 No Gallbladder: Strategies to Improve Digestive Health After Surgery
No Gallbladder: Strategies to Improve Digestive Health After Surgery
Did you know that about 600,000 people get their gallbladders removed each year? Did you know that about half of these people still experience digestive problems even after surgery? It doesn’t have to be this way. You can support your digestive health after surgery to create smooth digestion and live without symptoms. If you don’t have a gallbladder or are about to go through gallbladder removal surgery and want to improve your digestive health, this article is for you.
In this article, I will discuss the role of the gallbladder, the symptoms and major causes of gallbladder disease, and the prevalence of gallbladder surgeries. I will share my best digestive strategies to support your body after gallbladder surgery.
Role of the Gallbladder
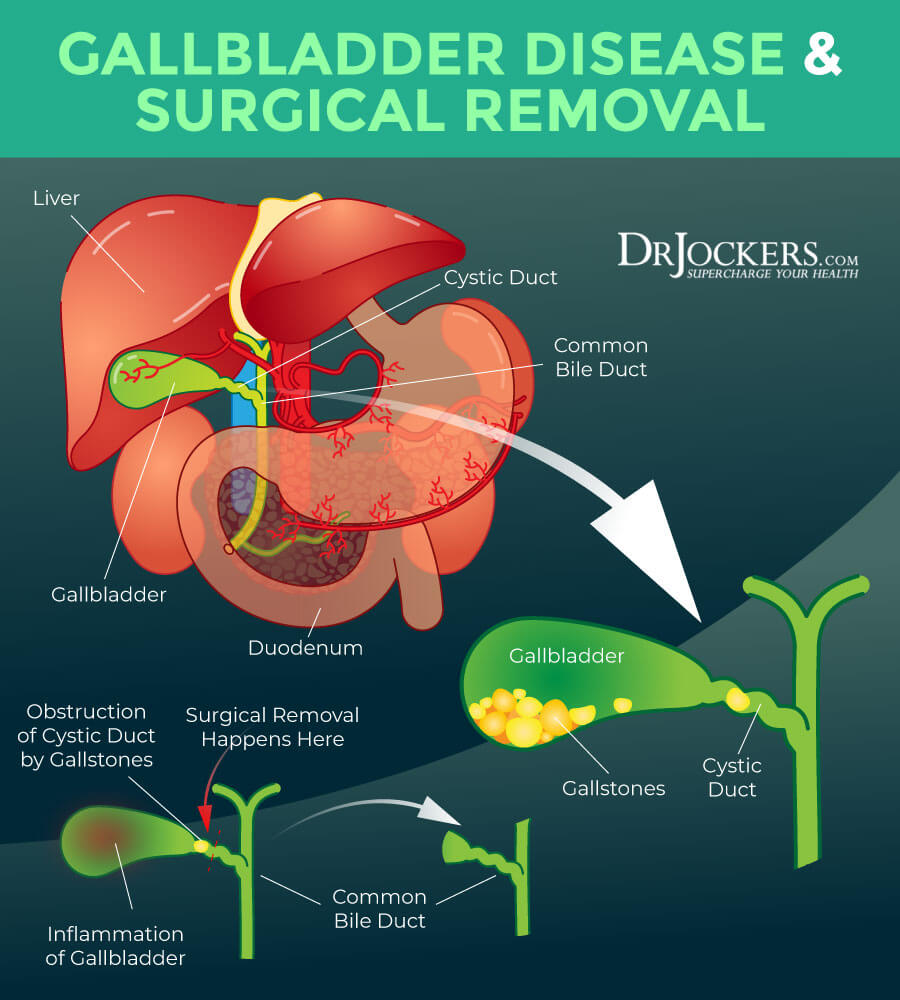
Your gallbladder is a thin-walled, pear-shaped, hollow, sack-like organ. It is located on the right side of your abdomen under your liver. It is about 2.7 to 3.9 inches long and 2 inches at its widest point.
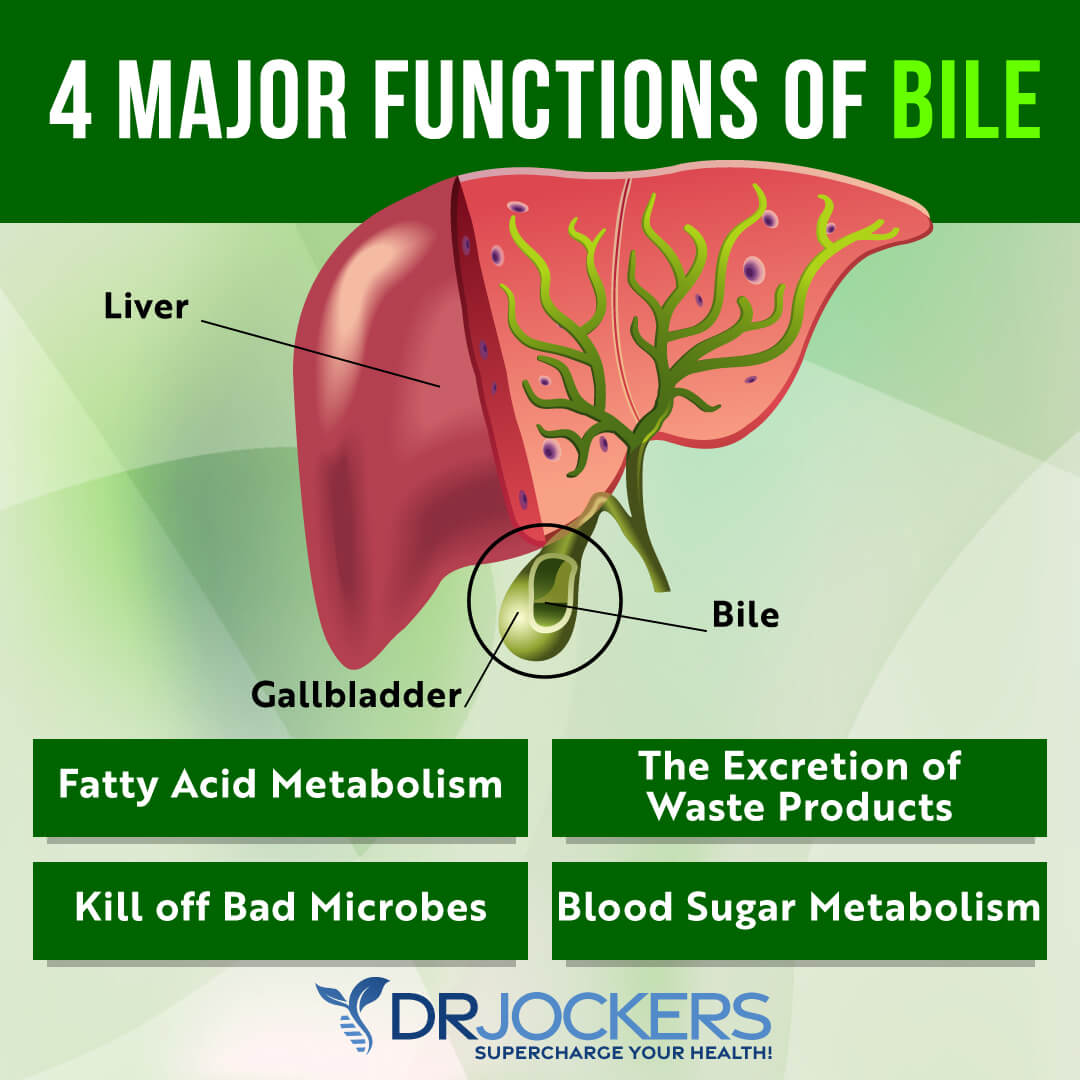
The main function of your gallbladder is to store and concentrate a yellow-brown digestive enzyme called bile created by your liver. Bile is made up of water, salt, cholesterol, lecithin, and bile pigments called bilirubin, created by your red blood cells. Bile allows your body to break down and absorb fats from your food.
Your liver produces between 27 and 34 fluid ounces of bile daily. They secrete them into your bile duct, which ends at your small intestines. During meals, the bile flows into your small intestine, and between meals, it is stored in your gallbladder, which holds between 1 to 2.7 fluid ounces of bile at one time.
When you eat fatty food, your gallbladder releases bile to mix with semi-ingested food and help to break down larger fat particles into smaller fat droplets to be further broken down with the help of digestive enzymes from your pancreas (1, 2, 3).
