 Hiatal Hernia: Symptoms, Causes and Natural Support Strategies
Hiatal Hernia: Symptoms, Causes and Natural Support Strategies
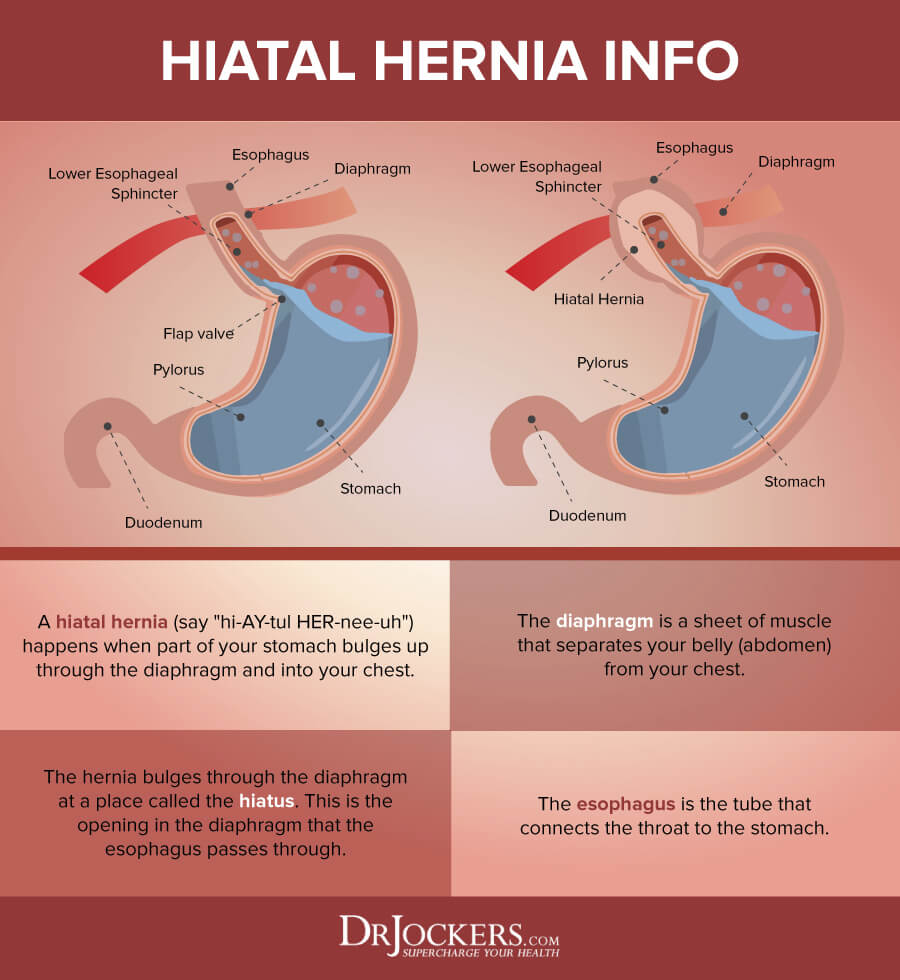
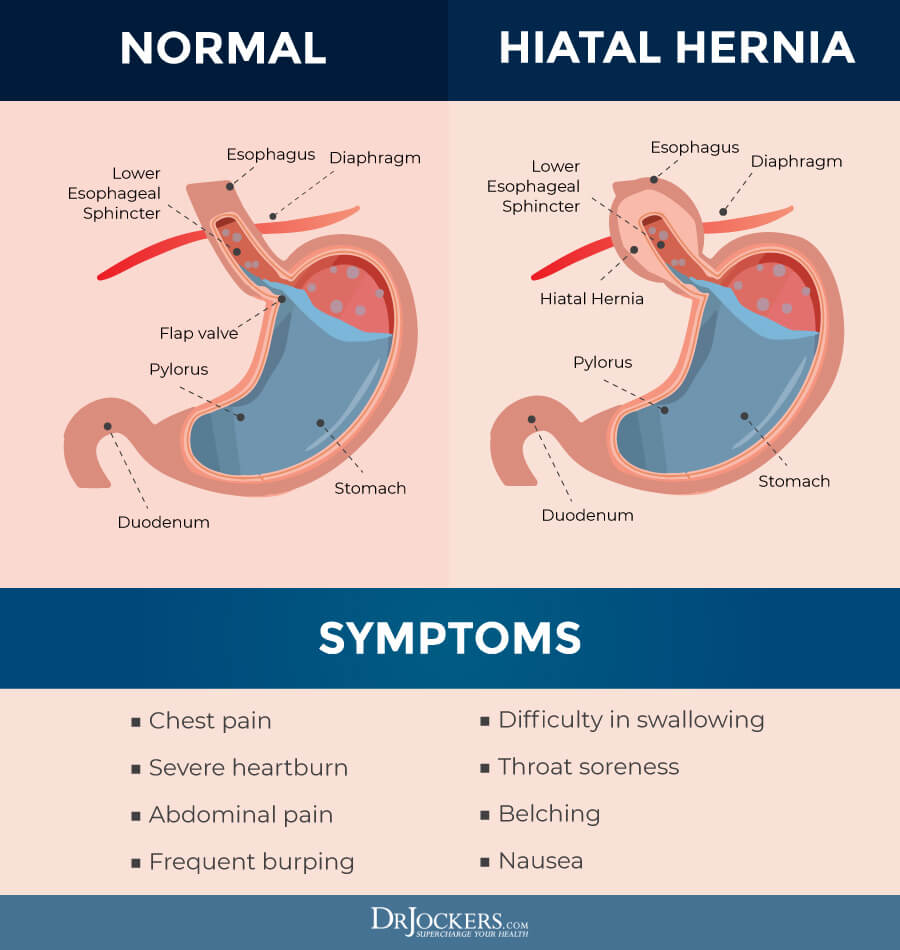
Any time an internal body part pushes into an area it doesn’t belong it’s called a hernia. A hiatal hernia forms inside the diaphragm, the muscular area between the chest and the lower abdomen. What develops is a bulging of the upper part of the stomach through a tear or a weakness in the diaphragm. Hiatus hernia, as it is commonly called, is the most common type of diaphragmatic hernia. It is estimated that up to 60 percent of adults have a hiatal hernia. Although studies show more than half of adults over age 50 have a hiatal hernia, many never have symptoms (1).
In people with a hiatal hernia, a portion of the stomach pushes up through the muscle. The opening it moves through is called the hiatus. The hiatus is part of the digestive system that connects the stomach to the esophagus (2). The esophagus normally goes through the hiatus and attaches to the stomach.
Types of Hiatal Hernia
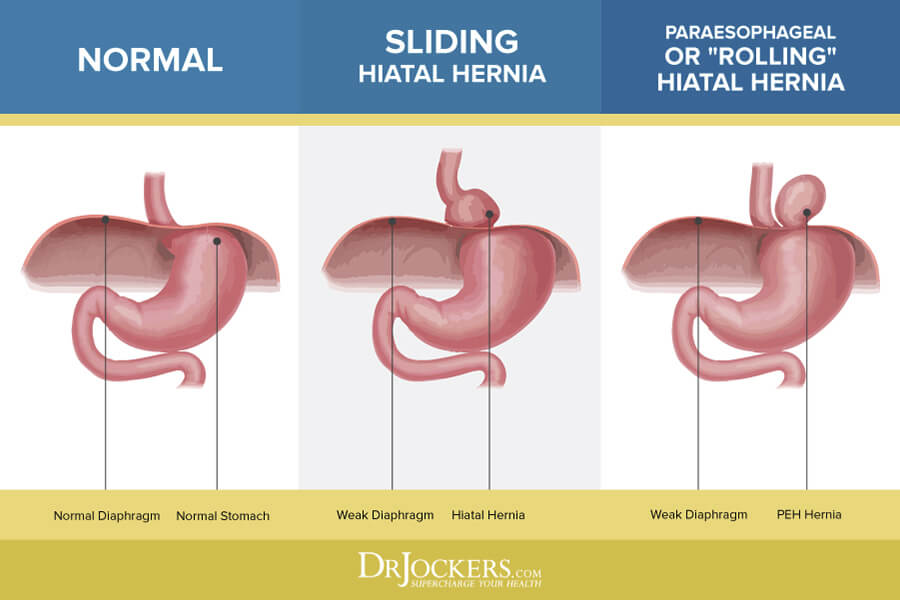
There are two main types of hiatal hernias, sliding and paraoesophageal hernias. In a sliding hiatal hernia, the stomach and the portion of the esophagus that joins the stomach slides up into the chest through the hiatus (3). A paraoesophageal hernia is less common, yet there is more cause for concern.
Although the esophagus and the stomach stay in their normal locations, part of the stomach squeezes through the hiatus, situating itself next to the esophagus. A paraoesophageal hernia can display no symptoms, the danger is that the stomach can become “strangled,” or have its blood supply cut off.
Hiatal Hernia Causes
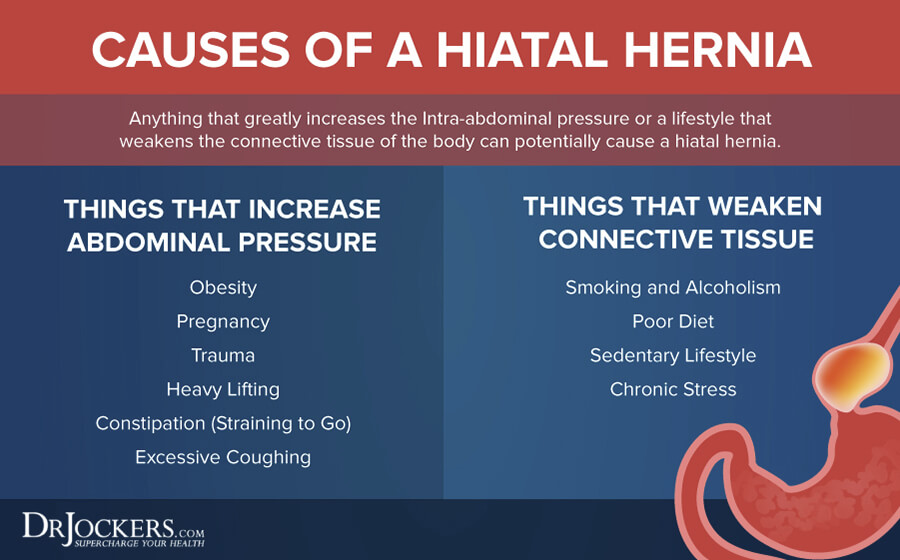
The abdomen consists of the lower part of the esophagus, stomach, small intestine, colon, rectum, liver, gallbladder, pancreas, spleen, kidney, and bladder. If the abdomen experiences intense pressure, injury, straining or inflammation – then dysfunction can result. Sometimes the cause can be an injury or a birth defect. It may also have to do with weaknesses in surrounding muscles.
You are considered high risk if you smoke or are obese. In addition to the natural aging process, middle to older age women are diagnosed with a hiatal hernia more than any other group. This risk increases if you are overweight, obese, or pregnant. Finally, it may have to do with weakness in the surrounding muscles (4).
Dr. Carolyn Dean believes, “hiatal hernias are common because we have so many digestive problems leading to gas and bloating, which can push the stomach into a herniation. We are overweight, which pushes up on the stomach – and we don’t exercise, which means our diaphragm doesn’t move with deep breathing – which massages the stomach into place. And when we are under stress we hold our breath and breathe shallowly and therefore don’t properly massage our internal organs with the diaphragm. Then there is magnesium deficiency” (5).
Symptoms of Hiatal Hernia
A hiatal hernia sounds like a painful condition, considering the stomach pushes through an opening in the diaphragm and into the chest, but most people don’t notice any symptoms. It is frequently discovered when a person has a chest x-ray or abdominal x-rays (including upper GI series and CT scans where the patient swallows barium or another contrast material) (6). It can also be found when a gastrointestinal endoscopy of the esophagus, stomach, and duodenum is performed.
