 Neuropathy: Risk Factors, Causes, and Support Strategies
Neuropathy: Risk Factors, Causes, and Support Strategies
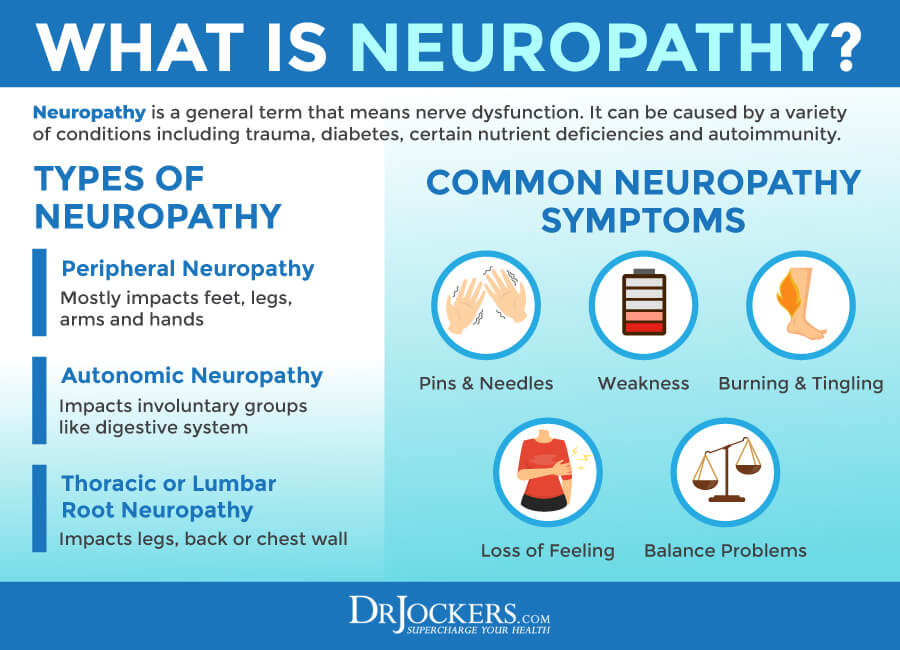
Neuropathy is a condition characterized by nerve damage. It may develop because of diabetes, metabolic issues, traumatic injuries, infections, chemotherapy, certain medications, and other reasons. Neuropathy can cause numbness, tingling, prickling, muscle weakness, pain, muscle shrinking, and other issues. These symptoms can be uncomfortable and, for some, even debilitating. The good news is that certain natural support strategies can help to improve your health.
In this article, you will learn what neuropathy is. You will learn about the symptoms of neuropathy. I will discuss the types of neuropathy. You will understand the risk factors and root causes of neuropathy. You will learn about diagnosis and conventional treatment options for neuropathy. I will share some specific labs I recommend for neuropathy. I will also share my top natural support strategies to improve your health and wellness.
What Is Neuropathy
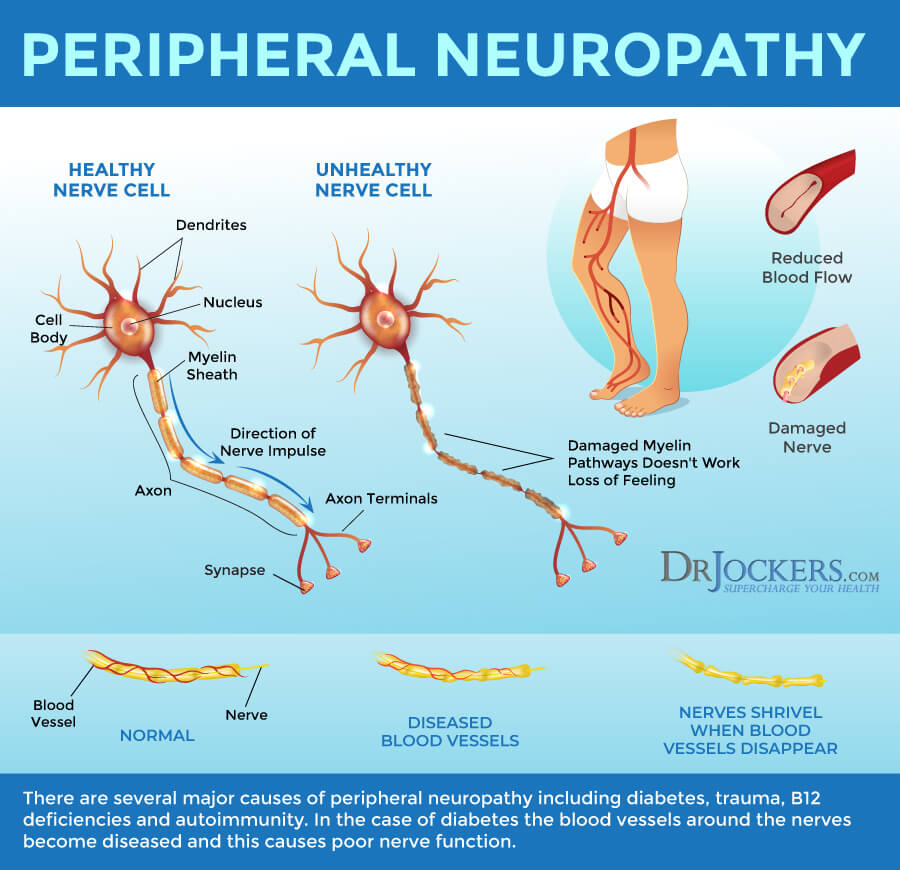
Neuropathy is a condition characterized by nerve damage that may develop because of diabetes, metabolic problems, chemotherapy, infections, traumatic injuries, or other reasons. The most common form of neuropathy is peripheral neuropathy. It is often caused by diabetes and develops from damage to your peripheral nerves (1).
According to the National Institute of Neurological Disorders and Stroke, peripheral neuropathy affects about 20 million people in the United States alone (1). Your peripheral nervous system plays a vital role in your body. Its role is to send messages from your brain and spinal cord to the rest of your body, as well as to deliver sensory information to your nervous system. If there is damage to your peripheral nerves, it can interrupt their function and cause numbness, weakness, pain, and other symptoms (1).
Symptoms of Neuropathy
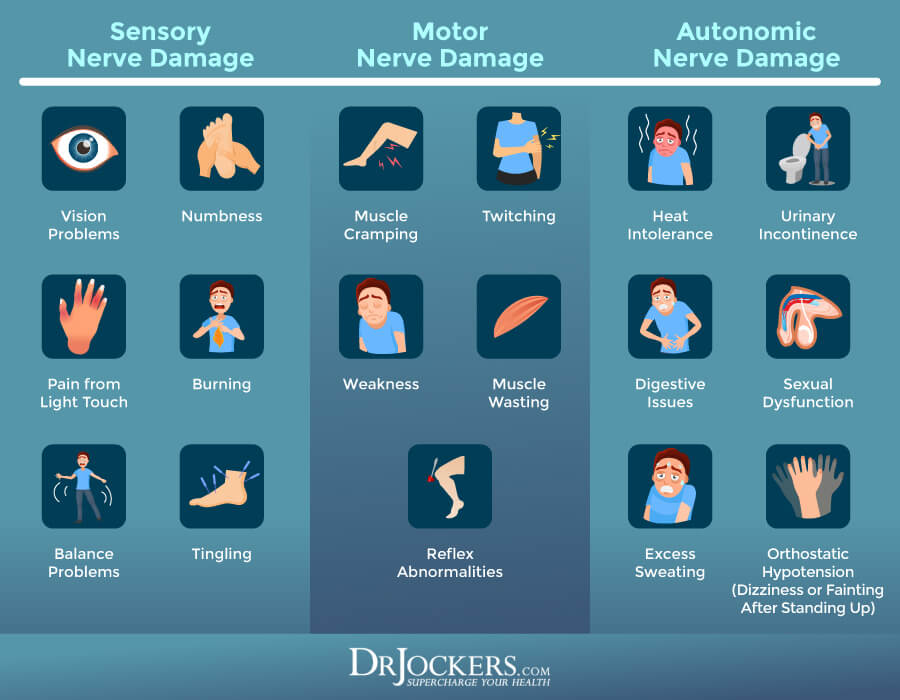
Symptoms of neuropathy may include (1):
- Temporary or permanent numbness
- Tingling or prickling sensation
- Muscle weakness
- Cramps
- Muscle shrinking
- Pain
- Increased sensitivity
- Impairment of urination or sexual function
- Dysfunction of certain glands or nerves
- Sweating or heat intolerance
- Gastrointestinal issues
Types of Neuropathy
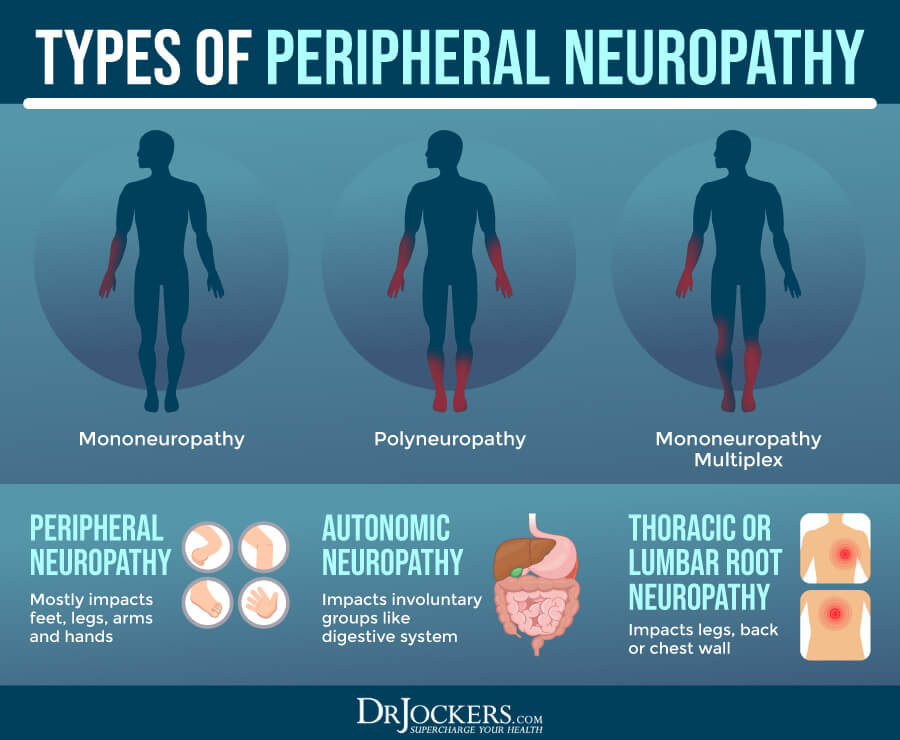
When it comes to neuropathy, we may talk about mononeuropathy or polyneuropathy. Mononeuropathy, as its name (mono) indicates, involves damage to only one single nerve. Polyneuropathy, again, as its name (poly) suggests, involves damage to multiple nerves that may affect a variety of bodily functions (1).
There are different types of polyneuropathy:
- Peripheral symmetric neuropathy: Peripheral symmetric neuropathy is the most common type of neuropathy. It is also the most common form of diabetic neuropathy. Peripheral symmetric neuropathy tends to affect the feet and hands.
- Autonomic neuropathy: Autonomic neuropathy is a type of neuropathy that affects the nerves that control your involuntary bodily functions, including your digestion, heart rate, and urination.
- Thoracic and lumbar root proximal neuropathy: Thoracic and lumbar root proximal neuropathy is a type of neuropathy that leads to damage to the nerves along with certain specific areas of your body, including your legs or chest wall.
