 Top 12 Nutrients and Herbs to Heal a Leaky Gut Lining
Top 12 Nutrients and Herbs to Heal a Leaky Gut Lining
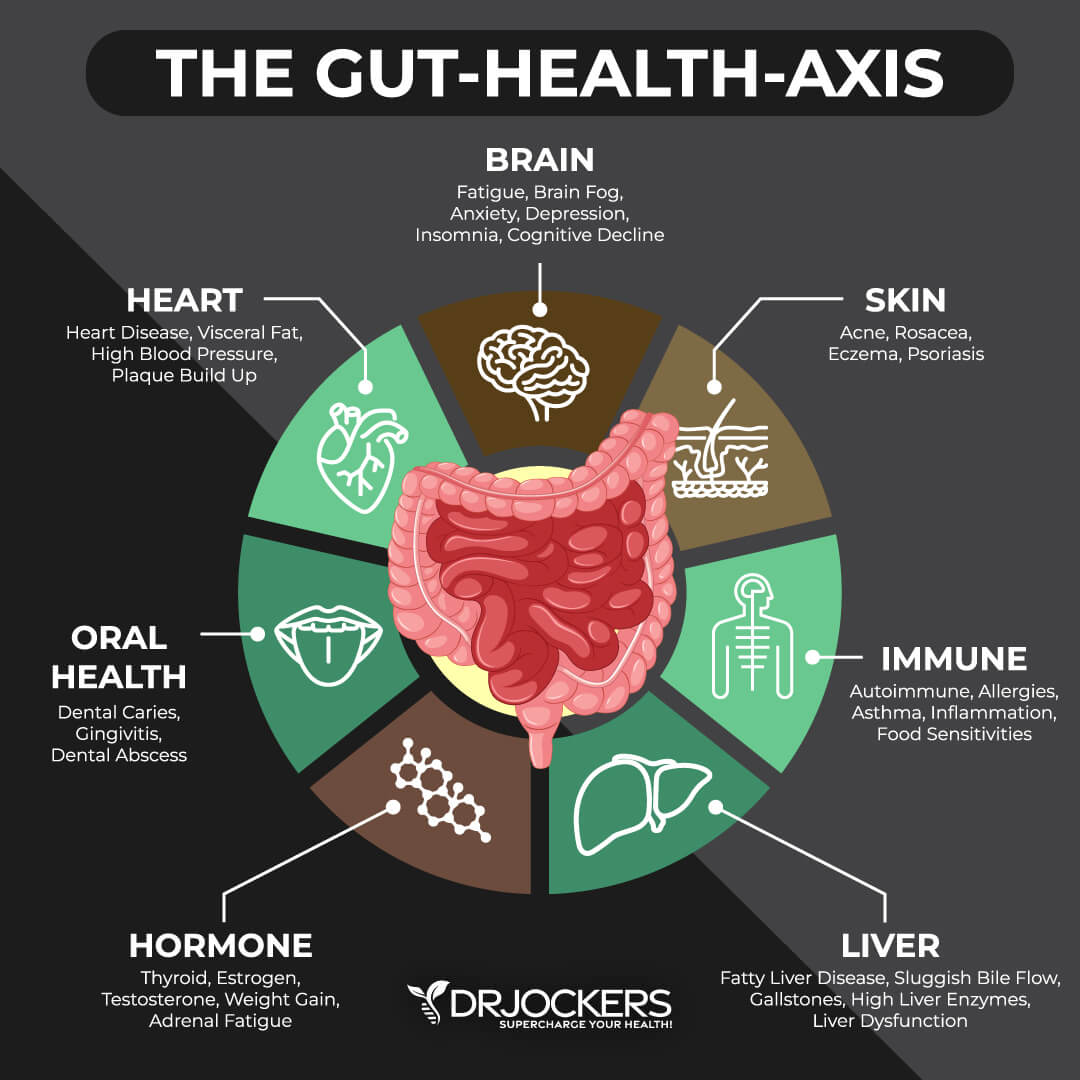
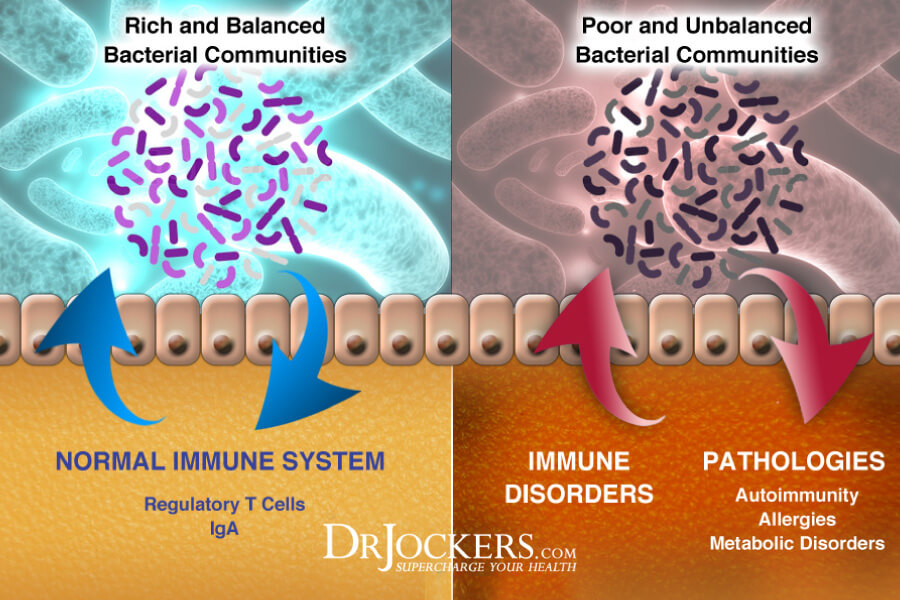
Your gut lining is incredibly important for your gut and overall health. If you develop leaky gut lining, it means that large food particles, microbes, and toxins pass from your gut to your bloodstream. This can increase the risk of chronic inflammation, gut inflammation, gut microbiome imbalance, chronic symptoms, autoimmunity, and chronic health issues. Fortunately, with the help of some nutrients and herbs, you can improve your leaky gut lining and regain your health.
In this article, I will discuss what leaky gut lining is. You will learn about the most common symptoms associated with leaky gut lining. I will go over the top root causes of gut inflammation. You will understand the importance of your gut mucosa. Finally, I will share my top 12 nutrients and herbs to repair leaky gut lining and recommend a powerful herbal supplement for leaky gut lining.
What is a Leaky Gut Lining
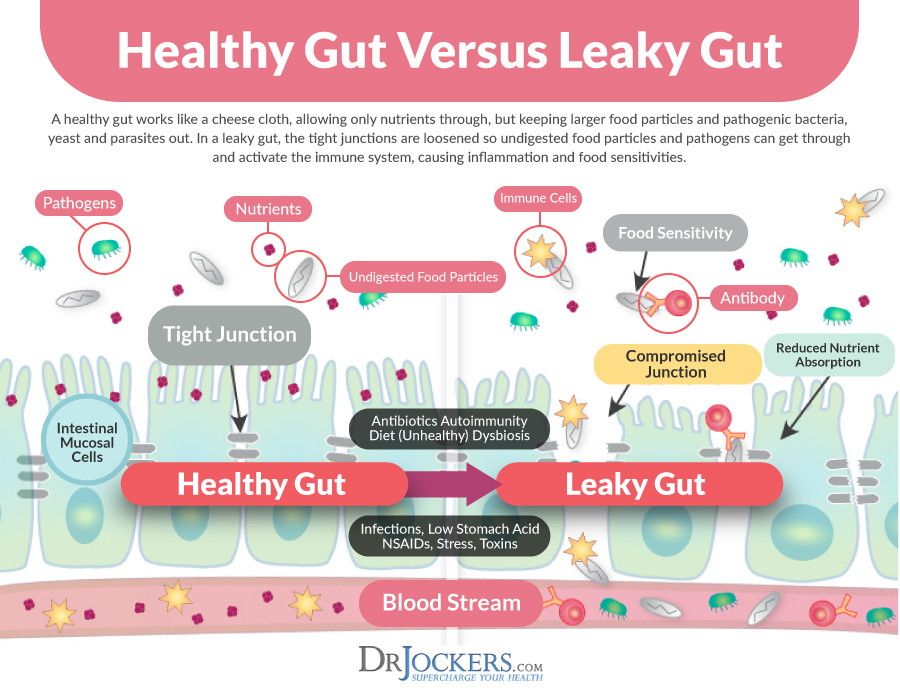
Your gut lining or mucous lining of your gut creates a barrier between your gut, your bloodstream, and the rest of your body. A healthy gut lining is naturally semi-permeable. This means that your gut lining has tiny little junctions of holes that allow micronutrients to pass through into your bloodstream. However, these junctions are not big enough for large food particles, microbes, and toxins to pass through. Pathogens will get eliminated through urine or stool instead of passing into your system. This keeps your gut and the rest of your body healthy.
