 Stomach Ulcers: Causes and Natural Support Strategies
Stomach Ulcers: Causes and Natural Support Strategies
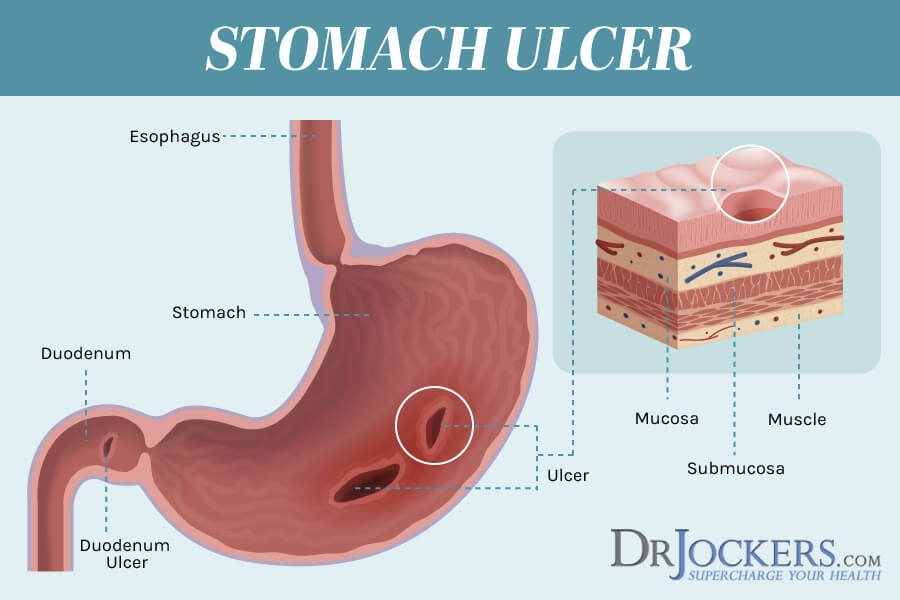
Ulcers are wounds that create small openings within the mucosa that lines the stomach or intestines. Ulcers form when any combination of excess gastric acids, bacteria, drugs or other toxins cause injury and small openings in the mucosa. In this article, you will discover the major causes of stomach ulcers and natural support strategies to help your body heal.
Stomach ulcers are also known as gastric ulcers. They are painful sores in the stomach lining. Stomach ulcers are a type of peptic ulcer disease. Any ulcer that affects both the stomach and the small intestine is known as a Peptic ulcer.
When the thick layer of mucus that protects the stomach from digestive juices is reduced a stomach ulcer can occur. The digestive acids eat away at the tissues that line the stomach, causing an ulcer.
Over 25 million Americans will have a peptic ulcer at some point in their lifetime. People of all ages suffer from ulcers. Men and women are equally affected. Research shows that about 60 percent of peptic ulcers are caused by a bacterial infection that can usually be cured. Another 20 percent are caused by non-steroidal anti-inflammatory drugs, lastly 20 percent are caused by miscellaneous causes such as smoking cigarettes or no known cause (1).
Different Types of Ulcers
The most common type of ulcers are Peptic ulcers, but there are many types of ulcers including:
- Arterial ulcers are open sores that develop on the outer side of your feet, ankle, heels and toes.
- Venous ulcers ‘are the most common type of leg ulcers. They are an open wound that forms on your leg, below your knee and the inner area of your ankle.
- Mouth ulcers are lesions or small sores that develop in the mouth or the base of your gums.
- Genital ulcers are sores that develop on genital areas.
Sores or wounds that develop on the inside lining of your stomach, the upper portion of your small intestine, or your esophagus are referred to as Peptic ulcers. They form when digestive juices damage the walls of your intestine or your stomach (2).
There are three different types of peptic ulcers:
- Duodenal ulcers are ulcers that develop in the duodenum (small intestine)
- Gastric ulcers are ulcers that develop in the stomach lining.
- Esophageal ulcers are ulcers that develop in the esophagus.
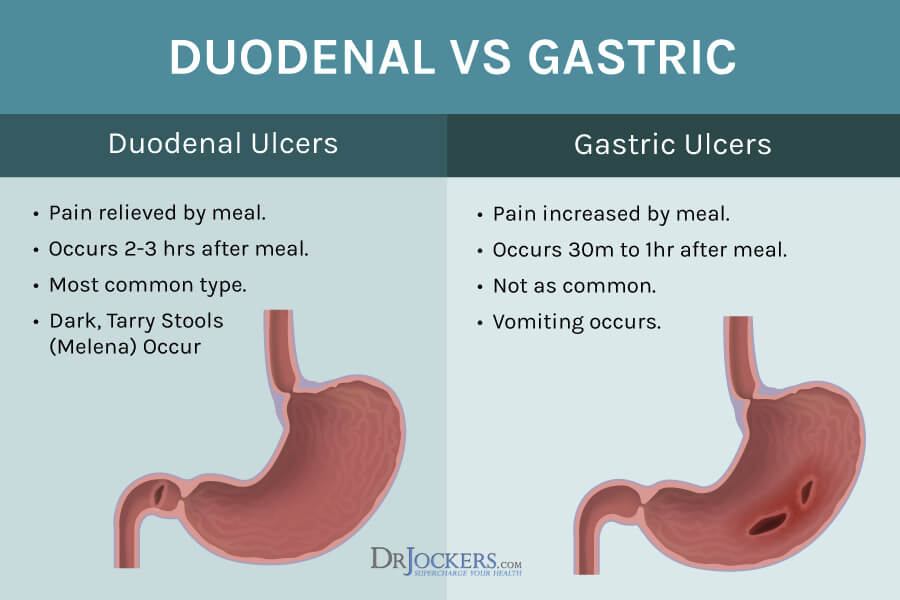
Differences between Stomach Ulcers and Duodenal Ulcers
Stomach ulcers (frequently called peptic ulcers) are painful sores that develop in the lining of your digestive system. Traditionally, they form in the stomach, but they may also develop in the small intestine (the portion called the duodenum) or the esophagus. Gastric and duodenal ulcers are two of the types of peptic ulcers that we will be discussing. There are many symptoms associated with stomach ulcers. The severity of the symptoms depends on the severity of the ulcer.
Ulcers can cause many symptoms, some that are mild and infrequent or others that cause a lot of pain and linger. Symptoms of ulcers are usually painful and noticeable. A high percentage of duodenal ulcers become severe.
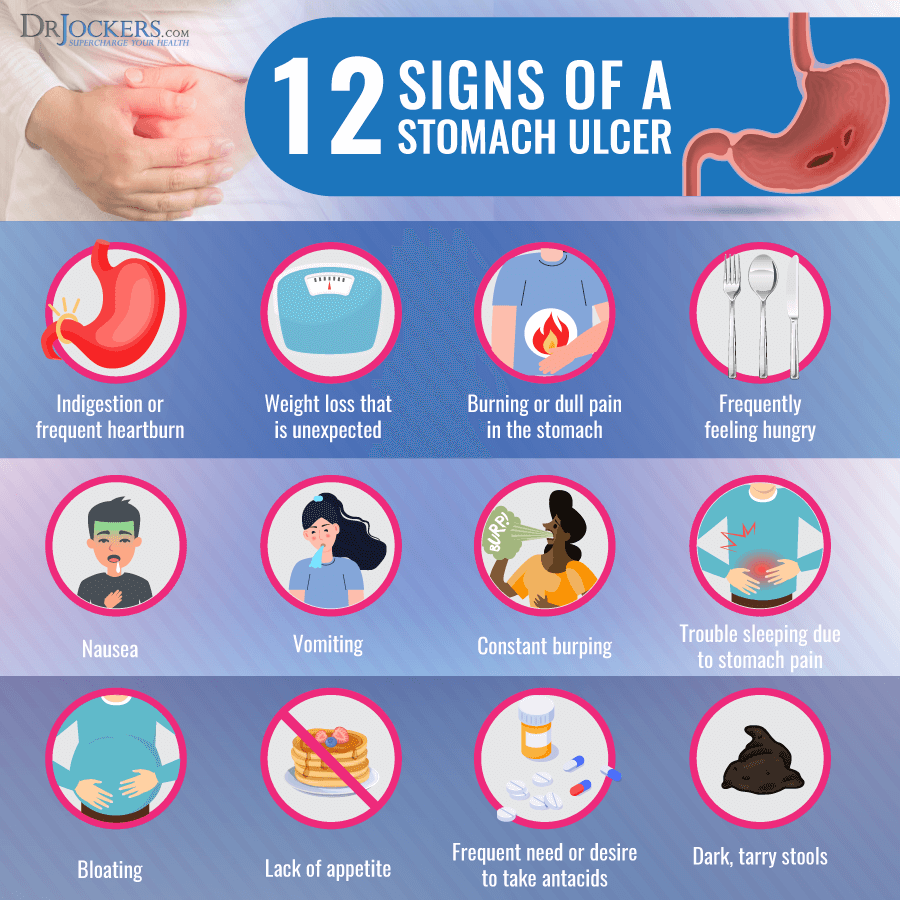
A common symptom is a burning sensation or pain in the middle of the stomach between your chest and your belly button.
