 Silent Reflux: Symptoms, Causes, and Support Strategies
Silent Reflux: Symptoms, Causes, and Support Strategies
Silent reflux is a condition that most people do not know much about. Heartburn, nausea, belching, and chest pain. These symptoms are usually signs of acid reflux. In some people, however, reflux is not that obvious and the symptoms are different. They may be dealing with silent reflux or laryngopharyngeal reflux (LPR).
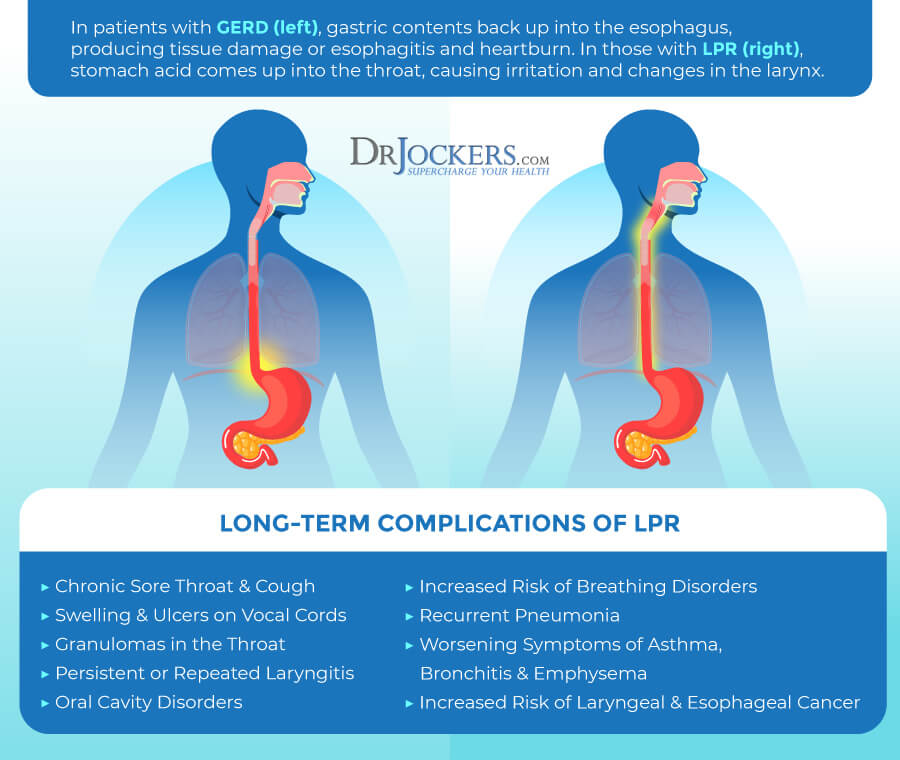
Silent reflux is caused by the backward flow of stomach acid affecting the lower part of your throat and voice box causing irritation, a burning sensation, sore throat, hoarseness, coughing, and other symptoms.
While silent reflux is highly treatable, untreated silent reflux can result in serious complications including increased risk of the oral cavity, lung, and breathing disorders, recurrent pneumonia, and increased risk of laryngeal and esophageal cancer. Fortunately, it is possible to support your body and improve your health naturally to reduce risks and complications.
In this article, you will learn what silent reflux is. I will discuss the main symptoms of silent reflux in both adults and children. You will understand the potential complications of untreated silent reflux.
You will understand the difference between silent reflux and gastroesophageal reflux disease (GERD). I will discuss how silent reflux is diagnosed and current conventional treatment methods. You will learn about the root causes of the disease. Finally, I will share my top natural support strategies for silent reflux to improve your health and well-being.
What Is Silent Reflux
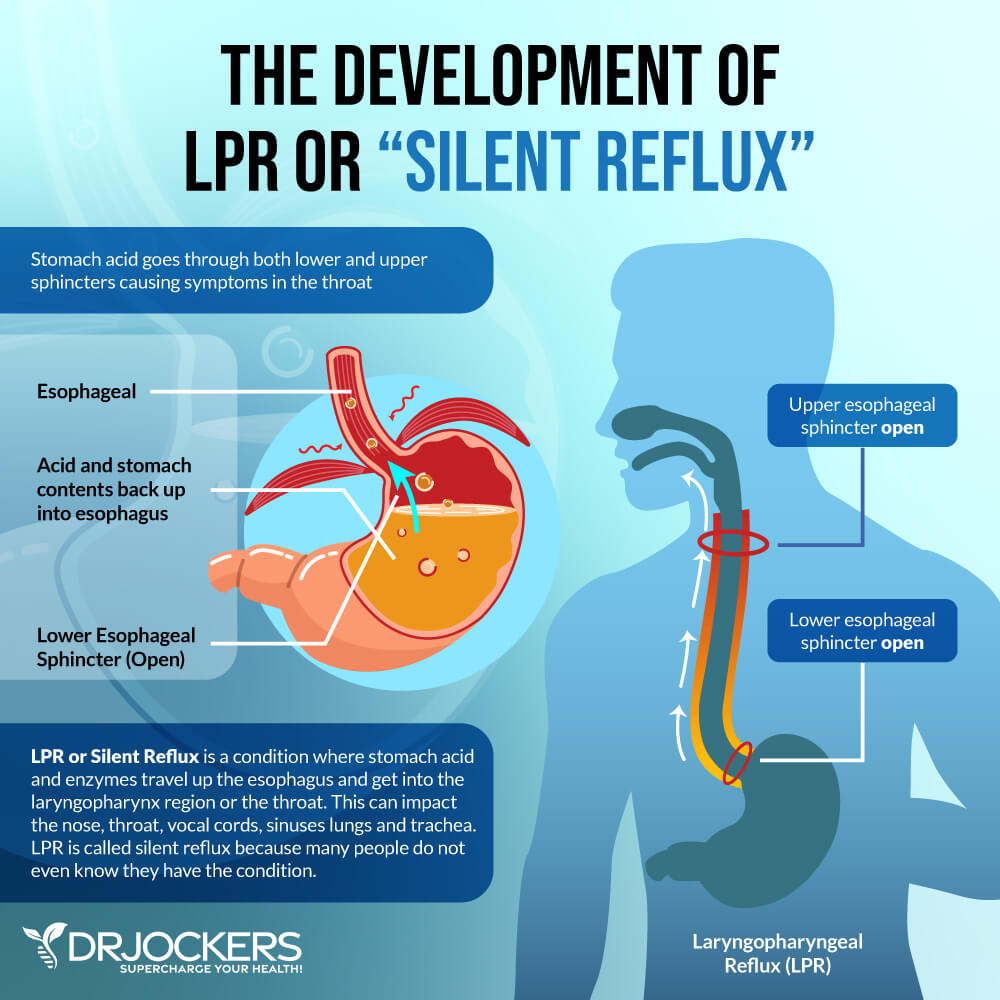
Laryngopharyngeal reflux (LPR) is a health condition characterized by throat discomfort behind the breastbone caused by stomach acid. It may develop in infants and adults and it’s a treatable health condition (1). According to a 2018 study published in the Saudi Journal of Gastroenterology, the occurrence of LPR and gastroesophageal reflux disease (GERD) may be correlated and some people may have both diseases (2).
Unlike acid reflux, it may not always come with the usual symptoms, like nausea, belching, heartburn, and chest pain, but irritates your throat and vocal cords. Reflux is a term that refers to a return flow. Silent reflux refers to the backward flow of stomach acid into the lower part of your throat causing symptoms (1).
When the stomach acid in your stomach comes in contact with your food pipe and vocal cords, it can cause irritation, discomfort, or a burning sensation. It may also damage your throat and vocal cords. Silent reflux is also often associated with coughing, throat clearing, and hoarseness (1).
Main Symptoms and Complications of Silent Reflux
Let’s talk about the main symptoms and complications of silent reflux.
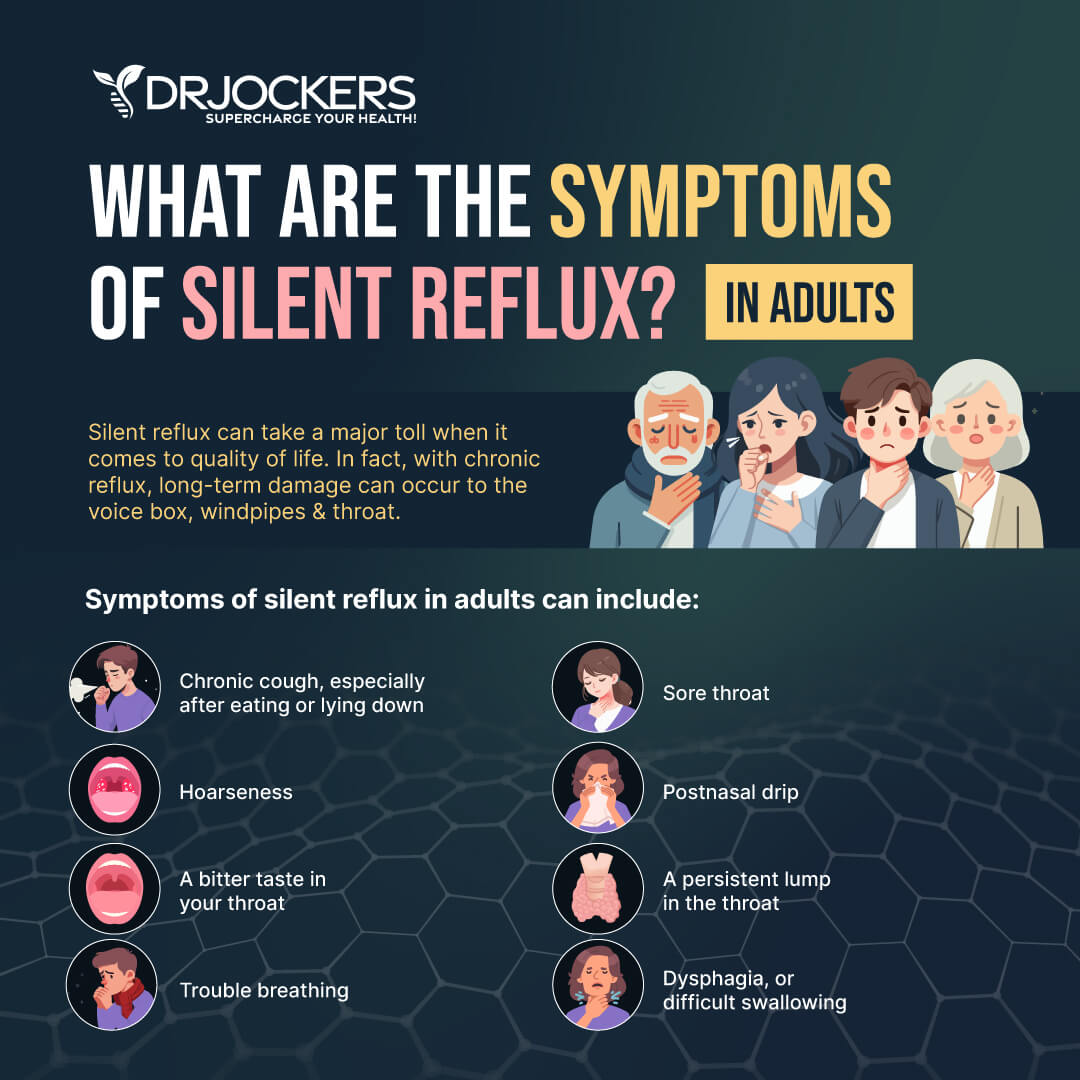
Main Symptoms of Silent Reflux
- Sore throat
- Burning sensation in the throat
- Bitter taste in the throat
- Need to clear the throat
- Hoarseness
- Chronic cough
- Feeling like there is a lump in the throat
- Difficulty swallowing
- A sensation of post-nasal drip
- A sensation of mucus build-up or sticking in the throat
- Red, swollen, or irritated vocal cords and larynx (voice box)
- Asthma
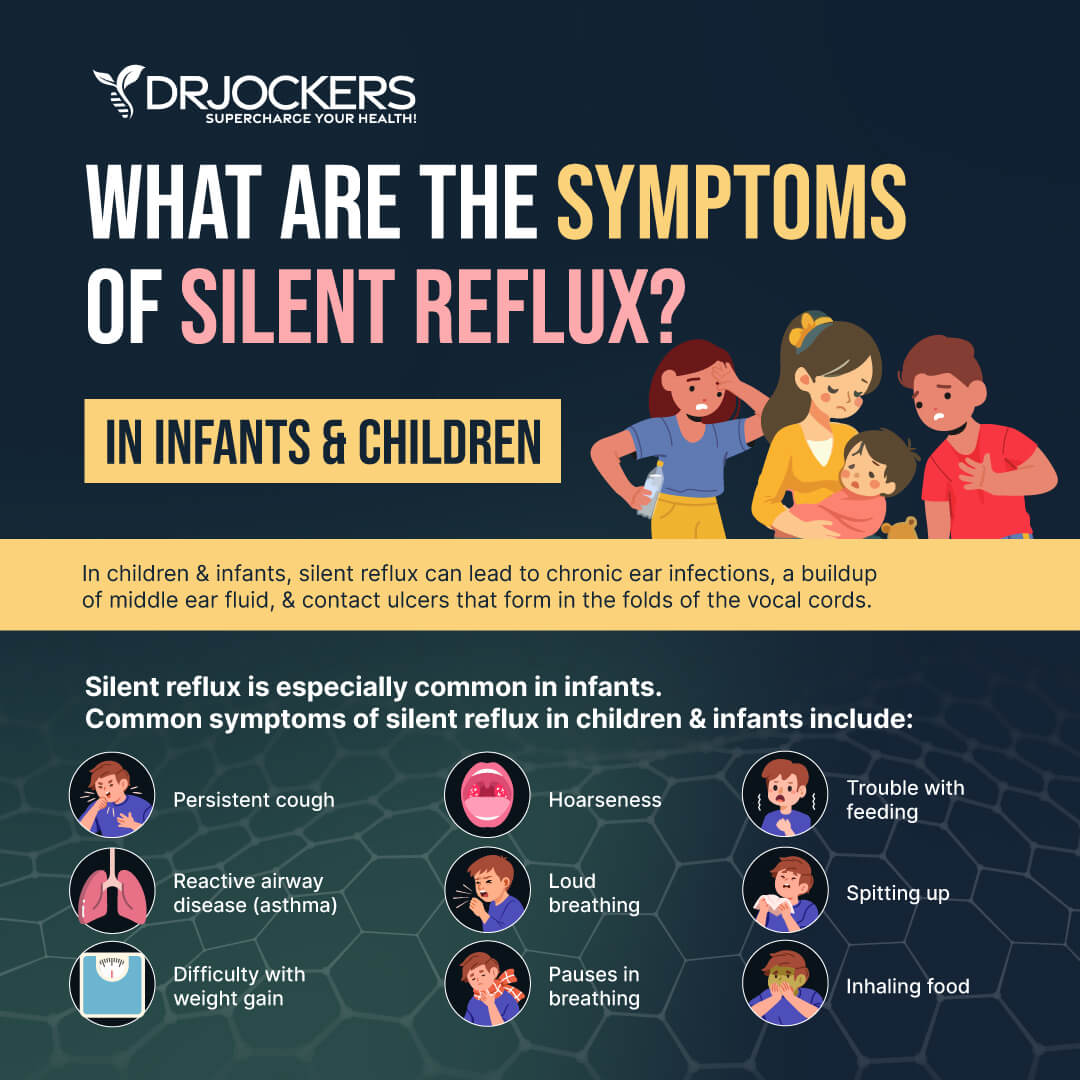
Symptoms of Silent Reflux in Children and Infants
- Coughing
- Vomiting
- Sore throat
- Noisy breathing
- Ear infections
- Hoarseness
- Failure to grow or gain weight
- Asthma
- Feeding difficulties
- Turning blue
Complications of Silent Reflux
When untreated, silent reflux can lead to a variety of issues and complications, including:
- Chronic cough
- Chronic sore throat
- Swelling of the vocal cords
- Ulcers on the vocal folds
- Development of granulomas (masses) in the throat
- Persistent or repeated laryngitis
- Oral cavity disorders
- Increased risk of lung and breathing disorders
- Increased frequency and worsening symptoms of asthma, bronchitis, and emphysema
- Recurrent pneumonia
- Increased risk of laryngeal cancer and esophageal cancer
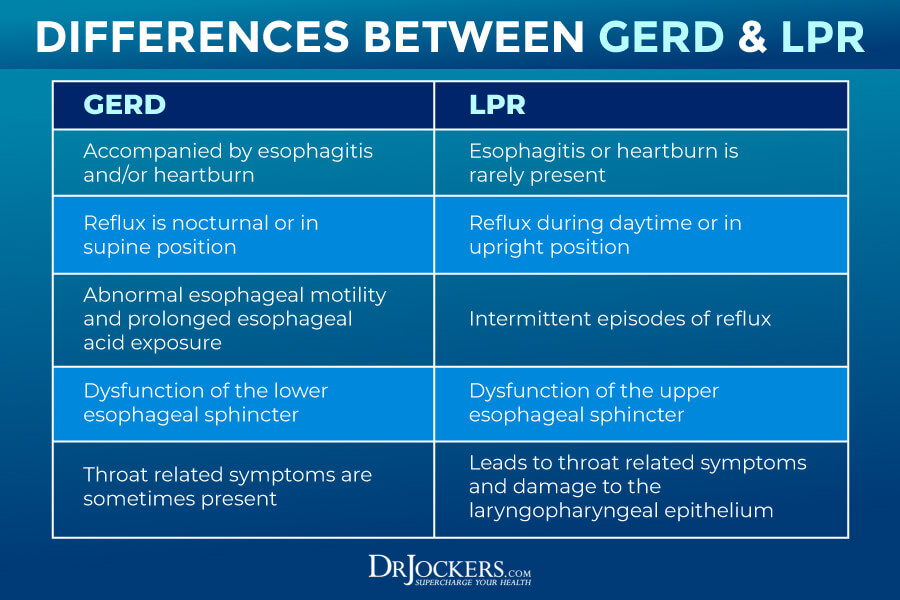
Difference Between GERD and Silent Reflux
While gastroesophageal reflux disease (GERD) and silent reflux may overlap, there are some major differences between the two conditions (2). GERD is a condition in which stomach acid and stomach enzymes backward flow into your esophagus. GERD is characterized by acid reflux, heartburn, nausea, belching, and pain in the chest. It can not only irritate by seriously damage the esophageal lining.
