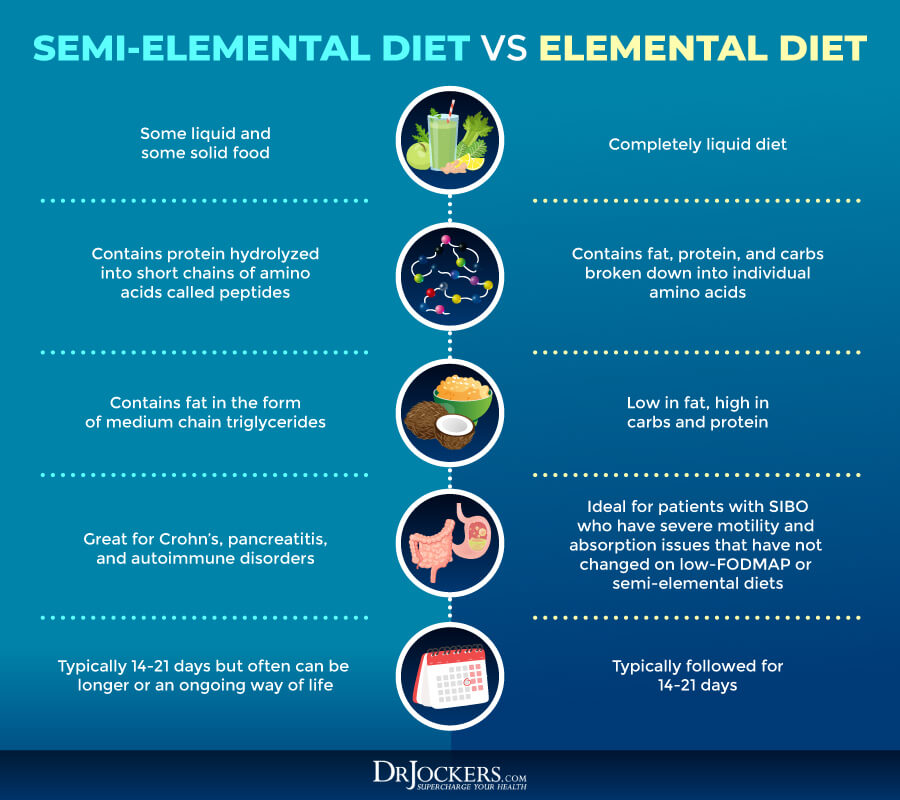
Consider a Liquid or Elemental Diet
If you already have a stomach ulcer as a result of gastritis, an elemental diet may help. The elemental diet is a diet using nutritional formulas with pre-digested foods. These powders include vitamins, minerals, and complete macronutrients, and are used to replace all or some of your meals.
The elemental diet or a semi-elemental diet is used for SIBO, Crohn’s disease, and eosinophilic esophagitis. According to a 2004 study published in Digestive Diseases and Sciences, a 14-day elemental diet can improve gut flora (23). I only recommend this diet short-term and with the guidance of your healthcare professional.
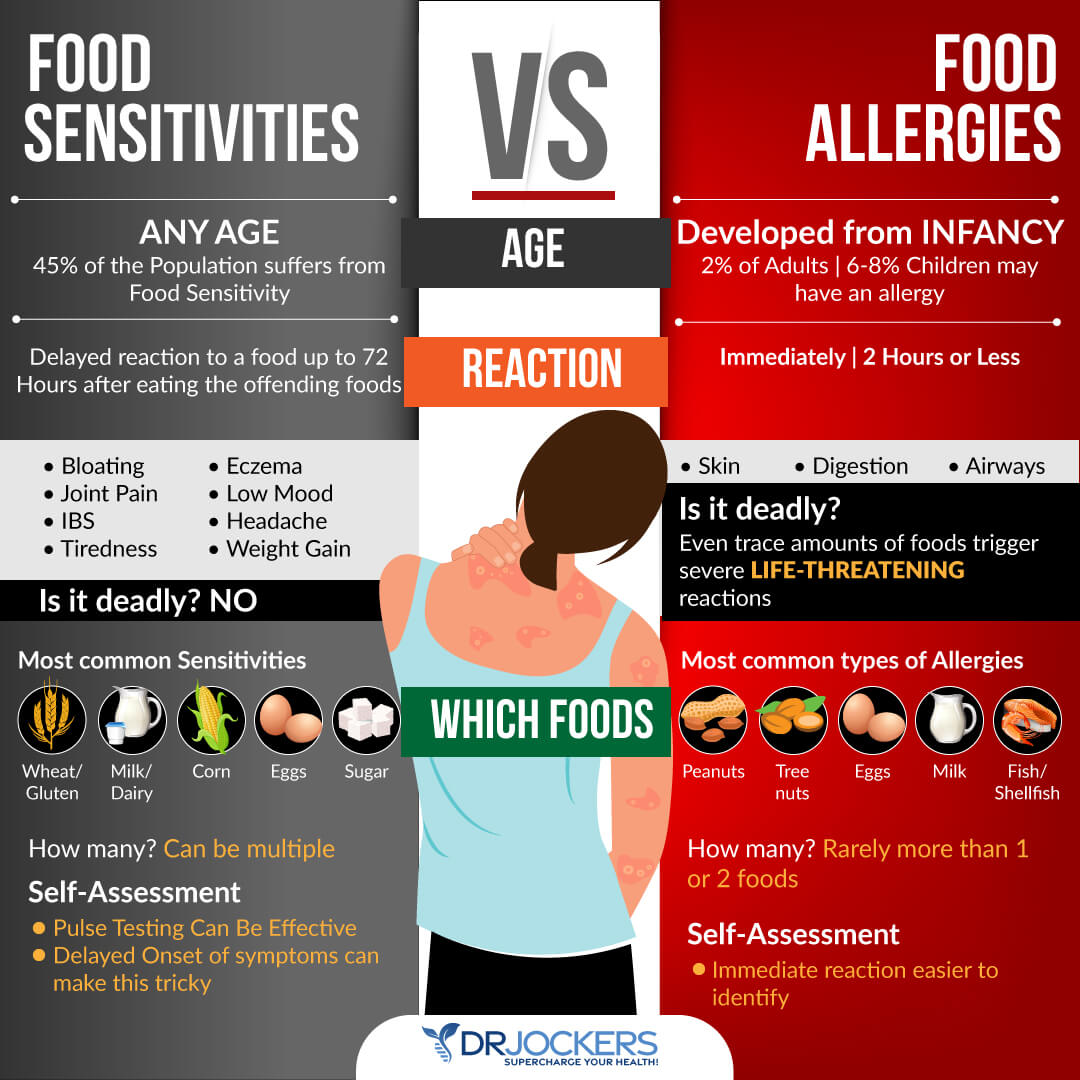
Test For and Remove Food Sensitivities
According to a 2000 comparative study published in Medicine Science Monitor, there may be a connection between H pylori infection and food allergies in chronic gastritis (24). Food sensitivities can be just as triggering for symptoms of gastritis as food allergies. Food sensitivities are different from food allergies.
Food allergies cause an immediate reaction in your body, such as hives, difficulty breathing, puffiness, digestive issues, or other symptoms after eating a food that you are allergic to. Food sensitivities, on the other hand, don’t result in an immediate reaction but cause issues over time. You may eat food and only experience symptoms a few hours or days later and inflammation and internal damage may also occur over a period of weeks, months, or even years.
Testing for food sensitivities and removing them is critical. There are various blood tests that can help identify food sensitivities, however, they don’t test for every food, and false results can also happen. Additionally, I also recommend that you try an elimination diet, pulse test, or muscle response testing.
Once you find your sensitivities, it is important that you immediately remove them from your diet. Since food sensitivities can change over time, I recommend that you test for them regularly, at least once a year, or if new symptoms occur.
