 Beta Amyloid: Link to Alzheimer’s and Healing Strategies
Beta Amyloid: Link to Alzheimer’s and Healing Strategies
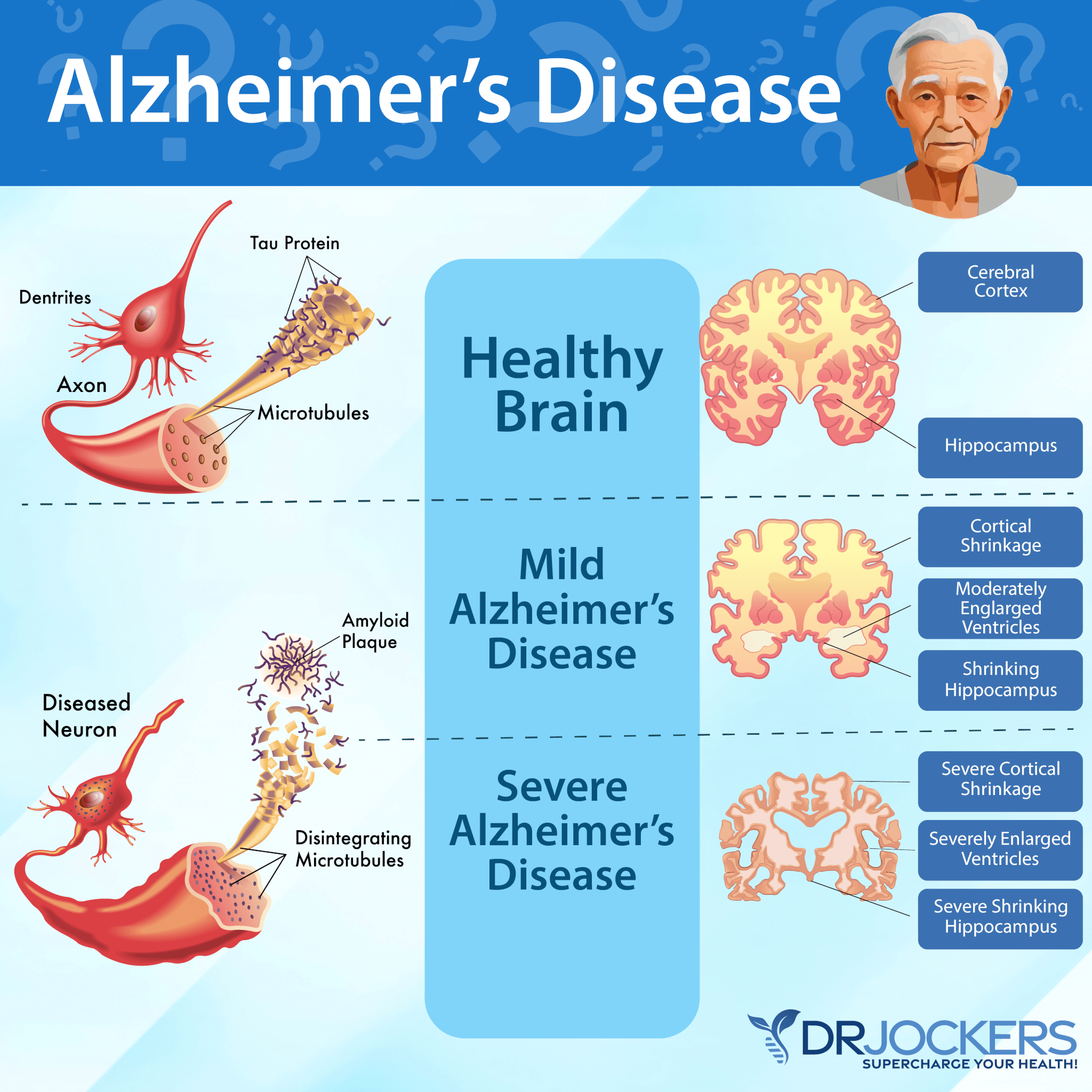
Alzheimer’s disease is the most common form of dementia. It is a progressive disease. It usually starts with mild memory loss, but as it progresses, it will increasingly impair memory, cognitive abilities, language, control of thought, and the ability to take care of daily activities. Eventually, it will lead to a loss of independence and will end with death.
To understand how Alzheimer’s disease develops, you have to understand what beta amyloids are. Beta amyloid plaques are the main cause of Alzheimer’s disease. Preventing beta amyloid plaque formation may be key to your brain health.
In this article, you will learn what beta amyloid is. You will learn about the connection between beta amyloid and Alzheimer’s disease. You will understand how beta amyloid accumulates and causes plaques.
You will learn about the connection between the APOE4 gene and beta amyloids. I will explain why beta-amyloid-targeted drugs don’t work. I will discuss the root causes of beta amyloid accumulation. You will learn about some key labs I recommend looking at. Finally, I will recommend my top natural support strategies for brain health.
What is Beta Amyloid
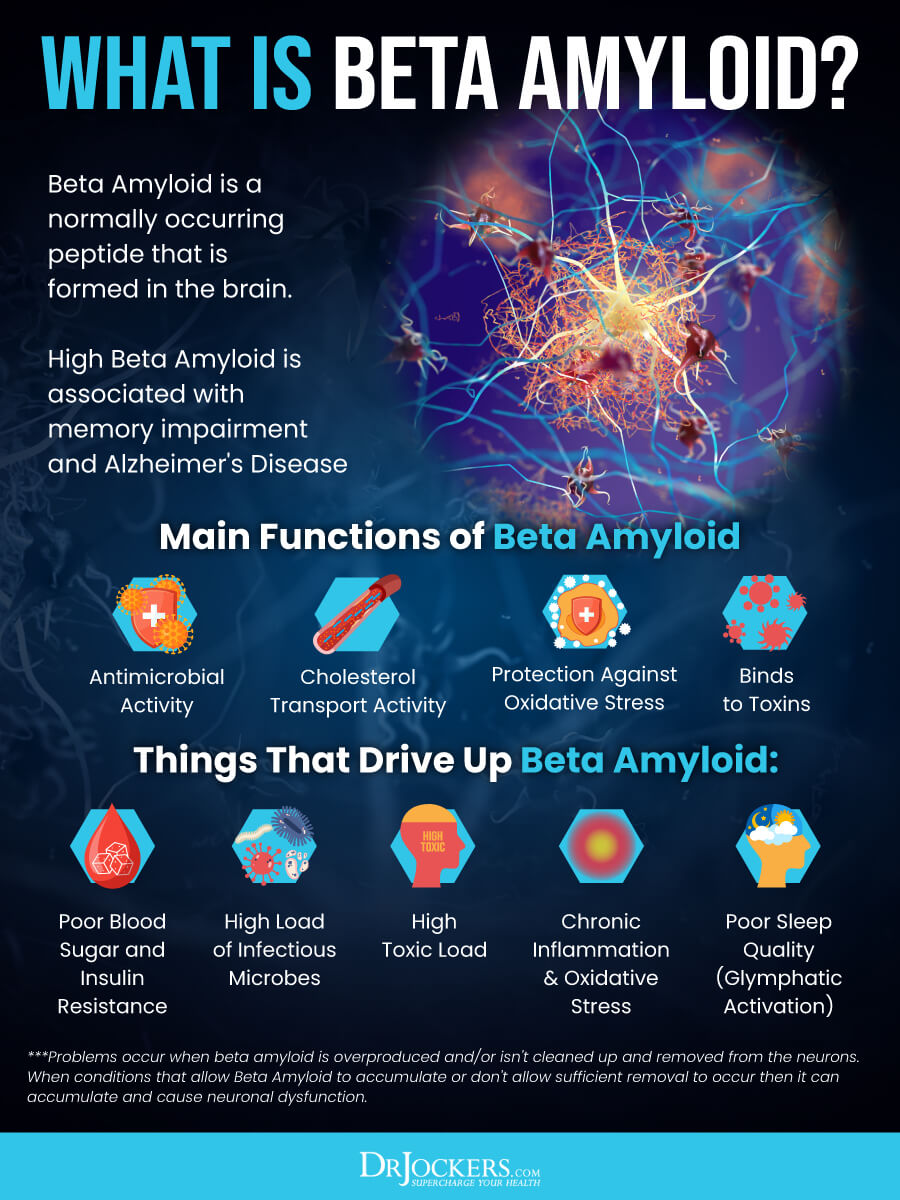
Beta amyloid or amyloid beta is (Aβ or Abeta) “a heterogeneous mixture of small peptides 37–43 amino acids in length that are generated by sequential cleavage of the amyloid precursor protein (APP) by β- and γ-secretase” (1). They are the main ingredient of the amyloid plaques found in the brain in Alzheimer’s disease.
While the normal function of beta amyloid is not completely understood, it seems that it may play a role in anti-microbial activity, cholesterol transport regulation, and protection against oxidative stress. According to a 2016 study published in Science Translational Medicine, beta amyloid is a key protein that plays a role in the pathology of Alzheimer’s disease (2).
The study found that beta amyloid may offer protection against certain fungal and bacterial infections. According to the study, beta amyloid may have a dual protective/damaging quality. It may be protective in innate immunity but may also have pro-inflammatory qualities driving amyloidosis.
According to a 2002 study published in FASEB Journal, increased cholesterol levels may encourage higher levels of beta amyloid, which may lead to neurotoxicity (3). According to a 2002 study published in the Journal of Neuroscience, it may serve as an antioxidant, offering protection against oxidative stress (4).
A 2018 review published in Frontiers in Aging Neuroscience has found that targeting beta amyloids may be an effective and safe way to approach Alzheimer’s treatment (5). According to a 2017 review published in Acta Pharmacologica Sinica, beta amyloids are a major component of senile plaques, causing neurotoxicity and Alzheimer’s disease (6). Targeting beta amyloid may offer new therapeutic approaches for Alzheimer’s disease, and there are currently various options under development to inhibit beta amyloid oligomerization.
This is an important development because currently existing medications only address the symptoms of Alzheimer’s but don’t reverse or cure the disease. In the last decade, many candidate drugs have failed. Drugs that inhibit beta amyloid production and aggregation, beta amyloid antibodies, and vaccines are currently undergoing clinical trials. Later in this article, I will share that current beta amyloid drugs don’t work and will offer some strategies to support normal beta amyloid levels naturally.
Beta Amyloid and Alzheimer’s Disease
Your brain is the home of tens of billions of neurons. These are specialized cells that help to transport and process information through chemical and electrical signals. They move information between different parts of your brain and other parts of your body, such as your organs and muscles. In Alzheimer’s disease, neural communication is interrupted, leading to loss of function, cellular death, and neurodegeneration.
The function, health, and survival of neurons depend on:
- Communication: Your neurons are in constant communication with neighboring brain cells and the rest of your body through synaptic connections.
- Metabolism: Metabolism refers to the breakdown of chemicals and nutrients within a cell. For this essential function for cellular health and survival, your cells need plenty of energy through oxygen and glucose supplied by the blood moving through your brain.
- Repair and regeneration: Most cells in your body are short-lived, but neurons can live for a long time. To live and function well, they need to constantly maintain, repair, and regenerate themselves. For example, synaptic connections may strengthen or weaken throughout your life, affecting cognition, memory, and brain health.
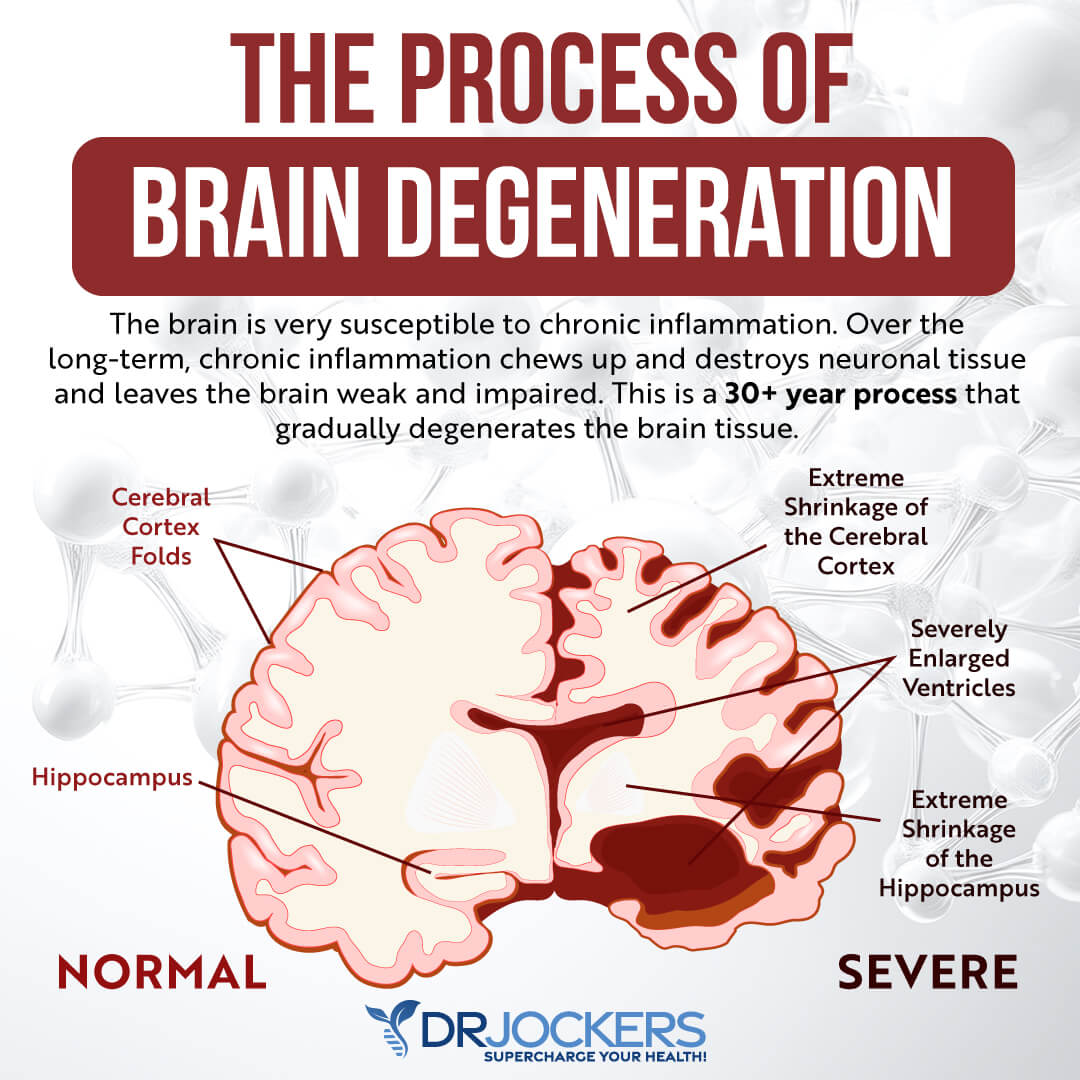
Your neurons are key players in your central nervous system and brain function. In Alzheimer’s disease, they are greatly affected. While it’s a normal part of aging for your brain to shrink and lose some neurons to a certain degree, losing neurons in large numbers is not normal. In Alzheimer’s disease, neural damage is widespread.
