 Visceral Fat: What is It and How it Drives Up Inflammation
Visceral Fat: What is It and How it Drives Up Inflammation
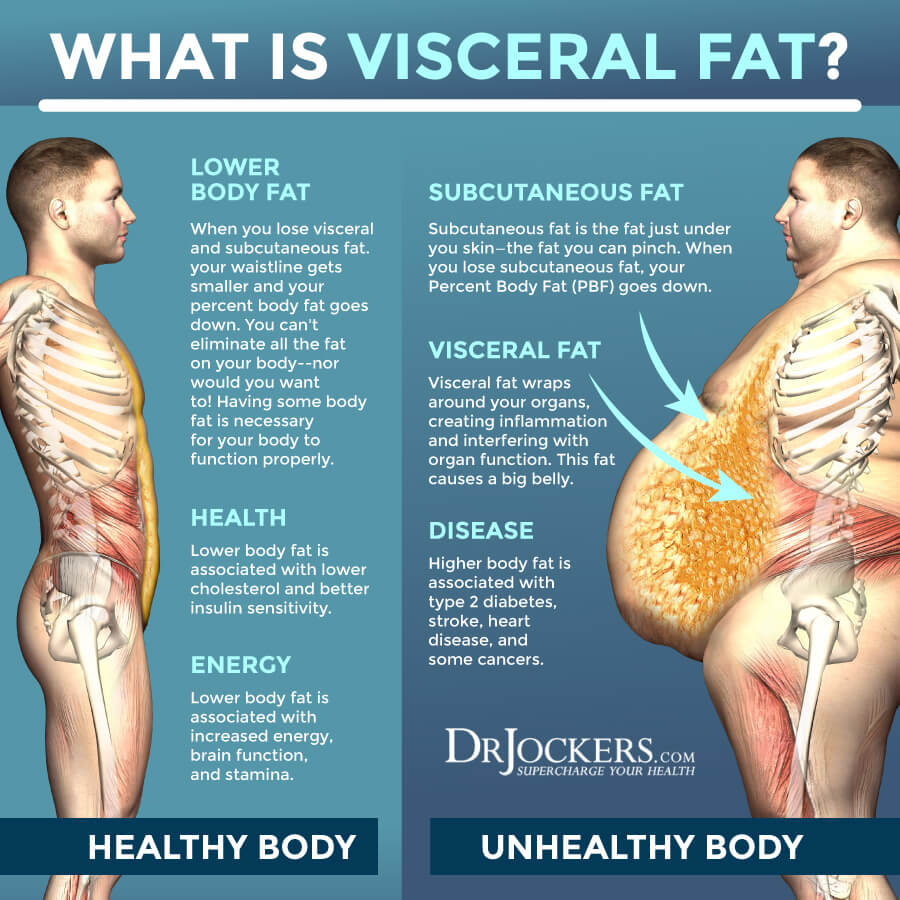
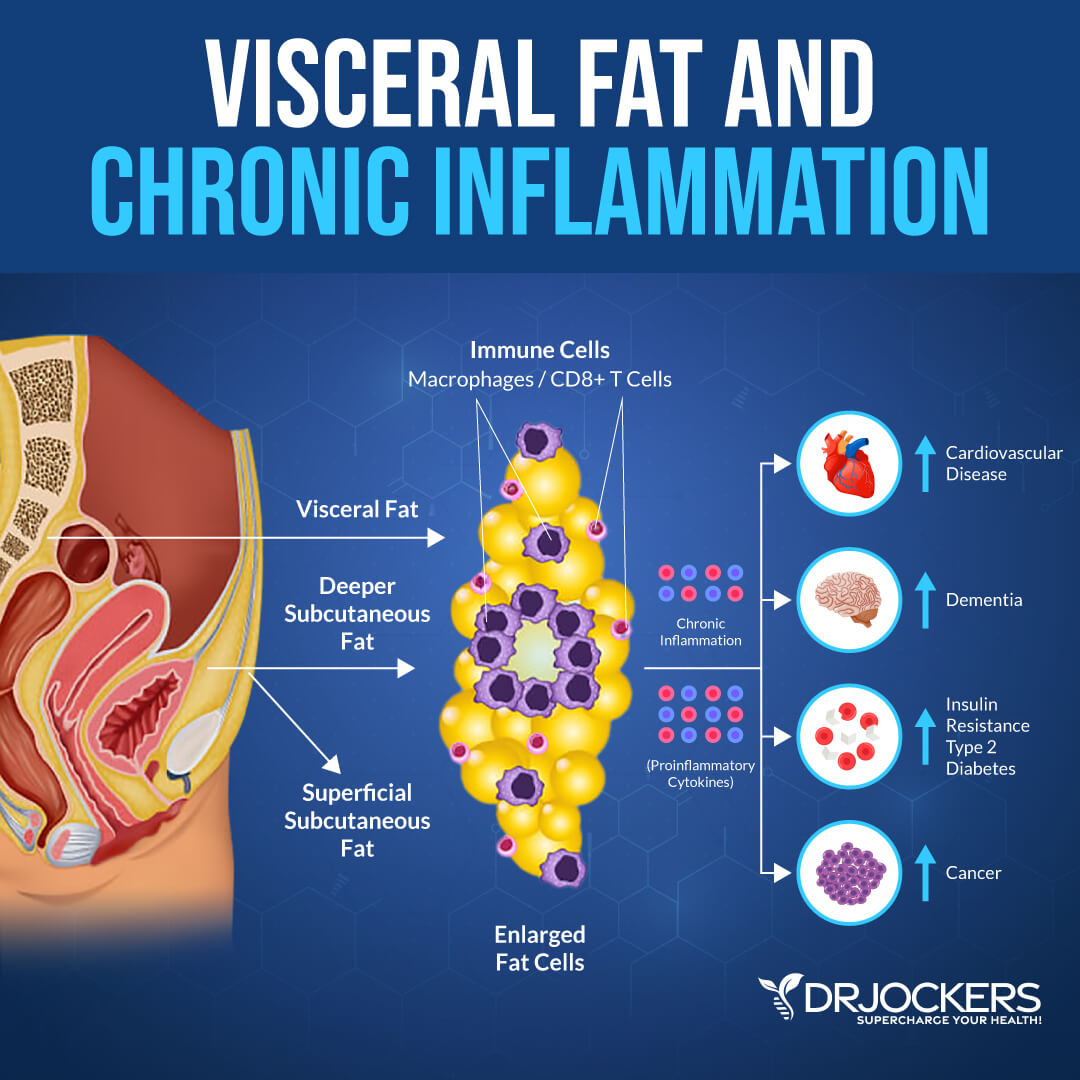
Visceral fat is a fat that accumulates in your abdomen. Visceral fat is not the fat that you can pinch on your belly, but the fat that wraps around your organs inside your abdomen, including your liver, kidneys, and pancreas. Excess visceral fat is a serious problem.
It is linked to obesity, chronic inflammation, insulin resistance, increased risk of heart disease, increased risk of cancer, estrogen dominance, mood imbalances, and increased risk of dementia. Since it’s an underlying root cause of many chronic health issues, it is important that you understand everything about it.
In this article, we are going to do a deep dive into fat cell physiology and the immune and endocrine components of fat cells. You will understand what visceral fat is. I will explain how visceral fat develops. You will learn about the difference between hypertrophic and hyperplastic fat cell growth.
You will understand how visceral fat sends out immune signals and what’s the problem with that. You will learn about ceramide formation and its connection to visceral fat. You will learn how to measure your visceral fat levels at home. I will recommend some lab analysis to check for inflammation and your risk factor for health issues. You will also learn about 7 problems with excess visceral fat.
What Is Visceral Fat
Visceral fat is a type of fat that accumulates in your intra-abdominal adipose tissue. It is not the belly fat you can pinch. Subcutaneous fat is the belly fat that you can see and touch around your middle. Visceral fat, on the other hand, is a gel-like fat that wraps around and in-between your organs inside your abdomen. It may be found around your liver, pancreas, and kidneys.
A large waist and a protruding belly are signs of having too much visceral fat. According to a 2016 study published in Nature Communications, visceral fat is a much more serious problem than subcutaneous fat (1).
Too much visceral fat can interfere with organ function and how your body operates. Visceral fat can trigger your body’s inflammatory pathways and increase inflammation (1). It can interfere with signaling between molecules and normal hormonal functions. As a result, it may interfere with your hunger levels, weight, brain function, and other areas of your health.
Visceral fat can increase the risk of an array of health issues, including:
- Obesity
- Coronary heart disease
- Stroke
- Diabetes
- Cancer
- Dementia
- Arthritis
- Sleep disorders
- Sexual dysfunction
- Depression
- Hormonal health issues
How Visceral Fat Develops
A lean belly is not only about vanity. It is a critical indicator of your health. Your body is a well-refined system of chemicals that let you know when you should eat and when you should stop eating because you are full. In a healthy body, there is clear communication between your brain and your other major organs. Together they help you stay healthy and keep visceral fat low. However, certain factors can make you more susceptible to visceral fat storage and weight gain.
When it comes to a healthy weight, appetite, and mood, your blood glucose (or blood sugar) levels are critical. Your blood glucose levels are controlled by a hormone called insulin. Insulin helps to decrease your blood sugar levels after eating a sugary or high-carbohydrate meal.
When your body is digesting your food, it breaks down sugar and starches into smaller units, glucose or fructose. Glucose and fructose can then enter your bloodstream. This urges your pancreas to release insulin to help move blood sugar into your cells across your body. Blood sugar is then stored and used for energy to support brain, muscular, and tissue function.
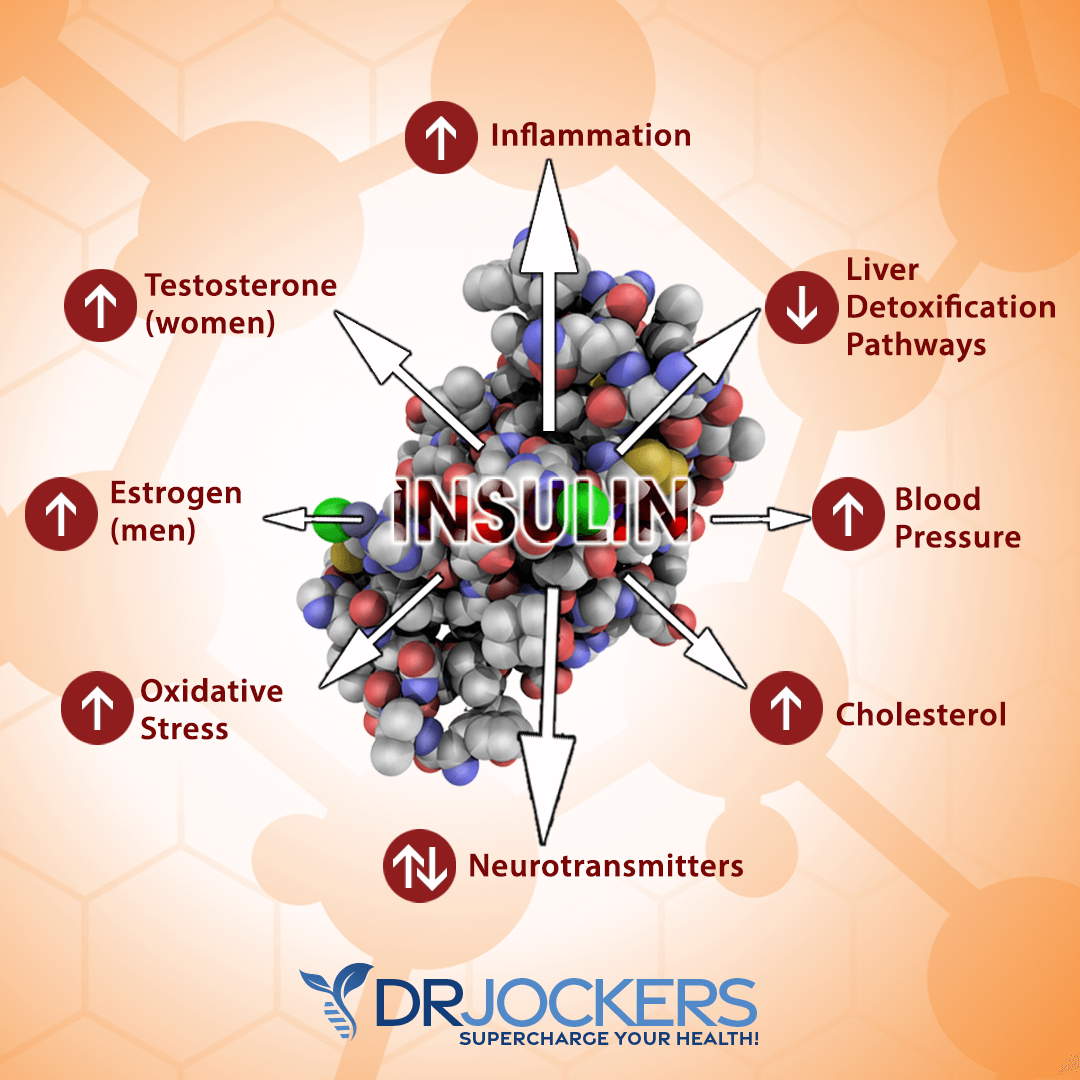
Insulin doesn’t only take care of your blood glucose, though. It is in communication with your body’s fat store, including your visceral fat. No wonder that some people call insulin the “fat-storage hormone”.
