 How to Eat to Reduce Pain and Inflammation
How to Eat to Reduce Pain and Inflammation
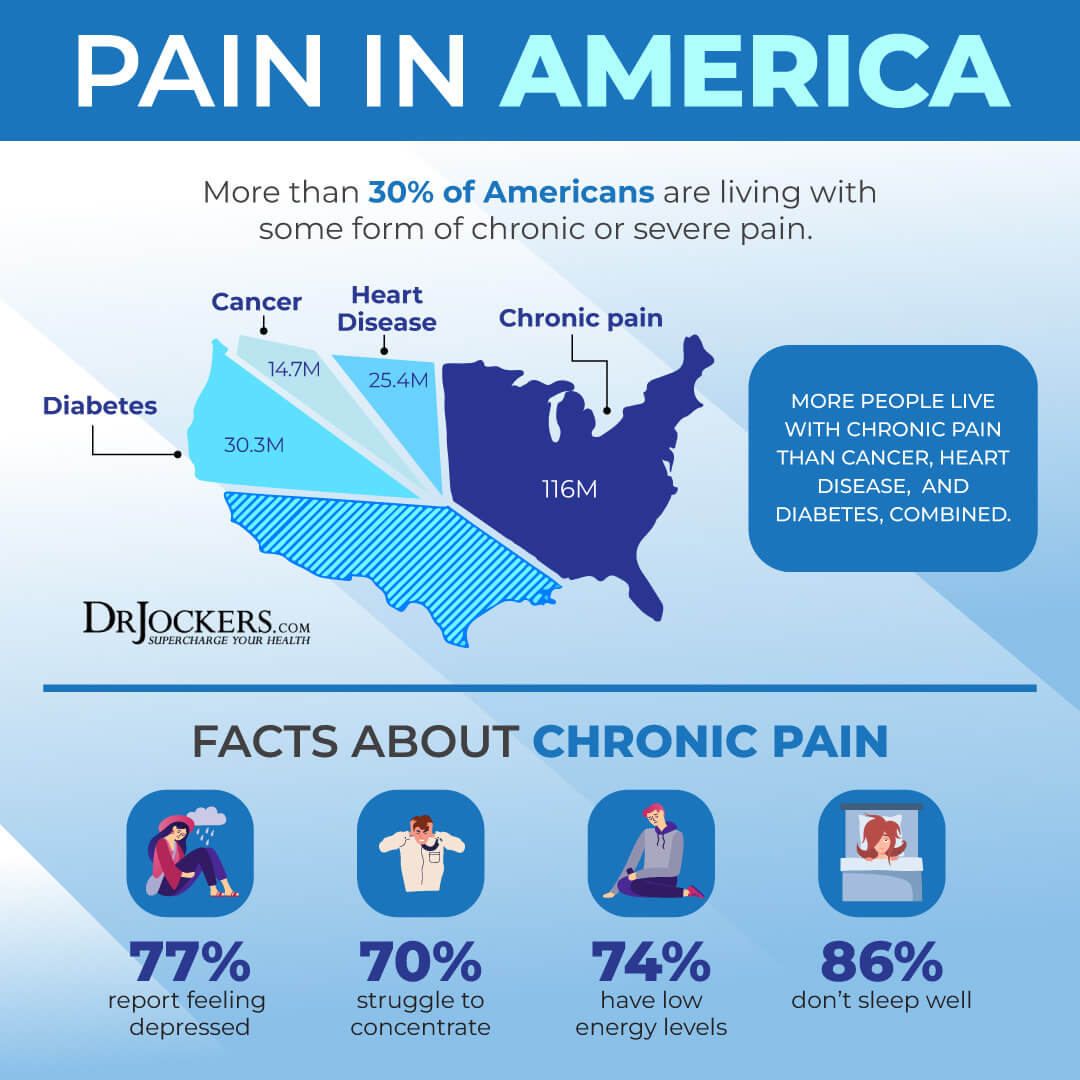
Chronic pain is a common health issue in today’s world. Many people deal with chronic pain related to specific diseases or injuries. Others experience chronic pain without an apparent reason or known disease.
Chronic pain can affect your daily life, work, learning, and social life, and it may even lead to disabilities. Chronic pain is often connected to underlying inflammation. Fortunately, with the right diet and supplementation, you can reduce pain and inflammation.
In this article, you will learn about the role of nutrition in pain. I will share my top meal planning tips to reduce pain. You will learn about the best foods to reduce pain. Finally, I will share the best supplements to reduce tips, including my favorite formulas.
The Role of Nutrition in Pain
According to the systematic analysis of the Global Burden of Disease Study published in The Lancet, consuming a poor diet may increase the risk of various chronic diseases and related mortality (1). The study looked at the health effects of various dietary factors in 195 countries between 1990 and 2017.
Researchers found that poor dietary factors, including high sodium intake, low intake of fruits, low in vegetables, low in omega-3 fatty acids, and low in nuts and seeds, may increase the risk of disease and mortality.
According to research, each of these factors may account for over 2 percent of global deaths. According to the researchers, one in every five deaths globally could be prevented if we improved our diets. Current trends our mainly focusing on our sugar and fat intake. However, it seems that we need to focus on our overall diet and overall nutrient intake instead.
Chronic pain is a common modern-day health issue, which may or may not be associated with specific chronic diseases. Research has shown that chronic pain is often linked to being overweight, following a poor diet, and risk of multi-morbidities.
According to 2017 research published in Healthcare (Basel), in the past, treatment programs for chronic pain included medical, physical, and psychosocial options, however, it seems that nutrition is just as important, and optimizing dietary behaviors may help to improve non-cancer pain (2).
A 2015 study published in Nutrients has also found that improving one’s participant’s nutrient intake helped to improve their health and reduce morbidity and mortality (3). They particularly found that improving vitamin A, vitamin C, beta-carotene, calcium, potassium, magnesium, other minerals, and fiber levels is important.
Diet affects all parts of the body. Improving your diet may help to improve your immune health, endocrine system health, and nervous system health. These areas may all impact your pain experience. Excess weight may also put a load on your joints, causing joint and muscle pains. Weight loss through a healthier diet thus may improve these pains.
Following a nutrient-dense diet and achieving or maintaining a healthy weight may also reduce the risk, improve the symptoms, or slow the progression of various diseases that may increase the risk or cooccur with chronic pain, including diabetes, cardiovascular disease, anxiety, or depression. As the 2017 research published in Healthcare (Basel) suggests, nutritional interventions may improve the self-reported severity of pain (2).
In this article, you will learn about dietary strategies that may help to improve pain and inflammation. However, it’s important to consider other factors. People with chronic pain may be dealing with isolation, mental health co-morbidities, limited mobility or strength, or lack of sleep that may also need to be addressed.
For example, if someone’s limited mobility affects their ability to shop, cook, or prepare meals, we need to consider help or ordering healthier meal options until their health improves. Therapy or joining support groups may help with mental health limitations and isolation. If a lack of sleep or an irregular sleep schedule is an issue causing irregular eating habits, improving sleep should be a priority as well (I recommend this article on sleep).
Now that you understand the general role of nutrition in pain, let’s look at some specific dietary factors that may be underlying issues behind chronic pain and inflammation.
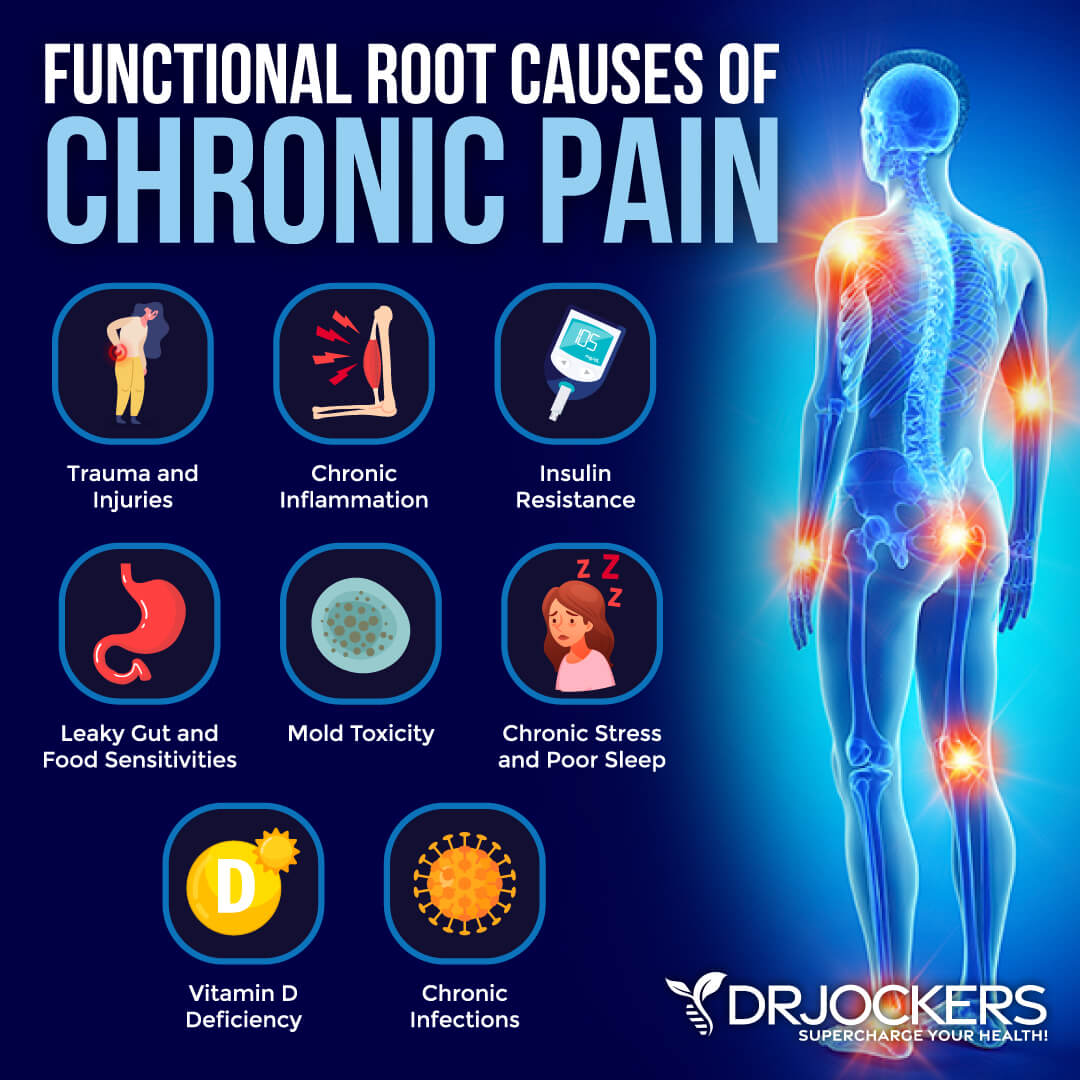
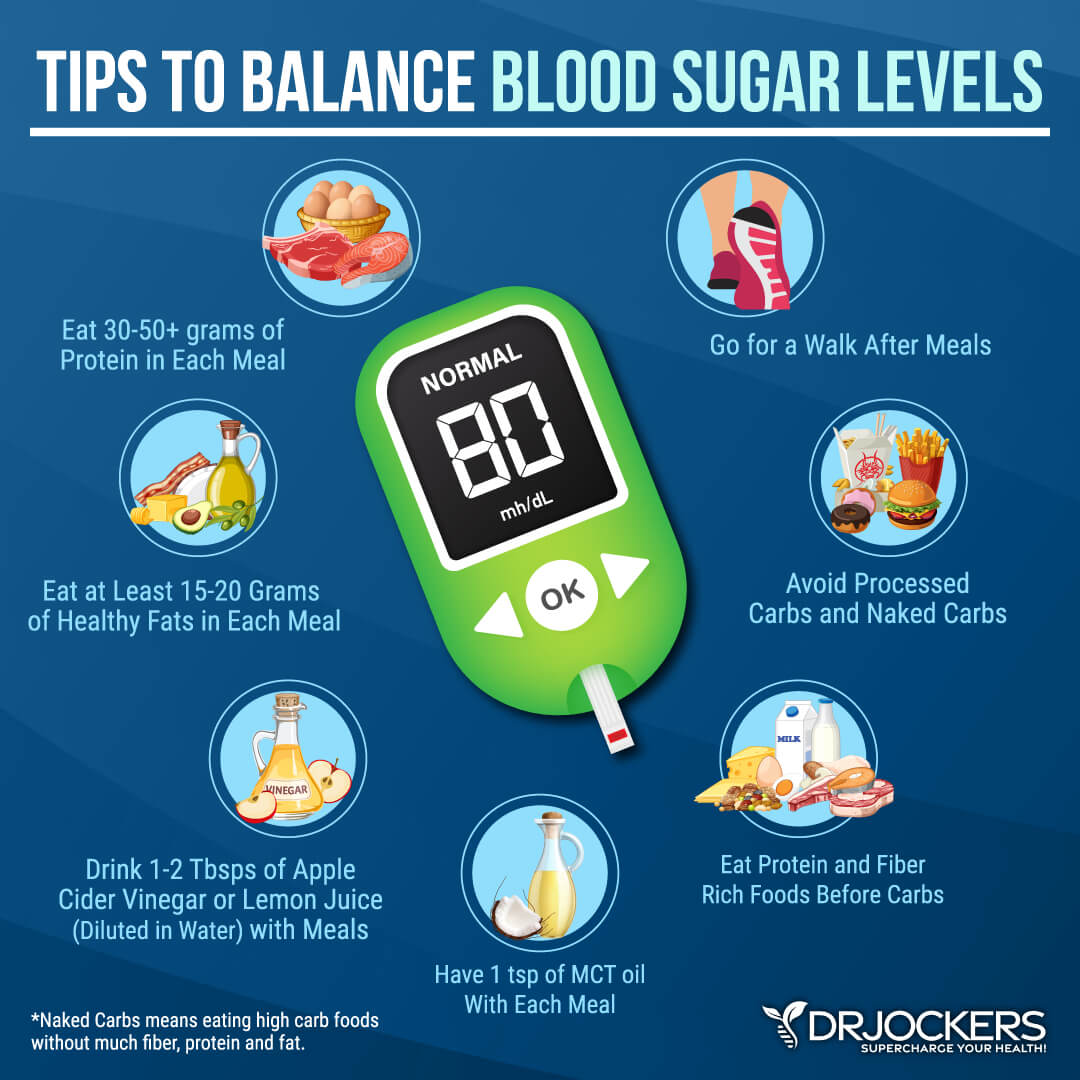
Poor Blood Sugar & Insulin Resistance
Blood sugar imbalances and insulin resistance may be underlying issues behind chronic pain. According to a 2016 study published in the Journal of Biomedical Sciences, the development of insulin resistance and increased inflammatory responses in your body may be interconnected (4).