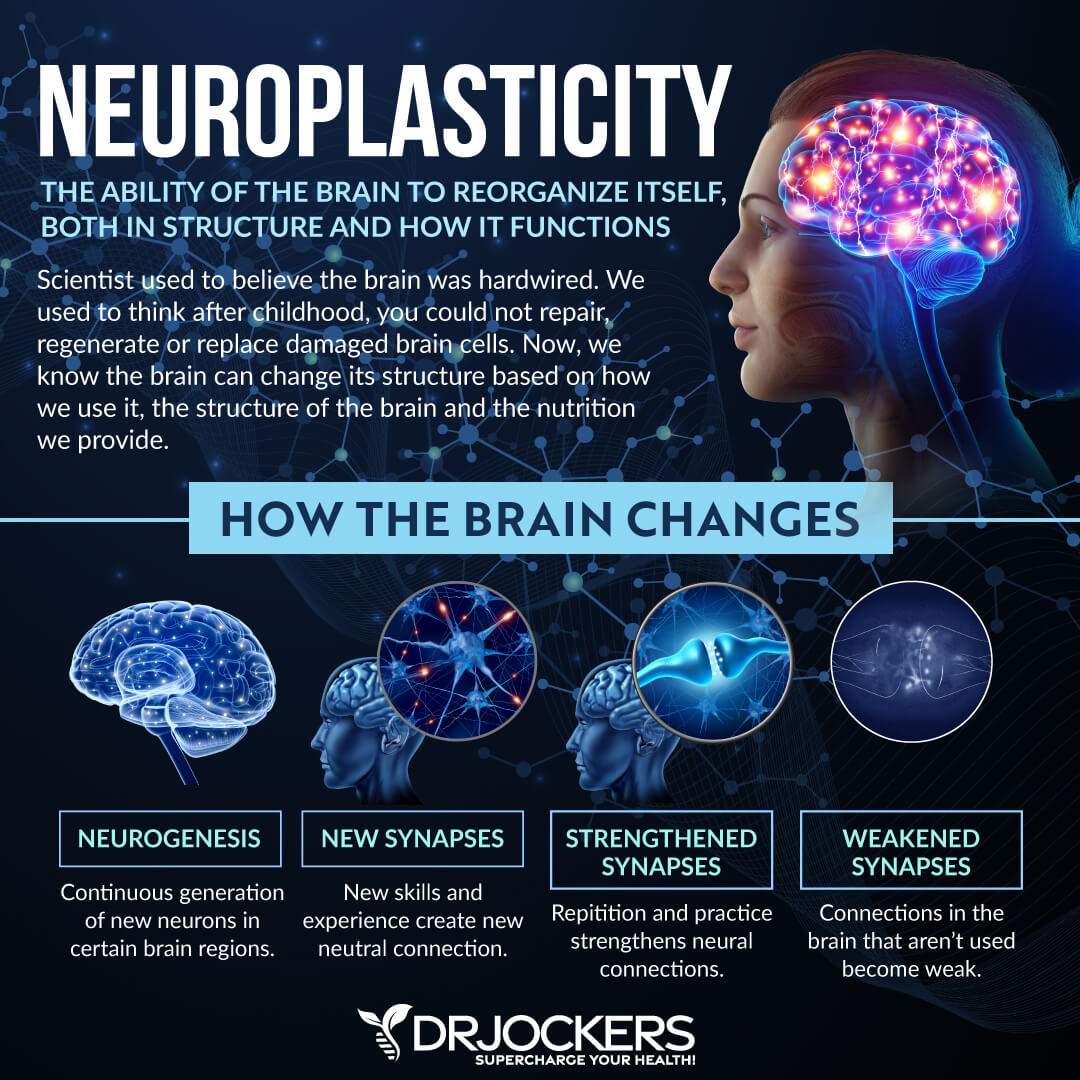
Your neurons will stop functioning properly, start to lose connection, and end up dying in large numbers because the disease disrupts communication, metabolism, repair, and regeneration processes. This will affect your memory and cognitive abilities.
If you have Alzheimer’s, you will gradually lose your cognitive functions, and eventually, you will lose your ability to function and live your life independently. As a progressive disease, Alzheimer’s ultimately ends with death.
In Alzheimer’s disease, we can observe many molecular and cellular changes. One of these is in amyloid plaques. As you know, beta amyloid is a protein that’s involved in Alzheimer’s disease. Beta amyloid is made due to the breakdown of the amyloid precursor protein.
Beta amyloid 42, a type of beta amyloid, is particularly toxic. It is found at abnormal levels in Alzheimer’s, clumping together causing plaques that interrupt communication between neurons and cellular function.
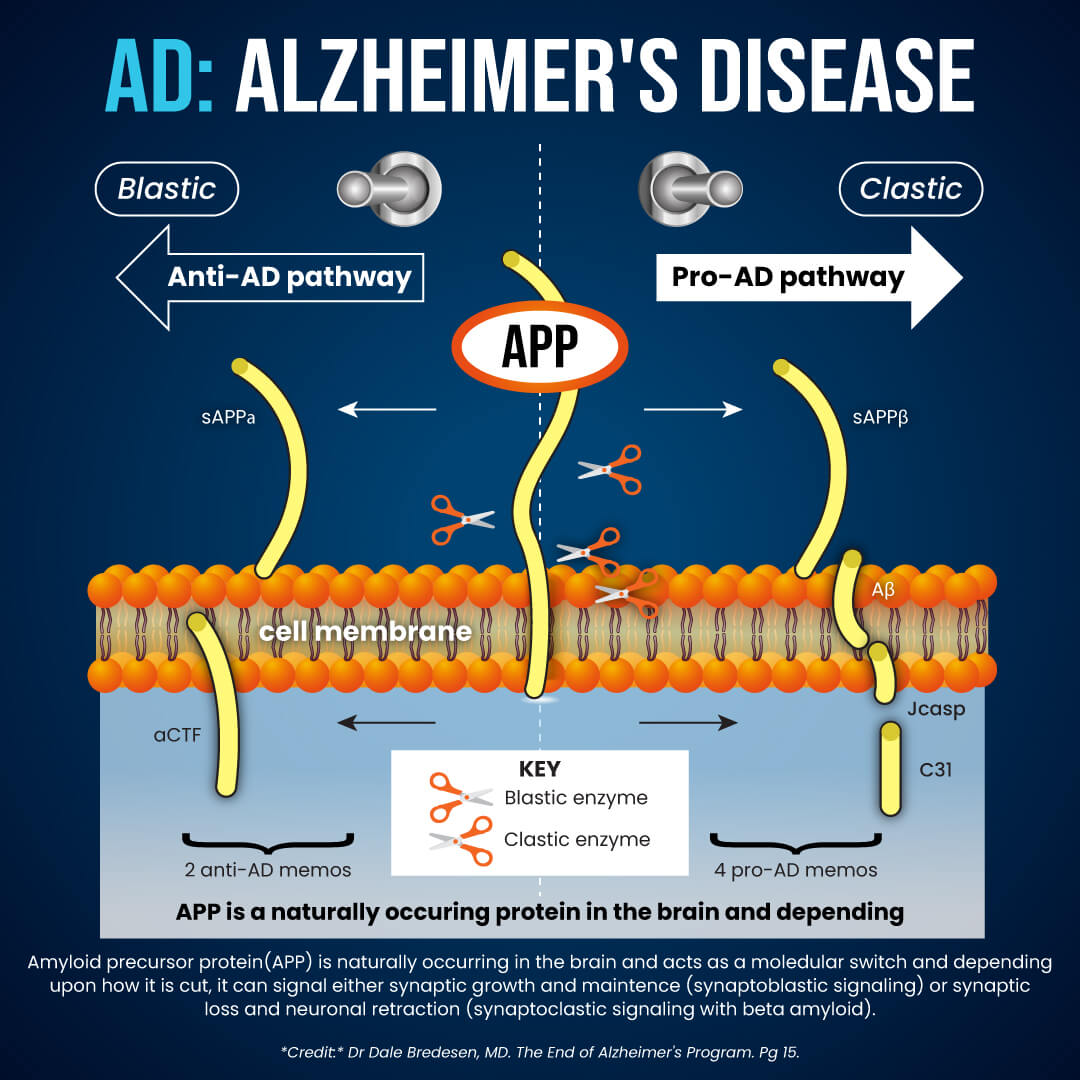
Other characteristics of Alzheimer’s disease include neurofibrillary tangles, chronic inflammation, and vascular issues. Neurofibrillary tangles are an abnormal buildup of the tau protein inside the neurons that may block the neuron’s transport system and synaptic communication.
High levels of beta amyloid may increase the spread of tau in the brain. Alzheimer’s patients also experience chronic inflammation when the microglia cannot clean up waste, debris, beta-amyloid plaques, and other protein buildup.
This chronic inflammation can cause further neuron damage. Furthermore, due to beta amyloid buildup in the brain arteries, people with Alzheimer’s may experience vascular problems, atherosclerosis, and mini strokes. Over time, Alzheimer’s disease causes brain atrophy or loss of brain volume, brain function, and eventually death (7, 8).

How Does Beta Amyloid Accumulate
It is not exactly clear where beta amyloid starts to accumulate in early Alzheimer’s disease. According to a 2017 research published in Nature, abnormal levels of beta amyloid 42 can be found in the cerebrospinal fluid (CSF) in preclinical Alzheimer’s disease through PET scans (9).
Accumulation of beta-amyloid seems to begin in the precuneus, medial orbitofrontal, and posterior cingulate cortices. These are all areas of the default mode network (DMN), which is a network of brain regions that are active when you are not focusing on the outside world. It’s basically your ‘monkey mind’ responsible for daydreaming, remembering experiences, and mind-wandering.
Early accumulation of beta amyloid can be found in those with normal beta amyloid 42 levels. This early accumulation may be linked to hyperconnectivity within the DMN and between the frontoparietal network of the brain. The frontoparietal network is the area where the frontal and parietal regions of your brain meet. According to the research, beta amyloids mainly accumulate in the DMN in preclinical Alzheimer’s disease and can already affect brain function.
APOE4 Gene and Beta Amyloid
The APOE4 gene is a gene that is responsible for a strong risk factor for Alzheimer’s disease. According to a 2019 review published in the Journal of Clinical Investigation, the APOE4 gene may increase the risk of beta amyloid accumulation (10). Individuals carrying one APOE4 Allele have a 2-3 fold greater risk of developing Alzheimer’s. Those carrying 2 APOE4 Allele have a 10-15 fold greater risk of developing Alzheimer’s (11).
According to the National Institute of Health – National Institute on Aging, about 25 percent of people carry one copy, and 1 to 2 percent carry copies of the APOE4 gene (12). Though inheriting the APOE4 gene increases the risk of Alzheimer’s disease, it does not mean that you will definitely develop it. According to a 2021 study published in the Science of Translational Medicine, lipid imbalances may affect APOE4 gene expression (13).

Why Beta Amyloid Targeted Alzheimer’s Drugs Don’t Work
You may think that beta amyloid targeted Alzheimer’s drugs are the answer. Unfortunately, it seems like that may not be the case. First, though a new drug Aduhelm was approved by the Food & Drug Administration (FDA), it doesn’t seem effective enough for insurance to cover it for most patients. Other medications in development got sidelined due to not-too-convincing results in clinical trials.
And most recently, we learned that 16 years ago, researchers actually faked images in a paper that most research has relied on since (14). Most of the research on beta amyloid-targeted drugs has been relying on this one research paper with fake results. So should we even focus on beta amyloid?
Yes, but maybe in a different way. According to the Michigan Alzheimer’s Disease Center, beta amyloid and beta amyloid plaques do play a role in dementia and Alzheimer’s disease (15). However, it seems like the issue of neurodegeneration is more complex than just one molecule. The paper with the fake results focused on a specific form of beta amyloid, beta amyloid 56. However, seeing the lack of results focusing on this specific form of beta amyloid, many researchers haven’t been paying much attention to it for years.
Researchers think that it’s still important to study beta amyloid and its effects on the brain, however, we need to focus on different forms of beta amyloid. We also need to look at other various factors, including environmental factors, immune health, tau, other molecules, and other proteins that may play a role in beta amyloid plaque formation and Alzheimer’s disease.
Alzheimer’s disease and dementia are complex diseases. Since there are likely many things going wrong in the brain, we need to look at the entire picture and multiple factors, not just one molecule. Nutrition, sleep, exercise, social engagement, and other factors may all play a role in reducing the risk and addressing Alzheimer’s disease.
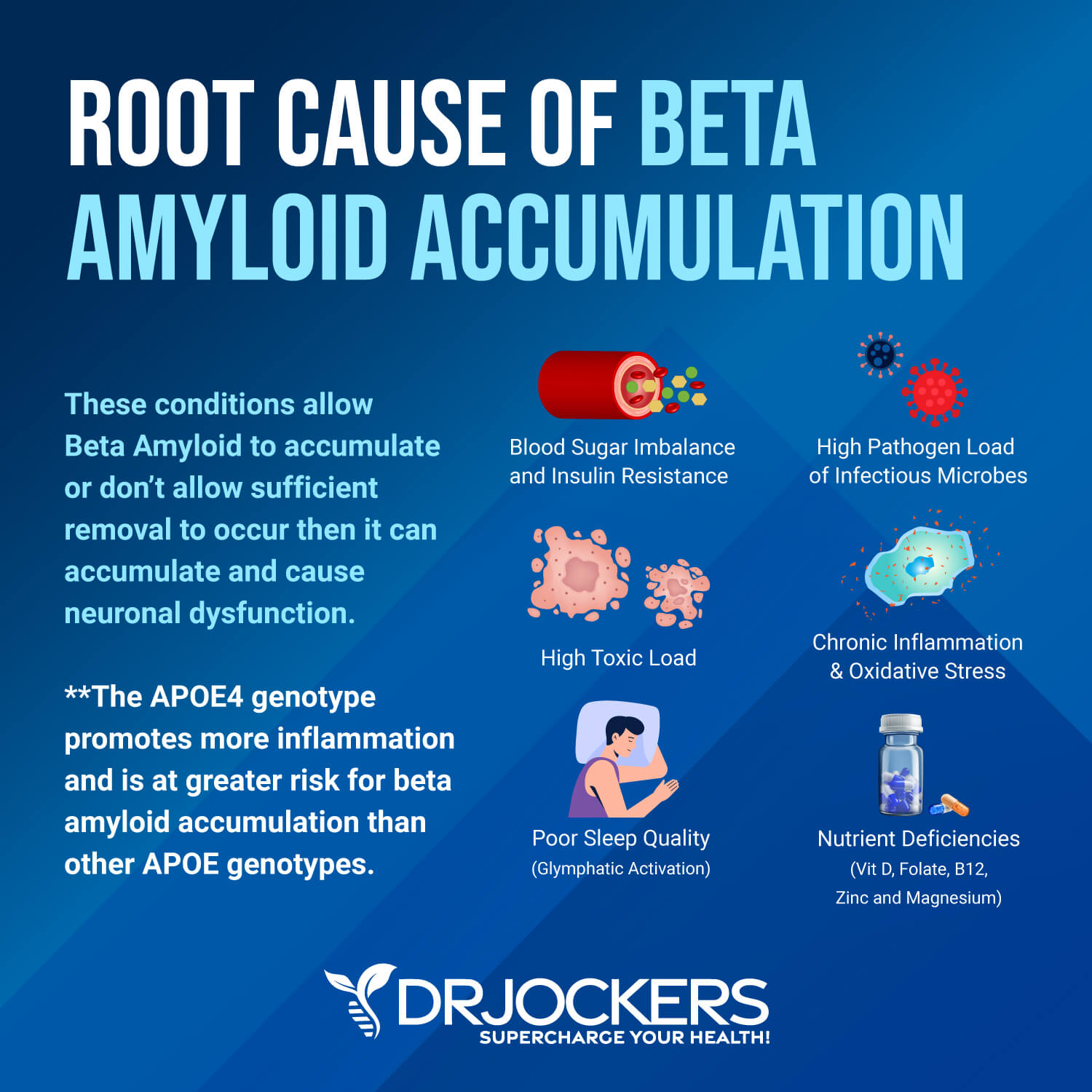
Root Causes of Beta Amyloid Accumulation
As with every health issue, we need to look at the root causes of the issues to effectively address the problem. Let’s look at the root causes of beta amyloid accumulation.
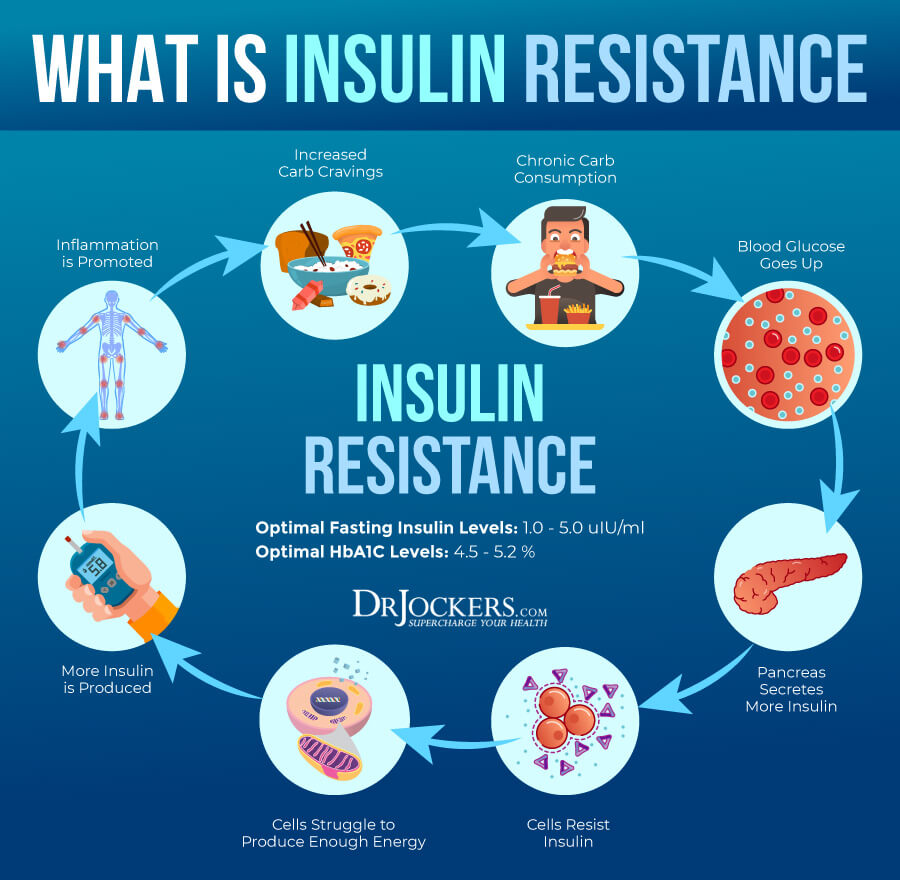
Insulin Resistance
Insulin resistance means that your body cannot respond to insulin well and cannot handle sugar from your blood properly. As a result, your body has to make more and more insulin. Insulin resistance can increase the risk of prediabetes and type 2 diabetes. It may also increase the risk of various other health issues, including Alzheimer’s disease.