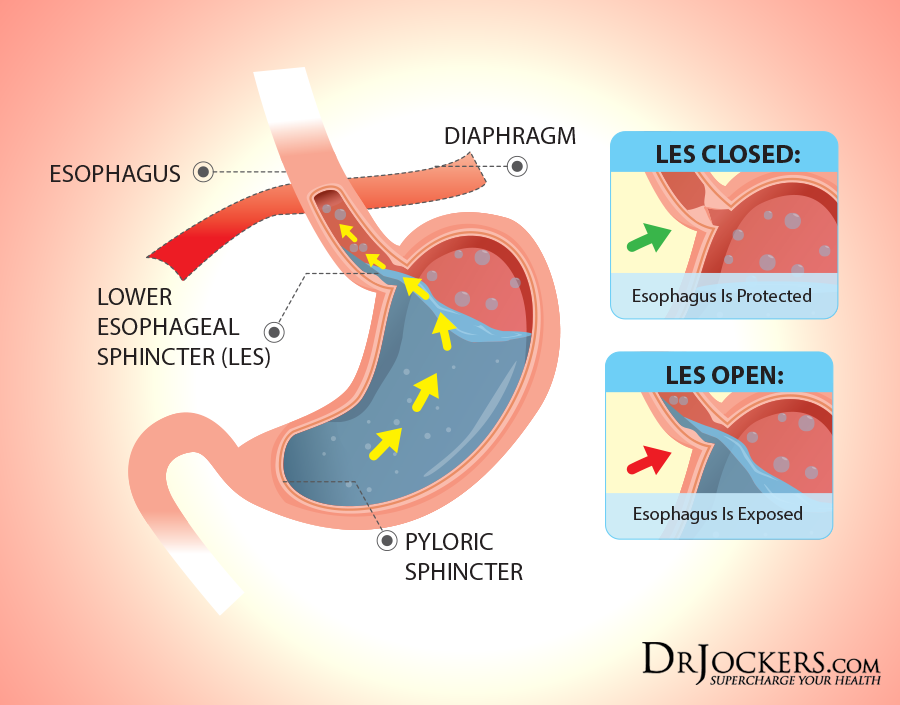
If you do experience symptoms they are usually caused by bile, stomach acid or air entering in through your esophagus (7). Many people with a hiatal hernia suffer from acid reflux, or heartburn, the hernia doesn’t seem to directly cause these symptoms. Unfortunately, whatever conditions contribute to acid reflux (inflammation and poor diet etc.) also contribute to hernias. When symptoms do occur, they can include symptoms of heartburn/acid reflux symptoms and a more serious condition referred to as gastroesophageal reflux disease (or GERD for short).
Of the different types of hernias, the sliding hiatal hernia is most closely associated with GERD (8). It is estimated that about 20 percent of adults experience these symptoms on a regular basis.
Symptoms of a Hiatal Hernia (Continued)
Symptoms of a hiatal hernia include chest pain, burning sensation, and irritation of the throat. Symptoms associated with acid reflux, heartburn and GERD are possible.
Symptoms associated with acid reflux include:
- Heartburn
- Bitter taste in your mouth –some people regurgitate food or sour liquid in the back of their throat
- Waking up feeling like your choking or coughing in the middle of the night
- Dry mouth
- Gum irritation-tenderness or bleeding
- Bad breath
- Bloating after meals
- Regurgitation of acidic meals
- Nausea
- The wearing away of your teeth
More Severe Symptoms Can Include:
- Gassiness, belching, burping, and flatulence after meals
- Hiccups that are difficult to stop
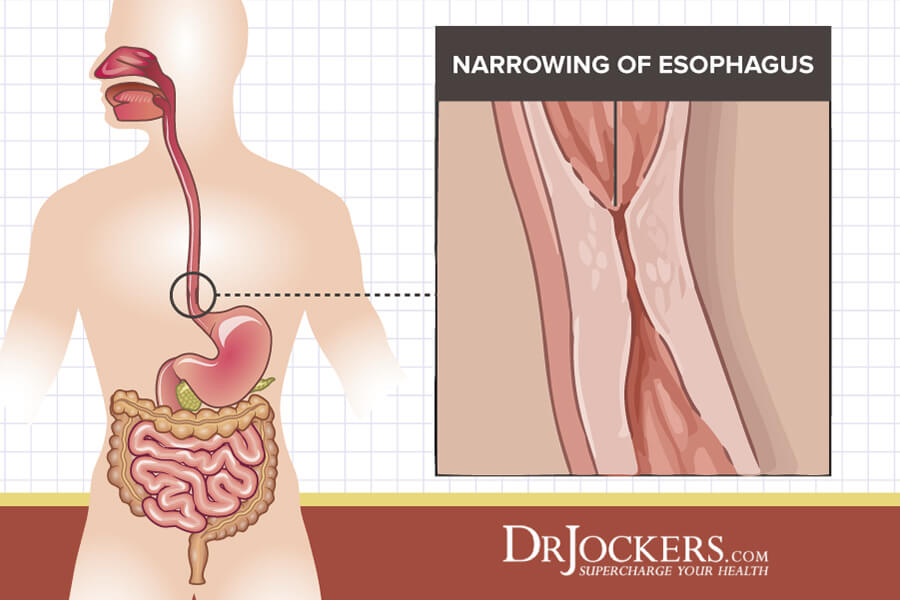
- Difficulty swallowing (potential narrowing of the esophagus)
- Bloody vomiting or black stools, (could indicate damage to the lining of the esophagus).
- Worsening discomfort lying down or bending
- Unexpected weight loss
- Hoarseness upon waking or throughout the day
- Sore, dry throat
- Throat irritation and chronic coughing
- Breathing problems
- GERD may lead to bleeding ulcers in the esophagus. In addition, it can lead to a serious condition called Barrett’s esophagus, which can lead to esophageal cancer.
Long-term Complications May Include:
Heartburn, acid reflux, and GERD are common occurrences surrounding a hiatal hernia.
Sliding hiatal hernias are closely related to reflux and GERD. Researchers believed for decades that a hiatal hernia and GERD were the same thing.
New information shows that although acid reflux and GERD have the same contributing factors that cause a hiatal hernia, they aren’t the same thing. Some of the many factors that contribute to both conditions include abnormal esophageal acid clearance, tissue resistance, delayed gastric emptying, abnormal gastric acid secretion, and other abnormalities of the lower esophageal sphincter. The relation between hiatal hernia and GERD is referred to as the “two- sphincter hypothesis” (9, 10).
If left untreated GERD can lead to serious problems including reflux esophagitis, Barrett’s and esophageal adenocarcinoma (cancer of the esophagus), esophageal ulcers or stricture and a strangulated hernia (11). Experts feel because of these risks, it is very important for doctors to evaluate whether a patient who has acid reflux symptoms also has a hiatal hernia and is more likely to experience GERD. The treatment of a hiatal hernia and GERD are similar; lifestyle and dietary changes that improve one will decrease the risk of occurrence.
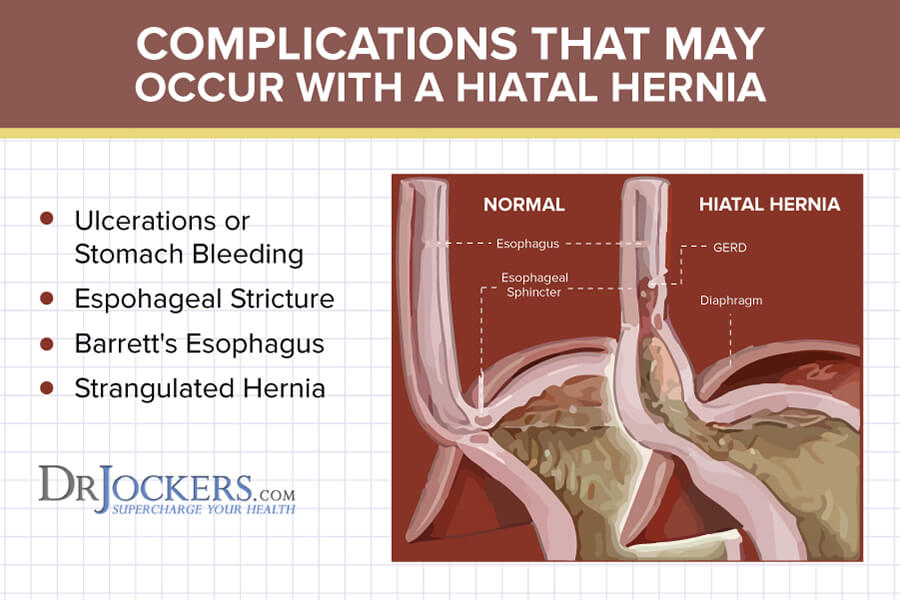
Ulcerations or Stomach Bleeding
Esophageal ulcers can occur due to the damage the stomach acid has on the lining of the esophagus which frequently leads to the formation of an ulcer. The ulcer may bleed, causing serious pain and difficulty in swallowing. Ulcers can be treated by implementing dietary changes, antacids, cholinolytics, and multivitamins (12).
Surgery may be necessary to control complications such as ulcerations, stomach bleeding, or strictures. When a lot of pressure is placed on the abdomen and digestive organs complications are likely to occur. Intra-abdominal pressure can be caused by abdominal straining and abdominal compression due to injury, chronic or strong coughing, or for any other reason that strain the tissues and the organs.
Esophageal Stricture
Continual damage to the lining of the esophagus will lead to scar tissue. If the tissue is not treated, scar tissue will build up and make the esophagus narrow. This condition is known as an esophageal stricture.
Barrett’s Esophagus
The continuous irritation of the esophagus by the stomach acid may lead to a change in the cells of the lower esophagus. This condition is known as Barrett’s esophagus.
Barrett’s esophagus doesn’t manifest any noticeable symptoms, but it increases the risk of esophageal cancer.
Strangulated Hernia
It is rare, but a hiatal hernia may cause a part of the stomach to push up into the esophagus. When this occurs the stomach acid doesn’t enter the esophagus, but it increases the risk of the hernia becoming strangulated. A strangulated hernia occurs when the blood supply to the herniated tissue has been cut off. The strangulated tissue can release toxins and infection into the bloodstream, which may lead to sepsis or death. Strangulated hernias are medical emergencies.
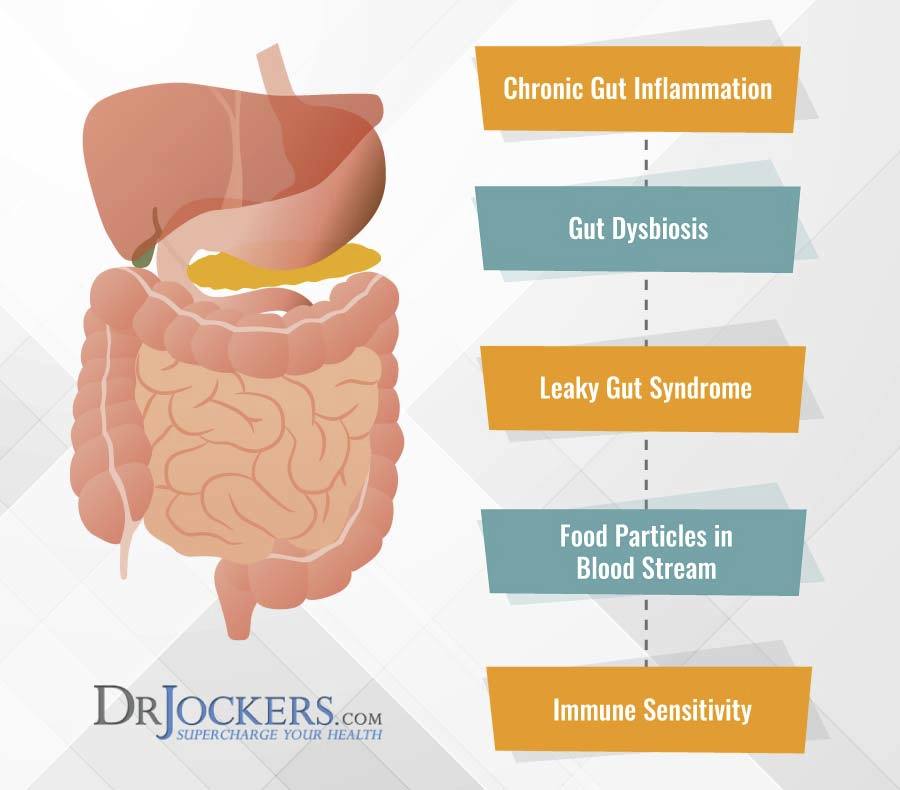
Inhibited Digestion
The primary digestive symptom of a hiatal hernia is indigestion. A proper diet and lifestyle can help reduce many digestive symptoms.