A 2005 study published in the Journal of Clinical Investigation has also found a link between inflammation, stress, and diabetes (5). Of course, chronic inflammation and increased inflammatory responses are often connected to chronic disease and chronic pain.
The Standard American Diet (SAD diet) is high in advanced glycation end products (AGEs) are harmful compounds. AGEs may develop when fat or protein combines with sugar in your bloodstream through glycation. They may also develop in foods through frying, grilling, or toasting at high temperatures.
According to a 2015 study published in the Journal of Clinical Endocrine Metabolism, the SAD diet may contribute to the increased risk of obesity and metabolic diseases, which are also linked to higher blood sugar levels, insulin resistance, inflammation, chronic diseases, and related pain (6).
According to a 2021 study published in Pain Physician, insulin resistance may increase central pain in those with fibromyalgia, which is a chronic condition characterized by chronic musculoskeletal pain (7).
A 2016 study published in The Journal of Pain has also found a link correlation between insulin resistance and chronic pain (8). Researchers found that nerve injury may contribute to poor glucose metabolism and the downregulated expression of insulin receptors, further accelerating neuropathy.

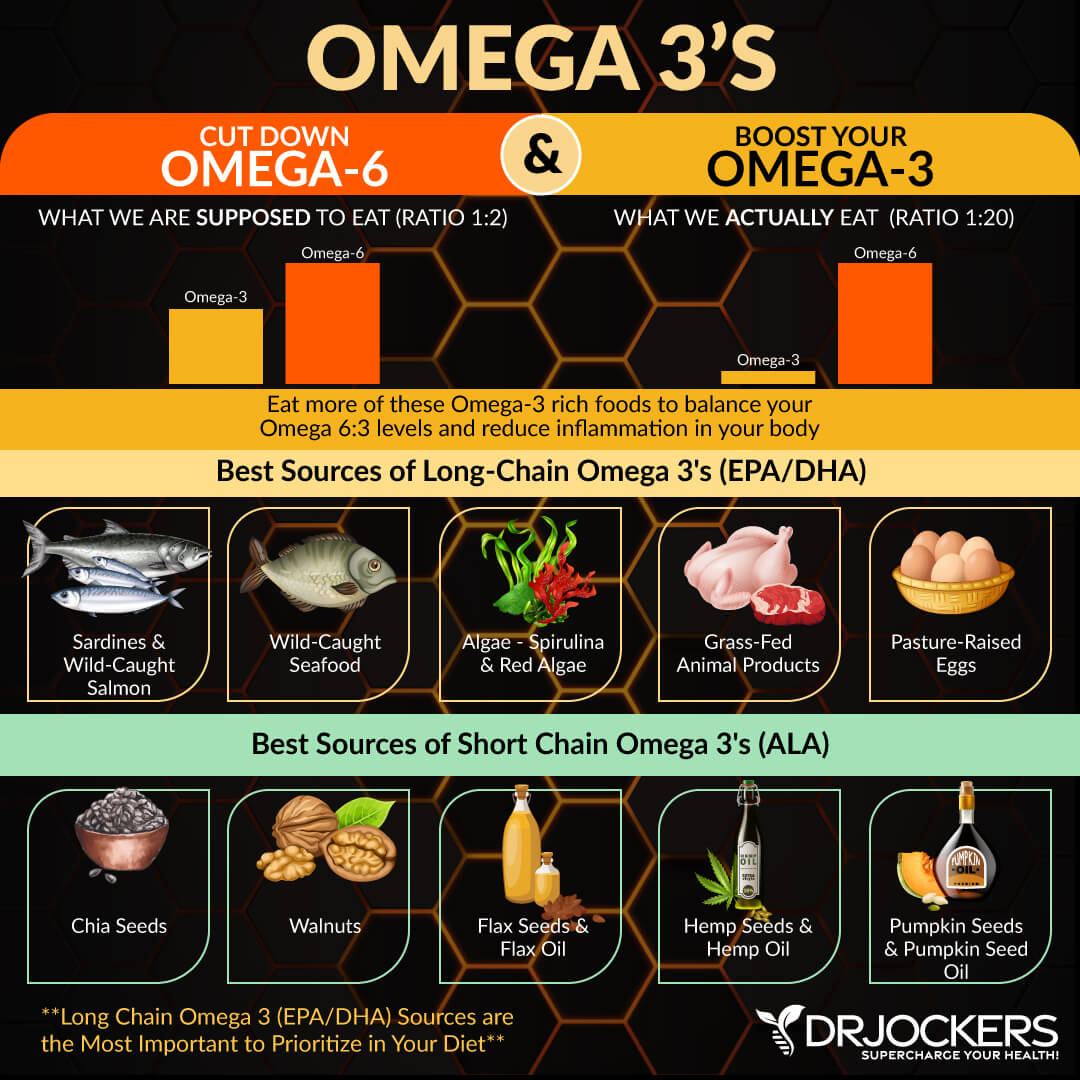
Omega 6:3 Ratio and Pain
Omega-3 fatty acids, found in fish, seafood, algae, hemp seeds, chia seeds, and flax seeds, are healthy fats that are known to have anti-inflammatory benefits. According to the systematic analysis of the Global Burden of Disease Study published in The Lancet, more omega-3 fatty acids in the diet may reduce health risks and mortality (1). According to a 2016 study published in Nutrients, omega-3 fatty acids can help to improve inflammation in older individuals (9).
However, it’s not just the amount of omega-3s that matters, but omega-6 fatty acids, too. The ratio of omega 6:3 fatty acids may be a critical factor we need to look at when it comes to pain.
A 2018 study published in the Clinical Journal of Pain has found that omega-6 and omega-3 ratios may be linked to pain and functioning levels in knee pain (10). According to a 2023 study published in the Journal of Pain, a lower ratio of omega-6 to omega−3s in red blood cells may be linked to lower levels of chronic pain (11).
Prooxidative Compounds in Diet
Prooxidative compounds in the diet, including trans fats, chemicals, pesticides, herbicides, heavy metals, and other toxins, may also increase the risk and levels of pain and inflammation. These compounds are known to increase oxidative stress, free radical damage, and chronic inflammation, which may increase the risk of pain and disease.
According to 2021 research published in Frontiers in Immunology, trans fats may increase intestinal inflammation and reduce glucose tolerance, causing related pain and symptoms (12). A 2020 systematic review and meta-analysis published in Toxics has found that pesticides may increase the risk of rheumatoid arthritis, an autoimmune condition characterized by chronic pain (13).
A 2023 study published in Bioengineered has found that herbicides may also have toxic, cell disruptive, neurological, and carcinogenic effects, thus may be contributing to inflammation, pain, and disease (14). According to a 2014 study published in Interdisciplinary Toxicology, heavy metals, which may also be hidden in some foods, may increase oxidative stress, which can contribute to pain and disease (15).

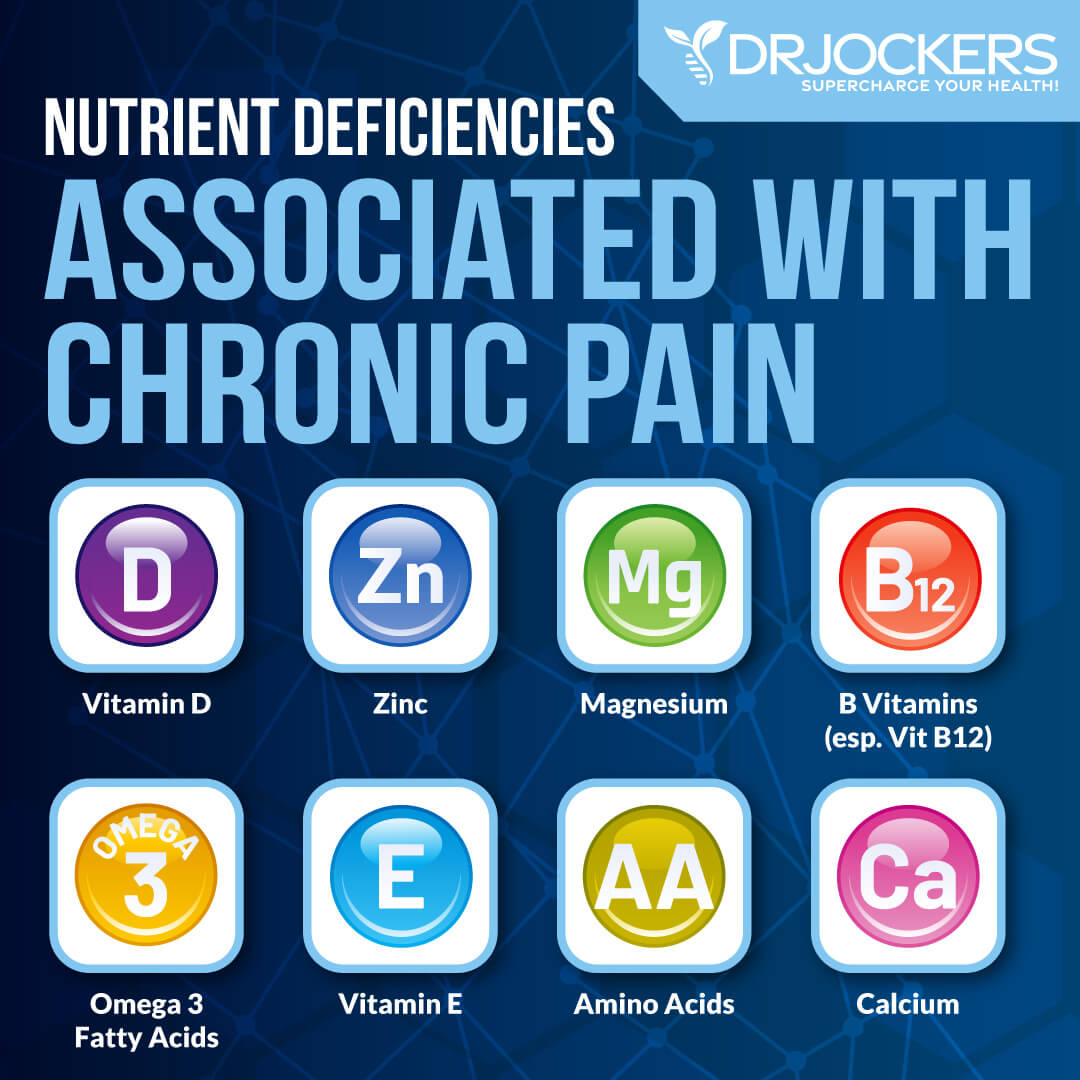
Nutritional Deficiencies and Pain
Nutritional deficiencies may also increase the risk of inflammation, pain, and disease. Deficiencies in vitamin D, vitamin B12, magnesium, calcium, omega 3 fatty acids, vitamin E, zinc, and amino acids are among common culprits behind pain. A 2023 animal study published in Biomedical Sciences has found that a deficiency in zinc may increase the sensation of pain (16).