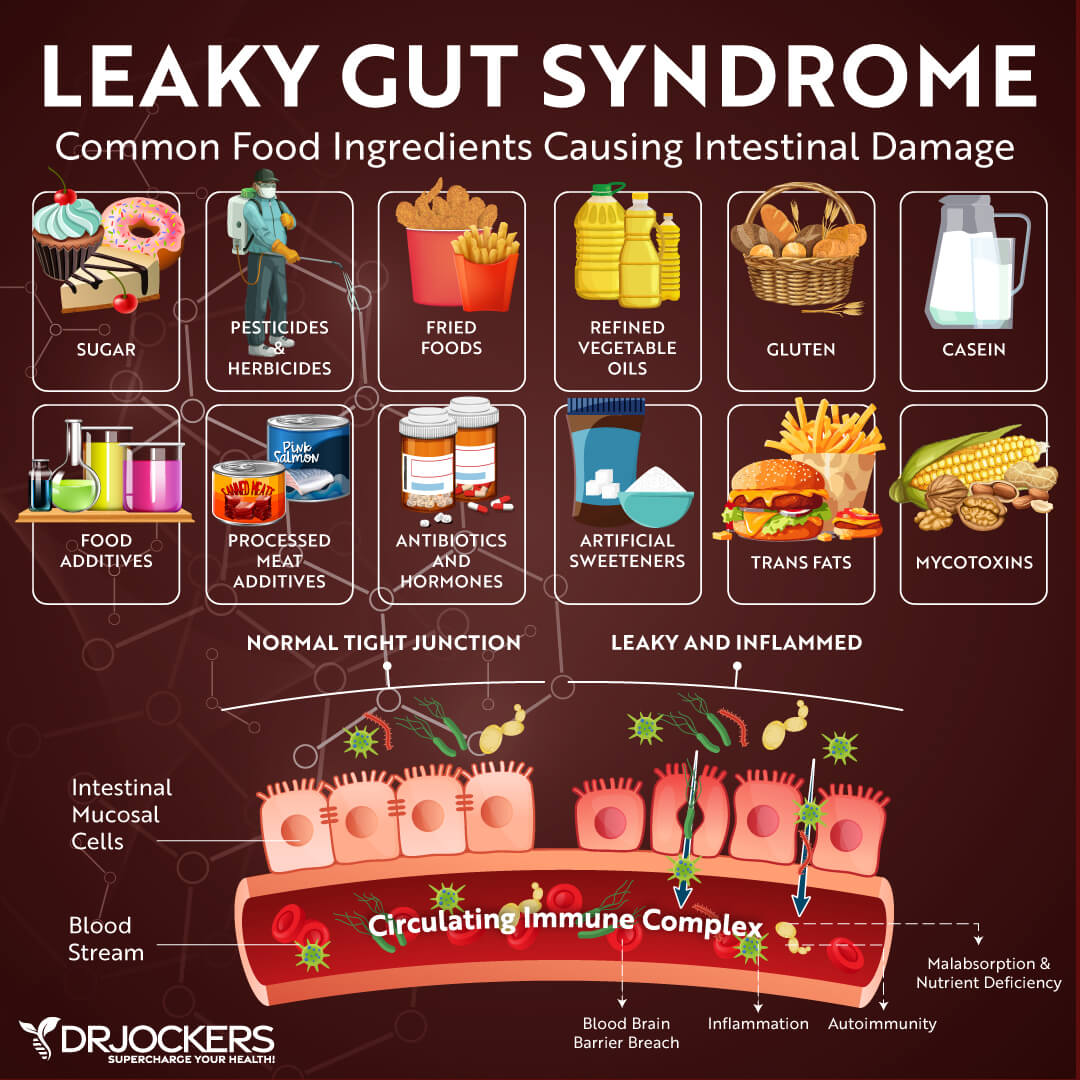
However, inflammatory foods, infections, environmental toxins, chronic stress, and other harmful external factors can damage your gut lining. Ongoing exposure to these negative factors can break apart these small holes in your gut lining causing them to be bigger. If these holes get too big and your gut lining becomes permeable instead of semi-permeable, larger food particles, microbes, pathogens, and toxins will be able to pass through into your bloodstream.
When this happens and these junctions get too big, it means you have leaky gut lining. This condition may also be referred to as intestinal permeability, gut permeability, leaky gut, or leaky gut syndrome. When big food particles, pathogens, microbes, and toxins pass through these junctions into your bloodstream, they can lead to serious gut health issues and chronic inflammation. This may lead to an ongoing chronic immune response, chronic symptoms, autoimmunity, and chronic health issues.
There is an increasing amount of research evidence on the serious risks and consequences of having a leaky gut lining. A 2012 review published in Clinical Reviews in Allergy and Immunology and a 2017 review published in Frontiers in Immunology have both found that leaky gut lining can increase the risk of autoimmune health issues (1, 2).
A 2021 study published in PLoS One has found that intestinal permeability may also increase the risk of metabolic health issues (3). According to a 2015 study published in Intestinal Research, leaky gut syndrome plays a role in the development of inflammatory bowel disease (4).
Symptoms Associated with a Leaky Gut Lining
Signs and symptoms of leaky gut lining may include:
- Digestive issues, including bloating, gas, constipation, diarrhea, nausea, or irritable bowel syndrome (IBS)
- Food allergies, food sensitivities, or food intolerances
- Skin problems, including acne, rashes, eczema, or rosacea
- Fatigue
- Insomnia or other sleep issues
- Brain fog, difficulties concentrating, memory troubles
- Mood imbalances, including anxiety and depression
- Headaches or migraines
- Chronic muscle or joint pain
- Getting sick often, slow recovery from illness, and other signs of poor immune health
- Seasonal allergies or asthma
- Hormonal imbalances, including irregular periods, PMS, or polycystic ovarian syndrome (PCOS)
- Autoimmune diseases, such as Celiac disease, Chron’s disease, rheumatoid arthritis, Hashimoto’s thyroiditis, lupus, or psoriasis
- Fibromyalgia
- Chronic fatigue syndrome
- Histamine intolerance and histamine reactions
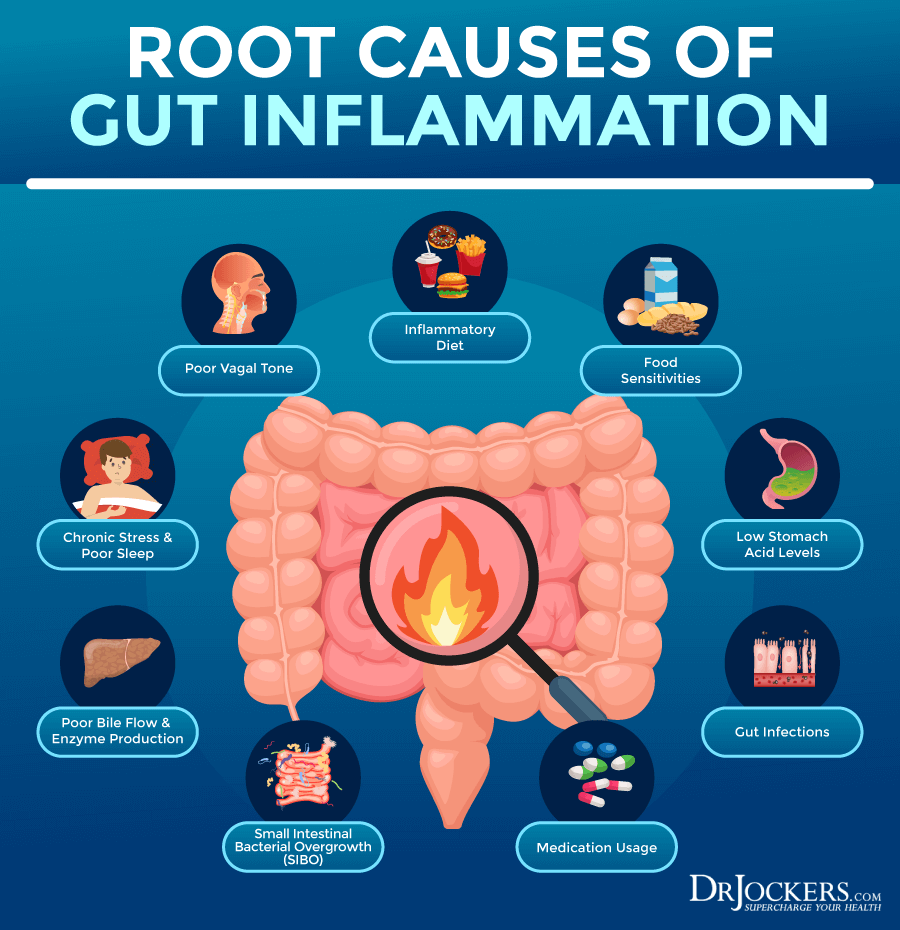
Root Causes of Gut Inflammation
You may develop gut inflammation for a variety of reasons. Let’s look at the main root causes of gut inflammation.