A 2017 study published in Frontiers in Aging Neuroscience has found that insulin resistance may increase the risk of beta amyloid and tau pathologies causing Alzheimer’s disease (16). A 2021 study published in Frontiers in Neurosciences has also found that insulin resistance may increase the risk of Alzheimer’s disease by increasing beta amyloid and tau buildup (17). Addressing insulin resistance may help to improve biomarkers of Alzheimer’s disease.

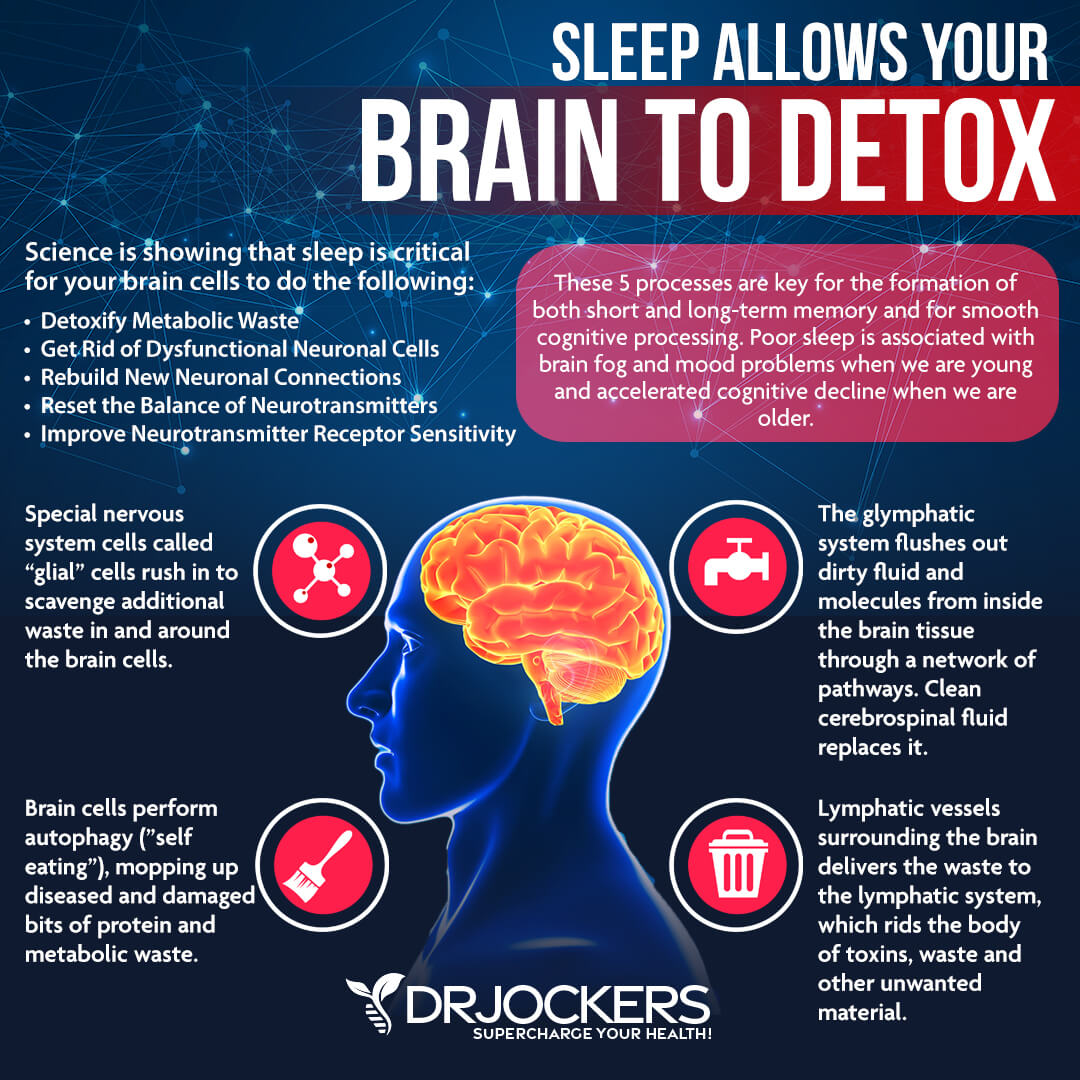
Poor Sleep Quality
Regular quality sleep is essential for your overall health and energy, including your brain health. Poor sleep can increase the risk of cognitive and brain health issues. It may interfere with glymphatic function and brain drainage.
According to the National Institute of Health, research has found that sleep helps to clear out beta amyloid from the brain (18). Sleep deprivation, poor sleep quality, or not enough sleep can negatively impact your beta amyloid levels and may increase the risk of buildup and consequent Alzheimer’s disease.
A 2020 study published in Current Biology has found that short sleep can change beta amyloid levels in the brain (19). Over time this can lead to long-term consequences, brain issues, and Alzheimer’s disease. According to a 2020 study published in Brain Sciences, poor sleep may interfere with glymphatic system function and glymphatic clearance and may increase the risk of buildup, brain damage, and neurodegeneration (20).
Chronic Infections
Chronic infections may also play a role in the increased risk of developing Alzheimer’s disease. A 2016 animal study published in the Science of Translational Medicine has also found beta amyloid may have a dual protecting/damaging effect on the brain (21). It may help to protect the body from bacterial infections, but it can also increase inflammation and, at increased levels, cause problems.
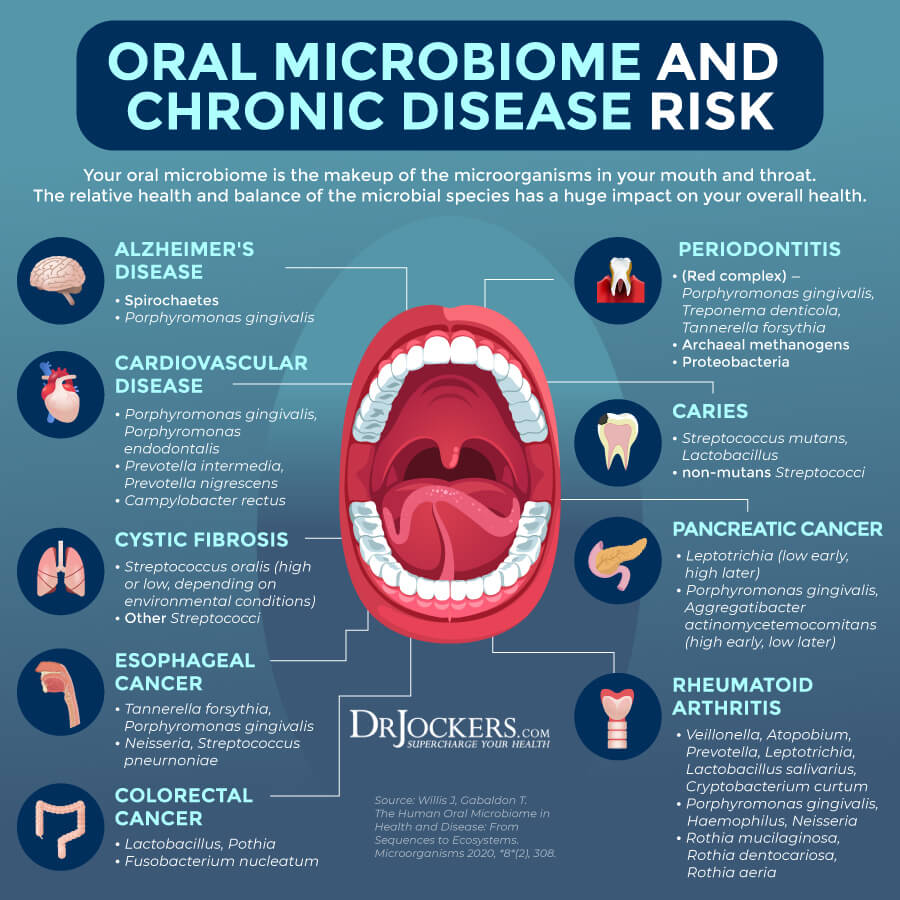
A 2018 review published in Frontiers in Aging Neuroscience has found infections may play a role in Alzheimer’s disease (22). Beta amyloid is an antimicrobial peptide that offers protection against bacterial, viral, and fungal infections. This means that infections increase the synthesis of beta amyloid.
This is not a problem with acute infections that clear up within a short time. However, when an infection becomes chronic, it will increase beta amyloid levels, which may have detrimental effects. Some of the most common chronic infections include Lyme disease, Herpes simplex virus, Epstein Barr virus (EBV), and oral bacterial infections.
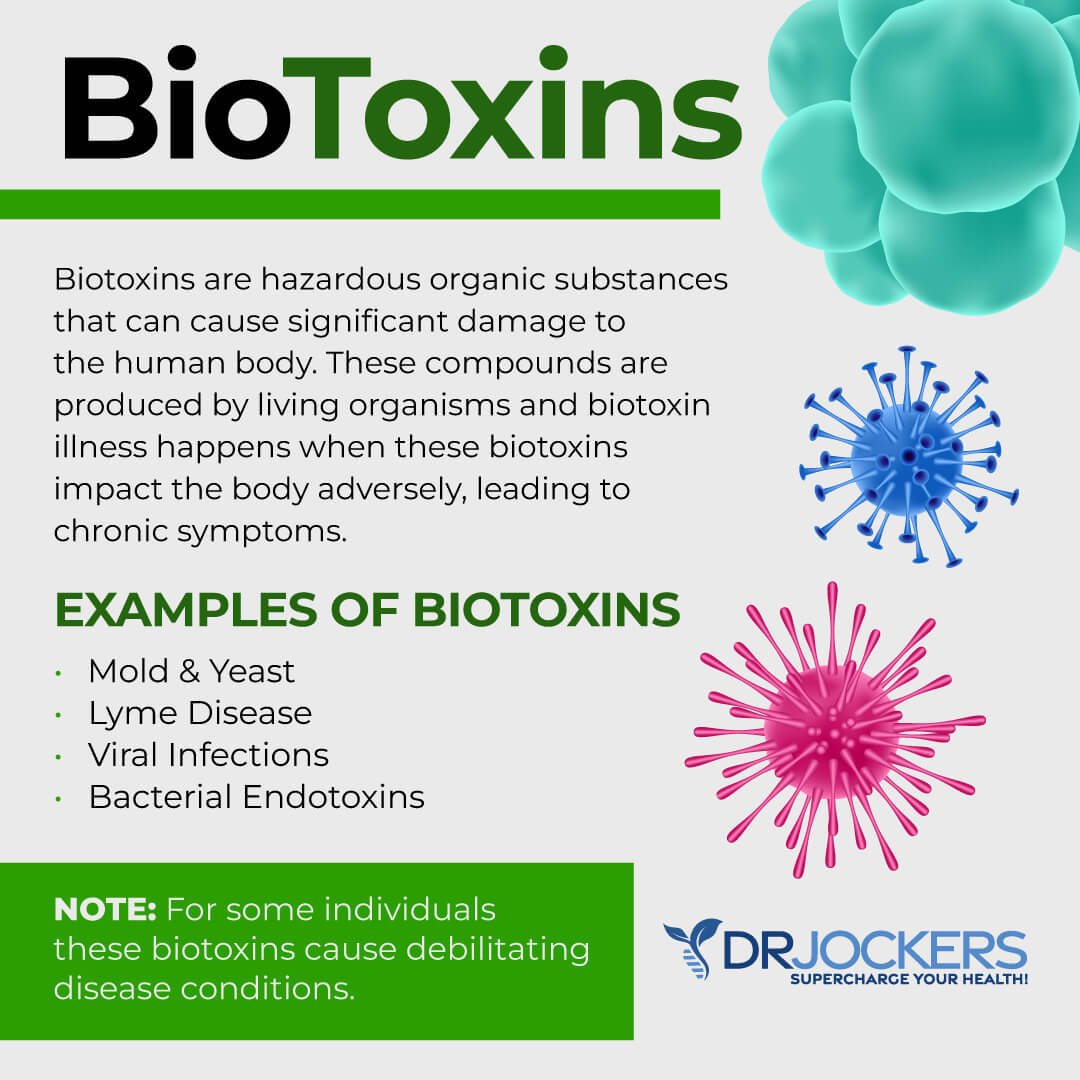
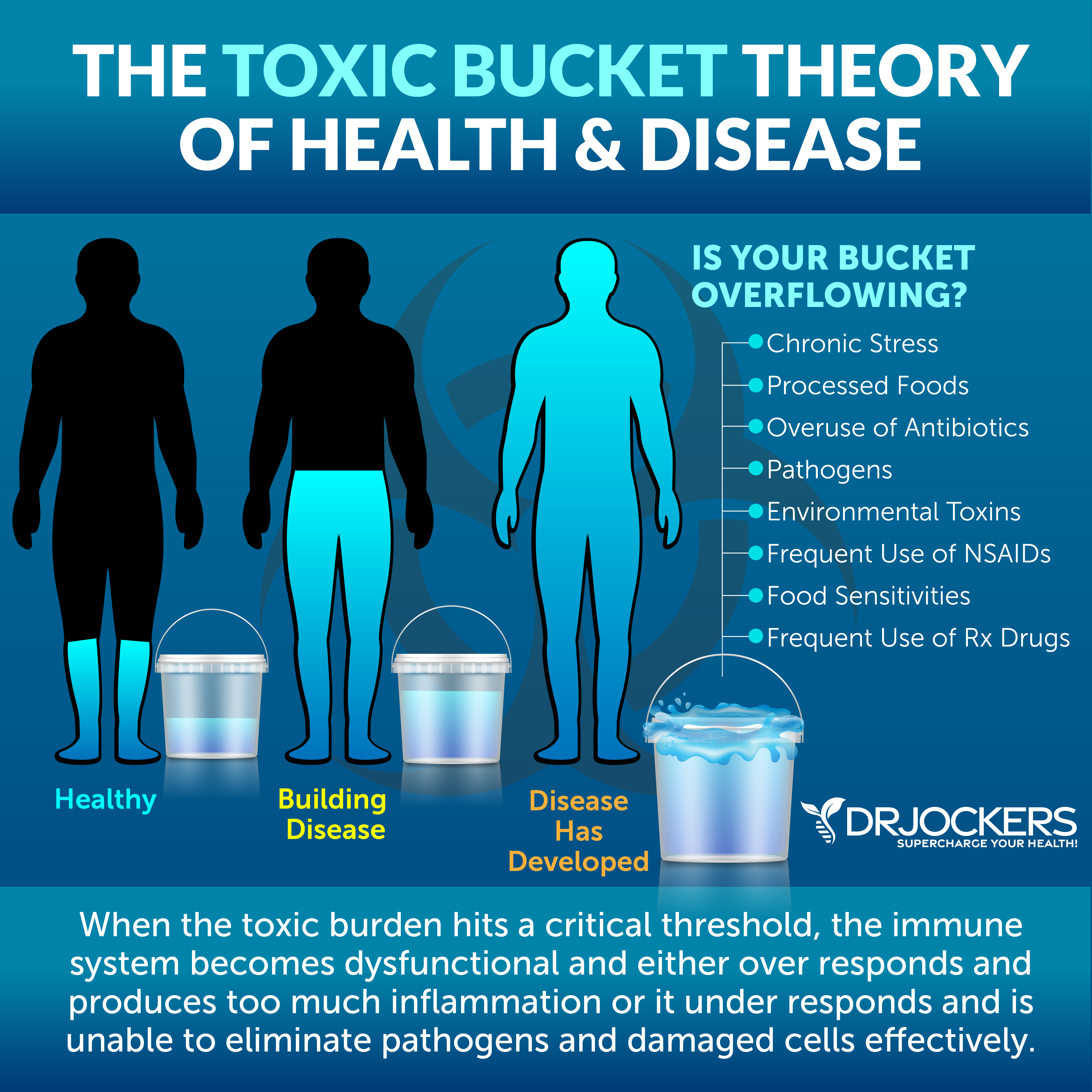
High Toxic Load
Toxins are everywhere, in our air, tap water, processed food products, cleaning, body, and beauty products, and everywhere else. High toxin load can increase chronic inflammation and increase the risk of all kinds of health issues, including Alzheimer’s disease.
