 GI MAP Interpretation: Discover The Health of Your Microbiome
GI MAP Interpretation: Discover The Health of Your Microbiome
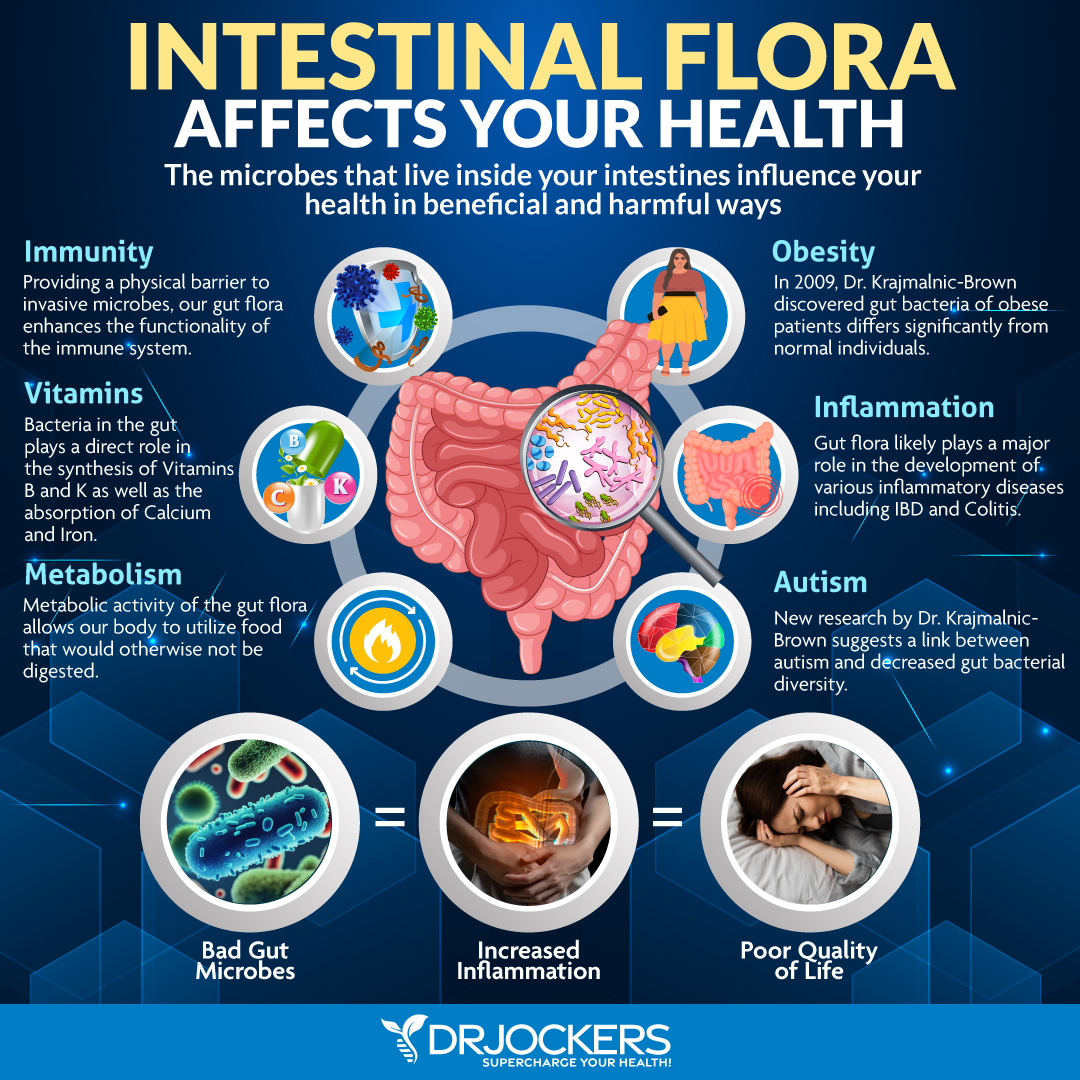
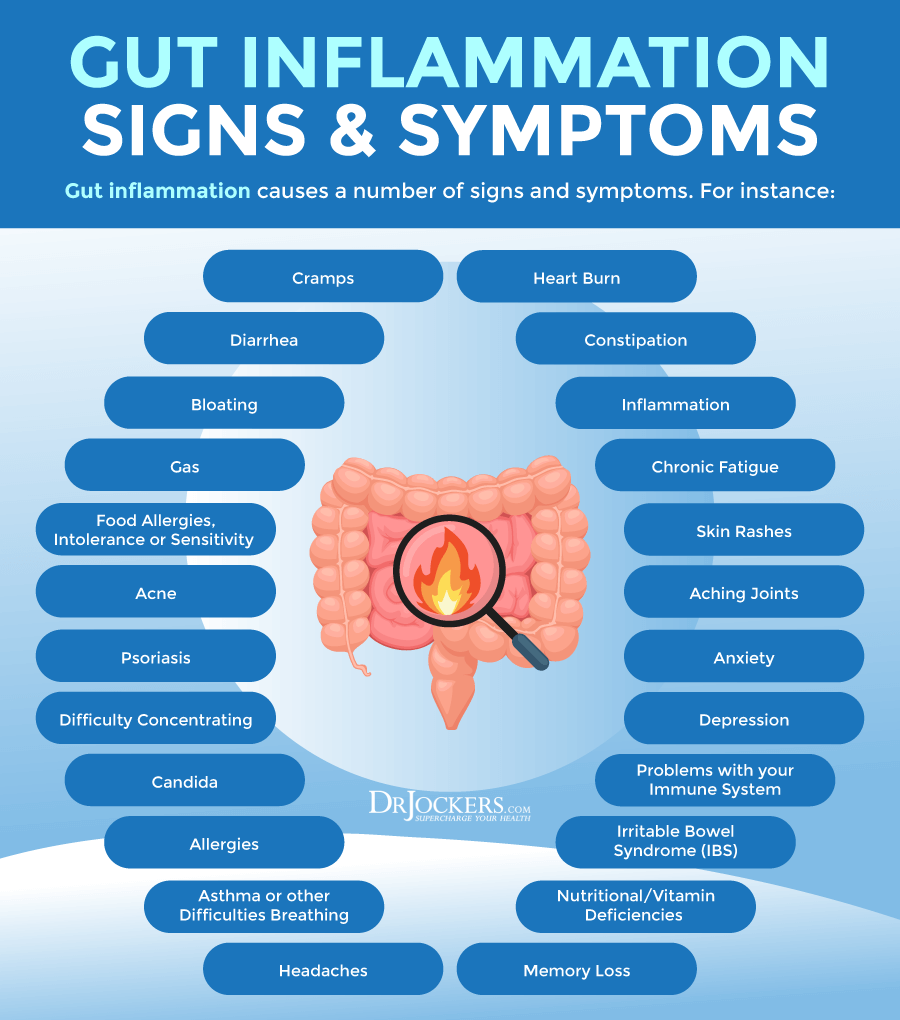
Your gut health plays an enormous role in your health. It is more than just digestion. Your gut is connected to everything. Your microbiome health is connected to your immune system, metabolism, mental health, and other areas. Imbalance in your microbiome and various pathogen overgrowth may contribute to the development of chronic symptoms, autoimmune, and other chronic health issues.
In this article, you will learn about the importance of your microbiome. I will go over the GI Map Stool Analysis in detail. This is the best and most comprehensive gut test I have found. It helps to identify bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora, potential autoimmune triggers, and all intestinal health markers.
What is the GI MAP Test
If you are experiencing unwanted symptoms or health issues, it is important to look at your gut microbiome health to uncover some of the root causes of your problems. Even if you are feeling great, a gut test can identify hidden problems, and allow you to course-correct and prevent future health issues. This is exactly why I love and recommend the GI Map Stool Analysis.
This test takes the guesswork out of your treatment. The GI Map Stool Analysis is a great tool that allows me to identify the root cause of my patients’ health issues and help them to repair their bodies and regain their health naturally. Today, I will go over this test in detail. You will learn what markers it is looking at and why it’s so important.
Importance of The Microbiome
When you think about your gut health, the first thing that probably comes to mind is digestion. But your gut has a much bigger role than simply digesting your food. It plays a role in your metabolism, immune system health, mental health, and all areas of your physical health. If your gut health is compromised, it will reflect on the health of the rest of your body.