2020 research published in Nutrients has found that improving magnesium levels may have beneficial effects on various pain issues, including diabetic neuropathy, postherpetic neuralgia, chemotherapy-related neurologia, migraines, headaches, and fibromyalgia (17).
A 2019 review published in Pain Physician has found that vitamin B12 may affect pain signaling and help the treatment of pain issues (18). A 2020 review published in Frontiers in Immunology has found that vitamin D may play a role in pain signaling and may help to reduce pain (19).
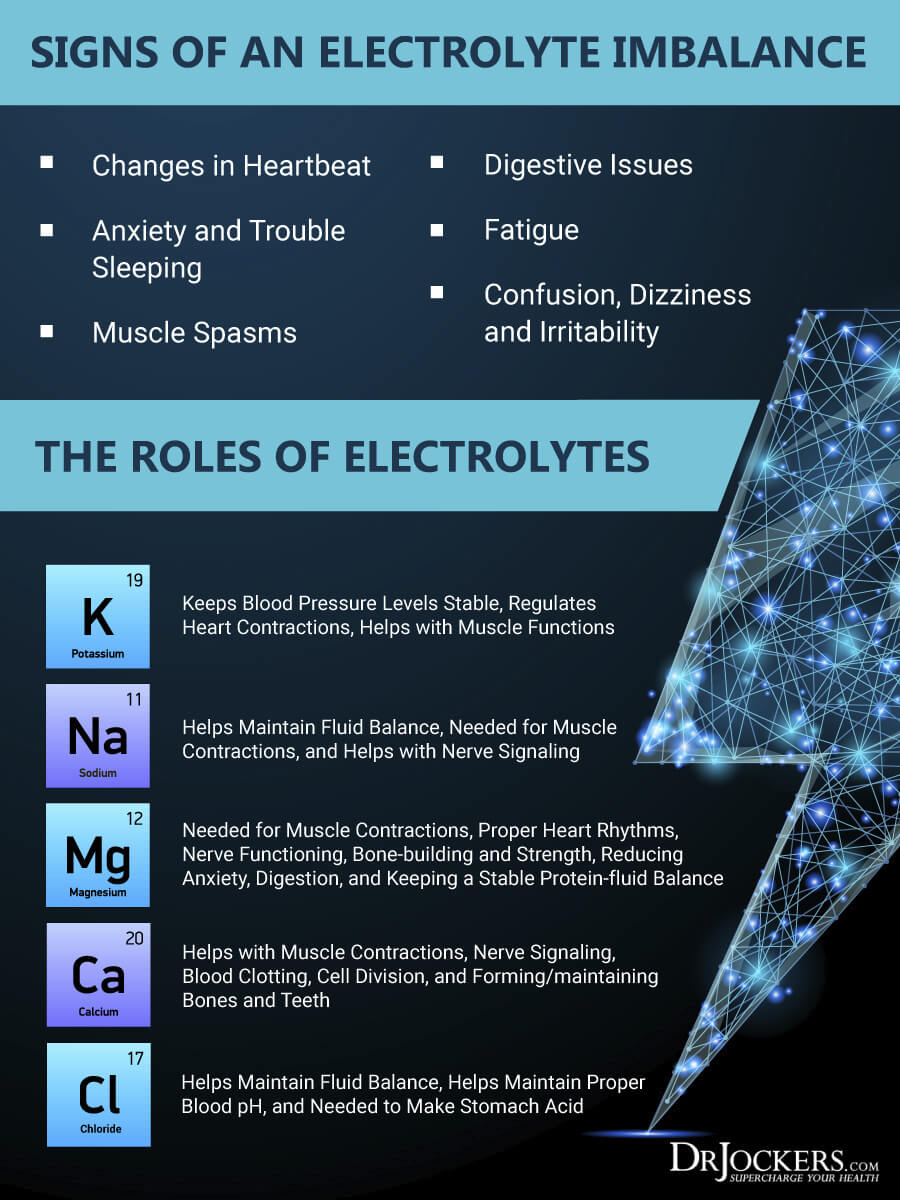
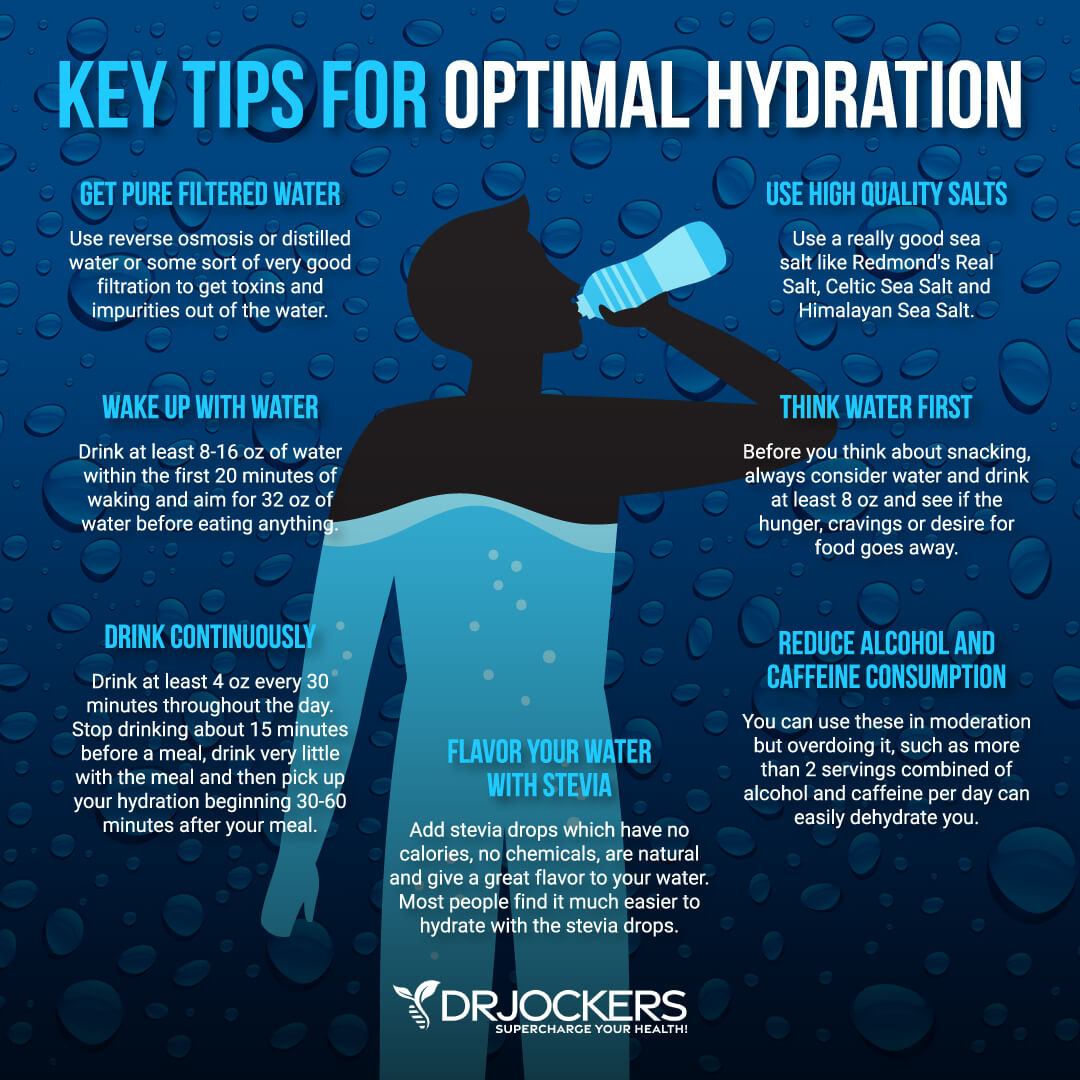
Dehydration and Pain
Dehydration and electrolyte loss may also play a role in pain. According to a 2016 study published in Psychophysiology, dehydration may affect pain sensitivity and pain threshold (20). Dehydration may also contribute to the loss of electrolytes, including sodium, potassium, chloride, magnesium, calcium, phosphate, and bicarbonates.
Electrolyte loss may also increase pain. According to a 2005 study published in the Journal of Athletic Training, improving hydration and electrolyte levels may improve exercise-related muscle cramps (21).
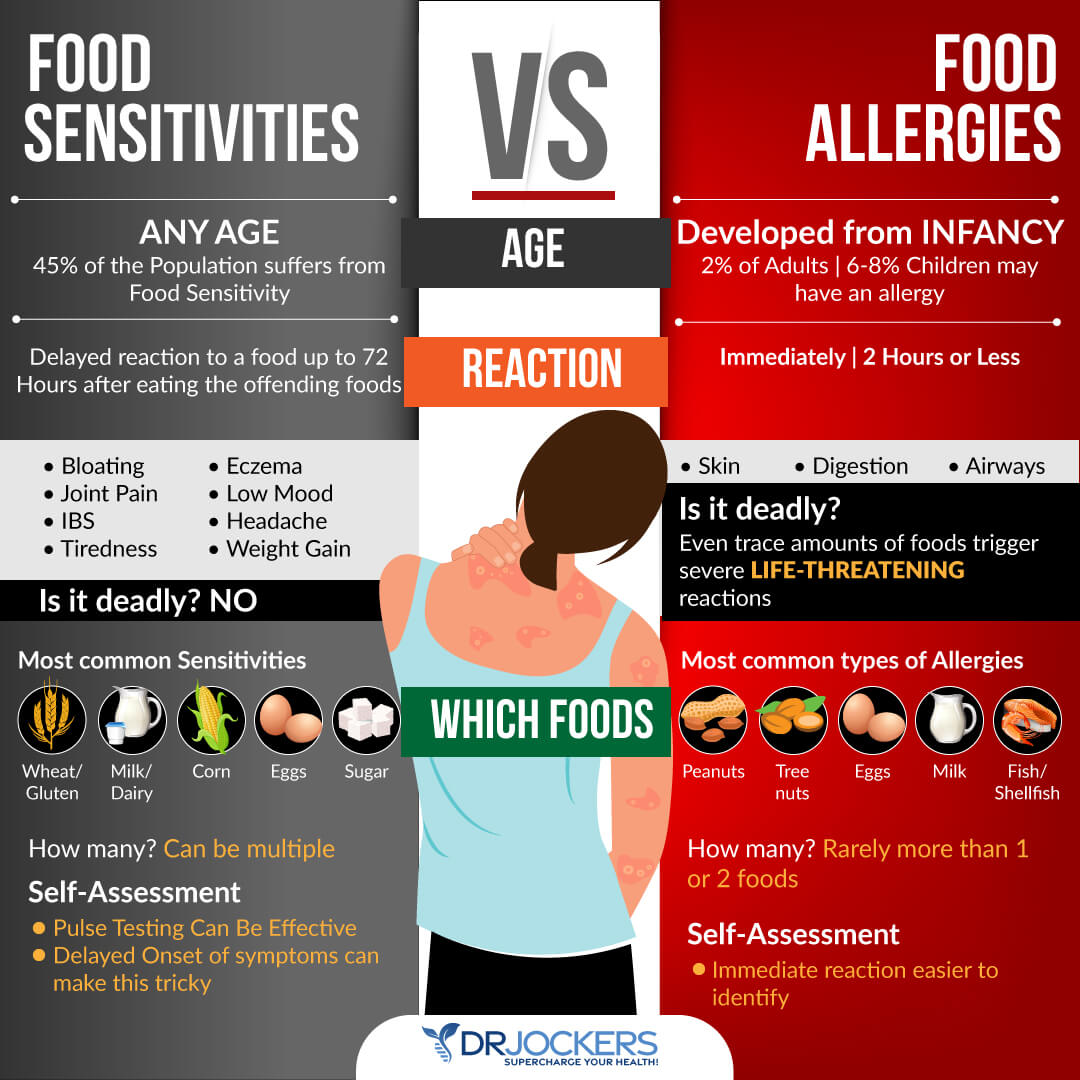
Food Sensitivities and Intolerances
Food sensitivities and intolerances may also contribute to pain. These issues may differ from person to person. Many people experience gluten sensitivities. According to 2022 research published in the American Journal of Lifestyle Medicine, gluten may contribute to inflammation (22).
Dairy-related sensitivities are also an issue. A 2019 review published in Advanced Nutrition has also found that dairy may also increase inflammation (23). Others have issues with various foods or food groups, for example, nightshades may trigger pain in certain individuals.
A 2020 study published in Contemporary Clinical Trials Communications has found that avoiding nightshades should be part of an anti-inflammatory diet for rheumatoid arthritis (24). In others, high-histamine foods may contribute to inflammation and pain.
A 2020 study published in the British Journal of Pharmacology has found that histamine may increase neuropathic pain (25). Since food sensitivities depend on the individual, it’s important to look at your specific food sensitivities and intolerances through blood testing, elimination diet, and other methods.