Inflammatory Diet
Following an inflammatory diet is one of the number one root causes of gut inflammation. Refined sugar and carbohydrates, refined oil, artificial ingredients, gluten, conventional dairy, additives, deep-fried foods, junk food, and overly processed foods can increase the risk of chronic inflammation, gut inflammation, and related health issues.
A 2021 study published in BMJ has found that dietary factors may determine the risk for gut inflammation (5). They found that inflammatory foods may increase gut inflammatory markers and gut imbalances, but an anti-inflammatory diet with lots of omega-3 fatty acids, vegetables, legumes, and fish may reduce the risk of gut inflammation.

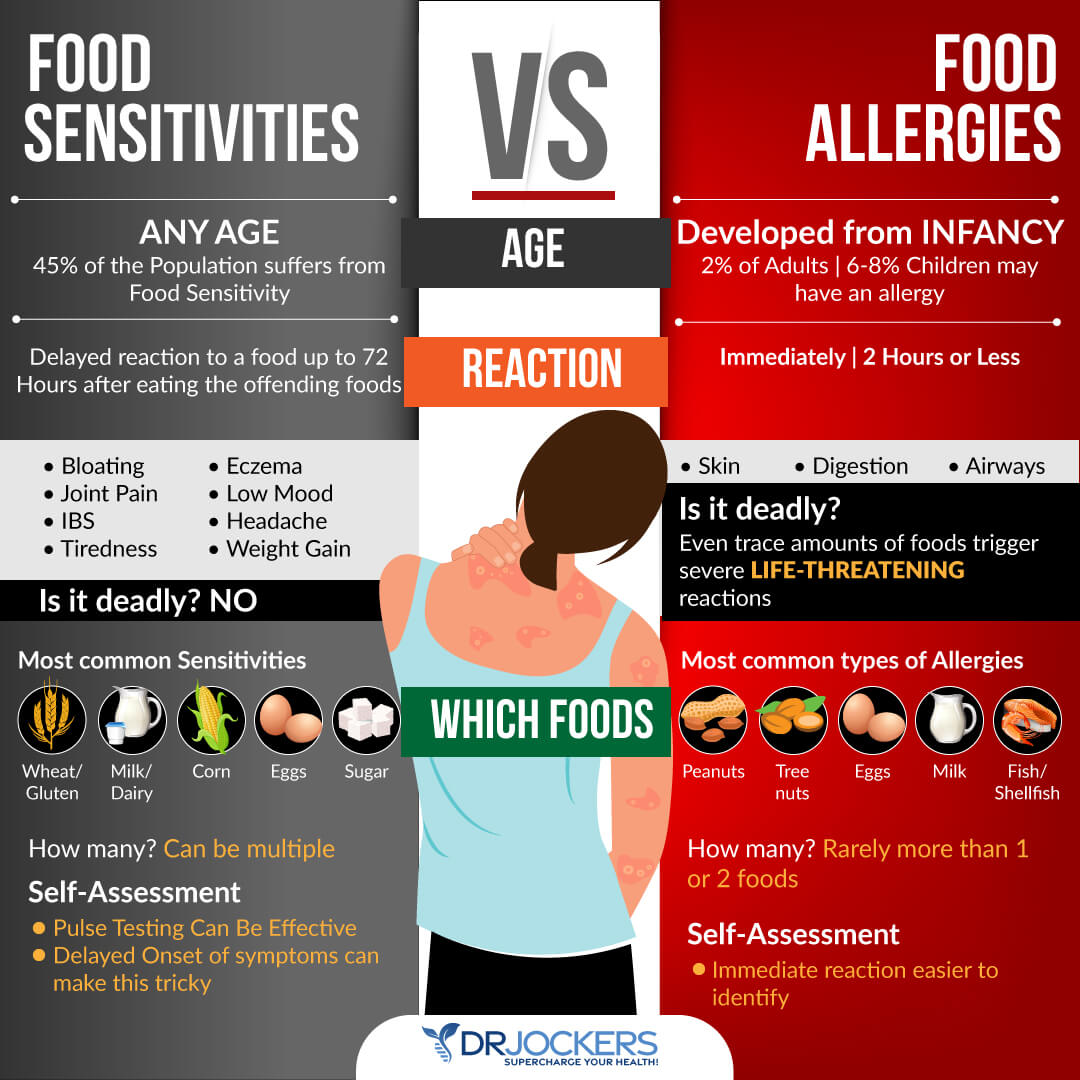
Food Sensitivities
Food sensitivities are another common root cause of gut inflammation. Unlike food allergies, food sensitivities generally don’t result in immediate symptoms. However, over time, they can lead to digestive issues, headaches, skin issues, fatigue, and other delayed and chronic symptoms. Consuming foods regularly that you are sensitive to can lead to gut inflammation. One of these common food sensitivities is gluten.
A 2016 study published in Tissue Barrier has found that gluten triggers the release of zonulin, which is a protein that causes the breakdown of tight protein junctions between intestinal epithelial cells, causing gut inflammation. (6). According to a 2019 study published in the International Journal of Molecular Sciences, gluten may also cause the activation of your mast cells, which release histamine, increasing the risk of gut inflammation (7).
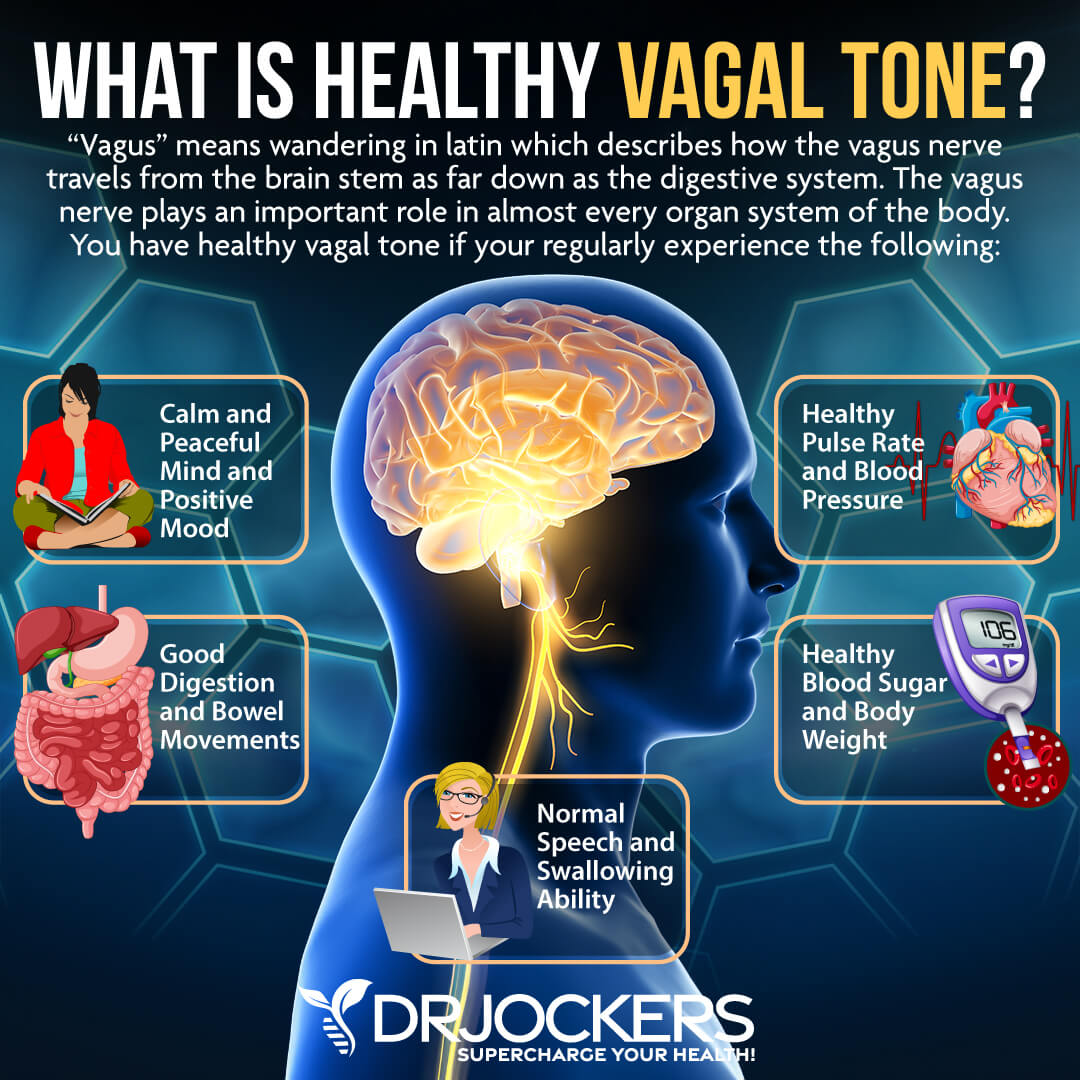
Poor Vagal Tone
Your vagus nerve is the tenth cranial nerve, which serves as your body’s major parasympathetic nerve. It helps to slow your heart rate, control gag reflex, allow involuntary constriction and relaxation of the muscles of your gut, control sweating, regulate blood pressure, and control vascular tone.