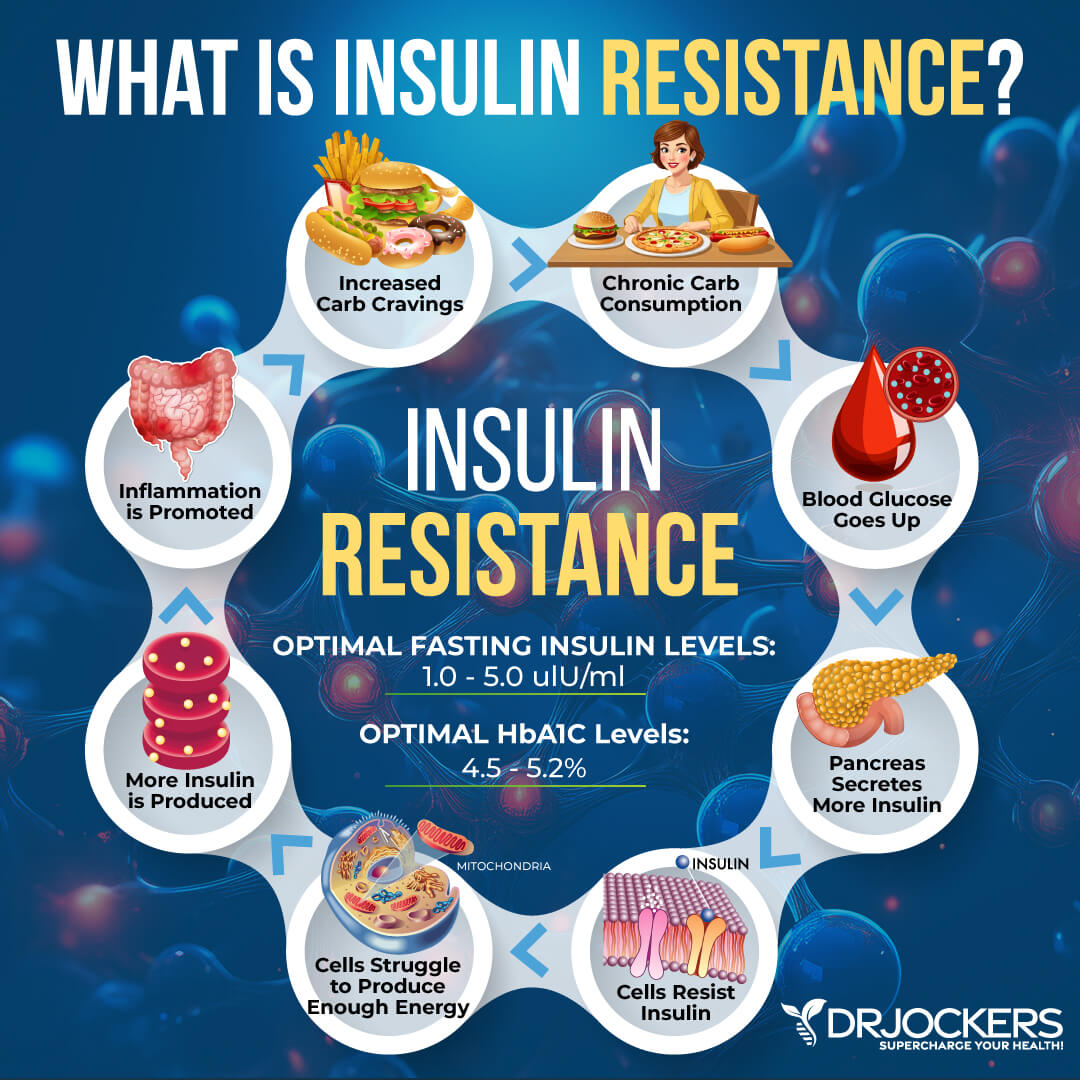
If there is too much blood glucose in your system, your body will store this excess glucose as fat. This usually happens if you are eating too much refined processed carbs and sugary foods, including white bread, white pasta, white rice, cakes, or candy.
These high-sugar, low-nutrient foods get quickly converted into simple sugars. They enter your bloodstream right away and cause a rapid release of insulin. This can not only lead to excess visceral fat and weight gain, but can also feed the vicious cycle of hunger, overeating, sweet cravings, and the inability to resist carbs.
The problem is that the longer this cycle continues and the longer your blood insulin levels stay high, the more likely you will gain excess visceral fat and the more likely you will battle with ongoing weight problems.
Insulin is also in constant touch with your other hormones, including your stress hormone cortisol made by your adrenal glands. Adrenal health issues, abnormally high cortisol, and other hormonal imbalances can lead to low energy, mood fluctuations, cravings, urges to eat, weight gain, inflammation, and an increased risk of chronic disease.

Hypertrophic vs Hyperplastic Fat Cell Growth
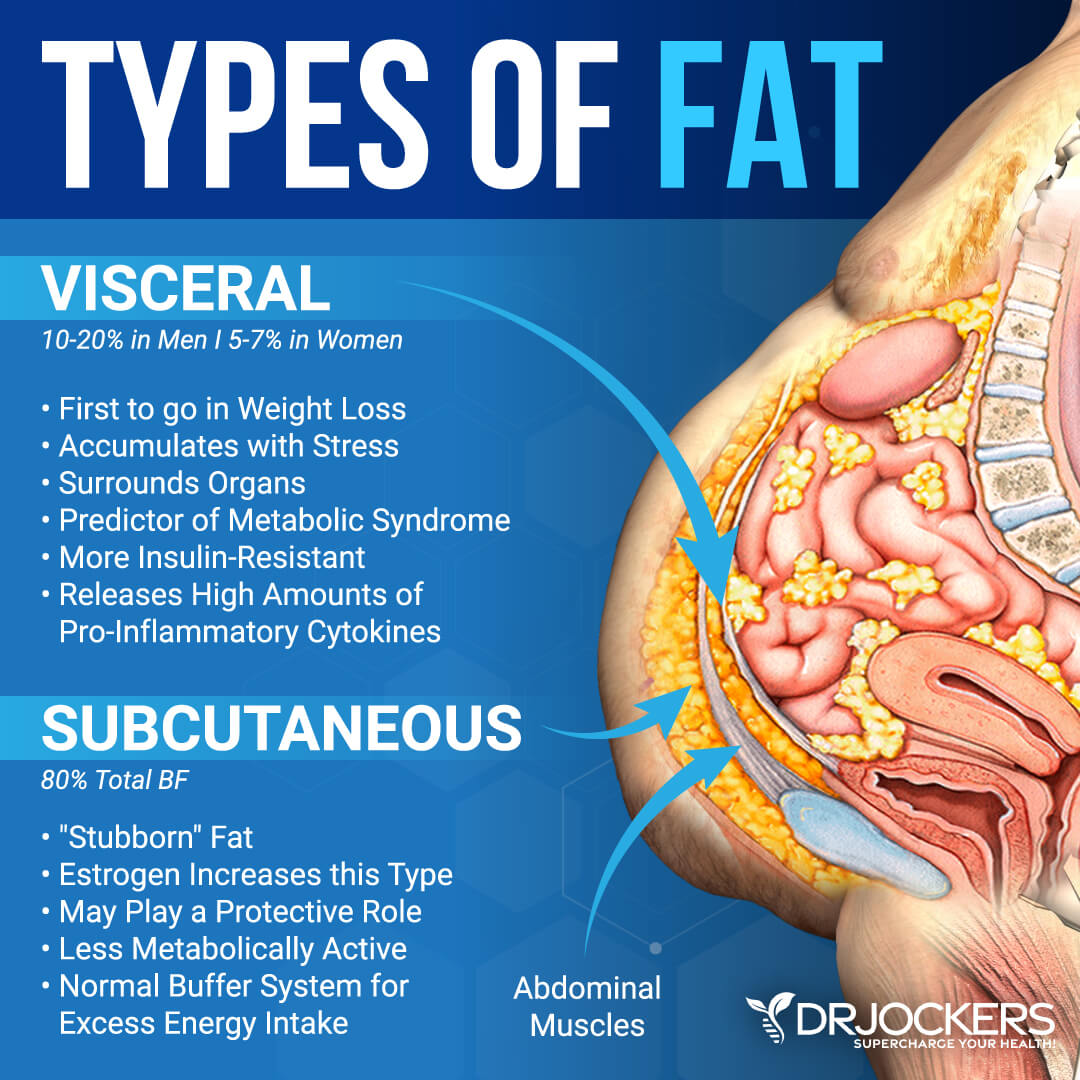
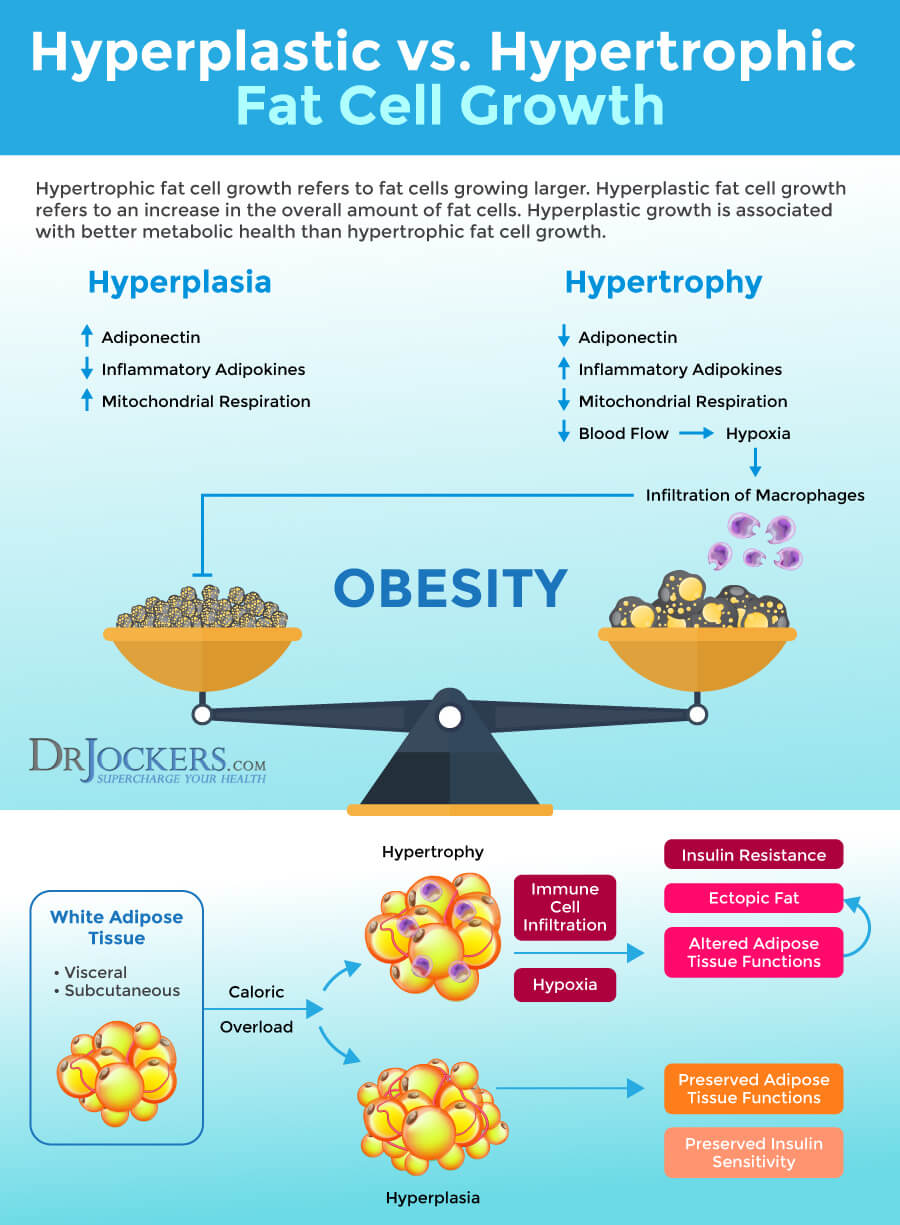
Obesity is characterized by excess fat and an enlargement of your adipose tissue to store excess that wasn’t used for energy. Your adipose tissue is a connective tissue consisting of lipid-rich cells. There are two possible growth mechanisms that can lead to this enlargement and fat cell growth: hyperplasia and hypertrophy. Hyperplasia means an increase in cell number and hypertrophy refers to an increase in cell size (2).
