 Endometrial Cancer: Symptoms, Causes, and Support Strategies
Endometrial Cancer: Symptoms, Causes, and Support Strategies
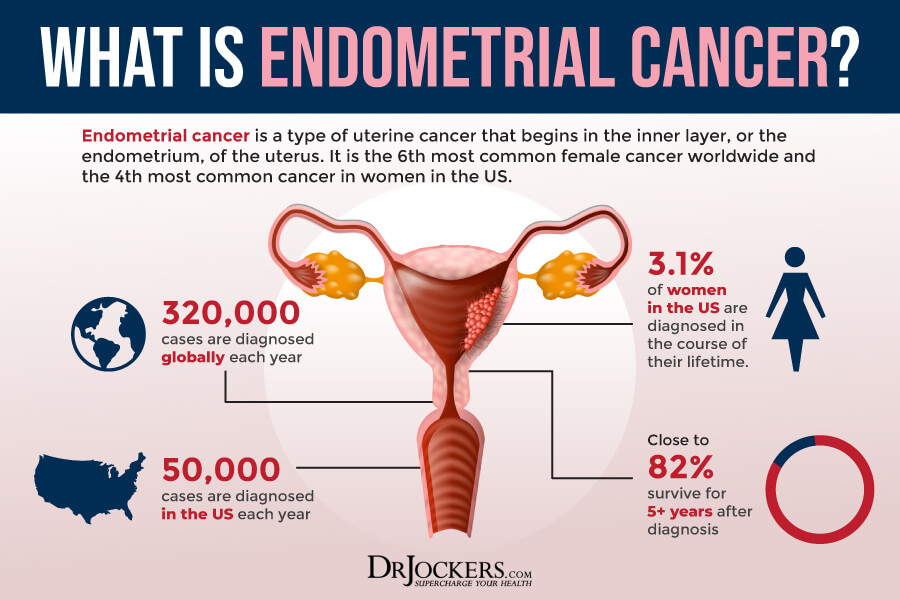
Endometrial cancer is a type of uterine cancer that will affect about 3 out of 100 women during their lifetime. Early detection is critical for treatment and successful recovery. Since many of the root causes of endometrial cancer are lifestyle-related, there are a number of natural support strategies that can reduce your risks and support your recovery from endometrial cancer.
In this article, you will learn what endometrial cancer is. You will understand the symptoms, stages, and risk factors of endometrial cancer. You will learn about diagnosis and conventional treatment options for endometrial cancer. I will explain the root causes of endometrial cancer. I will recommend some key functional labs to look at. Finally, I will offer some natural support strategies to support your health and well-being.
What Is Endometrial Cancer
Endometrial cancer is a form of uterine cancer. It starts in the endometrium, which is the inner lining of the uterus. It happens when cells in this area become cancerous and begin to grow out of control. According to the National Cancer Institute, 3.1 percent of women will be diagnosed with endometrial cancer during their lifetime (1). It accounts for about 3.5 percent of all cancer cases and 2.1 percent of all cancer-related deaths. Over 80 percent of them will survive for five years or longer after their initial diagnosis.
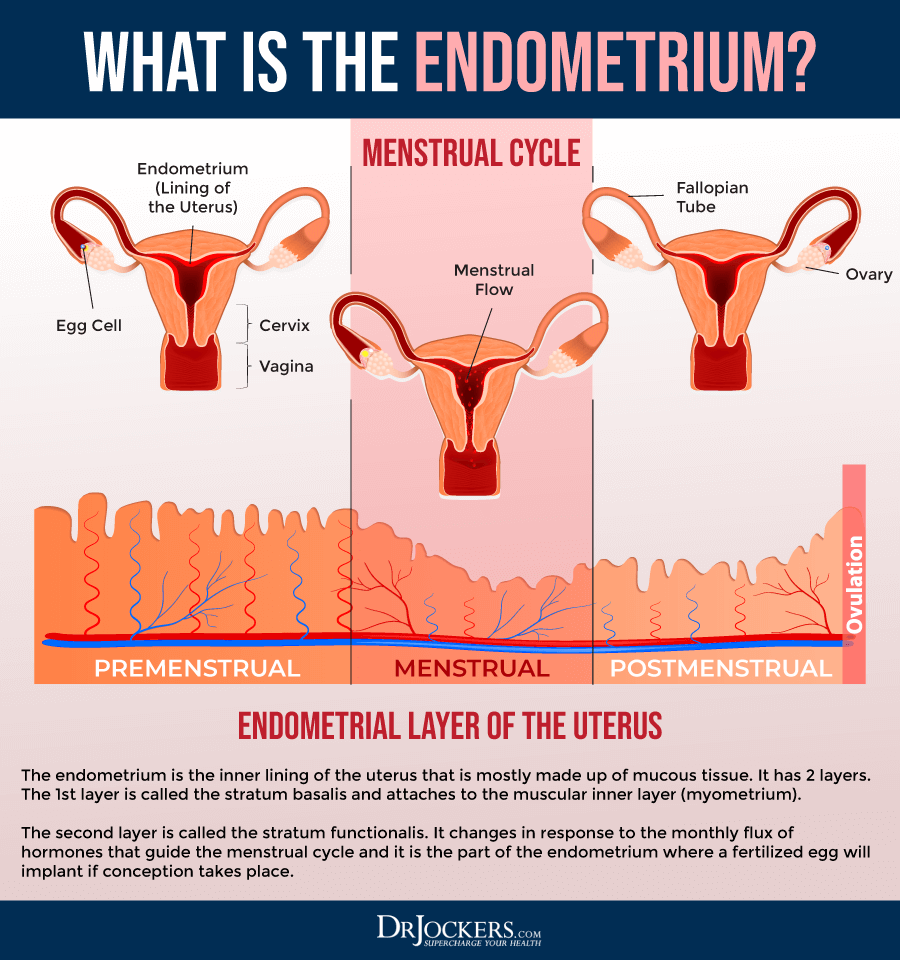
To understand endometrial cancer better, I want to talk about the uterus for a moment. It is a hollow organ resembling a medium-sized pear in both shape and size. It is the place for the baby to grow and develop during pregnancy (2).
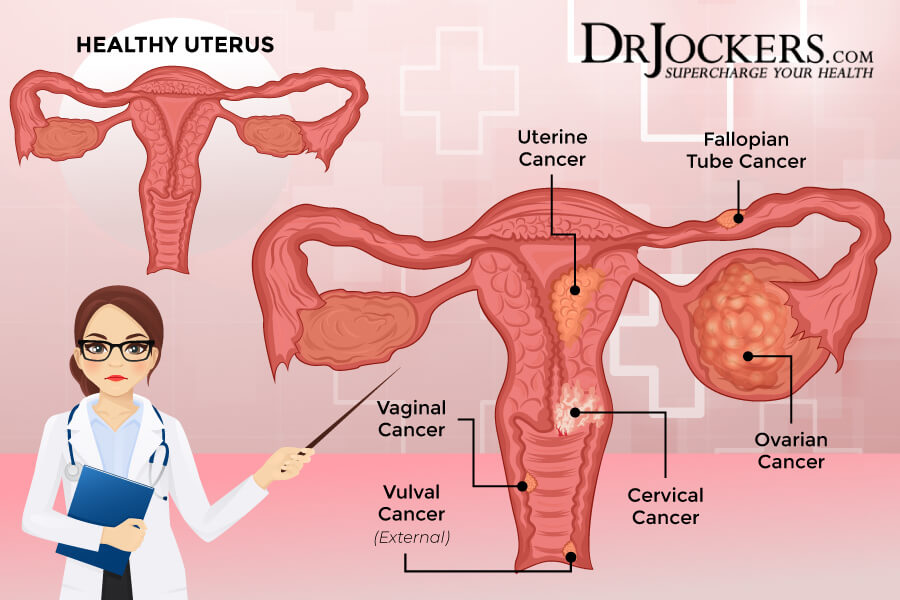
The uterus has two parts. The body (or corpus) is the upper part, and the cervix is the lower area that connects to the vagina. Uterine cancer is a type of cancer that starts in and affects the uterus, not the cervix. Cervical cancer is not the same as uterine or endometrial cancer, but a completely different type of cancer (2).
The upper area or corpus of the uterus has two main layers: the myometrium and the endometrium. The myometrium is the outer layer of the body of the uterus. It is a thick muscle layer that helps the mother push the baby out during labor (2).
Types of Endometrial Cancer
The endometrium is the inner layer, which changes throughout the menstrual cycle. Elevation of estrogen leads to thickening of the endometrium to prepare the body to nourish the baby if pregnancy occurs. If pregnancy doesn’t happen, progesterone will step in to cause the endometrial lining to shed during one’s period. These changes of the endometrium will occur each month until menopause happens (2).
Beyond these two main layers, there is another layer called serosa. The serosa is a layer of tissue that covers and protects the outside of the uterus. Out of these three layers, endometrial cancer affects the endometrium (2).
There are several types of endometrial cancer depending on how the cells look under the microscope, including (2):
- Adenocarcinoma
- Uterine carcinosarcoma (CS)
- Squamous cell carcinoma
- Small cell carcinoma
- Transitional carcinoma
- Serous carcinoma
All endometrial cancer starts in the endometrium. Some have squamous or flat, thin cells, while others also have glandular cells. The most common form of endometrial cancer is adenocarcinoma. There are several subtypes of endometrial cancers, including (2):
- Adenocarcinoma with squamous differentiation
- Adenoacanthoma
- Adenosquamous (or mixed cells)
- Ciliated carcinoma
- Secretary carcinoma
- Villoglandular adenocarcinoma
We can also classify two main types of endometrial cancer based on the rate of their growth. Type 1 endometrial cancer grows slowly and doesn’t spread quickly to other tissues. Type 2 endometrial cancer is more aggressive, grows fast, and spreads quickly. Type 1, slow-growing, endometrial cancer is much more common.
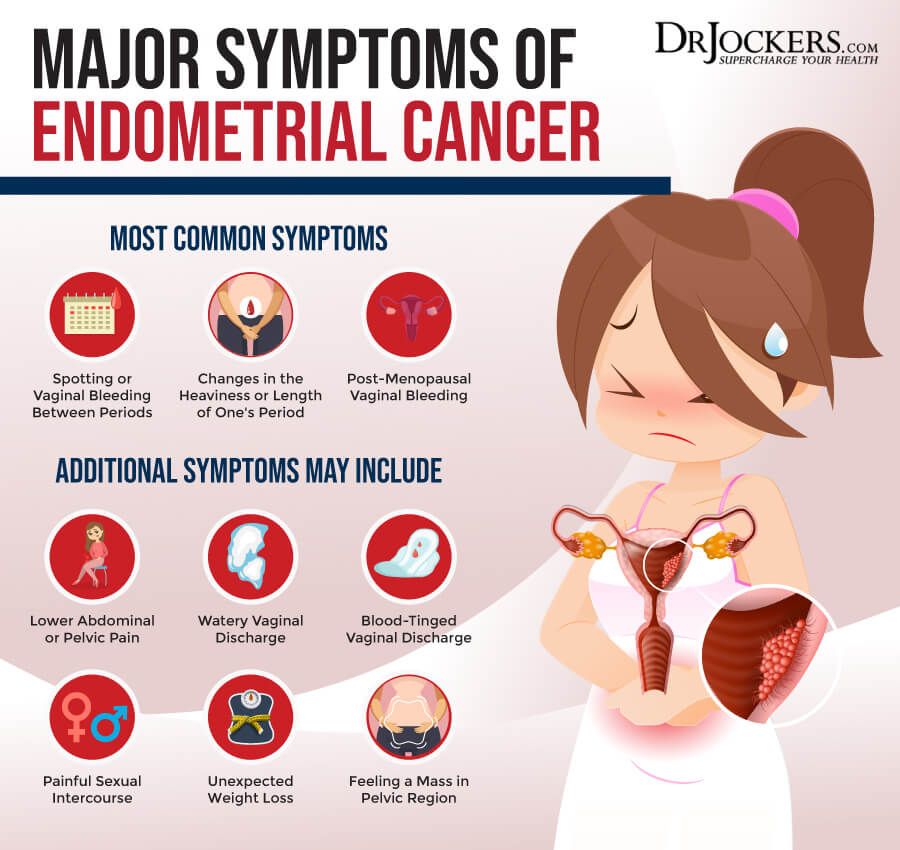
Symptoms of Endometrial Cancer
Endometrial cancer may have several symptoms. The most common one is abnormal vaginal bleeding, including (3):
- Spotting or vaginal bleeding between periods
- Changes in the heaviness or length of one’s period
- Post-menopausal vaginal bleeding
Other symptoms of endometrial cancer may include (3):
- Lower-abdominal or pelvic pain
- Watery vaginal discharge
- Blood-tingled vaginal discharge
- Painful sexual intercourse
- Feeling a mass
- Unexpected weight loss
Experiencing symptoms may not mean having endometrial cancer. They may be a sign of a less serious and non-cancerous conditions, including menopause, hormonal fluctuations, and even stress. They may also be a sign of another form of cancer. If you are experiencing these symptoms, it is critical that you visit your healthcare provider for appropriate diagnosis and treatment.
