 GlycA: A New Biomarker for Systemic Inflammation
GlycA: A New Biomarker for Systemic Inflammation
Chronic inflammation is the root cause of most chronic symptoms and modern-day diseases. There are many testing options to uncover chronic inflammation, and there is a new one on the horizon. GlycA may be a great new biomarker to test for systemic inflammation. It may be a more stable and reliable measure than other markers and may be used as a complementary strategy to other tests.
Testing for GlycA levels and other inflammatory biomarkers may help to find underlying chronic inflammation, hidden health issues, the root causes of your problems, and to create an appropriate treatment plan, measure your progress, decrease your health risks, and regain your health and vitality.
In this article, you will learn what inflammation is. You will understand the problem with chronic inflammation. I will discuss what GlycA is and the benefits of testing for GlycA as a biomarker for chronic inflammation. I will go over some additional testing options for chronic inflammation and the best option to test for these.
What is Inflammation?
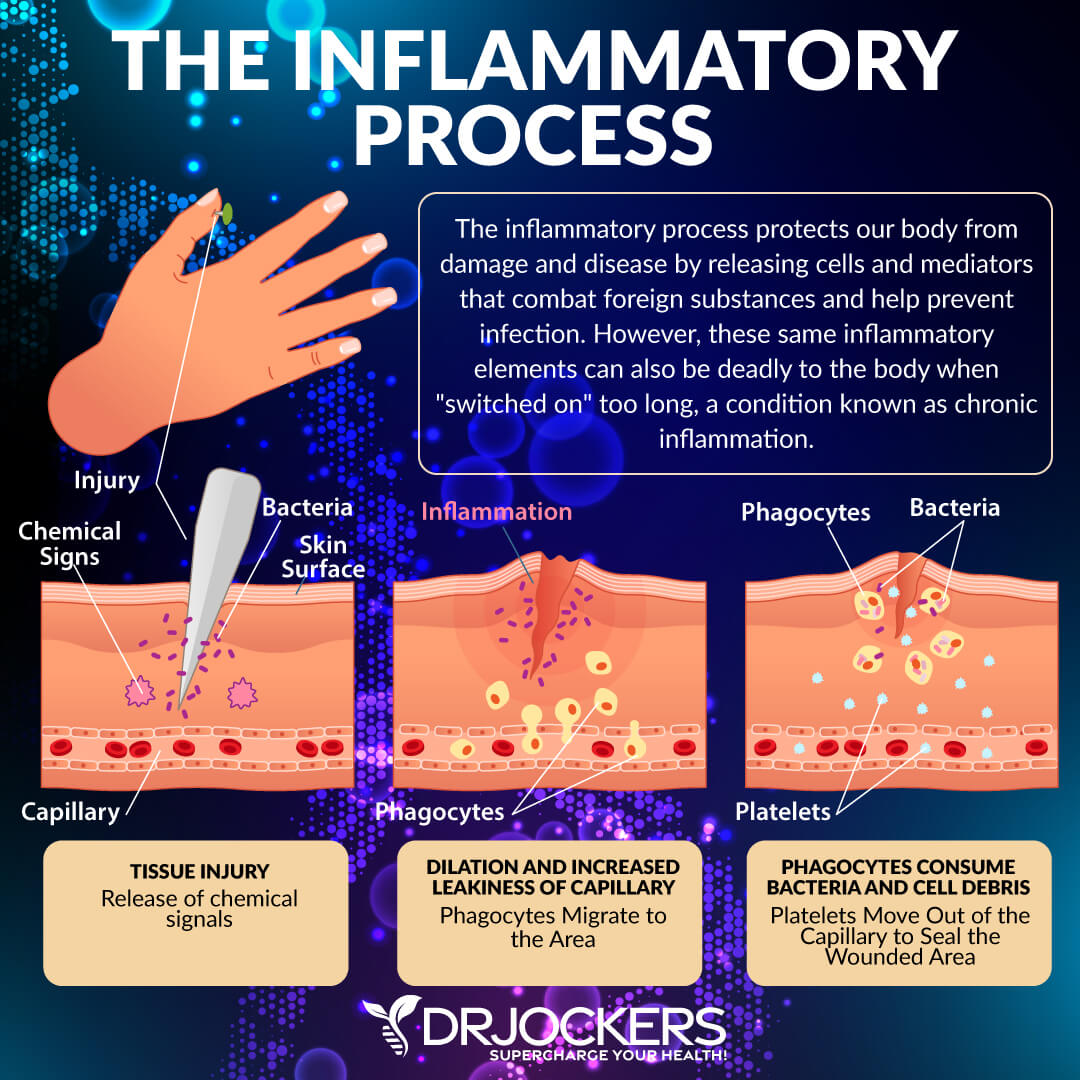
When you hear the word inflammation, you may think it’s a bad thing. It couldn’t be further from the truth. Inflammation is your body’s natural defense mechanism which helps to protect you from and aid your recovery from pathogens, allergens, toxins, injuries, and other harm. When you encounter any harm or cellular injury, your immune system will respond by increasing blood flow, capillary dilation, leukocyte infiltration, and the production of various chemical mediators.
This is a complex process that allows your body to make antibodies and inflammatory cytokines. This helps your body fight hostile pathogens, eliminate toxic agents, repair tissue damage, and protect you from further harm.
If you are dealing with an injury, inflammation helps to protect the affected area and support recovery. The redness, swelling, or pain is a necessary part of the recovery process. It is the same with allergies and infections. You may experience sneezing, congestion, or other uncomfortable symptoms, but it is part of the natural healing process.
Clearly, inflammation, or more specifically, acute inflammation in response to illness, allergens, injuries, and toxins, is necessary. It is a protective friend. However, as a 2015 article published in the British Journal of Nutrition and other research explains, chronic, low-grade, systemic inflammation can be problematic and harmful (1). Let’s get into the problem of chronic inflammation.
Acute Inflammation vs Chronic Inflammation
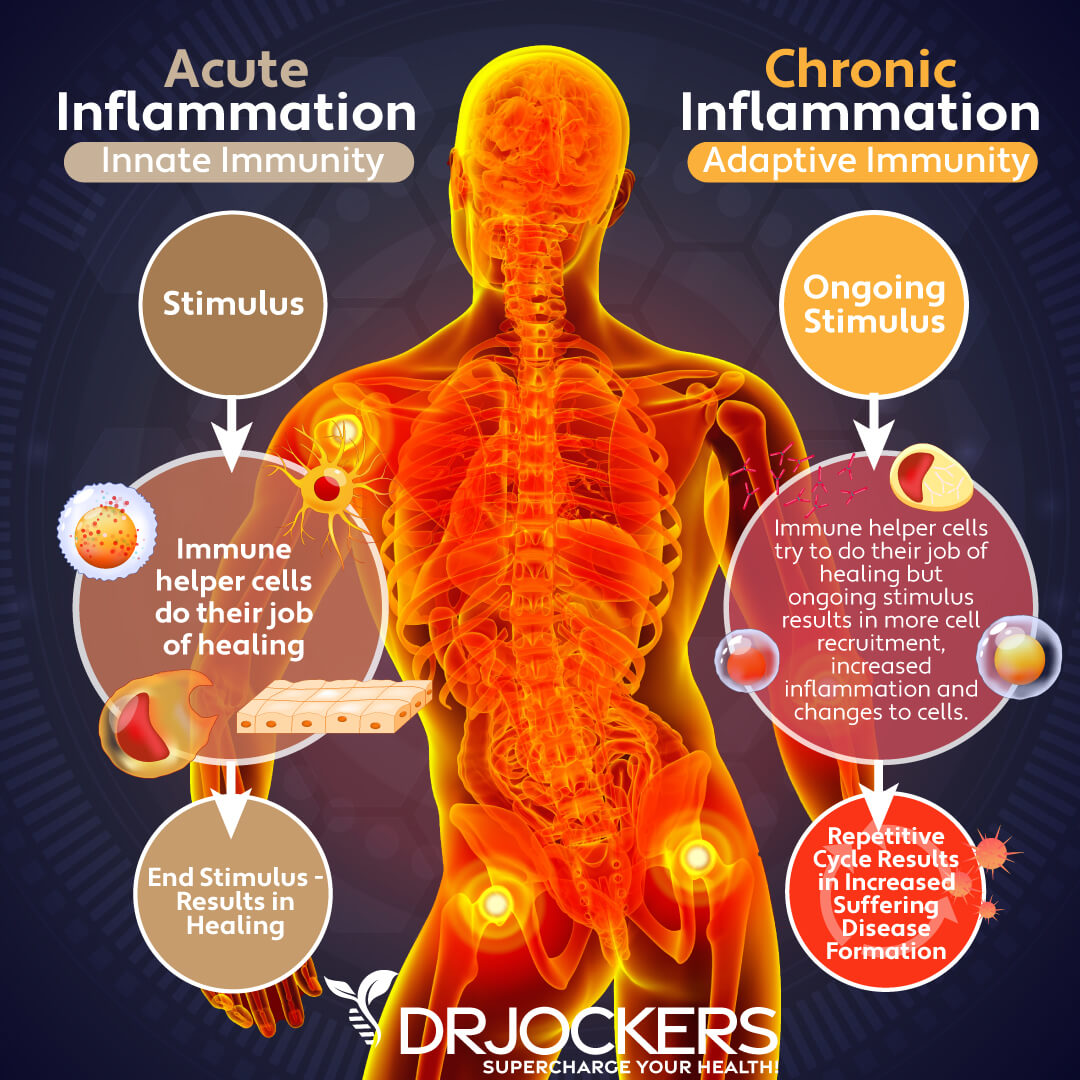
As I discussed earlier, acute inflammation is critical for your health. It is needed as a survival response to injury, infection, or illness. It protects you from pathogens and supports the recovery and repair of damaged cells. Chronic inflammation, on the other hand, is different. It can cause ongoing damage, chronic symptoms, and serious health issues.