Medical doctors may recommend surgery for severe cases, but for many people, the hiatal hernia is treatable with conservative care. Hiatal hernias can persist for years and they are a contributing factor for other chronic problems. Digestion is the foundation of health, so it is very important to treat a hiatal hernia. Anything that interferes with our stomach and the function of our digestive system needs to heal, for us to enjoy life-long health.
Many chiropractor, massage therapist, physiotherapist, and integrative doctors are trained to work with hiatal hernias.
Atrial Fibrillation
A Hiatal hernia appears to be associated with an increased frequency of Atrial Fibrillation in both men and women of all age groups, but particularly in young patients. Having a hiatal hernia under the age of 55 increases your chance of having Atrial Fibrillation by up to 19% (13).
One of the function changes in Atrial Fibrillation is a trigger. Gastroesophageal reflux could be a trigger for this arrhythmia. It is believed that atrial fibrillation should be considered as a possible extraesophageal syndrome (14).
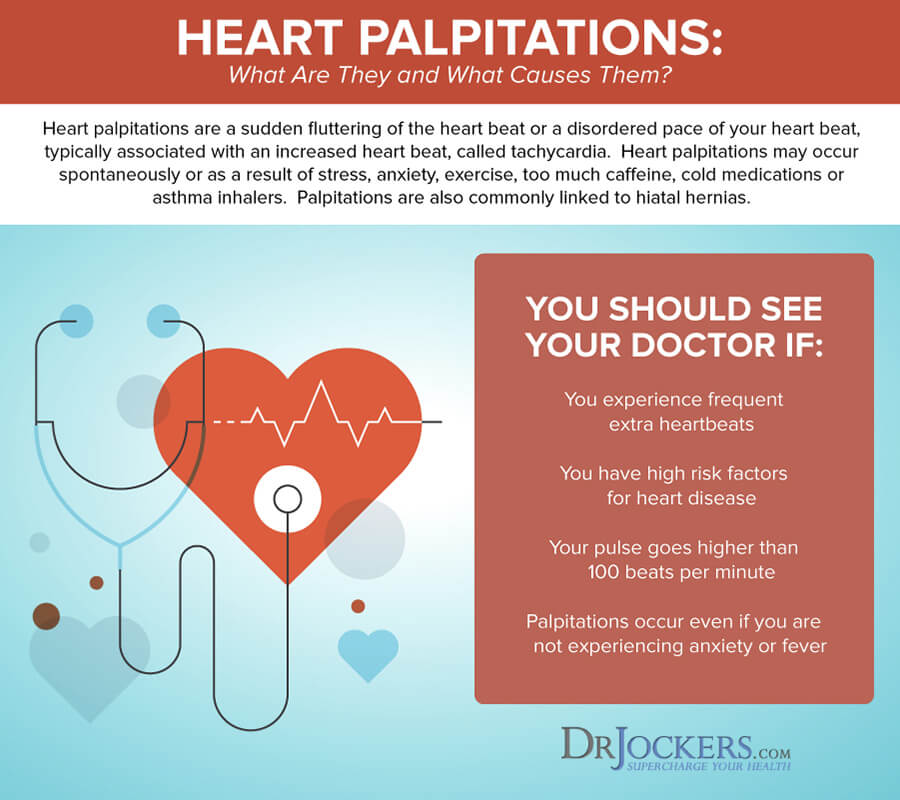
Hiatal Hernia Palpitations
Hiatal hernia palpitations are caused by the irritation of the vagus nerve. The vagus nerve is part of the parasympathetic system which lowers the heart rate causing bradyarrhythmia’s (slowing of the heart rate).
Larger hernias compress the left atrium causing ischemia (inadequate blood supply to the heart) which causes an anatomical block increasing the chance of developing atrial fibrillation. It is believed that reflux contributes to hiatal hernia palpitations but this is not clear (15).
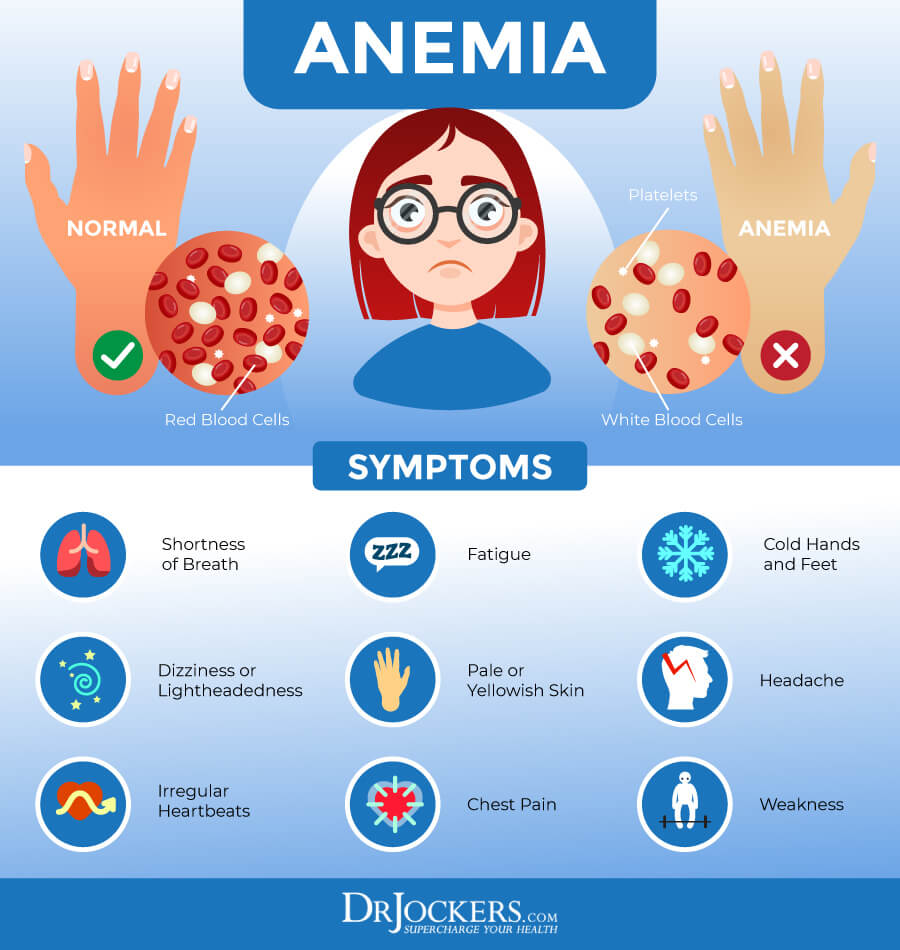
Iron Deficiency Anemia
Hiatal hernias can cause gastrointestinal bleeding which can result in vomiting and bloody stools. Excessive loss of blood all at once or a slow loss of blood over an extended period of time can lead to iron deficiency anemia.
A large hiatal hernia is a known cause of iron deficiency anemia. The presence of erosions at the neck of the hernia produce chronic blood loss. It is probably that both trauma and gastroesophageal reflux is involved (16). Iron deficiency anemia in men and postmenopausal women is largely due to chronic gastrointestinal blood loss. One of the most missed lesions while undergoing an upper endoscopy are Cameron lesions, located at the neck of a hiatal hernia (17).
Iron is a nutrient that affects many different parts of the body, including the heart. Anemia can occur when the body doesn’t have adequate red blood cells to transfer hemoglobin to various parts. Anemia can cause heart problems because low hemoglobin levels make it more difficult for the heart to pump blood and oxygen throughout the body. Anemia can cause a person’s heartbeat to become irregular because of the extra strain the heart endures to pump blood to the bodies’ tissues.
Tachycardia
Tachycardia is a condition characterized by an unusually elevated heart rate. Symptoms of chest pain, dizziness, shortness of breath, and fatigue can also occur.
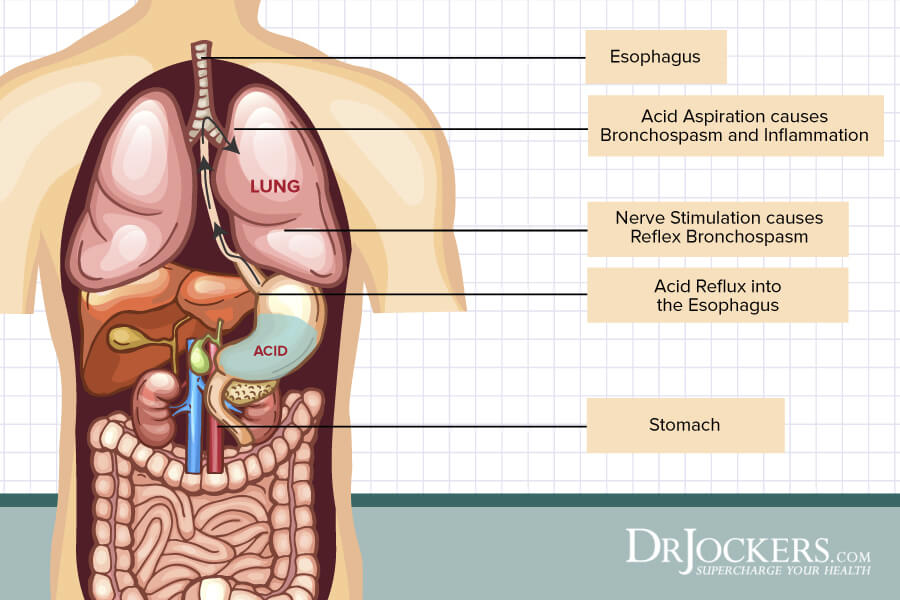
Asthma
Asthmas is a respiratory condition marked by spasms in the bronchi of the lungs causing difficulty breathing. It usually results from an allergic reaction or sensitivity.
Reflux may cause asthma symptoms in two ways. The stomach acid that leaks back into the esophagus leads to asthma symptoms. The refluxed gastric acid generates signals to the brain as it irritates the nerve endings in the esophagus. The brain responds with impulses to the lungs that stimulate the muscles and mucus production in the airways. The small airways of the lungs begin to constrict, resulting in asthma symptoms.
In many cases, physicians believe stomach acid enters the lungs directly. This is called aspiration. The foreign material irritates the airways causing sneezing, coughing, chest tightness, and other symptoms of asthma.
Some experts believe asthma can trigger GERD, this happens when asthma medications or breathing difficulties cause the esophageal sphincter muscle to relax and allow the contents of the stomach to reflux (18).