Excessive vagus nerve function and poor vagal tone can cause all kinds of issues, including anxiety, panic attacks, depression, other emotional health issues, dysautonomias, such as postural orthostatic tachycardia syndrome (POTS), migraines, headaches, tinnitus, hypertension, fibromyalgia, weight problems, and inflammatory issues.
It may also cause gut inflammation and gut health issues. According to a 2014 study published in PLoS One, people with gut inflammation-related problems, such as IBS and Crohn’s disease, tend to have reduced vagus nerve function and poor vagal tone (8).
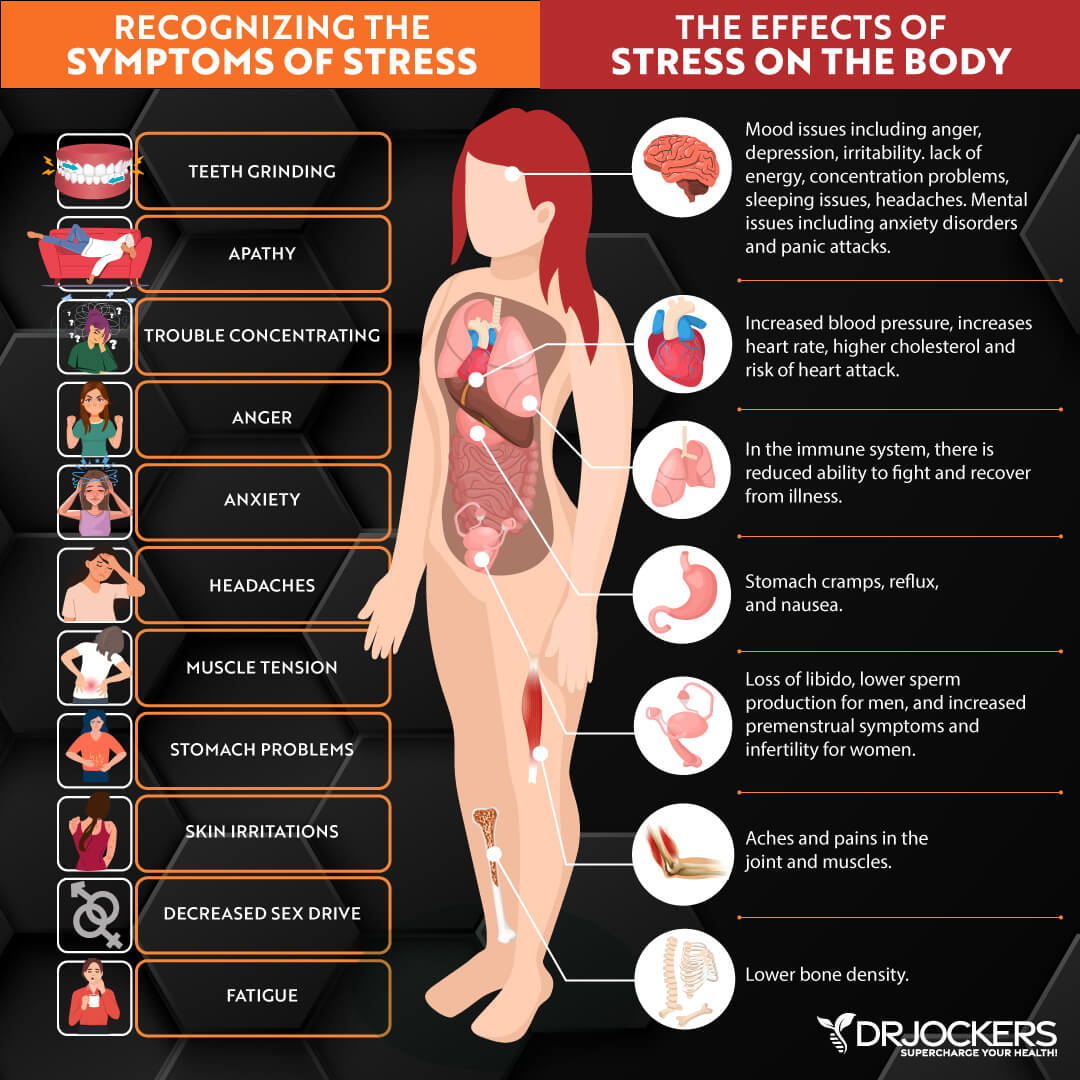
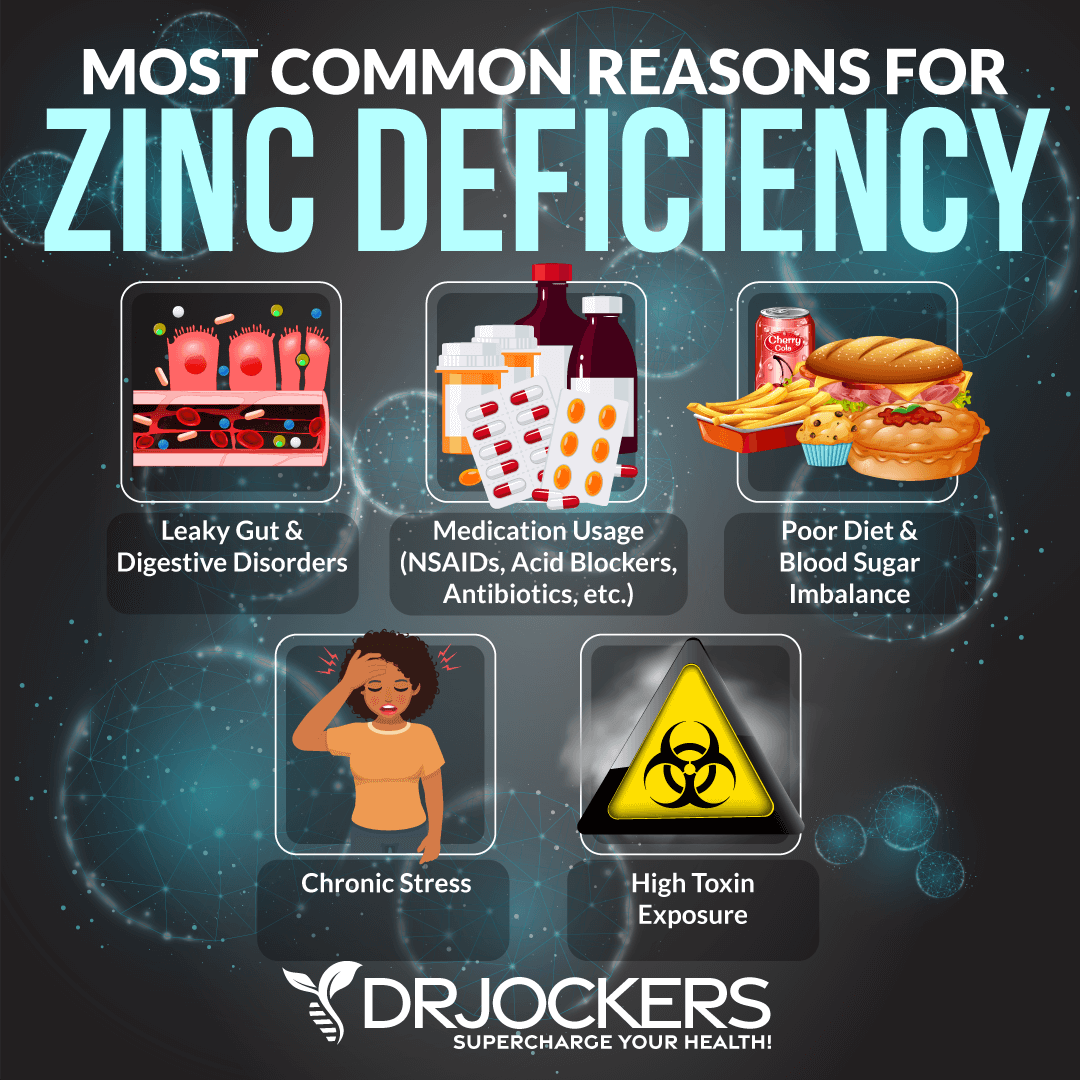
Chronic Stress, Poor Sleep, and Sedentary Lifestyle
Chronic stress, poor sleep, and a sedentary lifestyle are some of the top lifestyle factors involved with chronic inflammation, gut inflammation, and related problems. According to a 2017 study published in Oxidative Medicine and Cellular Longevity, a sedentary lifestyle can increase inflammatory molecules in the gut, while exercise can improve the gut microbiome and reduce inflammation (9).