Symptoms of Gallbladder Disease
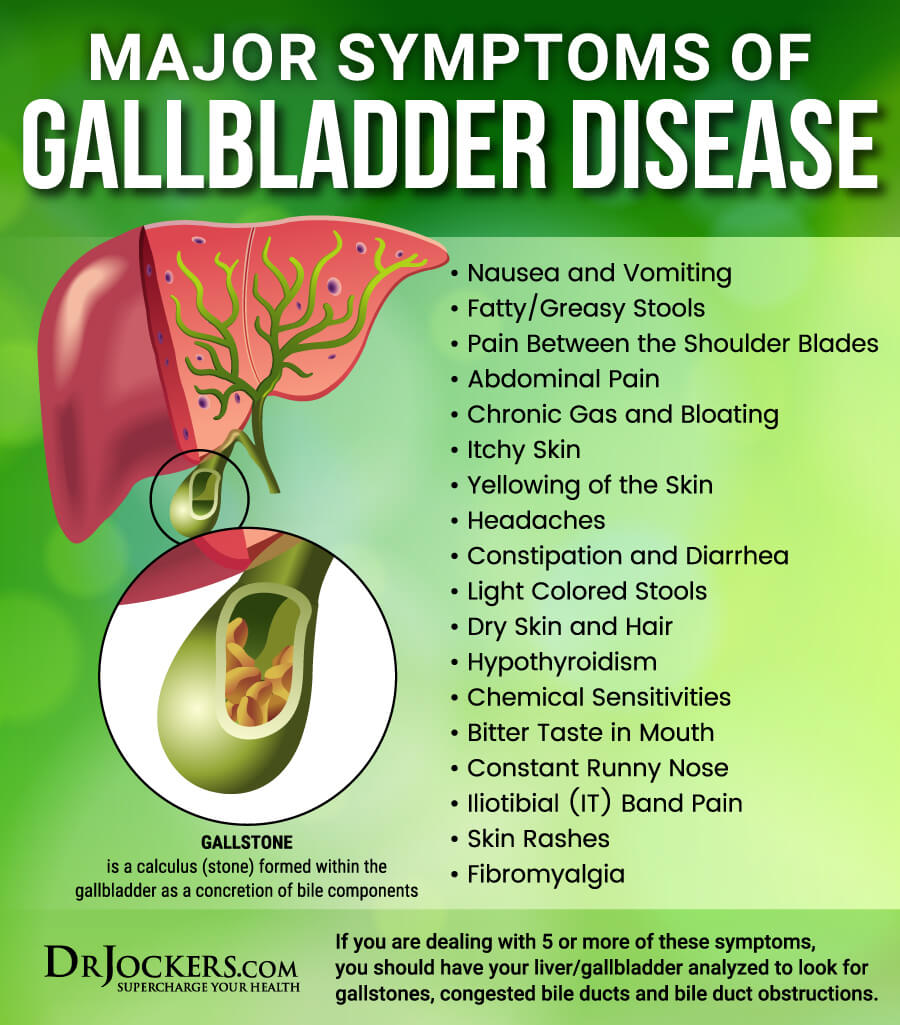
Gallbladder disease has a wide range of symptoms, including:
- Nausea
- Vomiting
- Fatty and greasy stools
- Pain between the shoulder blades
- Abdominal pain
- Bloating
- Gas
- Headaches and migraines
- Constipation
- Diarrhea
- Light-colored stools
- Sexual dysfunction
- Bitter taste in the mouth
- Fibromyalgia symptoms
- Hypothyroidism
- Loss of hunger
- Itchy skin
- Yellowish skin
- Dry skin and hair
- Skin rashes
- Chemical sensitivities
- Weight loss resistance
- Constant runny nose
- IT band pain
- History of prescription, over-the-counter, or illegal drug use
To learn more about the symptoms of gallbladder disease, I recommend reading this article.
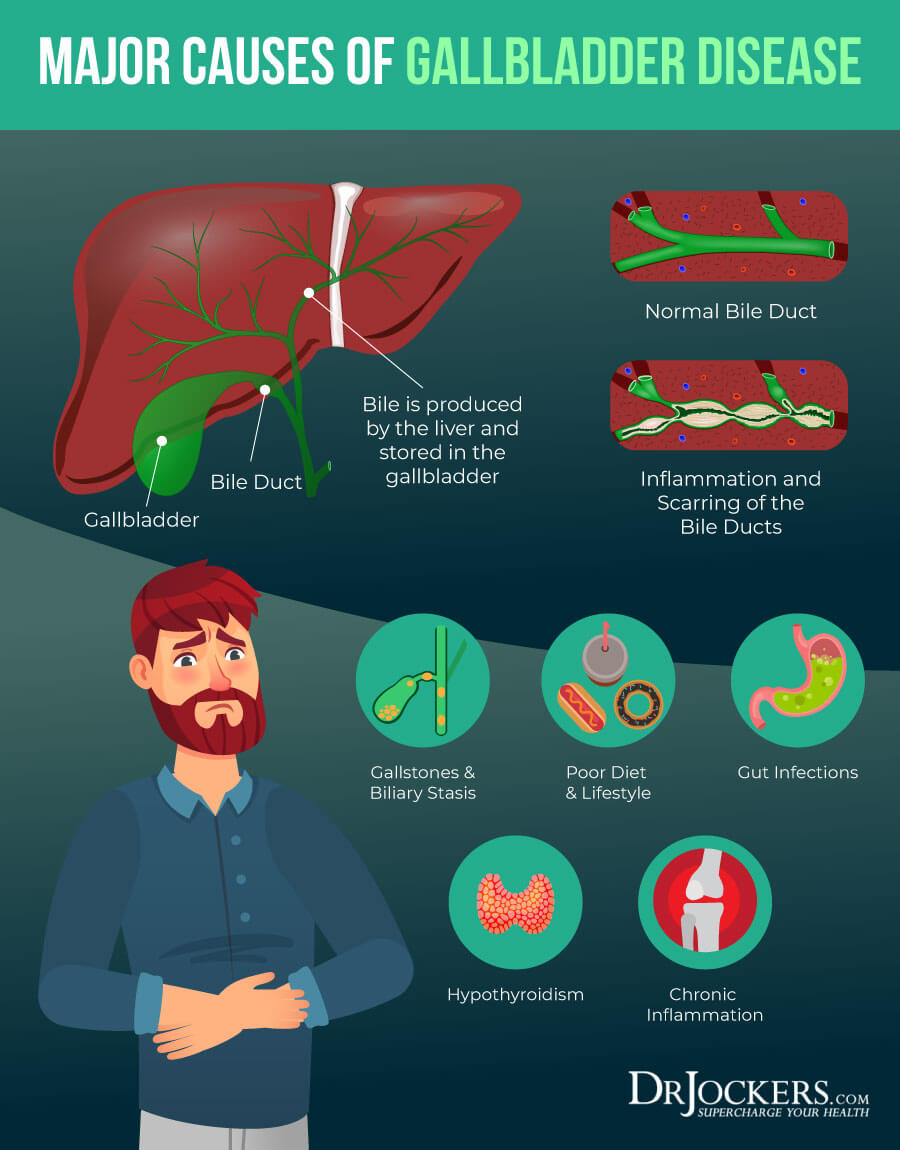
Major Causes of Gallbladder Disease
Gallbladder disease may be the result of a variety of dietary, lifestyle, and health factors. Let’s take a look at the major causes of gallbladder disease.