According to a 2016 study published in Aging (Albany), there are three types of Alzheimer’s disease: type 1 or inflammatory, type 2 or non-inflammatory or atrophic, and type 3 or cortical (23). Type 3 Alzheimer’s seems to be commonly connected to an exposure to certain toxins, most commonly connected to inhalational (IAD) manifestation of chronic inflammatory response syndrome (CIRS).
Common toxins that may cause this include biotoxins, such as mold mycotoxins. A 2021 study published in Toxins (Basel) has also found that mycotoxins may play a role in Alzheimer’s and Parkinson’s disease (24).
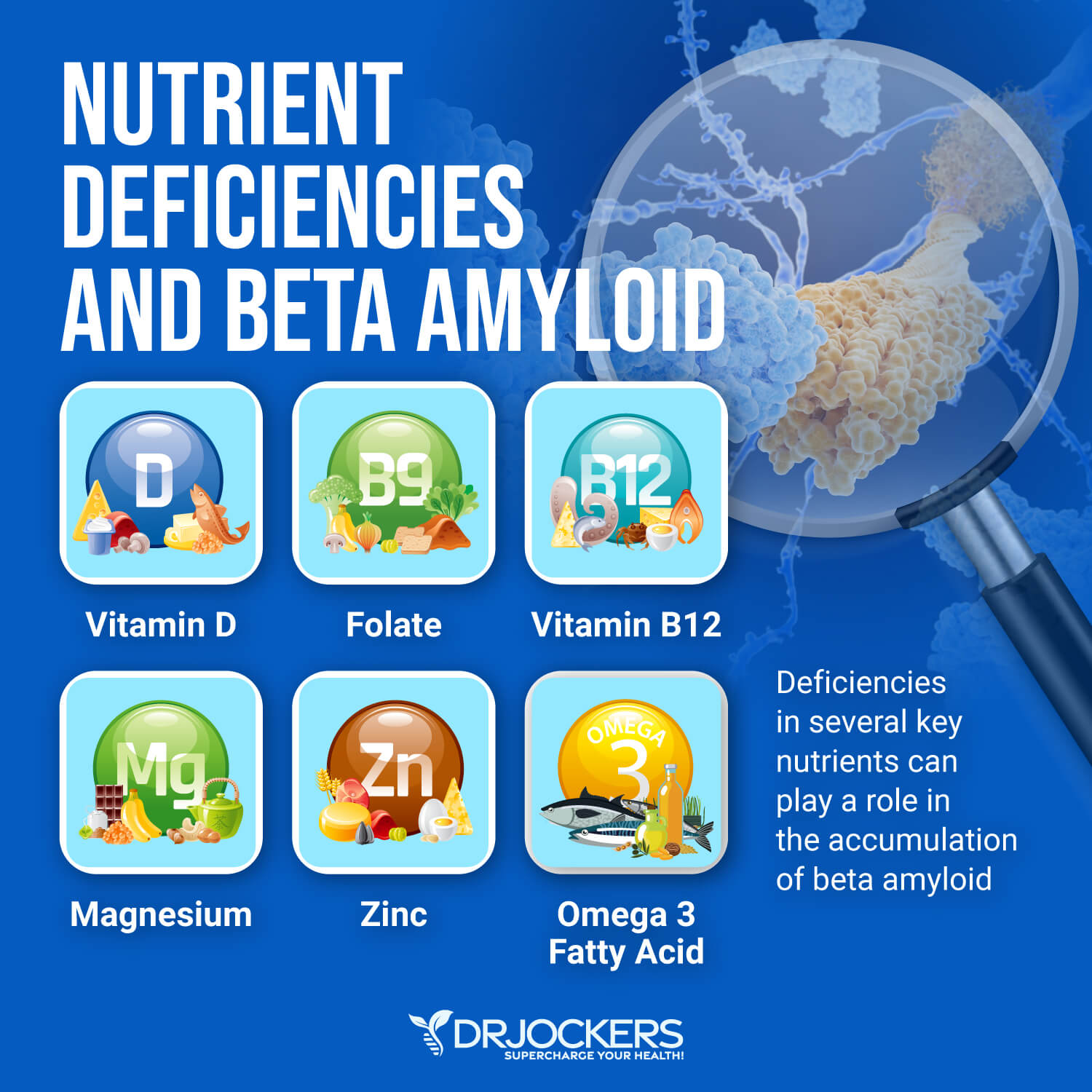
Nutrient Deficiencies
Certain nutrient deficiencies may also play a role in high beta amyloid levels and Alzheimer’s disease, including vitamin D, vitamin B12, folate, magnesium, and zinc deficiencies:
- Vitamin D deficiency: According to a 2018 study published in Alzheimer’s Research and Therapy, vitamin D deficiency may increase beta amyloid levels and the risk of dementia and Alzheimer’s disease (25).
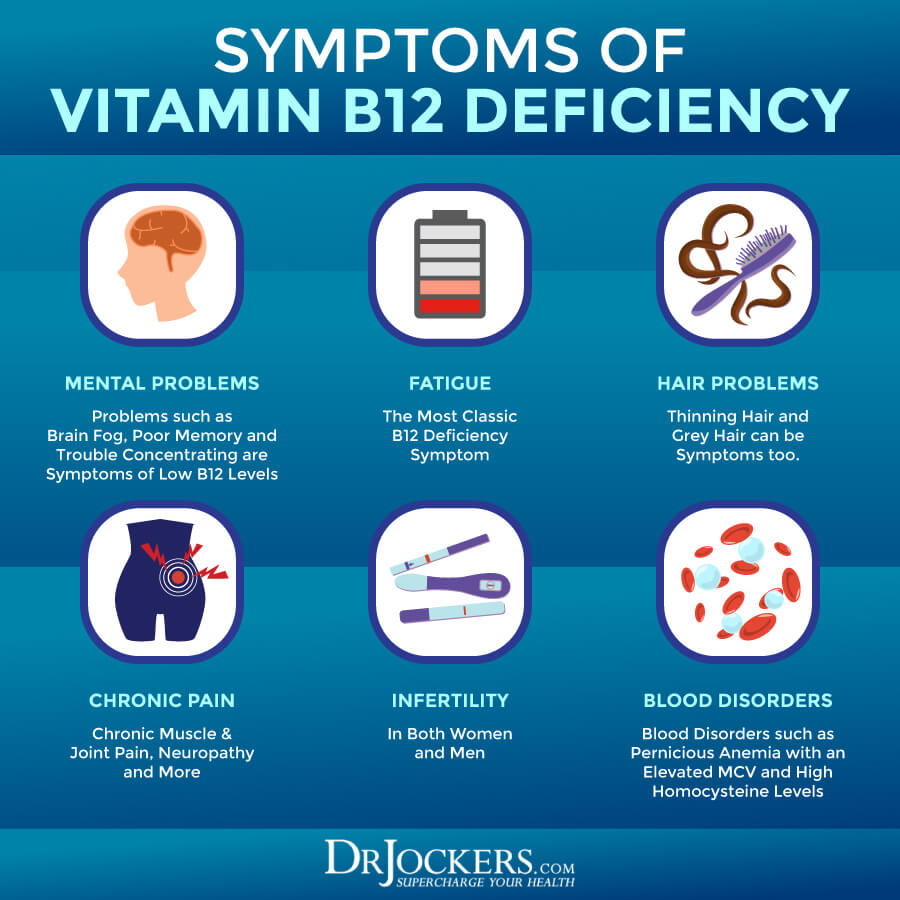
- Vitamin B12 deficiency: According to a 2021 study published in Antioxidants (Basel), vitamin B12 deficiency may increase beta amyloid and tau levels and increase the risk of Alzheimer’s (26).
- Folate deficiency: According to a 2021 systematic review, folate deficiency may increase the risk of Alzheimer’s disease (27).
- Magnesium deficiency: According to a 2011 book published by the University of Adelaide Press, magnesium may play a role in pathologies related to beta amyloid and the increased risk of Alzheimer’s disease (28).
- Zinc deficiency: According to a 2021 study published in Alzheimer’s Research & Therapy, zinc deficiency may be linked to high beta amyloid levels and an increased risk of Alzheimer’s disease (29).
Key Labs to Look At
To uncover some of the root cause factors and risk factors of beta amyloid plaques and Alzheimer’s disease, I recommend looking at some key labs.
HbA1C and Fasting Insulin
Blood sugar imbalances are one of the main causes of inflammation, so I recommend checking your hemoglobin A1C (HbA1C) levels. Your HbA1C levels measure your average blood sugar over the past 2 to 3 months. Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months, making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6, while the optimal range is 4.5 – 5.2.
Blood sugar imbalances may increase your risk of inflammation. In addition to testing your HbA1C levels, I recommend checking your fasting insulin levels. Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml, and the optimal range is 1.0 – 5.0 uIU/ml.
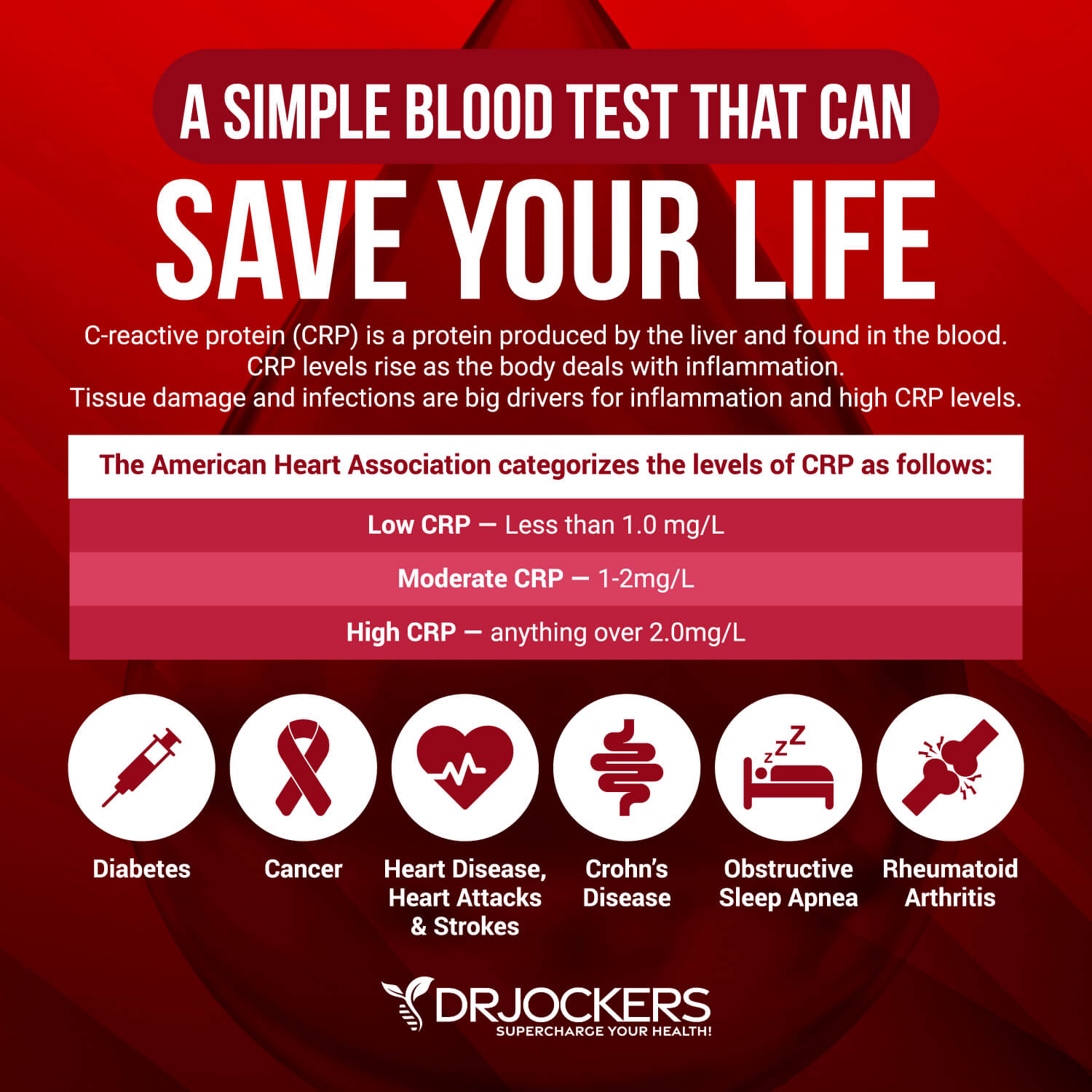
Hs-CRP
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L, while the optimal range is 0 to 1 mg/L.
When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions. Ideally, we want to see the CRP levels as low as possible, certainly under 1 mg/L and more like .01 mg/L.
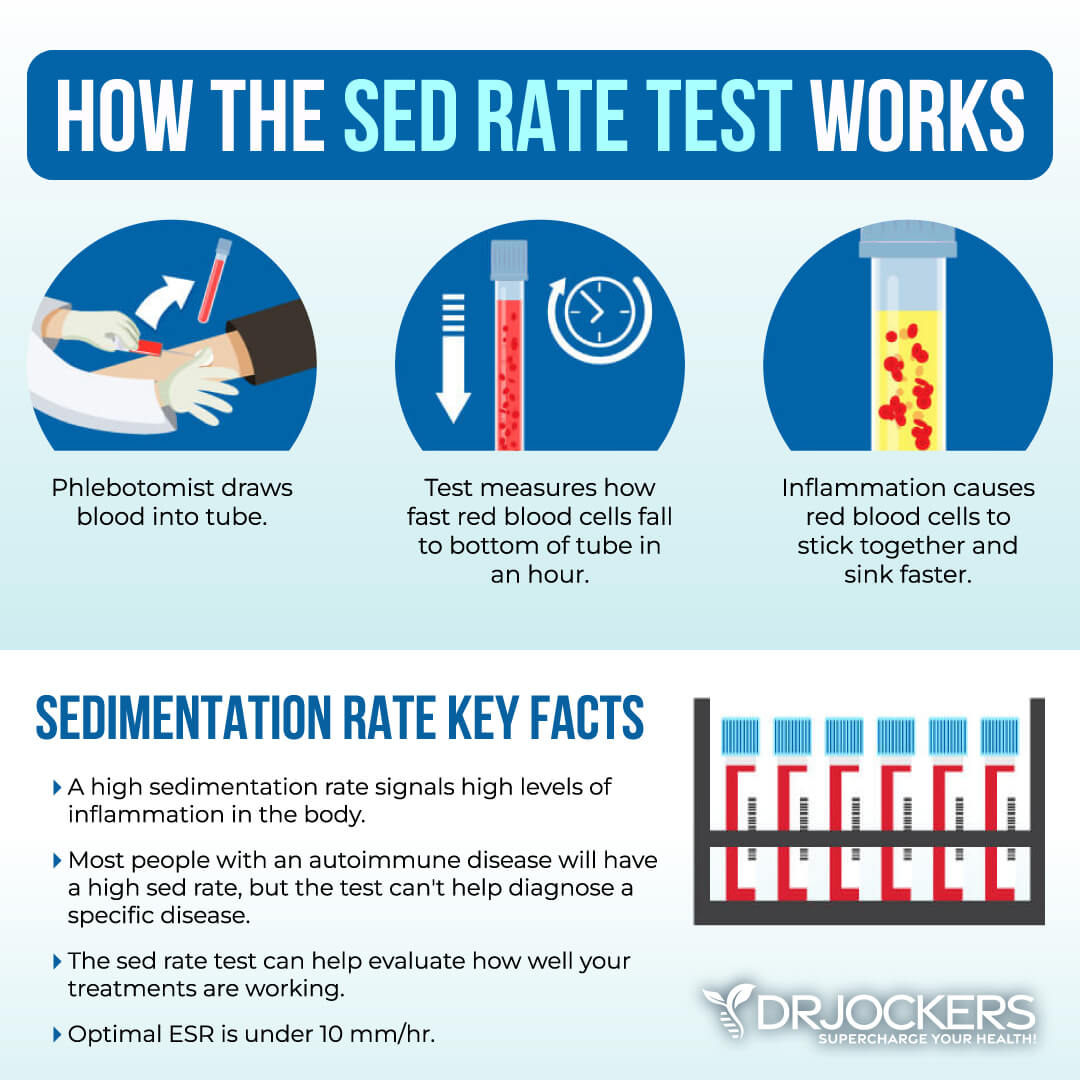
ESR and Platelets
The erythrocyte sedimentation rate (ESR) is a common hematology test to look for inflammation It refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Anything over 20 mm/hr is a sign of significant inflammation, and optimal results should be under 10 mm/hr.