Silent reflux also develops when your stomach acid or food enzyme backward glows, into the laryngopharynx, which is in the lower part of your throat. While some people have both conditions, many people with GERD don’t have silent reflux, while others with silent reflux don’t experience symptoms of GERD (2).
Without the presence of GERD, silent reflux usually doesn’t cause heartburn. Instead, it results in the irritation of the throat, voice box, and vocal cords. This area is incredibly sensitive, and back-flowing acid can seriously damage surrounding tissues. When only passing through the food pipe, acid doesn’t have time to irritate the voice box area, however, when backflowing, it causes increased and prolonged irritation resulting in a sore throat, a burning sensation, a need to clear your throat, hoarseness, and other symptoms of silent reflux.
Diagnosis and Conventional Treatments
Before you understand how silent reflux develops and what natural strategies I recommend, I want to go over how silent reflux is diagnosed and your conventional treatment options
Diagnosis of Silent Reflux
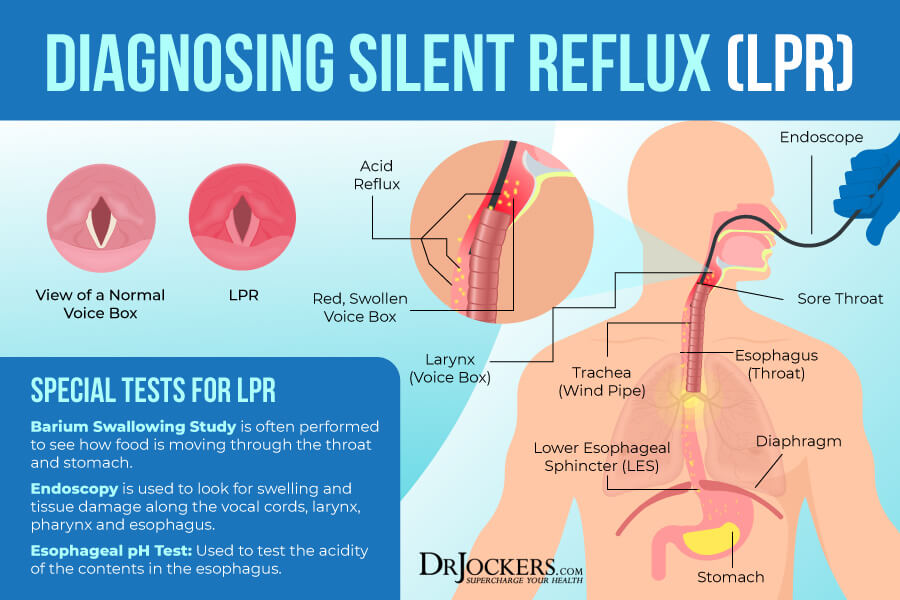
If you are experiencing symptoms of silent reflux, it’s important that you visit your healthcare professional for the correct diagnosis. Your healthcare professional, usually an ENT specialist or ear, nose, and throat doctor, will go over your medical history and your symptoms. After a physical exam, a variety of laboratory tests may be ordered.
Your doctor will recommend a swallowing study. During this swallowing study, you will be asked to swallow barium, a special liquid, that will cover your esophagus, stomach, and intestine. Barium shows up on an x-ray so your healthcare professional will be able to see how the food passes from your mouth through the esophagus and note any abnormalities.
Next, you will likely go through an endoscopic study. This way, your doctor will be able to take a look at your esophagus and stomach with an endoscope, which is a long, thin tube with a camera that can show your inside and detect abnormalities.
Your doctor will likely order an esophageal pH test that can check the pH level in the esophagus to indicate the level of acidity. To do this, a thin, small tube will be inserted through your nose down to your esophagus. The end of this tube has a small device that can sense acidity.
If your child or baby has silent reflux, contrast studies are not recommended. If the symptoms are serious, including swallowing difficulties, feeding difficulties, or vomiting is present, an endoscopy may be requested.
Conventional Treatment for Silent Reflux
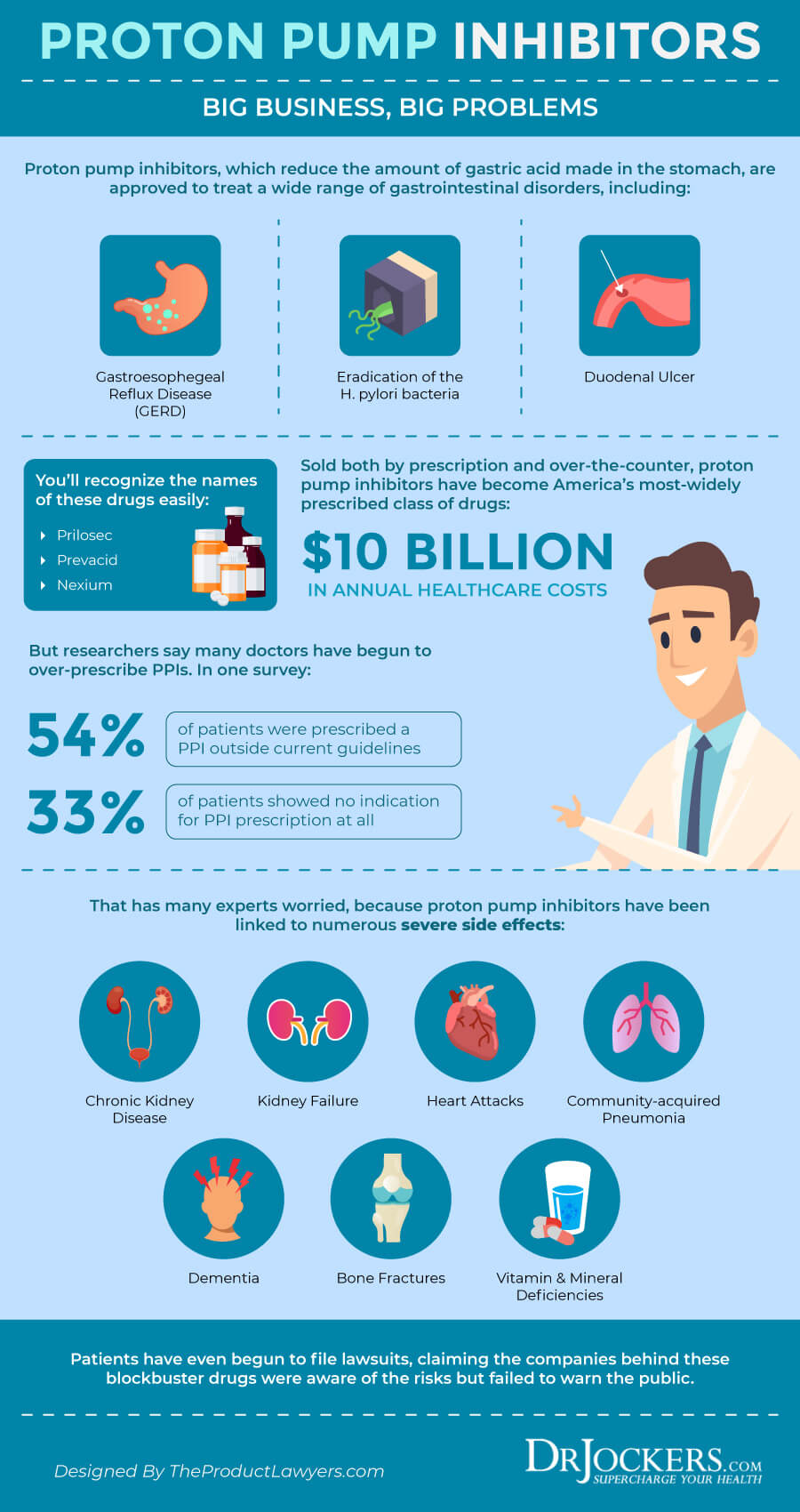
According to a 2013 study published in Therapeutic Advances in Chronic Disease, conventional treatment strategies for silent reflux usually include a combination of reflux medication and lifestyle recommendations (3). Medications prescribed for silent reflux are either designed to reduce stomach acid or prevent your body from creating too much stomach acid.
Common medications include antacids, proton pump inhibitors (PPIs), and H2 blockers. While these medications are designed to reduce your symptoms, they will not reverse or cure the condition. Most patients need to continue taking them for the rest of their lives to manage their symptoms (3).
Lifestyle recommendations may include some dietary recommendations, including increased fiber intake, increased intake of fruits and vegetables, reduced carbohydrate and sugar intake, avoiding spicy foods, reducing alcohol and coffee consumption, not eating close to bedtime, eating smaller amounts more frequently, removing triggering foods, and weight loss if needed. Lifestyle recommendations may include raising the head of the bed before sleeping, avoiding clearing your throat, quitting smoking, exercising regularly, and, avoiding strenuous workouts (3).
In serious cases, laparoscopic antireflux surgery (LARS) may be recommended to provide relief. If the vocal cords or vocal box are seriously affected, speech therapy and other rehabilitation techniques may be helpful as well (3).
Root Causes of Silent Reflux
Laryngopharyngeal reflux or silent reflux may develop for a variety of reasons. Let’s look at the root causes of the condition.
