 Vitamin D Resistance and Autoimmunity
Vitamin D Resistance and Autoimmunity
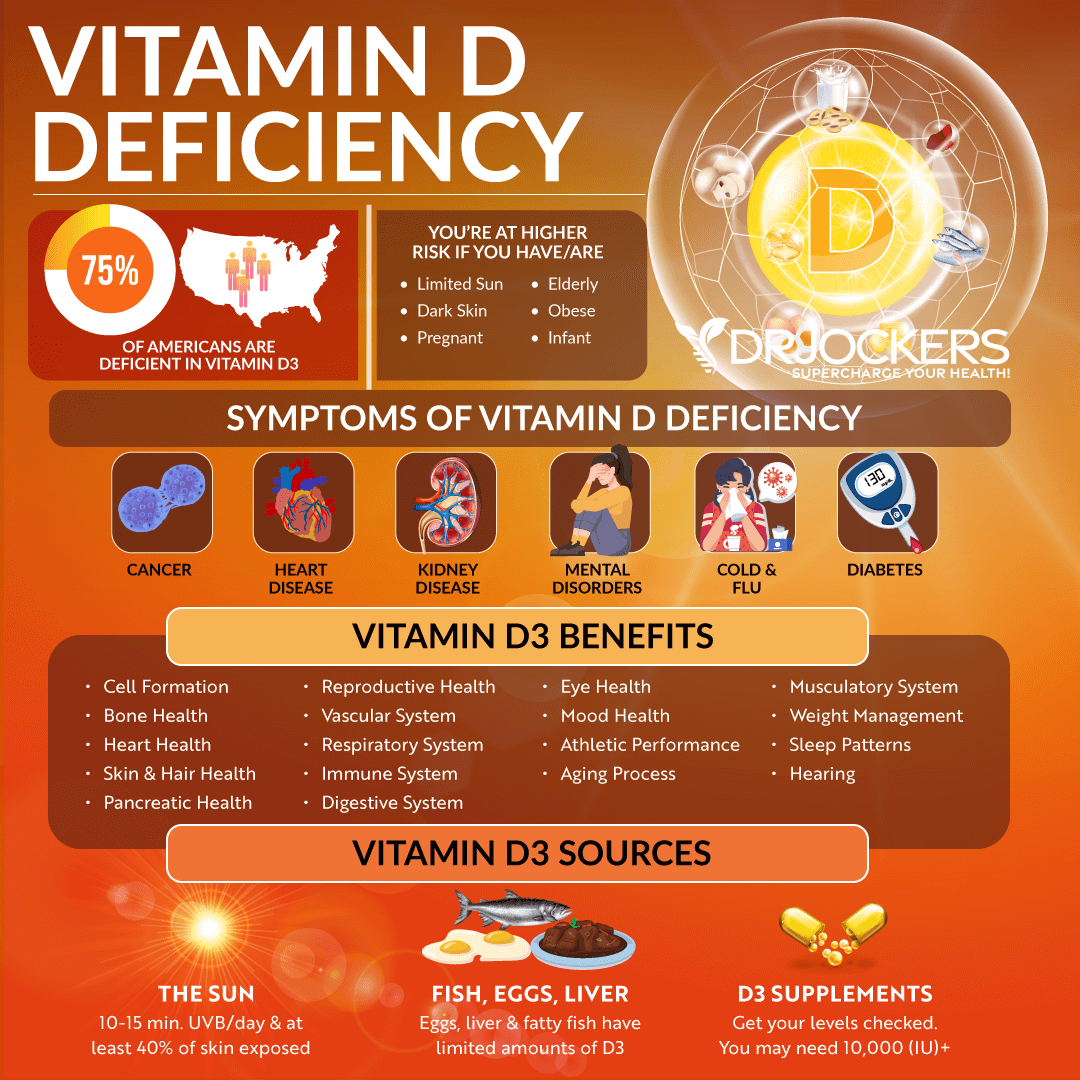
Vitamin D is a fat-soluble vitamin that’s important for immune function, bone and muscle health, brain and mental health, and other areas of your health. Vitamin D deficiency may play a role in autoimmunity. Most people see results when taking vitamin D supplements. Others have vitamin D resistance and don’t see improvement despite supplementation.
In this article, you will learn about vitamin D and its role in immune regulation. You will understand the connection between vitamin D deficiency and autoimmunity. You will learn about vitamin D resistance and the factors involved in low vitamin D levels.
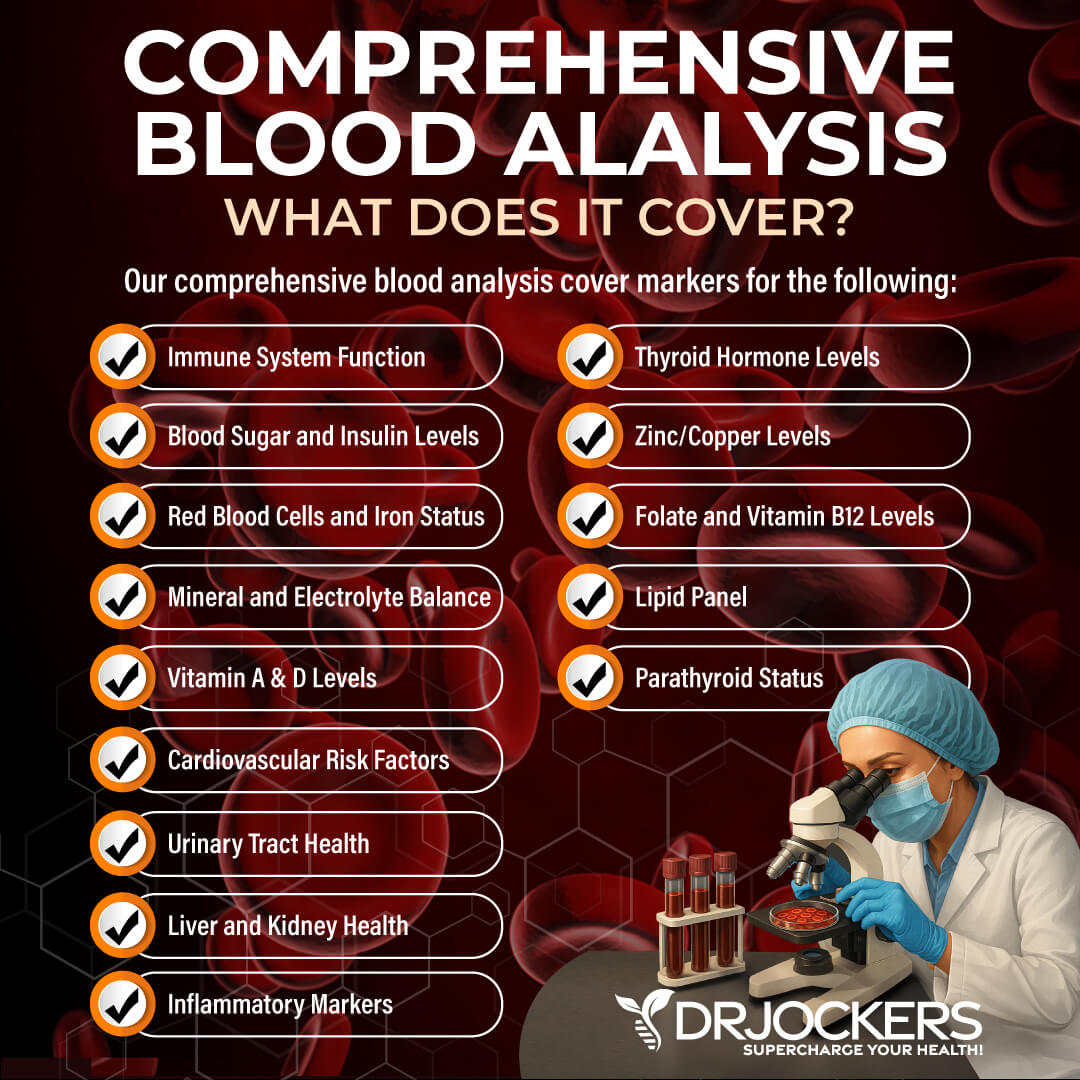
I will discuss the importance of vitamin D receptor activation, vitamin D and PTH balance, how 25-OH vitamin D converts to calcitriol, and the importance of vitamin A and magnesium. You will understand why you need to take vitamin D3 with vitamin K2. I will recommend a Comprehensive Blood Panel to test for vitamin D deficiency, vitamin A and calcium levels, and inflammatory markers.