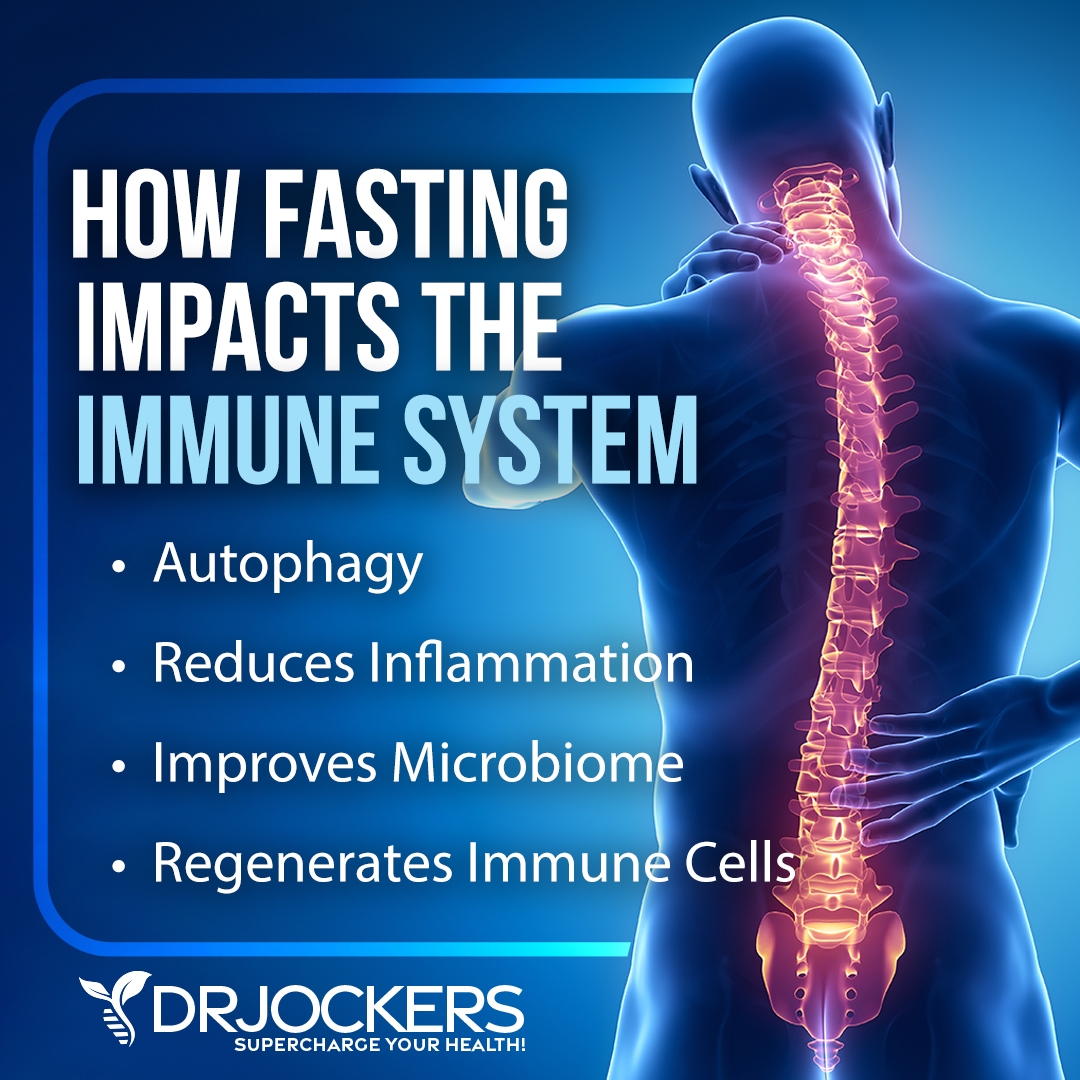
Intermittent Fasting
Intermittent fasting is a type of fasting cycle between not eating (fasting) and eating (feasting) over a period of time. According to a 2019 study published in the Turkish Journal of Gastroenterology, intermittent fasting helps to improve your microbiome diversity and support your good flora (25). It also allows cellular repair, increased autophagy, immune regulation, decreased, inflammation levels, lower inflammation, and better insulin sensitivity.
If you are new to intermittent fasting, I recommend that you start with the Simple Fast. This means that you would be fasting for 12 hours a day including your overnight sleep. I recommend that you stop eating after dinner and don’t eat again until 12 hours later at breakfast. Increase your fasting window gradually until you reach your sweet spot. Most people find that 16 hours of fasting work best for them.
Reduce Stress & Improve Sleep
Since gastritis can be stress-induced, it is important that you lower your stress levels and improve your sleep (11). I recommend that you try meditation, breathwork, gratitude, journaling, and prayer. Spend time in nature and exercise regularly. Spend time with loved ones. Seek a community. But also make sure that you have regular me-time.