Food Sensitivities
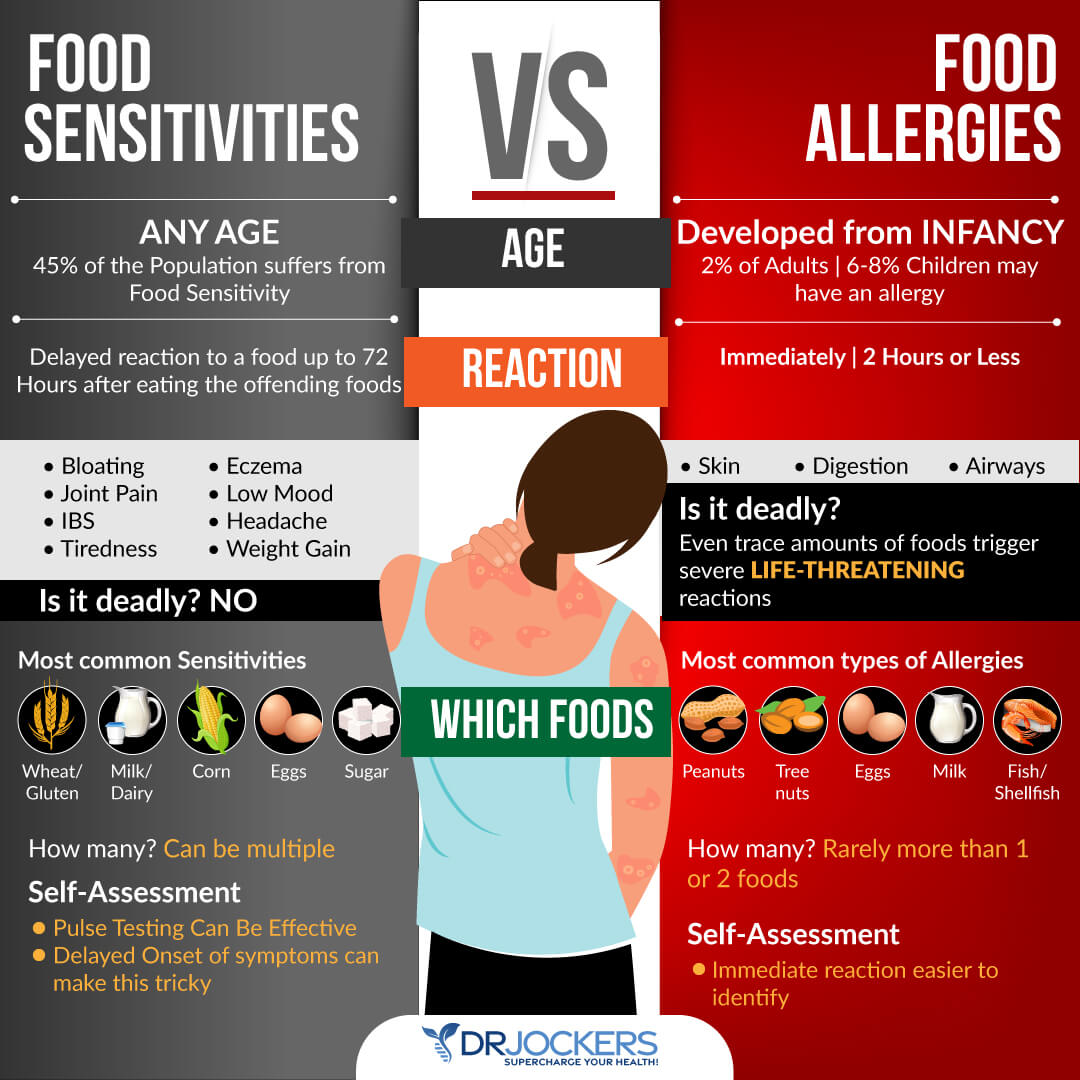
Certain foods may be more triggering for silent reflux than others. Food sensitivities are different from food allergies. Food allergies cause an immediate reaction in your body. You may experience hives, swelling, difficulty breathing, puffiness, digestive issues, or other symptoms immediately after eating a food that you are allergic to. In some cases, these symptoms can be life-threatening when not addressed right away.
Food sensitivities, on the other hand, don’t result in an immediate reaction but cause issues over time. You may eat food and only experience symptoms a few hours or even a few days later. When eating certain foods that you are sensitive to, you will experience chronic inflammation and chronic symptoms that you can’t seem to find a clear cause for.
One of these chronic symptoms caused by food sensitivities may be symptoms of silent reflux. According to a 2007 study published in the Journal of Pediatric Gastroenterology and Nutrition, esophageal cells in the esophagus may experience an allergic reaction to reflux disease that may be triggered by a reaction to food (4).
Histamine Intolerance
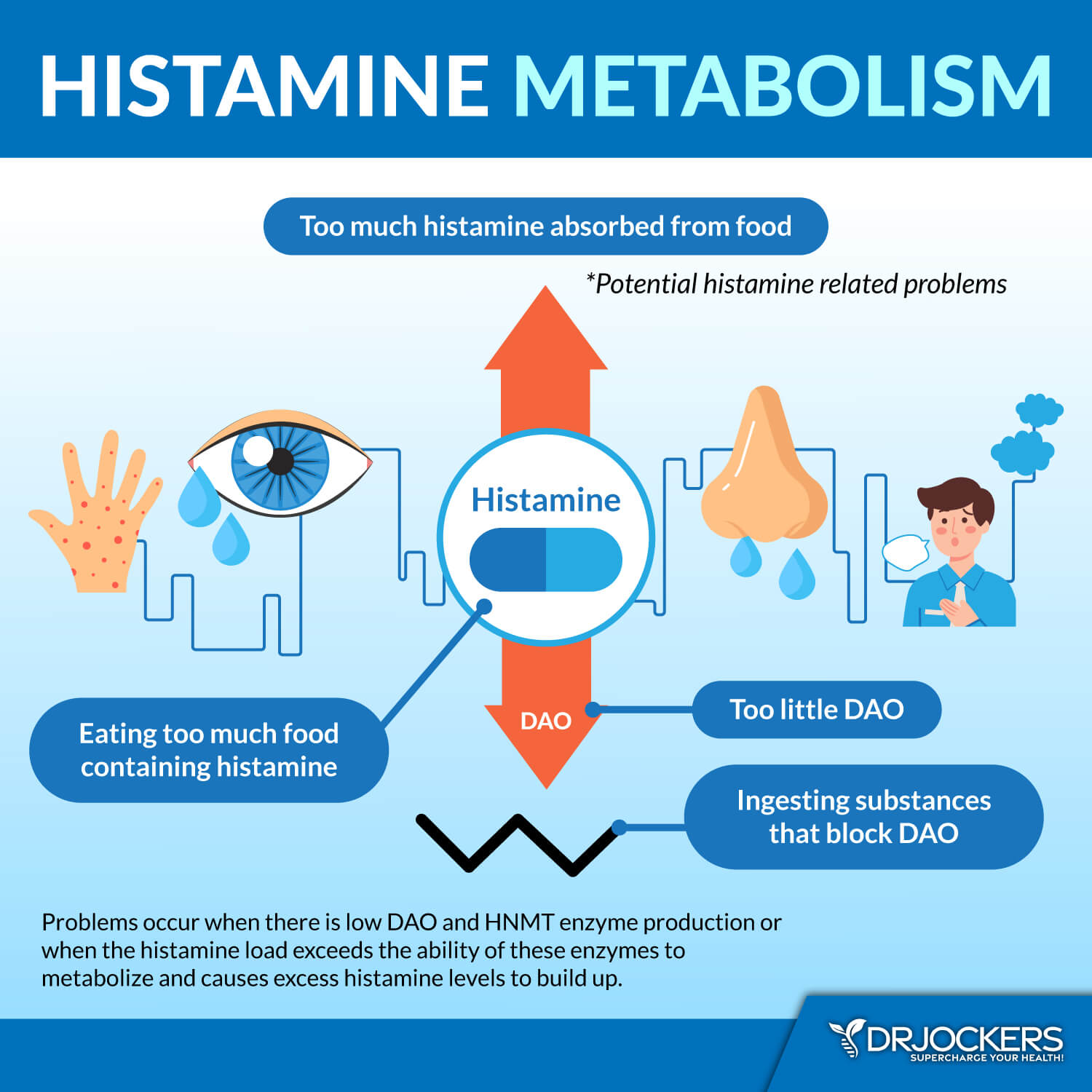
According to a 2020 case report published in the Ear, Nose, and Throat Journal, laryngopharyngeal reflux symptoms may be triggered by histamine intolerance (5). Histamine intolerance means that your body has too much histamine build-up and is unable to break down excess histamine.
High-histamine foods can cause histamine intolerance and symptoms, including acid reflux and silent reflux in some people. Furthermore, avoiding certain foods, including fatty cold cuts, fried foods, caffeine, alcohol, whole-fat dairy, sodas, onions, tomatoes, lemons, kiwi, oranges, grapefruit, pineapples, and acidic, spicy, and sugary foods, in general, seems to help many patients of silent reflux. You can read more about histamine intolerance in this article.
Poor Stomach Acid Production
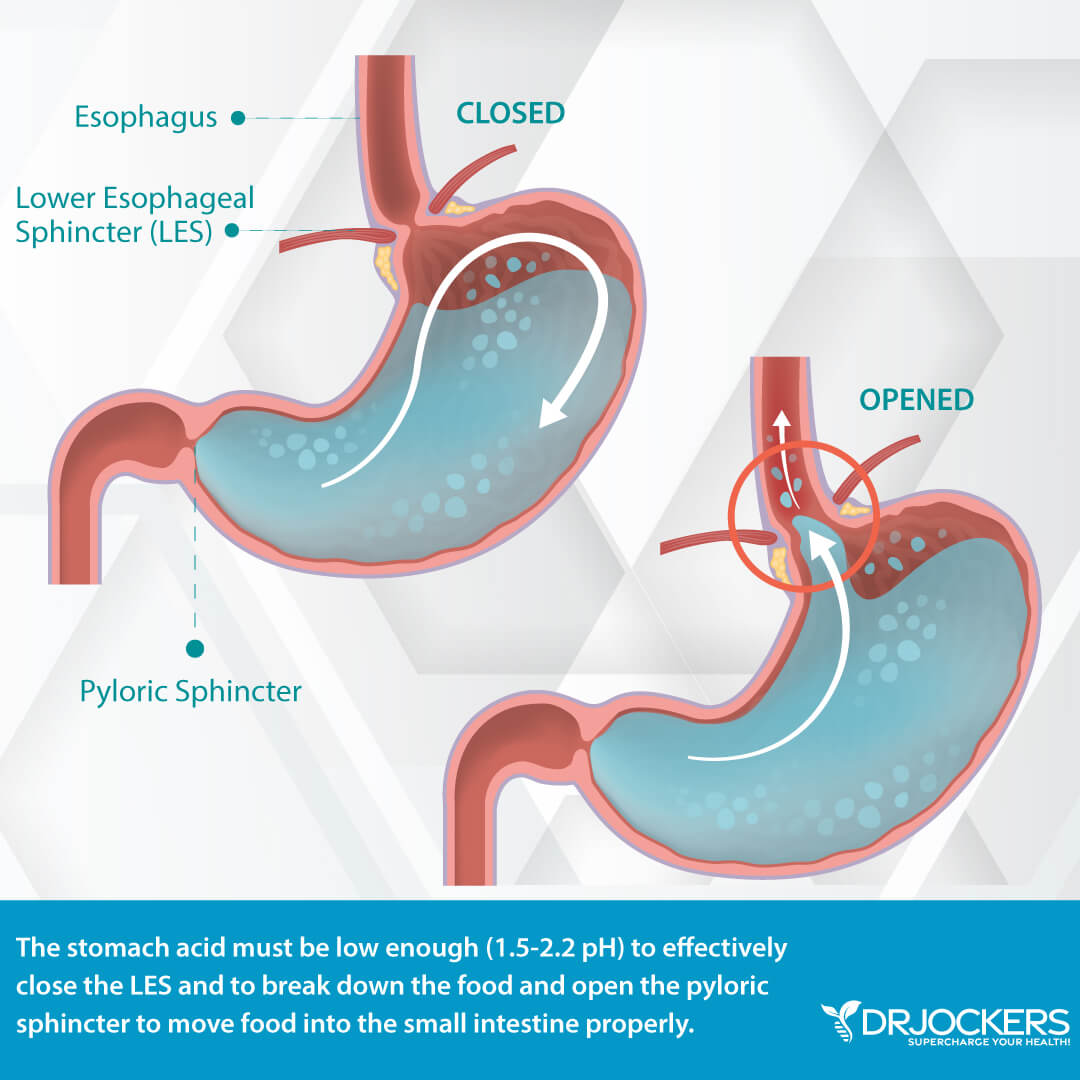
When it comes to acid reflux and silent reflux, the common misconception is that high stomach acid production is the problem, when in reality, low stomach acid is usually the culprit. But what is stomach acid? Stomach acid, or gastric acid, is one of the most important substances that help digestion.
Stomach acid is a digestive fluid created in your gut to help the digestion of food. Its main component is hydrochloric acid (HCL) along with potassium chloride and sodium chloride (6, 7). With the help of HCL, your stomach is able to transform a large solid meal into a semi-liquid soupy substance called chyme that can move through the rest of the digestion process without a problem.
However, if there isn’t sufficient HCL production or your body is unable to provide a healthy gut environment, your body cannot break food down properly. All this can lead to a backflow of acid and create symptoms of both GERD and silent reflux.
According to a 1986 study published in the Journal of the American Geriatrics Society, about 30 percent of people over 60 have atrophic gastritis, a condition characterized by no stomach acid production (8). On the other hand, a 2004 review published in the American Journal of Medicine has found that while stomach acid production decreases with age, the incidence and risk of reflux disorders increase with age (9).
Just think about it. If too much stomach acid was the culprit behind acid reflux and silent reflux, then we would see teenagers taking anti-acid medications, instead of middle-aged and older people who have much less stomach acid. These anti-acid medications would also be more effective than they are. The trust is that the real problem behind acid reflux and silent reflux is low stomach acid production.