Acute inflammation starts quickly, usually within minutes, upon infection, exposure to toxins or allergens, or injury. Acute inflammation doesn’t last too long. In most cases, it will only last for a few days or a few weeks. In the case of some injuries or surgeries, it may last for a few months.
However, it always decreases gradually and then completely disappears upon recovery. Signs of acute inflammation may include pain, swelling, redness, heat, itching, or in case of respiratory issues or allergies, sneezing, coughing, congestion, and watery eyes.
Chronic inflammation is different from acute inflammation. Low-grade, chronic inflammation is systemic. It can last for months or years. If not addressed appropriately or at all, it may last for a lifetime. When it comes to acute inflammation, you generally know the exact cause, such as an injury, infection, allergen, or toxic exposure.
Chronic inflammation doesn’t have one specific cause. In some cases, it may start with a specific acute inflammation after an injury or illness but turns chronic with symptoms remaining after recovery. In many cases, however, you can’t even point to an acute inflammation or any problem as a starting point.
The Problem with Chronic Inflammation
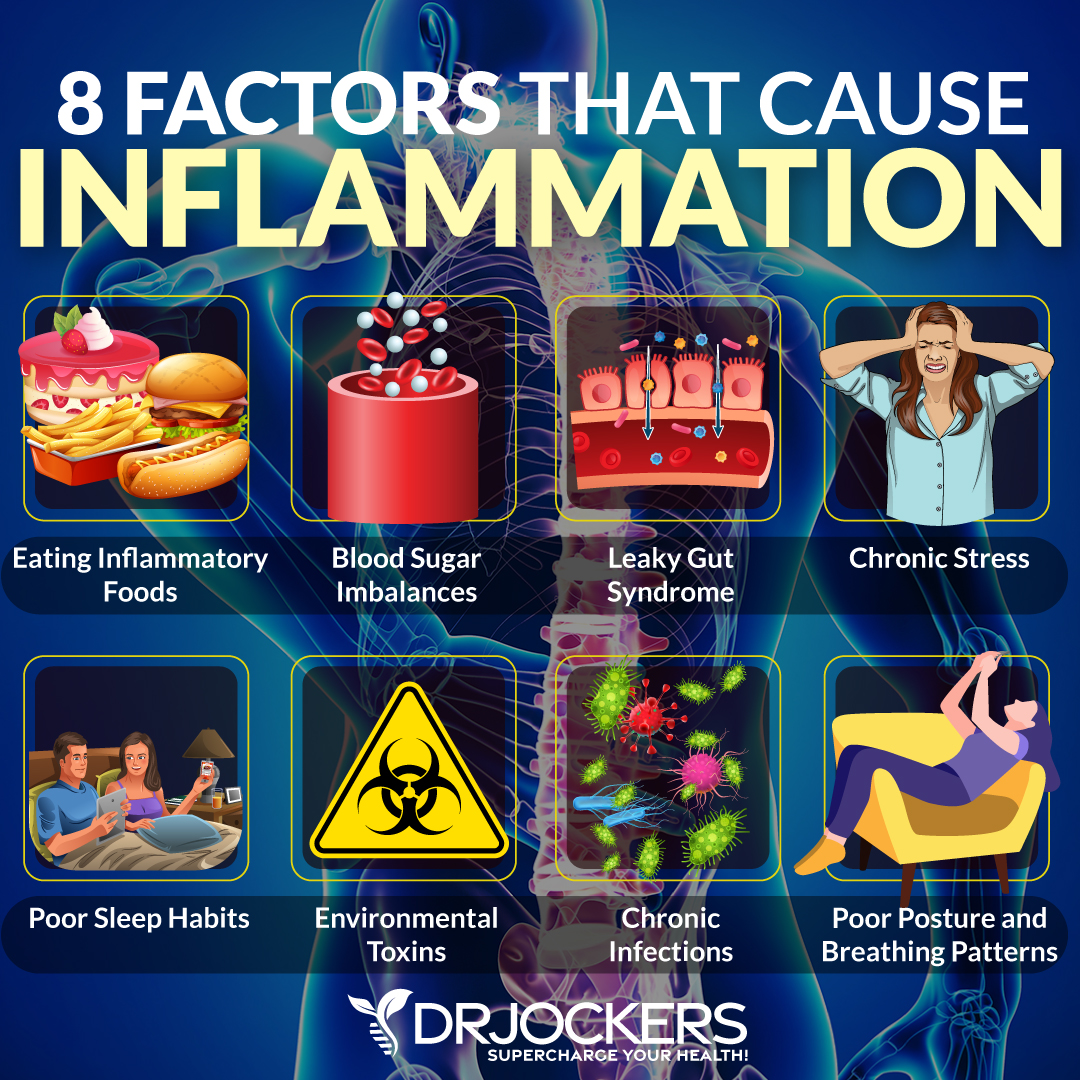
Chronic inflammation usually develops over time due to a combination of issues, including a poor diet, poor lifestyle choices, chronic stress, environmental toxin exposure, and other factors. These factors can put an excessive amount of stress on your body. As a response, your body produces inflammatory modulators across your body. This can seriously overwhelm your immune system and body overall.
Chronic and ongoing inflammatory stimuli can cause the recruitment of white blood cells, cellular changes, and increased inflammation. Excess white blood cells may end up attacking your cells, tissues, or internal organs, which will lead to a continuous inflammatory response and ongoing health issues.
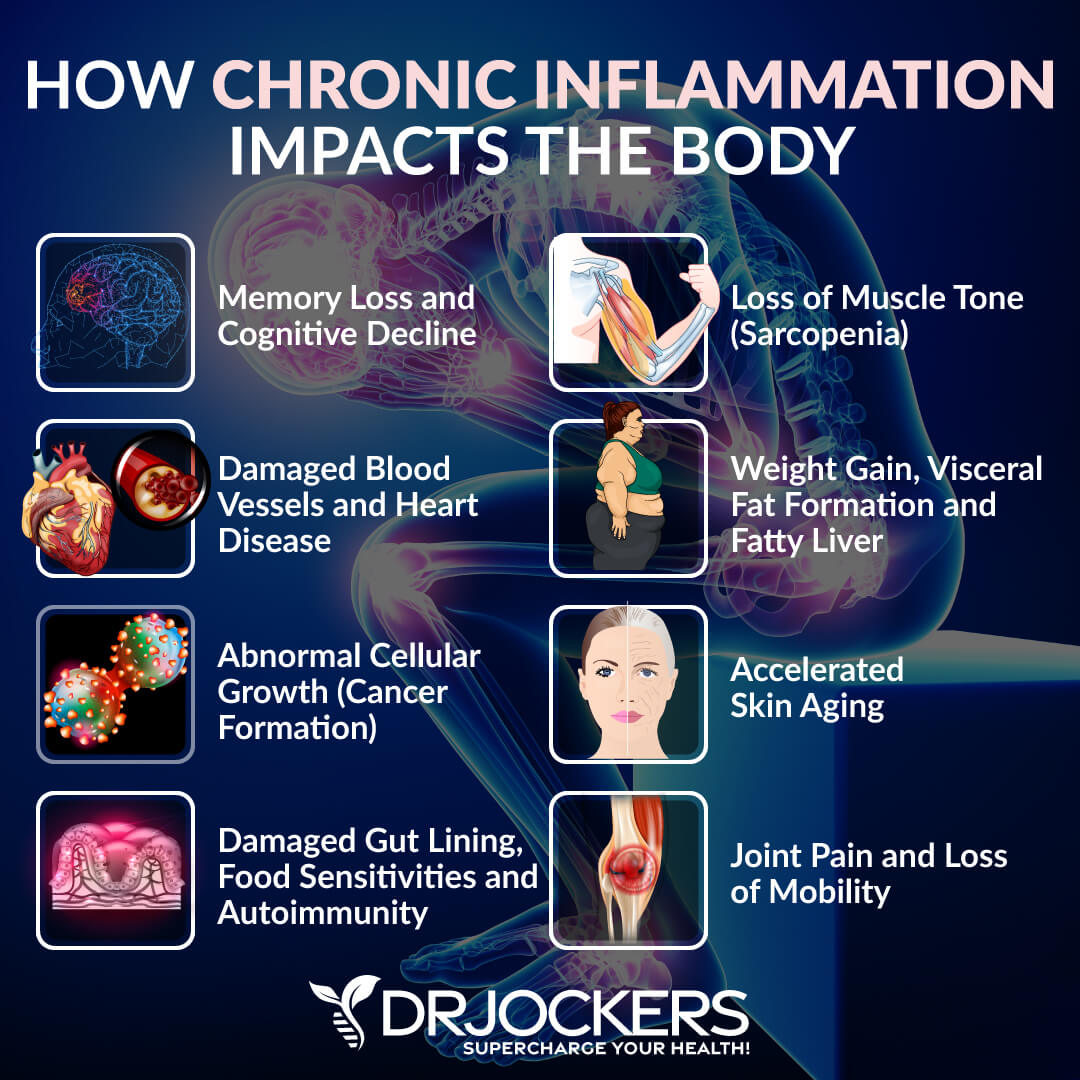
Chronic inflammation can be incredibly harmful to your body. Symptoms of chronic inflammation can vary from person to person and may include fatigue, chronic pain, muscle aches, joint pain, headaches, migraines, insomnia, skin issues, brain fog, memory issues, gastrointestinal issues, weight gain, weight loss, obesity, anxiety, depression, mood swings, hormonal issues, frequent infections, early signs of aging, and more.