Avoid electronics, food, alcohol, sugar, and caffeine in the evening. Find relaxing activities that help you relax and wind down, such as board games, playing cards, supportive conversation, reading, taking a healing bath, sipping on herbal tea, meditation, journaling, or prayer. Make sure that your bedroom is a supportive sanctuary with a supportive mattress, comfortable pillows and bedding, and maybe an essential oil diffuser with some calming oils like lavender oil.

Minimize or Eliminate NSAIDs and Alcohol
Since the overuse of NSAIDs and alcohol abuse are some of the top causes of gastritis, it is important that you minimize or eliminate those (3, 6, 7, 8, 9). Follow an anti-inflammatory nutrition plan to reduce inflammation naturally and choose natural means to reduce pain, such as turmeric or ginger.
Drink no more than occasionally. If you are dealing with alcohol addiction or alcohol abuse, I recommend that you seek support and quit completely.
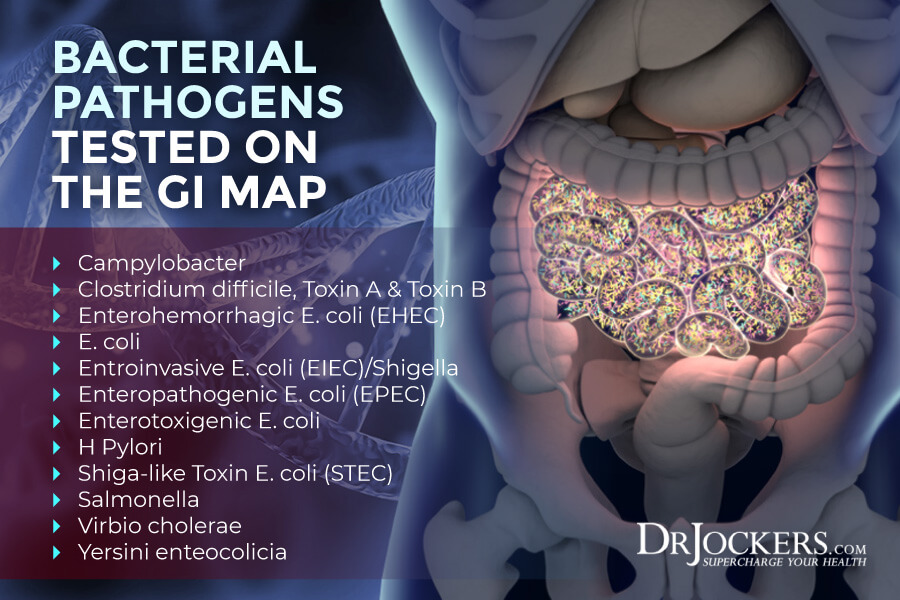
Test For and Address Gut Infections
Since H pylori overgrowth and other gut infections can cause and further worsen gastritis, it is important that you test for gut infections, including H pylori, other bad bacteria, viruses, Candida and other fungi, and parasites (5). To test for gut infections and understand your digestive health, I recommend a GI Map Stool Test for a comprehensive gut analysis.
Along with a gut-friendly, anti-inflammatory diet, I also recommend a variety of herbs to address gut infections, including:
- Mastic gum: A 2009 randomized plot study published in Phytomedicine, has found that mastic gum may help to reduce H pylori infection (26).
- Berberine: A 2020 systematic review and meta-analysis of randomized clinical trials published in Frontiers in Pharmacology has found that berberine therapy may help the eradication of H pylori (27).
- Sweet wormwood: A 2012 study published in Antimicrobial Agents in Chemotherapy has found that sweet wormwood has antimicrobial properties and may help to reduce H pylori overgrowth (28).
- Manuka honey: A 2006 study published in the Sultan Quaboos University Medical Journal has found that manuka honey has high antibacterial qualities that may be effective against H pylori overgrowth (29).
- Black walnut: A 2016 study published in Medicinal Chemical Research has found that black walnut has antibacterial and antifungal benefits and may be effective against H pylori (30).