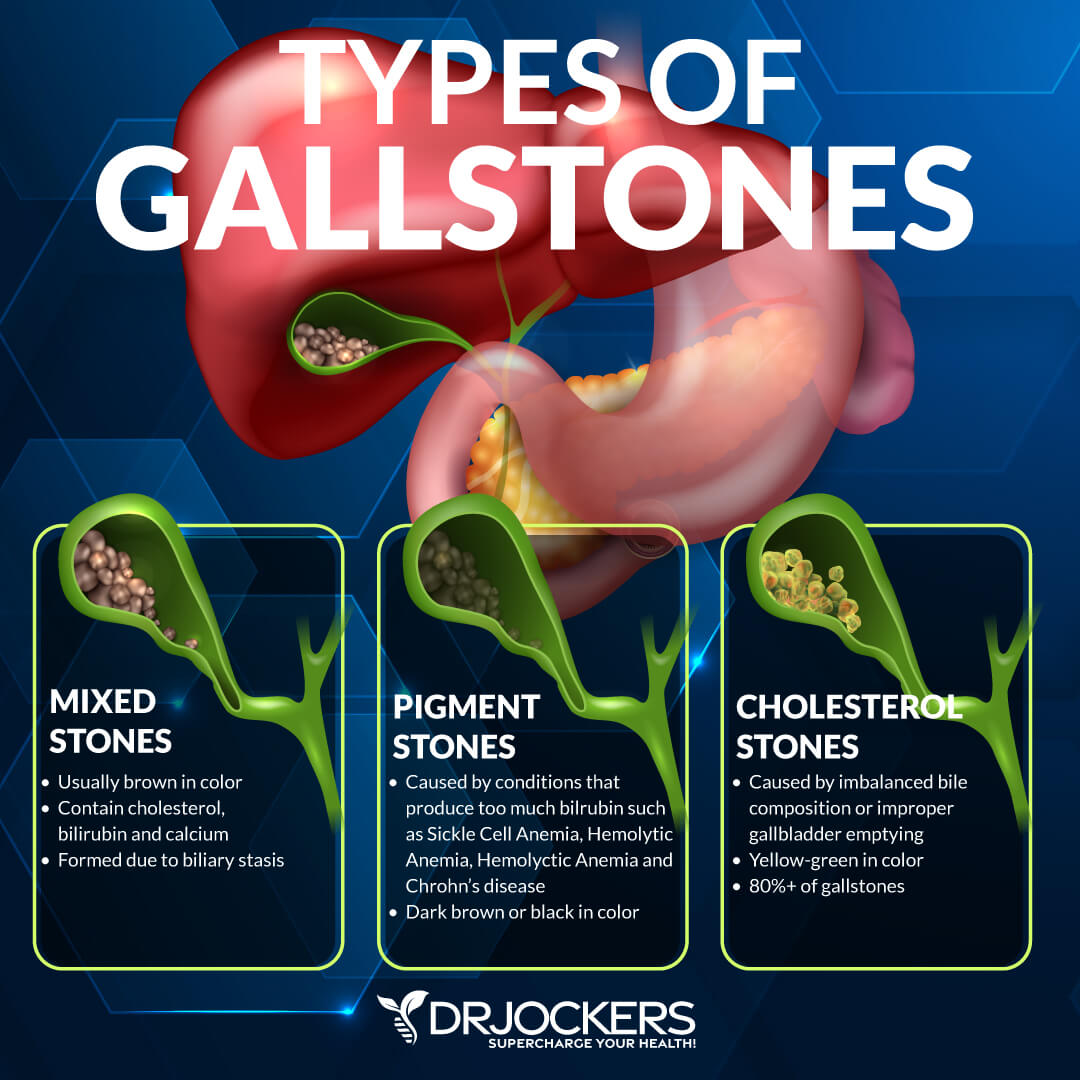
Gallstones & Biliary Stasis
Gallstones are harder deposits of bile that can occur and pile up in your gallbladder. Biliary stasis refers to the slowing or stopping of healthy bile flow. In the United States alone, about 20.5 million people have gallbladder disease, and about 3/4th of them are women.
When gallstones are stacking up in your gallbladder and your body is experiencing slowed bile production, it reduces your body’s ability to break down and absorb fat and compromises gallbladder function greatly. About 600,000 gallbladder surgeries are being performed each year. Most of these surgeries are performed due to too many gallstones piling up in the gallbladder, causing symptomatic gallbladder disease (4, 5).
Poor Diet & Lifestyle
Your diet and lifestyle play an enormous role in your health, including your gallbladder and digestive health. According to one hospital-based case-control study on 101 female cases and 204 control female participants, certain dietary and lifestyle patterns were identified as potential risk factors for gallbladder disease.
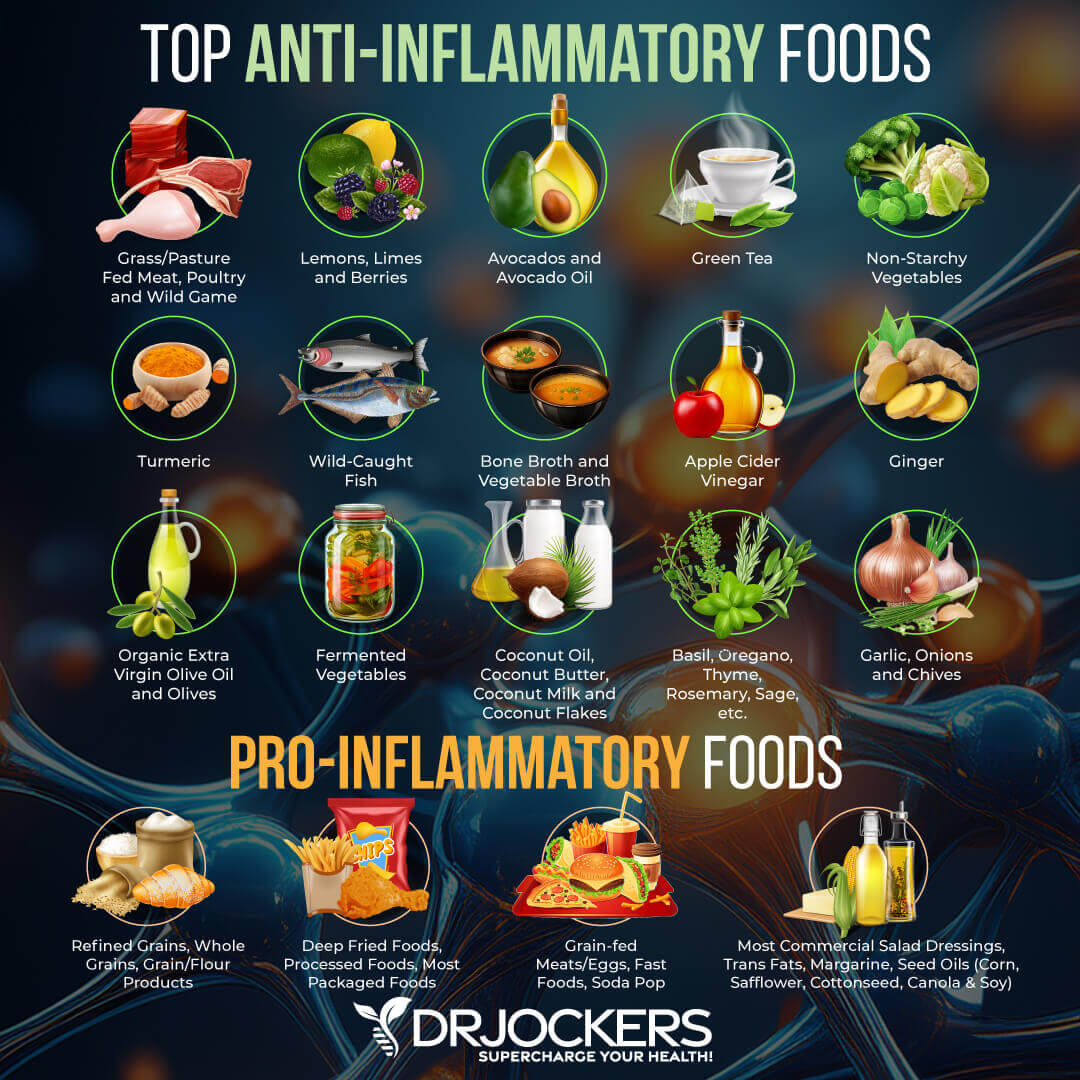
According to the results, eating refined grains, processed meats, high-fat dairy, sugar, tea, soft drinks, conventional red meat, eggs, salt, and pickled food increased the risk of gallbladder disease, whereas a high intake of vegetables, fruits, nuts, legumes, fish, spices, and a low intake of salt was identified as a health pattern not contributing to gallbladder issues.
Low physical activity, higher energy (calorie) intake, experience with rapid weight loss, being single, and having a family history of gallbladder disease increase the risk of gallbladder disease. This shows that regular physical activity, eating a balanced diet, not overconsuming calories, healthy weight loss instead of quick crash diets with rapid, unsustainable weight loss, and social connections may be important for your gallbladder health (6).