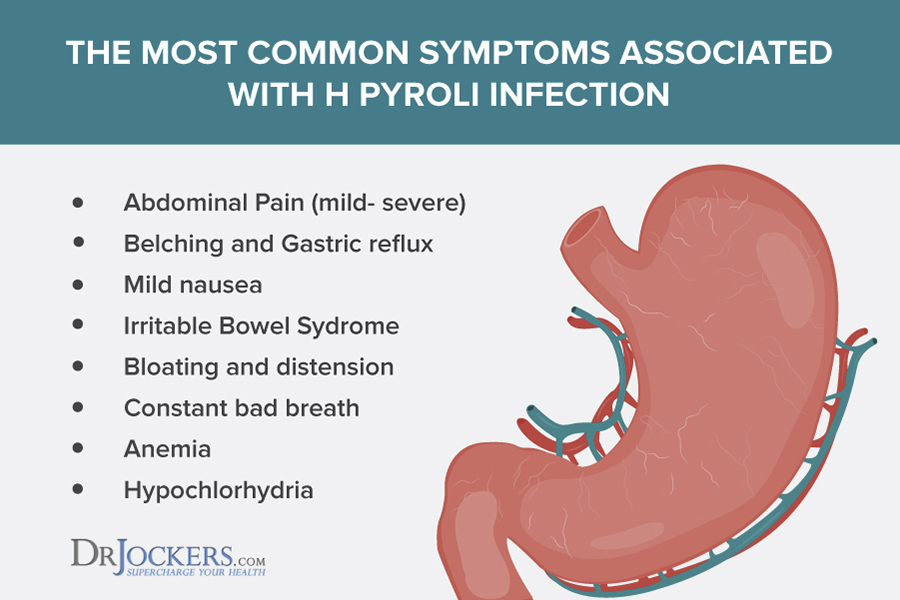
H. Pylori
Controversy still exists about the association between GERD and Helicobacter pylori infection. Significant evidence exists that suggests the potential role of Helicobacter pylori in the development of GERD (19). Pylori produces an enzyme called urease, which breaks down the urea in the stomach into carbon dioxide and ammonia. This causes bad breath and belching and it neutralizes the acidifying effects of hydrochloric acid.
An acidic environment in the stomach is necessary to digest protein and ionize minerals. In addition, this also stimulates bile release from the gallbladder to metabolize fat in the small intestine. If these key functions are not working properly we become at risk for anemia, thyroid problems, osteoporosis, and autoimmunity.
Swallowing Disorders
Swallowing involves a sequence of carefully timed events which take place without any effort or thought. Food or liquid is pushed into the back of the throat by the tongue, and contractions begin in the throat which pushes it slowly down the esophagus and into the stomach.
Once food passes through the upper throat, the vocal cords close to prevent food or drink from entering the windpipe. Normally, the sphincter or valve in the upper throat stays closed to prevent the contents of the esophagus from returning back into the mouth. The lower end of the esophagus has a similar valve that prevents stomach contents from passing back into the esophagus (20).
Natural Support Strategies for Hiatal Hernia
Along with medicines, lifestyle and dietary changes, simple home remedies can help eliminate the symptoms of a hiatal hernia. A small number of cases may require surgery.
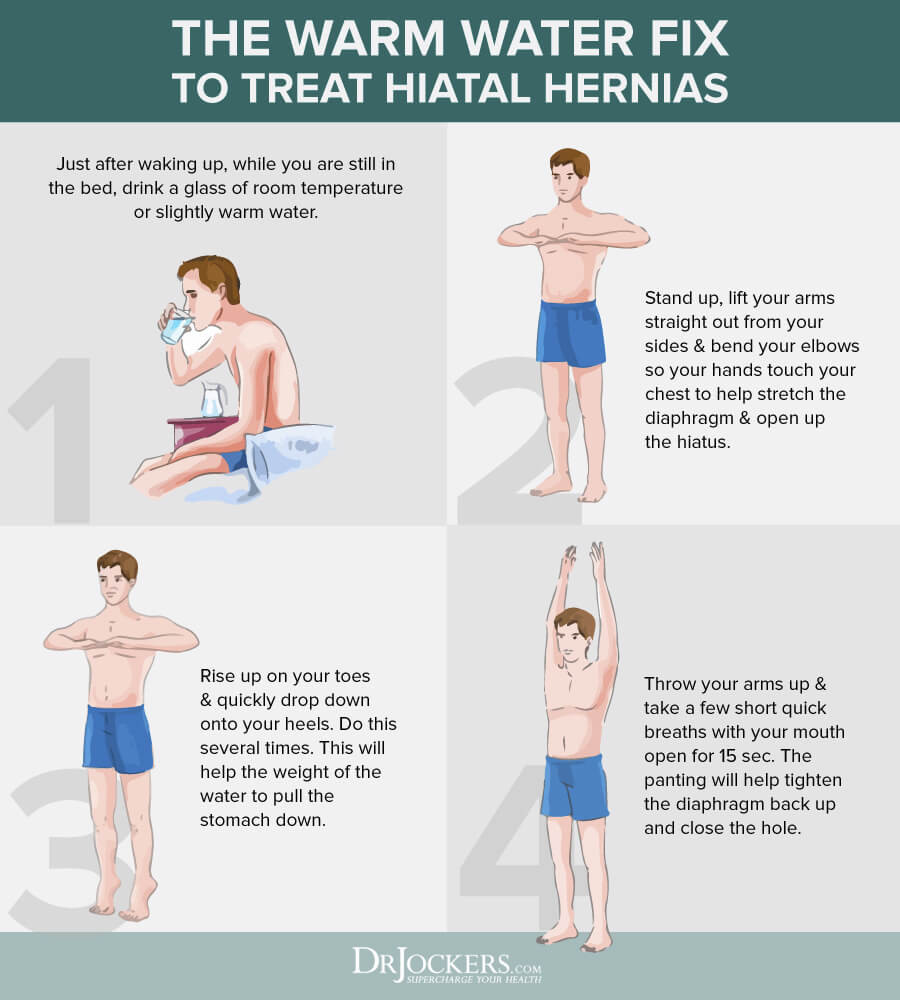
The Warm Water Fix
Drinking warm water first thing in the morning and then performing these exercises is a good way to bring down a hernia from the opening in the diaphragm. In the morning, avoid drinking coffee, tea, juice, and cold water.
- While you are still in bed, just after waking, drink a glass of slightly warm or room temperature water. This will relax the stomach muscles and the diaphragm and put some weight in the stomach.
- Stand up, while lifting your arms straight out from your sides bend your elbows, so your hands touch your chest. This opens the hiatus and stretches the diaphragm.
- Rise up on your toes as high as possible, while quickly dropping on your heels. Doing this several times in a row will allow the weight of the water to pull the stomach down.
- Standing with your arms up, take a few short, quick breaths with your mouth open for about 15 seconds. The panting will help to tighten the diaphragm back up and close the hole.
Self-Massage
Abdominal self-massage works on the uppermost portion of the abdominal cavity. It helps reduce the discomforts and symptoms of a hiatal hernia. It also helps strengthen the stomach muscles.
- Relax and lie on your back.
- Place your fingers just below the breast bones (sternum) where you can find your rib cage.
- While applying downward pressure slowly move towards your belly button.
- Repeat for 5 minutes.
Do this twice daily, once in the morning and once in the evening.
Working with a trained physiotherapist, massage therapist or a chiropractor that is trained in working with a hiatal hernia is beneficial. You may not be able to find a practitioner that is close to you or one that you can afford so this is something you can do at home.

Yoga
Yoga may ease pain and discomfort caused by a hiatal hernia. Poses like the Chair pose help to straighten the diaphragm and the stomach muscles. Avoid yoga poses that put pressure on your abdomen like the Cobra, Bow and Bridge pose.
- Begin by standing with your back straight and your arms perpendicular to the ground. Keep your feet about a hips width apart.
- Raise your arms above your head
- While bending your body forward to a 45-degree angle, bring your chest toward your thighs. Keeping your arms out straight, aligned with your back, turn your palms to face the floor.
- Gently bend your knees like you were about to sit in a chair.
- Pressing your weight toward the floor look forward. Hold this position for a few seconds, taking several deep breaths.
- While pressing your shoulder blades to your back, lower your tailbone towards the floor and pull in your abdomen. Focus on your breathing and hold this position for at least 30 seconds.
- Straighten up slowly
- Repeat this cycle a few more times

Apple Cider Vinegar
Apple cider vinegar is an excellent remedy to reduce heartburn and acidity. Although acidic in nature, apple cider vinegar produces an alkaline effect in the body.
- Add 1 to 2 teaspoons of raw, unfiltered apple cider vinegar to a glass of warm water.
- Sip it slowly before meals
- Repeat this whenever you have heartburn or acidity
Cinnamon
This popular spice helps calm and soothe the stomach. After eating a meal, it relieves abdominal pain and bloating. It can also work as a natural antacid. Don’t forget to add cinnamon to your cooking.
- To a cup of hot water add ½ a teaspoon of cinnamon
- Cover and steep for a few minutes
- Drink this tea when it is still warm, 2 to 3 times a day.
Chamomile
Chamomile is known for its natural anti-inflammatory properties. It can treat heartburn, relax the stomach muscles in the digestive tract while soothing an aching stomach.
- Mix 1 teaspoon of dried chamomile in a cup of water
- Cover and let steep for 5 minutes
- Strain and add honey
- Slowly sip a cup of chamomile tea, up to 4 times daily between meals
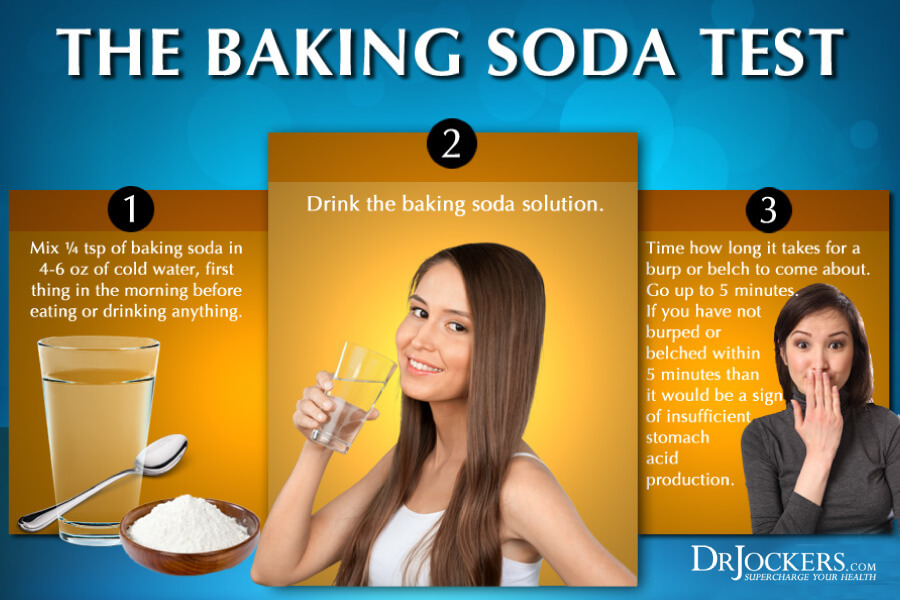
 Baking soda
Baking soda
Baking soda is a natural antacid. It provides quick relief from heartburn. Avoid using baking soda if you have high blood pressure.
- Add ½ teaspoon of baking soda in a glass of warm water.
- Drink it immediately
Repeat as needed, but do not drink this in excess. Baking soda is not a long-term solution and should absolutely not be used around meals as it will interfere with digestion. As a helpful test, baking soda can also be used to roughly determine your stomach acid levels! The instructions below detail how you can do this.