Risk Factors for Neuropathy
Risk factors for neuropathy may include (2):
- Poorly managed diabetes
- Trauma
- Poor Posture & Ergonomics
- Cancer
- HIV/AIDS
- Autoimmune conditions
- Chemotherapy
- Alcohol
- Kidney failure
- Carpal tunnel syndrome
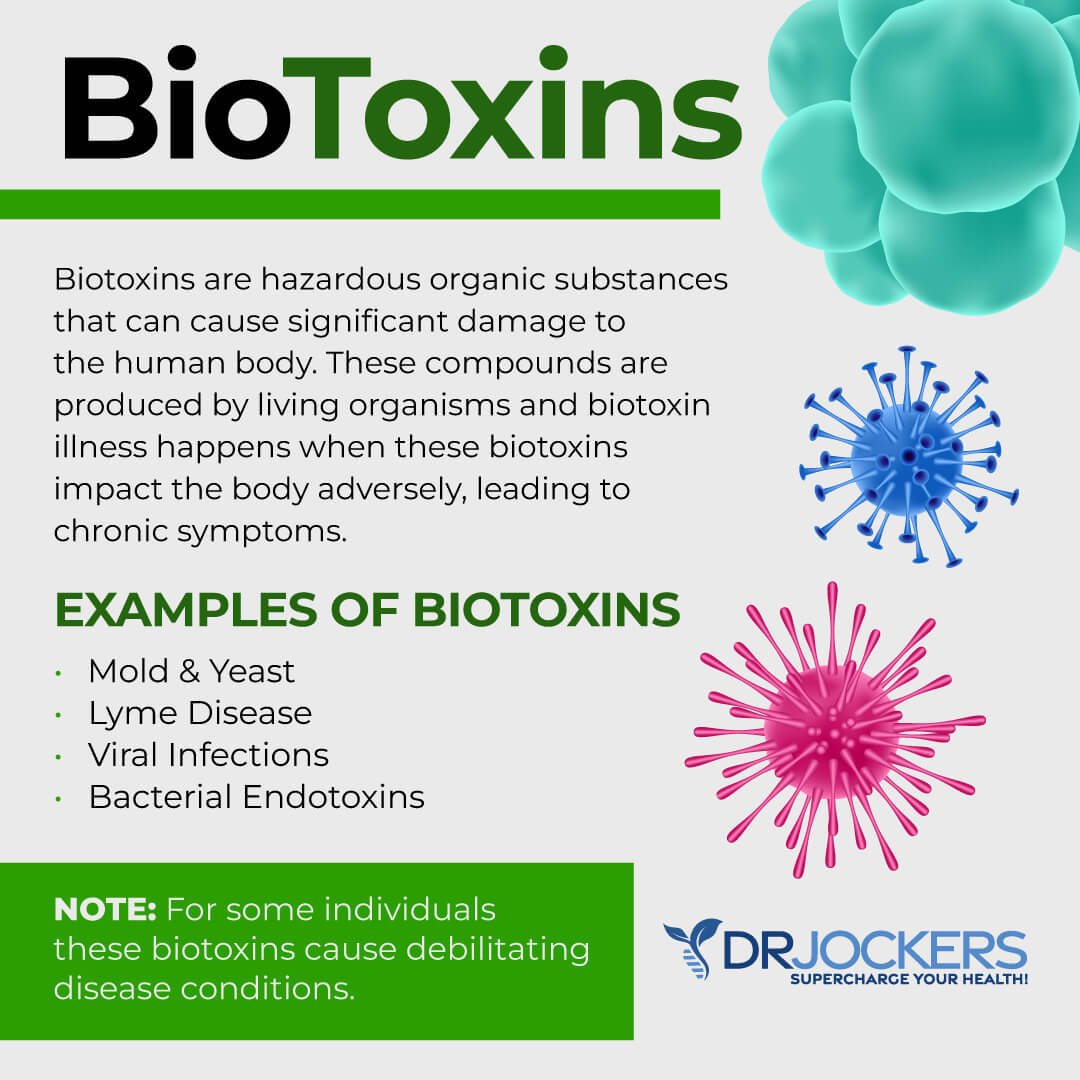
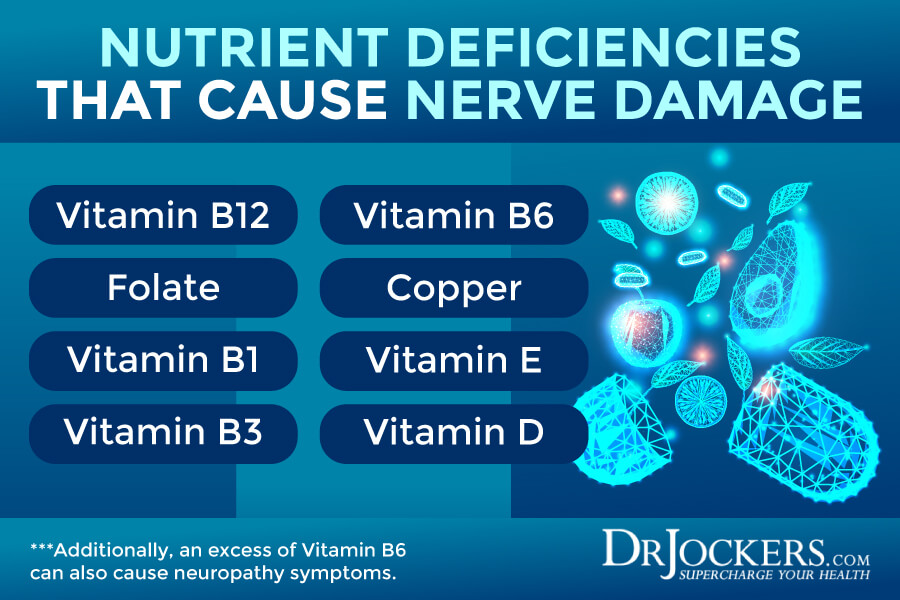
- Nutrient deficiencies, including vitamin B12 and copper
- Excess nutrient consumptions, especially excess of vitamin B6
- Toxins in food
- Inflammation
Root Causes of Neuropathy
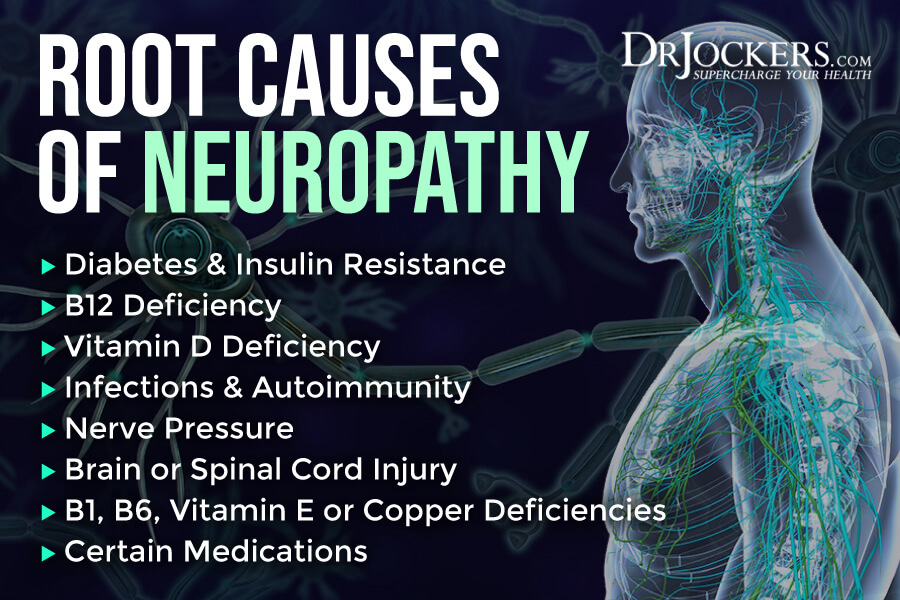
As a doctor of functional medicine, I always look at the root causes of your health issues. There are a number of root causes of neuropathy that your need to be aware of, including diabetes and insulin resistance, nutrient deficiencies, infections, autoimmunity, nerve pressure, brain and spinal cord injury, and certain medications.
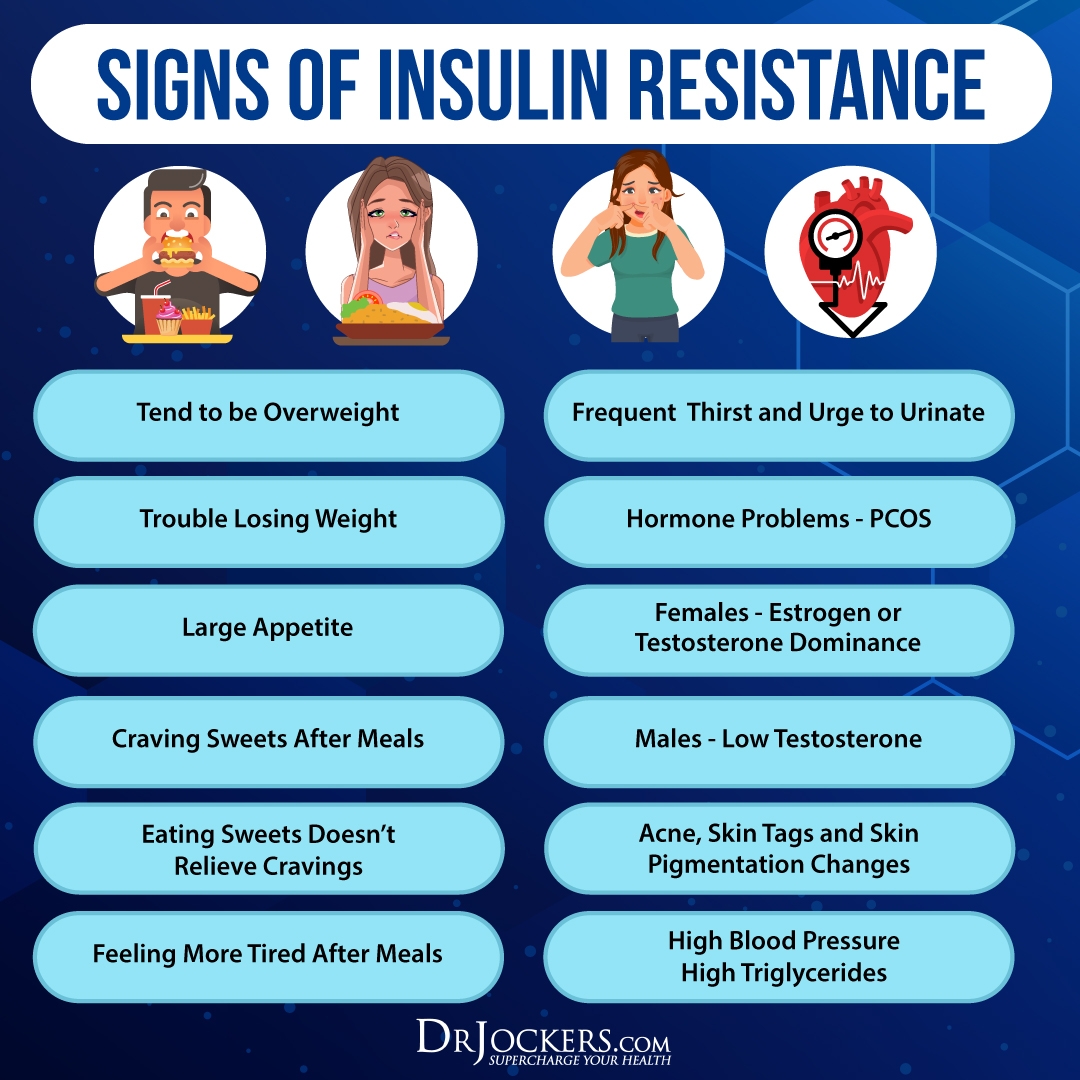
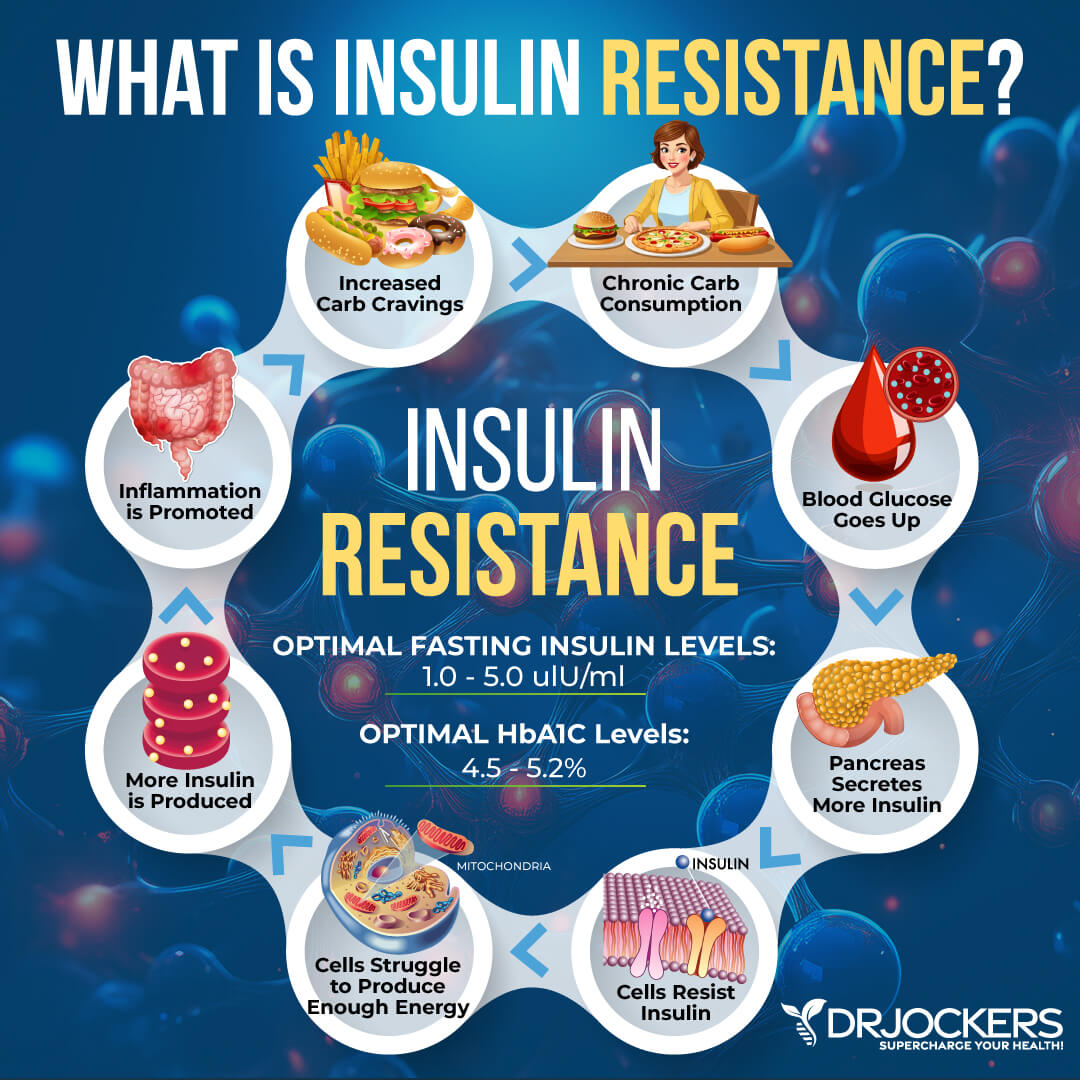
Diabetes and Insulin Resistance
Insulin resistance means that your body is not responding to insulin well and cannot handle the blood glucose levels. Insulin resistance increases your risk of prediabetes and diabetes. However, it may occur in those without diabetes. According to a 2015 study published in Diabetology and Metabolic Syndrome, insulin resistance can play a critical role in developing peripheral neuropathy (3).
According to a 2017 study published in the Journal of Diabetes Investigations, diabetes is one of the most common causes of peripheral neuropathy, accounting for at least 50 percent of cases (4). The study has found that lifestyle changes, glycemic control, and balancing blood sugar levels are powerful methods that can reduce the risk of diabetic peripheral neuropathy and some of its risk factors, including obesity, prediabetes, diabetes, and metabolic syndrome.
Peripheral neuropathy affects about 20 million people, and according to The Foundation for Peripheral Neuropathy, 68 percent of them have diabetes (5). About 8 percent of Americans have diabetes, and 60 to 70 percent of them experience peripheral neuropathy (5).
While diabetic neuropathy is more likely to develop in those with type 2 diabetes, individuals with type 1 diabetes may also experience neuropathy. While it’s prevalent in both sexes, women are more likely to experience nerve pain from peripheral neuropathy. As a complication from peripheral neuropathy in those with diabetes, amputations are increasingly common (6).