Try the Baking Soda Test
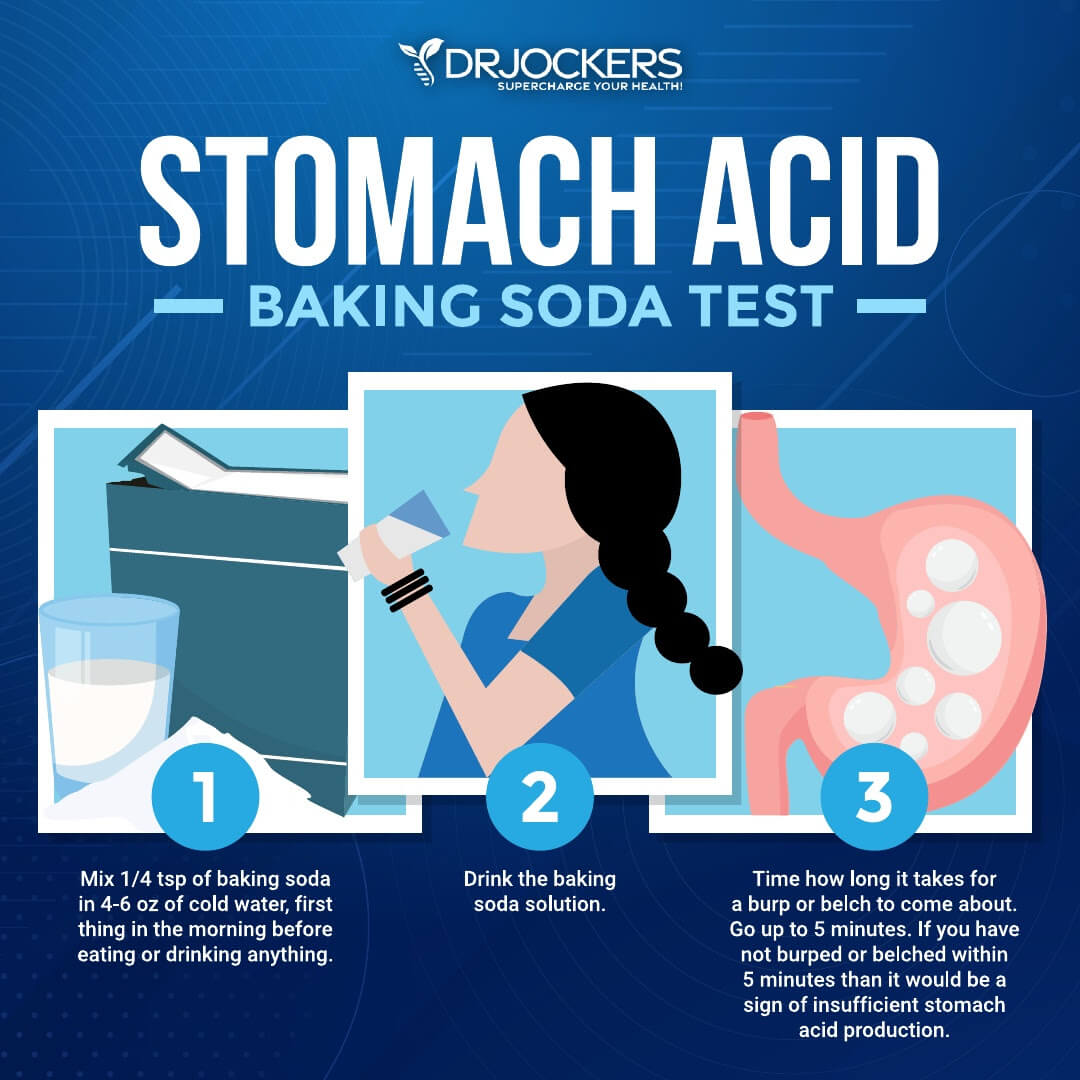
To test your stomach acid levels at home, I recommend taking the baking soda test. The baking soda test involves drinking baking soda and creating a chemical reaction within your stomach between the baking soda (sodium bicarbonate) and the hydrochloric acid (HCL). This normally results in carbon dioxide gas production which leads to burping. Don’t worry: it’s completely safe. Ingesting baking soda has been a natural remedy for upset stomachs for centuries.
The best part is that this test costs you about two or three dollars if you need to buy a new box of baking soda, so there is not much to lose. You can use the remainder of the box for baking, cleaning, or making natural DIY toothpaste. I recommend this test because of its safety and low cost and you could easily do it tomorrow.
However, this test is not perfect because there are a lot of variables to control. Trying to minimize all the variables can be tough and I recommend performing the test on three consecutive mornings to find an average. By repeating this test and looking at this average, you’re looking for more of a pattern than a one-time test of “yes” or “no.” Also, to increase the accuracy of the test, you must do it as soon as you wake up in the morning before eating or drinking anything.
There are no scientific studies proving this method as either reliable or unreliable. The results of this test can vary widely and it’s up to your interpretation, both of which are not ideal. Here is how to do the test:
- Mix 1/4 teaspoon of baking soda in 4-6 ounces of cold water first thing in the morning before eating or drinking anything.
- Drink the baking soda solution.
- Time how long it takes you to belch. Time up to five minutes.
If you have not belched within five minutes stop timing.
In theory, if your stomach is producing adequate amounts of stomach acid you’ll likely belch within two to three minutes. Early and repeated belching may be due to excessive stomach acid (but don’t confuse these burps with small burps from swallowing air when drinking the solution). Any belching after 3 minutes indicates a low acid level.
While this simple and affordable home test can guide you in the right direction, I always recommend that you visit your healthcare professional for further testing. Working with a functional health doctor can help you find other potential underlying issues and gut health problems that may be behind your silent reflux. My team and I are always happy to help your journey.
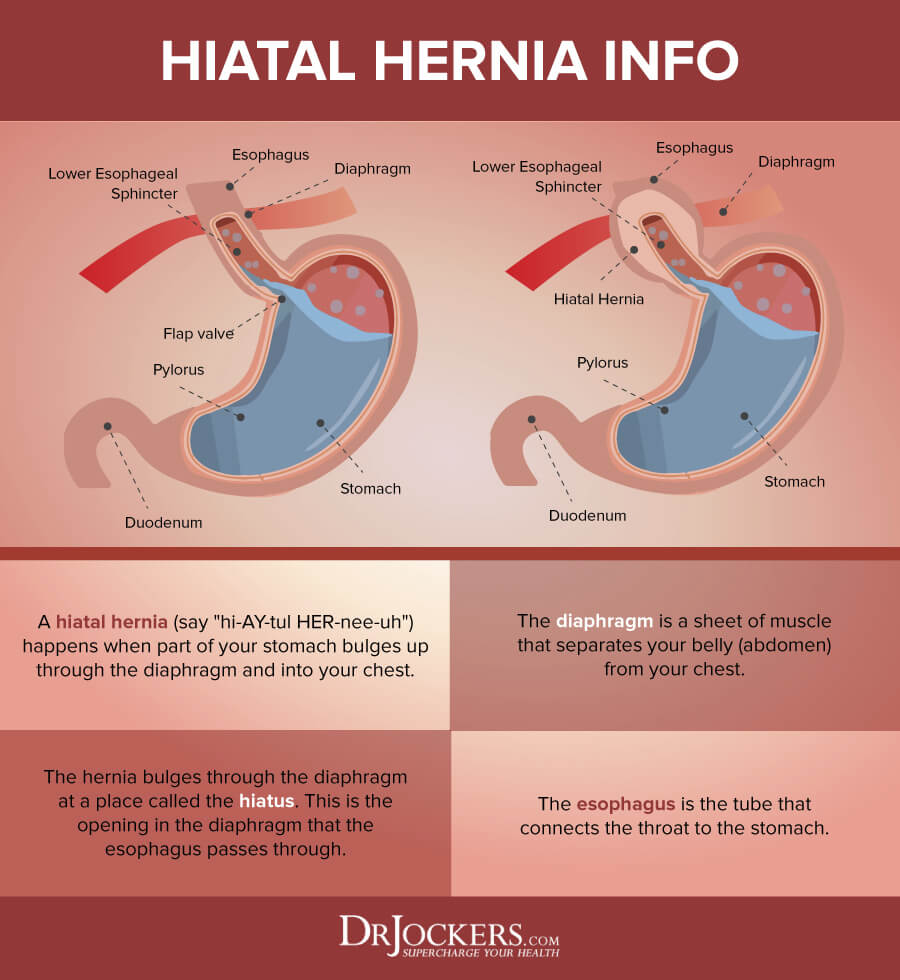
Hiatal Hernia
Hiatal hernia is a condition which your stomach pushes through an opening in your diaphragm and into your chest. While this sounds scary and painful, most people don’t notice any symptoms. It is usually discovered during a chest or abdominal x-ray, barium CT scan, or endoscopy. If you put your hand under your breast bone you may also feel a little bulge if you have a hiatal hernia.
Hiatal hernia can increase abdominal pressure which may also lead to discomfort, irritation, and symptoms of both acid reflux and silent reflux. A 2008 study published in the Journal of Gastroenterology found that 23 patients from the 167 participants with laryngopharyngeal reflux also had hiatal hernia (10). In these cases, addressing hiatal hernia is an important part of the treatment strategy.
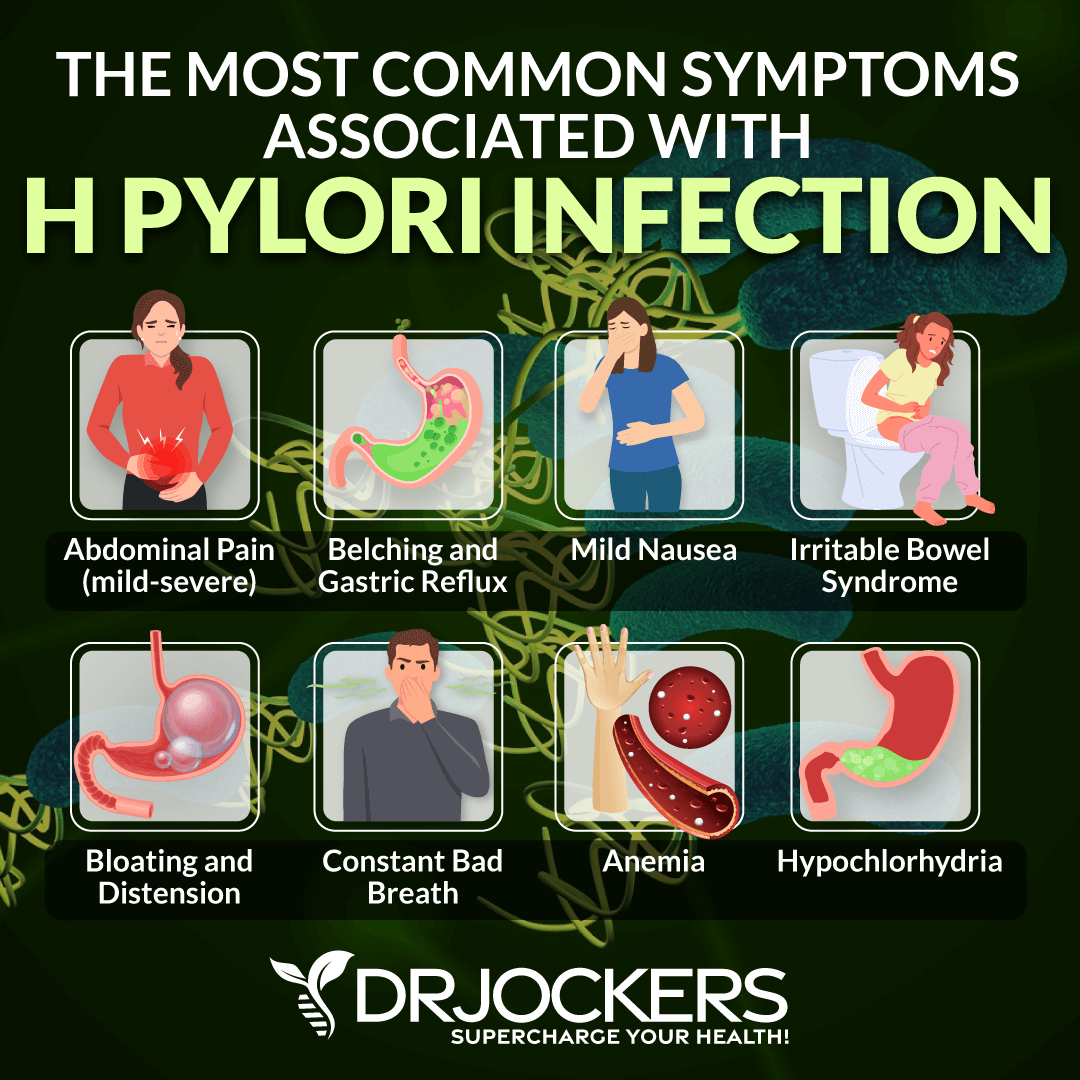
H Pylori Overgrowth
H Pylori is a very sophisticated microorganism that is able to survive in your stomach’s harsh and acidic environment. According to a 1995 review published in the Aliment Pharmacological Therapies, over 50 percent of the population is struggling with an overgrowth of H Pylori (11). H Pylori produces urease, an enzyme that breaks down the urea in the stomach into ammonia and carbon dioxide. This process can lead to belching and bad breath, both of which are signs of acid reflux.
Hydrochloric acid (HCL) is an acid that is necessary to create an acidic environment in your stomach to help digest protein, ionize minerals, stimulate bile, and metabolize fat. When your body is unable to release enough HCL, it will affect your digestion, protein absorption, and your ability to meet key dietary nutrients. The problem is that H Pylori disrupts the digestive process and interferes with HCL.
According to a 1997 study published in Gastroenterology, H Pylori disrupts stomach acid secretion which can lead to issues, including silent reflux (12). However, in a 1998 study published in the American Journal of Physiology, treating an H Pylori infection with antibiotics increased stomach acidity and reduced or eliminated symptoms (13). This indicates that addressing H Pylori overgrowth can reduce the risk of or improve silent reflux.
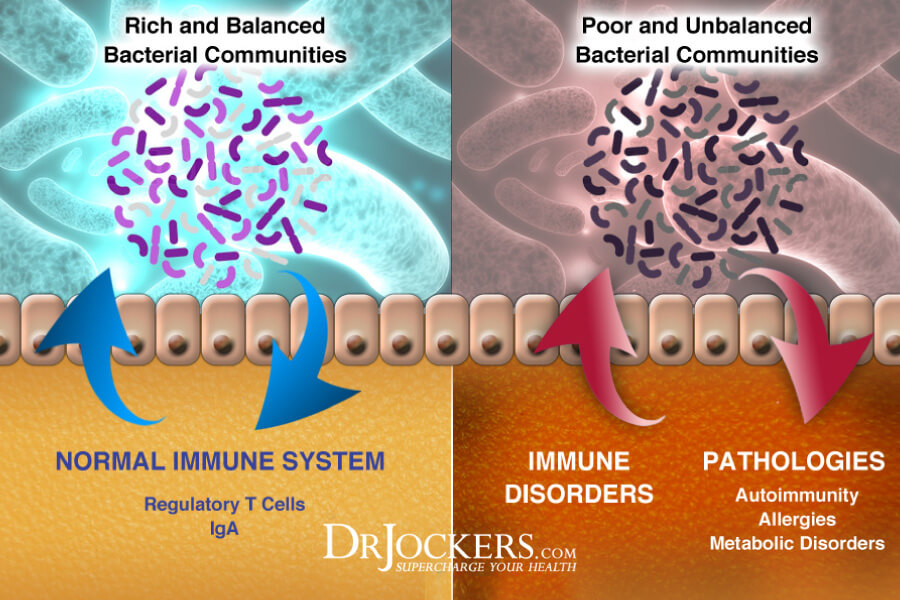
Gut Dysbiosis and SIBO
For a healthy body and healthy digestion, you need a healthy gut flora. When your gut microbiome is out of balance and there are too many bad bacteria and fungi and too few beneficial bacteria, gut dysbiosis occurs.