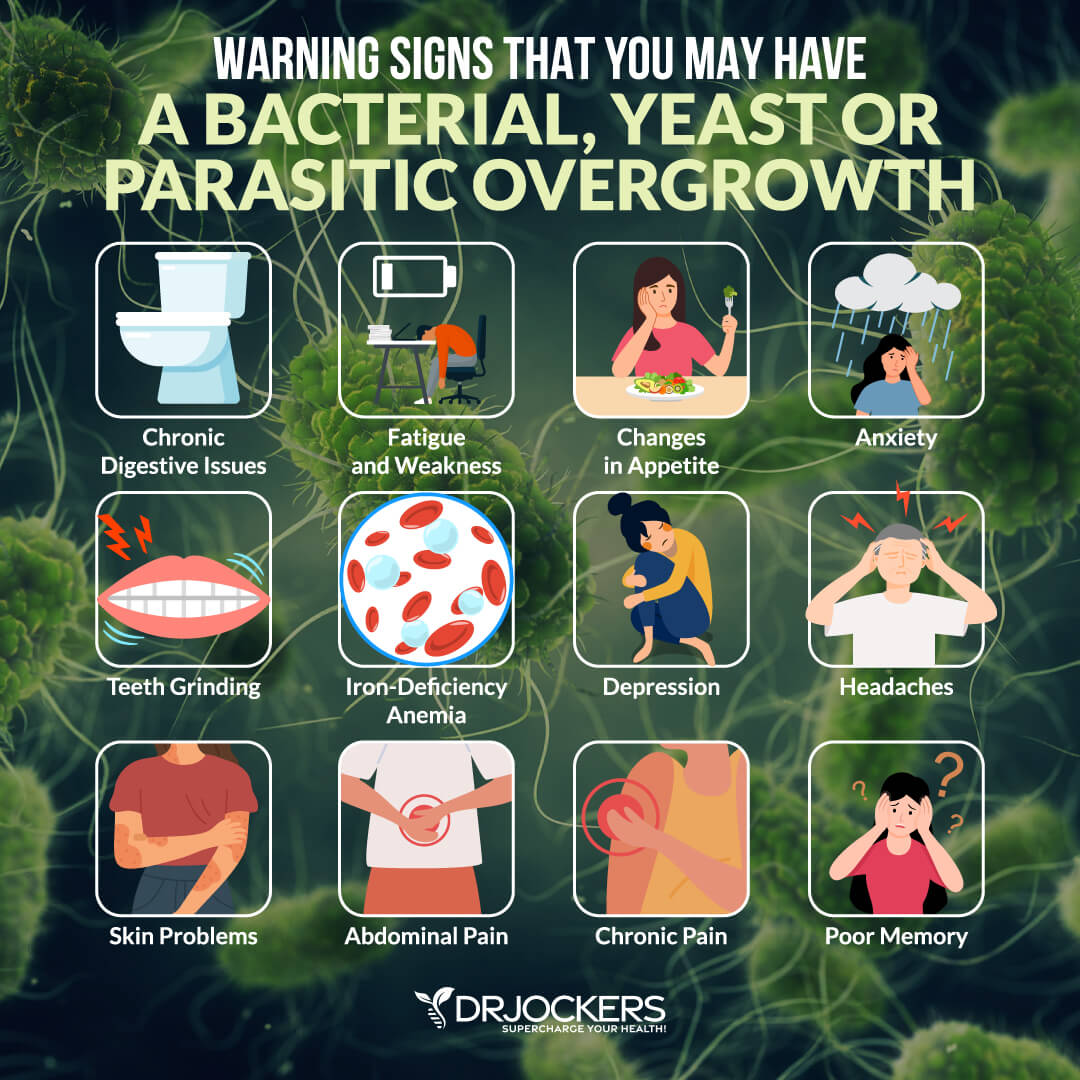
Gut Infections
Gut infections, including bacterial, viral, fungal, and parasitic infections, can greatly disrupt your digestion and may also lead to gallbladder disease. One study has found that a fish-borne liver fluke, Opisthorchis felineus can disrupt the gut microbiome and increase the risk of gallbladder disease.
Another study has found that an infection of Enterobacteriaceae may lead to acute cholecystitis, which is the inflammation of the gallbladder. On-going gut infections and gut microbiome imbalance can also slowly disrupt your bile flow and gallbladder health, leading to slowly developing gallbladder disease (7, 8).
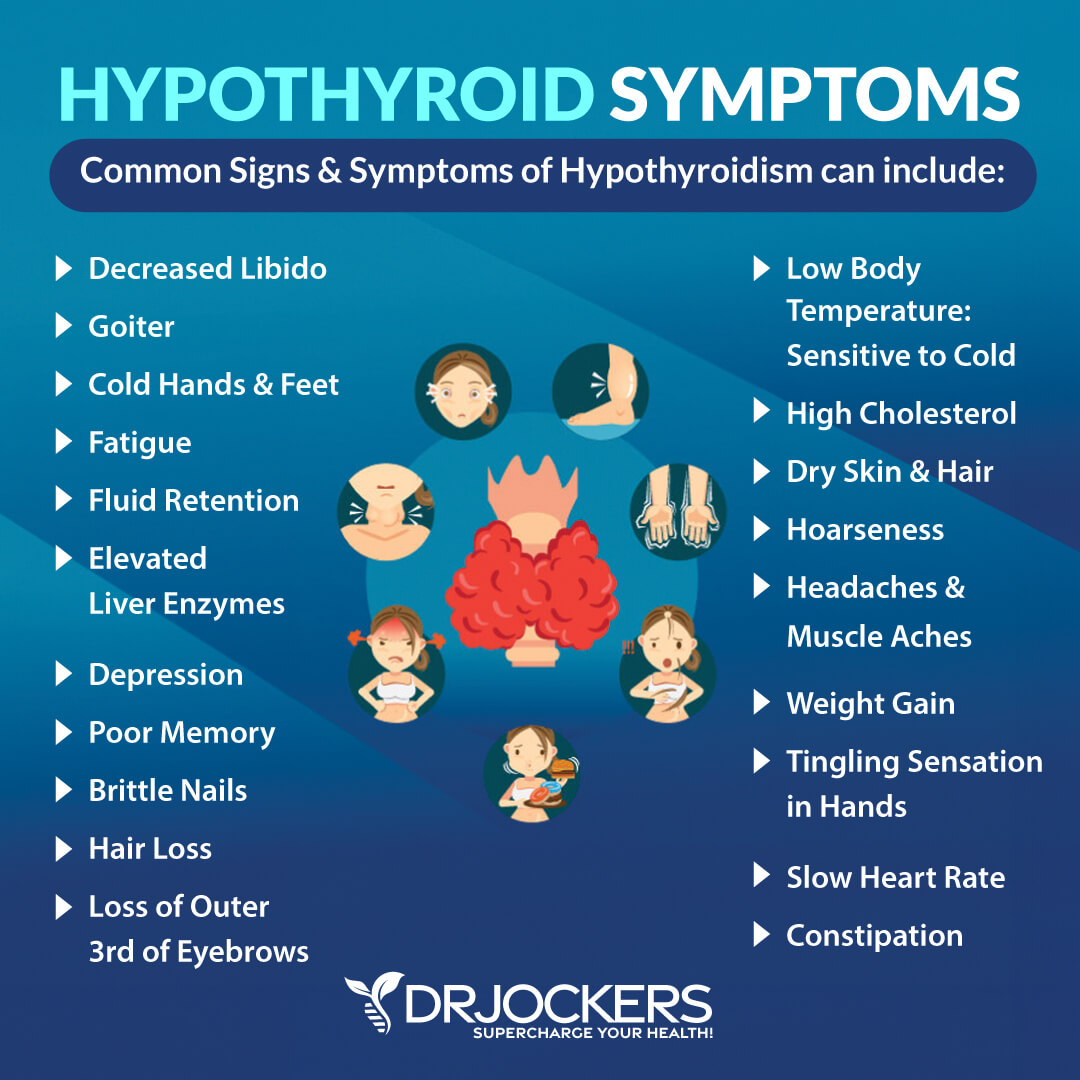
Hypothyroidism
Hypothyroidism means that you have an underactive thyroid gland that is not producing enough thyroid hormones. Hyperthyroidism means that your thyroid gland is overactive. Euthyroidism refers to the normal functioning of your thyroid.
Hypothyroidism, in particular, has been connected with gallbladder disease. According to one mouse study on the relationship between thyroid disease and gallstone formation, 83 percent with hypothyroidism and 22 percent with euthyroidism developed gallstones.
A human study on 3749 people between the ages of 20 and 79 has found a correlation between high TSH levels and gallbladder disease in men. A scientific review has also found that hypothyroidism may lead to gallbladder disease formation (9, 10, 11).