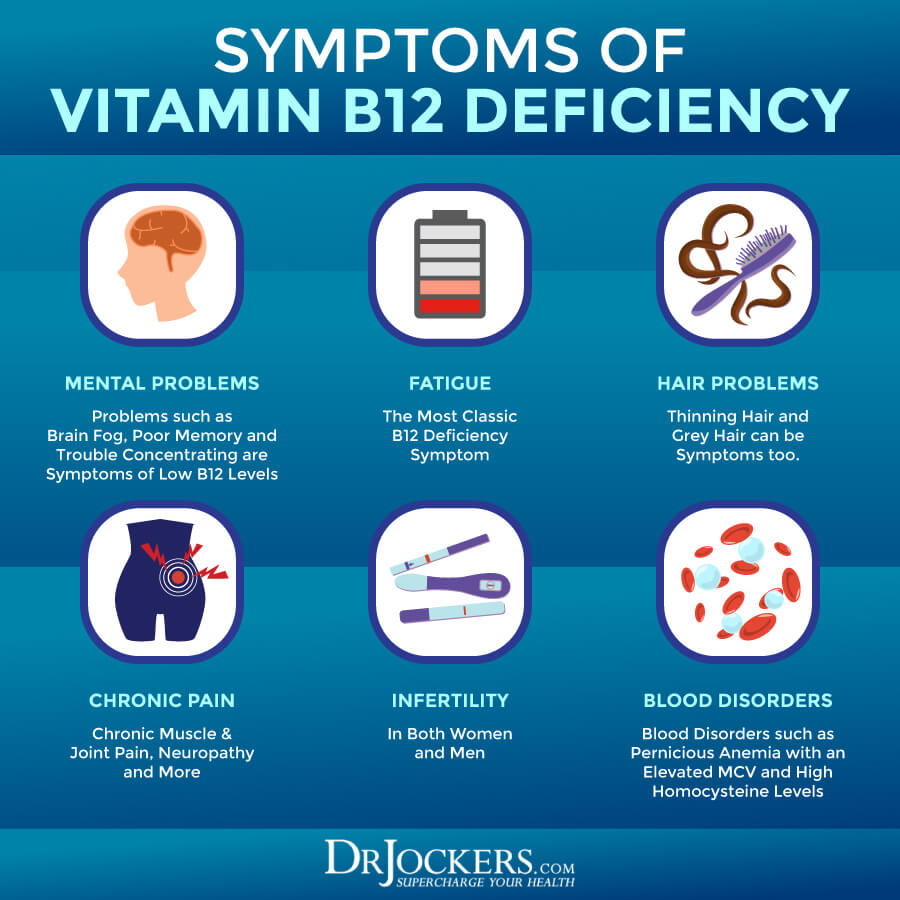
B12 Deficiency
According to a 2014 study published in Continuum (Minneapolis, Minnesota), nutrient deficiencies are one of the common root causes of neuropathy (7). Vitamin B12 deficiency is the number one nutrient deficiency that can lead to peripheral neuropathy.
Since vitamin B12 is naturally found in animal-based foods, including red meat, fish, poultry, eggs, and dairy, and fortified foods. Meeting your vitamin B12 needs on a vegan diet is impossible. However, deficiencies among those who consume animal-based foods are also common.
Poor levels of stomach acid can interfere with absorption and interfere with deficiency regardless of your diet. Certain medical conditions, including autoimmune diseases, pancreatic disease, gastritis, malabsorption syndrome, and pernicious or unexplained anemia, and certain medications, including histamine 2 receptor antagonists or proton pump inhibitors, may also reduce your ability to absorb vitamin B12 and cause a deficiency (8).
Vitamin B12 deficiency can affect anyone of any age, but it’s the most common among the elderly. According to The Foundation for Peripheral Neuropathy, about 10 to 25 percent of people over 80 are deficient in vitamin B12 (8). Symptoms of vitamin B12 deficiency may include nerve damage, nerve degeneration, anemia, and other issues.
Not having enough vitamin B12 can damage the myelin sheath that protects your nerve that can cause peripheral neuropathy. Even mild deficiencies can result in problems, but long-term and serious deficiencies can result in permanently debilitating problems. A 2014 case study in BMC Research Notes has found that vitamin B12 deficiency to be the cause of rare cases of peripheral neuropathy in youth (9).
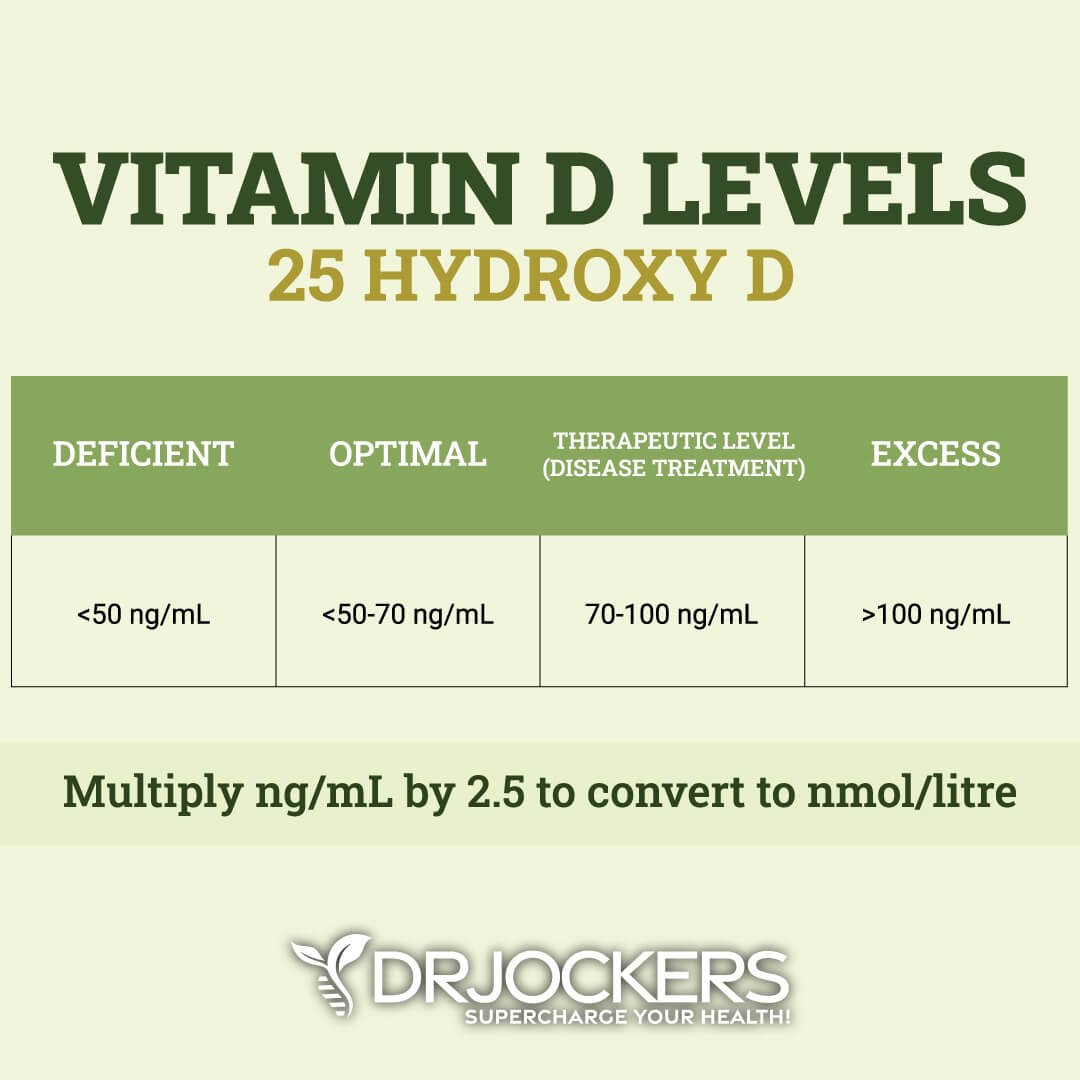
Vitamin D Deficiency
Vitamin D is a fat-soluble vitamin that is important for your bone, muscle, teeth, brain, immune system, and other areas of your health. Due to our indoor lifestyles and lack of supplementation, vitamin D deficiencies are very common among both people with type 2 diabetes and the general public. Neuropathy is a common complication of diabetes, and increasing research suggests that vitamin D deficiency may play a role in the development and symptoms of neuropathy.
A 2016 cross-sectional study published in Diabetes/Metabolism Research and Reviews has looked at 861 patients with diabetes. Researchers looked at their 25-hydroxyvitamin D levels and signs of peripheral neuropathy. They found that having a vitamin D deficiency can increase the risk of peripheral neuropathy in adults with type 2 diabetes (10).
A 2018 study published in Diabetic Medicine: A Journal of the British Diabetic Association has also found that vitamin D deficiency may increase the risk of painful diabetic peripheral neuropathy (11). Researchers looked at three groups of participants: one group with painful diabetic peripheral neuropathy, one group with painless diabetic neuropathy, and one group with no diabetic neuropathy.
Throughout the 3-months study between July and September, all participants receive seasonal (summer) sunlight exposure. Their 25-hydroxyvitamin D levels were measured, and they underwent a lower limb skin biopsy.
Researchers observed a significant difference in vitamin D levels between participants with painful diabetic peripheral neuropathy and other participants. Results suggest that vitamin D deficiency plays a role in the symptoms of peripheral neuropathy related to diabetes.

Infections & Autoimmunity
Infections and certain autoimmune conditions may increase your risk of neuropathy. Inflammatory neuropathy is specifically caused by an infection or autoimmunity. The infection or an autoimmune reaction attacks your nerves, which leads to symptoms of neuropathy. Sensory symptoms, such as numbness, tingling, or burning, are very common, however many patients also complain about muscle weakness or pain. Symptoms may be widespread or, in other cases, contained to your legs or arms (12).
Some common infectious agents that may cause neuropathy include hepatitis B, hepatitis C, herpes zoster (shingles), Lyme disease, HIV/AIDS, varicella, West Nile virus, cytomegalovirus, herpes simplex virus, and leprosy (1, 12). According to the National Institute of Neurological Disorders and Stroke, about 30 percent of people with HIV develop peripheral neuropathy at one point during their illness, and 20 percent will develop distal neuropathic pain (1).
Those infected with Lyme disease tend to develop neuropathic symptoms within a few weeks of the infection from a tick bite (1). However, chronic Lyme disease may also be characterized by neuropathic pain, which may develop weeks, months, or even years after the initial infection. According to a 2014 study published in The Neuroohospitalist, while peripheral neuropathy from viral, bacterial, and parasitic infections are common, they are manageable and treatable (13).
Neuropathy may also develop because of an autoimmune disease. Systemic autoimmune diseases, such as Sjögren’s syndrome, lupus, and rheumatoid arthritis (RA) affect multiple areas of your body. As your immune system mistakenly attacks its own tissues, it may affect your nerves or your tissues around your nerves in these diseases leading to neuropathic pain. In some autoimmune diseases, such as Guillan-Barre syndrome and chronic inflammatory demyelinating polyneuropathy, infections trigger your immune system to attack its nerve that can not only lead to a chronic autoimmune neuropathy but also visible muscle shrinking and weakness (1).
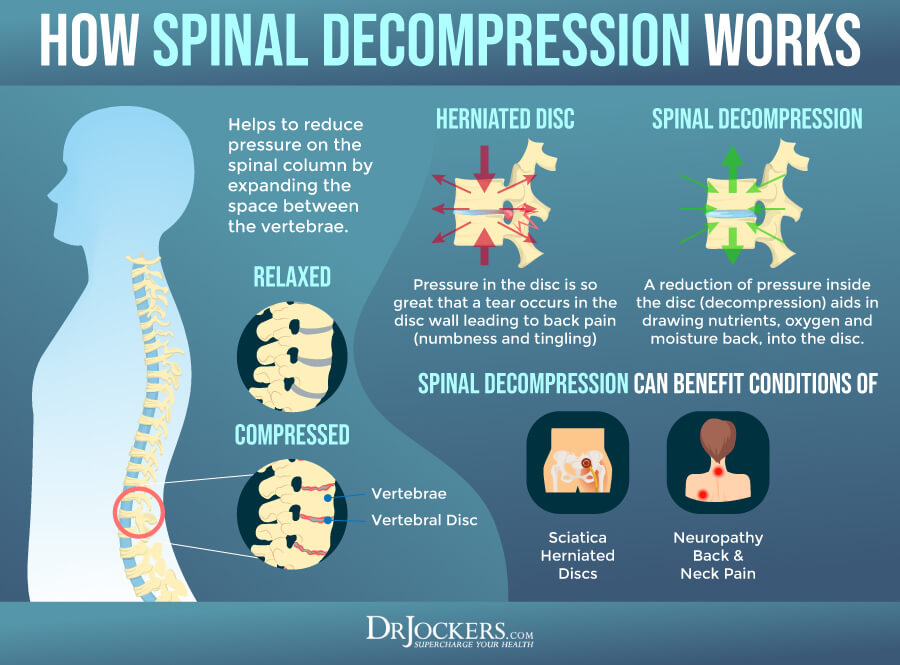
Nerve Pressure
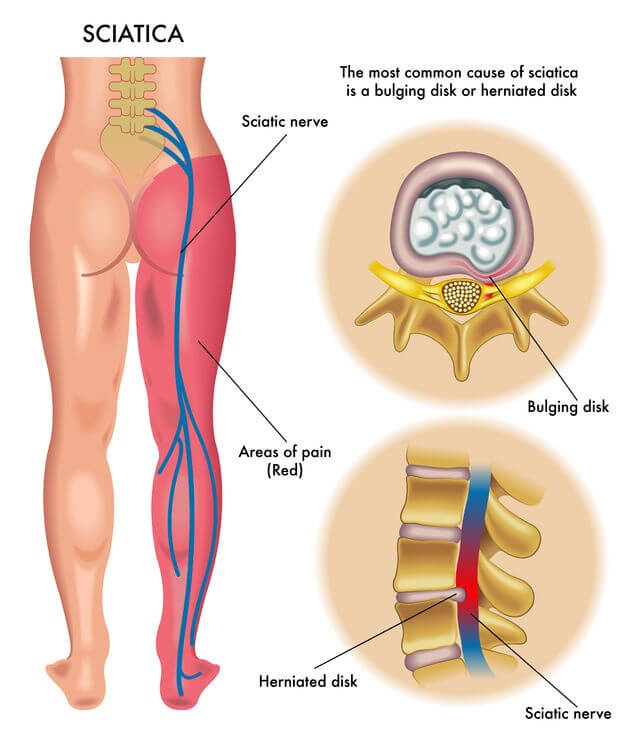
Nerve pressure is one of the most common causes of neuropathy. Experiencing an injury from playing sports, falls, car accidents, whiplash, or even from certain medical procedures can cause damage to or around your nerves, such as stretching, compressing, or crushing your nerves. Breaking or dislocating your bones or joints can contribute to slipped disks that can compress your nerve fibers and cause symptoms (1).
Repetitive or forceful activities or poor posture can also cause your ligaments or tendons to swell or your discs to move, narrowing your nerve pathways and compressing your nerve fibers. Sciatica, scoliosis, and spinal subluxation (misaligned vertebrae in your spine) can put prolonged pressure on and compress your nerve fibers increasing the risk of neuropathic pain.