Certain Antinutrients
Certain antinutrients, including oxalates and lectins, may also increase pain. A 1997 study published in the American Journal of Obstetrics and Gynecology found that high oxalate levels may increase vulvar pain (26). According to 2013 research published in Currents in Rheumatology Reports, oxalates may play a role in arthritis (27).
2017 research published in the Journal of Immunology has found that lectins may activate inflammasome and may increase inflammation and tissue damage (28). Whether one has issues with these foods may depend on the unique metabolism of the individual. Thus, individual testing is important to see if you have issues with antinutrients and whether they are contributing to your pain issues.

Meal Planning to Reduce Pain:
Now that you understand what may contribute to or increase chronic pain and inflammation, I want to offer some actionable nutritional strategies for meal planning to improve your diet and reduce pain.
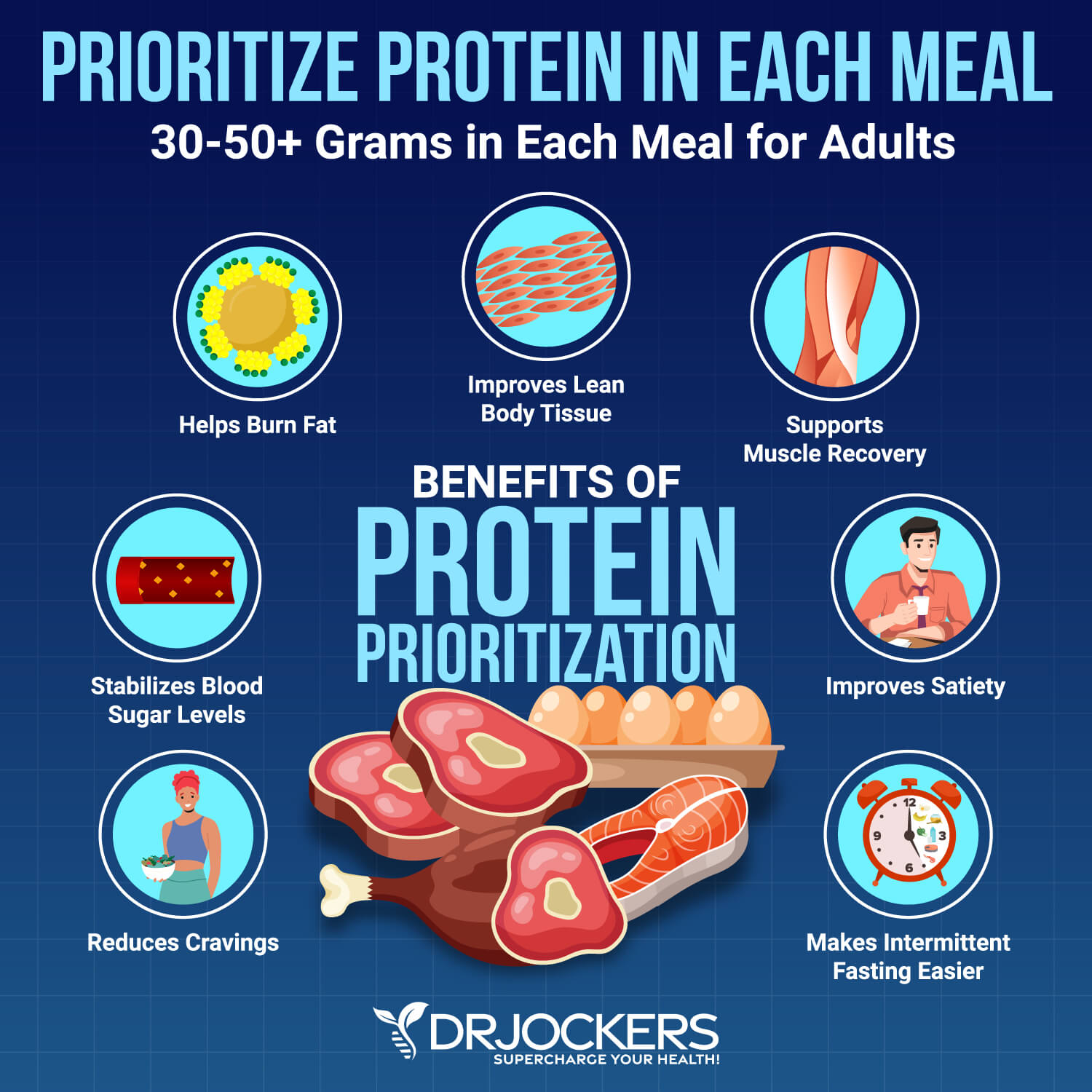
Prioritize Protein
Eating enough protein is incredibly important for building muscle, allowing the bloodstream to carry oxygen throughout your body, blood sugar balance, fat burning, supporting energy, and more. A 2022 study published in Nutrition Journal has found that a higher protein diet may help to reduce chronic low back pain (29).
I recommend 30 to 60 grams of protein per meal. When you are setting up your meal, really be considerate about the amount of protein and healthy fats on your plate. For most people, 30 to 60 grams of protein per meal is the right amount. You only need more if you are really trying to build muscle mass and doing very intense strength and muscle-building training.
Healthy sources of protein include grass-fed beef, pasture-raised poultry, pasture-raised eggs, wild-caught fish and seafood, and wild game. Nuts and seeds, and if you can tolerate legumes, can also add some extra protein.
If you do well on dairy, you may use that as a protein source, too. However, I recommend staying away from conventional dairy and choosing grass-fed raw milk, grass-fed pasteurized milk, goat milk, sheep milk, or camel milk instead, as you tolerate it.
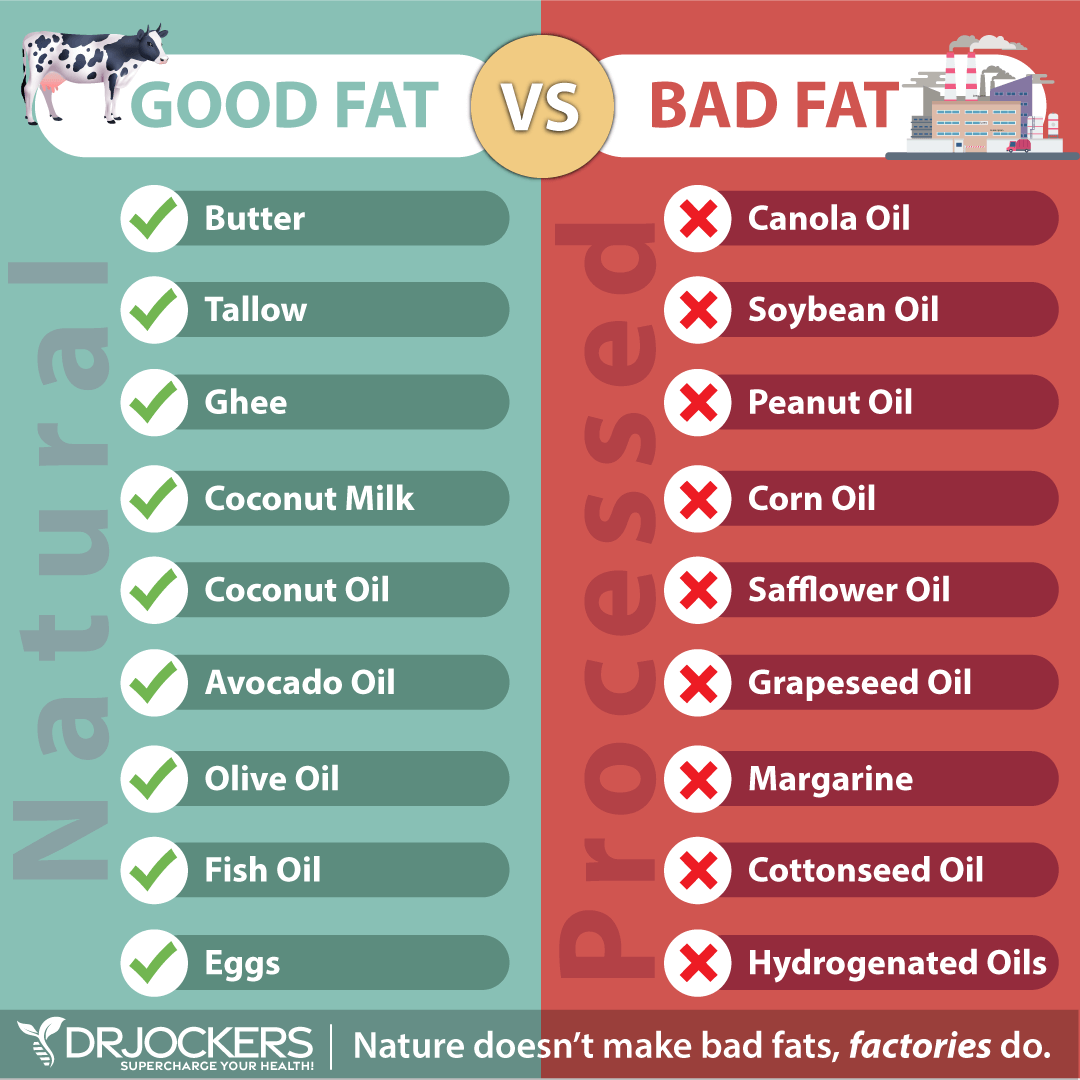
Include Healthy Fats
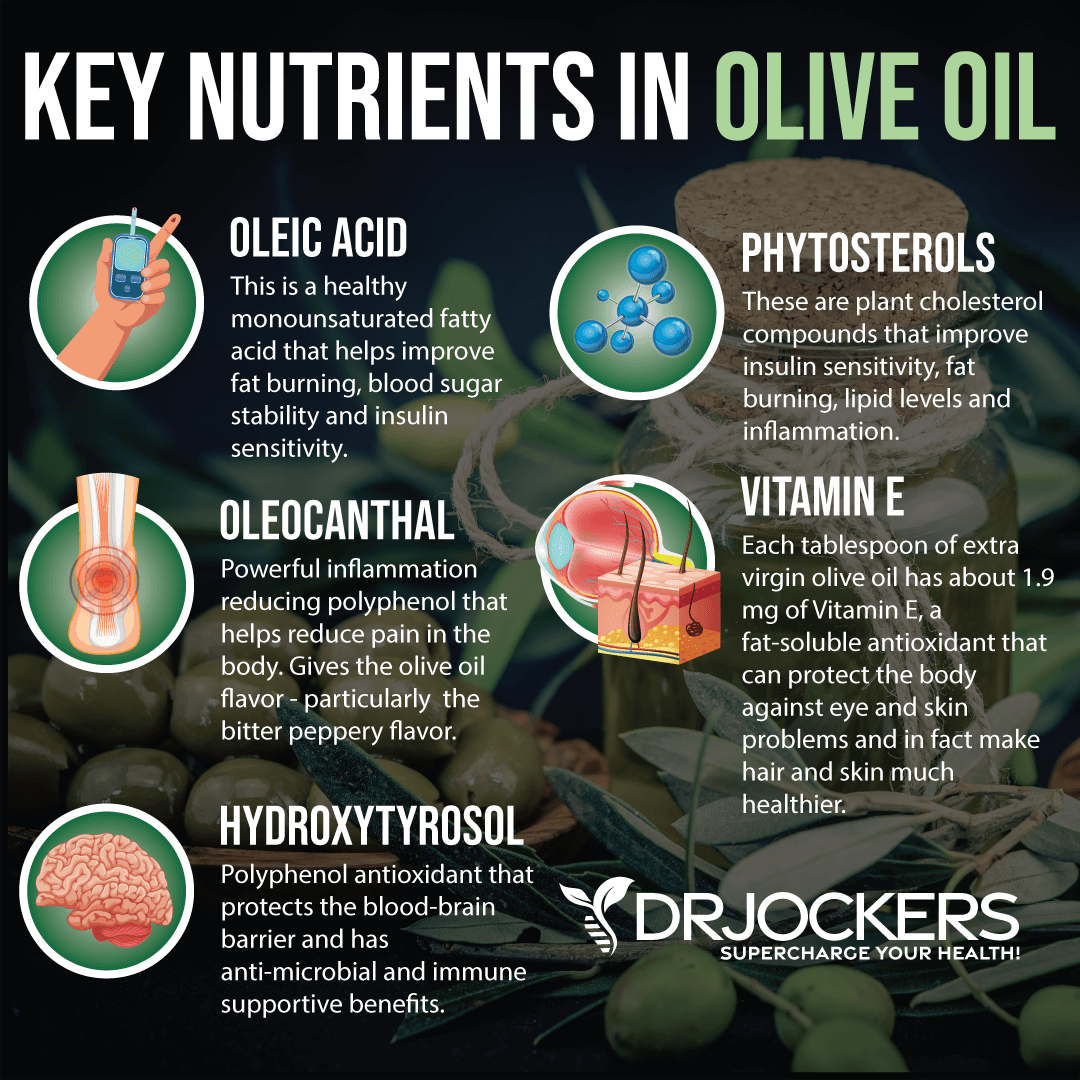
Paying attention to your fat intake is critical for your health. It may also help to reduce pain. For example, according to a 2024 study published in Nutrition Research, daily olive oil intake may help to reduce pain related to trigeminal neuralgia (30).