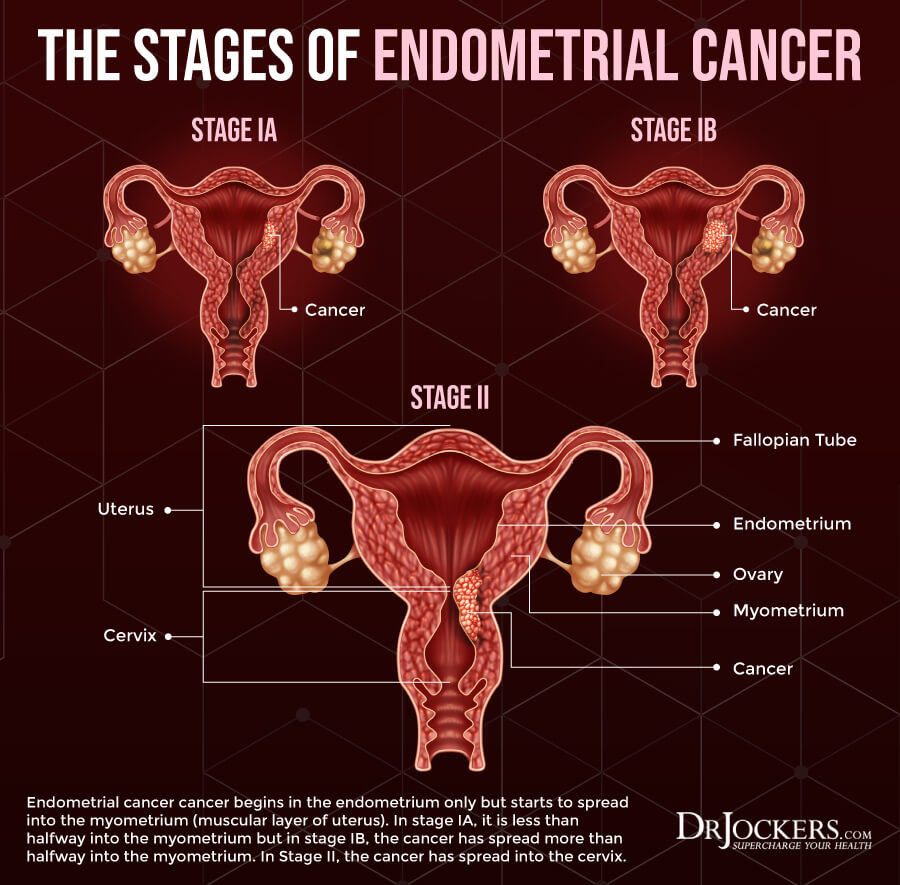
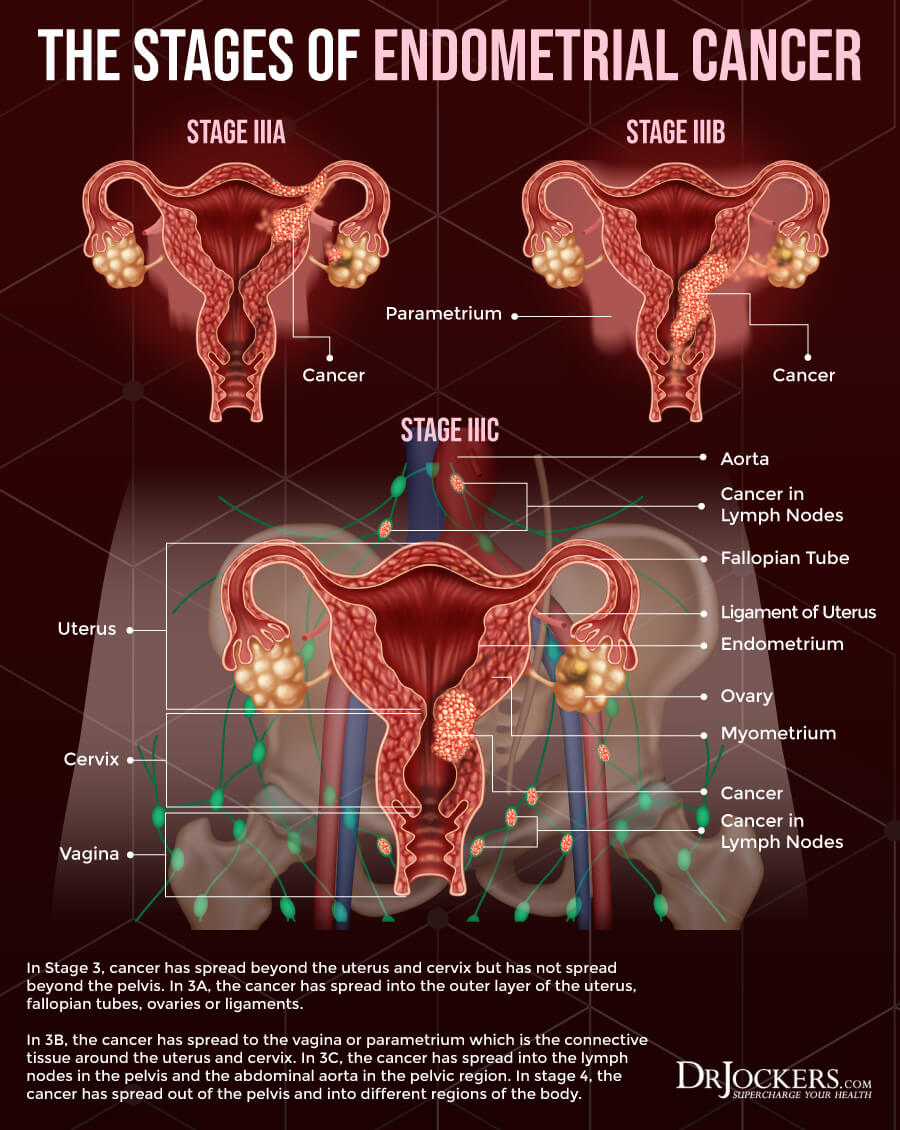
Stages of Endometrial Cancer
There are four stages of endometrial cancer depending on the size and how far its spread (2):
- Stage 1: At this stage, endometrial cancer is only found in the uterus and hasn’t spread elsewhere yet. Endometrial cancer at this stage is the easiest to treat and has the best outlook.
- Stage 2: At this stage, there is cancer in both the uterus and the cervix.
- Stage 3: At this stage, the cancer may have spread to the ovaries, fallopian tubes, vagina, or nearby lymph nodes, but not to the bladder or the rectum.
- Stage 4: At this stage, the cancer has spread beyond the pelvic area and may be found in the bladder, rectum, and even distant organs or tissues.
Since treatment is much easier and the outlook is much better at the early stages, early diagnosis is critical. If you have symptoms of endometrial cancer, don’t wait, visit your doctor. Here is a helpful article that goes into great detail on the stages of endometrial cancer.
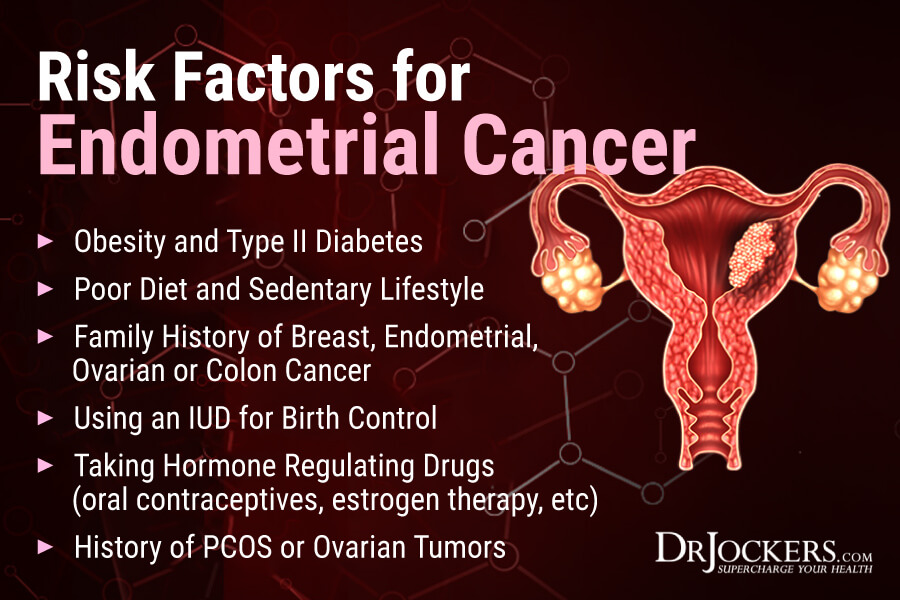
Risk Factors for Endometrial Cancer
There are various risk factors that may increase your chances of developing endometrial cancer (4):
- Obesity
- Age (the risk increases as you get older)
- Using an intrauterine device (IUD) for birth control
- Anything that affects hormonal levels, including taking oral contraceptives, taking tamoxifen to prevent breast cancer, estrogen therapy, taking estrogen after menopause, having ovarian tumors or polycystic ovarian syndrome (PCOS), pregnancy, and the number of menstrual cycles over a lifetime
- Family history of endometrial or colorectal cancer
- Having a personal history of ovarian or breast cancer
- Having a personal history of hyperplasia
- Past radiation therapy of the pelvis for another cancer
- Having type 2 diabetes
- Poor diet (high-calorie diets, diets high in unhealthy fats)
- Sedentary lifestyle
Diagnosis of Endometrial Cancer
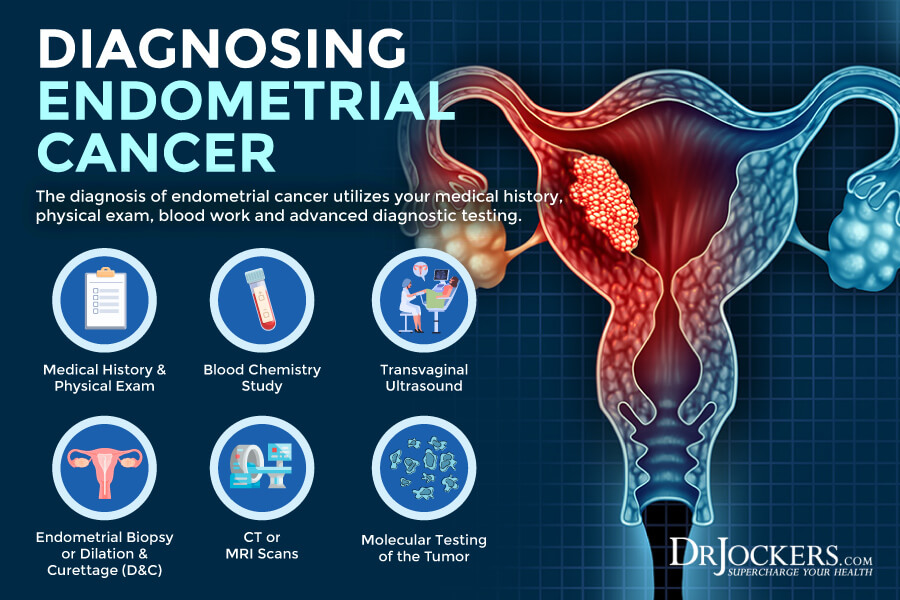
After going over your medical history and symptoms and performing a physical exam, your doctor may order an ultrasound to look at your pelvis, fallopian tubes, ovaries, and uterus. Using a pelvic ultrasound is usually not enough. A transvaginal ultrasound (TVUS) is able to look at your uterus better and detect signs of endometrial cancer (5).
If you are showing signs of endometrial cancer, tissue sampling is next. Your healthcare provider may order an endometrial biopsy, a hysteroscopy, or a dilation and curettage (D&C) procedure to test the endometrial tissue for abnormalities and cancer. They may also test for tissue and protein changes, especially if your doctor suspects hereditary non-polyposis colon cancer (HNPCC). If they notice DNA changes, they may also order some genetic testing (5).
If you have endometrial cancer, your doctor may order a chest x-ray, computer tomography (CT) scans, magnetic resonance imaging (MRI) scans, positron emission tomography (PET) scans, cystoscopy, and proctoscopy to check for spreading of the cancer and staging (5).
Your doctor may also order a complete blood count (CBC), CA-125 blood test. High CA-125 levels often mean that the cancer has spread outside the uterus. While this test is not always used, it can be helpful before surgery or other treatment (5).
Conventional Treatment Options
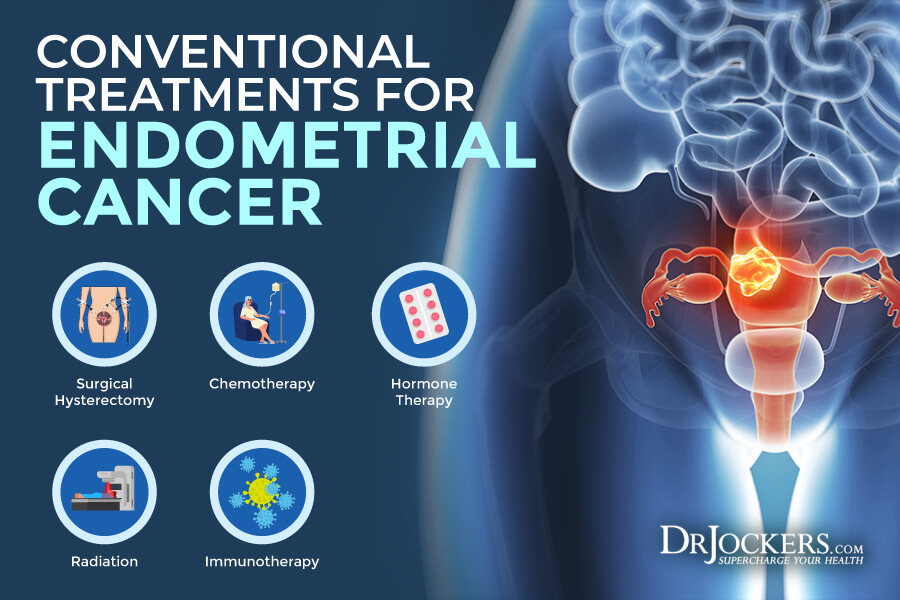
Endometrial cancer is usually treated with hysterectomy, which is a type of surgery that removes the uterus. In some cases, they use a bilateral salpingo-oophorectomy (BSO) to remove the ovaries and fallopian tubes during the same surgery. If the cancer has spread, they may remove the nearby lymph nodes as well through a lymphadenectomy or lymph node dissection procedure. If the cancer has spread even further, other surgeries may be recommended as well (6).
Radiation therapy is often used for endometrial cancer. It uses high-energy beams to kill cancer cells. They may use an external beam or internal radiation therapy or both. Radiation therapy may be used after surgery or if you can’t have surgery, instead of surgery (6).
Chemotherapy drugs are also often recommended to kill endometrial cancer cells. You may receive intravenous (IV) chemotherapy or chemo in pill form. Chemotherapy is often used if the cancer has spread to other parts of the body in later stages, or the cancer has returned after prior treatment (6).
Hormone therapy may be used to block certain hormones and slow cancer growth. It is often used in later stages in combination with chemotherapy. In other cases, targeted therapy using drugs that target certain changes in the cancer cells may be recommended. While in other cases, immunotherapy using immune checkpoint or PD-1 inhibitors may also be used (6).
In addition to surgery and these therapies, your doctor may recommend working with a mental health specialist and/or joining a support group for those living with cancer to learn to manage the emotional and mental effects of endometrial cancer and connect with others dealing with the same (6).
Root Causes of Endometrial Cancer
We have already talked about the main risk factors of endometrial cancers. Let’s talk about some of the underlying factors that can increase your risk and cause endometrial cancer. Understanding these root causes is important to determine your risk factors and support your treatment if you develop endometrial cancer.
The root causes of endometrial cancer may include chronic inflammation, insulin resistance, poor estrogen metabolism, vitamin D deficiency, zinc deficiency, high copper levels, and heavy toxic load.