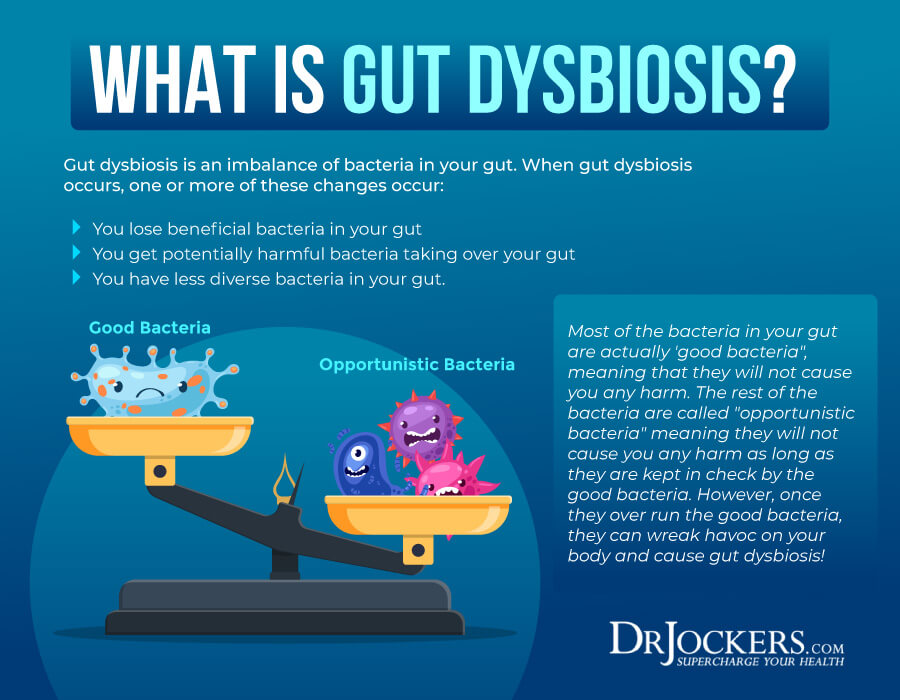
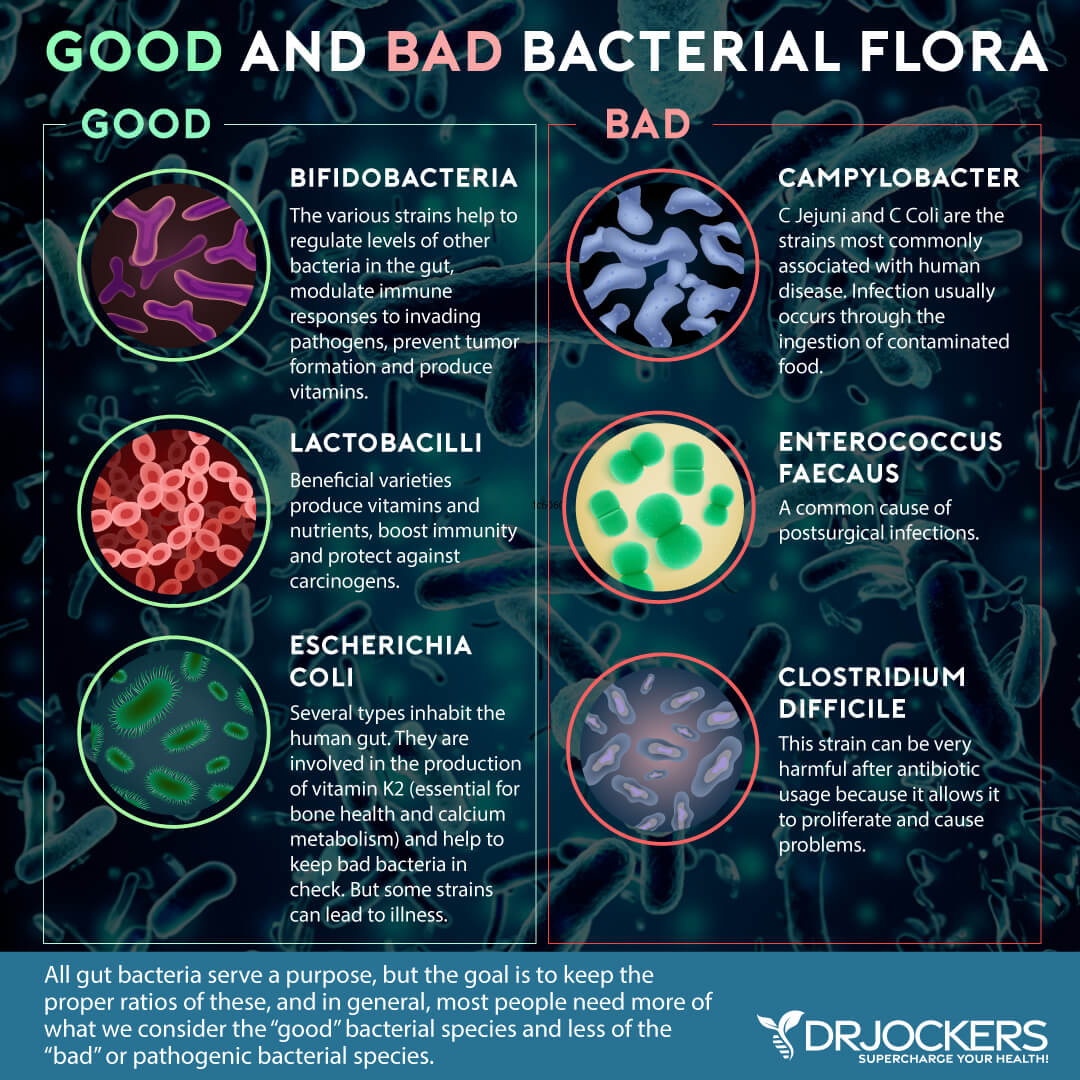
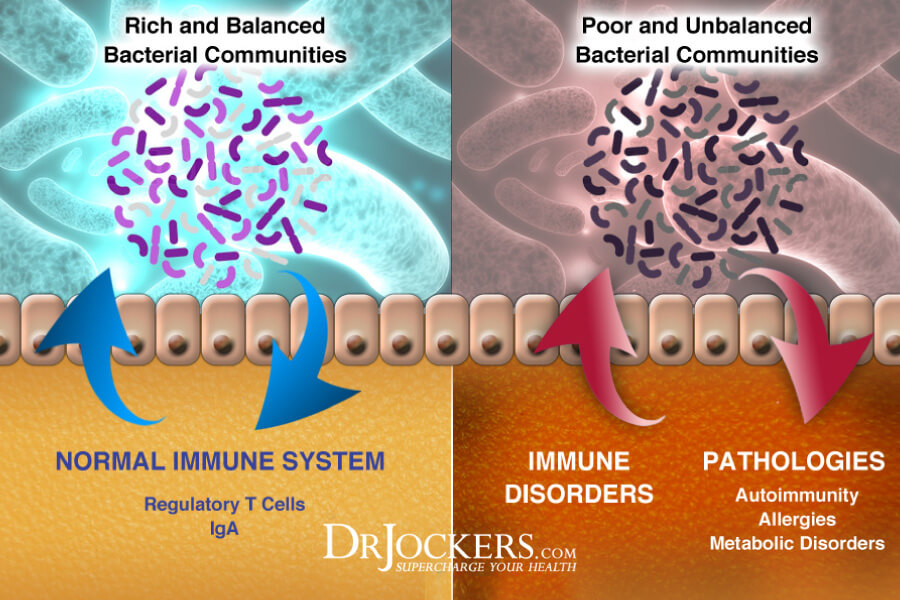
Your gut is filled with a diverse community of different types of bacteria. This is called your microbiome. Your microbiome plays an essential role in your health. If you have a healthy microbiome with good diversity and proper balance and filled with plenty of beneficial bacteria, it will provide a healthy base for the rest of your body and health.
However, if your gut microbiome is not diverse enough, there are too many bad and harmful bacteria and other pathogens, and there is a lack of healthy gut flora balance, it will increase your risk of inflammation and health issues, including autoimmune and inflammatory disease.
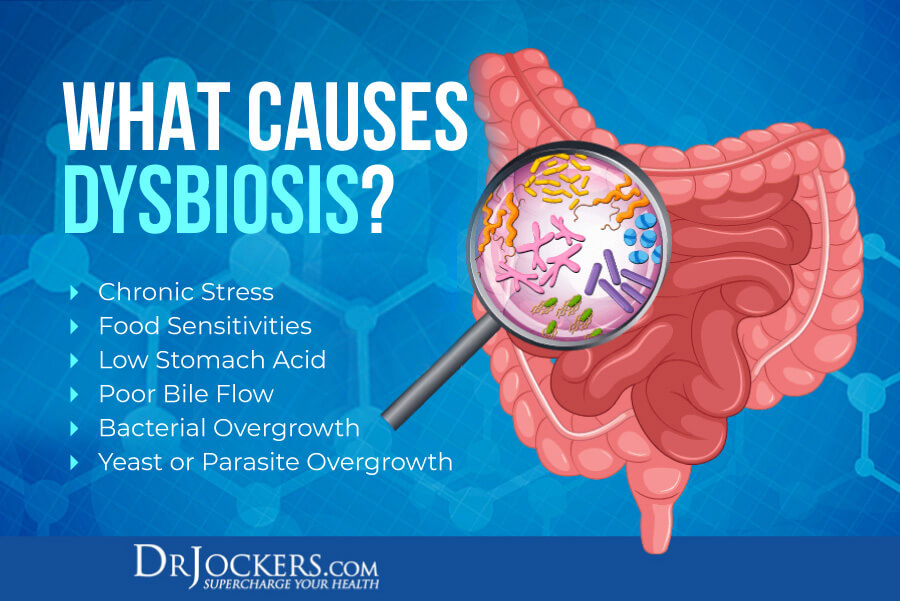
How Do We Develop Dysbiosis?
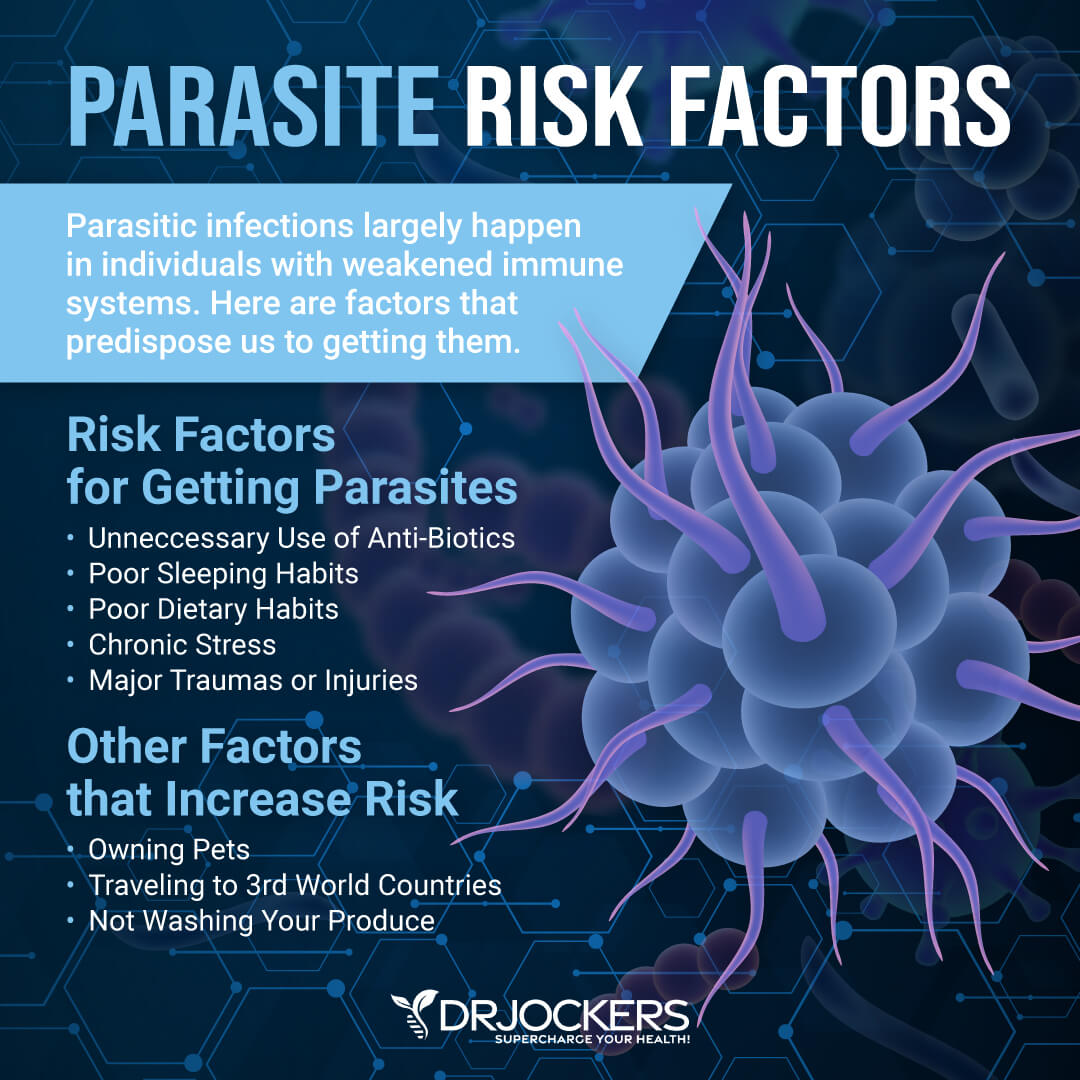
A poor diet low in nutrient-dense whole foods and high in inflammatory, processed, and artificial foods, a poor lifestyle, including poor sleep, poor hydration, a lack of exercise, and high stress, and high toxin exposure can compromise your gut microbiome.
Food sensitivities, poor stomach acid, poor bile flow, and bacterial, fungal and parasitic overgrowth can all lead to gut dysbiosis. Testing your gut microbiome health, identifying pathogen overgrowth, intestinal health markers, and underlying health issues, and making appropriate dietary and lifestyle changes is critical for recreating gut microbiome balance and improving your health.
What Is the GI MAP
My favorite test to look at your gut health and identify bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora, potential autoimmune triggers, and all intestinal health markers is the GI Map Stool Analysis. This is the best and most comprehensive gut test I have found and it helps me tremendously to identify the root cause of my patients’ health issues and help them to repair their body and regain their health naturally.
Most medically trained conventional GI doctors pay little to no attention to diet and lifestyle factors and their impact on your gut health. They look at drugs and surgeries as the first step in addressing digestive problems instead of as the very last resort.
While many natural and holistic health doctors offer probiotics and herbs to improve your gut microbiome, without proper testing, they can’t know if these suggestions are truly the right ones and won’t be able to see the actual effects of these probiotics and herbs on one’s unique terrain and the gut microbiome.