Arthritis puts ongoing pressure on your nerves. Carpal tunnel syndrome and ulnar neuropathy cause compressed nerves in your elbow or wrist, leading to pain and discomfort (1).
Brain or Spinal Cord Injury
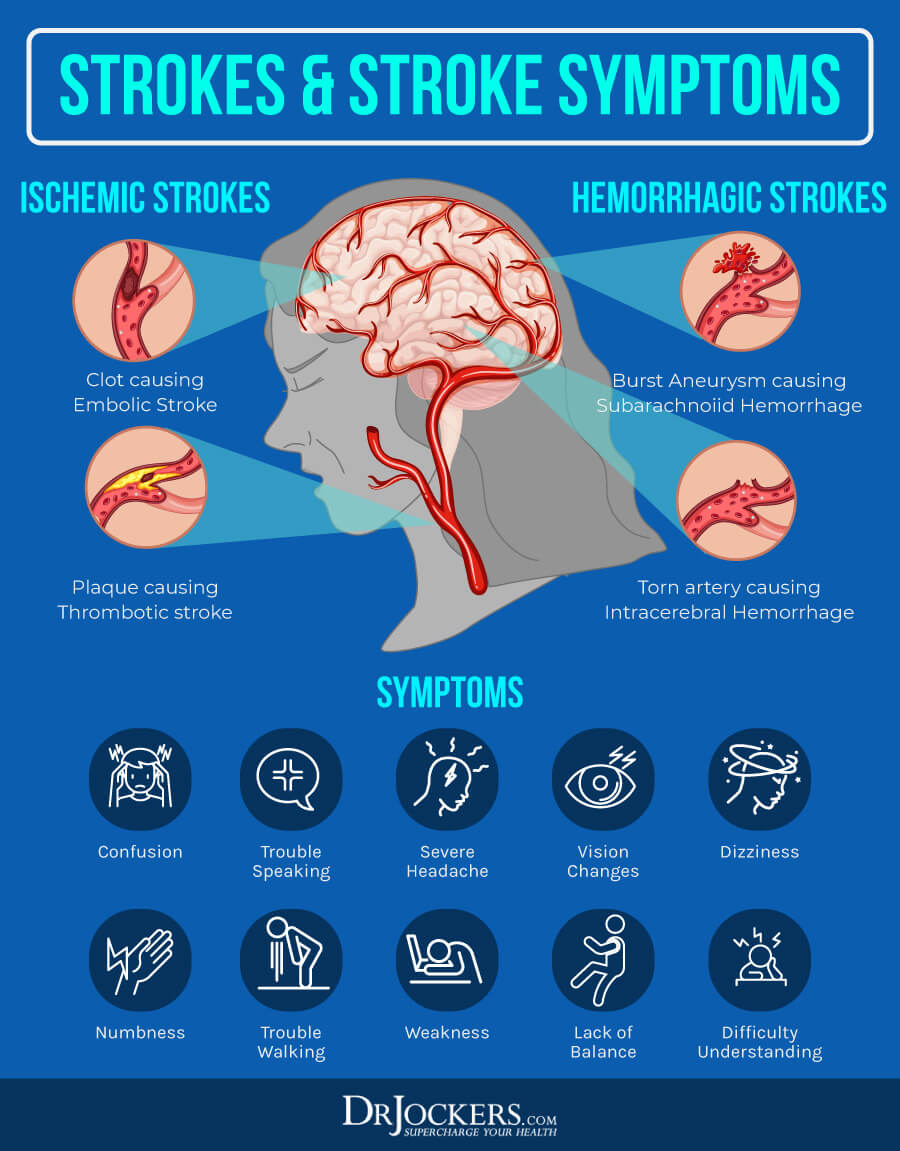
Brain and spinal cord injuries can also lead to neuropathy. Encephalitis, stroke, transverse myelitis, spinal cord injury, and traumatic brain injury can all contribute to or worsen neuropathy.
Encephalitis is a brain inflammation that is usually caused by a viral infection. Symptoms may include flu-like symptoms, seizures, fatigue, weakness, movement issues, and problems with sight or hearing. According to a 2017 case report and systematic literature review published in Brain and Behavior, encephalitis may cause acute neuropathy (14).
Strokes occur when there is an interruption to the blood supply to your brain causing your brain cells to start dying within minutes. Central neuropathy or central post-stroke pain is a common problem. According to the Stroke Association, it may affects up to 20 percent of stroke survivors (15).
Transverse myelitis is a neurological disorder and an inflammation that affects both sides of one section of your spinal cord and your nerve cell fibers. This can disrupt messages across your spinal cord nerves and your entire body. According to 2015 case reports published in the Annals of Rehabilitation Medicine, transverse myelitis can cause polyneuropathy (16).
Spinal cord injury means that there is damage that occurred at any part of your spinal cord or nerves located at the end of your spinal canal. A sudden blow or cut to your spine from a fall or accident can cause a traumatic spinal cord injury. Spinal cord injury can result in permanent loss of function, strength, or sensation below the location of the injury. It may result in a number of other issues. A 2013 review published in Critical Reviews in Physical and Rehabilitation Medicine has found that central neuropathic pain is common in spinal cord injury patients. Researchers also found that exercise, acupuncture, and psychological treatment options may help (17).
Traumatic brain injury may occur due to a severe sports injury, car accident, serious fall, violent blow to the head, or other outside force. It may lead to confusion, concentration troubles, blurry vision, headaches, and other symptoms. A 1988 case report published in Clinical Orthopedics and Related Research has found that traumatic brain injury can lead to peripheral neuropathy (18). According to a 2017 study published in Medical Hypotheses, traumatic brain injury in those with diabetes and diabetic neuropathy can increase psychiatric health issues, such as anxiety and depression, sustained brain trauma, and related issues (19).
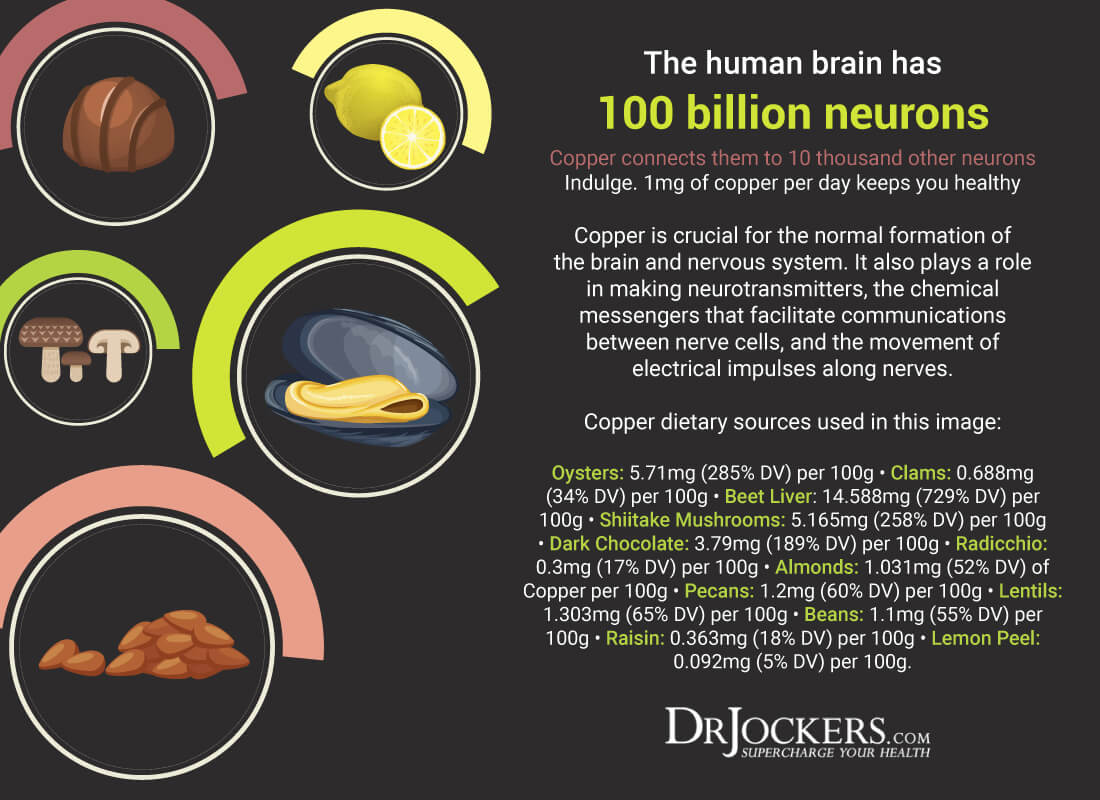
B1, B6, Vitamin E, or Copper Deficiencies
Vitamin deficiencies can also lead to neuropathy. Nutrition deficiencies may occur because of a poor, low-nutrient diet, malabsorption issues, certain medications or health issues that interfere with absorption, or the lack of essential supplementation.
According to a 2013 study published in Neurologic Clinics, thiamine (vitamin B1) deficiency, also known as beriberi can play a role in the development of neuropathy. It can also lead to Wernicke’s encephalopathy, Korsakoff’s syndrome, and heart failure (20).
The same study has found the vitamin E deficiency, niacin (vitamin B3) deficiency, copper deficiency, vitamin B12 deficiency, or copper deficiency can also cause neuropathy (20). When it comes to vitamin B6, researchers found that both deficiency and excess in vitamin B6 can contribute to the development of neuropathy (20).
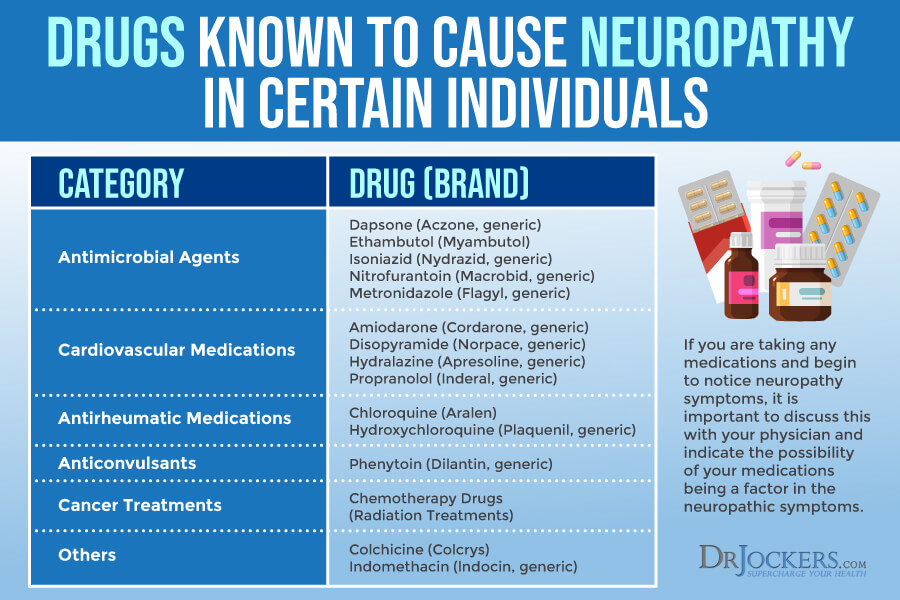
Certain Medications
Neuropathy commonly occurs as a side effect of using certain medications. For example, cancer drugs, like chemotherapy and medication for HIV/AIDS commonly cause symptoms of neuropathy. In many cases, medication-induced peripheral neuropathy goes away once you discontinue using the medication. Sometimes simply reducing the use can help. In other, more extreme cases, however, the nerve damage and the naturopathic symptoms may be long-term or permanent (21).
Medications that may result in peripheral neuropathy include cancer medications, anticonvulsants, anti-alcohol drugs, heart and blood pressure medications, infection-fighting drugs, hydralazine, perhexiline, vincristine, nitrofurantoin, INH, thalidomide, and certain skin condition treatment medications (21). Certain chemotherapy drugs may lead to polyneuropathy in 30 to 40 percent of patients.
In some cases, peripheral neuropathy symptoms may continue even after the end of your chemotherapy treatment. Radiation therapy may also lead to nerve damage and neuropathy that can affect you for months or even years after your treatment (1). If you are taking any medications, it is important that you talk to your doctor about the risk of neuropathy and what you can do to prevent or reduce it.
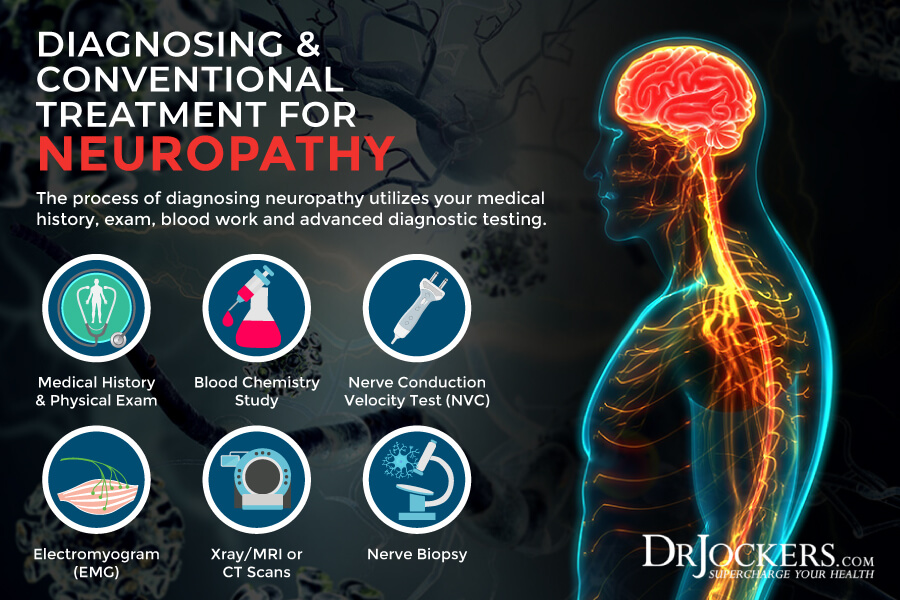
Diagnosis and Conventional Treatments
After going over your medical history, your symptoms, and a physical, your doctor may order a number of tests to diagnose neuropathy. They may order certain neurological exams to look at nerve damage, body fluid tests for infections, vitamin deficiencies, immune system problems, and diabetes, and genetic tests for inherited neuropathies. To look at nerve function, they may order a nerve conduction velocity test (NCV) to check the signal strength and speed of your large motor and sensory nerves and electromyography (EMG) to check the electrical activity of your muscles during rest and contraction (1).