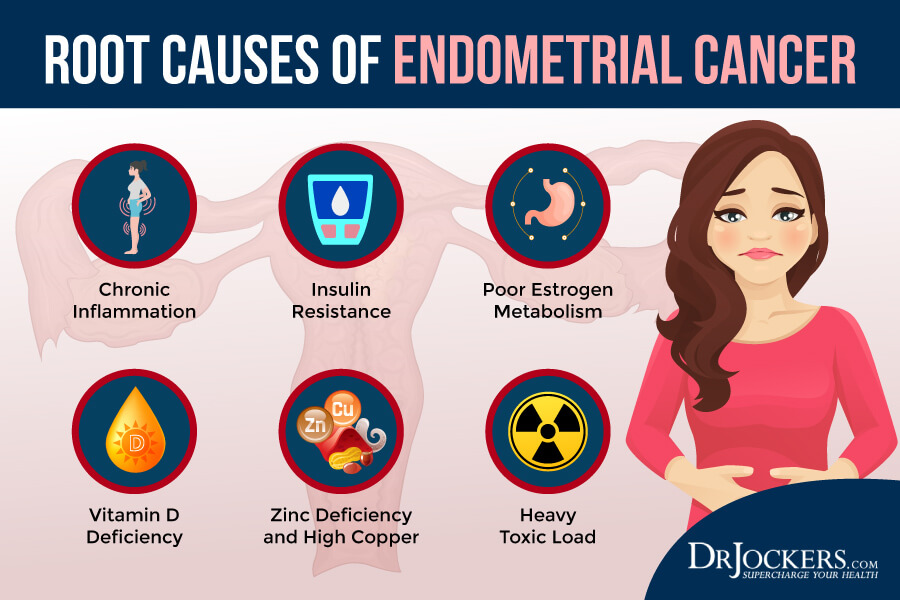
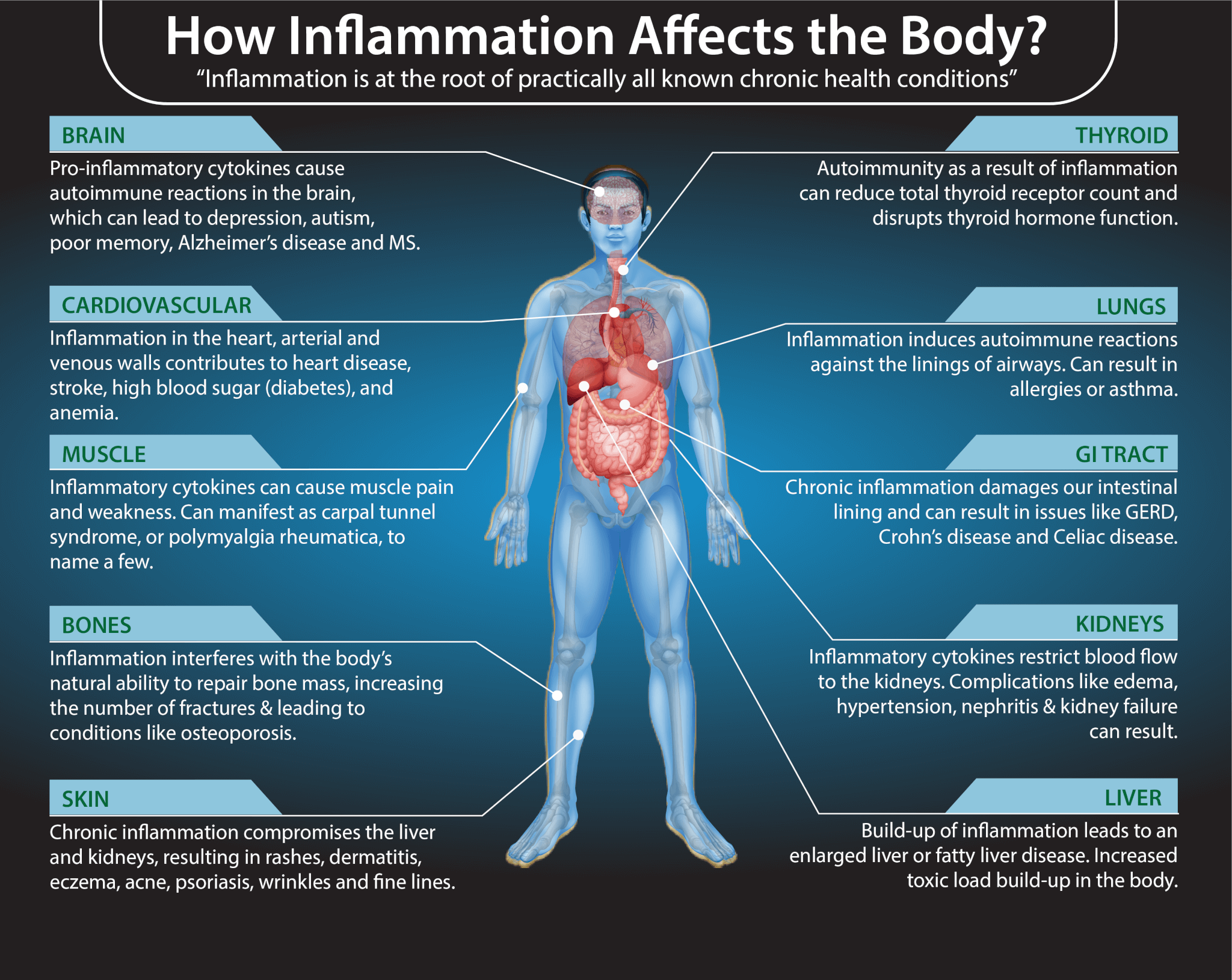
Chronic Inflammation
Chronic inflammation is the number one underlying cause of most chronic diseases and cancers. It is not surprising that it is also one of the main root causes of endometrial cancer. A 2005 review published in Cancer Epidemiology, Biomarkers, and Prevention found a connection between chronic inflammation and endometrial cancer (7).
Chronic inflammation can result in rapid cell division that may lead to replication errors, DNA damage, and mutations, which can result in cancer. They also found that in vitro non-steroidal anti-inflammatory drugs may reduce the growth of endometrial cancer.
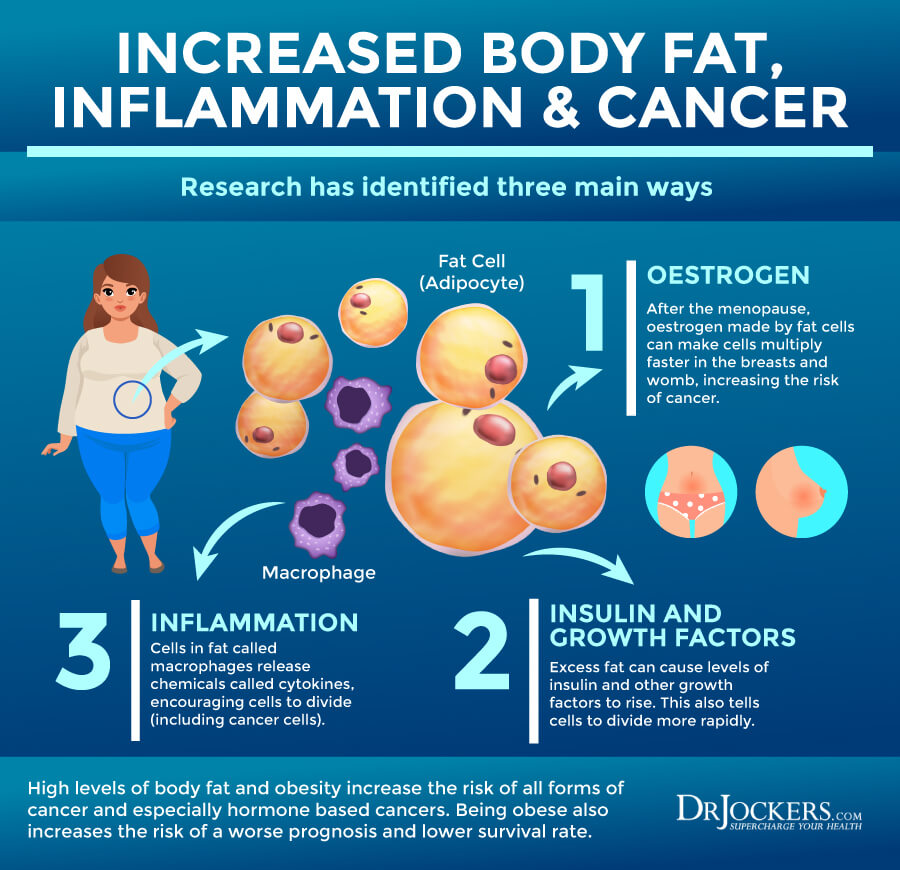
A 2010 prospective case study published in Endocrine-Related Cancer has also found a connection between chronic inflammation and endometrial cancer (8). They found that obesity and poor inflammatory markers may indicate an increased risk of endometrial cancer.
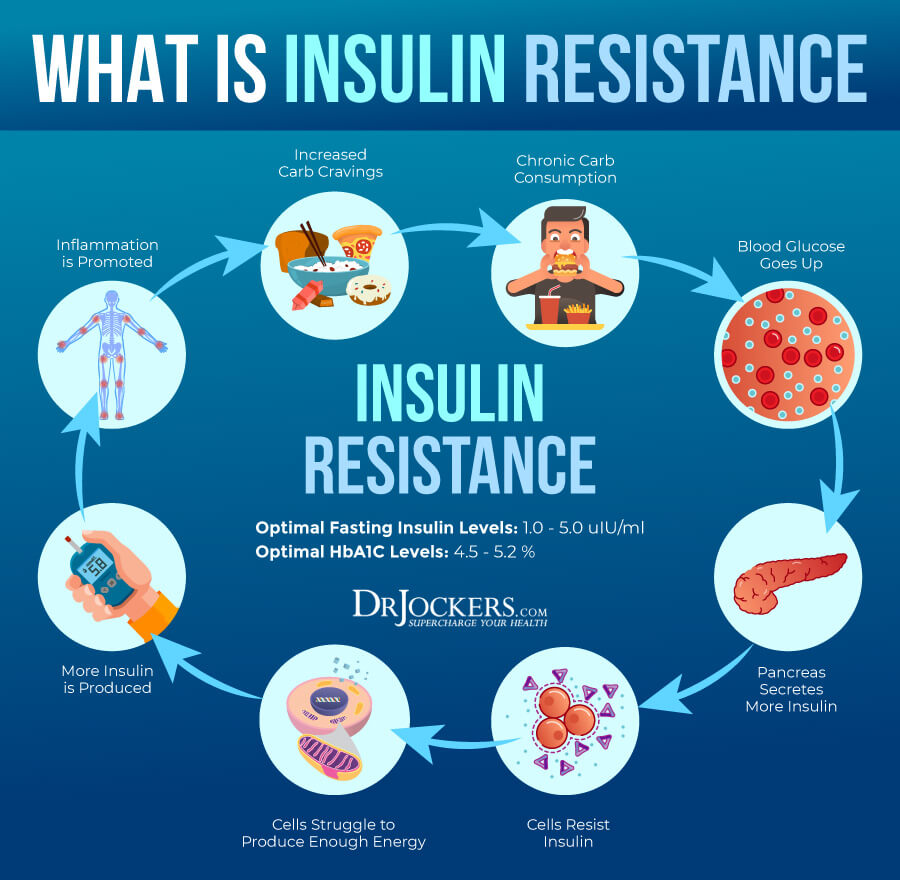
Insulin Resistance
Insulin resistance means that your body is unable to respond to insulin well. Insulin resistance can lead to prediabetes and diabetes. It is also one of the underlying root causes of a number of chronic health issues and cancer, including endometrial cancer.
A 2012 review published in Gynecologic Oncology found that high insulin levels and insulin resistance can increase inflammation and significantly increase the risk for endometrial cancer (9). A 2015 systematic review and meta-analysis has also found a link between insulin resistance and the increased risk of endometrial cancer (10).
A 2020 study published in Cancer (Basel) has also found that insulin resistance can modulate epigenetic dysregulation including miRNAs expression in endometrial cancer patients and insulin resistance can increase the risk of endometrial cancer (11).
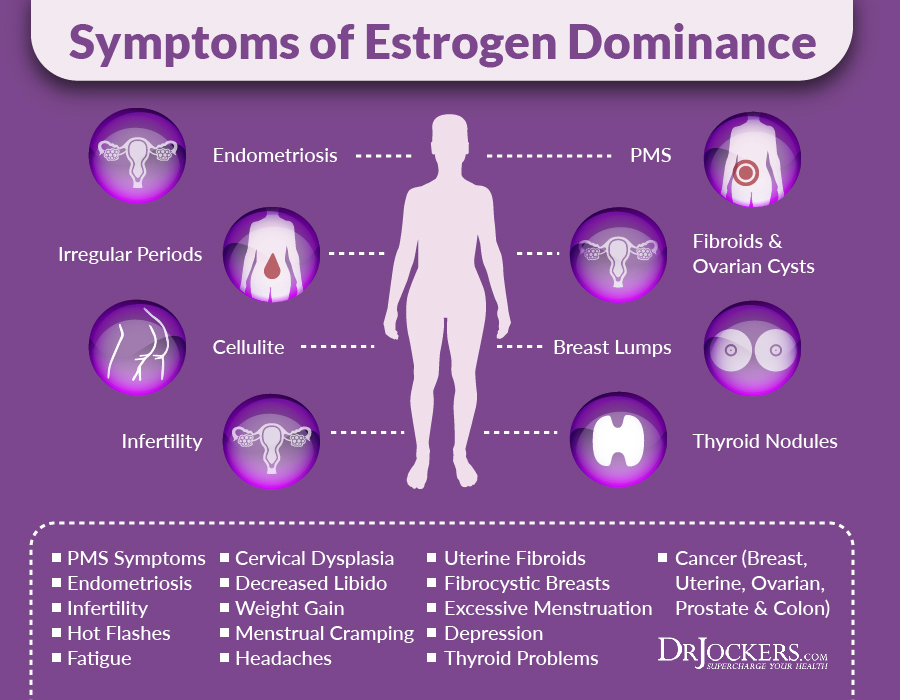
Poor Estrogen Metabolism
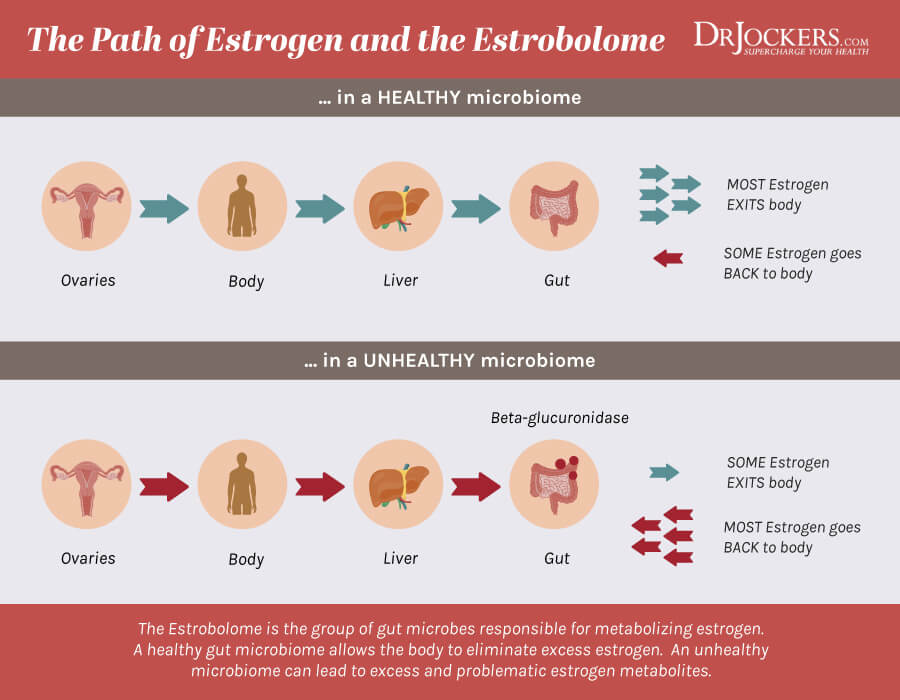
Poor estrogen metabolism can also increase the risk of endometrial cancer. The estrobolome are certain gut bacteria that are responsible for metabolizing estrogen. Beta-glucuronidase is an enzyme produced by the estrobolome that breaks the bond between glucuronic acid and toxins in your gut When your gut flora is imbalanced, beta-glucuronidase activity is also altered.