Other Common Signs and Symptoms of Ulcers Include:
- Weight loss
- Dull pain in the stomach
- Nausea or vomiting
- Burping or acid reflux bloating
- Not wanting to eat because of pain.
- Feeling easily full
- Heartburn, a burning sensation in the chest
- Anemia
- Dark, tarry stools
- Vomit that is bloody or looks like coffee grounds.
- Pain that may improve with eating, drinking or taking antacids.
- Trouble sleeping due to pain.
- Dehydration, weakness and fatigue (when the intake of food is decreased due to pain)
- Diarrhea
- Bleeding when going to the bathroom.
- The risk of perforation of the organ lining (this is a life-or-death emergency)
In my opinion the primary difference between stomach ulcers and duodenal ulcers is that with stomach ulcers the pain increases with eating because the acid irritates the ulcers and with duodenal ulcers there is more pain between meals. In duodenal ulcers, it is common for the pain to go away when the individual eats.
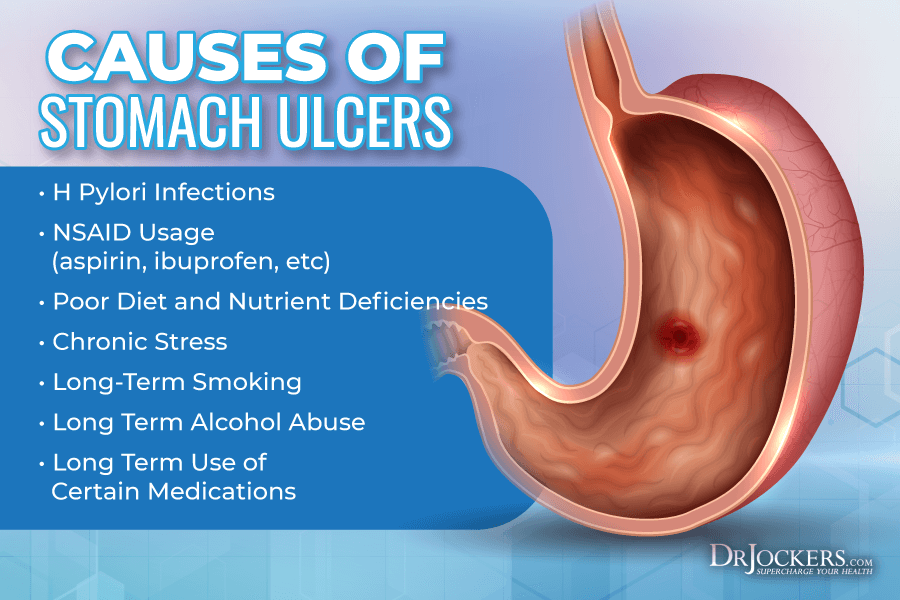
What Causes Stomach Ulcers?
Doctors once thought that high amounts of stress alone could cause a stomach ulcer to occur by increasing the stomach acid. In the 1980’s research emerged that began to show that long-term use of anti-inflammatory drugs (NSAIDs like aspirin, ibuprofen and or naproxen), a poor lifestyle that includes eating processed foods and a bacterial infection caused by the strain Helicobacter Pylori (H. pylori) were the more common causes (3).
Here is the full list of causes of stomach ulcers:
- Anti-inflammatory medicines are frequently called non-steroidal anti-inflammatory drugs (NSAIDs). This medicine can affect the mucous barrier and allow acid to cause an ulcer.
- An infection in the digestive system caused by the bacteria H. pylori.
- Smoking (research shows smokers have twice the risk of developing ulcers) stress, and drinking may increase the risk of having an ulcer.
- A run-down immune system caused by high levels of inflammation, a poor diet, high amounts of stress and excessive alcohol use.
- Very rarely from a growth of a tumor (which could be cancerous or non-cancerous) which forms in the stomach, pancreas or intestines. This condition is very rare and is known as Zollinger-Ellison syndrome. In these cases, stomach and intestinal ulcers are formed by increasing the body’s production of acid. This occurs in less than 1 percent of all peptic ulcers (4).
- Ulcers also tend to be more prominent in families. People who have a family history of stomach ulcers or duodenal ulcers are 2 to 3 times more likely to have ulcers themselves. In fact, 50 to 60 percent of people with duodenal ulcers have a family history (5).
- Osteoporosis treatments such as Alendronate (Fosamax) and Risedronate (Actonel), have been shown to increase the risk of bleeding.
- Anticoagulants, like warfarin (Coumadin) or clopidogrel (Plavix). Additionally, there is an increased risk among men over 60 years old who take aspirin and high blood pressure medications.
- Selective serotonin reuptake inhibitors (SSRIs) have been associated with increased risk for bleeding causing peptic ulcers (6).
- Certain chemotherapy medications can alter the normal bacterial flora that is present in the intestines. Steroids and other immunosuppressant medications may increase the probability of ulcers or other potentially serious abdominal complications.
16 Natural Support Strategies for Ulcers
While stomach and duodenal ulcers can be quite a challenge to live with, the good news is that overtime you can heal them naturally. Here are some of the best practices, nutrients and compounds to use to support the healing process. While these aren’t FDA approved to prevent, mitigate, treat or cure ulcers, many people have seen great results by applying these strategies.
This isn’t an exhaustive list as there are other agents and strategies that can help you, but this is a good start. It is always advisable to work with your health care practitioner when you change your diet and lifestyle and create a healing strategy.
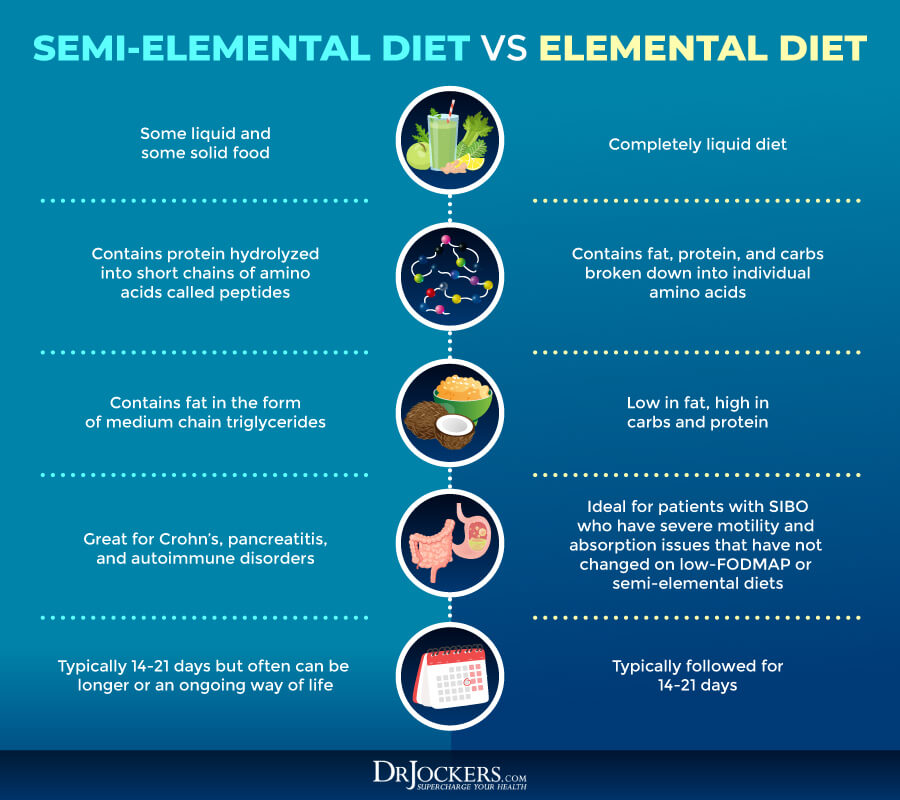
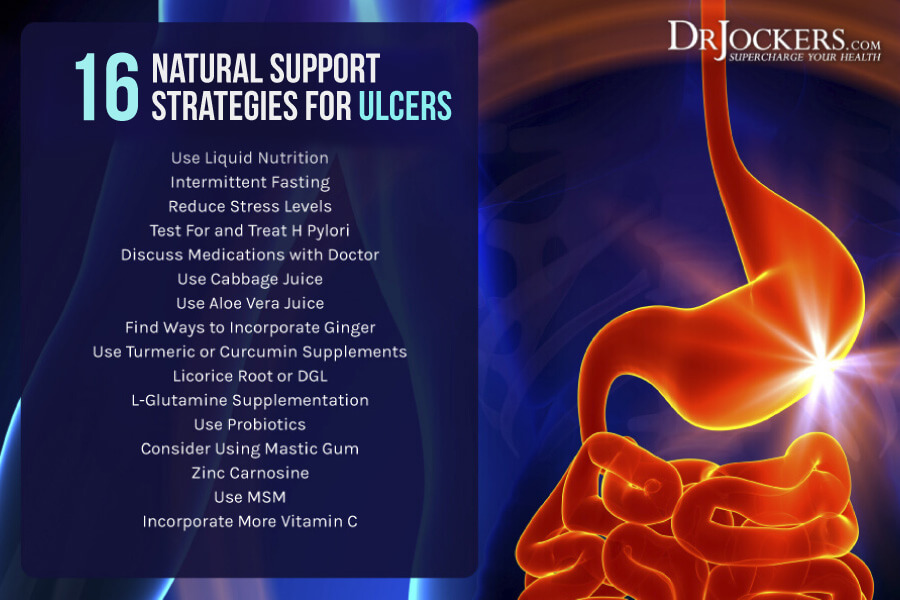 Liquid Nutrition
Liquid Nutrition
Digestive disorders are growing in their prevalence in our society today. Poor nutrition, bloating, heartburn, gas and colon disorders are more common. These things are not normal and can be quite disruptive to daily life. In my opinion, fasting and liquid nutrition are critical in the healing process.