What is Vitamin D
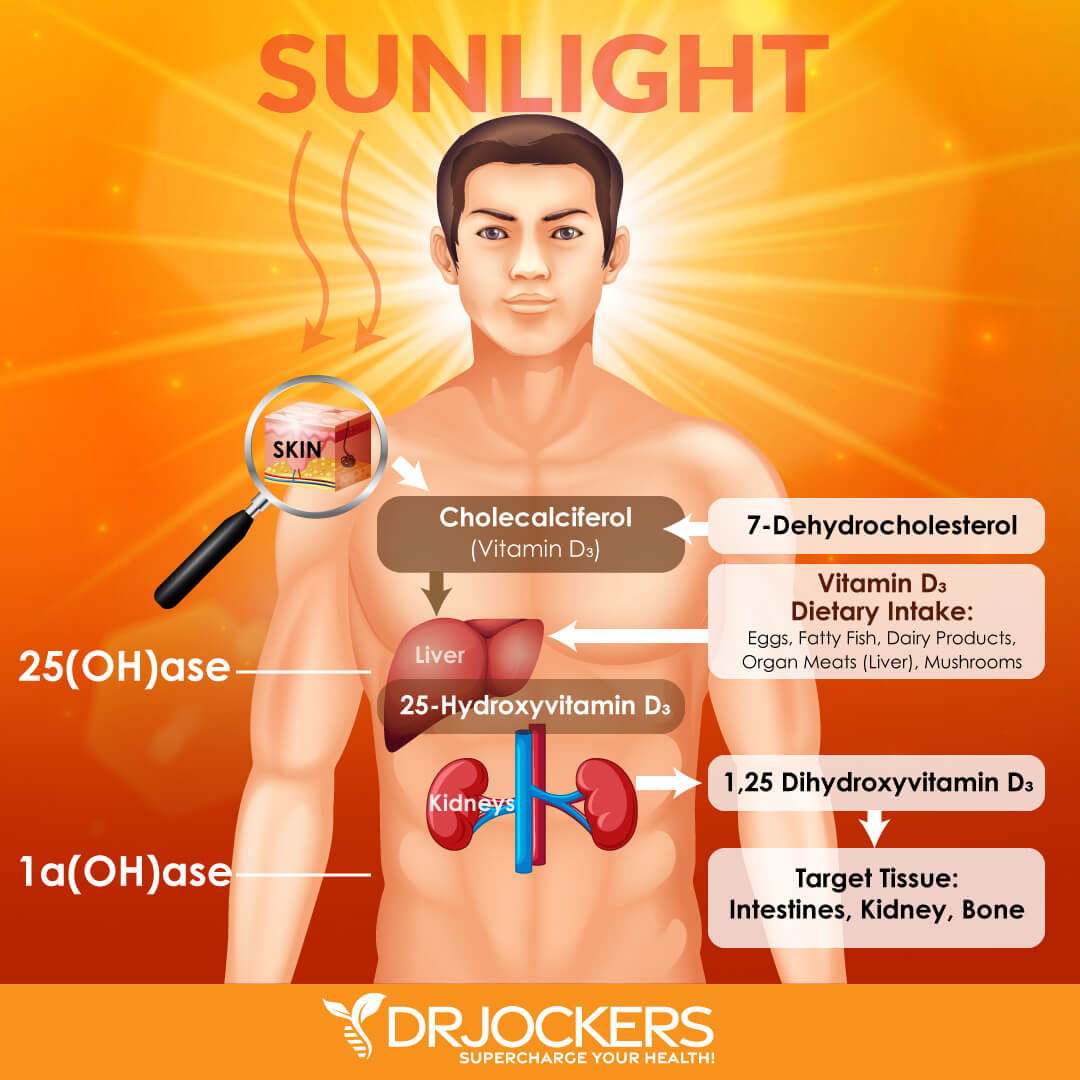
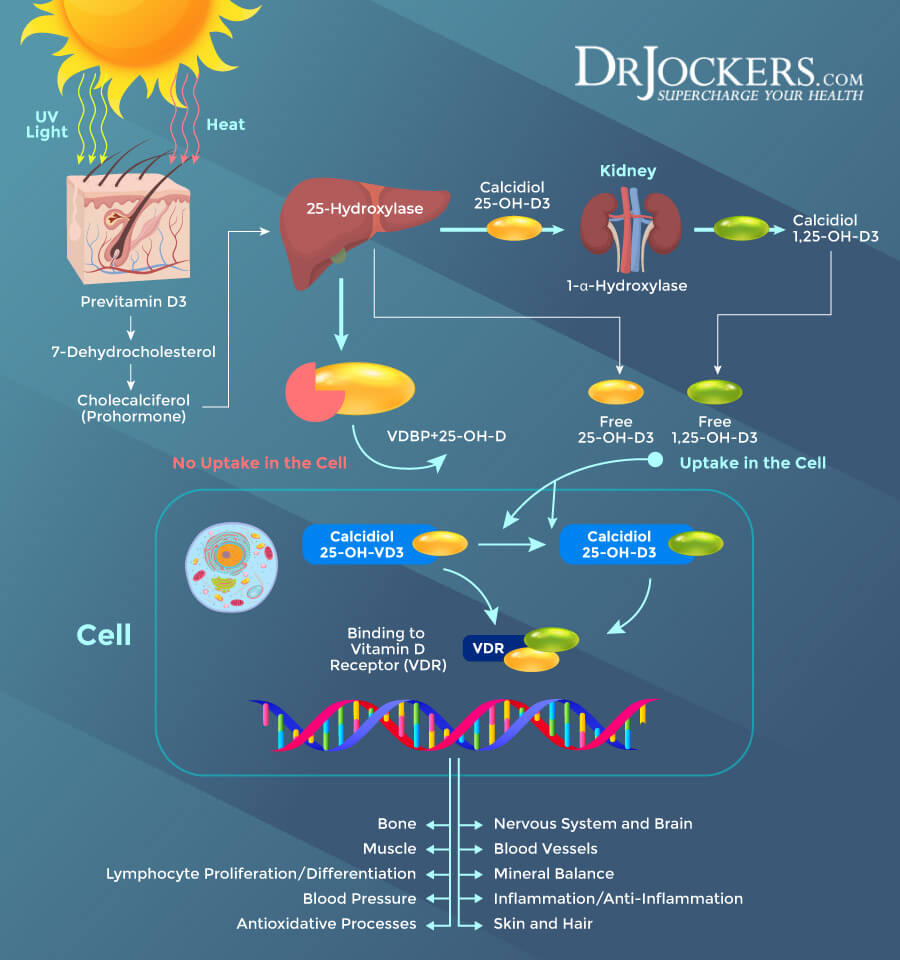
Vitamin D is a fat-soluble vitamin that’s critical for many areas of your health, including immune health, bone and muscle health, and brain and mental health. Vitamin D is obtained from the ultraviolet (UV) rays of the sun. When the UV rays reach your skin, it triggers vitamin D synthesis in your body.
Vitamin D is also available in certain foods, including fatty fish, including tuna, salmon, and mackerel, beef liver, egg yolks, and mushrooms. It is also available as a dietary supplement. Since it’s difficult to meet your needs through sunshine and diet alone, vitamin D supplementation is necessary for most people to maintain optimal vitamin D levels (1).
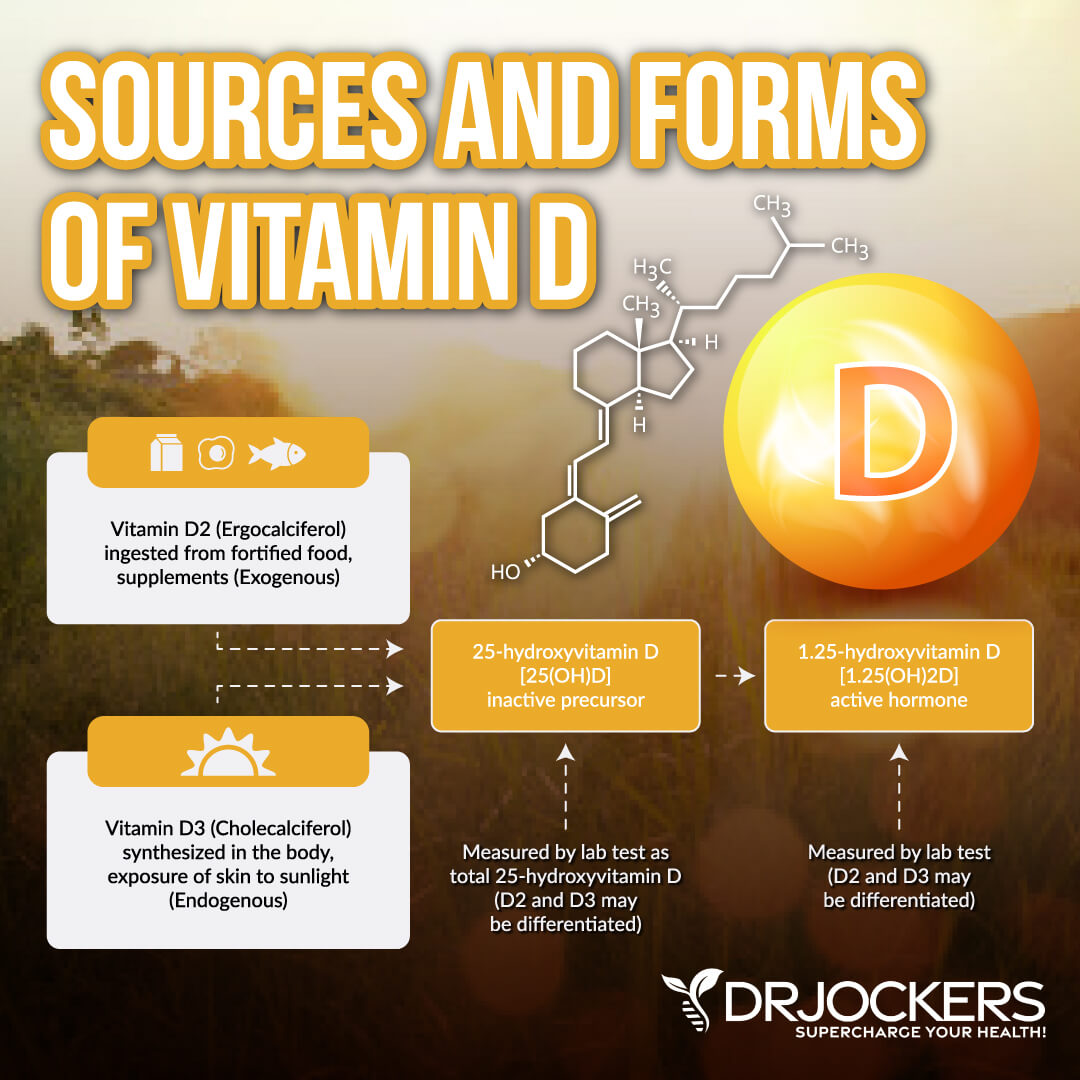
When you obtain vitamin D from sunshine or foods, it has to undergo two hydroxylations to get activated. The first hydroxylation takes place in your liver. This is where vitamin D converts into 25-hydroxyvitamin D (25(OH)D), or calcidiol. The second hydroxylation happens in the kidneys. This is where it changes into 1,25-dihydroxyvitamin D (1,25(OH)2D), or calcitriol, a physiologically active form of vitamin D (1).