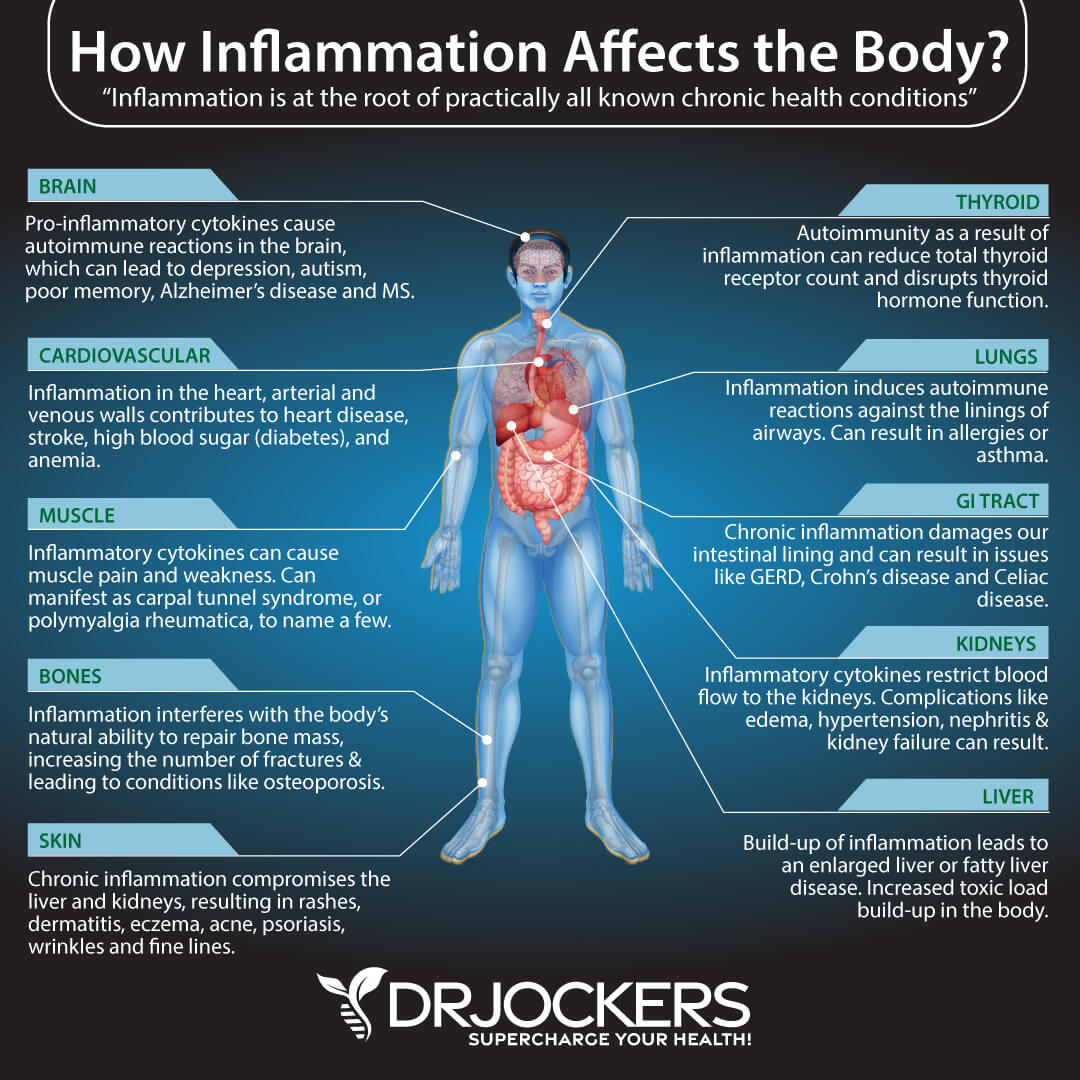
Chronic inflammation can affect all areas of your body. This includes your digestive system, kidneys, liver, lungs, brain, endocrine system, hormonal health, heart, skin, muscles, and bones. For example, a 2015 article published in the British Journal of Nutrition has discussed that chronic, low-grade, systemic inflammation is likely involved in the early stages of disease development. (1).
Chronic inflammation may seriously impact your gut microbiome and digestive health. A 2020 review published in the International Journal of Environmental Research and Public Health, along with other research, has found a link between chronic inflammation and the gut microbiome and related problems (2).
It may not be surprising that chronic inflammation may be a major underlying factor behind a number of chronic, modern-day, and degenerative diseases. A 2012 article published in EMBO Rep and other scientific studies has linked chronic inflammation to major degenerative diseases, including cancer, heart disease, diabetes, and amyotrophic lateral sclerosis (ALS) (4).
Chronic inflammation may drive your immune system into overdrive, leading to an autoimmune response. According to a 2010 review published in Autoimmune Reviews, chronic inflammation is also linked to autoimmune diseases (3).
A 2015 study published in JAMA Psychiatry has linked chronic inflammation to brain inflammation, mental health issues, and brain health problems (5). Chronic inflammation may be linked to depression, anxiety, addictions, other mental health issues, memory issues, and neurodegenerative diseases.
What is GlycA
GlycA is a composite biomarker that may serve as a new biomarker for systemic, chronic inflammation. The use of GlycA may be similar and complementary to looking at c-reactive protein (hs-CRP), fibrinogen, and other inflammatory biomarkers. It combines the protein levels and glycosylation states of some of the most abundant acute phase proteins, which are a more stable measure of systemic inflammation without much intra-individuality (6).
To look at inflammation levels, one measurement may be enough with GlycA testing. With hsCRP, on the other hand, it’s recommended to use two measurements at least two weeks apart. Research has found that GlycA may be a good biomarker for atherosclerotic CVD events, inflammation-related cardiovascular events, and chronic inflammatory diseases, including psoriasis and rheumatoid arthritis (6).
A 2020 study published in Circulation: Heart Failure has found that GlycA may be a good biomarker for heart failure risk (7). A 2017 study published in the Journal of Translational Medicine has also found that it may be a new biomarker for cardiovascular events and chronic inflammation (8).
A 2020 article published in the Journal of Laboratory and Precision Medicine has found the same (9). 2015 research published in Cell Systems has found that GlycA may be linked to chronic inflammation and may help to predict the risk factor for severe infections in the long run (10).
Results may not only determine risk factors and underlying inflammation behind health issues but may guide treatment and prevention. Research has shown that exercise, anti-inflammatory therapies, and lifestyle interventions may reduce GlycA levels (6).
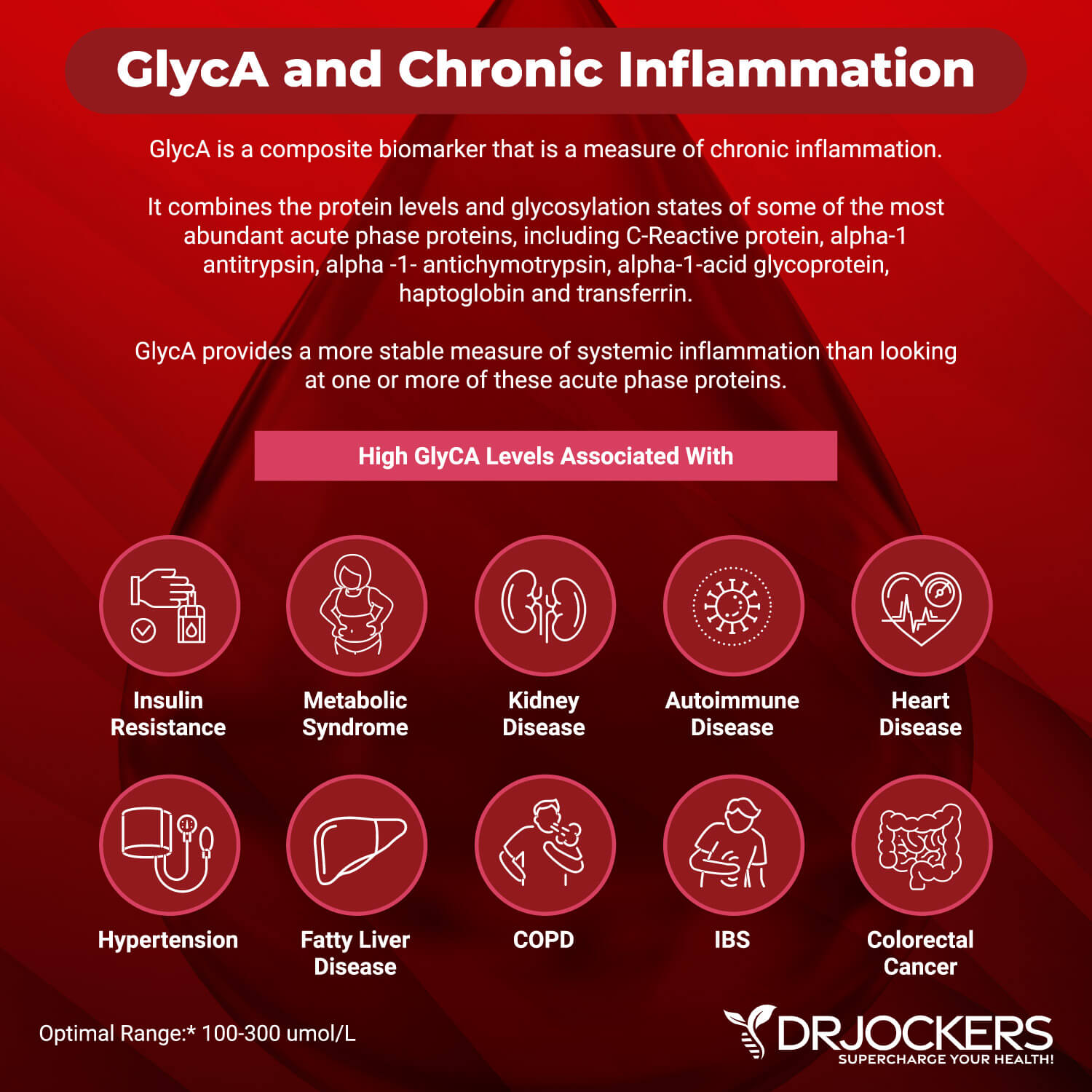
Low levels of GlycA may be seen in sickle cell anemia despite the presence of inflammation, apparently due to hemolysis (Fuertes-Martin 2020). Otherwise, in general, low GlycA suggests reduced inflammation and glycation.