According to a 2017 review published in Maturitas, beta-glucuronidase helps your gut to regulate estrogen secretion (12). Decreased beta-glucuronidase activity can affect estrogen levels. Coupled with lower estrogen levels can increase the risk of obesity, polycystic ovarian syndrome (PCOS), osteoporosis, and cardiovascular disease.
Increased beta-glucuronidase production, on the other hand, can increase circulating estrogens, cause estrogen dominance, and increase the risk of endometriosis, endometrial cancer, and other cancers related to estrogen dominance.
A 2020 study published in Biomedicine and Pharmacotherapy found a link between microbiome health, beta-glucuronidase, and women’s cancers, including endometrial cancer, other uterine cancers, ovarian cancer, and breast cancer (13). Having a healthy and balanced gut flora, on the other hand, can support proper beta-glucuronidase activity and reduce the risk of endometrial cancer and other issues.
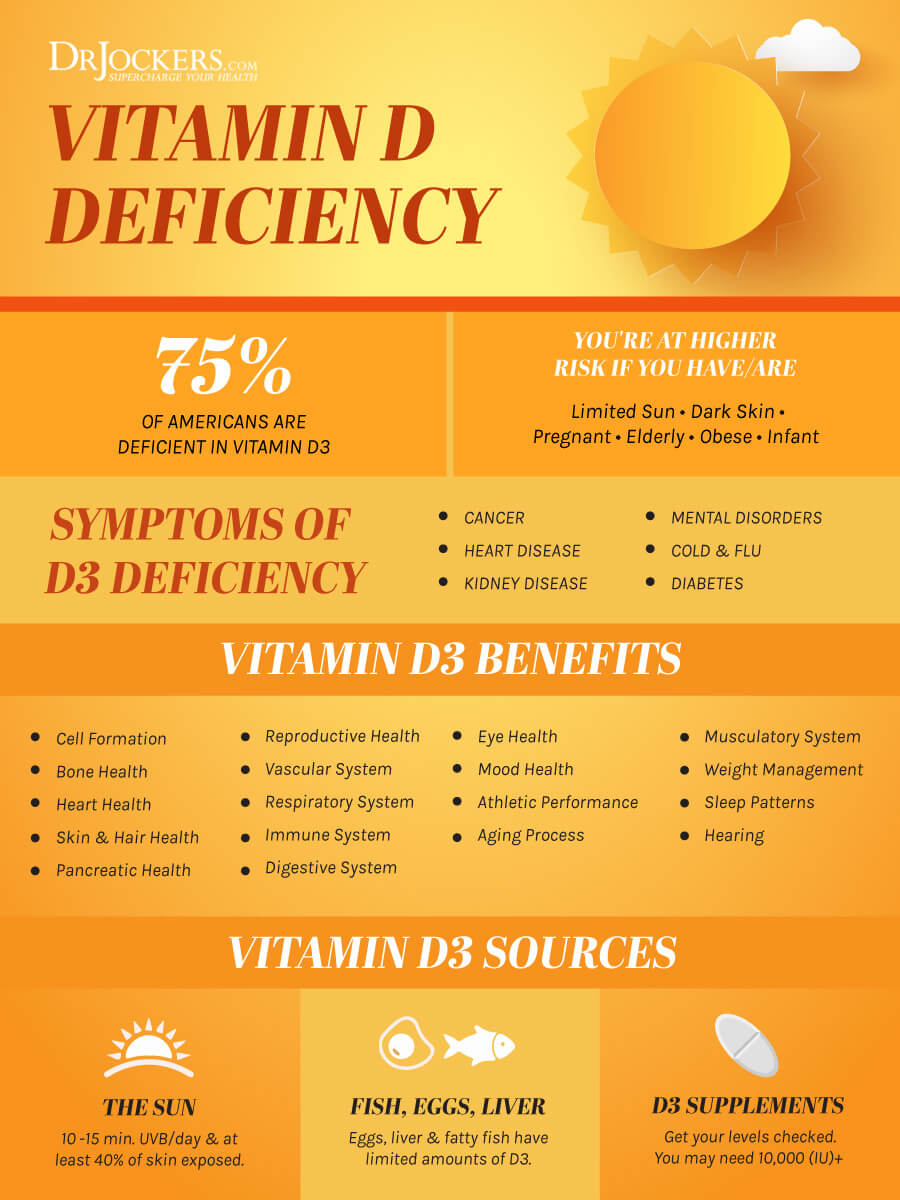
Vitamin D Deficiency
Vitamin D is a very important vitamin for muscle, bone, brain, immune, hormonal, and mental health. It turns out that vitamin D deficiency may play a role in endometrial health. A 2010 study found that vitamin D can help to decrease the risk of obesity-induced endometrial cancer (14). A 2018 review and meta-analysis of 8 studies published in Medicine (Baltimore) found a link between reduced vitamin D levels and female reproductive tumors, including endometrial cancer (15).
A 2018 systematic review published in the International Journal of Molecular Sciences has pointed out that vitamin D is a neglected area of women’s and endometrial health (16). They found that vitamin D deficiency can increase the inflammatory response of endometrial cells. They also found that low vitamin D levels can increase the risk of issues of the ovary, endometrium, and myometrium; hence may increase the risk of ovarian cancer.
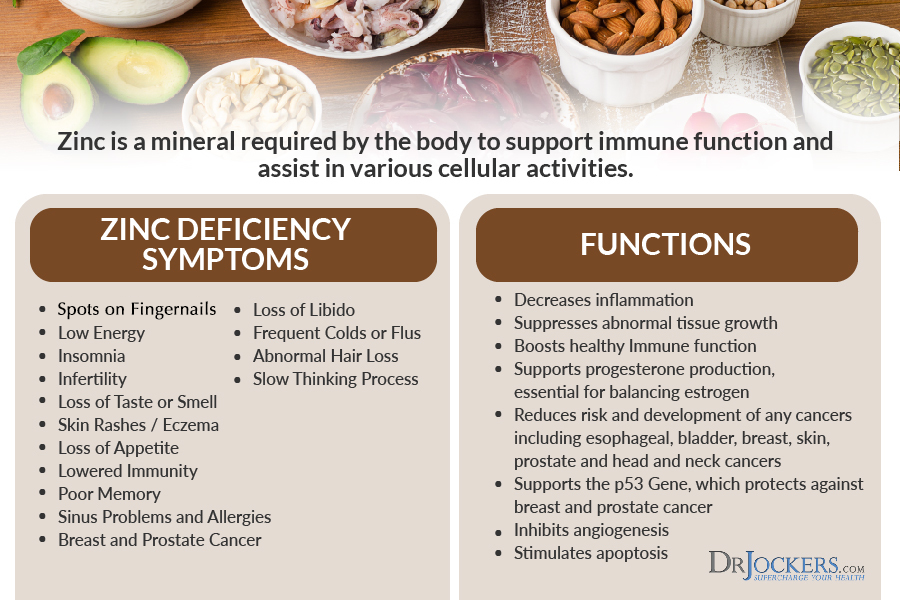
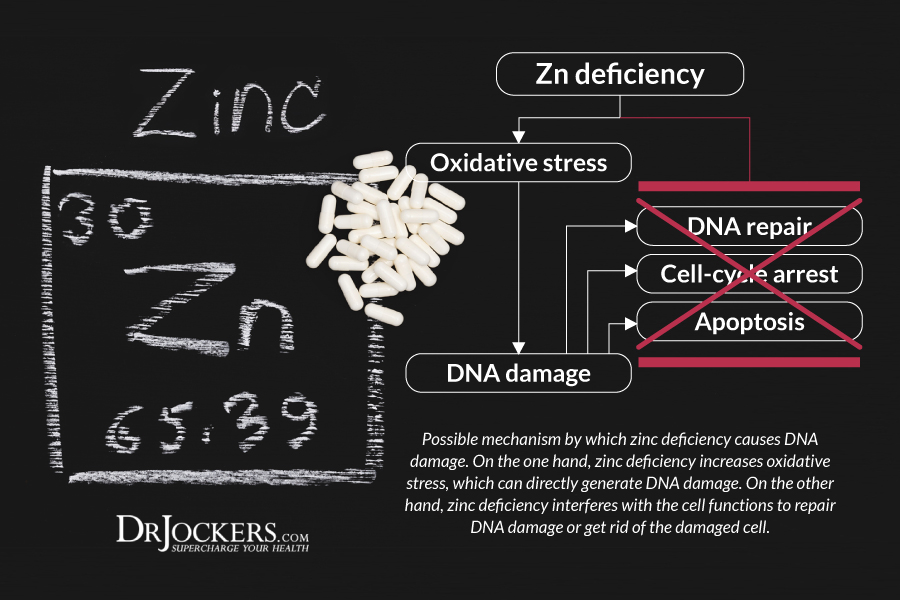
Zinc Deficiency and High Copper
Zinc is a critical mineral for immune health. Inefficient zinc levels can increase inflammation, immune-health issues, and the risk of disease. Copper is another essential mineral for immune, nerve, blood vessel, and bone health. However, too high copper levels combined with low zinc levels, creating a poor zinc: copper ratio can increase the risk of all kinds of health issues, including the risk of endometrial cancer and other female cancers.
A 2018 review published in Bioscience Reports found a link between high copper levels and the risk of cervical cancer (17). A 2018 review published in the International Journal of Medical Research, on the other hand, found that increasing zinc levels may decrease the risk of cervical cancer (18).
A 2019 study published in the Journal of Obstetrics and Gynecology found that a poor zinc:copper ratio can increase the risk of endometrial polyps (19). A 2020 study published in Nutrients found that low zinc levels, high copper levels, and a poor zinc:copper ratio can increase the risk of gynecological issues, including female cancers (20). A 2020 study published in Biological Trace Elements Research found that a poor zinc:copper ratio is common in endometrial cancer patients (21).
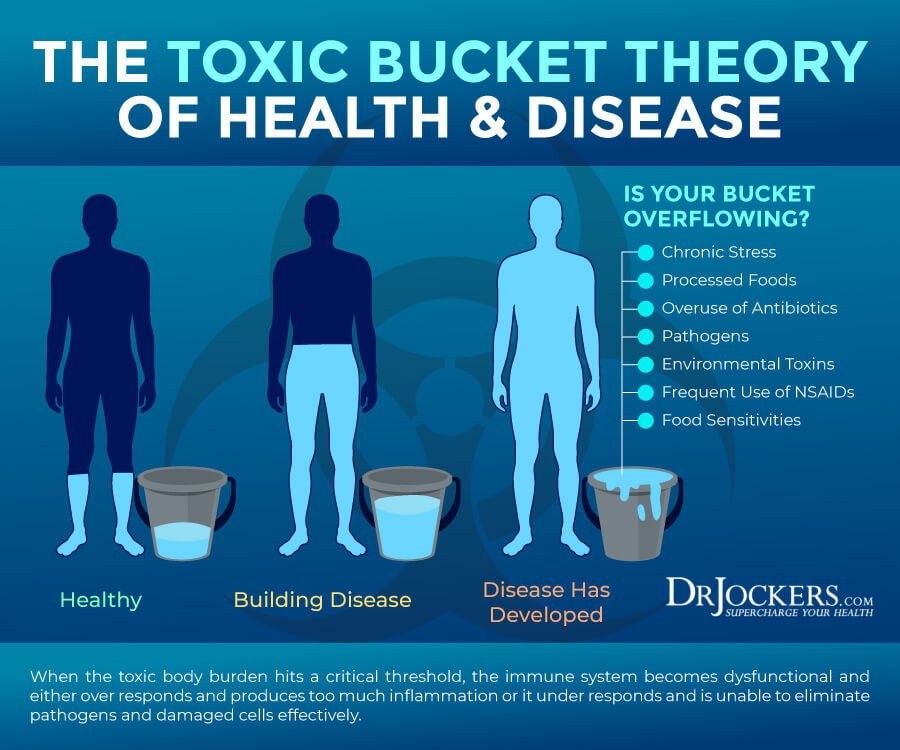
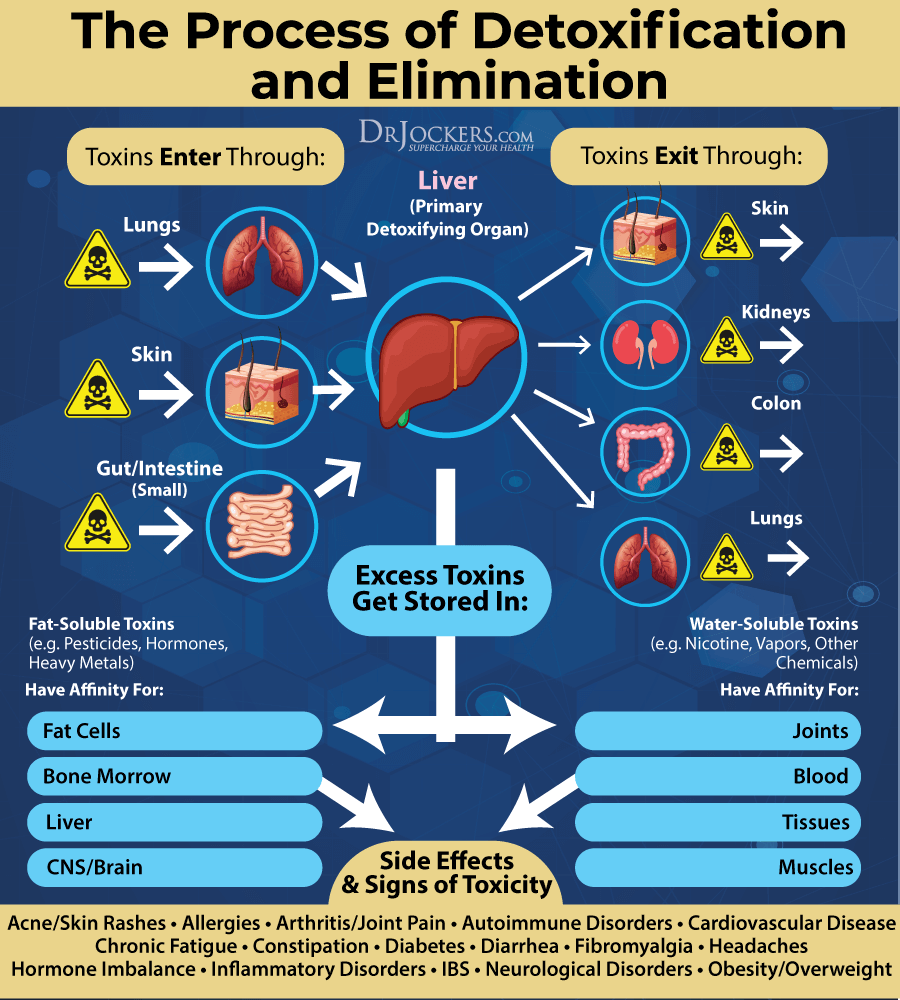
Heavy Toxic Load
Unfortunately, our modern world is full of chemicals, heavy metals, and toxins that can be carcinogenic and increase your risk of inflammation, cancer, and various chronic diseases. Certain heavy metals and chemicals are particularly problematic, and exposure to them can increase the risk of endometrial cancer and other female cancers.