The GI Map Stool Analysis is a comprehensive stool test that looks at all major factors of your gut health and helps us identify what compounds will work best for eliminating the various pathogenic microorganisms that may be causing your symptoms. This takes the guesswork out of the process and also helps to see your true progress.
I have found that the GI map is the most thorough stool test with actionable biomarkers. There are other complex stool tests that may give some interesting information, but often not clinically relevant ones.
Other tests may also show false negatives or are more confusing to understand. This test offers everything that I, as a natural health doctor, need to see to make good clinical decisions and offer a treatment protocol that can help to improve your gut microbiome and your overall health.
As a natural health doctor, I believe that your recovery and health is a collaborative effort between us. It is important that you understand how each test works and why I recommend certain natural support strategies. Today, I want to discuss everything the GI Map Stool Analysis has to offer and how to interpret this test.
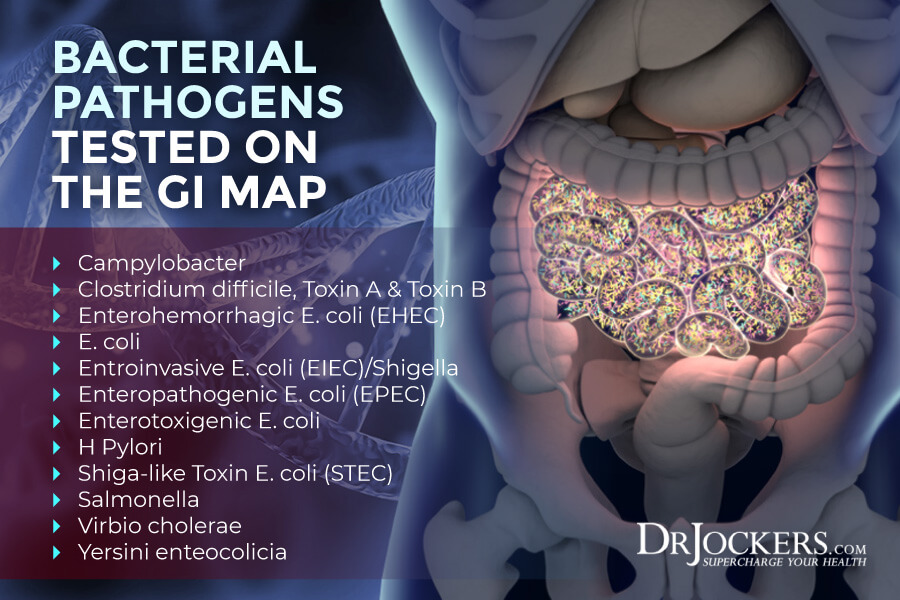
Pathogens
First, the GI Map Stool Analysis looks at bacterial, parasitic, and viral pathogens (1). It is very important to touch on these bacterial, parasitic, and viral infections as they are common culprits of abdominal pain, bloating, diarrhea, vomiting, and other digestive discomfort.
Some may only last for a few days and may clear up by itself, while others can last longer and need treatment. Besides understanding the cause of some acute digestive symptoms, it is important to uncover these pathogens as some of them may have long term effects. Salmonella, clostridium difficile, and a few other pathogens, for example, may lead to reactive arthritis (2).
According to a 2008 study published in the Emergency Infectious Diseases, bacterial gastrointestinal infections can have both short- and long-term effects (3). For example, campylobacter infections may increase your risk of ulcerative colitis one year after the original infection occurred.
You may think that you overcame a stomach bug’s acute symptoms, but the infection may disrupt your gut microbiome and cause long-term effects. This is why it is important to look for potential pathogens and address them. Let’s look at what bacterial, viral, and parasitic pathogens the GI Map Stool Analysis looks at.
Bacterial Pathogens
- Campylobacter: This is one of the most common causes of foodborne illness in the United States. It may cause abdominal pain, diarrhea, malaise, and fever (1).
- Clostridium difficile, Toxin A & Toxin B: About 2 to 10 percent of the population carried genes for toxin A and toxin B carried by this particular bacteria. It may cause inflammation, cramping, fever, diarrhea, and abdominal pain, and may result in reactive arthritis (1).
- Enterohemorrhagic E. coli (EHEC): You may get infected by this bacteria through contaminated food or water. It may cause abdominal cramping, fever, fatigue, diarrhea, and nausea (1).
- E. coli: You may catch this through contaminated food or water. It may cause severe abdominal cramps and diarrhea (1).
- Entroinvasive E. coli (EIEC)/Shigella: You may get infected by this bacteria through fecal contamination of ingested food. It may cause diarrhea, vomiting, fever, chills, abdominal cramping, and fatigue, as well as reactive arthritis (1).
- Enteropathogenic E. coli (EPEC): It spreads through fecal contamination of ingested foods. It may cause bloody and watery diarrhea (1).
- Enterotoxigenic E. coli: This bacteria is the most common cause of traveler’s diarrhea. It causes diarrhea (1).
- Shiga-like Toxin E. coli (STEC): You may get infected by this bacteria through fecal contamination of ingested foods. It may cause abdominal cramps and diarrhea (1).
- Salmonella: This is a very well-known bacteria that may spread through fecal contamination of ingested food and exposure to certain animals, such as baby chicks and reptiles. It causes vomiting, fever, and severe diarrhea (1).
- Virbio cholerae: This bacteria can be picked up during international travel through contaminated food. It may cause watery diarrhea, vomiting, thirst, low blood pressure, rapid heart rate, dry mucous membranes, irritability, and restlessness (1).
- Yersini enteocolicia: This bacteria also spread through contaminated food and water. It may cause vomiting, fever, diarrhea, and abdominal pain, possibly mimicking Crohn’s disease, and may trigger autoimmune thyroiditis or inflammatory arthritis (1).
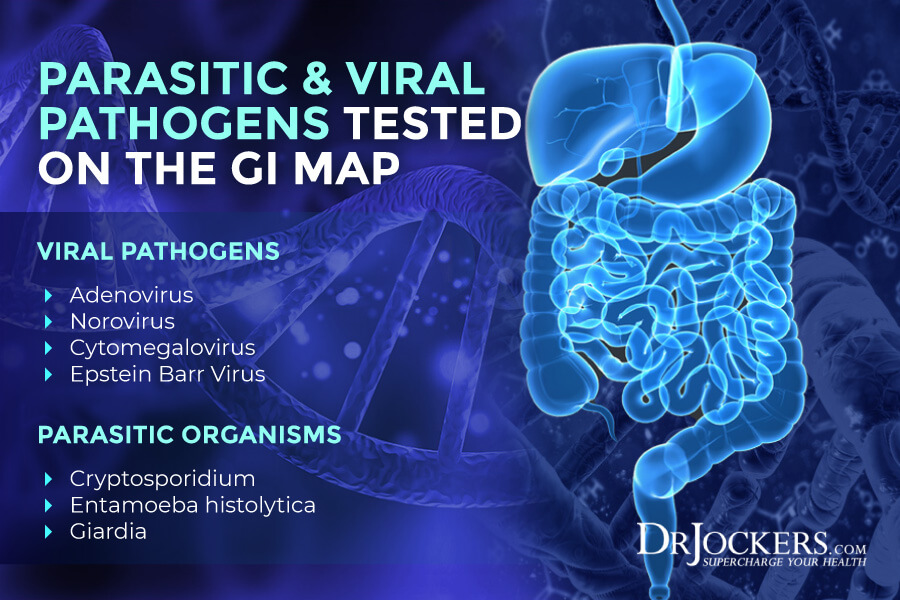
Parasitic Pathogens
- Cryptosporidium: This parasitic pathogen can be picked up through contaminated food and liquids and is a common cause of traveler’s diarrhea. It can cause diarrhea and reactive arthritis (1).
- Entamoeba histolytica: This may spread through contaminated food and water, pets, and sexual contact. It may cause diarrhea, dysentery, and fulminating colitis which resembles ulcerative colitis (1).
- Giardia: This is the most commonly isolated protozoa that spreads through outside water sources, animals, and daycare workers. It can cause diarrhea, cramps, bloating, intestinal malabsorption, malnutrition, weight loss, and steatorrhea (1).
Viral Pathogens
- Adenovirus 40/41: This can spread through fecal contamination and is a common cause of diarrhea in infants and children. It can cause watery diarrhea, fever, and gastroenteritis (1).
- Norovirus GI/GII: This viral pathogen can spread through contaminated food and water. It is a common cause of stomach flu on cruise ships. It can cause nausea, diarrhea, vomiting, fatigue, abdominal cramps, headaches, and fever (1).
H. Pylori
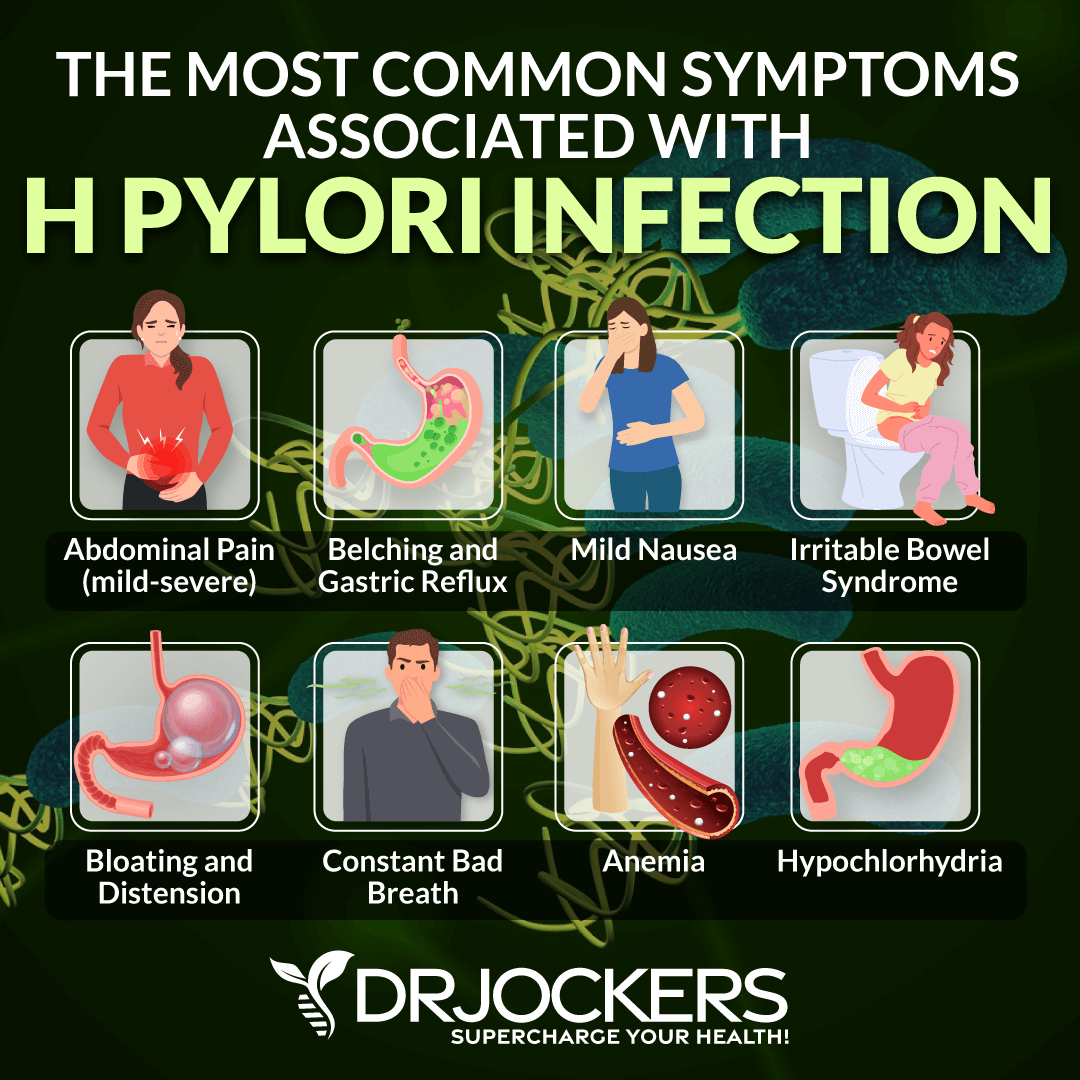
Helicobacter pylori (H. pylori) overgrowth is one of the many culprits of gut and other health problems. You may get infected through fecal contamination, oral to oral transmission, and family transmission. It may cause abdominal pain, vomiting, nausea, peptic ulcers, and other gastrointestinal issues (1).