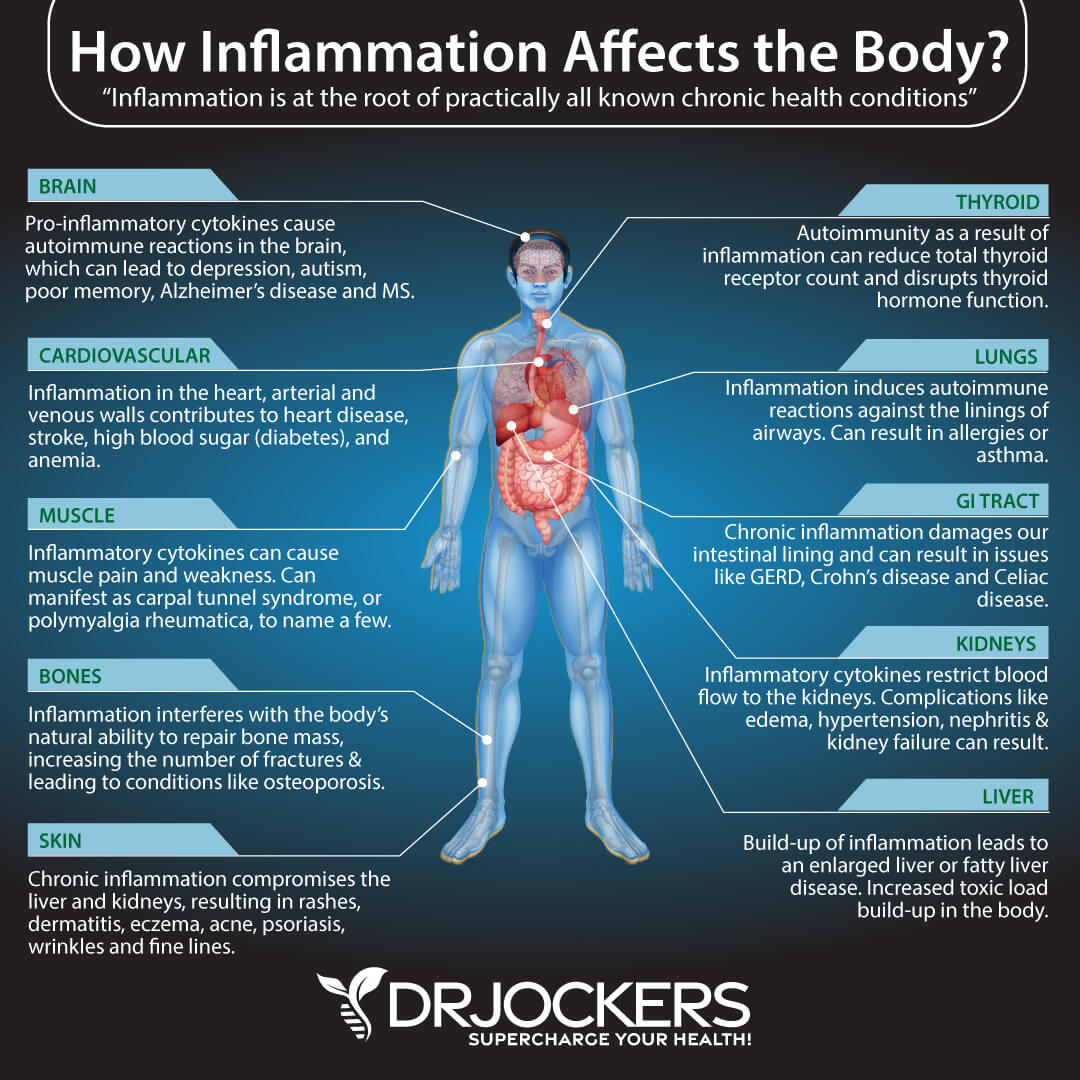
Chronic Inflammation
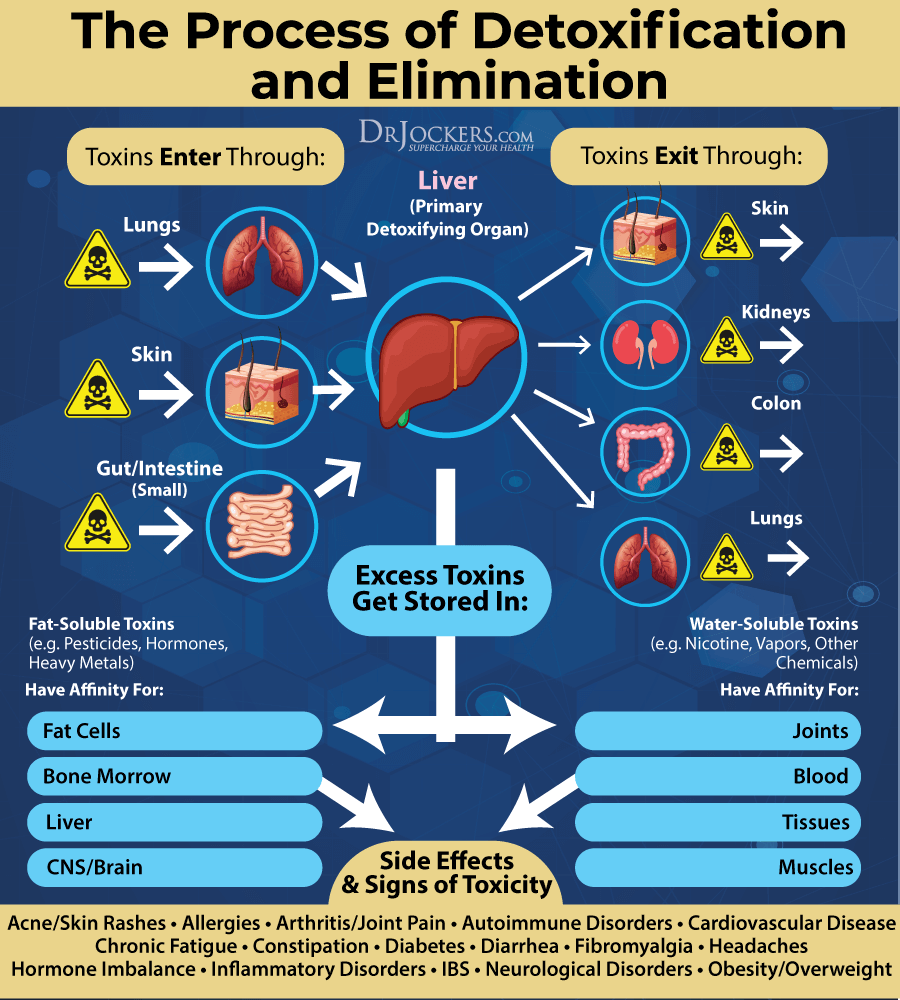
Chronic inflammation can develop in your body due to an unhealthy diet, lack of sleep, stress, smoking, other unhealthy lifestyle choices, toxic overload, and infections. Chronic inflammation can have a great toll on your digestion and compromise your digestive health. It may increase your risk of gallstones, leading to chronic gallbladder problems.
Chronic gallstones and gallbladder issues lead to inflammation in your gallbladder and further increase chronic inflammation in your body, leading to a vicious cycle. According to research, chronic inflammation may remain in the body even in the absence of or after the removal of gallstones (12, 13).
Prevalence of Gallbladder Surgeries
Clearly, bile and gallbladder health are critical for your digestion and overall health. Yet, gallbladder problems are rampant. Poor bile production, poor bile utilization, and metabolic problems can lead to gallbladder disease.
The problem is that our conventional medical system has no solution for sluggish bile production or biliary stasis. If you have poor bile production, your doctor will watch and wait until your gallbladder is full of gallstones. As a last resort, gall bladder removal surgery becomes the next step.
As a functional medicine doctor, I am incredibly concerned about this. Such levels of gallbladder issues not only take years to develop but are also completely avoidable through appropriate dietary and lifestyle support strategies. It’s even more concerning that a review published in the British Medical Journal found that 50 percent of patients who had their gallbladder removed didn’t see improvement in their digestive complaints.
Since surgery is not exactly effective and gallbladder issues can be prevented, it is important that you support healthy bile production and gallbladder function. To learn 25 ways to support your gallbladder, I recommend this article. If you already had your gallbladder removed, you don’t have to be one of those 50 percent of patients without symptoms. Read on to learn how to support your body even without a gallbladder (14).
Best Digestive Health Strategies
If you had gallbladder removal surgery, it is very important that you practice the best digestive health strategies to support your overall health. It is also important to remember that your liver is still producing bile, although it may be sluggish due to inflamed and clogged bile ducts.