Eating solid foods when you have an ulcer would be analogous to trying to walk on a sprained or broken ankle. The wear and tear will prevent it from healing.
Liquid nutrition would be like giving this individual with a sprained ankle some crutches so they can still get a round but not have the constant loading on the ankle. Liquid nutrition in the form of smoothies, broth, juices, etc. provides key nutrients to support healing without the mechanical irritation.
When I have an individual with a stomach ulcer, I will often have them do a water or bone broth fast for 3-7 days to begin with. I will then transition them to doing protein smoothies and possibly green juices. If we don’t begin with a fast, I will just have them do 3-4 protein smoothies each day using coconut milk, avocado, berries and a high-quality protein powder.
Using liquid nutrition in the form of smoothies, shakes, bone broth and juices will gently stimulate the digestive process, ingesting more gut healing nutrients, and providing adequate nutrition for the body.
Intermittent Fasting
One of my other top recommendations is Intermittent Fasting. It is a great starting point for reducing stress on the gut. Intermittent fasting is going longer periods of time without eating, which naturally confines eating to a smaller window of time. The benefit of intermittent fasting is that it allows your gut to heal while reducing inflammation. It improves hormone sensitivity and increases growth hormones while you are becoming a fat burner.
Intermittent Fasting can be helpful with an elimination diet that cuts out your unique food sensitivities. I would suggest beginning with a 12-hour fasting window between dinner and breakfast for 2 weeks. When you are comfortable progress to 14 hours for 2 weeks. Continue like this until you have reached a daily fasting segment of 16 to 18 hours.
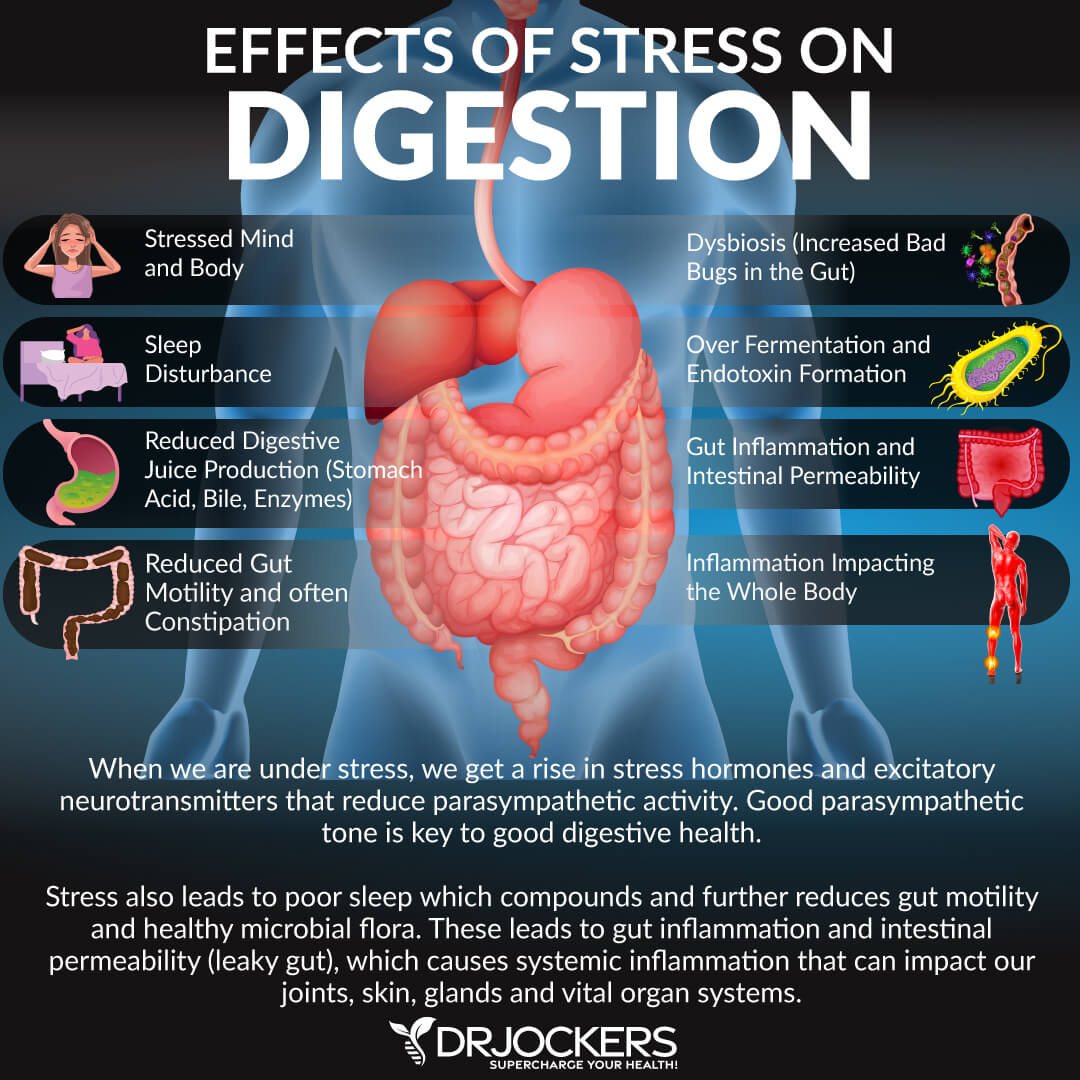
Reduce Stress
There is never a time I do not suggest reducing stress. When the body is under stress, digestion is not prioritized. This results in under-production of stomach acid and enzymes. Digestive juices provide a protective role in sterilizing the food we eat which maintains the optional balance in the microbiome.
Eating while chronically stressed slows down bowel motility, causing food to remain in the small intestines and the colon longer than necessary. This bowel stagnicity promotes dysbiosis bacterial growth and inflammation. This overgrowth of bacteria then produces toxins that enter the bloodstream which causes more inflammation throughout the body.