Gut dysbiosis can increase inflammation, gut health issues, chronic symptoms, and the risk of disease. Unlike your large intestines, your small intestine has relatively few bacteria. Small intestinal overgrowth (SIBO) refers to a condition when there is a bacterial overgrowth in your small intestines.
A 2019 study published in the Journal of Thoracic Diseases has found a connection between microbiome health and esophageal diseases (14). It turns out microbiome imbalance can lead to acid reflux and silent reflux. An overgrowth of bacteria in the small intestine can lead to extra gas that can lead to belching which is a common symptom of acid reflux.
SIBO can develop rapidly so SIBO-related acid reflux and silent reflux may develop quickly as well. If your silent reflux is related to SIBO, it is important that it’s not treated with Proton Pump Inhibitors (PPIs) as it can worsen the condition. If taking PPIs worsens your symptoms, it is a sign that SIBO is the root cause of your problem.
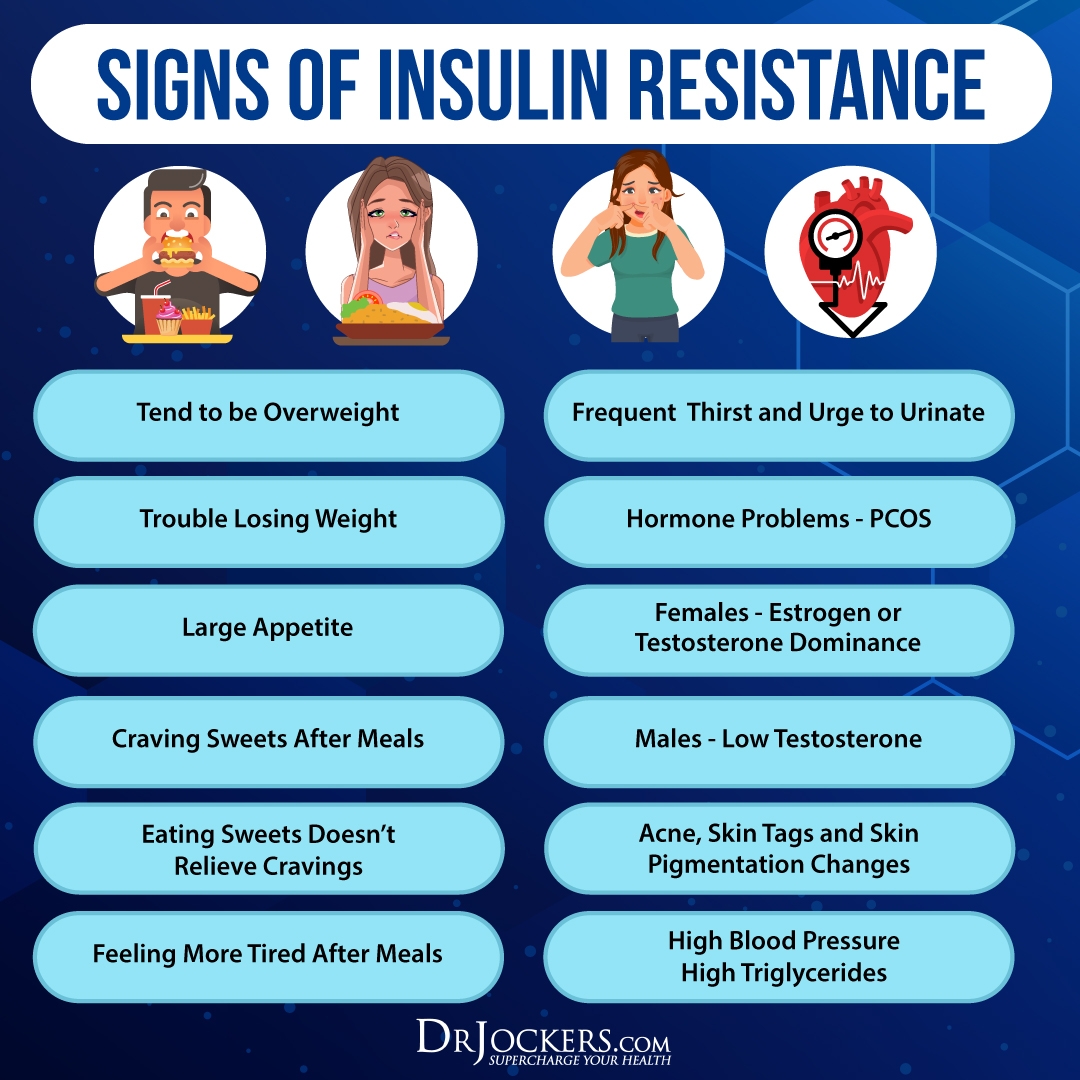
Insulin Resistance
Insulin resistance means that your body is unable to respond well to insulin and is unable to use glucose from your blood for energy. As a result, your pancreas will start to work extra hard to make even more insulin. This will lead to increased blood sugar levels over time. Insulin resistance increases your risk of prediabetes, diabetes, and related health issues. It may also increase your risk of silent reflux disease.
A 2011 study published in Aliment Pharmacological Therapies has found that insulin resistance can increase both the prevalence and severity of gastroesophageal reflux disease (15). Since acid reflux and silent reflux tend to develop because of the same reasons and sometimes occur at the same time, insulin resistance likely increases the risk of silent reflux as well. A 2013 study published in the Journal of Voice confirms this assumption by finding that patients with diabetes have an increased risk and prevalence of laryngopharyngeal reflux disease (16).
Natural Support Strategies for Silent Reflux
If you have silent reflux or are at risk of developing silent reflux, there are several natural support strategies you can try to support your health. This information has not been evaluated by the FDA and is not approved to prevent, treat or cure any health condition. This is for informational purposes only and does not replace the medical advice you get from your doctor.
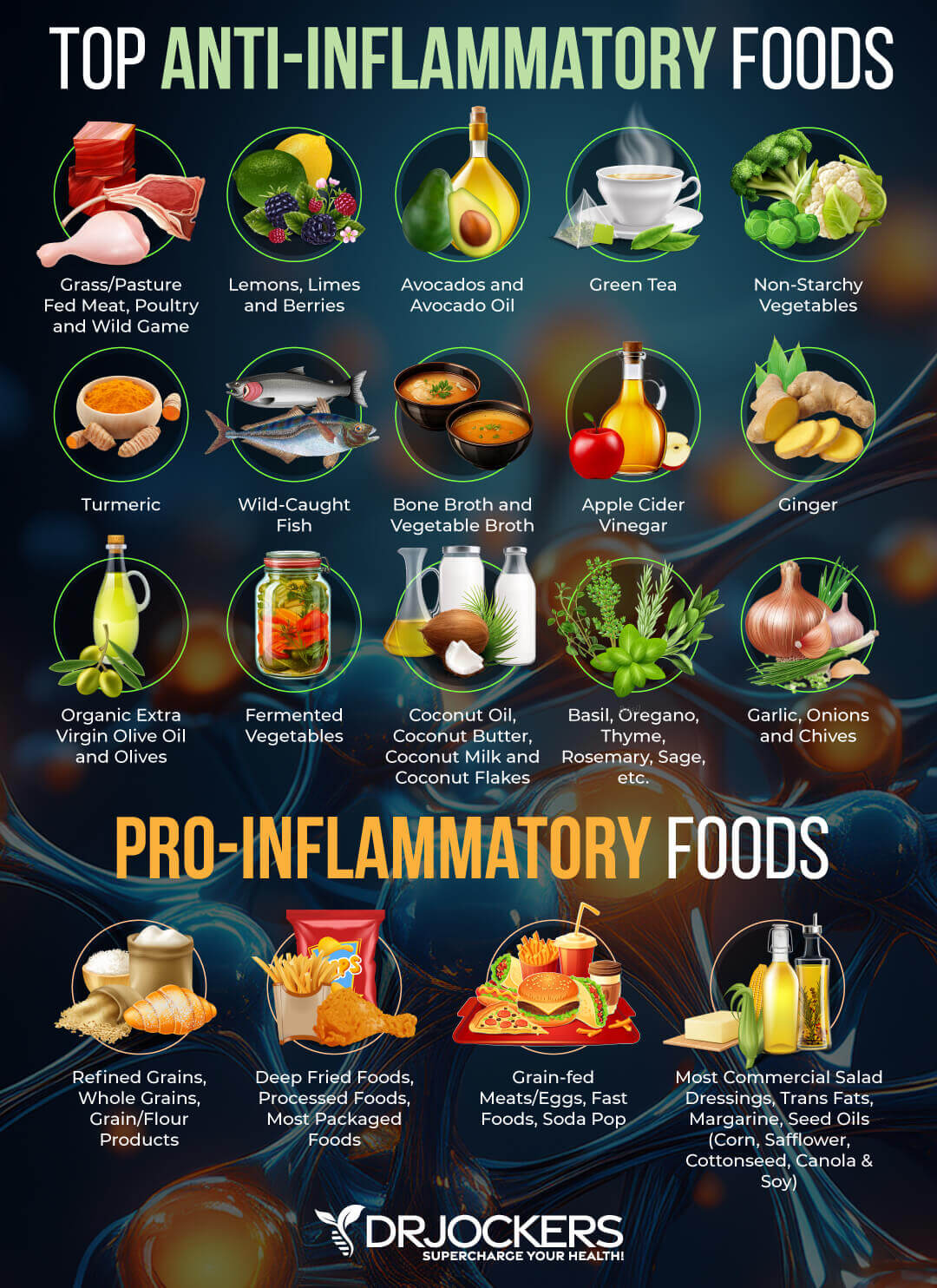
Anti-Inflammatory Nutrition Plan
A 2007 study published in the Journal of Clinical Biochemistry and Nutrition has found that pro-inflammatory factors, inflammation, and oxidative stress play a role in gastroesophageal reflux diseases and non-erosive reflux disease (NERD) (17). Furthermore, a 2019 study published in the Journal of Thoracic Disorders has found that diet may play a role in both the development and management of esophageal and reflux diseases (18).
For example, removing simple sugar, chocolate caffeine, alcohol, carbonation, mint, and spicy foods, avoiding large and calorie-dense meals, and not eating late at night may help to reduce the risk and improve symptoms.
An anti-inflammatory nutrition plan can help you achieve this goal and support your body. I recommend that you remove refined sugar, refined oils, deep-fried food, artificial ingredients, junk food, and highly processed foods.
Avoid any foods that may be a trigger, including spicy foods, carbonation, and food sensitivities. Focus on leafy greens, vegetables, low-glycemic index fruits, non-triggering herbs, healthy fats, and high-quality animal protein, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
Test for and Avoid Food Sensitivities
Food sensitivities are a huge problem and a silent trigger when it comes to silent reflux (4, 5). Common food sensitivities include gluten, sugar, soy, corn, shellfish, peanuts, and dairy. In silent reflux, chocolate, coffee, caffeine, alcohol, spicy foods, acidic foods, high-histamine foods, and carbonated drinks can lead to symptoms in many (18).
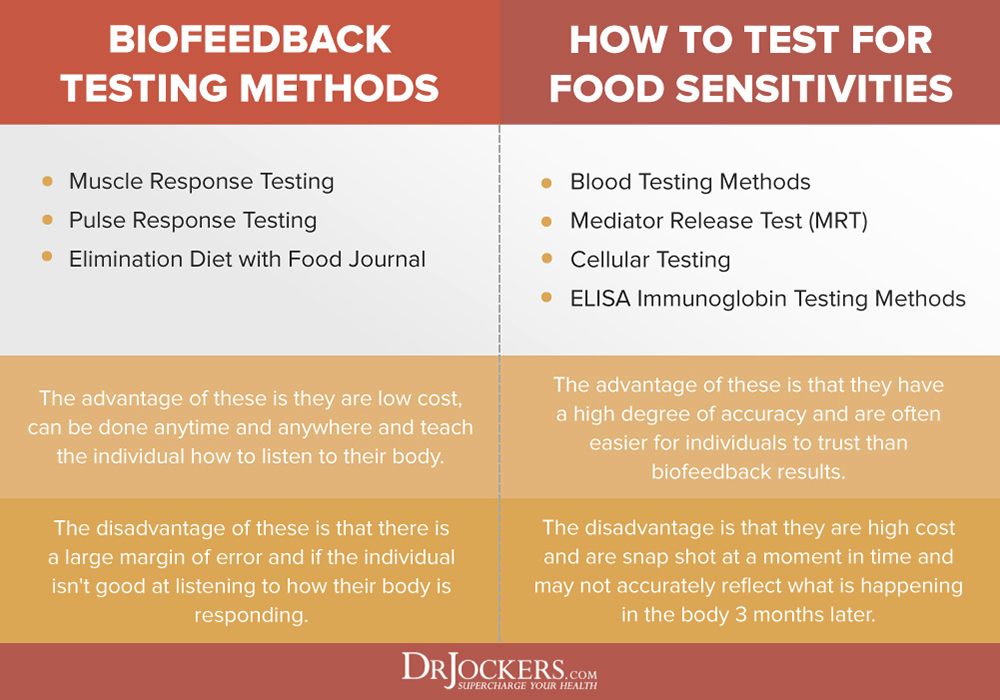
To find and avoid your personal food sensitivities, testing is very important. There are various blood tests that can help identify food sensitivities, however, they don’t test for every food, and false results can also happen. Additionally, I also recommend that you try an elimination diet, pulse test, or muscle response testing.