Hypertrophic and hyperplastic fat cell growth are not the same. They affect your body differently. With hypertrophic fat cell growth, your fat cells get too big. As a result, when they communicate with insulin they send the message that they are no longer able to store fat as insulin wants them to do. They will start breaking down triglycerides through lipolysis.
Lipolysis is the breakdown of fats and lipids to release fatty acids. Insulin will have no choice but to continue to force-feed the fat cells with fat. But your fat cells are already too big and unable to handle more fat without hurting your body or dying. Since the hypertrophic fat cells are unable to handle all the fat anymore, they will start leaking out free fatty acids through lipolysis. This increases the likelihood of these fats being stored elsewhere and increasing the risk of obesity and health issues.
These hypertrophic fat cells are also too big and not receiving enough space and support from the body. As a result, in addition to the release of fatty acids, hypertrophic fat cells also end up releasing pro-inflammatory cytokines to your body to trigger vascular growth. Hypertrophic fat cells also trigger and increase insulin resistance. Hyperplasia, on the other hand, can decrease insulin resistance.
So how does your body decide to trigger hypertrophic or hyperplastic cell growth? According to a 2009 study published in PLoS Computational Biology, there are both genetic and dietary factors behind it (2). While genetics certainly plays a role and some people are more predisposed to hypertrophy, it turns out that a high-fat diet can trigger hyperplasia.
Visceral Fat Sends out Immune Signals
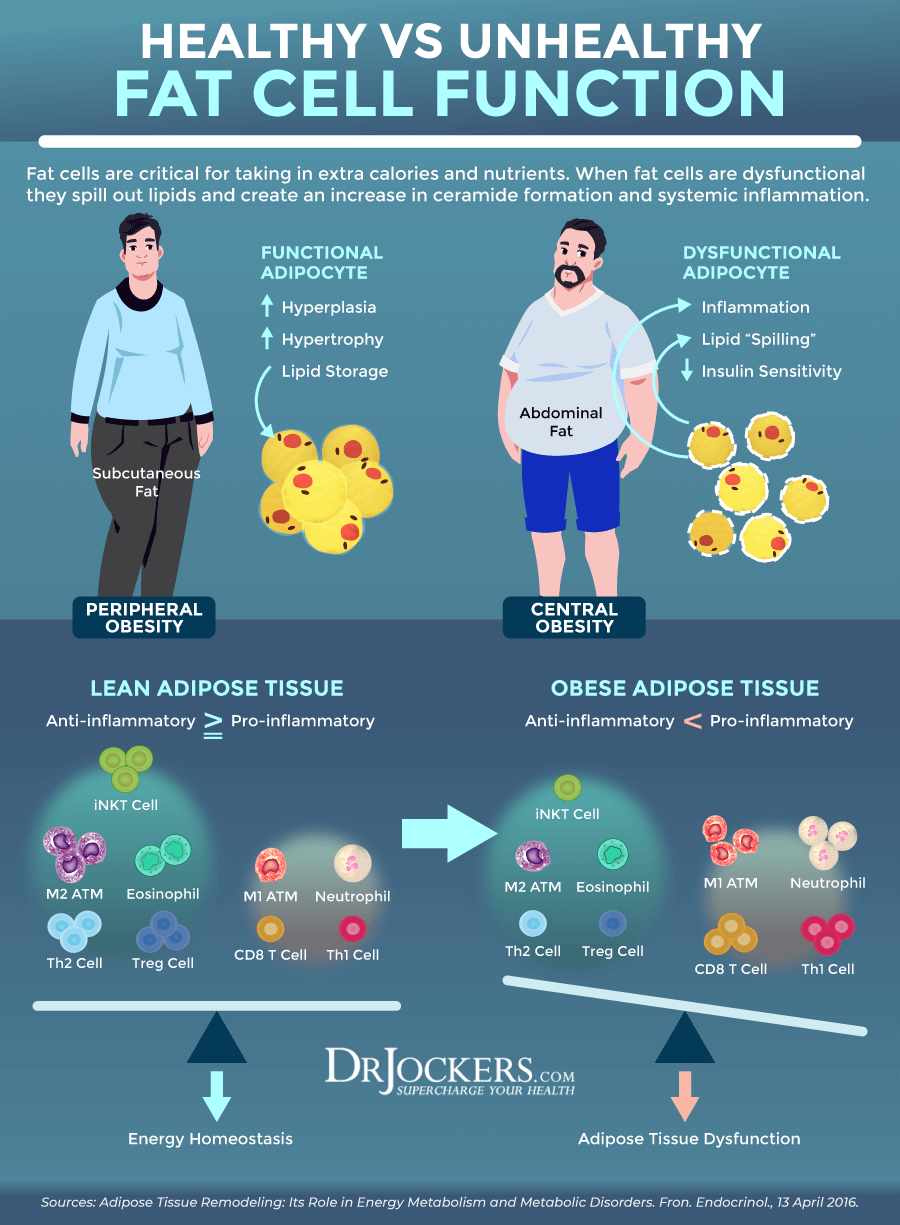
Excess fat in your fat cells is not a good thing. It leads to inflammation in the surrounding tissues and creates chronic, low-level inflammation, and increases inflammatory cytokine production in your entire body. This can increase your risk of obesity-related chronic diseases.
A recent 2020 animal study published in Nature Metabolism has found some linked between inflammation in the fat tissue and obesity (3). When you eat more calories than your body requires, your body will create triglycerides inside your fat tissue called white adipose tissue (WAT). If you are obese, your body has too many calories to deal with. Just like humans who have too many tasks on their plate at work, the WAT becomes overwhelmed and overworked by all this. As a result, your fat cells start dying, activating an immune response and creating inflammation.
Instead of studying the signaling molecules released by your fat or immune cells, this particular research looked at the vessels that carry your blood, inflammatory molecules, and immune cells into WAT. They discovered a new type of cell lining in these blood vessels, a type of adipose progenitor cell (APC) or precursor cell. APCs help to generate mature fat cells. Unlike other APCs, these particular cells release signals that trigger, encourage and mediate inflammation. They are fibro-inflammatory progenitors (FIPs).
Researchers found that just one day on an inflammatory diet leads to increased inflammatory molecule production by the FIPs in young male mice. 28 days on the inflammatory diet had to lead to a significant escalation in FIPs compared to other types of APCs. These are significant findings that show that these specific cells may play a significant role in inflammation in fat tissue.
To look at the role of FIPs, researchers removed Tlr4, the main immune signaling gene from FIPs, and looked at how mice without Tlr4 react to a five-month high-fat diet. They found that both mice with and without Tlr4 gained an equal amount of weight on a high-fat diet. However, mice without Tlr4 didn’t show high levels of inflammation. In fact, they had a similar level of inflammation in their WAT as mice fed on a low-fat diet. They also found that by increasing FZP423, signaling molecules, FIPS can benefit inflammation levels in fat cells of mice.
While these are only early findings on mice, results suggest potential ways to reduce the risk of disease in those with obesity. Looking at ZFP423 further is important as it may help to reduce inflammatory signals in these cells, thus may help to reduce chronic inflammation and obesity-related disease. More research is needed to better understand inflammatory signaling FIPs and potential dietary triggers in human fat.
Visceral Fat and Ceramide Formation
Ceramides are waxy lipid molecules that are found in the cell membrane of your eukaryotic cells, which are cells that contain membrane-bound organelles, including mitochondria, nucleus, and endoplasmic reticulum. Ceramides not only support structural elements in a cell membrane but also play an important role in various cellular signaling, including programmed cell death, cell differentiation, cell cycle, and senescence.
They play an important role in your nervous system function, brain health, skin health, and other areas of your health. They help adipocyte function to manage glucose and lipid metabolism.
A 2020 study published in Frontiers in Immunology has found that adipocyte ceramide formation plays a role in inflammation and metabolism (4). Adipose depots are areas where your adipose tissues are located.
They communicate with your organs regarding your body’s nutrition status by secreting cytokines, lipids, and adipokines or protein hormones. They also include immune cells that affect your body’s metabolic activity. They help to regulate the production of ceramides that affect both glucose and lipid metabolism in your body.
While ceramides play an important role, too much can be a problem. The study has found that an excess of ceramides can increase adipose tissue inflammation and dysfunction and increase your risk of metabolic syndrome and cardiometabolic disease.