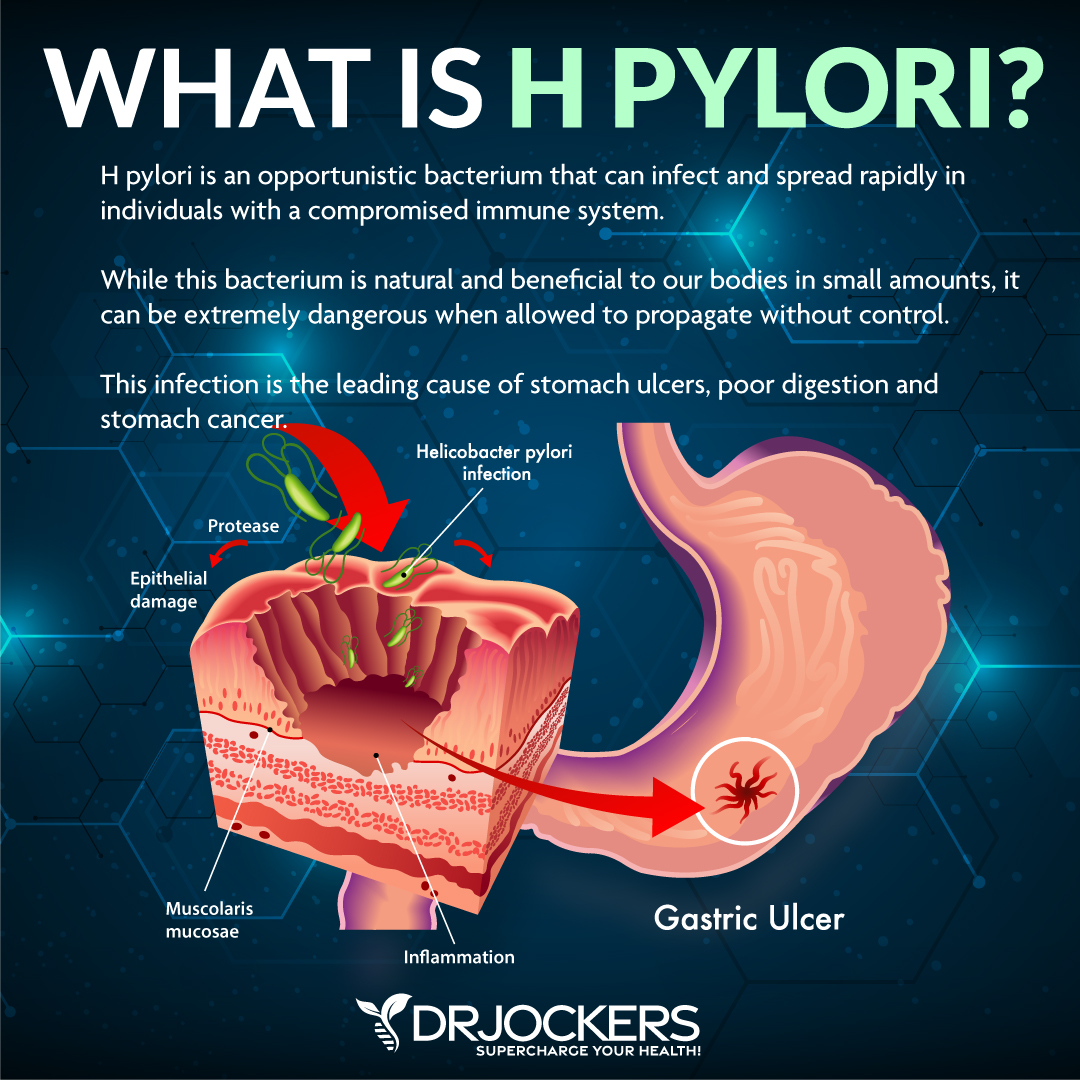
Treat H Pylori
H pylori is an opportunistic bacterium that will infect and spread rapidly in people with a compromised immune system. Although this bacterium is natural and beneficial in small amounts, it can be very dangerous when allowed to propagate without control. This infection is the leading cause of stomach ulcers and stomach cancer.
The secretion of mucus protects the stomach lining from irritation by food stuffs and microorganisms. H. pylori reduces the stomach’s ability to produce mucus and irritates the stomach lining. Inflammation is created and irritation becomes so severe that pain receptors fire off. This is how stomach ulcers are formed.
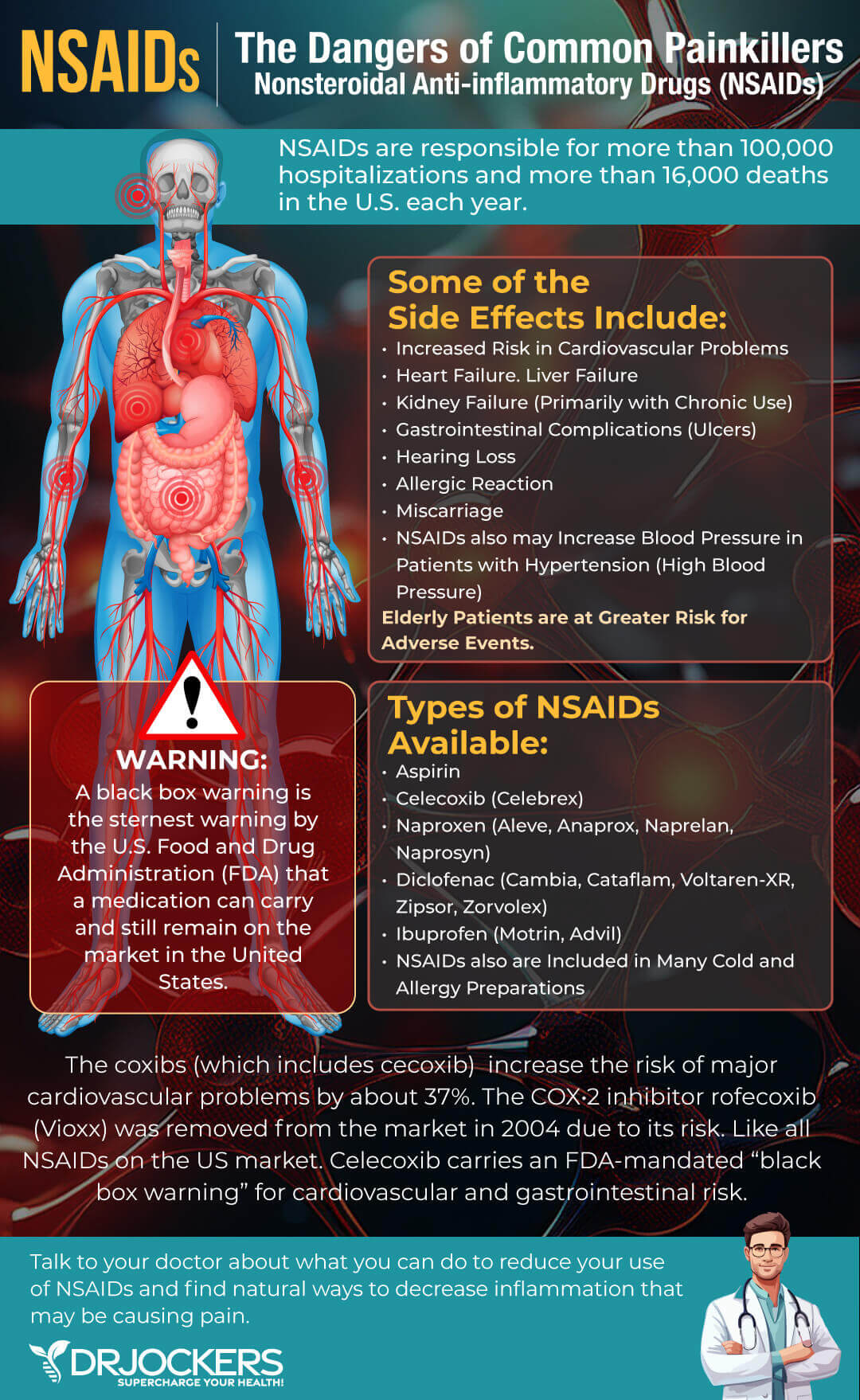
Discuss Medications with Your Doctor
It is important to discuss medications with your doctor. The goal should be to eliminate any medications that may be causing irritation or contributing to an ulcer.
Anti-inflammatory medicines are frequently called non-steroidal anti-inflammatory drugs (NSAIDs). This medicine can affect the mucous barrier and allow acid to cause an ulcer (7). Medications like NSAID’s and PPI’s have the potential to disrupt the intestinal barrier function and contribute to leaky gut.
There are many medications that can alter the mucosal lining and allow irritation to begin. Speaking with your doctor to either reinforce the health of the gut or heal the condition the medication is being prescribed for will help you to have a healthier, more fulfilling life.