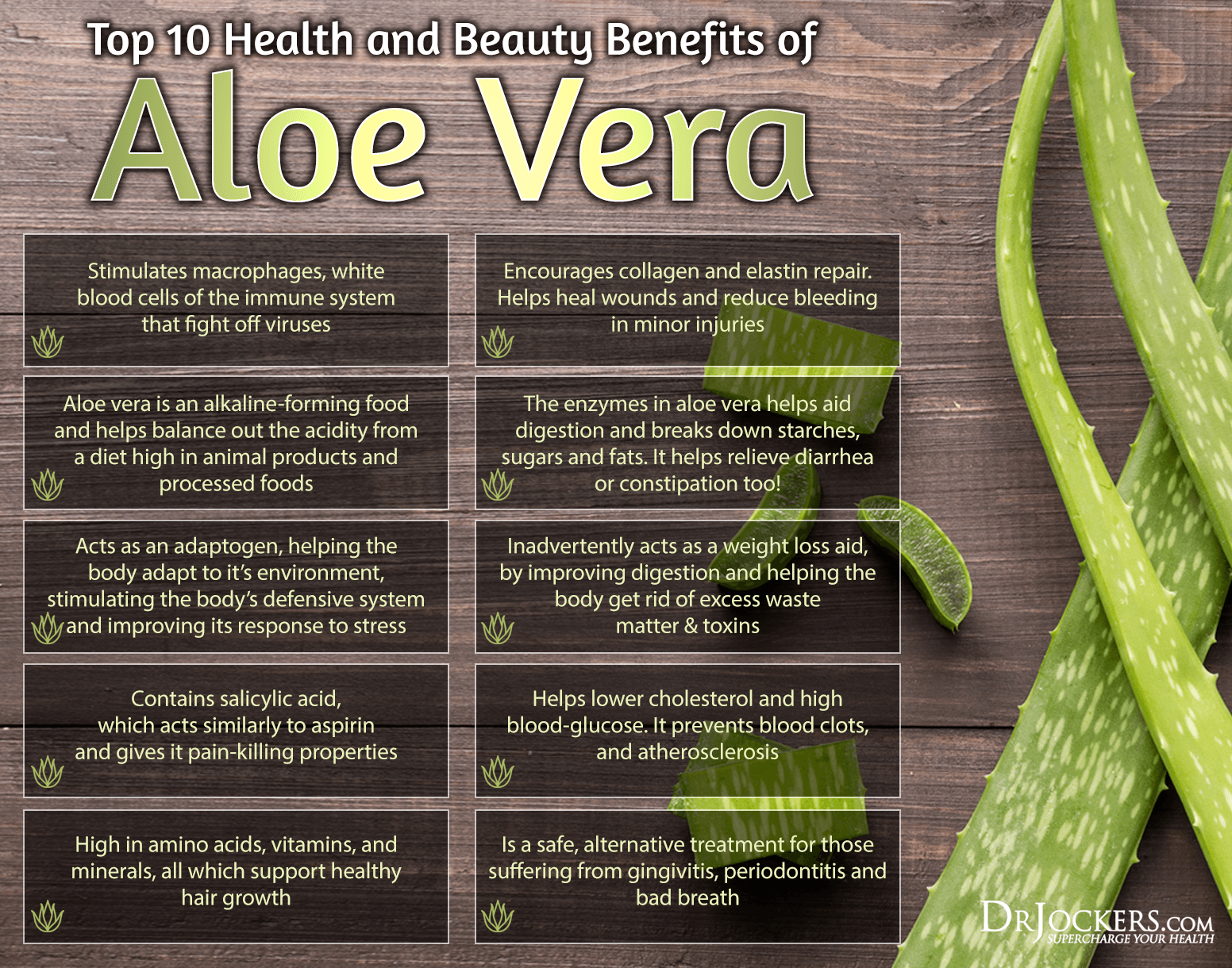
Aloe Vera
Aloe Vera soothes the inner lining of the intestines and reduces abdominal pain. It controls heartburn by reducing inflammation.
- Drink about ¼ cup Aloe Vera juice about 20 minutes before eating a meal.
- Do not use more than 2 tablespoons of Aloe Vera gel to make the juice. It may cause diarrhea.
Slippery Elm
This herb reduces stomach acidity and alleviates heartburn. Slippery elm also has a soothing, anti-inflammatory effect on the body.
- In 1 cup of hot water add 1 tablespoon of Slippery Elm Bark.
- Let it steep for about 10 minutes,
- Drink it twice a day, especially after eating your meals.
Change Your Diet
It is important to keep a close eye on your diet, when you are suffering from the symptoms of a hiatal hernia. Avoid foods that trigger or worsen your symptoms, and lose weight, this will reduce the pressure on your stomach.
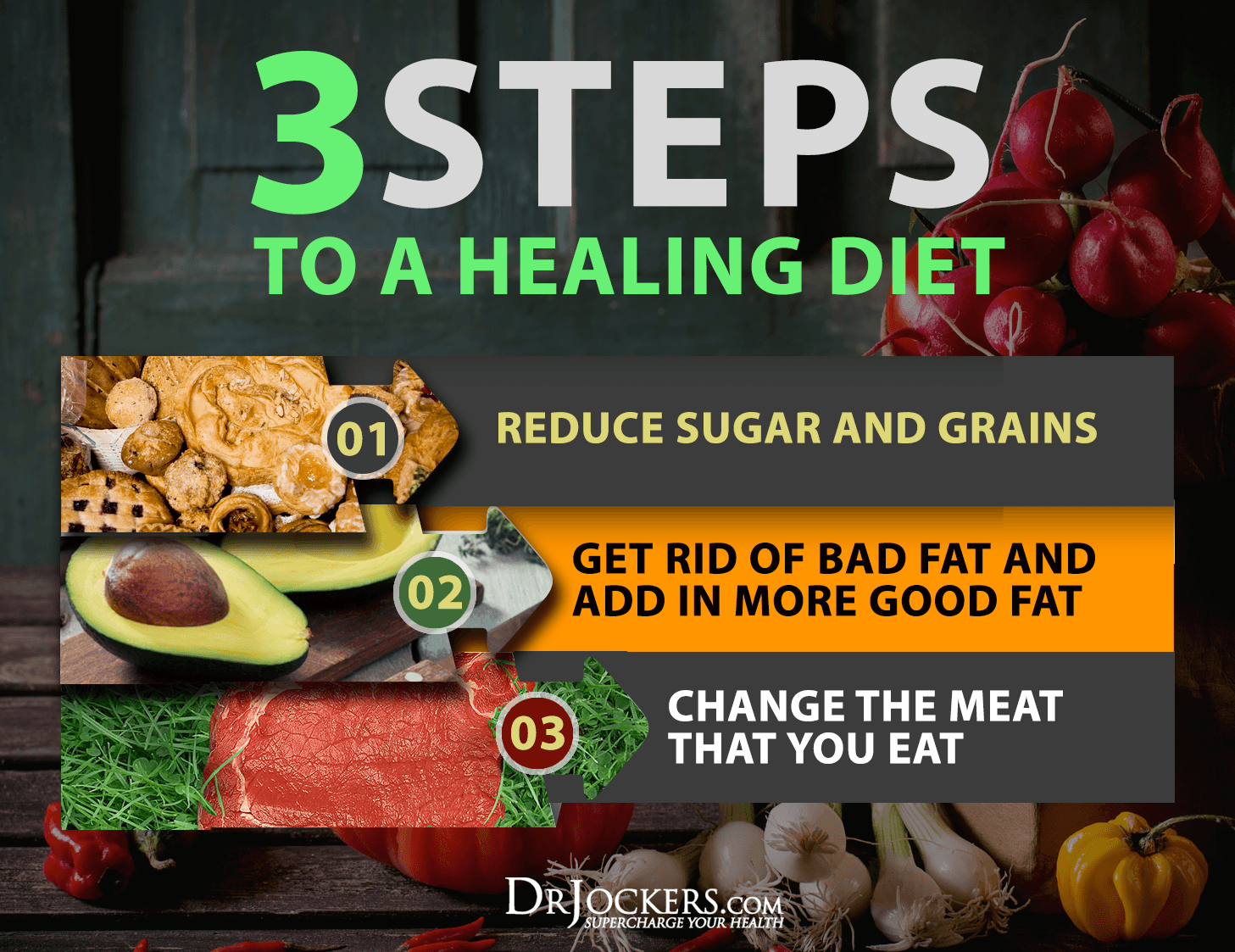
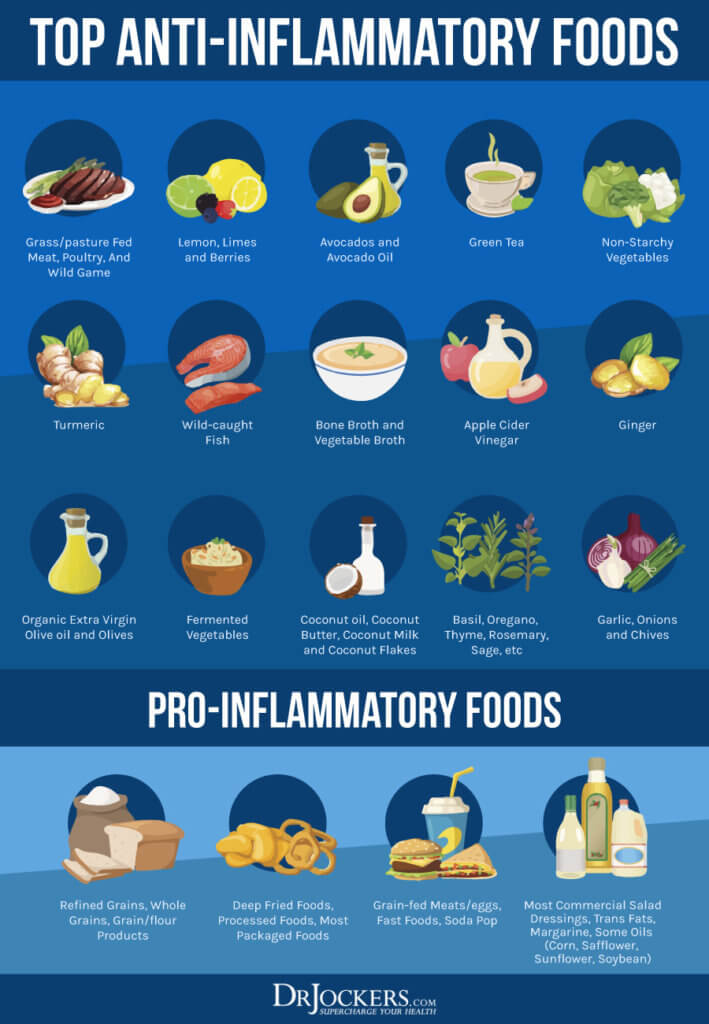
Foods to Eat
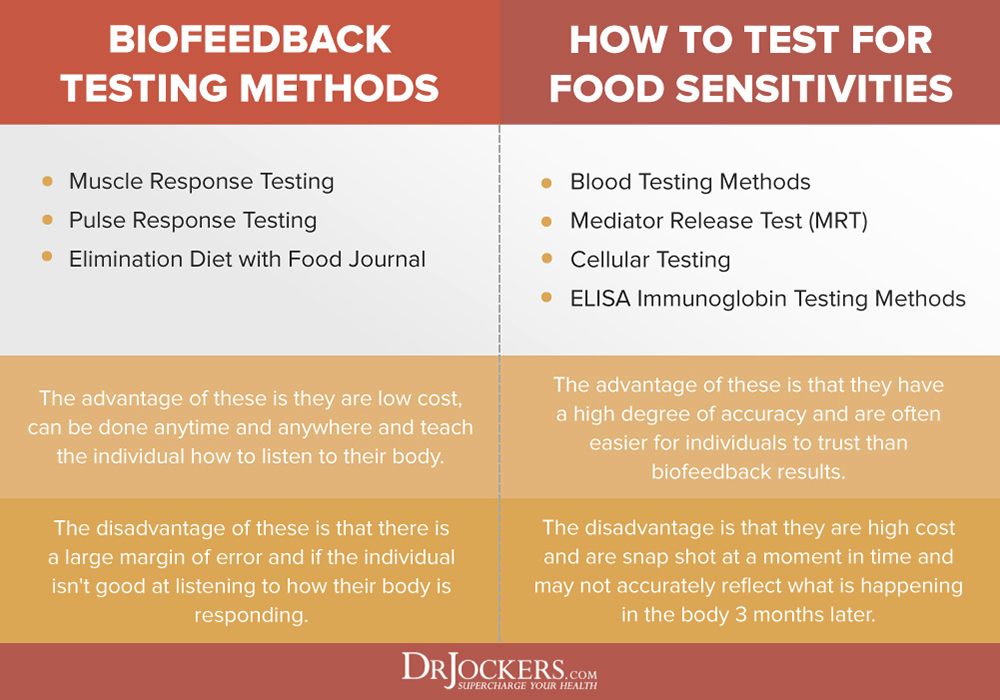
The best choices for people with hiatal hernias are non-acidic, minimally processed foods that contain dietary fiber. Exceptions would be made for people with food intolerances. Many times an elimination diet is necessary.