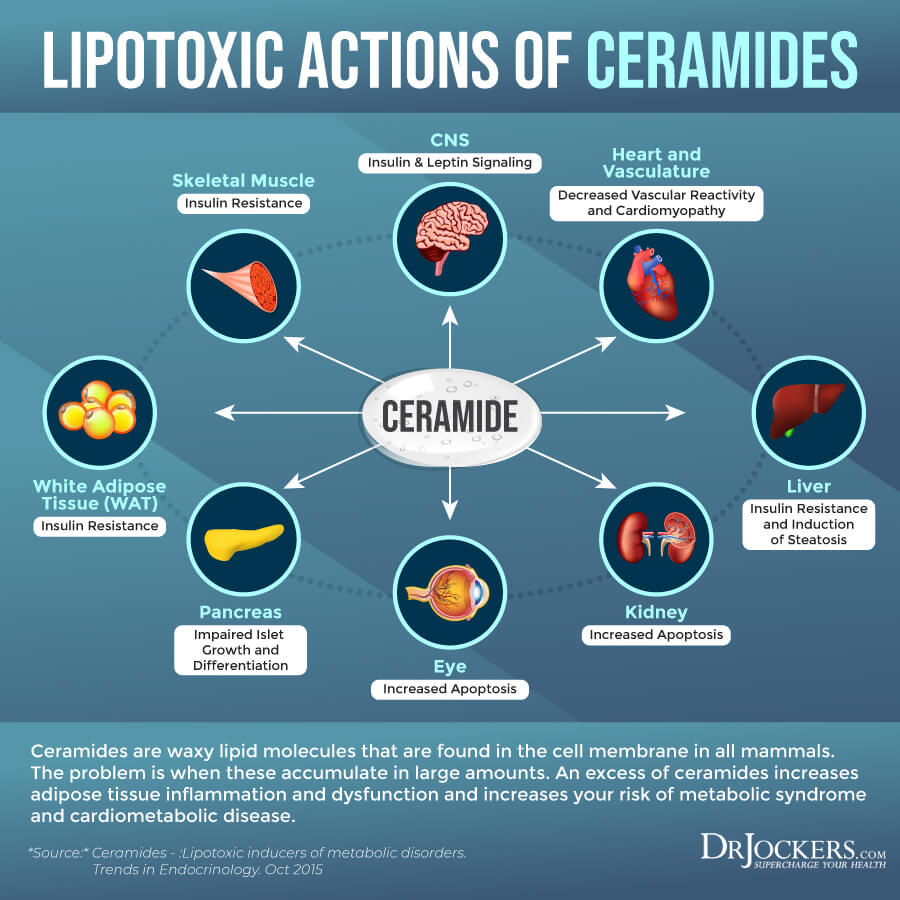
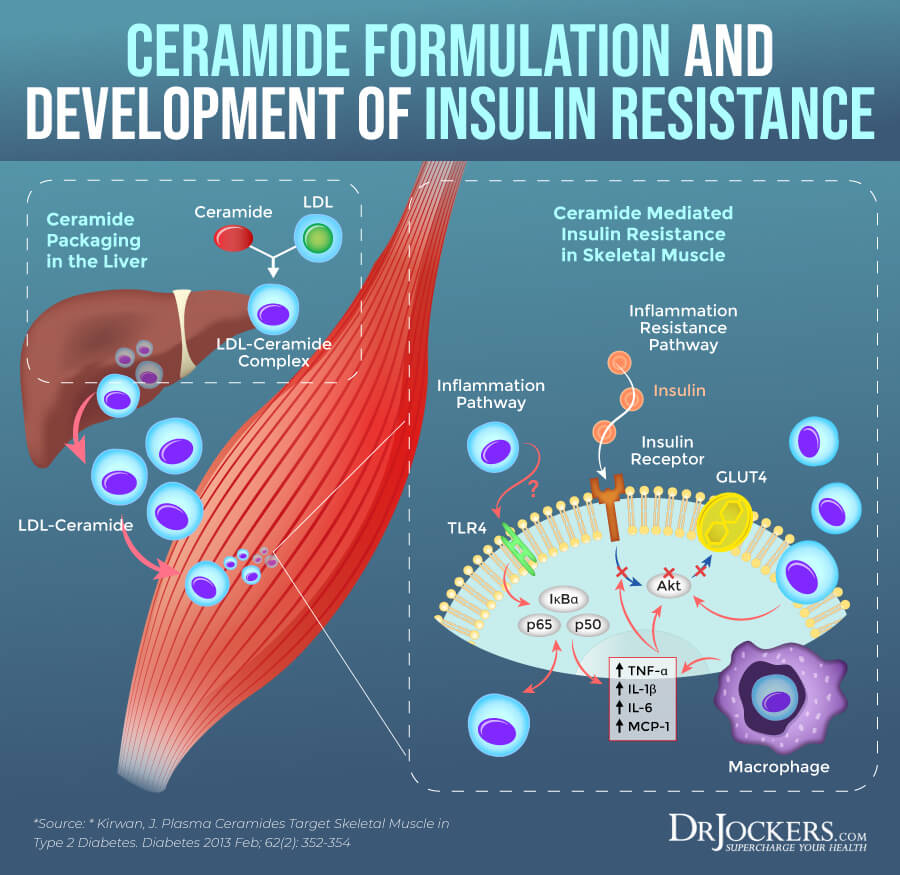
A 2019 review published in Frontiers in Endocrinology has found that ceramides also play a role in insulin resistance (5). Insulin resistance means that your body cannot respond to insulin well and cannot process blood glucose properly, which leads to increased blood glucose levels and increases your risk of prediabetes and type 2 diabetes.
There are about 1.9 billion overweight and 600 million obese adults around the world (5). Research suggests that insulin resistance may play a critical underlying role in fat accumulation in adipocytes and non-adipose tissue, which increases chronic inflammation. It turns out the sphingolipid ceramides may be the main reason behind excess saturated fatty acids and the increased release of inflammatory cytokines that can lead to insulin resistance, diabetes, hypertension, atherosclerosis, and cardiovascular disease.
Ceramides become upregulated by inflammation and prevent insulin-stimulated disposal of glucose and metabolic respiration contributing to metabolic syndrome. The review suggests that manipulating adipocyte ceramides may help to influence inflammation levels, however, further research is needed on the subject.
Measuring Visceral Fat Levels
The only way to measure your visceral fat levels exactly is by using an MRI or CT scan. However, these procedures are not only expensive but are also unnecessary. You can take some easy measurements at home or with the help of your doctor that can indicate your risk for visceral fat.
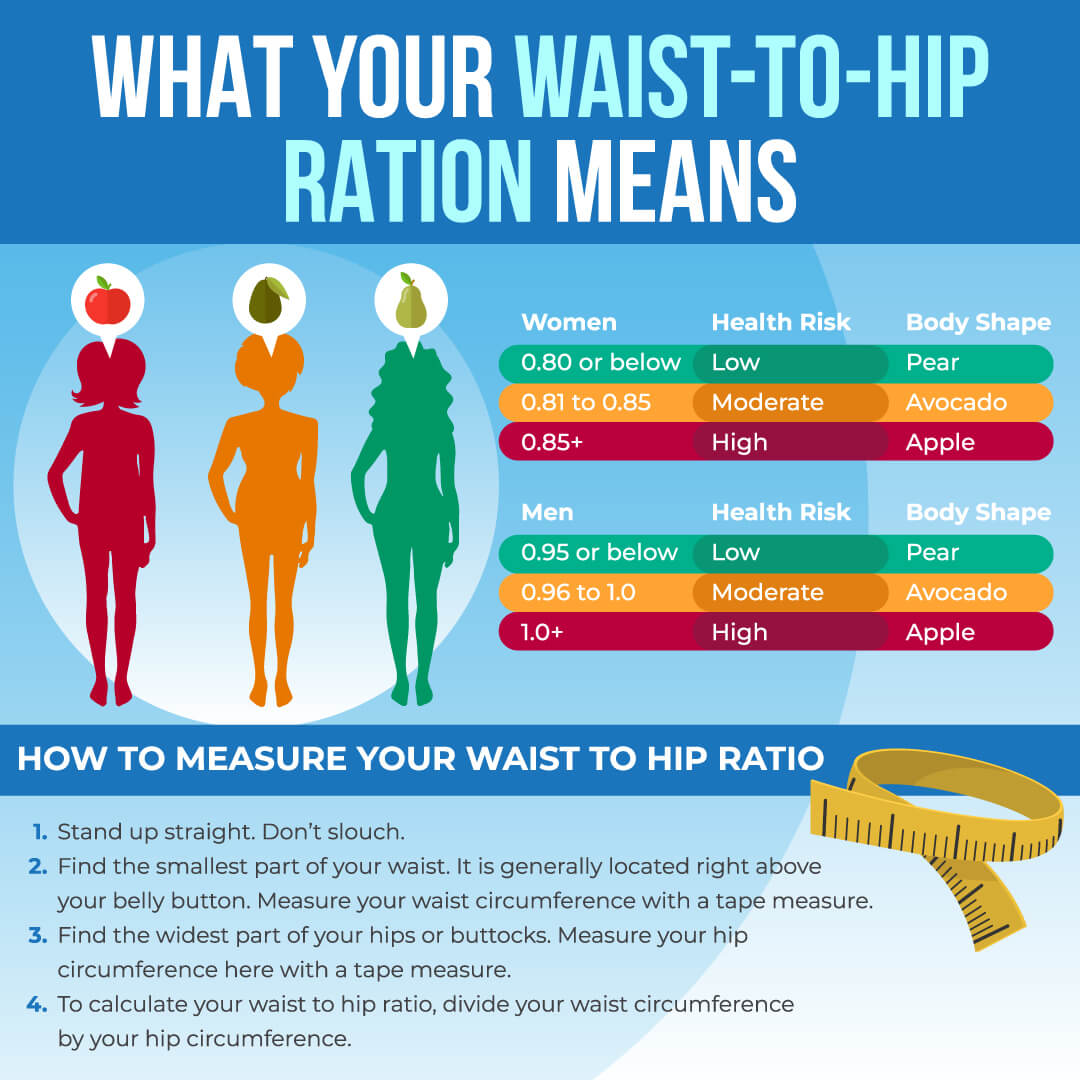
Calculating your waist to hip ratio and waist to height ratio is the best way to figure out your risk factors. It’s simple and completely free. Here is how to do it.
Waist to Hip Ratio
Calculating your waist to hip ratio (WHR) at home is simple. However, if you need help, you can always ask for assistance from your healthcare provider. Here is how to do it:
- Stand up straight. Don’t slouch.
- Find the smallest part of your waist. It is generally located right above your belly button. Measure your waist circumference with a tape measure.
- Find the widest part of your hips or buttocks. Measure your hip circumference here with a tape measure.
- TO calculate your waist to hip ratio, divide your waist circumference by your hip circumference.
According to the World Health Organization (WHO) and 2001 study published by the International Journal of Obesity and Related Metabolic Disorders a waist to hip ratio of .85 for women and .90 for men may indicate abdominal obesity and increases the risk of diabetes and other metabolic issues (6, 7).