This is why it is important to do things to help dilate and open up the bile ducts so you can get the fat emulsification, detoxification, and anti-microbial effects of the bile to help support your digestive health. Here is what I recommend:
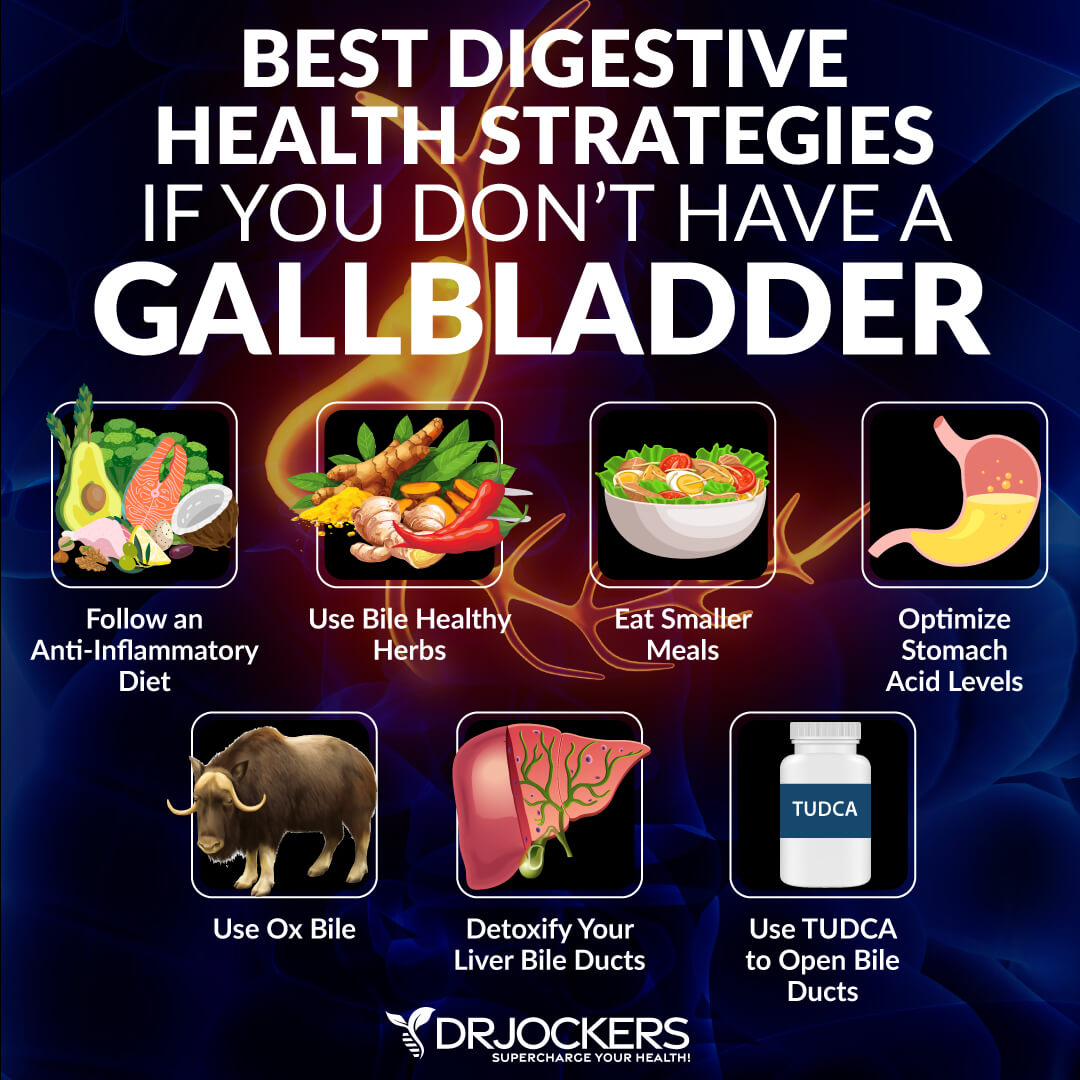
Anti-Inflammatory Diet
Eating an anti-inflammatory diet is the first step to healthy digestion and supporting your body if you don’t have a gallbladder. Remove all refined sugar and carbs, refined oils, heavily processed food, processed meat, non-organic dairy and meat, artificial ingredients, and other inflammatory foods.
Eat plenty of greens, vegetables, herbs, spices, sprouts, fermented foods, low glycemic index fruits, pasture-raised beef, wild-caught fish, free-range poultry, wild game, and healthy fats, such as avocados, coconut oil, organic butter, and ghee. To learn more about the anti-inflammatory ketogenic diet, I recommend reading this article.
You may also want to try intermittent fasting for further benefits. You may read about the benefits of intermittent fasting and the best intermittent fasting strategies in this article.
Use Bile Healthy Herbs
Add bile-healthy herbs and foods to your diet. I recommend apple cider vinegar, artichokes, lemon, lime, parsley, cucumber, celery, mint, cilantro, radishes, milk thistle, dandelion greens, turmeric, ginger, sauerkraut, and green tea for bile flow support.
Additionally, I recommend Bile Flow Support, a supplement supported with dandelion and celandine for optimal bile flow. To learn more about these bile-healthy herbs and foods, I recommend this article (15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29).

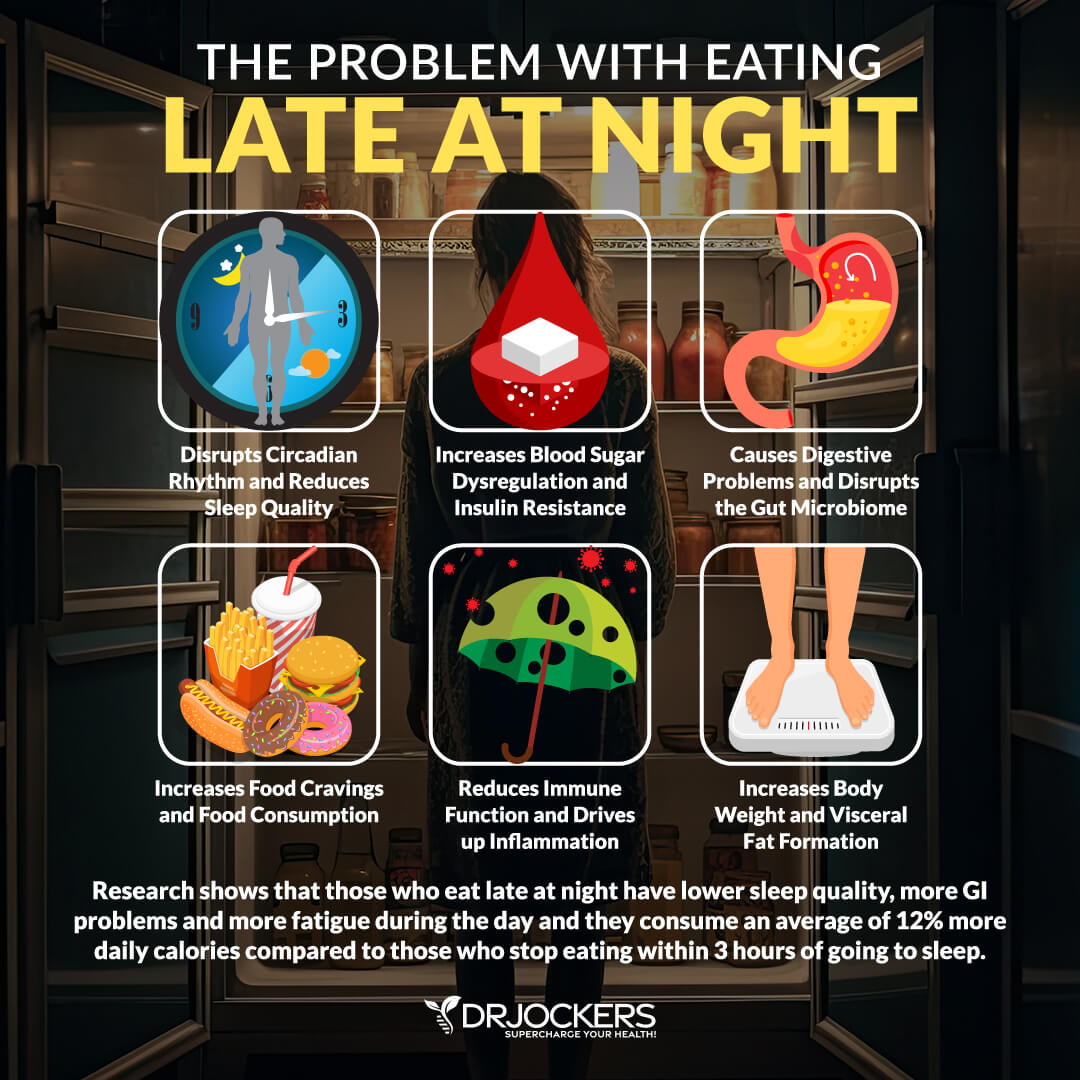
Eat Smaller Meals
If your gallbladder has been removed or you are hoping to improve your sluggish gallbladder and avoid surgery, you should avoid large meals. Your body has a difficult time emulsifying fats, which can lead to serious digestive stress and further problems.