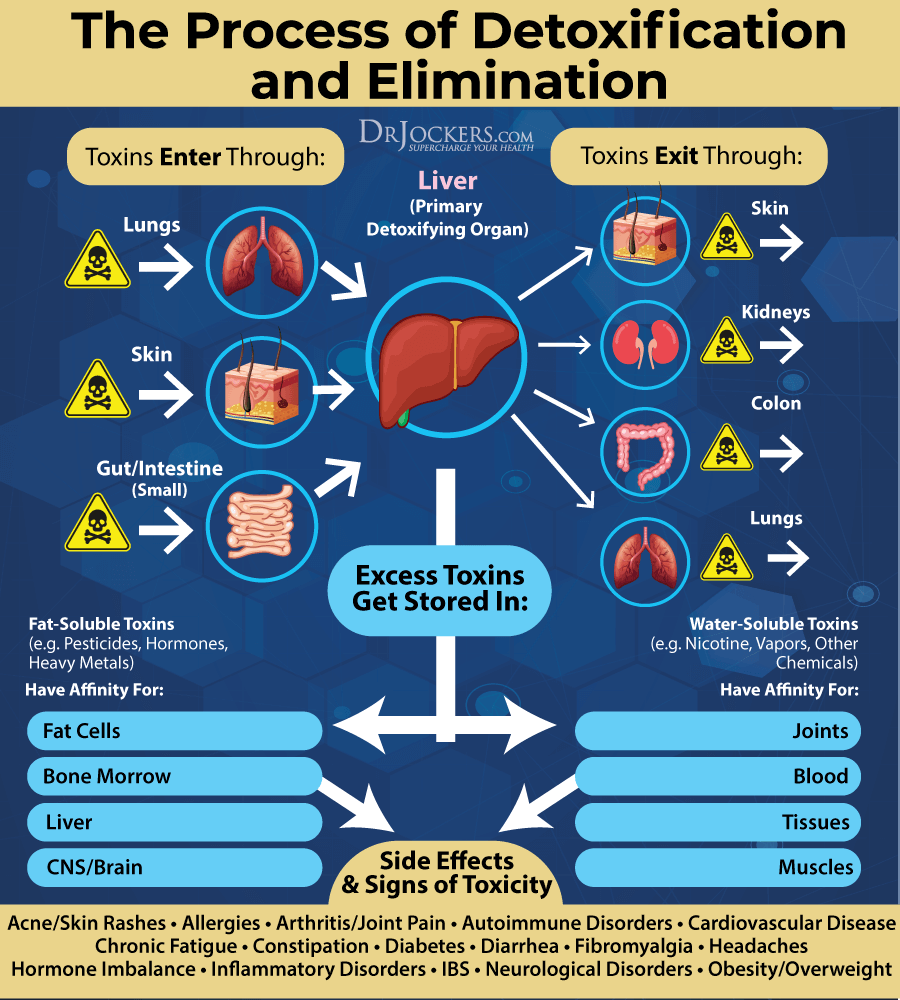
Open up Detoxification Pathways
Toxin overload in your body can increase the risk of H pylori overgrowth and other gut infections, gut inflammation, leaky gut syndrome, and autoimmunity that can all contribute to gastritis (1, 5). Opening up your detoxification pathways is critical.
A healthy gut function supports absorption, digestion, detoxification, and elimination. I recommend that you eat plenty of gut-supporting probiotic foods, such as kimchi, sauerkraut, and kefir, as well as prebiotic foods, such as Jerusalem artichokes, asparagus, and leek. Take daily probiotics as well and digestive enzymes to support digestion. Additionally, eat foods that support bile flow, including ginger, turmeric, celery, dandelion greens, radishes, milk thistle, cilantro, mint, cucumber, parsley, lemon, artichokes, apple cider vinegar, green tea, and sauerkraut.
Supporting your gut is important when it comes to gastritis, however, you can’t forget about your kidneys and liver either, especially when it comes to the detoxification and elimination of toxins and waste. Your liver is your primary detoxification organ. Your kidneys filter your blood to remove waste and support fluid balance.
Once a molecule is processed by your liver, it goes back into circulation to be removed via the bile in your intestines or your kidneys before being eliminated through feces. I recommend that you eat plenty of foods that support your kidneys and liver, including beets, grapefruit, green tea, garlic, spinach, broccoli, turmeric, citrus, avocado, cabbage, berries, and olive oil. Additionally, take a kidney and liver support supplement.
To further support detoxification, I recommend that you support your lymphatic pathways and encourage lymph flow. Rebounding is a great way to help that. Dry brushing your skin daily before your shower with a soft, natural brush is another good way to improve lymphatic flow. Make sure to always brush towards your heart. Lastly, exercise and infrared sauna use can also support detoxification through the skin by encouraging sweating.