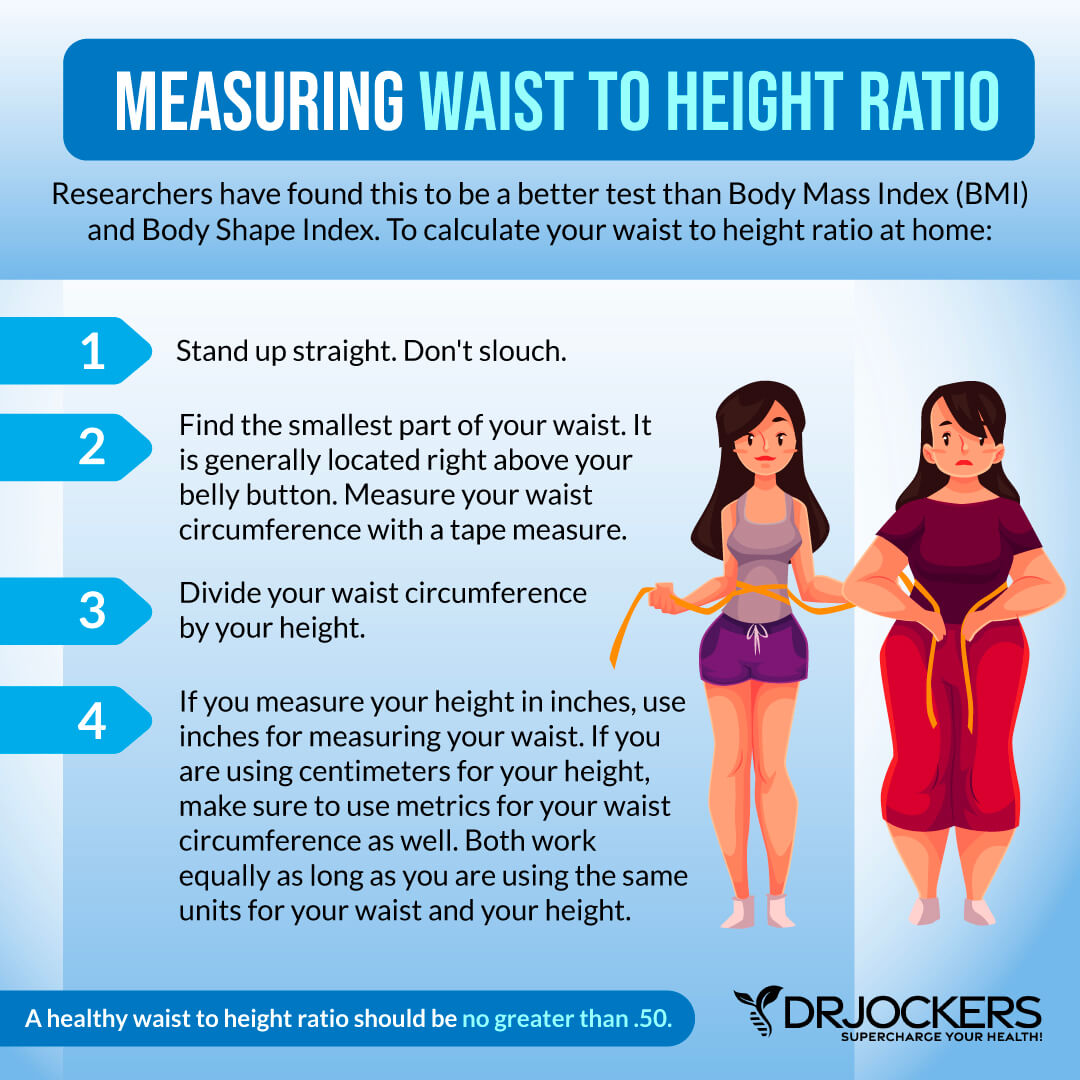
Waist to Height Ratio
You may also look at your waist to height ratio (WHtR). A 2020 study published in Nature has found that this number is a particularly good indicator of visceral fat in people with type 1 diabetes (8). Researchers linked larger waist circumference to higher visceral fat percentage. They have found that the waist to height ratio is a better indicator of health issues and mortality than body mass index (BMI) and body shape index (ABSI).
To calculate your waist to height ratio at home:
- Measure your waist circumference with a tape measure just like I explained earlier.
- Divide your waist circumference by your height.
- If you measure your height in inches, use inches for measuring your waist. If you are using centimeters for your height, make sure to use metrics for your waist circumference as well. Both work equally as long as you are using the same units for your waist and your height.
A healthy waist to height ratio should be no greater than .50. I recommend that you calculate both numbers to get a more accurate picture.
Testing for Inflammation
Measuring your waist to hip and waist to height ratio is not enough. Increased visceral fat holds an array of health risks, including chronic inflammation, insulin resistance, diabetes, cardiovascular issues, and other health problems. I will go over these health risks in the next section.
Checking certain labs for inflammation, blood sugar, and lipids is important to determine your risks, especially if your ratios for visceral fat are high. I recommend getting a Comprehensive Blood Analysis, which is a great blood test that allows us to look at all these factors of your health. These are the specific tests I recommend:
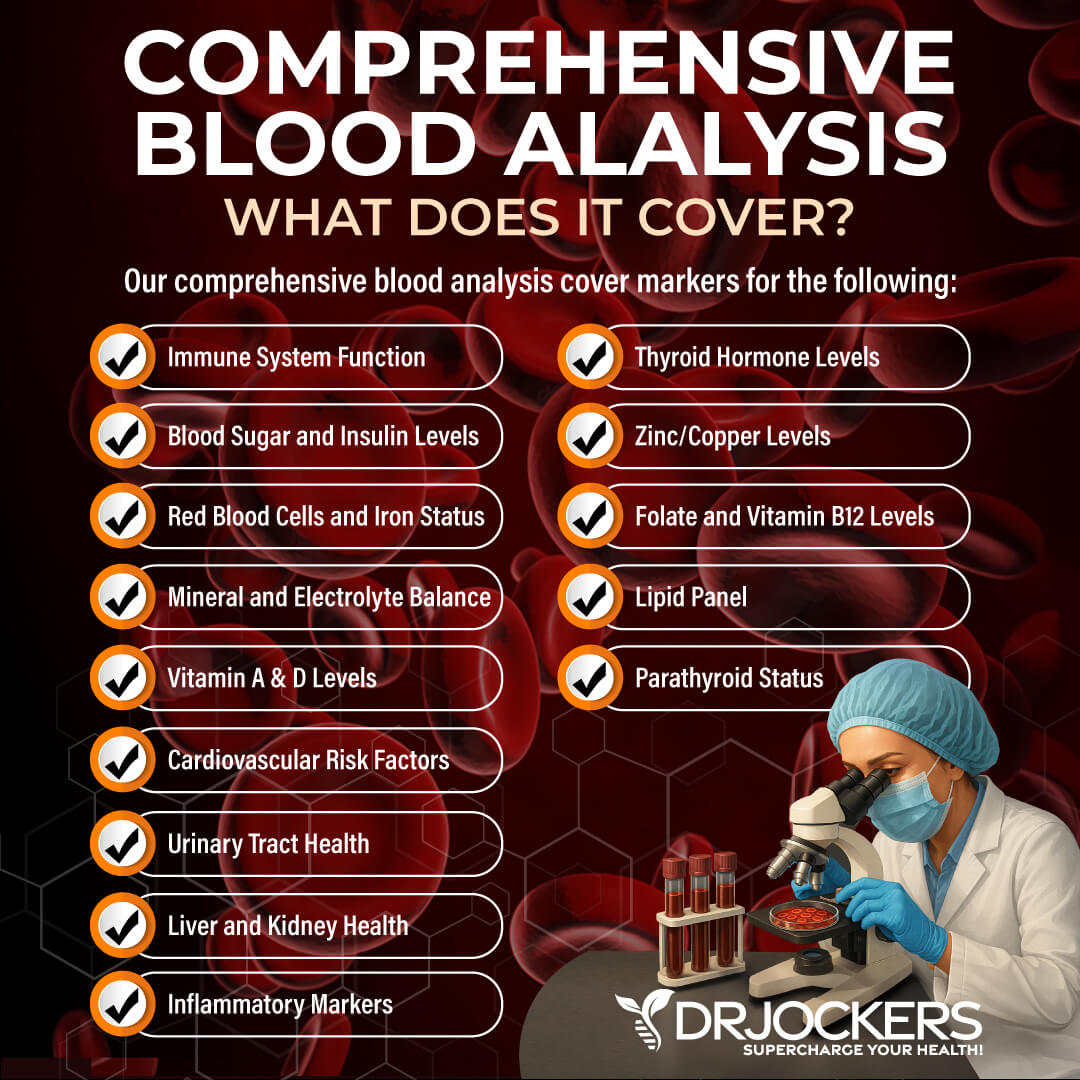
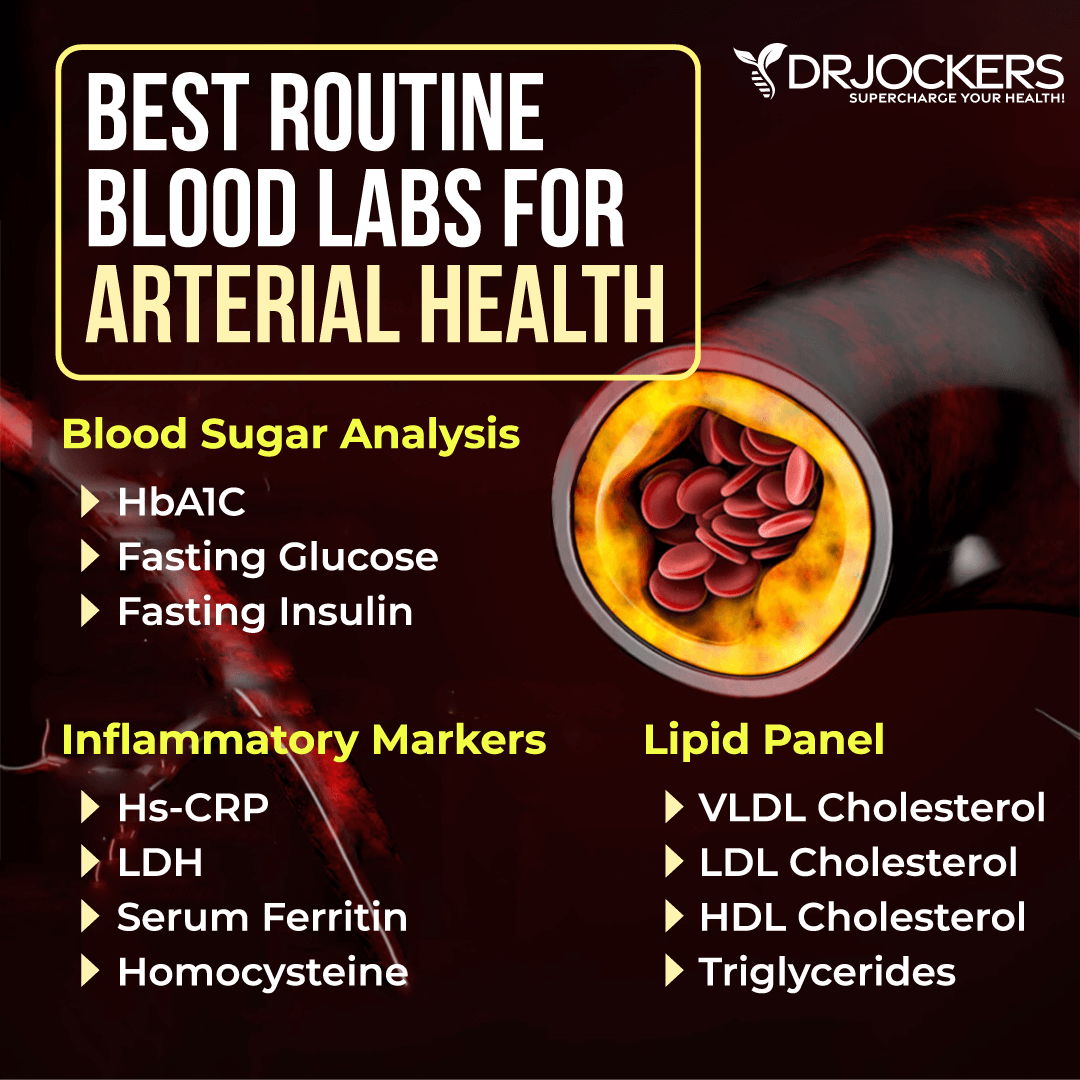
Blood Sugar
I recommend looking at your blood sugar levels:
- HbA1C: The ideal number is between 4 and 5.6 percent. Between 5.7 and 6.4 means that you have a high risk of developing diabetes, and over 6.4 means that you have diabetes.
- Fasting Glucose: Less than 100 mg/dL (5.6 mmol/L) is normal. 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. 126 mg/dL (7 mmol/L) or higher on two separate tests means you have diabetes.
- Fasting Insulin: Normal fasting insulin levels are between 75–95 mg/dL (4.2–5.3 mmol/L). Over 95 mg/dL (5.3 mmol/L) shows insulin resistance and over 110 mg/dL (>6.1 mmol/L) shows severe insulin resistance.