Though about 50 percent of the population is struggling with H. pylori, many careers are asymptomatic or do not know that their symptoms and health issues are connected to H. pylori overgrowth (4). This corkscrew-shaped bacteria can be the cause of bloating, stomach pains, unhealthy stools, chronic gastritis, ulcers, esophageal issues, and even stomach cancer.
H pylori can also lead to low stomach acid. Hydrochloric acid or stomach acid helps to sterilize food before it goes into your gut and helps to break down protein. Healthy stomach acid is critical for optimal digestion and gut microbiome balance and you may learn about its importance from this article (5).
The GI Map Stool Analysis looks at all virulence factors related to H. Pylori. Though about 50 percent of the population is affected by this bacteria, only about 2 percent develop gastric cancer (1). Looking at these virulence factors helps us understand the genetic potential for H. pylori to lead to pathology and know how aggressive we may have to be when it comes to treatment.
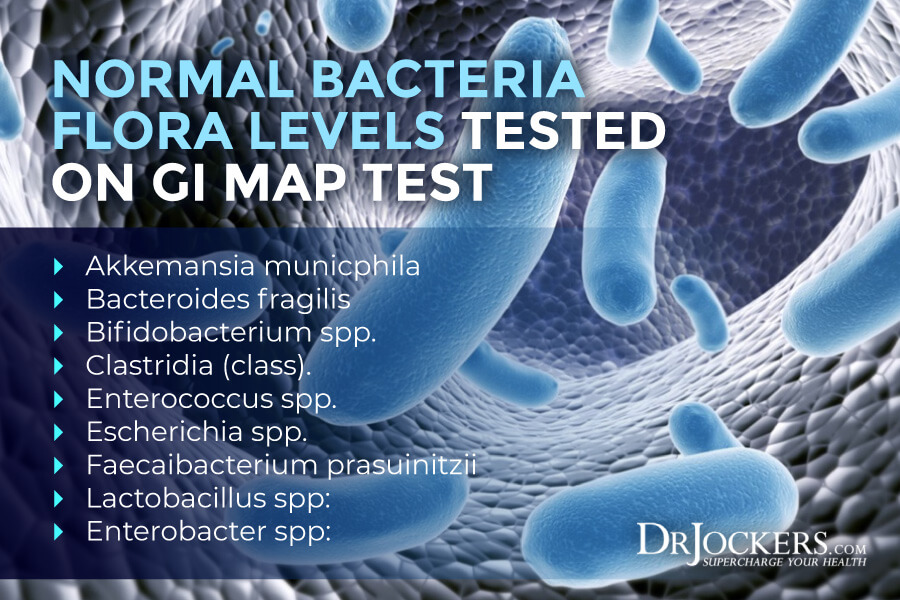
Normal Bacteria
There are trillions of microorganisms living in your microbiome. Many of these bacteria are normal or commensal or healthy that helps your body function better. They help to extract nutrients, produce vitamins, protect you from pathogens, and support the gut barrier function.
Bacteria have cell walls that give them rigidity, strength, and protection. These cell walls have a peptide polysaccharide layer called peptidoglycan, which is a polymer made up of amino acids and sugar mesh. Bacteria may be gram-positive or gram-negative which is a classification based on the physical and chemical cell wall properties.
Gram-positive bacteria have a thick cell wall of about 30 layers of peptidoglycan surrounding the monoderm. Gram-negative bacteria have a thin layer found between diderms. While both gram-positive and gram-negative can be harmful bacteria, gram-negative ones are more resistant to antibodies. When it comes to healthy bacteria, a 2017 study published in Frontiers in Immunology has found that gram-positive probiotics are more effective against infections and more protective of your immunity (6).
The GI Map Stool Analysis looks are the balance of your beneficial bacteria, including both gram-positive and gram-negative bacteria:
- Akkermansia mucinophila: This bacteria is a mucus degrader that helps to support mucus production and mucosal health. According to a 2020 study published in Frontiers in Microbiology, low levels may be linked to obesity and metabolic dysfunction (7). On the other hand, a 2018 study published in mSystems connected high levels with multiple sclerosis (8).
- Bacteroides fragilis: This gram-negative bacteria is important for microbial balance and neuroimmune health. According to a 2007 study published in Clinical Microbiology Review, they have the most antibiotic resistance (9). High levels may cause constipation and digestion issues while low levels may lead to reduce anti-inflammatory gut activities (1).
- Bifidobacterium spp.: This is a gram-positive bacteria found in breast milk that helps to colonize the gut at and after birth. It’s also commonly found in probiotics. Low levels may happen because of low fiber intake and high levels tend to happen in children instead of adults (1).
- Clostridia (class): This is an important bacteria in the large intestine that helps to protect the gut from pathogens, support immune balance, and promote a healthy mucosal barrier. According to a 2019 study published in the International Journal of Molecular Science, gut bacteria can lead to autoimmunity including autoimmune disorders without gut symptoms (10). Low levels are associated with autoimmunity and inflammation, while high levels have been linked to metabolic issues (1).
- Enterococcus spp.: This is a gram-positive lactate-producing bacteria. According to a 2017 study published in Gut Liver, high levels may be linked to small intestinal bacterial overgrowth (SIBO), irritable bowel syndrome (IBS), and related symptoms (11). Low levels may influence microbiome balance and good bacteria insufficiency (1).
- Escherichia spp.: This is a gram-negative bacteria. According to a 2014 study published in the World Journal of Gastrointestinal Pathophysiology, high levels may indicate inflammation and cause chronic inflammatory bowel diseases (IBD) (12). Low levels may reduce mucosal health and decrease protection against E. Coli (1).
- Faecalibacterium prausnitzii: This bacteria support anti-inflammatory processes and mucosal health and homeostasis. According to a 2019 study published in the International Journal of Molecular Science, low levels can lead to autoimmune conditions and inflammatory issues (10, 1).
- Lactobacillus spp: This is a lactate-producing bacteria often found in probiotics. High levels may happen because of high carb intake, while low levels may occur because of low carb or high salt intake. High levels may compromise digestion while low levels may affect mucosal health (1).
- Enterobacter spp: This is a gram-negative bacteria closely related to E. coli. According to a 2017 study published in Mucosal Immunology, high levels may drive inflammation and dysbiosis (13). Low levels may affect mucosal health (1).
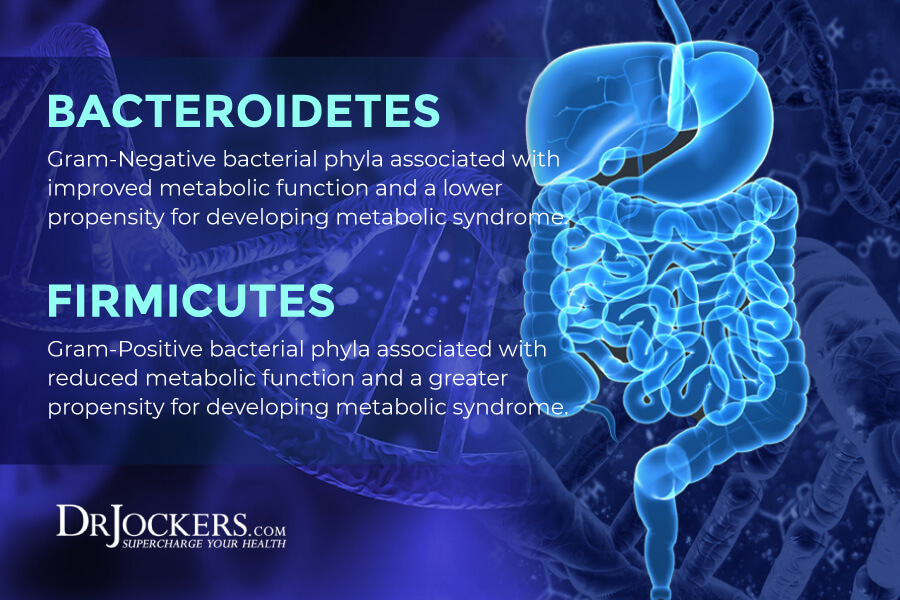
Firmicutes and Bacterioidetes Phyla
The test also looks at gram-negative bacteroidetes and gram-positive firmicutes, which are bacterial phyla that dominate your digestive health from your mouth to your colon. Abnormal results may occur because of gut dysbiosis, poor diet, and maldigestion, and create an imbalance microbiome and related symptoms (1).
Opportunistic Bacteria
The GI Map Stool Analysis also measures opportunistic pathogens that can cause inflammation, chronic symptom, illness, and disease. Symptoms like abdominal pain, loose stools, diarrhea, and constipation are common when these opportunistic bacteria are present in high amounts, however, other chronic symptoms may also occur.
Opportunistic bacteria overgrowth can become especially problematic if you also eat a poor diet, use or have used antibiotics, have a parasitic or fungal infection, or have a compromised immune system. The GI Map Stool Analysis looks at opportunistic bacteria overgrowth in your gut, including both gram-positive and gram-negative bacteria.
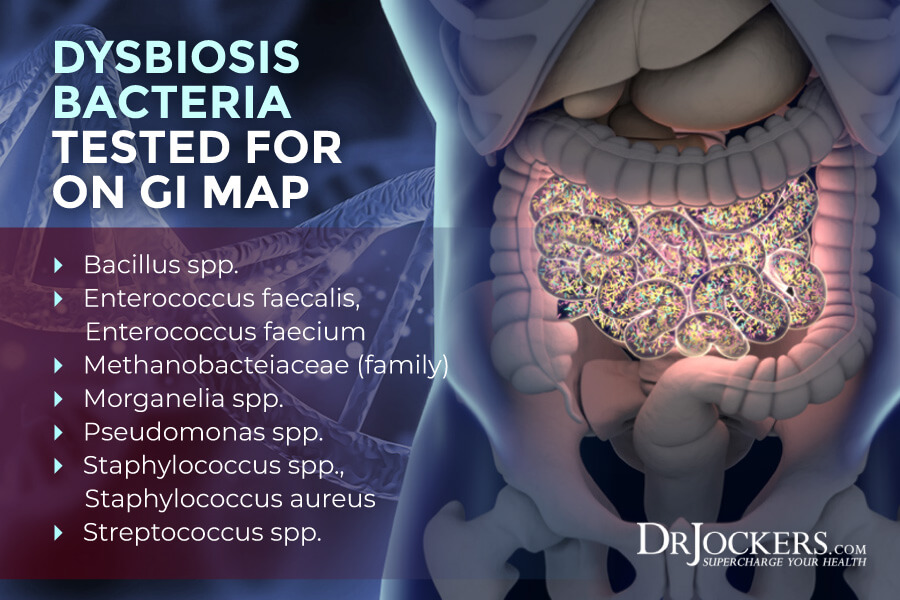
Additional Overgrowth or Dysbiosis:
- Bacillus spp.: This is a gram-positive bacteria. High levels may be connected to constipation, SIBO, and other digestive issues (1).