High levels of GlycA may indicate systemic inflammation, the risk or presence of cardiovascular, autoimmune, or metabolic problems, and all-cause mortality. Elevated levels may be linked to insulin resistance, type 2 diabetes, metabolic syndrome, hypertension, cardiovascular disease, renal disease, COPD, gut microbiome imbalances, colorectal cancer, alcoholic liver disease, inflammatory bowel disease, immune activation, arthritis, lupus, psoriasis, other autoimmune conditions, and other inflammatory problems.
Low levels of GlycA indicated low systemic inflammation levels. However, we may see low GlycA levels in sickle cell anemia because of the hemolytic destruction of red blood cells.
Standard and optimal ranges include:
- The standard range is 0.00 – 400.00 umol/L
- The optimal range is 100.00 – 300.00 umol/L
Additional Markers for Inflammation
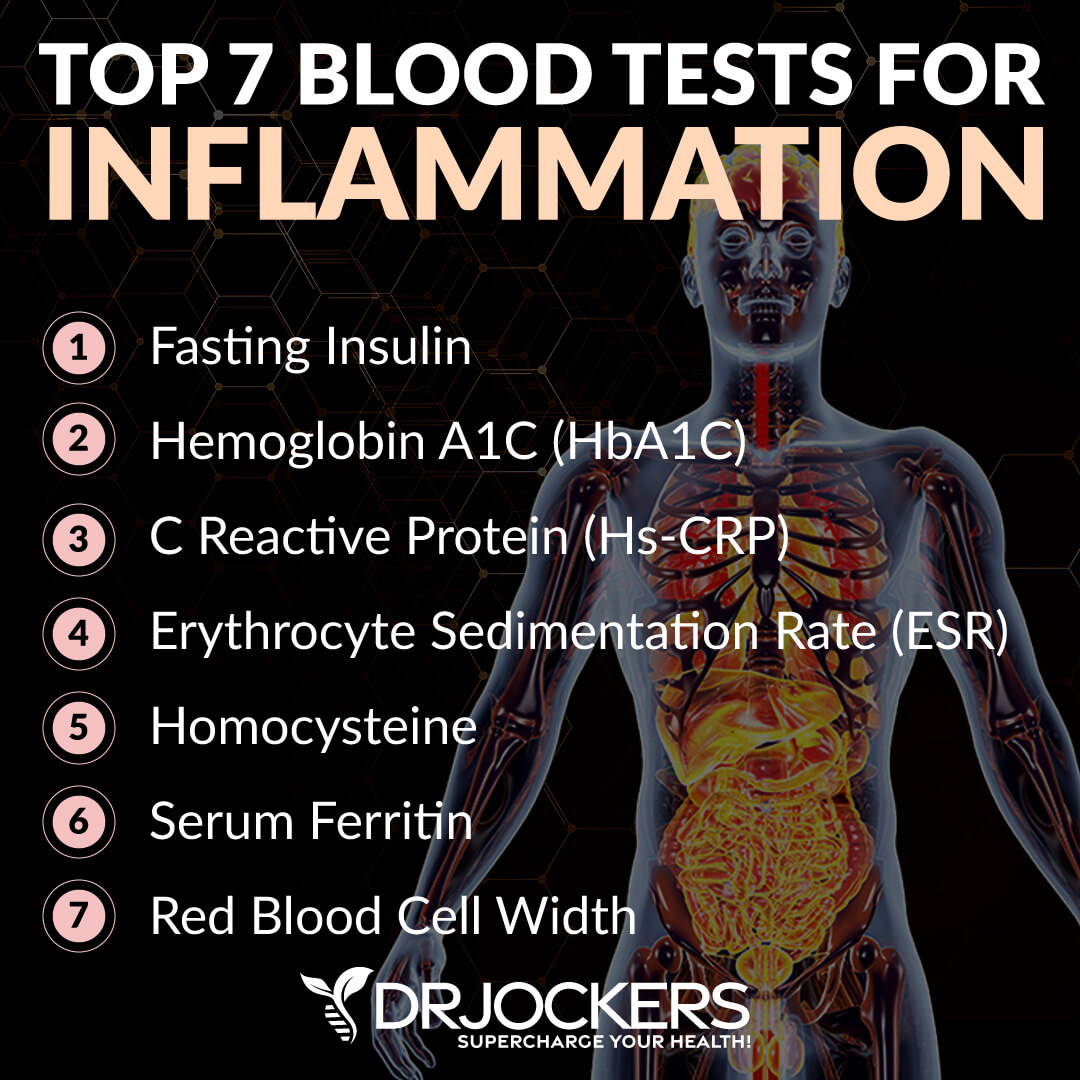
Besides looking at GlycA, we may also look at some additional markers of inflammation. Here is what I recommend:
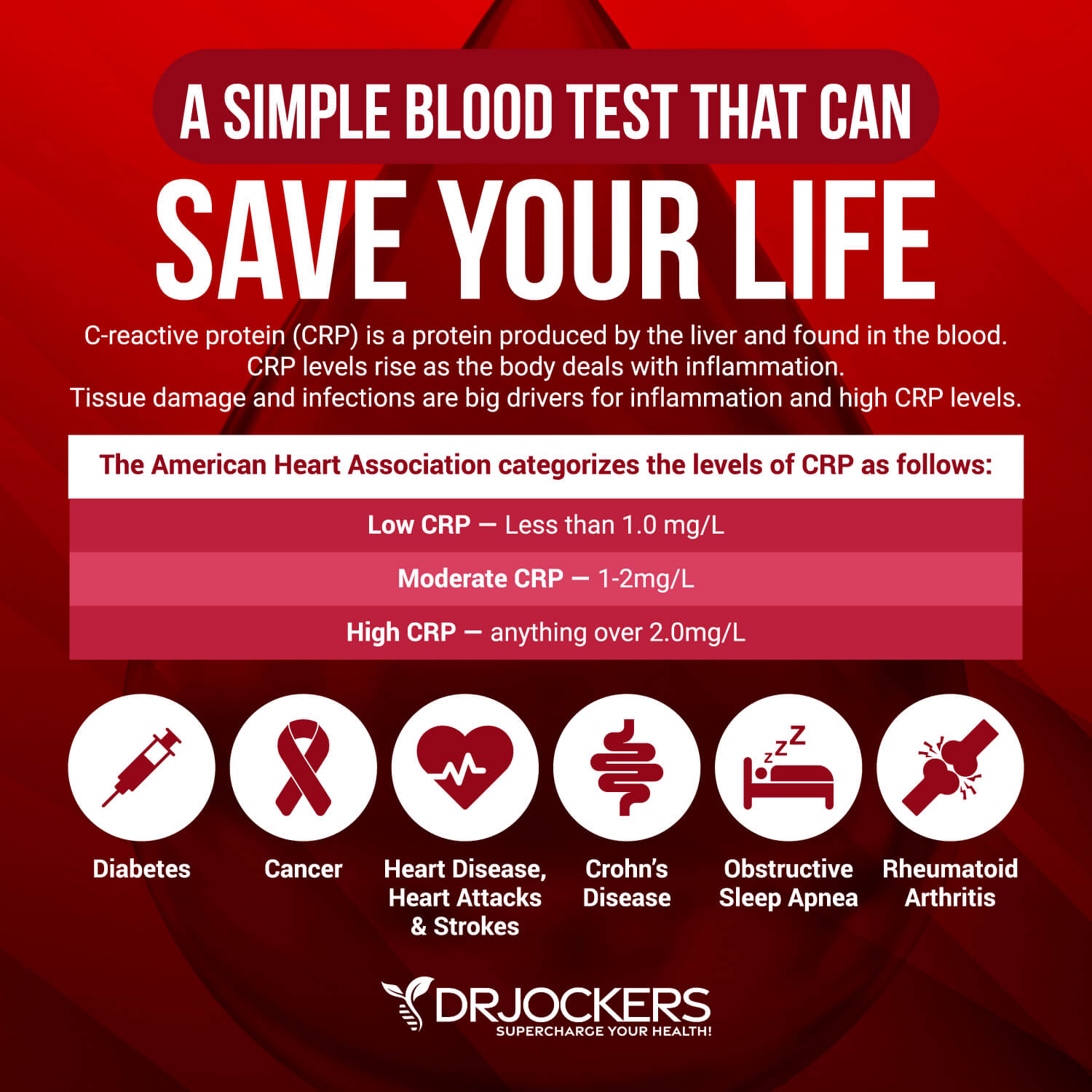
Hs-CRP
The C-reactive protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body.