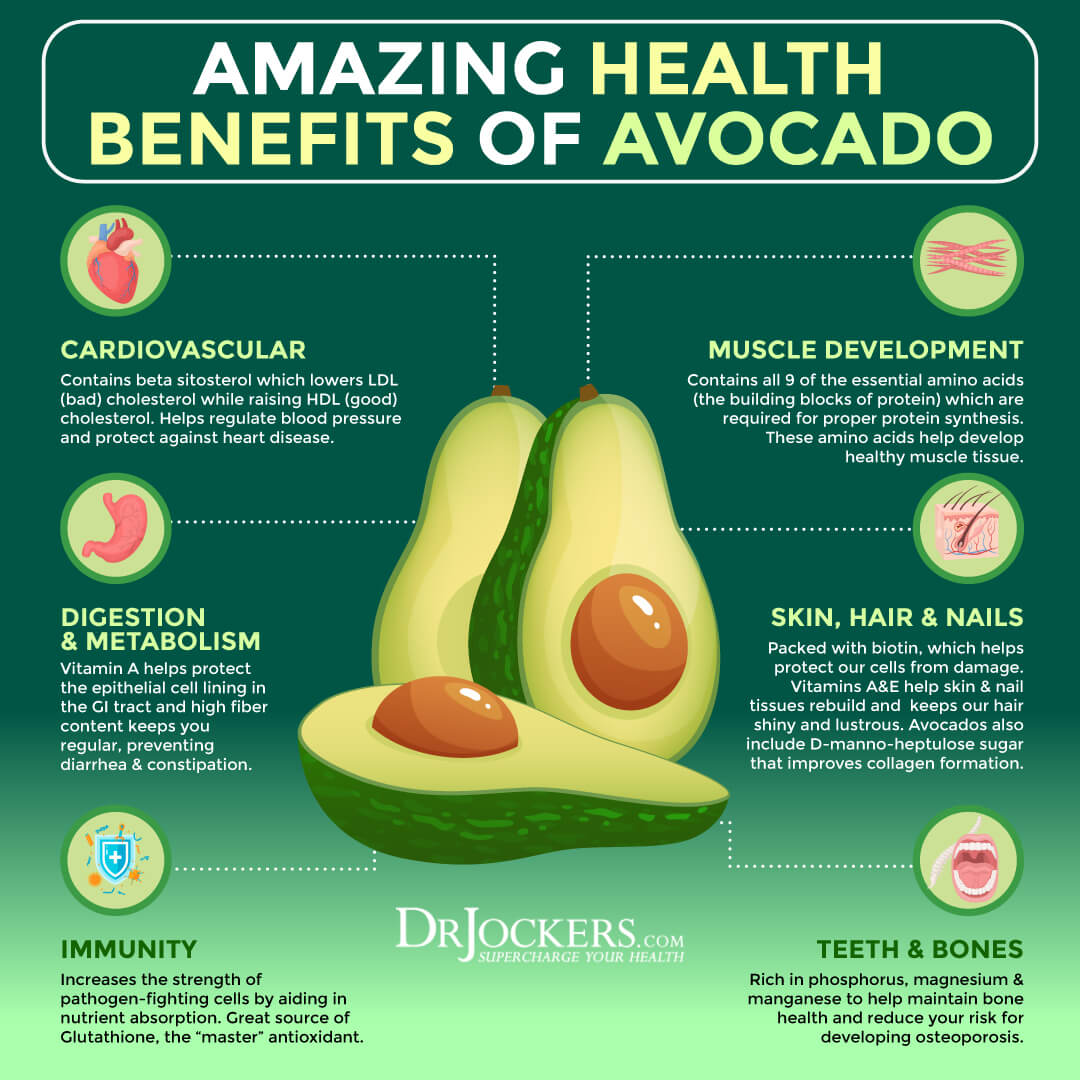
According to 2015 research published in Cartilage, avocado unsaponifiables may help to reduce osteoarthritis pain (31). According 2018 study published in the Clinical Journal of Pain, enough omega-3 fatty acids and omega-6 and omega-3 ratios may be linked to pain and functioning levels in knee pain (10).
How much meal you can take in a meal depends on you. I can take 60 grams of fats in a meal; others may do poorly even with 20 grams in a meal. People with poor bile flow or gallbladder issues may not do well with too much fat in a meal. Combining fats with protein in a meal may help to stabilize your blood sugar, reduce inflammation, and improve pain.
Avoid unhealthy fats, such as refined oils, fatty fried foods, and other sources of trans fats. Choose healthy fats, including avocados, avocado oil, coconut oil, coconut milk, MCT oil, olives, extra-virgin olive oil, grass-fed butter, ghee, and pasture-raised eggs. Fatty fish are also good sources of healthy fats and omega-3 fatty acids.
Eat Colorful Fruits and Vegetables that Your Body Digests Well
Of course, we cannot forget about colorful fruits and vegetables. For your meals, along for 30 to 60 grams of clean protein and plenty of healthy fats, add some greens, vegetables, sprouts, and fruits.
According to 2021 study published in the Journal of Clinical Medicine, eating lots of veggies and fruits may help to decrease non-cancer chronic pain (32). Fruits and veggies are full of fiber for healthy digestion and antioxidants, vitamins, and minerals to reduce inflammation and pain and improve energy.
Think about the rainbow, as different colors may indicate different nutrients to help reduce nutrient deficiencies and related pain. Great options for greens include kale, Swiss chard, collard greens, romaine lettuce, bok choi, and cabbage.
Some nutrient-rich veggies include cucumbers, celery, bell peppers, broccoli, cauliflowers, carrots, beets, snow peas, and sugar snap peas. If you have an issue with cruciferous vegetables, avoid those. You may also add some herbs, including mint, oregano, rosemary, thyme, dill, and basil. Some low-glycemic index fruits include berries, green apples, citrus, cherries, and plums.

Eat 2-3 Meals a Day
When it comes to meals, I recommend eating 2 to 3 meals a day. This should be enough for an average adult. Most people are good with 2 meals only. This means 2 to 3 meals and no snacking. Snacking may increase blood sugar and insulin.
If you eat fewer meals, you become a better fat burner, which may help to reduce oxidative stress. Eating a few meals and spacing out your meals may help to balance your blood sugar and reduce inflammation. If you are a high-level athlete, you may need more meals, and certain health issues may also indicate more, but for most 2 to 3 meals is the target.
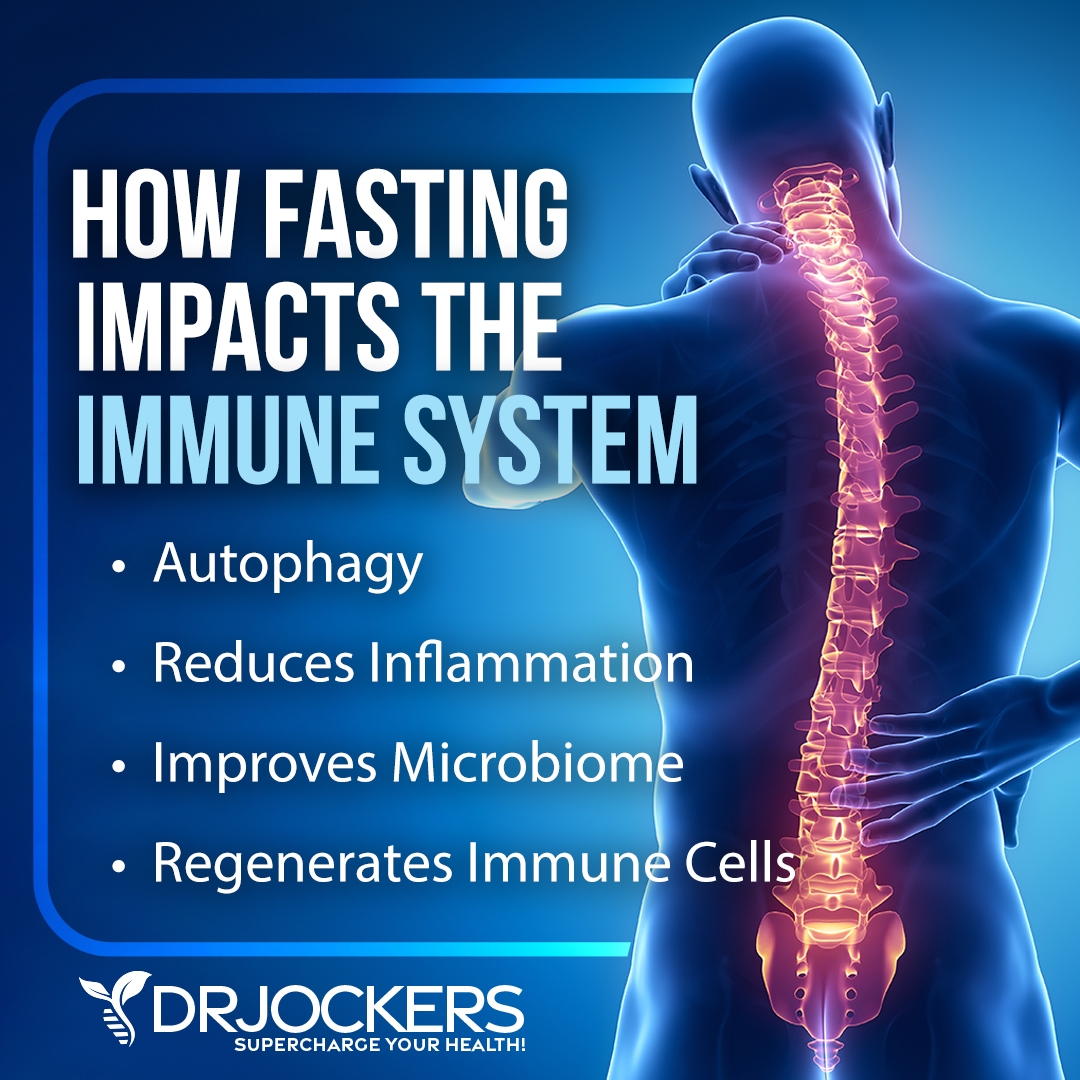
Intermittent Fasting
I recommend spacing out these 2 to 3 meals to fit into intermittent fasting principles. Intermittent fasting is a way of eating when you are cycling between periods of fasting or feasting.
Intermittent fasting is a fantastic way to reduce inflammation, improve insulin resistance, support cellular autophagy, and reduce your risk of chronic symptoms and health issues. According to 2022 research published in Nutrients, intermittent fasting may help to support the treatment of chronic pain (33).
If you are new to this strategy, begin with 12 hours of fasting, including your overnight sleep. For example, if you eat dinner at 6 pm, stop eating after 12 hours, and you will be ready to eat again at 6 am the next day. Increase your fasting period over time. You will notice that delaying breakfast until 7 am, 8 am, or even 10 am will come naturally to you over time. Most people feel the best with 16 hours of fasting a day. To learn more about intermittent fasting, I recommend reading this article.
Good Hydration
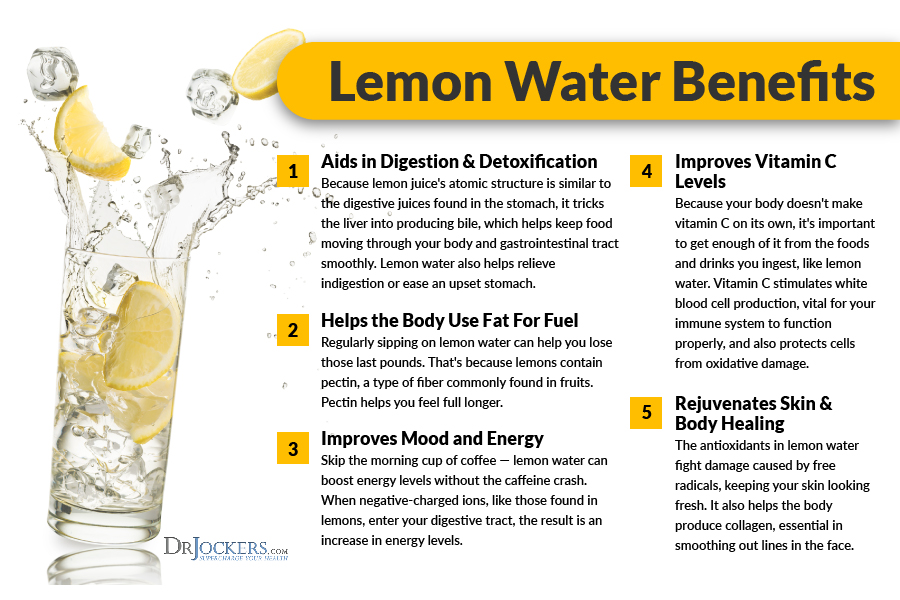
As you learned earlier, proper hydration and normal electrolyte levels are critical for your health. Drink lots of clean, purified water. Start your day with 16 to 32 oz of water. You may add some apple cider vinegar or lemon juice to kick-start your digestion.