- Enterococcus faecalis, Enterococcus faecium: These are gram-positive bacteria. High levels may occur due to SIBO, constipation, or other digestive issues, as well as antibiotic use (1, 11).
- Methanobacteriaceae (family): This family of bacteria produces methane and facilitates fermentation. High levels occur with SIBO, IBS, and chronic constipation, and low levels may be linked to inflammation or low short-chain fatty acid production (1).
- Morganella spp.: This is a gram-negative bacteria that may produce histamine. This can be an issue for those with histamine intolerance. High levels may mean inflammation and may lead to diarrhea or SIBO (1).
- Pseudomonas spp., Pseudomonas aeruginosa: These are gram-negative bacteria. High levels may occur due to inflammation and lead to loose stools and cramping (1).
- Staphylococcus spp., Staphylococcus aureus: These are gram-positive bacteria. High levels may mean inflammation. Certain strains may cause diarrhea due to toxins (1, 14).
- Streptococcus spp.: This is a gram-positive bacteria that can colonize the mucous membranes and the skin. High levels may occur because of low stomach acid, SIBO, constipation, or inflammation (1, 15).
Potential Autoimmune Triggers:
- Citrobacter spp, Citrobacter freundii: These are gram-negative bacteria. High levels may mean high inflammation in the gut and may be linked to rheumatoid arthritis (1).
- Fusobacterium spp: This is a gram-negative bacteria found in your mouth and intestines. High levels are associated with inflammation and autoimmunity (1). According to a 2016 article published in Arthritis Rheumatology, it may be associated with systemic sclerosis (16).
- Klebsiella spp., Klebsiella pneumoniae: These are gram-negative bacteria found in your oral cavity and respiratory system. It can lead to abdominal pain, bloating, gas, and diarrhea, or symptoms of inflammatory bowel disease. High levels may indicate gut inflammation. It may also release histamine which can be a problem for those with histamine intolerance (1). It may also cause pneumonia (17).
- Mycobacterium avium subsp. Paratuberculosis: High levels of this bacteria have been linked to rheumatoid arthritis and Crohn’s disease as indicated by a 2017 study published in the Korean Journal of Internal Medicine and a 2015 study published in Expert Review of Gastroenterology and Hepatology (1, 18, 19).
- Prevotella capri: These are gram-negative bacteria. In a 2019 study published in the Journal of Clinical Medicine, they have been linked to rheumatoid arthritis (20). It may be caused by a high-starch diet and reduced digestive capacity (1).
- Proteus spp. Proteus mirabilis: These are gram-negative bacteria. High levels may mean inflammation in the gut and may lead to diarrhea or loose stools (1). According to a 1999 study published in the Journal of Infections, it may be linked to rheumatoid arthritis (21).

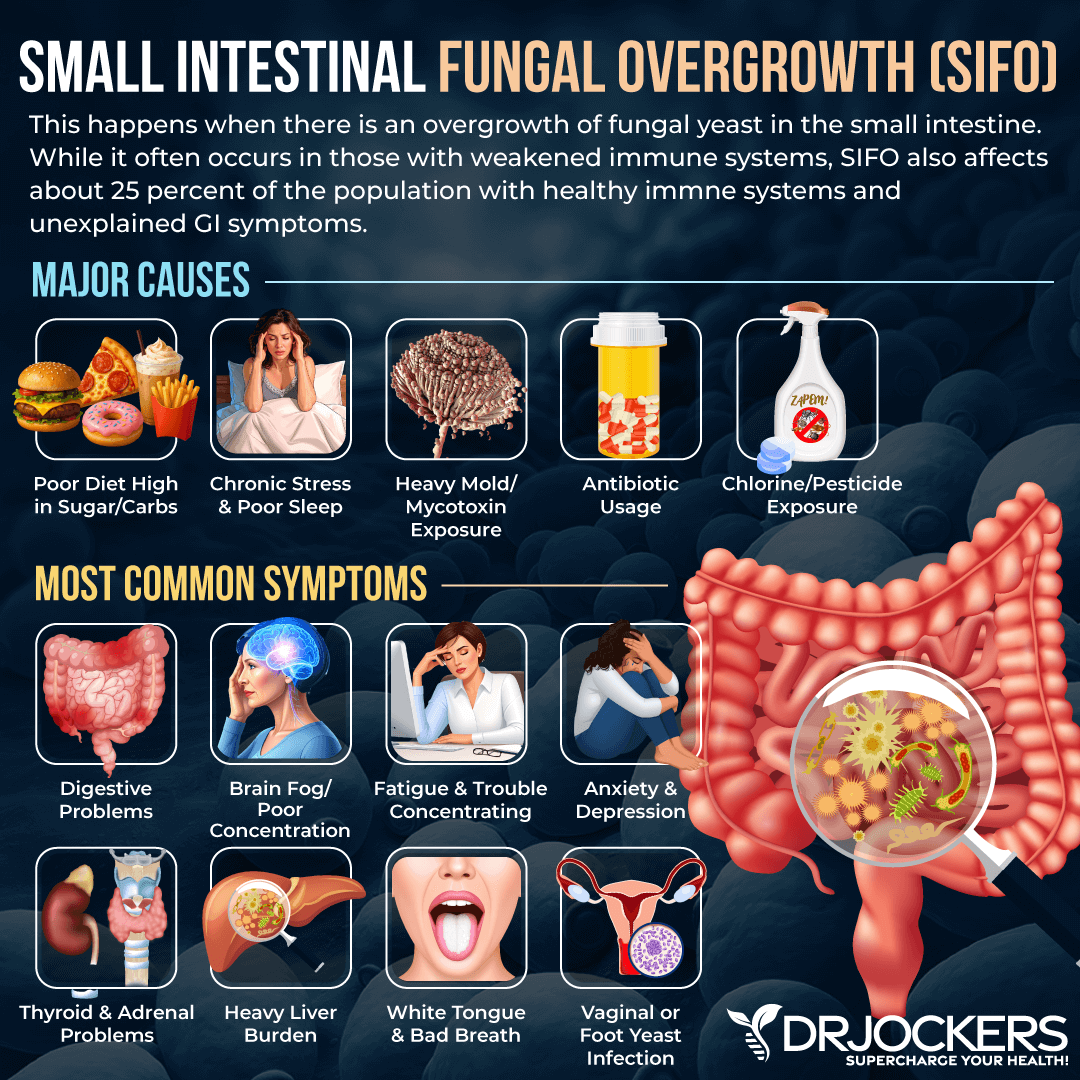
Fungal and Yeast
Fungal and yeast overgrowth is common, yet it can create serious gut health and other health issues and nagging symptoms. In many cases, fungal overgrowth is localized. For example, Candida may be present in the large intestines but not in the small one. Antibiotic use, high sugar intake, a diet high in starches, beer, bread, corn, cheese, and other dietary fungi (yeast), gut dysbiosis, hypochlorhydria, and poor immune health can increase your risk of fungi and yeast overgrowth (1).
The GI Map Stool Analysis tests for Candida Albicans and Candida spp. While in small amounts Candida is necessary and healthy, in larger quantities it can be problematic. A 2012 study published in Current Opinions in Microbiology has connected Candida colonization to inflammation and related issues (24).
A paper published in AGA Abstracts has also discussed the potential role of fungal overgrowth in the small intestines in gastrointestinal issues (24). Candida had been linked to microbiome imbalance, constipation, gas, yeast infections, abdominal pain, bloating, nausea, headaches, fatigue, skin issues, depression, anxiety, muscle pain, joint pain, and more (1, 22, 23, 24).
The GI Map Stool Analysis also tests for Geatrichum spp which may cause issues in immunosuppressed individuals (1). It also checks for Microsporidia found in soft cheeses that may cause diarrhea and wasting, as well as, Rhodotorula spp, found in soil, plants, bathrooms, water, juice, and milk, and may be a problem in those who are immunosuppressed (1).
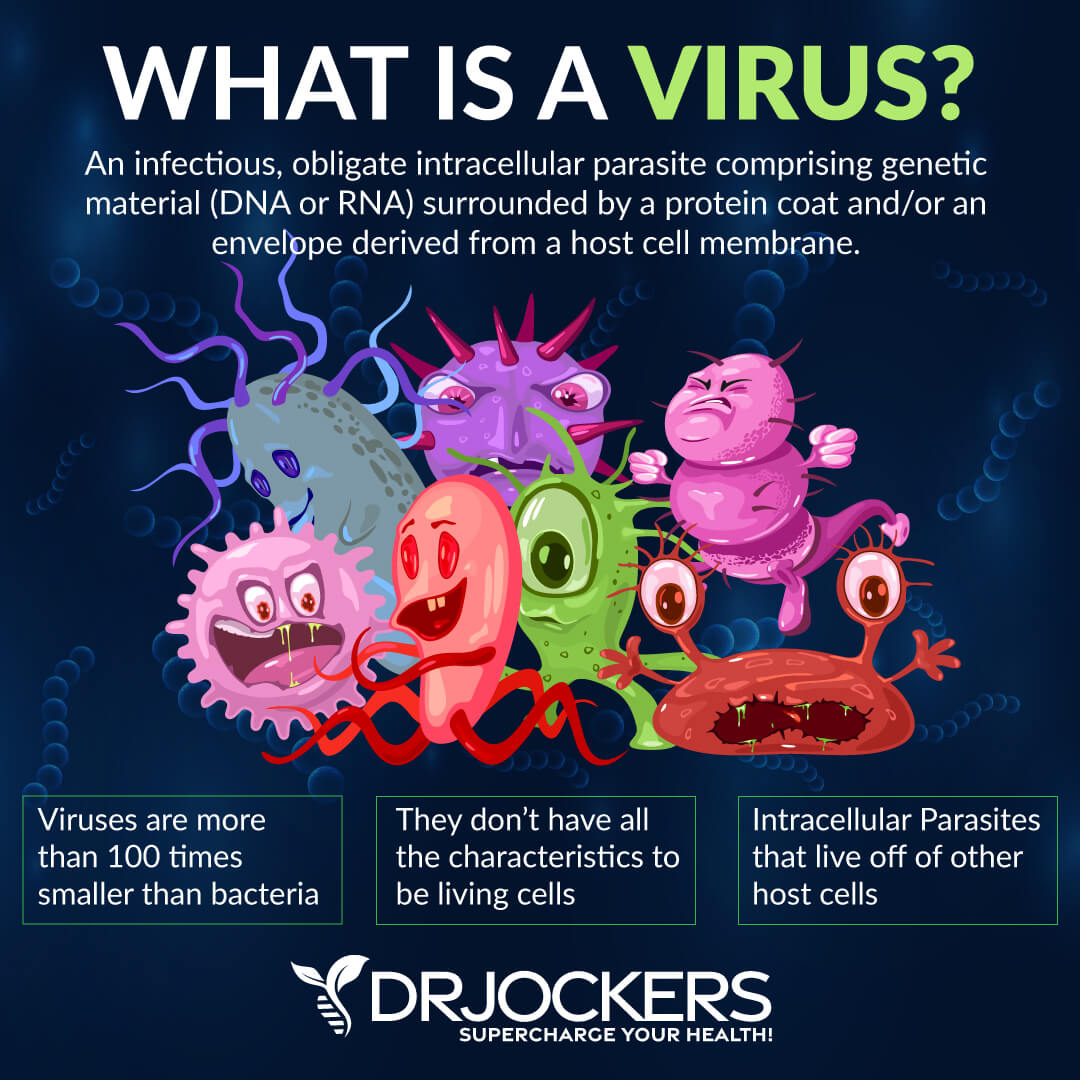
Viruses
Viruses can also lead to microbiome imbalance, gut health issues, an array of symptoms, and serious health issues. The GI Map Stool Analysis tests for the Cytomegalovirus (CMV) and the Epstein-Barr Virus (EBV) (1).