You can also look at platelets as a measurement tool for inflammation and the stickiness of blood. Platelets elevated above 250 are a sign of inflammation. The sweet spot for platelets is between 175 and 250. Below 175, immune function and blood clotting are compromised; the same is true for levels above 250.
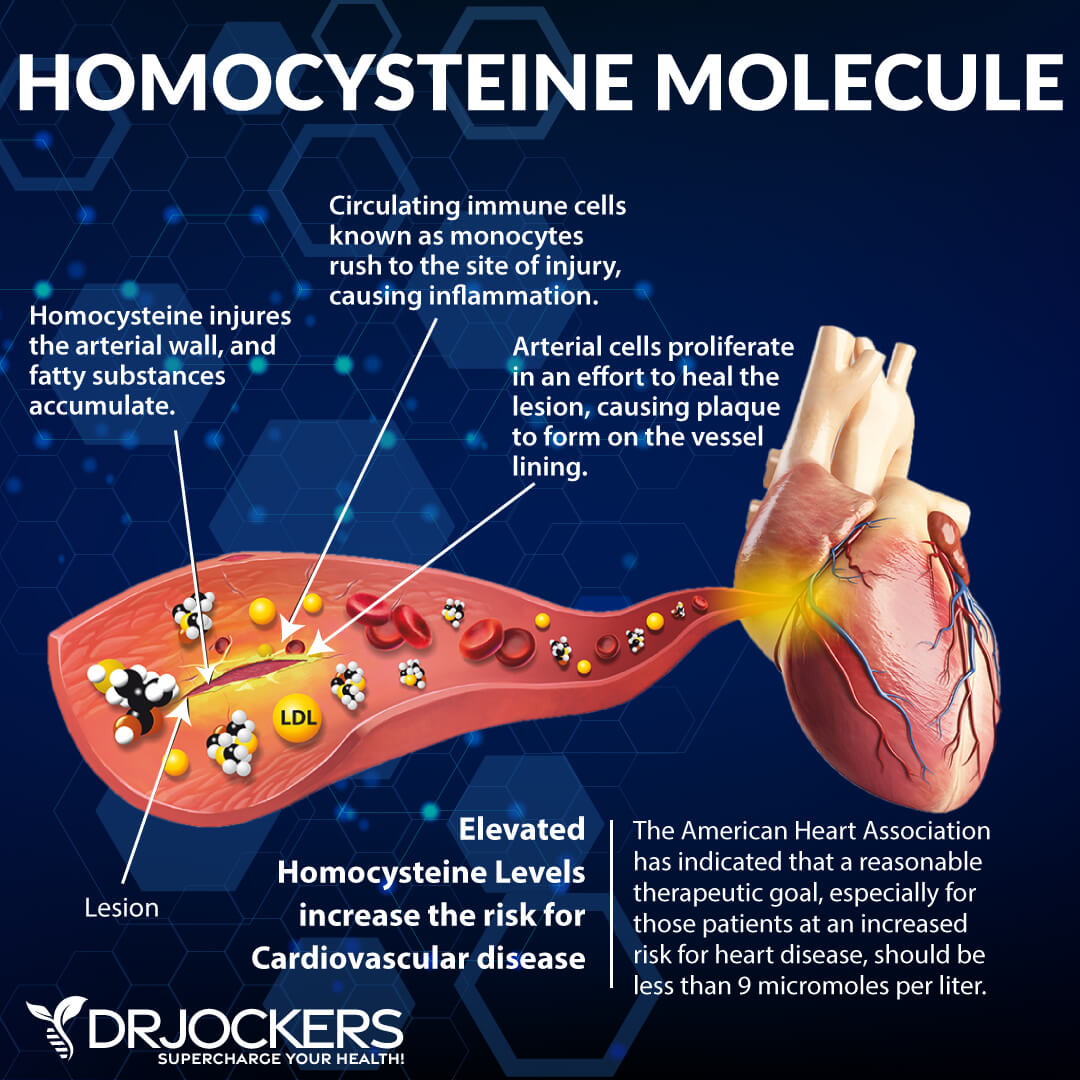
Homocysteine Levels
Homocysteine is a common amino acid in your blood that you mostly get from eating meat. Homocysteine is particularly a good marker for cardiovascular issues.
The optimal range for homocysteine is between 6 and 9 umol/L. Some practitioners like to see it under 8 umol/L.
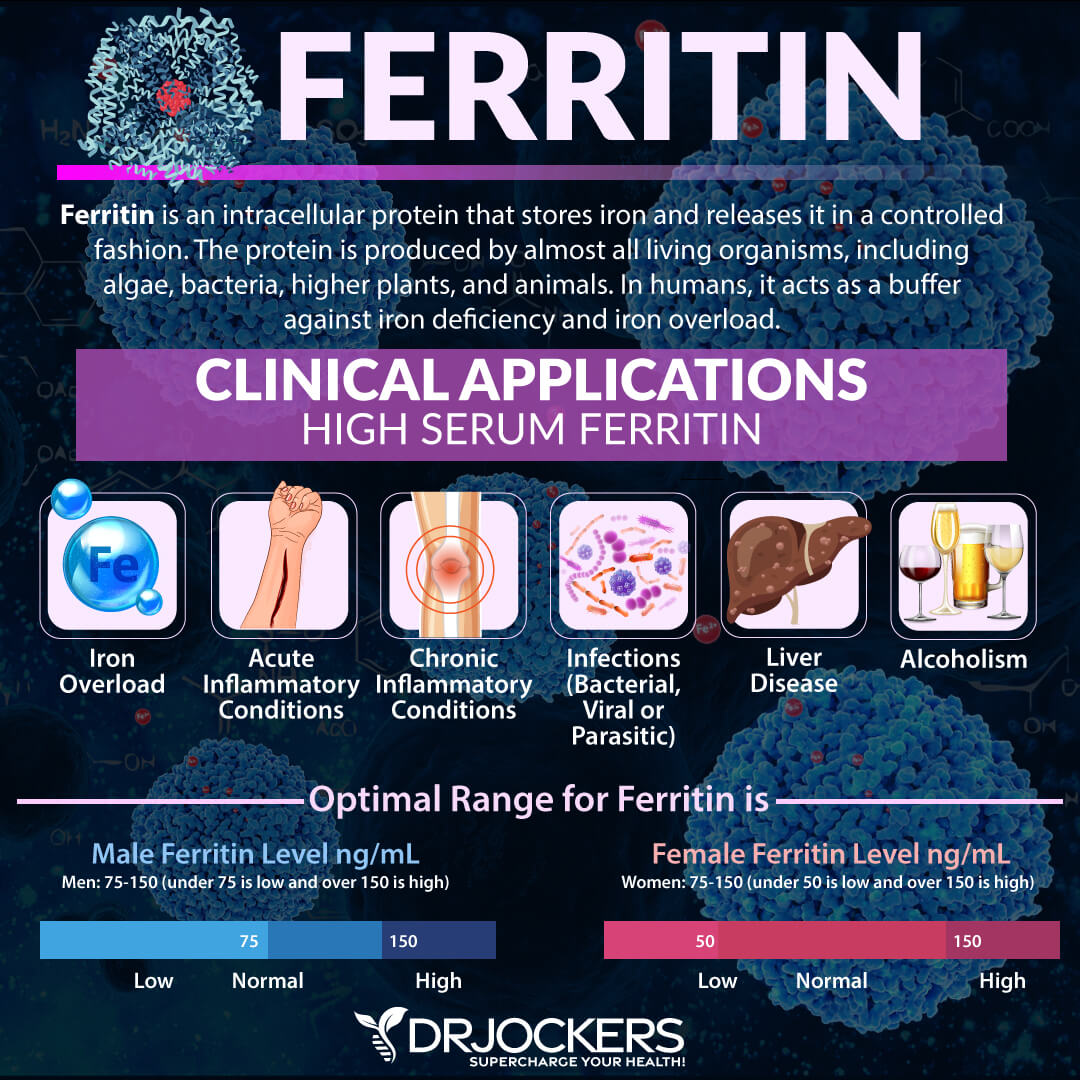
Serum Ferritin
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer.
The optimal range is 30 to 400, and the optimal range is 50 to 150 for females and 75 to 150 for males. High ferritin levels can be a risk factor for the accumulation of beta amyloid in the brain.
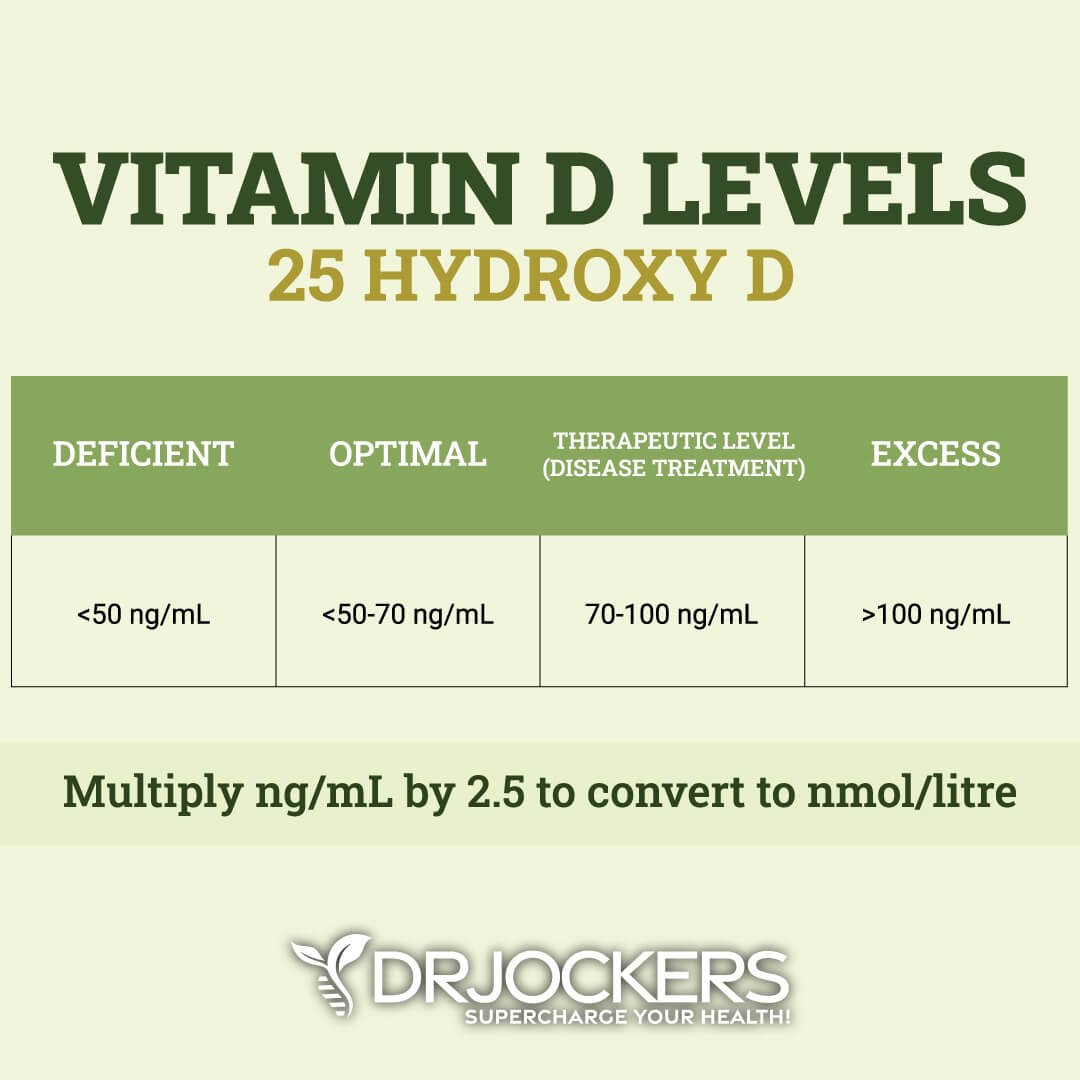
Vitamin D Levels
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation and are associated with higher levels of beta amyloid.
Optimal healthy levels of vitamin D are between 50 ng/mL and 70 ng/mL, while therapeutic levels are over 70 ng/mL up to 100 ng/mL.
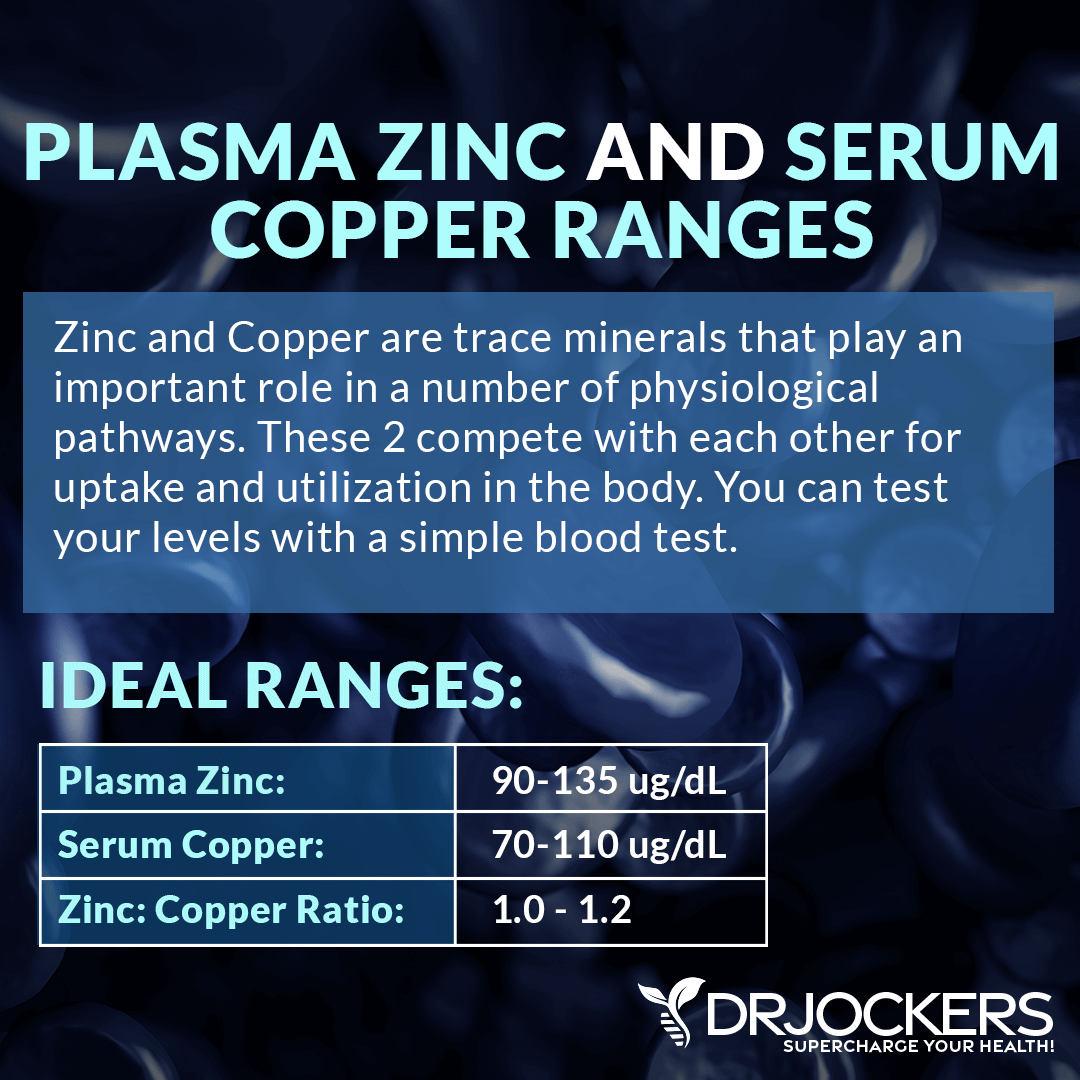
Copper: Zinc Ratio
Zinc and copper compete against one another as antagonists in order to properly regulate the physiological pathways in your body. The proper balance between the two trace minerals is critical to maintaining health.
Unlike zinc, copper can readily accumulate in the body in toxic concentrations. To maintain adequate zinc levels, a higher dose of zinc compared to copper is required daily. Zinc is only stored for short durations in the blood and bone and is quickly excreted through our urine and fecal matter.
Ideally, the proper intake of copper to zinc should be a 1:8 ratio. Fortunately, the foods that are high in zinc, such as meat, seafood, nuts and pumpkin seeds, are also very high in copper so you get both of these together in your diet.
We test plasma zinc and serum copper levels, and the ideal ratio is roughly 1-1.2, meaning you should have equal or slightly higher levels of plasma zinc than you have serum copper.