Use Herbs to Calm Inflammation
There are various herbs that you can also use to calm inflammation. Here is what I recommend:
Turmeric Tea and Curcumin Supplementation
Turmeric is one of the most well-researched herbs for inflammation and pain. It is often used for digestive issues. The powers of turmeric come from its active ingredient, curcumin.
A 2019 study published in the International Journal of Molecular Sciences has found that curcumin may be beneficial for esophageal and gastric disorders, including H pylori infections, acid reflux, gastritis, peptic ulcers, and gastric mucosal damage (31). I recommend that you drink turmeric tea regularly and use curcumin supplements to calm inflammation.
Ginger Tea, Pickled Ginger, and Ginger Supplementation
Ginger is another powerful herb that is similar to turmeric. The two are often used together, but ginger is powerful alone for inflammation, pain, and digestive issues.
According to a 2018 systematic review of clinical trials published in Food Science & Nutrition, ginger is beneficial for gastrointestinal disorders because of its anti-inflammatory, antimicrobial, and anti-ulcer activities (32). I recommend that you drink ginger tea, eat pickled ginger, and use ginger supplementation to reduce inflammation.

Chamomile Tea or Supplementation
Chamomile tea is an herb that comes from daisy-like flowers and is often used as a tea for relaxation, sleep, inflammation, and pain. A 2014 study in the Journal of Ethnopharmacology has found that it can be beneficial for H pylori infections, gastritis, and anti-gastric cancer (33).
I recommend that you try drinking chamomile tea or use chamomile supplements for inflammation. You can find chamomile in many tea blends that are marketed for digestive support and for sleep and relaxation.

Aloe Vera
Aloe vera is a plant that’s native to North Africa, the Canary Islands, and Southern Europe, but today it’s grown in tropical and warmer climates or even indoors in your home. It is often used for wound healing and sunburns topically and for digestive issues internally.
A 2016 study published in the Iranian Journal of Medical Sciences has found that aloe vera gel may be more effective for chronic ulcers than conventional treatments (34). A 2014 animal study published in the World Journal of Gastroenterology has found aloe vera to be effective for gastric injury and gastropathy (35). You can add aloe vera to your juices and smoothies or try aloe vera supplements for inflammation.

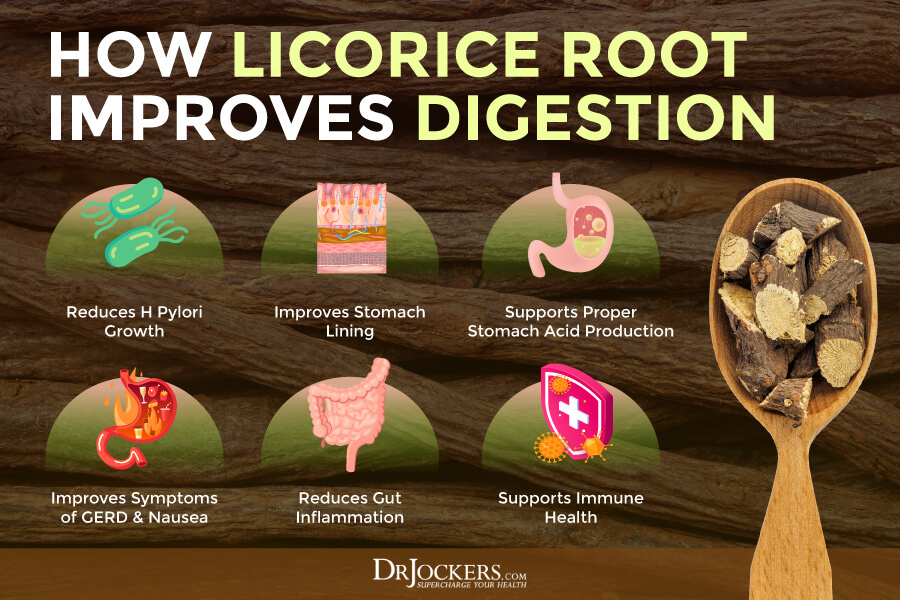
Licorice Root
Licorice root may be a popular flavoring in some candy, but it’s also a powerful herbal medicine used for inflammation, digestion, ulcers, and respiratory infection. Licorice is known to improve the production of the mucous membrane that protects the stomach lining and it also helps to reduce H Pylori levels.