Elimination diets remain the gold standard for confirming food sensitivities and figuring out your unique sensitivity to particular foods. By removing problematic foods, at least for a period of time, and then reintroducing certain foods, you can identify your trigger foods and which foods your body can handle. Maintaining a food diary will be a benefit in helping you to avoid symptoms.
Safe Foods to Eat Include
- Leafy greens
- Beans and peas
- Lean proteins, including beef, fish and chicken
- Non-citrus fruits and juices
- Nuts and seeds
- Cinnamon
- Ginger
- Artichoke and asparagus
- Grass-fed butter
- Cardamom
- Coriander
- Apple cider vinegar
- Non-caffeinated teas, especially ginger, dandelion and green teas
- Healthy fats like coconut, avocado, and olive oils
- Bone broth
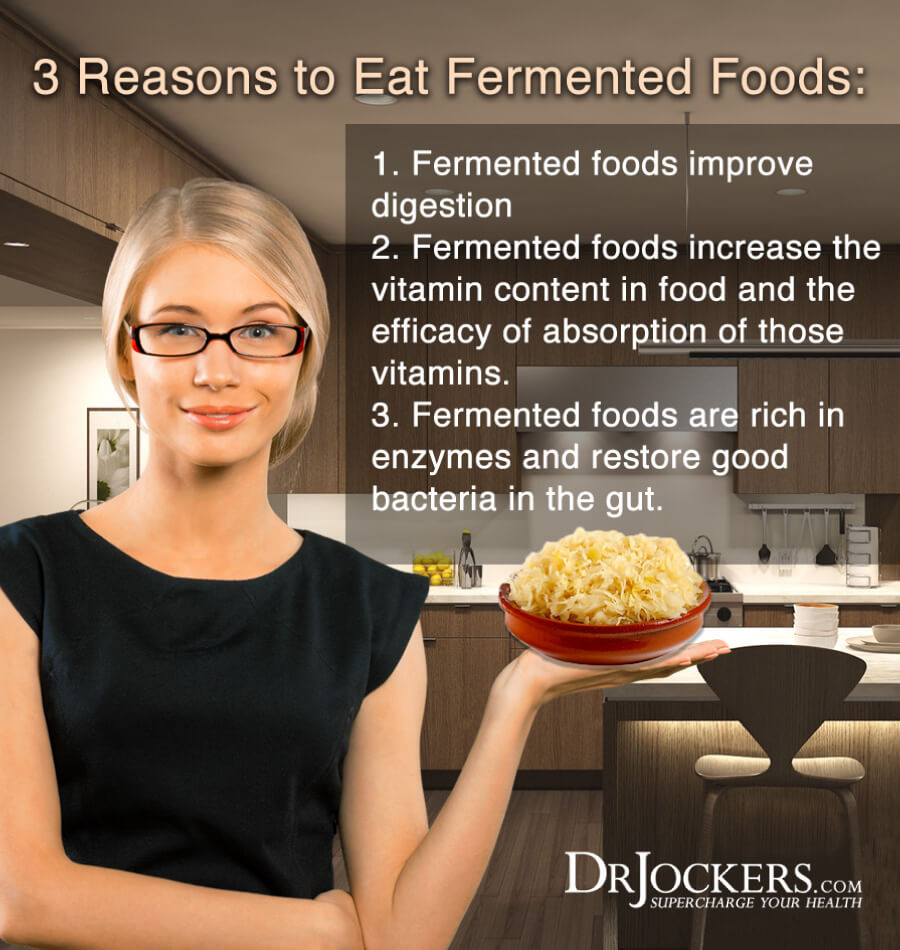
Fermented or cultured foods that are rich in probiotics (acid-reducing stomach bacteria) may also reduce hiatal hernia symptoms.
Popular Fermented Foods Include
- Unsweetened yogurt
- Pickles
- Kimchi
- Kefir
- Quark
- Sauerkraut
- Kombucha
- Cheese
- Miso
- Tempeh
- Buttermilk
- Natto
Consuming sugary products alongside probiotics isn’t helpful. Sugar allows the growth of stomach microbes that destroy and consume probiotics.
Foods to Avoid
Avoiding foods that are acidic, rich, oily and full of preservatives may help to prevent heartburn, gas, indigestion, bloating and regurgitation.
- Fatty foods
- Caffeine
- Fried or oily foods
- Cocoa and chocolate
- Alcohol
- Tomatoes and tomato sauces
- Candies
- Most types of mint
- Soft drinks and carbonated beverages
- Sweetened juices or teas
- Garlic, green onions, shallots, onions, leeks, and chives
- High amounts of cooking oils
- High- fat dairy products
- Salty foods
- Cereals and breads
- Deli meats
- Fast foods
Stress Reduction
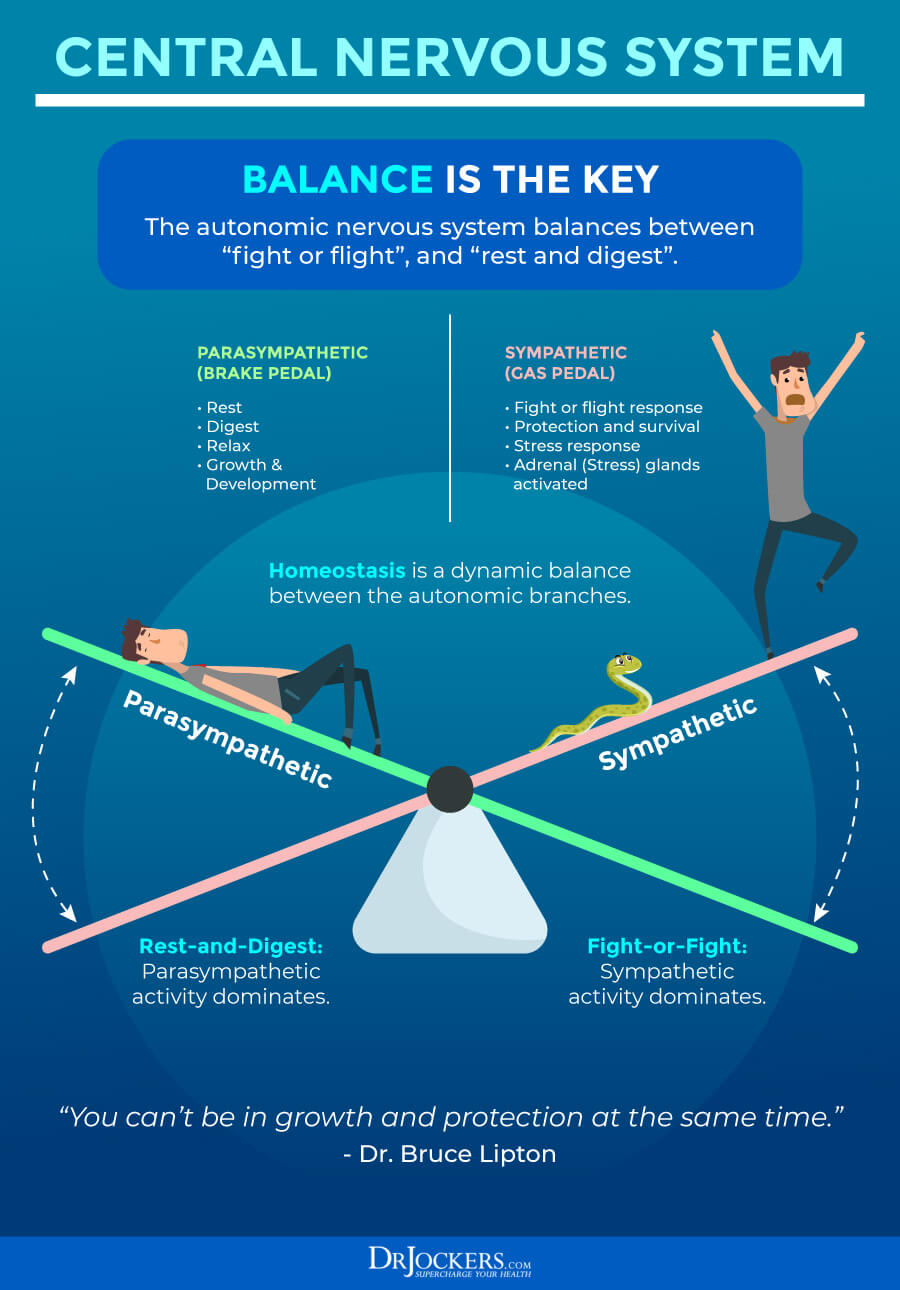
While stress doesn’t cause acid reflux, there is increasing evidence showing that stress can impact the way our bodies react to reflux symptoms (21). Emotional stress produces hundreds of changes in your body. If stress occurs too often or stays too long, those changes can push body systems beyond normal range and cause dysfunction. Chronic stress exhausts the body and decreases immune functions making you more vulnerable to many illnesses.
Relax, you deserve it. Meditating or praying a few minutes a day can ease anxiety as well as deep, focused breathing. Mentally tune into your body to see how stress is affecting you. A good belly laugh not only lightens your load it lowers your cortisol (stress hormones) and increases your endorphins (feel-good chemical) so laugh out loud, and dance to your favorite music. All forms of exercise including walking and yoga ease anxiety.
Digestive Enzyme Supplements
Digestive enzyme supplements are extremely helpful and often necessary for certain individuals for a short period of time. I personally use digestive enzymes whenever I am going to have a big meal. I notice better digestion, more energy, less digestive stress, and gas when I use enzymes.
Clinically, I find that people feel much better digestion and energy when they use enzymes along with an HCL support product. My favorite all-purpose digestive enzyme is Super DZyme.

Improve Your Stomach Acid
These are my tips to help improve your digestion if you have lower stomach acid levels. Following these strategies, you will reduce stress on your digestive system and absorb nutrients more effectively.
This will provide the resources your body needs to produce adequate stomach acid in the future. When you improve your stomach acid levels, it makes a huge difference in your overall quality of life.