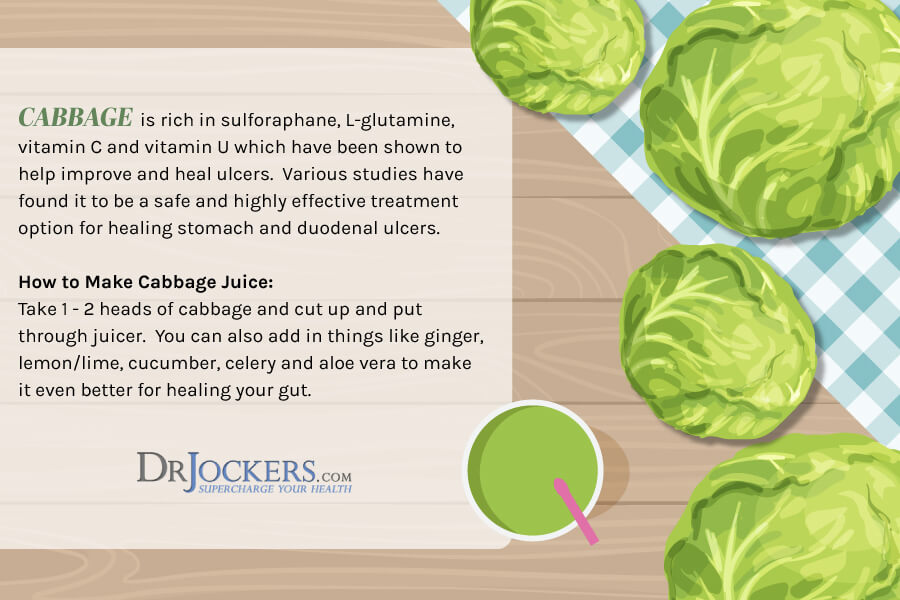
Cabbage Juice
Cabbage juice is a popular natural ulcer remedy. Doctors reportedly used it decades before antibiotics were available to help heal stomach ulcers. It-is rich in vitamin C, it is also an antioxidant shown to help prevent and treat H. pylori infections. As discussed above, these infections are the most common cause of stomach ulcers.
Additionally, cabbage juice is a great source of the amino acid L-glutamine and the antioxidant sulforaphane. These compounds help to protect and heal the gastric lining and the prevent and heal leaky gut syndrome.
Finally, cabbage is one of the best food sources of methionine S-methyl sulfonium (MMS) which was named Vitamin U in 1950 by Garnett Cheney for uncharacterized anti-ulcerogenic factors in raw cabbage juice that may help speed healing of peptic ulcers (8). Cheney called MMS vitamin U to signify how remarkable he thought this nutrient was for its impact on the healing of ulcers.
In one study, 13 participants suffering from stomach and upper digestive tract disorders were given one quart of fresh cabbage juice throughout the day. On average, these patients’ ulcers healed after 7-10 days of treatment. This is 3.5 to 6 times faster than the average healing time following conventional studies (9).
Aloe Vera
Aloe Vera is a plant commonly used in the cosmetic, pharmaceutical and food industries. It is widely known for its antibacterial and its skin-healing properties. Aloe vera may be an effective remedy against stomach ulcers.
In one study in rats, aloe vera had ulcer-healing effects similar to omeprazole, a common anti-ulcer medication (10). In another study it significantly reduced the stomach acid produced in rats suffering from stomach acid (11). Unfortunately, there are only a few studies looking at aloe vera usage for humans with ulcers. In one, a concentrated aloe vera gel was used successfully to treat 30 patients with stomach ulcers (12).

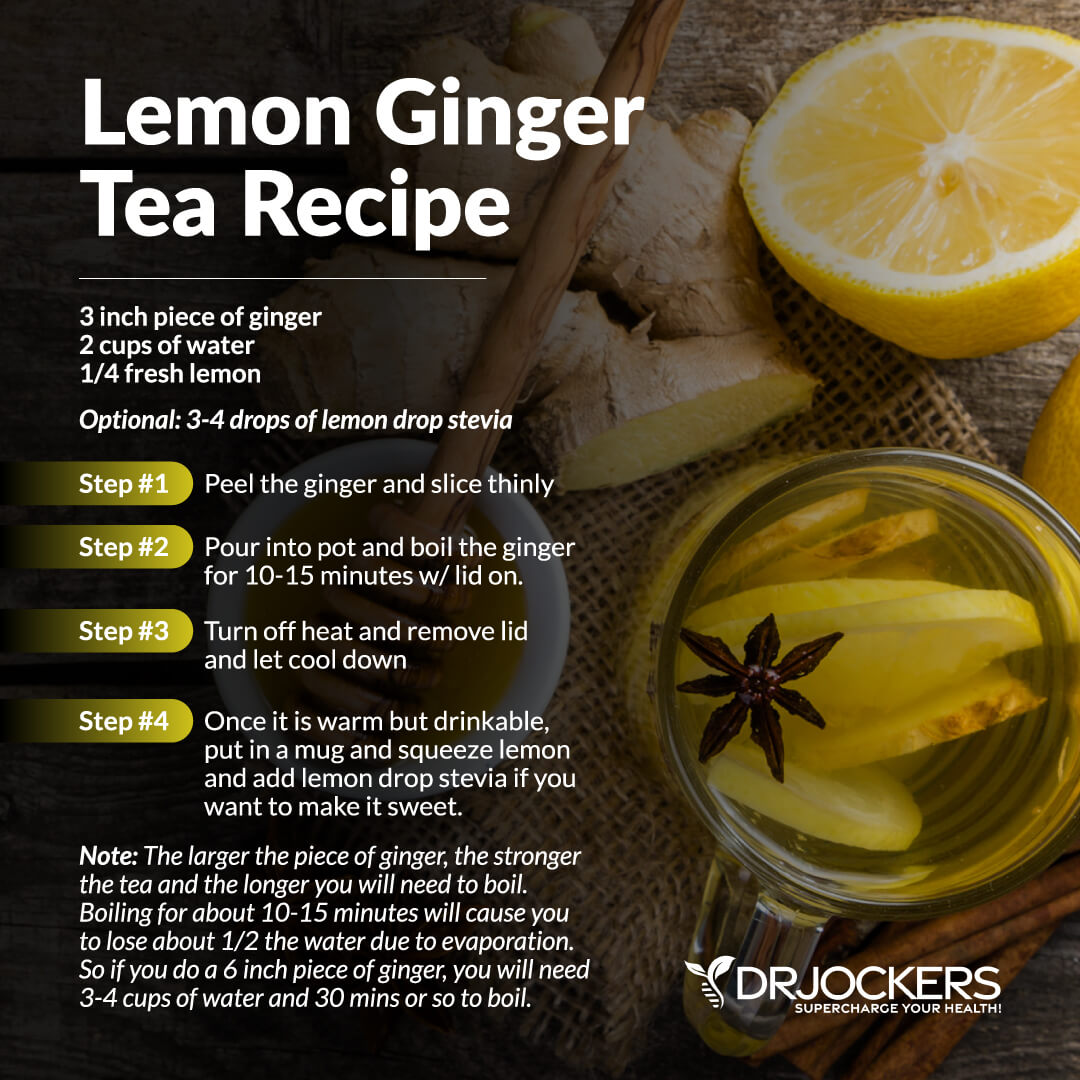
Ginger
Ginger is frequently used to improve the digestive process. Nine different substances have been found within ginger that stimulate serotonin receptors in the gut which provides enhanced benefits to the gastrointestinal system.
The stimulation of these serotonin receptors enhances bowel motility and helps to reduce gut related inflammation. Additionally, ginger has powerful anti-nausea benefits which is very helpful for individuals with stomach ulcers as that is a very common complaint.
Ginger has been found to have a gastro-protective effect as it balances digestive juices, improves digestive function and suppresses H. pylori. Add 2 to three slices of fresh ginger to two cups of hot water. Let it steep for about half an hour. Then drink 20 minutes before a meal.