CMV is the herpes virus that affects about 60 percent of the US population. It has been linked to various autoimmune diseases, including lupus, systemic sclerosis, type 1 diabetes, and rheumatoid arthritis (1). A 2013 study published in the International Journal of Clinical Rheumatology, have linked CMV to childhood-onset systemic lupus (25).
According to a 2005 study published in PLoS Medicine, CMV may trigger systemic sclerosis (26). A 2019 study published in Pediatric Diabetes has found that getting infected with CMV during early childhood may increase the progression of type 1 diabetes (27). A 2016 study published in Arthritis Rheumatology has linked CMV to rheumatoid arthritis (28).
EBV is one of the most common viral infection that affects 90 to 95 percent of the population even though most people don’t know it because they haven’t experienced any or only mild symptoms of the infection. EBV has been linked to a number of autoimmune diseases as well, including rheumatoid arthritis, lupus, multiple sclerosis, autoimmune thyroid disease, Sjorgen’s syndrome, as well as, chronic fatigue syndrome, and fibromyalgia (1).
A 2004 study published in Autoimmunity Reviews has found a link between EBV infections and rheumatoid arthritis (29). A 2019 study published in Neural Regeneration Research has found that EBV may play a role in the development of multiple sclerosis (30). A 2016 study published in the Central European Journal of Immunology has found a link between EBV and various autoimmune issues, including systemic lupus, rheumatoid arthritis, autoimmune thyroid disease, Sjogren’s syndrome, and autoimmune hepatitis (31).
A 1998 study published in the Journal of Athletic Training has discussed the potential role of EBV in fibromyalgia and chronic fatigue syndrome (32). You may learn more about EBV and natural remedies to improve your health in this article.
Parasites
Parasites are organisms that live inside and feed on a host organism. In the case of parasitic infections in humans, the host is you. Parasites can enter your body through contaminated food and drink. While some parasites are non-pathogenic, pathogenic parasites and protozoa are most often found in your gastrointestinal tract (1, 33).
As a 2019 study published in Biological Sciences discussed, parasites can remain in your body long-term (34). They can cause damage without you knowing about it.
Parasitic infections can lead to bloating, gas, constipation, diarrhea, digestive issues, chronic pain, fatigue, headaches, depression, and other symptoms. Parasite overgrowth can cause inflammation, cravings, and gut dysbiosis. To learn more about parasites and parasite overgrowth and natural strategies to kill them, I recommend reading this article.
Let’s look at the parasites the GI Map Stool Analysis looks at:
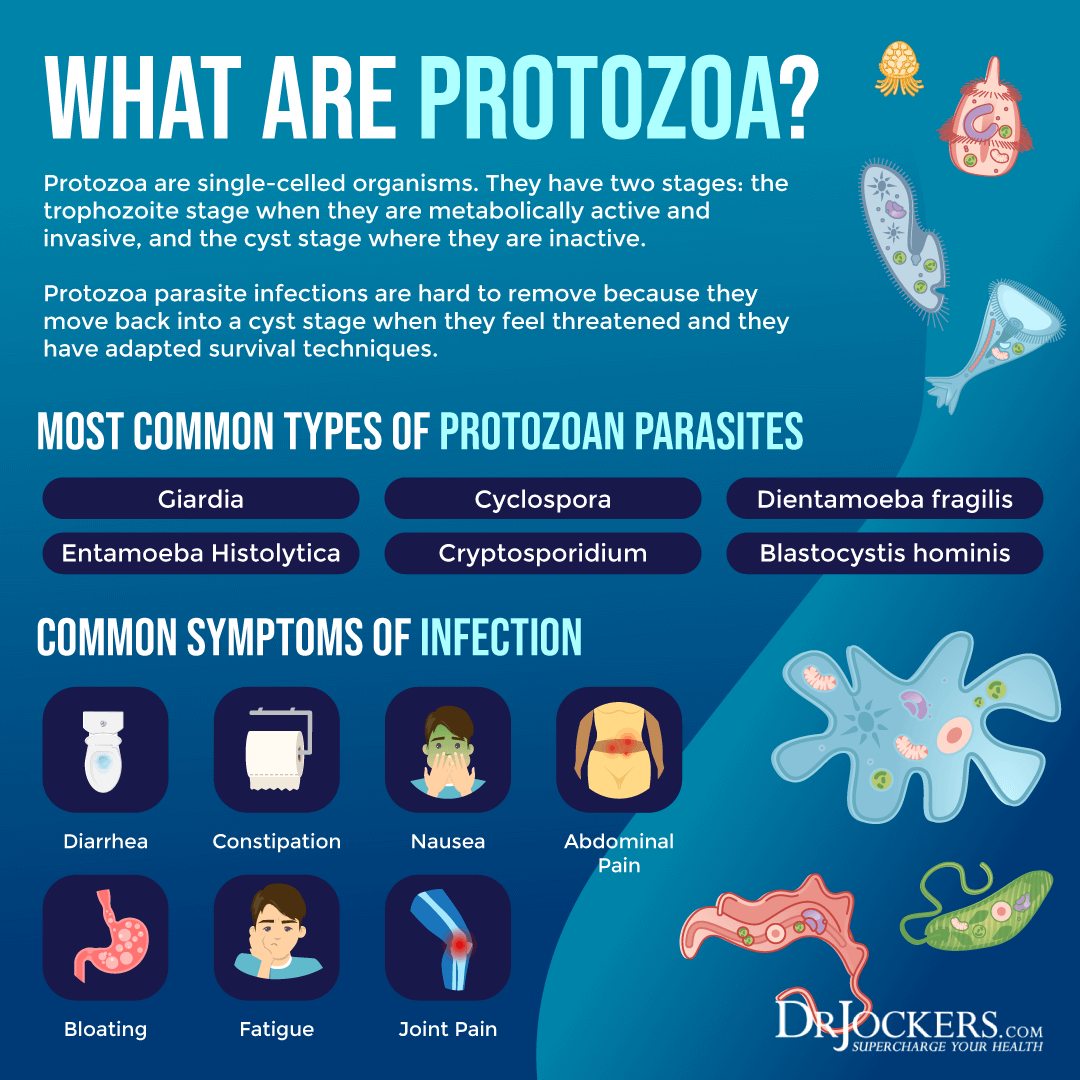
Protozoa
- Blastocystis hominis: These protozoa spread through fecal contamination of food and water. It causes abdominal pain, diarrhea, nausea, vomiting, fatigue, fever, symptoms of IBS, and infective arthritis (1).
- Chilomastix mesnili: These protozoa spread through fecal contamination of food and water. It generally doesn’t cause symptoms but may lead to gut dysbiosis or compromised immunity (1).
- Cyclospora spp (Cyclospora cayetanensis): These protozoa spread through fecal contamination of food and water and can commonly lead to foodborne outbreaks. It causes diarrhea, cramping, abdominal pain, nausea, vomiting, and weight loss (1).
- Dientamoeba fragilis: These protozoa spread through fecal contamination of food and water. It causes diarrhea, nausea, vomiting, abdominal pain, fatigue, fever, loss of appetite, and weight loss, but may also be asymptomatic (1).
- Endolimax nana: These protozoa spread through fecal contamination of food and water. It is often asymptomatic but may cause gut dysbiosis (1).
- Entameoba coli: These protozoa spread through fecal contamination of food and water. It may cause gut dysbiosis (1).
- Pentatrichomonas hominis: These protozoa spread through fecal contamination of food and water. It is usually asymptomatic but may cause gut dysbiosis (1).
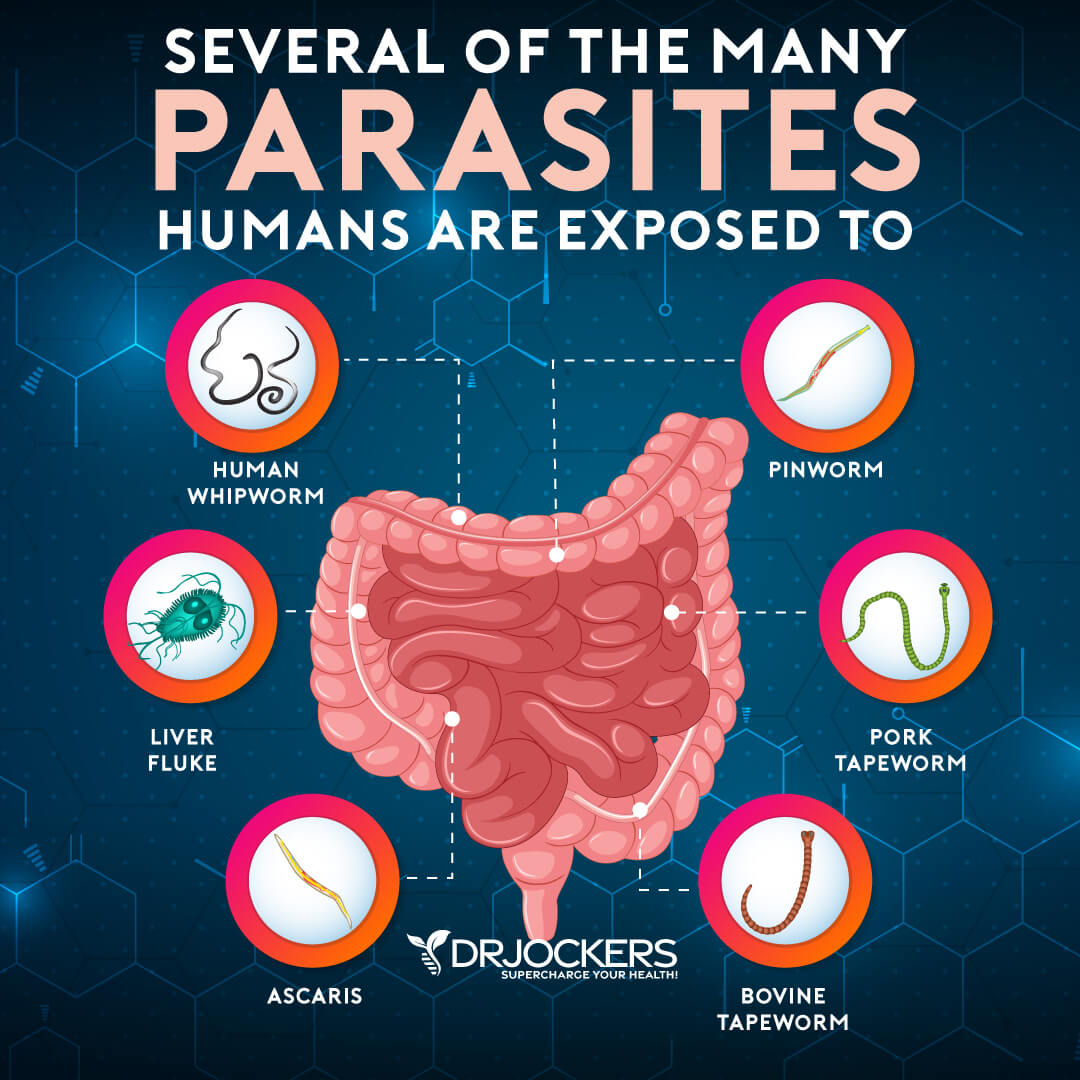
Worms
- Ancylostoma duodenale and Necatur americanus (hookworm): Hookworms may spread through skin contact with infected soils, infected dogs and cats, and sanitary issues. Early on, it may cause rashes or itching, then may lead to abdominal pain, fatigue, diarrhea, weight loss, loss of appetite, iron-deficiency anemia, and coughing (1).