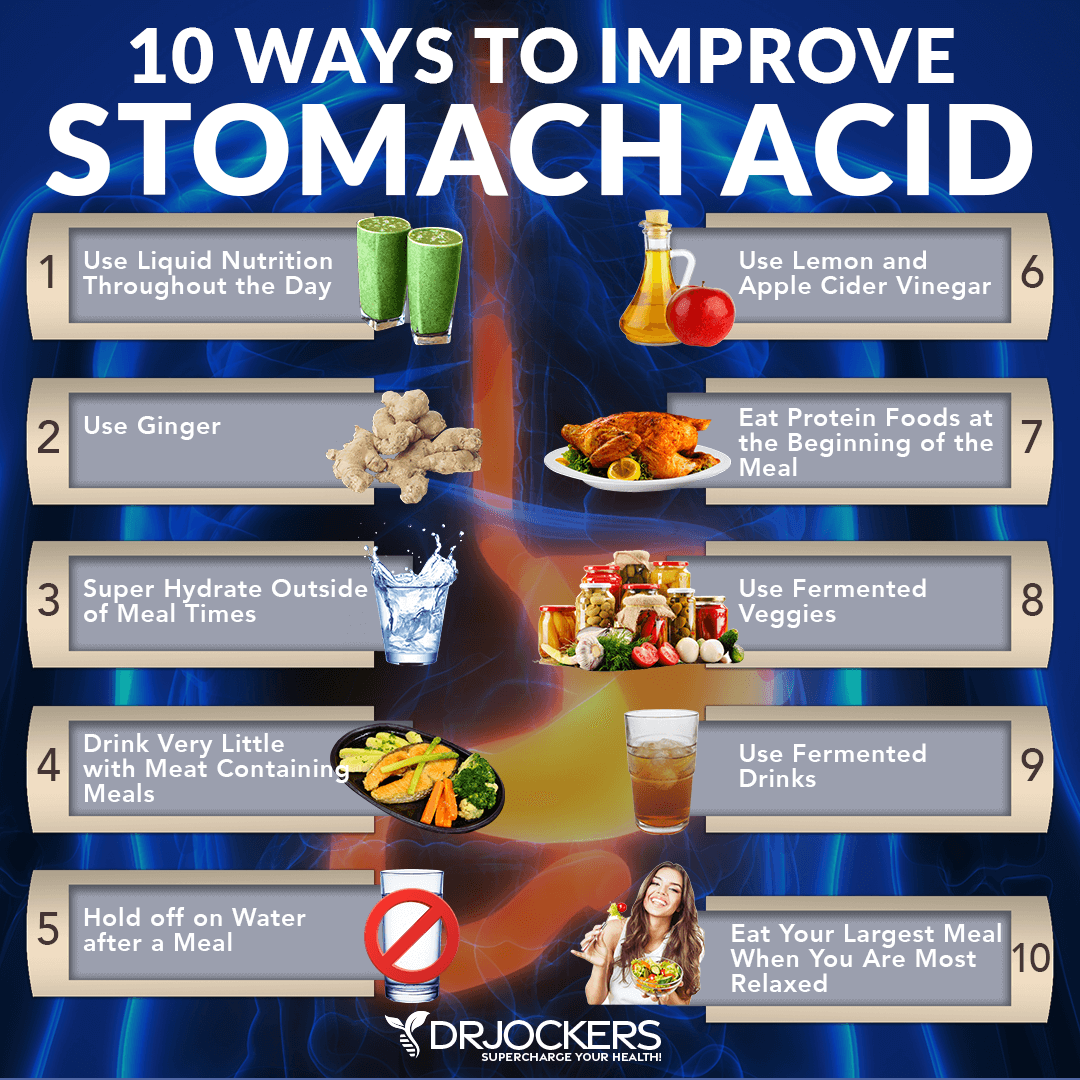
Use Liquid Nutrition Throughout the Day
You should make at least half of your meals in a liquid form such as a protein shake or a green smoothie. Making shakes that include the gut-healing compounds below is a great strategy. Gut Healing Protein and Bone broth are two great options.
Use Ginger
Ginger is one of the best things for improving digestive juices. Fresh ginger juice, ginger powder, and teas are all great options.
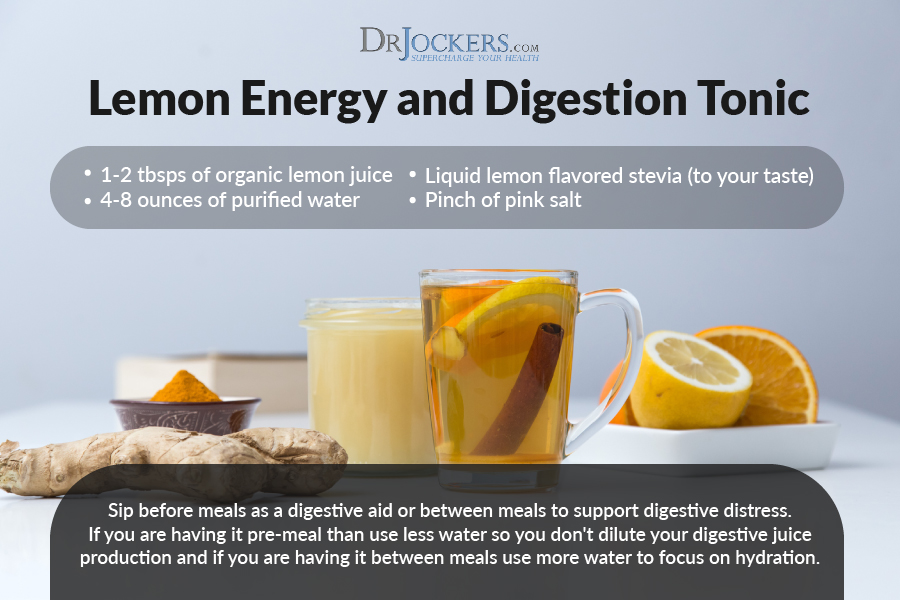
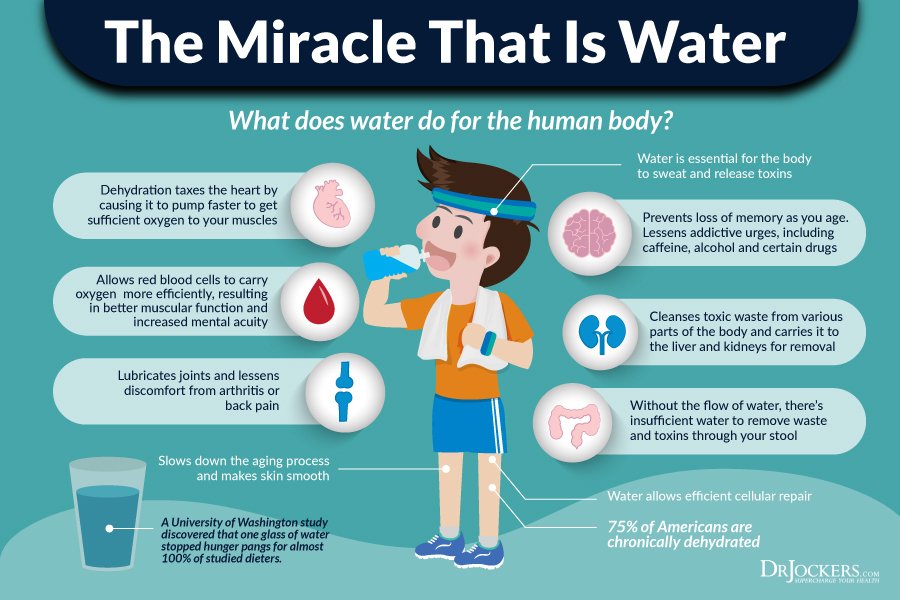
Super Hydrate Outside of Meal Times
I am a huge advocate of optimal hydration and it is especially important if you have low stomach acid. Also, keeping hydration periods separate from meals will help ensure you are not diluting digestive juices and inhibiting digestion. A good guideline to follow would be to cut off drinking an hour before and after meals.
 Use Lemon and Apple Cider Vinegar
Use Lemon and Apple Cider Vinegar
Squeezing fresh lemon or using lemon juice or apple cider vinegar on your meat and vegetables helps to pre-metabolize them. Check out these articles for great ways to use lemon and apple cider vinegar: 5 ways to use lemon here and 4 ways to use apple cider vinegar here and
 Eat Protein Foods at the Beginning of the Meal
Eat Protein Foods at the Beginning of the Meal
Dense proteins like meat require adequate stomach acid production to break down fully. In addition to not drinking around meals, consuming dense proteins first helps to ensure they are saturated in stomach acid.
Use Fermented Vegetables
Fermented foods such as sauerkraut, kimchi, pickles, and ginger all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions.
Use Fermented Drinks
Fermented drinks such as ACV, coconut water kefir and lemon water (not fermented) contain organic acids that have an antimicrobial effect. They also improve the microbiome and assist with stomach acid and enzyme production for optimal digestion.
Eat When Relaxed
In order to produce adequate stomach acid, your body needs to activate the parasympathetic nervous system. If you are on the go or stressed, you should fast or stick with liquid nutrition as mentioned above. Typically, dinner-time would be the best time to have a bigger meal that requires thorough digestion.

Using Gut Repair Supplements
L-Glutamine
- L-Glutamine is an amino acid that is foundational to the proper function of the digestive and the immune system. It is a primary fuel, not only for a healthy gut membrane but it also helps to regrow and repair the intestinal lining (22). Glutamine also helps water absorption in the gut, allowing for easier hydration of the whole body. I believe this is a necessary component for good health.
- Supplementing with L-Glutamine strengthens the junctions in the gut and is necessary for healing and sealing leaky gut. It also helps to ensure the right microorganism balance to produce a healthy gut flora (23).

Aloe Vera
- Aloe Vera contains polysaccharides that help to balance and modulate the immune system. Polysaccharides reduce inflammation throughout the body and in the gut. Aloe is also an adaptogen, meaning it helps the body adapt more effectively to stress. This helps to stimulate bowel movements in times of constipation and helps to form solid bowel movements in times of diarrhea (24).
- Aloe Vera has been found to have a positive influence on the microbial balance in our intestines. I would consider Aloe to be one of the best things to use on a regular basis to promote healthy gut flora. In addition, Aloe has compounds that help the body to remove intestinal worms and other parasites (25).
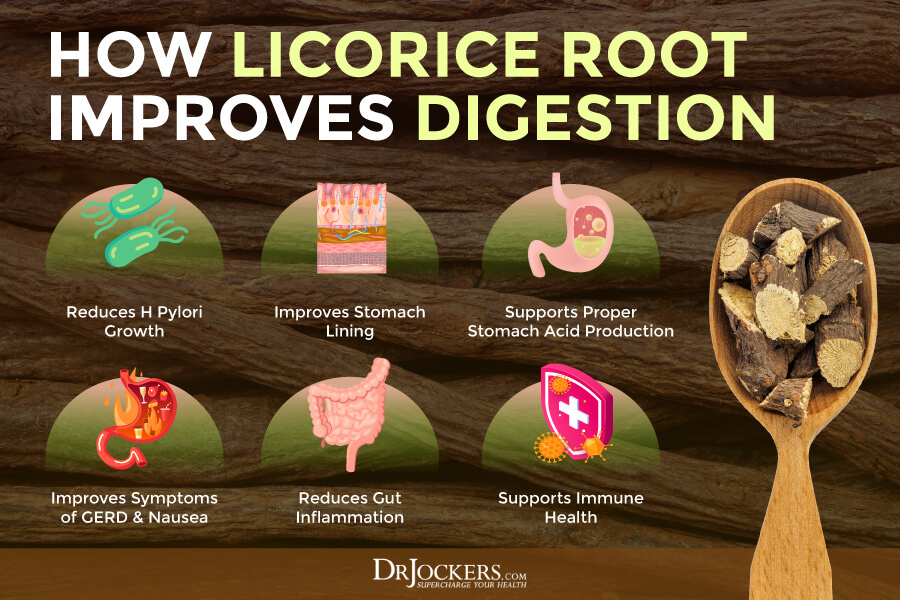
Deglycyrrhizinated Licorice Extract (DGL)
In various cultures throughout the world, licorice has been used to help with indigestion and ulcers. Licorice helps to encourage the release of secretin which enhances the stomach’s mucous lining. The demulcent properties soothe and relieve irritated mucosal membranes (26). Licorice is praised for its use with stomach ulcers because it helps protect and heal the gastric lining.