A 2014 study published in Pharmacognosy Research has found that licorice root may help to eradicate H pylori infection and help with gastritis and ulcers (36). I recommend that you use licorice root DGL form supplementation for inflammation and gut health.
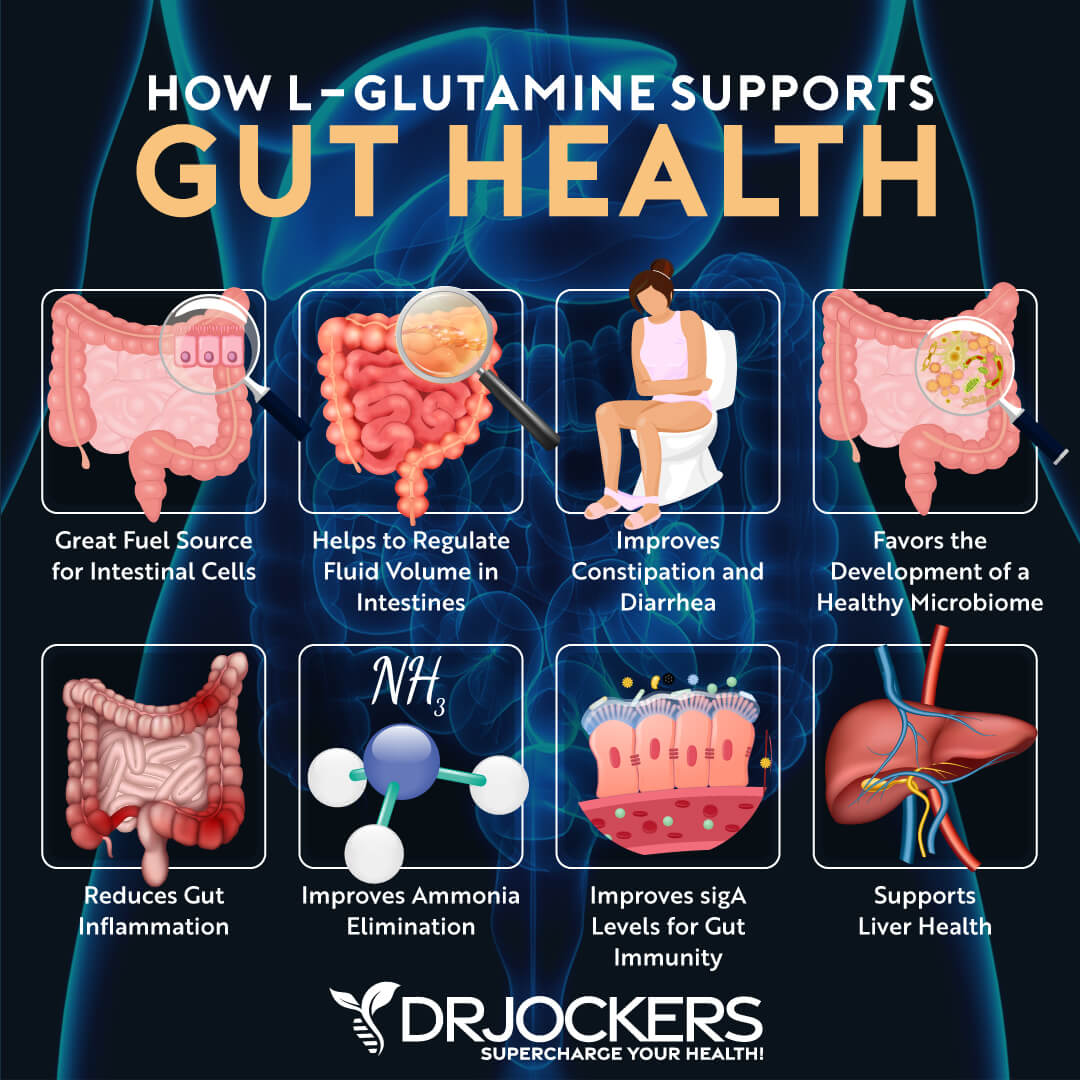
L-Glutamine
L-glutamine is an important amino acid for muscle health, gut health, and fat burning. It can help blood flow in the gut and support recovery and gut health. It is the primary nutrient for the cells of the intestinal lining where it helps regulate cellular reproduction. Through this mechanism, glutamine helps prevent damage to the stomach and intestinal lining and rebuild areas that are damaged.