Standard and optimal ranges include:
- The standard range is:
- Male: 0.00 – 2.9 mg/L (0.00 – 27.62 nmol/L)
- Female: 0.00 – 2.9 mg/L (0.00 – 27.62 nmol/L)
- The optimal range is:
- Male: 0.00 – 0.55 mg/L (0.00 – 5.24 nmol/L)
- Female: 0.00 – 1.00 mg/L (0.00 – 9.52 nmol/L)
When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
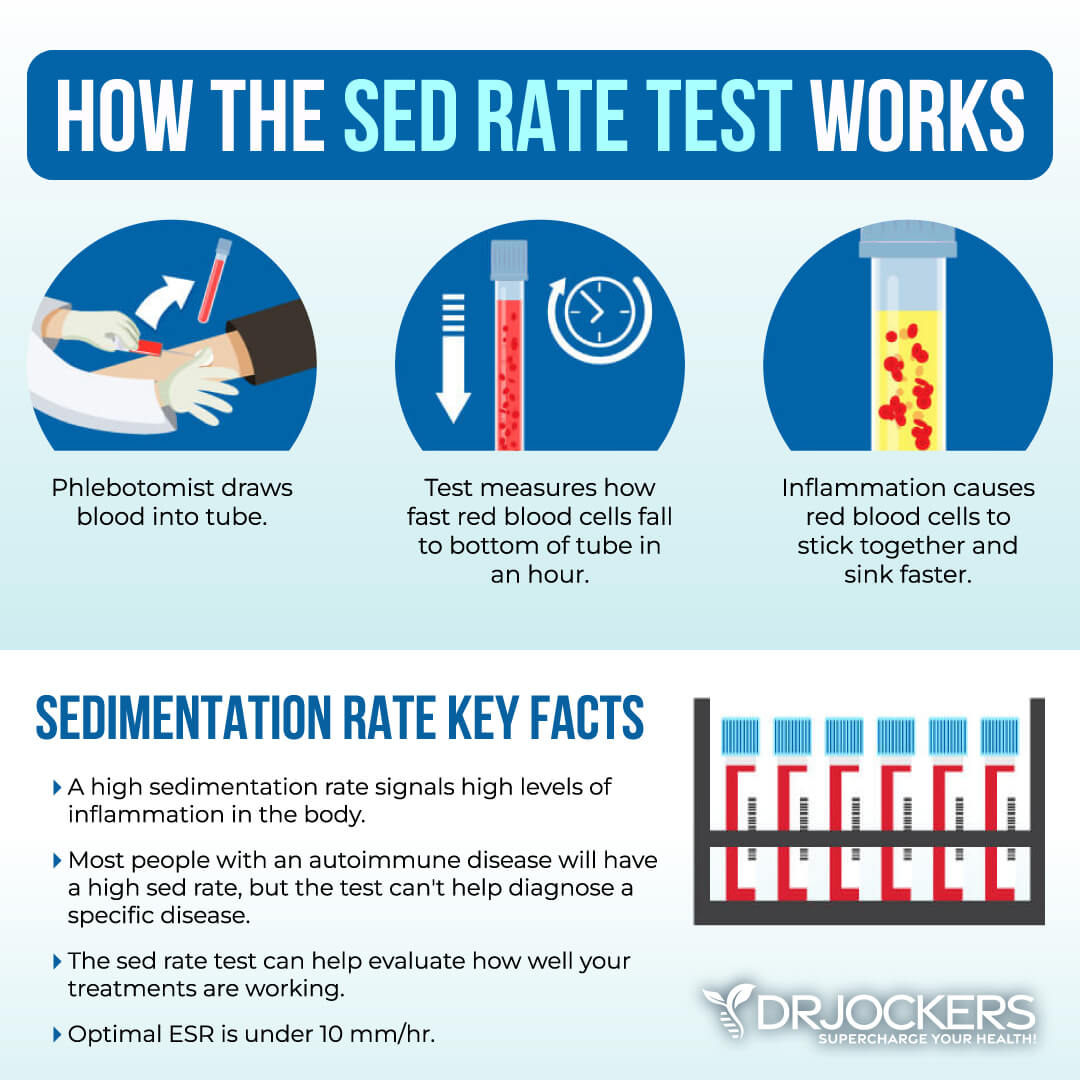
ESR
The erythrocyte sedimentation rate (ESR) can measure how fast red blood cells settle in a blood sample. High ESR levels may indicate inflammation, metabolic syndrome, infection, or cancer.
Standard and optimal ranges include:
- The standard range is:
- Male: 0.00 – 15.00 mm/hr
- Female: 0.00 – 20.00 mm/hr
- The optimal range is:
- Male: 0.00 – 5.00 mm/hr
- Female: 0.00 – 10.00 mm/hr
Fibrinogen
Fibrinogen is an acute phase reactant and clotting factor made in the liver. Elevated levels are linked to inflammation, cardiovascular disease, blood clots, peripheral artery disease, stroke, neurological issues, infections, and other issues.
Standard and optimal ranges include:
- The standard range is 175 – 425 mg/dL (5.14 – 12.50 umol/L)
- The optimal range is 175 – 300 mg/dL (5.14 – 8.82 umol/L)

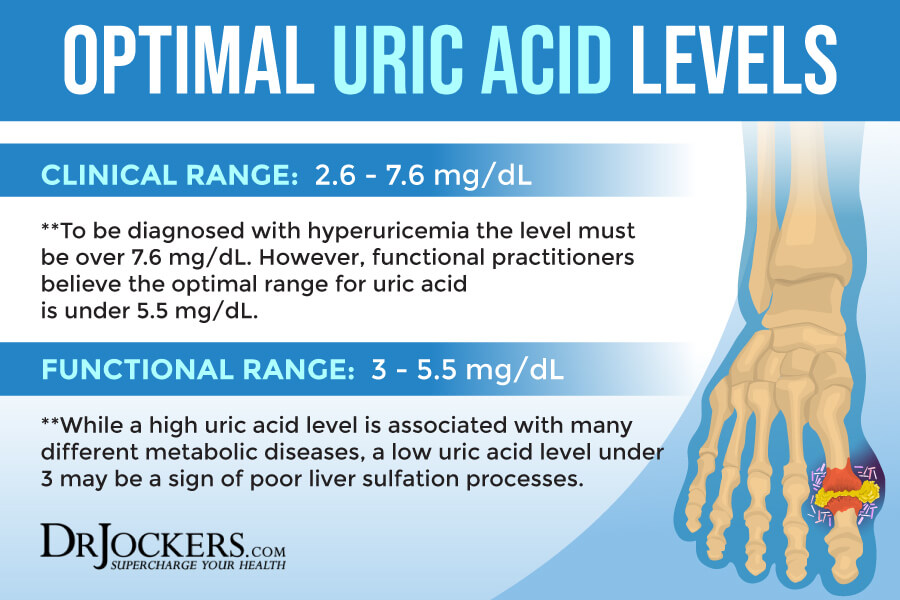
Uric Acid
Uric acid is a byproduct of purine metabolism. It serves as an antioxidant. High levels may be linked to heart disease, stroke, kidney stones, gout, and cognitive dysfunction from alcoholism, stress, ketoacidosis, cancer, and other issues.
Standard and optimal ranges include:
- The standard range is:
- Male: 3.45 – 8.00 mg/dL (205.21 – 475.84 umol/L)
- Female: 2.50 – 7.00 mg/dL (148.70 – 416.36 umol/L)
- The optimal range is:
- Male: 3.50 – 5.40 mg/dL (208.18 – 321.19 umol/L)
- Female: 3.00 – 4.70 mg/dL (178.44 – 279.57 umol/L)
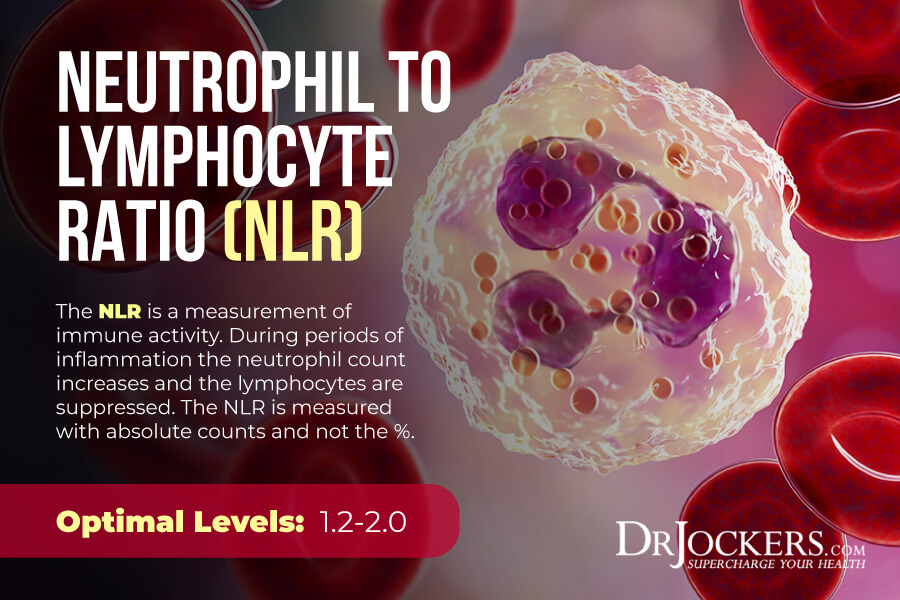
Neutrophil: Lymphocyte Ratio
The Neutrophil Lymphocyte Ratio (NLR) may indicate the body’s cell-mediated inflammatory response. High levels may be due to systemic inflammation due to shock, trauma, surgery, or disease. It may indicate diabetes, cardiovascular disease, viral or bacterial infections, hepatic dysfunction, or other issues.
Standard and optimal ranges include:
- The standard range is 1.00 – 3.00.