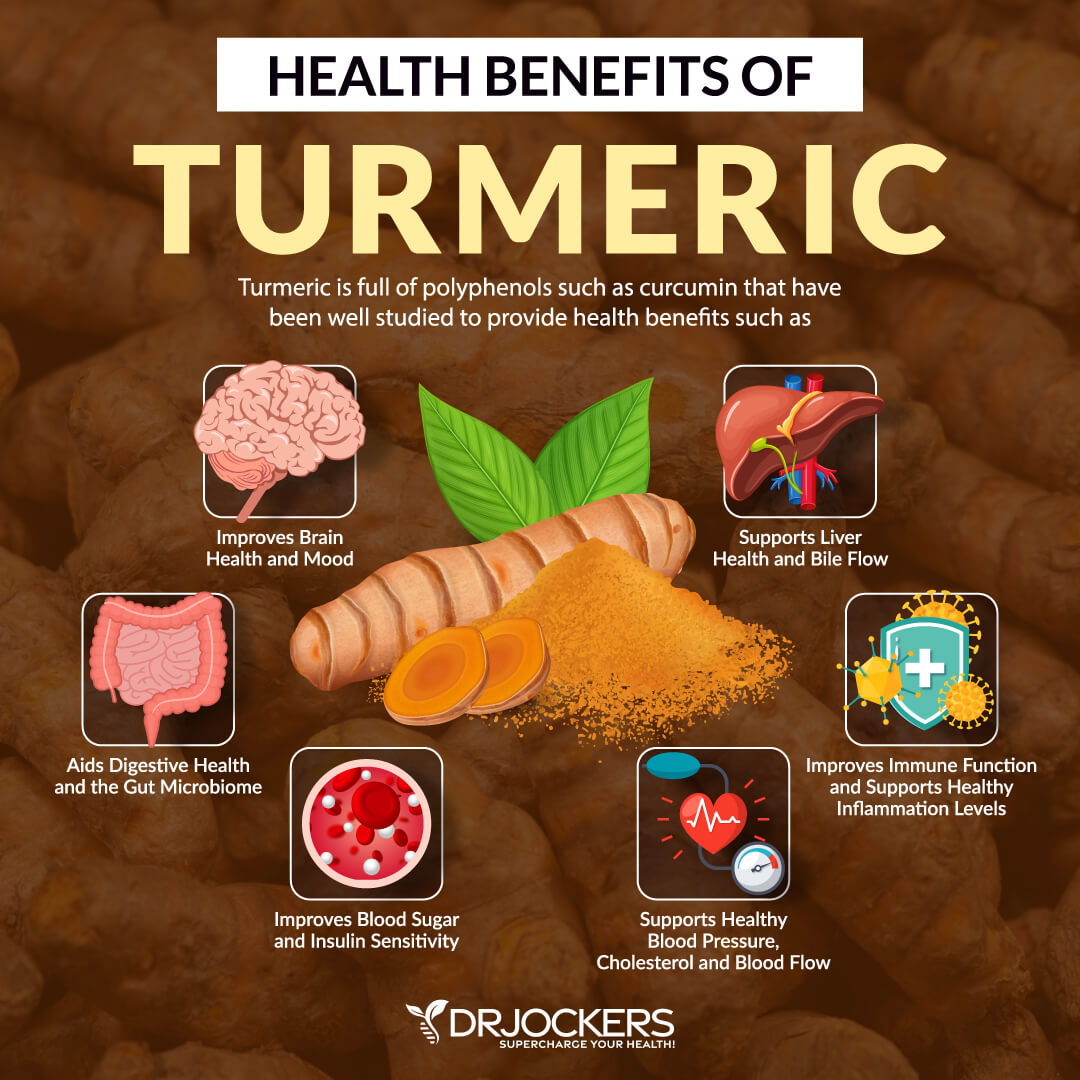
Turmeric
Turmeric is a frequently used spice from South Asia. It is used in many Indian dishes. Its rich, yellow color makes it easily recognizable. Curcumin, turmeric’s active ingredient, has many medical properties. These range from improved blood vessel function to reduced inflammation and heart disease risk.
Turmeric-appears to have immense therapeutic ability, especially in preventing damage from H. pylori infections. It may also increase mucus secretion, protecting the stomach lining against irritants. As a supplement, curcumin is considered turmeric’s active compound, and it has been shown to help protect the stomach lining and aid in the healing of ulcers.
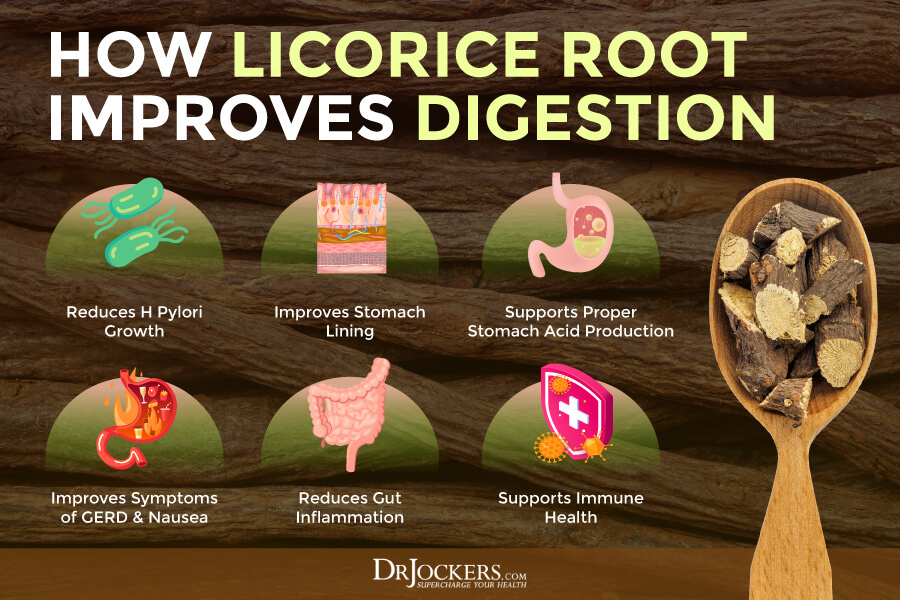
Licorice
Licorice is a powerful herb that has been used for thousands of years in various cultures to help with indigestion and ulcers. Licorice helps to stimulate the release of secretin which enhances the stomach’s mucus lining. This gives it its characteristic demulcent (agent that soothes and relieves irritation in mucosal membranes) properties (13). This is why licorice is revered for its use with stomach ulcers, because it helps protect and heal the gastric lining.
It is also a powerful defense against the H Pylori bacteria that is implicated with stomach ulcers and a number of other digestive health issues (14).DGL is made from licorice but the glycyrrhizin ingredient is removed. This is important because glycyrrhizin inhibits the metabolism of cortisol and thus it can cause an elevation in blood pressure. DGL supports the body’s natural healing process in the stomach and small intestine.
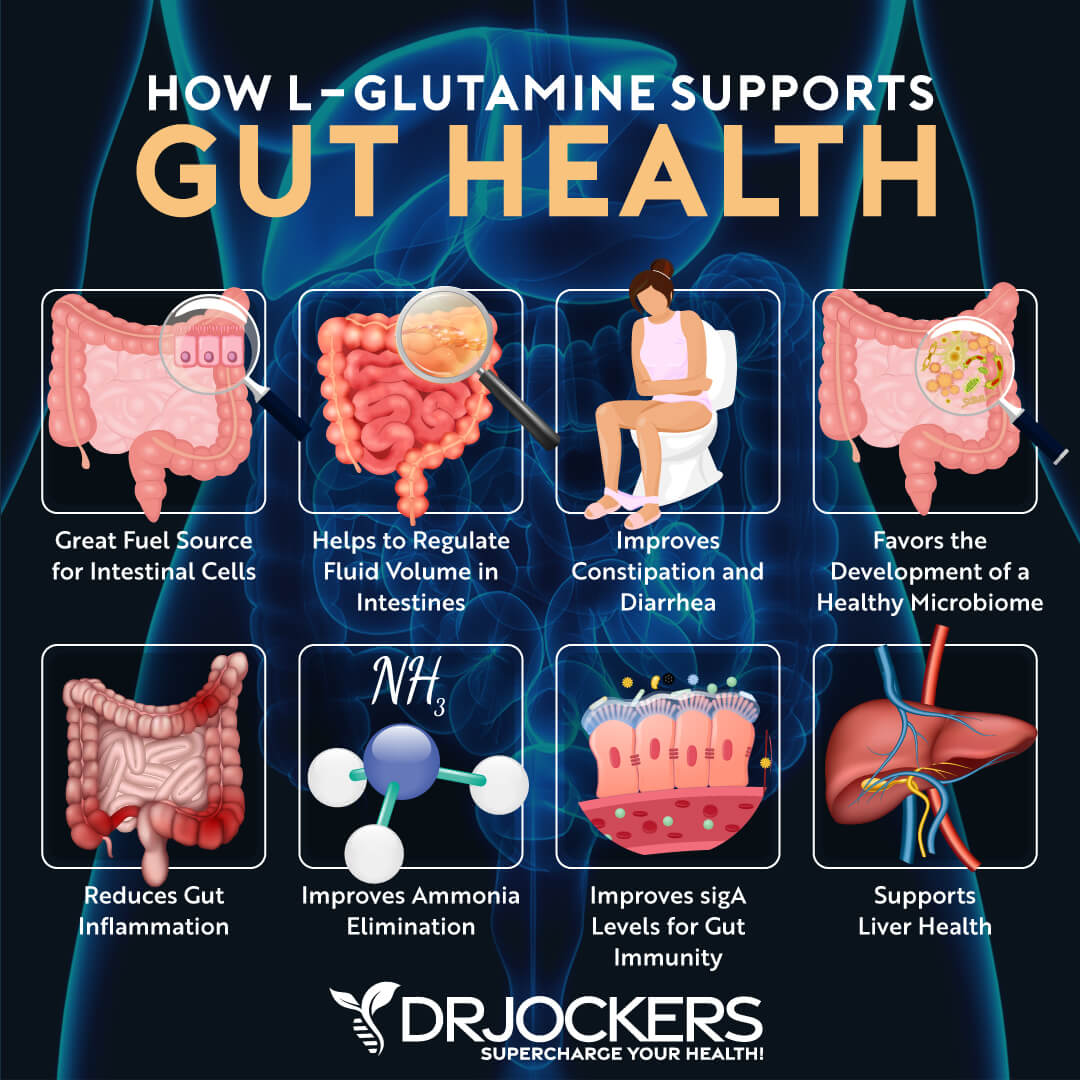
L-Glutamine
L-Glutamine is an amino acid that is imperative to the proper function of the digestive and the immune system. It is a primary fuel, not only for a healthy gut membrane but also regrowth and repair of the intestinal lining. Supplementing with L-Glutamine helps to ensure the right microorganism balance to produce a healthy gut flora.