Inflammatory Markers
I recommend looking at your inflammatory markers:
- HsCRP: The ideal number is under 1.
- LDH (lactose dehydrogenase): The optimal range is 140 to 180. High levels indicate chronic inflammation.
- Serum ferritin: The ideal range is under 150. High levels indicate inflammation.
- Homocysteine: The optimal range is 6 to 9.
Lipid Panel
I recommend a lipid panel test looking at the following areas:
- VLDL cholesterol: The ideal range is 5 to 30 mg/dl.
- HDL cholesterol: The idea range is 55 to 80. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The ideal range is 40 to 80.
Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. Ideally, we are looking for an LDL: HDL Ratio: 3:1 or less, 2:1 being optimal. For triglycerides, we are looking for an HDL Ratio: 2:1 or less, 1:1 being optimal.
Higher triglyceride and lower HDL levels are typically an indication of insulin resistance and high fasting insulin level. You can read this article for more info on blood markers for inflammation.
7 Problems with Excess Visceral Fat
Having excess visceral fat can lead to or increase your risk of a list of health issues, including chronic systemic inflammation, insulin resistance, diabetes, heart disease, estrogen dominance, cancer, mood disorders, and dementia. Let’s learn more about these health risks.
Increases Systemic Inflammation
One of the biggest problems with excess visceral fat is that it increases systemic inflammation in your body. It creates hormonal and inflammatory molecules. This puts enormous stress on your liver. If you have excess visceral fat around your liver, kidneys, pancreas, heart, and intestines, it creates even further inflammation and disrupts your metabolism feeding a vicious cycle of chronic inflammation and related health issues.
What’s interesting about visceral fat is that besides creating chronic inflammation in your body, it also becomes inflamed itself by creating and releasing an inflammatory molecule called interleukin-6. This can trigger autoimmune reactions and lead to a list of chronic diseases.
As you know, chronic inflammation is the root cause of most modern-day diseases. For example, a 2009 review published in Currents in Vascular Pharmacology has linked visceral fat to atherosclerosis (9). A 2006 review published in Current Diabetes Reviews has made the connection between visceral fat, metabolic obesity, type 2 diabetes, and cardiovascular disease (10).
Leads to Insulin Resistance, Diabetes, and Carb Cravings
You already learned that visceral fat plays a role in the development of insulin resistance. Insulin resistance increases your risk of prediabetes and diabetes, however, you can have insulin resistance without prediabetes or diabetes as well.
While being overweight or obese itself can increase your risk of various health issues, abdominal fat, and visceral fat more specifically, puts you at a higher risk of diabetes and other chronic diseases than hip or thigh fat.
A 2013 study published in Nutrients has found that your body fat distribution plays a large role in developing insulin resistance (11). It has found that visceral abdominal fat increases your risk of insulin resistance more than other fat. Improving adipose tissue function and reducing visceral fat can play an important role in reducing insulin resistance.
Whether you have diabetes or not, visceral fat can contribute to insulin resistance. A 2010 study published in the Journal of Nutritional Science and Vitaminology (Tokyo) has found that the amount of visceral fat can be used as a strong predictor of insulin resistance even in non-diabetic people (12).
A 2016 study published in the Yonsei Medical Journal has found a strong link between visceral fat and prediabetes and diabetes (13). This link was stronger than any other anthropometric obesity indicators measured.
Unfortunately, having excess visceral fat can further feed the cycle of obesity and the risk of insulin resistance or diabetes by increasing your cravings. While eating too many calories, and too many foods high in sugar and refined carbohydrates can increase your visceral fat in your body, visceral fat itself can increase your cravings for sugar and carbs.
A 2018 study published in the International Journal of Obesity (London) has found that visceral fat disrupts your brain’s sensitivity to interoceptive feedback (14). This can affect your eating behavior, appetite, and cravings.
Higher Risk of Heart Disease
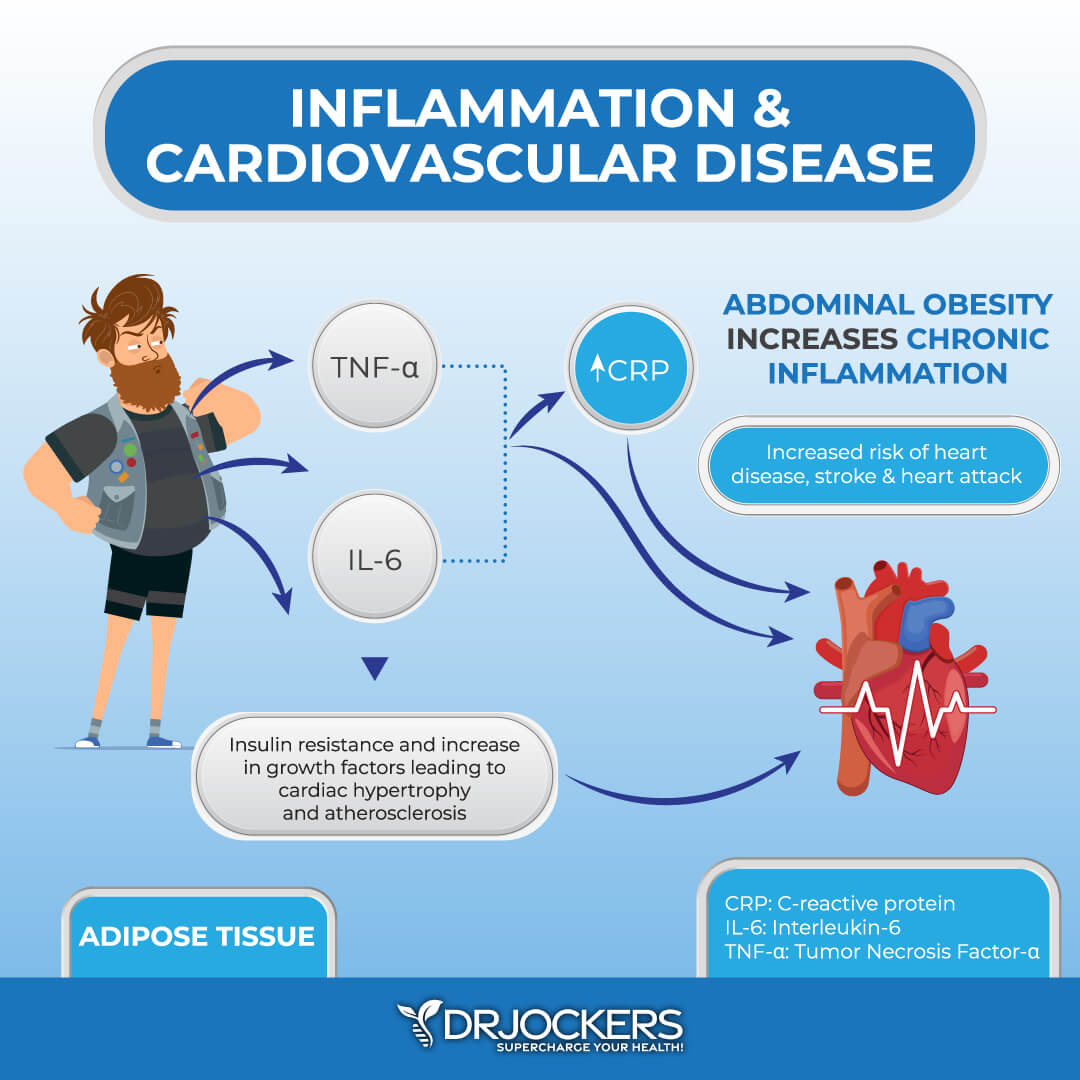
Excess visceral fat also increases your risk of heart disease. As you know, visceral fat increases chronic inflammation and inflammatory cytokines in your body. These fat-generated inflammatory cytokines are some of the top root causes of heart disease and other inflammatory conditions.
A 2013 review published in Physiological Reviews has found that visceral fat can lead to high triglycerides or hypertriglyceridemia (15). It can also increase pro-inflammatory cytokine production, inflammation, and liver insulin resistance. It may increase bad cholesterol levels and negatively affect metabolic functions. It may also lead to high blood pressure and the formation of plaque buildup in your arteries. All these are important cardiovascular disease markers that show an increased risk of cardiovascular disease.
Excess visceral fat around your abdomen increases the production of inflammatory cytokines like TNF-alpha and IL-6. This increases c-reactive protein (CRP) in your body. CRP is a protein made by your liver. Increased levels of CRP indicate inflammation in your body.
Visceral fat also creates an atherogenic environment that increases the risk for plaque buildup in your arteries. It increases insulin resistance and metabolic syndrome. The combination of inflammatory cytokine production, increased CRP, plaque buildup, insulin resistance, and metabolic syndrome increase your risk of acute coronary syndrome and heart disease.
Estrogen Dominance
Estrogen and progesterone are the two primary female sex hormones that, beyond reproduction and childbearing in women, are also responsible for your metabolism, thyroid health, hormonal health, cholesterol levels, brain health, mood, bone health, and skin health.
In a healthy body, estrogen and progesterone work together in a nice balance. However, when your body starts making too much estrogen and/or your progesterone levels drop too low, your estrogen and progesterone levels get out of balance, and you develop estrogen dominance.
Estrogen dominance is a common problem that can lead to premenstrual symptoms (PMS), endometriosis, infertility, hot flashes, menstrual cramps, decreased libido, fibrocystic breasts, uterine fibroids, ovarian cysts, weight gain, fatigue, headaches, depression, mood imbalances, brain fog, thyroid issues, and cancer. Estrogen dominance may affect men as well and lead to fatigue, insomnia, brain fog, weight gain, irritability, mood swings, depression, anxiety, and low libido.