A 2019 study published in the Journal of Obstetrics and Gynecology found that high heavy metal levels, including aluminum, lead, and nickel can increase the risk of endometrial polyps (19). A 2018 review published in Expert Review of Anticancer Therapy found that cadmium may increase the risk of endometrial cancer (22).
A 2017 review published in the International Journal of Environmental Research and Public Health found that endocrine disruptor compounds can have carcinogenic effects and can negatively affect women’s health (23). A 2021 case study published in Environmental Health Perspectives found that BPA, parabens, and phthalates can increase the risk of endometrial cancer (24).
Key Functional Labs
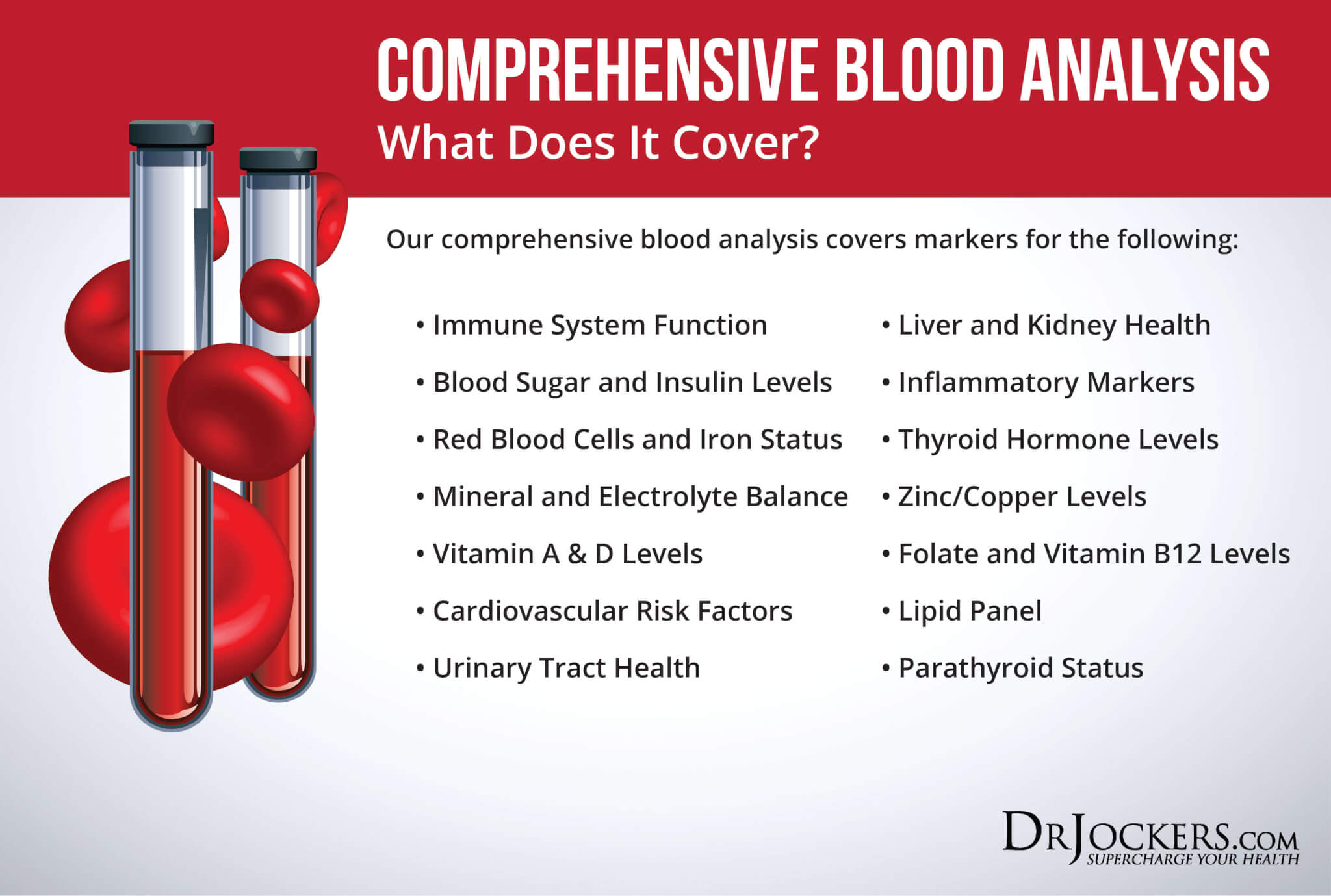
There are a number of key functional labs I use and recommend to determine your risk factors and uncover the root causes of endometrial cancer. Here is what I recommend.
Inflammation: Hs-CRP, ESR, LDH & Serum Ferritin
There are a number of tests I recommend to check for underlying inflammation, including Hs-CRP, ESR, LDH, and serum ferritin testing.
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L. When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
ESR refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Optimal ESR rates are between 0 and 10 mm/hr.
LDH is an enzyme found in all living cells. Elevated levels may indicate inflammation. Optimal levels are between 140-180. Levels over 180 indicate inflammation and levels under 140 indicate reactive hypoglycemia.
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer. The clinical range is 30 to 400, and the optimal range is 25 to 150 for females and 50 to 150 for males. You can get these labs done on our Comprehensive Blood Analysis here.
Insulin Resistance: Fasting Insulin, HbA1C, Lipid Profile
I recommend a number of tests to check for insulin resistance, including fasting insulin levels, HbA1C, and a lipid profile.
Blood sugar imbalances may increase your risk of inflammation. In addition to testing your HbA1C levels, I recommend checking your fasting insulin levels. Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml and the optimal range is 1.0 – 6.0 uIU/ml.
Blood sugar imbalances are one of the main causes of inflammation, so I recommend checking your hemoglobin A1C (HbA1C) levels. Your HbA1C levels measure your average blood sugar over the past 2 to 3 months. Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6 while the optimal range is 4.5 – 5.2.
Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. We are looking for low HDL or high triglycerides as a sign of insulin resistance. Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal.
Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal. We are also looking at a triglyceride: HDL ratio of 2:1 or less, 1:1 being optimal. Higher rates may indicate insulin resistance and inflammation. Optimal levels:
- HDL cholesterol: The idea range is 55 to 90. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The ideal range is 40 to 80.
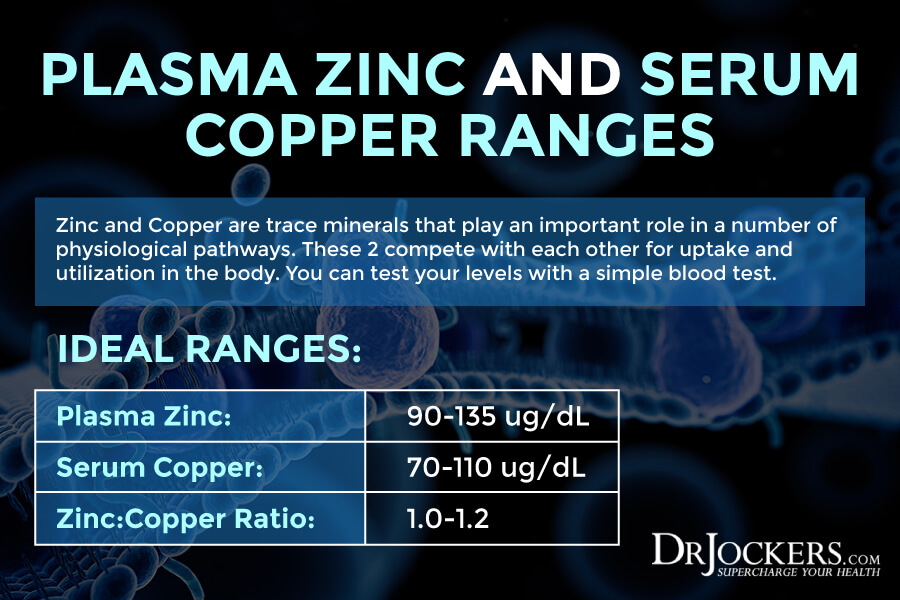
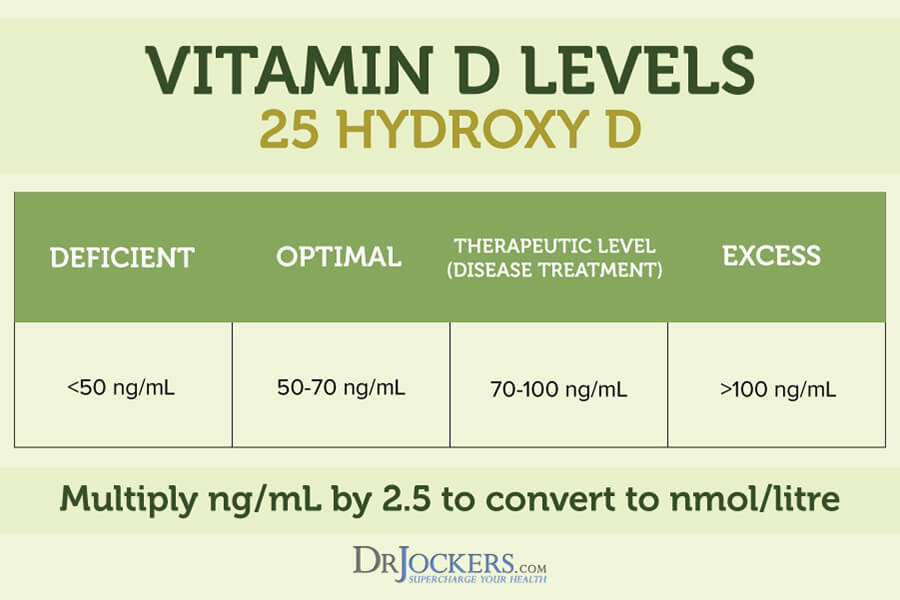
Vitamin D, Plasma Zinc: Serum Copper Ratio
Since vitamin D and zinc deficiencies and high copper levels may increase the risk of endometrial cancer, I recommend checking your vitamin D and zinc: serum copper ratio.
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. Normal levels of vitamin D are between 50-100 ng/mL
Checking your plasma zinc levels is the best way to determine zinc levels in your body. Ideal plasma zinc levels are between 90–135 ug/dL and for serum copper it should be 70–110 ug/dL. Zinc and copper compete against each other as antagonists to regulate physiological pathways. A proper balance between the two is essential for maintaining good health. I recommend checking your plasma zinc and serum copper levels and their balance. The proper zinc:copper ratio should be between 1–1.2.
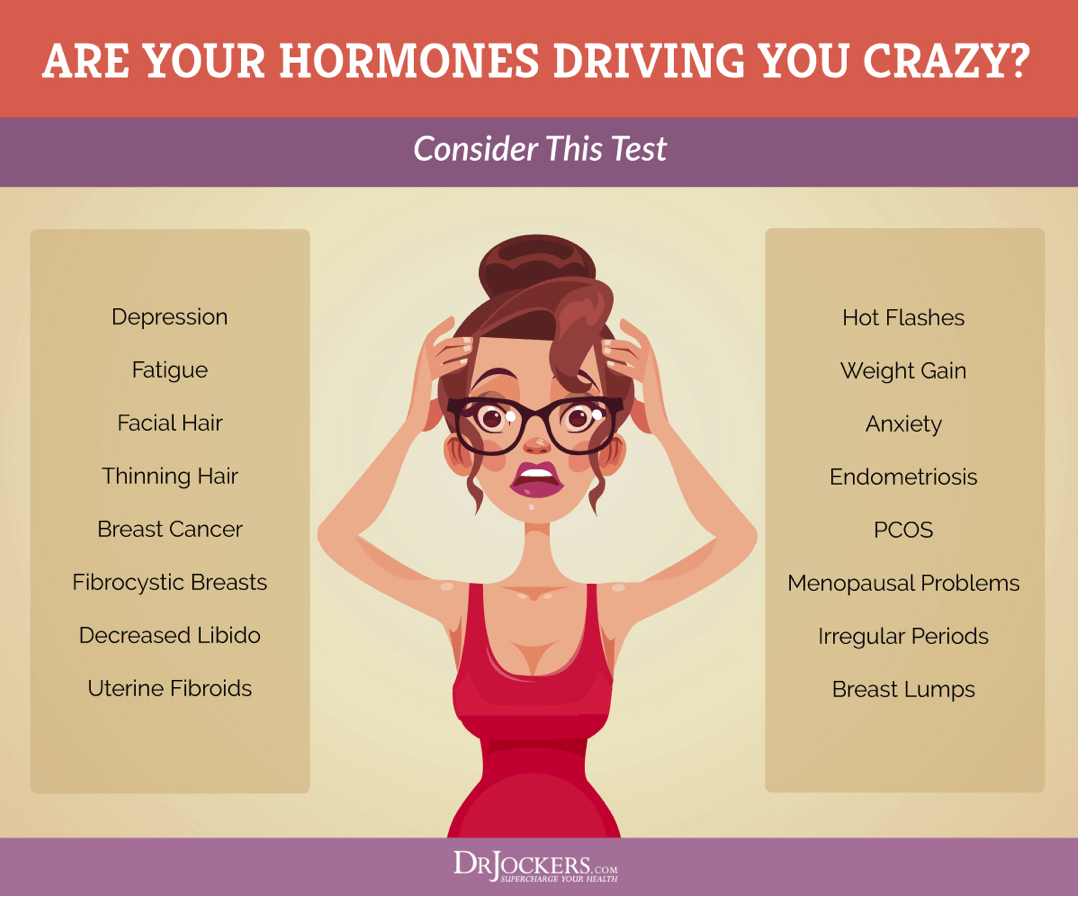
DUTCH Test to look at Estrogen Metabolites
I also recommend the DUTCH Test™ — Dried Urine Test Comprehensive Hormones to check for estrogen metabolites. This test offers a complete hormonal panel. Beyond estrogen metabolites and estrogen levels, it looks at progesterone, testosterone, cortisol, DHEA, and melatonin levels.