A 2015 review published in Exercise Immunology Reviews has found that exercise can improve the gut microbiome and gut health (10). According to a 2009 study published in Sleep Medicine, poor sleep and sleep deprivation can worsen gut inflammation and interfere with recovery from gut inflammation related to colitis (11).
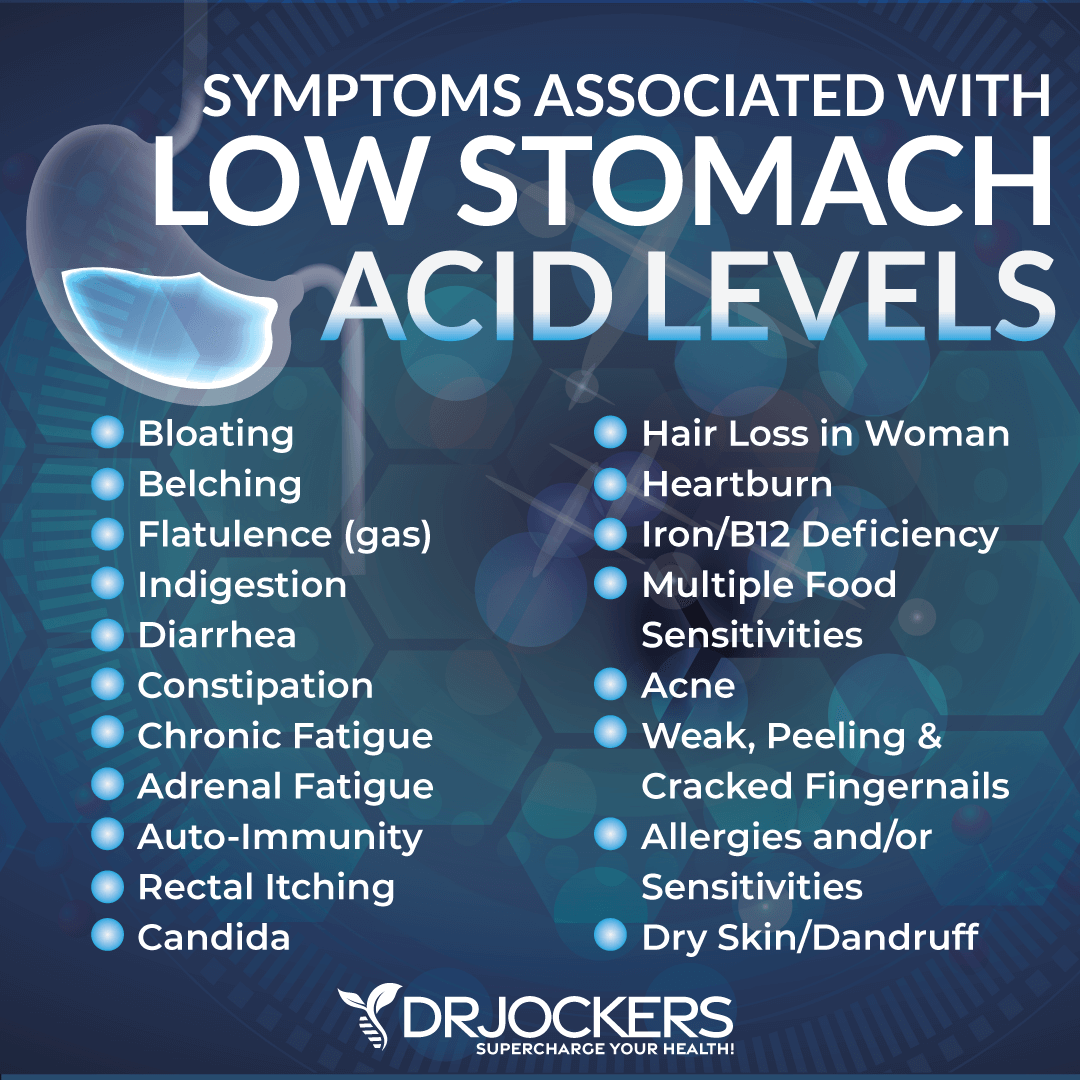
Low Stomach Acid Levels
Stomach acid is critical for disinfection, killing of microbes, and optimizing digestion. When your body is unable to produce enough stomach acid and you have low stomach acid, it may cause poor digestion, gut microbiome imbalance, and gut inflammation.
According to a 2008 study published in Infection and Immunology, low stomach acid can increase your risk of bacterial pathogen overgrowth, gut infections, and, consequently, gut inflammation (12).
Poor Digestive Juice Production
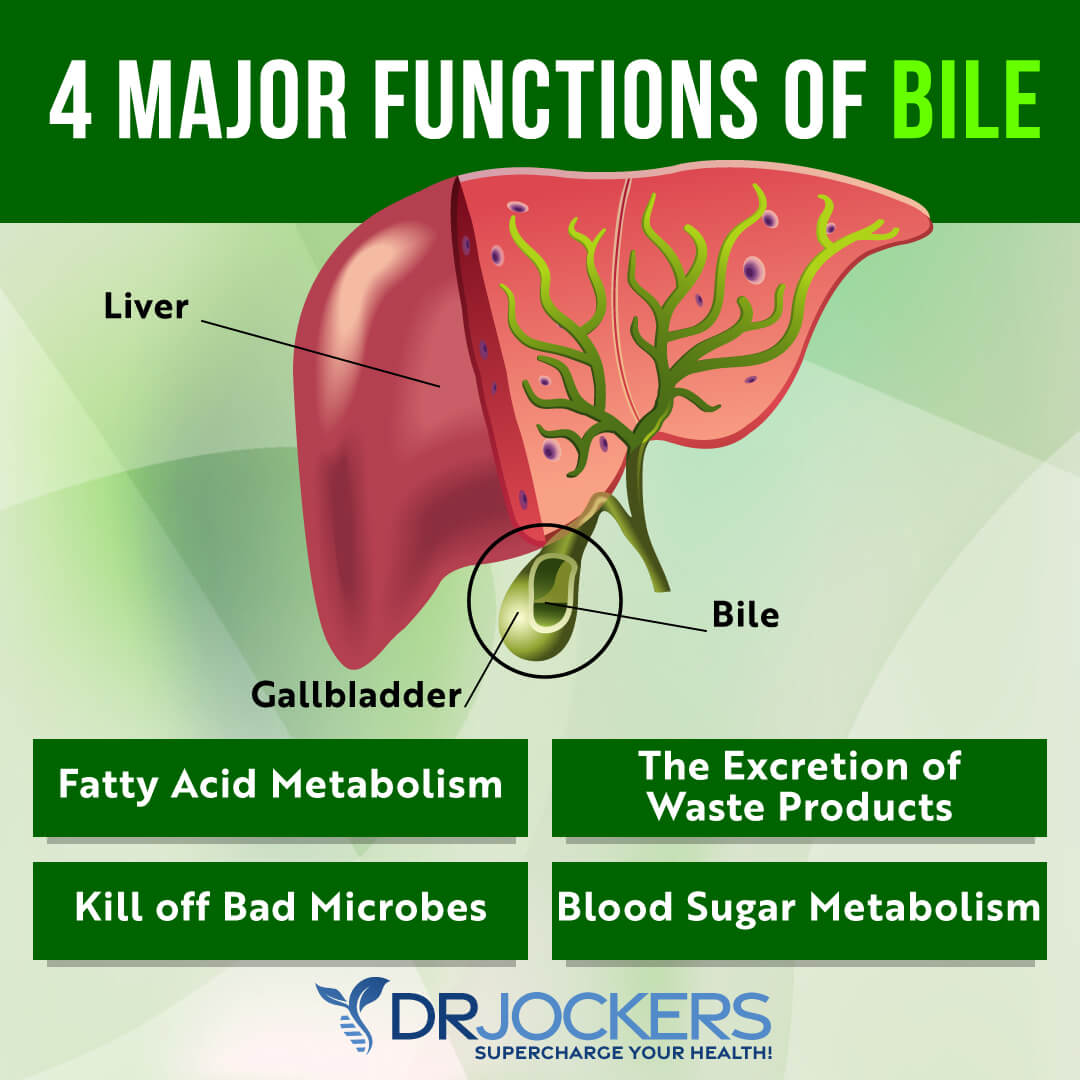
Bile is a greenish-brown liquid primarily made of cholesterol, bile salts, and bilirubin produced by your gallbladder. It’s important for digesting fats, overall digestion, and gut health. Pancreatic enzymes are secreted by your pancreas to break down fats, protein, and carbohydrates.
Problems with both bile flow and pancreatic enzyme production can result in gut inflammation. A 2018 study published in the Annals of Gastroenterology has found that poor bile flow can contribute to the development of inflammatory bowel disease (IBD) (13). A 2018 review published in the Journal of Clinical Medical Research has found that pancreatic dysfunction may be linked to IBDs (14).