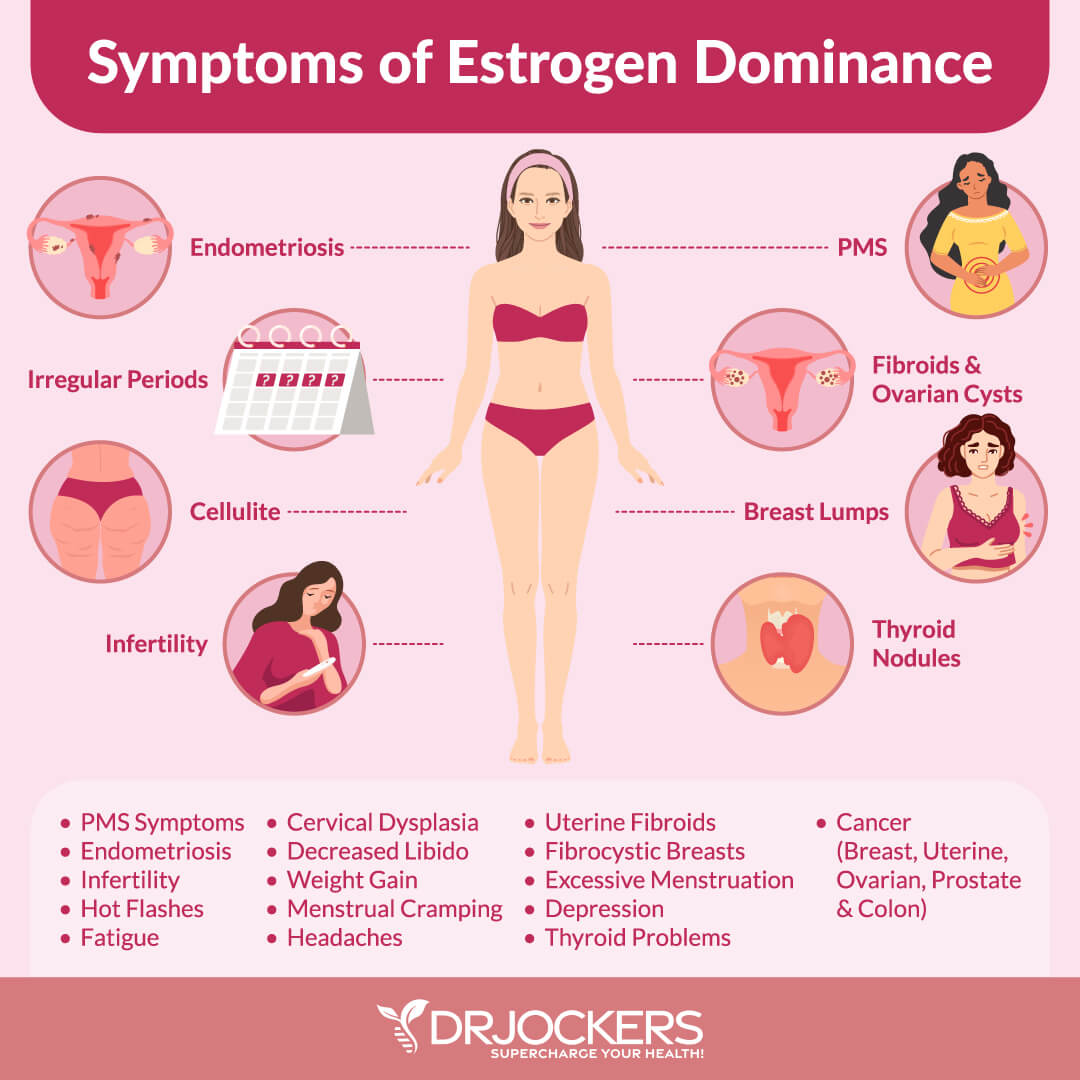
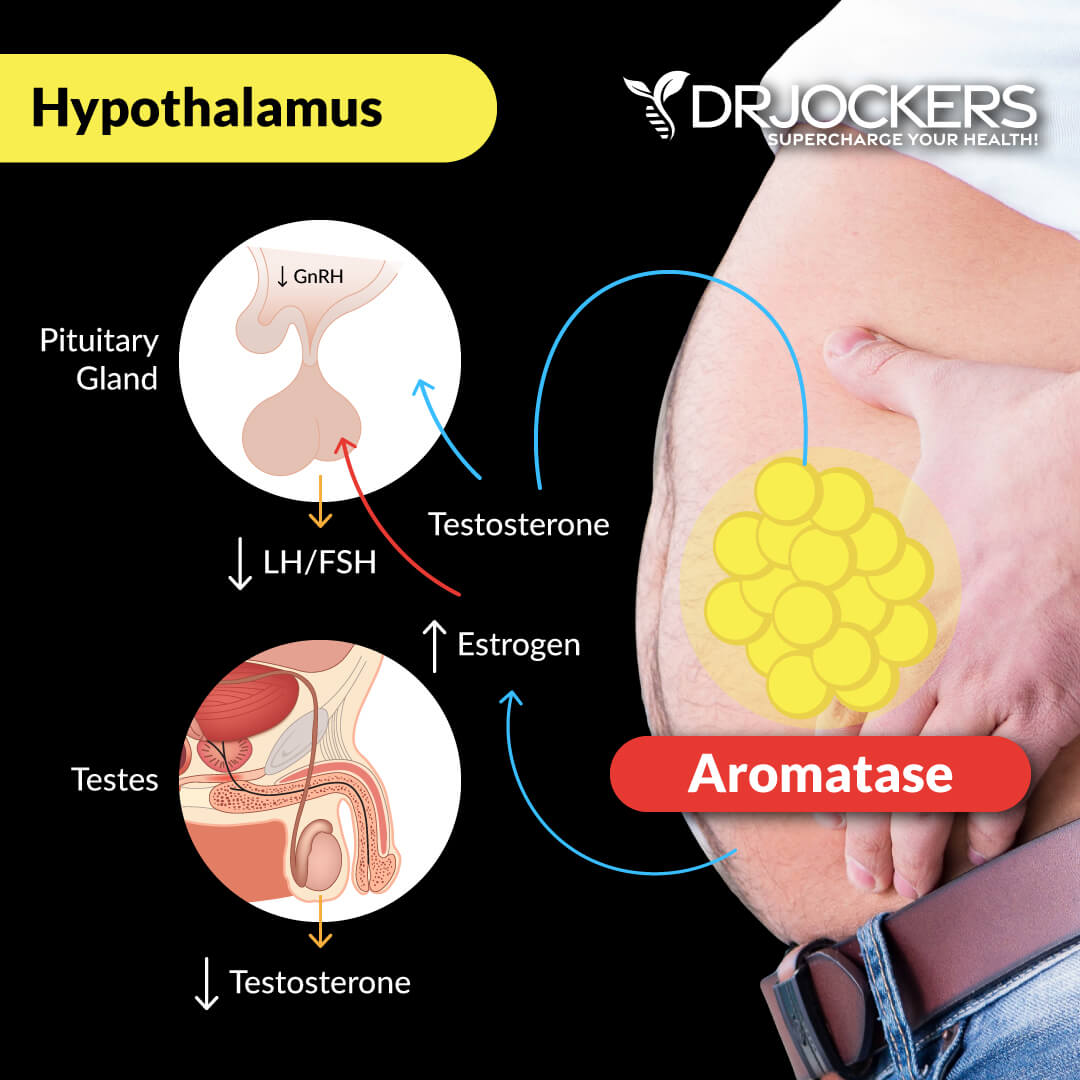
Visceral fat is one of the major risk factors for estrogen dominance and estrogen dominance can further feed the problem of visceral belly fat. Androgens are male sex hormones that can be found in and affect both males and females.
Aromatase is an enzyme in your body that converts androgens to estrogens. The problem is that visceral fat increases aromatase in your body that can lead to estrogen dominance and a long list of serious health issues.
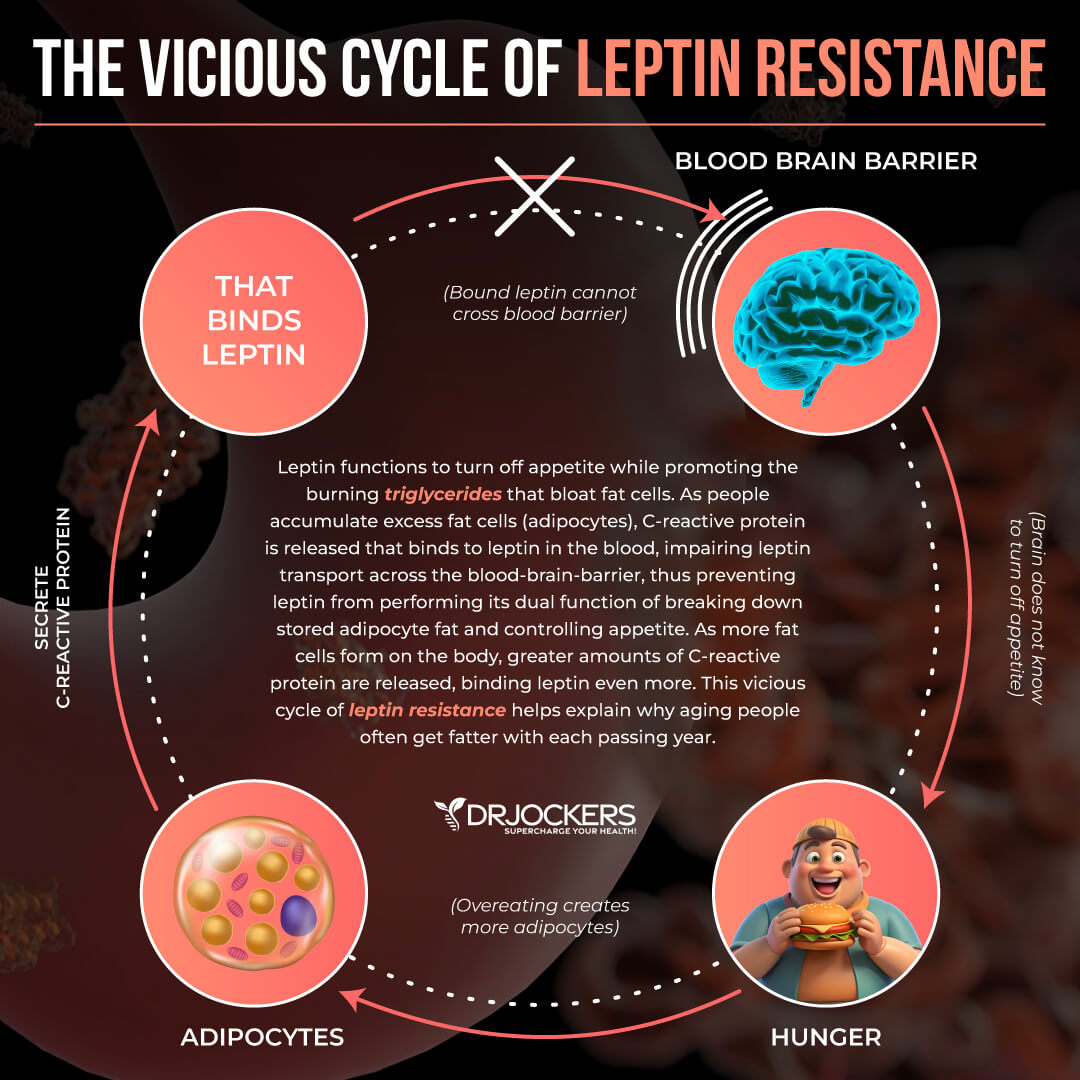
A 2001 study published in Medical Hypotheses has linked too much visceral fat and an increase in adipose tissue to an increase in aromatase (16). Since aromatase converts testosterone to one of the estrogen hormones, estradiol, it leads to a decrease in testosterone levels. Too much estrogen and too little estrogen favor the development of visceral fat and increase your total body fat index. It may also cause hormone resistance for insulin and leptin.
Too much leptin prevents your body from fighting weight gain but feeds the problem of visceral obesity and insulin resistance instead. Insulin resistance causes elevated triglyceride and bad cholesterol levels that can increase your risk for heart disease. The combination of these issues can increase your risk of hormonal imbalance, obesity, hypertension, heart disease, type 2 diabetes, extreme fatigue, sleep problems, and depression.
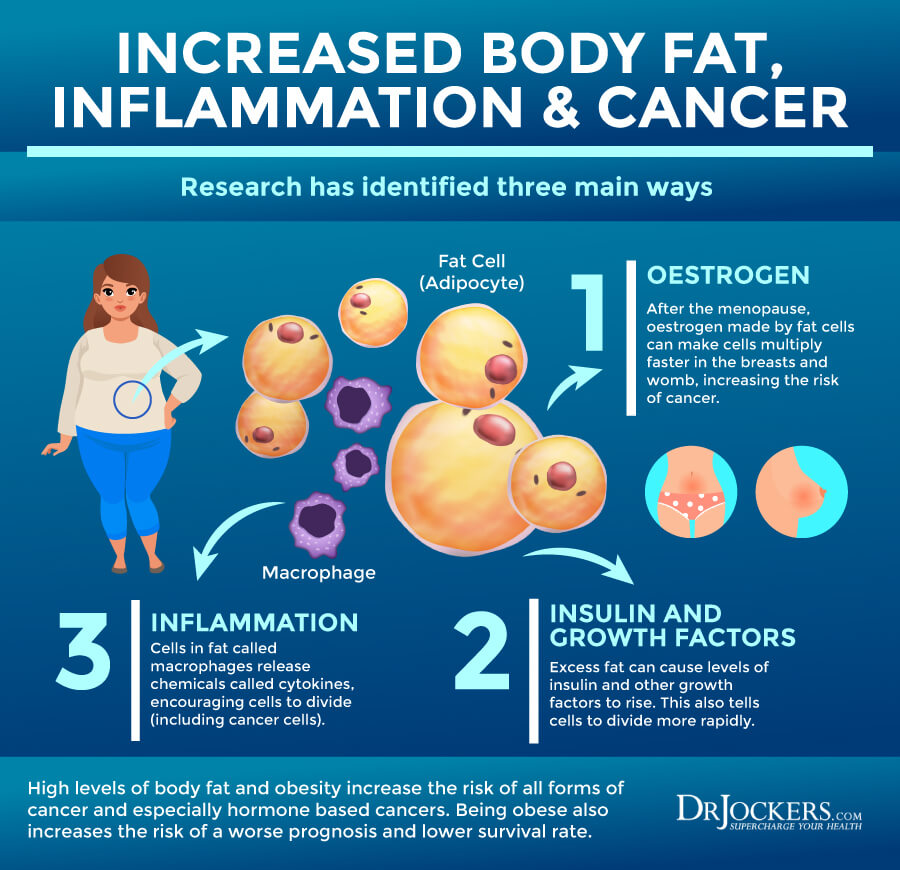
Cancer Risk
Cancer may develop for three main reasons. One reason may be an increase in estrogen. This may be increasingly problematic for women after menopause. After menopause, estrogen made by the fat cells of women starts to multiply faster in the breasts and the womb, increasing the risk of cancer.