Vitamin D supports calcium absorption, optimal serum calcium levels, and optimal phosphate concentration. It supports bone mineralization, bone growth, and bone strength. It helps to reduce the risk of osteomalacia, osteoporosis, muscle cramps , and muscle spasms. Vitamin D also helps to decrease inflammation. It supports immune health, neuromuscular function, glucose metabolism, and cellular growth (1).
Vitamin D and Immune Regulation
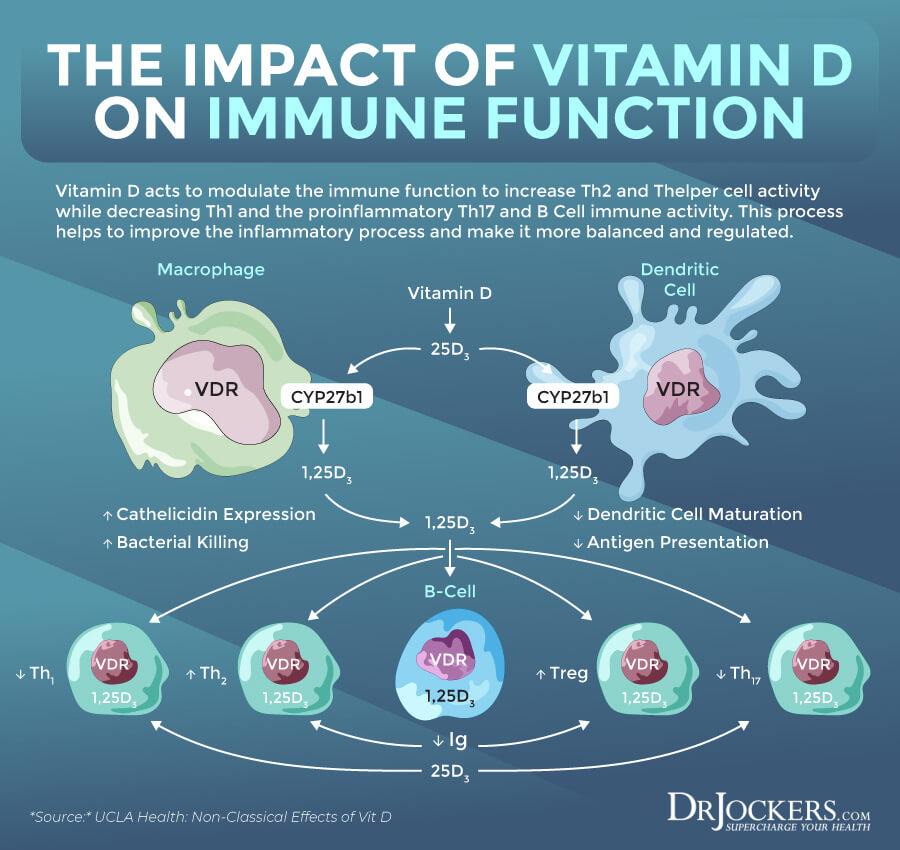
Vitamin D influences various physiological processes, including your immune function. According to a 2011 book, Vitamins and Hormones, 1,25(OH)2D, an active metabolite of vitamin D, plays a role in immune function regulation (2). Thus, it’s crucial for your innate and adaptive immune system and immune health.
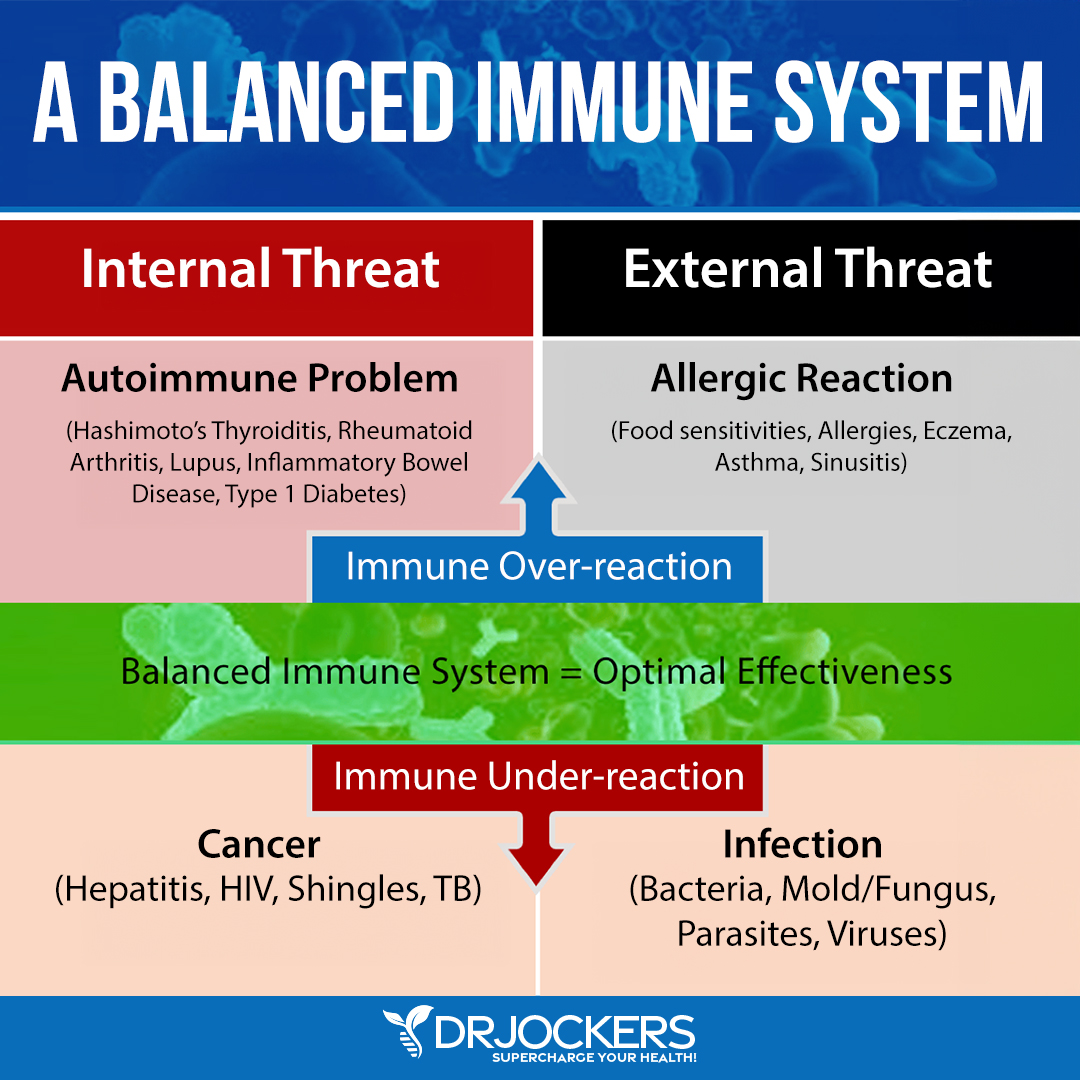
The authors found that vitamin D deficiency can result in immune dysfunction. Vitamin D deficiency can increase the risk of autoimmune diseases, including multiple sclerosis (MS) and type 1 diabetes. It can also increase the risk of infectious diseases, including tuberculosis and respiratory infections (2, 3). A 2018 review published in the International Journal of Molecular Sciences has found that vitamin D can reduce the risk of viral influenza infections (the flu) (3).
A 2011 study published in the Journal of Investigative Medicine has found that the vitamin D receptors are expressed on immune cells, including B cells, T cells, and antigen-presenting cells, which can synthesize active vitamin D metabolites and affect the immune system (4). Researchers found that vitamin D can affect the innate and adaptive immune response, and vitamin D deficiency can increase the risk of infections and autoimmunity.