Your doctor may order a variety of neuropathology tests for nerve appearance, including a nerve biopsy to check a sample of nerve tissue for pathologies and a neurodiagnostic skin biopsy to look at your nerve fiber endings. Your doctor may order autonomic testing to evaluate peripheral neuropathies and radiology imaging tests, such as an MRI or a CT to look for nerve root compression, tumors, bone, and vascular irregularities, herniated disks, and other issues (1).
Conventional treatment for neuropathy usually involves over-the-counter pain medication, including nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen. Along with OCTs, treatment usually involves one or several of a variety of prescription medications, including antidepressants, cyclooxygenase-2 inhibitors, tramadol, seizure medications, narcotics, lidocaine patches, and corticosteroid injections (1).
For men, treatment may also involve medications for sexual dysfunction. Other treatment options may include plasmapheresis, a blood transfusion removing irritating antibodies, transcutaneous electronic nerve stimulation (TENS), and ergonomic casts or splints. In certain situations, surgery may also be part of the treatment for pinched nerves (1).
Specific Labs
I recommend a variety of functional lab tests to evaluate your risk for neuropathy.
HbA1C, Fasting Blood Sugar, and Insulin Levels
Blood sugar imbalances are one of the main causes of inflammation. They also increase your risk of insulin resistance, diabetes, and related peripheral neuropathy. I recommend checking your hemoglobin A1C (HbA1C) levels. Your HbA1C levels measure your average blood sugar over the past 2 to 3 months.
Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6 while the optimal range is 4.5 – 5.2.
In addition to testing your HbA1C levels, I recommend checking your fasting insulin levels. Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml and the optimal range is 1.0 – 5.0 uIU/ml.
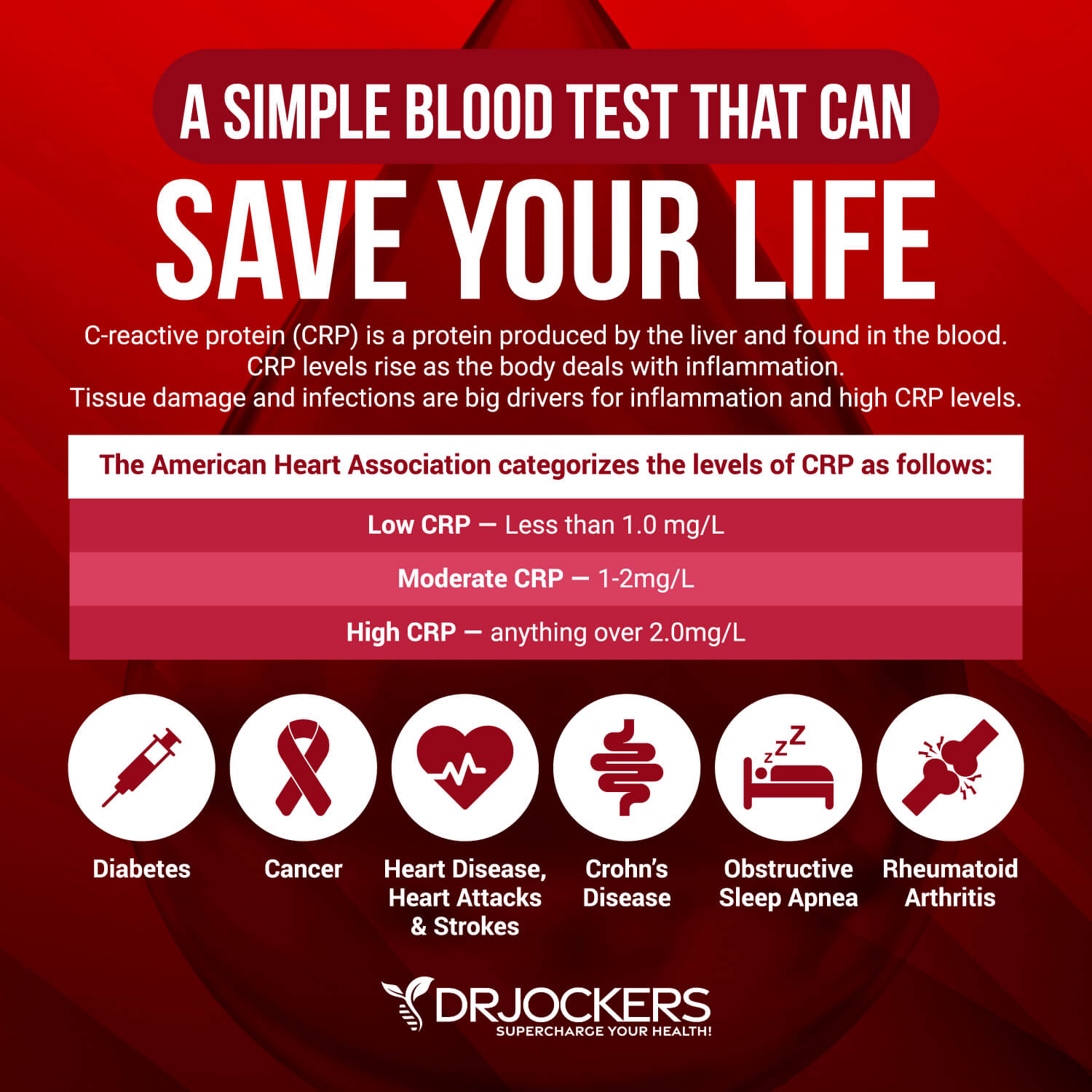
CRP and ESR
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L. When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
The erythrocyte sedimentation rate (ESR) is a common hematology test to look for inflammation. It refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Anything over 20 mm/hr is a sign of significant inflammation and optimal results should be under 10 mm/hr.
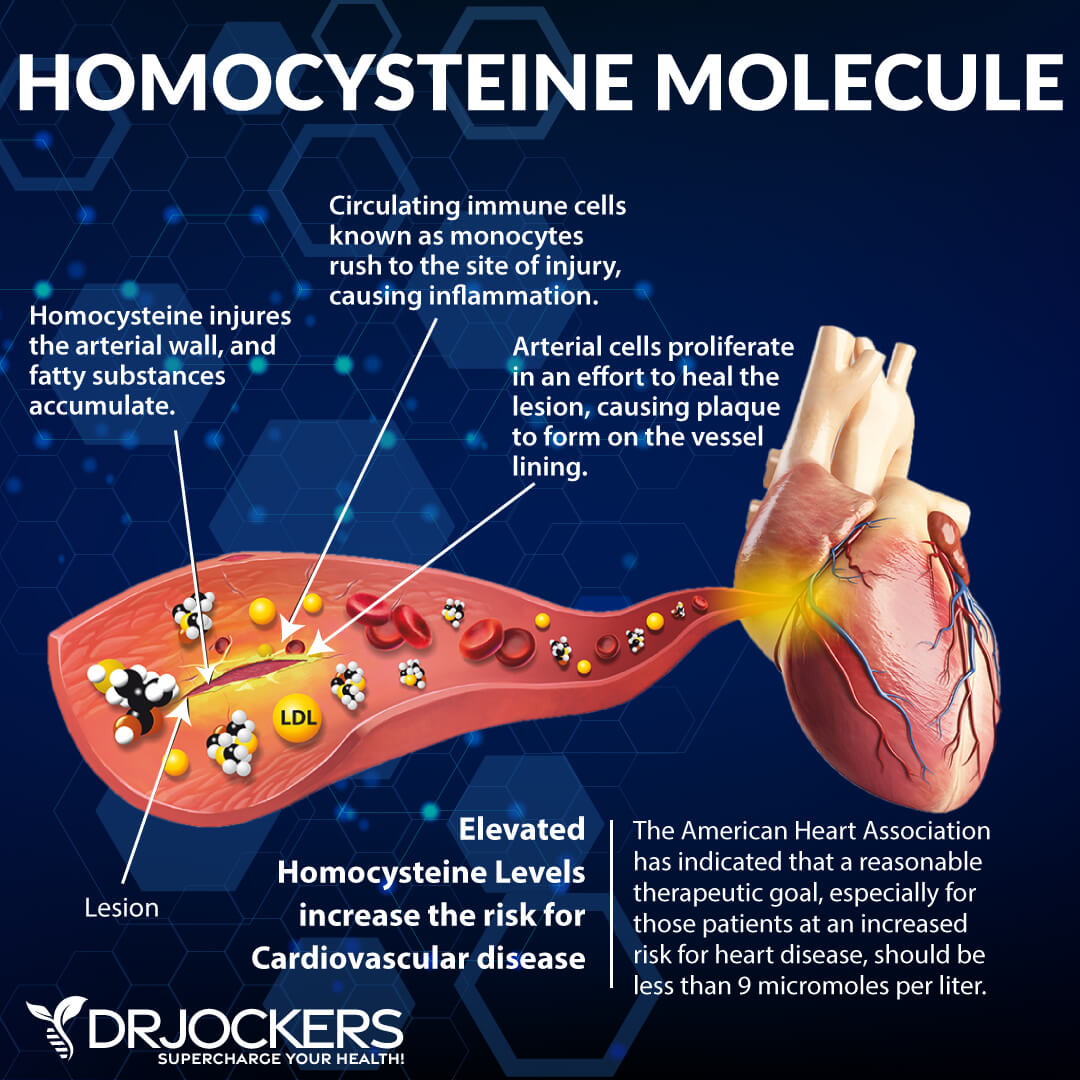
B12 and Homocysteine
Vitamin B12 is essential for the health of your nerves and blood cells, energy levels, DNA, and other areas of your health. Since it’s difficult to meet your need through food alone and near impossible on a vegan, vegetarian, or plant food-heavy diet, most people become deficient in vitamin B12 without supplementation.
Normal levels of vitamin B12 are between 200 and 950 picograms per milliliter (pg/mL). Below 200, your levels are too low and may indicate problems requiring further testing. Between 200 and 300 pg/mL, your B12 levels are considered borderline and may require further testing or supplementation.
Homocysteine is a common amino acid in your blood that you mostly get from eating meat. Homocysteine is particularly a good marker for cardiovascular issues. The optimal range for homocysteine is between 6 and 9.
Vitamin D Levels
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. Normal levels of vitamin D are 50 nmol/L (20 ng/mL) or more, while optimal levels are over 75 nmol/L (30 ng/mL).
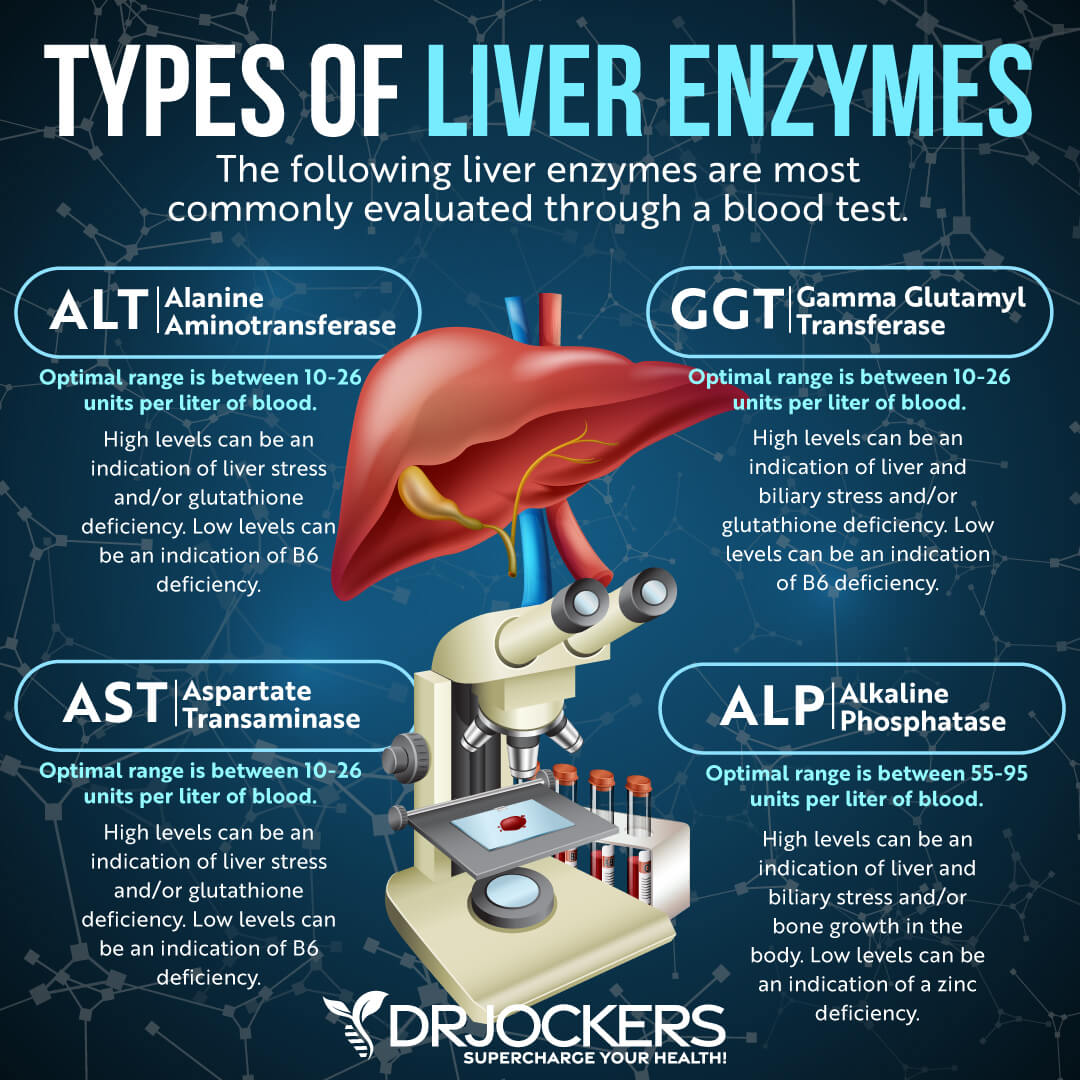
Liver Enzymes
Liver enzyme levels may indicate inflammation, liver stress, vitamin B6 deficiency, as well as liver, gallbladder, bile, or kidney issues.
Alkaline phosphatase is a liver enzyme that is made by the mucosal cells that line the bile system of the liver and helps normal bile flow. Elevated levels (over 95) may indicate inflammation and liver and gallbladder problems.
Alanine aminotransferase (AST) is a liver enzyme. Elevated levels may indicate inflammation. Normal levels are between 10 and 26 IU/L.
Aspartate transaminase (ALT) is an enzyme present in the liver that spills out during times of increased liver stress. Elevated levels may indicate inflammation Normal levels are between 10 and 26 IU/L.