L-Glutamine-may help to protect your stomach from H. pylori bacteria that is responsible for many stomach ulcers. L-Glutamine may also decrease inflammation and damage caused by H. pylori and NSAID usage (15).
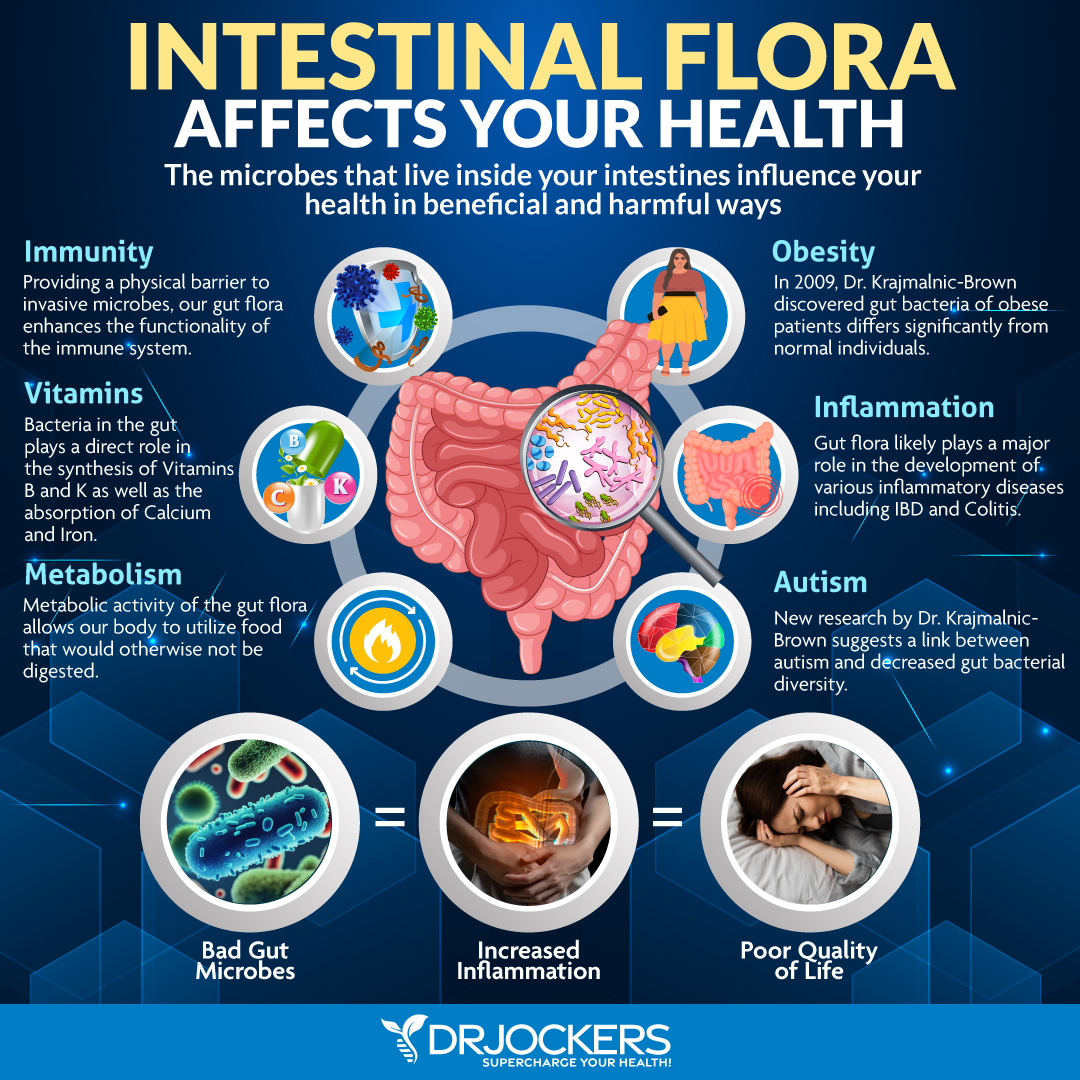
Probiotics
Probiotics are live organisms that offer many health benefits. Their benefits range from improving the health of your mind to the health of your gut, including its ability to prevent and fight infection. Probiotics seem to stimulate the production of mucus, which protects the stomach lining by coating it.
Probiotics may also promote the formation of new blood vessels, which eases transport of healing compounds to the site of the ulcer and speeds up the healing process. Probiotics also play a role in preventing H. pylori infections.
Mastic Gum
Mastic is a resin obtained from the mastic tree. The mastic tree generally grows in the Mediterranean. Its sap is dried into pieces of brittle, translucent resin. Mastic has been used in ancient medicine to treat gut disorders including stomach ulcers and Crohn’s disease.
Mastic Gum appears to have antibacterial activity against H. pylori. In one study, intake of 350 mg of mastic gum provides relief of gastric discomfort and promotes a healthy bacterial balance while providing antioxidant protection for mucosal cells (16).

MSM
It has been shown the sulfur compounds in fermented vegetables such as kimchi may provide benefits for those with leaky gut by protecting and supporting the mucosal barrier in the digestive tract. MSM can be a helpful strategy in for reducing inflammation and autoimmunity.
Ulcers caused by too much stomach acid can be reversed with MSM. MSM allows patients with chronic heartburn and peptic ulcers to experience fewer symptoms.