- Ascaris lumbricoides (roundworm): Roundworms can spread through fecal contamination of food and water and is common in international travel. Early on, it may cause fever, coughing, and wheezing, and later may lead to abdominal pain nausea, vomiting, dry cough, pancreatitis, and appendicitis (1).
- Trichurs trichiura (whipworm): Whipworms may spread through fecal contamination of produce, as well as, person to person contact. It often remains asymptomatic but may cause diarrhea with mucus or blood (1).
- Taenia spp. (tapeworm): Tapeworms can spread through fecal contamination of undercooked beef or pork. It may remain asymptomatic but may also cause abdominal pain, constipation, nausea, headaches, weakness, diarrhea, anemia, loss or increased appetite, hyperexcitability, and pruritus ani (1).
Intestinal Health Markers
Besides looking at bacterial, viral, fungal, and pathogenic presence and overgrowth, the GI Map Stool Analysis looks at some important intestinal health markers that can help us learn more about your gut health and create personalized treatment recommendations accordingly.
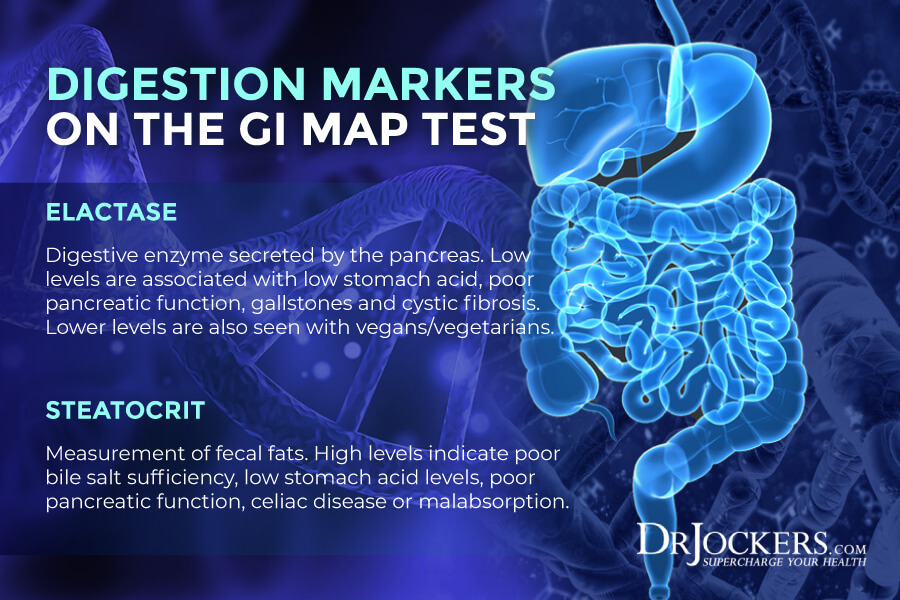
Digestion
This gut health test looks at Pancreatic Elastase 1 levels, which is a digestive enzyme secreted by your pancreas. According to a 2004 study published in the West African Journal of Medicine, testing for Pancreatic Elastase 1 is a noninvasive easy way to look at pancreatic function (35). Low levels have been associated with poor pancreatic function, gallstones, cystic fibrosis, and hypochlorhydria. Low levels are more common among vegans and vegetarians (1).
It also tests for steatocrit levels which measure fecal fats that in a healthy body are emulsified by bile and absorbed in the small intestines. High levels may indicate malabsorption or maldigestion and may be caused by poor bile salt sufficiency, hypochlorhydria, pancreatic insufficiency, celiac disease, improper mastication, malabsorption, or maldigestion (1).
Additional GI Markers
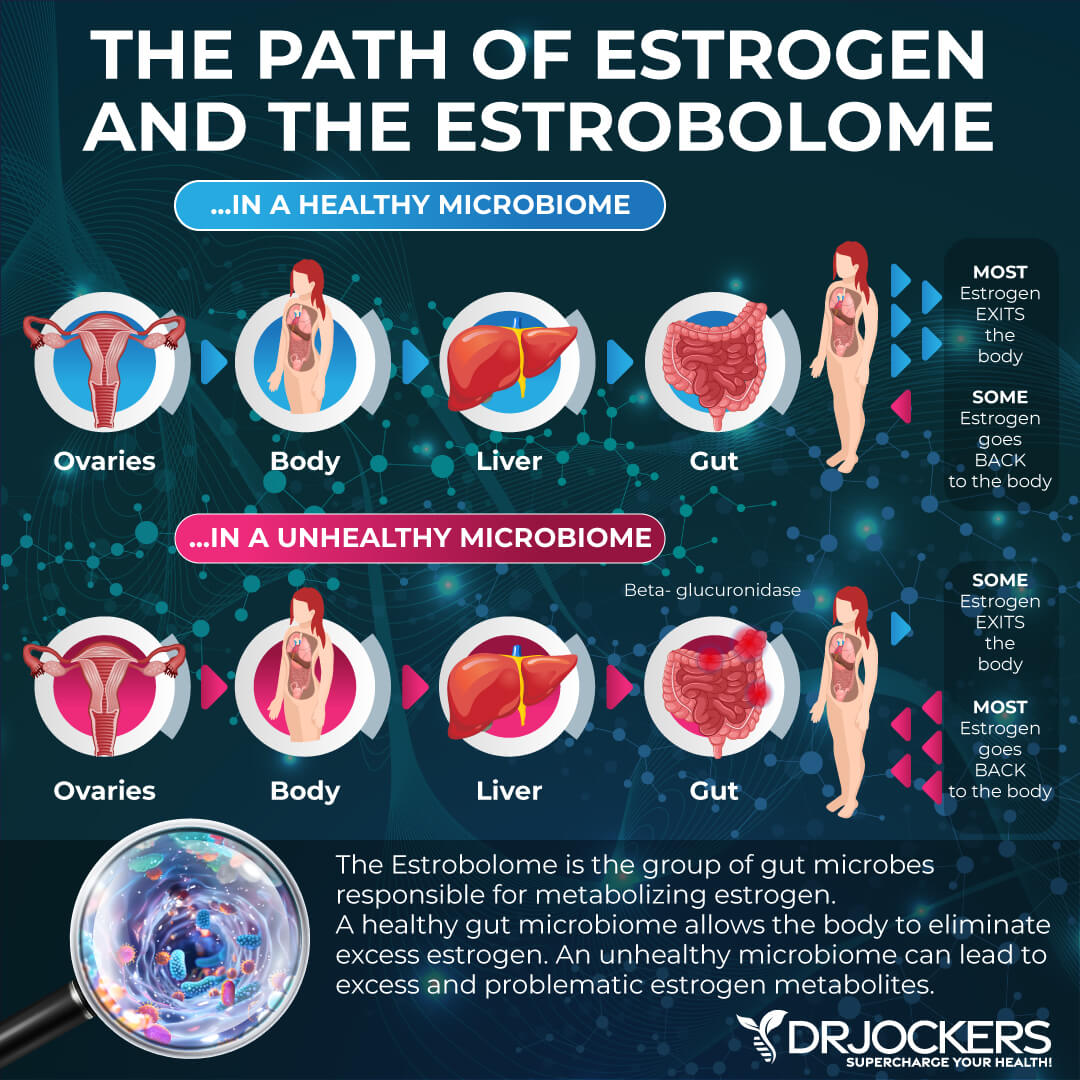
The test looks at Beta-Glucuronidase levels. According to a 2018 article published in Science Report, it is an opportunistic bacterium that can cause toxicity and gut issues (36).
In high levels, these markers may lead to metabolic changes in the colon, gut dysbiosis, detoxification issues, overexposure to toxins or drugs, and at very high levels even colon cancer (1).
Gut Mucosal & Immune Health
Occult Blood Fecal Immunochemical Testing (FIT) is also part of the test. It is a less invasive form of colorectal screening test (37). It checks for hemoglobin presence in the stool which may indicate bleeding ulcers, intestinal bowel disease, intestinal polyps, cancer, or upper GI bleeds. Lower than 10 ug/g may suggest anal fissures, hemorrhoids, pathogenic infections, upper GI infections, or liver disease (1).
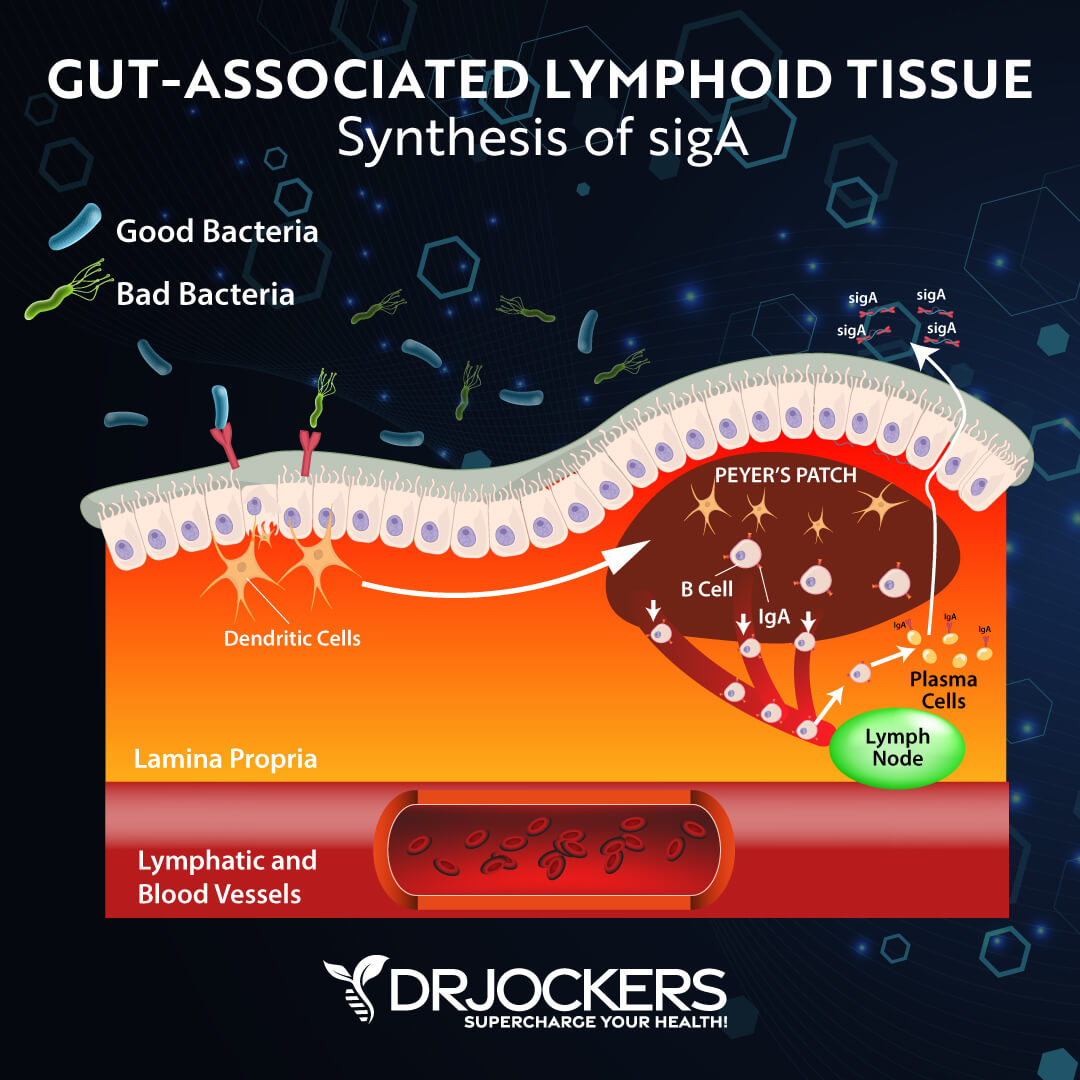
Part of the test is an immune response test (secretory IgA or sIgA and anti-gliadin IgA). According to a 2011 study published in Mucosal Immunology, this test can tell a lot about mucosal health and immune health (38).