Drink about one glass every hour. You may add lemon juice, berries, mint, or other herbs for taste. You may support your hydration with herbal tea, green juices, green smoothies, and hydrating vegetables and fruits.
Buying Organic and Local, if Possible
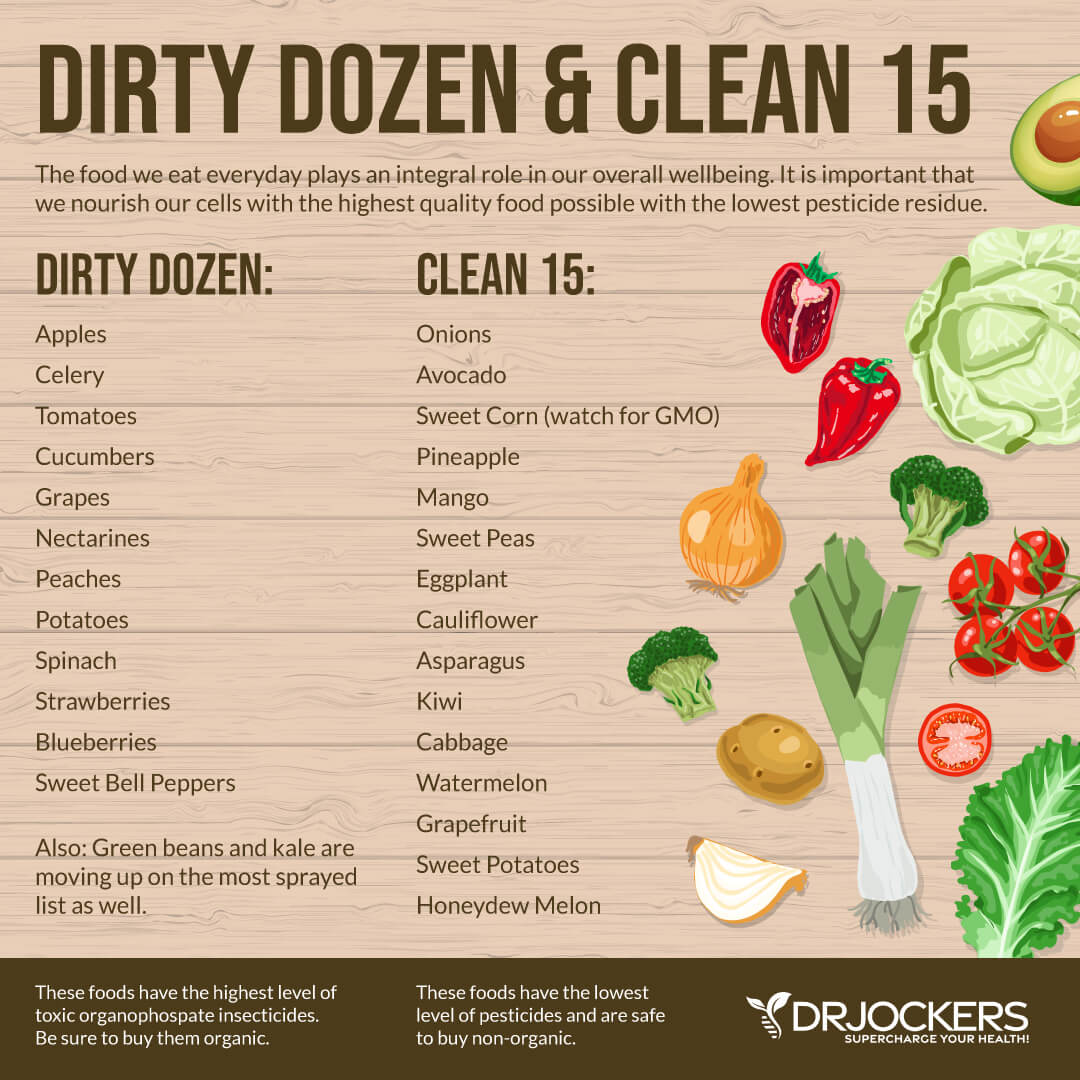
Since pesticides, herbicides, added hormones, and other toxins may increase inflammation and pain, buying organic is critical. Ideally, you want to buy organic at all times. If this is not available or affordable, pay attention to the Dirty Dozen & Clean 15.
Always shop organic from the foods on the Dirty Dozen list. Clean 15 foods may be okay non-organic, but always wash and peel them well. Shop locally as much as possible. Local farmer’s markets are great options. You may also try growing your own food using organic gardening principles.
Best Foods to Reduce Pain
Now that you have a general idea of great dietary principles for pain and inflammation, I want to share some of my favorite foods to reduce pain.
Wild Caught Salmon and Seafood
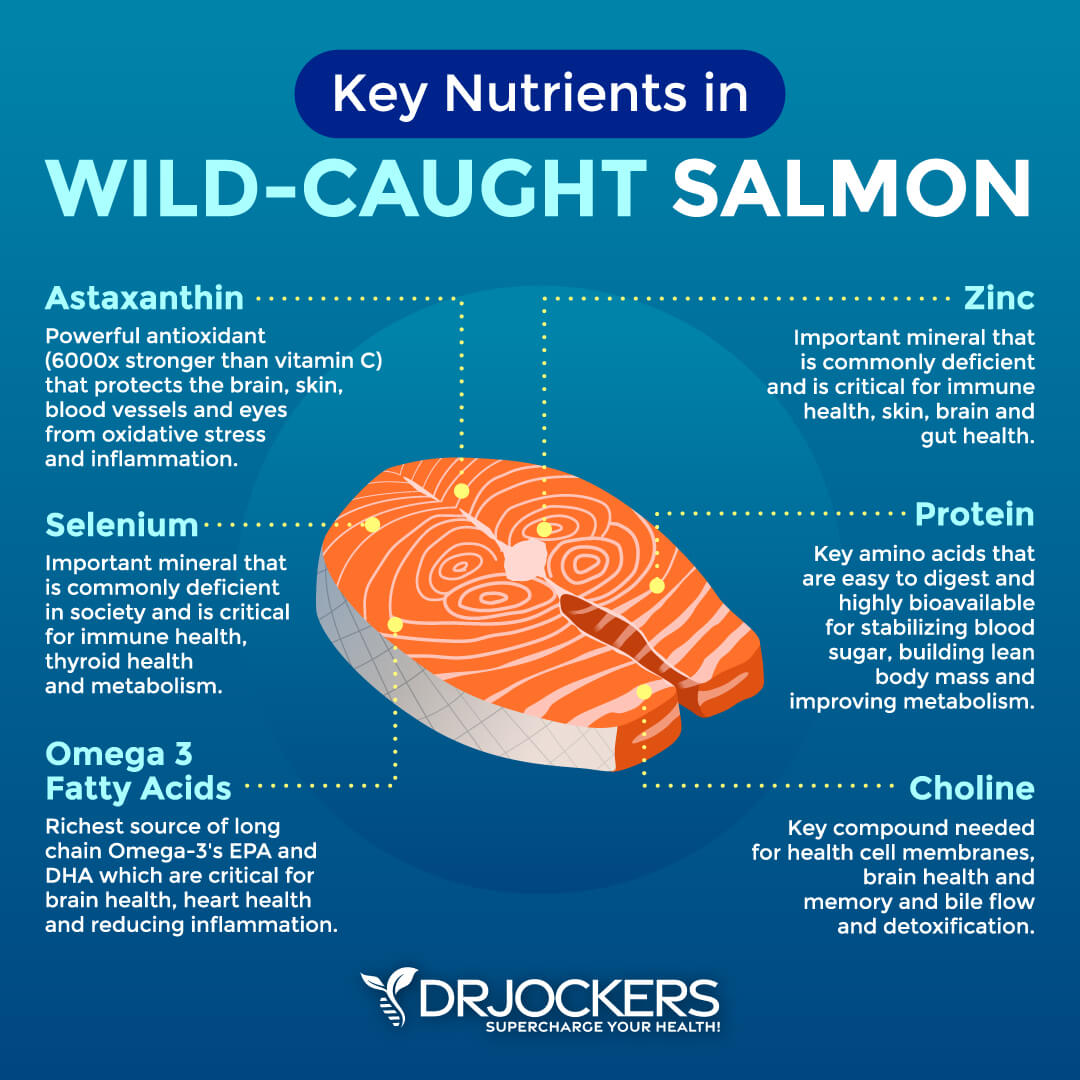
Wild-caught salmon and seafood are a great source of protein, healthy fats, omega-3 fatty acids, zinc, and other nutrients.
According to a 2022 study published in Clinical Nutrition, due to omega-3 content, eating fish may help to reduce pain (34). Salmon, cods, sardines, lake trout, tuna, herring, and mackerel are some great options.
Grass-Fed Red Meat
Grass-fed red meat, including beef, bison, and lamb. Make sure to get grass-fed, as conventionally raised animal products are full of pesticides, herbicides, and hormones.
Low-carbohydrate, ketogenic diets generally recommend eating grass-fed animal products and clean protein. According to a 2022 clinical trial published in Pain Medicine, a ketogenic diet may help to reduce pain (35).
Extra Virgin Olive Oil
Extra-virgin olive oil, high in polyphenols is one of the best antioxidants and anti-inflammatory foods. They are particularly great for brain inflammation and related issues.
For example, according to a 2024 study published in Nutrition Research, daily olive oil intake may help to reduce pain (30). Selecting the right olive oil is critical. I recommend following the principle in this article.
My Favorite Olive Oil
My favorite olive oil is this Fresh-Pressed Olive Oil. It is the most flavorful artisan olive oil you can find out there. It comes from award-winning artisan farms with a harvest-fresh taste to your table. These oils are independently lab-certified to be 100 percent extra virgin olive oil — so you can trust the quality. My family swears by it. We use it daily on our salads and meals. Our kids love it. I am sure your family will too.
I am excited to share a special offer with you. You can get this $39.00 bottle of Fresh-Pressed Olive Oil for only $1.00 to help with shipping if you click on the link here
Fruit
According to 2021 research published in the Journal of Clinical Medicine, an anti-inflammatory diet incorporating fruits may help to reduce chronic non-cancer pain (36). Fruit, in general, loaded with polyphenols and antioxidants.
Pineapples, oranges, and other fruits are loaded with structured water. They are also high in fiber which helps to reduce blood sugar issues from the sugar in fruit. I recommend eating whole food and avoiding fruit juices.
Avocados
Avocados are also another great source of healthy fats. They are also great sources of antioxidants and fantastic for skin health and anti-aging.
According to 2015 research published in Cartilage, avocados may help to reduce pain (31). You may check out my favorite avocado recipes here.
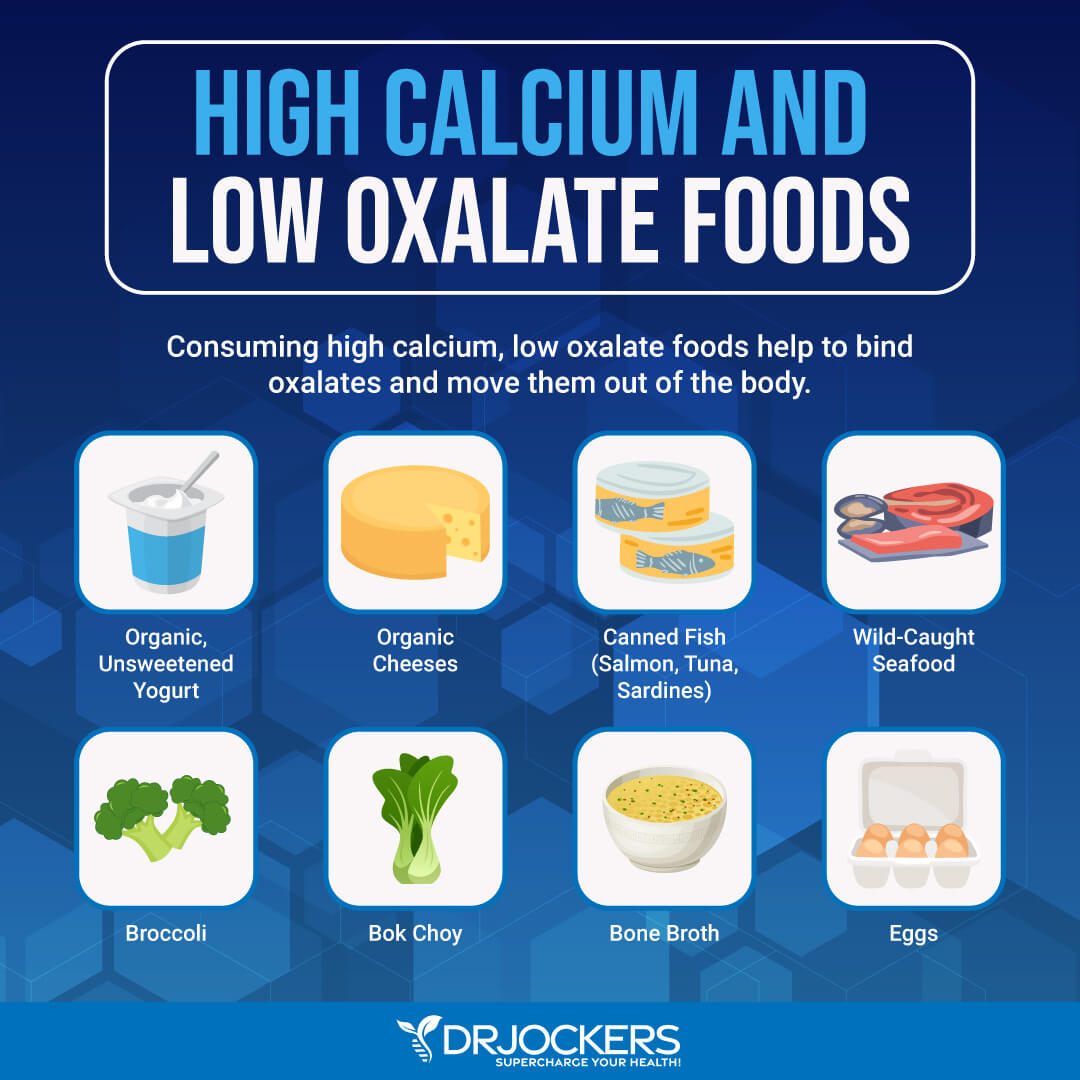
Low-Moderate Oxalate Vegetables
Oxalates are antinutrients or plant-based defense chemicals that can cause health issues and pain in some people (26, 27). If you find that high-oxalate issues cause gastrointestinal issues or other symptoms, I recommend focusing on low or moderate-oxalate vegetables.