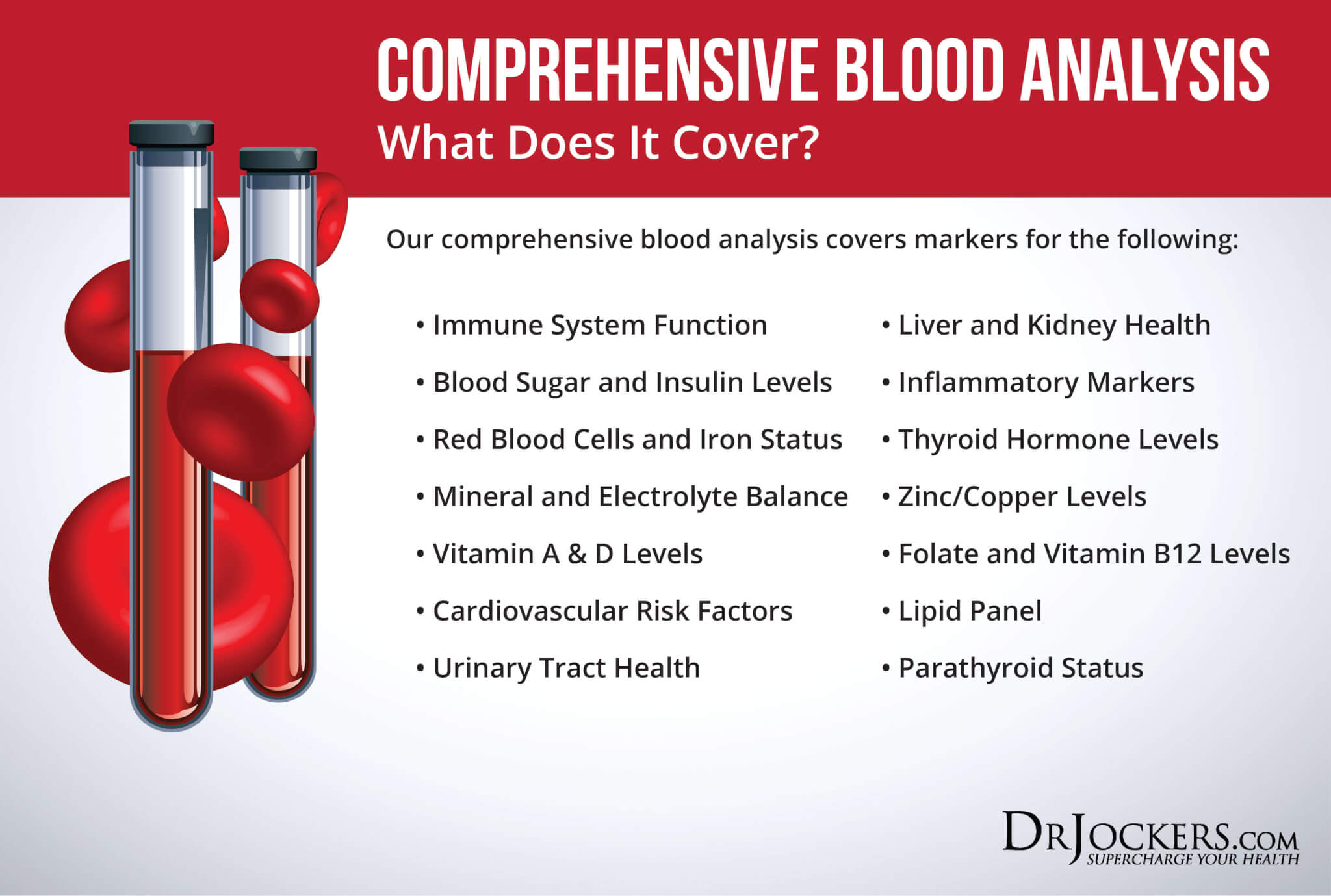
Comprehensive Blood Analysis
To receive a functional blood analysis and look at the optimal ranges of these markers, I recommend and regularly use a Comprehensive Blood Analysis (CBA), which is a very detailed blood test that looks at all of these markers of inflammation and other health functions.
This test is more sophisticated than most conventional doctors run. It looks at everything that a CBC and CMP do and more. It examines all parameters for inflammation, blood sugar levels, insulin levels, immune system function, thyroid function, parathyroid hormone levels, mineral and electrolyte balance, zinc and copper ratio, vitamin A and D levels, folate and vitamin B12 levels, a complete metabolic panel, complete blood count, liver function, kidney function, urinary tract health, nutrient deficiencies, and more.
I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your inflammation levels and progress if you are on a treatment plan. Remember, our team is always happy to help you understand your results and create a personalized treatment protocol to regain your health and well-being naturally.
Natural Strategies to Support Brain Health
Fortunately, you can support your brain health and reduce your risk of brain health issues with the help of some dietary and lifestyle strategies and the right supplementations. Here are the natural strategies I recommend supporting your brain health:
Anti-Inflammatory Nutrition Plan
Following an inflammatory diet is one of the major risk factors of chronic inflammation and consequent health issues. A 2018 study published in Alzheimer’s & Dementia (NY) has found a link between diet and Alzheimer’s disease (30). They found that this association may be due to the relationship between diet and beta amyloid.
They looked at 115 older female participants of an average age of 70 and examined their dietary patterns and beta amyloid deposition. They looked at four dietary patterns, including high-fat, low-fat, Mediterranean, and junk food diets. They found that eating too much junk food was a significant predictor of beta amyloid deposition and the risk of neurodegeneration and Alzheimer’s disease.
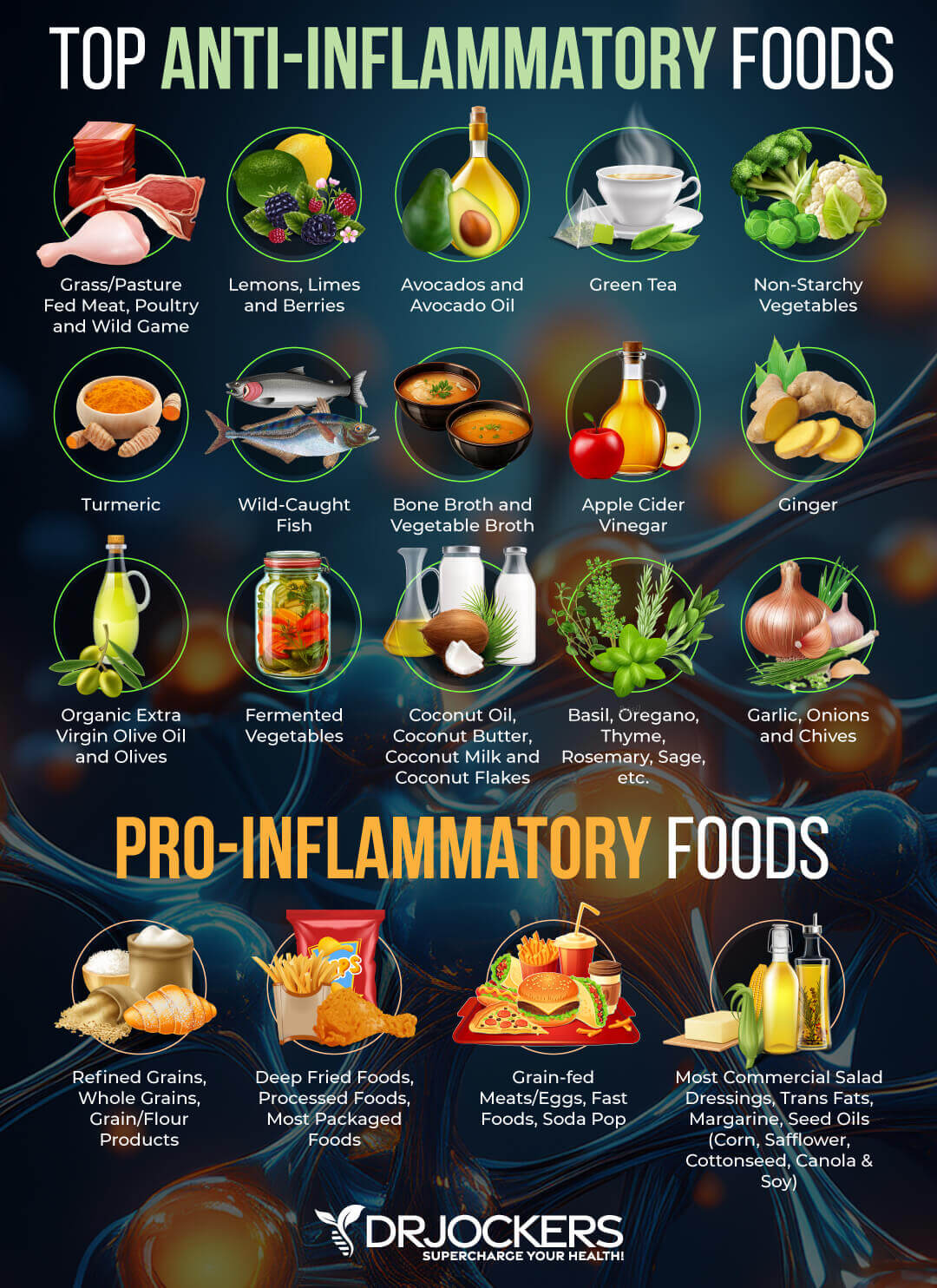
Following an anti-inflammatory diet rich in nutrient-dense foods may be one of the best things you can do for your brain health and to reduce your risk of neurodegeneration. First, eliminate all inflammatory foods, including refined sugar, gluten, refined oils, deep-fried and processed foods, conventional dairy, grain-fed meat and eggs, soda and sugary drinks, and foods that you are sensitive to.
Instead, I recommend eating an anti-inflammatory diet and loading up on greens, vegetables, low glycemic index fruits, herbs, spices, healthy fats, grass-fed meat, and wild-caught fish. To learn more about an anti-inflammatory diet, read this article as well.
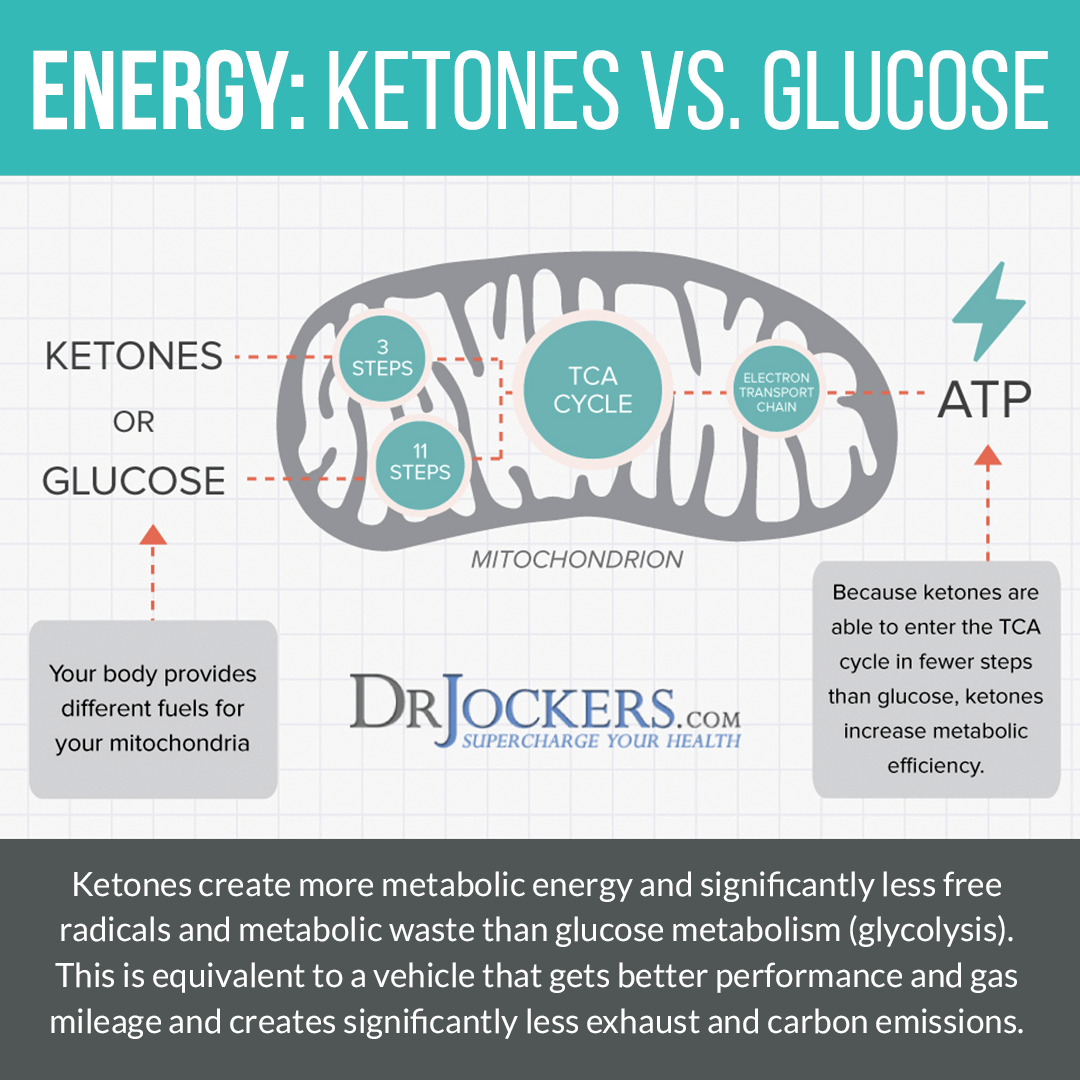
Get Into Ketosis
Most people eat a diet that is heavy or moderate in carbohydrates. Their body relies on glucose from dietary carbs to create energy. However, when your body doesn’t receive enough glucose because of a high-fat diet or fasting, it turns to dietary or stored body fat for energy.
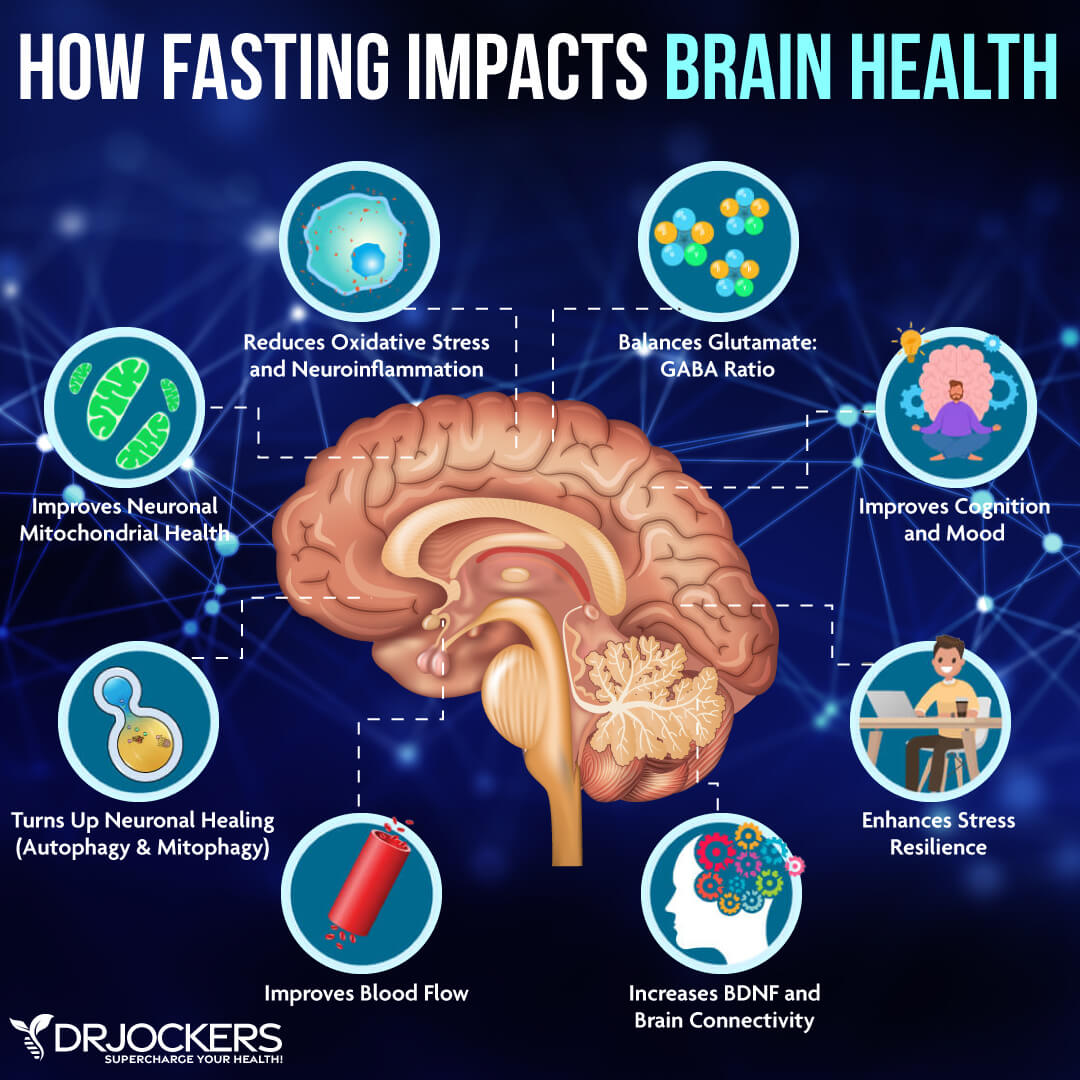
When this happens, fats get converted in the liver into ketones that enter your mitochondria inside your cells and then get turned into energy. The benefits of ketosis include reducing neuroinflammation and chronic inflammation, improved glutamate/GABA ratio, improved brain health, improved autophagy, and better mental sharpness.