The DUTCH Complete Hormone Panel is well-recognized for its ease-of-collection, coupled with comprehensive reporting that is not available from other laboratories. This test will give you the information you need to understand what is happening with your adrenals, melatonin levels and sex hormones including estrogen metabolites.
GI MAP
I also recommend a GI Map Stool Test to further understand your digestive health and help appropriate lifestyle changes for improved digestive health. This is the best and most comprehensive gut test I have found. It helps to determine whether you have underlying gut dysbiosis. It helps to identify bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora.
I specifically recommend looking for Beta Glucuronidase. This test also looks at potential autoimmune triggers and all intestinal health markers. This test takes the guesswork out of your treatment and allows us to identify the gut-related root causes of your health issues.
Natural Support Strategies
There are a number of natural support strategies you can try to reduce your risks and improve your health. Here is what I recommend:
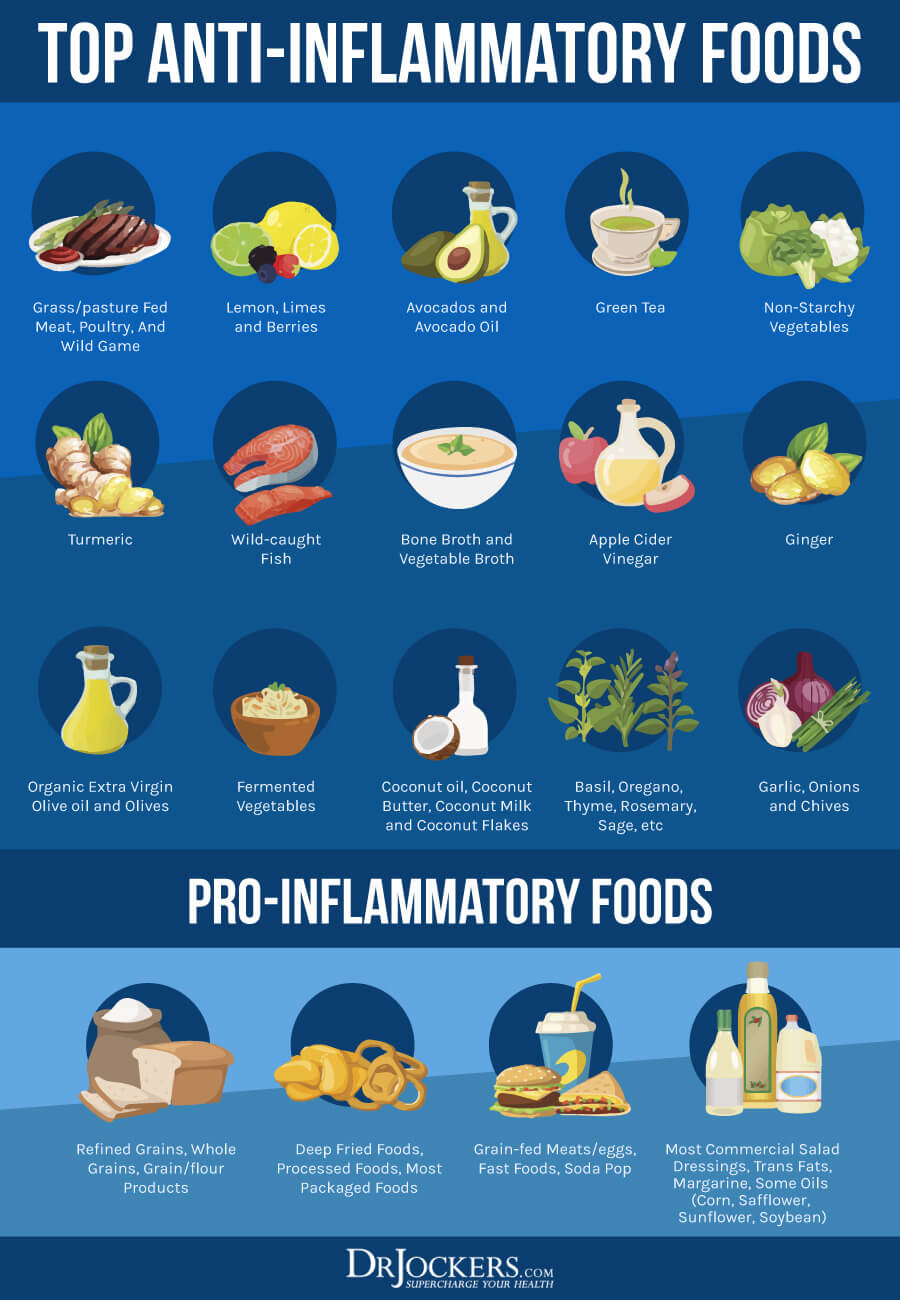
Anti-Inflammatory Nutrition Plan
A 2005 review published in Cancer Epidemiology, Biomarkers, and Prevention found that chronic inflammation may increase endometrial cancer (7). A 2016 study published in the British Journal of Nutrition found that eating an inflammatory diet is linked to an increased risk of endometrial cancer, while an anti-inflammatory diet can lower the risk. Following an anti-inflammatory nutrition plan may help to decrease your risk or support your health during treatment and recovery.
I recommend that you remove inflammatory foods from your diet, including refined sugar and carbs, refined oil, artificial ingredients, additives, deep-fried food, highly processed foods, and junk food. Remove inflammatory drinks, such as sodas, sugary drinks, and energy drinks, and limit or remove alcohol. Follow an anti-inflammatory diet rich in greens, vegetables, herbs, spices, fermented food, low glycemic index fruits, pasture-raised beef, grass-fed poultry and eggs, wild-caught fish and seafood, and wild game.
Eating plenty of healthy fats, including avocados, olives, coconut oil, extra virgin olive oil, pasture-raised organic butter, ghee, lard, nuts and seeds, and wild-caught fish is particularly important.
Get Into Ketosis
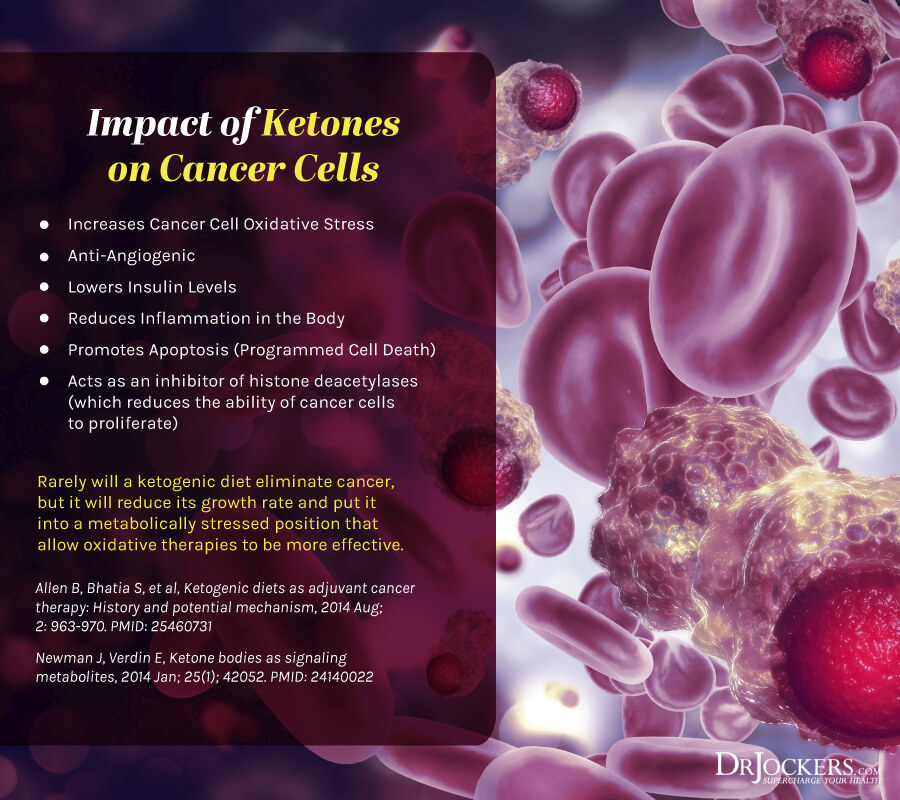
Normally, your body relies on dietary sugar for energy. However, if you are following a high-fat, low-sugar diet like the ketogenic diet or limiting your calories and sugar through fasting, your body will turn to fat for energy, starts producing ketones, becomes fat-adapted, and gets into ketosis. Getting into nutritional ketosis has multiple health benefits, including decreased inflammation, better cellular renewal, and a lower risk of cancer.
According to a 2017 study published in Nutrition and Metabolism (London), ketosis metabolically stresses cancer cells (26). Researchers explained that glucose and glutamine are the main fuels for tumor and cancer growth. They recommend the “Press-Pulse” approach for the metabolic management of cancer. Press disturbances create chronic stress while pulse disturbances trigger acute stress.
They found that press disturbance paired with acute metabolic stressors that limit glucose and glutamine can increase ketosis and decrease metabolic flexibility and genetic cell mutations. They found that using a press-pulse therapeutic strategy with ketosis as the metabolic press and the pulse being oxidative therapies may be effective for cancer management.
One of the best ways to achieve ketosis is following a low-carb, high-fat, whole foods ketogenic diet. A 2018 study published in the Journal of Nutrition found that the ketogenic diet can decrease insulin and obesity in endometrial and ovarian cancer (27). A 2018 randomized, controlled trial published in Nutrients has also found that following a ketogenic diet can increase energy and physical function in those with endometrial and ovarian cancer (28).
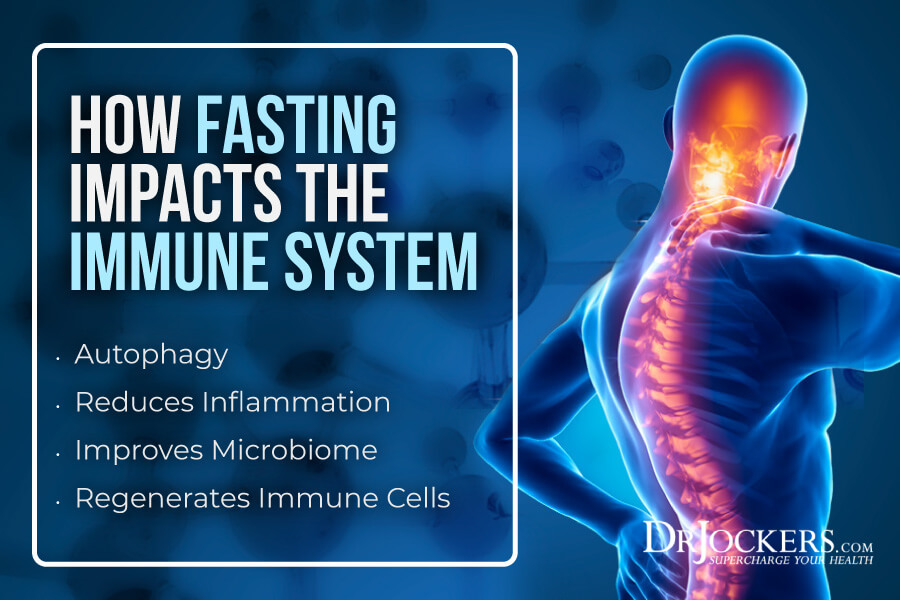
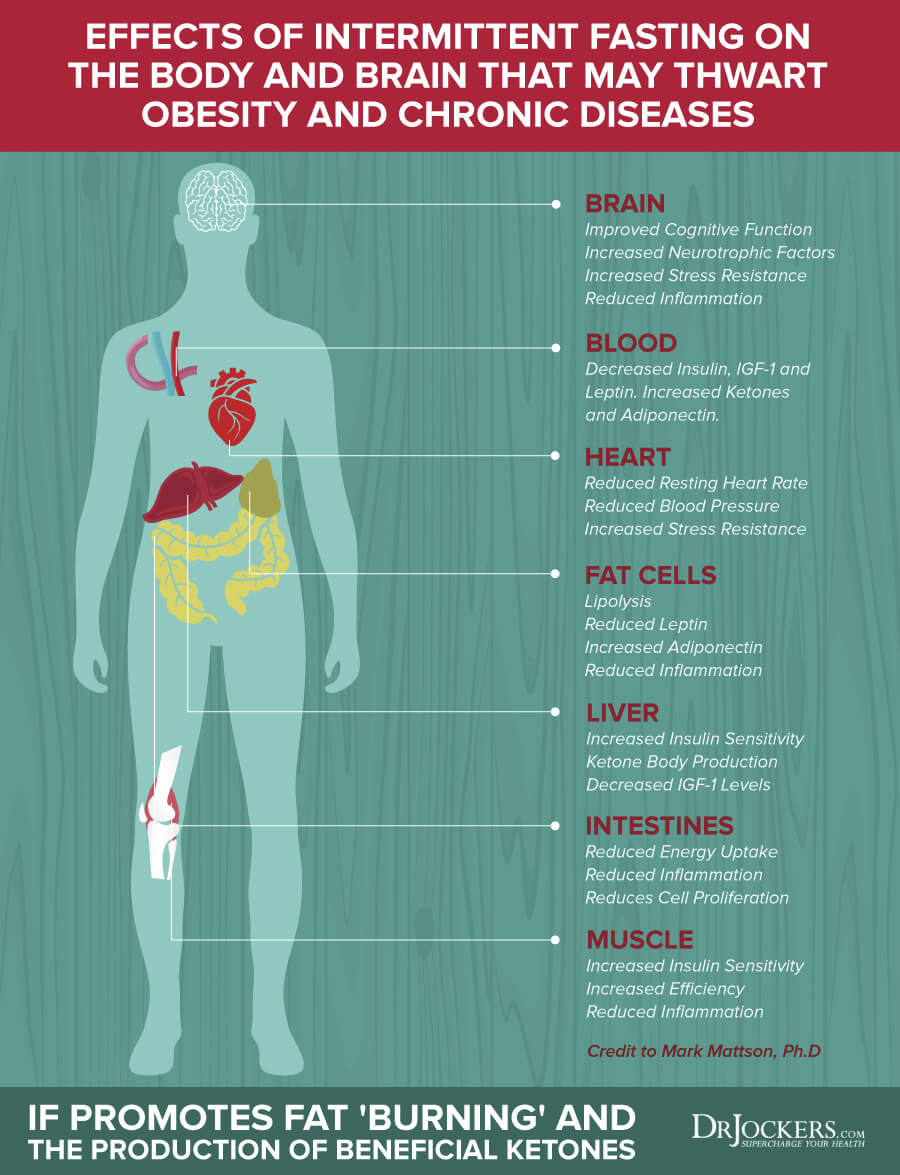
Intermittent Fasting
A 2016 review published in Recent Results in Cancer Prevention found that fasting and caloric restriction may help to reduce the risk of cancer and may support treatment (28). They found that periodic fasting (PF), fasting-mimicking diets (FMDs®), and dietary restriction (DR) without a reduction in calories can offer cellular protection and reduce chemotherapy resistance. A 2018 study published in Nature Reviews Cancer has also found that fasting and FMDs can promote the rejuvenation of healthy cells and may support cancer treatment (29).