Instead, I recommend that you consume 3 to 4 smaller meals during the day or during your eating window if you are practicing intermittent fasting. Also, be sure not to eat late at night because this will cause food to sit and cause more problems for the liver. Best to eat 3-4 hours before going to sleep.
Incorporating lighter liquid meals, such as green smoothies and protein shakes, is a great idea for liver, gallbladder, and digestive support. Experiment and watch your symptoms to see what time-frames, combinations, and amounts work the best for your body.
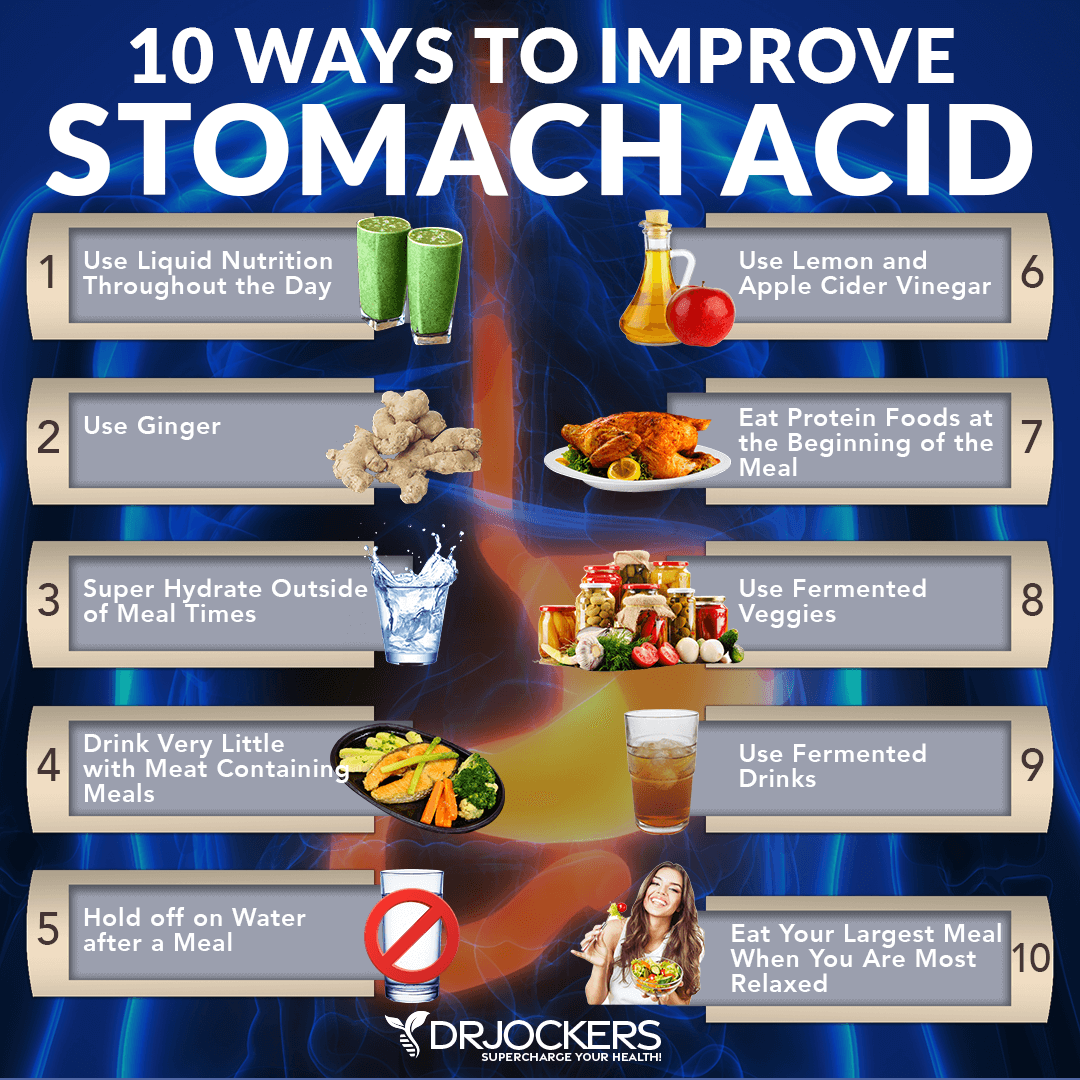
Optimize Stomach Acid Production
Stomach acid plays an important role in stimulating bile secretion into your small intestine. It is important that you support and optimize stomach acid production. Eating a healthy diet is key. Using apple cider vinegar water, adding ginger to your meals or tea, holding off on drinking water until after your meal, eating slowly, hydrating well outside of mealtimes, and liquid nutrition can also improve your stomach acid levels.
I also recommend that you supplement with betaine hydrochloric acid to support stomach acid production and bile flow. To learn more about how to improve your stomach acid levels, I recommend this article.
Use Ox Bile
I recommend Super Digest HCL for optimal digestion. It contains betaine hydrochloride (HCI) for proper stomach acidity and optimal breakdown of food, lactase to break down the milk sugar, lactose, dipeptidyl peptidase IV (DPPIV) for the breakdown of gluten and casein, and ox bile extract and lipase to emulsify and digest fats and fat-soluble vitamins.
This is my go-to supplement for anyone without a gallbladder because it supports optimal stomach acid, provides bile to help emulsify fats, and provides pancreatic enzymes to help with overall digestion. Start with one capsule with each meat and fat-containing meal and work up to 4 capsules and see which dosage works best for you. It is always best to take this in the beginning or in the middle of the meal and not right at the end.
If you notice an increase in acid reflux or burning in your stomach, it may mean that you have either a stomach ulcer or you are taking too much of the supplement. In this case, back down your dosage or eliminate altogether.
Detoxify Your Liver and Bile Ducts
To create a healthy gut environment and optimize your digestion, I recommend that you detoxify your liver and bile ducts. For ongoing liver and bile ducts detoxification, I recommend optimal hydration, drinking warm lemon water, and drinking herbal tea for digestion and detoxification support.
I recommend regular exercise and infrared saunas to support detoxification through sweating, and coffee enemas for cleansing through bowel movements. To learn more about liver cleansing, I recommend reading this article.