Gut Infections
Gut infections, including H Pylori, parasites, yeast, bacterial, and viral infections, can all increase the risk of gut inflammation. According to a 2019 study published in FEBS Open Biology, H Pylori infection can increase pro-inflammatory bacteria growth in the gut and gut inflammation (15).
According to a 2018 study published in Frontiers in Immunology, viral infections may also alter the gut microbiome and cause gut inflammation (16). A 2019 study published in Peer Journal has found that parasitic infections may also disrupt the gut microbiome health resulting in gut inflammation (17).
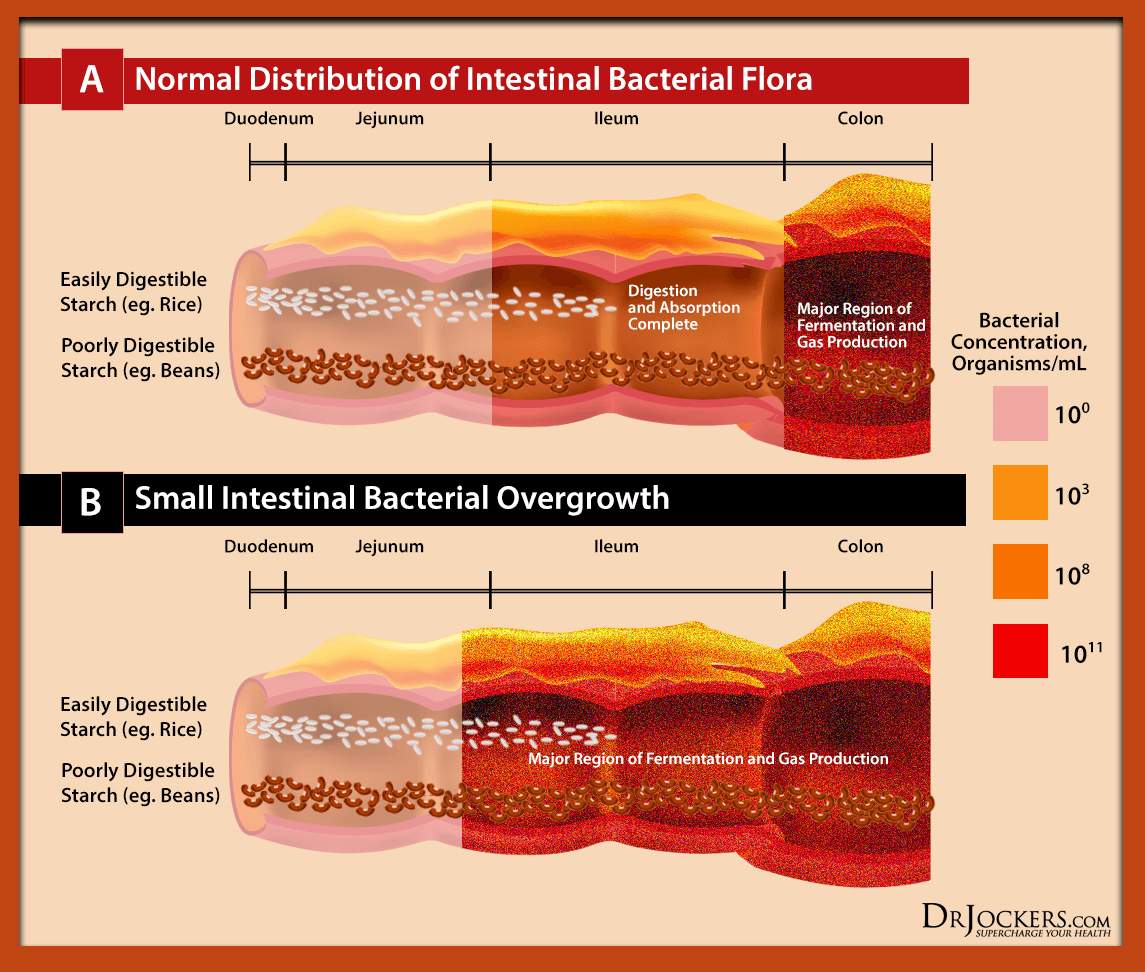
SIBO
Small intestinal bacterial overgrowth or SIBO refers to bacterial overgrowth in your small intestines. SIBO is characterized by abdominal pain, bloating, gas, constipation, diarrhea, fatigue, malnutrition, food sensitivities, and a list of other gut and non-gut-related chronic issues.
A 2007 review published in Gastroenterology and Hepatology has found that the excess bacteria in SIBO can trigger an intestinal inflammatory response and cause gut inflammation (18).
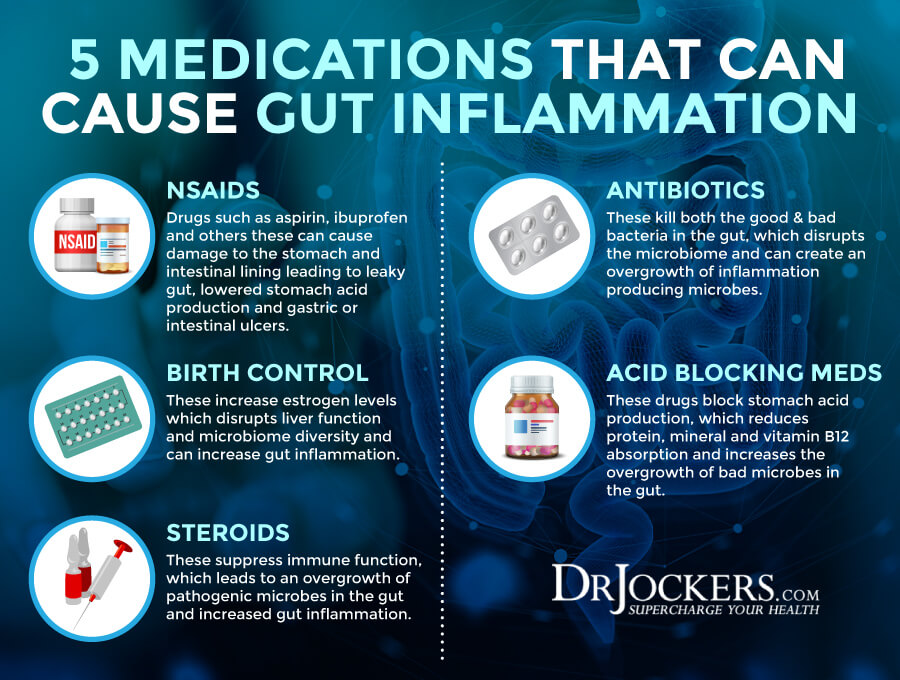
Medications
The use and overuse of certain medications can increase the risk of gut inflammation. Some of these medications that may lead to gut inflammation and related issues include antibiotics, proton pump inhibitors (PPI’s), selective serotonin reuptake inhibitors (SSRIs), non-steroidal anti-inflammatory drugs (NSAIDs), and oral contraceptives.
Even though antibiotics are created to fight bacterial infections, overuse or misuse of antibiotics or not rebalancing the gut flora with probiotics after antibiotic use can lead to gut issues. A 2015 study published in PLoS One has found that antibiotics may increase the risk of gut inflammation and leaky gut (19).
According to a 2019 study published in Scientific Reports, long-term PPI-use may reduce good, anti-inflammatory gut bacteria and increase bad bacteria overgrowth and gut inflammation (20). According to a 2019 study published in Peer Journal, SSRIs may increase the risk of gut dysbiosis and inflammation (21).
According to a 2015 study published in Clinical Microbial Infections, NSAIDs may also increase gut microbiome imbalance and gut inflammation (22). Finally, a 2016 study published in Gastroenterology has found that long-term use of oral contraceptives may also increase the risk of gut inflammation and complications in Crohn’s disease (23).
Importance of Gut Mucosa
Your gut mucosa or intestinal mucosa creates the inner lining of your intestinal tract. It is the innermost layer of your intestinal tract. It is made of epithelium cells, thin connective tissues, specialized goblet cells, and secretes sticky mucus throughout your gut. It helps absorption and secretion.
According to a 2020 review published in Frontiers in Cellular and Infection Microbiology, your gut mucosa is essential for creating intestinal homeostasis (24). A 2017 review published in Expert Reviews in Gastroenterology and Hepatology has found that the health of your gut mucosal and gut lining plays a fundamental role in your health and problems may lead to Celiac disease, inflammatory bowel diseases, (IBDs), and non-alcoholic fatty liver disease (25).
According to a 2012 review published in Current Opinions in Microbiology, an unhealthy mucus layer may also increase gut infections, gut inflammation, and chronic inflammation (26). The health of your gut mucosa may not only affect the health of your gut, but the health of your neurological and brain health and other areas of your health (24).
Top 12 Nutrients to Heal the Gut Lining
Keeping your gut lining healthy is critical for your overall health and well-being. Fortunately, nutrition is here to help. Let’s look at the top 12 nutrients that may help to support and improve your gut lining.