Gamma-Glutamyl Transpeptidase (GGT) is an enzyme in the liver, pancreas, and kidneys. Elevated levels may indicate inflammation and liver disease, usually due to alcoholism and/or sluggish gallbladder or gallstone obstruction. Normal levels are between 10 and 26 IU/L. Levels lower than 10 IU/L can be an indication of a vitamin B6 deficiency.
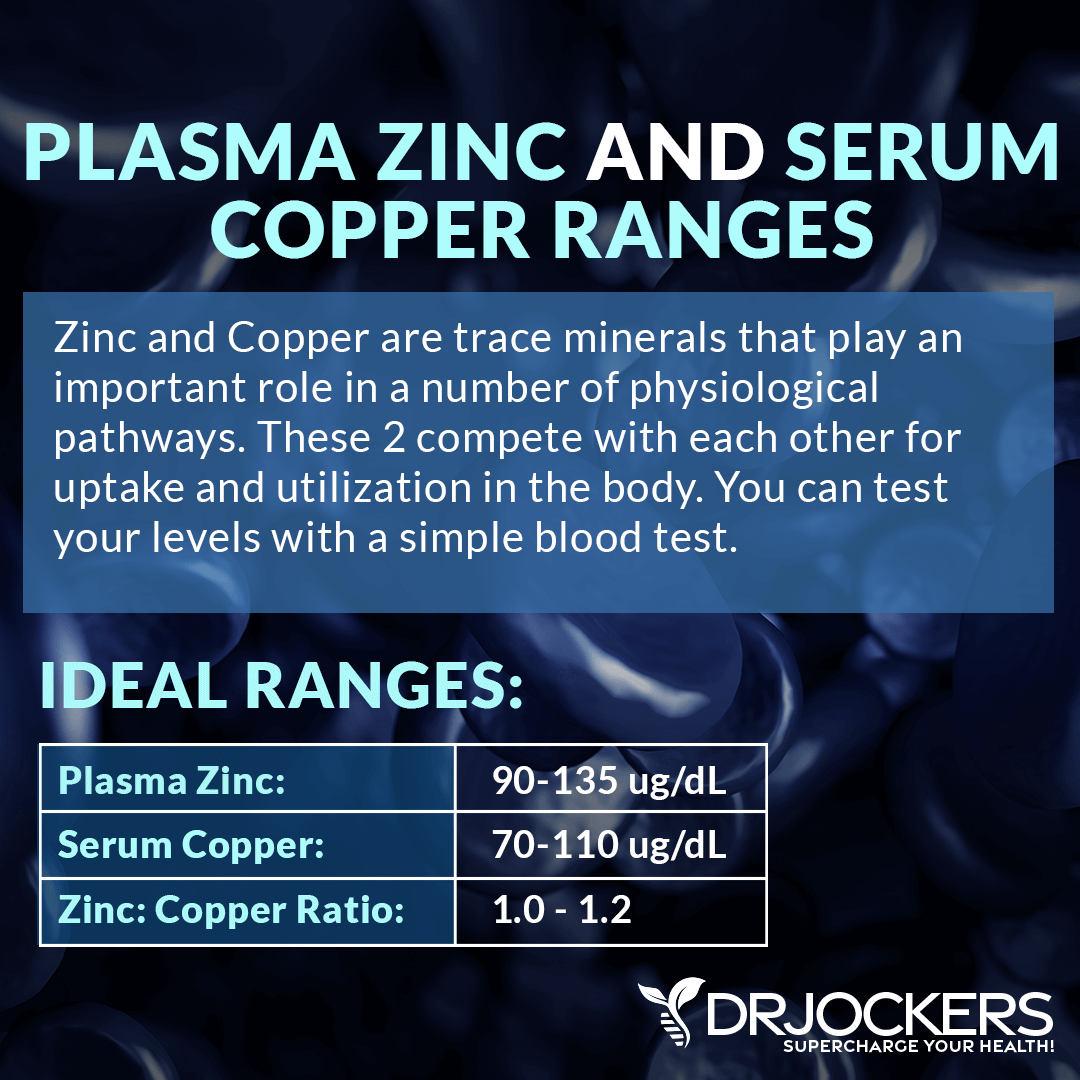
Zinc and Copper Levels
Zinc and copper compete against each other as antagonists to regulate physiological pathways. A proper balance between the two is essential for maintaining good health.
I recommend checking your plasma zinc and serum copper levels and their balance. The proper range for plasma zinc is 90-135µg/dL, and the serum copper should be 70-110 ug/dL. The proper plasma zinc:serum copper ratio should be between 1 and 1.2.
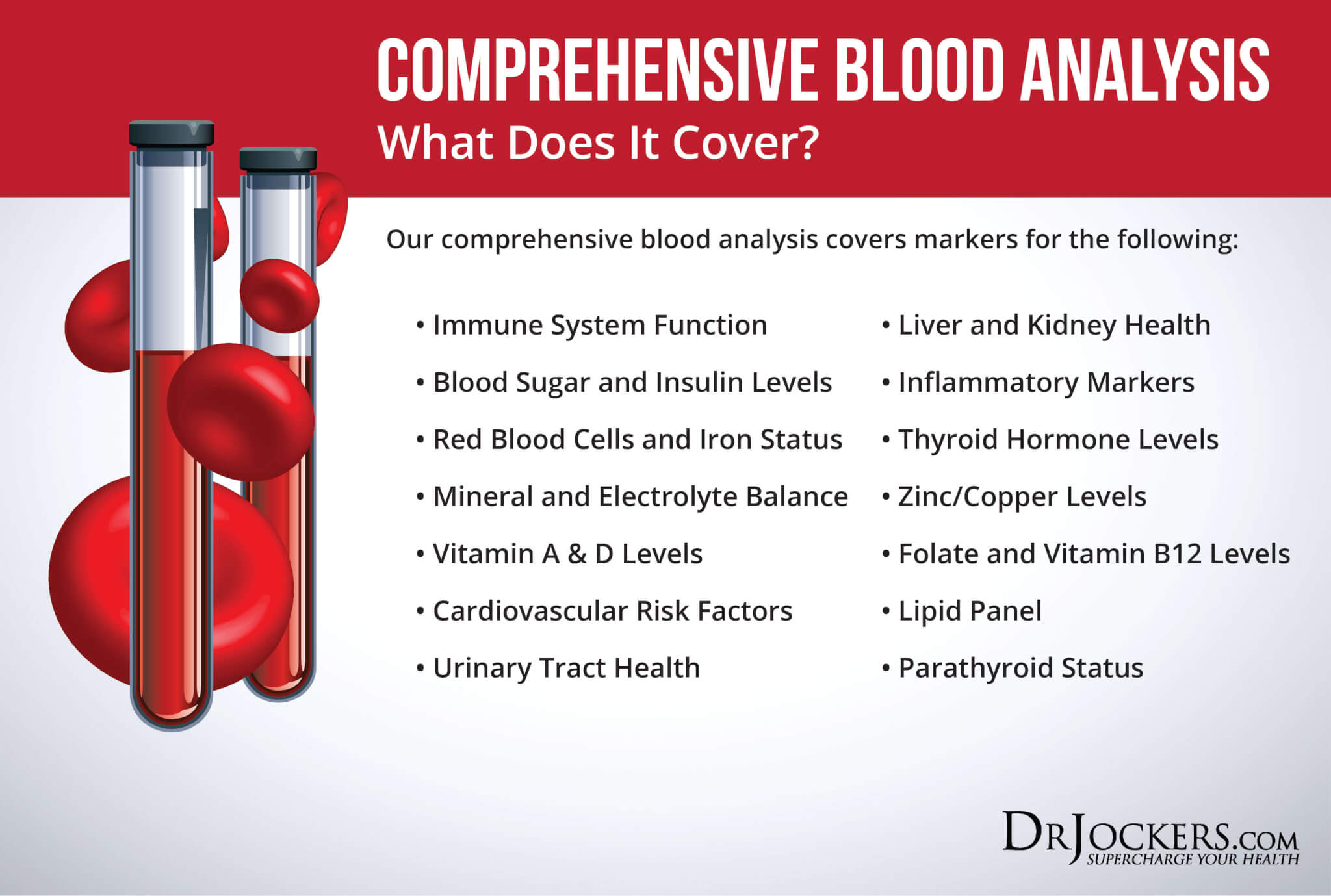
Complete Blood Analysis
To check for these lab markers, I recommend a Comprehensive Blood Analysis (CBA). This is the most detailed blood test I could find that looks at all of these markers of inflammation. This test is more sophisticated than most conventional doctors are able to order.
It examines all parameters for inflammation, blood sugar levels, thyroid function, zinc and copper ratio, vitamin B and D levels, a complete metabolic panel, complete blood count, liver function, nutrient deficiencies, and more. I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your inflammation levels and progress.
Natural Support Strategies
There are a number of natural ways that you can support your health, reduce your risks, and improve your symptoms. Here are the top natural support strategies I recommend for neuropathy.
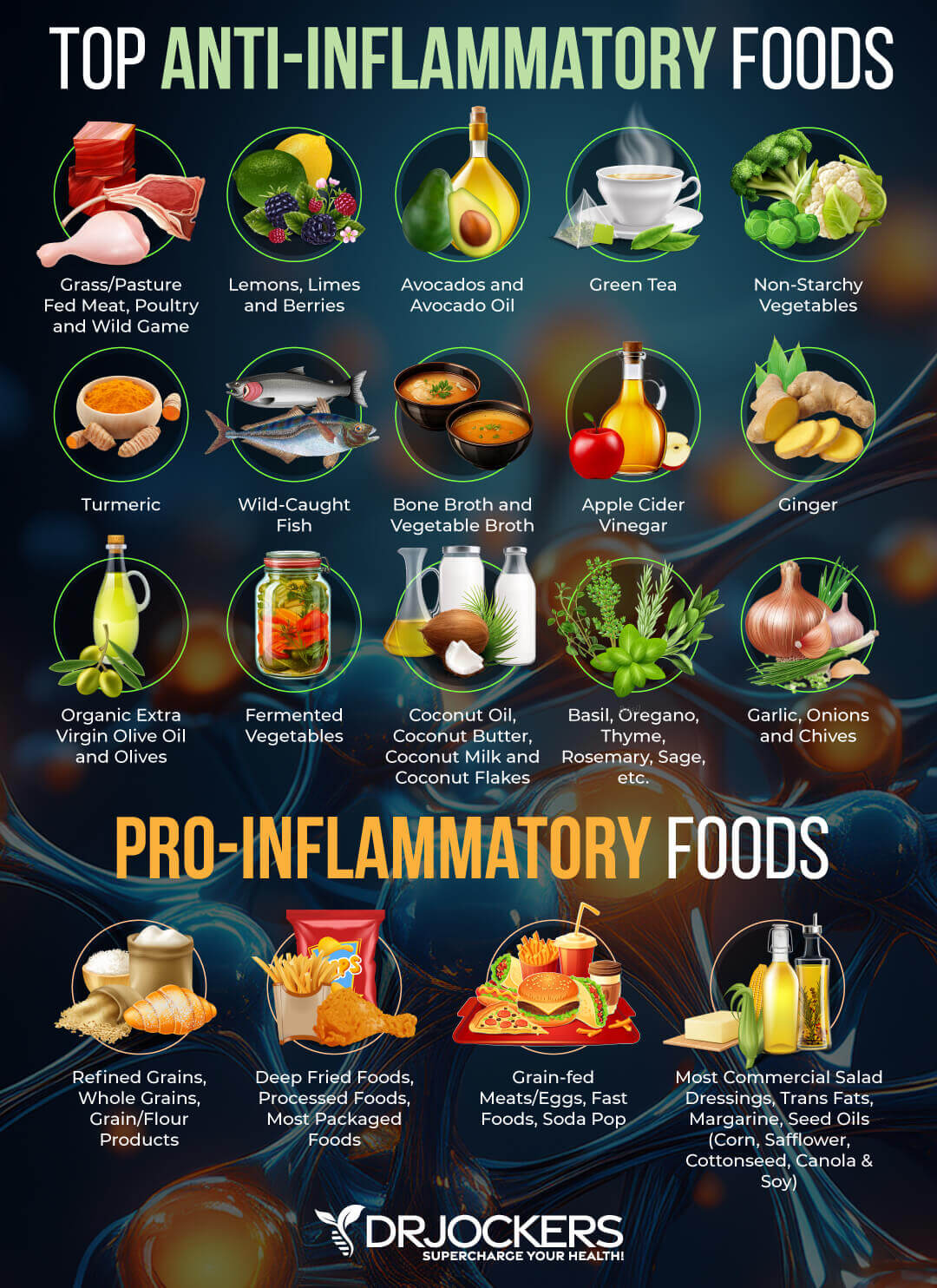
Anti-Inflammatory Nutrition Plan
A 2016 randomized clinical trial published in the Journal of Neuroinflammation has found that targeting inflammation may help neuropathic pain (22). Following an anti-inflammatory nutrition plan is one of the best ways to reduce inflammation in your body. According to The Foundation of Peripheral Neuropathy, eating a nutrient-dense diet rich in vegetables, fruits, and lean protein can help to improve peripheral neuropathy (23).
They also recommend reducing alcohol and removing foods that may trigger neuropathic pain. White, wheat, cake, and baking flour, refined grains, added sugar, and in some, saturated fats can increase symptoms of neuropathy.
I recommend that you remove all inflammatory foods from your diet, including refined sugar, refined oils, conventional dairy, conventionally raised and processed animal products, gluten, artificial ingredients, highly processed foods, deep-fried foods, junk food, food allergens, food sensitivities, and anything that’s triggering your symptoms.
Follow an anti-inflammatory nutrition plan rich in greens, vegetables, herbs, spices, fermented foods, low glycemic index fruits, healthy fats, such as coconut oil, MCT oil, organic grass-fed butter or ghee, avocadoes, nuts, and seeds, and clean animal protein, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
Foods rich in omega-3 fatty acids, such as algae, wild-caught fish and seafood, chia seeds, hemp seeds, and flax seeds, and anti-inflammatory herbs, such as turmeric and ginger may help to lower inflammation.
Resveratrol-rich foods, such as grapes, berries, and pistachio, and quercetin-rich foods, such as berries, cherries, black plums, black currants, cruciferous vegetables, raw kale, romaine lettuce, red leaf lettuce, snap peas, cabbage, sprouts, raw red onion, peppers, and raw asparagus may also help to lower inflammation in your body.