Low fecal sIgA may indicate a suppressed gut immune system, chronic dysbiosis, antigen exposure, protein malnutrition, immunocompromised state, or chronic stress. High fecal sIgA may indicate acute infections, acute stress, food sensitivities, or chronic dysbiosis. High anti-gliadin IgA may indicate an immune response to gluten (1).
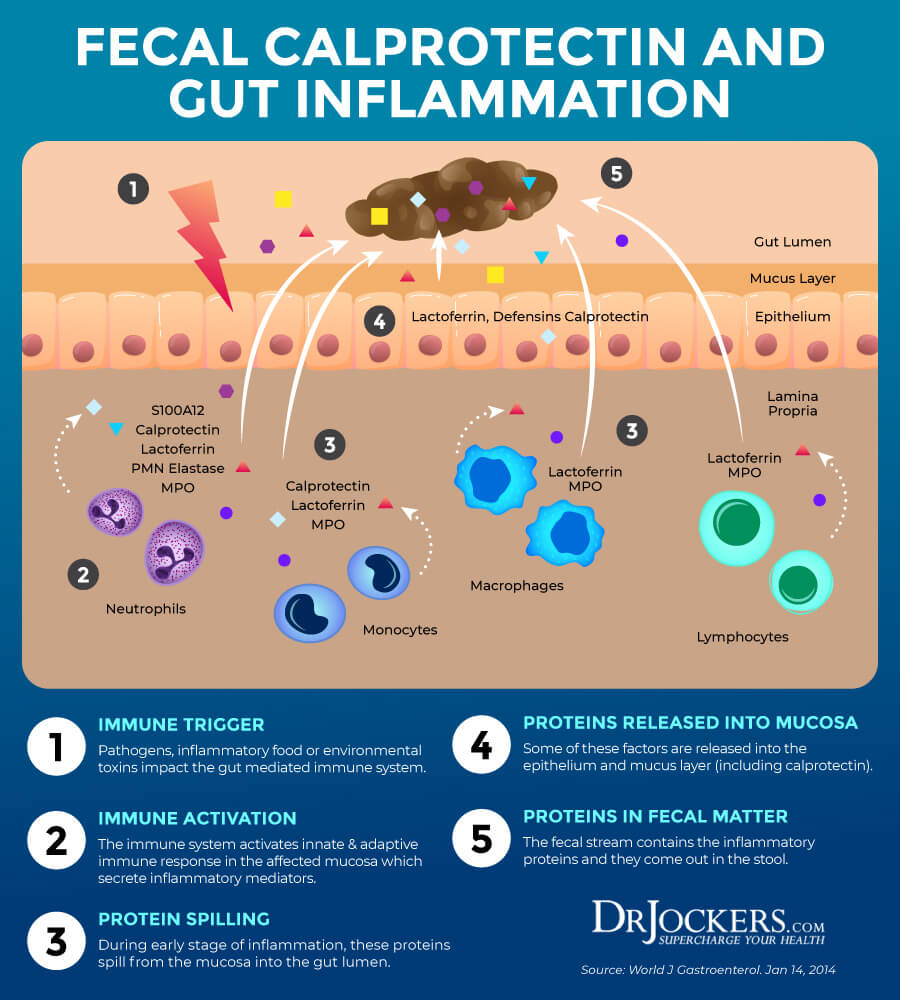
Gut Inflammation Markers
The test also checks for certain markers of inflammation. Calprotectin levels look for intestinal inflammation. According to a 2011 study published in Clinical Gastroenterology and Hepatology, this test is very important for the diagnosis of irritable bowel disease (39). High levels may indicate inflammatory bowel disease and help us to differentiate from irritable bowel syndrome. Food allergens, polyps, infections, diverticulitis, and colorectal cancer may also cause high calprotectin levels (1).
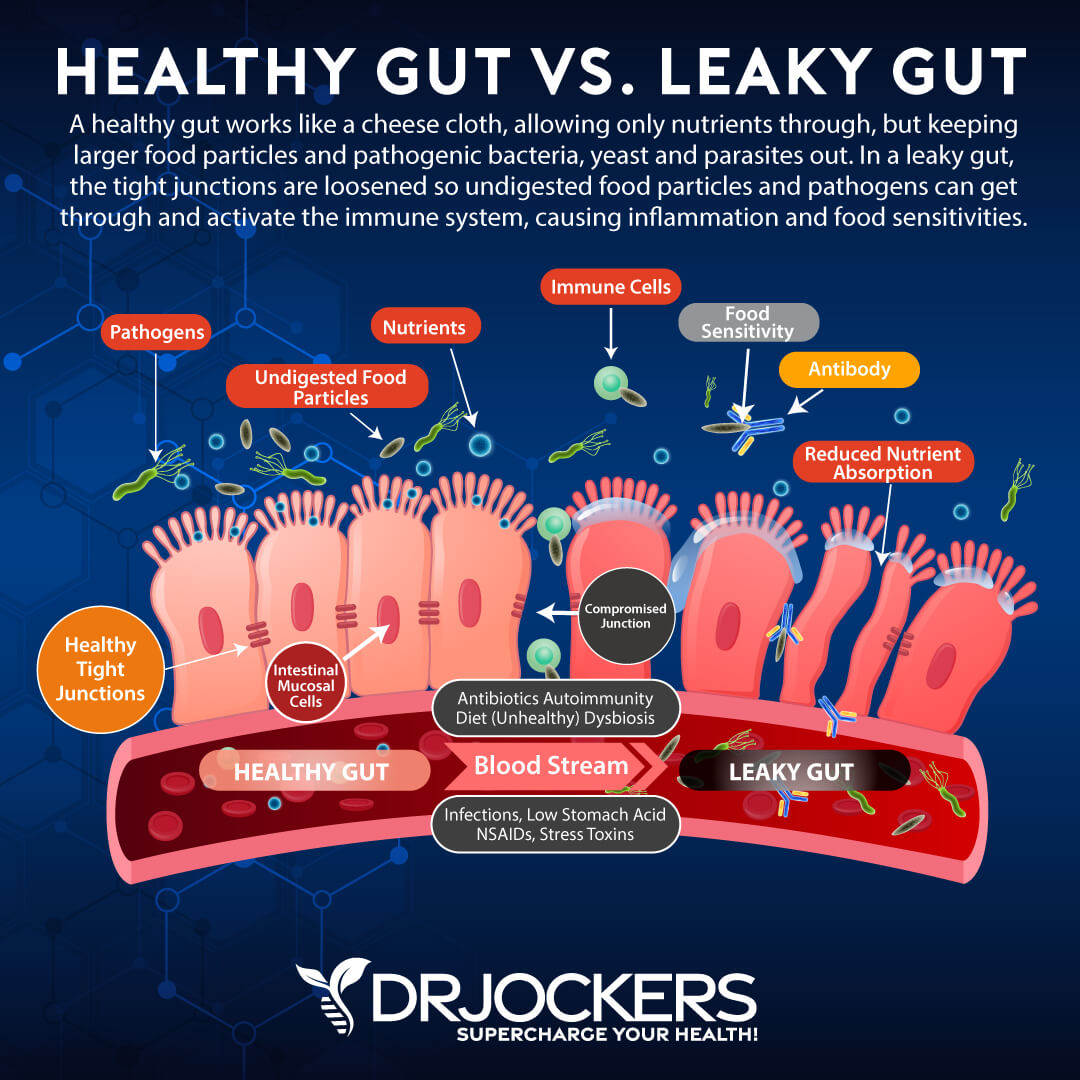
Another inflammation marker the test looks at is zonulin levels. Zonulin is a protein that helps to open junctions in your gut lining and its presence may increase the risk of leaky gut syndrome (1). According to a 2011 study published in Physiology review, this is a great test for intestinal barrier function which may indicate risk for inflammation, autoimmunity, and cancer (40).
Lastly, the test looks at certain genetic markers, including antibiotic resistance gene phenotypes, such as clarithromycin and fluoroquinolones, and universal microbiota resistance genes, such as b-lactamase, fluoroquinolones, macrlides, and vancomycin. These results can indicate resistance to certain antibiotics and may indicate that you need to avoid certain medications (1).
Final Thoughts
Your gut health plays an important role in your health. Your gut microbiome health is connected to your immune system, metabolism, mental health, and other areas. Imbalance in your microbiome and various pathogen overgrowth may contribute to the development of autoimmune and other chronic health issues.
The GI Map Stool Analysis is the best comprehensive gut test that helps to identify bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora, potential autoimmune triggers, and all intestinal health markers to help your functional or natural health doctor to develop a personalized treatment plan to repair your body and regain your health naturally. Take the guesswork out of your health, test your gut microbiome today with the GI Map Stool Analysis.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




Thank you for all the information. I was diagnosed with H.pylori a few months ago. I refused to take the protocol of antibiotics as I have shown sensitivity to every antibiotic I have ever taken. I am taking a pre/probiotic and as yet don’t see a lot of improvement. I would appreciate any additional information
Hey Joan, here is a helpful article on H Pylori https://drjockers.com/damaging-effects-h-pylori-infections/
So much great information and explanation! Thank you!
Thanks for all your support Meg! Blessings to you!
Thank you for your informative articles! Do you have more articles on staphylococcus aureus? My daughter’s naturopathic doctor believes she just got over it. She didn’t have any type of skin or gastro issue but did have a high white blood count, fast heart rate, extreme fatigue, and fever and was treated with IV antibiotics at a hospital. We are trying to understand it better. Thank you!
Sorry to hear that Rose. I don’t have any other articles on Staph but I would recommend working with a functional health coach. https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
What does dl mean on the gi test results? I’m waiting to get an appointment with my doctor and until then I’m curious what it means? Thanks
“< dl represents results below detectable limit." according to the test results.
Thank you for this great information. My son was vaccine injured and after 3 years of heavy metal chelation, parasite cleanse, supplementation and working on his gut, we have seen great improvement.
Somehow, I noticed bad breath, a bit distension and rare behaviors (heavy breathing more than usual) that he had not exhibited in a while and “my gut” told me to do the test again. Sure enough, H. Pylori was a bit high with Staph and Strep on his opportunistic/overgrowth section. I am happy to know there wasn’t more found but now we don’t have to guess on how to move forward to help him. I wish more parents would look into this testing and pay attention to the gut health- it truly makes a difference to repair the gut and microbiome.
Sorry to hear this! Here is a helpful article on our H Pylori protocol: https://drjockers.com/h-pylori-protocol/