If you find any food sensitivities, it’s important that you remove these foods from your diet. Food sensitivities can change over time, so it’s important that you test for sensitivities regularly, once a year, or if new symptoms pop up. As you repair your body with a healthy diet and lifestyle, certain food sensitivities may also disappear and you may eventually be able to reintroduce some foods again. However, I recommend that you continue to avoid refined sugar, gluten, conventional dairy, food additives, and artificial ingredients.
Elimination Diet
Follow an elimination diet by removing all common and suspected food sensitivities from your diet for 2 to 3 weeks. Keep a food diary and note how your symptoms change or disappear. After 2 to 3 weeks, start reintroducing each food one by one. After introducing one food, wait for 2 to 3 days and watch for delayed reactions.
If you notice any symptoms of silent reflux or other health issues, remove this food. You may try to re-introduce it again to make sure it is a true sensitivity. If you find any sensitivities, make sure to remove them from your diet.

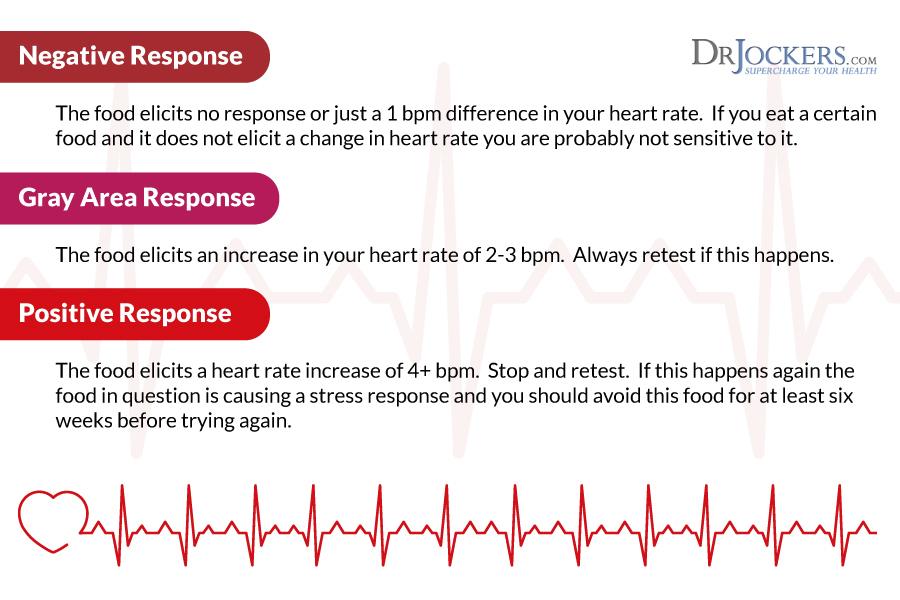
Pulse Test
Pulse testing is a biofeedback test for food sensitivities. Pulse testing measures the stress response caused by foods based on the increase in your heart rate. Problematic foods that cause food sensitivities activate the sympathetic branch of the autonomic nervous system, signaling a fight or flight response in the body and increasing blood pressure and heart rate. Measuring your pulse rate when exposed to specific foods can indicate whether the foods activate this stress response. If you don’t feel comfortable testing your pulse on your wrist, you can also purchase and use a pulse oximeter that records both your pulse and your oxygen concentration.
To try a pulse test, begin by sitting down and relaxing for a few minutes, then take 3 long deep breaths and afterward begin testing your resting pulse and get a number. Let’s say it is 60 beats per minute (bpm).
Next, take 3 long deep breaths again, take the food in question, place it on your tongue, and let it sit there for 20 seconds or do relaxed breathing, and then test your resting pulse again while in the same position. There should be no other variables that would affect your heart rate.
- Step 1: Sit down and relax for 5 mins
- Step 2: Take 3 long deep breaths
- Step 3: Test 60 second pulse rate and record
- Step 4: Take 3 long-deep breaths again
- Step 5: Put the food item in question on your tongue and wait for 20 seconds
- Step 6: Record your pulse with the food item still on your tongue
- Step 7: Check the difference between normal heart rate and food item challenged heart rate.
Negative Response:
The food leads to no response or just a 1 bpm difference in your heart rate. If you eat a certain food and it does not cause a change in heart rate you are probably not sensitive to it. However, if you still find this food triggering through daily experience or an elimination diet, it is best to avoid it.
Gray Area Response:
The food creates an increase in your heart rate of 2-3 bpm. Always retest if this happens.
Positive Response:
The food causes a heart rate increase of 4+ bpm. Stop and retest. If this happens again the food in question is causing a stress response and you should avoid this food.
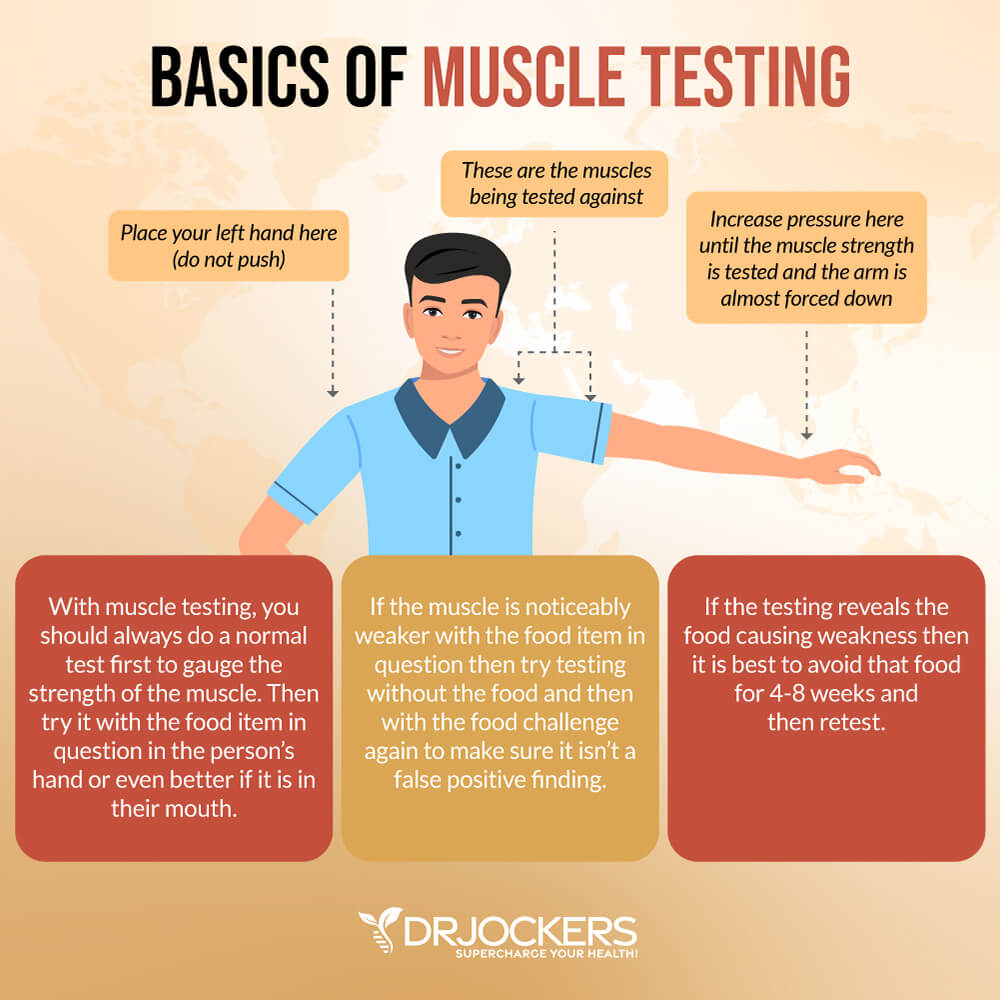
Muscle Response Testing
Nambudripad’s Allergy Elimination Techniques (NAET®) uses muscle response testing to confirm the presence of allergic reactivity. Changes in muscle strength are assessed while a person is exposed to food. Muscle weakness is thought to indicate that the food is problematic.
Once a food sensitivity or allergy is identified, NAET claims to be able to eliminate the allergy with chiropractic adjustments, acupressure and/or acupuncture, and energy balancing. The treatment strategy is to reprogram the brain’s negative responses towards food through desensitization.
However, muscle response testing does not look at immunoglobulins, the most important players in food sensitivities. This method is not generally accepted as an accurate test for food sensitivities, but it can still guide your journey.
If you try this method, it’s important that you check the results with the help of the other tests or by removing the food and checking for an improvement of symptoms. If you are still experiencing symptoms despite the NAET manipulation, continue to remove the triggering food from your diet.
Reduce Stress & Improve Sleep
We have learned from a 2007 study published in the Journal of Clinical Biochemistry and Nutrition that inflammation can play a role in reflux conditions (17). Chronic stress and poor sleep can increase inflammation and potentially contribute to the development of silent reflux. According to a 2018 study published in the European Archives of Otorhinolaryngology, there is a correlation between sleep apnea, poor breathing due to sleep disorders, and silent reflux (19).
I recommend that you reduce your stress levels and improve your sleep to improve your health and symptoms. Try meditation, guided relaxations, visualization, breathwork, gratitude, journaling, coloring, and yoga to reduce your stress levels. Approach life from a positive lens and work on an optimistic mindset. Spend time in nature and try grounding.
Seek out a supportive community, spend time with friends and family, and designate regular ‘me-time’ as well. Seek support from a therapist, counselor, life coach, or spiritual counselor if you need further support or strategies.
Commit to a regular sleep time by going to bed and waking up around the same time regularly. This will help to support your circadian rhythms. Avoid electronics, sugar, caffeine, heavy meals, and stress close to bedtime. Seek relaxing activities, such as taking a calming bath, reading, meditation, coloring, journaling, calm conversations, or prayer before bed. Make sure that your bedroom is a calm sanctuary with comfortable pillows and bedding, a supportive mattress, and blackout curtains.

Test for and Reduce Gut Infections
As you know, H Pylori overgrowth, SIBO, and gut dysbiosis may be the culprit behind your issues (11, 12, 13, 14). Testing for these gut infections with a GI Map Stool Test or other high-quality stool testing is important.
Working with a functional health professional can help you create a dietary protocol and recommend supplementation to reduce your specific gut infections. My team and I are always happy to help. You can also search my website for these specific issues to find my recommendation.
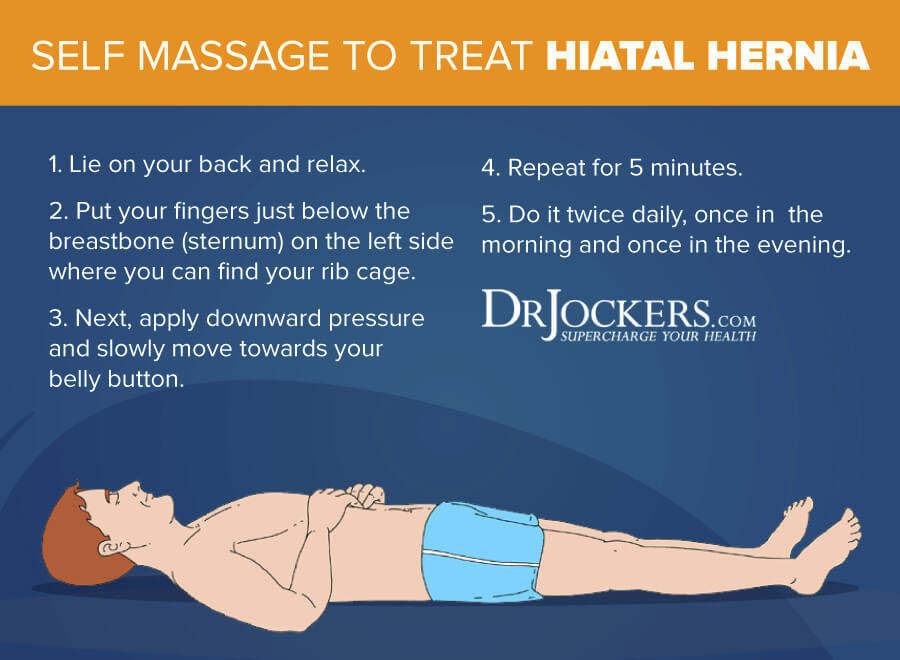
Reduce Hiatal Hernia If You Have It
We know from a 2008 study published in the Journal of Gastroenterology that hiatal hernia may cause silent reflux (10). To reduce hiatal hernia, you may try a variety of strategies.
Self-Massage
Practicing abdominal self-massage on the upper portion of your stomach may help with discomfort and symptoms:
- Relax and lie on your back.
- Place your fingers just below the breast bones (sternum) where you can find your rib cage.
- While applying downward pressure slowly move towards your belly button.
- Repeat for 5 minutes.