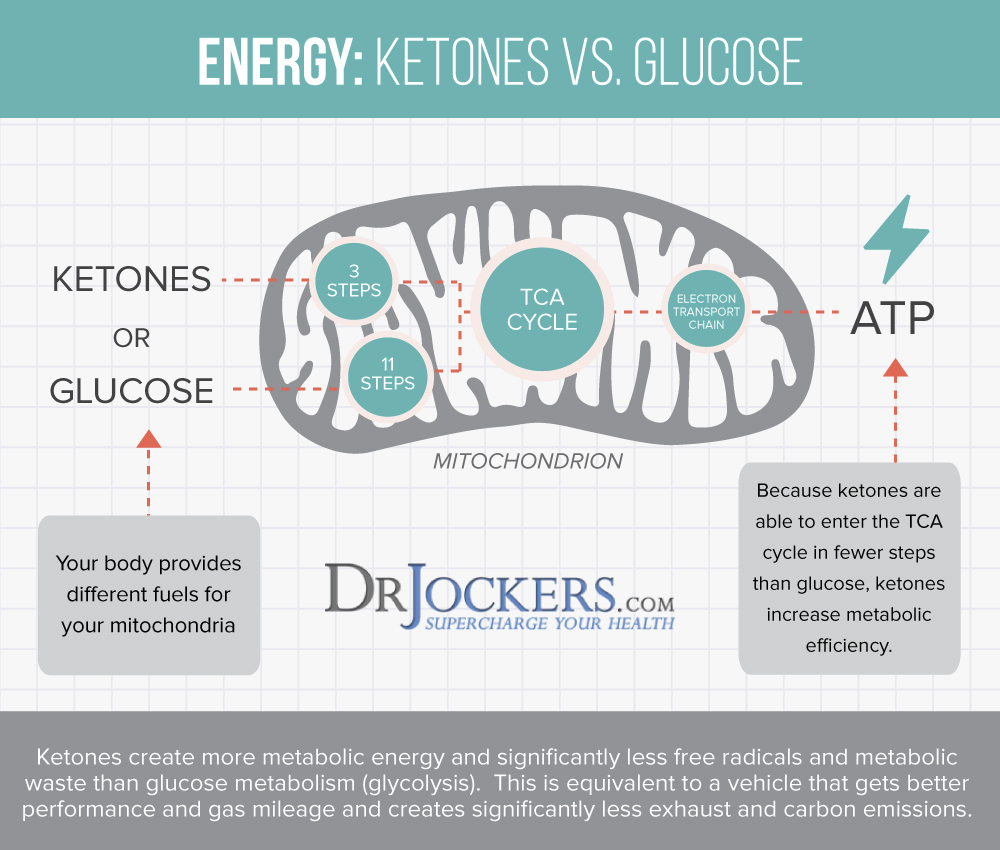
Consider Getting into Ketosis
Insulin resistance and diabetes are some of the number one causes of peripheral neuropathy (3, 4, 5, 6). Balancing your blood sugar levels and increasing insulin sensitivity is critical for reducing your risks and symptoms of neuropathy (23).
Following a ketogenic diet and getting into ketosis is one of the best ways to do this. A 2010 study published in Endocrinology has found that a ketogenic diet can improve insulin sensitivity and glucose tolerance (24).
Usually, your body burns glucose for energy. When your body doesn’t have enough dietary glucose to burn for energy as a result of carbohydrate restriction, caloric restriction, or fasting, it will turn to fat for energy instead and starts to make ketones in the process. Ketosis has many health benefits, from reduced inflammation, increased insulin sensitivity, improved cellular renewal to a decreased risk of disease.
Beyond improving insulin sensitivity and reducing the risk of diabetes, getting into ketosis may help neuropathy in other ways and help other forms of neuropathy besides diabetic peripheral neuropathy. A 2017 review published in Nutritional Neuroscience has found that a ketogenic diet may help to manage Leber hereditary optic neuropathy (25).
A 2021 study published in Science Reports has found that a ketogenic diet can help to reduce inflammation and improve inflammation-related conditions, including diabetic neuropathy and chemotherapeutic neuropathy (26). It may also improve rheumatoid arthritis, an autoimmune condition that may trigger autoimmune neuropathy (1, 26).
To follow the ketogenic diet, keep your carbohydrate levels very low at 5 to 10 percent, your protein levels moderate at 30 to 35 percent, and your fats high at 55 to 60 percent of your calories. Make sure to eat an anti-inflammatory real food keto diet with nutrient-dense whole foods, as I described earlier, instead of only focusing on your macronutrient ratios through fatty junk food.
Most of your diet should be abundant in healthy fats, including avocados, coconut oil, coconut butter, coconuts, avocado oil, extra-virgin olive oil, pasture-raised butter and ghee, lard, flax seeds, hemp seeds, chia seeds, pumpkin seeds, other seeds, olives, nuts, and any fats from clean animal foods, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
Optimize B Vitamin Levels
Research suggests that a deficiency in vitamin B1 and B12, and a deficiency or excess in vitamin B6 can result in neuropathy (7, 8, 9, 20). Optimizing your B vitamin levels is critical. If you’ve been following me, I don’t recommend following a vegan or vegetarian diet for a variety of reasons. One of the reasons is an increased risk of deficiency in vitamin B12.
Other than eating a diet that included high-quality animal-based foods, you need to be intentional to meet your B vitamin needs. I recommend that you eat foods that are rich in B vitamins on a regular basis. These foods include grass-fed meat, pasture-raised eggs, grass-fed or fermented raw dairy if you can tolerate it, dark leafy greens, sunflower seeds, almonds, avocados, and citrus.
I also recommend that you supplement with vitamin B12 and a high-quality B complex vitamin daily. Make sure that you are using a methylated form of B vitamin supplement to ensure proper absorption. Choosing a liquid form of vitamin may also help absorption.

Chiropractic Care and Physical Therapy
Nerve pressure for spinal subluxation, scoliosis, sciatica, poor posture, and injuries can cause neuropathy (1). Chiropractic care and physical therapy can help to relieve nerve pressure and possibly correct underlying structural issues.
Chiropractic care can help to correct spinal subluxations, scoliosis, and poor posture, and help to improve sciatica, injuries, disc issues, and other structural problems. A 2020 study published in Diabetes, Metabolic Syndrome, and Obesity: Targets and Therapy has found that physical therapy and exercise therapy may help to improve diabetic neuropathy (27).
Decompression therapy uses traction to stretch your spine, release tension between your vertebrates, increase the flow of oxygen, and reduce pain. It is often used for neuropathy and disc injuries and may be paired with Active Release Technique or cold laser therapy. A 2018 study published in Diabetes, Metabolic Syndrome, and Obesity: Targets and Therapy has found that decompression therapy may help diabetic neuropathy (28).
Transcutaneous electrical nerve stimulation (TENS) is a battery-operated device using electrical stimulation that’s used to relieve pain related to back pain, neck pain, joint pain, injuries, painful diabetic neuropathy, and other pain issues. A 2017 study published in Cochrane Database of Systematic Reviews has found that the TENS unit may help to relieve pain related to diabetic neuropathy (29).
Optimize Copper/Zinc Ratio
Research suggests that copper deficiencies may increase the risk of neuropathy (20). Besides copper, zinc is also important. A 2014 study published in Biological Trace Element Research has found that zinc supplementation may help diabetic peripheral neuropathy (30).
Zinc and copper compete against each other as antagonists to regulate physiological pathways. A healthy balance between these two minerals is critical for your health. I recommend checking your plasma zinc and serum copper levels and their balance. This should help you with a dietary and supplement strategy to improve your levels.
Your dietary choices can improve your copper/zinc ratio. Zinc-rich foods include grass-fed lean meat, pasture-raised poultry, nuts, seeds, oysters, peas, and chickpeas. Foods that are good sources of copper include oysters, leafy green, shitake mushrooms, liver, lobsters, nuts, and seeds. I also recommend that you take a high-quality zinc supplement. If you find that your copper levels are off, you can take a chelated copper supplement or a zinc supplement with copper to support a healthy copper/zinc ratio.
Optimize Vitamin D Levels
Research has shown that vitamin D deficiency can result in neuropathy (10, 11). Optimizing your vitamin D levels may help. A 2019 clinical trial has found that vitamin D supplementation can improve diabetic peripheral neuropathy (31). A 2020 systematic review has also found the same that supplementing with vitamin D can improve diabetic peripheral neuropathy (32).
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need to supplement to optimize their vitamin D levels. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
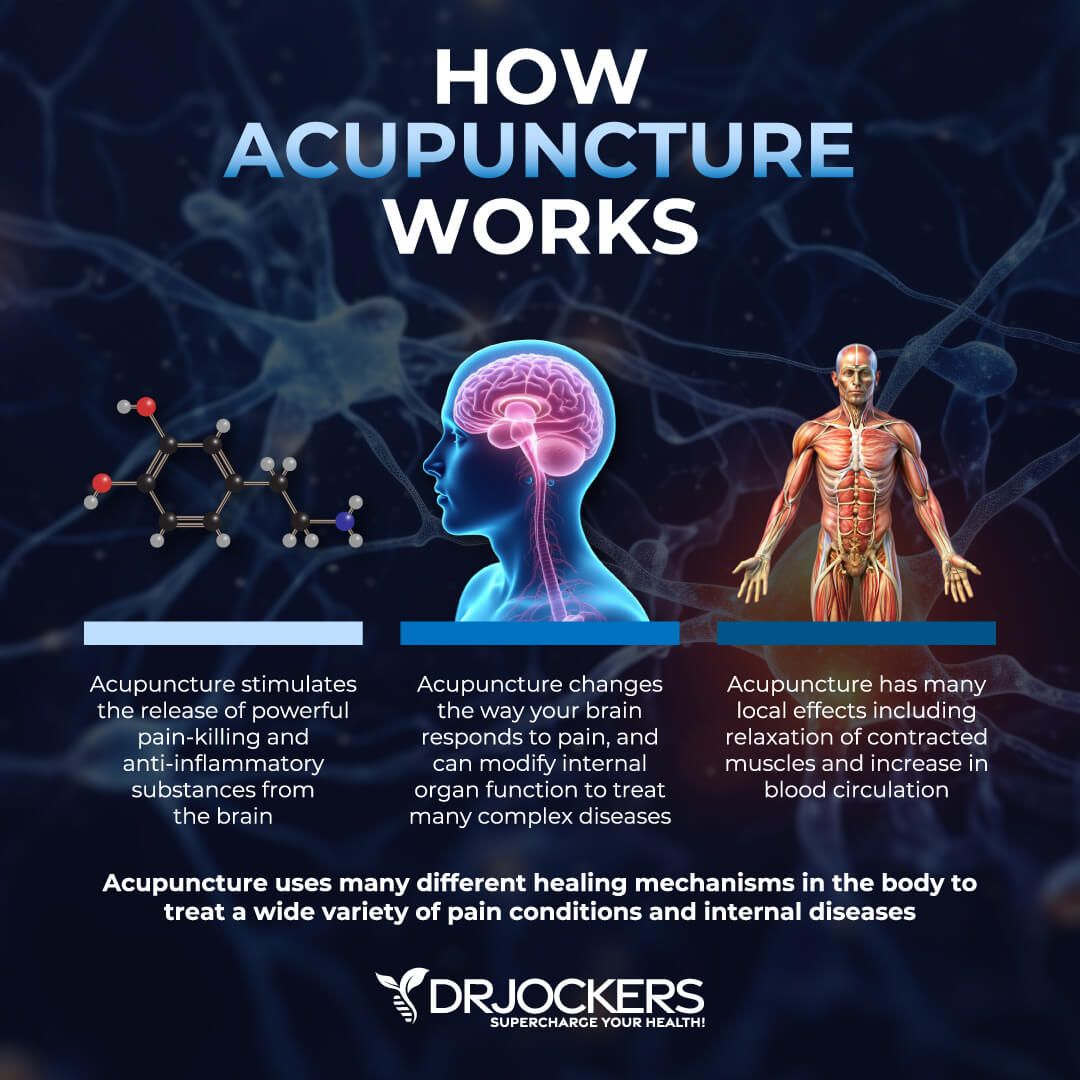
Consider Acupuncture
Acupuncture is a form of alternative medicine and an important part of traditional Chinese medicine. It uses thin needles placed strategically at certain points of your body to help recreate balance, improve blood flow, reduce symptoms, and improve your health.
According to a 2017 systematic review and meta-analysis published in the Journal of Alternative and Complementary Medicine, acupuncture helps with neuropathy (33). A 2019 systematic review published in Acupuncture Medicine has also found that acupuncture may help with diabetic peripheral neuropathy (34). If you have symptoms of neuropathy or experiencing any of its risk factors, I recommend that you visit an acupuncture practitioner.
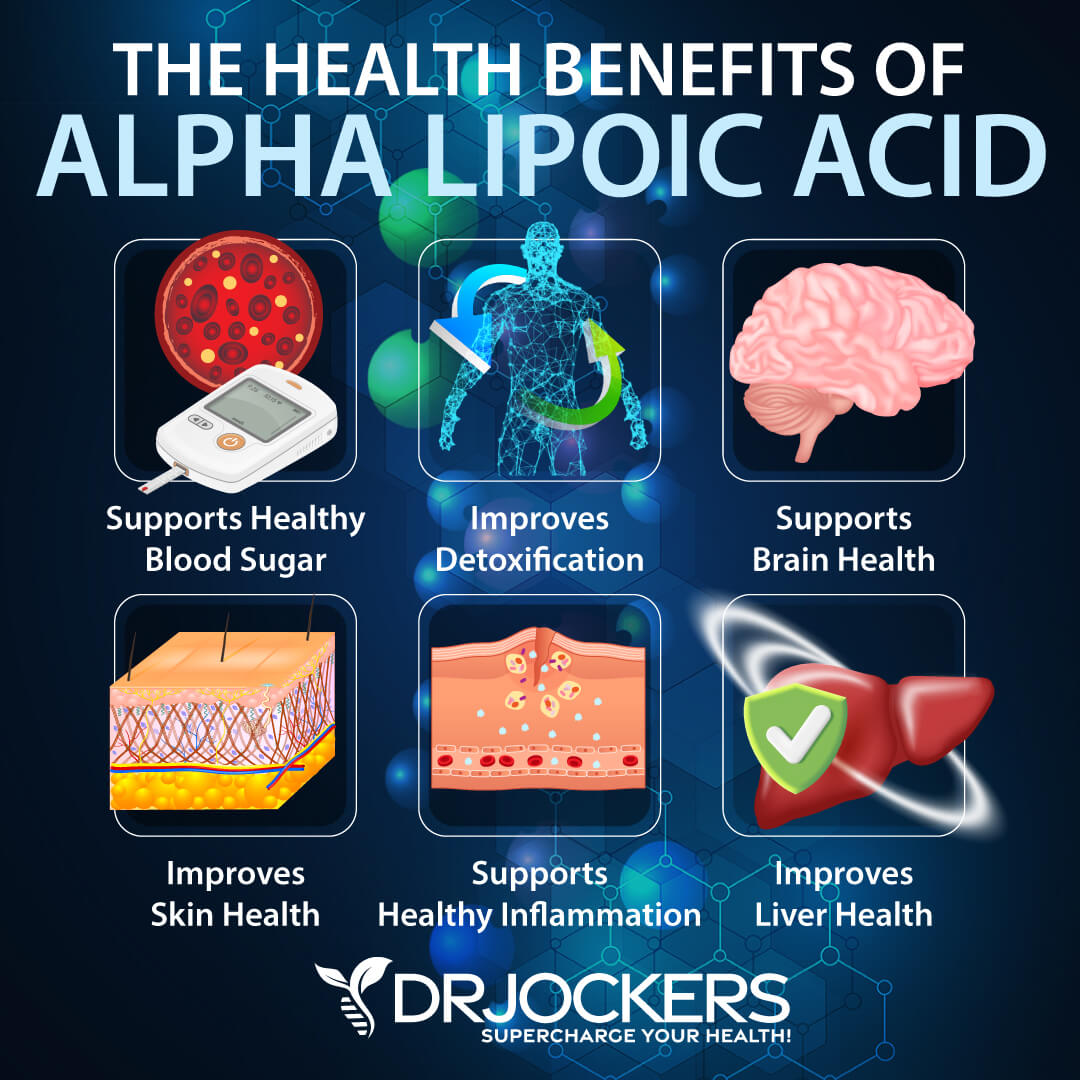
Consider Alpha-Lipoic Acid
Alpha-lipoic acid is a vitamin-like antioxidant that can offer a number of health benefits, including neuropathy. 2009 research published in The Review of Diabetic Studies has found that alpha-lipoic acid may support the treatment of diabetic neuropathy (35).