A 2019 study published in Nutrition has found that the ketogenic diet may help to reduce the risk or improve Alzheimer’s disease (31). This may happen because a ketogenic diet may help to reduce beta amyloid plaques. A 2021 review published in the Journal of Geriatric Psychiatry and Neurology has also found that the ketogenic diet may be beneficial for dementia and Alzheimer’s disease as it may help to reduce neuroinflammation and delay cognitive decline (32). Ketosis may help to improve the glutamate/GABA ratio in the brain, which may help to improve neurotransmission.
The ketogenic diet is one of the best ways to achieve ketosis. The ketogenic diet is a very low-carb, high-fat, and moderate-protein diet. I recommend focusing on nutrient-dense foods with lots of micronutrients instead of only focusing on your macros. I recommend that you eat plenty of healthy fats, including avocados, avocado oil, coconut oil, coconut butter, coconut milk, olives, extra virgin olive oil, organic butter and ghee, seeds, and fatty fish and meat.
Another great option is intermittent fasting, I will discuss it later in this article. The easiest and best way to achieve ketosis is through the combination of the keto diet and intermittent fasting. To learn more about ketosis, I recommend reading this article, and to learn more about the keto diet, I recommend this one.
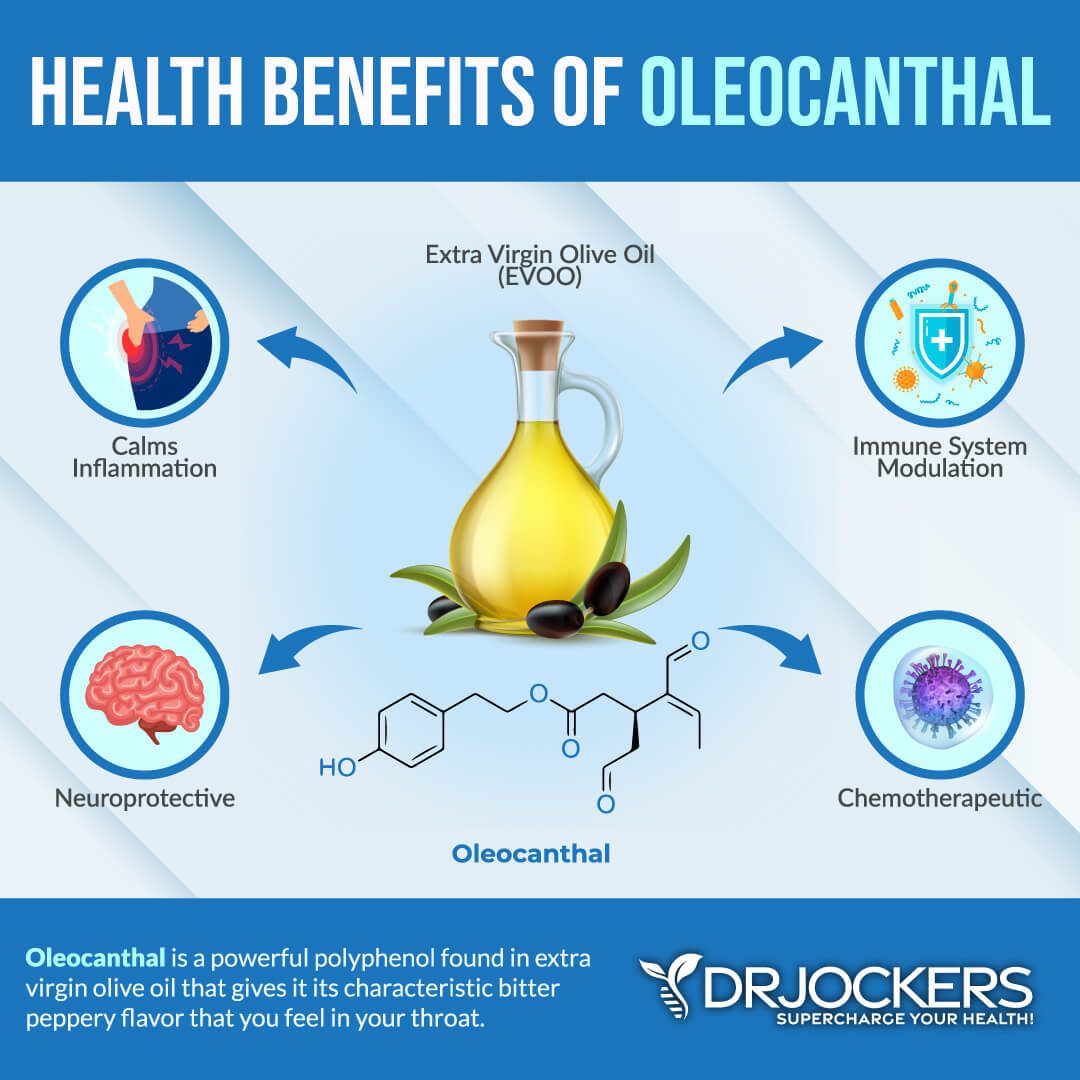
Use High Polyphenol Extra Virgin Olive Oil
Extra virgin olive oil is one of the best oils and healthy fats out there. It offers anti-inflammatory benefits. It may help to reduce inflammation, support health, aid weight loss, improve insulin sensitivity, support brain health, boost immune health, offer anti-aging effects, and support a healthy mood, among other health benefits. Research has shown that it may help to improve beta amyloid levels and offer neuroprotection.
A 2013 review published in ACS Chemistry and Neurosciences has found that oleocanthal from olive oil may help to clear beta amyloids and offer neuroprotective benefits reducing the risk of Alzheimer’s disease (33). A 2015 animal study published in The Journal of Nutritional Biochemistry has also found that extra virgin olive oil may help reduce beta amyloid and tau accumulation and brain pathologies (34). You may learn more about olive oil and the Fresh-Pressed Olive Oil I recommend from this article.
Intermittent Fasting
As I mentioned earlier, intermittent fasting is a great way to achieve ketosis. Intermittent fasting is a form of fasting cycle between not eating (fasting) and eating (feasting) over a period of time. The benefits of intermittent fasting include cellular repair, autophagy, immune regulation, inflammation levels, and insulin sensitivity.
It also helps to lower the risk of chronic diseases, including neurodegenerative conditions, such as dementia and Alzheimer’s. A 2020 review published in Nutrients has found that intermittent fasting may help to reduce beta amyloid buildup and the risk of Alzheimer’s disease (35).
If you are new to intermittent fasting, I recommend starting with a 12-hour fast. Stop eating after 7 PM or dinner, and don’t eat until breakfast the next day at 7 am. Increase your fasting window gradually by pushing breakfast to a later time and/or eating dinner earlier. Most people do their best with a 16-hour fasting window, but listen to your body and see what makes you feel your best. To learn more about the benefits of intermittent fasting and best intermittent fasting practices, I recommend this article.
Prioritize Good Sleep
Sleep is necessary for rest, repair, and cellular rejuvenation. This means that sleep allows your brain cells to regenerate and brain health to improve. As you know, poor sleep can increase the risk of chronic inflammation, beta amyloid buildup, and neurodegeneration (18, 19, 20). According to a 2020 study published in Current Biology, not sleeping enough can change beta amyloid levels in the brain (19).
To improve your sleep, avoid sugar and caffeine throughout the day, especially in the evening. Avoid late-night eating. Reduce your stress levels and turn off electronics several hours before bedtime. Wind down using relaxing activities, such as reading, crossword puzzles, healing baths, journaling, meditation, and prayer. Support your sleep with a comfortable bed, mattress, bedding, pillows, black-out curtains, and a sleep mask.

Regular Movement and Exercise
Regular movement and exercise help to support your brain health in a powerful way. According to a 2020 review published in the International Journal of Molecular Sciences, there is a link between skeletal muscle decline and cognitive decline (36). According to scientists, aging plays a role in both cognitive decline and a loss of skeletal muscle (sarcopenia). Studies found that physical inactivity, an unhealthy diet, smoking, and other lifestyle factors may contribute to both cognitive decline and muscle loss.
When looking at the link between exercise and brain health, we need to look at myokines, which are cytokines that play an important role in skeletal muscle health. Myokines are synthesized and released by myocytes, the smallest subunit of your muscle tissues, during muscle contractions.
According to a 2021 review published in Neuropharmacology, myokines help improve brain health (37). Myokines are made up of signaling proteins, which are responsible for a variety of physiological and metabolic mechanisms, including brain function.
Physical exercise and muscle-borne signals cause myokine release, which may play a critical role in brain physiology. Myokines may help to control memory, learning, mood, and other brain functions. Further investigating and understanding the link between skeletal muscle and the brain may help to develop therapeutic strategies to reduce the risk of brain degeneration and improve quality of life.
To support your brain health, I recommend moving your body and exercising regularly. You can read this article to learn more about how to build muscle to support your brain and overall health.

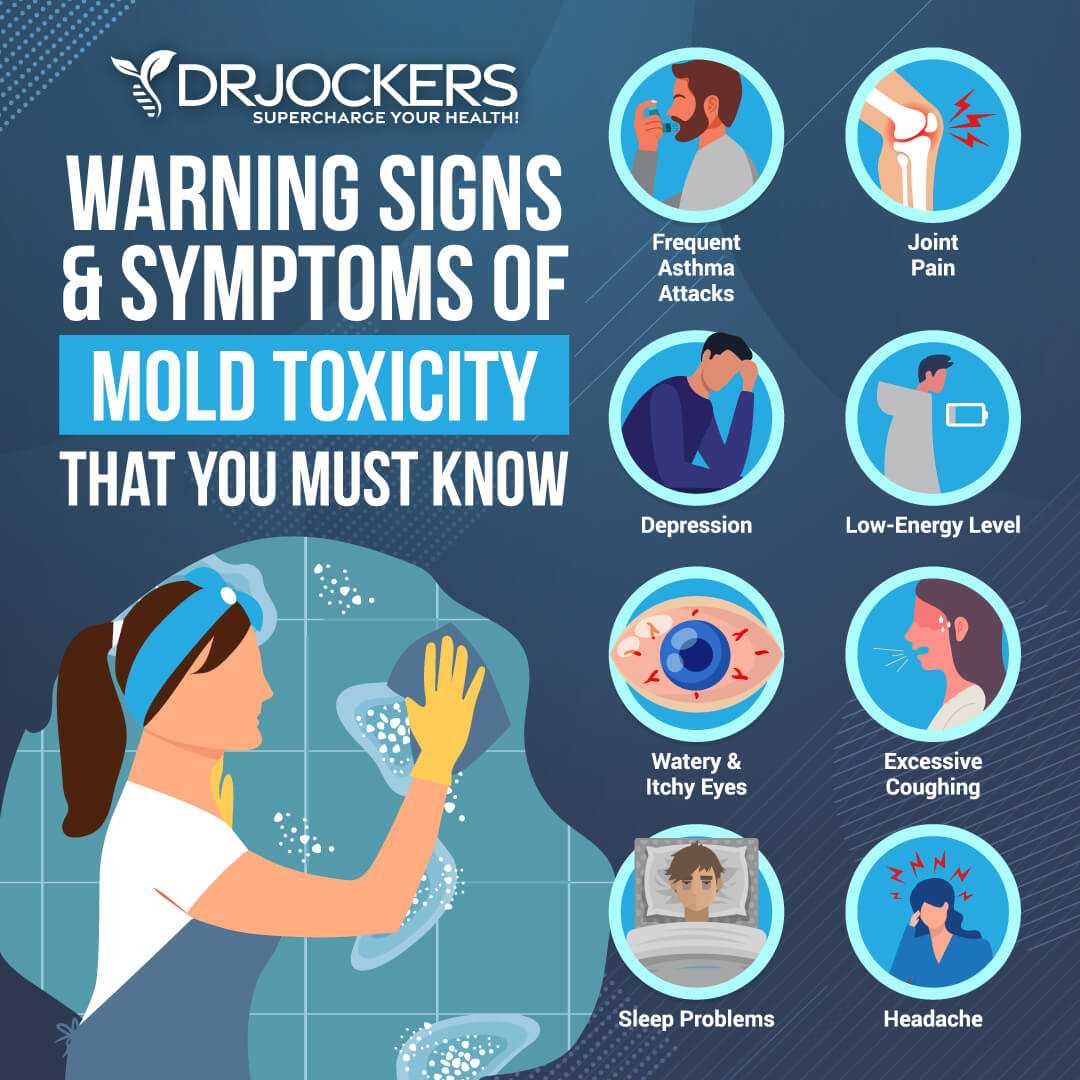
Reduce Mold Exposure & Improve Air Quality
I discussed earlier how mold mycotoxins and environmental toxins may increase the risk of beta amyloid buildup and neurodegeneration (23). For example, according to a 2021 study published in Toxins (Basel), mycotoxins may play a role in Alzheimer’s disease (24). Reducing mold exposure and improving your air quality is critical.
I recommend that you start by checking your home for mold. Mold loves to hide in your bathroom, basement, behind wallpaper, behind paint, under carpeting, and in areas of water damage. You can ask for professional help to check for mold or use an at-home kit. If you have mold, get it professionally removed. Address any underlying issues, such as leakage, water damage, old wallpapers, and poor ventilation. Check and clean sensitive areas regularly.
Improve your indoor air quality with the help of a high-quality air filtration system. They can help to remove mold, mycotoxins, microbes, allergens, and toxins from your indoor air. I recommend the Air Doctor. You can learn more about it here. You may learn more about mold toxicity here.
Improve Oral Health
According to a 2018 review published in Frontiers in Aging Neuroscience, infections may play a role in Alzheimer’s disease (22). Oral infections are among the major underlying health issues that may increase your risk of brain health issues. A 2020 study published in the Journal of Alzheimer’s Disease has found that gum disease may increase beta amyloid plaques and the risk of dementia (38).
A 2020 study published in the International Journal of Environmental Research and Public Health has found that taking care of their oral health can be difficult for elderly people with Alzheimer’s disease (39). This may further contribute to their symptoms and progress of the disease.
I recommend improving your oral care. Brush your teeth at least twice a day and floss regularly. Use fluoride-free, herbal, organic products. Try oil pulling with coconut oil every morning. Visit a holistic dentist to take care of any cavities and oral health issues using holistic principles and natural care options. You can learn more about holistic oral care here.