A 2017 study published in the Asian Journal of Pharmaceutical and Clinical Research has found that L-glutamine can help to reduce H pylori infection which can help with gastritis (37). I recommend that you take L-glutamine supplements for gut health.
Address Key Nutrients
In addition to herbal supplementation for inflammation, it is important that you address key nutrient deficiencies that may cause gastritis or may occur because of gastritis. Here is what I recommend:
Zinc
A 2005 study published in the Journal of Infection has found that short-term zinc supplementation is effective for gastritis (38). According to a 2010 study published in Collegicum Antropologicum, zinc may reduce inflammation, gastric mucosa damage, and oxidative stress in gastritis (39).
Foods that are rich in zinc include grass-fed meat, pasture-raised poultry, beans, nuts, and some seafood. Additionally, to zinc-rich foods, I recommend taking Zinc Carnosine form, which according to a 2020 study published in Nutrients is incredibly effective for gastrointestinal disorders (40).
Vitamin D
A 2016 study published in BMC Gastroenterology has found that vitamin D3 can help with oxidative injury and acid in gastritis (41). To improve your vitamin D levels, I recommend spending time outside in the sun every day when it’s possible and eating foods that are rich in vitamin D, including liver, oily fish (wild-caught only), grass-fed red meat, and egg yolks.
Meeting your needs through a little sunshine and diet alone is difficult for most, so I recommend that you take a daily vitamin D3 supplement with vitamin K2. Vitamin K2 helps the absorption of vitamin D and calcium in the bloodstream.
Typically taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml.
Vitamin C
A 2018 review published in Frontiers in Physiology has found that vitamin C can help to fight H pylori infections that may benefit those with gastritis (42). I recommend that you eat plenty of foods that are rich in vitamin C, including citrus, strawberries, black currants, peppers, broccoli, and Brussels sprouts.
Unfortunately, many of these foods actually aggravate gastritis symptoms as they are acidic and can drive up more inflammation if the stomach lining is already weak and inflamed. Therefore, it can be important to instead take a vitamin C supplement that you are able to tolerate.

Vitamin B12
A 2005 study published in the World Journal of Gastroenterology has found that vitamin B12 deficiency is common in those with gastritis and gastric issues (43). A 2016 study published in Wien Medizinische Wochenschrift has found that a deficiency in vitamin B12 can contribute to autoimmune gastritis (44).
Even though some animal products may contain some vitamin B12, meeting your needs through food alone is nearly impossible even if you are consuming animal-sourced foods. I recommend that you take a daily vitamin B12 supplement. I recommend the methylcobalamin form of B12 since it is the most bioactive form.
Iron
A 2009 study published in Acta Hematology has found that iron deficiency and iron-deficiency anemia (IDA) is very common among people with H pylori infections and autoimmune gastritis (45). Since too much iron can become a problem as well, I recommend that you first get your iron level tested and check for anemia.
If you are deficient in iron, I recommend supplementation. Additionally, I recommend eating an iron-rich diet with grass-fed red meat, pasture-raised poultry, wild-caught seafood, and dark leafy greens.
Glutathione
Using NSAIDs can deplete glutathione levels and contribute to problems with the gut lining and gastritis (8, 9). A 1995 study published in Research Communications in Molecular Pathology and Pharmacology has found that glutathione can support the gastric mucosa and benefit people with gastric ulcers (46).
A 2016 study published in Science Reports has found that oral supplementation with glutathione can lower H pylori levels and improve gastric pathologies (47). Foods that are rich in glutathione include avocados, okra, asparagus, and spinach. I also recommend daily supplementation with glutathione.

Final Thoughts
Gastritis is a gut condition characterized by inflammation of the stomach lining that can cause abdominal pain, bloating, nausea, vomiting, feeling of fullness, loss of appetite, and weight loss. Untreated and serious chronic gastritis can lead to long-term damage and stomach ulcers. I recommend that you try my natural support strategies to support your body and improve your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.

Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




Thanks for this educative article. Let me follow and hope my gut will be healed in Jesus name