Zinc
Zinc is a critical mineral for your immune health, metabolism, and other areas of your health. Zinc is also a mineral that your body cannot make on its own. This means that you need to get your required intake of zinc through food and supplement.
According to a 2001 study published in Inflammatory Bowel Diseases, zinc may have to tighten leaky gut lining in Crohn’s disease patients (27). A 2014 study published in the World Journal of Gastrointestinal Pathophysiology suggests that supplementing with zinc may help to prevent gastrointestinal disease (28).
Quercetin
Quercetin is a plant compound found in grapes, apples, blueberries, black currants, cherries, black plums, cranberries, cruciferous vegetables, kale, red leaf lettuce, romaine lettuce, chicory greens, cabbage, sprouts, snap pea, red onion, peppers, herbs, and olive oil.
It is known for its antioxidant, histamine-reducing, and anti-inflammatory properties. A 2009 study published in the Journal of Nutrition has found that quercetin may help to improve the gut barrier function (29). In a 2019 study published in Frontiers in Microbiology, quercetin helps to improve microbial diversity in the gut and reduce gut inflammation and inflammatory intestinal issues (30).

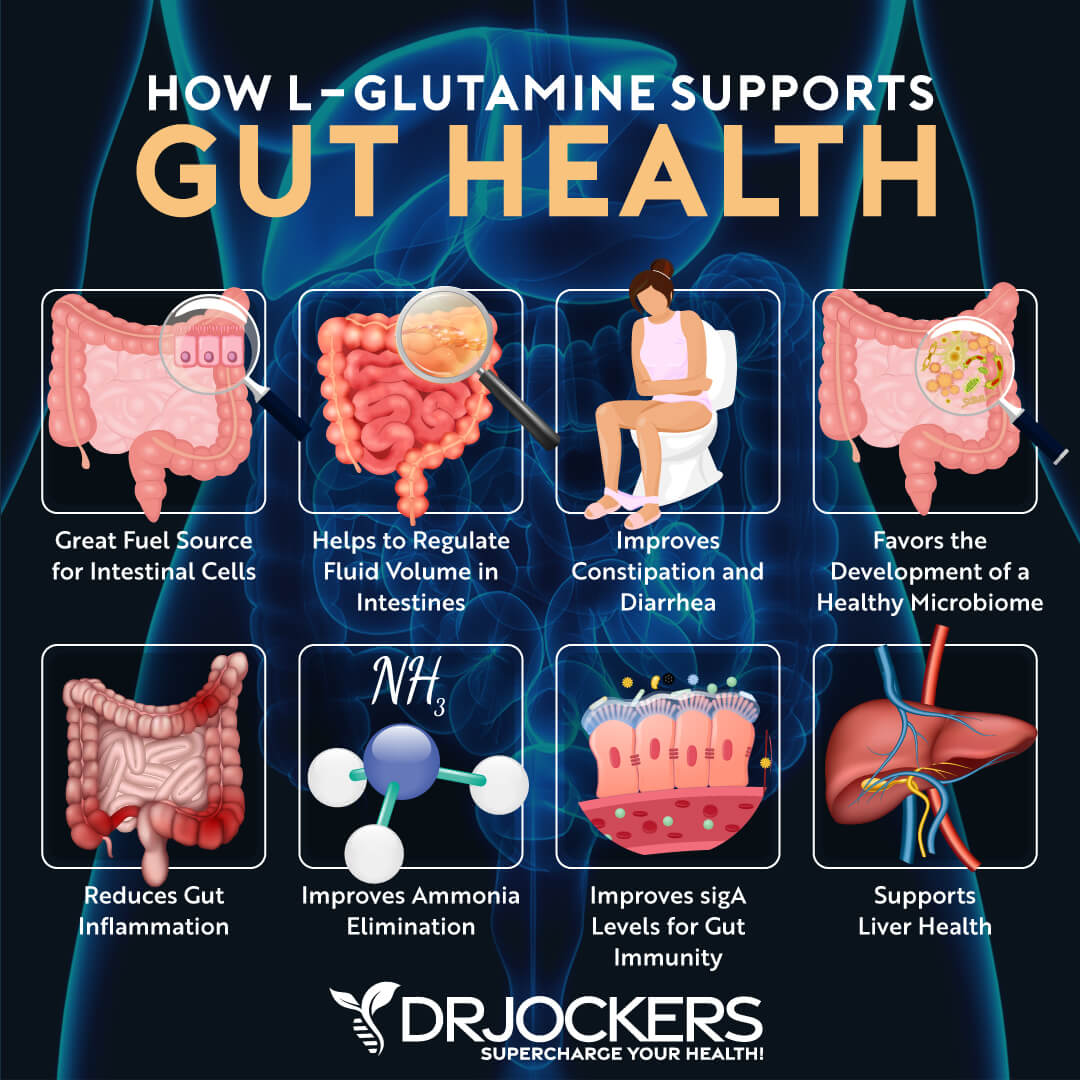
L-Glutamine
L-glutamine is a non-essential amino acid. Its role is to serve as an energy source for both your intestinal and immune cells. It also allows your gut lining to be healthy and helps the healthy growth and function of your intestinal cells.
A 2012 study published in the Journal of Epithelial Biology and Pharmacology has found that l-glutamine plays an important role in the gut barrier function, gut mucosal health, metabolism, and the reduction of gut inflammation (31). According to a 2017 study published in the Journal of Molecular Sciences, L-glutamine can be beneficial for intestinal diseases and gut inflammation (32).
Aloe Vera
Aloe vera is a medicinal plant commonly used topically for wounds, sunburn, and other skin concerns. Used internally, aloe vera may help to support digestion and detoxification. In natural medicine, aloe is renowned for its ability to support the gut mucosa and the integrity of the gut lining.
According to a 2021 study published in the International Journal of Molecular Sciences, aloe vera may help to keep your gut lining and intestinal junctions healthy (33). We recommend using aloe vera gel or supplementation to support the gut mucosa and strengthen the gut lining.

Slippery Elm
Slippery elm is a tree in North America with medicinal properties. Topically, it’s commonly used for sores, wounds, boils, and other skin inflammation and skin issues. Orally, it is often recommended for stomach problems, diarrhea, sore throat, and coughs.
According to a 2018 study published in the Journal of Alternative and Complementary Medicine, slippery elm may help to improve digestion and reduce the risk of gut health issues and related diseases (34).
MSM
MSM is a natural compound that may help to decrease inflammation, reduce joint pain, and support immune health. Foods sources of MSM include leafy green vegetables, alfalfa sprouts, apples, tomatoes, raspberries, tea, and coffee.
A 2016 study published in the Journal of Sports Medicine (Hindawi) has found that MSM can help to reduce inflammation (35). By reducing chronic inflammation, it may reduce gut inflammation and gut damage. It may also help to reduce inflammatory response if you already have a leaky gut lining.

N-Acetyl D Glucosamine
N-Acetyl D glucosamine is a bacterial metabolite that may be beneficial for inflammatory bowel diseases (IBDs) and arthritis. According to a 2018 study published in Gut Pathogens, N-Acetyl D glucosamine may help to reduce biofilm formation by harmful bacteria that may cause gut microbiome imbalance and leaky gut (38).
Marshmallow Root
Marshmallow root is a perennial herb from Western Asia, Northern Africa, and Europe. It is commonly used for digestive and skin problems. A 2015 study published in the Journal of Natural Science, Biology, and Medicine has found that marshmallow extract may be protective against peptic ulcers and may help to reduce inflammation and histamine release often associated with leaky gut lining (37).

Mucin
Mucins are macromolecules found in mucus supporting its biochemical and biophysical properties. It supports lubrication, cell signaling, and other functions in your body. According to a 2020 study published in Gut, mucins support the mucus barrier, gut lining, and gut microbiome (39).
Chamomile
Chamomile is one of the most well-known herbal medicines. It is commonly recommended as a digestive relaxant, for digestive complaints, and for sleep.
According to a 2020 study published in Biomolecules, chamomile flower extract may help to reduce inflammation, stabilize the intestinal barrier, and improve intestinal mucosal health (36). I recommend drinking a cup of chamomile tea every night to support relaxation, sleep and gut health.

Cat’s Claw
Cat’s claw is an herbal medicine grown in the Amazon forest and tropical areas. It is commonly used for inflammation and for fighting viral infections. According to a 2002 study published in the Alimentary Pharmacology and Therapeutics, cat’s claws may help to reduce inflammation and may be beneficial for digestive complaints (40).