A 2020 study published in JBMR Plus has found that 1,25(OH)2D plays a vital role in your immune function (5). They found that 1,25(OH)2D can increase autophagy in the body, and as a result, it can effectively fight infections. It helps to mediate T cell responses and reduce inflammation, and offer antibacterial and antiviral benefits. Researchers found that vitamin D supplementation can improve your immune health.
Vitamin D Deficiency and Autoimmunity
Emerging evidence suggests that vitamin D deficiency plays a role in and can increase your risk of autoimmunity. A 2013 review published in Clinical Reviews in Allergy and Immunology has found that vitamin D plays an important role in immune processes, T cell response, and modulating an immunological response (6).
They found that vitamin D receptor polymorphism and vitamin D deficiency can play a role in the development and symptoms of autoimmune diseases, including MS, systemic lupus erythematosus (lupus), and type 1 diabetes mellitus. In contrast, vitamin D supplementation may help to improve the progression and severity of these conditions.
A 2016 review published in the Scandinavian Journal of Rheumatology has found that vitamin D deficiency may increase the risk of autoimmune diseases, including MS, rheumatoid arthritis (RA), scleroderma or systemic sclerosis (SSc), primary biliary cirrhosis (PBC), and autoimmune thyroid diseases (7).
Another 2016 study published in Frontiers in Immunology has found that vitamin D deficiency may play a role in autoimmune diseases, including Crohn’s disease, RA, MS, lupus, and type 1 diabetes (8). They also found that vitamin D supplementation may offer immunomodulatory effects and may support the treatment of autoimmune conditions.
A 2017 review published in the Israeli Medical Association Journal has found that vitamin D deficiency is common in autoimmune diseases thus there may be a link between low vitamin D levels and autoimmunity (9). A 2019 review published in Autoimmune Reviews has also found that vitamin D deficiency may play a role in the pathophysiology of autoimmune diseases, including Crohn’s disease, ulcerative colitis, MS, SLE, seropositive RA, type 1 diabetes, psoriasis vulgaris, polymyalgia rheumatica, iridocyclitis, and thyrotoxicosis (10). Check out this article for more on vitamin D’s role in inflammation.
Healthy Sun Exposure
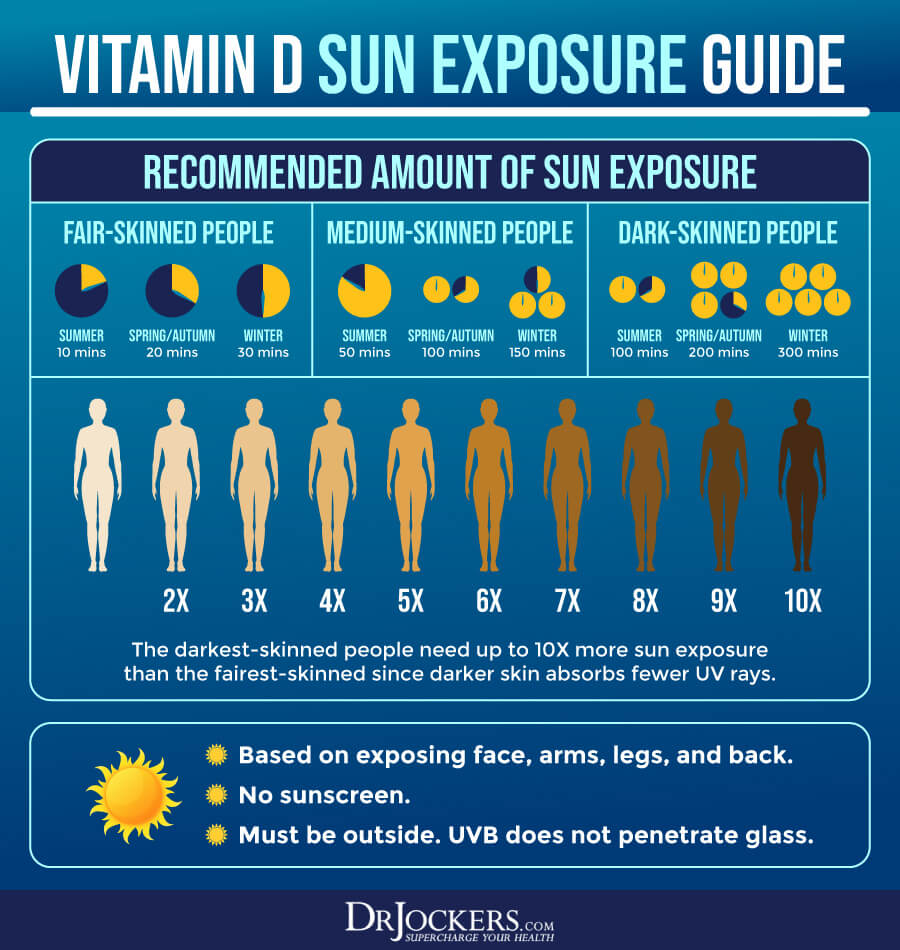
The sun is the best source of vitamin D. In areas where there is sufficient UVB exposure, there are several factors to consider in determining how much sun exposure is appropriate. These factors include the portion of skin exposed to the sun, the color of your skin, and the strength of the UV rays. If 60% of the body is exposed to the sun, it is ideal to seek 10,000 to 20,000 IU of vitamin D3 from sun exposure.
Intentionally sunbathe no less than 3 times per week according to the following recommendations based on your skin color:
- Light skin = 15–20 minutes daily
- Medium Skin = 25–30 minutes daily
- Dark Skin = 40–45 minutes daily
Obviously, our geographical locations and modern occupational demands and lifestyle habits make it very challenging to get this level of sun exposure on a regular basis for optimal vitamin D synthesis. This is why supplementing with vitamin D is so important for many individuals. But what if you struggle with vitamin D resistance?
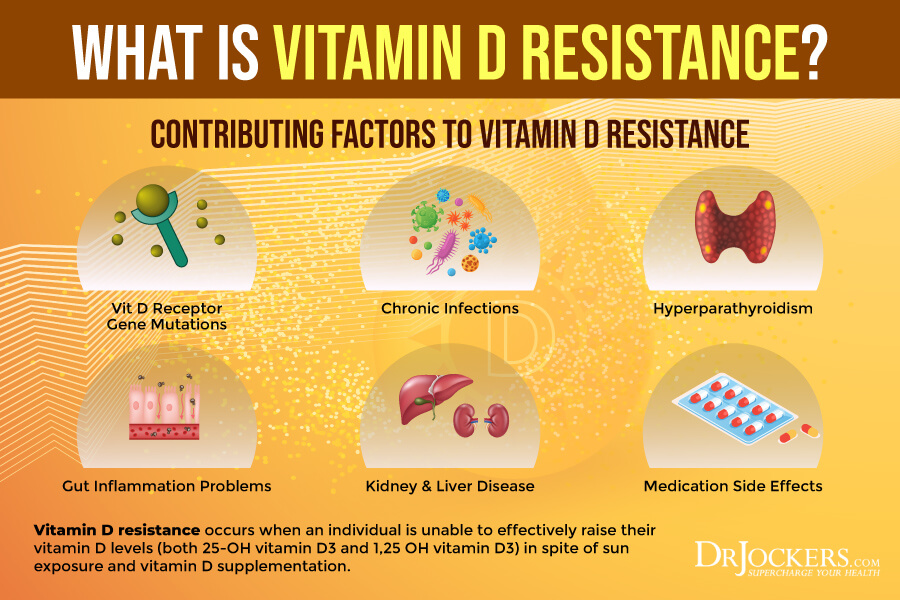
Vitamin D Resistance
A 2021 article published in Frontiers in Immunology has found that vitamin D resistance may be the underlying cause of autoimmunity (11). Researchers looked at the vitamin D serum markers of autoimmune patients where even high one-time doses of supplementation made a little difference. In one study that they looked at, about 55 to 62 percent of patients responded well to vitamin D supplementation. Other studies found similar results.
It turns out that while many patients are very responsive to vitamin D supplementations, others respond very little or not at all to the same dose. The authors of the paper suggest that vitamin D resistance may be the culprit, and in these cases, larger doses of vitamin D may down-regulate the immune system.
The papers suggest that many of the same factors that can result in chronic health issues may also cause vitamin D resistance. One of these issues is a genetic predisposition to polymorphism which may interfere with vitamin D function. Environmental factors, including reduced sunlight exposure, toxic exposure, and pathogens, may also increase the risk of vitamin D resistance.

This may interfere with enzyme activity necessary for the conversion of vitamin D from inactive to active. It may interrupt vitamin D transport across the body. It may impact the job of the vitamin D receptor (VDR) and other receptors to allow the body to use and store vitamin D.
Interference with VDR receptors is the most common issue. However, any problems within this system may interfere with your body’s ability to achieve optimal vitamin D levels. This polymorphism may increase the risk of autoimmunity.
The paper also discussed the role of VDR-related pathogens in vitamin D resistance and autoimmunity. We’ve long known that viruses and other pathogens can trigger autoimmunity and other chronic diseases. Pathogens can also interrupt vitamin D signaling pointing out a missing link between infections and autoimmune diseases.