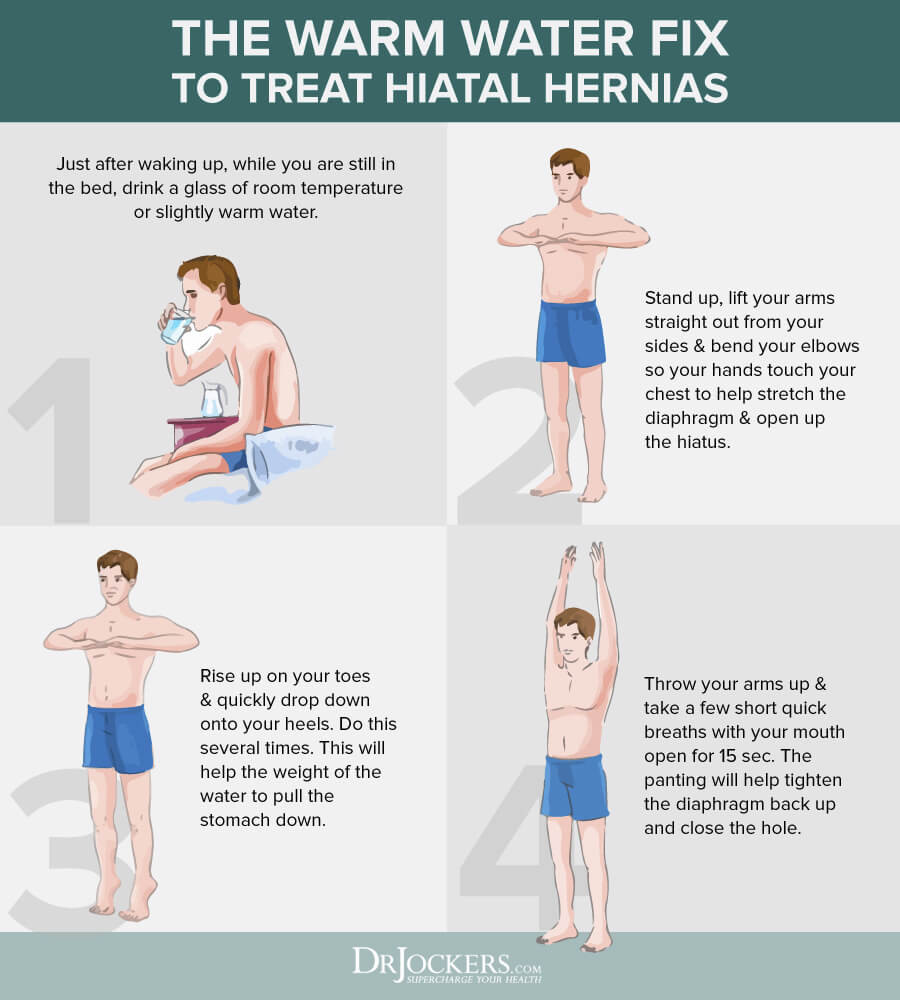
The Warm Water Fix
Drinking warm water and performing certain exercises in the morning may also help your symptoms:
- While you are still in bed, just after waking, drink a glass of slightly warm or room temperature water. This will relax the stomach muscles and the diaphragm and put some weight on the stomach.
- Stand up, while lifting your arms straight out from your sides bend your elbows, so your hands touch your chest. This opens the hiatus and stretches the diaphragm.
- Rise up on your toes as high as possible, while quickly dropping on your heels. Doing this several times in a row will allow the weight of the water to pull the stomach down.
- Standing with your arms up, take a few short, quick breaths with your mouth open for about 15 seconds. The panting will help to tighten the diaphragm back up and close the hole.
Yoga
Practicing the Chair pose may help your condition, however, avoid Cow, Bow, and Bridge poses:
- Begin by standing with your back straight and your arms perpendicular to the ground. Keep your feet about a hips-width apart.
- Raise your arms above your head
- While bending your body forward to a 45-degree angle, bring your chest toward your thighs. Keeping your arms out straight, aligned with your back, turn your palms to face the floor.
- Gently bend your knees like you were about to sit in a chair.
- Pressing your weight toward the floor look forward. Hold this position for a few seconds, taking several deep breaths.
- While pressing your shoulder blades to your back, lower your tailbone towards the floor and pull in your abdomen. Focus on your breathing and hold this position for at least 30 seconds.
- Straighten up slowly.
- Repeat this cycle a few more times.

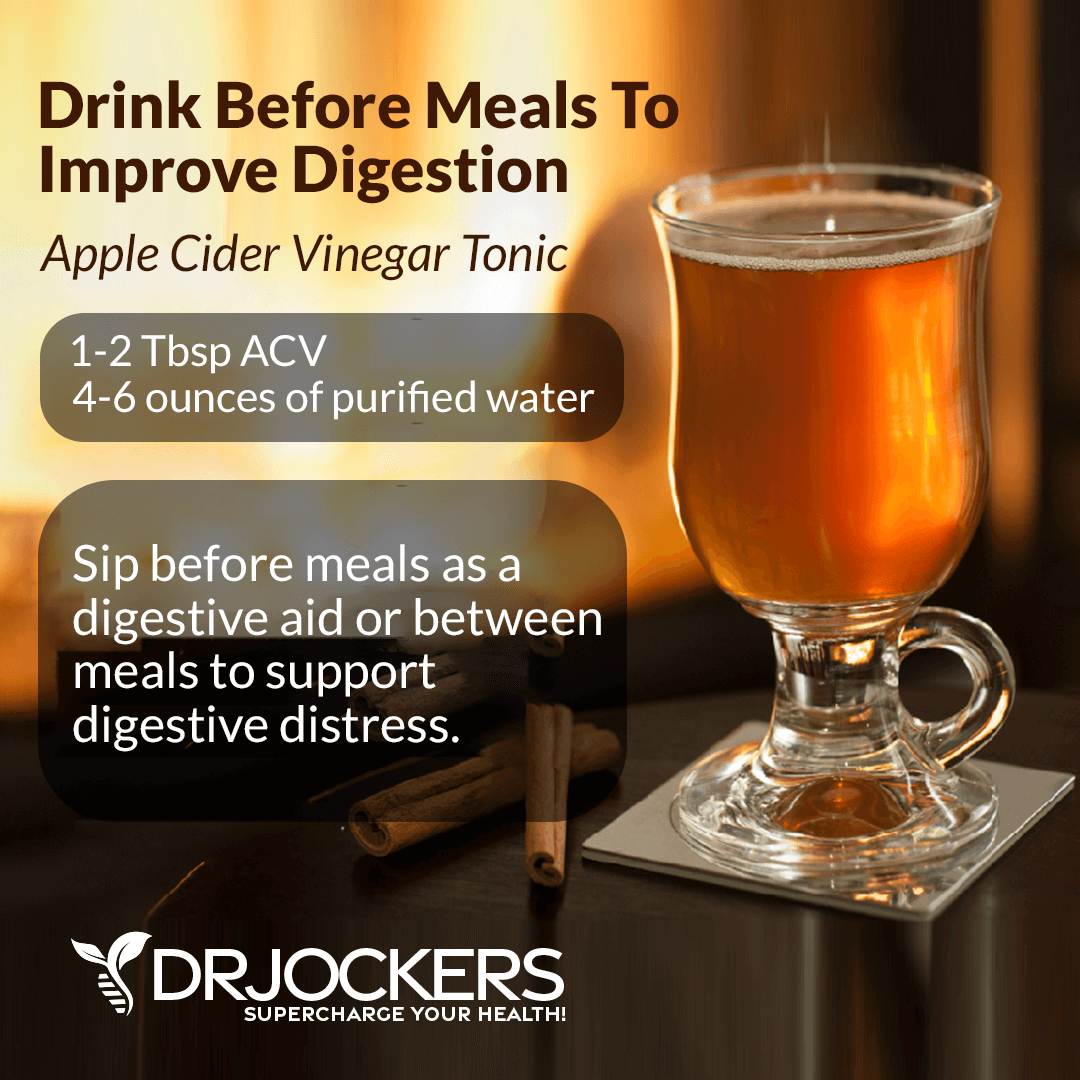
Apple Cider Vinegar
Apple cider vinegar can help with symptoms of heartburn and may help with silent reflux as well. However, make sure it is not triggering:
- Add 1 to 2 teaspoons of raw, unfiltered apple cider vinegar to a glass of warm water.
- Sip it slowly before meals.
- Repeat this whenever you have heartburn or acidity.
Chamomile
Chamomile has anti-inflammatory properties that can calm your stomach muscles:
- Mix 1 teaspoon of dried chamomile in a cup of water.
- Cover and let steep for 5 minutes.
- Strain and add honey.
- Slowly sip a cup of chamomile tea, up to 4 times daily between meals.

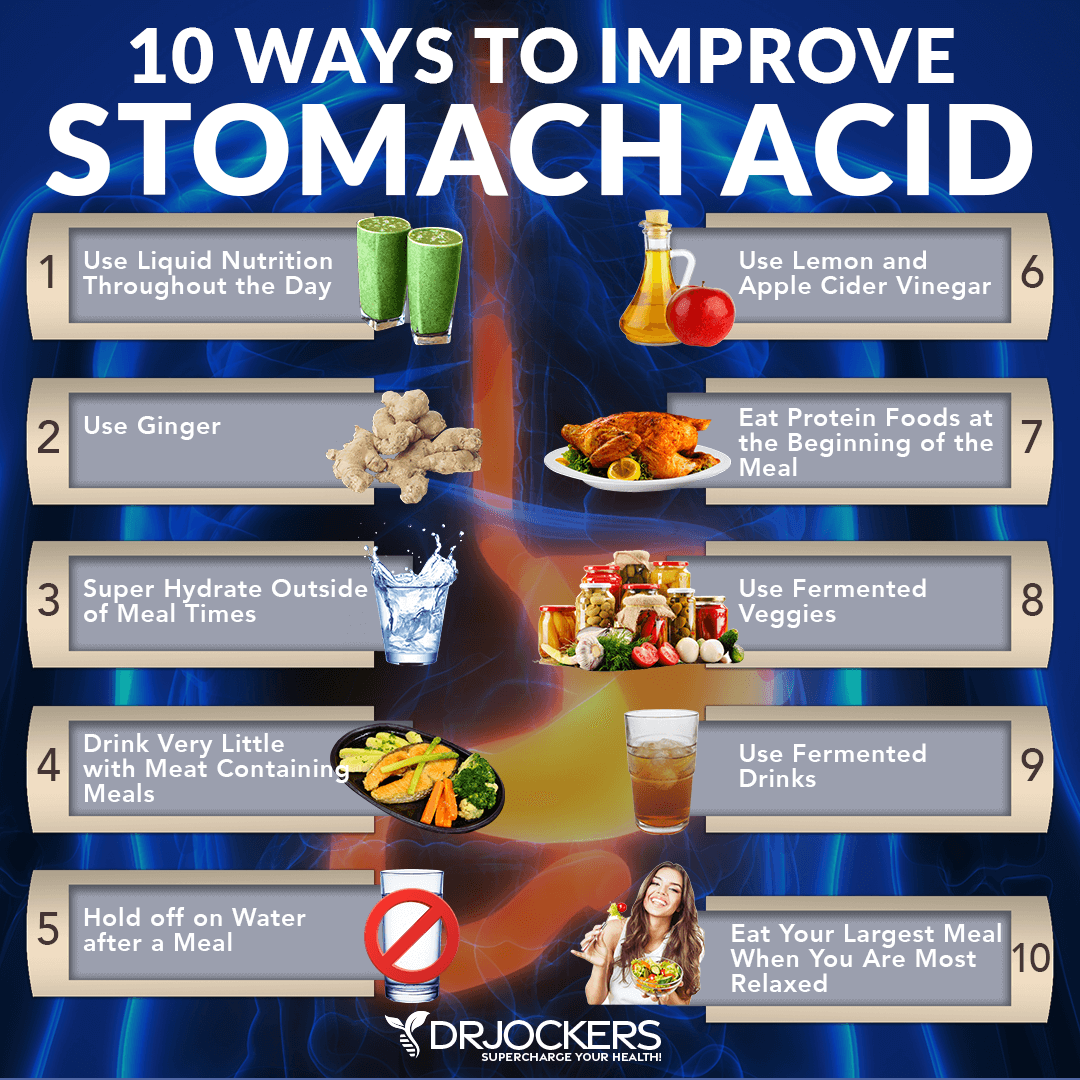
Improve Stomach Acid Levels
The culprit behind silent reflux is usually low stomach acid levels, so improving your stomach acid levels is critical (6, 7, 8, 9). To improve your stomach acid levels, I recommend the following:
- Use Liquid Nutrition Throughout the Day: Try to make sure that at least half of your meals are in a liquid form such as a protein shake or green smoothie. Protein shakes are pre-metabolized and very easy to digest and do not depend upon HCL production. If you have low HCL it may be helpful to drink one to two protein shakes daily to support amino acid absorption, reduce extra stress on your digestion, and support healthy stomach acid levels.
- Use Ginger: Ginger is one of the best things for improving digestive juices. I recommend drinking 2 to 3 cups of ginger tea each day, you can put ginger essential oil in water (2 to 3 drops in 8 oz of water), juice a ½ inch of fresh ginger root in green juice each day, and use ground ginger on your foods. You can also add fermented ginger to your diet which is common in Asian dishes such as kimchi. Since spicy foods can be triggering for silent reflux, make sure that it is not triggering for you. If it is, focus on the other steps.
- Super Hydrate Outside of Mealtimes: Good hydration can help activate bowel motility and push contents through the digestive system which will reduce microbial fermentation and toxicity in the body. This can help to support your stomach acid levels.
- Drink Very Little with Meat Containing Meals: When you are eating meat or any sort of heavier food, you should stop drinking water or other liquids at least 30 minutes before the meal, except if you need to take a supplement with 2 ounces of water. Holding off water during these meals will reduce any potential dilution of the gastric juices and allow for better digestion.
- Hold Off on Water After a Meal: To allow for optimal digestion, I also recommend not drinking water or other liquids until at least 30 minutes after a meal. This allows for proper stomach acid activity, sterilization, and protein metabolism.
- Use Lemon and Apple Cider Vinegar: Squeezing fresh lemon or using lemon juice or apple cider vinegar on your meat and vegetables helps to pre-metabolize the food and support better digestion and nutrient absorption. You can either marinate foods in a lemon or ACV base or just add them as a dressing right before you consume them. Again, make sure that apple cider vinegar is not triggering your silent reflux symptoms and if it is, focus on my other recommendations.
- Eat Protein Foods at the Beginning of the Meal: The stomach will begin churning out its stomach acid when you begin eating, especially when you are consuming protein. While it’s culturally common to have a salad before their protein dish, this is not great for your HCL production. It is a much better idea to eat your protein with salad or vegetables instead of after.
- Use Fermented Veggies: Fermented foods such as sauerkraut, kimchi, pickles, pickled ginger, and other fermented vegetables all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions I recommend using one of these with all of your heavier meals, and especially any meal with protein.
- Use Fermented Drinks: Fermented drinks such as apple cider vinegar, coconut kefir, and kombucha offer anti-microbial benefits and help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Keeping H Pylori levels down is critical for the body to be able to produce enough stomach acid.
- Eat Your Largest Meal When You Are Most Relaxed: Your body needs to activate the parasympathetic nervous system to produce enough stomach acids. If you are busy and on the go, you will be in fight or flight sympathetic mode. If you struggle with low stomach acid, this fight or flight state is not going to allow your body to produce anywhere near enough. Relaxing before the meal is important to improve stomach acid production.