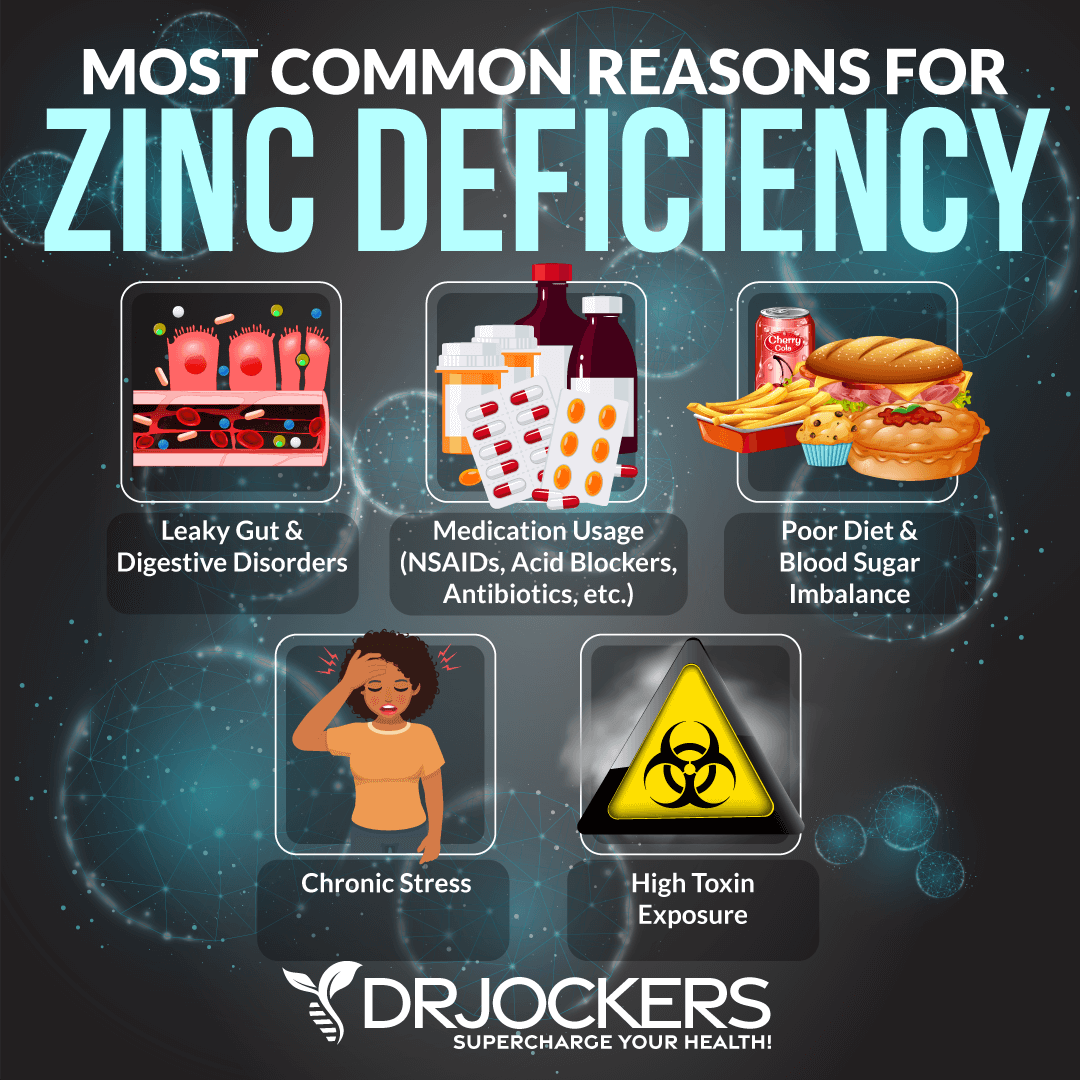
Zinc Carnosine
Zinc is an essential trace mineral that is used in over 300 genetic proteins in the body and roughly 25% of the world’s population is zinc deficient. Zinc is critical for healing wounds throughout the body and essential for the health of the gastrointestinal system.
Zinc carnosine is zinc connected to the L-carnosine dipeptide. A 2007 article published in the medical journal “Gut,” discussed zinc carnosine’s remarkable ability to stabilize the gut mucosa and promote repair (17).
Another 2017 study looked at zinc carnosine in combination with antibiotic therapy for H Pylori infection. It demonstrated that the eradication rate was improved, and the individuals had fewer negative reactions to the antibiotic (18).
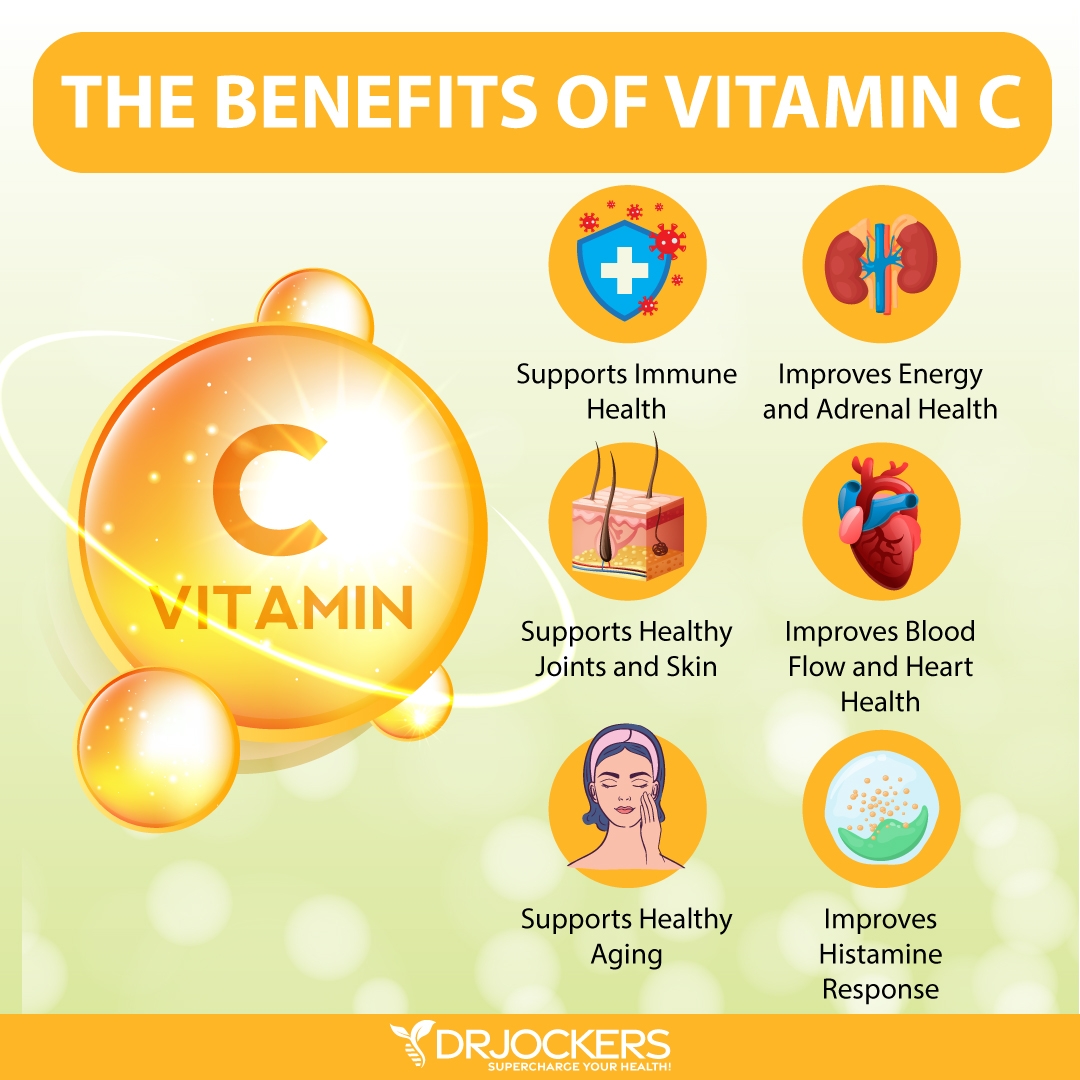
Vitamin C
Vitamin C therapy plays a key role in healing and protection of the gastric mucosa from injury. The lower levels of vitamin C in the blood, the more likely you are to be infected with H. pylori.
Vitamin C deficiency has been repeatedly linked with peptic ulcer disease and gastric cancer. Vitamin C plays a key role in protecting and healing the stomach and intestinal mucosa (18).
Ulcer Healing Strategy
In my opinion, the best strategy to prevent and or heal ulcers naturally is to allow time for the body to heal, being patient and combining the 16 support strategies that will continue to improve your health.
Many of the strategies incorporate vitamins, herbs and other natural compounds. None of these are FDA approved to prevent, mitigate, treat or cure stomach ulcers but they can be very helpful for the healing process.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our fantastic team of functional health coaches. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!
Sources For This Article Include:



I was severely anemic that was probably building over 2 years then really hit in March, requiring a blood transfusion and 3 iron infusions so far. I was down 6 pints of blood with no real signs of bleeding up or down. The hemotologist prescribed pantoprazole a couple of weeks ago before my colonoscopy and endo which I had this past Wednesday. The endo found a small stomach ulcer. I haven’t really had many symptoms other than some burping. I had burning before the blood transfusion but since that and my iron infusions plus supplements that has gone away. No gerd either but I do eat simple clean food and no grains. (For 11 years). I have used some aspirin the last year for minor pain (I’m 76 yo) I have stopped aspirin for 3 weeks. The GI doc also Rx the same PPI. I have not started taking these because I have looked into them—not great. Would a stomach ulcer indicate too much acid and a need to lower acid? Would stopping aspirin bring me back to normal? I was going the route to test for acid with betaine but not sure what to do. The doc said it could be a ferritin absorbing issue and not bleeding and low acid can cause that absorption issue. I just got some DGL. Is this all wrapped up together or 2 separate issues. Ulcer and anemia. I do see my functional med doc in May but wonder if I should start the PPI. Thanks.