- The optimal range 1.00 – 1.70
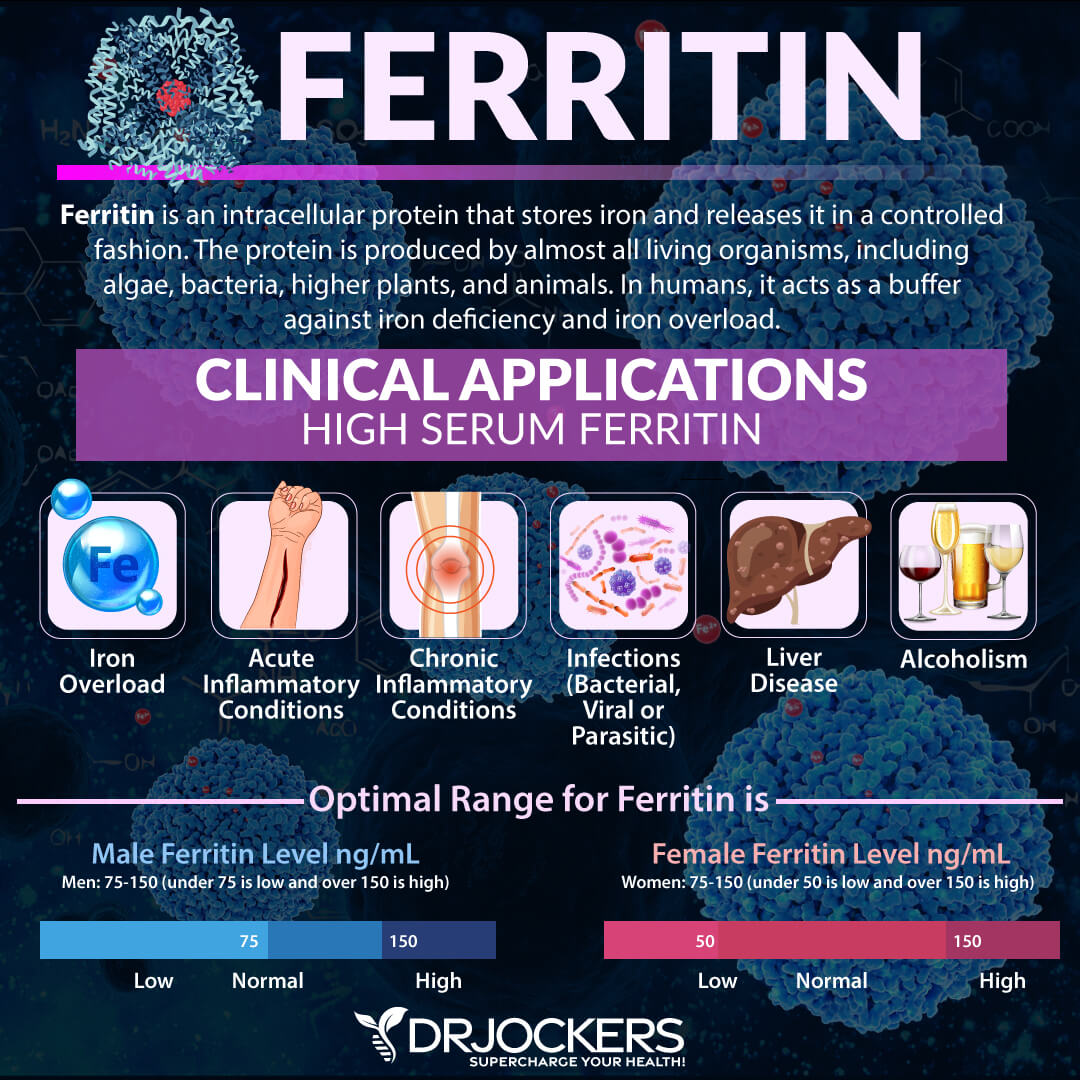
Serum Ferritin
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer.
Standard and optimal ranges include:
- The standard range is 16 – 232 ng/mL (16 – 232 ug/L)
- The optimal range is 45 – 79 ng/mL (45 – 79 ug/L)
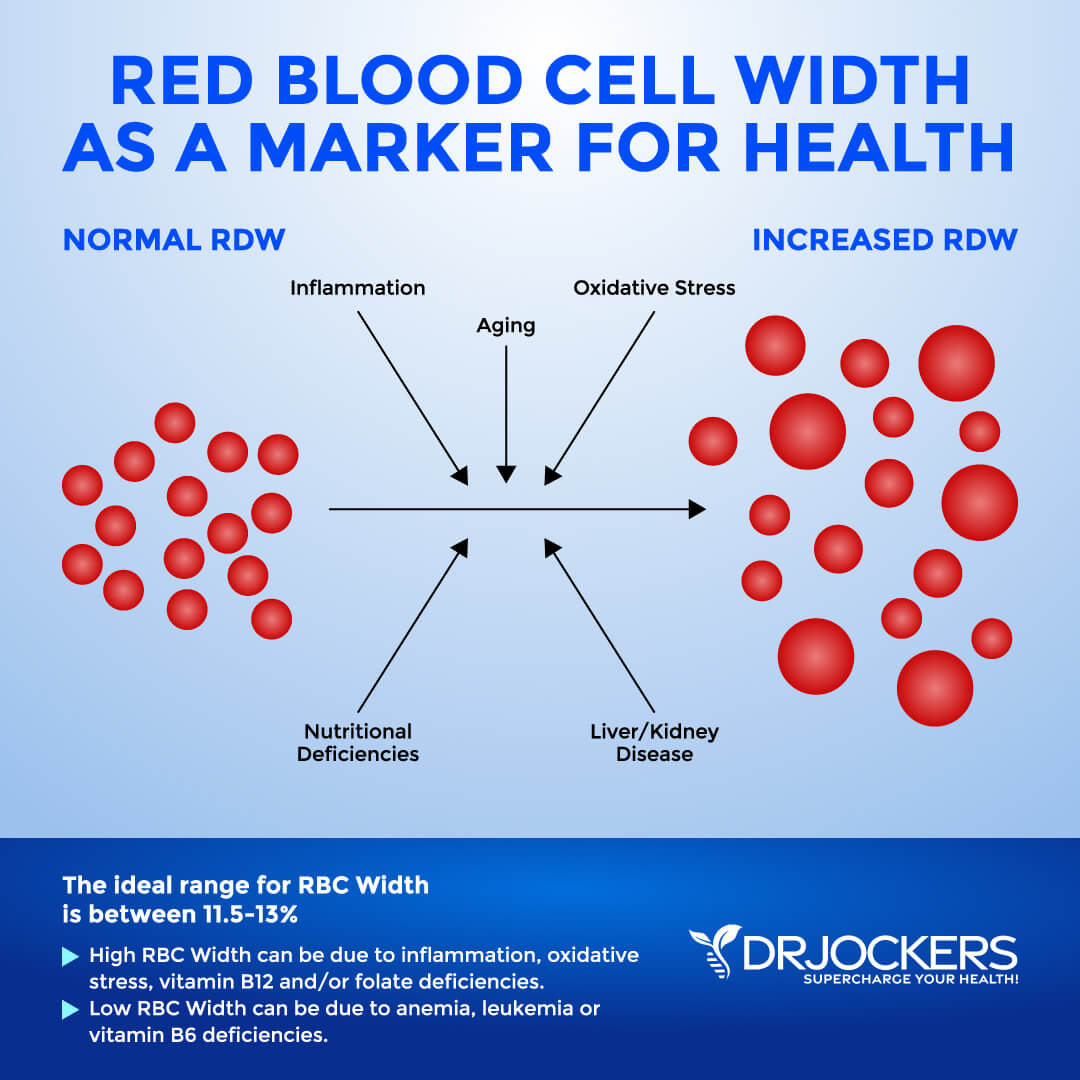
Red Blood Cell Width
The size of your blood cells has to do with maturation and also depends on methylating agents, such as folate and vitamin B12. Red Blood Cell Distribution (RDW) markers are a great way to detect underlying inflammation in your body.
Standard and optimal ranges include:
- The optimal range is 11.5 and 13 percent.
- The clinical range: 12.3 and 15.4 percent
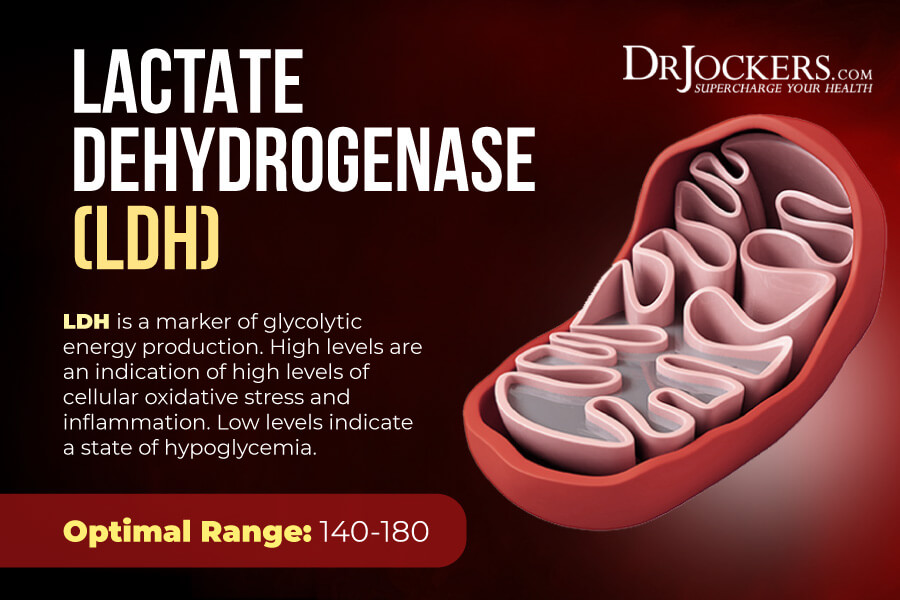
LDH
Lactate Dehydrogenase (LDH) is an enzyme found in all living cells. Elevated levels may indicate inflammation.
Standard and optimal ranges include:
- The standard range is 100.00 – 200.00 IU/L
- The optimal range is 140.00 – 180.00 IU/L
Platelet: Lymphocyte Ratio
The platelet: lymphocyte ratio (PLR) is a marker for looking at systemic inflammation, cardiovascular risks, and various cancer risks. High levels may indicate rheumatoid arthritis, cardiovascular issues, various types of cancer, bipolar disorder, and other health issues.
Standard and optimal ranges include:
- The standard range is below 150.
- The optimal range is below 128.