Low and moderate oxalate vegetables include cucumber, arugula, celery, broccoli, bok choy, green beans, mushrooms, onions, carrots, hearts of carrots, and artichokes.
Apple Cider Vinegar or Lemon/Lime
Apple cider vinegar taken with meals may help digestion and reduce acid reflux and other digestive issues. According to a 2007 study published in BMC Gastroenterology, apple cider vinegar may help gastric emptying (37).
By supporting digestion, it may help your body to absorb minerals and other nutrients better. It is also rich in postbiotics to support your microbiome health. Lemon and lime juice may also help to support your digestion. It’s also loaded with vitamin C for immune health.
Polyphenol-Rich Herbs
Polyphenol-rich herbs may also help to reduce inflammation and pain. According to a 2019 study published in PLoS One, dietary polyphenols may help to reduce pain (38). When I say polyphenol-rich herbs, I’m talking about aromatic herbs with a strong smell.
Some of my favorites include oregano, basil, thyme, garlic, rosemary, sage, and parsley. They support gut microbiome health and fight fungi, parasites, and bacteria. They may also support bile health and digestion. They also make your foods taste better.
Best Supplements
A healthy diet is important but you may also benefit from some anti-inflammatory herbs that may help to reduce pain and disease.
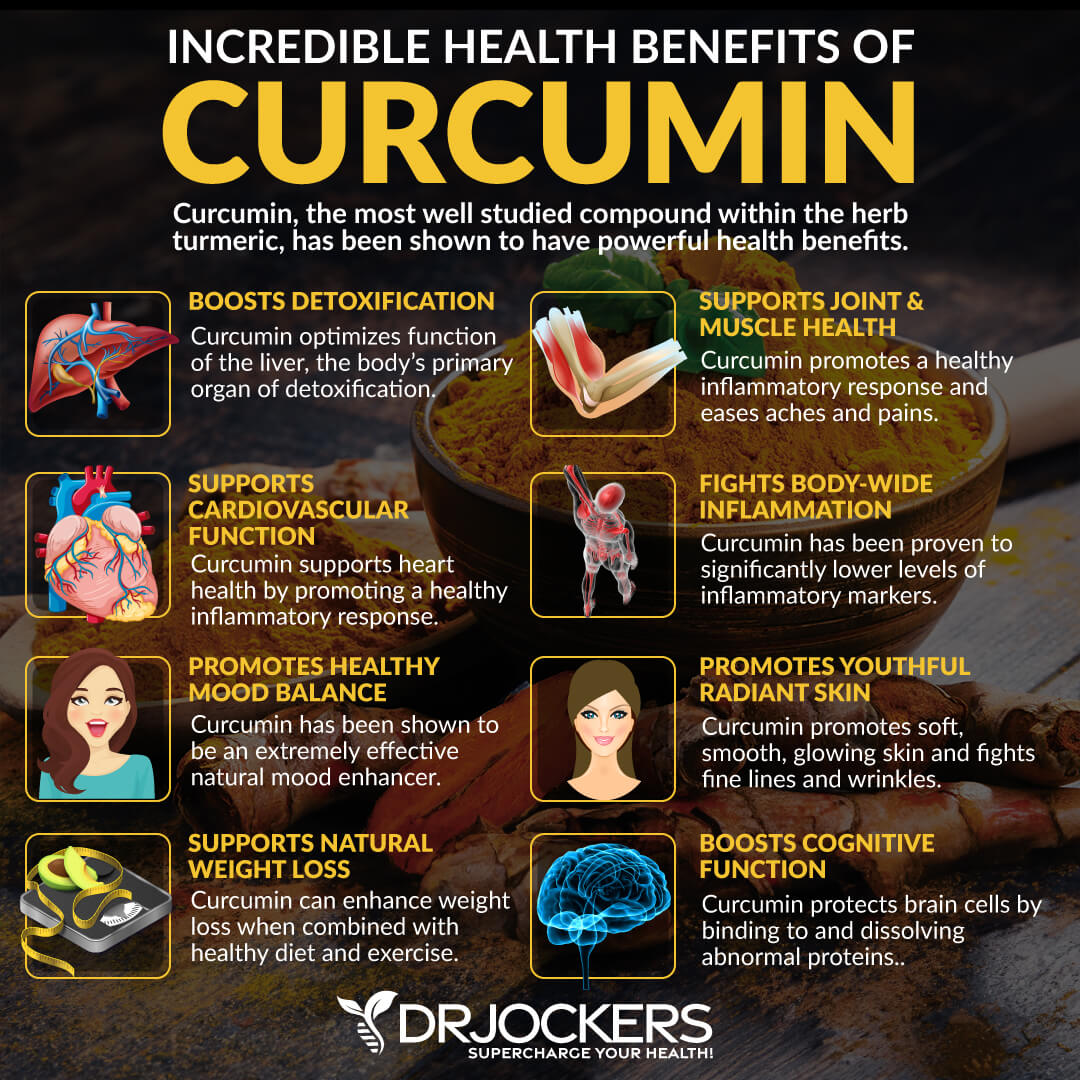
Curcumin
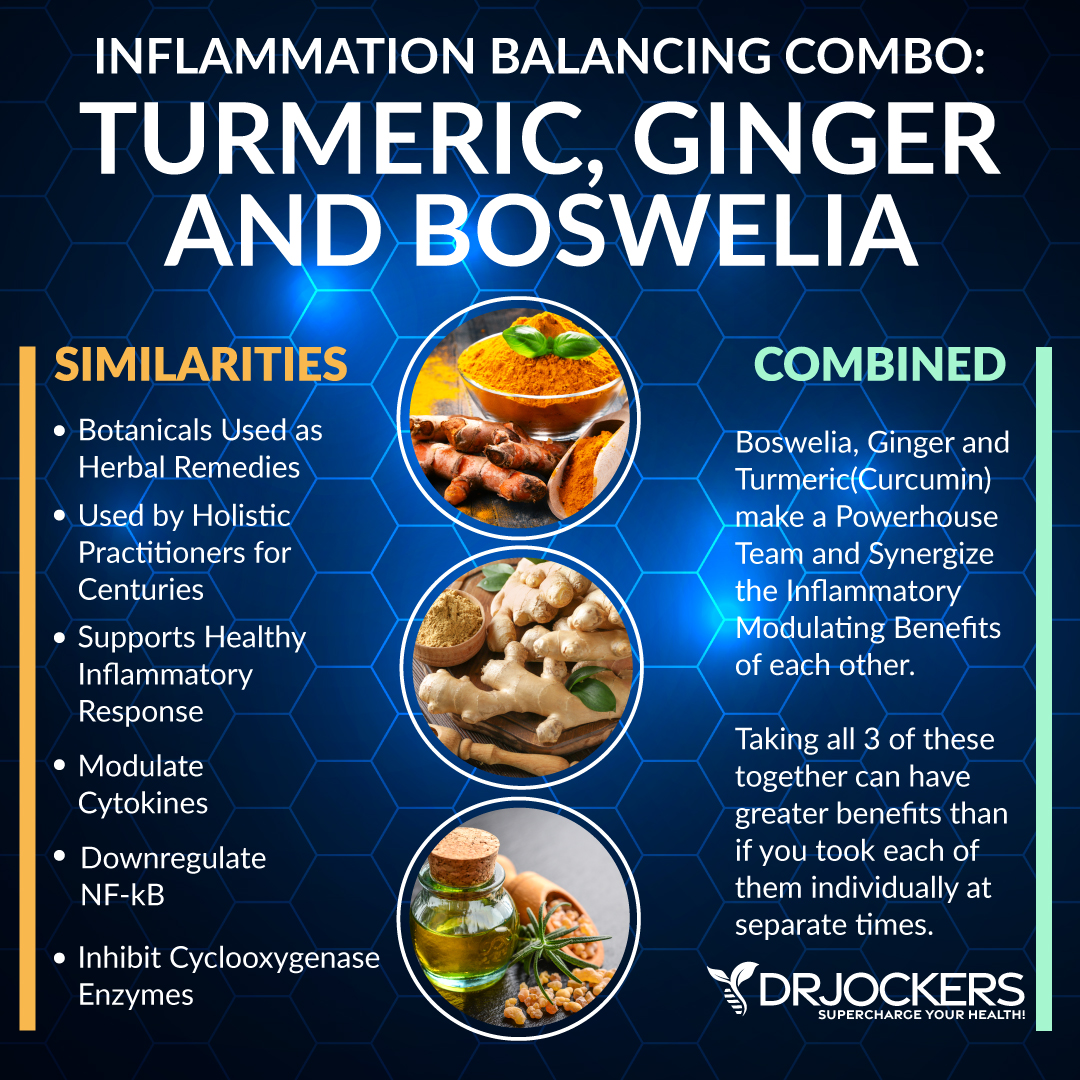
Turmeric is one of the most potent anti-inflammatory herbs. It is a staple in Indian cuisine and is the main spice used in popular curry dishes. It’s known for its unique, warm, and somewhat bitter taste. Turmeric is used to flavor and color various foods and condiments, including curry powder, mustard, butter, and even cheese.
Curcumin is the active compound of turmeric, responsible for its anti-inflammatory and pain-reducing properties. According to a 2021 systematic review published in BMJ Open Sport and Exercise Medicine, curcumin may help to reduce pain and improve function in knee osteoarthritis (39).
You may use turmeric in your meals, including curries, soups, dressings, baked potato and vegetable dishes, golden tea, ginger-turmeric tea, and smoothies. However, if you want to reduce pain and inflammation, I recommend using it as a daily curcumin supplement.
Ginger
Ginger is similar to another anti-inflammatory herb, turmeric. They both belong to the rhizome family, which means that they have an underground stem that grows horizontally, forming roots downwards while growing sprouting stems and leaves above ground. It has been used for its anti-inflammatory and medicinal properties in China and India for thousands of years, then made its way to Europe during the Roman Empire trade.
Today, it’s well-research for its anti-inflammatory benefits. According to a 2020 review published in Phytotherapy Research, ginger may be helpful for reducing pain, including in migraine, osteoarthritis, and delayed muscle soreness (40).
You may use ginger in your meals, including ginger tea, soups, dressings, baked potato and vegetable dishes, and smoothies. However, if you want to reduce pain and inflammation, I recommend using it as a daily supplement.

Boswellia
Boswellia, or otherwise known as Indian Frankincense, is a potent herbal extract that comes from the boswellia serrata tree. It has been a popular anti-inflammatory herb used by Asian and African cultures for its medicinal properties to treat a number of health conditions, including. chronic inflammatory illness.
A 2023 study published in Nutrients has found that boswellia helped to reduce pain in knee pain more effectively compared to placebo and ibuprofen (41). Research also found that the combination of boswellia and omega-3 fatty acids was more effective than boswellia or omega-3s alone. This is interesting since we’ve talked about the benefits of omega-3 fatty acids several times throughout this article.
Proteolytic Enzymes
Proteolytic enzymes are powerful biocatalysts that carry out and speed up chemical reactions in your body. They support your digestion and may reduce inflammation.