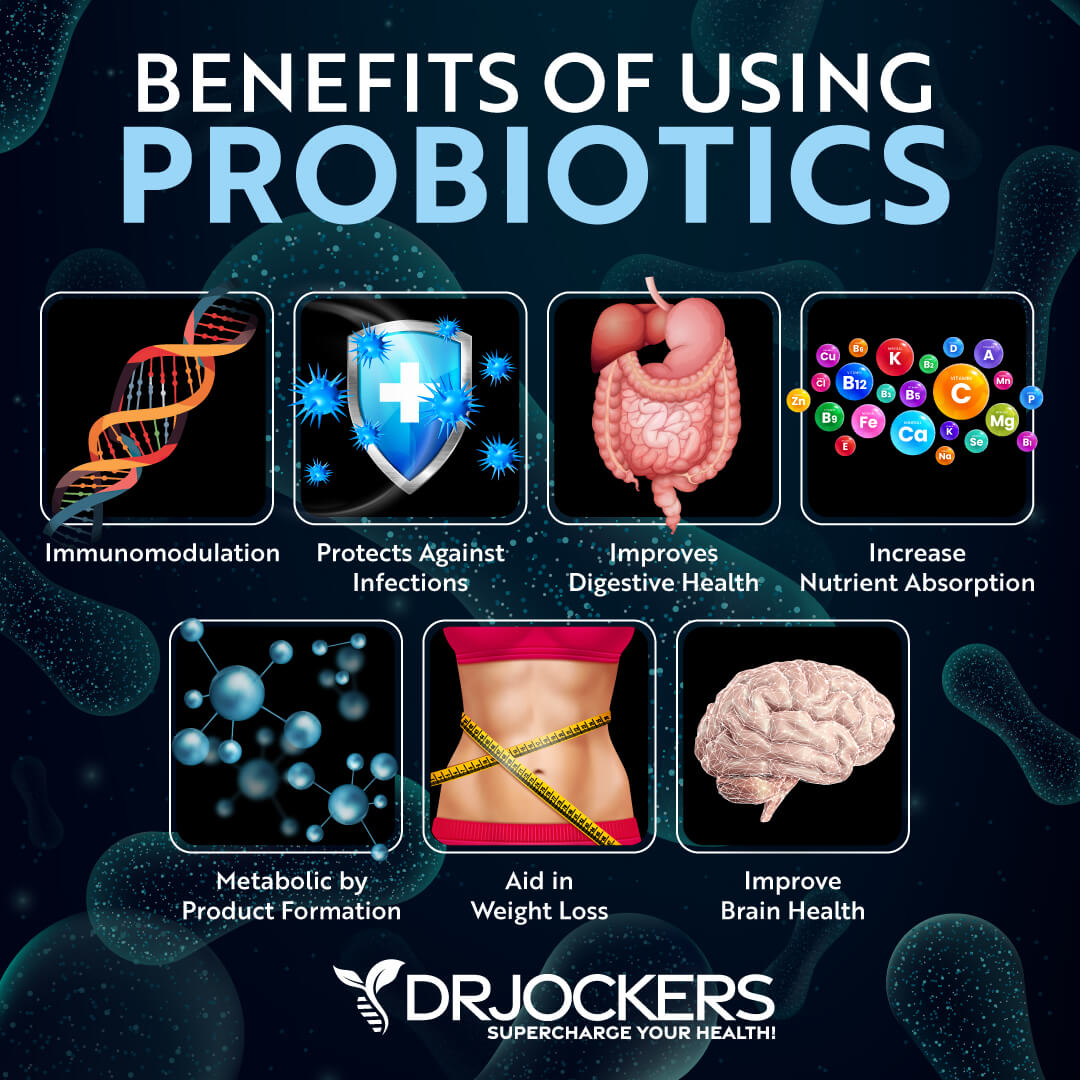
Use Probiotics and Digestive Enzymes
A poor gut microbiome and bad bacteria overgrowth can contribute to the development and symptoms of silent reflux (11, 12, 13, 14). Probiotics may be able to help. According to a 2020 systematic review published in Nutrients, probiotics may alleviate the symptoms of GERD and acid reflux (20). They may also help with silent reflux.
I recommend eating probiotic-rich foods, such as sauerkraut, fermented vegetables, kimchi, and coconut kefir and to support these probiotics, eat prebiotic-rich foods as well, including jicama, Jerusalem artichokes, dandelion greens, and apples. Additionally, take a high-quality probiotic supplement to support your microbiome. If you have SIBO, make sure to choose soil-based probiotics as certain good bacteria in other probiotics may be triggering SIBO.
Gut microbiome imbalance and H Pylori overgrowth can interfere with the production of digestive enzymes and are commonly seen in silent reflux and acid reflux (12). To further support your digestion and absorption, I also recommend the use of digestive enzymes before each meal.
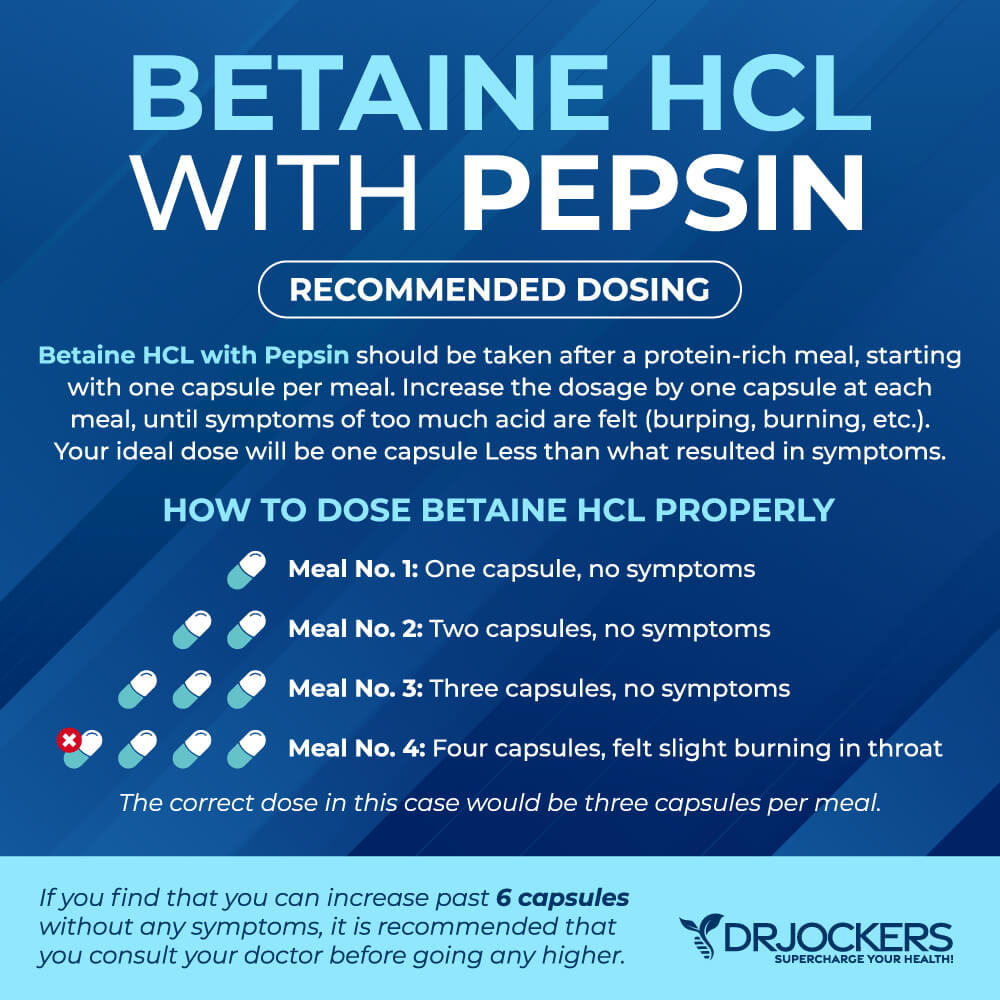
Consider Using Betaine HCL
Betaine Hydrochloride (Betaine HCL) helps to increase stomach acid, promote a healthy stomach pH, support nutrient and protein absorption, and reduce symptoms of acid reflux and silent reflux.
According to a 2016 case report published in Integrative Medicine (Encinitas), betaine HCL may help patients with gastroesophageal reflux, irritable bowel syndrome, and hypochloremia (21). I recommend daily supplementation with betaine HCL for silent reflux.
Consider Using Aloe Vera, Ginger, and Licorice Root
Using aloe vera, ginger, and licorice root may also help with silent reflux. A 2015 pilot randomized positive-controlled trial has found that aloe vera may be a safe and effective treatment for the symptoms of reflux disease (22). Ginger is an anti-inflammatory herb that can reduce inflammation and irritation. According to a 2018 systematic review of clinical trials published in Food Science and Nutrition, ginger can be beneficial for gastrointestinal disorders, including gastroesophageal and silent reflux (23).
Furthermore, in a 2013 study published in Clinical and Experimental Gastroenterology, licorice root may also be beneficial in the treatment of reflux diseases (24). You may use these herbs by drinking aloe vera juice, drinking ginger or licorice tea, or using it as a supplement for reflux and digestive disorders.

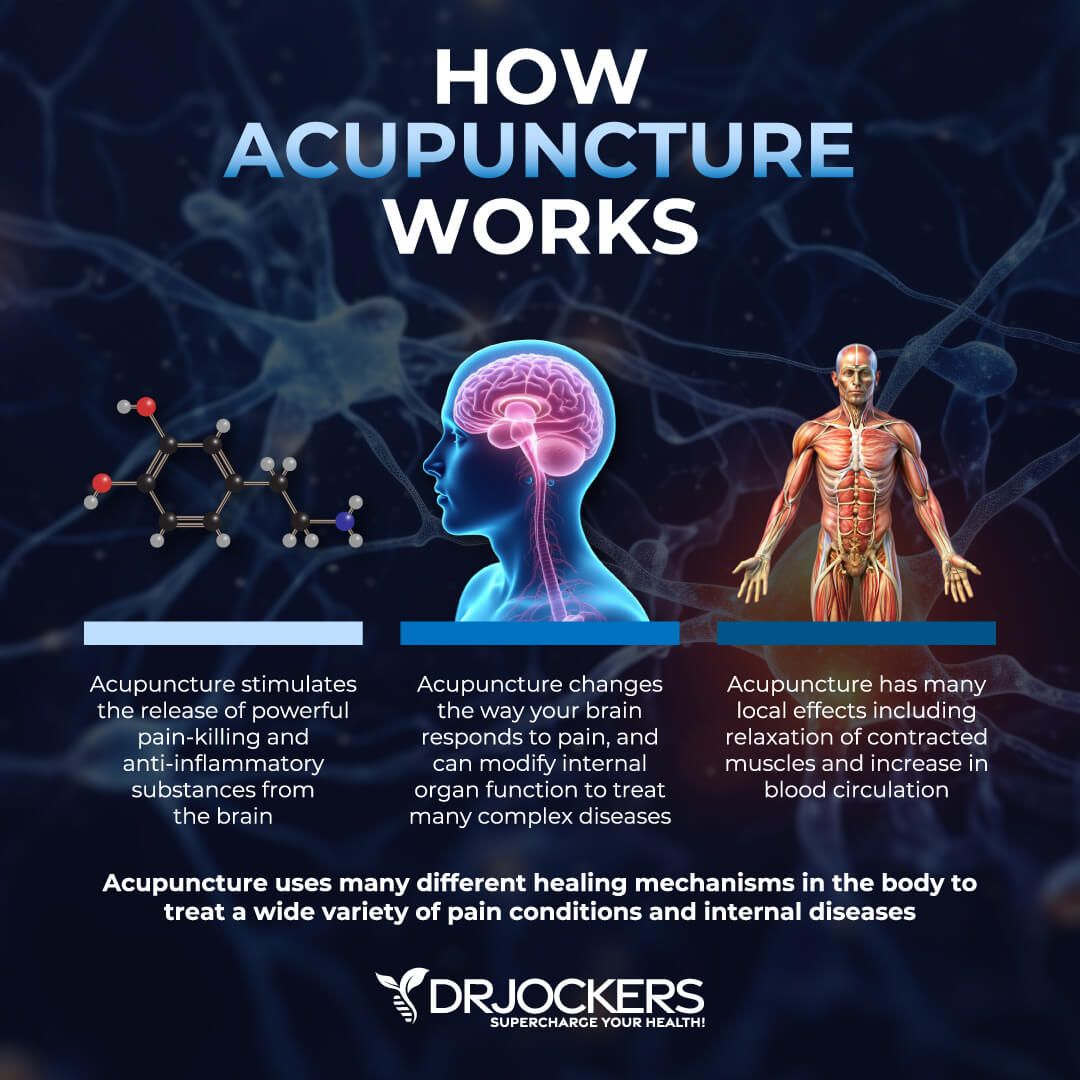
Consider Using Acupuncture
Acupuncture is an alternative medicine technique that helps to restore the flow of energy inside your body by using thin needles placed in specific points of your body. A 2010 randomized controlled clinical trial published in the Chinese Journal of Integrative Medicine has found that acupuncture may be an effective treatment method for gastroesophageal reflux (25).
This indicates that it may be beneficial for silent reflux as well, which is supported by a new study. A 2020 Chinese randomized controlled clinical trial published in Zhongguo Zhen has found that acupuncture may help silent reflux (26). Getting acupuncture treatments may help to restore your health and reduce symptoms of silent reflux.
Final Thoughts
Laryngopharyngeal reflux (LPR) or silent reflux is caused by the backward flow of stomach acid affecting the lower part of your throat and voice box causing irritation, a burning sensation, sore throat, hoarseness, coughing, and other symptoms. Untreated silent reflux can result in serious complications including increased risk of the oral cavity, lung, and breathing disorders, recurrent pneumonia, and increased risk of laryngeal and esophageal cancer.
Fortunately, it is possible to support your health naturally to reduce risks and complications. I recommend that you follow my natural support strategies for silent reflux to improve your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



This article is FANTASTIC! I’ve suffered with LPR for many years…This article pretty much sums up ALL the things you can do to help restore your throat – Bookmarking this page, as always a good reminder, and to forward to others i know suffering…Great Job!!
Glad to hear this Anthony!
An excellent dissemination work on how to improve digestive health, with simple and very practical recommendations
Thanks for your work