The authors suggest that while testing for vitamin D is important, it’s not enough to determine vitamin D resistance. It’s important to also look for high parathyroid hormone (PTH) levels as vitamin D resistance is often accompanied by high PTH markers. Therefore, they recommend PTH as an accessible and reliable way to detect vitamin D resistance if other diseases and dietary issues have been ruled out. I will cover the importance of PTH balance in a later section.
Factors Involved in Low Vitamin D Levels
If you have low vitamin D levels, there may be a variety of contributing factors involved. Factors involved in low vitamin D levels include:
- Skin type: Having darker skin can lower your body’s ability to absorb UV from sunlight, therefore, decrease your body’s chance of producing vitamin D.
- Sunscreen: Protecting your skin is important, however, using a sunscreen with a high sun protection factor (SPF) can decrease your body’s ability to synthesize vitamin D. According to a 2013 study published in Dermatoendocrinology, this reduction may be 95 to 98 percent when using SPF 30 or over (12).
- Skin covering: The sun has to meet your skin to produce vitamin D. Clothing over the skin can inhibit vitamin D production.
- Geography: Living in Northern areas of the world with less sunlight or in areas with high populations reduces your ability to get vitamin D from the sun.
- Indoor lifestyle: Working nightshifts, not spending much time outdoors, or being homebound for any reason also decreases your chances of getting vitamin D from the sun.
- Diet: Not consuming foods that are rich in vitamin D also reduces the opportunity to get optimal levels of vitamin D. Since most foods that are rich in vitamin D are animal-derived, this can be a particular problem for vegans and vegetarians.
- Breastfeeding: Breastfeeding is the best way to nurture your baby. However, it is important to give vitamin D supplements to infants who are exclusively breastfed, especially if they don’t get much sun or have darker skin. The American Academy of Pediatrics and the Centers for Disease Control and Prevention (CDC) recommend 400 international units (IUs) of vitamin D per day to breastfed infants (13).
- Age: As people age, their kidney’s ability to convert vitamin D to its active form also decreases which increases the risk of low vitamin D levels.
- Gut problems: Crohn’s disease, celiac disease, cystic fibrosis, and other health issues can reduce your body’s ability to absorb vitamin D from food which can result in lower vitamin D levels.
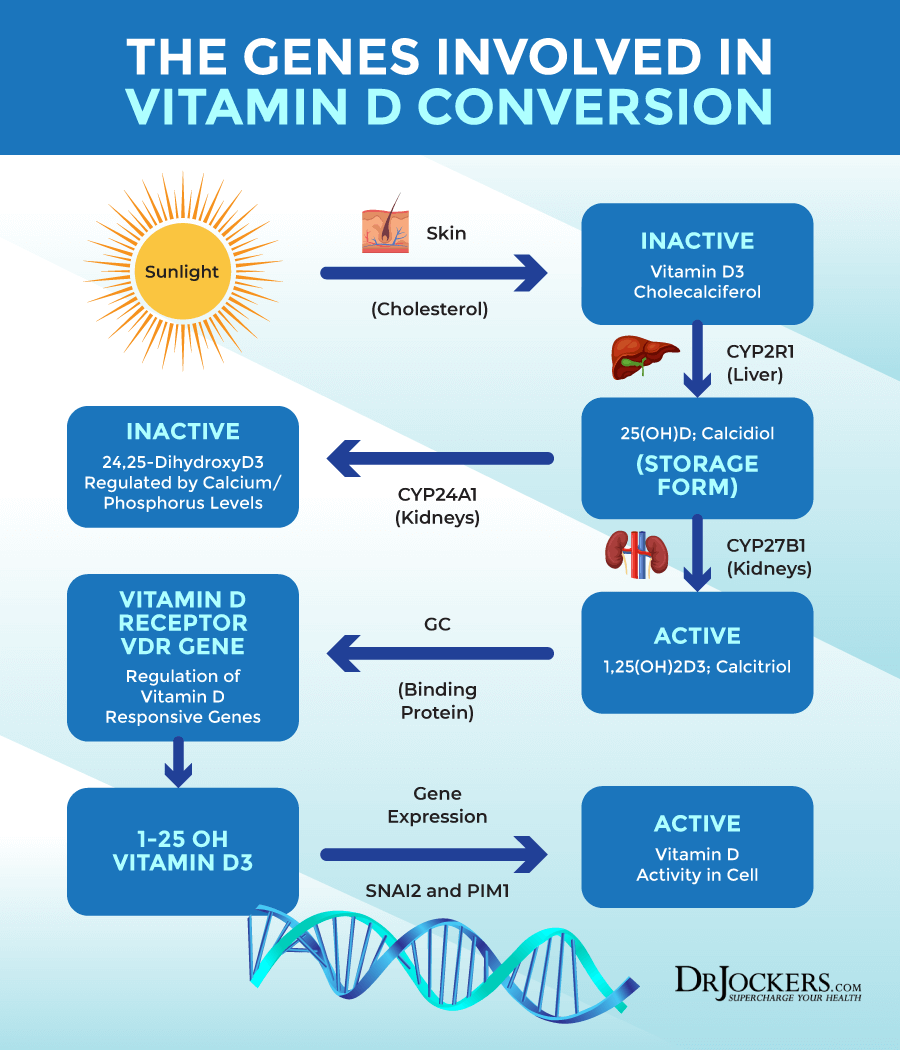
- Genetic Polymorphisms: Key genes that impact vitamin D conversion include CYP2R1, CYP27B1, GC Binding Protein and the VDR Receptor. More info on these later in the article.
- Obesity: Individuals with a body mass index 30 and over can result in reduced blood levels of vitamin D.
- Weight loss surgeries: Weight loss surgeries that reduce the size of the stomach or bypass the small intestine can make it difficult to consume enough macronutrients and may reduce your ability to obtain enough vitamin D from food.
- Hyperparathyroidism: Parathyroid Hormone (PTH) works to maintain calcium and phosphorus levels. High PTH levels (as seen in hyperparathyroidism) will inhibit the hydroxylation of 25-OH vitamin D to the active 1,25 OH vitamin D levels.
- Kidney and liver problems: Kidney and liver diseases decrease the amount of enzyme necessary to change vitamin D into 25(OH)D then into 1,25(OH)2D so the body can use it. Lower levels or lack of these enzymes can result in low levels of active vitamin D.
- Magnesium or Vitamin A Deficiencies: Both magnesium and vitamin A are critical players in the conversion and utilization of vitamin D.
- Medications: Certain medications, including certain laxatives, steroids, seizure, cholesterol-reducing, weight loss, and tuberculosis medication can lower vitamin D levels in your body.
- Lack of supplementation: Meeting your vitamin D needs through sunshine and food alone can be difficult. Most people require supplementation with vitamin D. Without vitamin D supplementation, you may experience low levels of vitamin D, even if you are consuming foods rich in vitamin D and spend time outdoors.
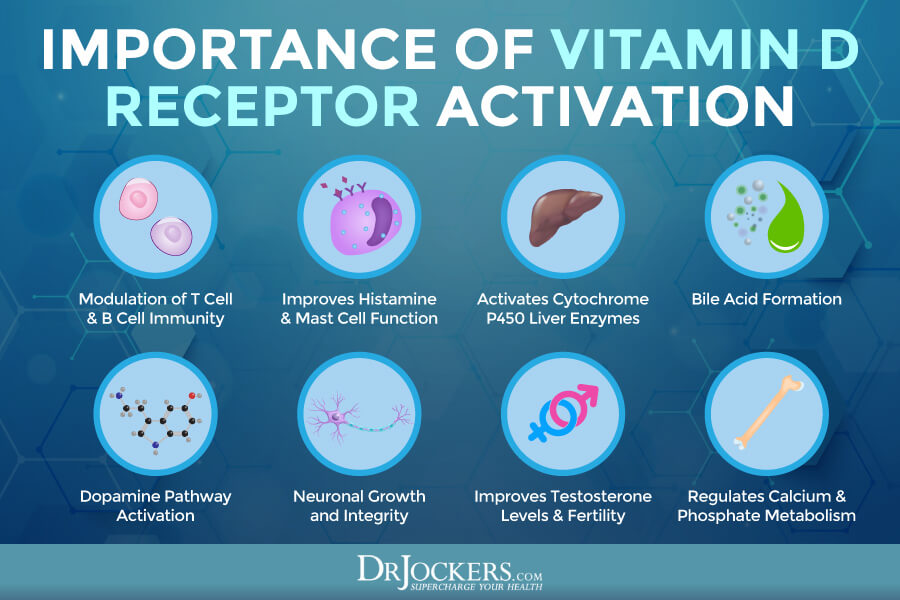
Importance of Vitamin D Receptor Activation
Vitamin D is not enough. Your body needs it in its active form, 1,25(OH)2D, or calcitriol. Many physiological functions get activated when calcitriol binds to the nuclear VDR receptor site making calcitriol essential for these bodily functions.
Functions that VDR activation is necessary for include:
- Modulation of immune T-cell & B-cell behavior: According to a 2015 study published in Nutrients, calcitriol can regulate the T cells and promote an anti-inflammatory response through anti-inflammatory T-regulatory cells (TREGs) (14).