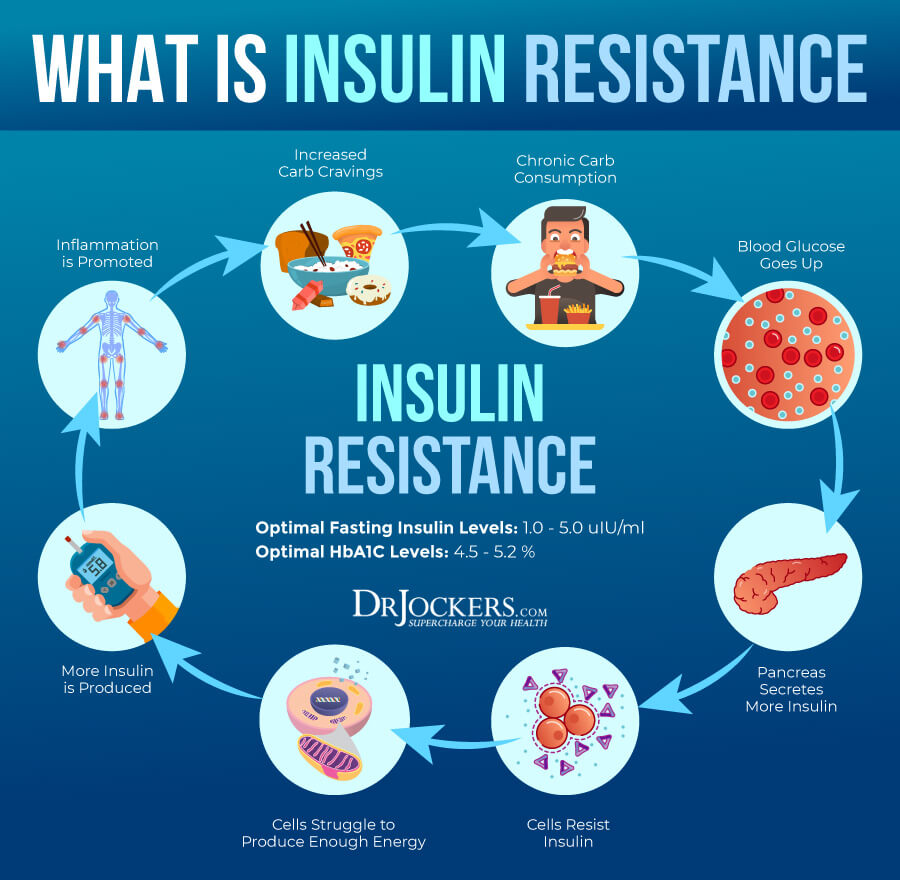
Fasting Insulin Levels
Blood sugar imbalances may increase your risk of inflammation. In addition to testing your HbA1C levels, I recommend checking your fasting insulin levels. Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes.
Standard and optimal ranges include:
- The standard range is 2 – 18.4 uIU/mL (13.89 – 127.78 pmol/L)
- The optimal range is 2 – 5 uIU/mL (13.89 – 34.72 pmol/L)
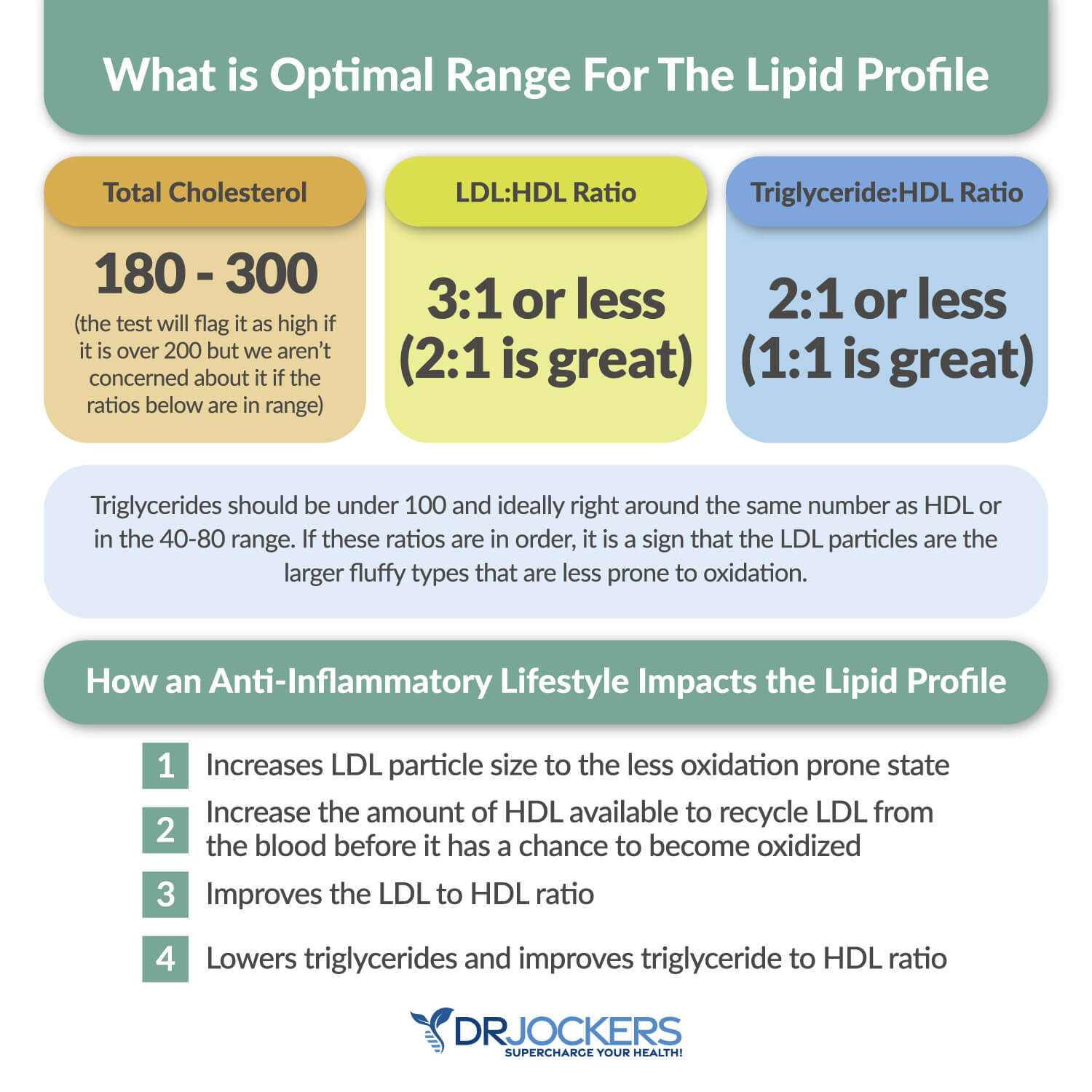
Lipid Panel
Your lipid paneer may be another indication of inflammation and related issues, such as clogged arteries and cardiovascular issues.
Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal. For triglycerides, we are looking for an HDL ratio: 2:1 or less, 1:1 being optimal. Higher rates may indicate insulin resistance and inflammation.
Optimal ranges include:
- VLDL cholesterol: The optimal range is 5 to 30 mg/dl.
- HDL cholesterol: The optimal range is 55 to 80. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The optimal range is 40 to 80.
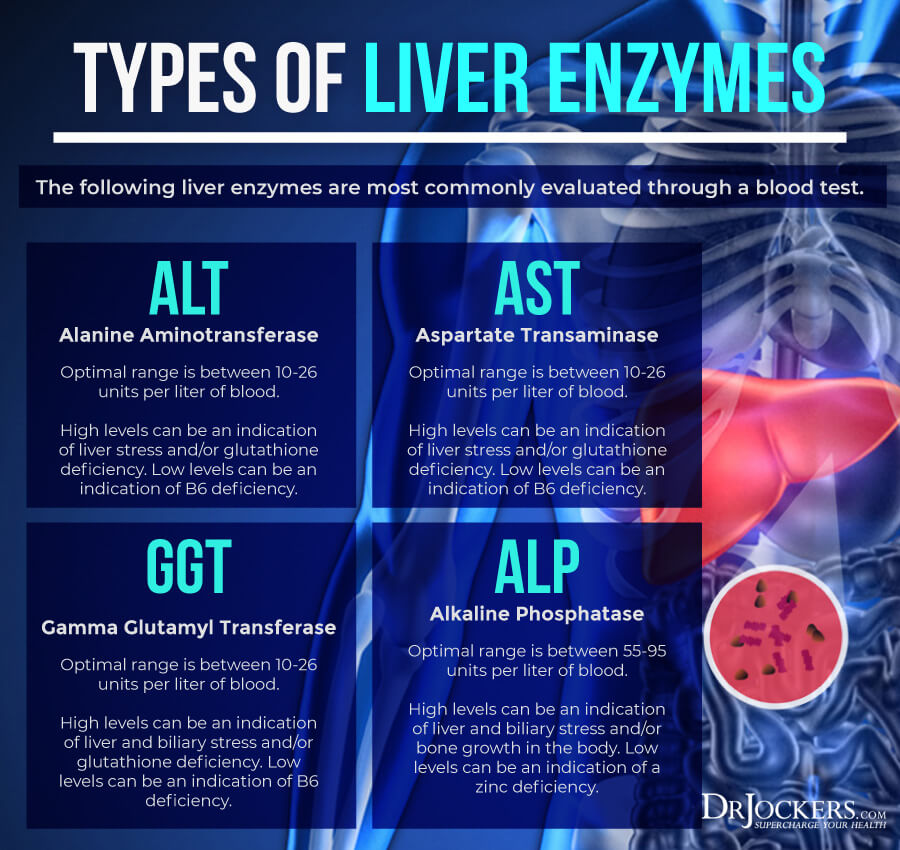
Liver Enzymes
Liver enzyme levels may also indicate inflammation, as well as liver, gallbladder, bile, or kidney issues.
