Hypothyroidism: Symptoms, Causes and Natural Support Strategies
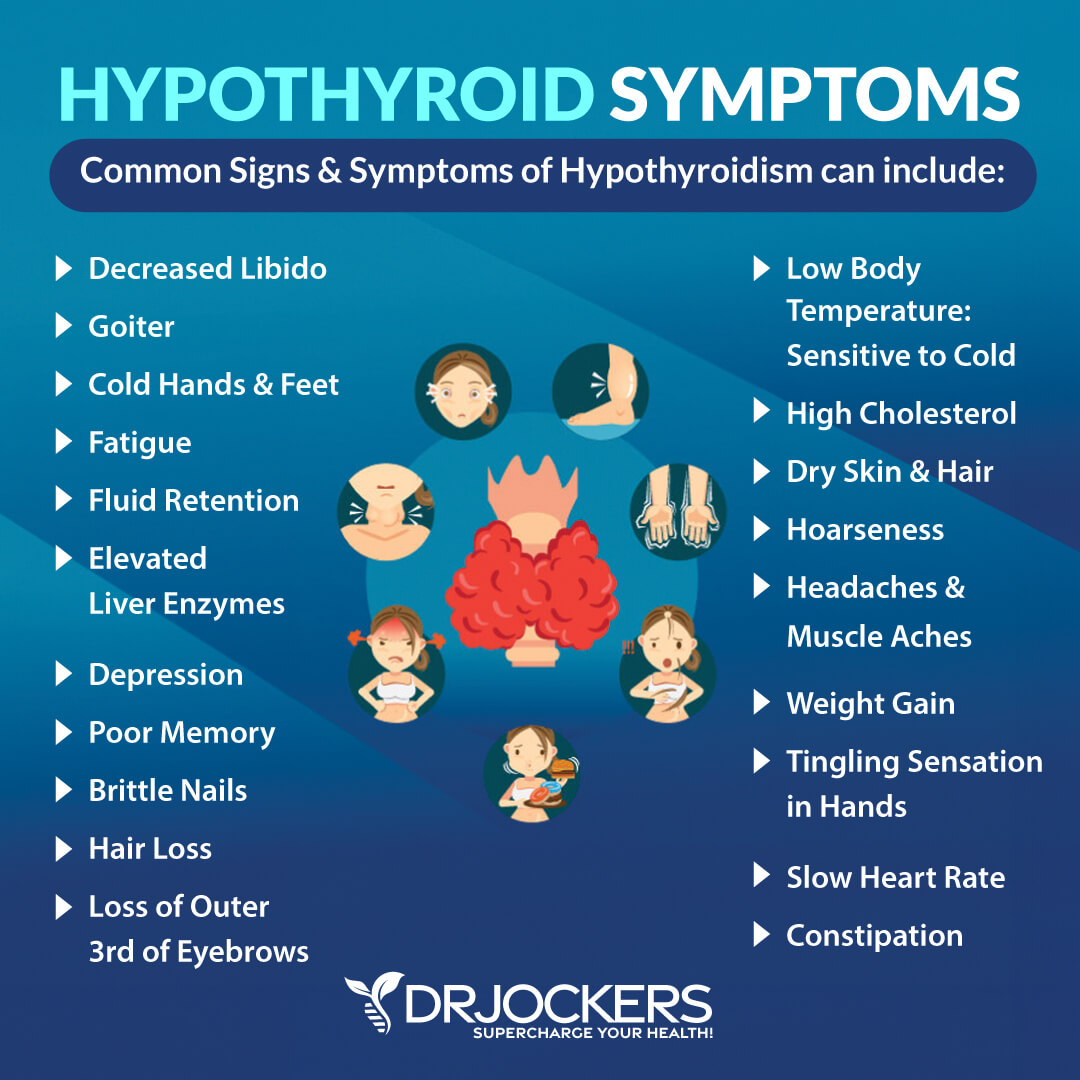
One of the fastest rising health conditions in the US is hypothyroidism. The most common symptoms experienced are lethargy, depression, and weight gain. More than 12% of the US population will develop a thyroid condition during their lifetime with most of these being hypothyroidism (1). In this article, I take a deep dive into thyroid physiology and go over natural strategies to help the immune response and support thyroid health.
An estimated 27 million Americans have some form of thyroid disease. Up to 60 percent of those with thyroid disease are not aware of their condition. Women are five to eight times more likely than men to develop thyroid problems. 80% of hypothyroid conditions in the US are thought to be autoimmune conditions (2).
The Importance of the Thyroid:
The thyroid gland sits right under the top of the sternum at the base of the neck. From this seat, it secretes hormones called T3 (triiodothyronine) and T4 (thyroxine). These hormones circulate in the bloodstream and interact with every cell in the body.
Lack of ideal thyroid hormone function leads to a global decline in cellular functionality in all bodily systems. The thyroid is a central player in the complex web of human metabolism and is very sensitive to even minor imbalances in other areas of physiology. The thyroid gland is the most common site for the development of an autoimmune disease.
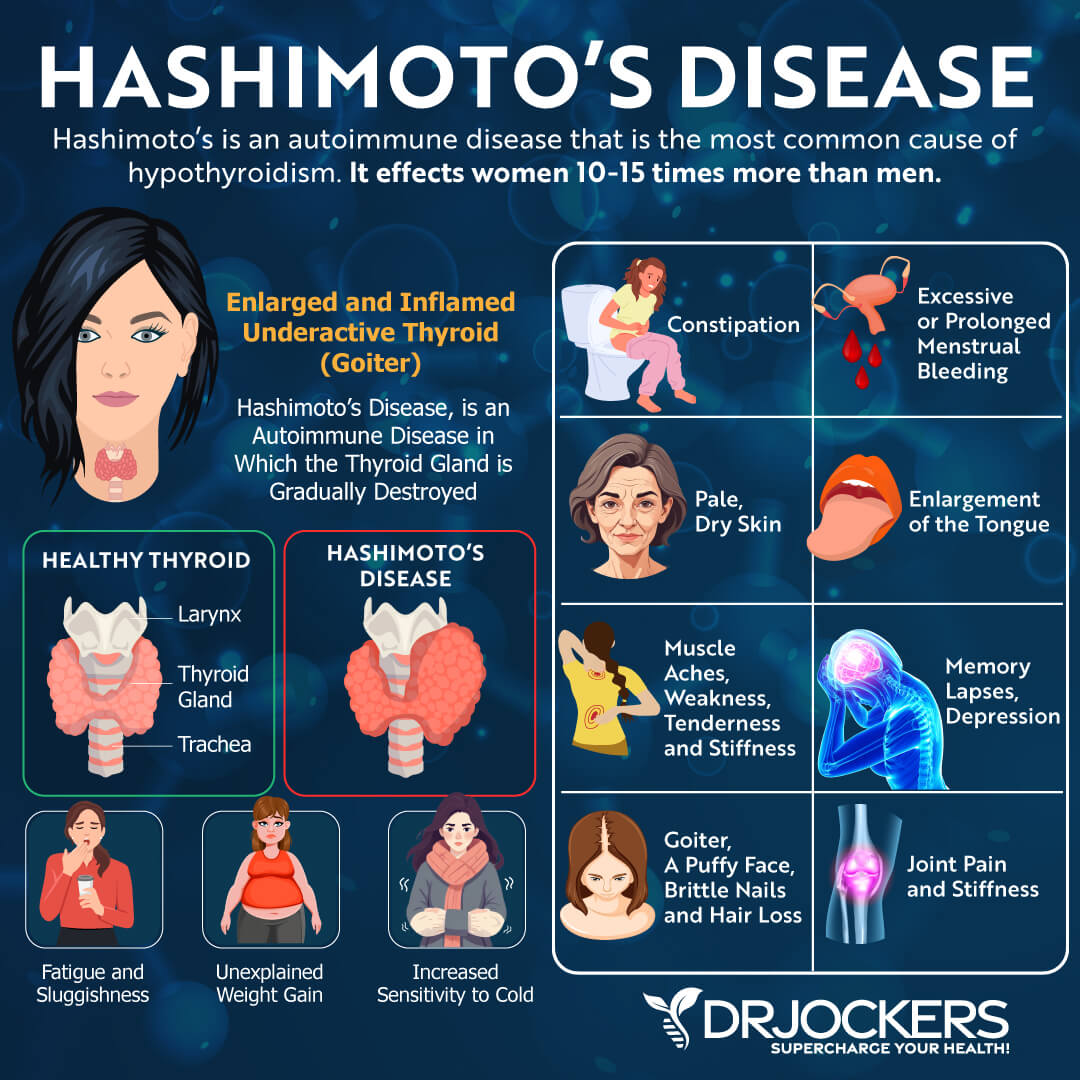
Hashimoto’s thyroiditis is an autoimmune condition of the thyroid that is considered the most prevalent autoimmune condition (3). Hashimoto’s is said to account for up to 80% of all cases of hypothyroidism in the US (4).
Oftentimes, this condition is misdiagnosed and improperly treated. This results in a continual worsening of the thyroid gland as it gets destroyed by the immune system. Over time, these individuals decline in their basal metabolic rate and lose energy, mental function, mood, and gastrointestinal motility.
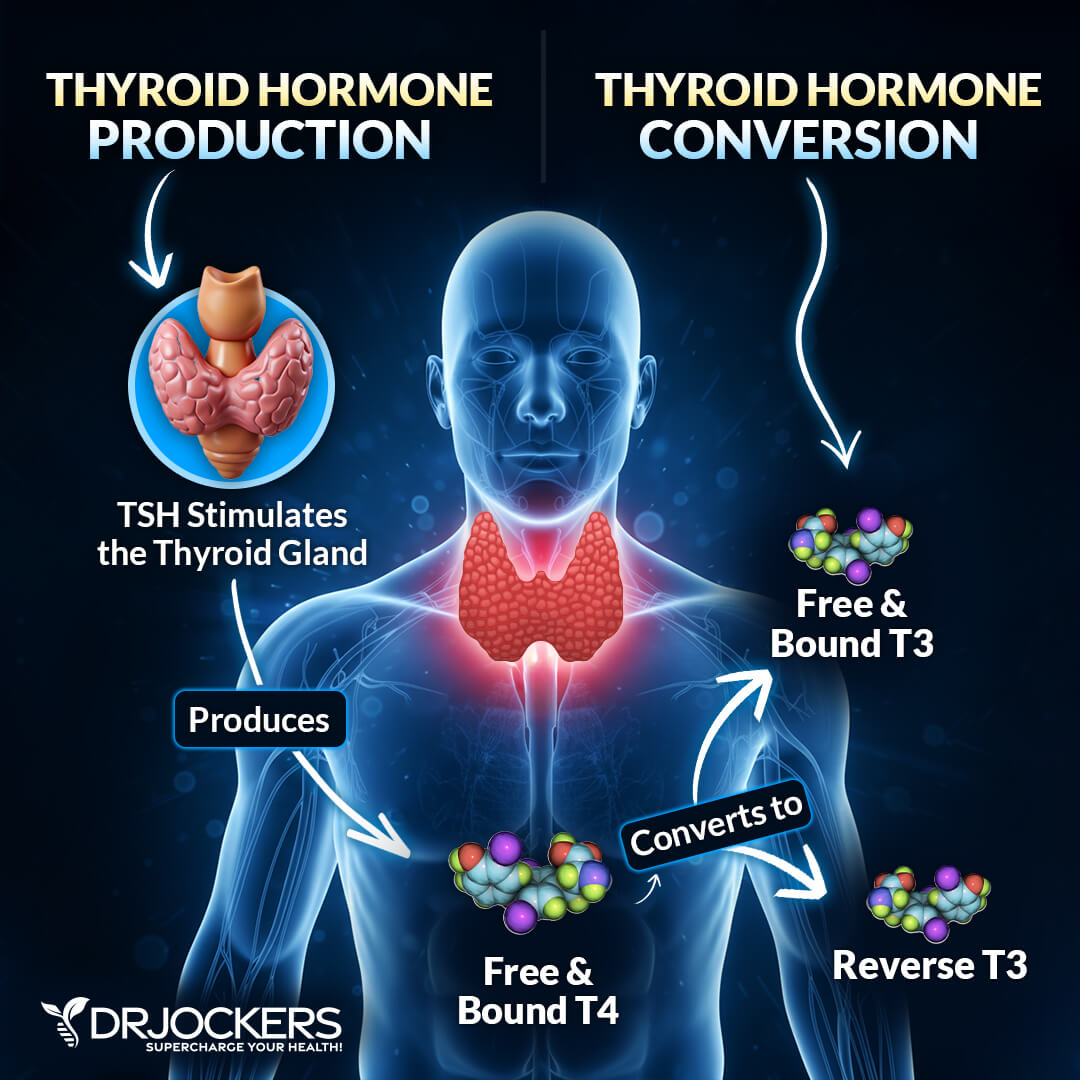
Thyroid Physiology:
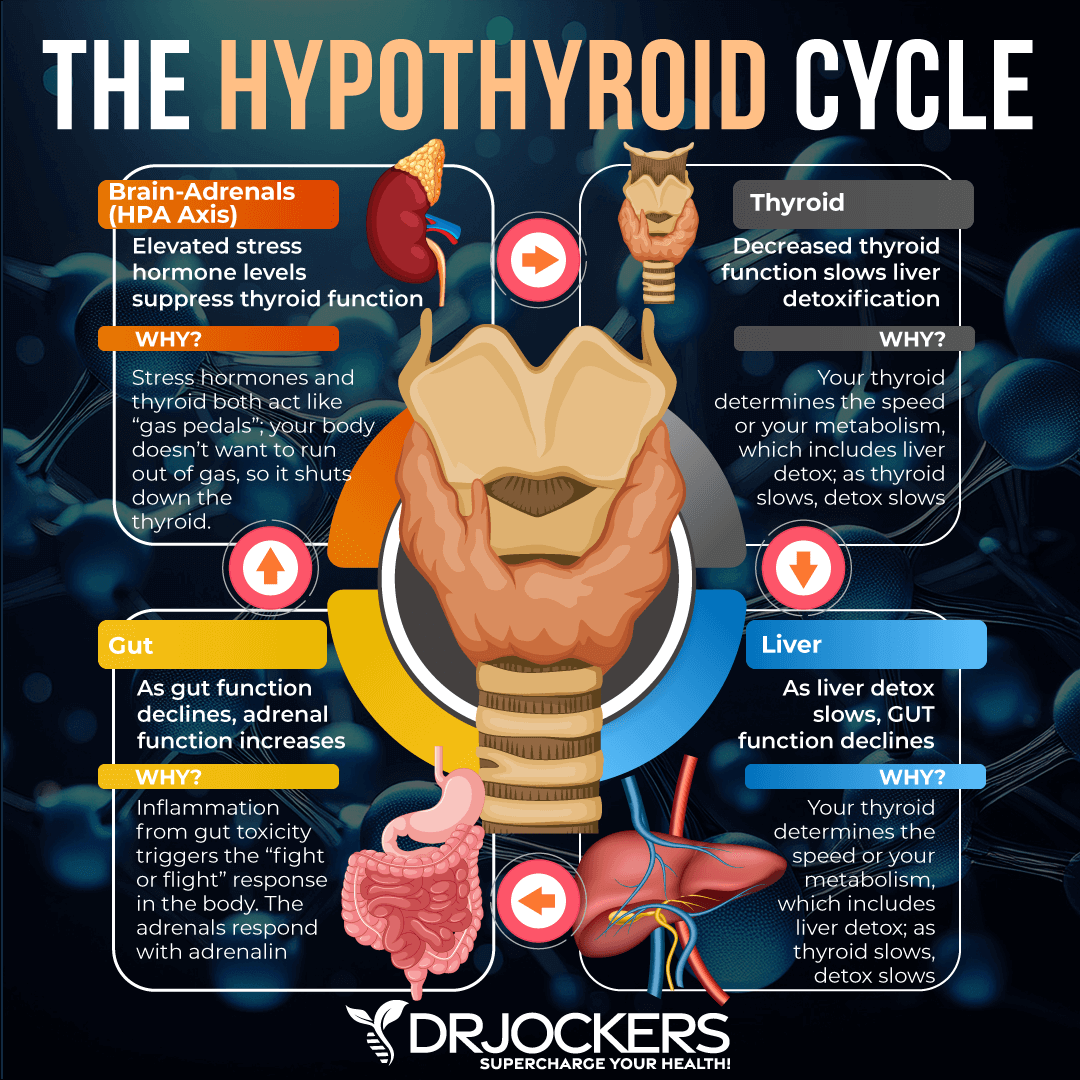
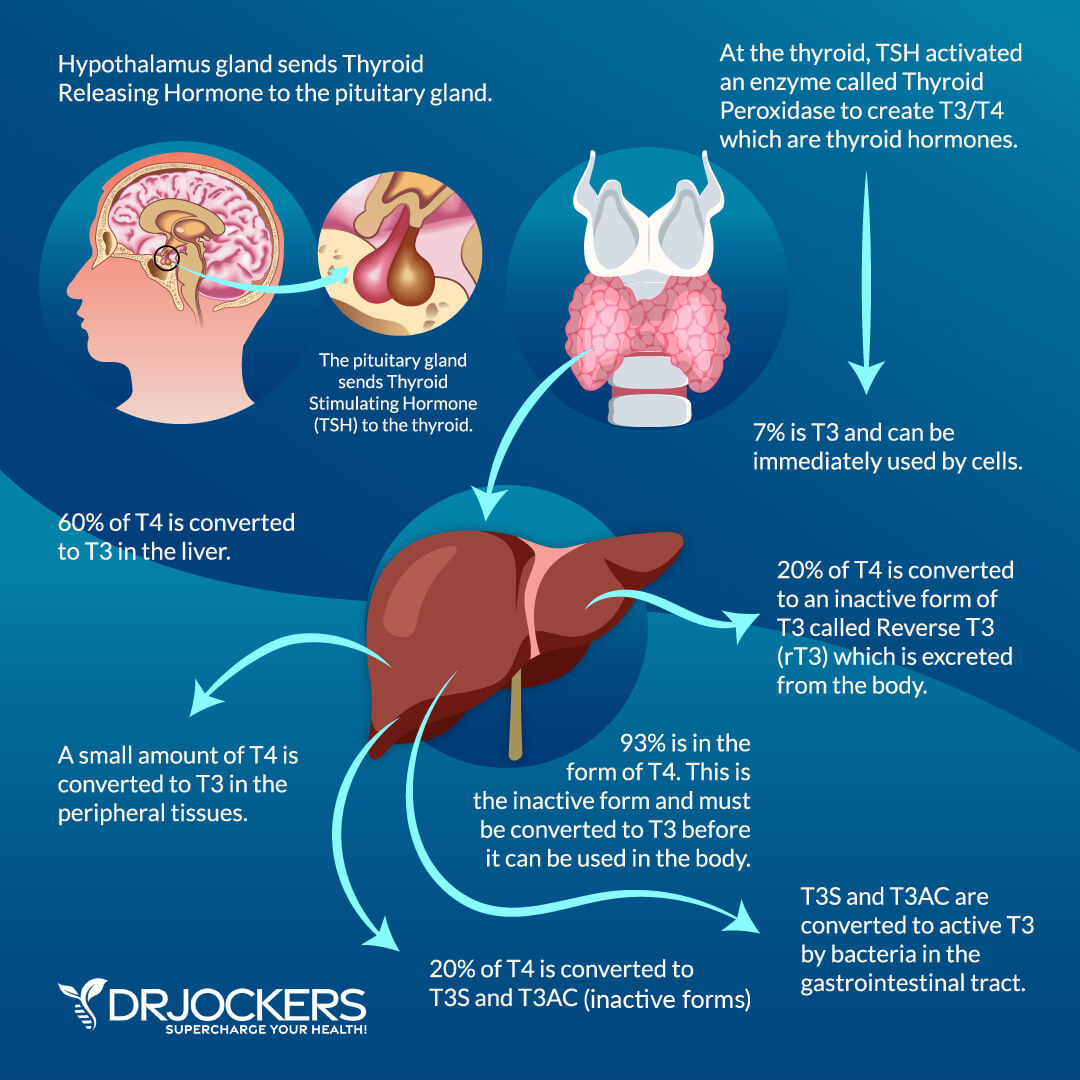
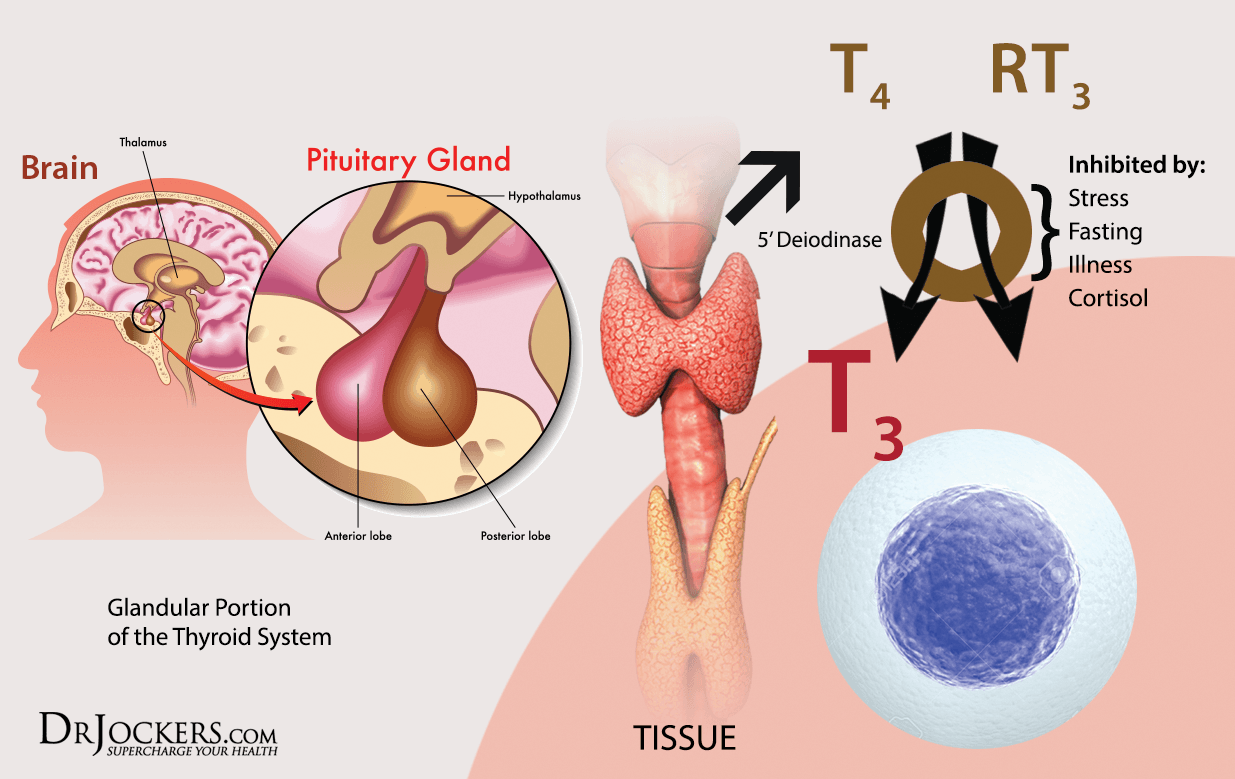
The thyroid responds to messages from the hypothalamus and pituitary gland to get out and interact with the cells of the body. The hypothalamus is like the thermometer of the body and is constantly checking the blood environment for optimal balance of hormones, nutrients, and neurotransmitters.
When the hypothalamus decides we need more thyroid hormone in circulation (cold weather or increased activity level for example) it sends a chemical messenger called thyrotropin-releasing hormone (TRH) which goes to the pituitary gland. The pituitary then sends thyroid stimulating hormone (TSH) over to the thyroid. TSH activates the production of a protein called thyroglobulin.
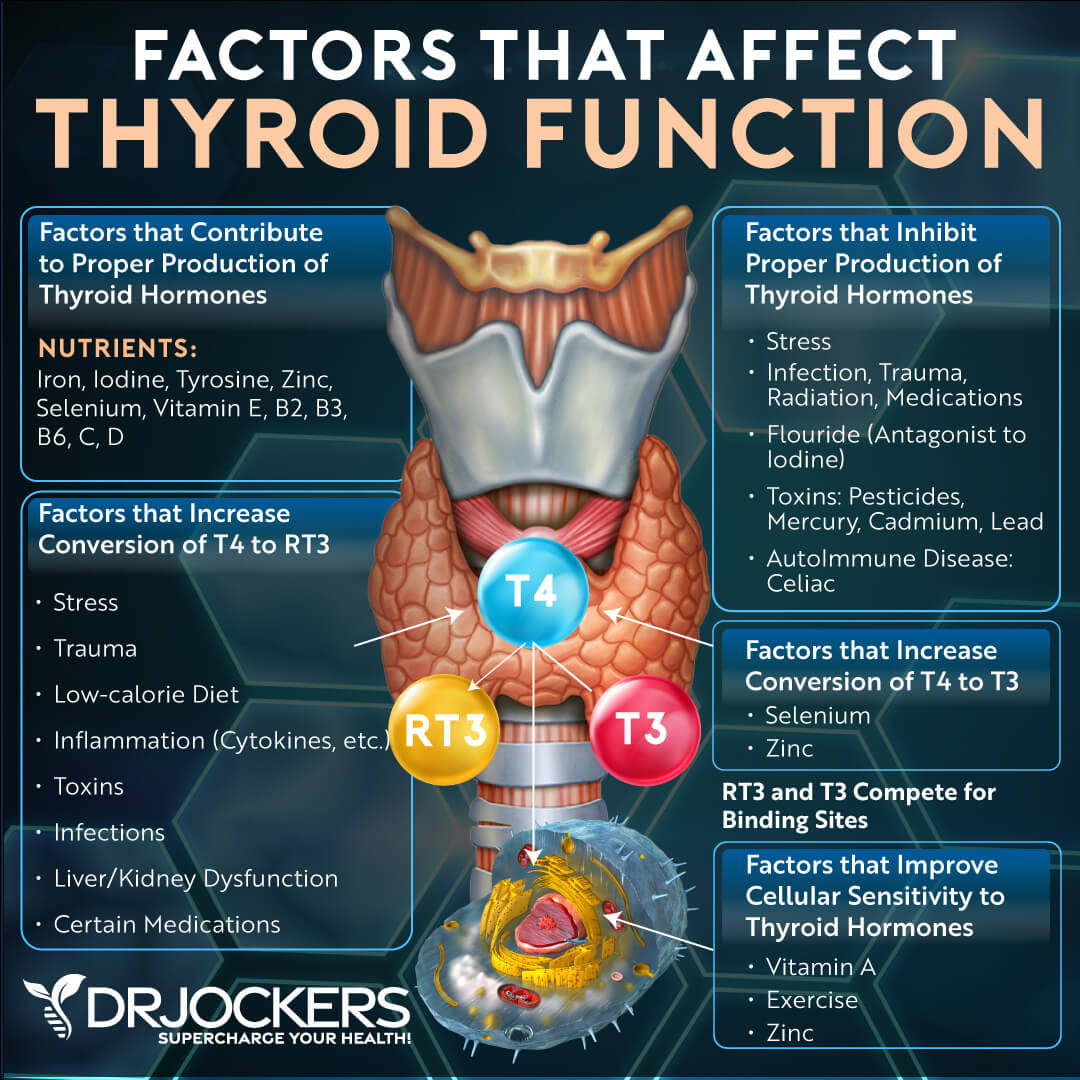
TSH also activates an enzyme called thyroid peroxidase (TPO). This enzyme combines thyroglobulin, iodine, and hydrogen peroxide to create both T3 and T4. About 93% of the hormone made in the thyroid gland is T4 with 7% being T3 (5).
T4 circulates through to the liver where 60% of it is converted into T3 through the glucoronination and sulfation pathways. If the liver is sluggish, it will cause a problem in T4-T3 conversion (6). Another 20% is converted into reverse T3 which is permanently inactive. The final 20% is converted into T3 sulfate and T3 acetic acid which can then be further metabolized by healthy gut bacteria to produce more active T3 (6).
Problems with T4-T3 Conversion:
One common problem with hypothyroidism is a poor T4-T3 conversion. As we have discussed, the thyroid produces 93% T4 and then the T4 travels into the liver for conversion to T3 and reverse T3.
The gut converts the other 20% of T4-T3. T4 is inactive and cannot perform normal thyroid function. It must be converted to T3 to be used by the cells. Here are possible scenarios of why someone would have normal T4 but low T3:
1. Liver Problems: If the liver is sluggish, then it will not be able to convert the normal 60% of T4-T3 by the 5’deiodinase enzymes. This will result in lower T3 levels. A sluggish liver could be due to a liver disease, an infection like Hep C, a toxic body, nutrient deficiencies, methylation, and glutathione problems, etc (7, 8).