- Mast cell inhibitory effects: According to a 1996 study published in the Archives of Dermatology Research, calcitriol may inhibit the effects of mast cells, hence decreases histamine release, histamine intolerance, and inflammation (15).
- CYP3a4 activation: According to a 2010 study published in Biochemical Pharmacology, VDR can activate CYP3a4, which is the most abundant cytochrome P450 liver enzyme and plays an important role in metabolism and hormonal health (16).
- Bile acid formation: According to a 2008 study published in the Journal of Lipid Research, Lithocholic Acid, a bile acid can activate VDR (17).
- Dopamine pathway activation: According to a 2015 study published in Neuroscience, calcitriol and VDR activation play a role in dopamine pathway activation by regulating tyrosine hydroxylase expression (18).
- Neural growth and integrity: According to a 2014 study published in Noro Psikiyatri Arsivi – Archives of Neuropsychiatry, VDR activation supports nerve growth factor (NGF) release (19).
- Testosterone levels, sperm count, and fertility: According to a 2012 study published in Clinical Endocrinology (Oxford), VDR activation supports testosterone synthesis and other sexual reproductive processes (20).
- Calcium and phosphate metabolism: According to a 2007 study published in the Journal of Steroid, Biochemical and Molecular Biology, calcitriol and VDR activation are necessary for the regulation of calcium and phosphate mineral metabolism (21).
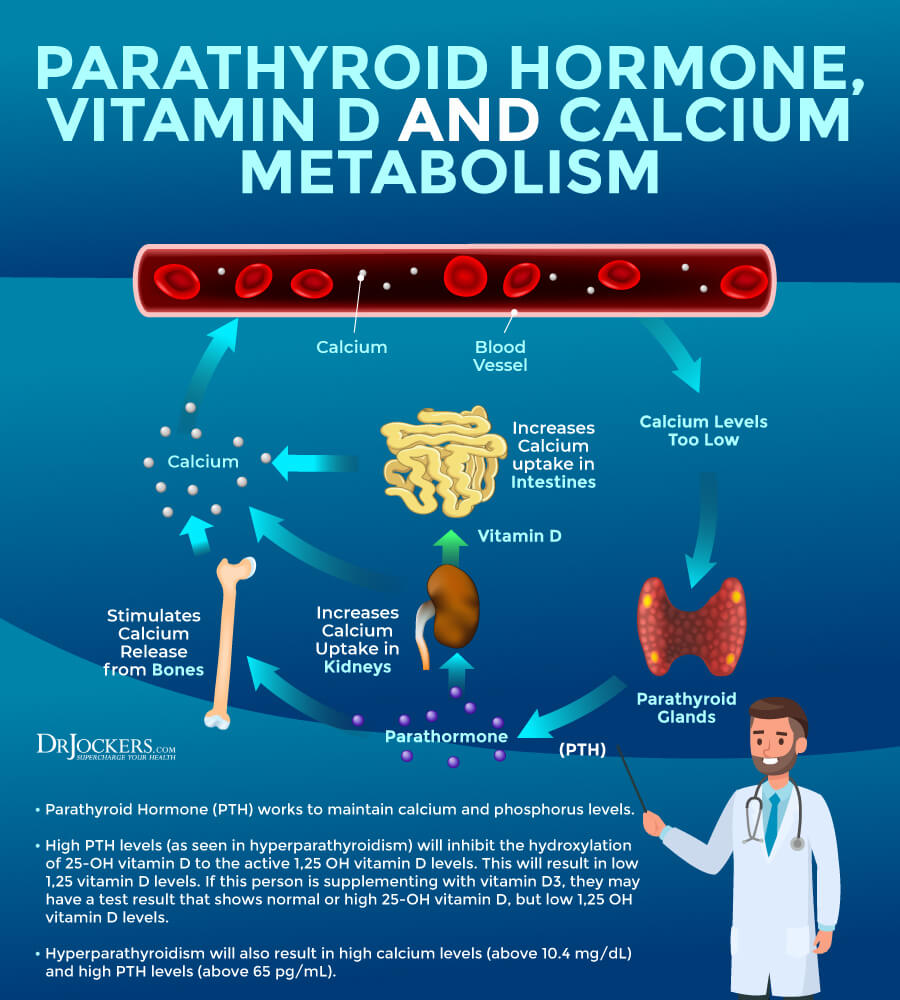
Vitamin D and PTH Balance
Vitamin D plays a role in autoimmune thyroid conditions and the parathyroid hormone (PTH) may impact your vitamin D and calcium levels. According to a 2017 study published in the International Journal of Dermatology, VDR inactivation may result in hair loss, which is a common symptom of Hashimoto’s thyroiditis (22).
A 2015 study published in Endokrinologia Polska has found that the Epstein Barr virus (EBV) may cause autoimmune thyroid issues (23). According to a 2010 study published in Cell Molecular Life Sciences, however, EBV can also result in VDR inactivation (24). This suggests a connection between EBV, vitamin D problems, and autoimmune hypothyroidism.
According to a 2014 study published in Mithochonrion, endotoxins from gram-negative bacteria can also cause VDR inactivation and Hashimoto’s thyroiditis (25). Endotoxins trigger a so-called cell danger response (CDR), which results in the upregulation of CYP24a1 (24α-hydroxylase) and causes the creation of an inactive form of calcitriol.
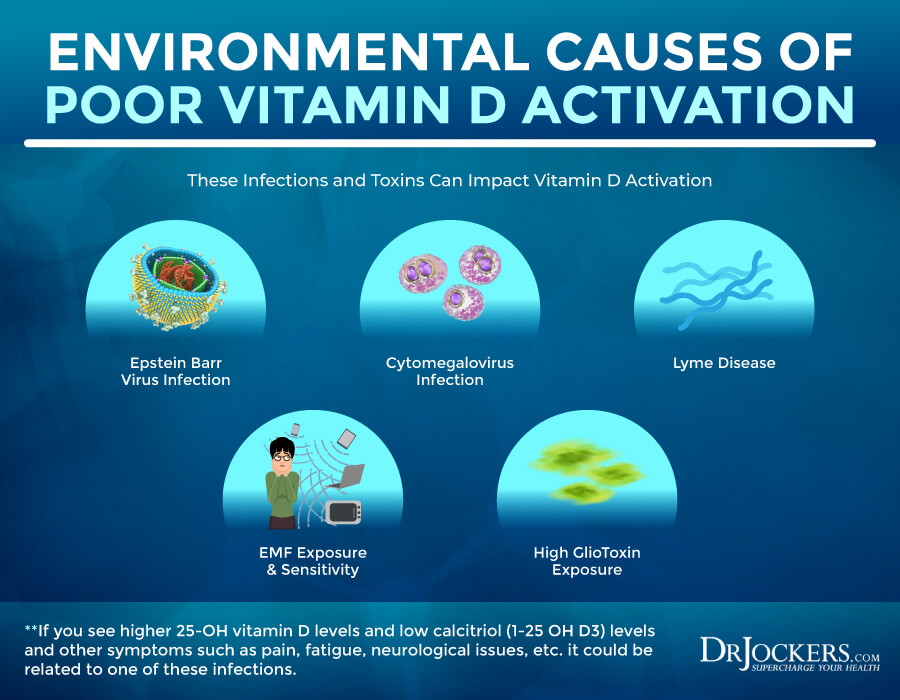
25-OH Vitamin D to Calcitriol Conversion
Normal conversion from 25(OH) vitamin D to calcitriol is critical. If your 25(OH) vitamin D levels are higher than your calcitriol levels, it may be the result of various infections and other issues, including:
- Epstein Barr virus (EBV): According to a 2010 study published in Cell Molecular Life Sciences, however, EBV can also result in VDR inactivation (24).
- Cytomegalovirus (CMV): According to a 2017 study published in the Journal of Steroids, Biochemical and molecular Biology, CMV infections may cause VDR downregulation (26).
- Borrelia burdorferi, Lyme bacteria: According to a 2018 study published in the International Journal of General Medicine, there may be an interconnection between VDR inactivity and Lyme disease (27).
- Electrosmog: According to a 2017 study published in Immunology Research, electrosmog, such as WiFi radiation, may result in VDR dysfunction and contribute to autoimmunity (28).
- Gliotoxin: According to a 2012 study published in the American Journal of Respiratory Critical Care and Medicine, gliotoxins produced by spergillus fumigatus can interfere with VDR expression (29).
It is not surprising that vitamin D resistance and vitamin D deficiency are common among those with autoimmune disease, Lyme disease, and other chronic diseases. Their 25(OH)d levels tend to be higher than normal. These issues may interrupt VDR activation, cause vitamin D resistance. This explains why vitamin D supplementation may not always work for some individuals.
Vitamin D Genes
There are certain genetically coded enzymes that are critical for the conversion of sunlight into active 1,25 (OH) vitamin D and active vitamin D activity within the cell. The CYP2R1 gene encodes for hepatic 25-hydroxylase in the liver that converts cholecalciferol into 25 (OH) vitamin D. Studies have shown that mutations in this gene can cause a form of vitamin D resistance and vitamin D deficiency (30, 31, 32).