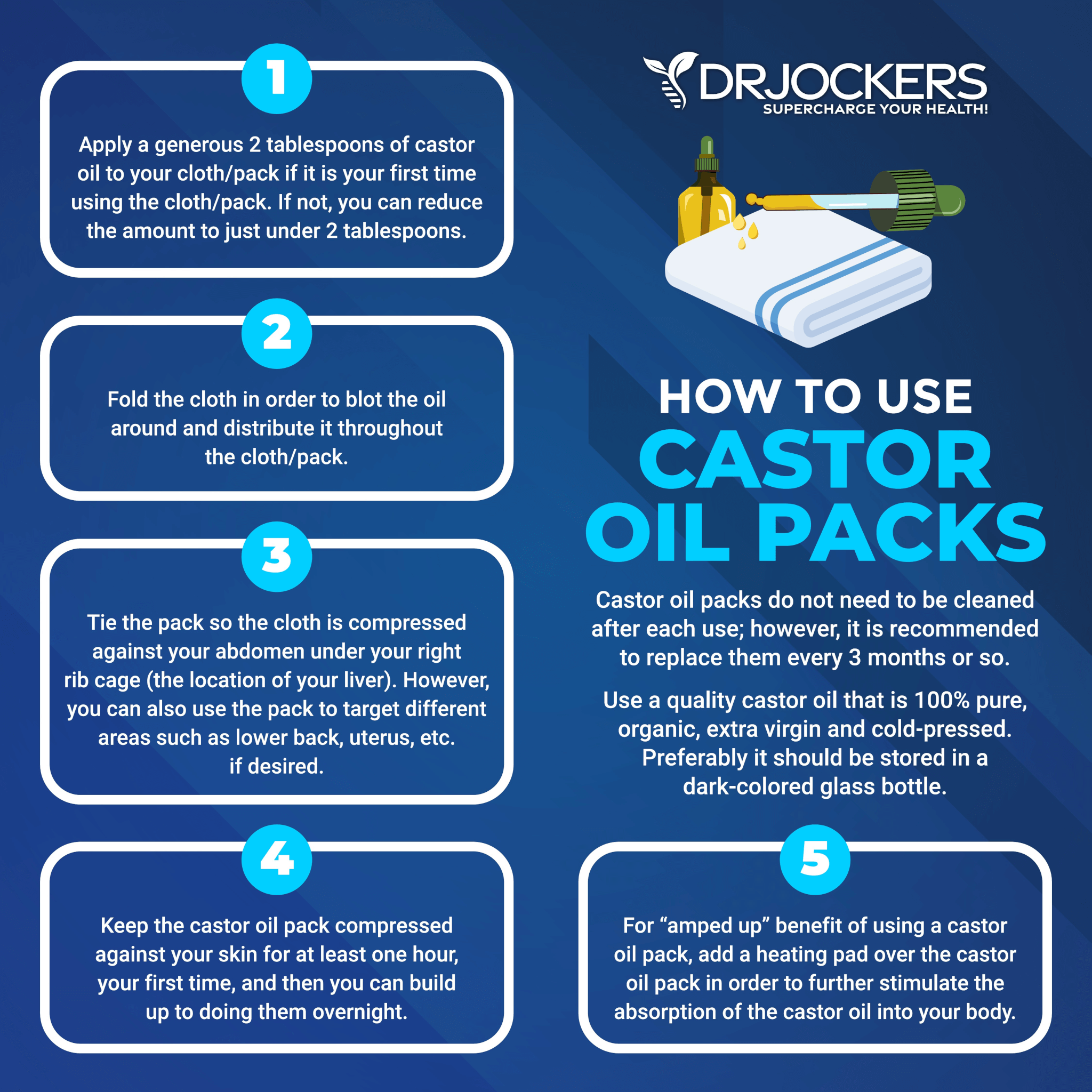
Use a Castor Oil Pack to Improve Bile Flow
Castor oil can help to dilate the bile ducts of the liver, so bile flows more effectively (3). Castor oil packs have the same therapeutic properties when applied to the skin following absorption. Applying castor oil packs to the right upper quadrant (where the liver is) can help dilate the bile ducts and improve bowel movements.
It is important to get organic castor oil in a glass jar because pesticide residue contained in the castor oil and the plastic residue (phthalates) from the bottle can be absorbed through the skin.
Use TUDCA to Open Bile Ducts
Supporting and opening your bile ducts are critical for optimal bile flow and digestive health. Advanced TUDCA is a fantastic supplement that helps to thin the bile and dilate your bile ducts. TUDCA is a vital component of liver bile that helps to break down fats and aids in regulating glucose levels.
One study has found that TUDCA can increase bile flow by 250 percent. Other studies have found that taking TUDCA can support both liver and kidney health. Moreover, a promising study on mice has found that TUDCA may reduce intestinal inflammation. I recommend that you take it for optimal results (30, 31, 32, 33).
Bile Flow Support is my go-to for boosting bile formation in the liver. It contains the necessary amino acids along with herbs like dandelion that not only provide the nutrients necessary for bile but also stimulate the proper flow from the gallbladder.
Final Thoughts
Gallbladder disease takes a while to develop and gallbladder removal surgery is preventable. Yet, 600,000 Americans get their gallbladder removed yearly and many still struggle with digestive discomfort after. Follow my digestive support strategies to improve your digestion support after gallbladder removal surgery.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!







what do you recommend to avoid kidney stones ?
No gluten (wheat/barley/rye..oats/corn/rice). Rice is low in gluten. Wild rice has no gluten…is a grass. Gluten may cause kidney/gall stones. Taurine may help gall stones dissolve. Kidney stones…Hair tests shows good mineral levels. Restoring low minerals and lowering high minerals may help and no gluten so the gut lining heals and can absorb nutrients/minerals may help.
Thank you so much for this great article. It is by far the most comprehensive one I have ever read.
Thanks so much for your support Judy!
What protocol do you recommend for one who has chronic diarrhea after gallbladder removal? Surgery was 20 years ago and is a daily problem without taking cholestrymine multiple times a day.
Sorry to hear that! I would recommend adding in the activated charcoal and the TUDCA. Take 2 charcoal about 1 hour before each meal and take 2 TUDCA – 2x daily (morning and night). https://store.drjockers.com/products/tudca-plus
Excellent info, thank you. I was startled to see a mention of fibromyalgia in relation to gallbladder issues, and would love to pursue that line. (It hits home with me most startlingly) Do you have any pointers, please?
Yes here is a helpful article on Fibromyalgia: https://drjockers.com/fibromyalgia/
Gallbladder was removed 30 years ago. What should I be taking to improve digestion, elimination (chronic constipation), and healthy gut/microbiome? Bile salts? Why?How much? I’m 78 yo.
Yes absolutely, I would recommend the Super Digest HCL that was discussed in the article.
My brother has had his gallbladder removed and following developed chronic pancreatitis that he has lived with for 10 years now. takes oxe bile. What happens to the bile the liver produces when the bladder has been removed? Does it just flow into the small intestine without regulation by fat being consumed? Have you ever heard of Pancreatitis being reversed? He has been a vegetarian/vegan since he was 14.
Yes the bile continues to drip from the bile duct into the small intestine. Yes pancreatitis can be reversed and here is a helpful article: https://drjockers.com/pancreatitis/
Any advice or suggestions on supplements to support my 11 year old special needs son? We found out he has gallstones. He already eats a he healthy anti inflammatory diet. I know his doctor will want to schedule him for a gallbladder removal soon.
Sorry to hear that! He may have parasites. I would suggest working with a functional health practitioner. https://drjockers.leadpages.co/long-distance-coaching-dr-jockers/
Hi. I am 2 years w/out GB. Have Crohn’s (which is under control) and propensity for kidney stones. Any recommendations on ox bile or TUDCA? Do people take both at the same time? It sure how to chose which one to take. Thanks.
Thank you for breaking away from the normal health care advice of just throwing a pill at someone instead of trying to get to the root of the problem. My mother had her gallbladder out and she developed high cholesterol, heart disease, high blood pressure and fatty liver. She died of cirrhosis of he liver. No doctor ever told her of the risks of having her gall bladder removed or how to prevent it. To make matters worse, I had my gall bladder out and now have high cholesterol and a vitamin deficiency. The doctors want me on Statins to bring it down. I am hiring a nutritionist instead. I am determined to get my health back.
Sorry to hear about this! Hope you are doing better now after reading this article and following these strategies!
Hello Dr.Jockers, I have gallbladder but I have 2 polyps which are being monitored on yearly basis. If they change in size, I’d need my gallbladder removed. What can I do to prevent this? I don’t seem to find much information about the polyps and if the standard liver/gallbladder support applies or can something I decide to do trigger the growth? I am working hard to come to the bottom of this and how it’s all connected, I believe my root issue is mercury (had amalgam for 20+ years), affected my thyroid and my gallbladder/liver (also have Gilbert syndrome) and gut (Sibo/ constipation) so I’m working on correcting these issues.
Thank you, Dr Jockers!
Your article connects many dots for me and gives me ideas on how I might further mitigate the effects of a strong genetic tendency toward inflammation that manifests any and everywhere, including chronic gallbladder dysfunction. I already do many of the actions you suggest, but the article explains clearly why and how each thing works…or why it might not be working, and suggests a few ideas new to me. Feeling both grateful and appreciative.
Thank you so much for all of this great information. Is there a substitution for vinegars? Mass produced vinegar is made using a defoaming agent because the foam generated in such large quantities is virtually unmanageable. This agent is created by fermenting black mold on corn similar to manufactured citric acid. Ingesting any mold hurts me sometimes seriously.
Thanks!
I have a gallbladder stone that is 2.9 cm without symptoms presently. Meaning no pain, there is bloating, loose stools. So the doctor said, Go have it surgically removed. At this point, I have changed my diet, herbs, dandelion, chanca piedra to avoid surgery over the years. But I realized it may need to be removed since its so big and the gallbladder is 2.7 cm to 3.9cm big. After this I would like to follow your recommendations and find I have heartburn with the lemon and apple cider vinegar. I use 4 oz lemon and 1 oz apple cider vinegar in 2liters of water. Is this something to be changed?