One common problem is estrogen dominance where the individual has taken in too many exogenous estrogen compounds from the environment through food, plastics, cosmetics, etc. This can cause the liver to become sluggish and unable to perform its role effectively (9, 10).
2. High Stress: When someone has high stress or trauma they will often overproduce rT3. rT3 is inactive and it functions to slow the body down (thyroid has a speeding up effect) which is necessary in times of stress or trauma for the body to heal.
Chronic stress can drive rT3 up for a prolonged period of time which results in less T3 activity with the cell and functional hypothyroidism (11, 12). Low selenium and zinc can also drive up rT3 levels. Other causes of high rT3 may include iron-deficiency anemia and low B12 (13, 14, 15).
3. Gut Dysbiosis: 20% of the active T3 is formed in the gut. If the individual struggles with small intestinal bacterial overgrowth (SIBO) or Candida and they have an overpopulation of bad microbes it can result in lowered T3 formation (16).
On a lab test, this sort of a problem can show up with TSH being normal or high, T4 is normal but T3 is low and T3 uptake is low. If you are testing for rT3, that can often be elevated in cases of low T3 uptake.
Free & Bound Thyroid Hormone:
Thyroid hormones (T4, T3, and RT3), in the bloodstream, exist either as protein bound or in a free form. The main protein that binds them is called thyroid hormone binding globulin (TBG) which acts as a sponge or reservoir to which hormones bind and then can be freed.
Hormones in the free form are then available to interact with a cell’s receptor site to produce its hormonal effect. It is only the free-form hormone that is biologically available or active. When the hormone is bound to a protein it is restrained from interacting with a cell’s receptor site.
Most of the hormone is bound to proteins (TBG, albumin, and pre-albumin). Albumin has the lowest affinity and the fastest release at tissue sites. TBG has the highest affinity and the slowest release (17). It is important to differentiate and look at both Total T3 & T4 as well as free T4 & T3 to understand how well these hormones are interacting.
Anything that boosts estrogens (artificial sources that can come from birth control pills, non-bio-identical hormone replacement, or pregnancy) or estrogen dominance can increase the amount of the protein that binds T4. This will produce misleading elevated Total T4 values which can look like ‘hyperthyroidism’ when it is not (18).
Autoimmunity and Hypothyroidism
As we described before the thyroid is the most common organ that is affected by autoimmunity. The autoimmunity can be to either be to thyroid peroxidase (TPO antibodies) or to thyroglobulin (TGB antibodies). In some cases of severe autoimmune thyroid disease, antibodies to T4 and T3 can develop which leads to hypothyroidism (19).
It is absolutely critical for any physician who is treating someone with hypothyroidism to test for thyroid antibodies. Unfortunately, few mainstream medical doctors test for thyroid antibodies, so most do not ever get the proper diagnosis. In the medical system, an autoimmune condition, a sluggish thyroid, a burned-out pituitary gland, and a T4-T3 conversion problem are all treated the same way, with synthetic T4 such as Synthroid or a T3 medication like levothyroxine.
Because the treatment is the same, most doctors do not concern themselves with testing for thyroid antibodies. From a natural health perspective, it is especially important to understand if it is a sluggish thyroid, a sluggish liver or pituitary gland, elevated sex hormones, or if it is an autoimmune condition.
Functional Lab Testing:
TSH: Reflects the blood level of thyroid stimulating hormone. Although clinical ranges are 0.5–4.5, the optimal function range is 0.8–2.0. Anything above 4.5 is considered hypothyroidism although you may have less than optimal thyroid function when levels are between 2.0–4.5
Total T4: Reflects the total amount of T4 present in the blood, i.e., the protein bound (unavailable) T4 and the Free T4. Estrogen dominance can create an effect where you have high total T4 even though you may have low free T4. This could be inaccurately diagnosed as hyperthyroidism.
Total T3: Reflects the total amount of T3 present in the blood, i.e., the protein bound (unavailable) T3 as well as the Free T3. Again, estrogen dominance creates the same effect as mentioned in relation to T4 above.
Free T4: Reflects the biologically active (free) form of T4. This T4 can be converted to T3 or RT3.