A 2004 clinical trial has also found that alpha-lipoic acid may help the treatment of autonomic diabetic neuropathy (36). If you have neuropathy, I recommend supplementing with alpha-lipoic acid.
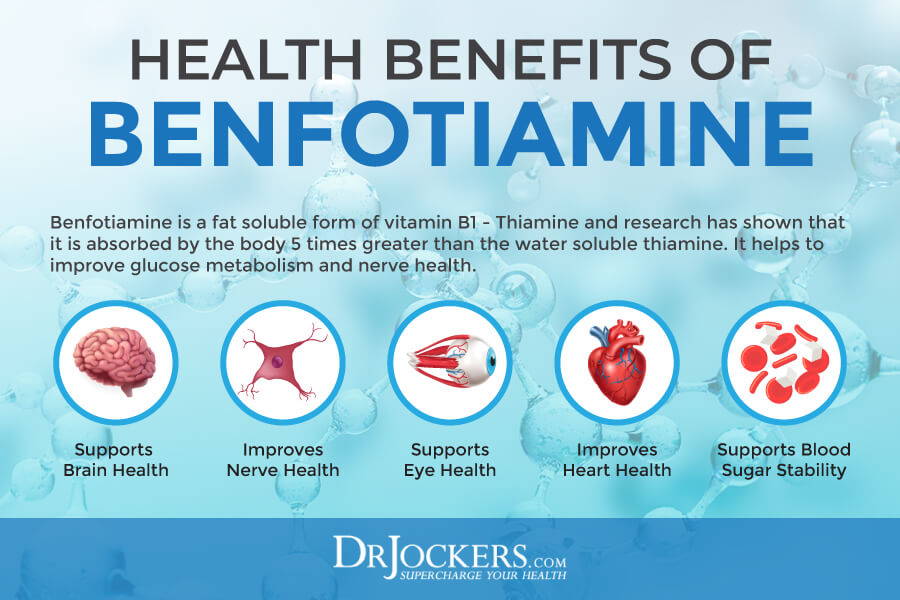
Consider Benfotiamine
Benfotiamine is a dietary supplement. It is derived from vitamin B1 and is also found in certain foods, including nuts, seeds, legumes, rice, and certain meat and fish. It is often used for nerve pain related to diabetes.
A 2005 clinical randomized, controlled pilot study published in the International Journal of Clinical Pharmacology and Therapy has found that benfotiamine helped to improve diabetic polyneuropathy after 3 weeks only (37). A 2006 study published in the European Journal of Pharmacology has also found that it can help to reduce inflammation and neuropathic pain (38). If you are experiencing neuropathic pain, I recommend benfotiamine supplementation.
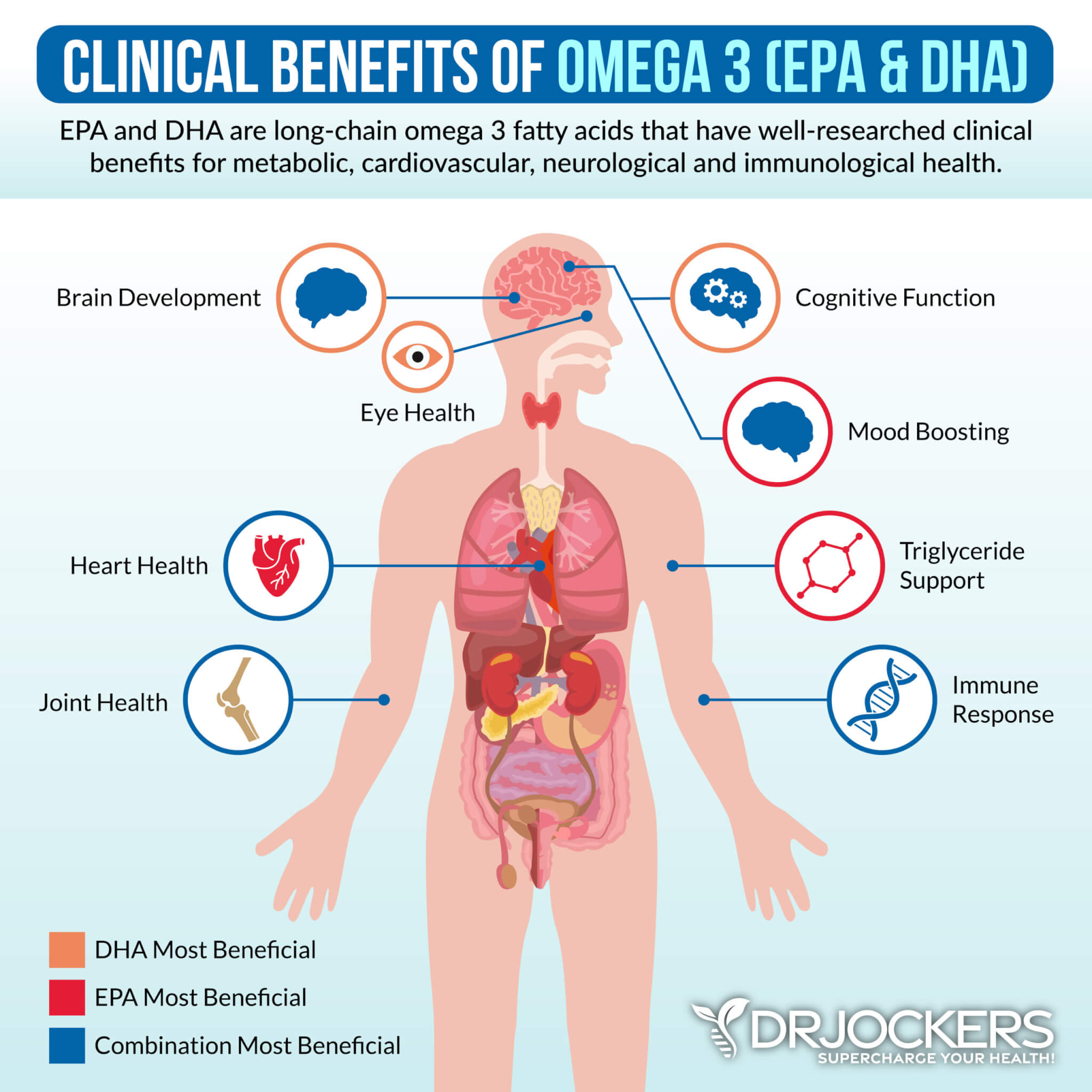
Consider Omega-3 Fatty Acids
Omega-3 fatty acids are fatty acids with anti-inflammatory benefits that may benefit those with neuropathic pain and symptoms. A 2019 study published in Diabetes, Metabolic Syndrome, and Obesity: Targets and Therapy has found that omega-3 supplementation may help to reduce symptoms of neuropathy in participants with type 2 diabetes (39).
I recommend consuming foods rich in omega-3 fatty acids, such as algae, wild-caught fish and seafood, chia seeds, hemp seeds, and flax seeds. Additionally, I recommend taking a high-quality omega-3 fish oil supplement daily.
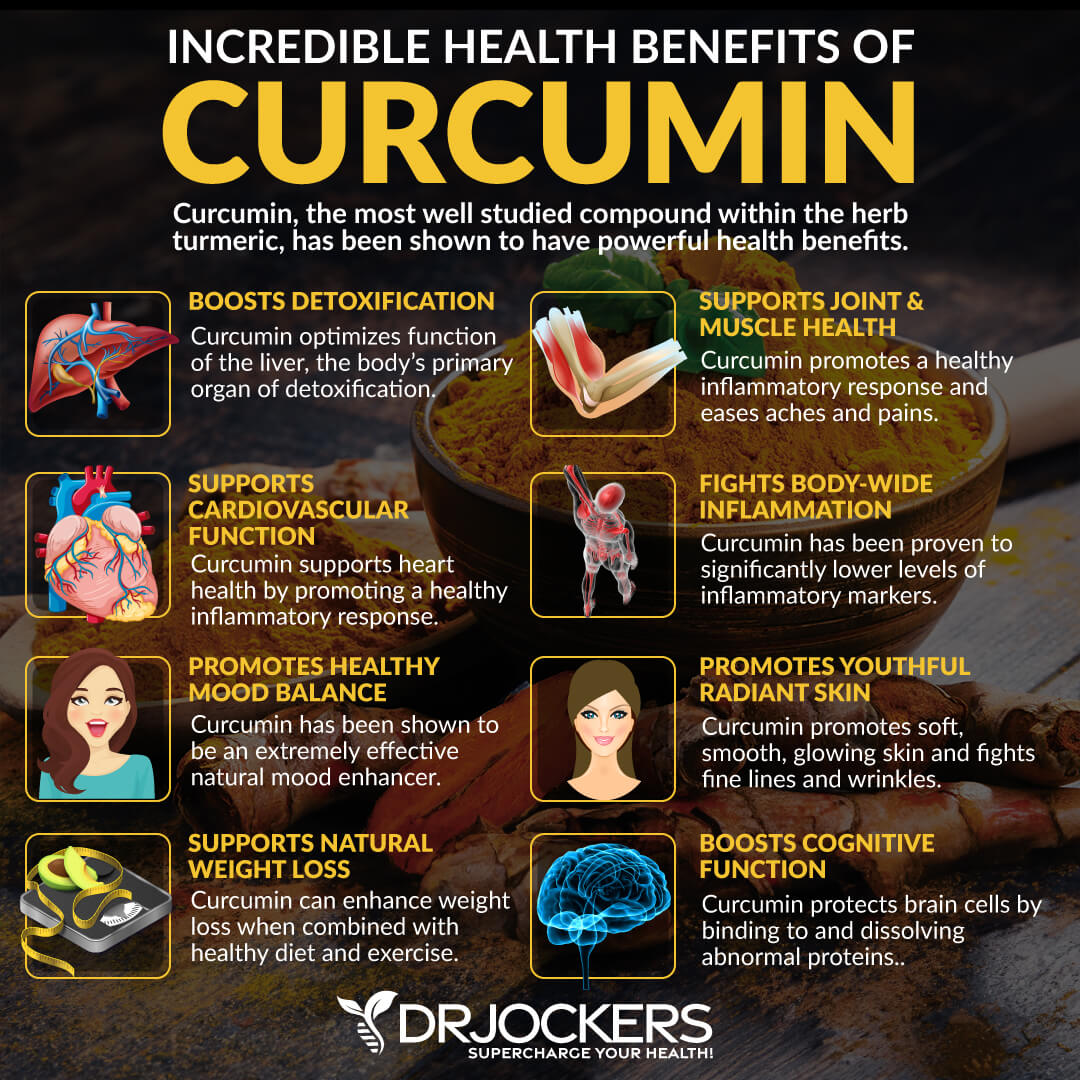
Consider Using Turmeric – Curcumin
Curcumin is the active compound of one of the most research anti-inflammatory herbs-turmeric. Due to its anti-inflammatory and pain-relieving benefits, curcumin may be a great option for neuropathy.
A 2014 study published in PLoS One has found that curcumin may help to reduce neuropathic pain (40). A 2020 study published in Antioxidants (Basel) has also found that curcumin may be a potential and effective therapeutic option for peripheral neuropathy (41). I recommend adding turmeric to your curries, soups, vegetable dishes, dressings, sauces, juices, and smoothies. I also recommend daily supplementation with a high-quality curcumin supplement.
Final Thoughts
Neuropathy is a condition characterized by nerve damage. It can cause a number of symptoms, including numbness, tingling, prickling, muscle weakness, pain, muscle shrinking, and other issues. I recommend that you follow my natural support strategies to support your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. We do offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



I am a French neurologist and I totally agree with this article. Most neuropathies are unrelated to serious illnesses, and sometimes even all laboratory tests are negative. You have to be careful to consider the levels of vitamins B 12 and folate in the low range of normal values and at this time supplement anyway. For my part, I think that the consumption of dairy products is one of the main factors of neuropathies apart from serious diseases because it often disrupts the intestinal function and leads to malabsorption and deficiencies. These neuropathies are quite often associated with ductal syndromes such as carpal tunnel syndrome, which therefore does not always have to be operated on first; I have had patients who improved a lot when they stopped consuming milk and dairy products on carpal tunnel symptoms. Best regards.
Thanks for sharing Aranda. Yes, food sensitivities and allergies can be significant triggers of neural inflammation.
Could you please consider the value of adding information about the impact of ceramides, as well as genetics behind the metabolic form of neuropathy?
I am particularly interested in foods (dairy, nuts, grains, etc) that are high in ceramides, and genes within the Serine Palmitoyltransferase Complex that are linked to the processing of ceramides, acid ceramidase enzymes and fatty acids/sphingolipids and how they might contribute to progressive neuropathies.
Thank you!