It is also a strong defense against the H Pylori bacteria that is correlated with stomach ulcers and a number of other digestive issues (27). DGL is made from licorice and the Glycyrrhizin is removed. Glycyrrhizin inhibits the metabolisms of cortisol and it can cause an elevation in blood pressure. DGL is supportive of the body’s healing process in the stomach and the small intestines.
Gut Repair
I have formulated a product that takes the guesswork out of the quantity and quality of the product you are taking for optional gut health. Gut Repair features four specialized ingredients for enhanced gastrointestinal support. This unique formula contains concentrated extract of licorice that has been processed to remove glycyrrhizin, reducing the risk of side effects connected with licorice. Glutamine serves as the predominant fuel and nitrogen source for the mucosal lining of the gastrointestinal tract (28).
Arabinogalactan from the North American larch tree is a naturally occurring polysaccharide that provides excellent support for GI health. Research suggests it plays a role in the promotion of gut microflora and may increase beneficial short-chain fatty acid production (29). The Aloe Vera leaf extract in Gut Repair has been processed to remove bitter principles and prevent a laxative effect.


This is a very informative and helpful article. Thank you!
I was diagnosed with a hiatal hernia last year (I am 28) with a Barium swallow test and I was put on a PPI to manage my symptoms (severe acid reflux). I was able to get that under control and discontinue the PPI use. I’ve had other flare ups and have used the PPI for short bursts (5-7 days) to good effect. This last time my Dr recommended that I stay on the PPI for 6 weeks after a flare up to totally cool it down. So even though I was symptom free, I tried the PPI for 6 weeks. It’s been 10 weeks now and I’ve been struggling on and off with reflux the whole time. These last two weeks have been especially uncomfortable. Do you think the PPI is actually causing my problem or is it the hernia?
Sorry to hear that! I would work on your diet and reducing the hiatal hernia and come off of the PPIs as they are going to cause a lot of problems long term.
Hello: Glad that I have read this, answered so many questions for me. As a health professional there is still so much to learn. Five years ago I had a gastric sleeve due to weight and health issues – glad I did. Have lost over 60 kgs, and still trying to lose more.
Main issue now is that few years ago I was passing out, blood pressure jumped, HR high (normally low as I am bradycardic) was taken to hospital twice. They thought it was cardiac, and not the case. Ended up seeing my bariatric surgeon again for review, he did endoscopy and discovered hiatus hernia. I am constantly watching diet; exercise and trying to stay as healthy as I can. I walk, ride horses, gym doing as much as I can – am almost 63. Work has been very stressful and I see that as a trigger, am about to start working one day less per fortnight – transition to retirement.
My biggest issues now are: reflux (take nexium twice day); hot flushes; dizziness at times; feelings of asthma type symptoms at times (can be when stressed and at home) and trying to lose more weight (want to drop another 10kg at least)
What are your suggestions/thoughts please?
Sorry to hear this! I would be sure to follow all the suggestions in this article. Blessings!
I would consult with a classical homeopath as soon as possible. I know they can help with menopause, weight loss and some digestion issues, not sure about hiatus hernia. They usually give a 15-20 free consultation. I did my free consult with my homeopath, Jason by phone then went to his office to meet him, then booked my appointment. I found my homeopath in Burlington, Ontario from research I did on the internet. He is fabulous, practicing homeopathy for 18 years and reasonably priced.
Don’t be fooled by someone with 20 to 30 reviews. Many could be relatives and not necessarily
honest. My homeopath had about 5 reviews, but the moment I spoke with him by phone, I knew I could work with him. He has helped me with menopause, fatigue plus stomach issues (h. pylori) and treats other things that come up along the way. He resolved my anxiety issue during my second visit. Had this all my life and no one ever helped me with it until now.
I had 2 homeopaths recently before I found this one. He is brilliant and honest and even consults with you by phone, no charge. It is about a 40 minute drive from west Toronto to his office and I wouldn’t go anywhere else. Wishing you perfect health.
I’m dealing with acid reflux and take Dexilant. I want to know this….”how will I know when it is time to stop taking the Dexilant?” I would hate to assume that I don’t need it and then one day I have chest pains and think I’m having a heart attack and ……… can I stop taking the PPI and take an over the counter acid reducer?
By the way, great website! Very informative!
So sorry to hear this! I would be sure to follow the specific instructions I laid out in this article. Blessings!
I had a CT scan this week showing two thirds of my stomach as hiatal hernia. Will the massage exercises still benefit.? Or will I inadvertently cause more damage? I’ve had a persistent cough for years, hoping to get that under control. Cc
Yes these exercises will really help!
Good Day,
First of all thank you for this very interesting article. I was diagnosed last year December with a stomach hernia the Doctor told me the hernia can not be removed due to the fact its to big. My question is that can this hernia really not be removed cause its causing weight loss and lost of appetite.
Please Advise
Thank You
God Bless
Sorry to hear this! I would be sure to follow the suggestions in the article. Blessings!
Hi Dr. Jockers!
I have a question about the “Warm Water” to fix hernies? How many times each day can I do this exercise?
Thank you forward
Best wisches
Igor
Hey Igor, I recommend doing this several times in a row upon waking in the morning!
Dear Dr. Jockers,
Thanks a lot for this article.
Referring to your recommendations on how to improve stomach acid. It is not clear to me why you suggest having liquid nutrition but at the same time you say to avoid drinking water during meals. Obviously the liquid meals are mostly water based; as you wrote water can dilute digestive juices and inhibit digestion especially if they are protein shakes. Could you please explain?
Already thanks for your reply,
Daniele Sindaco
Hey Daniele, Liquid nutrition in the form of a protein shake gently stimulates digestive processes. The blender breaks down the components of the shake into very small particles and the digestive system doesn’t have to work hard to absorb the nutrients. When water is consumed with meals the digestive system has to work harder and requires digestive juices to break down the components.
Dear Dr Jockers.My email address Margaret.mcdonagh6@upcmail.ie.i had surgery nine months ago for a large hernia repair .Would you recommend physiotherapy
Hey Margaret, I’m sorry to hear this! Physiotherapists are trained to work with hiatal hernias. I would recommending consulting with one to learn if this type of therapy is best for your situation and health journey.
whish to talk abot products
610 247 8905
Hey Barry, Please feel free to reach out to our sales team who will be happy to help!
I don’t want to try the exercise that has you raising up high and then coming down hard on your heels. Supination makes the rise difficult and concerned that coming down on heels could be harmful because I have osteoporosis. Any other suggestions, in addition to the massage? Thank you.
Hey Maureen, For osteoporosis, you could try bouncing on a mini-trampoline and have one hand on the side of a wall to make sure you do not fall.
Hi Dr. Jockers, I just want to say how impressed I am with all your information and research on this subject of Hiatus Hernia, which I was diagnosed with a couple of days ago from an endoscopy, from severe pain all the time under my ribs in my stomach. By far the best website on the subject!
However, one question I cannot find anywhere and my endoscopy doctor could not answer it while in the hospital. So I am hoping you can bring some light to the situation, and if you have ever heard this before?
The last 4 months I wake up every morning and every time I eat after about a half an hour, I end up with red blotches across the top of my lips, where it feels like acid has eaten away at my skin with a burning feeling, coupled with wet saliva lips. I have been eating about 95% of what you talked about, just for digestion purposes, anyways. Do you think this is part of the symptoms of the hiatus hernia, backing up? I just would like to understand why it is happening, after learning everything on your site, I never saw this symptom. It is so embarrassing too.
Thank you ever so much if you have time to reply to my query.
All the best for the weekend ahead.
Sorry to hear that Kim, that is typically associated with a histamine or inflammatory condition and is most likely related to a food sensitivity you may have. Here are some helpful articles https://drjockers.com/7-ways-reduce-food-sensitivities/
https://drjockers.com/suffering-histamine-intolerance/
After experiencing abdominal pain for several months, I was recently diagnosed with a 7 centimeter hiatal hernia after completing a barium x-ray. My primary care physician put me on Famotidine twice a day and and a gastrologist has me on Carafate 4 times a day. They want me to do this for 2 weeks and “see what happens”. I am frightened to ingest all of these chemicals into my body. Can you please tell me what you think would be a better approach? I eat a very clean diet of mainly fruits and vegetables with only small amounts of lean meat, such as chicken and turkey.
Thank you.
Very sorry to hear this Cindy! I would be sure to follow the recommendations in the article!!
I have a sliding 2mm hiatus hernia just found out with camera.pain in tummy but no heart burn feel very ill stop ppi as I had the camera but hate drugs .how do I get your tablets .and I can’t eat much at moment but celery’s and apple are ok .just hurt after food .
Sorry to hear that! Be sure to do the exercises in this article.
Doc,
Can I do the hiatal hernia exercises even if I’m not sure that I have one? I have burning in my stomach and my nutritionist says it’s probably a hiatal hernia. Constant belching after eating and drinking.
Yes you can do them, they won’t cause harm.
I saw my kinesiologist yesterday and she tested me for a hiatal hernia and then adjusted it. Since then I have had terrible GI symptoms and it feels like it’s difficult to breathe. Bad acid reflux, mild nausea after eating, and it feels like my stomach is one big rock, especially where the adjustment was. Burning pains on and off where the adjustment was. Scratchy throat due to acid I’m guessing. Have to take a break while chewing and take a big gulp of air because my stomach feels like a rock.
I can’t get a hold of the kinesiologist until Monday…any suggestions on what to do? Should I just let it be or try to adjust it further?
When she did the adjustment, I felt no pain at all, and it took literally 10 seconds…
Great to hear that! I would recommend doing the exercises in this article.
Not sure if you read what I was saying correctly…all these terrible GI symptoms started AFTER she did the hiatal adjustment on Friday…any suggestions?
Not sure if you read what I was saying correctly…all these terrible GI symptoms started AFTER she did the hiatal adjustment on Friday…any suggestions? Would it be hepful to do the self exercises some more?
Yes and I would follow up with your practitioner about it as well.
I followed up with my practitioner and she said since I had such an unusual reaction to the adjustment, I need to see a GI doctor before she will treat me again…if I schedule a consultation with Danielle (your coach) would she be able to consult me on the hiatal hernia exercises?
I would recommend seeing a GI Doctor to rule out certain red flags.
Dr. Jockers
It’s my pleasure to read all your patience and explanations in detail for the digestive system works.
your explanations 100% correct.
I just share my experience for the above friend’s queries on how to reducing the hernia or how to healing hernia.
1. we don’t drink water before and after a meal.
the region behind our stomach keeps on releasing a few acids.
whatever we eat food those breakdowns small particles in 1and half-hour.
2. If we drink water with food the acids mix and food reflect acid burs highly.
3. when you drink water min 500ml each time if possible warm water.
warm water can kill bacterias in the stomach system.
warm water can clear fat cells, kill anti reflex.
4. Dr. Jocker suggested healing the hernia exeresis. It may be 60 to 70% of people can heal. but few people may not heal but 100% I’m assurance this anti-reflux problem will resolve. if you follow all the time above trips.
Thanks
veeru
Thanks for sharing!
Dr J.
Would I take Betaine HCL and/or enzymes with a protein shake or only for solid proteins?
Only solid proteins!
Great article, clearly lots of work has been put into this! Thank you
Thank you!
Hi,
I had a CT scan this week and report is showing “small sliding hiatus hernia”.
I am getting chest pain and burning issue and after taking medicine it is improving.
Can I reverse this “small sliding hiatus hernia” without surgery?
Thanks,
Parhi
Sorry to hear this! I would recommend the strategies in this article to help you!
Hi, Dr. Jockers,
Thank you for this information.
I have one question:
Can some people heal paraesophageal hiatal hernias without surgery, or does this type always require surgery?
Thank you!
Amy
This is a great question and it may occasionally require surgery but you can keep it under control with the suggestions in this article.