Intermittent fasting is a form of fasting that rotates between periods of fasting (not eating) and periods of feasting (eating) within one day. If you are new to intermittent fasting, I recommend that you start by practicing Simple Fasting. A Simple Fast is only 12 hours of fasting, including your overnight sleep.
During your eating window, load up on a nutrient-dense, anti-inflammatory, and ketogenic diet. Increase your fasting window slowly and gradually over the next few weeks until you find what works for your body. Most people do the best with a 16-hour fasting window using the 16:8 method, but you may find that a shorter or longer window may work better for your body.
Partial Fasting
Partial fasting is a step between intermittent fasting and extended fasting if you are ready to challenge yourself but not quite ready to go completely without food. Partial fasts usually involve a strategy that focuses on liquids or caloric reduction. Green Juice Fasting, Bone Broth Fasting, FMD®, Fat or Keto Fasting are the most common partial fasts that you may benefit from.
Green Juice and Bone Broth Fasting have been very popular forms of liquid fasts and cleansing methods in recent years. You may buy cold-press green juice and bone broth at most health food stores and grocery stores or order a Green Juice or Bone Broth Cleansing kit online to avoid preparation and make it simple for yourself. Green Juice Fasting focuses on green juices, while Bone Broth Fasting recommends drinking bone broth for a few days.
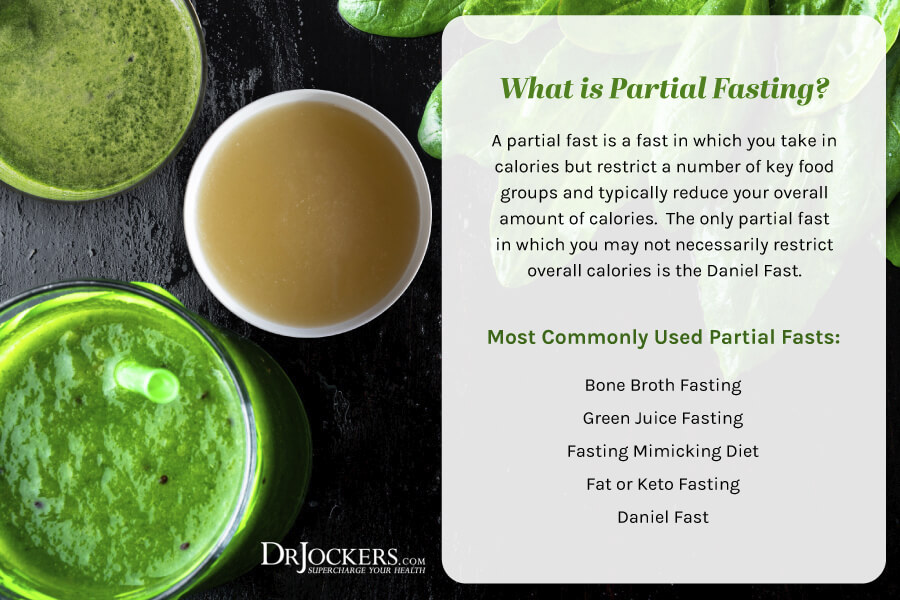
The Fasting Mimicking Diet® or FMD® is a partial fasting plan that is high in nutrients, low in protein, and low in carbohydrates. On Day 1, restrict your calories to 1,100 calories a day. 500 of these calories should come from complex carbohydrates and 500 from healthy fast. About 100 calories or 25 grams of plant-based proteins are also allowed, mainly from nuts. On Days 2–5, your calories are restricted to 800 calories only, with 400 calories from complex carbs and 400 calories from healthy fats.
The Fat or Keto Fast combines Partial Fasting with the principles of the ketogenic diet. It recommends that you eat 500–1000 calories a day, with 90 percent of those calories coming from healthy fats. This fasting strategy is a great way to achieve ketosis while fasting.
If you are ready and doing well on longer intermittent fasting or partial fasting strategies, you may try an extended fast. During an extended fast or water fast, you are only drinking non-caloric drinks, including purified water and may herbal tea for a day or several days.
This strategy is only for those who are experienced in other fasting methods and doing well on them. It may not be right for you if you are malnourished or very underweight due to your illness. I recommend that you talk to your healthcare provider if you are about to embark on an extended fast, especially if you are dealing with endometrial cancer or other serious health issues. You may learn about all these fasting methods by searching my website.
Regular Movement & Exercise
Movement and exercise are very important for overall health. It can be an important aspect of cancer prevention, treatment, recovery, and the post-recovery period. According to a 2005 population study published in Cancer Epidemiology, Biomarkers, and Prevention, exercising during adolescence and adulthood may decrease the risk of endometrial cancer by 40 percent compared to those who didn’t exercise (30).
The study found that performing household tasks, walking as transportation, and other lifestyle activities also matter. Non-exercisers leading an active lifestyle also experienced a 40–45 percent reduction in endometrial cancer risk. Those who exercised regularly but didn’t lead an active lifestyle otherwise experienced a 35 percent reduction suggesting that moving your body throughout the day and leading an active lifestyle is just as important as exercise.
Movement and exercise are not only important for health and prevention. It is also critical during and after recovery. According to a 2019 study published in Health Quality and Life Outcomes, endometrial cancer patients and survivors are more likely to experience physical limitations, and physical activity intervention may benefit their physical and mental health and well-being (31). A 2014 study published in Gynecologic Oncology found that exercise can benefit the fitness, mental health, quality of life, and overall health of survivors of endometrial cancer (32).

Leading an active lifestyle, moving your body, and staying active throughout the day are critical. Begin your day with stretching, yoga, rebounding, or a short walk. Get up and stretch regularly throughout the day. Move your body, walk around the office, take the stairs instead of the elevator, turn on your favorite song and try some dance moves, try a treadmill desk, or find other creative ways to move throughout the day regularly. Take a walk or try a workout during your lunch hour or mid-day before you eat. Walk or bike instead of driving for closer distances or park away from the store to add some steps to your day.
Exercise at least three days a week for at least 20–30 minutes a day. The most effective form of exercise is resistance training, and it is good to combine regular movement such as walking on a daily basis.
If you are currently undergoing treatment for endometrial cancer, you may feel tired and unable to complete harder or even easy workouts. That is completely okay. Listen to your body and do what you are able to and what supports your body. If that’s a short walk, a short light yoga session, or even stretching in your bed, that’s great. You will slowly regain your strength and health and will be able to do more. Working with a physical therapist, occupational therapist, or yoga therapist that is experienced working with cancer patients may help to regain your strength and improve at your own pace.
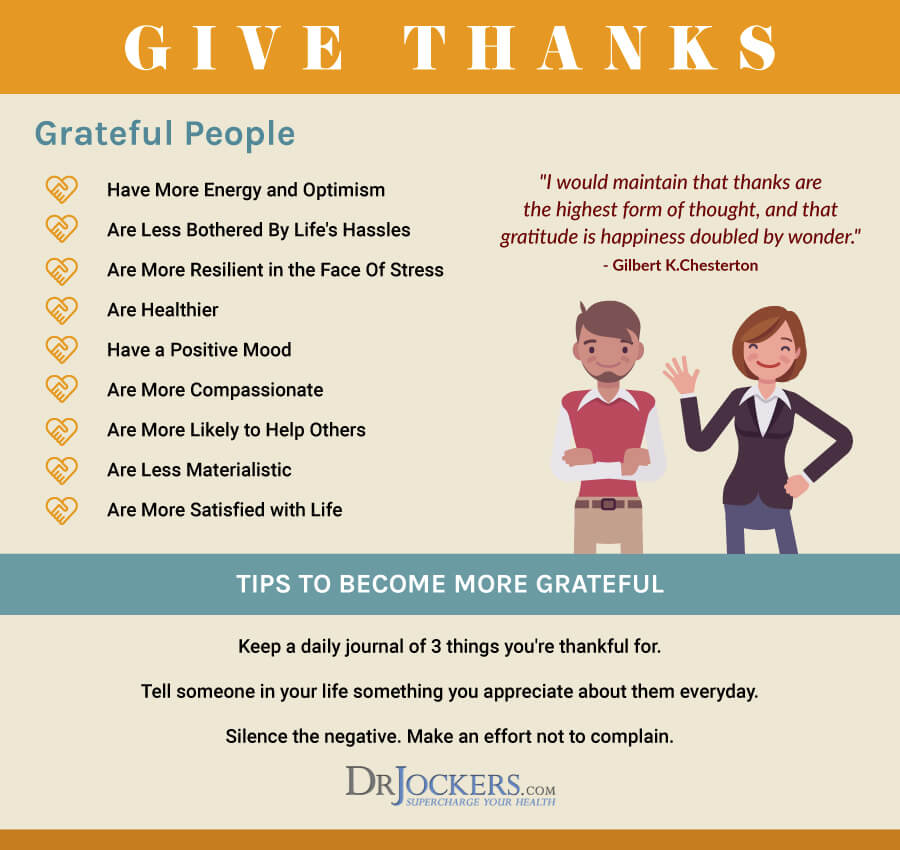
Reduce Stress and Prioritize Good Sleep
Chronic stress and poor sleep can both increase chronic inflammation and the risk of health issues, including endometrial cancer. Reducing stress and prioritizing sleep is important for prevention, the recovery period, and post-recovery for overall health and a good quality of life.
A 2007 prospective cohort study found that chronic stress may be associated with the increased risk of endometrial cancer (33). A 2019 study published in Gynecological Oncology found that poor and inadequate sleep is a common problem among survivors of endometrial cancer (34). A 2020 study published in Support Care Cancer found that poor sleep, depression, and a poor quality of life are common among endometrial cancer survivors with obesity (35).
Reduce stress in your life as much as possible. Avoid stressful situations as much as possible. Reduce the time you spent with people that bring you down or bring your stress. Stop scrolling the news or social media all day. I recommend choosing a designated time to check news, social media, and personal email. Use social media to your benefit! Follow pages and groups that inspire, uplift, and educate you and remove the rest.
Completely avoiding stressful situations, people, and things is impossible. Learning strategies that help you to manage stress and respond to stress better, decrease your anxiety, and calm your mind and body is critical. Create positive mindset shifts and practice positive affirmations.
Practice gratitude. Journal regularly to help work through emotions, spot patterns, and express yourself. Try meditation, guided relaxation, breathwork, visualization, prayer, and spiritual practices. Move your body and practice grounding to release tension from your body. Time in nature, taking a healing bath, doing arts and crafts, calming essential oils, like lavender, or sipping on herbal tea may also help to create calm in mind, body, and spirit.
Going through health challenges alone can be difficult. Surrounding yourself with supportive and loving friends and family is key. However, you may be dealing with trauma, deeper emotional issues, or illness-related emotional stress, and may benefit from professional support.
Working with a therapist, counselor, spiritual counselor, or life coach can help you learn some strategies and work through emotional difficulties, trauma, and non-supportive cognitive patterns. You may join a support group for cancer patients or survivors to gain support from individuals going through similar challenges.
To support nighttime relaxation, sleep, and overnight rejuvenation, reduce the use of electronics at night. Use blue-light blocking glasses if you must turn on your screen. Avoid sugar, caffeine, alcohol, heavy foods, and stress in the evening. Engage in calming and supportive conversations. Instead of being engrossed in electronics, choose board games, cards, crossword puzzles, singing, listening to calming music, reading fiction or poetry, knitting, crocheting, coloring, drawing, journaling, or other calming activities. Practicing gratitude, prayer, meditation, and visualization exercises are great before going to bed can put your mind into a state of calm.
Support your body’s circadian rhythms by going to bed and waking around the same time every day. Invest in a supportive and comfortable mattress, pillows, and beddings. Use blackout curtains or eye pillows to create a dark, sleep-promoting environment. Keep your room cool. Most people generally sleep the best at around 65 Fahrenheit or 18.3 degrees Celsius, but there are individual fluctuations, and you may find that a somewhat cooler or warmer room works better for you.

Optimize Gut Health and the Estrobolome
Research has shown that poor microbiome balance, poor estrobolome health, and high beta-glucuronidase levels can increase the risk of endometrial cancer (12, 13). A 2020 study published in Biomolecules found that improving the microbiome can improve endometrial health (36). Optimizing your gut health and the estrobolome may help to reduce your risks.
Support your gut health by eating an anti-inflammatory and gut-friendly diet. Take digestive enzymes to support your digestion and HCL betaine to support your stomach acid levels. Eat probiotic-rich fermented foods, such as sauerkraut, kimchi, fermented vegetables, kombucha, and coconut kefir. Take a daily probiotic supplement.
You may also benefit from prebiotic-rich foods that feed probiotics, including jicama, Jerusalem artichokes, apples, leeks, garlic, onions, asparagus, and dandelion greens. However, prebiotics are not right for everyone, however. Some people thrive on a prebiotic-rich diet while others get worse and need to minimize prebiotics by following a low-FODMAP diet or even a carnivore diet for a period of time. If needed, support good elimination through a herbal supplement.