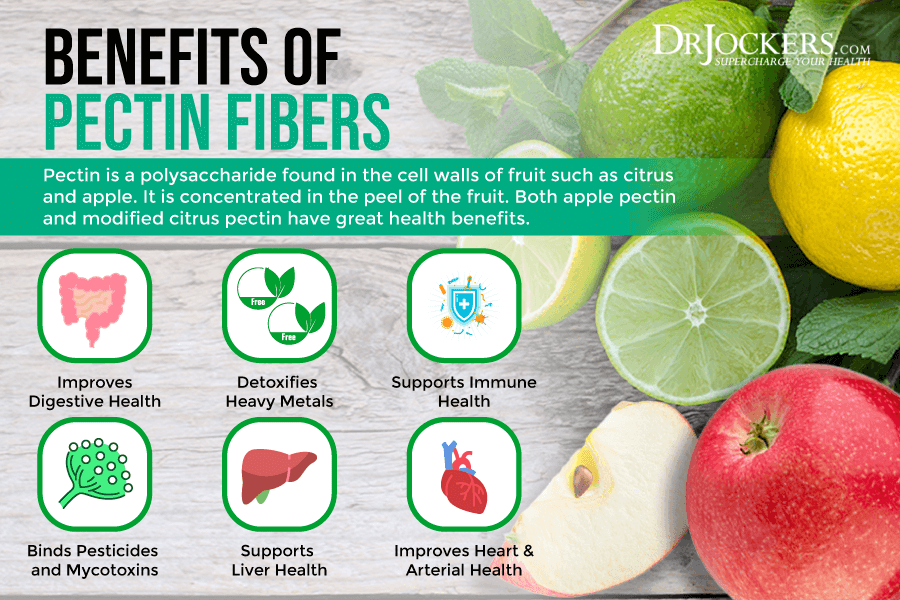
Citrus Pectin
Citrus pectin is a soluble fiber often recommended for diarrhea, digestive issues, satiety, and low cholesterol. According to a 2016 study published in Nutrients, pectin may help to improve the gut barrier function, reduce leaky gut lining, support gut microbiome balance, and reduce the risk of diet-induced obesity (41).
Introducing GI Synergy
To improve your gut lining, recover from leaky gut lining or reduce your risk of leaky gut lining, and support your gut health with the help of these herbs, I recommend GI Synergy. GI Synergy is formulated with specific amino acids, botanical extracts, and minerals to offer comprehensive support for gastrointestinal (GI) health and function. The gastrointestinal lining has unique functions and nutritional needs. It must be permeable or porous enough for nutritional absorption, yet also provide a barrier against toxins, allergens, and pathogenic microbes.
GI Synergy features L-glutamine, an amino acid that provides structural and metabolic support for intestinal cells. Zinc L-carnosine provides support for the health of the intestinal lining. N-acetyl-D-glucosamine supports a normal inflammatory response in the GI tract.
GI Synergy also contains a botanical blend of deglycyrrhizinated licorice (DGL) extract, aloe vera, marshmallow, okra extract, and cat’s claw that provides support for healthy intestinal function by coating and soothing the intestinal lining, and these ingredients promote the body’s natural gastrointestinal repair process.
Prune powder and citrus pectin support bowel regularity. Methylsulfonylmethane (MSM) supports the structure, integrity, and permeability of the GI cell walls and a healthy inflammatory response. The blend helps to improve intestinal function and regularity, support the intestinal mucosal lining, improve gut-associated immune function, support a healthy immune response, and improve the gastrointestinal tract. I recommend taking 7 capsules per day or as directed by your healthcare practitioner.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!
Final Thoughts
Your gut lining is incredibly important for your gut and overall health. A leaky gut lining may increase the risk of chronic inflammation, gut inflammation, gut microbiome imbalance, chronic symptoms, autoimmunity, and chronic health issues. Keeping your gut lining healthy is key to health. I recommend that you try the nutrients and herbs and herbal supplements shared in this article to improve a leaky gut lining and regain your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.




I really messed up and ruined my life
Help…. I have EoE
My GI dr. Insists on PPI
I break out in a rash, and it is hard on my gut
I have chronic inflammation in my esophagus,
My eosinophil count is at 100. !!!!!!
And have Schatzi ring at the bottom of it
He is mad that I stopped taking the PPI
Any other suggestions better than PPI. ??
Hi Annelie
Sorry to hear about your situation.
I was put on PPIs about 3 years ago for high stomach acid, which made me worse in the first 3 days of taking them, so I stopped.
I ended up going to a well known alternative health shop. They then gave contact details of alternative health people in my area, but told me to try aloevera juice, and fennel (tea or the vegetable). I tried these and was better in under a week.
However, I was given about 60 patches on my back a year later to check allergies for many ingredients, and my symptoms came back worse than ever, and I was finding tightness in my chest when trying to breath, and tingling sometimes, as well as severe wind, stomach cramps etc. which worried me. I went back to the hospital (no idea, told me to see my Dr), and the Dr and he wanted me to go back on Omeprazole again, as well as depression, Migraine tablets. I asked if there was an alternative and was told that these were the best for my problem, (I left, but didn’t get them). I wasn’t even asked to go back for a follow up to the Dr months later. But was told my another Dr prior to this that I had IBS, (another tablet to take).
Thankfully I still had the contact details and the qualified alternative informed me I had a bacterial imbalance, and a possible leaky gut.
I went on an extended Mediterranean diet, cut out all sugar, refined, fake food, and ate healthily with various food combinations to aid digestion, and avoided other combinations relating to bad digestion: Avoiding fat, protein with starchy, sugary food (lasagne, shepherds pie, hotdog, shop bought cakes, bread, wheat, icecream etc.
I also took ACV, digestive enzymes, pectin and HCL (Coconut oil) as well as a thin slice of lemon in warm water on a morning and natural “Live bacteria” as well as Goat milk instead or cows milk. it worked for me.
I realised that I had low stomach acid, not high. (took spearmint for low stomach acid). Ginger, peppermint when I had indigestion to help digestion and calm down my stomach issues.
When I queried low stomach acid with the Dr I was told low stomach acid doesn’t exist. Yet I have found out by my own issues and from a qualified alternative it does.
Many of our Drs are taught to treat the symptom not the root cause, and that there is no low stomach acid, only high.
My advice is see a well known health shop to see if they can help (many are well qualified). Do your own research, or get a well known, qualified and recommended health specialist, or a Dr who knows alternative cures and is well qualified.
The rash sounds like a reaction to an ingredient in the tablets, or the body trying to expel toxicity building up inside.
Good luck.
Hi Annelie.
I was told by an alternative: PPIs only treat the issues not the cause.
The cause is probably Low stomach acid.
I have just remembered a trick from the alternative that helped me.
Steam inhalation Your throat, esophagus needs moisture as well. If it gets dry it can cause issues (spasms, dryness etc). There is a valve that should close to stop gas gong back up. If there isn’t enough gas/stomach acid, the valve may not close enough, which may cause esophagus issues as the acid may rise (but from undigested food in the gut causing the issue).
In relation to your eosinophil count, this does seem very low, but unfortunately I cannot give you any answers for this only guess from my own research from personal issues. However, the gut is also related to Cortisol (stress, and the immune system).
It sound as if your immunity, white blood cells is very low.
If the gut is weakened it won’t digest nutrition: vitamins, minerals which could mean a deficiency and issues related, or internal issues relating to the gut not acting as a first line of defence so that undigested foods, inflammation, bacteria are causing the rise in esophagus issues, causing inflammation as the bodys natural defence causes inflammation so that it can try to repair the issue, but excess inflammation in this case is the issue, ie: allergic reaction or a disease, bacterial etc issue.
The Schatzi ring issue. I presume that this means that it is narrowing via inflammation.
Many things start in the gut. There is a connection between the gut, brain, stress/Cortisol and the Vagus Nerve). If the PPI or another medication is hard on your gut, it will weaken it and not cure the underlining issue.
When I was having severe issues, I had a weakened gut, low stomach acid and a Vagus nerve that was not functioning correctly, as the Vagus Nerve Connects to the gut, Brain.
It could also be from allergy related to something else: medicine ingredient, food allergy.
For other ideas, please read my other post. However, I was taught to breath properly for calming and destressing myself which does help. (5 Finger Breathing Techneque, and Pranayama:Yoga Technique).
I am no expert, but hope this helps. See if you can get help from a qualified person who will get to the route, source of the issue.
Hello Annelie, yes I go through some much better options in this article: https://drjockers.com/heartburn-medications/
Excellent article. thank you.
I have been able to help clients with Rheumatoid Arthritis into remission and off injections and methotrexate using high doses of MSM plus Quercetin.
Would you recommend GABA or Ashwaganda for stress relief and if so, best time to take and with or without food. Thanks!
Great to hear that! Yes, GABA and Ashwagandha are both great for helping improve the stress response and reduce anxiety. Both are best taken away from meals (although they can still work with meals) and can be taken at anytime during the day to help reduce tension, racing mind, anxiety, fear, etc. and create a more balanced and calm mind.
My ENT doctor advised that I take PPI’s for GERD with a hiatal hernia. However, what I found works for me is 1 tablespoon of apple cider vinegar “with the mother” daily and elevation of the head of my bed.
Can you open the capsule for the gi, I can’t swallow pills?
Will this heal H pylori too?
Also how to you heal poor vagal tone vagus nerve?