Another root cause of the development of obesity-related cancer is insulin and growth factors. Excess fat can cause levels of insulin and other growth factors to rise, which can lead the cells to divide more rapidly.
The third important root cause of cancer is chronic inflammation. Cells in your fat are called macrophages that release inflammatory cytokines that encourage cell division, including cancer cell division, that can increase your risk of cancer. Unfortunately, excess visceral fat can increase estrogen dominance, increased insulin and growth factors, and increased chronic inflammation. The combination of these three issues can become a breeding ground for cancer.
High levels of body fat, abdominal visceral fat, and obesity may increase your risk of all forms of cancer, especially hormone-based cancers, such as ovarian, breast, and prostate cancer. Being obese and having high levels of visceral fat can also worsen your prognosis and survival rate.
As you know, visceral fat and obesity increase inflammatory cytokines, TNF-alpha and IL-6, in your body and lead to increased levels of CRP which indicates increased chronic inflammation in your body. Obesity and visceral fat also increase insulin resistance and growth factors. The combination of this can increase cellular division, DNA damage, and the risk of cancer.
A 2017 study published in Oncogene has found that visceral fat increases the risk of cancer more than subcutaneous fat does (17). They found that this may be happening because of the increased release of the FGF2 protein, a basic fibroblast growth factor, and estrogen from visceral fat that may influence your risk for cancer.
A 2017 study published in Diabetology and Metabolic Syndrome has found a link between visceral fat, obesity, insulin resistance, and cancer (18). They found that obesity leads to systemic changes in the body, including chronic inflammation, changes in adipokines and sex steroids, an increase in insulin and insulin-like growth factor. These systemic changes affect tumorigenesis and increase your risk of cancer.
A 2018 case control study published in Nutrition Hospitalaria has found that excess visceral fat can increase the risk of breast cancer (19). A 2019 study published in Science Reports has found an increased risk for cancer in postmenopausal obese women (20). A 2017 study published in the Oncologist has found that obesity, a high waist to hip ratio, and increased visceral fat increase the risk of hormone-receptor-negative breast cancer compared to those with less visceral fat (21). A 2021 retrospective cohort study published in Gynecologic Oncology has found an increased risk for complications in advanced ovarian cancer in women with visceral obesity (22).
Breast cancer and ovarian cancer are cancers that affect women. But men are also not free from the risk of obesity-related cancer. A 2019 study published in Cancer has found that increased visceral fat and obesity increases the risk and prognosis of prostate cancer (23).
Moreover, visceral fat and obesity can increase the risk of other types of cancers that may affect both men and women. A 2013 study published in Cancer Prevention Research has found that visceral fat increases the risk of intestinal cancer (24). A 2015 study published in Clinical Cancer Research has found a link between visceral fat, obesity, and chronic inflammation, and an increased risk of pancreatic cancer (25).

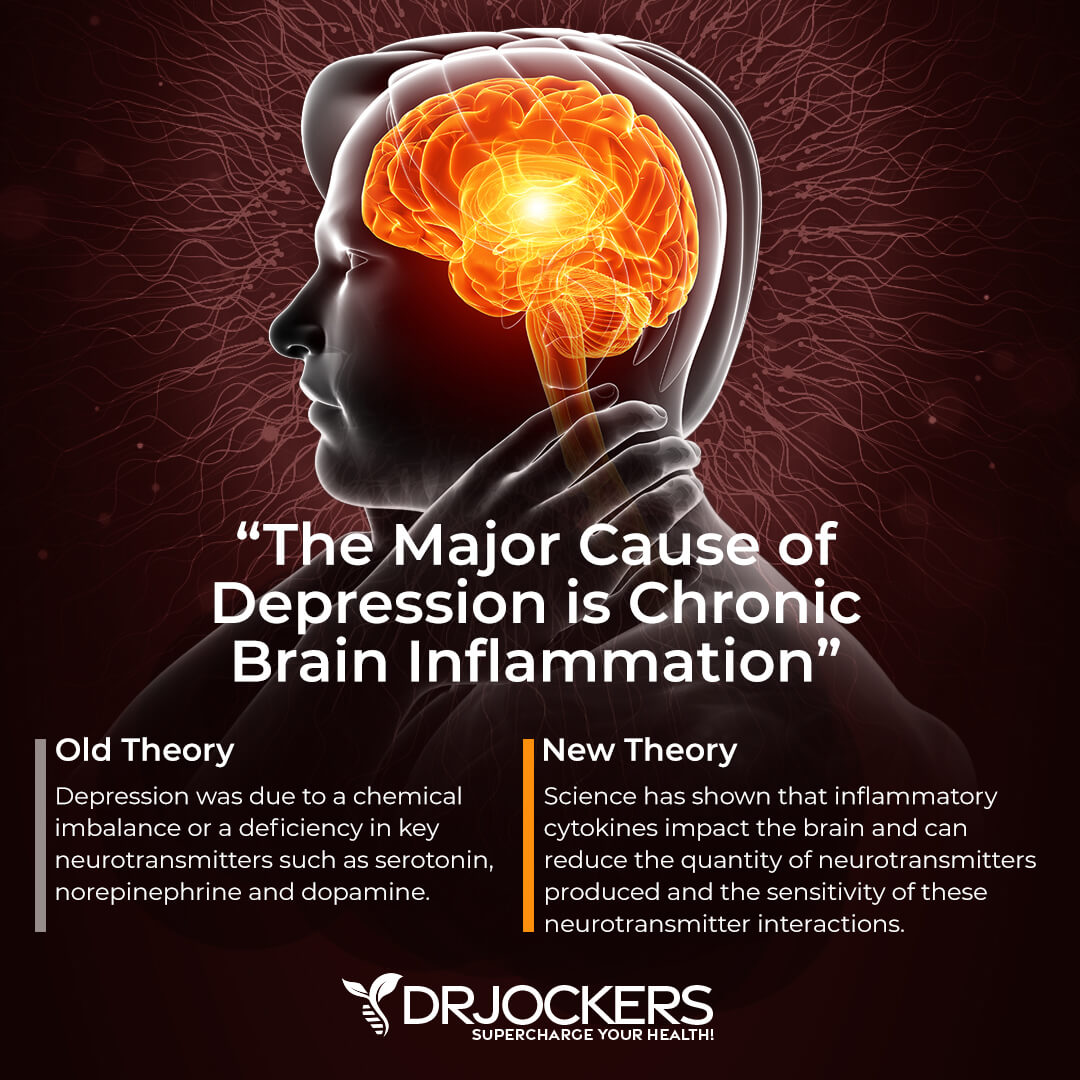
Mood Disorders
Excess visceral fat can also increase your risk of mood disorders, including depression and anxiety. A 2013 study published in Frontiers in Neuroscience has found a link between obesity and depression (26). They found that your mood is greatly affected by your diet. A poor diet and overeating increase the risk of obesity which can negatively affect your mood.
A low mood and stress can increase overeating and cravings for sugary and unhealthy foods that may feed this cycle. An increase in visceral fat can impact your brain and impair insulin and leptin signaling.
It may be surprising, but leptin and insulin play a role in your emotions and mood and an imbalance can increase depression and anxiety. Visceral fat and obesity increase your risk of metabolic issues, poor metabolic signaling, and chronic inflammation which also negatively affect your mental health and increase the risk of anxiety and depression.
A 2012 study published in Obesity has also found a link between increased visceral fat and depression in middle-aged men and women (27). They examined 1,581 women and 1,718 men around the age of 50 and looked at their visceral adipose tissue and depressive symptoms.
They found that increased visceral adipose tissue is linked to the increased risk of depression. This likely happens because visceral fat is a metabolically active fat that interferes with neurotransmitter function. Since depression may cause greater fat storage in women, it’s particularly important for women to follow a healthy diet that reduces visceral fat and depressive symptoms.
Increased Risk of Dementia
Excess visceral fat and obesity can also increase your risk of Alzheimer’s disease and dementia. A 2008 study published in Neurology has found that visceral fat can increase the risk of dementia and Alzheimer’s disease after three decades of the initial research. Researchers looked at the abdominal measurements of 6,583 male and female middle-aged participants between 1964 and 1973.
Three decades later, between 1994 and 2006 they followed up with the same patients who were between 73 and 87 at the time. They found that a whopping 1,049 of the original participants had dementia.
Comparing the rates of dementia and their abdominal measurements for visceral fat in middle age during the initial part of the study, they found that people with higher visceral fat had a higher likelihood of developing dementia. People with an apple shape tend to have a higher waist to hip ratio and have a higher likelihood of dementia than people with a pear shape and low waist to hip ratio.
They also found that obese participants with the highest abdominal measures and highest BMI had a 360 percent higher chance of developing dementia than those with the lowest abdominal measures and a healthy BMI.
A 2007 review published in Age and Aging has found the increased visceral fat and visceral adipose tissue presents a higher risk factor for dementia compared to high BMI (29). BMI measurements are commonly used to predict risk factors for health issues, however, it may not be the best indicator.
Prior research suggests that a high BMI can certainly indicate an increased risk for dementia, however, according to these findings, looking at visceral abdominal fat may be an even better indicator. Increased visceral adipose tissue and visceral fat can cause chronic inflammation, hormonal imbalance, and neurochemical imbalances which can lead to a decline in cognitive functions.
Excess visceral fat also leads to increased cardiovascular risk factors, including insulin resistance, inflammation, high blood pressure, and atherosclerosis, that may also contribute to a decline in cognitive functions.
The authors suggest that even the bodies of individuals who are at a healthy weight or are even underweight may successfully mask excess visceral fat with a normal or low BMI. As a result, they may also have an increased risk for dementia and other health problems without knowing about it.
Looking at visceral fat and waist to hip ratio instead of only BMI is important to look at one’s risk factors for dementia or other chronic or progressive health issues. Here is a great article and image on the relationship between increased visceral fat and dementia.
Final Thoughts
Visceral fat is a fat that accumulates in your abdomen. Excess visceral fat is a serious health risk. It can increase your risk of obesity, chronic inflammation, insulin resistance, diabetes, heart disease, cancer, estrogen dominance, mood imbalances, and dementia.
Since visceral fat is an underlying root cause of many chronic health issues, I recommend that you bookmark this article as a future reference and share it with your friends and family.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
 Inflammation Crushing Ebundle
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