Free T3: Reflects the biologically active (free) form of T3 that can generate the production of energy (in the form of ATP). Typical functional lab range is 300–450 pg/ml 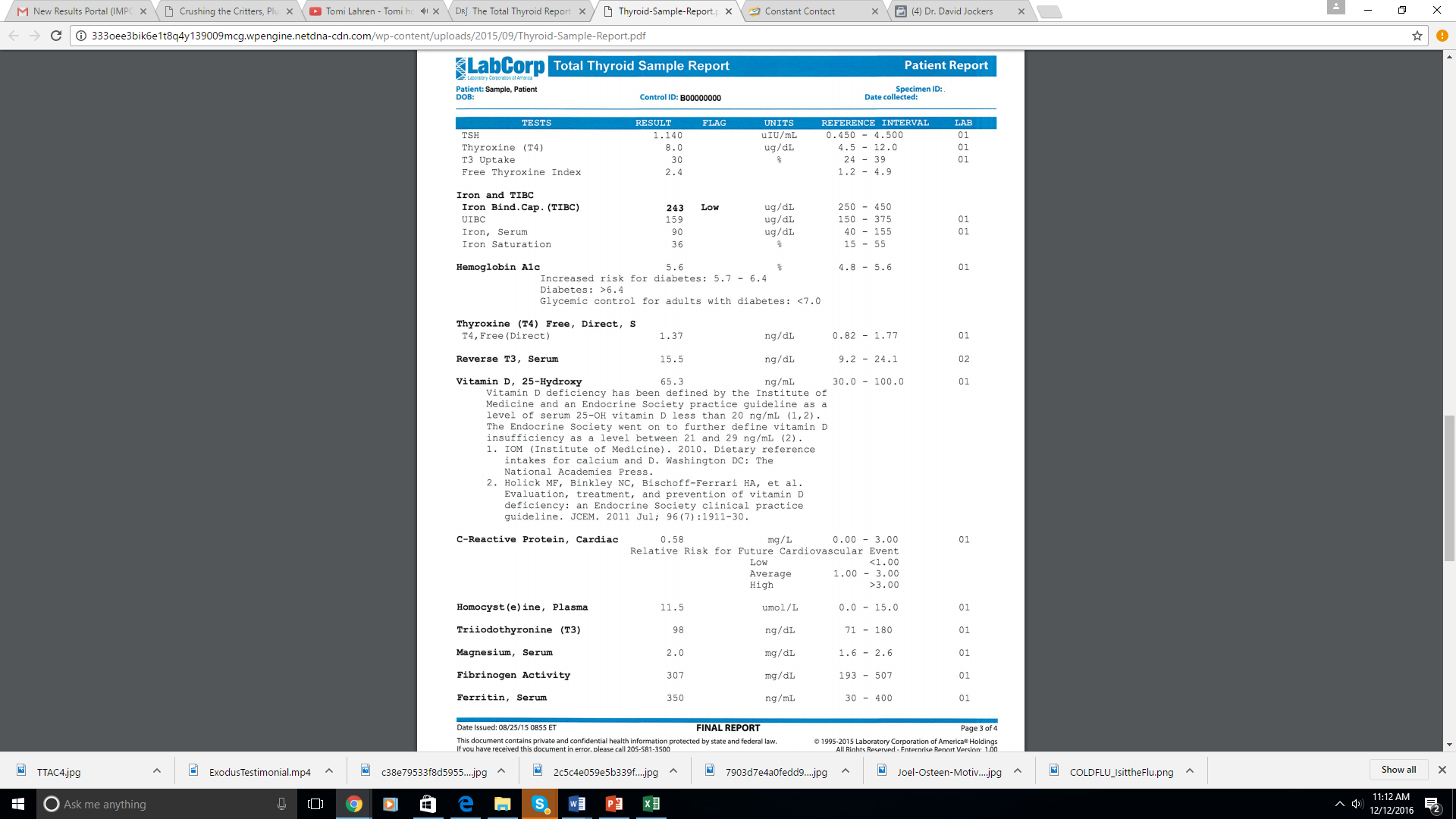 RT3: Reflects the level of Reverse T3. As discussed above, this is inactive and raises during times of stress, fasting, and trauma. This shouldn’t be over 30.
RT3: Reflects the level of Reverse T3. As discussed above, this is inactive and raises during times of stress, fasting, and trauma. This shouldn’t be over 30.
T3 Uptake: This measures the sites for active or unbound T3 to bind with proteins. The more binding sites that are open, the lower the uptake result will be. High testosterone can cause high T3 uptake because it lowers binding sites. Meanwhile, estrogen dominance increases binding sites leading to higher T4 and lower T3 uptake.
Free Thyroxine Index: This test looks at total T4 and T3 uptake to measure the activity of free or unbound T4. If TT4 is low, then T3 uptake should be high. And if TT4 is high, then T3 uptake should be low. Functional range is between 1.2–4.9 mg/dl.
Antibodies: Autoimmune thyroid disease falls into two main categories: Hashimoto’s Thyroiditis and Grave’s Disease. Hashimoto’s Thyroiditis is typically identified by checking antibodies that attach to the thyroid tissue.
We find Antithyroglobulin Antibody (TG Antibodies) in 70% of the cases and Thyroid Peroxidase (TPO) antibodies are found in 95% of the cases. Grave’s Disease is typically diagnosed using Thyroid-Stimulating Immunoglobulin (TSI) and TSH-Binding Inhibiting Immunoglobulin (TBII). These are different names for the same test.
Immune Modulation:
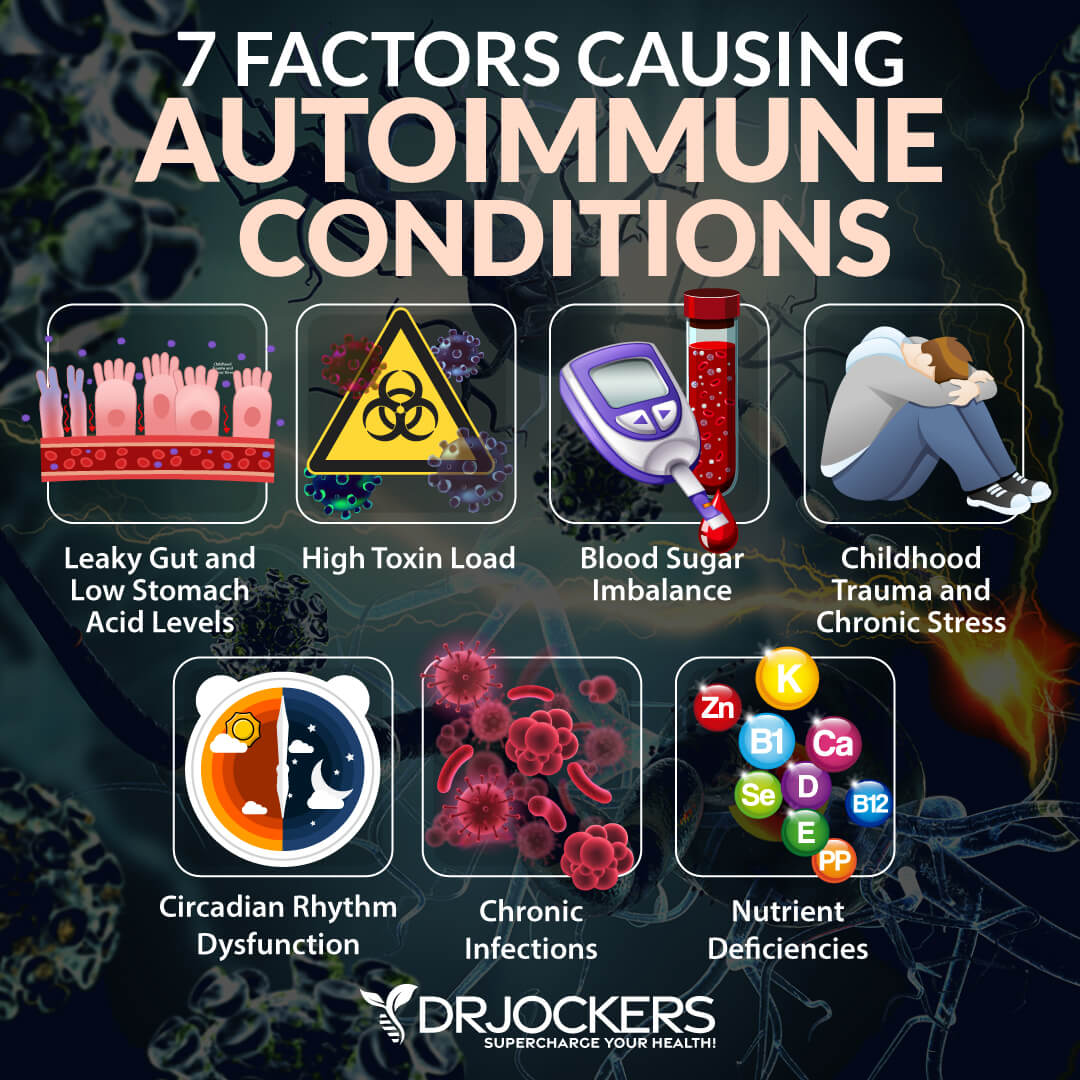
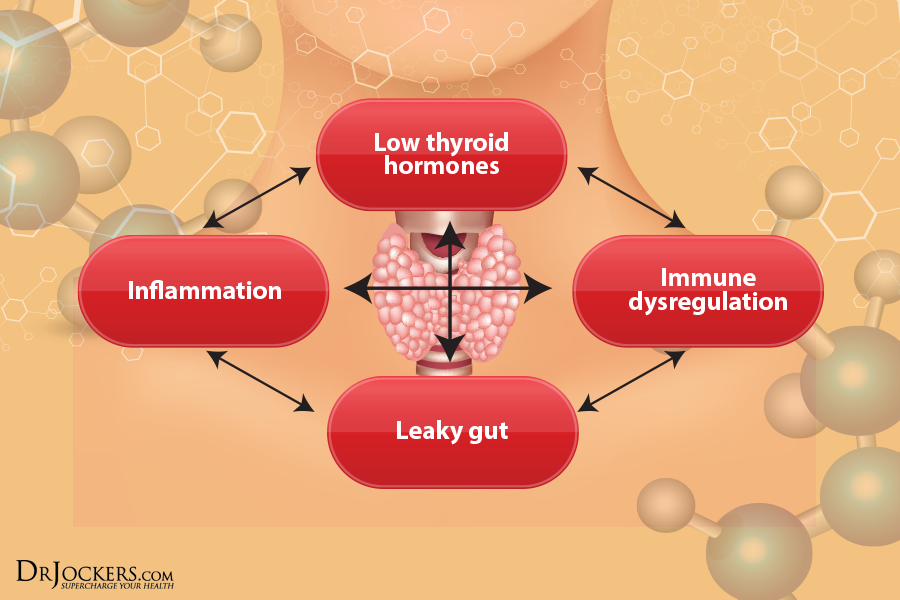
Most cases of hypothyroidism are characterized by a hyper responsive immune system and autoimmunity. There are several key factors that must be addressed to regulate and better coordinate the immune system.
1. Poor Blood Sugar Stability: Blood sugar imbalances cause immune dysfunction and malcoordination. Stable blood sugar is critical for a healthy immune response.
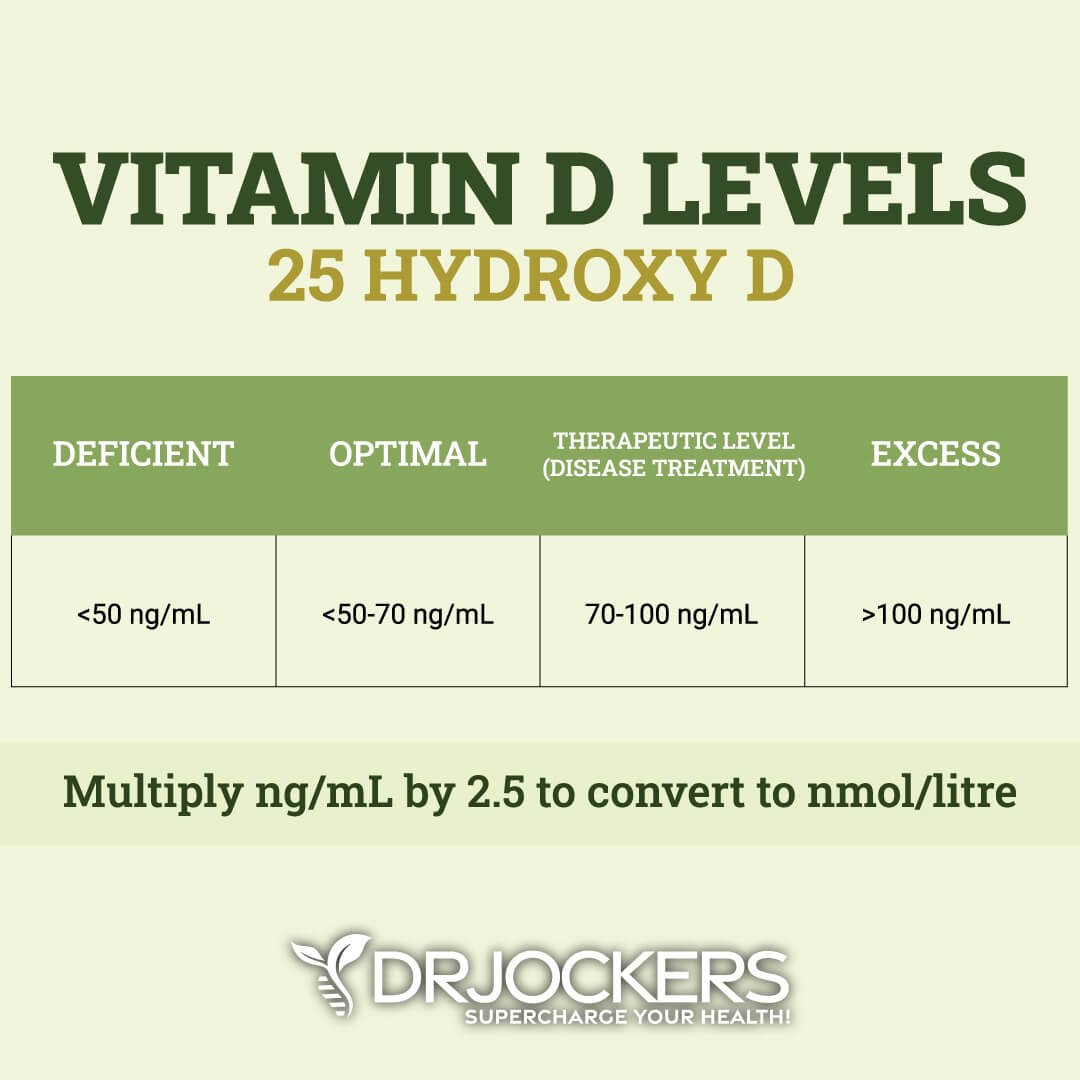
2. Low Vitamin D Levels: Individuals with low vitamin D3 levels (below 40 ng/ml) are at significant risk for developing chronic inflammation and autoimmunity (20).
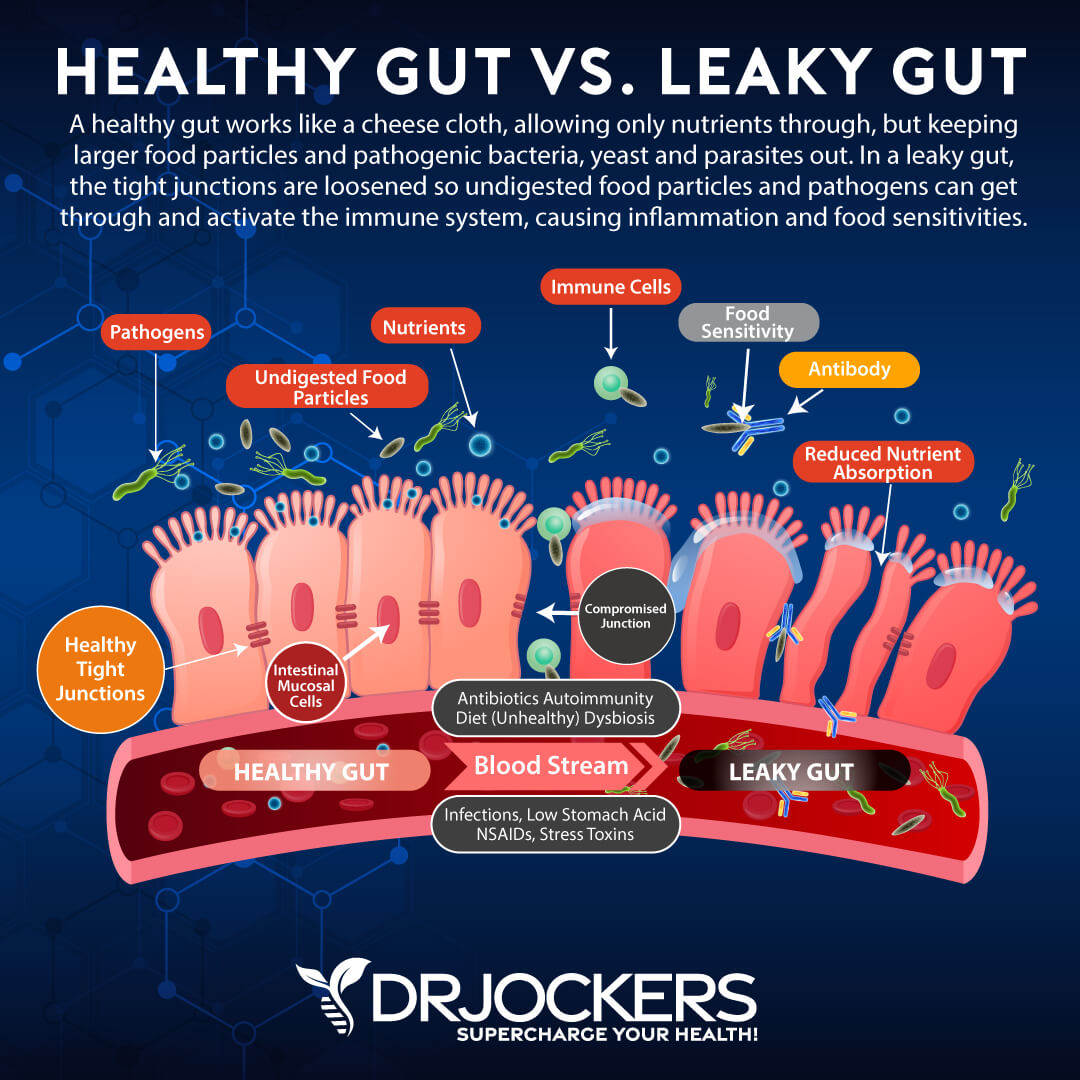
3. Gut Dysbiosis: Poor microbial balance in the gut microbiome leads to leaky gut syndrome, autoimmune conditions, and chronic inflammation (21). Eating an unhealthy diet, exposure to toxins, food sensitivities, chronic stress, and gut dysbiosis may lead to leaky gut.