Improve your estrobolome by eating an anti-inflammatory diet. Avoid xenoestrogens that can throw off your hormonal health. Examples of xenoestrogens include plastic bottles, food cans, detergents, flame retardants, cosmetics, and pesticides that may contain these endocrine-disrupting substances. Avoid hormonal birth control and the use of antibiotics. Support your liver and gut health and elimination pathways.
Open up Detoxification Pathways
Toxins and heavy metals can increase your risk of endometrial cancer (19, 22, 23, 24). I recommend opening up your detoxification pathways to reduce toxicity and improve your health. Support your digestion, absorption, and elimination pathways by following an anti-inflammatory diet.
Drink plenty of water to support elimination through urine and sweating and avoid dehydration. Support detoxification through the skin by sweating by using an infrared sauna regularly and exercising. Detox phthalates through urine, sweating, and stool.
Use activated coconut charcoal that binds to heavy metals and toxins. Activated charcoal supports the elimination of toxins and decreases oxidative stress and inflammation. Try bioactive carbons derived from multiple sources of humic acid, fulvic acid, and humic acid to support the elimination of heavy metals and other toxins and improve detoxification pathways.
Try coffee enemas to help pull out and eliminate toxins and old waste from your colon. Support elimination with herbal supplements, if needed.
Improve Vitamin D Levels
Poor vitamin D levels can increase your risk of endometrial cancer, while improved vitamin D levels can support recovery (14, 15, 16). I recommend improving your vitamin D levels through sunshine, diet, and supplementation. Daily sunshine exposure and eating foods high in vitamin D, including fatty fish, liver, and egg yolks, is critical, but also not enough.
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need to supplement to optimize their vitamin D levels. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000–5,000 IUs of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1–2 times each year and get your levels between 50–100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70–100 ng/ml.
Improve Zinc Levels
Zinc deficiency, high copper levels, and poor zinc:copper ratio can increase the risk of endometrial cancer (17). A 2018 review published in the International Journal of Medical Research, on the other hand, found that increasing zinc levels may decrease the risk of cervical cancer (18, 19, 20, 21). According to a 2009 review published in Nutrition and Cancer, zinc can help to decrease inflammatory cytokines, and the better apoptosis of cancer cells thus may help to prevent cancer (37). Improving your zinc levels and zinc: copper ratio is critical for your health.
Zinc and copper compete against each other as antagonists to regulate physiological pathways. Achieving a healthy balance between these two minerals is critical for your health. I recommend checking your plasma zinc and serum copper levels and their balance. This should help you with a dietary and supplement strategy to improve your levels.
Your dietary choices can improve your copper/zinc ratio. Zinc-rich foods include grass-fed lean meat, pasture-raised poultry, nuts, seeds, oysters, peas, and chickpeas. Foods that are good sources of copper include oysters, leafy green, shiitake mushrooms, liver, lobsters, nuts, and seeds.
I also recommend that you take a high-quality zinc supplement. If you find that your copper levels are off, you can take a chelated copper supplement or a zinc supplement with copper to support a healthy copper/zinc ratio. However, if you find that your zinc levels are too low but your copper levels are too high, focus on taking only a zinc supplement without copper.
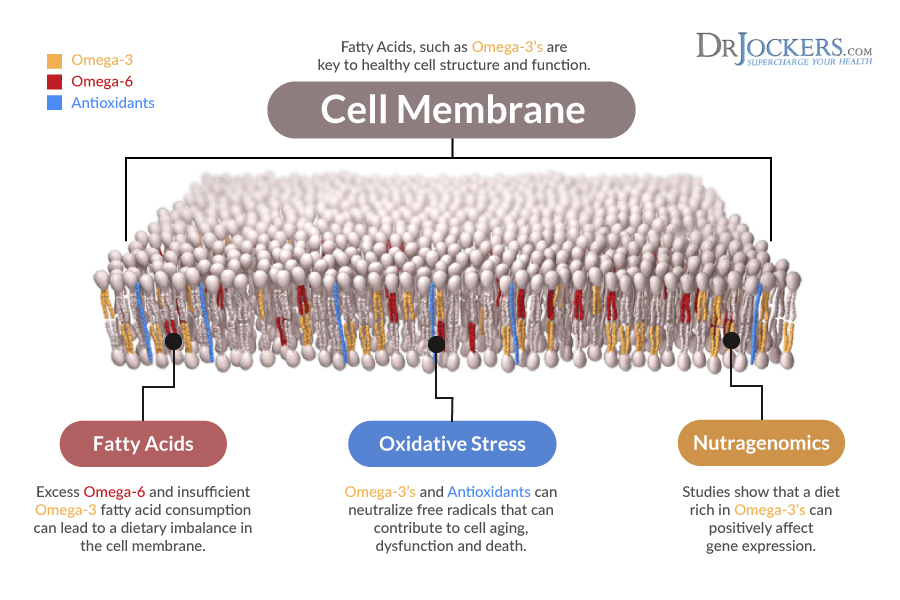
Optimize Omega-3 Fatty Acid Levels
Chronic inflammation is one of the underlying root causes of endometrial cancer (7, 8). Omega-3 fatty acids have anti-inflammatory benefits and may help to reduce your risks.
A 2012 population-based case-control study published in the European Journal of Nutrition found that omega-3 fatty acids have anti-carcinogenic effects and omega-3 fish oil supplements may help to reduce the risk of endometrial cancer (38). A 2015 study published in the American Journal of Clinical Nutrition found that omega-3 fatty acids may help to reduce inflammation and the risk of endometrial cancer (39).
I recommend eating plenty of foods rich in omega-3 fatty acids, including fish, seafood, algae, hemp seeds, chia seeds, flax seeds, and walnuts, to improve your omega-3 fatty acid levels. I also recommend taking a daily high-quality omega-3 fish oil supplement to ensure optimal levels and support your health.
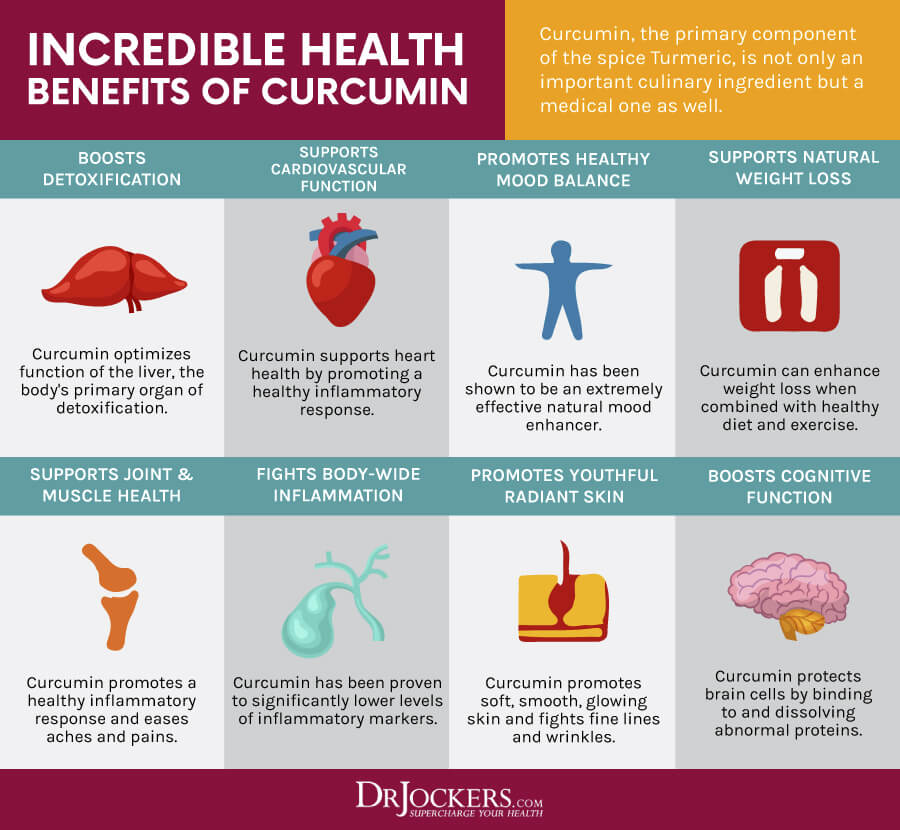
Consider Using Curcumin
Curcumin is the active compound of the spice turmeric. It is known for its anti-inflammatory effects and for a list of health benefits that can support your body. A 2019 study published in the International Journal of Women’s Health found that curcumin has anti-cancer benefits and may support those with endometrial cancer (40). A 2021 study published in Cancer Cell International also found that curcumin offers anti-tumor benefits for endometrial cancer (41).
I recommend using turmeric in your kitchen. You can add turmeric spice to your soups, curries, vegetable dishes, casseroles, smoothies, juices. You can make your own turmeric golden milk. I also recommend that you take a high-quality curcumin supplement daily.
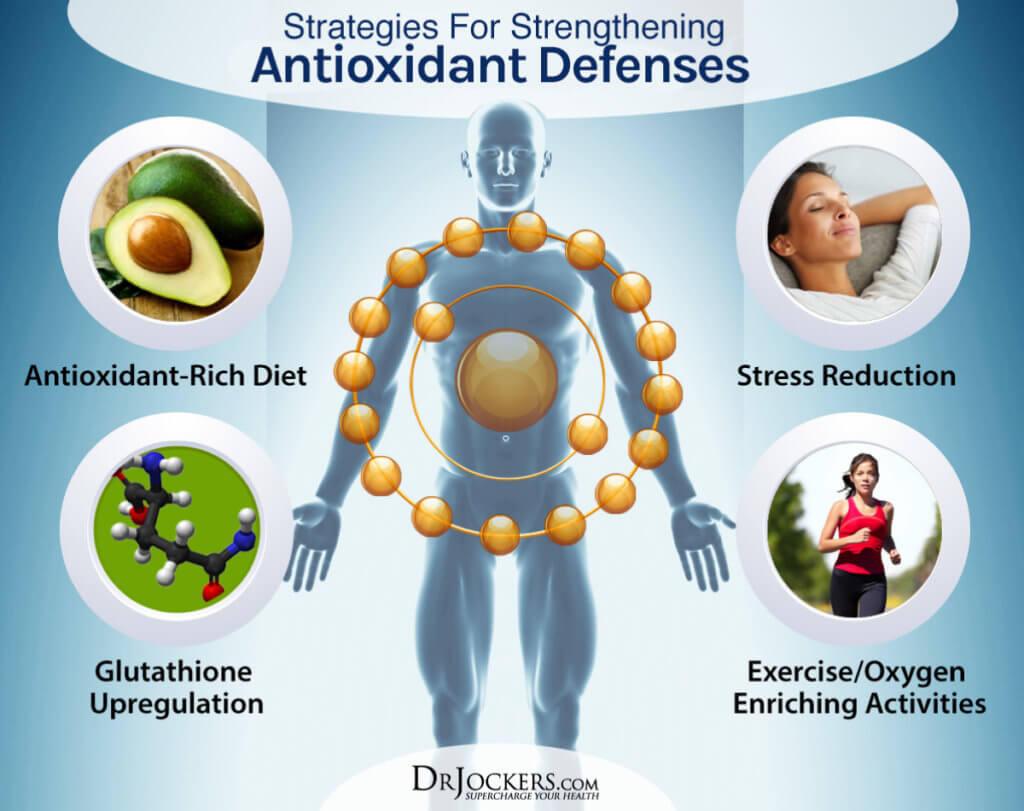
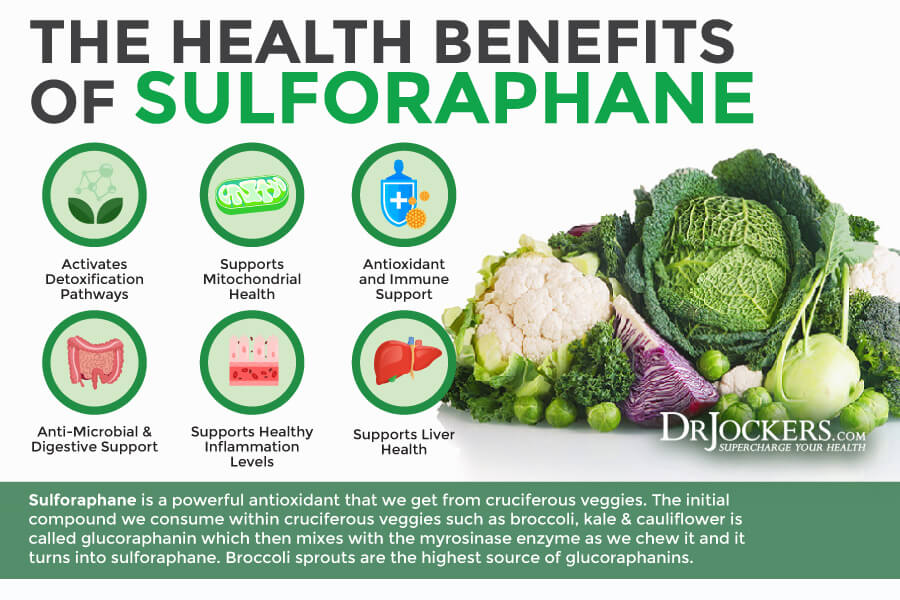
Consider Using Sulforaphane
A 2015 review published in Antioxidants Redox Signaling found that sulforaphane may have chemopreventive properties (42). A 2018 study published in Oxidative Medicine and Cellular Longevity found that sulforaphane helps to activate Nrf2 signaling and reduces oxidative stress and the risk of cancer (43). A 2020 study published in Cancers (Basel) found that sulforaphane may have anticancer effects for endometrial cancer (44).
I recommend eating sulforaphane-rich foods, including kale, broccoli, cauliflower, Brussels sprouts, cabbage, cress salads, kohlrabi, collard greens, cabbage, bok choy, mustard greens, broccoli sprouts, arugula, avocado, lime, artichokes, green beans, and celery. I also recommend supplementing with sulforaphane.
Consider Using Calcium D-Glucarate
A 2002 review published in Alternative Medicine Reviews found that calcium d-glucarate may help to reduce beta-glucuronidase (45). As a result, it may help to reduce the risk of endometrial, breast, prostate, and colon cancer. It also helps to improve estrogen metabolism.
I recommend eating foods rich in calcium d-glucarate, including spinach, broccoli, apples, and oranges. I recommend using calcium d-glucarate to reduce beta-glucuronidase and improve endometrial health.

Final Thoughts
Endometrial cancer will affect about 3 out of 100 women during their lifetime. Since many of the root causes of endometrial cancer are lifestyle-related, there are several natural support strategies that can reduce your risks and support your recovery. To identify some major root causes and risk factors, I recommend looking at the functional lab tests mentioned in this article. I recommend that you follow my natural support strategies to support your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.