The kidney has major gene called CYP27B1 that codes for the 1-alpha-hydroxylase enzyme which is necessary in converting the inactive 25 (OH) vitamin D to the active 1,25 (OH) vitamin D. Polymorphisms in this gene can impact the conversion and lead to vitamin D resistance and vitamin D deficiency (33, 34).
The next gene involved is the GC binding protein and severe mutations can cause vitamin D resistance and vitamin D deficiency (35, 36). The Vitamin D receptor gene (VDR) may also be mutated and slow down the process of vitamin D upregulation into the cell leading to a form of vitamin D resistance and vitamin D deficiency (37, 38).
Information is still coming out on the percentages of these gene polymorphisms but you can get your genes tested through companies like 23andme.com to see if you have any homozygous mutations here that may be impacting your vitamin D conversion and cellular utilization pathways.
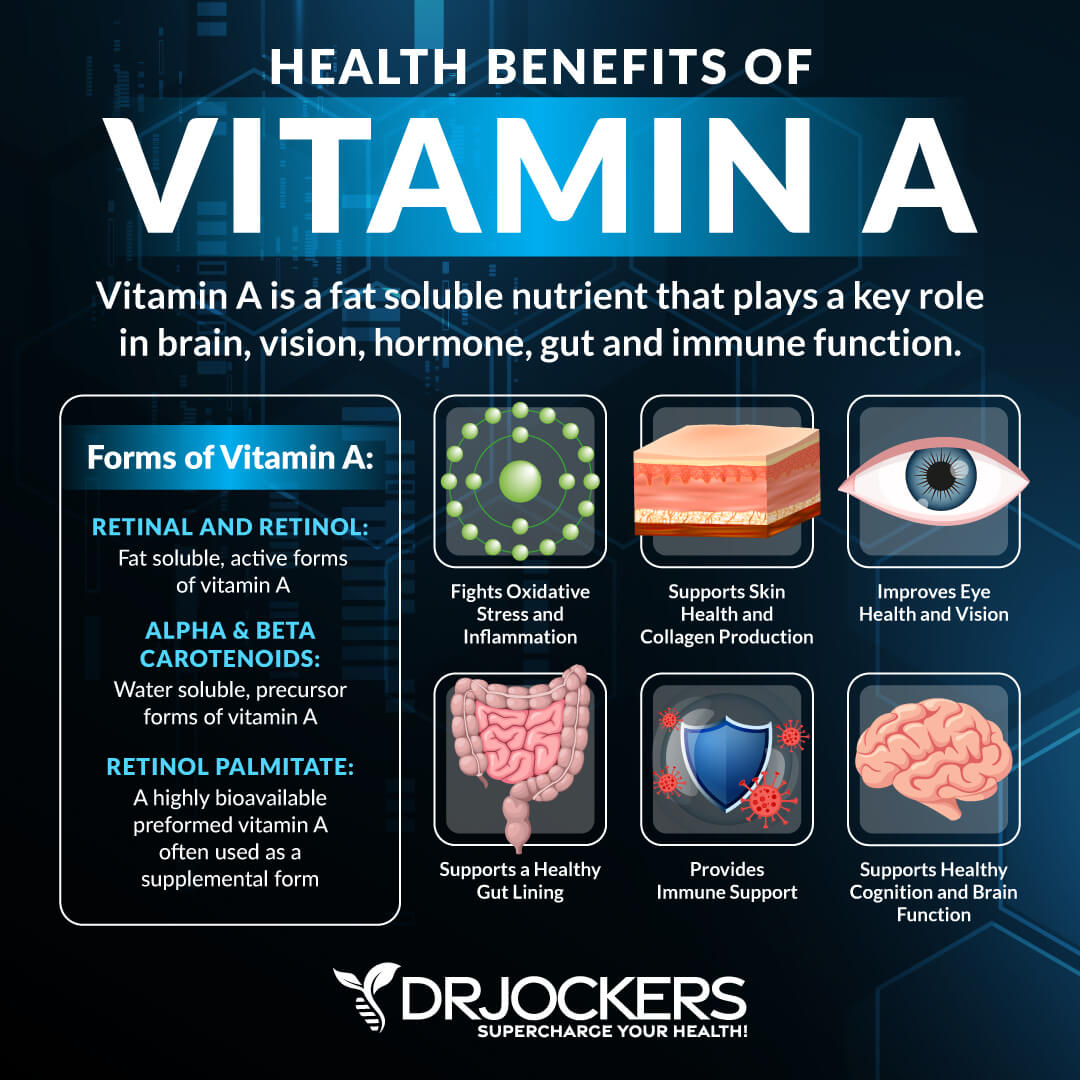
Importance of Vitamin A
Vitamin D and vitamin A (retinol) are connected and work together. Calcitriol binds to the VDR in the cell nucleus. Once this happens, the vitamin A receptor (RXRA and RXRB) helps the activation of the VDR targets. A 2008 study published in the National Reviews in Immunology has found that vitamin D and A play an important role in various immune processes and may help to prevent or treat inflammation and autoimmunity (39).
Besides immune health, vitamin A is also critical for eye, bone, skin health, healthy growth, and reproduction. Optimal vitamin A levels are between 35 and 60 ug/dl. If you are taking supplemental vitamin D and not seeing positive changes in your health, it is wise to test your vitamin A levels as well to make sure you are sufficient.
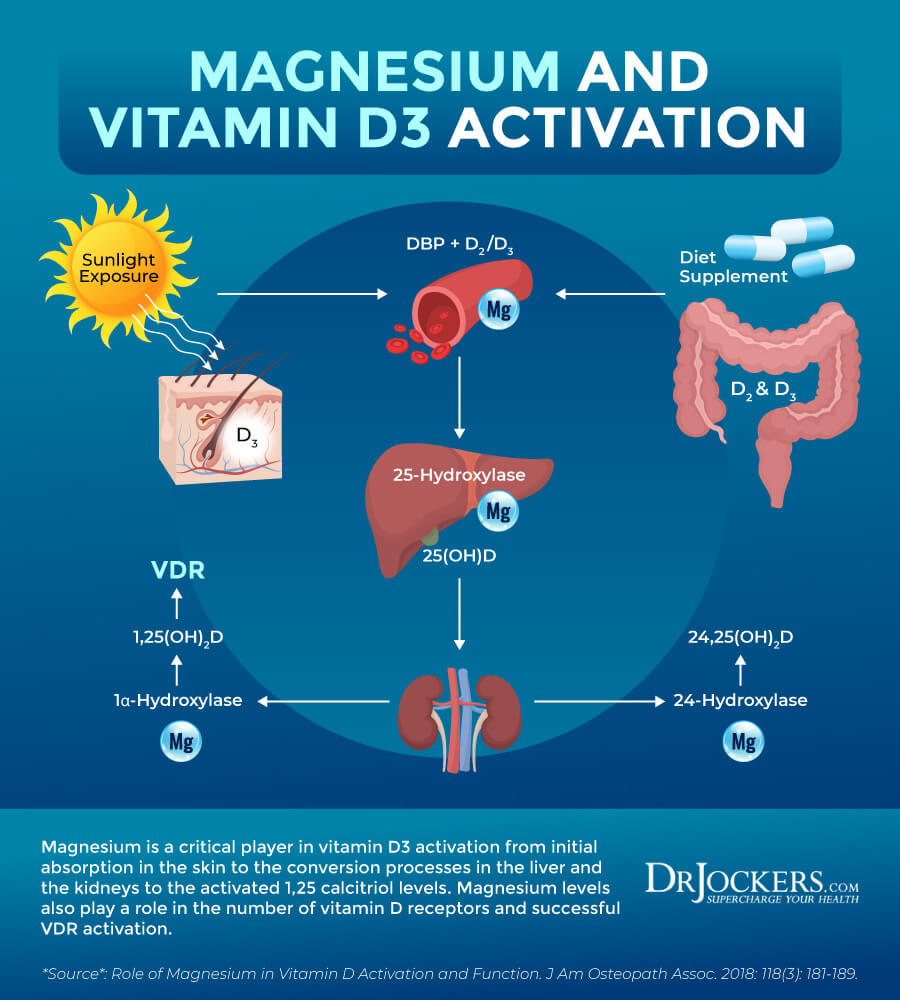
Importance of Magnesium
Magnesium is an essential cofactor for vitamin D synthesis, and activated vitamin D, in turn, can increase intestinal absorption of magnesium and, therefore, can form a feed-forward loop to maintain its homeostasis. Studies have suggested that magnesium could influence PTH synthesis and determine the number of vitamin D receptors; therefore, a deficiency in magnesium levels may lead to diminished synthesis and secretion of PTH and a reduced number of available vitamin D receptors in the target cells (40).
Additionally, magnesium also plays an important role in the conversion of the inactive form of vitamin D in the liver to 25-OH D3 and then into the active 1,25 calcitriol in the kidneys. A magnesium deficiency would lead to poor uptake and conversion of D3 and symptoms associated with vitamin D3 deficiency (41).