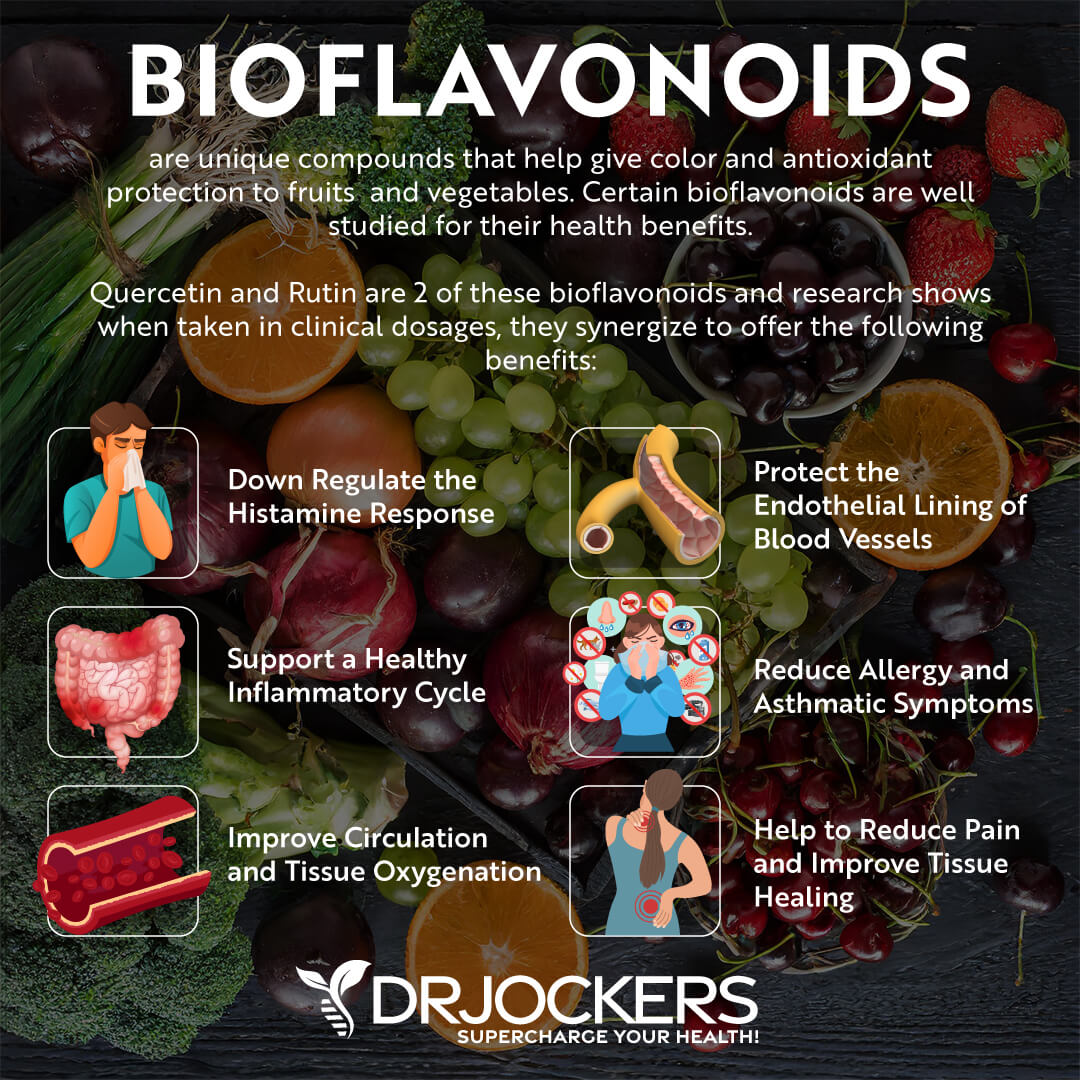
To experience the anti-inflammatory and pain-reducing benefits of curcumin, ginger, boswellia, and proteolytic enzymes, I recommend Inflam Defense. It is a powerful combination of anti-inflammatory herbs, such as curcumin, boswellia, ginger, and rosemary extract, as well as nutrients from quercetin and rutin and proteolytic enzymes.
I love Inflam Defense because it can help downregulate the inflammatory process. It can help you if you are dealing with the negative impact of acute or chronic inflammatory conditions. Take one capsule twice a day with meals or for advanced protection, take two or more capsules twice a day or as directed by your health care practitioner.
Omega-3 (EPA/DHA)
I have already talked about the benefits of omega-3 fatty acids for reducing pain and inflammation (1, 9, 10, 11). A 2023 study published in Nutrients has found that omega-3 supplementation helped to reduce pain in knee pain (41). Research also found that the combination of omega-3 fatty acids and Boswellia, an herb I mentioned earlier, was more effective than boswellia or omega-3s alone.
It’s important that you are getting both EPA and DHA forms of omega-3 fatty acids from fish, seafood, and fish oil. I recommend taking high-quality fish oil supplements daily to reduce pain with omega-3 fatty acids.
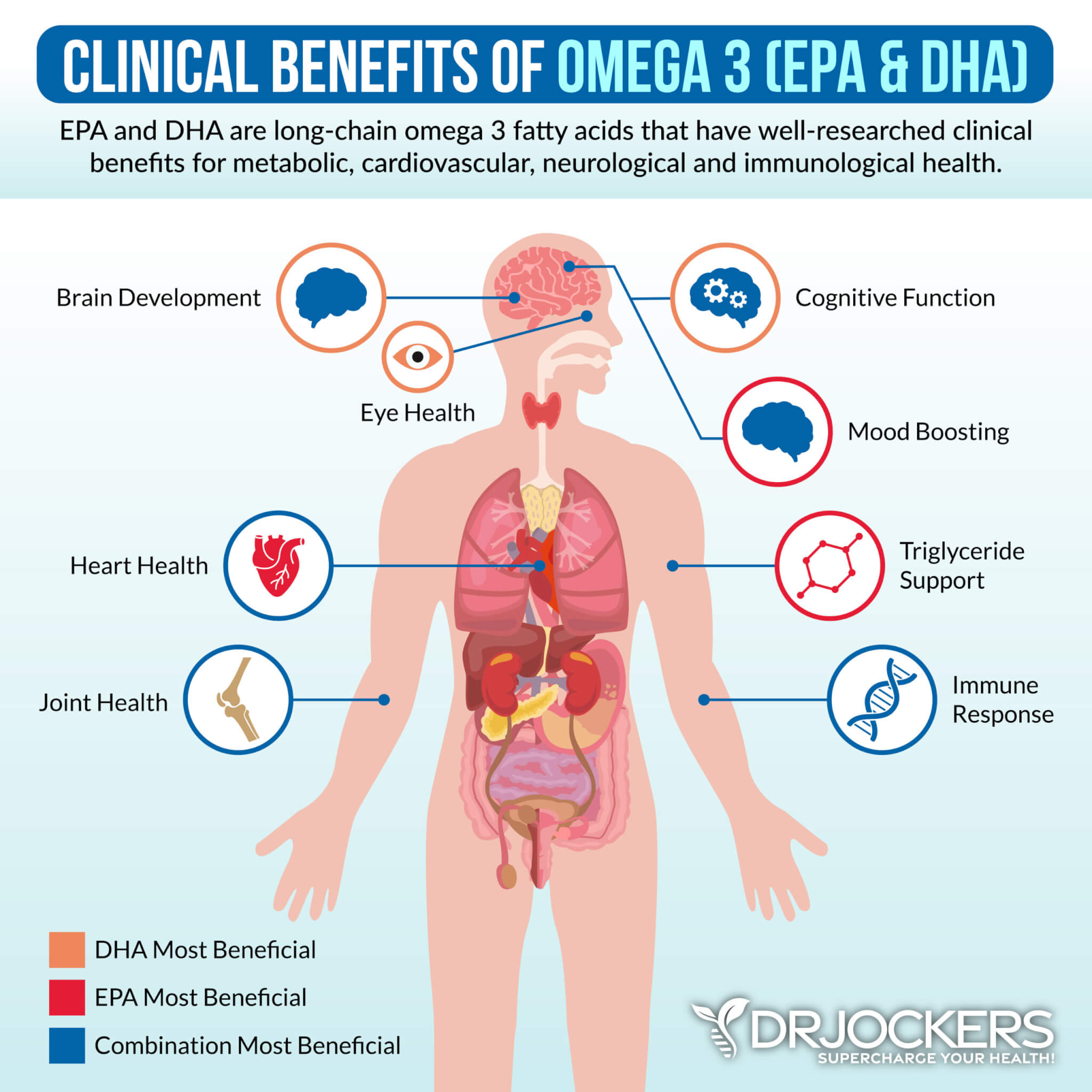
Glutathione
Glutathione is made from three amino acids: cysteine, glutamate, and glycine. It is an important antioxidant that helps to fight free radical damage and inflammation.
It may also help to reduce pain. For example, according to a 2020 review published in the Journal of Clinical Orthopeadics and Trauma, glutathione may help to reduce pain in osteoarthritis (42).

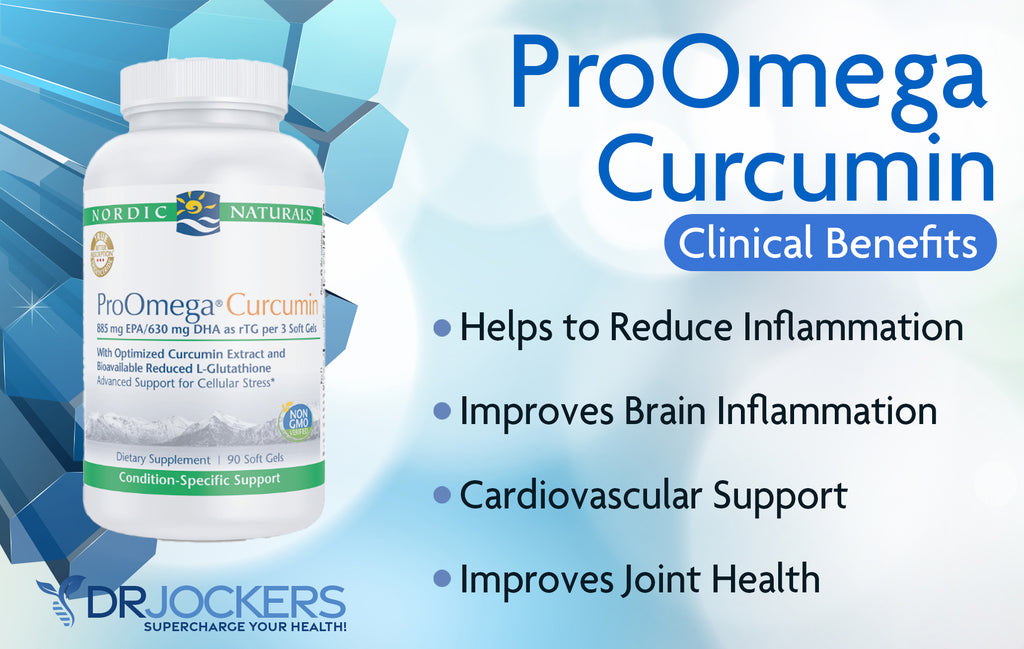
Introducing Pro Omega Curcumin:
To reduce pain, with the help of omega-3 fatty acids, glutathione, curcumin, and N-acetyl cysteine, I recommend Pro Omega Curcumin. ProOmega® Curcumin offers a powerful new solution for systemic cellular stress. This unique formulation combines concentrated omega-3s plus optimized curcumin and the potent antioxidants L-Glutathione and N-Acetylcysteine (NAC) to achieve complete functional support for long-term health.
This combination of nutrients synergizes to impact all the major inflammatory pathways, while strengthening both the inside cellular mechanics and the outer cell membrane. The omega 3’s and curcumin help to reduce inflammation on the outer cell membrane. The L-glutathione and N-Acetyl Cysteine help to balance the immune system and protect the mitochondria and DNA.
Each nutrient plays a unique and yet complementary role in promoting a balanced immunological response by supporting optimal cell function. Together, these nutrients work within cells, tissues, and organs to improve antioxidant status, normalize metabolic activity, and fine-tune the critical cell signals. Additionally, they help to strengthen the body’s detoxification capabilities.
This product uses meticulous quality control processes to ensure their fish are naturally high in omega-3 fatty acids and low in environmental toxins. All the fish used are wild-caught and sustainably sourced, so there is no worry of shortage as they keep the species strong and plentiful.
The fish used include Arctic cod from Norwegian waters (such as in the Cod liver oil), anchovies, and sardines from the South Pacific and Atlantic oceans, which are the purest and the most sustainable fish species in the world. I recommend using 3 capsules once a day with food.
Final Thoughts
Chronic pain and inflammation is a common and serious problem. It can affect your daily life, work, learning, and social life, and it may even lead to disabilities. I recommend following the tips listed in this article to reduce pain and inflammation.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!






Turmeric is high in oxalates.