Leaky gut happens when the gap junctions between the cells in your intestinal wall become too wide and allow large particles, such as toxins and undigested food molecules to enter your bloodstream.
Your immune system mistakes these molecules for foreign invaders and creates antibodies to fight them off. This immune response and your body’s way of attacking itself leads to chronic inflammation and autoimmunity. To learn more about leaky gut syndrome and how to repair it, read this article.
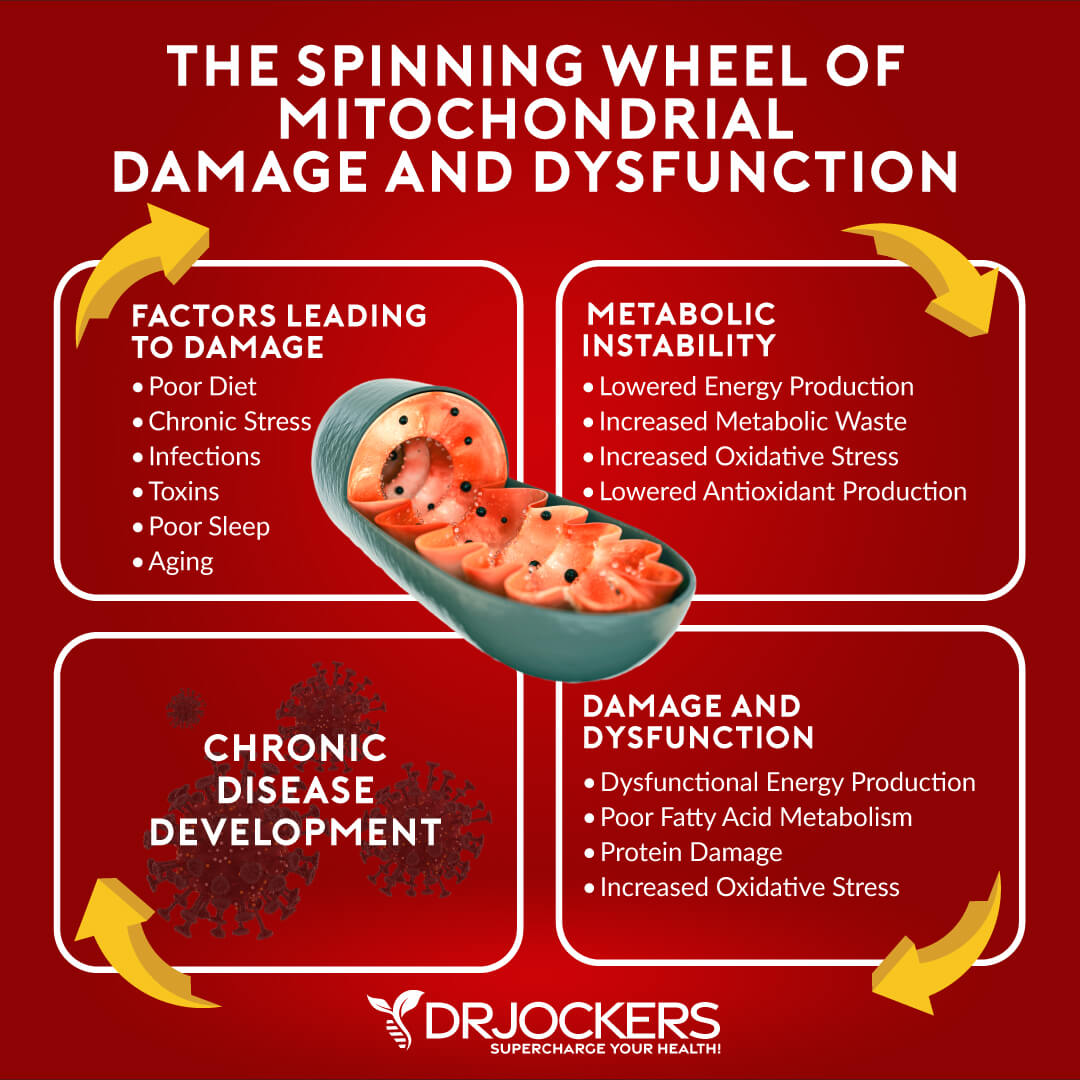
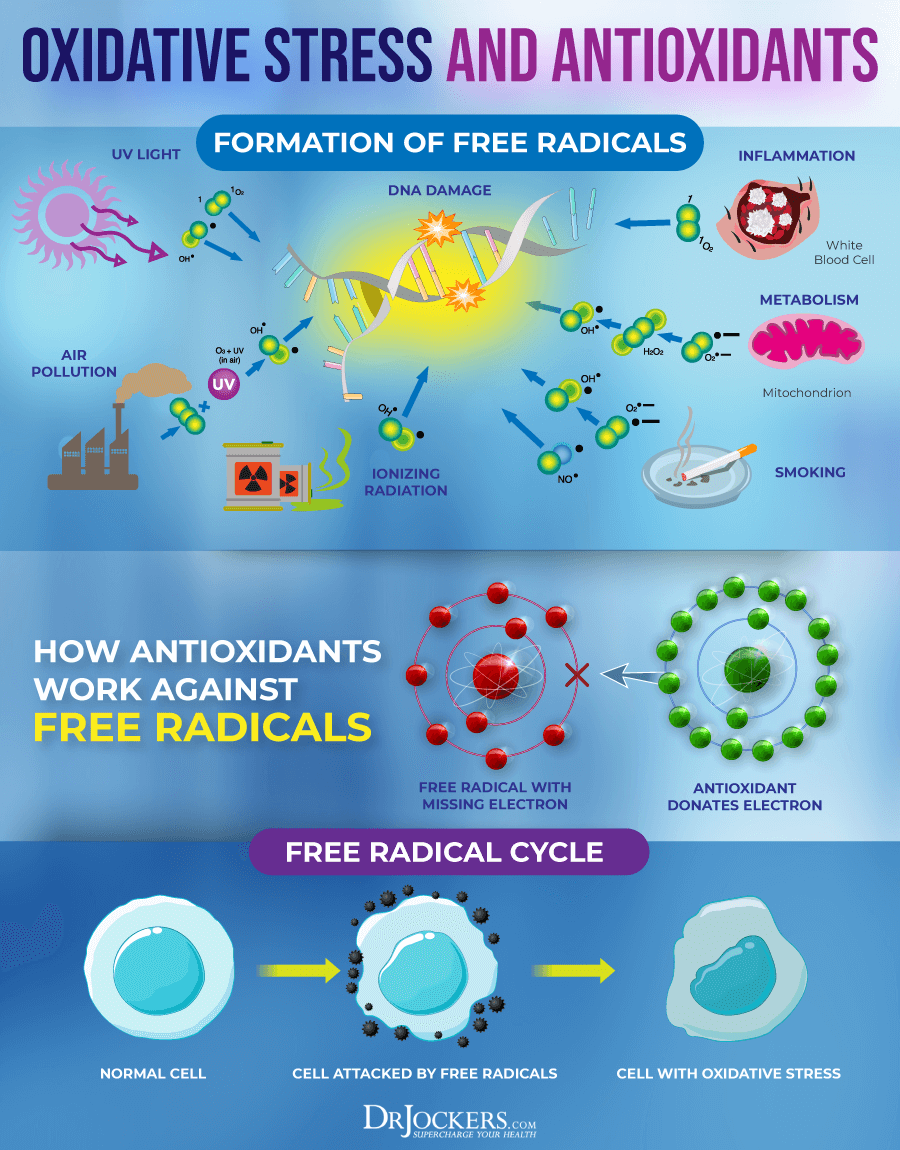
4. Mitochondrial Dysfunction: The mitochondria are the energy producing organelles in each cell of the body. They are extremely key in the body’s ability to handle oxidative stress.
Dysfunction in the mitochondria leads to increased free radical and oxidative stress which creates immune alterations. This is a classic sign in Hashimoto’s autoimmune pathophysiology (22).
5. Low Glutathione Levels: Glutathione is the major antioxidant within every cell of the body. It is critical for white blood cell (WBC) function as the WBCs encounter tremendous amounts of free radicals and oxidative stress every second of the day. Low glutathione leads to chronic inflammation and often to autoimmunity (23).
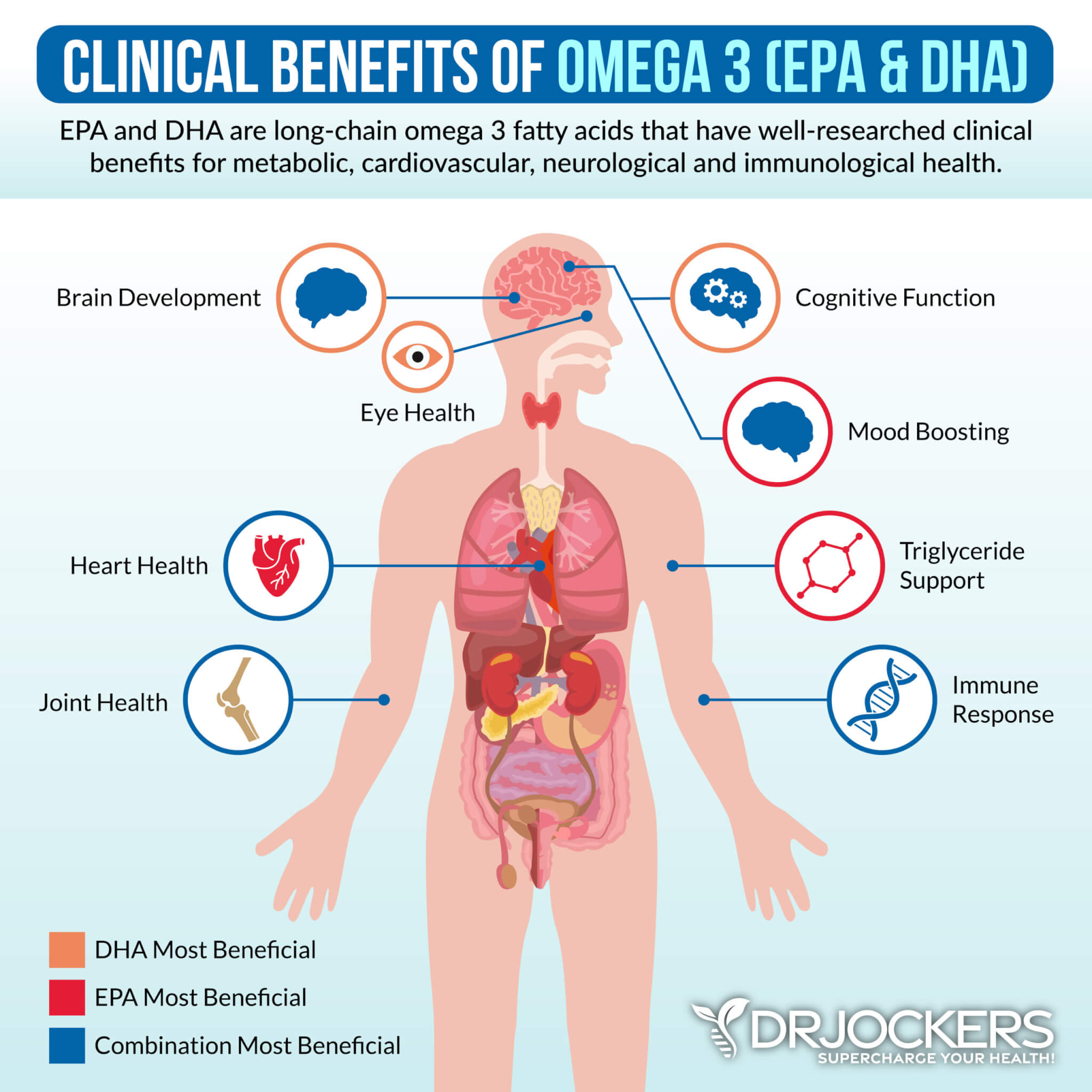
6. Poor Omega 6:3 ratio: The average person has significantly more omega 6 fats than omega 3 fats. The increased omega-6 stimulates the release of pro-inflammatory mediating prostaglandin molecules. This is a key factor in the development of chronic inflammation and autoimmunity (24).
7. Upper Cervical Subluxation: The bottom of the skull (occiput) and the first bone (atlas) play a significant role in the coordination patterns of the brain and immune system. Dysfunction at this joint torques and compresses the top of the spinal cord and increases inflammatory activity in the body (25).
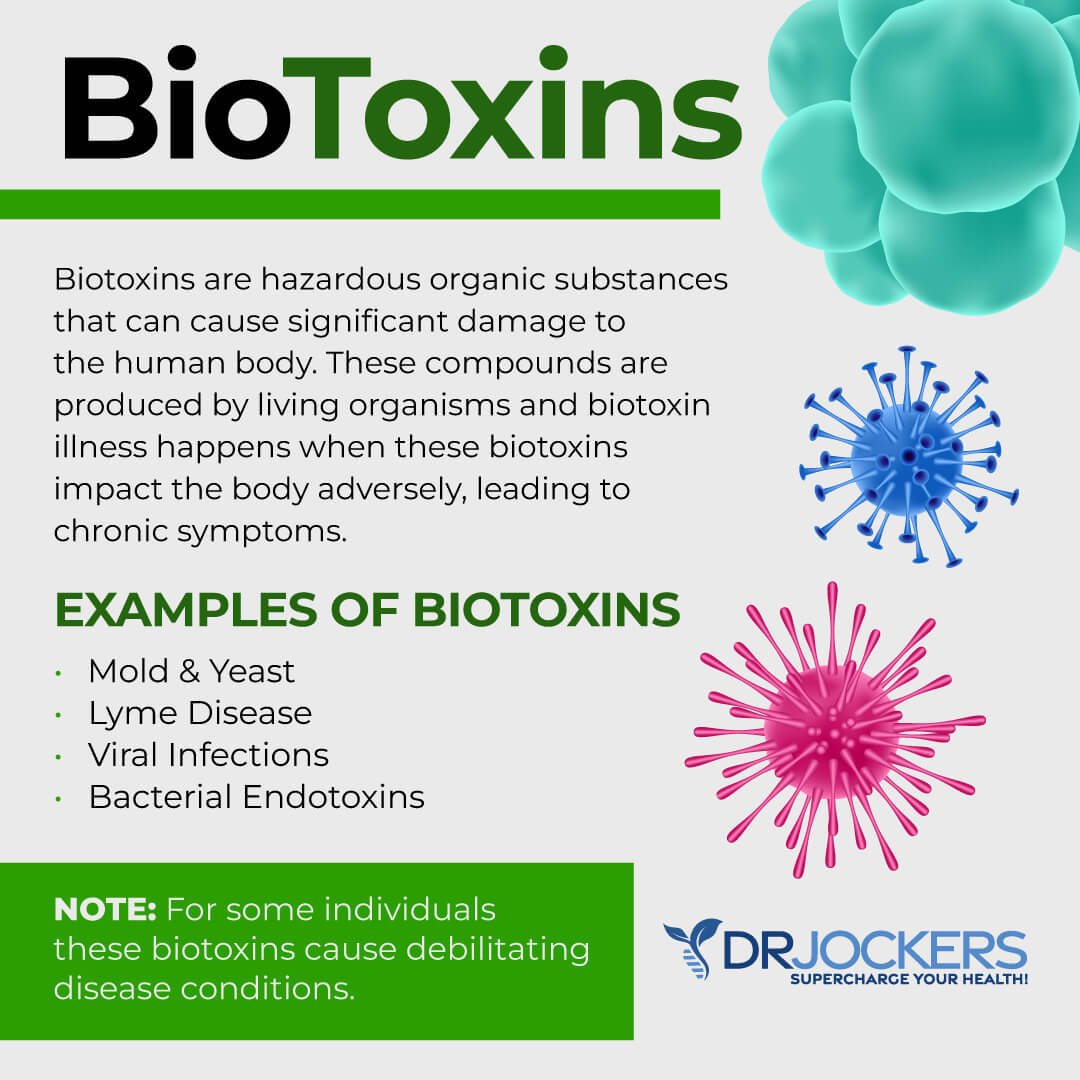
8. Environmental Toxins: Exposure to high levels of infectious microbes, environmental chemicals such as plasticizers, pesticides, herbicides, personal care products, heavy metals, and biotoxins such as mold, viruses, and parasites wear down the body’s glutathione levels, alter the gut microflora and increase inflammatory activity in the body (26, 27, 28).