Alkaline phosphatase is a liver enzyme that is made by the mucosal cells that line the bile system of the liver and helps normal bile flow. Elevated levels (over 95) may indicate inflammation and liver and gallbladder problems.
Alanine aminotransferase (AST) is a liver enzyme. Elevated levels may indicate inflammation.
Aspartate transaminase (ALT) is an enzyme present in the liver that spills out during times of increased liver stress. Elevated levels may indicate inflammation.
Gamma-Glutamyl Transpeptidase (GGT) is an enzyme in the liver, pancreas, and kidneys. Elevated levels may indicate inflammation and liver disease, usually due to alcoholism and/or sluggish gallbladder or gallstone obstruction.
Optimal ranges include:
- Normal alkaline phosphatase is under between 55-95 IU/L.
- Normal AST levels are between 10 and 26 IU/L.
- Normal ALT levels are between 10 and 26 IU/L.
- Normal GGT levels are between 10 and 26 IU/L. Levels lower than 10 IU/L can be an indication of a vitamin B6 deficiency.
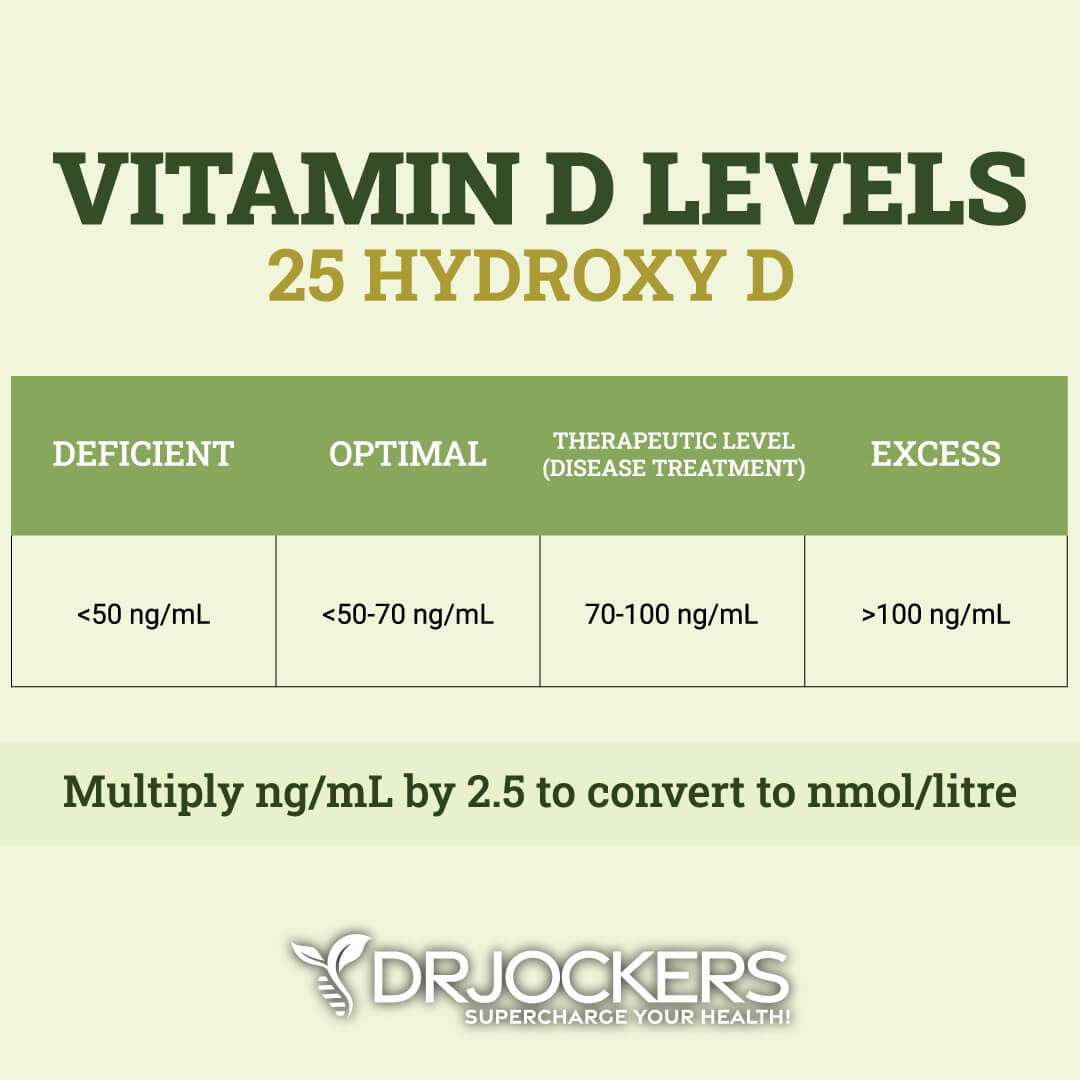
Vitamin D3 Levels
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation.
Standard and optimal ranges include:
- The standard range is 30.00 – 100.00 ng/mL (74.88 – 249.60 nmol/L)
- The optimal range is 50.00 – 90.00 ng/mL (124.80 – 224.64 nmol/L)
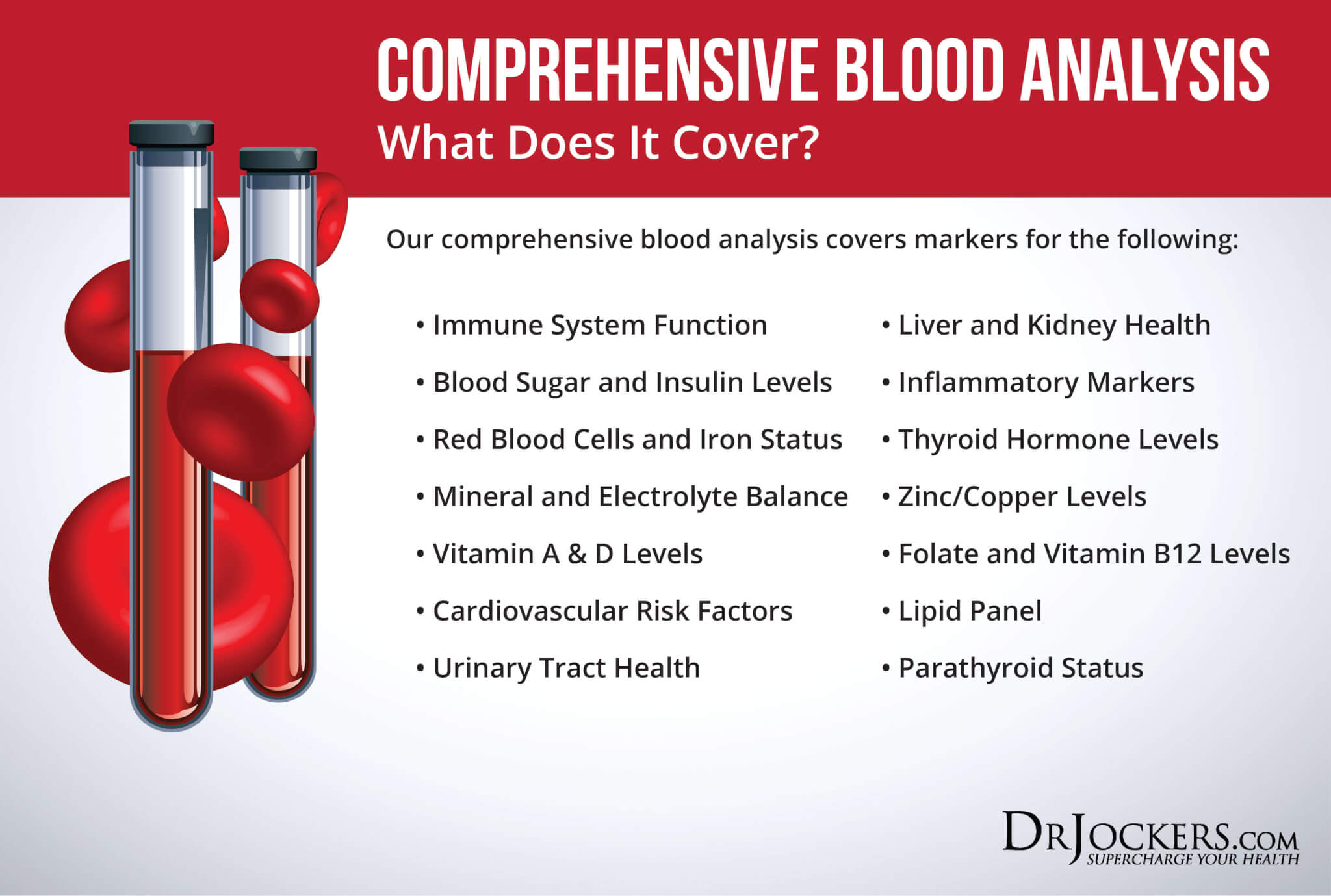
Comprehensive Blood Analysis
To check for these health markers, I recommend a Comprehensive Blood Analysis (CBA). This is the most detailed blood test that looks at all of these markers of inflammation. This test is more sophisticated than most conventional doctors are able to order.
It examines all parameters for inflammation, blood sugar levels, thyroid function, zinc and copper ratio, vitamin A and D levels, a complete metabolic panel, complete blood count, liver function, nutrient deficiencies, and more. I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your inflammation levels and progress.
Final Thoughts
Chronic inflammation is the root cause of most chronic symptoms and diseases. Testing for Glyca levels and other inflammatory biomarkers may help to find underlying chronic inflammation, hidden health issues, and the root causes of your problems, and to create an appropriate treatment plan, measure your progress, decrease your health risks, and regain your health and vitality. I recommend the Comprehensive Blood Analysis to test for GlycA and these other inflammatory biomarkers.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.

Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!