Taking Vitamin D3 with K2
Vitamin D is essential for ensuring that the calcium levels in your blood are high enough. However, vitamin D is not enough. Vitamin K helps to regulate calcium in your body. According to a 1986 review published in Haemostasis, vitamin K activates osteocalcin, which is a protein that ensures calcium build-up in your bones and teeth thus helps calcification of your bones (42). According to a 2012 review published in Advanced Nutrition, vitamin K helps to decrease calcification of soft tissues by activating the matrix GLA protein that prevents calcium build-up in your blood vessels, kidneys, and other soft tissues (43).
When you are choosing vitamin K, I recommend that you look for menaquinone-7 (MK-7) instead of menaquinone-4 (MK-4). MK-4 is a short-chain menaquinone found in egg yolks, butter, and other animal foods. MK-5 to MK-10 are longer chain menaquinones found in fermented foods. MK-7 is the predominant form of menaquinone found in natto, a Japanese fermented soy food.
A 2015 clinical trial published in the Natural Medicine Journal has found that MK-7 is more bioavailable and offers more benefits over MK-4 (44). To improve your vitamin D and K levels, I recommend vitamin D3/K2 Power and Liposomal D3 with K2, both made with MK-7.
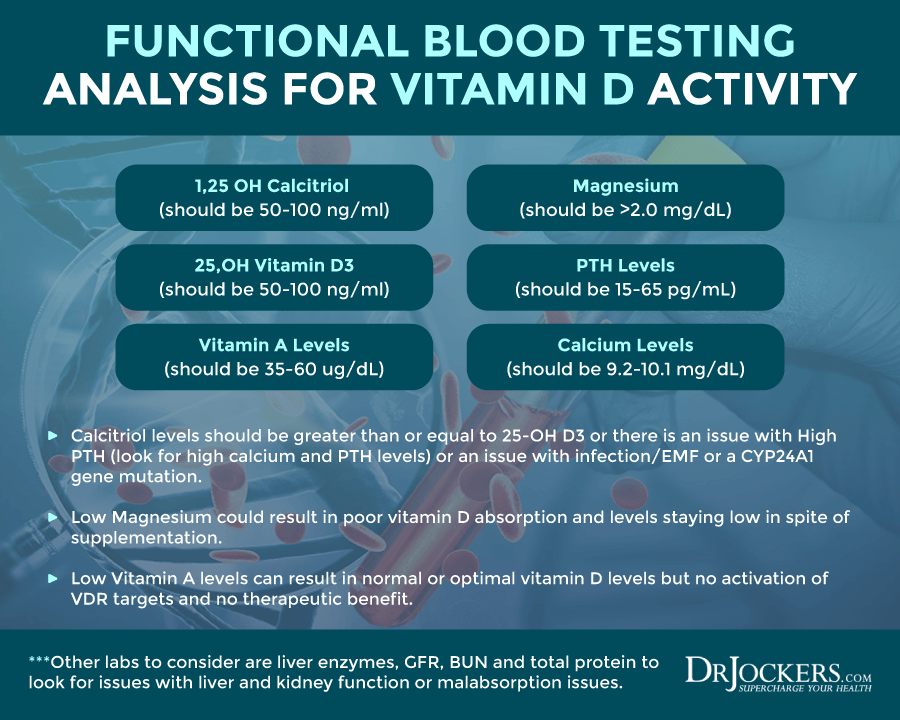
Testing Vitamin D Levels
When analyzing vitamin D levels, it is important to put all of this information together. You want to find a lab that will look at 1,25-OH Calcitriol levels, 25-OH cholecalciferol D3, vitamin A levels, magnesium, calcium and PTH levels. Here are the functional ranges for these.
1,25 OH Calcitriol (should be 50–100 ng/ml)
25,OH Vitamin D3 (should be 50–100 ng/ml)
Vitamin A Levels (should be 35–60 ug/dL)
Magnesium (should be >2.0 mg/dL)
PTH Levels (should be 15–65 pg/mL)
Calcium Levels (should be 9.2–10.1 mg/dL)
Calcitriol levels should be greater than or equal to 25-OH D3 or there is an issue with High PTH (look for high calcium and PTH levels) or an issue with infection/EMF or a CYP24A1 gene mutation. Low Magnesium could result in poor vitamin D absorption and levels staying low in spite of supplementation.
Low Vitamin A levels can result in normal or optimal vitamin D levels but no activation of VDR targets and no therapeutic benefit. Other labs to consider are liver enzymes, GFR, BUN and total protein to look for issues with liver and kidney function or malabsorption issues.
Comprehensive Blood Panel
I recommend a Comprehensive Blood Analysis (CBA). This test is more sophisticated than most conventional doctors are able to order. This test looks at your 25(OH), 1,25(OH), vitamin A, PTH, calcium, magnesium and inflammatory markers.
It also offers a complete metabolic panel, complete blood count, liver function markers, blood sugar levels, nutrient deficiencies, and more. I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your progress.
Final Thoughts
Vitamin D is important for immune function and other areas of your health. Vitamin D deficiency may play a role in autoimmunity, and it can be related to a number of factors.
While most people see results when taking vitamin D, others have vitamin D resistance and don’t see improvement despite supplementation. I recommend a Comprehensive Blood Panel to test for vitamin D deficiency, vitamin A and calcium levels, and inflammatory markers, and take vitamin D3/K2 using MK-7.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




Where May we order the lab panel mentioned in this article?
Hey Theresa – here it is: https://drjockers.com/comprehensive-blood-analysis/
Thank you so much. Is there an additional fee to review the labs. Would this in any way tell whether one was Vit D resistant?
Our coaches will do a short follow up with you on the lab to review the results and yes the comprehensive blood analysis looks for the factors involved in vitamin D resistance.
Please Dr. Jockers, what is the best brand of vitamin D I can take if I have multiple gene mutations related to Vitamin D?
Thank you!
Hello Johanna,
Yes we would recommend this one here: https://store.drjockers.com/products/micelle-liposomal-d3-k2?_pos=2&_sid=644e766a6&_ss=r
I have had problems with consuming Vitamin D for many years – doesn’t matter what form it is. My calcitriol levels tend to be in your recommended range, but my Vitamin D 25, Hydroxy levels are almost non-existent (last test was done 2+ years ago showed calcitriol at 86.3 and vitamin D 25, hydroxy at 6.2).
Taking any Vitamin D supplements causes terrible side effects (EXTREME fatigue, mood issues, and joint pain). I have tried multiple forms of the D3 supplements – both with and without K-2. I have also tried taking a boron supplement. Nothing helps. My current multivitamin has about 200 IU of Vitamin D2.
My genetic testing was inconclusive for genetic defects. I have NEVER tested positive for Epstein Barr or Lyme Disease – been tested multiple times. Also my parathyroid levels have always been normal.
Any suggestions? Or should I just continue to ignore the problem?
Hello Christine,
This is an interesting case. It may be a lab error to have such a discrepancy between calcitriol and 25-OH. If that lab was 2 years ago, I would be sure to get new labs and would recommend the comprehensive blood analysis to be able to look at the factors discussed in this article. https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
What do we do if we might have vitamin D resistant if we have Lyme or EPSTEIN Barr? Should we take more vitamin D??
Yes higher dosages and working on reducing the bacterial and viral loads is important.
Interesting article, but there may be a few things missing, morning sun exposure in Florida 8 to 9:30 AM by walking outside, after that the sun may be to strong up north may be different. Go swimming great sun exposure. Now here are my questions d3 needs magnesium for better absorption as per your article what about zinc? was mentioned the last 2 years, vitamin c, so what kind of vitamins would you suggest maybe more than one. Thanks
Yes magnesium is critical for vitamin D utilization. Zinc is not as important for vitamin D function but overall very important for a wide variety of issues.
Excellent summary article!
I was diagnosed with HT in 2018, and tried (with no success) various methods to find the root cause of my autoimmune response. The Frontiers In Medicine article in 2021 was a real breakthrough for me, and since then I’ve confirmed vitamin D resistance in myself and have reverse-engineered the Coimbra protocol, and (working with my endocrinologist) have seen my PTH levels go from 77 to 28 pg/mL (I’m aiming for 20), and my TPO AB go from 312 to 79 IU/mL. (I’m expecting another drop next month when I’m tested again, and obviously, my goal is to be as near to 0 as possible.)
Maybe I’ll win over one or two of my allopathic medical doctors to some of the advantages of a functional medicine approach. From the fifty thousand foot view, it should be pretty obvious that what we’re doing in our current western medical system has some huge problems. (We’re still very good at acute medical care – it’s chronic diseases and “one size fits all” that are literally killing us. Imagine how ludicrous it would be to take your car into a shop that brags about only using one “standard” repair manual for all vehicles.)
You did a great job summarizing where we are now in research in this area. One thing I found extremely helpful was the genetic confirmation of variant SNPs in my VDR and CYP2R1 genes. However, while I started with 23&Me, I was frustrated at how often they had not sequenced relevant nucleotides of interest because they only read about .02% of the genome. For about 1/3 more in price, I was able to get my entire genome parsed 30X (Nebula), and that has been incredibly helpful, especially in discussions with doctors, who respond better to data than anecdotes or “Dr. Google”. You might consider recommending full genome sequencing for people who really want to take the reins in their health and who enjoy doing some of their own research.
Thanks for sharing that!