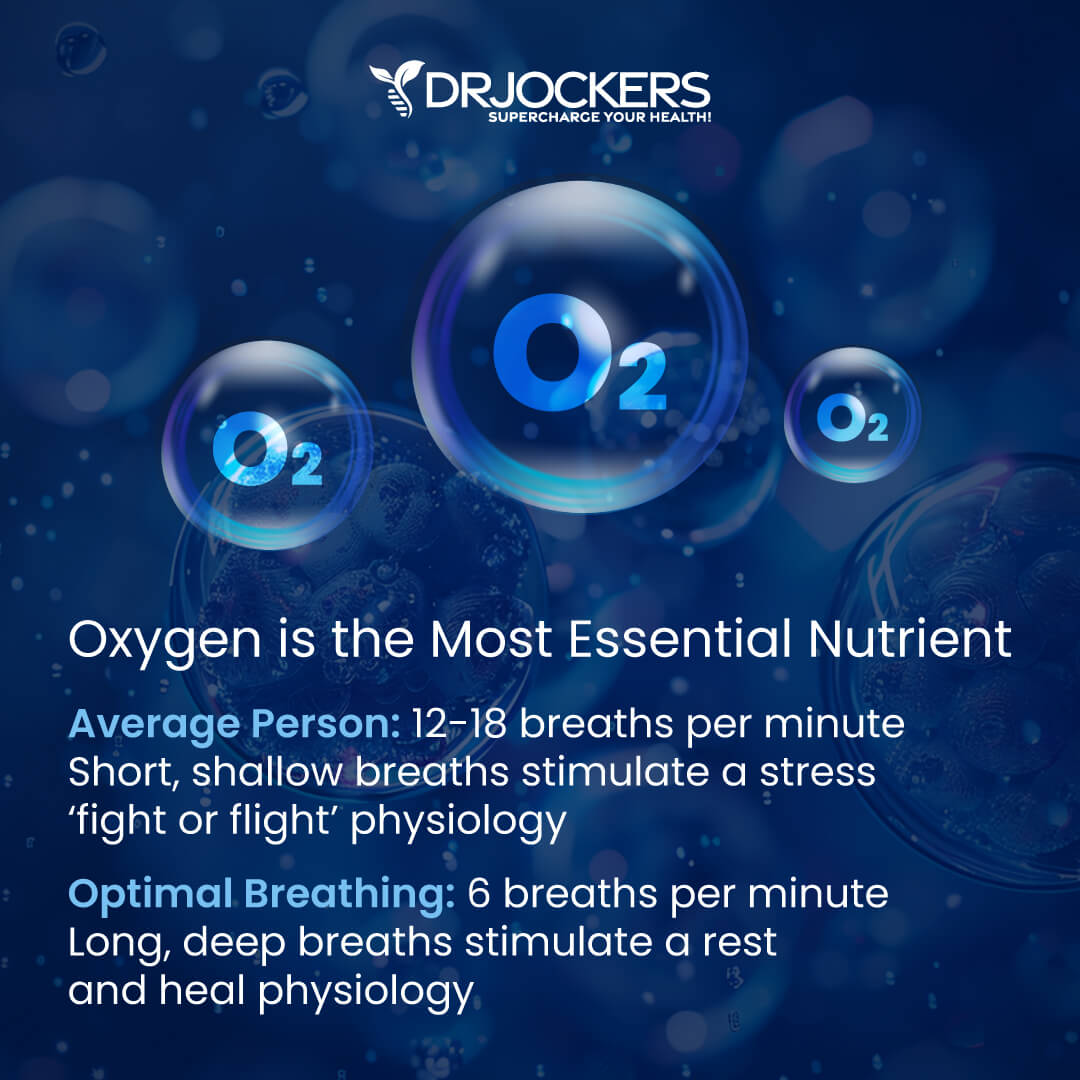
9. High Stress and Poor Breathing Habits: High mental and emotional stress increases stress hormone production which induces inflammatory activity within the body. Short and shallow breathing habits can simulate chronic mental and emotional stressors on the physiological level (29).
10. Lack of Sleep: Poor sleep promotes immune dysfunction and increased inflammation. Good sleeping habits and optimal melatonin secretion reduce inflammation and promote improved tissue healing (30).
11. Methylation: Methylation is a key process that protects DNA, turns on and off genetic traits, and helps to detoxify environmental chemicals. Many individuals have certain genetic polymorphisms that limit their ability to appropriately methylate. Methylation plays a very important role in T cell function and poor methylation status is associated with the development of autoimmunity (31).
12. EMF Exposure: Electromagnetic frequency exposure has been shown to alter the function of the immune system and increase one’s susceptibility to developing an autoimmune condition (32) I will touch on a few of these key areas and how they relate to hypothyroidism in this article.
Environmental Toxins and Thyroid:
The thyroid gland is one of the most sensitive regions of the body to environmental toxins. The most common environmental toxins affecting thyroid function include:
1) Industrial Pollutants: This includes the various pollutants we find in our air, food, and water that negatively affect the immune system and thyroid function. These come from our vehicle emissions, industrial chemical waste, and chlorine in our water supply. Pesticides, herbicides, and artificial chemicals in our food supply (33, 34, 35).
2) Ionizing Radiation: We are exposed to these through medical devices such as CT scans and mammograms, microwaves, and cell phones. We also are exposed to ionizing radiation when we fly in an airplane.
There is also thought to be nuclear radiation from powerplant explosions that is around us in varying amounts depending upon our geography. All ionizing radiation has a negative effect on thyroid function (36).
3) Heavy Metals: This includes mercury, lead, and aluminum. We find these in vaccines, fish and water supply, old paints, amalgam fillings, aluminum cans, etc (37, 38, 39).
4) Perfluorooctanoate (PFOA) These are dangerous chemicals found in nonstick pans. Be sure to avoid all nonstick pans, especially those that are not labeled as PFOA-free (40).
5) Fluoride: Fluoride is a halogen that competes with iodine uptake in the thyroid gland. Iodine is needed for the production of thyroid hormones. Fluoride is found in tap water, toothpaste, and many processed foods (41).
6) Bromide: Like fluoride, bromide is a halogen that competes for iodine uptake in the thyroid gland. Bromide is found in soft drinks and baked goods (42).
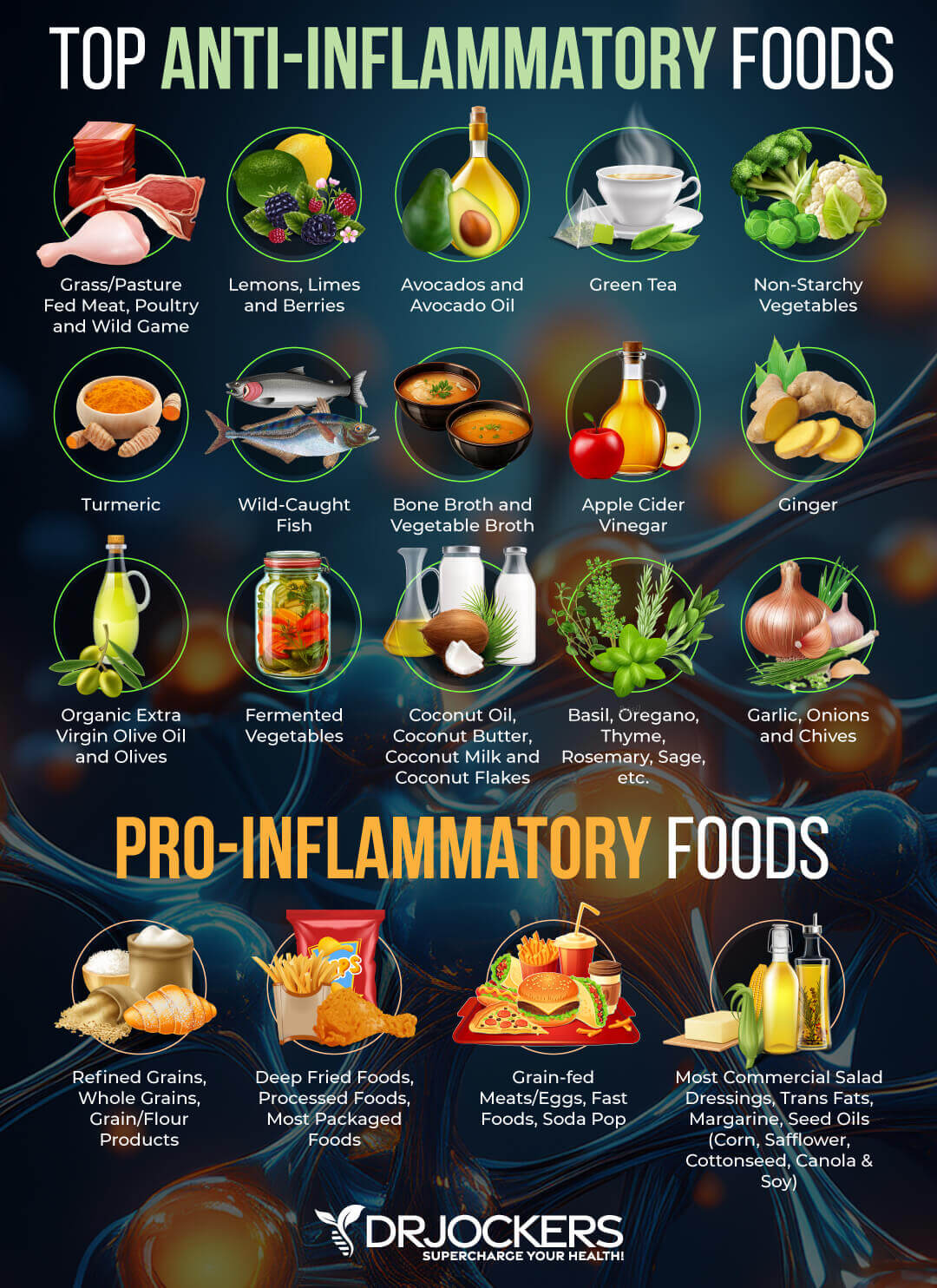
7) Inflammatory Foods: This includes industrial vegetable oils, high omega-6 fatty acids, GMOs, added sugar and artificial sweeteners, preservatives, gluten and soy containing foods.
Key Nutrients Needed:
Iodine: Iodine is critical for thyroid hormone production in the body. A true iodine deficiency will cause hypothyroidism (43). In western culture we often see subclinical iodine deficiencies which contribute to hypothyroidism (44). I typically don’t recommend high doses of iodine as it could be problematic with individuals with Hashimoto’s—especially with TPO antibodies.
I almost always have my clients take high doses (200–400 mg) of selenomethione each day and this reduces antibody formation and allows for better iodine utilization in the thyroid (45).
I have my clients get their iodine from a teaspoon of high quality sea vegetables each day in the form of kelp, dulse, nori, and dulse. Kelp is the richest source of iodine, so if the client is very iodine deficient, kelp usage gets the levels up the quickest.
Tyrosine: L-Tyrosine is the key amino acid for the production of thyroid hormones. This provides the necessary raw material for the formation of the backbone of thyroid hormone.
Vitamin A: The thyroid hormone binds to thyroid receptors and undergoes a process called intercellular transduction (46). This carries the message of binding to the nuclear receptors. Thyroid hormone nuclear transcription is dependent upon vitamin A in order to be activated (47).
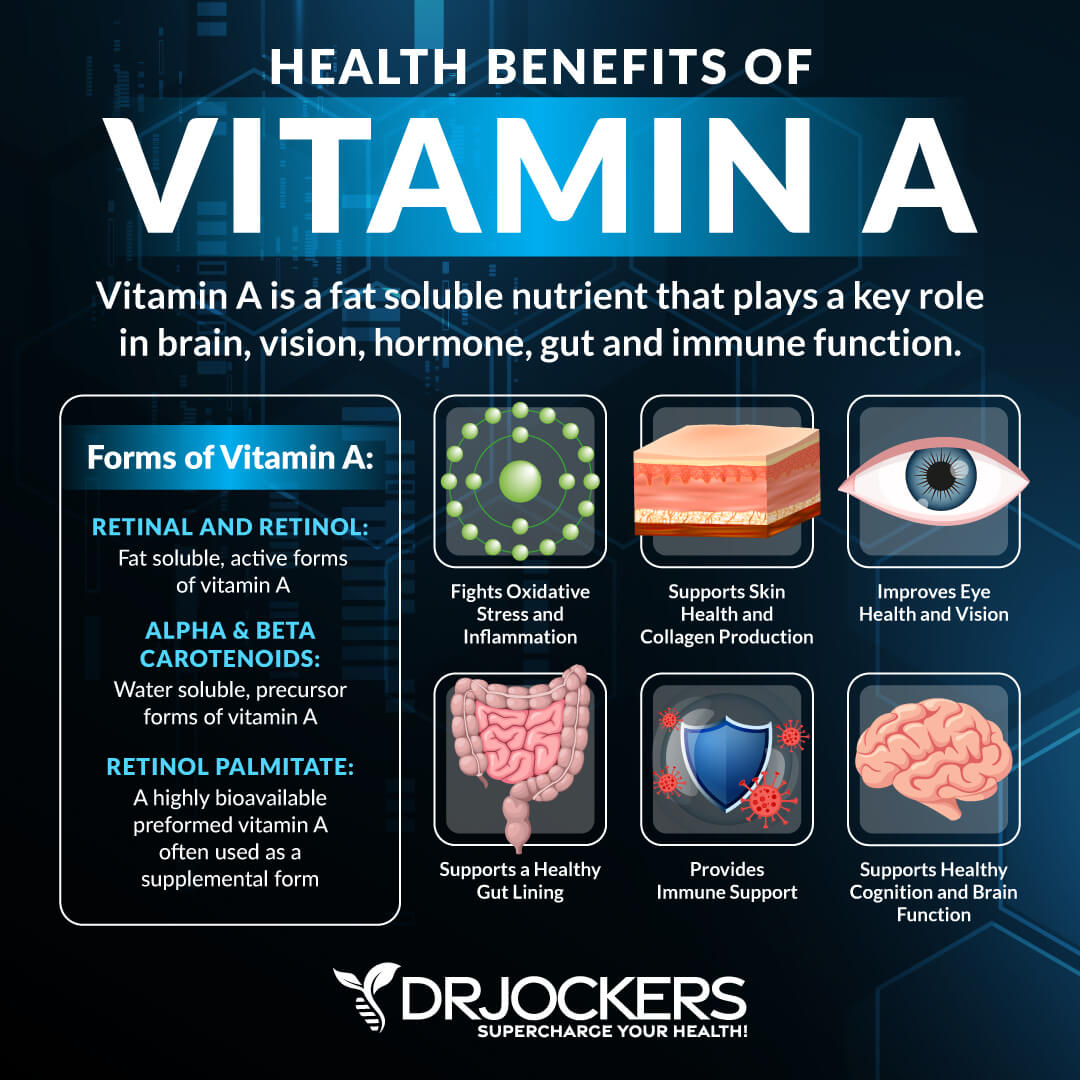
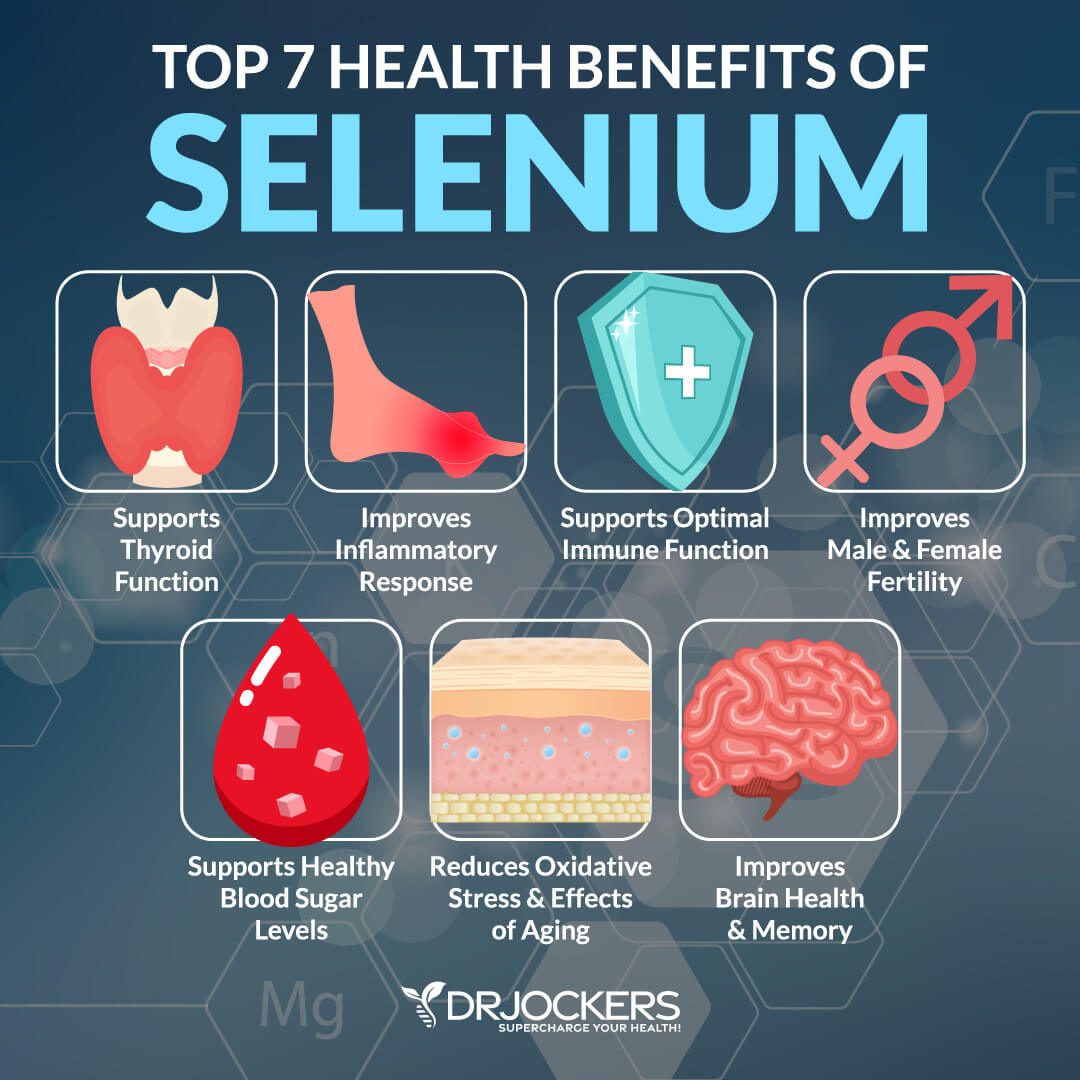
Selenium: Selenium is one the MOST IMPORTANT nutrients when it comes to healthy thyroid function! It is incorporated into key enzymes involved in several metabolic pathways implicated in thyroid hormone metabolism. Additionally, it plays an antioxidant role in the regulation of the immune system. There are strong links between selenium deficiencies and autoimmune thyroid problems (48, 49).
It has been hypothesized that these compounds activate a complex defense system that maintains normal thyroid function by protecting the gland from both hydrogen peroxide (H2O2), produced by thyrocytes and oxidative stress. This is the major cofactor for the key thyroid enzyme 5’deiodinase which is what converts T4 into T3. 5’deoidinase also degrades the inactive rT3.
Studies have indicated that individuals with lower selenium levels are at higher risk for low T3 (50). Selenium has been shown to reduce rT3 levels and improve active T3 status (51). It also reduces anti-thyroid antibody formation (52). Be sure to get selenomethionine which is the most effective form of selenium for reducing antibody formation and improving thyroid function.
Zinc: Low zinc status has been shown to compromise T3 production. Zinc plays an important role in immune modulation which may reduce thyroid antibodies (53). Additionally, it is a key player in 5’deiodinase activity.
Riboflavin – B2: Hypothyroidism induces the symptoms of riboflavin deficiency. This is because thyroid hormone is needed for the production of the enzyme flavin kinase, which is in turn needed to generate flavin adenine dinucleotide (FAD). Riboflavin deficiency and thyroid hormone deficiency lead to the same low FAD levels in both rats and humans.
Vitamin B6: Pyrodixal 5’phosphate is a co-enzyme participating in more than 100 enzymatic reactions in the human body. The activity of the hypothalamic-pituitary-thyroid axis in the setting of vitamin B6 deficiency has been studied in rats (54).
Well-conducted experiments have shown that vitamin B6 deficiency leads to hypothyroidism. B6 supplementation also helps quiet an overactive immune system which is helpful in cases of autoimmune thyroid disorders (55).
Vitamin C & E: These are both key antioxidants that protect the thyroid gland from oxidative stress and improve immune regulation.

Blood Sugar Balance:
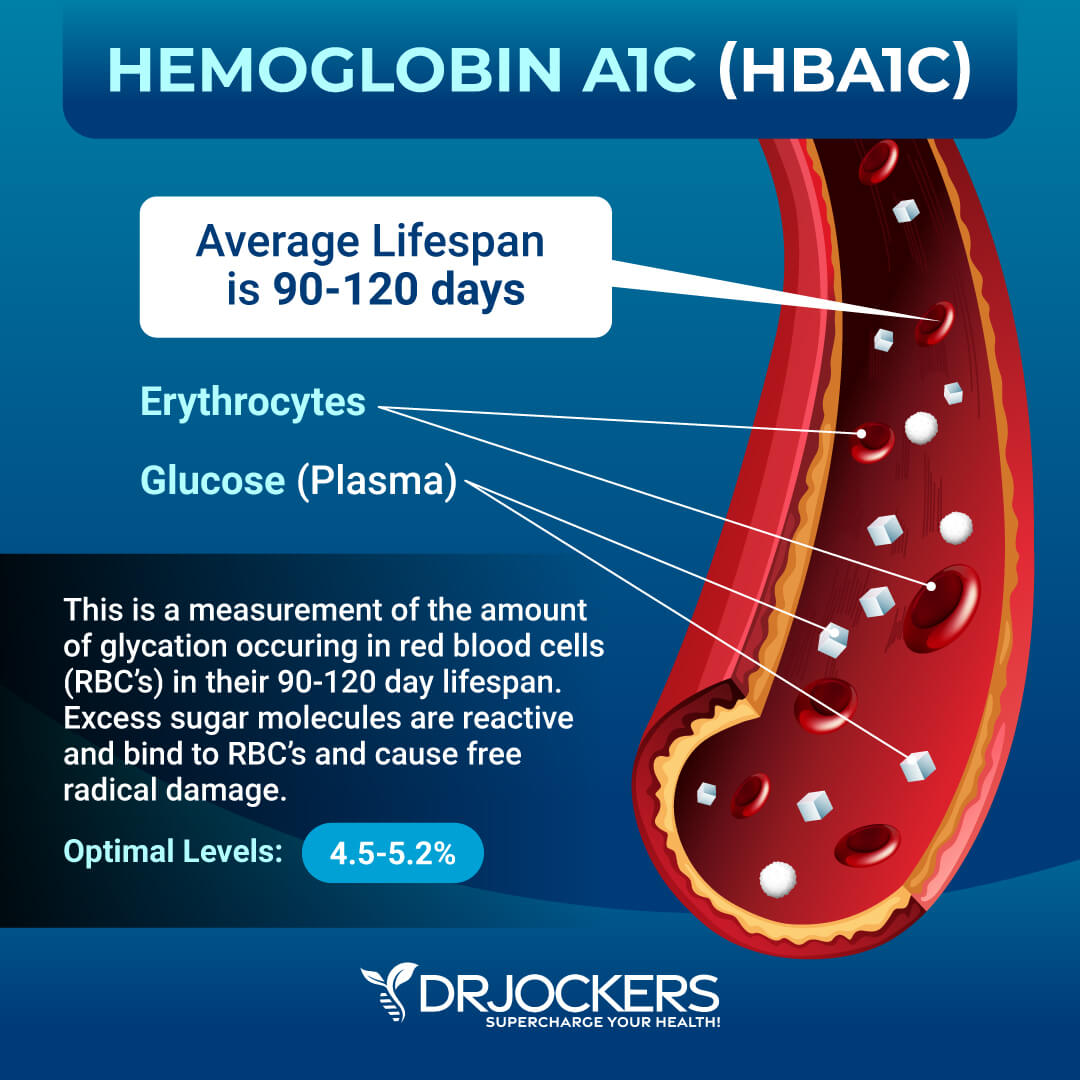
Blood sugar imbalances are major contributors to the development of hypothyroidism. When our blood sugar gets too high (hyperglycemia) the sugar molecules bind to proteins in the body and create Advanced Glycolytic Enzymes (AGEs) (56). The AGEs destroy cell membrane function and damage insulin receptor activity creating a vicious cycle of elevated blood sugar and inflammatory stress.
AGEs cause massive destruction throughout the body and have an affinity for thyroid tissue. Elevated HbA1C (a measure of glycation) is correlated with increased TSH and decreased free T3 & T4 (57). When the blood sugar drops too low (hypoglycemia), it increases stress hormones (cortisol and adrenaline) to boost blood sugar. Cortisol directly inhibits the enzyme (5’-deiodinase) which converts inactive T4 into active T3.
This can lead to low T3 levels (58). In addition, elevated cortisol will cause thyroid hormone receptor insensitivity meaning that even if T3 levels are high enough, they may not be able to bind normally to receptor sites. And when this happens it doesn’t get into the cells. Cortisol will also increase the production of reverse T3 (rT3), which is inactive (11).
The MicroBiome and Thyroid Disease:
The gut microbiome is made up of over 1000 different species of microbes and it plays a huge role in nutrient absorption, detoxification, and the development and maturation of the immune system (21). Certain bacteria of the gram negative classification are known to release a potent inflammatory mediator called lipopolysaccharide (LPS).
Individuals with hypothyroidism and Hashimoto’s are known to have dysfunctional characteristics involved in their microbiome (59, 60). Elevated levels of LPS have been shown to affect pituitary TSH stimulation, T4 production, and TBG production.
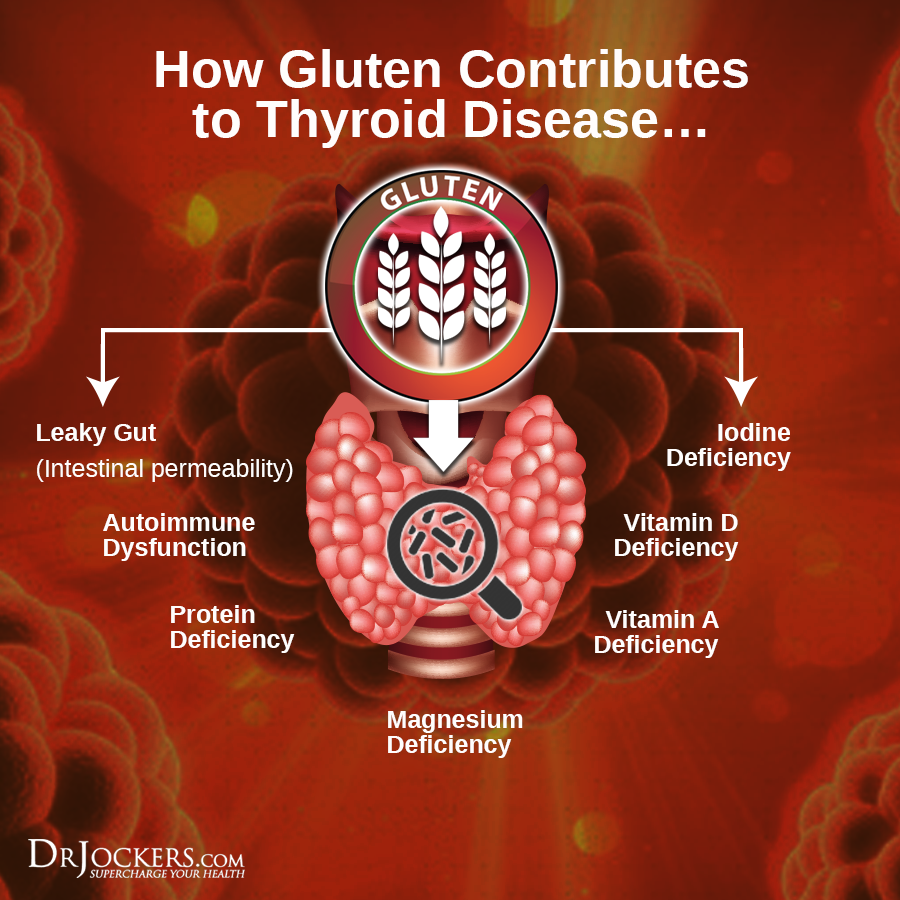
Gluten and Thyroid Disorders:
Gluten is the common protein found in wheat, barley, and rye. Gluten is a sticky, storage protein that is challenging for the digestive tract because it binds to the small intestinal wall where it can cause digestive and immune system disorders. Gluten sensitivity is an epidemic that is a major contributing factor to inflammatory and autoimmune diseases (61, 62).
Gluten intolerance is highly associated with inflammatory disorders of all kinds (63). It is also a contributing factor in many autoimmune diseases such as celiac disease, rheumatoid arthritis, type I diabetes, Hashimoto’s thyroiditis, autoimmune cardiomyopathy, lymphoma, and dermatitis herpetiformis (skin disease) among others (64, 65). If you have a thyroid problem or just want to avoid having a future thyroid problem, the first step to begin a gluten-free nutrition program!
Anti-Inflammatory Lifestyle:
An anti-inflammatory lifestyle is critical for full recovery from hypothyroidism. Anti-inflammatory foods help to modulate the immune system and give it a more accurate pair of eyes so as to not over-inflame when stimulated. To effectively de-inflame one must completely avoid man-made foods, sugars, and food sensitivities as listed above.
This nutrition plan is rich in phytonutrient dense vegetables, healthy fat, and clean protein sources. Non-starchy vegetables, herbs, and teas are great sources of antioxidants. Healthy fat sources include coconut products, grass-fed ghee, avocados, olive oil, nuts, seeds, and purified omega-3 fish oil supplements.
Healthy protein includes wild-caught fish, grass-fed red meat, free-range chicken, turkey, and eggs (although these are usually eliminated for the first 30 days, then added slowly to see if the individual to tolerate them). Be careful to watch for any hidden food sensitivities.
Tips For Supporting Thyroid Health
Here are the best action steps to get started with on your journey to support your thyroid health. It is important to note that these strategies are not currently FDA-approved to prevent, mitigate, treat, or cure hypothyroidism and should not be confused as such.
You should always consult with your physician before stopping or changing medications or taking on new health strategies. Additionally, you should be working with a functional health practitioner to help guide you through these strategies. This is not an exhaustive list and there are other natural therapeutic strategies that I and functional health practitioners will utilize to help individuals with Hypothyroidism.
Change Your Diet:
Eating an anti-inflammatory diet rich in nutrient-dense foods is the first best thing you can do to prevent autoimmunity and thyroid problems. First, eliminate all inflammatory foods, including refined sugar, gluten, refined oils, deep-fried and processed foods, conventional dairy, grain-fed meat and eggs, soda and sugary drinks, and foods that you are sensitive to.
Instead, it is important to eat an anti-inflammatory diet that is rich in nutrient-dense vegetables, low glycemic index fruits, herbs, spices, healthy fats, grass-fed meat, and wild-caught fish. These foods provide an array of important nutrients that support healthy thyroid function and a healthy inflammatory response.
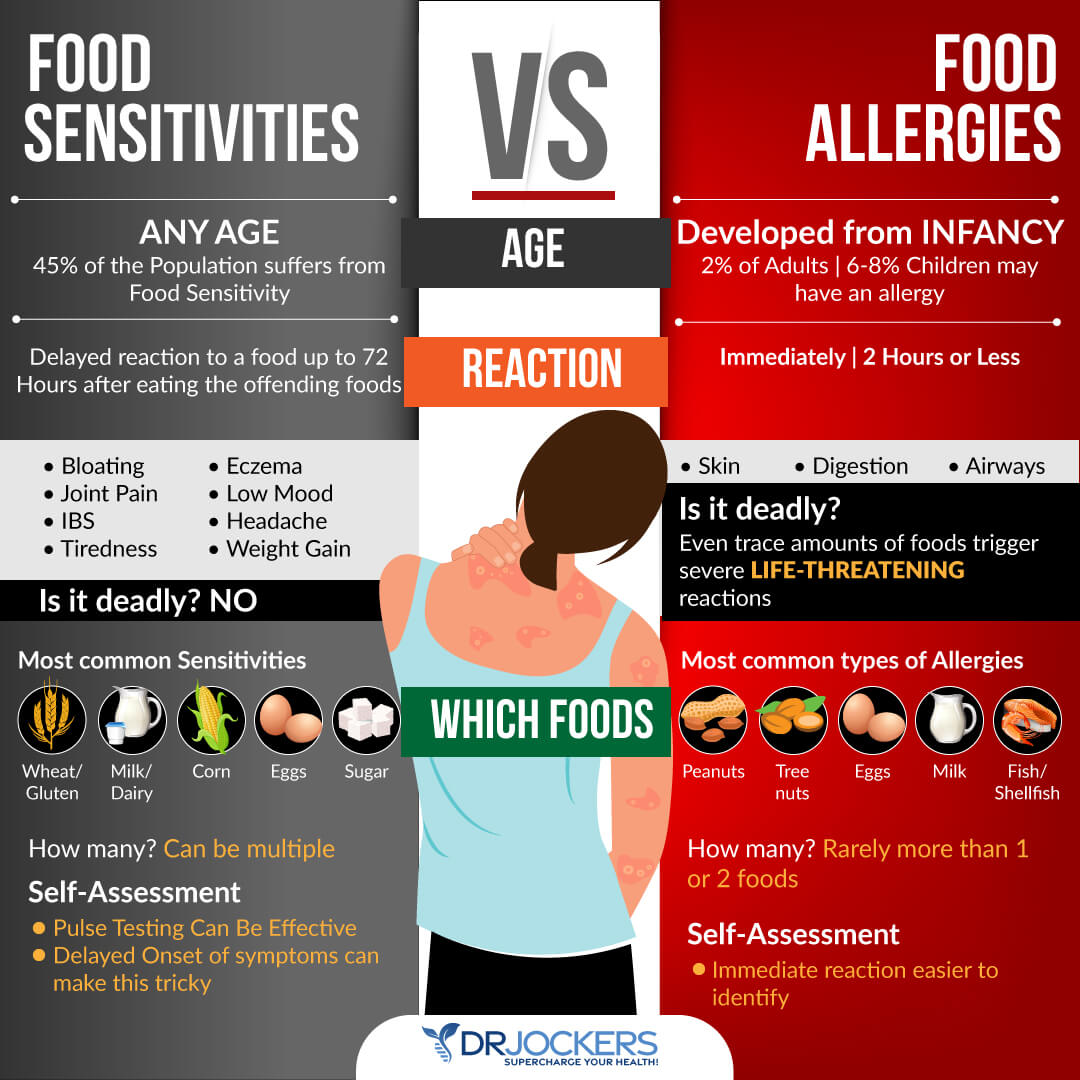
Test For Food Sensitivities:
Most people with autoimmune conditions have a leaky gut and food sensitivities. These sensitivities can be hard to pinpoint as they result in delayed symptoms that are not life threatening.
The most common food sensitivities include gluten, corn, dairy, soy, peanuts, and sugar. Some other potential food sensitivities to consider include all grains, eggs, nuts, seeds, and nightshade vegetables (tomatoes, potatoes, peppers, and eggplant).
It can be helpful to do a 28-day elimination diet where you remove all of these and then slowly add these back in one at a time. You can also do both biofeedback and blood testing to determine what foods are causing stress in your system and an elimination diet to test how you are responding to eliminating certain foods for periods of time.
Reduce Stress:
Reducing stress is a critical for reducing inflammation and improving immune and thyroid health. I recommend that you reduce stressors in your life as much as possible. Turn off the news, and only look at it once a day or a few times a week for a specific period. Reduce your social media use and time on the internet.
Avoid people and situations that bring you down. Surround yourself with loving and uplifting people. Engage in uplifting and relaxation-promoting activities. Read, try some arts and crafts, play cards or board games, sing, and dance.
Spend time in nature and do some grounding walking barefoot on grass. Practice daily gratitude and try positive affirmations. Practice self-love and laugh with friends and family. Meditate, pray, journal, and try daily breathing exercises. Be grateful and smile more.
Improve Your Sleep:
Prioritizing good sleep is just as important as reducing your stress levels. Develop a regular schedule of going to bed and getting up at the same time every day to support your circadian rhythms.
Avoid electronics, sugar, caffeine, heavy foods, and stress close to the bed. Engage in relaxing activities, including stretching, relaxing baths, meditation, and prayer. Make sure that you have a supporting bed, pillow, and bedding, and sleep in a dark calming room.

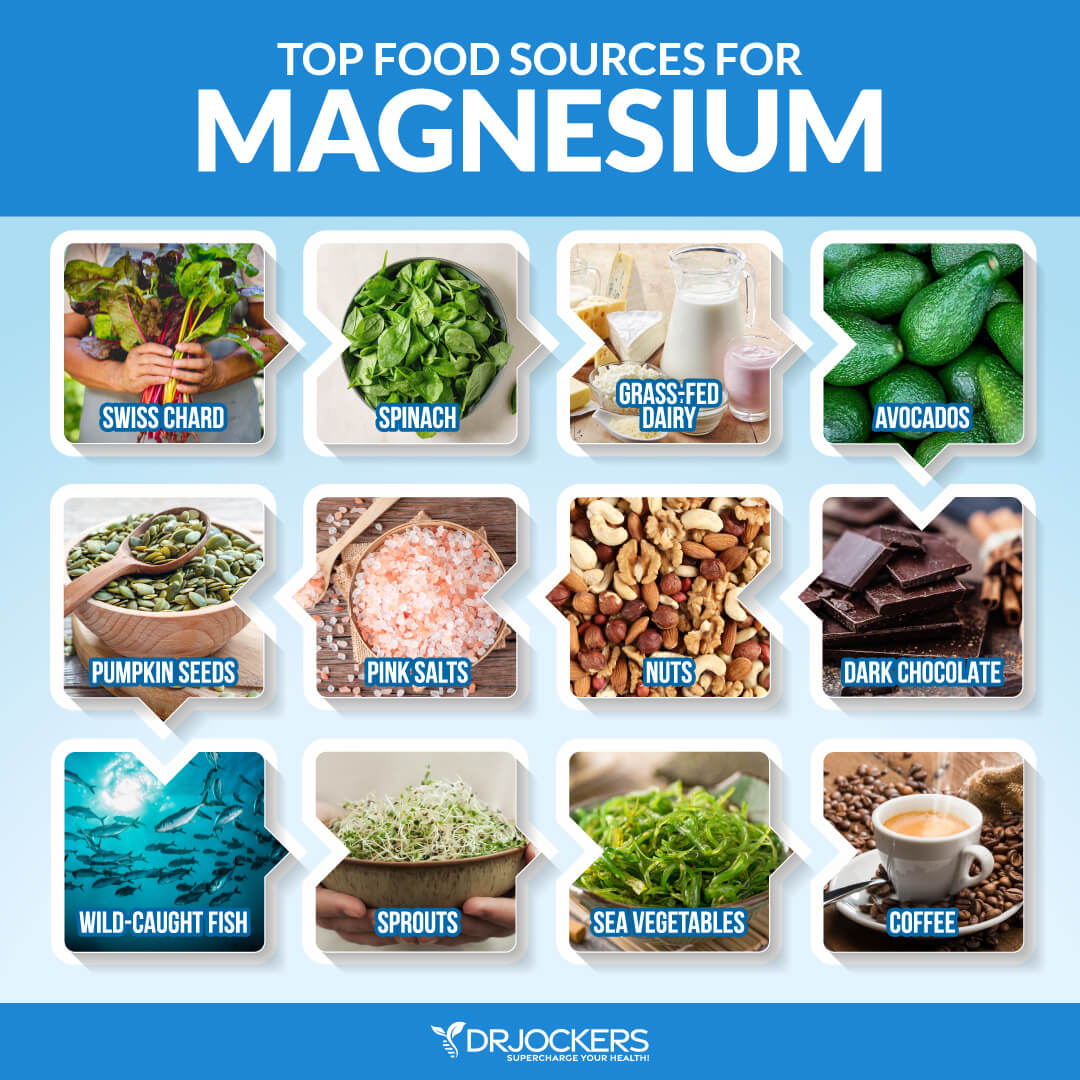
Include Magnesium & B Vitamin Rich Foods:
Magnesium helps to improve blood sugar signaling patterns and improves mitochondrial health. The best magnesium and B vitamin-rich foods include dark green leafy vegetables, avocados, grass-fed animal products, raw cacao, and pumpkin seeds.
You can also do Epsom salt baths to support your magnesium levels. It would also be wise to supplement with a good magnesium and B complex supplement. Look for magnesium L-threonate which is the best form of magnesium for crossing the blood-brain barrier.
When it comes to B vitamins, it is best to look for one with pre-activated forms such as methyl-folate, methyl-cobalamin (B12), Pyridoxal-5-Phosphate form of B6, and Riboflavin-5-phosphate form of vitamin B2. The methyl groups are in the active form and will be better utilized by the body.
Focus on Deep Breathing:
Improving your posture, seeing a high-quality chiropractor, and optimizing your breathing patterns are highly recommended. Taking time to slow down your breathing and take long, deep breaths for a few minutes every hour will help reduce the sympathetic, fight-or-flight part of the nervous system.
The better we breathe, the better we will heal, the more blood flow we will get, and the better our immune and inflammatory health will be. Follow these tips here to improve your breathing patterns.
Use Antioxidant Rich Herbs:
Carminatives are herbs that help to improve digestive health by reducing pathogens in the gut, stimulating the production of stomach acid, bile, and pancreatic enzymes, and modulating the gut microbiome.
Examples of these herbs include turmeric, ginger, oregano, garlic, basil, thyme, and rosemary. These herbs help to improve digestion, reduce inflammation, and support a healthy thyroid. There are a number of ways to use these that I discuss in the following image. I like putting herbs on foods, using herbal teas, fermented foods, and essential oils.
Supplement With Omega 3s:
Omega 3 fatty acids and in particular the long chain variety EPA and DHA are critical for stabilizing blood sugar, reducing inflammation and autoimmunity, and improving thyroid health. Consume grass-fed meat, grass-fed butter, wild-caught fish, seafood, and spirulina to get omega-3s in your diet.
Plant-based omega 3s such as flax oil only contain the small chain omega 3 called ALA and do not have any DHA. It is very hard for our body to convert ALA into DHA so it is best to get a high-quality fish or krill oil that is rich in EPA and DHA. You want to find a brand that is molecularly distilled to take out any heavy metals and other unwanted contaminants.
Be sure to discuss with your physician before using, as fish oils have a blood thinning effect and can be contraindicated if you are on blood thinning medications.
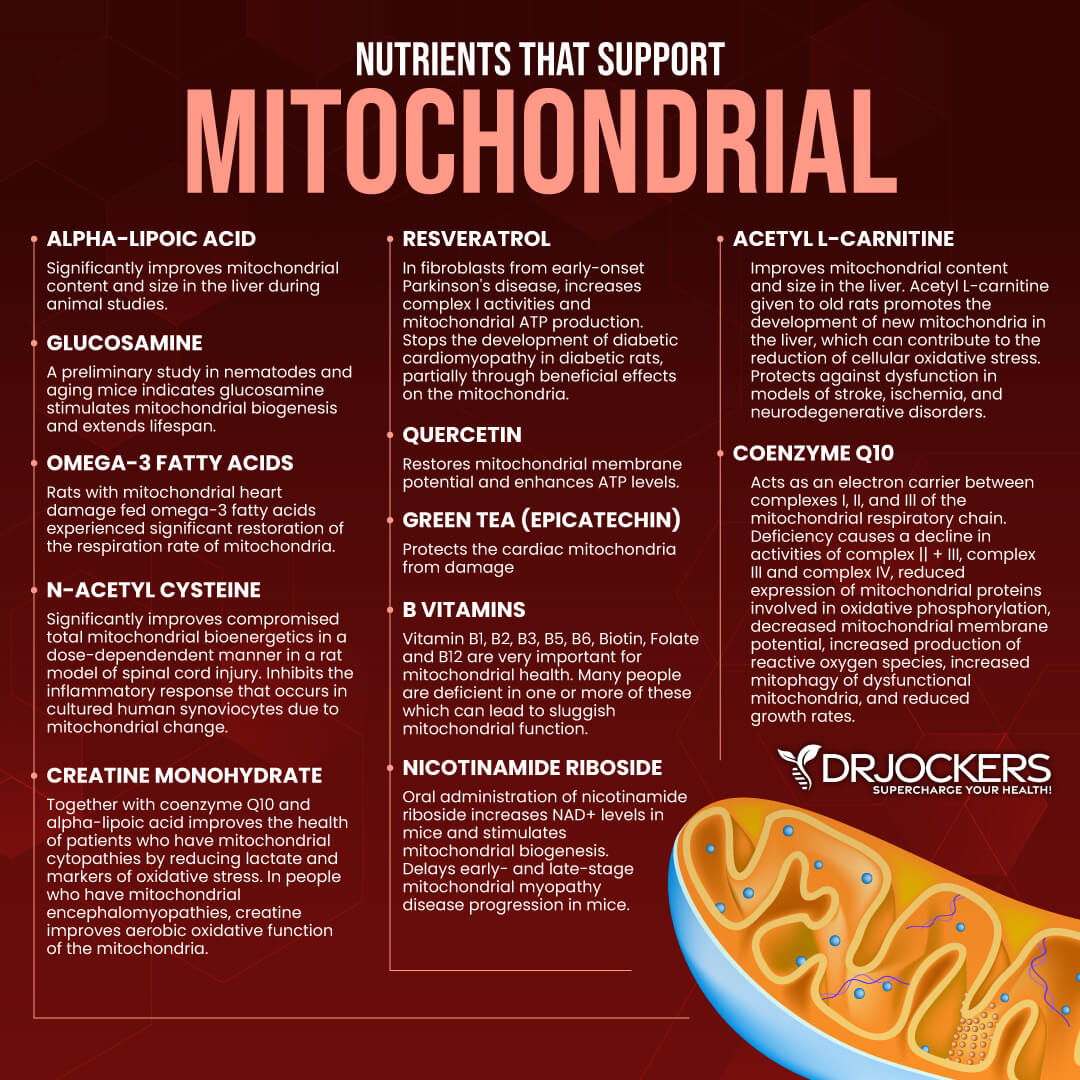
Improve Your Mitochondria:
The mitochondria are the energy powerhouses of every cell. When someone has an autoimmune disorder or chronic fatigue it is a clinical sign that they have dysfunctional activity going on in the mitochondria. This is especially important when it comes to hypothyroidism.
Support your mitochondria with clinical doses of CoQ10, L-carnitine, N-acetyl cysteine, creatine monohydrate, B vitamins, magnesium, alpha lipoic acid, and D-ribose. You can find mitochondrial support supplements that have most if not all of these key nutrients.
Optimize Your Vitamin D:
Low vitamin D3 is associated with chronic inflammation and autoimmune conditions. Vitamin D is arguably one of the most powerful nutrients responsible for modulating and coordinating the immune system.
In autoimmune disease, the immune system has a hard time differentiating self from non-self (foreign invaders). Vitamin D helps the immune system make this important distinction, which reduces autoimmune disease formation (48). Vitamin D also helps to modulate the immune system to reduce inflammation throughout the body (49).
Support Gut Health
To reduce inflammation and autoimmunity, you have to repair and heal your intestinal lining. I recommend eating a gut friendly diet that works best for your body type.
Consuming liquid nutrition is great for stimulating the digestive process, increasing nutrient absorption, and improving gut health. Liquid nutrition does not require as much energy to digest, so your body can focus on healing and repair. You can combine liquid nutrition with fasting strategies for quicker healing.
Using a good quality bone broth collagen in a shake or smoothie is a great way to include liquid nutrition in your diet. Collagen contains amino acids, including glycine and glutamine, which are essential for healing leaky gut. These amino acids seal the holes in the gut by healing damaged cells and building new tissue. Collagen also makes up the villi, small finger-like structures on the intestinal wall and assists with water absorption in the intestines.
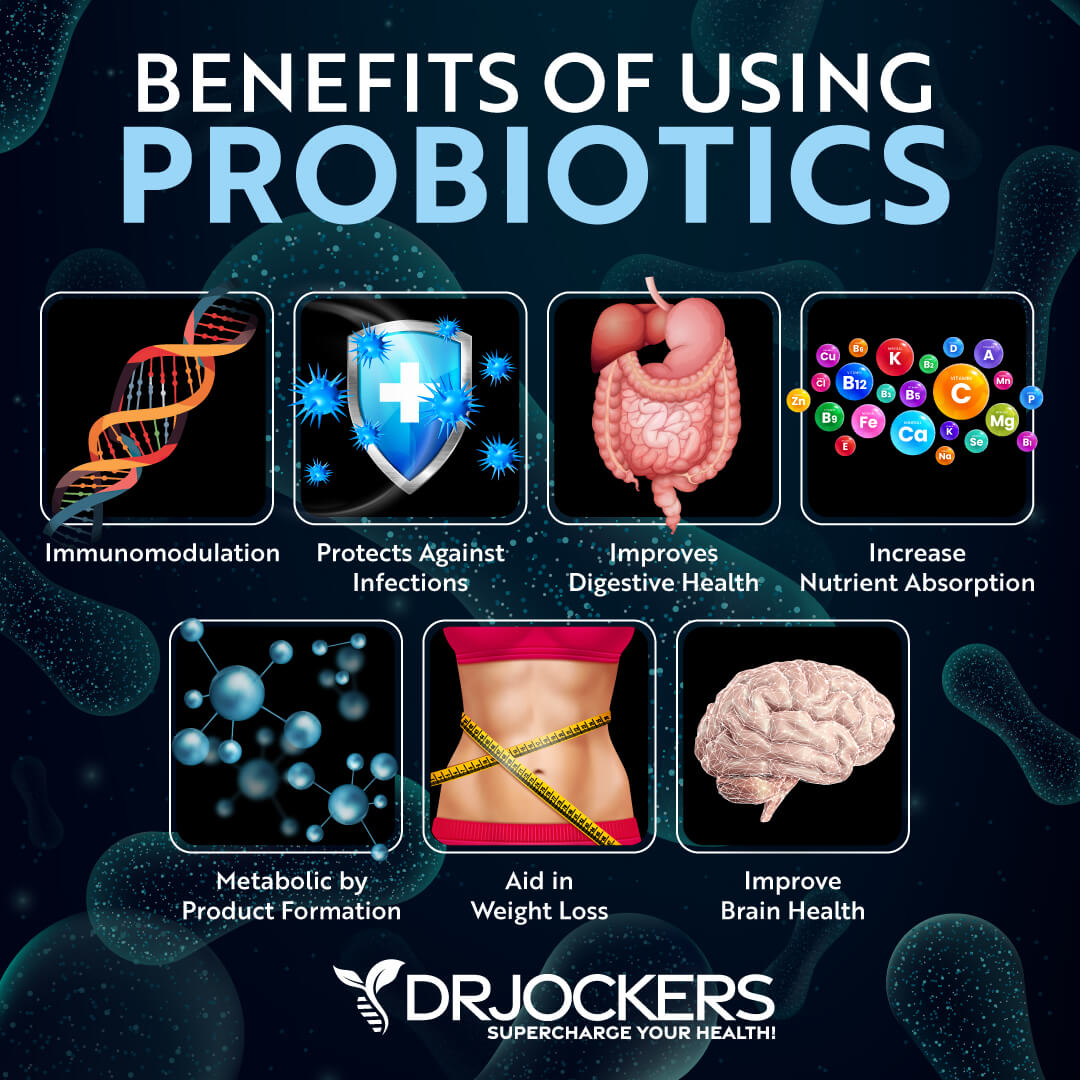
Additionally, I recommend taking a daily probiotic supplement. Probiotics help to optimize your gut health and improve your nutrient absorption while reducing gut related inflammation. When gut inflammation goes down it also reduces inflammatory mediators that impact thyroid health. In addition, a healthy microbiome is important for converting T4 into T3 for optimal thyroid hormone expression.
Ground Your Body:
In our society, we are surrounded by toxic electromagnetic frequencies (EMF). These EMFs increase stress and inflammation within the body and can be a trigger for autoimmune activity in some individuals.
By going outside daily and walking barefoot on grass, dirt, or sand you absorb natural EMFs from the ground that balance your electrical rhythms. Follow the steps in this article here.

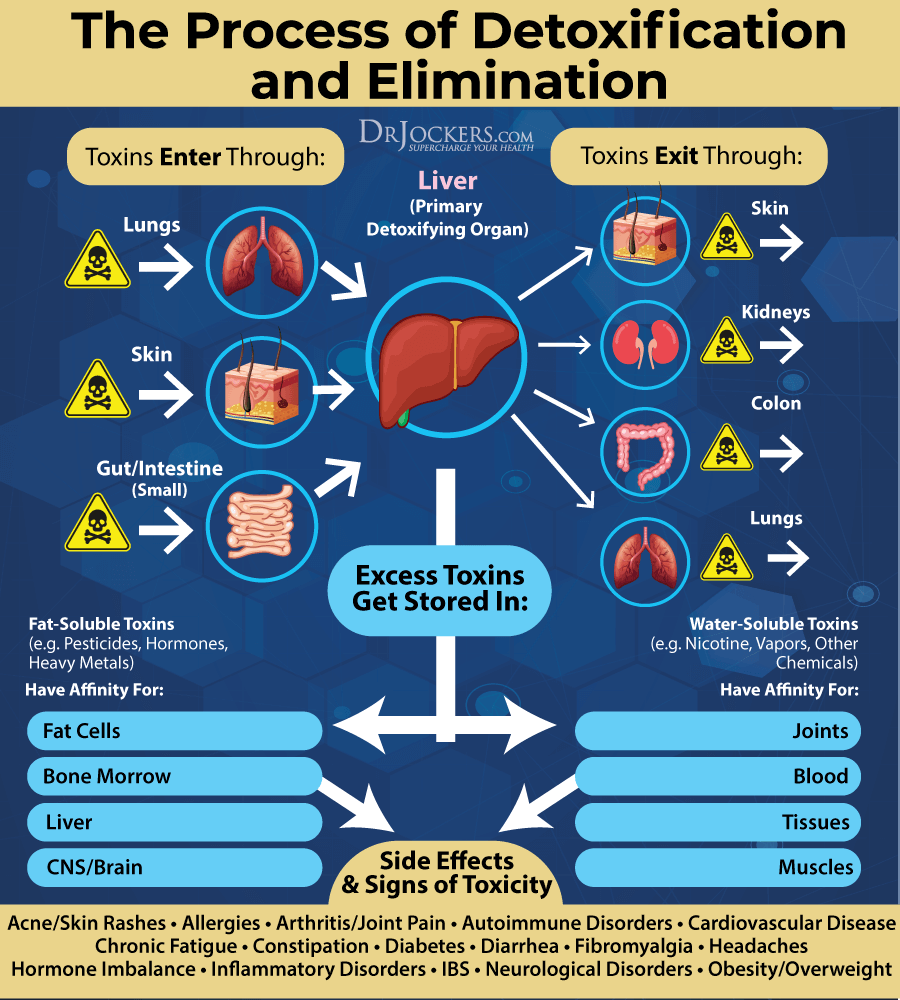
Reduce Toxin Exposure
Reducing your toxic exposure is critical for improving liver function and reducing inflammation. Buy organic food as much as possible. Stop using conventional beauty, body, and household products, and replace them with organic, natural, or homemade alternatives.
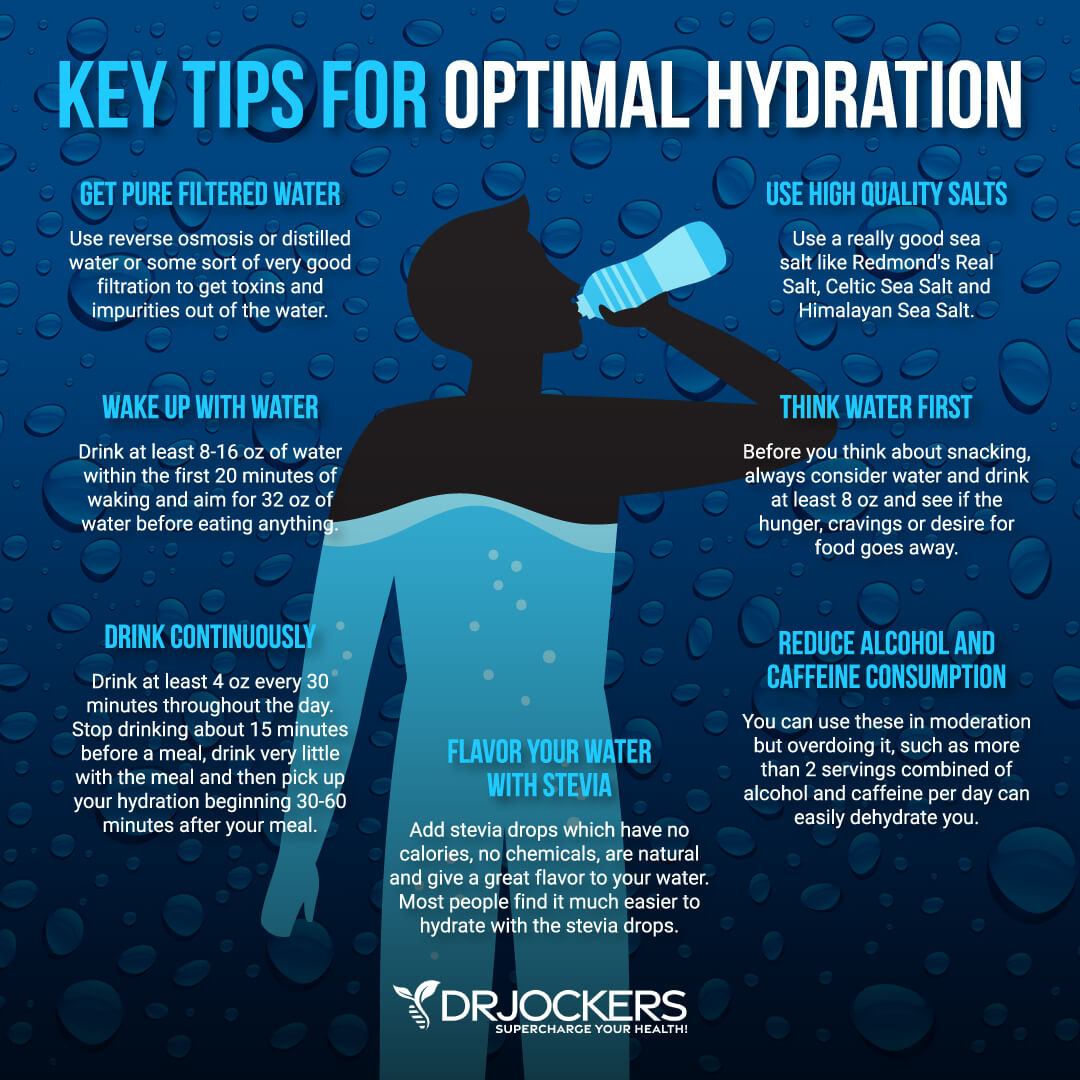
Use glass, stainless steel, wood, and bamboo products instead of plastic. Spend time in nature and breathe in the fresh air. Use a good indoor air filtration system. Make sure that you drink clean, toxin-free water by using a high-quality reverse osmosis system.
I recommend systems like Aquatrue or the Berkey system for low-cost filtration. The best water is the UltraLux Triple Action Hydrogen Water Machine which is what I use at home as it is powered by molecular hydrogen which reduces oxidative stress in the body and improves immune function. Add a slice of lime for some extra flavor.
Support Detoxification Pathways
It is not enough to put good things into your body, you have to make sure that the bad things come out as well. Drink plenty of water to support detoxification through sweating and urine. Support your detoxification pathways to protect your body from brain inflammation.
I recommend using infrared saunas to promote detoxification through sweating. Try rebounding and dry skin brushing to support your lymphatic pathways. Support two major detoxifying organs, your kidneys and liver with herbs like milk thistle, parsley, dandelion, and bioactive carbons which can penetrate and remove toxins from deep within the tissues and cells.
Final Thoughts
Hypothyroidism is a serious issue that affects millions of people around the world. The symptoms of hypothyroidism include fatigue, weight gain, constipation, hair loss, dry skin, brain fog, and depression.
To protect yourself from thyroid problems, follow the recommendations in this article. You may notice improvements in your brain health, weight loss, energy, and overall health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!






Hi,
Quick question on this article…
The statment saying eggs and heavy proteins are typically not tolerated well by those with thyroid disorders. What is meant by “heavy proteins?” and why are eggs not typically tolerated well (because of it being a more typical allergen, I’m thinking).
Thank you
Jodi,
These individuals very often have intestinal permeability and dysbiosis so the heavy proteins can be challenging on their digestive system. Eggs are also one that many people in this category have a sensitivity too. I get them doing just small amounts of proteins and loading up on anti-oxidant rich vegetables and herbs and good fats like coconut oil/butter, etc.
I’m almost 300 lbs and about to undergo gastric sleeve surgery. They want me on a high protein diet. I’ve had arguments with my doctors about my thyroid. I’ve wanted to take natural thyroid replacement from bovine sources, and they say levothyroxine is better. My mom had hypothyroidism too. What do you suggest I do?
Hey Sara,
It is hard for me to tell you what to do without a thorough health history…but I would start by following my anti-inflammatory nutrition plan as mentioned in this article. A natural thyroid hormone replacement like Armour is typically cleaner (levo and synthroid contain GMO corn in the coloring dies) so that would be a good idea. If you would want to consult so I could learn more about your case and customize an appropriate plan for you we could arrange that. Blessings!
It is your body, and you have every right to insist that the doctor changes your medication to something more suitable.
I had a doctor do the same with me back in the early 1990’s. Although I do not recommend this course of action for everyone, I stopped going to doctors since that time and am now a reasonably healthy 67 years old.
Great article. Thanks for all of the information. Is there anything that you know of that combat or reduce the negative side effects of ionizing radiation? Even if it is years later? Especially from ct scans? Thank you!
make a shield for your smart meter youtube it that will really help,Also get some radiation stickes for your wifi micro wave phone computer and other wireless devices
Thanks for sharing!!
Do you have any suggestions for treatment after a thyroid ablation? I’ve given up hope that things will change, but living with this is so miserable. Thanks.
Carmen LaCrue
Hey Carmen,
From my understanding you will typically need some thyroid hormone support for the rest of your life, but I would do all of the strategies discussed in this article to enhance your overall functionality!
Hi dr jockers. Can you reverse the autoimmunity? I have high levels of tpo antibodies (89), normal T3 T4, estrogen dominant, low vit D, low iron, low T. I know that my body is undergoing an autoimmunity with joint pain, eczema, hair loss, raynauds….. Would love to know I can reverse this vicious struck my body is on. Thank you in advance for a reply,
Hey Lori,
Yes, it is possible to lower antibodies. Following the strategies I discuss in this article would be the best start! If you want coaching for this, send me an email and we can set up a long-distance consultation. drjockers@drjockers.com
Hi Dr. Jockers!
This article has great information! I was diagnosed approx. 5 yrs ago with Hashimoto’s by an endocrinologist who specialized in thyroid disorders. He did test for antibodiesand said they were way too high, my TSH was normal. He then got transferred and the many other doctors and endocrinologists said that they won’t test for antibodies and put me on levothyroxine. It helped at first but then I became very sick and miserable. I just stopped taking it and feel better, but I really would like some helpin getting back to optimal health! I have taken small steps like using a Berkey water filter, eating fresh produce, making my own nut milks, baking with nut or rice flours to eliminate gluten, and chiropractic. I really need help from someone knowledgeable, it is very hard to do on my own.
Thank you,
Vicki
I am sorry to hear of your health struggles Vicki! So glad to hear you are on your way to getting better with all the great lifestyle activities you are now doing.
It would be wise to work with a functional medicine doctor to get to the underlying root cause. I do local and long-distance consultations and help coach people to get well if you would like to work with me. Blessings!
Love the info.. I have multiple non cancerous (as of now) thyroid nodules.. I never hear them talked about… What causes the nodules?hypo/hyper/hashi?… Can they be reversed/dissolved? I never hear anyone address them…
Hey Lisa,
Sorry to hear this! It is usually related to autoimmune activity and/or excess hydrogen peroxide burning the thyroid leading to abnormal/mutated cells – like a callus on your hand when you are rough with your hands. I would recommend following the principles in this article. Not sure if it can be fully reversed, but you must STOP THE CAUSE and help the body to heal itself.
Thank you so much… I am grateful for a response… I am doing most if not all of what you suggest with a DC over the past two years…so I believe almost there but still need to find that missing piece of the puzzle.. So still working on it..stopping the cause… Totally have changed my life habits .. So just need to find the next step.. I still have hair loss .. Not as bad …and am able to rejoin my life which has been great.. Also DC doing some genetic testing .. Getting that back soon along with a full panel thyroid blood work to see where I am now …. Taking many things in your thyroid pack ..maybe I need to look to see if yours includes something I am missing.. Thanks again for your reply..I truly consider it a blessing..truly grateful
You are welcome. Glad you are getting to the cause. Blessings!
I don’t know all your symptoms or health challenges, but if you have thyroid issues and if you are losing hair (alopecia areata?), you may want to consider getting tested for celiac disease. It is quite common for people to have celiac disease and thyroid disease. It’s important not to eliminate gluten from your diet before being tested as it would cause a false-negative test result.
Great point LuLu! Yes, it would be good to tested for a gluten sensitivity.
Is there anything suggestion on eliminating the hydrogen peroxide? I read that an over growth of it can cause gray hair and hair loss..so maybe that is what needs to be addresses.. Will mention it to my DC.. This is a new discovery for me…only heard it mentioned recently by Suzy Cohen…. Any suggestions on how to combat it ? In your program or anything nutritionally to eat?
Thanks
Selenium and glutathione are the key to reducing hydrogen peroxide build up.
Thank you.. Is there a supplement you have to support those two things? Also I was on your live webinar ..but I could not see a link to purchase your program for $97.. Can I be sent a link if you think I would still benefit from it?
Thank you again
Hey Lisa,
Thanks for writing. Here is the link to the AutoImmune Program and be sure to use the code AI50 to save $50 https://drjockers.com/autoimmune-elimination-program/
For supplements – my favorite for the thyroid is the ThyroLiver protect here: https://store.drjockers.com/products/thyroliver-protect
Thanks , this is the best , most informative page about hypothyroid ever written on internet
Thank you SO MUCH May! Our goal is to create information and resources to inspire and empower people to take back control of their health!
Hi Dr. Jockers:
Your article is really helpful. I was diagnosed with hypothyroid almost 7 years back using imaging of gland and started off with 50 mcg of thyroxine which gradually increased to 100 mcg. My mother and both the brothers also have the problem but they live a normal life. However, I feel chronic throat infection (almost every month), viral fever (mild fever running for long duration), my throat reacts to the cold weather, dust etc. I feel extreme fatigue most time. Since last two years, my condition has worsen. My T3 level is usually at the lower end (even after medication). I used to take protein suppliments which caused me lot of stomach troubles and eggs too. Now I have stopped all the heavy proteins. How can I live a normal life? I am 43 years old male (a scientist) and want to have an active life and career. Please help me.
I’m so sorry to hear about this Pankaj! You can get started with some of the strategies in this article but your case might benefit from some investigation and one on one time with a functional nutrition specialist. Email nutrition@drjockers.com and we can get something set up for you!
Can you give me the reference(s) for vehicle emissions impacting hypothyroidism or autoimmune disease in general?
“1) Industrial Pollutants: This includes the various pollutants we find in our air, food and water that negatively effect the immune system and thyroid function. These come from our vehicle emissions”
I am hypothyroid with adrenal fatigue, HPA axis and mito dysfunction…symptoms all the same. I am on a hi protein/hi fat diet to treat mito, but have concern about my diet because a sluggish thyroid accumulates LDL…and btw: I’m skinny and both my MD and ND told me that many skinny people are hypo.