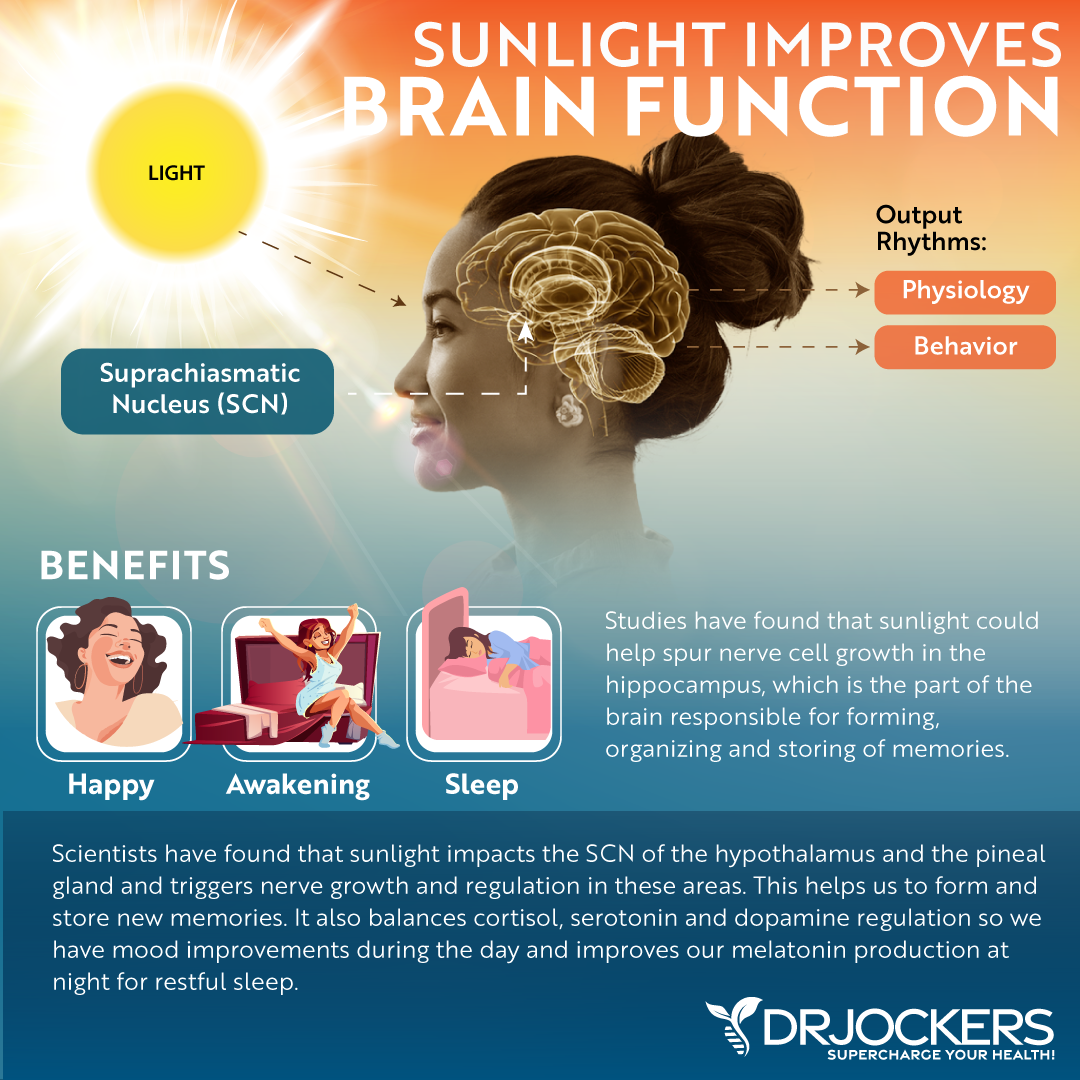
Optimize Vitamin D Levels
Vitamin D deficiency is one of the major underlying risk factors for beta amyloid buildup and Alzheimer’s disease (25). Improving your vitamin D levels may help. A 2017 study published in the International Journal of Molecular Sciences has found that vitamin D supplementation may help to reduce beta amyloid plaque formation and improve beta amyloid degradation (40).
Spending time outside in the sun daily is important for optimal vitamin D levels. Eating foods rich in vitamin D, such as cod liver oil, fatty fish, and beef liver, can help too. However, vitamin D supplementation is essential for all of us for optimal levels.
Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2. I highly recommend this Vitamin D3/K2 Power. Both of these supplements support your immune, skin, cardiovascular, and bone health.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
Use Magnesium
Magnesium deficiency is another common nutrient deficiency that may contribute to beta amyloid buildup (28). According to a 2010 study published in the Journal of Alzheimer’s Disease, magnesium may help to modulate beta amyloid and prevent buildup (41).
A 2022 study published in the World Journal of Psychiatry has found that magnesium L-threonate specifically may be particularly beneficial for neuroprotection, reducing oxidative stress damage, and reducing the risk of Alzheimer’s disease (42). I recommend using Brain Calm Magnesium daily which contains magnesium L-threonate.
Optimize Folate and B12 Levels
Vitamin B12 and folate deficiencies are also common causes of beta amyloid buildup and neurodegeneration (26, 27). According to a 2021 study published in Cell Reports, vitamin B12 may help to reduce beta amyloid-related proteotoxicity (43).
A 2015 study published in the International Journal of Molecular Sciences has found that folate may help to stop beta amyloid production (44). I recommend taking B12 Power for vitamin B12 and B Strong for folate and other B vitamins.
Consider Zinc and Omega-3 Fatty Acids
Zinc deficiency is another underlying root cause of beta amyloid buildup and neurodegeneration (29). According to a 2021 study published in the Journal of Neuroscience, zinc may help to reduce the progression of Alzheimer’s disease (45). To improve your zinc levels, I recommend Zinc Charge.
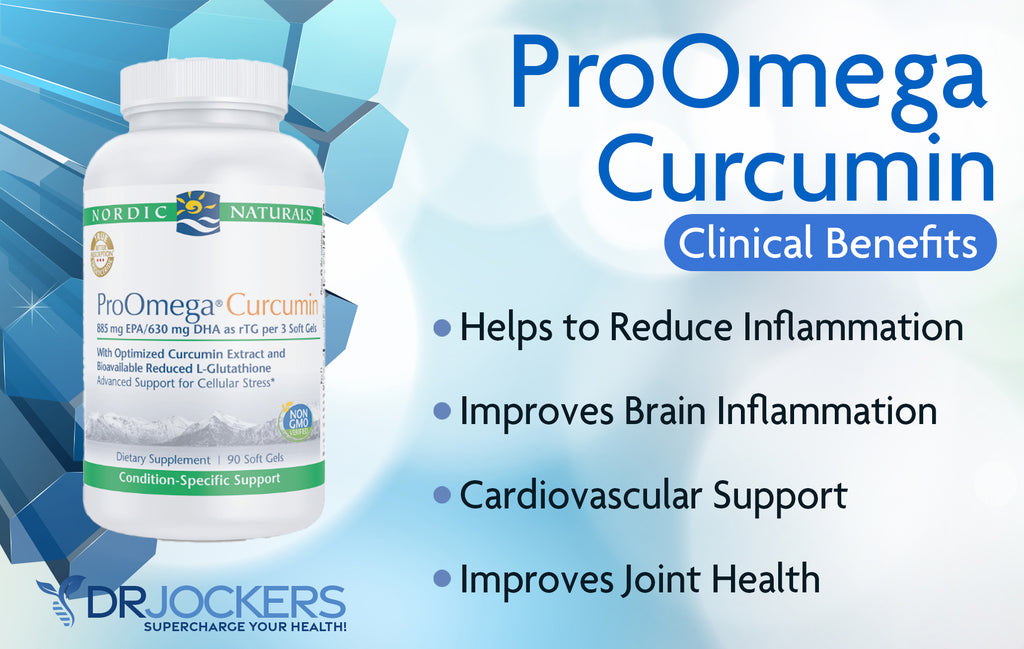
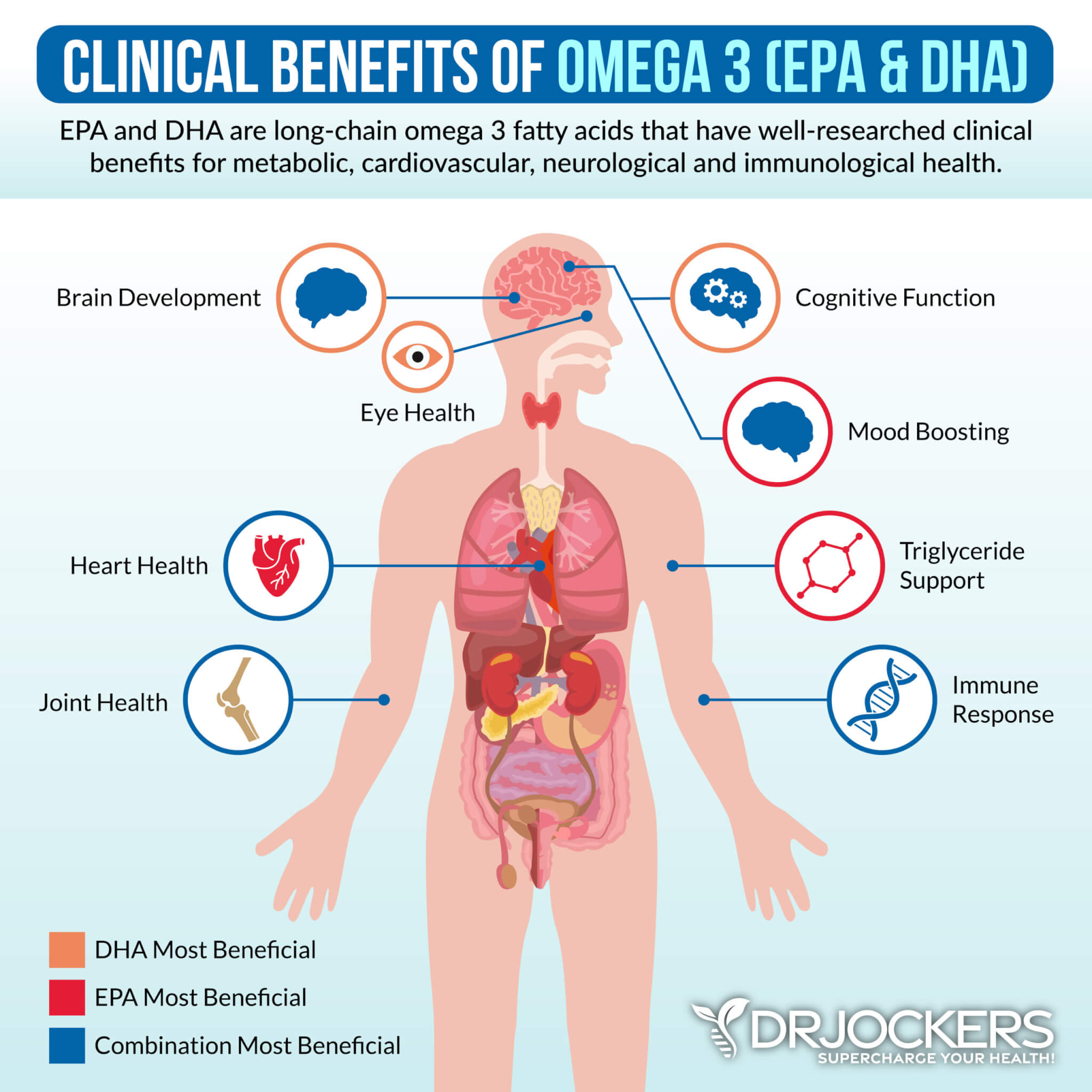
Omega-3 fatty acids are essential fatty acids that help to reduce inflammation and support brain health. The key long-chain omega-3 fatty acids are EPA and DHA, which have clinically significant benefits for brain health.
A 2016 study published in the FASEB Journal has found that omega-3 fatty acids may help beta amyloid clearance (46). A 2020 study published in Brain, Behavior, and Immunity has also found that omega-3 fatty acids support the brain-to-blood clearance of beta-amyloid and may reduce the risk of Alzheimer’s disease (47). To improve your omega-3 levels, I recommend Pro Omega Curcumin.
Consider NAC and Curcumin
To reduce inflammation and protect your brain health, you may also consider N-Acetylcysteine (NAC) and curcumin. NAC is a powerful antioxidant and is also a precursor of L-cysteine that helps glutathione elevation biosynthesis. A 2021 study published in Science Reports has found that NAC may help to prevent beta amyloid secretion (48).
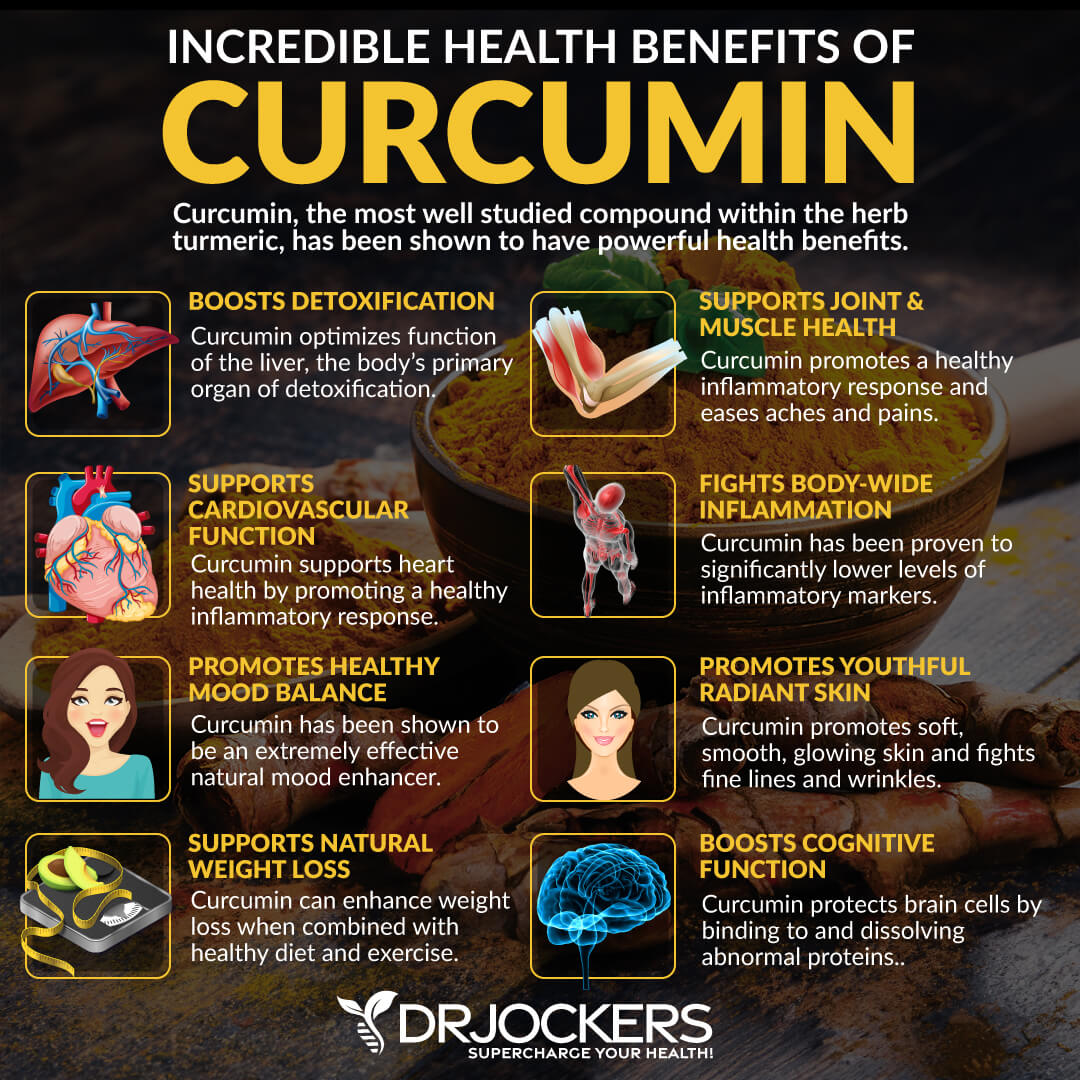
Curcumin is the active compound of the anti-inflammatory spice, turmeric. A 2018 study published in the Journal of Alzheimer’s Disease has found that curcumin may prevent beta amyloid aggregation and may offer neuroprotective benefits (49).
A 2020 study published in the Journal of Chemical Information and Modeling has found that curcumin may help to prevent beta amyloid formation and reduce neurodegeneration (50). In the next section, I will share my favorite supplement for NAC, curcumin, and omega-3 fatty acids.
Pro Omega CRP
To benefit from omega-3 fatty acids, NAC, and curcumin and to improve your brain health, I recommend Pro Omega Curcumin. This supplement offers a powerful new solution for systemic cellular stress. This unique formulation combines concentrated omega-3s plus optimized curcumin and the potent antioxidants L-Glutathione and N-Acetylcysteine (NAC) to achieve complete functional support for long-term health.
This combination of nutrients synergizes to impact all the major inflammatory pathways while strengthening both the inside cellular mechanics and the outer cell membrane. The omega 3’s and curcumin help to reduce inflammation on the outer cell membrane. The L-glutathione and N-Acetyl Cysteine help to balance the immune system and protect the mitochondria and DNA. I recommend taking 3 capsules once a day with food or, for advanced dose 3 to 6 capsules twice a day with food.
Brain Regeneration Guide:
If you have struggled with your mood, memory or had trouble concentrating…we have good news!
In the last 10 years, there has been several amazing breakthroughs in neuroscience that are showing that we can actually heal and regenerate our brain cells and improve our neurological health with healthy lifestyle practices.
There are scientifically validated strategies to improve your mood, memory and cognition no matter how old you may be! You can get immediate access to this life changing science and strategies today in the Brain Regeneration guide!
—>Download the Brain Regeneration Guide Today!
Final Thoughts
Alzheimer’s disease is a progressive disease and is the most common form of dementia. Beta amyloid plaques are the main cause of Alzheimer’s disease. Preventing beta amyloid plaque formation may be key for your brain health.
To improve your brain health and reduce your risk factors for neurodegeneration, I recommend following my top natural support strategies for brain health. If you want further help with your health, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!
Sources in This Article Include: